Abstract
Purpose of the review
Though it is well known that cirrhosis is associated with significant morbidity and mortality, management of symptoms in cirrhosis can be difficult. This review serves to offer practical guidance in the management of liver-specific symptoms of cirrhosis as well as other symptoms with special hepatic considerations.
Recent findings
We discuss liver-specific symptoms and management, including ascites and refractory ascites, hepatic encephalopathy, pruritus, and muscle cramping. We also discuss the challenges of treating more generalized symptoms in cirrhosis, including pain, depression/anxiety, appetite, and fatigue. Medication management is, especially complex in this population given the altered metabolism of drugs, and we consider some strategies to approach this.
Summary
With the right tools, provided throughout this review, hepatologists should be well equipped to manage the nuanced liver-specific and generalized symptoms in patients with cirrhosis.
Keywords: Cirrhosis, End-stage liver disease, Palliative hepatology, Hepatic encephalopathy, Ascites, Pruritis
Introduction
Each year in the USA, growing numbers of people are being diagnosed with and dying from cirrhosis. According to the Center for Disease Control, in 2020 alone, there were 51,642 deaths attributable to cirrhosis [1]. In addition to high mortality rates, patients with cirrhosis suffer considerable morbidity. In fact, patients with cirrhosis have been shown to have similar negative levels of health-related quality of life to patients with chronic obstructive pulmonary disease or congestive heart failure [2].
Given the growing incidence of disease and symptom burden, palliative hepatology has emerged as an area of interest to clinicians, researchers, and patients to improve the quality of life for those with cirrhosis. While much of the literature in palliative hepatology has focused on methods to measure patient quality of life, referral rates to palliative care, and caregiver burden, there remains a dearth of guidance on how we, as hepatologists, can better manage our patients’ symptoms. In addition to the high symptom burden in patients with cirrhosis, there are physiological changes associated with cirrhosis that impact the metabolism of many medications, thereby creating challenges in treatment [3•].
Despite these challenges, we need to ensure that we approach symptom management aggressively at all phases of care—whether on the waiting list for transplant or transitioning to hospice care. Providers should be malleable and work together with patients to create an open dialogue where patients feel comfortable discussing their symptoms. Providers must also acknowledge both their limitations and that treatment for one symptom could worsen others.
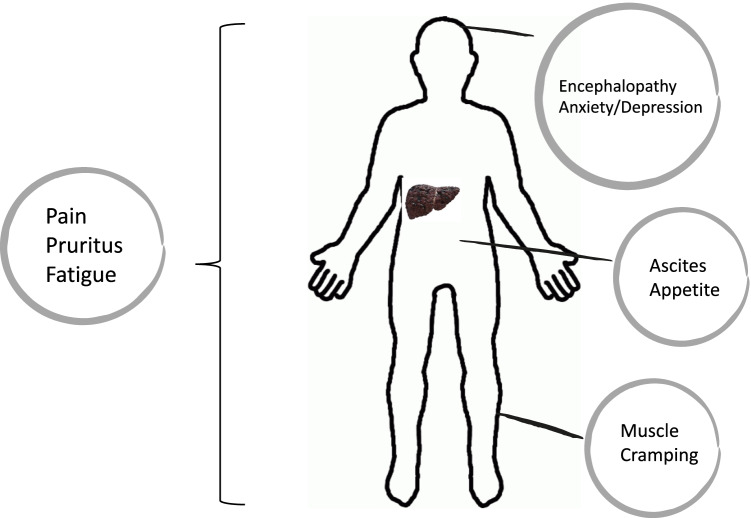
This review summarizes what we know about the symptoms experienced by patients with cirrhosis and offers practical guidance on how to best manage them. We will discuss liver-specific symptoms, including ascites, hepatic encephalopathy, pruritus, and muscle cramping, as well as more generalized symptoms such as pain, appetite, depression and anxiety, and fatigue, with special liver considerations (Fig. 1). Though understanding the pathophysiology for each of these symptoms is important, this review will be focused specifically on treatments and their potential adverse effects.
Fig. 1.
Liver-specific and generalized symptoms in cirrhosis. Various symptoms are addressed as part of this review. Liver-specific symptoms include ascites, encephalopathy, muscle cramping, and pruritus. Generalized symptoms with liver-specific considerations include pain, anxiety/depression, appetite, and fatigue
Liver-specific symptoms
Ascites
The development of ascites in cirrhosis is the most common decompensation event and indicates a 50% 2-year mortality. When refractory, ascites is associated with 1-year mortality rates as high as 70% [4]. Hepatic hydrothorax, which develops by similar mechanisms to ascites, can cause even more symptoms as smaller volumes of fluid accumulation can cause substantial respiratory distress. In addition to its association with poor prognosis, the presence of ascites, whether in the abdomen or thorax, is also a significant predictor of poor quality of life [5].
New guidelines on the management of ascites were recently published by the American Association for the study of liver diseases [6•]. Ascites is typically initially managed with a combination of dietary counseling and prescription of diuretics. Patients are advised to follow a sodium-restricted diet (2 g or 90 mmol/day), though adherence to a low sodium diet is difficult [7], and we would recommend consideration of formal consultation with a dietician. Fluid restriction is not recommended; sodium restriction is both more important and sufficient.
The choice of diuretics usually involves a combination of aldosterone antagonists with loop diuretics. Aldosterone antagonists are particularly effective in the cirrhosis population given that hyperaldosteronism plays a significant role in ascites formation. The initial starting doses of diuretics are typically 100 mg/day of spironolactone and 40 mg/day of furosemide. Once natriuresis is achieved, diuretic doses should be reduced to the lowest effective dose to achieve minimal or no ascites.
