Abstract
Objective
To determine whether the variation in prices paid for cardiac medical devices was associated with management practices in cardiac units.
Study setting
Cardiac units in US hospitals.
Study design
We regressed unit prices on management practice scores and other hospital characteristics, with and without controls for device fixed effects, for the 11 top‐spending cardiac device categories.
Data collection
A trusted third party that had entered into a confidentiality agreement combined de‐identified medical device price data for N = 213 US hospitals from ECRI's Supply Guide benchmarking service, with survey responses regarding management practices in those hospitals' cardiac units; the resulting merged data were made available to researchers for analysis with hospital identifiers removed. N = 1980 hospitals with interventional cardiac catheterization laboratories and at least 25 annual acute myocardial infarction discharges in 2010 were eligible for inclusion; N = 648 responded to the management practices survey; N = 213 subscribed to Supply Guide and purchased at least one of 11 top cardiac medical device categories.
Principal findings
Cardiac units with better management practices paid lower prices for cardiac devices (percent decrease in price for one standard deviation increase in management score = 1.33%, 95% confidence interval 0.99–1.67). This was comparable in magnitude to the price decrease associated with a one standard deviation increase in patient volume.
Conclusions
Better management practices were associated with lower device prices. This relationship is robust, but modest in magnitude. This modest magnitude is similar, though, to other events expected to lower input prices, such as transparency in the form of benchmarking information and hospital mergers.
Keywords: healthcare costs, hospitals, management practices, medical devices
What is known on this topic
Management practices that have been successful in the manufacturing and technology sectors have been associated with improved quality, lower mortality, and greater market share within hospitals.
Hospital supplies and devices account for a large share of hospital operating costs, and there is wide variability in the prices that hospitals pay for these devices.
Relatively little is known about the extent to which hospital management skill may be associated with the prices that hospitals pay for devices.
What this study adds
This study finds that hospitals with better management practices paid lower prices for medical devices.
The magnitude of the association was modest (e.g., a one standard deviation change in management score was associated with average savings of $61,000 per year) but robust across multiple specifications.
Well‐managed hospitals may be able to control or reduce their internal costs more effectively than poorly managed hospitals. Management‐driven efforts to reduce expenditures may serve as one part of a larger effort to control costs.
1. INTRODUCTION
Hospitals vary widely in the prices they pay for the exact same medical devices. 1 Despite the fact that hospitals often rely on group purchasing organizations (GPOs), third‐party logistics service providers, and consolidated service centers to achieve scale economies and reduce complexity, hospital supply chains are typically characterized as fragmented and inefficient. 2 , 3 This matters for hospitals' bottom lines because hospital supplies and devices account for 23% of hospital operating costs. 4 In the long run, these costs are passed on to patients through their relationship to negotiated prices with private payers and the updating process for payments from the Centers for Medicare and Medicaid Services. 5 For example, hospital supplies and devices accounted for a quarter of the growth in inpatient hospital spending between 2001 and 2006. 6
Better management practices and managerial skill have been found to be associated with better quality outcomes in cardiac units 7 and hospitals in general. 8 They have also been associated with better procurement outcomes 9 and higher overall productivity 10 in settings outside of health care. Some of the deficiencies in hospital purchasing—such as insufficient quantification of costs, inability to standardize products, and diverging priorities of hospitals and decision‐making clinicians—could theoretically be addressed by improved management practices. 3 , 11 If better management practices are associated with lower prices for the exact same hospital inputs, that would offer one promising avenue for reducing healthcare costs without sacrificing quality. Prior research suggests that hospital management practices can be improved through access to medically focused managerial training. 12
The goal of this study was to measure the relationship between management practices and the prices paid for major cardiac device categories. To accomplish this, we used rich survey data that assessed and scored management practices in a large set of cardiac units and linked those data to a unique dataset of medical device purchase orders.
2. METHODS
2.1. Sample selection
We used de‐identified purchase order data from a sample of US hospitals that subscribed to the ECRI Supply Guide service 2010–2015 and participated in a survey of cardiac unit management practices in 2010. The purchase order data groups devices into categories using ECRI's Universal Medical Device Nomenclature System (UMDNS) codes. The UMDNS system is an international taxonomy system for medical devices. For this study, we identified the top 50 device categories by spend in the purchase order data and restricted that sample to devices used in cardiac catheterization, electrophysiology, and cardiac rhythm management. This resulted in 11 device categories: pacemakers cardiac implantable, prostheses cardiac valve biological, catheters vascular angioplasty balloon, catheters vascular guiding, leads implantable defibrillator/pacemaker, defibrillator/cardioverter/pacemakers implantable, catheters cardiac mapping/ablation, defibrillator/cardioverter/pacemakers implantable resynchronization, stents vascular coronary balloon‐expandable drug‐eluting, stents vascular coronary balloon‐expandable, and stent/grafts vascular aortic.
2.2. ECRI supply guide data
ECRI, a nonprofit healthcare research organization, collects and organizes data on purchase orders made by over 1000 member hospitals in the United States as part of its Supply Guide benchmarking service. For each transaction during 2010–2015, the Supply Guide data contain price, quantity, transaction month, vendor, manufacturer, and manufacturer catalog number for the device purchased. The reported data are of high quality because they are typically transmitted as a direct extract from a hospital's materials management database. Depending on hospital procedures, these prices may or may not be inclusive of rebates or other nonlinear contracting features, but prior work suggests that any such features have a small role in the types of physician preference item categories we study. 1 Hospitals also have strong incentives to report numbers relevant to their bottom line; analytics provided by the benchmarking service's web portal are based on data submitted by the hospital and compared to others in the database.
