Abstract
Introduction
Violence against women (VAW) affects one in three women globally. In some countries, women are at much higher risk. We examined risk factors for VAW in countries with the highest 12-month prevalence estimates of intimate partner violence (IPV) to develop understanding of this increased risk.
Methods
For this systematic review, we searched PUBMED, CINAHL, PROQUEST (Middle East and North Africa; Latin America and Iberia; East and South Asia), Web of Science, EMBASE and PsycINFO (Ovid) for records published between 1 January 2000 and 1 January 2021 in English, French and Spanish. Included records used quantitative, qualitative, or mixed-methods, reported original data, had VAW as the main outcome, and focused on at least one of 23 countries in the highest quintile of prevalence figures for women’s self-reported experiences of physical and/or sexual violence in the past 12 months. We used critical interpretive synthesis to develop a conceptual model for associations between identified risk factors and VAW.
Results
Our search identified 12 044 records, of which 241 were included for analysis (2 80 360 women, 40 276 men, 274 key informants). Most studies were from Bangladesh (74), Uganda (72) and Tanzania (43). Several quantitative studies explored community-level/region-level socioeconomic status and education as risk factors, but associations with VAW were mixed. Although fewer in number and representing just one country, studies reported more consistent effects for community-level childhood exposure to violence and urban residence. Theoretical explanations for a country’s high prevalence point to the importance of exposure to other forms of violence (armed conflict, witnessing parental violence, child abuse) and patriarchal social norms.
Conclusion
Available evidence suggests that heightened prevalence of VAW is not attributable to a single risk factor. Multilayered and area-level risk analyses are needed to ensure funding is appropriately targeted for countries where VAW is most pervasive.
PROSPERO registration number
The review is registered with PROSPERO (CRD42020190147).
Keywords: public health, systematic review, epidemiology
Key messages.
What is already known?
There are large differences in the prevalence of violence against women both within and between countries.
There is limited understanding of which contextual factors drive high rates of violence against women (VAW) in certain countries.
Countries with the highest VAW prevalence estimates have largely been excluded from previous reviews.
What are the new findings?
This is the first review of VAW risk factors to focus specifically on high-prevalence settings.
Multiple, overlapping risks are responsible for a heightened prevalence of VAW, rather than a single factor.
Population-level exposure to other forms of violence (armed conflict, witnessing parental violence, child abuse) and patriarchal social norms appear to drive high levels of violence against women.
What do the new findings imply?
There is a dearth of evidence on how the risk factors operating at community, regional, national and global levels impact on violence, and on how risk factors may change over time.
Additional longitudinal and cross-national analyses are needed to inform VAW interventions in high-prevalence settings.
Introduction
Violence against women (VAW) has severe consequences for women’s health and well-being globally.1 While violence affects women in every country, it does so unevenly, with large differences in prevalence both within and between countries. Recent estimates suggest that between 10% and 53% of ever-partnered women have experienced physical and/or sexual violence by an intimate partner in their lifetime, with past 12-month prevalence estimates ranging between 2% and 36%.2 Some of the highest VAW prevalence estimates are found in informal settlements,3 Indigenous communities,4 conflict zones5 and certain regions of the world, such as the Pacific.6 Contextual factors proposed to shape violent behaviours towards women include inequalities in income and education, gendered cultural norms and practices, exposure to other forms of violence, and racial or class-based discrimination.7 8
Currently, however, there is limited understanding of which contextual factors drive high rates of VAW in certain settings. Armed conflict has been proposed as one such risk factor, as highlighted in Afghanistan and the Democratic Republic of Congo (DRC), where prevalence estimates of intimate partner violence (IPV) in the past 12 months measured 46% and 37%, respectively.9 10 Yet many countries with a high prevalence of IPV have not experienced recent conflict, including Fiji and the Marshall Islands (where lifetime exposure to IPV measured 64% and 51%, respectively).11 Feminist scholars have focused on patriarchal norms as a critical driver of VAW globally.12 However, countries such as Sweden and Denmark, where gender equality is supported by relevant policy and frameworks, have relatively high levels of lifetime exposure to physical and/or sexual violence (28% and 32% respectively), an anomaly often referred to as the Nordic paradox.13
Countries with the highest prevalence estimates have largely been excluded from previous reviews. Research from such countries often fails to meet methodological or review inclusion criteria,14–17 and recent reviews have tended to focus on risk factors rather than settings, including reviews of the public justification of violence,18 community-level correlates,19 child abuse,20 natural disasters,21 forms of violence22 or subpopulations such as pregnant women,23 24 and elderly women.25
To our knowledge, this is the first review of risk factors to focus on high-prevalence settings. It builds on other reviews that have taken an area or regional focus.26–28 We aim to identify the risk factors for VAW in the highest prevalence countries to (1) inform analyses of relationships between risk factors, (2) identify gaps to be addressed through further research and (3) inform policy priorities for the leave-no-woman-behind agenda.29 The review was designed to identify the broadest possible list of potential risk factors and draws together both quantitative and qualitative evidence.
Methods
Search strategy and selection criteria
We developed a rigorous search strategy (online supplemental file 1) and searched 19 databases for records in English, French or Spanish published between January 2000 and January 2021. The year 2000 represents the start of data collection using the WHO methodology, widely recognised as best practice for measuring VAW at a population level.30 Bibliographic databases included EMBASE, MEDLINE (PubMed), PsycINFO, Web of Science, CINAHL, Latin America & Iberia Database (ProQuest), Middle East & Africa Database (ProQuest), East and South Asia (ProQuest), Scielo, Latin America and Caribbean Health Science Library (PAHO). Additionally, we searched 10 databases for grey literature, including World Bank Open Knowledge Repository, WHO Prevent Violence Evidence Base and Resources, WHO Institutional Repository for Information Sharing, UNFPA regional websites, UNDP, UN Women, WHO Reproductive Health Library, Human Rights Watch, Relief Web, Observatorio de Igualdad de Género de América Latina y el Caribe. Search terms were divided into two strings: the first related to types of VAW, high-prevalence countries and risk factors; the second related to VAW in general, risk factor analyses and the global/cross-national level. We also identified records through expert referrals, handsearching relevant journals and citation chaining.
bmjgh-2021-007704supp001.pdf (612.1KB, pdf)
Twenty-three countries were identified as high-prevalence settings for the review. These countries represent the top quintile of prevalence figures for women’s self-reported experiences of physical or sexual violence in the past 12 months (table 1). By classifying high-prevalence countries according to currently available WHO data, we have only included countries for which these data were available.31
Table 1.
Countries included in the review, by relevant characteristics
| Country | Prevalence of past 12-month experience of physical and or sexual IPV (%)* | WHO region | GINI coefficient† | High/ middle/low income‡ | Armed conflict since 1990§ |
| Angola | 25.9 (DHS 2016) | African | 0.513 | Lower-middle | Yes |
| Burundi | 27.8 (DHS 2017) | African | 0.386 | Low | Yes |
| Cameroon | 32.7 (MICS 2014) | African | 0.466 | Lower-middle | Yes |
| Central African Republic | 26.3 (MICS 2006) | African | 0.562 | Low | Yes |
| DRC | 36.8 (DHS 2014] | African | 0.421 | Low | Yes |
| Equatorial Guinea | 43.6 (DHS 2011) | African | Not available | Upper middle | Yes |
| Gabon | 31.5 (DHS 2012) | African | 0.380 | Upper middle | Yes |
| Liberia | 36.3 (DHS 2007) | African | 0.353 | Low | Yes |
| Sierra Leone | 28.7 (DHS 2013) | African | 0.357 | Low | Yes |
| Sao Tome and Principe | 27.9 (DHS 2009) | African | 0.563 | Lower middle | No |
| Tanzania | 29.6 (DHS 2016) | African | 0.405 | Lower middle | Yes |
| Uganda | 29.9 (DHS 2016) | African | 0.428 | Low | Yes |
| Zambia | 26.7 (DHS 2014) | African | 0.571 | Lower middle | No |
| Afghanistan | 46.1(DHS 2015) | Eastern Mediterranean | Not available | Low | Yes |
| Bangladesh | 28.8 (UNFPA 2015) | South-East Asian | 0.324 | Lower middle | Yes |
| Timor-Leste | 34.6 (DHS 2016) | South-East Asian | 0.287 | Lower middle | Yes |
| Bolivia | 27.1 (PAHO 2016) | The Americas | 0.416 | Lower middle | Yes |
| Fiji | 29.7(National Research on Women’s Health and Life Experiences 2011) | Western Pacific | 0.367 | Upper middle | Yes |
| Kiribati | 36.1(Family Health and Safety Study 2008) | Western Pacific | 0.370 | Lower middle | Yes |
| Micronesia | 26.0 (Family Health and Safety Study 2014) | Western Pacific | 0.401 | Lower middle | No |
| Solomon Islands | 41.8(Family health and safety study 2008) | Western Pacific | 0.371 | Lower middle | No |
| Tuvalu | 25.0 (DHS 2007) | Western Pacific | 0.391 | Upper middle | No |
| Vanuatu | 44.0 (National Survey on Women’s Lives and Family Relationships 2009) | Western Pacific | 0.376 | Lower middle | No |
*Data compiled by the WHO as part of commitment to United Nations Sustainable Development Goals Intimate Partner Violence data indicator 5.2.1, https://unstats.un.org/sdgs/unsdg
†The GINI coefficient, a statistical representation of income inequality within a country that ranges from 0 (perfect equality) to 1 (perfect inequality), https://data.worldbank.org/indicator/SI.POV.GINI
‡Income classifications source: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
§Heidelberg Institute for International Conflict Research HIIK database https://hiik.de/data-and-maps/datasets/?lang=en
DHS, Demographic and Health Surveys; DRC, Democratic Republic of Congo; IPV, intimate partner violence; MICS, Multiple Indicator Cluster Surveys.
The selection criteria used for abstract screening included primary research studies that were either qualitative (eg, used in-depth interviews, focus group discussions, or observations) or quantitative (eg, used cohort, case–control, cross-sectional or experimental designs). Titles and abstracts were double screened in Endnote by two reviewers (RM and LB) for records in high-prevalence countries that included at least one risk factor for violence against adult women (18 years or older) as the outcome. We excluded opinion pieces, editorials, policy briefs, general reports that did not present new empirical data, and conference abstracts. Disagreements over whether a record should be included were resolved by a third reviewer (JM).
We updated the initial database search in January 2021, resulting in 22 additional records, followed by a second search using a modified strategy that incorporated a new list of risk factors, resulting in 24 additional records. The list of risk factors for the first search was created from coding risk factors and relevant definitions from existing reviews and compiling these into a working template.32 For the second search, we modified this a priori template to include new risk factors or changes in definitions based on new codes identified during initial screening (online supplemental material), as a means of ensuring all potentially relevant risk factors had been included. No new risk factors were identified after the second search.