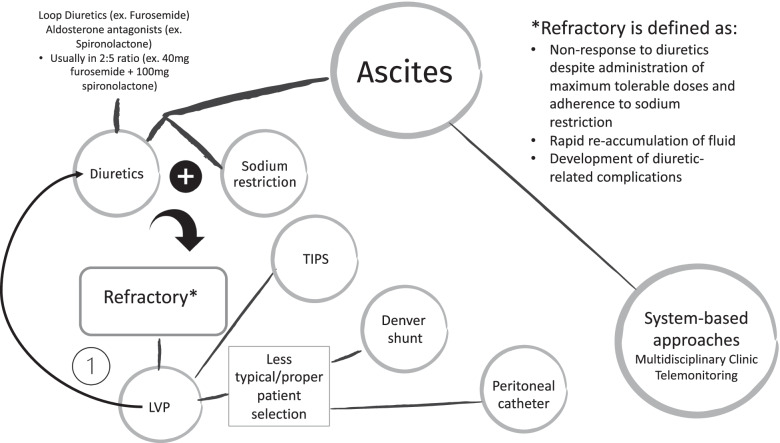
Though sodium restriction and diuretic therapy can be helpful, especially initially, they can become limited (Fig. 2). Refractory ascites (defined as a non response to diuretics despite administration of maximum tolerable doses and adherence to sodium restriction; rapid re-accumulation of fluid; or the development of diuretic-related complications) often occurs as liver disease progresses. The mortality rate associated with refractory ascites is quite high, and there are special considerations for this group of patients.
Fig. 2.
Treatment algorithm for ascites. A practical approach to the management of ascites in patients with cirrhosis is demonstrated. The first step in management involves a combination of diuretics and sodium restriction. The diuretic choice usually includes a combination of loop diuretics and aldosterone antagonists. If ascites is refractory despite diuresis and sodium restriction, the first step normally involves LVP. Sometimes, patients can return to diuretic therapy after LVP. Other patients, especially those with lower MELD scores, can be candidates for TIPS. Denver shunts are less commonly placed today given the potential for complications. In other patients, especially in those who may be palliative, an appropriate option to consider is a peritoneal catheter. *LVP, large volume paracentesis; TIPS, transjugular intrahepatic portosystemic shunt
First-line treatment for refractory ascites is frequent large volume paracenteses (LVPs). LVPs are generally safe and have very few contraindications—severe complications like intra-abdominal bleeding happen in < 1% of cases [8]. The co-administration of albumin when large volumes (> 5 L) of ascites are removed can help to prevent post-paracentesis circulatory dysfunction that can result from large fluid shifts [6•]. Frequent LVPs, however, can be burdensome for patients, especially during the COVID-19 pandemic. For those who live at a distance from a hospital, for example, travel for LVPs can be both timely and costly. Frequent introduction of needles into the abdomen can also increase the risk of spontaneous bacterial peritonitis [9]. Leakage of ascites after paracenteses can be not only a nidus of infection but also an irritant to the surrounding skin.
An alternative to frequent LVPs, especially for those with the model for end-stage liver disease (MELD) scores < 18 is to place a transjugular intrahepatic portosystemic shunt (TIPS). Placement of a TIPS has been demonstrated to improve symptoms in patients with refractory ascites, refractory bleeding from varices, or hepatic hydrothorax [10]. When compared to frequent LVPs for refractory ascites, early placement of a TIPS in the right patient is associated with improved survival (93 versus 53% in one study) [11•]. However, because of the shunting that occurs with TIPS placement, patients are more susceptible to hepatic encephalopathy (HE). The risk of HE after TIPS placement is about 25%, which is not insignificant [12], and 3–7% of patients can be medication refractory [13]. Some risk factors for HE after TIPS placement include sarcopenia, prior HE, higher MELD, and advanced age [14, 15]. Therefore, while there could be symptom benefits of the procedure, the risks and alternatives need to be carefully discussed, especially in high-risk groups.
It is worth noting that the LeVeen or Denver shunt is also a possibility for the management of ascites, though it is less commonly performed than TIPS. The procedure involves the placement of a shunt in the abdomen, often by interventional radiology that returns ascites to the central venous circulation. Though HE is not a concern with the Denver shunt, there are many potential complications, including occlusion, bleeding, and peritonitis. Additionally, because they are placed less often, it may be difficult to find physicians or centers that feel comfortable to place and manage them [16].
An additional option to consider, especially for patients who are not liver transplant candidates, is a long-term abdominal drain. In a randomized control trial of LVP versus peritoneal drain placement for those with refractory ascites who were not transplant candidates, placement of a drain was both effective and safe and reduced health resource utilization [17]. A meta-analysis suggested low complication rates, though in general, there is a lack of well-designed studies [18]. One qualitative study demonstrated that patients expressed a preference for this approach so that they could remain at home without requiring multiple hospital visits [19]. With drain placement, patients can also potentially avoid the discomfort and symptoms associated with the development of large volume ascites before an LVP.
Other than treatment-based approaches to the management of ascites, there are system-based techniques that have been demonstrated to reduce mortality and costs associated with ascites. One such method was described in a study by Morando et al. whereby a “care management check-up” team comprised of consultant hepatologists, dedicated nurses, and physicians in training were able to help make decisions for patients with ascites and to share these decisions with patients’ general practitioners. This approach was associated with a reduction in 12-month mortality, specifically related to liver disease compared to a standard model of outpatient care [20]. However, it does require significant resources and time, which are often not available. Another system-based technique that has been shown to be cost-effective and associated with improvement in quality of care is telemonitoring. Bloom et al. used weight telemonitoring to identify rapidly increasing or decreasing weight in patients with ascites. Using model analysis, for every 100 patients, telemonitoring led to a cost savings of > $150,000 over 6 months and prevented 9 hospital admissions [21].
Encephalopathy
HE is another symptom that is very common in patients with cirrhosis and is strongly associated with impaired quality of life. HE can be difficult to detect, especially in its early stages. Early or covert encephalopathy can be marked by sleep–wake cycle disturbances, forgetfulness, mood changes, or difficulties concentrating. Often these early stages are not detected by patients or their caregivers and may require formal psychometric testing to diagnose. Additionally, HE can be very distressing to patients and their families, especially in patients who were recently high-functioning.
