Abstract
Objectives
To identify the intergender variation of on-scene time (OST) for highly urgent emergency cases conveyed by emergency medical services (EMS) in Saudi Arabia and to assess other predictors of OST and hypothesise for possible factors delaying OST.
Design
A retrospective population-based registry study.
Setting
Riyadh Province is the largest province in terms of population and the second in terms of geographical area.
Participants
All highly urgent transported patients from the scene to emergency departments, be they medical emergencies or trauma emergencies during 2018.
Outcome measure
OST difference between men and women transported by EMS.
Results
In total, 21 878 patients were included for analysis: 33.9% women and 66.1% men. The median OST for women was 22 min (IQR 15–30) and 18 min (IQR 11–26) for men (p<0.001); for medical cases, median OST was 23 min (IQR 16–31) for women compared with 20 min (IQR 13 – 29) for men (p<0.001); for trauma cases, the median OST of both sexes was equal. We found the following additional predictors of OST: factors of emergency type, sex, age category, geographical areas, type of ambulance vehicle and hospital type were all significantly associated with OST in the crude or adjusted analyses. Factors of emergency type, sex, age category, geographical areas, type of ambulance vehicle and hospital type were also significantly associated with the odds of OST of more than 15 min in the crude and adjusted regression analyses.
Conclusions
The median OST was longer than 15 min for more than half of transported cases. For medical cases, women had a longer median OST than men. Additional predictors associated with prolonged OST were the patient’s age, area (ie, urban vs rural), type of ambulance vehicle and season. These findings are hypothesis generating and require further studies.
Keywords: ACCIDENT & EMERGENCY MEDICINE, HEALTH SERVICES ADMINISTRATION & MANAGEMENT, Health policy, PUBLIC HEALTH
Strengths and limitations of this study.
It is the first study conducted in the Arabian Gulf States that includes a large number of highly urgent cases.
The registry relies on the Saudi Red Crescent Computerised Aid Dispatching system for automated detection of time to compute the timeline.
Using registry data has provided us with much statistical power to detect between-group differences and associations for the available characteristics.
Registry lacks other important demographic factors related to social status: education, income and ethnicity, which might be associated with prolonged on-scene time.
Time registered in the database depends on the information provided by emergency medical services providers through wireless communications with the call centre; hence, any network failure leads to missed data.
Introduction
Emergency medical services (EMS) in Saudi Arabia have been well developed during the last decade. They provide different levels of emergency care around the clock and free of charge. Women’s lower EMS use is one of the challenges found; besides, the median total EMS time for highly urgent emergency cases was found to be greater than 1 hour.1 2 The on-scene time (OST) duration may take greater than half of the total period of EMS time and made up the largest proportion of total EMS delays.3 4 Long OST may lead to consequences affecting patient outcomes.5 6 In certain medical circumstances, patients’ transportation to a hospital as soon as possible is highly recommended.7–10 In the American Heart Association (AHA) guideline for the early management of patients who had a stroke, it is recommended that the OST should not exceed 15 min.7
The OST duration can result from the crews’ decision to collect patient history and medical examination.11 In addition, the period of OST varies according to the patient’s status with or without mortality and geographical areas as urban or rural locations. Sex may also play a factor in OST. For example, a US study found that OST in women complaining of acute chest pain was higher than that in men as the crew needed more time to apply ECG.12 Other barriers often prolong OST, particularly in trauma cases, when EMS providers’ accessibility to patients is difficult. These barriers can be considered inevitable causes such as waiting for the police to arrive in an incident resulting from criminal causes or waiting for the fire brigade to extract a patient from a vehicle or a building. It can also be affected in an outdoor address such as the street during a mass gathering after road traffic accidents.11 13 On the other hand, it can result from patient wishes and family intervention in crews’ performance and decision, especially when the crew is called to a patient’s house. Such intervention is significantly affected by culture and educational level and might differ between urban and rural areas.
Factors related to patient culture or demography that influence OST have not been thoroughly studied in the Arabian Gulf States. A recent systematic review found that EMS crews in Saudi Arabia consider mass gathering during road traffic accidents as one of the most frequent barriers affecting their performance to work effectively and in a timely manner, while the presence of the patients’ families or bystanders was cited as the second salient barrier.2 14 Furthermore, the median of total EMS time in the Riyadh Province of Saudi Arabia for trauma cases was longer in rural areas than in urban areas, and longer than what was found in other countries such as Denmark and the USA.1 15 16
The present study aimed to investigate OST and to identify differences between sexes regarding the amount of time spent at the scene by EMS crews. It also aims to identify other patient-related factors associated with time spent at the scene for all highly urgent emergency cases that were transported to healthcare facilities in the Riyadh Province in Saudi Arabia and to hypothesise for possible factors delaying OST.
Methods
Design
This retrospective population-based registry was conducted in the Riyadh Province of Saudi Arabia by using all EMS database records in the Saudi Red Crescent Computer Aid Dispatching (SRCCAD) system from 1 January to 31 December 2018. This study complies with Strengthening the Reporting of Observational Studies in Epidemiology.17
Setting
Riyadh Province is in the central part of Saudi Arabia. It has a geographical size of 404 240 km2. It has an approximate population of 6 792 776 million, according to the last national census. The province is composed of 39 different cities and Riyadh city is the capital and the largest city in Saudi Arabia. Besides, there are hundreds of rural villages dotted between or near these cities.18 In Saudi Arabia, EMS are free of charge and can be accessed by calling the call centre, and in certain exceptional conditions, patients can visit ambulance stations distributed all over the province, including along highways. EMS crews of Riyadh Province are mainly composed of two emergency medical technicians (EMTs). They are trained on basic life support (BLS) skills to respond to different levels of emergency cases but do not administer medicine. However, some crews are composed of physicians and emergency paramedics. These are called mobile intensive care units (MICUs) and respond to certain highly critical cases and provide advanced life support (ALS). A third type of EMS crew consists of senior paramedics and are dispatched in a rapid response non-transporting vehicle (RRNTV). These often arrive earlier to provide ALS before the essential transporting ambulances. Time indicators are built-in SRCCAD with 20 min for response time and 15 min for OST regardless of urgency level.
Saudi EMS implements a strategy of scoop and run, which emanated from the Anglo-American model. Most EMS chain periods are limited with a predefined time to end with the golden hour of total time.19 The OST comprises three consecutive periods which are access, treatment and loading time.20 Access time starts from ambulance vehicles’ arrival to the scene up to crew arrival to patients’ location. Treatment time is the period of patients’ examination and treatment. Loading time starts from moving patients on the stretcher until the crew starts to travel to the hospital. The policy underpinning this 15 min benchmark for OST is that the Saudi EMS policymakers, based on the number of available crews and the volume of patients’ demands, decided that 15 min at the scene fit their operational procedures as a policy target. An additional consideration was to avoid delaying ambulance resources from becoming unavailable for new assignments.