2.3. Management practices survey
We measure management using an approach developed by Bloom and Van Reenen for manufacturing firms. 10 These questions were adapted for the cardiac setting, resulting in a structured interview that queried hospital cardiac units on 18 management practices grouped into four primary management dimensions: Lean management (six practices), performance monitoring (five practices), targets (three practices), and employee incentives/talent management (four practices). The Lean grouping measured the unit's approach to standardizing care, minimizing variations, and clearly communicating between clinical and administrative personnel. The monitoring grouping focused on tracking key performance indicators and the existence of systematic processes for key activities, including purchasing. The targets grouping evaluated the clarity and ambition of unit targets (e.g., was the unit actively engaged in a drive toward a 0% bloodstream infection rate?). The incentives grouping examined the unit's methods for engaging and incentivizing employees. Units were scored between 1 and 5 on each question, with a higher score indicating better performance. The survey was conducted in 2010. Details of the survey approach and the method for mitigating self‐report bias have been described previously. 7 The study protocol was reviewed and approved by the institutional review board of Oregon Health and Science University.
We converted the cardiac units' management scores from the original scale ranging from 1 to 5, to z‐scores (mean 0 and standard deviation 1) for each of the 18 measured practices in order to standardize scaling across questions (e.g., interviewers might consistently give a higher score on Question 1 than on Question 2). We then compute the mean score across the questions in each of the four dimensions (Lean, monitoring, targets, incentives) to develop a dimension‐specific score for each hospital. Our main emphasis is on a composite score equaling the mean across these dimension‐specific scores for each hospital.
2.4. Hospital characteristics
We used a trusted third party, who had entered into a confidentiality agreement with ECRI, to link the management practice survey results and American Hospital Association (AHA) survey variables summarized in the paper to anonymous hospital identifiers that could then be merged with the de‐identified Supply Guide purchase order data. All analyses were run on this de‐identified data on a secure server, and only aggregate statistics and regression coefficients were extracted by researchers. As shown in Table 1, of the 1980 US hospitals with interventional cardiac catheterization laboratories and at least 25 annual acute myocardial infarction discharges in 2010, 648 responded to the management practices survey; 213 of those hospitals, in turn, appeared in the Supply Guide purchasing database with positive purchasing of any of the above cardiac device categories during 2010–2015. Hospitals joined Supply Guide over time, so cardiac device purchasing data were only observed for 111 hospitals in 2010, the year of the management practices survey. In our statistical analyses, we focus on two samples. In some analyses, we present results for 2010 only in order to focus on the association between management practices and contemporaneous prices. In order to increase our sample size and statistical power, we also present analyses for 2010–2015. Whether this longer time frame weakens or strengthens the relationship between management practices and prices depends on how much management changes over time, and on the lag with which any changes in management impact prices.
TABLE 1.
Representativeness of analytic sample
| Cardiac hospitals | Management survey | Management and purchase orders 2010–2015 | Management and purchase orders 2010 | |
|---|---|---|---|---|
| N hospitals | 1980 | 648 | 213 | 111 |
| Total management score | 3.13 (0.53) | 3.18 (0.51) | 3.16 (0.50) | |
| Lean score | 3.27 (0.56) | 3.30 (0.53) | 3.27 (0.53) | |
| Monitoring score | 3.37 (0.70) | 3.44 (0.66) | 3.39 (0.68) | |
| Target score | 3.02 (0.87) | 3.10 (0.86) | 3.08 (0.81) | |
| Talent score | 2.67 (0.67) | 2.72 (0.64) | 2.75 (0.61) | |
| Technology adoption score | 2.92 (0.92) | 3.25 (0.54) | 3.38 (0.52) | |
| Supply expense ratio | 0.16 (0.12) | 0.18 (0.12) | 0.17 (0.10) | 0.20 (0.14) |
| Supply expense ratio, missing | 0.21 (0.40) | 0.20 (0.40) | 0.14 (0.35) | 0.18 (0.38) |
| Total admissions | 13,151 (10807) | 17,066 (10831) | 18,994 (10959) | 19,804 (10950) |
| Technologies | 67 (25) | 77 (21) | 85 (22) | 86 (21) |
| Open heart surgery | 0.07 (0.25) | 0.10 (0.30) | 0.12 (0.32) | 0.11 (0.32) |
| Teaching | 0.45 (0.50) | 0.52 (0.50) | 0.57 (0.50) | 0.53 (0.50) |
| Nonprofit | 0.73 (0.45) | 0.75 (0.44) | 0.81 (0.39) | 0.82 (0.38) |
| Fraction Medicare | 0.43 (0.16) | 0.45 (0.09) | 0.45 (0.10) | 0.43 (0.10) |
| Fraction Medicaid | 0.18 (0.12) | 0.18 (0.08) | 0.19 (0.09) | 0.19 (0.08) |
| Urban | 0.98 (0.15) | 1.00 (0.06) | 0.99 (0.08) | 0.99 (0.09) |
| System member | 0.71 (0.45) | 0.64 (0.48) | 0.55 (0.50) | 0.53 (0.50) |
| N hospitals in system | 24 (43) | 24 (44) | 6 (14) | 8 (21) |
| Physician integration | 0.44 (4.88) | 0.25 (2.02) | 0.2 (0.67) | 0.22 (0.80) |
| Physician integration, missing | 0.03 (0.17) | 0.08 (0.26) | 0.05 (0.22) | 0.03 (0.18) |