The first step in assessing and treating HE is to reverse any precipitating causes. After, the standard of care treatment is lactulose. While lactulose reduces the risk of developing serious liver-related adverse events and reduces mortality [22], it can be very poorly tolerated given its propensity to cause gas, bloating, and diarrhea. One strategy that can be successful in mitigating these side effects is to titrate the dose based on the unique patient rather than based on standardized dosing regimens. Some patients will have no HE with two bowel movements per day, while others require four or more per day. In fact, there has been some recent controversy as to whether the frequency of bowel movements in cirrhosis is tied to cognitive function at all [23•]. A different strategy is to intermix polyethylene glycol (PEG) with lactulose, especially when bloating is an issue. Though the use of PEG alone for the treatment of HE is not widely accepted, in clinical practice, we find that patients often tolerate PEG mixed with lactulose better than lactulose alone. Especially for patients that cannot tolerate the taste or syrupy consistency of lactulose, alternative strategies include using the powder form of lactulose, kristalose, or diluting lactulose with water.
Rifaximin can be used in combination with lactulose as secondary prophylaxis to reduce the risk of recurrence of overt HE but should not be used as a primary agent to treat HE acutely [24]. Compared to other antibiotics that have been trialed to treat HE, rifaximin is safe and has a low propensity to induce bacterial resistance. Despite its demonstrated benefits, one of the main problems with rifaximin remains its cost [25]. Cost-effectiveness analyses have demonstrated that its addition to lactulose is cost-effective compared to lactulose monotherapy. This is a strong argument that its cost should be covered more broadly by insurance companies because currently, it is still quite inaccessible to many [26•].
Other treatment options for HE are less well studied, and some, such as ornithine-aspartate, are not even available in the USA. Because patients with cirrhosis often have zinc deficiency, and this can precipitate HE [27], zinc supplementation in combination with lactulose has been demonstrated to be effective in mild HE [28]. Nutrition is particularly important in managing HE. Patients should be counseled to take in at least 35 kcal/kg/day with 1.2–1.5 g/kg/day of protein (> 1.5 g/kg/day if the patient is already malnourished) [29]. Late-night snacks containing ≥ 50 g of complex carbohydrates have been shown to be particularly effective [30]. Though at one time it was felt that high protein diets could worsen HE given synthesis of ammonium, this is no longer felt to be true, and patients should not limit the protein in their diet [31]. In fact, nutritional therapy, including appropriate caloric and protein intake, has been associated with improvement in minimal HE and prevention of overt HE episodes [32].
Addressing HE at the end of life in patients with cirrhosis poses an additional ethical challenge. While the side effects of treatment for HE (ex. frequent bowel movements, diarrhea, and bloating) can be uncomfortable for patients, this must be balanced against the desire for mental clarity and lack of confusion at the end of life. It is important to recognize, however, that as patients approach end-of-life, they may become weaker and less mobile, eat less, and goals may shift away from continued lactulose treatment. Discussing with patients and their caregivers their values and desires for end of life early is important so that value-concordant care can be provided. Patients and their families will often look for guidance from their providers in making difficult decisions, and therefore, discussing expectations openly and honestly is imperative.
Pruritus
Though less common than some of the other liver-specific symptoms, pruritis can certainly impact patient quality of life. It is more common in some of the cholestatic etiologies of liver disease, such as primary biliary cholangitis or primary sclerosing cholangitis, but can be seen in other etiologies of liver disease as well. Itching can be generalized or localized, and the severity does not necessarily correlate with disease severity or bilirubin levels. The pathophysiology is not well understood, but bile acids, lysophosphatidic acid, and autotaxin have been implicated [33, 34].
Typical treatments that are tried initially are topical emollients, cool humidified air, and avoidance of frequent bathing, hot water, and harsh soaps or detergents. Once medications are needed, bile acid sequestrants, such as cholestyramine or colestipol, are often used [35]. Bile acid sequestrants, however, must be taken 1 h after or 4 h before other medications so as not to impact absorption. This can be difficult for patients to remember, so we often recommend setting alarms. More recently, nalfurafine hydrochloride, a κ-opioid receptor agonist, has been demonstrated to be effective in the treatment of refractory pruritus, though it has not been widely adopted in practice [36]. Additional options for pruritus include sertraline, rifampin, or naltrexone, though naltrexone can counteract the effects of any opioid medications the patient is taking.
Muscle cramping
Muscle cramping can be quite common in cirrhosis, occurring in up to 1/3 of patients, though the mechanism is not entirely understood. Thought at one time to be secondary to electrolyte disturbances, some of the original studies showed that electrolytes were similar in those with and without cirrhosis. Instead, ATP, which is needed for myosin to detach from actin in muscle, was much lower in those with cirrhosis than those without [37]. Therefore, it is possible that ATP may be implicated. Additionally, those with cirrhosis have lower circulating blood volume, and this could be associated with increased sympathetic nerve activity [38]. For patients with cirrhosis, restoration of effective circulating blood volume with albumin has been shown to result in improvement in cramping [39]. Other less traditional treatments include quinine, taurine, and potentially even baclofen [40–42]. Muscle cramping is a symptom that practitioners should specifically ask about, given patients may not realize it is connected to their liver disease and is associated with decreased quality of life [43].
