Abstract
Racial disparities in hospitalization rates for ambulatory care sensitive conditions (ACSCs) are concerning and may signal differential access to high-quality ambulatory care. Whether racial disparities are improving due to better ambulatory care versus artificially closing due to increased use of observation status is unclear. Using 2011–15 Medicare data, we sought to determine if black-white disparities in avoidable hospitalizations are improving and evaluated the degree to which changes in observations for ACSCs may be contributing to changes in these gaps. We found that, while the racial gap in avoidable hospitalizations due to ACSCs has narrowed, the decrease in the racial gap of avoidable hospitalizations seems to be explained by a concomitant increase in the gap of avoidable observation visits. This suggests that changes in admissions to observation status seem to be driving the reduction in racial disparities of avoidable hospitalizations rather than changes in the ambulatory setting.
Ensuring all Americans receive high quality and equitable ambulatory care is a key policy priority.1–3 One way that policymakers have assessed the effectiveness of high quality primary care is by examining rates of potentially avoidable hospitalizations for ambulatory care sensitive conditions (ACSCs).4, 5 The notion is that certain types of hospitalizations, such as those related to diabetes care, may be avoidable if patients have access to effective ambulatory care, including high-quality primary care services and outpatient ambulatory specialty care. Currently, racial and ethnic minorities have much higher rates of potentially avoidable hospitalizations.6, 7 Therefore, there is substantial concern that these disparities may reflect differences in the accessibility and quality of ambulatory care they receive.7, 8
In recent years, there has been an increase in attention on improving ambulatory care as a means to improve population health, and ideally, reduce disparities.3, 9 Prior work has shown that black patients are less likely to establish primary care as their usual source of care,10, 11 and instead are much more likely to use the emergency department (ED) compared to white patients.10 Therefore, part of the efforts stemming from the Affordable Care Act (ACA) in 2010 increased the focus on improving primary care among the Medicare population. In particular, alternative payment models, like accountable care organizations, incentivized providers to lower costs by reducing avoidable hospitalizations and readmissions. Another ACA program called the Hospital Readmission Reduction Program (HRRP) also encouraged hospitals to lower readmission rates or risk a financial penalty. However, although the HRRP seemed promising in early days, recent data has suggested that apparent drops in readmissions may be attributable to changes in the use of observation status and in diagnoses coding rather than improvements in care.12–14 That is, one way hospitals may reduce their reported readmission rate is by increasing use of observation status in place of hospital admissions. Indeed, the literature suggests that the use of observation has been increasing over time among the Medicare population.15, 16
Taken together, this context raises important questions around racial disparities in quality of care for the Medicare population. To date, it is unclear whether there has been a meaningful narrowing in the racial gap of avoidable hospitalizations, and whether the use of preventable hospitalizations as an outcome measure is appropriate given the changes in incentives. If the gaps in preventable acute care use have narrowed, the extent to which that narrowing may represent better care in the ambulatory setting or changes in admission rates to observation status would be helpful to quantify.
Therefore, using national Medicare data, we sought to answer the following questions. Are disparities in avoidable hospitalizations for ambulatory care sensitive conditions improving over time between black and white patients? If so, to what extent are increases in the use of observation status accounting for improvement in racial disparities across avoidable hospitalizations? Finally, are there specific types of conditions that are primarily driving this improvement?
Study Data and Methods
Data
We used the national 20% Medicare Inpatient and Outpatient File from 2011 to 2015 to identify avoidable hospitalizations and avoidable observation visits for ACSCs using the Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs) Software.17 These include visits for acute conditions (dehydration, bacterial pneumonia, urinary tract infections,(UTIs), perforated appendix) and chronic conditions (including diabetes short-term complications, diabetes long-term complications, uncontrolled diabetes, lower extremity amputation related to diabetes, asthma in adults, chronic obstructive pulmonary disease (COPD), hypertension, heart failure, and angina without procedure). This algorithm excludes certain types of patients depending on the condition, including transfer patients, pregnant patients, immunosuppressed patients, and those who have undergone certain types of urological procedures for UTIs, among others.17 To obtain patient characteristics, we used the Medicare Beneficiary Summary File. To identify patient comorbidities, we used the Chronic Condition Data Warehouse (CCW) File.18
Primary Outcome
Our primary outcomes were the number of avoidable hospitalizations or observation visits for ACSCs for each patient during each year.
