Abstract
Objective
To evaluate the effect of a specific communication training for neurologists on how to provide complex information about treatment options to patients with multiple sclerosis (MS).
Design
Single-centre, single-blind, randomised controlled trial.
Setting
One university hospital in Norway.
Participants
Thirty-four patients with early-stage MS.
Intervention
A 3-hour training for neurologists on how to provide complex information about MS escalation therapy.
Main outcome measures
Patient recall rate, measured with a reliable counting system of provided and recalled information about drugs.
Secondary outcome measures
Number of information units provided by the physicians. Effects on patient involvement through questionnaires.
Methods
Patients with MS were instructed to imagine a disease development and were randomised and blinded to meet a physician to receive information on escalation therapy, before or after the physician had participated in a 3-hour training on how to provide complex information. Consultations and immediate patient recall interviews were video-recorded and transcribed verbatim.
Results
Patient recall rate was 0.37 (SD=0.10) pre-intervention and 0.39 (SD=0.10) post-intervention. The effect of the intervention on recall rate predicted with a general linear model covariate was not significant (coefficient parameter 0.07 (SE 0.04, 95% CI (−0.01 to 0.15)), p=0.099).
The physicians tended to provide significantly fewer information units after the training, with an average of 91.0 (SD=30.3) pre-intervention and 76.5 (SD=17.4) post-intervention; coefficient parameter −0.09 (SE 0.02, 95% CI (−0.13 to −0.05)), p<0.001. There was a significant negative association between the amount of provided information and the recall rate (coefficient parameter −0.29 (SE 0.05, 95% CI (−0.39 to −0.18)), p<0.001). We found no significant effects on patient involvement using the Control Preference Scale, Collaborate or Four Habits Patient Questionnaire.
Conclusion
A brief course for physicians on providing complex information reduced the amount of information provided, but did not improve patient recall rate.
Trial registration number
Keywords: multiple sclerosis, patient information, communication, randomised controlled trial
Strengths and limitations of this study.
Randomised controlled trial design, adapted to health communication research.
Patients with multiple sclerosis with unique insight in the disease and emotional connection to the information.
Reliable measurement of recall of complex information given in free speech.
A small sample.
Introduction
Multiple sclerosis (MS) immunomodulatory treatment has become increasingly complex as new drugs have been introduced, differing in efficacy, risk/adverse effect profile and administration form.1 2 In Norway, guidelines for MS treatment issued by the Norwegian Directorate of Health state which disease-modifying therapies should be introduced initially, and which should be introduced as escalation therapy when relapse occurs3 or if the patient initially presents with a very active disease.1
Informing patients with MS about escalation therapy alternatives involves comprehensive exchange of situation-specific information, including risks and effects subject to uncertainty. This information is usually delivered by a neurologist in a task-based but unscripted dialogue with a patient who is experiencing an emotionally charged situation.4 5
Medical information should ideally be provided in a way that enables patient autonomy and involvement in treatment decisions.6 Patients desire tailored information.7–9 The quality of communication is therefore crucial, if not clearly proven to influence the patients’ ability to manage their disease,7 8 10 at least to improve patient adherence.11
Several studies have shown that recall of medical information is suboptimal.12–17 Cognitive impairments associated with MS make information processing more difficult.18–20 Even in early-stage MS, subtle memory disturbance has been shown to be common.21 22 Improvement of information recall among patients with MS is necessary to avoid lack of patient involvement, adherence and poor outcomes.
A few studies have investigated patient uptake of complex information as an outcome measure; most have directed interventions at patients.23 24 Intervention studies that link communication training of physicians to patient outcomes in general are rare,25 26 and to patient recall even more so. The question has been raised whether recall in complex chronic illness management could be improved by changing the communication behaviour of healthcare personnel.24 Various oral communication strategies have been examined and found to improve patient recall in various ways like repetition,27 28 simplification of language, pauses, personal relevance28–30 and structuring.28 31 One recent study has shown recall rate improvement by information structuring and categorisation, but only for disadvantaged subgroups of a population.32 Other studies have not showed such an effect, and the phenomena remain understudied in clinical populations.33 Lehmann et al did show that providers should tailor both portioning and amount of information to patient preferences, as those wanting more, also recalled more information.34
However, the interventions investigated have usually been long, and most often involved video-vignettes studies or analogue patients, that is, healthy subjects pretending to be patients. Studies have usually tested single, generic strategies, not a set of strategies selected and tailored to the needs of a specific group of professionals and rarely performed in unscripted conversations with real patients. Hence, ecological validity remains unclear. Furthermore, increasing demand on cost control in healthcare makes long training interventions for physicians less attractive to administrators.
In order to accommodate these shortcomings, this study tested a very brief communication training intervention, performed in natural conversations with real patients, although in a fictitious setting, with a set of information provision strategies selected to tailor the needs of physicians working with patients with MS. We tested whether a brief intervention focused on how to deliver complex information, tailored to a selected population of physicians, improved patient recall rate.