However, when there are multiple calls for different emergencies at once, SRCCAD may prioritise cases based on three levels of urgency and dispatch crews accordingly. Patients or their families who have guardianship have the right to refuse transportation to hospital after they have signed a formal paper of refusal against medical advice. However, EMS crews can either transport patients to the closest hospitals or treat them at the scene.
Participants and public involvement
Patients and the public were not involved in developing the research question, commenting on the database, study design, outcome measures, conduct of the study, or contributing to the writing or editing of this study.
Data collection
The data were obtained through the operations and information department in the Riyadh branch directorate of Saudi Red Crescent Authority. Data were exported from Microsoft Excel (V 16.58) saved in an encrypted file on a hard disc and converted to an IBM SPSS file V.25 for further analyses.
Selection of participants
According to the Saudi EMS definition, highly urgent emergency cases are the cases that contacted EMS for support after exposure to serious or life-threatening illness or injuries that require immediate medical intervention and quick transportation to hospital emergency departments (EDs). In this study, all incoming calls for patients who were triaged at the dispatching centre of SRCCAD as highly urgent emergency cases were included. Gynaecological emergencies were excluded because of the scope of the study to compare both sexes. In addition, we excluded records of patients for whom age, sex or area was missing and cases categorised by the SRCCAD as cases ended by non-conveyance. We considered the potential source of bias; therefore, we excluded the lower extreme outliers with values equal to zero due to system error. Records of missions dispatched for two patients or more in one incident were excluded. Similarly, missions that involved only an RRNTV were also removed.
Methods of measurement
We included all variables related to patient demographics and information related to dispatching missions from the time period perspective, starting from calling the call centre and ending with the patients’ arrival to private and governmental hospitals. The EMS time intervals are composed of four different periods21: first, the response time, which is the time elapsed starting from receiving a call in the call centre and ending by the ambulance’s crew’s arrival to the scene; second, the OST, which is the time elapsed, starting from arrival to the scene and ending by starting to travel back to EMS centre or travelling forward toward healthcare facilities; third, the travel time, which is the time elapsed from starting to move from the scene until the crew’s arrival to healthcare facilities; and fourth is the hospital period, defined as the time elapsed from arrival to the healthcare facility until handover to emergency room staff. EMS database registry recorded all events starting from activation time and ending by the crew’s departure from the hospitals in the cases where the patient had been transported or when the crew leaves the scene when transportation had been refused. It measures only response time period and total EMS time period in seconds. Therefore, the total EMS time in this study reflects the four periods. We calculated the OST, travel time and hospital time according to standard EMS definition.21 Those periods in Saudi EMS have individual target indicators, such as the response time, 20 min; the OST is 15 min, while the travel time has no indicator because of EMS providers’ and patients’ safety issue arise if the time indicator is too strict due to the risk of driving too fast on the way to the hospital. Saudi EMS would consider the OST if it exceeded 15 min as a prolonged OST. In cases where the call centre dispatched two or more EMS crews, we selected by calculating the actual time spent with the patient from when the first crew arrived either the RRNTV or the main transporting ambulance until the patient was transported by ambulance.
In this study, we focused only on the EMS missions that had been registered by SRCCAD as highly urgent and ended by transporting patients into hospitals. Therefore, we clustered emergency cases into two cohorts. The first cohort was the cluster of EMS mission that were dispatched for highly urgent medical emergencies (HUMEs) such as acute coronary syndrome, stroke and out-of-hospital cardiac arrest. The second cohort was the missions dispatched for highly urgent trauma emergencies (HUTE) such as road traffic accidents. Demographic features available in the registry that were extracted were sex, age and geographical area. Patients’ age was divided into three categories according to Saudi Arabian law: child: patient with an age below 15 years old, adult: patient equal to or over 15 years old but younger than 60 years old, and elderly: patient equal to or more than 60 years old. Urban area was defined as an area where metropolitan and micropolitan cities are located and have a total population of equal to or more than 5000 inhabitants. On the other side, areas with less than 5000 people or outside urban geographical area were considered rural.
We considered the differences in various EMS operational times from the data collected in a 1-year time period. In Saudi Arabia, the weekdays are considered from Sunday to Thursday, while Friday and Saturday are the weekends. Period of the day is categorised into two categories: office time, which is the time that starts from 08:00 to 16:00 from Sunday to Thursday, while the home time is defined as the time that starts from 16:01 on the same day up to the next day 07:59 side by side with 48 hours of the weekend Friday and Saturday. Working shifts are the two daily periods that Saudi EMS schedules to provide emergency services. It is composed of two periods: the day shift from 08:00 to 20:00 and the night shift from 20:00 to 08:00. We also included season. The winter season officially starts from mid-December to mid-March, then the spring, which starts from mid-March to mid-June. Summer starts from mid-June to mid-December, followed by autumn, which starts from mid-21 September and ends by mid-December.22
Operating vehicle types represented by the three types of crews providing EMS for the clustered emergencies were included. The first, ambulance type II transporting vehicle (BLS ambulance) is the vehicle equipped by two EMTs, who can perform BLS and rapid patient transport to hospitals. MICU is another transporting vehicle capable of highly qualified physician-based or paramedics exposed to long-term training equal to or more than 4 years. The last type of vehicle is RRNTV, which is operated in the last decade to arrive at the scene earlier than the transporting vehicle, and it is also operated by highly experienced EMS providers, often EMS paramedics. The crew of RRNTV can give ALS and do the necessary medical work to prepare the patients to be transported. Hospitals that receive emergency patients are of two types. We also included EDs based on the two types of hospitals. Governmental hospitals are non-profit healthcare organisations funded by the Saudi authorities to provide health services for all Saudi citizens. Private hospitals are for-profit healthcare organisations operated by non-governmental healthcare firms for healthcare services.
Statistical analysis
The median and IQR were computed for response time, OST, travel time, hospital time and total EMS time, and compared between men and women using the Mann-Whitney U test. The Kruskal-Wallis and Mann-Whitney U test were conducted to test for differences in OST based on different demographics related to patients, stratified by sex. The following factors were considered: age category, geographical area, period of requesting EMS services, season, emergency type (medical or trauma), emergency vehicles and type of hospital to which the patient was transferred.