Data analysis
Four reviewers (HL, RM, LB and JM) completed full text review of a subsection of records and extracted study characteristics, effect estimates and a summary of findings from included articles using a piloted form. Any discrepancy or query about data extraction was discussed by the review team. We developed a tailored approach to quality assessment which involved using set criteria as part of a fatal flaw analysis across all study types, consistent with the critical interpretive synthesis (CIS) approach used for meta-synthesis of the data (online supplemental materials).33 This approach to quality assessment prioritises the conceptual relevance of included studies over the degree to which they meet particular methodological standards for minimising the risk of bias, and is particularly useful for mixed-methods reviews that aim to make a theoretical or conceptual contribution.34
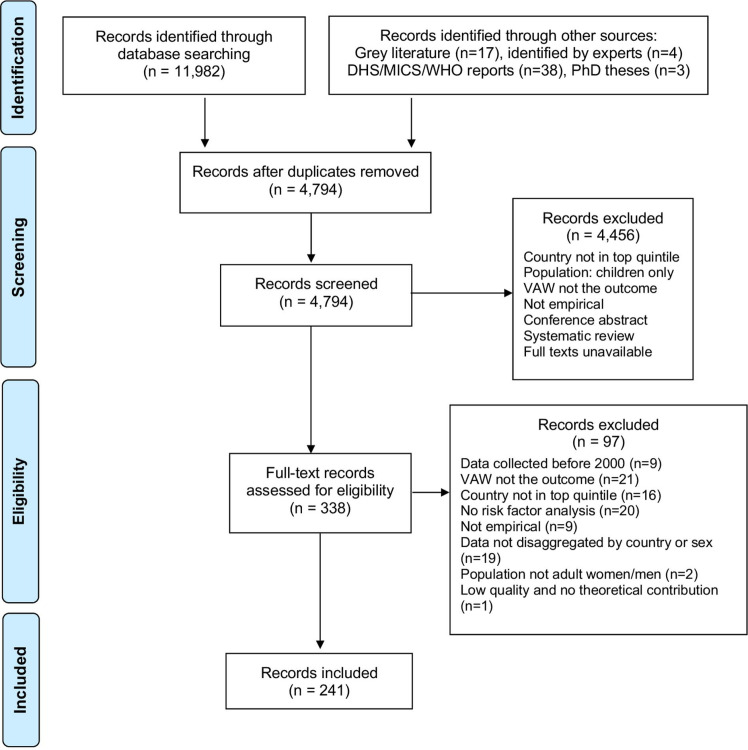
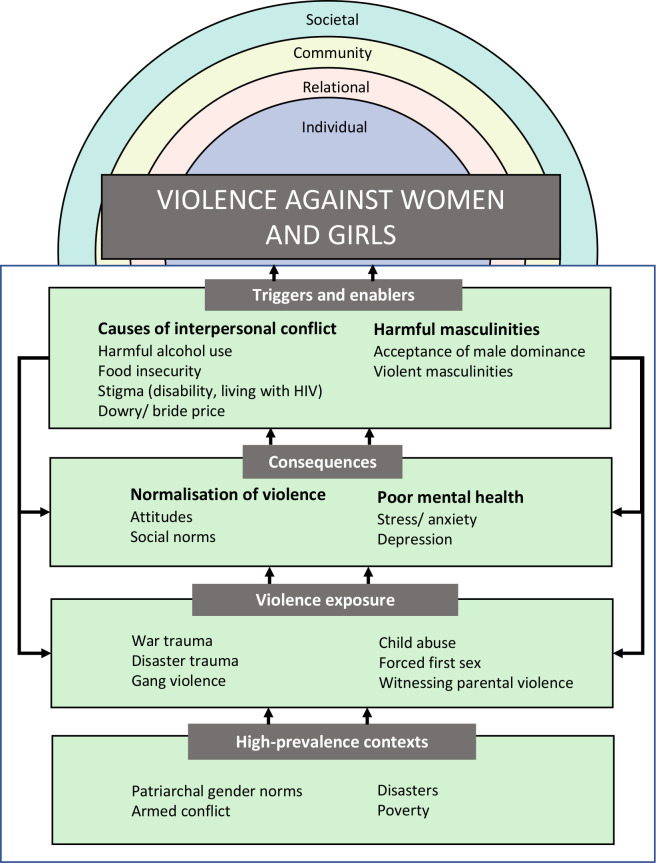
We first categorised identified risk factors thematically as part of a narrative literature summary. We then used CIS to generate theoretical insights from the integration of qualitative, quantitative and mixed-methods studies.34 CIS is differentiated from other meta-synthesis methods by its critical stance towards the presentation of the literature by primary authors, and its ability to generate theoretical insights through synthesis.33 HL and RM developed summary statements for each record (eg, how specific risk factors are linked to VAW), and grouped these statements into thematic categories. The review team then used these summary statements to develop a synthetic construct for how each risk factor was related to VAW and to other risk or protective factors. These synthetic constructs were linked together visually and formed our conceptual framework (figure 1).
Figure 1.
Study selection. Adapted from Moher et al.189 HS, Demographic and Health Surveys; MICS, Multiple Indicator Cluster Surveys; VAW, violence against women.
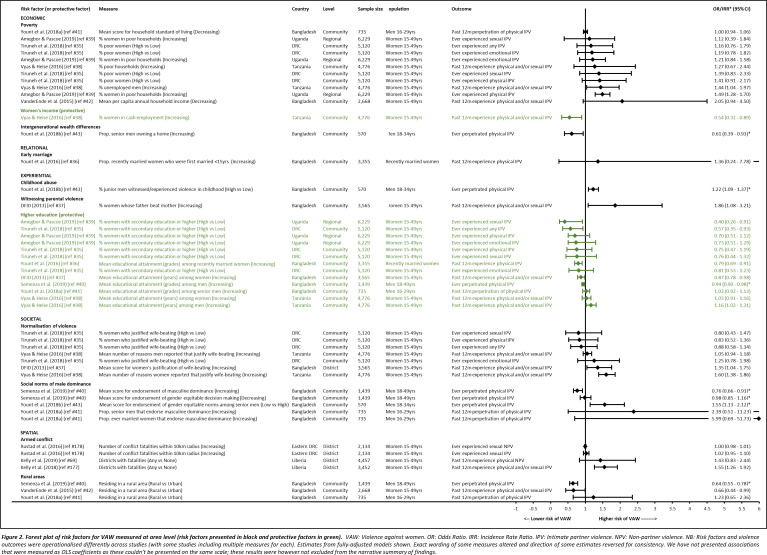
We collated quantitative estimates measured at the community, district and region-level and presented these as ORs or incidence rate ratios in a forest plot to provide a visual summary of area-level risk factors, their effect sizes and directions of association with VAW. We presented area-level rather than individual-level estimates (and included studies that used aggregated individual data to create area-level measures), as these provide insights into contextual and structural factors shaping high prevalence settings. We decided against a meta-analysis because few records reported on the same risk factors at area level, and because of heterogeneity in how exposures and outcomes were measured.
Results
Our search identified 12 044 records. We screened titles and abstracts of 4794 unique records. A total of 338 met the criteria for full-text review. Records were excluded at the full review stage if VAW was not the outcome (n=21), there were no data on targeted countries (n=16), no risk factor analysis was included (n=20), data were not disaggregated by country or sex (n=19), no empirical data were provided (n=9), data were collected before 2000 (n=9), the population were not adult women or men (n=2), or the paper was of low quality and made no theoretical contribution (n=1) (see figure 2). Table 2 summarises characteristics of the 241 included records.
Figure 2.
Forest plot of risk factors for VAW measured at area level. VAW, violence against women.
Table 2.
Characteristics of included records
| Characteristic | No of records (%) |
| Year of publication | |
| 2000–2010 | 41 (17.0) |
| 2011–2021 | 200 (83.0) |
| Publication type | |
| Peer-reviewed journal article | 222 (92.1) |
| Grey literature report | 12 (5.0) |
| DHS/MICS/WHO reports | 4 (1.7) |
| PhD theses | 3 (1.2) |
| Country | |
| Bangladesh | 74 |
| Uganda | 72 |
| Tanzania | 43 |
| Zambia | 23 |
| Democratic Republic of the Congo | 23 |
| Cameroon | 12 |
| Sierra Leone | 10 |
| Bolivia | 10 |
| Liberia | 9 |
| Timor-Leste | 9 |
| Afghanistan | 8 |
| Burundi | 7 |
| Gabon | 6 |
| Sao Tome and Principe | 5 |
| Angola | 5 |
| Central African Republic | 2 |
| Vanuatu | 2 |
| Micronesia | 2 |
| Kiribati | 1 |
| Solomon Islands | 1 |
| Fiji | 1 |
| Equatorial Guinea | 0 |
| Tuvalu | 0 |
| Data source | |
| Primary | 133 (55.2) |
| Secondary | 104 (43.2) (62% DHS) |
| Both primary and secondary | 4 (1.6) |
| Methods | |
| Quantitative | 175 (72.6) |
| Qualitative | 58 (24.1) |
| Mixed | 8 (3.3) |
| Study methods | |
| Quantitative designs | |
| Cross-sectional | 169 (70.1) |
| Longitudinal (prospective cohort n=2, retrospective cohort n=1, longitudinal analysis of baseline/endline data n=2) | 5 (2.1) |
| Retrospective | 1 (0.4) |
| Qualitative methods | |
| Individual interviews | 26 (10.8) |
| Focus group discussions | 9 (3.7) |
| Ethnography | 2 (0.8) |
| Case study | 1 (0.4) |
| Combination of qualitative methods | 20 (8.3) |
| Type of violence studied | |
| Physical | 211 |
| Sexual | 163 |
| Psychological | 87 |
| Economic | 22 |
| Controlling behaviour | 11 |
| Language | |
| English | 239 (99.2) |
| Spanish | 2 (0.8) |
| Total studies=241 | |
Percentages not included for country and type of violence because some studies included data from more than one country and for more than one type of violence.
DHS, Demographic and Health Surveys; MICS, Multiple Indicator Cluster Surveys.