Methods
Study design
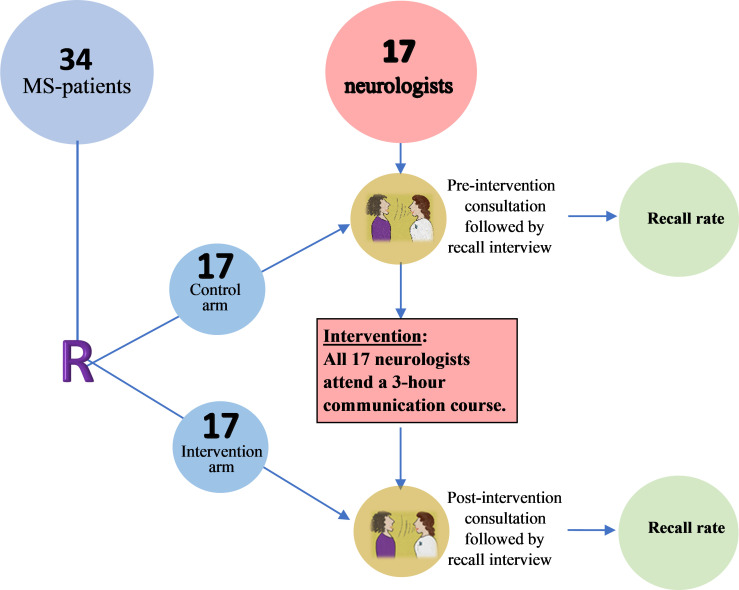
This was a single-centre, single blind randomised controlled pilot trial to determine the effect of brief communication skills training for physicians on patient recall of information provided by the physician. Patients with early-stage MS were randomised to be exposed to a physician either before or after training, see an overview of the study design visualised in figure 1.
Figure 1.
Study design overview. Result: Patient recall rate. MS: multiple sclerosis.
Participants and setting
Patients
The ability to recall information provided depends on its relevance, degree of patient involvement and the emotional state of the recipient.17 30 35–37 When designing this experiment, we therefore wanted to recruit real patients with MS, who know how it is to live under the sword of Damocles, that is, any time and day symptoms of exacerbations of the disease may appear.38 To set up an experiment in a communication lab, however, we could not rely on the unpredictable influx of patients in need of escalation therapy. Hence, we approached outpatients identified in the electronic patient records at Akershus University Hospital (Ahus), a teaching hospital in the capital region of Norway with a population uptake area of 575 000 inhabitants.39 The patients had to meet the following eligibility criteria to be asked for participation and included:
Being 18 years old or above.
Diagnosed with relapsing remitting MS between 2009 and 2012.
Currently on no or first-line treatment.
Not yet exposed to a decision about choice of escalation treatment.
Not yet received thorough information about escalation treatment options and their pros and cons by a neurologist.
Eligible patients were asked if they were willing to imagine themselves having experienced exacerbations, and meet a physician to discuss further treatment. If willing, they were included in the study.
Physicians
We presented the planned study for the physicians working in the Neurology Department at Ahus on staff meeting and through email. Participating physicians were required to regularly meet patients with MS in their work. To compensate for differences in their level of experience, participants were provided with an overview of information including risk–benefit stratification for the three most relevant escalation medications commonly used in Norway in 2016: natalizumab, alemtuzumab and fingolimod.2 40 41
Setting
Consultations and post-consultation recall interviews with patients were video recorded in a communication lab facility on hospital grounds. The patients were instructed beforehand to imagine that they had recently experienced two unspecific, function-reducing attacks and had undergone an MRI scan and blood tests. They were now to consult with a physician about the tests and scan results, receive information about escalation treatment and discuss options. Except for this fictitious setting, the patients were instructed to use their personal history and behave as themselves. The physicians were fully informed about the fictitious setting. They received information in advance on which and how few details the patients had been given, and were asked not to go into details about previous or recent clinical findings or attacks, nor to examine the patient. They also received an exacerbation history, results of a recent MRI scan showing new lesions and a John Cunningham virus (JCV) antibody index of 0.8,42–45 all framed as a journal exempt. Physicians were given approximately 20 min for the consultation, to mirror the usual timing of a busy scheduled day. They were instructed to handle the situation as they would have done in their everyday work, basing the discussion of treatment escalation on the individual situation and risk profile of the patient.1 40
Intervention
The intervention was a 3-hour communication training course, specifically focused on structured and patient-centred information provision, and targeted at physicians working in neurology. The course was developed and held by a professor specialised in health communication research with extensive experience in teaching medical students and physicians communication skills (PG). It was a condensed version of patient-centred communication skills training46 with an emphasis on strategies which have been tested or have been expected to improve recall and understanding (creating a safe environment, exploring the patient’s understanding and perspectives, prioritising and adapting the amount of information to the patient’s prior understanding and needs, using signposting, short sentences, pauses, explanations without jargon and checking for understanding).27 28 32 47–49 The 3-hour course comprised a 50/50 mix of theoretical instruction and practical training with role plays. Whereas strategies discussed are not specific for communication with patients with MS, examples and practice cases aimed to illustrate treatment decision-making in MS were used. The course was provided in three sessions, for five to six physicians at a time, 21–27 September 2016.
Study procedures
A researcher not involved in the development and delivery of the training (JMN) observed the consultation on-screen in an adjacent room while taking notes with the help of an observational sheet. Immediately after the physician had left the room, JMN performed the recall interview with the patient while the recording proceeded uninterrupted (figure 2). The recall interview guide was strict, with initial open questions, followed by a tailored part in which JMN anchored the questions specifically to the information the doctor had provided during the visit, based on the notes collected during the observation of the specific consultation.
Figure 2.
