Abstract
Objective
To examine the responsiveness of primary care providers to pro‐social and financial incentives to participate in a learning collaborative for the treatment of opioid use disorder (OUD).
Study setting
We conducted a statewide experiment in North Carolina from January 2019 to November 2019 to expand access to support for providers learning to treat opioid use disorder using different types of messaging and incentives.
Study design
We randomly assigned 15,835 primary care providers (physicians, nurse practitioners, and physician assistants) in North Carolina (NC) to receive one of four letters recruiting providers to participate in an online learning collaborative for providers learning to treat opioid use disorder. The four versions of the recruitment letters contained either pro‐social messaging, mention of financial reimbursement for time spent in the learning collaborative, both, or neither.
Data collection
We created a primary data source, tracking provider responses to the recruitment letters and emails.
Principal findings
We found a 47.5% greater (p < 0.05) response rate using pro‐social recruitment messaging that provided a greater description of the local conditions in each provider's region compared to the control group; this effect increased with higher overdose opioid death rates. Mention of financial reimbursement only modestly increased provider response rates. Some heterogeneity was observed by provider type, with NPs having the largest response to pro‐social messaging.
Conclusions
Prosocial nudges had strong effects on efforts to enhance the behavioral health workforce in NC through participation in an ECHO for medication‐assisted treatment (MAT) learning collaborative. The prosocial approach can and should be employed by states and professional societies in their efforts to create training programs for medication for OUD (MOUD), in order to expand access to lifesaving treatments for opioid use disorder.
Keywords: opioid use disorder, pro‐social messaging, randomized trial, workforce
What is known on this topic
Numerous barriers exist in creating an adequate support of providers comfortable with and able to provide treatments for opioid use disorder.
Understanding how to encourage provider participation in training is a key to increase the supply of qualified providers capable of addressing the opioid overdose epidemic.
Few studies have applied behavioral economic insights to encourage the greater provision of care for addressing public health needs, and to our knowledge, no studies have explored the use of monetary incentives or behavioral nudges to address the shortage of providers needed to address the opioid epidemic.
What this study adds
This is the first statewide randomized trial assessing primary care providers' response to pro‐social and reimbursement messaging.
We find a relatively large effect of pro‐social messaging in recruitment letters inviting primary care providers to participate in an online learning collaborative focused on treatment for opioid use disorder.
We found that recruitment letters including a mention of potential financial reimbursement for participation only modestly improved provider response.
1. INTRODUCTION
Between 1999 and 2019, almost 450,000 people in the United States died from opioid overdoses 1 and the provisional drug overdose death rates for 2020 show large increases in fatal drug overdoses during the COVID‐19 pandemic. 2 1.6 million Americans have an opioid use disorder (OUD) 3 but less than one‐fifth of those with OUD are estimated to receive one of three evidence‐based medication treatments for OUD – buprenorphine, methadone, and naltrexone. 4 , 5
Expanding access to medications for OUD (MOUD) may be vital to addressing the opioid epidemic, yet the supply of providers qualified to administer MOUD is severely limited. 6 The shortage of MOUD providers is especially critical in rural areas, which rely more heavily on primary care providers for behavioral health treatment than urban areas. 7
In light of the OUD treatment provider shortage, primary care providers have the potential to play a significant role in stemming the tide of rising overdose deaths by providing MOUD in their offices. 8 , 9 , 10 Research suggests that primary care providers can safely deliver buprenorphine–naloxone, even in sites that lack specialized resources, 11 and that the quality of care provided by primary care providers is equivalent to that provided by behavioral health specialists. 12 To be qualified as a MOUD provider, a physician must pass an 8‐h course to obtain a waiver of the Drug Addiction Treatment Act of 2000 (DATA 2000) that allows them to prescribe medications for the treatment of opioid addiction in an office‐based setting. The waiver requirement is currently under review by the US DHHS for physicians who prescribe to a small number of patients, but the policy change is still awaiting publication in the Federal Register in order to be effective. 13 Advanced practitioners, including nurse practitioners (NPs) and physician assistants (PAs), were only given prescription authority for office‐based opioid addiction treatment in the 2016 Comprehensive Addiction and Recovery Act on November 17, 2016, 14 yielding a large group of primary care professionals in need of support as they begin to initiate medication treatments for opioid use disorders. Training requirements for advance practitioners are greater than for physicians, with 24 hr of training required.