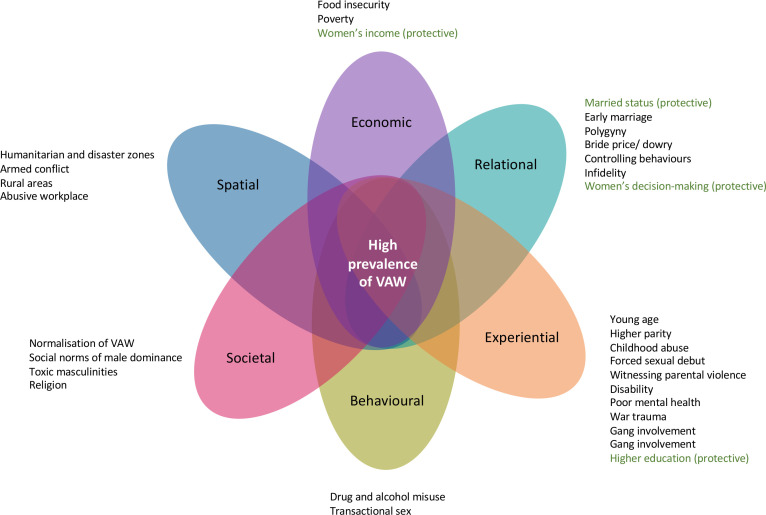
figure 3 presents included quantitative studies that measured area-level (community, district, region) risk factors. This provides a visual account of the rather limited information currently available about associations between the characteristics of high-prevalence settings and VAW. Education was the most explored risk factor (with higher education seen as protective), with a total of seven separate studies from four different countries looking at its area-level association with VAW.35–41 However, with different directions of effect and not all associations significant, the evidence for the association between area-level education and VAW was mixed and appears to be context-specific.35–41 Area-level poverty was also relatively frequently explored, but while the five separate studies from four different countries that looked at this found consistent directions of association,35 38 39 41 42 only two were significant.38 39 Mixed directions of association were also found for normalisation of violence and social norms of male dominance, but the direction of the only significant associations38 43 suggested increasing normalisation was associated with increased risk of VAW. Community-level childhood abuse (men) and witnessing parental violence (women) were only looked at in one study each37 43 but statistically significant effect sizes suggest some evidence for their role in VAW perpetration and experience.
Figure 3.
Overlapping risk factors for VAW in high-prevalence settings. VAW, violence against women.
At the individual and relational level, the most commonly studied risk factors in quantitative analyses were education, age, alcohol use and socioeconomic status. Less commonly studied risk factors included natural and environmental disasters, male partner’s experiences of violence, social support networks (for non-pregnant women), and the influence of peer networks. A more substantial picture of the drivers of VAW in high-prevalence settings arises from the results of all quantitative, qualitative and mixed-methods studies together, which are organised thematically.
Economic factors
Food insecurity was associated with different forms of VAW across numerous studies.44–49 An association between VAW and household socioeconomic status or asset wealth index was also observed at individual50–54 and regional levels.55 Theoretically, this association has been linked to how poverty-related stress increases the use of violence in households or between individuals who perceive it as an appropriate response to conflict.56 Contrary to theory, however, a study in Zambia found violence to be significantly higher among non-poor women compared with other women.57
Qualitative and quantitative data supported an association between women’s higher earnings and lower levels of past-year physical IPV.58–60 However, context played an important role. When women contributed equally or more than their husbands in Bangladesh, they were less likely to experience psychological, physical and sexual IPV than when their husbands contributed more or all income.61 In Tanzania, however, women had a greater risk of experiencing physical and sexual IPV when their financial contributions were greater than their partners’.58 In Bangladesh, young men were also less likely to perpetrate physical IPV in communities where more senior men owned homes, suggesting that intergenerational wealth differences may also be a risk factor for VAW.43
Relational factors
Compared with being unmarried and being in a cohabiting relationship, being married offered women protection against IPV in several studies.41 49–51 This finding could align with commitment theories that assert that cohabitation is an indicator of weakened relationships,62 or it could be that women are less likely to marry their violent partners. Being married was also protective against IPV when compared with being separated or divorced,63 64 although this may also be a reflection of women who experience violence leaving their violent partners. However, being married was found to increase the risk of sexual IPV compared with being unmarried,65 66 while single and unmarried women appeared to be at the highest risk of non-partner sexual67 and physical violence.68
Younger age at marriage was associated with increased domestic violence (from a partner or other family member),69 and with IPV.52 70–73 An association between the village-level prevalence of child marriage (<15 years) and IPV was found in Bangladesh, suggesting that women who lived in villages with high levels of child marriage were also at increased risk of IPV even if they married as adults themselves.36 In Afghanistan, women who were married before age 15 were reported to have a higher risk of sexual violence, compared with those married as adults (≥18 years).74 Generally, the risk of past year IPV reduced as marital duration increased,75–78 while lifetime IPV increased.72 79 80
Polygyny, often classified as an indicator of gender inequality, was strongly associated with increased IPV across several studies.44 81–84 A qualitative study from Bangladesh suggested polygyny created conflict between partners, with several female participants believing their inquiries about co-wives led to them being physically beaten.85 In Uganda, unequal love, neglect and jealousy created conflict in relationships that led to IPV.86 In Tanzania, polygyny was an indicator of women’s lower status, which increased their vulnerability to IPV.60
Women whose marriages involved dowry payment were more likely to experience IPV than women whose marriages did not.87–90 This was supported by qualitative data from Uganda and Tanzania where bride price was perceived to worsen gender inequalities by representing women as ‘bought’, reducing their decision-making power and increasing their risk of violence.91–93 Issues surrounding unpaid or partially paid dowry were highlighted as an additional source of relationship conflict triggering violence.85 94
There were strong, consistent associations between controlling behaviours and multiple types of IPV (physical, sexual and psychological) across countries.35 49 51 54 61 72 80 88 95–101 A study in Uganda found that male partners’ controlling behaviours were the strongest predictors of sexual IPV.102 This was supported by qualitative evidence demonstrating how IPV ensures a woman’s submissiveness and obedience and reaffirms her partner’s perceived masculinity,85 103 consistent with theoretical assertions that coercive control forms part of the overall pattern of women’s experiences of violence.104
A number of studies demonstrated that women who were involved in more egalitarian household decision making were less likely to experience IPV.35 59 70 105–107 However, a study from Bangladesh found that women’s risk of experiencing physical or sexual IPV increased with greater participation in household decision making.108
Infidelity by men was found to be a risk factor for IPV in both quantitative and qualitative studies.54 100 101 109–111 In Bangladesh, women whose partners had other sexual relationships were more likely to experience IPV than women whose partners did not.87 Moreover, when men suspected their female partner’s infidelity, or vice versa, women were more likely to experience IPV.51 60 98
Experiential factors
Young age was associated with increased risk of VAW in many studies.72 81 106 111–119 Ever-married or cohabiting women aged 20–24 years were significantly more likely to experience past year physical or sexual IPV than women aged 35 years or over.117 Having a greater number of children was also associated with an increased risk of IPV among women,49 59 63 64 69 72 106 111 113 120–125 possibly suggesting higher parity reinforces structural norms keeping women dependent on their partners.
Childhood abuse was associated with IPV perpetration (among men) or victimisation (among women) in a large number of studies.48 53 54 96 100 101 111 116 126 127 In Cameroon, a woman’s experience of physical abuse in childhood predicted sexual IPV victimisation in adulthood, which the authors suggested was the result of poor conflict resolution skills in adulthood.128 Childhood maltreatment was a strong predictor of IPV perpetration in adulthood among men in Burundi.129 Across many countries, forced sexual debut was a risk factor for IPV in later life among female sex workers,88 126 130 131 and among adolescent girls and young women.111 116 132
Witnessing IPV between parents during childhood was associated with IPV victimisation and perpetration in adulthood at the individual level,50 53 54 72 82 101 111 133 and at the community level.37 Qualitative data from Uganda highlighted negative role modelling in families and how boys from households with parental IPV were growing up to become violent husbands themselves.12
Women with disabilities were more likely to experience physical, sexual and emotional violence than women without disabilities.134–137 Qualitative findings from the DRC suggested that this may be related to an inability to fulfil expected gender roles in the household.138 Women who experienced mental ill health were similarly at risk of experiencing violence in intimate relationships and family settings,46 47 63 139 but also in the workplace140 and by strangers.47 141 VAW was perpetrated by caregivers, partners (including men who also suffered with poor mental health) and strangers.96 142–144
In conflict and postconflict settings including Afghanistan, Liberia, Uganda and Sierra Leone, war violence exposure was associated with increased IPV perpetration among men and IPV victimisation among women.46 139 145–147 In Liberia, this association was independently mediated by anxious attachment styles and attitudes justifying wife beating.139 In South Kivu, DRC, men discussed how their experiences of wartime violence were a risk factor for their perpetration of rape.148 In Timor Leste, women linked men’s war exposure to increased emotional problems and alcohol consumption, increasing IPV risk in the home.149 Men who were involved with gangs were more likely to perpetrate both physical and sexual IPV,96 as were men involved in fights with other men.95 100 101 111 132
Although the effect of education on VAW varied across different geographies and population groups, higher levels were generally associated with reduced violence perpetration and victimisation.35 50 86 87 112 120 Women’s higher education protected against IPV at both the individual and community level in Bangladesh and DRC,35 37 and at the regional level in Uganda.39 150 Participants in Bangladesh linked high rates of VAW to poverty and a lack of education, suggesting that deprivation leads to violence,94 while others suggested that women’s increased education reduced IPV through expanding opportunities for income generation.151
Behavioural
Several studies across countries supported the hypothesis that alcohol use affects cognitive functioning, raises aggression and increases men’s perpetration of VAW.35 48 50 54 82–84 100 101 111 152 153 Partner’s illicit drug use was also associated with increased IPV perpetration in Vanuatu154 and Bangladesh.75 120
Past year transactional sex was associated with increased verbal, physical, and sexual IPV among women in Uganda.155 156 Adolescent girls and young women who were out of school and engaged in sex work within the past 6 months in Tanzania were also at increased risk of IPV.63 Evidence from Cameroon, the DRC and Uganda points to how stigmatisation and structural discrimination of sex work leads to further violence, for example, from the police.130 157–159
Societal factors
A large number of studies found that acceptance of violence among both men and women was a strong predictor of men’s perpetration and women’s experiences of different types of violence,50 54 68 77 79 80 83 87 100 101 116 126 133 139 160 with the strongest associations found when both partners supported the use of violence in relationships.82 161 Similarly, the severity of IPV increased when male partners had more accepting attitudes to violence.162 This widespread normalisation of violence was evident in qualitative reports of misogyny in Afghanistan’s social and institutional frameworks,163 and quantitative evidence of an association between community-level attitudes that support the use of VAW in relationships and an increase in women’s experiences of IPV in Tanzania.38
There is strong qualitative evidence supporting the role of patriarchal social norms and masculine ideals in contributing to VAW. In Bangladesh, men’s views on gender and sexuality were aligned with patriarchal norms suggesting that wives should obey their husbands, which helped justify VAW when women transgressed or men felt the need to reinforce these gender roles.12 164 In Tanzania and postconflict DRC, men discussed using violence against their wives to reassert their authority and position as household head.165 166 Hegemonic masculinities that see a violent man as the ideal also contributed to IPV.167
Religious affiliation, often measured as a sociodemographic variable, was associated with IPV in several studies.79 84 120 161 168–170 However, this was context-specific: while two studies found that identifying as Muslim was protective against IPV,120 161 others showed an increased risk associated with identifying as Muslim,84 89 169 or belonging to ‘other religions’.79 170
Spatial
Two studies explored violence against internally displaced persons (IDPs) in refugee camps. In an IDP camp in Northern Uganda, participants described how existing drivers of VAW, such as gender inequality, economic deprivation and alcohol abuse, were exacerbated and led to increased VAW, as did the physical layout and social characteristics of the camp itself.171 Qualitative data from four refugee camps in Uganda suggested that unequal power relations, poverty and unequal access to resources increased VAW.172
In Northern Uganda and Afghanistan, armed conflict has exacerbated existing structural factors that contribute to VAW, including gender inequalities, police corruption and poverty.163 173 174 Living in districts that experienced conflict increased women’s risk of experiencing IPV and non-partner sexual violence at the district level.68 175 176 Rape and gang rape of civilian women was widespread in conflict settings, with violent events often taking place in women’s homes during the night.67 177
Two studies explored the relationship between environmental shocks and VAW.178 179 In a qualitative study in Bangladesh, participants perceived VAW as having worsened immediately before, during, and after cyclones due to the need to move to shelters, staying in damaged homes and having to travel to collect relief and receive healthcare.179
Women living in rural areas were at greater risk of IPV than women in urban areas in Afghanistan, Liberia, Zambia and Bangladesh.74 81 86 161 180 Conversely, living in a rural area protected women against IPV in Zambia, Bolivia and Tanzania.53 79 113 One study suggested that urban social environments may be more stressful triggering conflict in relationships that leads to violence.79
A study in Bangladesh examined violence experienced by women working in the garment industry, including emotional abuse, physical and sexual violence, and economic control in the workplace and the home.181 Another study, also from Bangladesh, suggested that workplace VAW was driven by manager pressure to ensure intense productivity and the hierarchical structure within factories that fostered a culture of violence.140
figure 4 visually represents risk factors identified in all quantitative, qualitative and mixed-methods records. It highlights how overlapping categories magnify the risk of experiencing violence for women living in high-prevalence settings.