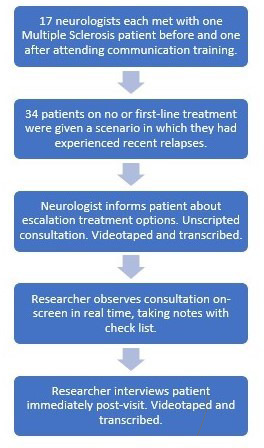
Data collection procedure.
Each physician saw two patients, one before and one after attending the communication training. Pre-intervention consultations took place 16 August–15 September 2016, post-intervention consultations took place 3 October–3 November 2016.
Outcomes
Primary outcome measure
The from protocol primary outcome measure was the patient recall rate measured as the amount of information recalled by the patient divided by the amount of information given by the doctor, based on transcripts of the videos. We limited the measurement to information concerning the three most relevant drug alternatives when initiating second-line MS treatment.41 We developed a specific system for measuring complex oral information transfer in medical consultations, counting the number of information units provided by the physician, and the proportion of these units recalled by the patients.50 This measure contains a sophisticated system of definitions that enables a coder to break down complex conversation into the smallest countable units that carry meaningful medical information. One quite simple example would be the statement, ‘One option is Tysabri, which you get in the hospital as a monthly infusion’. Here, the smallest possible units of information are:
One option is Tysabri [a]—name of medication 1p.
In the hospital [b]—administration place 1p.
Infusion [c]—administration manner 1p.
Monthly [d]—administration frequency 1p.
The system involved three researchers (JMN, MN, PG) and demonstrated high inter-rater reliability (IRR).50 After establishment of the IRR, JMN coded all transcripts for this study.
Secondary outcome measures
The from protocol secondary outcome measure was the effect of the intervention on the mean amount of oral information provided by the physicians. We also explored possible effects on patient involvement using the Control Preference Scale (patient),51 Collaborate52 53 and the Four Habits Patient Questionnaire,54 55 all of these after the consultation.
Sample size estimation
The study was designed as a preclinical trial. No previous ways of measuring orally provided information were available, so the numerical effect size of the measure we developed,50 as well as its natural variability, was unknown. For a high effect size, we decided to consider the SD of the measured effect as proxy of the average effect of the intervention. Under standard assumptions of a two-sided t-test of statistical significance at 5% and 80% power, 16 patients in each arm of the study were necessary.
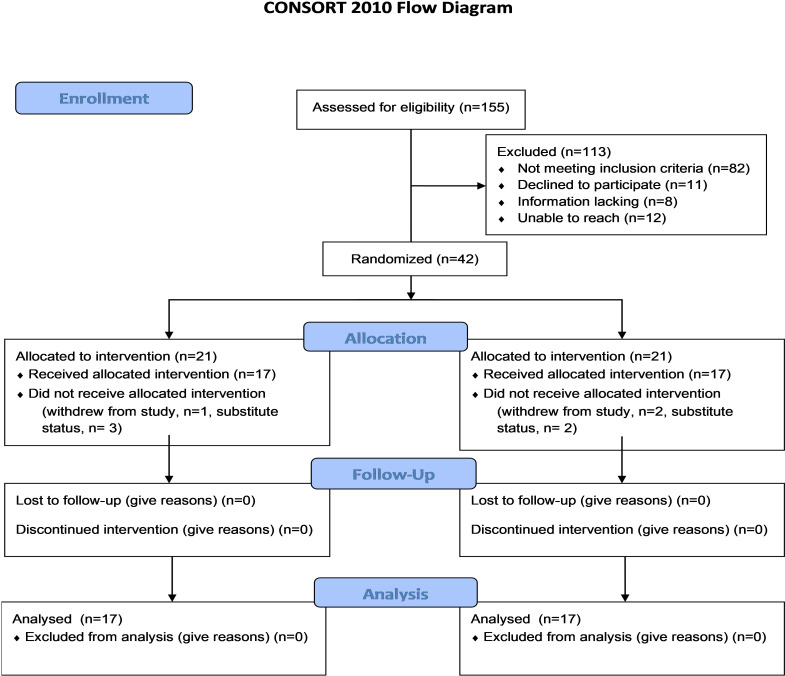
Randomisation
An independent statistician performed the randomisation of patients agreeing to participate. The R-method sample (1-42, 21) was used to draw a random subsample of size 21 from the set of 42 patients (figure 3). The four last patients on each list were given substitute status. The random sample was generated without any blocking or stratification restrictions beyond its size. JMN enrolled participants and assigned them blinded to either the control or the intervention group.
Figure 3.
CONSORT 2010 participant flow. CONSORT, Consolidated Standards of Reporting Trials.
Statistical methods
We investigated the effect of the intervention on the recall rate, alongside various secondary outcomes. This was done with separate generalised linear mixed models, using the doctor ID as a random effect and the variables of interest as dependent variables and fixed effects. Likelihood functions were chosen appropriately for the distribution of the dependent variable. Standard maximum likelihood estimates inference was pursued, giving corresponding confidence intervals and p values.
Pre-trial registration
The trial was registered in ISRCTN (www.isrctn.com) on 23 June 2016 (registration number: ISCRTN42739508).
Patient and public involvement
A representative patient with MS and a professor of medical ethics constituted an advisory group for the project.