We now know that DATA 2000 waiver training alone is not enough to facilitate prescribing for people with OUD seeking treatment; an estimated 40% of waivered physicians have never prescribed MOUD. 1 Lack of prescribing is due to a complex set of barriers, including lack of institutional resources and support to facilitate development as MOUD prescribers. 15 , 16 , 17 , 18
Learning collaboratives such as the ECHO model, which originated at the University of New Mexico, are evidence‐based approaches for providing support to primary care providers in new areas of practice through participation in videoconference sessions. 19 The ECHO model is a hub‐and‐spoke learning collaborative model, with the “hub” comprised of content and process experts who create content for didactic training and provide expertise for de‐identified case presentations. The spokes are members of the health care workforce seeking additional training and support. Because the approach requires only an internet connection and a computer with a video camera, it is especially well suited for providers in rural areas, or those under stay‐at‐home restrictions or furloughs, who may not have access to a network of specialists or other primary care providers experienced in MOUD implementation. The ECHO model has growing evidence base 20 comparing it favorably to standard referral approaches to care. 21
UNC ECHO for medication‐assisted treatment (MAT) was developed to provide primary care providers statewide in North Carolina with resources to support the treatment of OUD that their practices may lack, using a collaborative training infrastructure. 20 However, only a small minority of providers in the state had participated in the learning collaborative and the vast majority are still lacking their DEA waiver. 22 Figuring out how to encourage provider participation in MOUD training is a key to increasing the supply of qualified providers capable of addressing the opioid overdose epidemic.
One effective strategy to increase participation may be the use of direct monetary incentives for participation. Monetary incentives are an often‐used strategy to promote health care innovations. Yet a robust finding in behavioral economics is that traditional monetary incentives can be ineffective—or even counter‐productive—depending on how incentives are structured, who is being incented, and for what purpose. 23 , 24 Possibly most relevant for understanding how to encourage provider engagement to address the opioid epidemic is that monetary incentives for pro‐social tasks, or tasks seen as benefiting society as a whole at some cost to the individual, can reduce engagement by crowding‐out pro‐social motivation. 23 , 25 , 26 For pro‐social tasks, informational “nudges” such as presenting choices in a way that appeals to social needs, may be more effective. To date, few studies have applied behavioral economic insights to encourage greater provision of care for addressing public health needs, 27 and to our knowledge, no studies have explored the use of monetary incentives or behavioral nudges to address the shortage of providers needed to address the opioid epidemic. In order to address this gap in the literature, we conducted a randomized controlled trial of primary care providers to examine whether pro‐social messaging, with or without mention of financial reimbursement, affects rates of participation in an OUD learning collaborative.
2. METHODS
2.1. Study design
We obtained lists of all active, licensed providers from the North Carolina Medical Board and Board of Nursing. We randomly assigned the 15,835 primary care providers in North Carolina, including physicians, NPs, and PAs, to receive one of four letters recruiting providers to participate in UNC's ECHO for MAT. We randomized at the practice level and stratified by North Carolina's 100 counties. We initially focused on 22 counties with opioid overdose death rates greater than the US average in 2017 and sent both snail‐mail recruitment letters as well as identical email letters when the email address was available. We quickly expanded efforts to all 100 NC counties and relied on email recruitment only. 28 The four versions of the recruitment letters are described by two binary dimensions and contain either a pro‐social recruitment approach for participating in the UNC ECHO for MAT intervention or standard recruitment practice; 50% of which also contained a mention of potential reimbursement for time spent in the learning collaborative. Assignment to pro‐social arm, provided information customized specifically to each provider's county in terms of the latest statistics available on the prevalence and consequences of opioid overdoses, and the number of providers per population in that community currently waiver‐trained to provide MOUD. The control arm included a standard approach to recruitment that did not contain a pro‐social recruitment message.