Figure 4.
Conceptualising pathways of how structural country characteristics contribute to high VAW prevalence. VAW, violence against women.
For example, VAW may result from the widespread social acceptance of violence, economic challenges that magnify interpersonal conflict, gender norms that condone male violence towards women, or as a response to unresolved trauma. Studies from high-prevalence countries included in this review draw attention to the extent of the violence in contexts where there is evidence all of these factors occur at the same time.
Discussion
This is the first review, to our knowledge, to assess risk factors for VAW with a focus on high-prevalence countries. The evidence suggests that multiple and overlapping risk factors drive high rates of VAW in these settings, rather than a single risk factor such as armed conflict or gender inequalities. While some risk factors can be considered ‘universal’ with robust support across countries at both individual and area levels (ie, child marriage, child abuse, witnessing parental IPV, social norms of violence and hegemonic masculinities of men as naturally violent), other risk factors behave differently in different contexts, including education, women’s employment and religious affiliation.
These findings point to several potential pathways between risk factors and VAW. The theorised pathways with the strongest supporting evidence across settings are summarised in figure 1. Structural characteristics observed in many high-prevalence settings (eg, armed conflict, gender inequality, widespread poverty) expose large numbers of people to violent events, increasing mental ill health and consolidating acceptance of violence as normal. This subsequently instigates VAW when interpersonal relationships are arranged patriarchally and interpersonal conflict is triggered (eg, via harmful alcohol use, food insecurity, stigma). This conceptualisation of how area-level risks lead to the use of violence within interpersonal relationships contributes to recent discussions of how risk factors for VAW may be interrelated.7
Our review highlights notable gaps in analyses of risk factors at an area level (including regional, national and global spheres). Global drivers of risk for VAW are increasingly recognised as important,182 but vastly understudied in high-prevalence settings. This obscures critical understandings of how financial flows, remittances and global aid might influence the national prevalence of VAW,183 or the role of global communication and new technology in the rise of alternative forms of violence, including cyber sexual abuse and trafficking.184 Other sizeable gaps include studies of forms of violence other than IPV and non-partner sexual violence. Although IPV is the most common form of VAW globally,1 the focus on IPV has largely obscured attention to VAW in obstetrics,185 child and forced marriage186 and femicide.187
Perhaps most surprising is that after over 20 years of VAW risk factor research and thousands of published studies on the topic, our capacity to draw meaningful conclusions about why some countries have higher rates of VAW than others is limited. Many countries with the highest prevalence of VAW are under-researched for example, Fiji, Equatorial Guinea and Tuvalu. Most research in high-prevalence settings focuses on only three countries: Bangladesh, Uganda and Tanzania (67% of included studies). There are also few longitudinal or cross-national risk factor studies, leaving a weak body of evidence around the context-specific nature of risks, which risk factors are potentially modifiable or how they may change over time.
Inevitably, the recent COVID-19 pandemic has also changed patterns of risk for VAW in high-prevalence settings. There has been an increase in evidence around the impact of lockdown measures on the perpetuation of VAW globally,188 which has not been captured by this review. While the evidence synthesised in the review remains relevant for thinking about contextual risks more broadly, the pandemic is likely to corroborate evidence on the role of natural disasters in perpetrating VAW.
The review has several limitations. First, we decided against a broader review strategy that would allow for a comparison between risk factors in high-prevalence settings with risk factors in countries with lower prevalence. We decided to prioritise the identification of risk factors from both qualitative and quantitative evidence from an under-represented list of countries over and above this comparative analysis. As highlighted by our results, there is a need for more cross-comparative analyses of VAW risk and its associations with national characteristics, but these are better suited to quantitative analyses of secondary data than systematic review methods. The measure used to assess high prevalence in this review was past year physical and/or sexual IPV because of widespread availability of these data as part of Sustainable Development Goal country assessments, but this may have limited the inclusion of countries that experience high levels of other forms of VAW, notably Papua New Guinea. The limited number of studies examining area-level risk factor for VAW constrain what we were able to say about high-prevalence settings, and we were unable to compare differences in prevalence and associated risk factors within countries, which would be useful areas for future research. In addition, some countries included in the review may have publication records in languages other than English, French or Spanish (eg, Angola) that were not found through our search.
While an extensive body of evidence exists on risk factors for VAW globally, the breadth of research is limited for the highest prevalence countries. Extensive researcher time and energy have gone into secondary analyses of Demographic and Health Surveys data. This has been helpful in mapping context-specific risk profiles, but VAW research in high-prevalence settings must expand beyond a handful of well-researched countries and risks. Further area-level analyses that look at under-researched contexts, forms of violence and protective factors are needed to inform future interventions in areas where VAW is pervasive.
Addressing multiple intersecting forms of violence and discrimination as part of the leave-no-woman-behind agenda will require improved understandings of how certain contexts can contribute to a woman’s increased risk of violence. At a global level, such analyses can help contribute to more targeted and appropriate multicomponent programming for VAW prevention programmes, offering a valuable tool for international donors. For policy-makers in countries with high VAW prevalence, better understandings of the contextual factors driving within-country variations are essential for addressing structural inequalities and uneven access to existing services, and for identifying protective factors that could be better leveraged as part of national strategies. However, this requires a meaningful shift away from national analyses of risk factors and towards more advanced understandings of the contexts that create them.
Acknowledgments
We would like to sincerely thank Ruby Bailey and Jessica Gardner for their assistance with the early design and search strategy for this review.
Footnotes
Handling editor: Seye Abimbola
Twitter: @jvmannell, @hattiemlowe, @Lolabear88, @LuGram12, @audreyprost2
Contributors: JM, DD, NM, DO, AP, LG and GS conceptualised the study and developed the registered protocol for the review. JM and HL completed the searches, and HL, RM and LB screened abstracts and full texts, with JM acting as a fourth reviewer when needed. HL, RM and LB extracted the data and completed the meta-synthesis. LB, HL and NM analysed the quantitative data and produced figure 2 summarising effect sizes of relevant studies. JM and HL drafted the manuscript, with substantial written input from HAFMJ, SV, AP, DD, LB, RM and DO. All authors reviewed and edited multiple versions of the manuscript, and all authors approved the final version. JM acquired funding for the study and is the guarantor.
Funding: Funding was provided by UKRI (grant no: MR/S033629/1).
