Abstract
Introduction and importance
Fabella syndrome is a rare cause of posterolateral knee pain. The definitive diagnosis and management of this syndrome remain unclear.
Case presentation
We report a case of a 19-year-old patient who is a Vietnamese professional football player. He presented with persistent pain in the posterolateral aspect of the knee joint for 12 months that was unrelated to trauma. He was treated conservatively for 6 months without any improvement in the previous hospital. He was diagnosed with fabella syndrome and underwent open surgery to remove the bone. Evaluation after surgery 12 weeks revealed the symptoms disappeared and he was able to return to practice.
Clinical discussion
In order to diagnose fabella syndrome, the clinicians need to be vigilant and base on the clinical signs as well as imaging to exclude other causes of posterolateral knee pain. Conservative therapy is always the first choice of treatment although the recurrence rate is high, especially in professional athletes. If the initial conservative therapies failed, the fabella surgical removal surgery should be made in athletes.
Conclusion
Fabella syndrome is a rare cause of posterolateral knee pain in professional athletes. The definitive diagnosis and management of this syndrome remain unclear. Our case shows that surgical removal of the bone fragments can be considered if failure after the initial conservative therapies.
Keywords: Fabella syndrome, fabella excision, Posterolateral knee pain, Sesamoid bone
Highlights
-
•
Fabella syndrome is a rare cause of posterolateral knee pain in professional athletes.
-
•
The definitive diagnosis and management of this syndrome remains unclear.
-
•
Fabella surgical removal should be made after the failure of conservative treatment.
-
•
This is an effective method which can help patient to return early to training and competition.
1. Introduction and importance
Fabella is a sesamoid bone located in the tendon of the human gastrocnemius muscle. The presence of fabella is about 10–30% in the population [1]. Fabella is a normal anatomical structure and rarely becomes pathological.
Fabella syndrome was first described by Weiner in 1977, presenting with the following signs: posterolateral knee pain associated with mechanics, the pain increases with terminal extension, the pain increases with local pressure on the site of fabella [2]. Studies in the literature have noted that fabella syndrome can occur in non-traumatic situations: Athletes with high-intensity exercise [3], [4], chondromalacia of the fabella, degeneration [3], posttraumatic: Fabella fracture [5], dislocation [6], and postoperative: High tibial osteotomy [7], distal femoral osteotomy [8], total knee replacement [9].
Fabella syndrome is a rare syndrome and the definitive diagnosis is relatively challenging. The treatment of this disease is still controversial. Some authors recommend initial conservative treatment including physiotherapy, local anesthesia, and steroid injection around the bone, splinting of the knee joint [10]. However, there was a high recurrence rate and surgical removal of the fabella was done in these cases. Some studied reported good results postoperative with a short follow up period, small number of patients and the lack of control group. There was also a case whose pain symptoms improved after the operation but the pain only went away completely after a year [1]. Therefore, we report a case of a 19-year-old male patient, a Vietnamese professional football player with fabella syndrome, he failed conservative treatment after 6 months and underwent surgery to remove the fabella. 12 weeks post-operation, he was able to return to training and competition.
2. Case presentation
This case followed 2020 SCARE guidelines for reporting of cases in surgery [11]. The patient was a 19-year-old male professional football player who was competing at a professional league in Vietnam.
Since January 2019, the patient began to feel pain in the posterolateral aspect of the left knee joint which was unrelated to injury. The pain appeared immediately after intense exercise. After 1 h of rest, the pain almost disappeared. There was no pain when exercising with low intensity, the patient did not receive any treatment.
From June 2019, the above symptoms became more severe. The patient had pain with swelling on the posterolateral side of the knee joint after exercise. The swelling was relieved with rest but the pain remained. The patient was treated at the previous hospital with conservative methods including NSAIDs combined with physiotherapy, even with steroid injection and local anesthetic 3 times, but the disease did not improve.