Generalized symptoms with liver-specific considerations
Pain
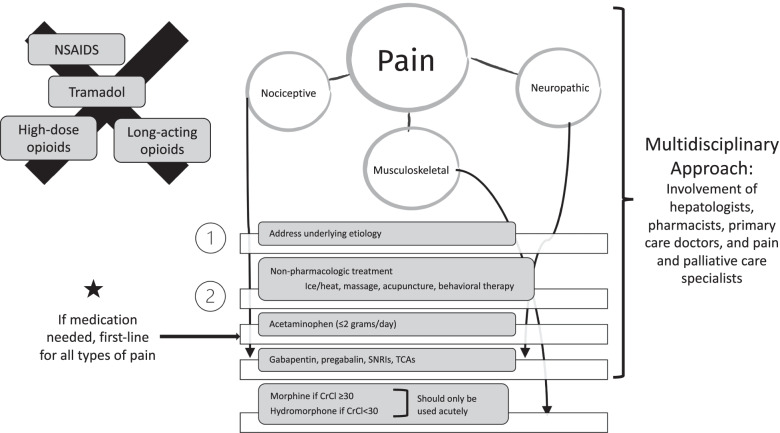
Pain is a common and debilitating symptom in patients with cirrhosis. Patients may have pain syndromes outside of their liver disease or may experience pain or discomfort that is disease-related, such as abdominal pain associated with ascites [3•]. Pain can be acute (12 weeks or less) or chronic and can be nociceptive, neuropathic, or musculoskeletal in origin. The pain management approach depends on individual factors, as well as the duration and type of pain experienced. Pain is best treated in a multimodal fashion, with the involvement of hepatologists, pharmacists, primary care doctors, and pain and palliative care specialists, and with the use of nonpharmacologic, pharmacologic, procedural, and behavioral treatments (Fig. 3).
Fig. 3.
Management of pain. A practical approach to pain management in patients with cirrhosis is demonstrated. Because pain management is complex in this patient population, a multidisciplinary approach should always be implemented, including specialists from various disciplines. In all kinds of pain (nociceptive, musculoskeletal, or neuropathic), underlying etiologies should be addressed, and non-pharmacologic options should be trialed. If medication is required, acetaminophen (≤ 2 g/day) can be successful in treating all types of pain and should be first-line. If not responsive to acetaminophen, neuropathic or nociceptive pain can be treated with gabapentin, pregabalin, SNRIs, or TCAs. Side effects, including sedation, should be monitored. If necessary, opioids can be used for short periods of time but should be titrated to the lowest effective dose. *NSAIDs, non-steroidal anti-inflammatory drugs; SNRIs, serotonin norepinephrine reuptake inhibitors; TCAs, tricyclic antidepressants
The first step in addressing any kind of pain experienced by patients with cirrhosis is to try to address its underlying etiology. If from ascites, for example, LVPs can be helpful. If pain is more generalized or not responsive to symptom-specific treatment, alternatives must be considered. Because of the altered bioavailability and metabolism of pain medications in cirrhosis, pain is often difficult to treat. Additionally, many patients with cirrhosis also have some degree of renal dysfunction, which can limit options further. For these reasons, non-pharmacologic therapies for all types of pain are often first-line and include physical therapy, ice/heat, massage, acupuncture, or cognitive behavioral therapy. Topical therapies such as lidocaine may help, especially for musculoskeletal pain.
Once medications are being used, acetaminophen (max dose of 2000 mg/day) is first line. For neuropathic pain, agents like pregabalin or gabapentin are typically trialed. NSAIDs such as ibuprofen should be avoided given the propensity to develop renal dysfunction or bleeding events [44, 45]. Tramadol used to be prescribed frequently in patients with cirrhosis given its low affinity for opioid receptors, partial inhibition of serotonin uptake, and because it was thought to result in less sedation, respiratory distress, and potential for tolerance. Now, it is generally avoided given its half-life doubles in patients with cirrhosis, it decreases the seizure threshold and has been associated with hypoglycemia [44]. Other potential medications that can help with both depression and pain in patients with cirrhosis, especially in those with nociceptive or neuropathic pain, include serotonin-norepinephrine reuptake inhibitors (SNRIs) [46] and tricyclic antidepressants [44], though the latter can be associated with anticholinergic side effects and altered mental status.
If opioids are necessary, low dose, short-acting ones given at longer dosing intervals should be started with uptitration as needed. Opioids, however, should not be used as part of a chronic pain management plan. Morphine is the preferred agent for those with eGFR ≥ 30 mL/min/1.73 m2, while hydromorphone is preferred for those with eGFR < 30 mL/min/1.73 m2. Intravenous fentanyl is also a good choice for those with cirrhosis given it is metabolized to nontoxic metabolites and no dose adjustments are needed for a single dose, however, intravenous medications are limited to the inpatient or hospice setting [47•]. Hydrocodone and oxycodone are metabolized via a different pathway that can result in more variability in serum levels and are thus less commonly used [44]. Transdermal patches are also avoided given a longer duration of action.
With the use of opioids, it is important to monitor carefully for the development of constipation or to even place patients on a prophylactic bowel regimen given constipation can exacerbate abdominal pain and symptoms or can worsen or lead to HE. Additionally, given shorter dosing intervals, with increasing doses, opioids can accumulate and lead to respiratory depression and worsening delirium or encephalopathy [48]. Some studies have even suggested patients with cirrhosis on opioids are at increased risk of hospitalization and readmission as well as increased graft failure and death [49, 50].
Depression and anxiety
As with the treatment of pain in cirrhosis, treatment of depression can also be challenging given altered drug metabolism and pharmacokinetic changes. Most prescribers feel that the safest class of anti-depressant drugs is selective serotonin reuptake inhibitors (SSRIs) [51]. These drugs usually have minimal and non-life-threatening side effects. SSRIs have a prolonged half-life and reduced drug clearance in cirrhosis, and thus, typically, patients are prescribed the same initial dose as healthy patients, but maintenance dosing may need to be reduced.
Though tricyclic antidepressants are sometimes used to manage pain, they are often used with caution in depression given the availability of other safer options and their adverse side effect profile, including anticholinergic symptoms, orthostatic hypotension, cardiac dysrhythmia, and neurological side effects [52]. If they are chosen, initial doses usually should not exceed 50% of standard starting doses [51]. Monoamine oxidase inhibitors (MAOIs) are also typically avoided in cirrhosis given their risk of inducing hepatocellular injury. Though in practice, bupropion is sometimes used, it can lower the seizure threshold and therefore should likely be avoided in those with alcohol-related liver disease and the potential for withdrawal seizures [53].