Disclaimer: The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organisation, . Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva, Switzerland, 2013. [Google Scholar]
- 2.World Health Organisation . Violence against women prevalence estimates, 2018. Geneva, Switzerland, 2021: 87. [Google Scholar]
- 3.Gibbs A, Jewkes R, Willan S, et al. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18-30) women and men in urban informal settlements in South Africa: a cross-sectional study and structural equation model. PLoS One 2018;13:e0204956. 10.1371/journal.pone.0204956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valdez-Santiago R, Híjar M, Rojas Martínez R, et al. Prevalence and severity of intimate partner violence in women living in eight Indigenous regions of Mexico. Soc Sci Med 2013;82:51–7. 10.1016/j.socscimed.2013.01.016 [DOI] [PubMed] [Google Scholar]
- 5.Hossain M, Zimmerman C, Kiss L, et al. Men’s and women’s experiences of violence and traumatic events in rural Côte d'Ivoire before, during and after a period of armed conflict. BMJ Open 2014;4:e003644. 10.1136/bmjopen-2013-003644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jewkes R, Fulu E, Tabassam Naved R, et al. Women's and men's reports of past-year prevalence of intimate partner violence and rape and women's risk factors for intimate partner violence: a multicountry cross-sectional study in Asia and the Pacific. PLoS Med 2017;14:e1002381. 10.1371/journal.pmed.1002381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibbs A, Dunkle K, Ramsoomar L, et al. New learnings on drivers of men’s physical and/or sexual violence against their female partners, and women’s experiences of this, and the implications for prevention interventions. Glob Health Action 2020;13:1739845. 10.1080/16549716.2020.1739845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montesanti SR. The role of structural and interpersonal violence in the lives of women: a conceptual shift in prevention of gender-based violence. BMC Womens Health 2015;15:93. 10.1186/s12905-015-0247-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Central Statistics Organization/Afghanistan, M.o.P.H.A., and ICF . Afghanistan demographic and health survey 2015. Kabul, Afghanistan: Central Statistics Organization, 2017. [Google Scholar]
- 10.The DHS Program, . Congo Democratic Republic SPA, 2017-18 - Key Findings. Kinshasa: L’École de Santé Publique, Université de Kinshasa, 2019. [Google Scholar]
- 11.UNFPA . kNOwVAWdata phase I report. Bangkok, Thailand, 2021: p. 56. [Google Scholar]
- 12.Namy S, Carlson C, O'Hara K, et al. Towards a feminist understanding of intersecting violence against women and children in the family. Soc Sci Med 2017;184:40–8. 10.1016/j.socscimed.2017.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gracia E, Merlo J. Intimate partner violence against women and the Nordic paradox. Soc Sci Med 2016;157:27–30. 10.1016/j.socscimed.2016.03.040 [DOI] [PubMed] [Google Scholar]
- 14.Yakubovich AR, Stöckl H, Murray J, et al. Risk and protective factors for intimate partner violence against women: systematic review and meta-analyses of Prospective-Longitudinal studies. Am J Public Health 2018;108:e1–11. 10.2105/AJPH.2018.304428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stith SM, Smith DB, Penn CE, et al. Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review. Aggress Violent Behav 2004;10:65–98. 10.1016/j.avb.2003.09.001 [DOI] [Google Scholar]
- 16.Costa BM, Kaestle CE, Walker A, et al. Longitudinal predictors of domestic violence perpetration and victimization: a systematic review. Aggress Violent Behav 2015;24:261–72. 10.1016/j.avb.2015.06.001 [DOI] [Google Scholar]
- 17.Capaldi DM, Knoble NB, Shortt JW, et al. A systematic review of risk factors for intimate partner violence. Partner Abuse 2012;3:231–80. 10.1891/1946-6560.3.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waltermaurer E. Public Justification of intimate partner violence: a review of the literature. Trauma Violence Abuse 2012;13:167–75. 10.1177/1524838012447699 [DOI] [PubMed] [Google Scholar]
- 19.Vanderende KE, Yount KM, Dynes MM, et al. Community-level correlates of intimate partner violence against women globally: a systematic review. Soc Sci Med 2012;75:1143–55. 10.1016/j.socscimed.2012.05.027 [DOI] [PubMed] [Google Scholar]
- 20.Guedes A, Bott S, Garcia-Moreno C, et al. Bridging the gaps: a global review of intersections of violence against women and violence against children. Glob Health Action 2016;9:31516. 10.3402/gha.v9.31516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rezaeian M. The association between natural disasters and violence: a systematic review of the literature and a call for more epidemiological studies. J Res Med Sci 2013;18:1103–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Gracia-Leiva M, Puente-Martínez A, Ubillos-Landa S, et al. Dating violence (DV): a systematic meta-analysis review. Anales de Psicología 2019;35:300–13. 10.6018/analesps.35.2.333101 [DOI] [Google Scholar]
- 23.Shamu S, Abrahams N, Temmerman M, et al. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS One 2011;6:e17591. 10.1371/journal.pone.0017591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brownridge DA, Taillieu TL, Tyler KA, et al. Pregnancy and intimate partner violence: risk factors, severity, and health effects. Violence Against Women 2011;17:858–81. 10.1177/1077801211412547 [DOI] [PubMed] [Google Scholar]
- 25.Verdejo IC, Calvo CB. Analysis of violence against elderly woman. In: Social exclusion and gender-based violence. 161. Amsterdam: Elsevier Science Bv, 2014: 110–4. 10.1016/j.sbspro.2014.12.018 [DOI] [Google Scholar]
- 26.McCloskey LA, Boonzaier F, Steinbrenner SY, et al. Determinants of intimate partner violence in sub-Saharan Africa: a review of prevention and intervention programs. Partner Abuse 2016;7:277–315. 10.1891/1946-6560.7.3.277 [DOI] [Google Scholar]
- 27.Muluneh MD, Stulz V, Francis L, et al. Gender based violence against women in sub-Saharan Africa: a systematic review and meta-analysis of cross-sectional studies. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17030903. [Epub ahead of print: 01 02 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bourey C, Williams W, Bernstein EE, et al. Systematic review of structural interventions for intimate partner violence in low- and middle-income countries: organizing evidence for prevention. BMC Public Health 2015;15:1165. 10.1186/s12889-015-2460-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.BMJ . Leaving no woman, no child, and no adolescent behind, 2020. Available: https://www.bmj.com/content/368/bmj.l6986
- 30.World Health Organization . WHO multi-country study on women’s health and domestic violence against women REPORT - Initial results on prevalence, health outcomes and women’s responses. Geneva, 2005. [Google Scholar]
- 31.Department of Economic and Social Affairs Statistical Division . Data series: 5.2.1 Proportion of ever-partnered women and girls subjected to physical and/or sexual violence by a current or former intimate partner in the previous 12 months, by age (%) [Internet] SDG Indicators Database (old interface). United Nations, 2020. [Google Scholar]
- 32.Bonell C, Hinds K, Dickson K, et al. What is positive youth development and how might it reduce substance use and violence? A systematic review and synthesis of theoretical literature. BMC Public Health 2016;16:135. 10.1186/s12889-016-2817-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heyvaert M, Hannes K, Onghena P. Using mixed methods research synthesis for literature reviews. SAGE mixed methods research series. Los Angeles: SAGE, 2017: 324. [Google Scholar]
- 34.Dixon-Woods M, Cavers D, Agarwal S, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6:35. 10.1186/1471-2288-6-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tiruneh FN, Chuang K-Y, Ntenda PAM, et al. Unwanted pregnancy, pregnancy loss, and other risk factors for intimate partner violence in the Democratic Republic of the Congo. Women Health 2018;58:983–1000. 10.1080/03630242.2017.1377800 [DOI] [PubMed] [Google Scholar]
- 36.Yount KM, Crandall A, Cheong YF, et al. Child marriage and intimate partner violence in rural Bangladesh: a longitudinal multilevel analysis. Demography 2016;53:1821–52. 10.1007/s13524-016-0520-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Department for International Development . From evidence to policy: addressing gender-based violence against women and girls in Bangladesh. London, UK, 2013. [Google Scholar]
- 38.Vyas S, Heise L. How do area-level socioeconomic status and gender norms affect partner violence against women? Evidence from Tanzania. Int J Public Health 2016;61:p. 971–980. 10.1007/s00038-016-0876-y [DOI] [PubMed] [Google Scholar]
- 39.Amegbor PM, Pascoe L. Variations in emotional, sexual, and physical intimate partner violence among women in Uganda: a multilevel analysis. J Interpers Violence 2021;36:NP7868–98. 10.1177/0886260519839429 [DOI] [PubMed] [Google Scholar]
- 40.Semenza DC, Roof KA, James‐Hawkins L, et al. Gender‐equitable parental decision making and intimate partner violence Perpetration in Bangladesh. J Marriage Fam 2019;81:920–35. 10.1111/jomf.12579 [DOI] [Google Scholar]
- 41.Yount KM, Roof KA, Naved RT. Multilevel influences on men’s partner violence justification, control over family decisions, and partner violence perpetration in Bangladesh. Psychol Violence 2018;8:367–78. 10.1037/vio0000171 [DOI] [Google Scholar]
- 42.VanderEnde KE, Sibley LM, Cheong YF, et al. Community economic status and intimate partner violence against women in Bangladesh: compositional or contextual effects? Violence Against Women 2015;21:679–99. 10.1177/1077801215576938 [DOI] [PubMed] [Google Scholar]
- 43.Yount KM, James-Hawkins L, Cheong YF, et al. Men's perpetration of partner violence in Bangladesh: community gender norms and violence in childhood. Psychol Men Masc 2018;19:117–30. 10.1037/men0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gibbs A, Corboz J, Jewkes R. Factors associated with recent intimate partner violence experience amongst currently married women in Afghanistan and health impacts of IPV: a cross sectional study. BMC Public Health 2018;18:593. 10.1186/s12889-018-5507-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jewkes R, Corboz J, Gibbs A. Trauma exposure and IPV experienced by Afghan women: analysis of the baseline of a randomised controlled trial. PLoS One 2018;13:e0201974. 10.1371/journal.pone.0201974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jewkes R, Corboz J, Gibbs A. Violence against Afghan women by husbands, mothers-in-law and siblings-in-law/siblings: risk markers and health consequences in an analysis of the baseline of a randomised controlled trial. PLoS One 2019;14:e0211361. 10.1371/journal.pone.0211361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Logie CH, Okumu M, Mwima S, et al. Social ecological factors associated with experiencing violence among urban refugee and displaced adolescent girls and young women in informal settlements in Kampala, Uganda: a cross-sectional study. Confl Health 2019;13:60. 10.1186/s13031-019-0242-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Messersmith LJ, Halim N, Steven Mzilangwe E, et al. Childhood trauma, gender inequitable attitudes, alcohol use and multiple sexual partners: correlates of intimate partner violence in northern Tanzania. J Interpers Violence 2021;36:0886260517731313. 10.1177/0886260517731313 [DOI] [PubMed] [Google Scholar]
- 49.Naved RT, Mamun MA, Parvin K, et al. Magnitude and correlates of intimate partner violence against female garment workers from selected factories in Bangladesh. PLoS One 2018;13:e0204725. 10.1371/journal.pone.0204725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pengpid S, Peltzer K. Intimate partner violence victimization and perpetuation among female adolescents and adults in Timor-Leste. Gender & Behaviour 2018;16:11055–64. [Google Scholar]
- 51.Akhter R, Wilson JK. Using an Ecological Framework to Understand Men’s Reasons for Spousal Abuse: An Investigation of the Bangladesh Demographic and Health Survey 2007. J Fam Violence 2016;31:27–38. 10.1007/s10896-015-9741-7 [DOI] [Google Scholar]
- 52.Islam TM, Tareque MI, Sugawa M, et al. Correlates of intimate partner violence against women in Bangladesh. J Fam Violence 2015;30:433–44. 10.1007/s10896-015-9683-0 [DOI] [Google Scholar]
- 53.Meekers D, Pallin SC, Hutchinson P. Prevalence and correlates of physical, psychological, and sexual intimate partner violence in Bolivia. Glob Public Health 2013;8:588–606. 10.1080/17441692.2013.776093 [DOI] [PubMed] [Google Scholar]
- 54.Centre VWs. Vanuatu national survey on women’s lives and family relationships. Port Villa, Vanuatu, 2011. [Google Scholar]