Statistical Analysis
We first tabulated patient characteristics and comorbidities for black and non-Hispanic white patients in the Medicare dataset across the first and last year of our study period, and also of those with at least 1 observation or hospitalization stay. We used chi square tests for categorical variables and t-tests for continuous variables.
To illustrate changing rates over time, we estimated yearly risk-adjusted rates for black and white patients using linear regression. We treated time as a categorical predictor of avoidable hospitalizations and observation visits, adjusting for age, sex, dual eligibility, and CCW comorbidities. We also included hospital referral region (HRR) fixed effects. To quantify the changes in rates over time and allow comparison between white and black patients, we also estimated risk-adjusted slopes using time as a continuous predictor. The primary predictors were race and its interaction with time, and the model was adjusted for the same factors as described above. We repeated the analysis for acute and chronic conditions separately and by individual type of condition. Additionally, we stratified patients into high-risk and low-risk patients based on their hierarchical condition category (HCC) risk score, with those with the highest 25% HCC risk score defined as “high-risk” and the remaining 75% as “low-risk.” We then repeated the models as stated above for these patients. Of note, we chose to use linear models given that our primary hypothesis is that there is a one-to-one substitution effect between observation stays and avoidable hospitalizations.
Analyses for this study were performed using SAS (Version 9.4). The Harvard T.H. Chan School of Public Health (HSPH) Institutional Review Board’s Committee on the Use of Human Subjects approved this study.
Limitations
Our study has several limitations. Although we used well-established algorithms to define preventable acute care episodes, it is likely that these represent a spectrum of preventability, with some individual admissions likely not preventable through better outpatient care. However, since this analysis is comparing races, the potential misclassification of preventability is not systematically different for minority populations vs. non-minority populations. Second, the observational nature of this study does not allow us to draw causal inferences of the relationship between increased observation use and decreased hospitalization use. Third, given that we used administrative claims data, our lack of granular clinical information limits our risk-adjustment models. In addition, our study is limited to a five-year period. Finally, our data are limited only to Medicare patients. Whether our findings would hold for commercially insured or Medicaid patients is unclear.
Study Results
Patient Characteristics
We first compared characteristics of black vs. white Medicare beneficiaries within each year. In 2011, black patients were on average younger, more likely dual-eligible for Medicaid and Medicare, and on average had a higher number of chronic conditions than non-Hispanic white Medicare beneficiaries (Appendix Exhibit A1).19 This included higher rates of dementia, chronic kidney disease, diabetes, and history of stroke or transient ischemic attack among black patients compared to white patients. White patients, however, had higher rates of certain types of chronic conditions, including atrial fibrillation and chronic obstructive pulmonary disease (COPD), than black patients. Similar differences in patient demographics and comorbidities were observed in 2015. Furthermore, patients with at least one hospitalization stay were older and had more comorbidities than those with at least one observation stay (Appendix Exhibit A2).19
Trends in avoidable hospitalizations and observation visits over time
In 2011, black patients experienced 674.8 per 10,000 hospitalizations while white patients had 546.7 per 10,000 (Exhibit 1). By 2015, the rate of avoidable hospitalizations dropped to 483.9 per 10,000 for black patients and 407.8 per 10,000 for white patients. The yearly slope change was −46.2 per 10,000/year for black patients and −33.2 per 10,000/year for white patients. The difference in slopes was −13.1 per 10,000/year (95% CI: −15.6 to −10.6, p<0.001), which means that black patients experienced a greater decline in avoidable hospitalizations during this time. In terms of relative improvement, black patients experienced a 28% relative decrease while white patients experienced a 25% relative decrease in hospitalizations (data not shown).
EXHIBIT 1.