Before recruitment, the study team piloted alternative versions of the pro‐social messaging materials developed based on evidence from behavioral economics. The study arms were balanced in the timing of mailed and emailed recruitment letters. Figure 1 displays a sample recruitment letter that has both the pro‐social approach, demonstrated by the box on the right side of the letter that contains county‐specific estimates, as well as a mention of monetary support being available in the blue font toward the bottom of the letter.
FIGURE 1.
Sample recruitment letter. This is an example of a pro‐social letter with monetary support mentioned [Color figure can be viewed at wileyonlinelibrary.com]
We monitored the rate of response by providers through the recruitment process, measured by provider calls to the recruitment phone line set up for ECHO for MAT, or via email response. Providers responding to the recruitment materials were invited to participate in the study and were sent a web‐based consent form and baseline survey.
2.2. Analysis methods
We analyzed data from 15,835 providers from just under 8000 practices across the four types of primary care professionals (Table 1). We compared response rates by study arms using linear models with county‐level fixed effects to adjust for county‐level stratification. To account for the clustered experimental design, we follow recommended practice and estimated cluster‐robust standard errors using the Liang–Zeger (1986) cluster adjustment 29 by practice. 30 We examined the rate of response by the treatment arm compared to the control arm (without either type of messaging). We obtained similar results from both linear and logit models but report the average marginal effects from the linear models since the county‐fixed effects resulted in perfect prediction for many small counties in logit models, reducing sample size. We ran models with and without controls for provider type and also ran regressions separately by the three provider types (physicians, NPs, and PAs). Because of the modest sample size, we use p < 0.10 to determine statistical significance although the “sample” represents the population of active, licensed providers in NC. In order to determine whether providers are more likely to take up training in counties with greater needs, we rank counties according to their opioid overdose death rate, and graph the cumulative number of respondents by county ranking.
TABLE 1.
Summary statistics in the full sample and by experimental group
| Overall | By experimental group | ||||
|---|---|---|---|---|---|
| Control | Compensation, not prosocial | No compensation, prosocial | Compensation, prosocial | ||
| Provider type | |||||
| MD or DO | 51.5% | 50.0% | 53.1% | 50.5% | 52.7% |
| Nurse practitioner | 34.4% | 36.1% | 33.4% | 35.1% | 32.7% |
| Physician assistant | 14.1% | 13.9% | 13.5% | 14.4% | 14.6% |
| Rural county | 18.8% | 16.4% | 18.7% | 19.5% | 20.9% |
| County population (1000s) | 358 (8.3) | 371.9 (17.2) | 347.1 (12.4) | 368.7 (20.3) | 341.9 (14.1) |
| Opioid overdose deaths per 100,000 population (2017) | 20.7 (0.4) | 19.8 (0.7) | 20.7 (0.7) | 20.4 (0.8) | 22.1 (0.8) |
| Total deaths from opioid overdoses, 2013–2017 | 172.1 (3.3) | 180.1 (6.7) | 166.9 (5.0) | 173.5 (8.2) | 166.9 (5.6) |
| Sample size | |||||
| Providers | 15,835 | 4150 | 3871 | 4121 | 3693 |
| Medical practices | 7994 | 2002 | 1994 | 1998 | 2000 |
Note: Standard deviations of continuous covariates are in parentheses.
Abbreviations: DO, Doctor of Osteopathy; MD, Doctor of Medicine.
3. RESULTS
The sample is made up of 52% physicians, 34% NPs, and 14% PAs. Nineteen percent of the sample were from rural counties in NC (Table 1). On average, providers were from counties with just under 21 overdose deaths per 100,000 population. The average county population was 358,000 residents, and the average overdose death rate was 20 per 100,000 residents in 2017, and 172 per 100,000 over the 5 years from 2013 to 2017.
In the control group, 36 out of 4150 or just under 8.7 providers per 1000 responded to recruitment emails. The response rate varied substantially by provider type, with NPs and PAs more likely to respond (11.4/1000 and 10.4/1000, respectively) than physicians (6.3/1000). Unadjusted response rates were greatest in the pro‐social plus compensation arm (44 out of 3693 or 11.9/1000), followed closely by the pro‐social no compensation arm (44 out of 4121 or 10.7/1000). Responses to the non pro‐social arm without compensation, were lowest (36 out of 3871 or 9.3/1000).