Results
Participants
All participants, patients and physicians, were included between 12 April 2016 and 2 May 2016. Among approximately 60 resident or consultant physicians employed at the Department of Neurology at Akershus University Hospital, 17 agreed to participate. All provided informed consent. Ten were male (59%), median age was 39 (range 29–57). They had between 2 and 29 years of work experience (median=11) (table 1).
Table 1.
Participant characteristics; neurologists and patients
| Neurologists | Patients | ||||||
| (n) | (%) | (n) | (%) | Control arm (n) | Intervention arm (n) | ||
| All | 17 | 100 | All | 34 | 100 | 17 | 17 |
| Female | 7 | 41 | Female | 25 | 74 | 12 | 13 |
| Male | 10 | 59 | Male | 9 | 26 | 5 | 4 |
| Age by first consultation | Age | ||||||
| <36 | 3 | 18 | 21–30 | 3 | 9 | 1 | 2 |
| 36–45 | 10 | 59 | 31–40 | 6 | 18 | 2 | 4 |
| >45 | 4 | 24 | 41–50 | 16 | 47 | 10 | 5 |
| Years of clinical experience | 51–60 | 7 | 21 | 3 | 4 | ||
| <5 | 4 | 24 | 61–70 | 2 | 6 | 0 | 2 |
| 6–10 | 3 | 18 | |||||
| 11–15 | 6 | 35 | |||||
| >15 | 4 | 24 | |||||
Patient recruitment is shown in figure 3. Out of the 53 eligible patients with MS we reached, 42 agreed to participate and provided informed consent (79%). They were randomised into two groups, each with 17 participants and 4 substitutes. Finally, 34 participated in the study. Median age was 48 (range 21–66 years old). Twenty-five were female (table 1).
An overview of the participant flow is shown in figure 3. Three patients opted out after the study had begun, but before partaking, and was replaced by substitutes already randomised to the same arm.
Both pre-intervention and post-intervention consultations lasted on average 21 min (range 8–29 min, median 20 min). From the consultation transcripts, 1652 physician statements containing information about the three predefined drug alternatives were identified.
Primary and secondary outcomes
The recall rate was 0.37 in the pre-intervention group and 0.39 in the post-intervention group. When predicting the recall rate with the intervention using a binomial likelihood, we found the general linear model covariate coefficient parameter 0.07 (SE 0.04, 95% CI (−0.01 to 0.15)), p=0.099.
The average number of oral information units provided by the physicians before and after the intervention were 91.0 and 76.5, respectively. When predicting this a priori secondary outcome with the intervention using a Poisson likelihood, we found the coefficient parameter −0.09 (SE 0.02, 95% CI (−0.13 to −0.05)), p<0.001. When predicting the recall rate with the amount of information provided, we found the coefficient parameter −0.29 (SE 0.05, 95% CI (−0.39 to −0.18)), p<0.001.
We found no significant effects of the intervention on patient involvement using the Control Preference Scale, Collaborate or Four Habits Patient Questionnaire. We also did not find effects of the patient’s gender or age on recall rate.
Discussion
We embarked on this study knowing that hospitals are reluctant to spend resources on extensive courses if strong effects are not demonstrated, and hoping that focus on a simple set of instructions could render a physician behavioural change strong enough to have a detectable effect on patient recall in a small pilot study. We did this, even though two systematic reviews on the effect of general communication skills courses suggested that brief interventions consistently yielded small effects.23 56 However, some papers suggested that courses of 5 hours or less could have effect.57–60 These studies addressed emotional communication, patient participation effect57 58 60 or a very simple instruction about one medication,59 and did not introduce patient adjusted information provision. Neither did they measure effect of the intervention by actual measurement of patient recall. Our study encompassed tailored information giving in a free dialogue with a real patient. Tailored information provision is a complex task, particularly so in the case of involving real patients in decision-making about second-line treatment for MS, which requires that they be well informed about pros and cons of options. The information given in our dataset was a lot more complex than in the studies referenced above. Our study suggests that complex information giving tasks require more extensive training than a 3-hour course to achieve substantial changes in patient recall, at least in decisions as difficult as choice of MS treatment.
In accordance with the principle of prioritising information tailored to the patient,34 which was one of the strategies taught to physicians in our training, we observed a significant decrease in the amount of information provided by physicians (secondary outcome) after having received the training. We also found that the recall rate decreased with increased amount of information provided, which is in line with previous findings.35 61
Questionnaires did not document changes in patient involvement. We did not expect to find changes in such proxy measures in a small pilot, particularly as the intervention was directed foremost to improve information provision, not patient involvement. However, in case we had found changes in patient involvement, we could have explored associations between observed physician behaviour (not reported in this paper) and involvement.
The strengths of this study, besides the randomised controlled trial design, are several. Real patients with MS could easily envision the fictitious position they were in during the consultation, so that information was highly relevant and with potential to evoke emotions. The physicians were not instructed to provide a prefixed set of information, but rather inform the patients according to what happened in the encounter, closely resembling real clinical situations. The recall interview used a technique with questions specifically anchored to the information that had been given, thus providing memory cues without ‘helping’ the patient. The effect measure was direct recall as fraction of information provided, not more commonly used proxy measurements using questionnaires.
Patients were blinded to training status of the physicians. Furthermore, more female than male patients participated (ratio 2.8), in accordance with population-based epidemiological data and data from the Norwegian MS Registry, in which the female to male ratio ranged from 1.7 to 2.7,62 suggesting that recruitment was not gender biased. The distribution of patient gender on pre-intervention and post-intervention observations was similar. There was no attrition, so we had a complete set of data, and only three substitutions among patients. The substitutes were already randomised, so an intention-to-treat analysis was not necessary.