Appetite
Malnutrition is a significant predictor of morbidity and mortality in patients with cirrhosis and tends to worsen with the increasing severity of liver disease. Because the etiology of this condition is multifactorial, the optimal treatment is best administered by a multidisciplinary team.
Though patients usually intend to follow dietary recommendations, it is often difficult for them to do so. Many have a poor appetite, which can be attributed to a variety of liver-specific factors, including early satiety from ascites, HE, gastroparesis and autonomic dysfunction, taste change, and restricted diets (ex. low-sodium diet). When patients present with poor appetite, for example, it is important to diagnose any of these potential etiologies and to reverse them (ex. LVP for large volume ascites and treatment of gastroparesis). Additionally, protein supplement shakes are rarely covered by insurance and are expensive. Nutrition can be a source of conflict between patients and their caregivers and must be carefully navigated by the care team so as not to exacerbate this conflict. We recommend addressing this openly and discussing with both patients and caretakers the unique challenges that each face. In our experience, this discussion helps both sides realize that they share a common goal—for the patient to improve.
For patients who cannot achieve adequate oral intake, temporary enteral nutrition is recommended. Parenteral nutrition should be reserved for cases in which even enteral nutrition is not sufficient, or there are other contraindications to enteral feeding. A meta-analysis of 13 randomized control trials of nutrition therapy revealed benefits, including lower mortality and lower risks of encephalopathy and infection, though the trials had a high degree of bias [54]. Enteral and parenteral nutrition are appropriate for consideration in hospitalized patients, but at the end of life, reduced appetite is normal and should not be treated aggressively with supplementation, feeding tubes, or parenteral nutrition. Additionally, appetite stimulants are rarely effective. In the right setting, especially for patients with concomitant depression, mirtazapine can be trialed to increase appetite.
Data on supplementation with branched-chain amino acids (BCAAs) has been mixed. Decreased levels of BCAA are present in cirrhosis, and therefore, theoretically, supplementation could be of benefit. There have been several clinical trials demonstrating the benefit of BCAA supplementation with regard to improvement in nutritional status, liver function, HE, quality of life, and event-free survival, but adherence to supplementation is poor-moderate [55, 56]. EASL actually recommends long-term oral BCAA supplements in patients with advanced cirrhosis, especially when nitrogen intake is not achieved by oral diet [29]. Other reviews, however, have demonstrated their benefit only on hepatic encephalopathy symptoms [57]. Supplementation of other nutrients, including vitamins and trace metals, can be helpful given known deficiencies in patients with cirrhosis. Given their known deficiency in cirrhosis, supplementation of zinc and magnesium, in particular, have been linked to improvements in taste perception [58].
Fatigue
Fatigue, both neuromuscular and central, is also commonly experienced by patients with cirrhosis. While neuromuscular fatigue or weakness can be present, central fatigue resulting from changes in the central nervous system can be much more debilitating and is often closely tied with other symptoms like anxiety and depression. Often it can actually be difficult to distinguish fatigue from psychiatric symptoms or HE [59].
Fatigue in cirrhosis is closely related to sleep disturbances, which are present in a large portion of patients. Many patients with cirrhosis, especially those with a cholestatic disease like primary biliary cirrhosis, report excessive daytime sleepiness [60]. Others, with NAFLD, for example, may have concomitant obstructive sleep apnea [61]. The pathophysiology of sleep disturbances in cirrhosis is likely multifactorial. Decreased sleep latency, frequent awakenings, reduced total sleep time, decreased sleep efficiency, lower amounts of slow-wave sleep, and REM sleep have all been implicated [62]. Restless leg syndrome is another commonly reported disorder in cirrhosis and can impact sleep quality. Additionally, poorly timed medications, such as diuretics in the late afternoon or lactulose in the evening, could lead to frequent awakenings to use the bathroom. We recommend working with patients to optimize timing based on their natural sleep schedules.
At this point, much of the management of fatigue is supportive in nature. There is actually a validated algorithm known as TrACE that was developed to provide an approach to the treatment of fatigue in primary biliary cirrhosis but has been applied to other etiologies of liver disease as well [59]. This algorithm focuses on treating factors related to fatigue (ex. treating other medical or psychiatric comorbidities) and teaching patients how to better manage their fatigue (ex. avoiding shift work, exercising, maintaining social structures) [63]. Other nonpharmacologic treatments, including mindfulness-based stress reduction, have been evaluated for sleep disturbance in patients with cirrhosis. Studies found that mindfulness-based techniques reduced depression and improved quality of life and sleep quality [64].
There is little evidence for the pharmacologic treatment of fatigue, specifically, in liver disease. Treatment of encephalopathy, however, with lactulose or rifaximin has been demonstrated to improve sleep disturbances. There has been some suggestion that treatment with ondansetron, a 5-HT3 receptor antagonist [65], can lead to improvements in fatigue, but this has not been well validated and is not routinely employed. Treatment with modafinil in patients with PBC has been trialed, and while safe and well-tolerated, it has not been shown to be beneficial for fatigue [66]. The antihistamine drug, hydroxyzine, has also been trialed, and patients reported an improvement in sleep, but the use of this drug is limited given its sedating effects and potential for precipitating HE [67]. Zolpidem has additionally has been studied and was shown to be safe, effective, and well-tolerated among patients with Child-Turcotte-Pugh class A and B cirrhosis [68], but again, concerns remain about its sedating effects. Though it has not been studied extensively, several providers have reported the successful use of trazodone for sleep with minimal side effects [69]. Lastly, melatonin, a drug that has antioxidant effects and plays an important role in sleep disorders and sleep quality, has been shown to be effective in sleep disorders for patients with cirrhosis, though most patients studied were Child–Pugh class A or B. Further investigation is required to recommend for or against its use, especially in more severe diseases.