The multivariate models show that all three active study arms had a greater response rate than the control arm, although only the pro‐social/compensation arm had a statistically significant increase in response over the control arm (Table 2). In relative terms, providers who were recruited with both prosocial messaging and financial compensation had a 47.5% greater response rate than the control arm (=4.12/8.67), while those recruited with prosocial messaging alone had a 27% (=2.3/8.67) greater response rate. Providers receiving only financial messaging had only a 6% (=0.52/8.67) higher response rate than the recruitment as usual arm. We did not observe a difference in response rates in urban versus rural counties (not reported).
TABLE 2.
Effects of nudge letters versus the control group for the full sample and by provider type
| Overall | By provider type | |||
|---|---|---|---|---|
| MD/DO | NP | PA | ||
| Average treatment effects by treatment arm | ||||
| Compensation, no pro‐social letter | 0.52 | 1.01 | 0.05 | −4.00 |
| No compensation, pro‐social letter | 2.3 | 2.44 | 4.41 | −3.04 |
| Compensation, pro‐social letter | 4.12** | 4.57* | 7.39* | −5.01 |
| Response rate in control group | 8.67 | 6.26 | 11.35 | 10.42 |
Note: Table shows estimated effects of letter types in responses per 1000 providers. All estimates are adjusted for county (randomization strata) fixed effects. Effects in the full sample (first “Overall” column) are additionally adjusted for provider type. One‐sided p‐values: *p < 0.10; **p < 0.05.
Abbreviations: DO, Doctor of Osteopathy; MD, Doctor of Medicine; NP, Nurse Practitioner; PA, Physician Assistant.
Source: Authors' analysis.
When we ran separate models by provider type (Columns 2–4 of Table 1), we see that both physicians and NPs respond most to the prosocial/compensation letter, but the NP response is much larger, representing a 61% increase over the physician response rate. Although PAs had a similarly high response rate in the control arm as NPs, we find that the addition of messaging had no effect for this type of provider.
Figure 2 shows the cumulative number of responses by treatment group over counties ranked by opioid overdose death rates in 2017, with 1 being the lowest county death rate and 100 being the county with the highest death rate. This figure shows that as you move from counties with lower death rates (left) to counties with higher death rates (right), the number of cumulative responses to the prosocial arms clearly diverges from the number of responses in the arms without prosocial messaging (control and financial only). This result would be directly tied to the explicit information on county opioid overdose deaths in the pro‐social version of the recruitment letter. Figure 2 also shows the additional separation between the pro‐social messaging arm with and without financial compensation that occurs in counties ranked in the higher percentiles of opioid overdose deaths.
FIGURE 2.
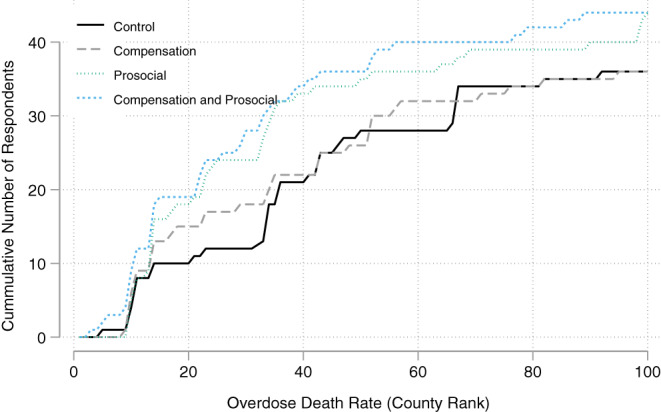
Response rate by county rankings by 2017 opioid overdose death rates. This figure shows the cumulative number of responses by treatment group over counties ranked by opioid overdose death rates in 2017, with 1 being the lowest county death rate and 100 being the county with the highest death rate. Source: Authors' analysis of study data [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
We highlight a number of important conclusions from this work. First, nudges and incentives had strong effects on efforts to enhance the behavioral health workforce in NC through participation in an ECHO for MAT learning collaborative. The large relative effects by different recruitment approaches, ranging from a 6% increase in the response rate for recruitment letters only mentioning financial compensation to a 48% relative increase using both pro‐social messaging together with financial compensation, can and should be employed by states and professional societies in their efforts to create training programs, whether for MAT or possibly other clinical areas.