To assess what variables were associated with OST, first simple linear regression was performed to identify the OST difference between different independent predictive variables. After that, multivariable linear regression was used to identify which variables were independently associated with OST.
Furthermore, we conducted logistic regression to assess the association between variables and the odds of an OST of more than 15 min based on the SRCCAD indicator. Data were presented as ORs with 95% CIs. We considered p values of <0.05 as statistically significant.
Results
Characteristics of study subjects
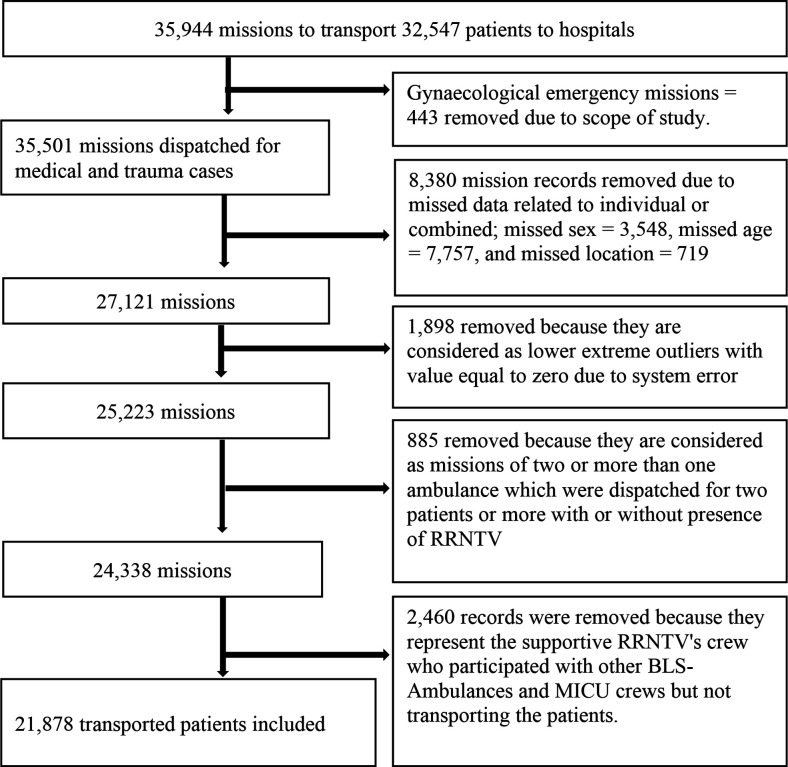
During the study period, 35 944 missions of two types—transporting and non-transporting vehicles—were dispatched to the scene. RRNTV accounted for 3397 (9.5%) missions, while the transporting vehicles were 32 547 (90.5%); BLS ambulance 25 988 (72.3%) and MICU 6559 (18.2%). Subsequently, 32 547 high emergency patients were transported to Riyadh Province hospitals.
Figure 1 presents the flowchart of the transported patients. The study exclusion criteria of records removal showed that 443 missions records were excluded because of gynaecological emergencies, and 8380 missions’ records were removed due to missing data related to sex, age and geographical area. Given to lower extreme outliers that registered the OST as a zero-value due to system errors, 1898 missions’ records were excluded to avoid bias. Therefore, 24 338 missions that represented 21 878 transported patients were initially included. However, 2460 additional records were excluded because they represented supportive RRNTV’s crews who participated as logistic support side by side to BLS ambulance crews, which were the primary transporting ambulances of the patients. Subsequently, 21 878 missions of highly urgent emergency patients were included in this study. We found that 14 454 (66.1%) of cases were male. In total, 14 454 (66.1%) missions were for HUME, and 7424 (33.9%) were for HUTE. Of all, 66.5% of cases were attended at the scene by BLS ambulance crews, 22.3% by MICU ambulances crews and 11.2% by two crews; 50% of them are RRNTVs, and the remaining 50% were BLS ambulances.
Figure 1.
Flowchart of included and excluded patients. BLS, basic life support; MICU, mobile intensive care unit; RRNTV, rapid response non-transporting vehicle.
Main results
Table 1 shows time periods of ambulance service runs, including response time, OST, travel time, and hospital time. The study showed that each duration of OST and travel time for the HUME cohort significantly differed between men and women. The median OST of HUME for women 23 min (IQR 16–31 min) was significantly longer than men 20 min (IQR 13–29 min), p<0.001. The median travel time for women 19 min (IQR 10–29 min) was significantly longer than men 18 min (IQR 10–29 min), p<0.001.
Table 1.
Consecutive time periods of EMS urgent missions according to the two clustered emergency case cohorts for 21 878 transported patients
| EMS intervals | Emergency type |
Male | Female | ||
| n | Median (IQR) | n | Median (IQR)* | ||
| Response time | HUM emergencies |
8686 | 17.0 (12.5–23.2) | 6912 | 17.0 (12.6–23.1) |
| HUT emergencies |
5768 | 15.7 (11.2–22.0) | 512 | 15.6 (11.5–21.5) | |
| On-scene time | HUM emergencies |
8686 | 20.0 (13.0–29.0) | 6912 | 23.0 (16.0–31.0)† |
| HUT emergencies |
5768 | 15.0 (9.0–21.0) | 512 | 15.0 (10.0–22.0) | |
| Travel time | HUM emergencies |
8686 | 18.0 (10.0–29.0) | 6912 | 19.0 (11.0–31.0)† |
| HUT emergencies |
5768 | 19.0 (11.0–30.0) | 512 | 18.0 (12.0–30.0) | |
| Hospital time | HUM emergencies |
8686 | 17.0 (6.0–27.0) | 6912 | 16.0 (5.0–27.0) |
| HUT emergencies |
5768 | 18.0 (6.0–28.0) | 512 | 17.0 (6.0–29.0) | |
| Total EMS time |
HUM emergencies |
8686 | 79.3 (63.7–97.1) | 6912 | 82.8 (67.0–99.8)† |
| HUT emergencies |
5768 | 73.8 (58.0–92.3) | 512 | 74.7 (60.8–91.5) | |
*Mann-Whitney U Test
†Statistically significant difference at a p value of <0.05
EMS, emergency medical services; HUM, highly urgent medical; HUT, highly urgent trauma.
Table 2 shows the median and IQR stratified by patients’ demographic and background factors for both HUTE and HUME causes. The total median OST was significantly longer for women 22 min (IQR 15–30 min) than men 18 min (IQR 11–26 min), p=0.001. Most differences related to OST between men and women were significant, all showing longer OST for women. In addition, all characteristics variables of patients and missions except the daily hours, weekdays, and working shifts were statistically significant among each group of men and women.