There are also limitations. First, our small sample. With a larger sample we might have been able to show smaller effects. The premise of choosing a small trial and expecting a high effect size proved too optimistic.
Second, the design of our study calls for caution in making causal inferences. As previous researchers have emphasised,63 64 the link between physician training and patient recall is indirect, and mediated by what actually happened during information provision sequences in these meetings: In other words, the lack of an effect on recall could be due to a lack of change in how the information was provided, even though the amount was reduced. Such a result would implicate something lacking in the training intervention. Equally possible is that the physicians applied what they were taught, but that this had no effect on patient recall. This result would call into question the content of the training course, while highlighting the efficacy of its methods.
It is a limitation that it was not feasible to do the study with patients in a real treatment escalation situation. The fact that it was not their own treatment that was being discussed may have affected their recall. This would be true for all patients, however, regardless of the training status of the physician they consulted with.
Treatment fidelity was not measured for physician training in this study, but whether they changed some of their behaviour according to the teaching intervention is briefly explored in a qualitative study that showed how to define and assess quantifiable outcomes for three of the information sharing strategies taught in this intervention. It did not show significant effects on the physicians use of those three strategies.65 We did endeavour to implement the training correctly and consistently for all participating physicians. Patient consultation fidelity was not measured. The amount of time available, setting and situation were, however, identical for all consultations.
Recall was only measured immediately after the consultation. It would have been interesting to have additional patient recall results after an amount of time had passed. On the other hand, this might have led to a risk for contaminated results, as patients in the meantime may have discussed with others or read other information. There is also a risk that the fictitious situation would make the patients less prone to remember multiple facts, as they would not discuss details with spouse or relatives in order to actually choose a treatment.
The research team that made this analysis was, with the exception of JMN, blinded to the intervention status of the transcripts from the consultations and recall interviews. Observer bias cannot be ruled out, although JMN made efforts to ignore not being blind. Some results suggest the measurement is indeed valid: (1) the measurement system was rigorously developed, yielding high IRR,66 (2) there was no significant negative effect of increasing age within the age span 21–66 years on recall rate, and (3) recall rate lessened with increased amount of information provided. These observations concur with findings in previous studies.47 67 68
We did not test pre-study health literacy, collect data on education levels nor did we make a neuropsychological assessment of the participating patients. This was abstained because we feared it could be a stressor that might influence performance. In retrospect, post-visit assessments of health literacy might have shed additional light on our findings. Finally, all the participating physicians were volunteers, and we do not know their baseline skills or motivation. Motivated physicians46 and physicians with lower skills benefit the most from training.69
Conclusion
We were able to demonstrate that a 3-hour course in providing complex information about treatment options to patients was sufficient to improve physicians’ ability to prioritise information. We found a significant negative association between the amount of information provided and recall rate, supporting previous findings that information provision should be limited to what is most relevant to the individual patient. Despite these effects, we could not demonstrate that patient recall rate improved significantly (p=0.099) in this study. There are still huge knowledge gaps in our understanding of what happens along all the steps from communication trainer to the physician to the patient’s recall, and further research is needed in this field.
Practice points
Patients with MS recalled less than 40% of information provided to them, and the recall percentage decreased the more information they received. Improving neurologists’ ability to enhance patients’ recall of complex information requires more extensive training than a 3-hour session including role-play practice.
Supplementary Material
Acknowledgments
We thank Reidun Førde and Henriette Høilund Kaupang for their contributions. We are grateful to Jonas Christoffer Lindstrøm for his contributions to this paper. We are grateful to the patients with MS and to the neurologists who have participated in this study.
Footnotes
Contributors: PG: Conception and design, methodology, material preparation, analysis and interpretation of data, writing—reviewing and editing, data curation. TH: Conception and design, methodology, material preparation, analysis and interpretation of data, writing—reviewing and editing. OT: Formal statistical analysis, analysis and interpretation of data, reviewing and editing. MN: Design, methodology, material preparation, analysis and interpretation of data, writing-reviewing and editing. JMN: Project administration, investigation, design, methodology, material preparation, data collection, analysis and interpretation of data, writing-original draft preparation, reviewing and editing, data curation, guarantor. All authors read and approved the final manuscript.
Funding: This work was supported by Stiftelsen Dam, previously named EkstraStiftelsen Helse og Rehabilitering, [grant number 7408].
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The data owner is Akershus University Hospital. Requests for anonymised data should be directed to coauthor Professor Pål Gulbrandsen.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants but the Regional Committee for Medical and Health Research Ethics (Southeast Norway) decided that this experiment is exempted from review (date: 24 March 2015). Reference ID # 2015/161 exempted this study. Participants gave informed consent to participate in the study before taking part.