In particular, the combination of pro‐social messaging using customized regional statistics describing the magnitude of the opioid overdose epidemic by county and the mention of funding to support providers' time in training maximized the response rate to recruitment. Given the modest additional costs of compiling and inserting county‐level statistics into the recruitment letters, the pro‐social messaging approach appears to be a highly cost‐effective strategy. In NC, with about 16,000 primary care providers, the estimated effect of prosocial messaging would translate to about 66 additional providers responding to the invitation. Under fairly optimistic assumptions, if even half of this group receives a waiver and treats the initial 30 allotted patients, this would result in 989 additional people receiving OUD treatment for the modest cost of adding pro‐social information to the invitation. Even if funding is not available for provider participation, pro‐social messaging without mention of compensation provided a 27% greater response rate than control arm letters that omitted pro‐social messaging.
The effects of pro‐social messaging and the joint pro‐social messaging and compensation letter are both relatively large for “nudging” generally. A recent systematic review of the nudging interventions—defined as any change to the choice architecture designed to alter behavior without forbidding any options or significantly changing economic incentives—found that the median effect size in any context was 21% overall and 21% in the area of health. 33 The finding of complementarity between pro‐social messaging and financial compensation is also a unique contribution to the literature on nudging as few studies have explored the interaction of different types of nudges or the interaction of nudging with more traditional economic incentives. While we are unaware of existing experiments testing the interaction of pro‐social nudges and financial compensation, our findings are in line with theoretical findings suggesting that effects may be larger for policies doing both as they affect different types of individuals. 34
Another important finding from this study was the difference in the response to recruitment approaches by provider types. NPs and PAs both responded at higher levels in the control arm than did physicians. NPs were much more responsive to both pro‐social messaging approaches than were physicians. The differences in the response to the different messaging approaches between NPs and PAs are striking. Both are advanced practitioners who were much more recently granted authority to prescribe office‐based outpatient treatments for OUD through CARA in late 2016. We had hypothesized that this would create a greater demand for additional training and support for both types of providers, given that many had completed professional training prior to the implementation of this expanded authority. However, only NPs exhibited substantially higher response rates to the ECHO learning collaborative invitations as well as greater response to pro‐social messaging in recruitment letters. While our study does not allow us to examine the reason for difference, the orientation of nurses toward more holistic rather than disease‐based care may be one of the factors driving this difference. 35 Another difference may be related to the relative professional independence NPs enjoy beyond that which is afforded to PAs. While this study did not test or account for those professional scope of practice or any actual or perceived practice orientation variances, the difference in response by these two categories of mid‐level professionals was notable and may deserve further investigation. Other research has found higher rates of waiver participation among NPs than PAs and substantial variation by provider characteristics such as gender and race. 22 The difference is unlikely to be driven by the opportunity costs of participation in the learning collaborative, since the median incomes for PAs are similar to those for NPs. 36
In April 2021, the Department of Health and Human Services confirmed a process to waiving the training required to prescribe buprenorphine to fewer than 30 patients with opioid use disorder. This policy is considerably weaker than the elimination of the “x‐waiver,” which has been a goal of policy advocates for years may be one important step toward the expansion of treatments available to individuals with OUD. The removal of the training requirement does not mitigate the need for additional supports for providers newly prescribing MOUD, such as through the learning collaborative approach used in this study.
These results should be interpreted in light of several limitations. This study reports the results from one state and may not be generalizable to other states. The target lists of NC providers may have omitted providers without active email addresses or may otherwise be incomplete. Response rates were low but likely would have been higher if we had been able to limit the sample to those providers with interests in treating people with OUD. Responses rates to unsolicited emails have been shown in other settings to also be low, ranging from 6.1% to 44% for surveys, which require a substantially lower time commitment than participation in an ongoing learning collaborative. 37 , 38
We believe this is the largest experiment of provider recruitment approaches to enhance the workforce able to address the opioid crisis ever conducted. The findings from this study should be useful to other states attempting to increase participation in training and possibly for other provider recruitment contexts.