| Reports GPO | 0.89 (0.31) | 0.89 (0.31) | 0.90 (0.30) | 0.92 (0.28) |
| Quantity purchased, hospital | 353 (1099) | 660 (2653) | ||
| Quantity purchased, system | 428 (1314) | 738 (2855) | ||
| Spend on other categories ($), hospital | 1,539,336 (1,844,649) | 1,481,796 (1,662,387) | ||
| Spend on other categories ($), system | 2,056,025 (2,545,463) | 1,953,576 (2,601,910) | ||
| Total spend ($) | 4,552,323 (4,413,913) | 4,660,369 (4,629,606) | ||
| N vendors | 4.31 (3.41) | 3.36 (2.37) |
Note: Author's calculations using merged, de‐identified American Hospital Association (AHA), Management Survey, and Supply Guide data. Each set of rows summarizes the counts and characteristics of hospitals in the data for various sample restrictions. Row 1 characterizes the 1980 hospitals in the AHA data with interventional cardiac catheterization laboratories and at least 25 heart attack discharges in 2010. Row 2 characterizes the subset of those hospitals (N = 648) that answered the management practices survey. Row 3 characterizes the subset of hospitals from row 2 matched to the Supply Guide transactions data (N = 213). Row 4 characterizes the subset of hospitals from row 3 that had Supply Guide transactions in 2010 (N = 111). Data on technologies, teaching status, admissions, nonprofit status, and Medicare and Medicaid shares come from the AHA Annual Survey for 2010. Following Acemoglu and Finkelstein13 and Cooper et al., 5 we measure technologies using the complete list of binary facility indicators available in the AHA. Management practice scores are simple sums of group‐specific and overall scores from the management practices survey. N vendors is the count of unique vendors purchased from for the average top cardiac category‐hospital in 2010–2015 (column 3) or 2010 only (column 4), and $ spend is the average total spend per hospital across all top cardiac categories in 2010–2015 (column 3) or 2010 only (column 4), both from the Supply Guide data.
The hospital characteristics in our analyses included several variables from AHA survey data: the hospital's overall supply expense ratio as validated by Abdulsalam and Schneller, 2 total hospital admissions, level of technology adoption as quantified by number of technologies available in the hospital (see Table 1 notes), an open heart surgery capability indicator, a teaching status indicator, a nonprofit ownership indicator, proportion of patients insured by Medicare, proportion of patients insured by Medicaid, Census division indicators, an urban versus rural indicator, an indicator for whether the hospital is part of a hospital system, and the number of hospitals in that system. We followed Dynan, Bazzoli, Burns, and Kuramoto 14 in coding management services organizations, integrated salary models, medical foundation models, and equity models, as “high‐integration” affiliations, and calculated a “Physician Integration” measure as the sum of physicians reported as being in each of the high‐integration affiliations at each hospital, normalized by the total count of physicians with privileges at the hospital. The AHA data also included the identity of a GPO used by the hospital for purchasing, if any. Unfortunately, we do not observe in our data whether a given price was negotiated via a GPO, consolidated service center, or other intermediary, and it bears noting that is relatively common for physician preference item prices to be negotiated off contract. 3 , 15 Finally, we used the merged, de‐identified AHA and Supply Guide data to calculate the total quantities purchased from the focal vendor within the focal product category at the hospital and system levels, and total expenditures with the focal vendor across other product categories at the hospital and system levels.
2.5. Statistical analysis
For each device category, we conducted regressions of the natural logarithm of price paid on the overall hospital management practice score. In all regressions, we control for indicator variables for interviewer, interviewee job position (e.g., nurse manager vs. unit director), interviewee location (e.g., intensive care unit vs. telemetry), and the duration, day, and week of the interview. In order to explore potential mechanisms and robustness, and to give context for magnitudes, we also considered regressions with fixed effect indicator variables for each device catalog number (to compare prices across hospitals within the exact same product) and several hospital characteristics that might also impact device prices. For analyses pooling 2010–2015, the catalog number fixed effects were interacted with year fixed effects in order to appropriately compare hospitals purchasing the same product at different points in its life cycle. Our control variables included all hospital characteristics noted previously, as well as the total number of unique vendors from which the hospital sourced its devices (as a proxy for device “standardization”). We focus our discussion on a pooled regression across all device categories, weighted by each category's overall spend, for 2010–2015. We also ran the same regressions for 2010 only and separately by product category. Standard errors were clustered at the hospital‐medical device level to allow for arbitrary correlations in unobservables across observations within a hospital‐medical device. All statistical analyses were performed using Stata 16.1 (College Station, TX).