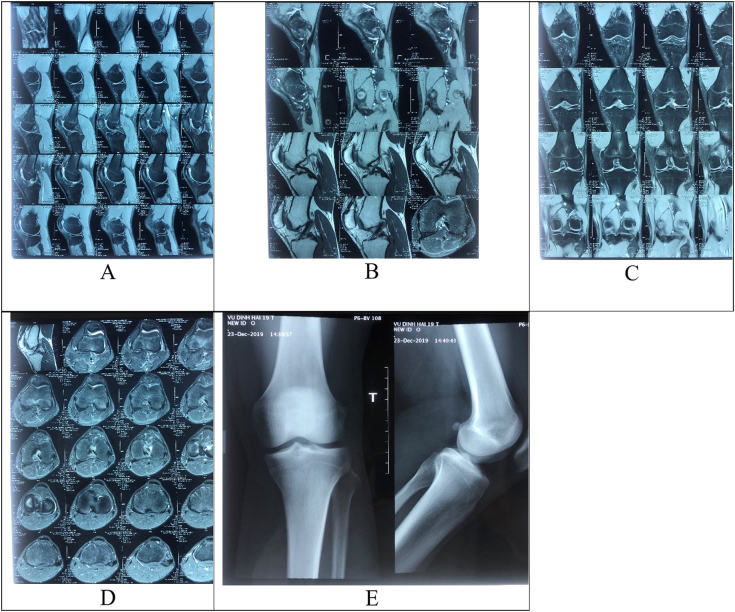
Since December 2019, the patient came to our hospital (level I Institutions of Trauma and Orthopaedics) because of unexplained pain in the posterolateral aspect of the knee joint. Clinical examination including Lachman test, anterior and posterior drawer tests, examination of medial collateral ligament, lateral collateral ligament, popliteal tendon, meniscal examination tests, and superior tibiofibular joint examination were negative. Examination of the posterolateral corner revealed a 1 × 1 cm mass which was well-defined border, movable and had pain on palpation. The knee range of movement was not restricted. However, there was an increased pain when his knee was in extension. Conventional X-ray of the knee joint showed the image of the sesamoid bone located on the posterolateral side of the knee joint and no image of bone damage. Knee MRI did not show damage to the ligaments, meniscus and structures in the posterolateral corner of the knee joint. Additionally, the sesamoid bone within the lateral head of gastrocnemius muscle was reflected with no signs of tendonitis (Fig. 1).
Fig. 1.
X-ray and MRI pre-operative. A, B, C, D, the sesamoid bone is embedded in the lateral head of gastrocnemius muscle on MRI. E, the fabella located on the posterolateral side of the knee joint on X-ray.
The patient's past medical history showed no familial diseases, no neurological lesion and no knee joint diseases. The patient did not consume alcohol or cigarette.
The patient was diagnosed with fabella syndrome of the left knee joint. After being explained about the risks and benefits of surgery, the patient agreed to the surgical option: Open surgery to remove fabella in the lateral head of gastrocnemius muscle. The surgery was performed by the senior surgeons (V.D.M, T.D.D). The patient underwent surgery in the supine position with spinal anesthesia. Prophylactic antibiotic of Cefuroxim 2 g was injected 30 min before thigh tourniquet. Fabella and the fibula head were located, a 5 cm skin incision on the posterolateral surface of the knee joint was made, and the iliotibial band was divided to expose the lateral head of gastrocnemius muscle. The fabella was located (Fig. 2A), the lateral head of gastrocnemius muscle was divided to expose and remove the fabella (Fig. 2B). The fabella shape resembled the small size patella with dimensions of 1.5 × 1.0 cm (Fig. 3). The lateral head of gastrocnemius muscle and the iliotibial band were closed with Vicryl 2.0 suture. The wound was sutured and bandaged and the knee joint was splinted.
Fig. 2.
A, the fabella was located in the lateral head of gastrocnemius muscle. B, exposed and removed fabella.
Fig. 3.
Resected fabella.
After the operation, there was no nerve or blood vessels complication and no wound infection. The knee joint was splinted in the extension position in 2 weeks. The patient was not permitted weight bearing. Two weeks after operation, the stitches were removed, and the patient was allowed weight bearing. After 4 weeks, the patient did not need crutched. He was instructed to practice to achieve the initial knee joint range of motion, muscle tone and limb proprioception. The patient reported no pain in the posterolateral side of the knee joint. After 12 weeks, the patient was able to return to training and competition. The patient satisfied with the condition after the surgery.
3. Discussion
In 1909, Pancoast was the first author to report the existence of fabella. However, unlike other anatomical structures, the sesamoid bones often attracted less interest in structure and function [12].
Fabella was often seen in Asian populations [13], [14]. This condition may be related to unique habits such as kneeling or squatting, as these are position that place increased strain on the flexor system of the knee joint. However, this hypothesis is still unclear [9].
According to the literature, fabella syndrome was a rare cause of posterolateral knee pain. However, this syndrome was often related to trauma or surgery. There were few reports about it in professional athletes. On the PUBMED database, we only found 3 case reports mentioning this syndrome in sports athletes: Kuur (1986) – Football player [15], Zenteno (2010) – runner [4] and Loscos (2020) – Swimmer [3]. These athletes did not have any traumatic injuries, so the authors believed that the high intensity training could cause micro-injury to the posterolateral region beyond the knee joint that causes fabella syndrome [4]. Details derived from three case reports which are shown in Table 1.
Table 1.
Details derived from three case reports on PubMed database.
| Kuur E. 1986 [15] | Zenteno B. 2010 [4] | Loscos S. 2020 [3] | |
|---|---|---|---|
| Number of patients | 1 | 1 | 1 |
| Level of activity | Soccer player | Runner | Swimmer |
| History of trauma | No | No | No |
| Symptoms | 3–4 years history of intermittent posteriolateral knee pain and slight swelling, painful in knee extension | Posteriolateral knee pain after running a distance longer than 2 km | Posteriolateral knee pain when walking during the knee extension phase and when turning over and kicking against the water |
| Conservative treatment | Injection of steroid and anti-inflammatory medication | Local injection of steroid. Physical therapy: ultrasound, laser and ozone therapy | Manual therapy, muscular strengthening, masotherrapy and radial shock waves |
| Operative treatment | Open fabellectomy | Open fabellectomy | Open fabellectomy |
| Follow | 2.5 years | 4 months | 3 months |
| Symptoms post operation | Pain free | Pain free | Pain free |
| Activity post operation | Work and compete in sports | Participate in high performance national and international competitions. | Compete in sport with excellent performance |
Fabella is adjacent to many surrounding anatomical structures, so the definitive diagnosis was very difficult and late. Most of the patients in these studies had clinical signs such as pain, swelling of the posterolateral aspect of the knee joint during vigorous exercise, had pain when performing squats and knee extension, and the pain increased when pressing on fabella [1], [2], [4], [15]. In addition to the above clinical signs, other causes of posterolateral knee pain were done to definitive diagnosis of fabella syndrome. Clinical examination, imaging such as conventional X-ray, ultrasound and magnetic resonance imaging should be used to exclude other causes of posterolateral knee pain.
In our case, the patient had no history of trauma and had all the signs of fabella syndrome as described by Weiner, especially the increased pain with local pressure on the site of fabella, which is very valuable in diagnosis. Besides, the combination with imaging methods such as conventional X-ray and magnetic resonance imaging helped to rule out the other causes of posterolateral knee pain such as Baker's cyst, lateral meniscus tear and gastrocnemius tendonitis.
In the literature, there were few studies on fabella syndrome, so the treatment principle was still unclear. Nearly all of the patients in the previous reports were treated with initial medical therapy, but it was not effective. In Weiner's largest study of fabella syndrome (n = 16), 11 out of 16 failed conservative treatment cases had fabella surgically removed. All of those showed no signs or symptoms at the time of follow-up after 22 months. 5 cases of conservative treatment improved but the patients still complained of cyclic pain at the time of follow-up after 6 months [2]. It was noteworthy that all the case of sports athletes failed conservative treatment, the patients had to have fabella surgically removed and all of them were able to return to professional competition [3], [4], [15]. Lapoutre performed the first open surgery to remove fabella in a 13-year-old female patient with chronic posterolateral knee pain. After that, most of the authors performed open surgery to remove fabella with posterolateral incision of the knee joint. Recently, Provencher [16] performed arthroscopy-assisted open surgery and Dannawi [1] performed arthroscopic surgery only. Most of the studied did not report postoperative complications and all patients showed no signs or symptoms in quite a short time after surgery. In the study of Dannawi, there was one case of patient whose pain symptoms improved after operation but the pain went away completely after 12 months and the patient was able to be back to sport [1].
In our case, the patient had fabella syndrome for 1 year, after 6 months of failed conservative treatment which made the patient unable to compete for a long time, so we performed surgery to remove fabella. After 4 weeks of surgery, the patient no longer had symptoms as before and 12 weeks later he returned to competition. We found that the professional athlete patient with fabella syndrome, who has a high frequency and high intensity of practice, conservative treatment often fails as previously mentioned [3], [4], [16]. We performed surgery with a small incision on the posterolateral side of the knee joint, dividing the iliotibial band and the lateral head of gastrocnemius muscle to remove fabella, we believe that this is a simple surgical method without requirement of arthroscopic skill surgery. However, during the surgery, careful dissection should be done to avoid damage to the lateral collateral ligament, popliteal tendon and common peroneal nerve.
Through this research, we have realized some limitations. First, failing to perform arthroscopy to examine and rule out the internal structures of the knee, especially the lateral meniscus may be one of the reasons for posterolateral knee pain. Second, the follow up period was short and lack of control group in our reports and previous reports and reviews.
4. Conclusion
Fabella syndrome is a rare cause of posterolateral knee pain. Definitive diagnosis of Clinical examination combined with appropriate imaging to rule out all other causes of posterolateral knee pain. We reported a good result of the patient underwent surgical after failure of conservative therapy. Our report contributes experience in the diagnosis and the treatment strategy for Fabella syndrome.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Funding
No financial support was received for the completion of this study.
Ethical approval
All procedures were approved by the 108 Central Military Hospital's Institutional Review Board, Hanoi, Viet Nam.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors' contributions
Dr. Dung Quoc Nguyen: Conceptualization, Writing - Review & Editing, Supervision.