References
- 1.Maarouf A, Boutière C, Rico A, et al. How much progress has there been in the second-line treatment of multiple sclerosis: a 2017 update. Rev Neurol 2018;174:429–40. 10.1016/j.neurol.2018.01.369 [DOI] [PubMed] [Google Scholar]
- 2.Pardo G, Jones DE. The sequence of disease-modifying therapies in relapsing multiple sclerosis: safety and immunologic considerations. J Neurol 2017;264:2351–74. 10.1007/s00415-017-8594-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myhr KM, Lehmann A.K:, Giæver A. Nasjonal faglig retningslinje for diagnostikk, attakk- OG sykdomsmodifiserende behandling AV multippel sklerose. Health NDo, 2017: 11–16. [Google Scholar]
- 4.de Ruiter J. Alignment in communication: towards a new theory of communication: Chpt. 5. In: Methodological paradigms in interaction research. Amsterdam; Philadelphia: John Benjamins Publishing Company, 2013: 24–5. [Google Scholar]
- 5.Heesen C, Kleiter I, Meuth SG, et al. Benefit-Risk perception of natalizumab therapy in neurologists and a large cohort of multiple sclerosis patients. J Neurol Sci 2017;376:181–90. 10.1016/j.jns.2017.03.001 [DOI] [PubMed] [Google Scholar]
- 6.Heesen C, Kasper J, Segal J, et al. Decisional role preferences, risk knowledge and information interests in patients with multiple sclerosis. Mult Scler 2004;10:643–50. 10.1191/1352458504ms1112oa [DOI] [PubMed] [Google Scholar]
- 7.Thorne S, Con A, McGuinness L, et al. Health care communication issues in multiple sclerosis: an interpretive description. Qual Health Res 2004;14:5–22. 10.1177/1049732303259618 [DOI] [PubMed] [Google Scholar]
- 8.Köpke S, Kern S, Ziemssen T, et al. Evidence-Based patient information programme in early multiple sclerosis: a randomised controlled trial. J Neurol Neurosurg Psychiatry 2014;85:411–8. 10.1136/jnnp-2013-306441 [DOI] [PubMed] [Google Scholar]
- 9.Somerset M, Campbell R, Sharp DJ, et al. What do people with MS want and expect from health-care services? Health Expect 2001;4:29–37. 10.1046/j.1369-6513.2001.00111.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Köpke S, Solari A, Rahn A, et al. Information provision for people with multiple sclerosis. Cochrane Database Syst Rev 2018;10:CD008757. 10.1002/14651858.CD008757.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zolnierek KBH, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care 2009;47:826–34. 10.1097/MLR.0b013e31819a5acc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kortman B. Patient recall and understanding of instructions concerning splints following a zone 2 flexor tendon repair. Aust Occup Ther J 1992;39:5–11. 10.1111/j.1440-1630.1992.tb01740.x21790640 [DOI] [Google Scholar]
- 13.Lewkovich GN, Haneline MT. Patient recall of the mechanics of cervical spine manipulation. J Manipulative Physiol Ther 2005;28:708–12. 10.1016/j.jmpt.2005.09.014 [DOI] [PubMed] [Google Scholar]
- 14.Pickney CS, Arnason JA. Correlation between patient recall of bone densitometry results and subsequent treatment adherence. Osteoporos Int 2005;16:1156–60. 10.1007/s00198-004-1818-8 [DOI] [PubMed] [Google Scholar]
- 15.McCarthy DM, Waite KR, Curtis LM, et al. What did the doctor say? health literacy and recall of medical instructions. Med Care 2012;50:277–82. 10.1097/MLR.0b013e318241e8e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sandberg EH, Sharma R, Sandberg WS. Deficits in retention for verbally presented medical information. Anesthesiology 2012;117:772–9. 10.1097/ALN.0b013e31826a4b02 [DOI] [PubMed] [Google Scholar]
- 17.Richard C, Glaser E, Lussier M-T. Communication and patient participation influencing patient recall of treatment discussions. Health Expect 2017;20:760–70. 10.1111/hex.12515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demaree HA, DeLuca J, Gaudino EA, et al. Speed of information processing as a key deficit in multiple sclerosis: implications for rehabilitation. J Neurol Neurosurg Psychiatry 1999;67:661–3. 10.1136/jnnp.67.5.661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol 2008;7:1139–51. 10.1016/S1474-4422(08)70259-X [DOI] [PubMed] [Google Scholar]
- 20.Bakirtzis C, Ioannidis P, Messinis L, et al. The rationale for monitoring cognitive function in multiple sclerosis: practical issues for clinicians. Open Neurol J 2018;12:31–40. 10.2174/1874205X01812010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grant I, McDonald WI, Trimble MR, et al. Deficient learning and memory in early and middle phases of multiple sclerosis. J Neurol Neurosurg Psychiatry 1984;47:250–5. 10.1136/jnnp.47.3.250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rao SM, Leo GJ, Bernardin L. Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology 1991;41:685–91. [DOI] [PubMed] [Google Scholar]
- 23.Rao JK, Anderson LA, Inui TS, et al. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care 2007;45:340–9. 10.1097/01.mlr.0000254516.04961.d5 [DOI] [PubMed] [Google Scholar]