3. RESULTS
3.1. Sample descriptive statistics
Table 1 reports summary statistics as they are available for: all nonfederal US hospitals with cardiac care units, the subset of these hospitals that completed the management practices survey, and the subset of these that were linked to the Supply Guide purchasing data. We identified 213 hospitals that were included in both the purchase order and management survey data. This represented 12% of 1980 total nonfederal US hospitals with cardiac care units. Hospitals in our sample had a mean supply expense ratio of 0.17 (standard deviation 0.10), admitted a mean of 18,994 total patients (standard deviation 10,959), and used a mean of 85 different technologies (standard deviation 22) in comparison with the sample of all cardiac care unit hospitals, which had a mean supply expense ratio of 0.16 (standard deviation 0.12), admitted a mean of 13,151 total patients (standard deviation 10,807), and used a mean of 67 different technologies (standard deviation 25). Approximately 57% of the hospitals in our sample were teaching hospitals and 81% were nonprofit, in comparison with 45% teaching and 73% nonprofit among all cardiac care unit hospitals. Our sample had a mean patient payer mix of 19% Medicaid and 45% Medicare, compared to all cardiac care unit hospitals at 18% Medicaid and 43% Medicare; 55% of hospitals in our sample were members of hospital systems with a mean system size of six hospitals, compared to 71% and 24 for all cardiac care unit hospitals. Finally, the mean hospital in our sample had a ratio of highly integrated physicians to privileged physicians of 0.20, compared to 0.44 for all cardiac care unit hospitals.
Put succinctly, hospitals that answered the management practices survey were larger and more “high‐tech” than the average hospital with a cardiac unit, and hospitals appearing in the Supply Guide data were even larger and more high‐tech, but less likely to be part of a large hospital system with highly integrated physicians.
3.2. Device purchase order descriptive statistics
The 213 hospitals with purchase order data spent a mean of $4.6 million (standard deviation $4.4 million) annually on the 11 cardiac device categories we considered. As illustrated in Figure 1, average prices that hospitals paid in a given device category varied across devices and hospitals, with coefficients of variation (the ratios of the standard deviations to the means) ranging from 0.03 (drug‐eluting stents) to 1.21 (guiding catheters). These means are greatly driven by variation in prices across devices within hospitals, with a coefficient of variation of 0.29 for the average category. However, there was also substantial variation across hospitals, within devices: after conditioning on product fixed effects, the coefficient of variation ranged from 0.04 (aortic stents) to 0.11 (angioplasty catheters). Our data included device categories with a wide range of unit prices, from fairly inexpensive guiding catheters ($82 mean price per unit) to very expensive resynchronization defibrillators ($21,247 mean price per unit).
FIGURE 1.
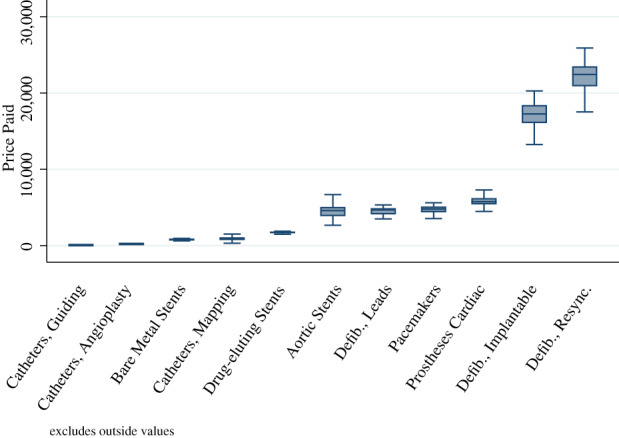
Variation in prices of important medical device categories. Box–Whisker plot of the distribution of average price per unit across hospitals within each top cardiac device category in 2010, for the sample of hospitals in column 4 of Table 1. Top cardiac device categories are ordered from left to right in the ascending order of mean price per unit: catheters vascular guiding, catheters vascular angioplasty balloon, stents vascular coronary balloon‐expandable, catheters cardiac mapping/ablation, stents vascular coronary balloon‐expandable drug‐eluting, stent/grafts vascular aortic, leads implantable defibrillator/pacemaker, pacemakers cardiac implantable, prostheses cardiac valve biological, defibrillator/cardioverter/pacemakers implantable, and defibrillator/cardioverter/pacemakers implantable resynchronization. Authors' calculations using de‐identified Supply Guide data [Color figure can be viewed at wileyonlinelibrary.com]
3.3. Management practice descriptive statistics
Among our sample hospitals, the average management score was 3.18, compared to an average score of 3.13 in the full management survey sample. However, there was a wide distribution in management practices, with a standard deviation of 0.51 in our sample and 0.53 in the full sample.
3.4. Relationship between device prices, management practices, and other hospital characteristics
Table 2 reports the results of our regression of log prices on management practices and various controls, for 2010–2015 and all cardiac device categories pooled. In the regression with all possible hospitals and controls included (column 3), a one standard deviation change in management score was associated with 1.33% lower cardiac medical device prices (95% confidence interval [CI] 0.99–1.67). This price differential was about three to four times the differential observed between higher and lower volume hospitals. For example, in the same regression, a one standard deviation increase in the number of patients admitted was associated with a 0.34% decrease in price. This result was robust to dropping all hospital control variables (column 2) or limiting the sample to device transactions in 2010 only (column 4). The coefficient on management practices without hospital control variables or product‐year fixed effects (column 1) was −0.06, consistent with better management practices being associated with purchasing lower priced devices, in addition to achieving lower prices than other hospitals for the same devices.
TABLE 2.