Table 2.
Median on-scene time difference between sexes for high urgent transported patients (N=21 878)
| Male | Female | |||
| n (%) | Median (IQR)* | n (%) | Median (IQR)*,† | |
| Patients (no./N) | 14 454 (66.1) | 18.0 (11.0–26.0) | 7424 (33.9) | 22.0 (15.0–30.0)** |
| Emergency type | ||||
| HUME | 8686 (60.1) | 20.0 (13.0–29.0)†† | 6912 (93.1) | 23.0 (16.0–31.0)‡‡ |
| HUTE | 5768 (39.9) | 15.0 (9.0–21.0)†† | 512 (6.9) | 15.0 (10.0–22.0)†† |
| Age category | ||||
| Child <15 | 550 (3.8) | 14.5 (9.0–22.0)†† | 267 (3.6) | 18.0 (11.0–25.0)‡‡ |
| Adult 15–<60 | 9803 (67.8) | 16.0 (10.0–24.0)†† | 3299 (44.4) | 21.0 (14.0–29.0)‡‡ |
| Elderly ≥60 | 4101 (28.4) | 22.0 (15.0–30.0)†† | 3858 (52.0) | 23.0 (17.0–31.0)‡‡ |
| Scene location | ||||
| Urban | 13 562 (93.8) | 18.0 (12.0–26.0)†† | 7238 (97.5) | 22.0 (16.0–30.0)‡‡ |
| Rural | 892 (6.2) | 11.0 (6.0–19.0)†† | 186 (2.5) | 15.0 (9.0–21.0)‡‡ |
| Daily hours | ||||
| Home time | 10 901 (75.4) | 18.0 (11.0–26.0) | 5433 (73.2) | 22.0 (15.0–30.0)** |
| Office time | 3553 (24.6) | 18.0 (11.0–26.0) | 1991 (26.8) | 22.0 (15.0–30.0)** |
| Week days | ||||
| Sunay–Thursday | 10 300 (71.3) | 18.0 (11.0–26.0) | 5333 (71.8) | 22.0 (15.0–30.0)** |
| Weekend | 4152 (28.7) | 18.0 (11.0–26.0) | 2091 (28.2) | 22.0 (15.0–30.0)** |
| Working shift | ||||
| Day shift | 6770 (46.8) | 18.0 (11.0–26.0) | 3652 (49.2) | 22.0 (15.0–30).0** |
| Night shift | 7684 (53.2) | 18.0 (11.0–26.0) | 3772 (50.8) | 22.0 (15.0–30.0)** |
| Season | ||||
| Winter | 3512 (24.3) | 19.0 (12.0–27.0)†† | 1901 (25.6) | 23.0 (16.0–31.0)‡‡ |
| Spring | 3583 (24.8) | 18.0 (11.0–26.0)†† | 1756 (23.7) | 22.0 (15.0–30.0)‡‡ |
| Summer | 3573 (24.7) | 17.0 (11.0–25.0)†† | 1771 (23.9) | 22.0 (15.0–30.0)‡‡ |
| Autumn | 3786 (26.2) | 18.0 (12.0–25.0)†† | 1996 (26.9) | 22.0 (15.0–29.0)‡‡ |
| Vehicle types | ||||
| BLS | 9722 (67.3) | 17.0 (10.0–24.0)†† | 4817 (64.9) | 21.0 (14.0–29.0)‡‡ |
| MICU | 3204 (22.2) | 20.0 (13.0–28.0)†† | 1675 (22.6) | 24.0 (17.0–31.0)‡‡ |
| Two crews‡ | 1528 (10.6) | 22.0 (16.0–30.0)†† | 932 (12.6) | 25.0 (19.0–33.0)‡‡ |
| Receiving EDs | 14 391§ | 7402¶ | ||
| Governmental | 12 165 (84.2) | 18.0 (11.0–26.0)†† | 6271 (84.5) | 22.0 (15.0–30.0)‡‡ |
| Private | 2226 (15.4) | 19.0 (13.0–28.0)†† | 1131 (15.2) | 23.0 (17.0–31.0)‡‡ |
*Kruskal-Wallis test.
†Mann-Whitney test.
‡Missions attended by rapid response non-transporting vehicles and the essential transporting vehicle.
§63 removed because of undocumented hospital.
¶22 removed because of undocumented hospital.
**Statistically significance at p-value <0.05 between groups.
††Statistically significant at a p value of <0.05 within groups.
‡‡Statistically significant at a p value of <0.05 within groups and between groups.
BLS, basic life support; ED, emergency department; HUME, highly urgent medical emergency; HUTE, highly urgent trauma emergency; MICU, mobile intensive care unit.
Table 3 illustrates the association between different variables and OST. Emergency type, sex, age category, geographical areas, types of vehicles and hospital type were all significantly associated with OST in the crude or adjusted analyses. When adjusted for other variables, all besides working hours were retained in the model.
Table 3.
Simple linear and multivariable linear regression of on-scene time according to different predictors (N=21 878)
| Predictors’ variable | n (%) | Crude | Adjusted |
| Regression coefficient (95% CI) |
Regression coefficient (95% CI) |
||
| Emergency type (ref), n/N (%) | |||
| HUME | 15 598 (71.3) | ||
| HUTE | 6280 (28.7) | −6.5 (−6.9 to −6.1)‡ | −4.2 (−4.6 to −3.8)‡ |
| Sex (ref), n/N (%) | |||
| Male | 14 454 (66.1) | ||
| Female | 7424 (33.9) | 3.9 (3.6 to 4.3)‡ | 1.8 (1.5 to 2.2)‡ |
| Age category (ref), n/N (%) | |||
| Adult | 13 102 (59.9) | ||
| Child (<15) | 817 (3.7) | −1.5 (−2.4 to −0.5)‡ | −2.3 (−3.2 to −1.4)‡ |
| Elderly (≥60) | 7959 (36.4) | 4.7 (4.3 to 5.1)† | 2.1 (1.7 to 2.5)‡ |
| Scene location (ref), n/N (%) | |||
| Urban | 20 800 (95.1) | ||
| Rural | 1078 (4.9) | −5.5 (−6.3 to −4.7)‡ | −2.6 (−3.4 to −1.8)‡ |
| Daily hours (ref), n/N (%) | |||
| Home time | 16 334 (74.7) | ||
| Office time | 5544 (25.3) | 0.5 (0.15 to 0.95)‡ | 0.4 (−0.1 to 1.0) |
| Seven days (ref), n/N (%) | |||
| Weekdays | 15 633 (71.5) | ||
| Weekend | 6245 (28.5) | −0.2 (−0.4 to 0.4) | 0.2 (−0.2 to 0.6) |
| Working shift (ref), n/N (%) | |||
| Day shift | 10 422 (47.6) | ||
| Night shift | 11 456 (52.4) | −0.5 (−0.84 to −0.14)‡ | −0.1 (−0.5 to 0.3) |
| Season (ref), n/N (%) | |||
| Summer | 5344 (24.4) | ||
| Winter | 5413 (24.8) | 1.4 (0.9 to 1.9)‡ | 0.8 (0.3 to 1.2)‡ |
| Spring | 5339 (24.4) | 0.3 (−0.2 to 0.8) | 0.1 (−0.3 to 0.6) |
| Autumn | 5782 (26.4) | 0.2 (0.3 to 0.6) | −0.2 (−0.7 to 0.3) |
| Ambulance vehicle (ref), n/N (%) | |||
| BLS | 14 539 (66.5) | ||
| MICU | 4879 (22.3) | 2.8 (2.3 to 3.2)‡ | 2.3 (1.9 to 2.7)‡ |
| Two crews* | 2460 (11.2) | 4.9 (4.4 to 5.5)‡ | 3.7 (3.2 to 4.3)‡ |
| Receiving EDs† (ref), n/N (%) | |||
| Governmental | 18 436 (84.6) | ||
| Private | 3357 (15.4) | 1.6 (1.1 to 2.0)‡ | 0.9 (0.5 to 1.4)‡ |
*Missions attended by rapid response non-transporting vehicles and the essential transporting vehicle.