- 55.Tumwesigye NM, Kyomuhendo GB, Greenfield TK, et al. Problem drinking and physical intimate partner violence against women: evidence from a national survey in Uganda. BMC Public Health 2012;12:399. 10.1186/1471-2458-12-399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Straus MA. Social stress and marital violence in a national sample of American families. Ann N Y Acad Sci 1980;347: :229–50. 10.1111/j.1749-6632.1980.tb21275.x [DOI] [PubMed] [Google Scholar]
- 57.Bamiwuye SO, Odimegwu C. Spousal violence in sub-Saharan Africa: does household poverty-wealth matter? Reprod Health 2014;11:45. 10.1186/1742-4755-11-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abramsky T, Lees S, Stöckl H, et al. Women's income and risk of intimate partner violence: secondary findings from the MAISHA cluster randomised trial in north-western Tanzania. BMC Public Health 2019;19:1108. 10.1186/s12889-019-7454-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reese BM, et al. Prevalence and Risk Factors of Women’s Past-Year Physical IPV Perpetration and Victimization in Tanzania. J Interpers Violence 2017:886260517738775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vyas S, Mbwambo J, Heise L. Women’s Paid Work and Intimate Partner Violence: Insights from Tanzania. Fem Econ 2015;21:35–58. 10.1080/13545701.2014.935796 [DOI] [Google Scholar]
- 61.Karim R, Swahnberg K. Does female authority prevent male marital violence? Evidence from rural Bangladesh. J Interpers Violence 2021;36:0886260518801023. 10.1177/0886260518801023 [DOI] [PubMed] [Google Scholar]
- 62.Stets JE. Cohabiting and marital aggression: the role of social isolation. J Marriage Fam 1991;53:669–80. 10.2307/352742 [DOI] [Google Scholar]
- 63.Nyato D, Materu J, Kuringe E, et al. Prevalence and correlates of partner violence among adolescent girls and young women: evidence from baseline data of a cluster randomised trial in Tanzania. PLoS One 2019;14:e0222950. 10.1371/journal.pone.0222950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bott S, Guedes A, Goodwin M, et al. Violence against women in Latin America and the Caribbean: a comparative analysis of population-based data from 12 countries. Washington, DC: Pan American Health Organization, 2012. [Google Scholar]
- 65.Conroy AA, Tsai AC, Clark GM, et al. Relationship power and sexual violence among HIV-positive women in rural Uganda. AIDS Behav 2016;20:2045–53. 10.1007/s10461-016-1385-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zablotska IB, Gray RH, Koenig MA, et al. Alcohol use, intimate partner violence, sexual coercion and HIV among women aged 15-24 in Rakai, Uganda. AIDS Behav 2009;13:225–33. 10.1007/s10461-007-9333-5 [DOI] [PubMed] [Google Scholar]
- 67.Bartels SA, Scott JA, Mukwege D, et al. Patterns of sexual violence in Eastern Democratic Republic of Congo: reports from survivors presenting to Panzi hospital in 2006. Confl Health 2010;4:9. 10.1186/1752-1505-4-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kelly J, Colantuoni E, Robinson C, et al. From political to personal violence: links between conflict and non-partner physical violence in post-conflict Liberia. Glob Public Health 2019;14:1639–52. 10.1080/17441692.2019.1650949 [DOI] [PubMed] [Google Scholar]
- 69.Haque MA, Choudhury N, Ahmed SMT, et al. Factors associated with domestic violence in rural Bangladesh. J Interpers Violence 2022;37:1248–69. 10.1177/0886260520922353 [DOI] [PubMed] [Google Scholar]
- 70.Haque MA, Moniruzzaman S, Janson S, et al. Children's exposure to psychological abuse and neglect: a population-based study in rural Bangladesh. Acta Paediatr 2021;110:257–64. 10.1111/apa.15340 [DOI] [PubMed] [Google Scholar]
- 71.Rahman M, Hoque MA, Mostofa MG, et al. Association between adolescent marriage and intimate partner violence: a study of young adult women in Bangladesh. Asia Pac J Public Health 2014;26:160–8. 10.1177/1010539511423301 [DOI] [PubMed] [Google Scholar]
- 72.Gubi D, Nansubuga E, Wandera SO. Correlates of intimate partner violence among married women in Uganda: a cross-sectional survey. BMC Public Health 2020;20:1008. 10.1186/s12889-020-09123-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Odimegwu C, Frade S. The influence of adolescent age at first Union on physical IPV and fertility in Uganda: a path analysis. South African Journal of Child Health 2018;12:51–6. 10.7196/SAJCH.2018.v12i2b.1498 [DOI] [Google Scholar]
- 74.Qamar M, Harris MA, Tustin JL. The association between child marriage and domestic violence in Afghanistan. J Interpers Violence 2020:886260520951310. 10.1177/0886260520951310 [DOI] [PubMed] [Google Scholar]
- 75.Johnson KB, Das MB. Spousal violence in Bangladesh as reported by men: prevalence and risk factors. J Interpers Violence 2009;24:977–95. 10.1177/0886260508319368 [DOI] [PubMed] [Google Scholar]
- 76.Karim KMR, Law CK. Microcredit and Marital Violence: Moderating effects of Husbands’ gender ideology. J Fam Violence 2016;31:227–38. 10.1007/s10896-015-9763-1 [DOI] [Google Scholar]
- 77.Murshid NS, Murshid N. Intergenerational transmission of marital violence: results from a nationally representative sample of men. J Interpers Violence 2018;33:211–27. 10.1177/0886260515604413 [DOI] [PubMed] [Google Scholar]
- 78.Murshid NS. Men's report of domestic violence Perpetration in Bangladesh: correlates from a nationally representative survey. J Interpers Violence 2017;32:290–307. 10.1177/0886260515585544 [DOI] [PubMed] [Google Scholar]
- 79.Klomegah RY. Intimate partner violence (IPV) in Zambia: an examination of risk factors and gender perceptions. J Comp Fam Stud 2008;39:557–69. 10.3138/jcfs.39.4.557 [DOI] [Google Scholar]
- 80.Ogland EG, Xu X, Bartkowski JP, et al. Intimate partner violence against married women in Uganda. J Fam Violence 2014;29:869–79. 10.1007/s10896-014-9640-3 [DOI] [Google Scholar]
- 81.Coll CVN, Ewerling F, García-Moreno C, et al. Intimate partner violence in 46 low-income and middle-income countries: an appraisal of the most vulnerable groups of women using National health surveys. BMJ Glob Health 2020;5:e002208. 10.1136/bmjgh-2019-002208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vyas S, Jansen HAFM. Unequal power relations and partner violence against women in Tanzania: a cross-sectional analysis. BMC Womens Health 2018;18:185. 10.1186/s12905-018-0675-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tlapek SM. Women's status and intimate partner violence in the Democratic Republic of Congo. J Interpers Violence 2015;30:2526–40. 10.1177/0886260514553118 [DOI] [PubMed] [Google Scholar]
- 84.Dalal K, Rahman F, Jansson B. Wife abuse in rural Bangladesh. J Biosoc Sci 2009;41:561–73. 10.1017/S0021932009990046 [DOI] [PubMed] [Google Scholar]
- 85.Das TK, Alam MF, Bhattacharyya R, et al. Causes and contexts of domestic violence: tales of help-seeking married women in Sylhet, Bangladesh. Asian Social Work and Policy Review 2015;9:163–76. 10.1111/aswp.12055 [DOI] [Google Scholar]
- 86.Karamagi CAS, Tumwine JK, Tylleskar T, et al. Intimate partner violence against women in eastern Uganda: implications for HIV prevention. BMC Public Health 2006;6:284. 10.1186/1471-2458-6-284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abramsky T, Watts CH, Garcia-Moreno C, et al. What factors are associated with recent intimate partner violence? findings from the WHO multi-country study on women's health and domestic violence. BMC Public Health 2011;11:109. 10.1186/1471-2458-11-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naved RT. Sexual violence towards married women in Bangladesh. Arch Sex Behav 2013;42:595–602. 10.1007/s10508-012-0045-1 [DOI] [PubMed] [Google Scholar]
- 89.Ruchira Tabassum Naved, Persson LA. Dowry and spousal physical violence against women in Bangladesh. J Fam Issues 2010;31:830–56. 10.1177/0192513X09357554 [DOI] [PubMed] [Google Scholar]
- 90.Naved RT, Persson LA. Factors associated with spousal physical violence against women in Bangladesh. Ann N Y Acad Sci 2006;1087:320–38. [DOI] [PubMed] [Google Scholar]
- 91.Hague G, Thiara RK, Turner A. Bride-price and its links to domestic violence and poverty in Uganda: a participatory action research study. Womens Stud Int Forum 2011;34:550–61. 10.1016/j.wsif.2011.06.008 [DOI] [Google Scholar]
- 92.Kaye DK, Mirembe F, Ekstrom AM, et al. Implications of bride price on domestic violence and reproductive health in Wakiso district, Uganda. Afr Health Sci 2005;5:300–3. 10.5555/afhs.2005.5.4.300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rehema M, Prisca K. The causes of intimate partner violence in Babati district. International Journal of Innovation and Applied Studies 2016:1400–6. [Google Scholar]
- 94.Schuler SR, Islam F. Women's acceptance of intimate partner violence within marriage in rural Bangladesh. Stud Fam Plann 2008;39:49–58. 10.1111/j.1728-4465.2008.00150.x [DOI] [PubMed] [Google Scholar]
- 95.Black E, Worth H, Clarke S, et al. Prevalence and correlates of intimate partner violence against women in conflict affected Northern Uganda: a cross-sectional study. Confl Health 2019;13:35. 10.1186/s13031-019-0219-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fulu E, Jewkes R, Roselli T, et al. Prevalence of and factors associated with male perpetration of intimate partner violence: findings from the UN Multi-country cross-sectional study on men and violence in Asia and the Pacific. Lancet Glob Health 2013;1:e187–207. 10.1016/S2214-109X(13)70074-3 [DOI] [PubMed] [Google Scholar]
- 97.Garcia-Moreno C, Jansen HAFM, Ellsberg M, et al. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet 2006;368:1260–9. 10.1016/S0140-6736(06)69523-8 [DOI] [PubMed] [Google Scholar]
- 98.Kwagala B, Wandera SO, Ndugga P, et al. Empowerment, partner's behaviours and intimate partner physical violence among married women in Uganda. BMC Public Health 2013;13:1112. 10.1186/1471-2458-13-1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Islam MJ, Mazerolle P, Broidy L, et al. Exploring the prevalence and correlates associated with intimate partner violence during pregnancy in Bangladesh. J Interpers Violence 2021;36:0886260517730029. 10.1177/0886260517730029 [DOI] [PubMed] [Google Scholar]
- 100.Secretariat of the Pacific Community . Solomon Islands family health and safety study. Honiara, Solomon Islands: Ministry of Women, Youth & Children’s Affairs, 2009. [Google Scholar]
- 101.Secretariat of the Pacific Community . Kiribati family health and support study: a study on violence against women and children. Noumea, New Caledonia, 2010. [Google Scholar]
- 102.Wandera SO, Kwagala B, Ndugga P, et al. Partners' controlling behaviors and intimate partner sexual violence among married women in Uganda. BMC Public Health 2015;15:214. 10.1186/s12889-015-1564-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Samuels F, Le Masson V, Gupta T. One step forwards half a step backwards: changing patterns of intimate partner violence in Bangladesh. J Fam Violence 2019;34:107–18. 10.1007/s10896-018-0003-3 [DOI] [Google Scholar]
- 104.Stark E, Hester M. Coercive control: update and review. Violence Against Women 2019;25:81–104. 10.1177/1077801218816191 [DOI] [PubMed] [Google Scholar]
- 105.Zegenhagen S, Ranganathan M, Buller AM. Household decision-making and its association with intimate partner violence: examining differences in men's and women's perceptions in Uganda. SSM Popul Health 2019;8:100442. 10.1016/j.ssmph.2019.100442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sambisa W, Angeles G, Lance PM, et al. Prevalence and correlates of physical spousal violence against women in slum and nonslum areas of urban Bangladesh. J Interpers Violence 2011;26:2592–618. 10.1177/0886260510388282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Camargo E. Gender inequality and intimate partner violence in Bolivia. Rev Colomb Soc 2019;42:257–77. 10.15446/rcs.v42n2.69629 [DOI] [Google Scholar]
- 108.Rahman M, Hoque MA, Makinoda S. Intimate partner violence against women: is women Empowerment a reducing factor? A study from a national Bangladeshi sample. J Fam Violence 2011;26:411–20. 10.1007/s10896-011-9375-3 [DOI] [Google Scholar]
- 109.Stieglitz J, Gurven M, Kaplan H, et al. Infidelity, jealousy, and wife abuse among Tsimane forager-farmers: testing evolutionary hypotheses of marital conflict. Evol Hum Behav 2012;33:438–48. 10.1016/j.evolhumbehav.2011.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Stöckl H, Watts C, Kilonzo Mbwambo JK. Physical violence by a partner during pregnancy in Tanzania: prevalence and risk factors. Reprod Health Matters 2010;18:171–80. 10.1016/S0968-8080(10)36525-6 [DOI] [PubMed] [Google Scholar]
- 111.Centre FWsC. Somebody’s life, everybody’s business! National Research on Women’s Health and Life Experiences in Fiji (2010/2011): A survey exploring the prevalence, incidence and attitudes towards intimate partner violence in Fiji 2013.