ACKNOWLEDGMENTS
We are grateful for support from NIDA (R21‐DA047286) for this study. We also acknowledge additional support from Agency for Healthcare Research and Quality and NC DHHS for the ECHO for MAT study. We are grateful for project management support from Dawn Bergmire and Kristen Jarman, and research assistance by Lexie Grove.
Domino ME, Sylvia S, Green S. Nudging primary care providers to expand the opioid use disorder workforce. Health Serv Res. 2022;57(2):403-410. doi: 10.1111/1475-6773.13894
Funding information National Institute on Drug Abuse (one of the NIH Institutes), Grant/Award Number: R21DA0472862; Agency for Healthcare Research and Quality; NC DHHS
REFERENCES
- 1. Opioid Data Analysis and Resources . Drug overdose. CDC injury center. Published January 25, 2021. Accessed March 4, 2021. https://www.cdc.gov/drugoverdose/data/analysis.html
- 2. Products ‐ Vital statistics rapid release ‐ Provisional drug overdose data. Published July 9, 2021. Accessed July 20, 2021. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- 3. McCance‐Katz EF. The National Survey on Drug Use and Health. 2019.
- 4. 2019 NSDUH detailed tables. CBHSQ data. Accessed March 4, 2021. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables
- 5. Comer S, Cunningham C, Fishman MJ, et al. National practice guideline for the use of medications in the treatment of addiction involving opioid use. Published Online 2015, 66.
- 6. Jones CM, Campopiano M, Baldwin G, McCance‐Katz E. National and state treatment need and capacity for opioid agonist medication‐assisted treatment. Am J Public Health. 2015;105(8):e55–e63. doi: 10.2105/AJPH.2015.302664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosenblatt RA, Andrilla CHA, Catlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13(1):23‐26. doi: 10.1370/afm.1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mannelli P, Wu L‐T. Primary care for opioid use disorder. Subst Abus Rehabil. 2016;7:107‐109. doi: 10.2147/SAR.S69715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saitz R, Daaleman TP. Now is the time to address substance use disorders in primary care. Ann Fam Med. 2017;15(4):306‐308. doi: 10.1370/afm.2111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Loxterkamp D. Medication‐assisted treatment should be part of every family physician's practice: yes. Ann Fam Med. 2017;15(4):309‐310. doi: 10.1370/afm.2103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mintzer IL, Eisenberg M, Terra M, MacVane C, Himmelstein DU, Woolhandler S. Treating opioid addiction with buprenorphine‐naloxone in community‐based primary care settings. Ann Fam Med. 2007;5(2):146‐150. doi: 10.1370/afm.665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gertner AK, Robertson AG, Powell BJ, Jones H, Silberman P, Domino ME. Primary care providers and specialists deliver comparable buprenorphine treatment quality. Health Aff. 2020;39(8):1395‐1404. doi: 10.1377/hlthaff.2019.01559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Division N . HHS expands access to treatment for opioid use disorder. HHS.gov. Published January 14, 2021. Accessed March 4, 2021. https://www.hhs.gov/about/news/2021/01/14/hhs-expands-access-to-treatment-for-opioid-use-disorder.html
- 14. ASAM . Nurse practitioners and physician assistants prescribing buprenorphine. Accessed January 29, 2018. https://asam.org/resources/practice‐resources/nurse‐practitioners‐and‐physician‐assistants‐prescribing‐buprenorphine
- 15. Walley AY, Alperen JK, Cheng DM, et al. Office‐based management of opioid dependence with buprenorphine: clinical practices and barriers. J Gen Intern Med. 2008;23(9):1393‐1398. doi: 10.1007/s11606-008-0686-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hutchinson E, Catlin M, Andrilla CHA, Baldwin L‐M, Rosenblatt RA. Barriers to primary care physicians prescribing buprenorphine. Ann Fam Med. 2014;12(2):128‐133. doi: 10.1370/afm.1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andrilla CHA, Coulthard C, Larson EH. Barriers rural physicians face prescribing buprenorphine for opioid use disorder. Ann Fam Med. 2017;15(4):359‐362. doi: 10.1370/afm.2099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huhn AS, Dunn KE. Why aren't physicians prescribing more buprenorphine? J Subst Abus Treat. 2017;78:1‐7. doi: 10.1016/j.jsat.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Korthuis PT, McCarty D, Weimer M, et al. Primary care‐based models for the treatment of opioid use disorder: a scoping review. Ann Intern Med. 2017;166(4):268‐278. doi: 10.7326/M16-2149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shea CM, Gertner AK, Green SL. Barriers and perceived usefulness of an ECHO intervention for office‐based buprenorphine treatment for opioid use disorder in North Carolina: a qualitative study. Subst Abus. 2021;42(1):54‐64. doi: 10.1080/08897077.2019.1694617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199‐2207. doi: 10.1056/NEJMoa1009370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Grove LR, Rao N, Spero J, Fraher E, Domino ME. Which providers obtain DATA 2000 waivers for opioid use disorder treatment? Working paper (under review).
- 23. Kamenica E. Behavioral economics and psychology of incentives. Annu Rev Econom. 2012;4(1):427‐452. doi: 10.1146/annurev-economics-080511-110909 [DOI] [Google Scholar]
- 24. Miller G, Babiarz KS. Pay‐for‐performance incentives in low‐ and middle‐income country health programs. 2013. NBER Working paper 18932. https://www.nber.org/system/files/working_papers/w18932/w18932.pdf
- 25. Bénabou R, Tirole J. Incentives and prosocial behavior. Am Econ Rev. 2006;96(5):1652‐1678. doi: 10.1257/aer.96.5.1652 [DOI] [Google Scholar]
- 26. Francois P, Vlassopoulos M. Pro‐social motivation and the delivery of social services. CESifo Economic Studies. 2008;54(1):22‐54. doi: 10.1093/cesifo/ifn002 [DOI] [Google Scholar]
- 27. King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff. 2013;32(4):661‐668. doi: 10.1377/hlthaff.2012.1348 [DOI] [PubMed] [Google Scholar]
- 28.We abandoned snail‐mail recruitment approach given after these counties given the very low response rates and higher mai.
- 29. Liang K‐Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13‐22. doi: 10.2307/2336267 [DOI] [Google Scholar]
- 30.Provider lists were drawn in two separate batches from the NC medical and nursing board. While the first draw contained.
- 31. NCDHHS Opioid action plan data dashboard. Accessed March 7, 2021. https://www.ncdhhs.gov/about/department-initiatives/opioid-epidemic/opioid-action-plan-data-dashboard
- 32. USDA ERS —Urban influence codes. Accessed March 7, 2021. https://www.ers.usda.gov/data-products/urban-influence-codes/
- 33. Hummel D, Maedche A. How effective is nudging? A quantitative review on the effect sizes and limits of empirical nudging studies. J Behav Exp Econ. 2019;80:47‐58. doi: 10.1016/j.socec.2019.03.005 [DOI] [Google Scholar]
- 34. Bao J, Ho B. Heterogeneous effects of informational nudges on pro‐social behavior. BE J Econ Anal Policy. 2015;15:1619‐1655. [Google Scholar]
- 35. Drass KA. Discourse and occupational perspective: a comparison of nurse practitioners and physician assistants. Discourse Process. 1988;11(2):163‐181. doi: 10.1080/01638538809544697 [DOI] [Google Scholar]
- 36. Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners . Occupational outlook handbook: U.S. Bureau of Labor Statistics. Accessed March 7, 2021. https://www.bls.gov/ooh/healthcare/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm
- 37. Heerman WJ, Jackson N, Roumie CL, et al. Recruitment methods for survey research: findings from the mid‐south clinical data research network. Contemp Clin Trials. 2017;62:50‐55. doi: 10.1016/j.cct.2017.08.006 [DOI] [PubMed] [Google Scholar]
- 38. Poynton TA, DeFouw ER, Morizio LJ. A systematic review of online response rates in four counseling journals. J Couns Dev. 2019;97(1):33‐42. doi: 10.1002/jcad.12233 [DOI] [Google Scholar]