†85 records of undocumented hospitals were removed and not counted.
‡Statistically significant at a p value of <0.05.
BLS, basic life support; EDs, emergency department; HUME, highly urgent medical emergency; HUTE, highly urgent trauma emergency; MICU, mobile intensive care unit.
We found that 59.4% of men had an OST of more than 15 min compared with 75% for women (p<0.001). Table 4 shows the findings of the crude and adjusted logistic regression models. Emergency type, sex, age category, geographical areas, types of vehicles and hospital type were all significantly associated with the odds of OST of more than 15 min, both in crude and adjusted models.
Table 4.
Association of predictor variable and on-scene time longer than 15 min (N=21 878)
| Predictive variable | n (%) | Crude OR (95% CI) | Adjusted OR (95% CI) |
| Emergency type (ref), n/N (%) | |||
| HUME | 15 598 (71.3) | ||
| HUTE | 6280 (28.7) | 0.3 (0.3 to 0.4)‡ | 0.5 (0.47 to 0.55)‡ |
| Sex (ref), n/N (%) | |||
| Male | 14 454 (66.1) | ||
| Female | 7424 (33.9) | 2.0 (1.9 to 2.2)‡ | 1.4 (1.3 to 1.5)‡ |
| Age category (ref), n/N (%) | |||
| Adult | 13 102 (59.9) | ||
| Child (<15) | 817 (3.7) | 0,72 (0.63 to 0.83)‡ | 0.61 (0.5 to 0.7)‡ |
| Elderly (≥60) | 7959 (36.4) | 2.5 (2.4 to 2.70)‡ | 1.7 (1.6 to 1.8)‡ |
| Scene location (ref), n/N (%) | |||
| Urban | 20 800 (95.1) | ||
| Rural | 1078 (4.9) | 0.3 (0.3 to 0.3)‡ | 0.5 (0.4 to 0.6)‡ |
| Daily hours (ref), n/N (%) | |||
| Home time | 16 334 (74.7) | ||
| Office time | 5544 (25.3) | 1.05 (1.0 to 1.1) | 1.0 (0.9 to 1.1) |
| Seven days (ref), n/N (%) | |||
| Weekdays | 15 633 (71.5) | ||
| Weekend | 6245 (28.50 | 1.0 (0.9 to 1.0) | 1.0 (0.9 to 1.0) |
| Working shift (ref), n/N (%) | |||
| Day shift | 10 422 (47.6) | ||
| Night shift | 11 456 (52.4) | 1.0 (0.9 to 1.0) | 1.0 (0.9 to 1.1) |
| Season (ref), n/N (%) | |||
| Summer | 5344 (24.4) | ||
| Winter | 5413 (24.8) | 1.2 (1.1 to 1.3)‡ | 1.1 (1.0 to 1.2)‡ |
| Spring | 5339 (24.4) | 1.0 (1.0 to 1.1) | 1.0 (0.9 to 1.1) |
| Autumn | 5782 (26.4) | 1.0 (1.0 to 1.1) | 1.0 (0.9 to 1.1) |
| Ambulance vehicle (ref), n/N (%) | |||
| BLS | 14 539 (66.5) | ||
| MICU | 4879 (22.3) | 1.7 (1.6 to 1.8)‡ | 1.5 (1.4 to 1.7)‡ |
| Two crews* | 2460 (11.2) | 2.7 (2.5 to 3.0)‡ | 2.2 (2.0 to 2.5)‡ |
| Receiving EDs† (ref), n/N (%) | |||
| Governmental | 18 436 (84.6) | ||
| Private hospital | 3357 (15.4) | 1.5 (1.4 to 1.6)‡ | 1.3 (1.2 to 1.5)‡ |
*Missions attended by rapid response non-transporting vehicles and the essential transporting vehicle.
†85 records of undocumented hospitals’ EDs were removed and not counted.
‡Statistically significant at a p value of <0.05.
BLS, basic life support; ED, emergency department; HUME, highly urgent medical emergency; HUTE, highly urgent trauma emergency; MICU, mobile intensive care unit.