- 112.Kapiga S, Harvey S, Muhammad AK, et al. Prevalence of intimate partner violence and abuse and associated factors among women enrolled into a cluster randomised trial in northwestern Tanzania. BMC Public Health 2017;17:190. 10.1186/s12889-017-4119-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kiwuwa-Muyingo S, Kadengye DT. Prevalence and risk factors for women's reports of Past-Year intimate partner violence: a comparative analysis of six East African national surveys. J Interpers Violence 2020:886260520969374. 10.1177/0886260520969374 [DOI] [PubMed] [Google Scholar]
- 114.Nimi T, Fraga S, Costa D, et al. Prevalence, determinants, and effects of violence during pregnancy: a maternity-based cross-sectional study in Luanda, Angola. J Public Health Afr 2019;10:116–22. 10.4081/jphia.2019.1050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Parmar P, Agrawal P, Greenough PG, et al. Sexual violence among host and refugee population in Djohong district, eastern Cameroon. Glob Public Health 2012;7:974–94. 10.1080/17441692.2012.688061 [DOI] [PubMed] [Google Scholar]
- 116.Affairs, F.D.o.H.a.S . Federated states of Micronesia family health and safety study. Pohnpei State, FSM, 2014. [Google Scholar]
- 117.Decker MR, Latimore AD, Yasutake S, et al. Gender-Based violence against adolescent and young adult women in low- and middle-income countries. J Adoles Health 2015;56:188–96. 10.1016/j.jadohealth.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 118.Peterman A, Bleck J, Palermo T. Age and intimate partner violence: an analysis of global trends among women experiencing victimization in 30 developing countries. J Adolesc Health 2015;57:624–30. 10.1016/j.jadohealth.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 119.Wilson N. Demographic characteristics and intimate partner violence. Journal of International Development 2019;31:632–57. [Google Scholar]
- 120.Aklimunnessa K, Khan MMH, Kabir M, et al. Prevalence and correlates of domestic violence by husbands against wives in Bangladesh: evidence from a national survey. J Men's Health Gender 2007;4:52–63. 10.1016/j.jmhg.2006.10.016 [DOI] [Google Scholar]
- 121.Anyango JF, Muliira JK. Intimate partner violence among pregnant women in rural Uganda. Afr J Midwifery Women’s Health 2013;3. [Google Scholar]
- 122.Kabwama SN, Bukenya J, Matovu JKB, et al. Intimate partner violence among HIV positive women in care - results from a national survey, Uganda 2016. BMC Womens Health 2019;19:130. 10.1186/s12905-019-0831-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Speizer IS. Intimate partner violence attitudes and experience among women and men in Uganda. J Interpers Violence 2010;25:1224–41. 10.1177/0886260509340550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McCloskey LA, Williams C, Larsen U. Gender inequality and intimate partner violence among women in Moshi, Tanzania. Int Fam Plan Perspect 2005;31:124–30. 10.1363/3112405 [DOI] [PubMed] [Google Scholar]
- 125.Prabhu M, McHome B, Ostermann J, et al. Prevalence and correlates of intimate partner violence among women attending HIV voluntary counseling and testing in northern Tanzania, 2005-2008. Int J Gynaecol Obstet 2011;113:63–7. 10.1016/j.ijgo.2010.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kouyoumdjian FG, Calzavara LM, Bondy SJ, et al. Risk factors for intimate partner violence in women in the Rakai community cohort study, Uganda, from 2000 to 2009. BMC Public Health 2013;13:566. 10.1186/1471-2458-13-566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mulawa MI, Reyes HLM, Foshee VA, et al. Associations between peer network gender norms and the Perpetration of intimate partner violence among urban Tanzanian men: a multilevel analysis. Prev Sci 2018;19:427–36. 10.1007/s11121-017-0835-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wadji DL, Ketcha Wanda GJM, Wicky C, et al. From the mother to the child: the intergenerational transmission of experiences of violence in mother-child dyads exposed to intimate partner violence in Cameroon. J Interpers Violence 2020:886260520948148. 10.1177/0886260520948148 [DOI] [PubMed] [Google Scholar]
- 129.Crombach A, Bambonyé M. Intergenerational violence in Burundi: experienced childhood maltreatment increases the risk of abusive child rearing and intimate partner violence. Eur J Psychotraumatol 2015;6:26995. 10.3402/ejpt.v6.26995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Erickson M, Goldenberg SM, Master A, et al. Interpersonal and structural contexts of intimate partner violence among female sex workers in conflict-affected Northern Uganda. Women Health 2018;58:759–73. 10.1080/03630242.2017.1342742 [DOI] [PubMed] [Google Scholar]
- 131.Malama K, Sagaon-Teyssier L, Parker R, et al. Client-Initiated violence against Zambian female sex workers: prevalence and associations with behavior, environment, and sexual history. J Interpers Violence 2021;36:0886260519860083. 10.1177/0886260519860083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Stöckl H, March L, Pallitto C, et al. Intimate partner violence among adolescents and young women: prevalence and associated factors in nine countries: a cross-sectional study. BMC Public Health 2014;14:751. 10.1186/1471-2458-14-751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Islam TM, Tareque MI, Tiedt AD, et al. The intergenerational transmission of intimate partner violence in Bangladesh. Glob Health Action 2014;7:1–11. 10.3402/gha.v7.23591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Valentine A, Akobirshoev I, Mitra M. Intimate partner violence among women with disabilities in Uganda. Int J Environ Res Public Health 2019;16. 10.3390/ijerph16060947. [Epub ahead of print: 16 03 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Birbeck G, Chomba E, Atadzhanov M, et al. The social and economic impact of epilepsy in Zambia: a cross-sectional study. Lancet Neurol 2007;6:39–44. 10.1016/S1474-4422(06)70629-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hasan T, Muhaddes T, Camellia S, et al. Prevalence and experiences of intimate partner violence against women with disabilities in Bangladesh: results of an explanatory sequential mixed-method study. J Interpers Violence 2014;29:3105–26. 10.1177/0886260514534525 [DOI] [PubMed] [Google Scholar]
- 137.Chirwa E, Jewkes R, Van Der Heijden I, et al. Intimate partner violence among women with and without disabilities: a pooled analysis of baseline data from seven violence-prevention programmes. BMJ Glob Health 2020;5. 10.1136/bmjgh-2019-002156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Scolese A, Asghar K, Pla Cordero R, et al. Disability status and violence against women in the home in North Kivu, Democratic Republic of Congo. Glob Public Health 2020;15:985–98. 10.1080/17441692.2020.1741661 [DOI] [PubMed] [Google Scholar]
- 139.Sileo KM, Kershaw TS, Gilliam S, et al. Trauma exposure and intimate partner violence among young pregnant women in Liberia. J Interpers Violence 2021;36:10101. 10.1177/0886260519881533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gibbs A, Jewkes R, Willan S, et al. Workplace violence in Bangladesh's garment industry. Soc Sci Med 2019;235:112383. 10.1016/j.socscimed.2019.112383 [DOI] [PubMed] [Google Scholar]
- 141.Lundberg P, Nakasujja N, Musisi S, et al. Sexual risk behavior, sexual violence, and HIV in persons with severe mental illness in Uganda: hospital-based cross-sectional study and national comparison data. Am J Public Health 2015;105:1142–8. 10.2105/AJPH.2014.302479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Nandi C, Elbert T, Bambonye M, et al. Predicting domestic and community violence by soldiers living in a conflict region. Psychol Trauma Theory Res Pract Policy 2017;9:663–71. 10.1037/tra0000262 [DOI] [PubMed] [Google Scholar]
- 143.Rees S, et al. Risk of perpetrating intimate partner violence amongst men exposed to torture in conflict-affected Timor-Leste. Global Mental Health 2018;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sambisa W, Angeles G, Lance PM, et al. Physical and sexual abuse of wives in urban Bangladesh: husbands' reports. Stud Fam Plann 2010;41:165–78. 10.1111/j.1728-4465.2010.00241.x [DOI] [PubMed] [Google Scholar]
- 145.Alleyne-Green B, Kulick A, Matsuzaka S, et al. War violence exposure, reintegration experiences and intimate partner violence among a sample of War-Affected females in Sierra Leone. Global Social Welfare 2019;6:97–106. 10.1007/s40609-018-0125-9 [DOI] [Google Scholar]
- 146.Kinyanda E, Weiss HA, Mungherera M, et al. Intimate partner violence as seen in post-conflict eastern Uganda: prevalence, risk factors and mental health consequences. BMC Int Health Hum Rights 2016;16:5. 10.1186/s12914-016-0079-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Saile R, Neuner F, Ertl V, et al. Prevalence and predictors of partner violence against women in the aftermath of war: a survey among couples in northern Uganda. Soc Sci Med 2013;86: :17–25. 10.1016/j.socscimed.2013.02.046 [DOI] [PubMed] [Google Scholar]
- 148.Kelly J, Kabanga J, Cragin W, et al. 'If your husband doesn't humiliate you, other people won't': gendered attitudes towards sexual violence in eastern Democratic Republic of Congo. Glob Public Health 2012;7:285–98. 10.1080/17441692.2011.585344 [DOI] [PubMed] [Google Scholar]