Association between management score and cardiac medical device prices
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Total management score (z) | −0.0602** (0.0230) | −0.00899*** (0.00158) | −0.0133*** (0.00173) | −0.0172* (0.00778) | |
| Lean score (z) | −0.0137*** (0.00250) | ||||
| Monitoring score (z) | 0.00911*** (0.00214) | ||||
| Target score (z) | −0.00747*** (0.00148) | ||||
| Talent score (z) | −0.00851*** (0.00170) | ||||
| Supply expense ratio (z) | 0.00396*** (0.00108) | 0.0124* (0.00621) | 0.00153 (0.00121) | ||
| Total admissions (1/0) | −0.00342** (0.00120) | −0.000374 (0.00795) | −0.00386** (0.00128) | ||
| Technologies (z) | 0.0000302 (0.00123) | 0.00239 (0.00675) | 0.000375 (0.00134) | ||
| Open heart surgery (1/0) | 0.0125*** (0.00340) | 0.00798 (0.0200) | 0.0221*** (0.00367) | ||
| Teaching (1/0) | −0.00529** (0.00204) | −0.0422** (0.0141) | −0.00590** (0.00211) | ||
| Nonprofit (1/0) | −0.0302*** (0.00227) | 0.00392 (0.0111) | −0.0234*** (0.00242) | ||
| Fraction Medicare (z) | −0.00742*** (0.000996) | 0.0294*** (0.00736) | −0.00495*** (0.00102) | ||
| Fraction Medicaid (z) | −0.00121 (0.000865) | 0.0374*** (0.00755) | −0.000136 (0.000903) | ||
| Urban (1/0) | 0.0543*** (0.0117) | 0.228*** (0.0300) | 0.0739*** (0.0124) | ||
| System member (1/0) | −0.00172 (0.00202) | 0.000895 (0.00980) | −0.00381 (0.00214) | ||
| N hospitals in system (z) | −0.000155 (0.00134) | 0.0256*** (0.00542) | 0.00332* (0.00152) | ||
| Physician integration (z) | −0.000473 (0.000637) | −0.00752*** (0.00175) | −0.000279 (0.000631) | ||
| Quantity purchased, hospital (z, log) | −0.00400* (0.00187) | 0.00802 (0.00431) | −0.00326 (0.00192) | ||
| Quantity purchased, system (z, log) | −0.0240*** (0.00203) | −0.0304*** (0.00488) | −0.0244*** (0.00206) | ||
| Spend on other categories ($), hospital (z, log) | −0.00410 (0.00342) | −0.00536 (0.0105) | −0.00479 (0.00343) | ||
| Spend on other categories ($), system (z, log) | −0.00705 (0.00425) | −0.00138 (0.0126) | −0.00671 (0.00425) | ||
| N vendors (z) | 0.00284*** (0.000684) | −0.00415** (0.00148) | 0.00268*** (0.000673) | ||
| R 2 | 0.0141 | 0.996 | 0.996 | 0.997 | 0.996 |
| N | 1,513,341 | 1,503,087 | 1,466,079 | 164,171 | 1,466,078 |
| N hospitals | 213 | 213 | 213 | 111 | 213 |
Note: Author's calculations using merged, de‐identified American Hospital Association (AHA), Management Survey, and Supply Guide data. Point estimates and standard errors for the relationship (clustered by hospital‐product) between average unit price and aggregate hospital management practice score, as well as other characteristics, pooled across top cardiac device categories. Regression sample is at the hospital‐month‐device category‐catalog number level. Device categories are weighted by total expenditure across all 2010 regression sample hospitals. (1/0) indicates binary variables. (z) indicates continuous variable was transformed into a z‐score. (z, log) indicates continuous variable was log‐transformed and then transformed into a z‐score. Column 1 does not include controls. Columns 2–4 control for category‐catalog number‐year fixed effects. Columns 3 and 4 include hospital characteristics of interest and Census division fixed effects. Columns 1–3 include all hospital‐years 2010–2015; column 4 includes 2010 only.
*p < 0.05, **p < 0.01, and ***p < 0.001.
At the mean hospital spend in our data, a 1.33% price decrease across all devices would translate into savings of $61,000 annually. At a larger hospital with spending one standard deviation above the mean, the savings would be $120,000 annually.
Figure 2 plots the coefficients (point estimates and 95% confidence intervals) on management scores obtained by running the same regression for 2010–2015 and with the full set of controls for each category separately. The price difference associated with better management scores varied across the device categories we considered. The coefficients were negative and significant for 7 of 11 device categories, close to zero and insignificant for three categories, and positive and significant for one category. The minimum coefficient indicated a price decrease of 1.68% (implantable defibrillators); the maximum coefficient indicated a price increase of 0.44% (cardiac valve prostheses).
FIGURE 2.