Discussion
The present study showed that more than 50% of emergency cases had an OST of greater than 15 min, which is the Saudi EMS standard time for all crews to perform the standard operational procedures during OST regardless of urgency level. Although the median OST for HUTE was closer than HUME to the benchmark of 15 min, about 25% of those missions still took more than 22 min. OST was also prolonged when EMS ambulance missions were dispatched for women, the elderly, in urban areas, during winter, as advanced EMS services or for transport to private hospitals. Several studies demonstrated that an increase in OST was associated with adverse outcome.3 5 23–26 In addition, the American Stroke Association guideline recommends OST to be ≤15 min.7
Children represented 3.7% of EMS missions and had significantly shorter OST. Our study is consistent with multiple studies that found children’s OST to be significantly shorter than adults.27 28 In our study, elderly patients had by far the longest median OST. Cultural restrictions of face coverage for elderly women reduce with an increase in age. Elderly people of both sexes in Saudi Arabia most ordinarily live on the first floor due to comorbidities and difficulties climbing up to the upper floors. In our study, although the median OST for elderly people was longer than adults and children, the intergender variation in the OST duration for elderly people was negligible compared with adults and children. A plausible explanation for prolonged OST for the elderly might be attributed to the difficulty in communication with them about the severity of their medical conditions and that more time was required to stabilise them.29 A Swedish study found that an increase in age is directly proportional to an increase in OST.30 Sullivan et al found oldest people are significantly associated with longer OST.31 However, in another study, no association between age and sex and prolonged OST was found.32
Although EMS crews had spent more than 15 min for most patients at the scene before they transported them to hospitals, women were most likely to have longer time than men regardless of any explanatory factor. For example, in looking at EMS crew types, we found EMS missions that were dispatched by MICU crews had longer OST than BLS crews, and the dispatching of MICU crews increased the odds of prolonged OST regardless of the patients’ gender. This finding is line with Schull et al, who found dispatching ALS crews compared with the BLS crews at the scene increase the OST by 5.6 min.33 Yet, we found that the median OST for MICU crews was longer for women than men, although our data did not include the type and number of interventions at the scene. Our study revealed EMS crews staying a half-hour or more at the scene for 25% of adult women regardless of the calls’ reasons. We compared this finding with their counterpart of adult men, and we found the difference was at a minimum of 5 min. Given the unavailable data elucidating number and type of medical interventions at the scene, we are unable to clarify the medical reasons triggering this difference. Moreover, our study data cannot reveal whether women could receive less or more intervention than men at the scene. For example, studies in the USA showed women had received less EMS interventions and treatment compared with men.34 35 Although we look for explanations in Saudi EMS setting, the gender differences are not confined to our study. Our findings are in line with several studies from other countries which often found that women had a longer median or average OST compared with men.12 28 29 31 33 34 None of these studies investigated the impact of different sociocultural factors on spent time at the scene for patients. One of these found that women had more extended OST than men for non-ST-elevation myocardial infarction and ST-elevation myocardial infarction, despite ECG being implemented for both men and women.12
In our study, OST and total EMS time for HUME were longer for women than men, while missions dispatched to HUTE did not show any difference. HUME missions may be more often for patients in household buildings than to HUTE missions that may be dispatched more often to open areas such as streets (eg, for vehicle accidents). Most HUTEs are involved by third parties like the Saudi police, which limit any cultural barriers. While in HUME, the profound sex difference in median OST in HUME missions might primarily be explained by Saudi house design and culture. It is customary in Saudi Arabia for the upper floors and rooms far from the residential home’s main entrance to be a suitable residence for women. It has been proven that house design has an impact on delaying the access time to the patient after crew arrival to the scene.36 37 Saudi houses are relatively large due to the high average number of family members.38 When EMS crews arrive at the scene, they must usually walk a longer distance to reach the female-patient locations. Moreover, cultural differences in Saudi Arabia require women to be fully covered at the presence of non-primary relative men such as the EMS all-male crews, and that is why it might take a considerable time before the crew are allowed access to the patient.
Another possible reason for the delay during the scene period for Saudi women is the loading process into ambulance vehicles by all-male crews. This process would require strict adherence by crews’ members to use the ambulance stretchers even if the patient can walk independently or with crew members’ support, while for Saudi men, the stretcher could be waived if the patient prefers walking without it. However, to the best of our knowledge, no previous study has investigated the influence of culture and home design and whether they have a role in prolonging the OST duration for men or women. Thus, further research on this topic is warranted.
In Saudi culture, men are usually involved in decision-making related to the transportation of children and elderly of both sexes, and women of all ages. Some Saudi women demand that their primary male relative be present to discuss their health status and plan further action. Some still need guardianship for signing the consent for medical intervention, although they have the right to sign it themselves.39 40 In specific circumstances, the women’s guardian can prohibit them from transportation to the hospital by ambulance.41 A Saudi study found that Saudi women had lower health literacy than men.42 Two other Saudi studies revealed that Saudi women were less likely to use EMS and were more likely to refuse transportation by ambulance than men.1 43 Therefore, the longer OST among women might be explained by their reluctance to be transported and that the ambulance crew spent more time to educate them and their guardians about the importance of ambulance transportation. Further qualitative research may be needed to identify factors that lead to prolonged OST at households. This study lacks the data necessary to do so. No previous narrative inquiry has been performed to study this phenomenon in Saudi Arabia. An Australian qualitative study investigated the barriers confronting paramedics because of cultural barriers of middle eastern people living in Australia who might have a cultural resemblance to Saudi people.44 The informants’ paramedics stated that they found difficulties in providing care due to specific norms and behaviour emanating from Middle East culture, and time management at the home locations was affected.44
A significant delay on the scene can deprive women of receiving important medical intervention, unable to be provided by the ambulance crew, in a timely manner in definitive care especially in life-threatening cases. Due to the longer OST for women, they are more exposed to unexpected adverse events such as late or unsafe arrival to hospitals, especially when the crews are committed to not exceeding the golden hour, the benchmark related to the total EMS time, and risk road accidents themselves.
Strengths and limitations
Our study as a retrospective study has several limitations, all pertaining to the EMS registry. The registry relies on the SRCCAD automated detection of time to compute the timeline. However, one-fourth of data were missing, and we observed impossible outliers that may have arisen due to network failure during the communication between call centre and crews at the scene. Our exclusion of those missing data and outliers might have induced selection bias. Another limitation is the non-availability of variables that may explain the gender differences in more detail, such as socioeconomic characteristics, time between onset of symptoms and EMS call, type of treatment at the scene and OST stratified by its four phases: arrival at the scene until accessing the patient, patient assessment time, treatment phase and loading time. On the other hand, using registry data has provided us with much statistical power to detect between-group differences and associations for the characteristics that were available.
Perceived urgency and severity rely on the call centre’s triaging system and additional confirmation by crews during arrival at the scene, which might not reflect the real patient condition when the patients arrive at the hospital. Therefore, some misclassification in the urgency types may have occurred. However, our data do reflect daily practices in which urgency levels are determined as early as possible during the mission as possible. However, with future involvement in the EMS data set, researchers could explain those reasonable and unavoidable causes that lead to the lateness.
Considering the linking of the registry data to outcomes data on patients’ receiving hospital data such as mortality, 28-day survival and 6-month survival, we showed OST statistical significance between sexes but limited to show the clinical significance. The last limitation belongs to the study design of clustering heterogeneous emergency types into two cohorts and the Saudi benchmarks of 15 min. As a result, our study cannot compare our finding of OST with the essential international guideline like AHA of the recommended OST for specific emergency cases like out-of-hospital cardiac arrest, acute coronary syndrome and stroke. However, our study showed that female time to access definitive care during medical emergencies is more extended. With future involvement in the EMS data set, researchers could explain the relationship between time performance and EMS outcomes.