- 149.Rees S, Thorpe R, Tol W, et al. Testing a cycle of family violence model in conflict-affected, low-income countries: a qualitative study from Timor-Leste. Soc Sci Med 2015;130:284–91. 10.1016/j.socscimed.2015.02.013 [DOI] [PubMed] [Google Scholar]
- 150.Amegbor PM, Rosenberg MW. What geography can tell us? Effect of higher education on intimate partner violence against women in Uganda. Appl Geogr 2019;106:71–81. 10.1016/j.apgeog.2019.03.009 [DOI] [Google Scholar]
- 151.Schuler SR, Lenzi R, Nazneen S, et al. Perceived decline in intimate partner violence against women in Bangladesh: qualitative evidence. Stud Fam Plann 2013;44:243–57. 10.1111/j.1728-4465.2013.00356.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Mootz JJ, Muhanguzi FK, Panko P, et al. Armed conflict, alcohol misuse, decision-making, and intimate partner violence among women in Northeastern Uganda: a population level study. Confl Health 2018;12:37. 10.1186/s13031-018-0173-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Yaya S, Ghose B. Alcohol drinking by Husbands/Partners is associated with higher intimate partner violence against women in Angola. Safety 2019;5:5. 10.3390/safety5010005 [DOI] [Google Scholar]
- 154.McKelvie S, Leodoro B, Sala T, et al. Prevalence, patterns, and determinants of intimate partner violence experienced by women who are pregnant in Sanma Province, Vanuatu. J Interpers Violence 2020:886260520969235. 10.1177/0886260520969235 [DOI] [PubMed] [Google Scholar]
- 155.Miller AP, Pitpitan EV, Nabukalu D, et al. Transactional sex, alcohol use and intimate partner violence against women in the Rakai region of Uganda. AIDS Behav 2021;25:1144–58. 10.1007/s10461-020-03069-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Emusu D. Sexual violence and correlates among women in HIV discordant union, Uganda. Birmingham: University of Alabama, 2007. [Google Scholar]
- 157.Lim S, Peitzmeier S, Cange C, et al. Violence against female sex workers in Cameroon: accounts of violence, harm reduction, and potential solutions. J Acquir Immune Defic Syndr 2015;68(Suppl 2):S241–7. 10.1097/QAI.0000000000000440 [DOI] [PubMed] [Google Scholar]
- 158.Kiernan B, Mishori R, Masoda M. 'There is fear but there is no other work': a preliminary qualitative exploration of the experience of sex workers in eastern Democratic Republic of Congo. Cult Health Sex 2016;18:237–48. 10.1080/13691058.2015.1073790 [DOI] [PubMed] [Google Scholar]
- 159.Schwitters A, Swaminathan M, Serwadda D, et al. Prevalence of rape and client-initiated gender-based violence among female sex workers: Kampala, Uganda, 2012. AIDS Behav 2015;19(Suppl 1):S68–76. 10.1007/s10461-014-0957-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Okenwa L, Lawoko S. Social indicators and physical abuse of women by intimate partners: a study of women in Zambia. Violence Vict 2010;25:278–88. 10.1891/0886-6708.25.2.278 [DOI] [PubMed] [Google Scholar]
- 161.Alio AP, Clayton HB, Garba M, et al. Spousal concordance in attitudes toward violence and reported physical abuse in African couples. J Interpers Violence 2011;26:2790–810. 10.1177/0886260510390951 [DOI] [PubMed] [Google Scholar]
- 162.Fine SL, Kane JC, Murray SM, et al. The role of violence acceptance and inequitable gender norms in intimate partner violence severity among couples in Zambia. J Interpers Violence 2021;36:NP10744–65. 10.1177/0886260519876722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ahmad L, Anctil Avoine P, Avoine PA. Misogyny in ‘post-war’ Afghanistan: the changing frames of sexual and gender-based violence. J Gend Stud 2018;27:86–101. 10.1080/09589236.2016.1210002 [DOI] [Google Scholar]
- 164.Islam M, Karim KMR. Men's views on gender and sexuality in a Bangladesh village. Int Q Community Health Educ 2011;32:339–54. 10.2190/IQ.32.4.f [DOI] [PubMed] [Google Scholar]
- 165.Kohli A, Perrin N, Mpanano RM, et al. Family and community driven response to intimate partner violence in post-conflict settings. Soc Sci Med 2015;146:276–84. 10.1016/j.socscimed.2015.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Manji K, Heise L, Cislaghi B. Gender norms and intimate partner violence in Kirumba, Tanzania. Violence Against Women 2020;26:2062–82. [DOI] [PubMed] [Google Scholar]
- 167.Anwary A. Construction of hegemonic masculinity: violence against wives in Bangladesh. Womens Stud Int Forum 2015;50:37–46. 10.1016/j.wsif.2015.02.011 [DOI] [Google Scholar]
- 168.Naved RT, Azim S, Bhuiya A, et al. Physical violence by husbands: magnitude, disclosure and help-seeking behavior of women in Bangladesh. Soc Sci Med 2006;62:2917–29. 10.1016/j.socscimed.2005.12.001 [DOI] [PubMed] [Google Scholar]
- 169.Stake S, Ahmed S, Tol W, et al. Prevalence, associated factors, and disclosure of intimate partner violence among mothers in rural Bangladesh. J Health Popul Nutr 2020;39:14. 10.1186/s41043-020-00223-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Yaya S, Kunnuji M, Bishwajit G. Intimate partner violence: a potential challenge for women’s health in Angola. Challenges 2019;10:21. 10.3390/challe10010021 [DOI] [Google Scholar]
- 171.Ager A, Bancroft C, Berger E, et al. Local constructions of gender-based violence amongst IDPs in northern Uganda: analysis of archival data collected using a gender- and age-segmented participatory ranking methodology. Confl Health 2018;12:10. 10.1186/s13031-018-0140-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kwiringira JN, Mutabazi MM, Mugumya F, et al. Experiences of gender based violence among refugee populations in Uganda: evidence from four refugee camps. East Afr Soc Sci Res Rev 2018;34:291–311. 10.1353/eas.2018.0010 [DOI] [Google Scholar]
- 173.Annan J, Brier M. The risk of return: intimate partner violence in northern Uganda's armed conflict. Soc Sci Med 2010;70:152–9. 10.1016/j.socscimed.2009.09.027 [DOI] [PubMed] [Google Scholar]
- 174.Mannell J, et al. A Qualitative Study of Women’s Lived Experiences of Conflict and Domestic Violence in Afghanistan. Violence Against Women 2020:1077801220935191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kelly JTD, Colantuoni E, Robinson C, et al. From the battlefield to the bedroom: a multilevel analysis of the links between political conflict and intimate partner violence in Liberia. BMJ Glob Health 2018;3:e000668. 10.1136/bmjgh-2017-000668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Rustad SA, Østby G, Nordås R. Artisanal mining, conflict, and sexual violence in eastern DRC. Extr Ind Soc 2016;3:475–84. 10.1016/j.exis.2016.01.010 [DOI] [Google Scholar]
- 177.Amowitz LL, Reis C, Lyons KH, et al. Prevalence of war-related sexual violence and other human rights abuses among internally displaced persons in Sierra Leone. JAMA 2002;287:513–21. 10.1001/jama.287.4.513 [DOI] [PubMed] [Google Scholar]
- 178.Epstein A, Bendavid E, Nash D, et al. Drought and intimate partner violence towards women in 19 countries in sub-Saharan Africa during 2011-2018: a population-based study. PLoS Med 2020;17:e1003064. 10.1371/journal.pmed.1003064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Rezwana NP. Gender-Based violence before, during and after cyclones: slow violence and layered disasters. Disasters 2020. 10.1111/disa.12441 [DOI] [PubMed] [Google Scholar]
- 180.Afiaz A, Biswas RK, Shamma R, et al. Intimate partner violence (IPV) with miscarriages, stillbirths and abortions: identifying vulnerable households for women in Bangladesh. PLoS One 2020;15:e0236670. 10.1371/journal.pone.0236670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Naved R, Rahman T, Willan S, et al. Female garment workers' experiences of violence in their homes and workplaces in Bangladesh: a qualitative study. Soc Sci Med 2018;196:150–7. 10.1016/j.socscimed.2017.11.040 [DOI] [PubMed] [Google Scholar]
- 182.Fulu E, Miedema S. Violence against women: globalizing the integrated ecological model. Violence Against Women 2015;21:1431–55. 10.1177/1077801215596244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.True J. The political economy of violence against women. Oxford University Press, 2012. [Google Scholar]
- 184.Albright K, Greenbaum J, Edwards SA, et al. Systematic review of facilitators of, barriers to, and recommendations for healthcare services for child survivors of human trafficking globally. Child Abuse Negl 2020;100:104289. 10.1016/j.chiabu.2019.104289 [DOI] [PubMed] [Google Scholar]
- 185.Minckas N, Gram L, Smith C, et al. Disrespect and abuse as a predictor of postnatal care utilisation and maternal-newborn well-being: a mixed-methods systematic review. BMJ Glob Health 2021;6. 10.1136/bmjgh-2020-004698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kalamar AM, Lee-Rife S, Hindin MJ. Interventions to prevent child marriage among young people in low- and middle-income countries: a systematic review of the published and gray literature. J Adolesc Health 2016;59:S16–21. 10.1016/j.jadohealth.2016.06.015 [DOI] [PubMed] [Google Scholar]
- 187.Stöckl H, Devries K, Rotstein A, et al. The global prevalence of intimate partner homicide: a systematic review. Lancet 2013;382:859–65. 10.1016/S0140-6736(13)61030-2 [DOI] [PubMed] [Google Scholar]
- 188.BMJ . Violence against women during covid-19 pandemic restrictions, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-007704supp001.pdf (612.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable.