Abstract
Background
The proliferating and malignant proliferating trichilemmal cysts (MPTC) are rare adnexal tumors. We report 3 cases through which we will detail the anatomo-clinical characteristics of these tumors.
Cases
Two patients, 60 and 56 years old, consulted for multiple scalp nodules, one of which had changed with the appearance of a central ulceration. The removal of the remaining scalp nodules was in favor of PTCs. The third patient presented with an ulcerative lesion occupying the vertex. Skin biopsy found trichilemmal-type keratinization associated with areas of necrosis concluding with a MPTC.
Discussion
The PTC is a transitional form between the trichilemmal cyst (TC) and the MPTC. The increase in the size of a TC and ulceration are sufficient signals to suspect this evolution.
Keywords: Proliferating trichilemmal cyst, Malignant proliferating trichilemmal cyst, Benign adnexal tumor, Malignant adnexal tumor
Established Facts
Proliferating trichilemmal cyst (PTC) is a benign adnexal tumor.
Malignant PTC is a malignant adnexal tumor.
Novel Insights
Malignant proliferating trichilemmal cyst is not a squamous cell carcinoma.
All scalp cysts should be referred for histological study even in the absence of central ulceration.
Introduction
Proliferating trichilemmal cyst (PTC) and malignant PTC (MPTC) are rare adnexal tumors, often under-diagnosed. These tumors develop from the isthmic portion of the hair follicle [1]. They can appear de novo or complicate a trichilemmal cyst (TC). We report 2 cases of PTC and 1 case of MPTC through which we will detail the anatomo-clinical characteristics of these 2 adnexal tumors.
Observations
Case 1
A 60-year-old patient, without pathological history, consulted for multiple nodules of the scalp dating back >15 years. She reported that one of these nodules had been altered by a rapidly progressive increase in size and the appearance of ulceration following minimal trauma. The clinical examination revealed 8 firm scalp nodules, and one of them was painful on palpation, measuring 2 cm, with ulceration in the center.
Case 2
A 56-year-old patient with no previous pathological history consulted following the appearance of a little painful ulceration sitting at the center of an old nodular lesion of the scalp dating back >11 years (Fig. 1). The clinical examination revealed 6 firms, painless nodules of the scalp, one of which was 1 cm and had an ulceration in the center.
Fig. 1.

Occipital nodule of the scalp, measuring 1 cm in diameter and presenting a central ulceration.
The clinical examination in the 2 patients was unremarkable. The biopsy of the ulcerated nodule, which had been removed from the skin, showed the presence of calcified trichilemmal keratinisation, and few typical mitoses (Fig. 2). Removal of the other nodules of the scalp was in favor of TC. The diagnosis of PTC following a pre-existing TC associated with TCs was retained in both our patients. The follow-up is 22 and 13 months, respectively, and our patients have no local recurrence or new lesions.
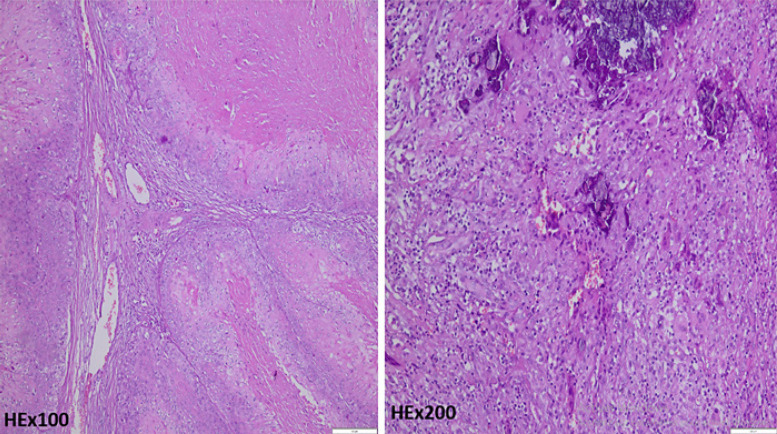
Fig. 2.
Calcified trichilemmal-type keratinization associated with few, nontypical mitoses.
Case 3
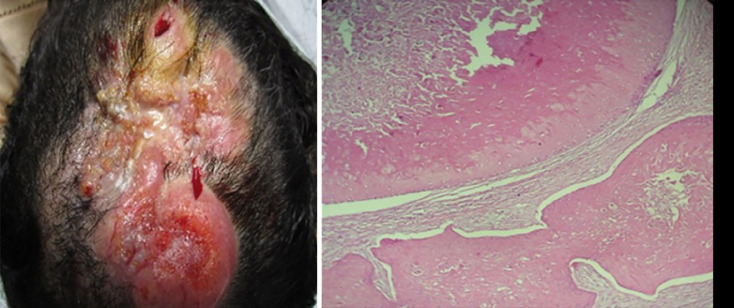
A patient with no pathological history, consulted for the modification of a firm nodular lesion of the scalp and this by the appearance of a budding and ulceration on it. The clinical examination showed the appearance of an ulcerous tumor, infiltrating and bleeding in places, measuring 10 × 6 cm and occupying the entire vertex. Examination of the lymph node areas revealed lenticular cervical adenopathies. Skin biopsy revealed trichilemmal keratinization associated with strong mitotic activity, the presence of cytonuclear atypia and areas of necrosis with frank infiltration of the stroma which indicated MPTC (Fig. 3). The brain scan showed bone lysis of the outer table of the parietal vault. And the rest of the extension examens was unremarkable. Patient management consisted of surgical removal of the periosteum, with lymph node dissection and insertion of a scalping flap. The histological study of the excision piece confirmed the appearance of a MPTC. The resection limits were healthy and the bone cross-section without abnormality with the presence of reactive hyperplastic lymphadenopathy. Local radiotherapy was indicated. However, 3 weeks later an ischemia of the distal part of the flap motivated a necrosectomy with skin grafting, delaying the radiotherapy. The evolution was complicated 2 months later by tumor recurrence, then death after few months.
Fig. 3.
Ulcerating and infiltrating ulcerous tumor, 10 × 6 cm in diameter, with a histological appearance at the top of a benign and invasive trichilemmal cyst at the bottom.
Discussion
The particularity of our observations lies in the rarity of the PTC and the MPTC but also the presence of a nosological problem of this entity. In fact, since 1966, the year of the first description of the PTC by Jones [2]; to 2018, only 187 cases are reported in the literature [3]. PTC, also known as Wilson Jones scalp tumor, is a transitional form between TC and the true malignant pilar tumor; MPTC. A TC can transform into a PTC and the notion of multiple trauma and/or iterative inflammation may be a cause of this transformation [4], in our first patient we raised the notion of a precessive trauma only a few days before the onset of ulceration. The increase in the size of a TC and ulceration are sufficient signals to suspect this proliferation; however, ulceration is not always obligatory. PTC is a benign tumor that usually occurs in older women with an average age of 65 years [5]. PTC usually appears in areas of high hair density, especially the scalp [6], but other atypical localizations are reported in the literature [3, 7, 8]. Clinically, it is a nodule between 1 and 10 cm in size that can become secondarily ulcerated and often coexists with TC, which is the case of our first 2 patients. PTC is histologically distinguished by the presence of trichilemmal keratinization, the tumor cells do not show anisokaryosis, mitoses are few, and there are also some areas with moderate cytonuclear atypia [9]. In IHC, strong expression of CK10 and involucrin are also histological signs of benignity. In the other hand, the presence of trichilemmal keratinization, strong mitotic activity, numerous cytonuclear atypia, aneuploidy, as well as the presence of necrotic areas and clear infiltration of the stroma are signals in favor of MPTC [9]. The MPTC IHC can show a high number of cells expressing the nuclear proliferation antigen and CK16, as well as loss of CD34 expression.
The MPTC was first described by Saida et al. [10] and since then a very limited number of cases have been reported in the literature. It can occur de novo or as a result of a PTC that undergoes a progressive malignant transformation from adenomatous and epitheliomatous to carcinomatous MPTC [10]. Clinically, MPTC is exophytic, ulcerative, or polypoid in appearance. It is mainly located in the occipital region and is characterized by rapid growth, invasion of neighboring tissues with lysis of the cranial vault, and by its recurrences, as in the case of our third patient. The extension assessment is based on cerebral CT scan, the search for cervical regional adenopathy or remote metastases, particularly pulmonary metastases, using cervical ultrasound, pulmonary CT scan, or PET scan. MPTC generates a real nosological problem, and it is very often confused with squamous cell carcinoma. Nevertheless, the presence of a trichilemmal keratinization in the histology, as well as the absence of expression of anti-monoclonal AE13 and AE14 antibodies, and finally the clinical absence of a precancerous intraepithelial lesion or Bowen's disease, make it possible to definitively rule out the diagnosis of squamous cell carcinoma [11]. MPTC can also be confused with pilomatricial carcinoma of the scalp because of its clinical, sometimes histological similarity, and especially its aggressiveness (recurrence and metastases) [11].
Therapeutically, the removal of PTC with scalp ulceration is recommended to avoid the risk of local recurrence estimated at 3.7% within 6 months to >10 years. The evolution of the PTC is slow and often benign. The treatment of MPTC is based on exeresis arriving at the periosteum with 1 cm margins in the absence of metastasis and the combination of exeresis with palliative chemotherapy (cisplatin and 5-FU) followed by palliative radiotherapy for MPTC with distant metastases. Close monitoring is recommended in view of the high risk of recurrence and metastases [1].
Conclusion
All scalp cysts should be referred for histological study and the use of a qualified and specialized pathologist is sometimes essential. Enlargement of a long-standing scalp nodule should be investigated for PTC or MPTC, as the risk of malignant transformation is not to be neglected. Follow-up of these patients is necessary for the early identification of recurrence or degeneration.
Statement of Ethics
This study was carried out in accordance with the principles set out in the declaration of Helsinki and with local ethical guidelines (Ethics Committee for Biomedical Research, Faculty of Medicine and Pharmacy, Casablanca, Morocco). Written informed consent was obtained from the patient 1, 2, and the son of the third patient for publication of this cases report and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have no funding sources to declare.
Author Contributions
Ibtissam Benslimane Kamal contributed to acquisition, analysis, and interpretation of data and redaction. Fouzia Hali contributed to revising critically the work. Farida Marnissi contributed to interpretation of data. Soumiya Chiheb contributed to revising critically the work.
References
- 1.Ui Geon K, Dong Bee K, Tae Hun K, Chung Hun K. Trichilemmal carcinoma from proliferating trichilemmal cyst on the posterior neck. Arch Craniofac Surg. 2017;18((1)):50–3. doi: 10.7181/acfs.2017.18.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones EW. Proliferating epidermoid cysts. Arch Dermatol. 1966;94:11–9. [PubMed] [Google Scholar]
- 3.D'Avila DG, Kanno DT, de Castilho da Silva D, Pastro VR, Novelli PCS, de Paula Freitas PZ, et al. A proliferating trichilemmal cyst in the perianal region: a case report. Int J Surg Case Rep. 2018;53:175–8. doi: 10.1016/j.ijscr.2018.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leyendecker P, de Cambourg G, Mahé A, Imperiale A, Blondet C. 18F-FDG PET/CT findings in a patient with a proliferating trichilemmal cyst. Clin Nucl Med. 2015;40:598–9. doi: 10.1097/RLU.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 5.Viarnaud A, Alhazmi K, Constant G, Gaudron S, Hirsch G, Janier M, et al. Proliferating trichilemmal cyst. An unusual presentation. Ann Dermatol Venereol. 2017;144:326–8. doi: 10.1016/j.annder.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 6.ElBenaye J, Sinaa M, Elkhachine Y, Sakkah A, Jakar A, Elhaouri M. Proliferating trichilemmal cyst of the scalp: nine cases and literature review. Otorhinolaryngol Head Neck Surg. 2018;3((5)):2–3. [Google Scholar]
- 7.Makhlouf Z, Verola O, Senejoux A, Duval A, Terris B, Balaton A, et al. Tumeur trichilemmale proliférante de la région ischio-rectale. Annales de pathologie. 2011;31((4)):316–9. doi: 10.1016/j.annpat.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Capurso-García MA, Bautista-Piña V, Pomerantz A, Galnares-Olalde JA, Blachman-Braun R, Rodríguez-Rodríguez S, et al. Atypical proliferating trichilemmal cyst with malignant breast skin transformation: a case report and review of the literature. Case Rep Oncol Med. 2016;2016:7481569. doi: 10.1155/2016/7481569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiffenbach A, Katz K, Rupley K, Carter A, Gottlieb A, Shulman K. Rapidly enlarging malignant proliferating trichilemmal tumor in a young female. J Drugs Dermatol. 2018;17((12)):1325–7. [PubMed] [Google Scholar]
- 10.Saida T, Oohara K, Hori Y, Tsuchiya S. Development of a malignant proliferating trichilemmal cyst in a patient with multiple trichilemmal cysts. Dermatologica. 1983;166:203–8. doi: 10.1159/000249868. [DOI] [PubMed] [Google Scholar]
- 11.ElBenaye J, Elkhachine Y, Sakkah A, Sinaa M, Moumine M, Jakar A, et al. Kyste trichilemmal proliférant malin du scalp: une nouvelle observation. Ann Chir Plast Esthet. 2018;63((1)):97–101. doi: 10.1016/j.anplas.2017.06.003. [DOI] [PubMed] [Google Scholar]