Finally, our study’s generalisability might apply to urban and rural areas of other different Saudi provinces and the other Arabian Gulf States having similar EMS systems except for Macca city in Saudi Arabia because of Hajj and the influx of Muslims gathering during different seasons.
Conclusions
This study shows that median OST was longer than 15 min for more than half of transported cases. In addition, it was longer for women for HUME at every time and place, regardless of age category, crew type and receiving hospital. For those EMS missions that had been dispatched for HUTE, there was no difference. Furthermore, missions to children, in rural areas, for trauma patients, for crews dispatched by BLS ambulances, in summer as a season, or transported to EDs of governmental hospitals were all significant predictors for shorter OST. These findings are hypothesis generating and require further studies.
Supplementary Material
Acknowledgments
The authors thank Ms Jordan Phillips from Berlitz Language Centre Maastricht, The Netherlands, for her proofreading of the manuscript.
Footnotes
Contributors: All authors conceived the study, conceptualised the ideas, and supervised the study design and definition of essential terms and study measures. HNM, SvK and DMA performed the data cleaning, management and analysis. HNM drafted the manuscript, performed the formal analysis, and takes responsibility for the integrity of the data, the accuracy of the data analysis and the paper as a whole. SvK provided statistical advice on study design and analysis. HNM and DMA had full access to all of the data in the study. HNM, SvK, MEM and HH interpreted the data. HNM and HH were the project administrators. HH was the primary supervisor. All authors contributed substantially to the manuscript's revision. HNM is the guarantor for the work and responsible for the overall content of the work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. Data available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants. The study proposal was reviewed and approved by the ethical committee in Jazan University (registry number REC39/9-S085). The ethics committee, based on no need to contact patients, agreed that informed consent was not required because of the anonymity of the data collected for routine ambulance missions and the study’s retrospective design. The study data take into consideration privacy and confidentiality.
References
- 1.Moafa HN, van Kuijk SMJ, Alqahtani DM, et al. Disparities between rural and urban areas of the central region of Saudi Arabia in the utilization and Time-Centeredness of emergency medical services. Int J Environ Res Public Health 2020;17:7944. 10.3390/ijerph17217944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moafa HN, Kuijk SMJvan, Franssen GHLM, et al. What is known about the quality of out-of-hospital emergency medical services in the Arabian Gulf states? A systematic review. PLoS One 2019;14:e0226230. 10.1371/journal.pone.0226230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown JB, Rosengart MR, Forsythe RM, et al. Not all prehospital time is equal: influence of scene time on mortality. J Trauma Acute Care Surg 2016;81:93–100. 10.1097/TA.0000000000000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alrawashdeh A, Nehme Z, Williams B, et al. Emergency medical service delays in ST-elevation myocardial infarction: a meta-analysis. Heart 2020;106:365–73. 10.1136/heartjnl-2019-315034 [DOI] [PubMed] [Google Scholar]
- 5.Ruelas OS, Tschautscher CF, Lohse CM, et al. Analysis of prehospital scene times and interventions on mortality outcomes in a national cohort of penetrating and blunt trauma patients. Prehosp Emerg Care 2018;22:691–7. 10.1080/10903127.2018.1448494 [DOI] [PubMed] [Google Scholar]
- 6.Seamon MJ, Fisher CA, Gaughan J, et al. Prehospital procedures before emergency department thoracotomy: "scoop and run" saves lives. J Trauma 2007;63:113–20. 10.1097/TA.0b013e31806842a1 [DOI] [PubMed] [Google Scholar]
- 7.Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke. Stroke 2013;44:870–947. 10.1161/STR.0b013e318284056a [DOI] [PubMed] [Google Scholar]
- 8.Campbell BCV, De Silva DA, Macleod MR, et al. Ischaemic stroke. Nat Rev Dis Primers 2019;5:70. 10.1038/s41572-019-0118-8 [DOI] [PubMed] [Google Scholar]
- 9.Lockey DJ, Weaver AE, Davies GE. Practical translation of hemorrhage control techniques to the civilian trauma scene. Transfusion 2013;53 Suppl 1:17S–22. 10.1111/trf.12031 [DOI] [PubMed] [Google Scholar]
- 10.Salomone JP, Ustin JS, McSwain NE, et al. Opinions of trauma practitioners regarding prehospital interventions for critically injured patients. J Trauma 2005;58:509–17. 10.1097/01.TA.0000152807.63559.2E [DOI] [PubMed] [Google Scholar]
- 11.Vincent-Lambert C, Mottershaw T. Views of emergency care providers about factors that extend on-scene time intervals. Afr J Emerg Med 2018;8:1–5. 10.1016/j.afjem.2017.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aguilar SA, Patel M, Castillo E, et al. Gender differences in scene time, transport time, and total scene to hospital arrival time determined by the use of a prehospital electrocardiogram in patients with complaint of chest pain. J Emerg Med 2012;43:291–7. 10.1016/j.jemermed.2011.06.130 [DOI] [PubMed] [Google Scholar]
- 13.Luo W, Yao J, Mitchell R, et al. Spatiotemporal access to emergency medical services in Wuhan, China: accounting for scene and transport time intervals. Int J Health Geogr 2020;19:52. 10.1186/s12942-020-00249-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alanazi AF. Emergency medical services in Saudi Arabia: a study on the significance of paramedics and their experiences on barriers as inhibitors of their efficiency. Int J Appl Basic Med Res 2012;2:34–7. 10.4103/2229-516X.96803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mell HK, Mumma SN, Hiestand B, et al. Emergency medical services response times in rural, suburban, and urban areas. JAMA Surg 2017;152:983–4. 10.1001/jamasurg.2017.2230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mills EHA, Aasbjerg K, Hansen SM, et al. Prehospital time and mortality in patients requiring a highest priority emergency medical response: a Danish registry-based cohort study. BMJ Open 2019;9:e023049. 10.1136/bmjopen-2018-023049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 18.The General Authority for Statistics in Saudi Arabia . Saudi Arabian census report for 2010 Saudi Arabia: the general authority for statistics in Saudi Arabia, 2021. Available: https://www.stats.gov.sa/en/73 [Accessed 15 March 2021].
- 19.Lerner EB, Moscati RM. The golden hour: scientific fact or medical "urban legend"? Acad Emerg Med 2001;8:758–60. 10.1111/j.1553-2712.2001.tb00201.x [DOI] [PubMed] [Google Scholar]
- 20.Meislin HW, Conn JB, Conroy C, et al. Emergency medical service Agency definitions of response intervals. Ann Emerg Med 1999;34:453–8. 10.1016/S0196-0644(99)80046-8 [DOI] [PubMed] [Google Scholar]
- 21.Spaite DW, Valenzuela TD, Meislin HW, et al. Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med 1993;22:638–45. 10.1016/S0196-0644(05)81840-2 [DOI] [PubMed] [Google Scholar]
- 22.Saudi Tourism Authority . The seasons and climate in Saudi Arabia Riyadh, Saudi Arabia: Saudi tourism authority, 2021. Available: https://www.visitsaudi.com/en/understand/climate-and-seasons#:~:text=Contrary%20to%20popular%20belief%2C%20it’s,overview%20of%20the%20kingdom’s%20weather.March15,2021
- 23.Johnson NJ, Carr BG, Salhi R, et al. Characteristics and outcomes of injured patients presenting by private vehicle in a state trauma system. Am J Emerg Med 2013;31:275–81. 10.1016/j.ajem.2012.07.023 [DOI] [PubMed] [Google Scholar]
- 24.McCoy CE, Menchine M, Sampson S, et al. Emergency medical services out-of-hospital scene and transport times and their association with mortality in trauma patients presenting to an urban level I trauma center. Ann Emerg Med 2013;61:167–74. 10.1016/j.annemergmed.2012.08.026 [DOI] [PubMed] [Google Scholar]
- 25.Hang AP, Ki Ok A, Eui Jung L. Association between survival and time of On-Scene resuscitation in refractory out-of-hospital cardiac arrest: a cross-sectional retrospective study. International Journal of Environmental Research and Public Health;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poppe M, Krammel M, Clodi C, et al. Management of EMS on-scene time during advanced life support in out-of-hospital cardiac arrest: a retrospective observational trial. Eur Heart J Acute Cardiovasc Care 2020;9:S82–9. 10.1177/2048872620925681 [DOI] [PubMed] [Google Scholar]
- 27.Wyen H, Lefering R, Maegele M, et al. The golden hour of shock - how time is running out: prehospital time intervals in Germany--a multivariate analysis of 15, 103 patients from the TraumaRegister DGU(R). Emerg Med J 2013;30:1048–55. 10.1136/emermed-2012-201962 [DOI] [PubMed] [Google Scholar]
- 28.Ashburn NP, Hendley NW, Angi RM, et al. Prehospital trauma scene and transport times for pediatric and adult patients. West J Emerg Med 2020;21:455–62. 10.5811/westjem.2019.11.44597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fok PT, Teubner D, Purdell-Lewis J, et al. Predictors of prehospital on-scene time in an Australian emergency retrieval service. Prehosp Disaster Med 2019;34:317–21. 10.1017/S1049023X19004394 [DOI] [PubMed] [Google Scholar]
- 30.Hjalmarsson A, Holmberg M, Asp M, et al. Characteristic patterns of emergency ambulance assignments for older adults compared with adults requiring emergency care at home in Sweden: a total population study. BMC Emerg Med 2020;20:94. 10.1186/s12873-020-00387-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan AL, Beshansky JR, Ruthazer R, et al. Factors associated with longer time to treatment for patients with suspected acute coronary syndromes: a cohort study. Circ Cardiovasc Qual Outcomes 2014;7:86–94. 10.1161/CIRCOUTCOMES.113.000396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nagata I, Abe T, Nakata Y, et al. Factors related to prolonged on-scene time during ambulance transportation for critical emergency patients in a big City in Japan: a population-based observational study. BMJ Open 2016;6:e009599. 10.1136/bmjopen-2015-009599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schull MJ, Morrison LJ, Vermeulen M, et al. Emergency department overcrowding and ambulance transport delays for patients with chest pain. CMAJ: Canadian Medical Association Journal 2003;168:277–83. 10.1016/j.annemergmed.2003.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lewis JF, Zeger SL, Li X, et al. Gender differences in the quality of EMS care nationwide for chest pain and out-of-hospital cardiac arrest. Womens Health Issues 2019;29:116–24. 10.1016/j.whi.2018.10.007 [DOI] [PubMed] [Google Scholar]
- 35.Rothrock SG, Brandt P, Godfrey B, et al. Is there gender bias in the prehospital management of patients with acute chest pain? Prehosp Emerg Care 2001;5:331–4. 10.1080/10903120190939454 [DOI] [PubMed] [Google Scholar]
- 36.Morrison LJ, Angelini MP, Vermeulen MJ, et al. Measuring the EMS patient access time interval and the impact of responding to high-rise buildings. Prehosp Emerg Care 2005;9:14–18. 10.1080/10903120590891679 [DOI] [PubMed] [Google Scholar]
- 37.Drennan IR, Strum RP, Byers A, et al. Out-Of-Hospital cardiac arrest in high-rise buildings: delays to patient care and effect on survival. CMAJ 2016;188:413–9. 10.1503/cmaj.150544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abdul Salam A, Elsegaey I, Khraif R, et al. Population distribution and household conditions in Saudi Arabia: reflections from the 2010 census. Springerplus 2014;3:530–30. 10.1186/2193-1801-3-530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Amoudi S. The right of Saudi women to sign for their health care in Saudi Arabia, fact and fiction. Life Science Journal-acta Zhengzhou University Overseas Edition 2012;9:3143–6. [Google Scholar]
- 40.Al-Amoudi SM. Health empowerment and health rights in Saudi Arabia. Saudi Med J 2017;38:785–7. 10.15537/smj.2017.8.19832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aldosari H. The effect of gender norms on women’s health in Saudi Arabia: Arab Gulf States Institute in Washington Washington, DC 2017;7. [Google Scholar]
- 42.Almubark R, Basyouni M, Alghanem A, et al. Health literacy in Saudi Arabia: implications for public health and healthcare access. Pharmacol Res Perspect 2019;7:e00514. 10.1002/prp2.514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moafa HN, van Kuijk SMJ, Moukhyer ME, et al. Non-Conveyance due to patient-initiated refusal in emergency medical services: a retrospective population-based registry analysis study in Riyadh Province, Saudi Arabia. Int J Environ Res Public Health 2021;18. 10.3390/ijerph18179252. [Epub ahead of print: 02 09 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hartley PR. Paramedic practice and the cultural and religious needs of pre‐hospital patients in Victoria. Victoria University 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. Data available upon reasonable request.