Dr. Trung Duc Do: Conceptualization, Surgery, Writing - Review & Editing, Supervision.
Dr. Viet Dac Mai: Surgery, Writing - Review & Editing, Supervision.
Dr. Luong Van Nguyen: Writing - Review & Editing, Supervision.
Dr. Cuong Duc Do: Writing - Review & Editing, Supervision.
Registration of research studies
None. This is not ‘First in Man’ study.
Guarantor
Dr. Trung Duc Do.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Contributor Information
Trung Duc Do, Email: Bstrungctch108@gmail.com.
Luong Van Nguyen, Email: luongbv108@yahoo.com.vn, luongnv108@gmail.com.
References
- 1.Dannawi Z., Khanduja V., Vemulapalli K.K., Zammit J., El-Zebdeh M. Arthroscopic excision of the fabella. J.Knee Surg. 2007;20(4):299–301. doi: 10.1055/s-0030-1248063. [DOI] [PubMed] [Google Scholar]
- 2.Weiner D., Macnab I., Turner M. The fabella syndrome. Clin. Orthop. Relat. Res. 1977;126:213–215. [PubMed] [Google Scholar]
- 3.Loscos S., López-Vidriero R., López-Vidriero E. Fabella syndrome in an elite swimmer. Rev.Esp.Cir.Ortop.Traumatol. 2020;64(5):361–364. doi: 10.1016/j.recot.2020.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Zenteno Chávez B., Morales Chaparro I.F., De la Torre I.G. Fabella syndrome in a high performance runner. Case presentation and literature review. Acta Ortop. Mex. 2010;24(4):264–266. [PubMed] [Google Scholar]
- 5.Zhou F., Zhang F., Deng G., Bi C., Wang J., Wang Q., et al. Fabella fracture with radiological imaging: a case report. Trauma Case Rep. 2017;12:19–23. doi: 10.1016/j.tcr.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franceschi F., Longo U.G., Ruzzini L., Leonardi F., Rojas M., Gualdi G., et al. Dislocation of an enlarged fabella as uncommon cause of knee pain: a case report. Knee. 2007;14(4):330–332. doi: 10.1016/j.knee.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Kim T., Chung H., Lee H., Choi Y., Son J.H. A case report and literature review on fabella syndrome after high tibial osteotomy. Medicine. 2018;97(4) doi: 10.1097/MD.0000000000009585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rankin I., Rehman H., Ashcroft G.P. Fabella syndrome following de-rotation surgery to correct a femoral malunion. Open Orthop.J. 2018;12:346–352. doi: 10.2174/1874325001812010346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okano E., Yoshioka T., Yanai T., Kohyama S., Kanamori A., Yamazaki M., et al. Fabella syndrome as an uncommon cause of posterolateral knee pain after total knee arthroplasty: a case report and review of the literature. Case RepOrthop. 2016;2016:4328462. doi: 10.1155/2016/4328462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Driessen A., Balke M., Offerhaus C., White W.J., Shafizadeh S., Becher C., et al. The fabella syndrome - a rare cause of posterolateral knee pain: a review of the literature and two case reports. BMC Musculoskelet. Disord. 2014;15:100. doi: 10.1186/1471-2474-15-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Group S. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 12.Zipple J.T., Hammer R.L., Loubert P.V. Treatment of fabella syndrome with manual therapy: a case report. J.Orthop.Sports Phys.Ther. 2003;33(1):33–39. doi: 10.2519/jospt.2003.33.1.33. [DOI] [PubMed] [Google Scholar]
- 13.Zeng S.X., Dong X.L., Dang R.S., Wu G.S., Wang J.F., Wang D., et al. Anatomic study of fabella and its surrounding structures in a Chinese population. Surg.Radiol.Anat. 2012;34(1):65–71. doi: 10.1007/s00276-011-0828-4. [DOI] [PubMed] [Google Scholar]
- 14.Tabira Y., Saga T., Takahashi N., Watanabe K., Nakamura M., Yamaki K. Influence of a fabella in the gastrocnemius muscle on the common fibular nerve in Japanese subjects. Clin.Anat.(New York, NY) 2013;26(7):893–902. doi: 10.1002/ca.22153. [DOI] [PubMed] [Google Scholar]
- 15.Kuur E. Painful fabella. A case report with review of the literature. Acta Orthop. Scand. 1986;57(5):453–454. doi: 10.3109/17453678609014771. [DOI] [PubMed] [Google Scholar]
- 16.Provencher M.T., Sanchez G., Ferrari M.B., Moatshe G., Chahla J., Akamefula R., et al. Arthroscopy-assisted fabella excision: surgical technique. Arthrosc.Techn. 2017;6(2):e369–e374. doi: 10.1016/j.eats.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.