Conclusions
Given the morbidity associated with cirrhosis, interventions implemented require careful consideration of their impact on both mortality and quality of life. This review summarizes the main symptoms that patients with cirrhosis present with and suggests treatment algorithms for each. Not every treatment is perfect, and some treatments could exacerbate other symptoms or create new ones. Partnering with patients to ensure that their symptoms are addressed and goals prioritized should be the goal of every practicing gastroenterologist and hepatologist. Doing so can help improve the quality of life for those with cirrhosis.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
This article is part of the Topical Collection on Liver
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Centers for Disease Control and Prevention. CDC Wonder.
- 2.Younossi ZM, Boparai N, Price LL, Kiwi ML, McCormick M, Guyatt G. Health-related quality of life in chronic liver disease: the impact of type and severity of disease. Am J Gastroenterol. 2001;96:199–205. doi: 10.1111/j.1572-0241.2001.03956.x. [DOI] [PubMed] [Google Scholar]
- 3•.Waterman BL, Ramsey SU, Whitsett MP, et al. Top ten tips palliative care clinicians should know about end-stage liver disease. J Palliat Med. 2021;24(6):924–931. doi: 10.1089/jpm.2021.0097. [DOI] [PubMed] [Google Scholar]
- 4.Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4:1385–1394. doi: 10.1016/j.cgh.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Hansen L, Chang MF, Lee CS, et al. Physical and mental quality of life in patients with end-stage liver disease and their informal caregivers. Clin Gastroenterol Hepatol. 2021;19(1):155–161. doi: 10.1016/j.cgh.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6•.Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the study of liver diseases. Hepatology. 2021;74(2):1014–1048. doi: 10.1002/hep.31884. [DOI] [PubMed] [Google Scholar]
- 7.Morando F, Rosi S, Gola E, et al. Adherence to a moderate sodium restriction diet in outpatients with cirrhosis and ascites: a real-life cross-sectional study. Liver Int. 2015;35(5):1508–1515. doi: 10.1111/liv.12583. [DOI] [PubMed] [Google Scholar]
- 8.De Gottardi A, Thévenot T, Spahr L, et al. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol. 2009;7:906–909. doi: 10.1016/j.cgh.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 9.De Gottardi A, Thévenot T, Spahr L, et al. Risk of Complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol. 2009;7(8):906–909. doi: 10.1016/J.CGH.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Parker R. Role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Clin Liver Dis. 2014;18(2):319–334. doi: 10.1016/J.CLD.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 11•.Bureau C, Thabut D, Oberti F, et al. Transjugular intrahepatic portosystemic shunts with covered stents increase transplant-free survival of patients with cirrhosis and recurrent ascites. Gastroenterology. 2017;152:157–163. doi: 10.1053/j.gastro.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Yin X, Zhang F, Guo H, et al. A nomogram to predict the risk of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in cirrhotic patients. Sci Rep. 2020;10(1):1–8. doi: 10.1038/s41598-020-65227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forauer AR, McLean GK. Transjugular intrahepatic portosystemic shunt constraining stent for the treatment of refractory postprocedural encephalopathy: a simple design utilizing a Palmaz stent and Wallstent. J Vasc Interv Radiol. 1998;9(3):443–446. doi: 10.1016/S1051-0443(98)70296-9. [DOI] [PubMed] [Google Scholar]
- 14.Bai M, Qi X, Yang Z, et al. Predictors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in cirrhotic patients: a systematic review. J Gastroenterol Hepatol. 2011;26(6):943–951. doi: 10.1111/J.1440-1746.2011.06663.X. [DOI] [PubMed] [Google Scholar]
- 15.Nardelli S, Lattanzi B, Torrisi S, et al. Sarcopenia is risk factor for development of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt placement. Clin Gastroenterol Hepatol. 2017;15(6):934–936. doi: 10.1016/J.CGH.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 16.LaFond JP, Shah NL. Bursting with symptoms: a review of palliation of ascites in cirrhosis. Clin Liver Dis. 2016;8(1):10–12. doi: 10.1002/CLD.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macken L, Bremner S, Gage H, et al. Randomised clinical trial: palliative long-term abdominal drains vs large-volume paracentesis in refractory ascites due to cirrhosis. Aliment Pharmacol Ther. 2020;52(1):107–122. doi: 10.1111/apt.15802. [DOI] [PubMed] [Google Scholar]
- 18.Macken L, Hashim A, Mason L, Verma S. Permanent indwelling peritoneal catheters for palliation of refractory ascites in end-stage liver disease: a systematic review. Liver Int. 2019;39(9):1594–1607. doi: 10.1111/liv.14162. [DOI] [PubMed] [Google Scholar]
- 19.Cooper M, Pollard A, Pandey A, et al. Palliative long-term abdominal drains versus large volume paracentesis in refractory ascites due to cirrhosis (REDUCe Study): qualitative outcomes. J Pain Symptom Manage. 2021;62(2):312–325. doi: 10.1016/j.jpainsymman.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 20.Morando F, Maresio G, Piano S, et al. How to improve care in outpatients with cirrhosis and ascites: A new model of care coordination by consultant hepatologists. J Hepatol. 2013;59(2):257–264. doi: 10.1016/j.jhep.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Bloom PP, Ventoso M, Tapper E, Ha J, Richter JM. A Telemonitoring intervention for cirrhotic ascites management is cost-saving. Dig Dis Sci. 2021;1:1. doi: 10.1007/S10620-021-07013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gluud LL, Vilstrup H, Morgan MY. Nonabsorbable disaccharides for hepatic encephalopathy: a systematic review and meta-analysis. Hepatology. 2016;64(3):908–922. doi: 10.1002/hep.28598. [DOI] [PubMed] [Google Scholar]
- 23•.Duong N, Reuter B, Saraireh H, et al. Bowel movement frequency is not linked with cognitive function in cirrhosis. Clin Gastroenterol Hepatol. 2021 doi: 10.1016/J.CGH.2021.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362(12):1071–1081. doi: 10.1056/nejmoa0907893. [DOI] [PubMed] [Google Scholar]
- 25.Rifaximin. GoodRx.