- 24.Watson PWB, McKinstry B. A systematic review of interventions to improve recall of medical advice in healthcare consultations. J R Soc Med 2009;102:235–43. 10.1258/jrsm.2009.090013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Griffin SJ, et al. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med 2004;2:595–608. 10.1370/afm.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Back A. Patient-Physician communication in oncology: what does the evidence show? oncology (Williston Park) 2006;20:67–74. [PubMed] [Google Scholar]
- 27.Bertakis KD. The communication of information from physician to patient: a method for increasing patient retention and satisfaction. J Fam Pract 1977;5:217–22. [PubMed] [Google Scholar]
- 28.Ley P. Communicating with patients: improving communication. satisfaction and compliance. 11 New Fetter Lane, London EC4P 4EE: Croom Helm Ltd 1988;44. [Google Scholar]
- 29.Bradshaw PW, Ley P, Kincey JA. Recall of medical advice: comprehensibility and specificity. Br J Soc Clin Psychol 1975;14:55–62. 10.1111/j.2044-8260.1975.tb00149.x [DOI] [PubMed] [Google Scholar]
- 30.Reynolds PM, Sanson-Fisher RW, Poole AD, et al. Cancer and communication: information-giving in an oncology clinic. BMJ 1981;282:1449–51. 10.1136/bmj.282.6274.1449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Langewitz W, Ackermann S, Heierle A, et al. Improving patient recall of information: harnessing the power of structure. Patient Educ Couns 2015;98:716–21. 10.1016/j.pec.2015.02.003 [DOI] [PubMed] [Google Scholar]
- 32.Siegrist V, Langewitz W, Mata R, et al. The influence of information structuring and health literacy on recall and satisfaction in a simulated discharge communication. Patient Educ Couns 2018;101:2090–6. 10.1016/j.pec.2018.08.008 [DOI] [PubMed] [Google Scholar]
- 33.Lehmann V, Labrie NHM, van Weert JCM, et al. Provider caring and structuring treatment information to improve cancer patients' recall: does it help? Patient Educ Couns 2020;103:55–62. 10.1016/j.pec.2019.07.011 [DOI] [PubMed] [Google Scholar]
- 34.Lehmann V, Labrie NHM, van Weert JCM, et al. Tailoring the amount of treatment information to cancer patients' and survivors' preferences: effects on patient-reported outcomes. Patient Educ Couns 2020;103:514–20. 10.1016/j.pec.2019.09.024 [DOI] [PubMed] [Google Scholar]
- 35.Anderson JL, Dodman S, Kopelman M, et al. Patient information recall in a rheumatology clinic. Rheumatol Rehabil 1979;18:18–22. 10.1093/rheumatology/18.1.18 [DOI] [PubMed] [Google Scholar]
- 36.Pugh KJ, Bergin DA, Pugh B. Motivational influences on transfer. Educ Psychol 2006;41:147–60. 10.1207/s15326985ep4103_2 [DOI] [Google Scholar]
- 37.Bol N, Smets EMA, Burgers JA, et al. Older patients' recall of online cancer information: do ability and motivation matter more than chronological age? J Health Commun 2018;23:9–19. 10.1080/10810730.2017.1394400 [DOI] [PubMed] [Google Scholar]
- 38.Apsler R, Sears DO, Warning SDO. Warning, personal involvement, and attitude change. J Pers Soc Psychol 1968;9:162–6. 10.1037/h0021248 [DOI] [PubMed] [Google Scholar]
- 39.Ø M. Annual Hospital Board Document, Akershus University Hospital Board, Norway. In:. 2. Board AUH, 2018. [Google Scholar]
- 40.Dörr J, Paul F. The transition from first-line to second-line therapy in multiple sclerosis. Curr Treat Options Neurol 2015;17:354. 10.1007/s11940-015-0354-5 [DOI] [PubMed] [Google Scholar]
- 41.Torkildsen Ø, Myhr K-M, Bo L. Disease-modifying treatments for multiple sclerosis - a review of approved medications. Eur J Neurol 2016;23:18–27. 10.1111/ene.12883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gorelik L, Lerner M, Bixler S, et al. Anti-JC virus antibodies: implications for PML risk stratification. Ann Neurol 2010;68:295–303. 10.1002/ana.22128 [DOI] [PubMed] [Google Scholar]
- 43.Plavina T, Subramanyam M, Bloomgren G, et al. Anti-JC virus antibody levels in serum or plasma further define risk of natalizumab-associated progressive multifocal leukoencephalopathy. Ann Neurol 2014;76:802–12. 10.1002/ana.24286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwab N, Schneider-Hohendorf T, Pignolet B, et al. Therapy with natalizumab is associated with high JCV seroconversion and rising JCV index values. Neurol Neuroimmunol Neuroinflamm 2016;3:e195. 10.1212/NXI.0000000000000195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reuwer AQ, Heron M, van der Dussen D, et al. The clinical utility of JC virus antibody index measurements in the context of progressive multifocal leukoencephalopathy. Acta Neurol Scand 2017;136:37–44. 10.1111/ane.12840 [DOI] [PubMed] [Google Scholar]
- 46.Fossli Jensen B, Gulbrandsen P, Dahl FA, et al. Effectiveness of a short course in clinical communication skills for hospital doctors: results of a crossover randomized controlled trial (ISRCTN22153332). Patient Educ Couns 2011;84:163–9. 10.1016/j.pec.2010.08.028 [DOI] [PubMed] [Google Scholar]
- 47.Ley P, Bradshaw PW, Eaves D, et al. A method for increasing patients' recall of information presented by doctors. Psychol Med 1973;3:217–20. 10.1017/S0033291700048558 [DOI] [PubMed] [Google Scholar]
- 48.Kreuter MW, Bull FC, Clark EM, et al. Understanding how people process health information: a comparison of tailored and nontailored weight-loss materials. Health Psychol 1999;18:487–94. 10.1037/0278-6133.18.5.487 [DOI] [PubMed] [Google Scholar]