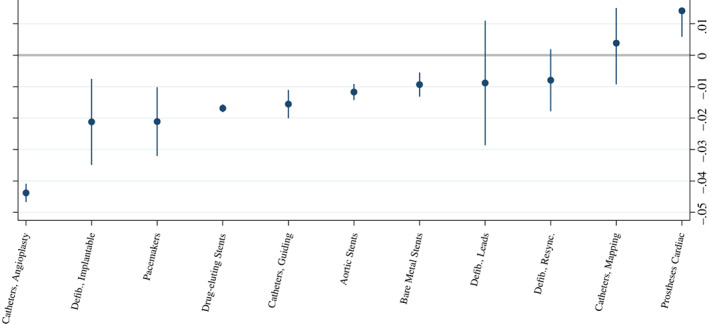
Associations between management score and medical device prices, by category. Author's calculations using merged, de‐identified American Hospital Association (AHA), Management Survey, and Supply Guide data. Point estimates and 95% confidence interval (based on robust standard errors clustered at the hospital‐product level) for the relationship between average unit price and aggregate hospital management practice score, as well as other characteristics, within each top cardiac device category. Top cardiac device categories are ordered from left to right in the ascending order of point estimates: catheters vascular angioplasty balloon, defibrillator/cardioverter/pacemakers implantable, pacemakers cardiac implantable, stents vascular coronary balloon‐expandable drug‐eluting, catheters vascular guiding, stent/grafts vascular aortic, stents vascular coronary balloon‐expandable, leads implantable defibrillator/pacemaker, defibrillator/cardioverter/pacemakers implantable resynchronization, catheters cardiac mapping/ablation, and prostheses cardiac valve biological. Each regression sample is at the hospital‐month‐catalog number level. Specification controls for category‐catalog number‐year fixed effects, Census division fixed effects, and hospital characteristics of interest from columns 3 and 4 of Table 2. Sample includes all hospital‐years 2010–2015 [Color figure can be viewed at wileyonlinelibrary.com]
In Table 2, column 5, we replaced the composite management practices score in the regression in column 3 with each of the four disaggregate primary management practice dimensions: Lean management, performance monitoring, targets, and employee incentives/talent management. A one standard deviation change in each primary management score dimension was associated with 1.37% lower cardiac medical device prices for the Lean grouping (95% CI [0.88–1.86]); 0.91% higher cardiac medical device prices for the monitoring grouping (95% CI [0.49–1.33]); 0.75% lower cardiac medical device prices for the target grouping (95% CI [0.46–1.03]); and 0.85% lower cardiac medical device prices for the talent grouping (95% CI [0.52–1.18]).
The only control variable that we estimated to be associated with similar savings to management practices and equally robust across regression specifications was quantity of the same device purchased from the same vendor at the same hospital system. A one standard deviation increase in the log of this quantity measure was associated with 2.40% lower cardiac medical device prices (95% CI [2.00–2.80]) in column 3. This coefficient should be interpreted with care, however, because it may capture a combination of quantity discounting and/or physician reluctance to use more expensive devices (i.e., downward sloping demand). The small coefficient on hospitals' overall supply expense ratio, and the limited impact of controlling for supply expense ratio on the estimated relationship between management practices and cardiac device prices, suggests that conditional on all other controls, the factors governing the relationship between cardiac management practices and cardiac medical device prices are somewhat independent of the factors governing the relationship between cardiac management practices and overall supply expense.
4. DISCUSSION
This article linked data on device purchase orders, hospital characteristics, and survey data on management practices in cardiac units and assessed the relationship between management and prices paid for medical devices. We found that hospitals with higher management scores paid lower prices for cardiac devices. The association was modest but robust. At the average size hospital in our sample, a one standard deviation higher management practice score would be associated with $61,000 less spending on the device categories we study.
The connection between lower prices and higher management scores may reflect a variety of management attributes. The aggregate management score may reflect exposure to managerial training, which may extend beyond Lean and talent management to include skills in negotiation, bargaining, or cost control. Interestingly, when we disaggregated the composite management score into its four primary dimensions, we found that the overall relationship between better management practices and lower device prices was made up roughly in equal parts by Lean management, target setting, and talent management. Better performance monitoring processes, which focused directly on strategies for collecting and tracking key performance indicators such as cost, were actually correlated with slightly higher input prices. These results should be interpreted with caution given that the data generating process is observational and not experimental. However, they are at least consistent with it being important for hospitals to hire the right talent, set their target goals appropriately, and facilitate communication among clinical and nonclinical stakeholders. Monitoring processes may either interfere with activities that reduce supply costs or perhaps be undertaken by hospitals that struggle with negotiating device prices for other reasons.
4.1. Comparison with prior findings
Our findings are consistent with other studies of management practices. McConnell et al. found that management practices were correlated with lower mortality, 7 better patient satisfaction, and more admissions for acute myocardial infarction. 16 Tsai and colleagues found that higher‐rated hospital boards (measured by their attention to clinical quality) were more likely to have high management scores, suggesting that board priorities may have translated to managerial skill within cardiac units. 17 Hospitals' management practices also appear to be correlated with their proximity to business schools. 12 Although the effects are often modest, they are consistent across a variety of measures and studies. The management score may be noisy, but appears to measure some component of managerial skill that is correlated with patient outcomes and hospital performance. In our study, the correlation extends to device purchasing.
Our findings are also consistent with other studies of device purchasing, which have in general found modest associations between other mechanisms and device prices. Grennan and Swanson found that transparency in the form of access to benchmarking information was associated with an average 1.3% price decrease in coronary stents. 1 Craig and colleagues found that hospital mergers were associated with 0.5% price decreases on average across a large number of device categories. 4 Despite the apparent potential for lower device costs indicated by the large price variation across hospitals, our study echoes these in finding that any single mechanism seems to be associated with modest savings. This makes it all the more important to continue research on the many factors that could each chip away at the large potential savings in hospital purchasing.
Finally, our article complements a rich literature on the widely‐noted inefficiencies in supply chain and operations management in healthcare systems, which analyze variation in hospital supply expenses 2 and other measures of operational efficiency, and the potential for a variety of organizational and strategic interventions to yield improvements. These interventions include the use of consolidated service centers, 3 GPOs, 18 hospital purchasing alliances, 19 physician integration, 20 , 21 and product standardization, 11 to name just a few. Many of these interventions are at least partially correlated with the management practices that are the focus of this study, although our results are robust to the inclusion of controls for their use, where available. Our article contributes to this literature by analyzing novel data on management practices in cardiac units, and by focusing on a dependent variable capturing the performance of those units (negotiated prices within narrowly defined products). This allows us to isolate the association between management practices and performance, removing concerns that variation in supply costs vary with the quantity or quality of products purchased, or with the case mix of patients treated. 2
4.2. Relevance for hospital management and policy making
Our findings suggest that well‐managed hospitals may be able to control or reduce their internal costs more effectively than poor‐managed hospitals. This, in turn, suggests that it may be profitable for hospitals to invest in improving management practices. Several prior experimental and quasi‐experimental studies have found large causal effects of management practices assistance on manufacturing firm productivity, 22 , 23 , 24 and this strikes us as an important open area for future research in the hospital setting. Although our study suggests the effects may be modest, they are not trivial, and management‐driven efforts to reduce expenditures may serve as one part of larger effort to control costs. Cooper and Scott Morton 25 suggest that tackling healthcare spending may be best accomplished through a series of discrete incremental actions, which address what they call “one percent problems.” They outline efforts that focus on eliminating narrow inefficiencies in the health system, such as expanding preferred pharmacy networks 26 or decreasing cost barriers for living kidney donations. 27 Although each measure may have a small effect, they add up to substantial reductions. To the extent that our findings of savings in devices extend to broader hospital savings, management practices may be one more incremental mechanism to address costs.
Our findings may also have salience in states and regions where hospitals face greater scrutiny to control costs. A combination of market power and fee‐for‐service arrangements may have blunted hospitals' incentives to reduce spending growth. Efforts to grow or sustain margins by expanding revenues may have been easier than efforts to reduce a hospital's internal costs while holding revenue constant. However, a variety of policies and payment reforms may cap revenue growth, creating greater incentives for hospitals to preserve margins by addressing their expenses. In 2012, Massachusetts initiated a Health Care Cost Growth Benchmark, aiming to hold total state spending to a rate of 3.6% or lower, with other states, including Delaware, Rhode Island, and Oregon following suit.
4.3. Limitations
The study was limited to hospitals that responded to a management practices survey and subscribed to the Supply Guide benchmarking service, and it is possible that these hospitals may differ from the average hospital with cardiac services in observable (e.g., they were slightly larger and used more technologies) and unobservable ways. However, the distribution of management scores was not statistically different among hospitals with and without purchase order data. It is not clear what implications any differences might have for the association between management practices and medical device prices. We studied 11 cardiac device categories where hospitals spend the most, and relationships may also differ for lower spend cardiac devices or for device categories outside of cardiology. We analyzed management practices survey data from 2010 and medical device price data from 2010 to 2015 because more recent data on hospital management practices do not exist. Finally, this cross‐sectional study can only be taken as suggestive evidence of a potential causal effect of management practices on medical device prices. While our analysis controls for a number of potentially important determinants of prices, there may be unobserved factors that impact performance in hospital purchasing that are also correlated with management practices.
4.4. Summary
For a sample of 213 US hospitals with detailed data available on management practices and medical device purchase orders, we found that better management practices were associated with lower device prices. Given the substantial level and growth in hospital spending on such devices, even the modest relationship we document could point to one useful tool for decreasing the cost of care associated with the use of medical technology.
CONFLICT OF INTEREST
Dr. Matthew Grennan provided consulting services to Analysis Group unrelated to this work. The other authors have no conflicts of interest to disclose.
ACKNOWLEDGMENTS
We thank ECRI for providing the data, Stuart Craig for assistance managing and merging the data, and Grace Nie for research assistance.
Grennan M, Kim GH, McConnell KJ, Swanson A. Hospital management practices and medical device costs. Health Serv Res. 2022;57(2):227-236. doi: 10.1111/1475-6773.13898
Funding information McConnell's work in developing and fielding the survey was supported by a grant from the Agency for Healthcare Research and Quality (Grant No. 1R01HS018466). Grennan and Swanson gratefully acknowledge support from the National Science Foundation (SES‐1559485).
REFERENCES
- 1. Grennan M, Swanson A. Transparency and negotiated prices: the value of information in hospital‐supplier bargaining. J Polit Econ. 2020;128(4):1234‐1268. doi: 10.1086/705329 [DOI] [Google Scholar]
- 2. Abdulsalam Y, Schneller E. Hospital supply expenses: an important ingredient in health services research. Med Care Res Rev MCRR. 2019;76(2):240‐252. doi: 10.1177/1077558717719928 [DOI] [PubMed] [Google Scholar]
- 3. Abdulsalam Y, Gopalakrishnan M, Maltz A, Schneller E. The emergence of consolidated service centers in health care. J Bus Logist. 2015;36(4):321‐334. doi: 10.1111/jbl.12107 [DOI] [Google Scholar]
- 4. Craig SV, Grennan M, Swanson A. Mergers and marginal costs: New evidence on hospital buyer power. RAND J Econ. 2021;52(1)151‐178. doi: 10.1111/1756-2171.12365 [DOI] [Google Scholar]
- 5. Cooper Z, Craig S, Gaynor M, Van Reenen J. The Price Ain't right? {hospital} prices and health spending on the privately insured. Q J Econ. 2019;134(1):51‐107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maeda JL, Raetzman SO, Friedman BS. What hospital inpatient services contributed the most to the 2001‐2006 growth in the cost per case? Health Serv Res. 2012;47(5):1814‐1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McConnell KJ, Lindrooth RC, Wholey DR, Maddox TM, Bloom N. Management practices and the quality of care in cardiac units. JAMA Intern Med. 2013;173(8):684‐692. [DOI] [PubMed] [Google Scholar]
- 8. Bloom N, Sadun R, Van Reenen J. Does management matter in healthcare?. 2014.
- 9. Decarolis F, Giuffrida LM, Iossa E, Mollisi V, Spagnolo G. Bureaucratic competence and procurement outcomes. J Law Econ Organ. 2021;36(3):537‐597. doi: 10.1093/jleo/ewaa004. [DOI] [Google Scholar]
- 10. Bloom N, Van Reenen J. Measuring and explaining management practices across firms and countries. Q J Econ. 2007;122(4):1351‐1408. doi: 10.1162/qjec.2007.122.4.1351 [DOI] [Google Scholar]
- 11. Montgomery K, Schneller ES. Hospitals' strategies for orchestrating selection of physician preference items. Milbank Q. 2007;85(2):307‐335. doi: 10.1111/j.1468-0009.2007.00489.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bloom N, Lemos R, Sadun R, van Reenen J. Healthy business? Managerial education and management in health care. Rev Econ Stat. 2020;102(3):506‐517. doi: 10.1162/rest_a_00847 [DOI] [Google Scholar]
- 13. Acemoglu D, Finkelstein A. Input and technology choices in regulated industries: Evidence from the health care sector. J Polit Econ. 2008;116(5):837‐880. doi: 10.1086/595014 [DOI] [Google Scholar]
- 14. Dynan L, Bazzoli GJ, Burns R. Assessing the extent of integration achieved through physician‐hospital arrangements. J Healthc Manag Am Coll Healthc Exec. 1998;43(3):242‐261, discussion 261‐262. [PubMed] [Google Scholar]
- 15. Schneller ES The value of group purchasing ‐ 2009: meeting the needs for strategic savings. Health Care Sector Advances, Inc. 2009, p. 26.
- 16. McConnell KJ, Lindrooth RC, Wholey DR, Maddox TM, Bloom N. Modern management practices and hospital admissions. Health Econ. 2016;25(4):470‐485. doi: 10.1002/hec.3171 [DOI] [PubMed] [Google Scholar]
- 17. Tsai TC, Jha AK, Gawande AA, Huckman RS, Bloom N, Sadun R. Hospital board and management practices are strongly related to hospital performance on clinical quality metrics. Health Aff. 2015;34(8):1304‐1311. doi: 10.1377/hlthaff.2014.1282 [DOI] [PubMed] [Google Scholar]
- 18. Rhea S. Above and beyond. Regional GPOs work to offer value, services that their national counterparts often don't provide. Mod Healthc. 2009;39(35):S1‐S5. [PubMed] [Google Scholar]
- 19. Burns LR, Briggs AD. Hospital purchasing alliances: ten years after. Health Care Manag Rev. 2020;45(3):186‐195. doi: 10.1097/HMR.0000000000000215 [DOI] [PubMed] [Google Scholar]
- 20. Young GJ, Nyaga GN, Zepeda ED. Hospital employment of physicians and supply chain performance: an empirical investigation. Health Care Manag Rev. 2016;41(3):244‐255. doi: 10.1097/HMR.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 21. Zepeda ED, Nyaga GN, Young GJ. The effect of hospital‐physician integration on operational performance: evaluating physician employment for cardiovascular services. Decis Sci. 2020;51(2):282‐316. doi: 10.1111/deci.12401 [DOI] [Google Scholar]
- 22. Giorcelli M. The long‐term effects of management and technology transfers. Am Econ Rev. 2019;109(1):121‐152. doi: 10.1257/aer.20170619 [DOI] [Google Scholar]
- 23. Bloom N, Eifert B, Mahajan A, McKenzie D, Roberts J. Does management matter? Evidence from India*. Q J Econ. 2013;128(1):1‐51. doi: 10.1093/qje/qjs044 [DOI] [Google Scholar]
- 24. Bruhn M, Karlan D, Schoar A. The impact of consulting services on small and medium enterprises: evidence from a randomized trial in Mexico. J Polit Econ. 2018;7:635‐687. doi: 10.1086/696154 [DOI] [Google Scholar]
- 25. Cooper Z, Scott MF. Health care reform: one (percent) step at a time. Health Affairs Blog doi: 10.1377/hblog20210209.381915 [DOI]
- 26. Starc A, Swanson A. Preferred pharmacy networks and drug costs. Am Econ J Econ Pol. 2021;13:406‐446. doi: 10.1257/POL.20180489 [DOI] [Google Scholar]
- 27. Elías JJ, Lacetera N, Macis M. Paying for kidneys? A randomized survey and choice experiment. Am Econ Rev. 2019;109(8):2855‐2888. doi: 10.1257/aer.20180568 [DOI] [Google Scholar]