- 26•.Jesudian AB, Ahmad M, Bozkaya D, Migliaccio-Walle K. Cost-effectiveness of rifaximin treatment in patients with hepatic encephalopathy. J Manag care Spec Pharm. 2020;26(6):750–757. doi: 10.18553/JMCP.2020.26.6.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katayama K, Katayama K, Kawaguchi T, et al. The prevalence and implication of zinc deficiency in patients with chronic liver disease. J Clin Med Res. 2018;10(5):437–444. doi: 10.14740/jocmr.v10i5.3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shen YC, Chang YH, Fang CJ, Lin YS. Zinc supplementation in patients with cirrhosis and hepatic encephalopathy: a systematic review and meta-analysis. Nutr J. 2019;18(1):1–9. doi: 10.1186/S12937-019-0461-3/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merli M, Berzigotti A, Zelber-Sagi S, et al. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70(1):172–193. doi: 10.1016/J.JHEP.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Plank LD, Gane EJ, Peng S, et al. Nocturnal nutritional supplementation improves total body protein status of patients with liver cirrhosis: a randomized 12-month trial. Hepatology. 2008;48(2):557–566. doi: 10.1002/HEP.22367. [DOI] [PubMed] [Google Scholar]
- 31.Córdoba J, López-Hellín J, Planas M, et al. Normal protein diet for episodic hepatic encephalopathy: results of a randomized study. J Hepatol. 2004;41(1):38–43. doi: 10.1016/J.JHEP.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 32.Maharshi S, Sharma BC, Sachdeva S, Srivastava S, Sharma P. Efficacy of nutritional therapy for patients with cirrhosis and minimal hepatic encephalopathy in a randomized trial. Clin Gastroenterol Hepatol. 2016;14(3):454–460.e3. doi: 10.1016/J.CGH.2015.09.028. [DOI] [PubMed] [Google Scholar]
- 33.Jones EA, Bergasa N. Evolving concepts of the pathogenesis and treatment of the pruritus of cholestasis. Can J Gastroenterol. 2000;14(1):33–39. doi: 10.1155/2000/747495. [DOI] [PubMed] [Google Scholar]
- 34.Kremer AE, Martens JJWW, Kulik W, et al. Lysophosphatidic acid is a potential mediator of cholestatic pruritus. Gastroenterology. 2010;139(3):1008–18. doi: 10.1053/J.GASTRO.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 35.Xander C, Meerpohl JJ, Galandi D, et al. Pharmacological interventions for pruritus in adult palliative care patients. Cochrane Database Syst Rev. 2013;9(6):CD008320. doi: 10.1002/14651858.CD008320.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Kumada H, Miyakawa H, Muramatsu T, et al. Efficacy of nalfurafine hydrochloride in patients with chronic liver disease with refractory pruritus: a randomized, double-blind trial. Hepatol Res. 2017;47(10):972–982. doi: 10.1111/HEPR.12830. [DOI] [PubMed] [Google Scholar]
- 37.Moller P, Bergstrom J, Furst P, Hellstrom K. Muscle biopsy studies in patients with moderate liver cirrhosis with special reference to energy-rich phosphagens and electrolytes. Scand J Gastroenterol. 1984;19:267–272. doi: 10.1080/00365521.1984.12005719. [DOI] [PubMed] [Google Scholar]
- 38.Takeuchi M, Low PA. Dynamic peripheral nerve metabolic and vascular responses to exsanguination. Am J Physiol - Endocrinol Metab. 1987;253(4):349–353. doi: 10.1152/ajpendo.1987.253.4.e349. [DOI] [PubMed] [Google Scholar]
- 39.Angeli P, Albino G, Carraro P, et al. Cirrhosis and muscle cramps: evidence of a causal relationship. Hepatology. 1996;23(2):264–273. doi: 10.1002/hep.510230211. [DOI] [PubMed] [Google Scholar]
- 40.Henry ZH, Northup PG. Baclofen for the treatment of muscle cramps in patients with cirrhosis: a new alternative. Hepatology. 2016;64(2):695–696. doi: 10.1002/hep.27988. [DOI] [PubMed] [Google Scholar]
- 41.Vidot H, Cvejic E, Carey S, et al. Randomised clinical trial: oral taurine supplementation versus placebo reduces muscle cramps in patients with chronic liver disease. Aliment Pharmacol Ther. 2018;48(7):704–712. doi: 10.1111/apt.14950. [DOI] [PubMed] [Google Scholar]
- 42.Lee FY, Lee SD, Te TY, et al. A randomized controlled trial of quinidine in the treatment of cirrhotic patients with muscle cramps. J Hepatol. 1991;12:236–240. doi: 10.1016/0168-8278(91)90944-7. [DOI] [PubMed] [Google Scholar]
- 43.Chatrath H, Liangpunsakul S, Ghabril M, Otte J, Chalasani N, Vuppalanchi R. Prevalence and morbidity associated with muscle cramps in patients with cirrhosis. Am J Med. 2012;125(10):1019. doi: 10.1016/J.AMJMED.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chandok N, Watt KDS. Pain management in the cirrhotic patient: the clinical challenge. Mayo Clin Proc. 2010;85:451–458. doi: 10.4065/mcp.2009.0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilcock A, Charlesworth S, Prentice W, et al. Prescribing in chronic severe hepatic impairment. J Pain Symptom Manage. 2019;58:515–537. doi: 10.1016/j.jpainsymman.2019.04.034. [DOI] [PubMed] [Google Scholar]
- 46.Rakoski M, Goyal P, Spencer-Safier M, Weissman J, Mohr G, Volk M. Pain management in patients with cirrhosis. Clin Liver Dis. 2018;11(6):135. doi: 10.1002/cld.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47•.Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis - a practical guide. Aliment Pharmacol Ther. 2013;37(12):1132–1156. doi: 10.1111/APT.12324. [DOI] [PubMed] [Google Scholar]
- 48.Moon AM, Jiang Y, Rogal SS, Tapper EB, Lieber SR, Barritt AS. Opioid prescriptions are associated with hepatic encephalopathy in a national cohort of patients with compensated cirrhosis. Aliment Pharmacol Ther. 2020;51:652–660. doi: 10.1111/apt.15639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tapper EB, Henderson JB, Parikh ND, Ioannou GN, Lok AS. Incidence of and risk factors for hepatic encephalopathy in a population-based cohort of Americans with cirrhosis. Hepatol Commun. 2019;3:1510–1519. doi: 10.1002/hep4.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Randall HB, Alhamad T, Schnitzler MA, et al. Survival implications of opioid use before and after liver transplantation. Liver Transplant. 2017;23:305–314. doi: 10.1002/lt.24714. [DOI] [PubMed] [Google Scholar]
- 51.Mullish BH, Kabir MS, Thursz MR, Dhar A. Review article: depression and the use of antidepressants in patients with chronic liver disease or liver transplantation. Aliment Pharmacol Ther. 2014;40(8):880–892. doi: 10.1111/APT.12925. [DOI] [PubMed] [Google Scholar]
- 52.Surman OS, Cosimi AB, Dimartini A. Psychiatric care of patients undergoing organ transplantation. Transplantation. 2009;87(12):1753–1761. doi: 10.1097/TP.0B013E3181A754D4. [DOI] [PubMed] [Google Scholar]
- 53.Schlatter C, Egger SS, Tchambaz L, Krhenbhl S. Pharmacokinetic changes of psychotropic drugs in patients with liver disease: implications for dose adaptation. Drug Saf. 2009;32(7):561–578. doi: 10.2165/00002018-200932070-00003. [DOI] [PubMed] [Google Scholar]
- 54.Fialla AD, Israelsen M, Hamberg O, Krag A, Gluud LL. Nutritional therapy in cirrhosis or alcoholic hepatitis: a systematic review and meta-analysis. Liver Int. 2015;35(9):2072–2078. doi: 10.1111/LIV.12798. [DOI] [PubMed] [Google Scholar]
- 55.Muto Y, Sato S, Watanabe A, et al. Effects of oral branched-chain amino acid granules on event-free survival in patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2005;3(7):705–713. doi: 10.1016/S1542-3565(05)00017-0. [DOI] [PubMed] [Google Scholar]
- 56.Marchesini G, Bianchi G, Merli M, et al. Nutritional supplementation with branched-chain amino acids in advanced cirrhosis: a double-blind, randomized trial. Gastroenterology. 2003;124(7):1792–1801. doi: 10.1016/S0016-5085(03)00323-8. [DOI] [PubMed] [Google Scholar]
- 57.Gluud LL, Dam G, Les I, et al. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane database Syst Rev. 2017;5(5):CD001939. doi: 10.1002/14651858.CD001939.PUB4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Palmer LB, Kuftinec G, Pearlman M, Green CH. Nutrition in Cirrhosis. Curr Gastroenterol Rep. 2019 doi: 10.1007/s11894-019-0706-5. [DOI] [PubMed] [Google Scholar]
- 59.Swain MG, Jones DEJ. Fatigue in chronic liver disease: new insights and therapeutic approaches. Liver Int. 2018 doi: 10.1111/liv.13919. [DOI] [PubMed] [Google Scholar]
- 60.Newton JL, Gibson GJ, Tomlinson M, Wilton K, Jones D. Fatigue in primary biliary cirrhosis is associated with excessive daytime somnolence. Hepatology. 2006;44(1):91–98. doi: 10.1002/HEP.21230. [DOI] [PubMed] [Google Scholar]
- 61.Ahmed MH, Byrne CD. Obstructive sleep apnea syndrome and fatty liver: association or causal link? World J Gastroenterol. 2010 doi: 10.3748/wjg.v16.i34.4243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bruyneel M, Sersté T. Sleep disturbances in patients with liver cirrhosis: prevalence, impact, and management challenges. Nat Sci Sleep. 2018;10:369. doi: 10.2147/NSS.S186665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jopson L, Dyson JK, Jones DEJ. Understanding and treating fatigue in primary biliary cirrhosis and primary sclerosing cholangitis. Clin Liver Dis. 2016;20(1):131–142. doi: 10.1016/J.CLD.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 64.Bajaj JS, Ellwood M, Ainger T, et al. Mindfulness-based stress reduction therapy improves patient and caregiver-reported outcomes in cirrhosis. Clin Transl Gastroenterol. 2017;8(7):e108. doi: 10.1038/CTG.2017.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Piche T, Vanbiervliet G, Cherikh F, et al. Effect of ondansetron, a 5-HT3 receptor antagonist, on fatigue in chronic hepatitis C: a randomised, double blind, placebo controlled study. Gut. 2005;54(8):1169–1173. doi: 10.1136/GUT.2004.055251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Silveira MG, Gossard AA, Stahler AC, et al. A randomized, placebo-controlled clinical trial of efficacy and safety: modafinil in the treatment of fatigue in patients with primary biliary cirrhosis. Am J Ther. 2017;24(2):e167–e176. doi: 10.1097/MJT.0000000000000387. [DOI] [PubMed] [Google Scholar]
- 67.Spahr L, Coeytaux A, Giostra E, Hadengue A, Annoni JM. Histamine H1 blocker hydroxyzine improves sleep in patients with cirrhosis and minimal hepatic encephalopathy: a randomized controlled pilot trial. Am J Gastroenterol. 2007;102(4):744–753. doi: 10.1111/J.1572-0241.2006.01028.X. [DOI] [PubMed] [Google Scholar]
- 68.Sharma MK, Kainth S, Kumar S, et al. Effects of zolpidem on sleep parameters in patients with cirrhosis and sleep disturbances: a randomized, placebo-controlled trial. Clin Mol Hepatol. 2019;25(2):199. doi: 10.3350/CMH.2018.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ge PS, Runyon BA. Treatment of patients with cirrhosis. N Engl J Med. 2016;375(8):767–777. doi: 10.1056/NEJMRA1504367. [DOI] [PubMed] [Google Scholar]