- 49.Albada A, Ausems MGEM, Bensing JM, et al. Tailored information about cancer risk and screening: a systematic review. Patient Educ Couns 2009;77:155–71. 10.1016/j.pec.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 50.Nordfalk JM, Gulbrandsen P, Gerwing J, et al. Development of a measurement system for complex oral information transfer in medical consultations. BMC Med Res Methodol 2019;19:139. 10.1186/s12874-019-0788-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Degner LF, Sloan JA, Venkatesh P. The control preferences scale. Can J Nurs Res 1997;29:21–43. [PubMed] [Google Scholar]
- 52.Elwyn G, Barr PJ, Grande SW, et al. Developing collaborate: a fast and frugal patient-reported measure of shared decision making in clinical encounters. Patient Educ Couns 2013;93:102–7. 10.1016/j.pec.2013.05.009 [DOI] [PubMed] [Google Scholar]
- 53.Barr PJ, Thompson R, Walsh T, et al. The psychometric properties of collaborate: a fast and frugal patient-reported measure of the shared decision-making process. J Med Internet Res 2014;16:e2. 10.2196/jmir.3085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gulbrandsen P, Krupat E, Benth JS, et al. "Four Habits" goes abroad: report from a pilot study in Norway. Patient Educ Couns 2008;72:388–93. 10.1016/j.pec.2008.05.012 [DOI] [PubMed] [Google Scholar]
- 55.Fossli Jensen B, Gulbrandsen P, Benth JS, et al. Interrater reliability for the four habits coding scheme as part of a randomized controlled trial. Patient Educ Couns 2010;80:405–9. 10.1016/j.pec.2010.06.032 [DOI] [PubMed] [Google Scholar]
- 56.Col NF, Solomon AJ, Springmann V, et al. Whose preferences matter? A patient-centered approach for eliciting treatment goals. Med Decis Making 2018;38:44–55. 10.1177/0272989X17724434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Szmuilowicz E, el-Jawahri A, Chiappetta L, et al. Improving residents' end-of-life communication skills with a short retreat: a randomized controlled trial. J Palliat Med 2010;13:439–52. 10.1089/jpm.2009.0262 [DOI] [PubMed] [Google Scholar]
- 58.Clayton JM, Butow PN, Waters A, et al. Evaluation of a novel individualised communication-skills training intervention to improve doctors' confidence and skills in end-of-life communication. Palliat Med 2013;27:236–43. 10.1177/0269216312449683 [DOI] [PubMed] [Google Scholar]
- 59.Tarn DM, Paterniti DA, Orosz DK, et al. Intervention to enhance communication about newly prescribed medications. Ann Fam Med 2013;11:28–36. 10.1370/afm.1417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kasper J, Liethmann K, Heesen C, et al. Training doctors briefly and in situ to involve their patients in making medical decisions-Preliminary testing of a newly developed module. Health Expect 2017;20:1254–63. 10.1111/hex.12565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ley P, Spelman MS. Communications in an out-patient setting. Br J Soc Clin Psychol 1965;4:114–6. 10.1111/j.2044-8260.1965.tb00449.x [DOI] [PubMed] [Google Scholar]
- 62.Kampman MT, Aarseth JH, Grytten N, et al. Sex ratio of multiple sclerosis in persons born from 1930 to 1979 and its relation to latitude in Norway. J Neurol 2013;260:1481–8. 10.1007/s00415-012-6814-x [DOI] [PubMed] [Google Scholar]
- 63.Cegala DJ, Lenzmeier Broz S, Broz SL. Physician communication skills training: a review of theoretical backgrounds, objectives and skills. Med Educ 2002;36:1004–16. 10.1046/j.1365-2923.2002.01331.x [DOI] [PubMed] [Google Scholar]
- 64.van Weel-Baumgarten E, research Ilinking. Is linking research, teaching and practice in communication in health care the way forward? Patient Educ Couns 2016;99:1441–5. 10.1016/j.pec.2016.07.011 [DOI] [PubMed] [Google Scholar]
- 65.Nordfalk JM, Menichetti J, Thomas O, et al. Three strategies when physicians provide complex information in interactions with patients: how to recognize and measure them. Patient Educ Couns 2021. 10.1016/j.pec.2021.10.013. [Epub ahead of print: 13 Oct 2021]. [DOI] [PubMed] [Google Scholar]
- 66.Nordfalk JM, Gulbrandsen P, Gerwing J, et al. Development of a measurement system for complex oral information transfer in medical consultations. BMC Med Res Methodol 2019;19:139–48. 10.1186/s12874-019-0788-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McGuire LC. Remembering what the doctor said: organization and adults' memory for medical information. Exp Aging Res 1996;22:403–28. 10.1080/03610739608254020 [DOI] [PubMed] [Google Scholar]
- 68.Lundervold AJ, Wollschläger D, Wehling E. Age and sex related changes in episodic memory function in middle aged and older adults. Scand J Psychol 2014;55:225–32. 10.1111/sjop.12114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bylund CL, Banerjee SC, Bialer PA, et al. A rigorous evaluation of an institutionally-based communication skills program for post-graduate oncology trainees. Patient Educ Couns 2018;101:1924–33. 10.1016/j.pec.2018.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The data owner is Akershus University Hospital. Requests for anonymised data should be directed to coauthor Professor Pål Gulbrandsen.