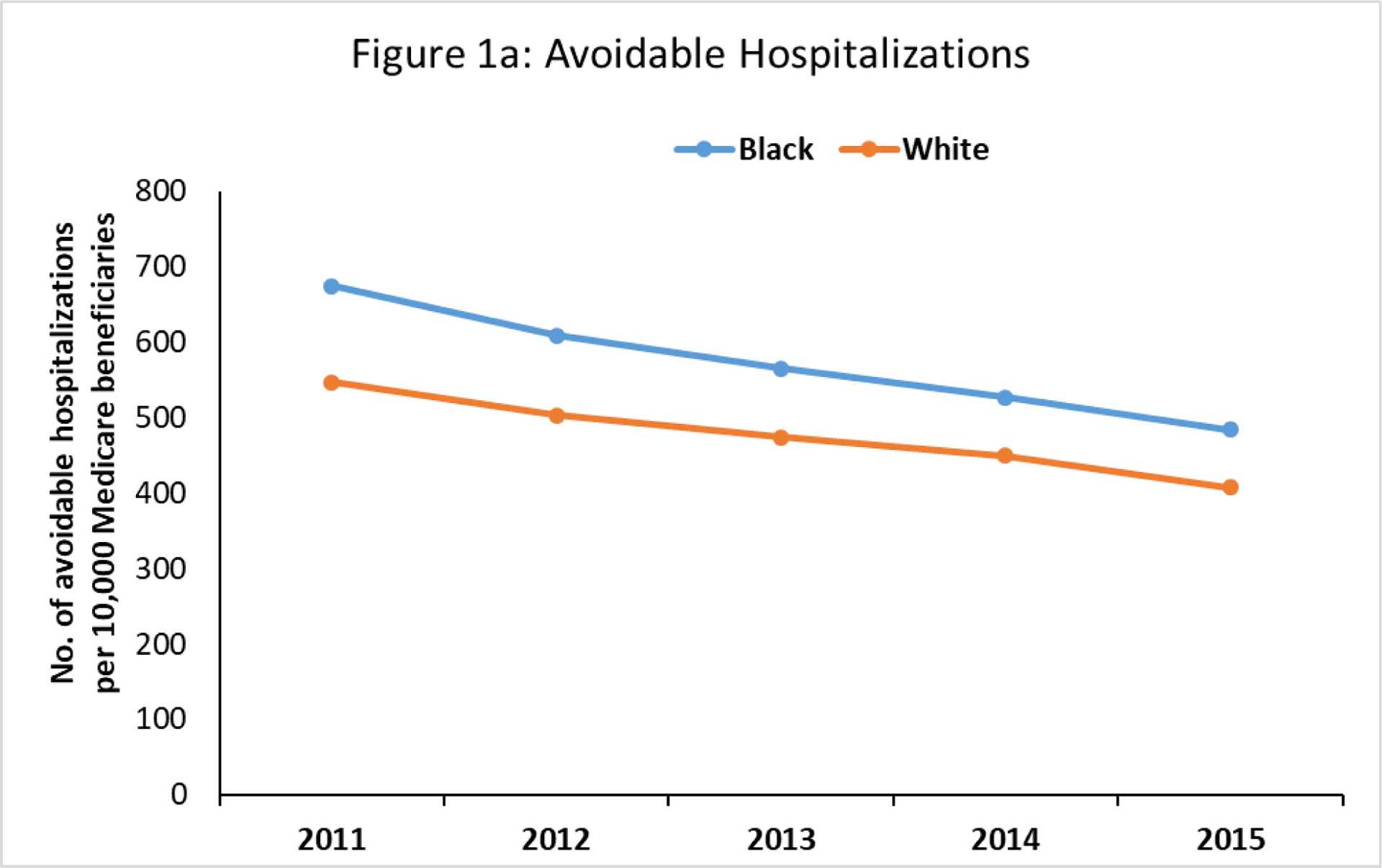
Trends in avoidable hospitalizations between black and white Medicare beneficiaries for ambulatory care sensitive conditions, 2011–15.
SOURCE: Authors’ analysis of 2011–15 data from 20% Medicare Inpatient and Outpatient Files and Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs) Software
NOTES: Yearly point estimates are based on a risk-adjusted linear regression model where year is included as a categorical predictor.
We next examined yearly rates of avoidable observation visits. In 2011, the rate of avoidable observation visits was 417.9 per 10,000 for black patients and 378.8 per 10,000 for white patients (Exhibit 2). By 2015, the rates of observations increased for black patients to 570.6 per 10,000 and for white patients to 470.6 per 10,000. The yearly slope change was 39.2 per 10,000/year for black patients and 23.2 per 10,000/year for white patients. The difference in slopes was 16.0 per 10,000/year (95% CI: 11.3 to 20.6, p<0.001), which means that black patients experienced a greater increase in avoidable observation visits during this time. In terms of relative improvement, black patients experienced a 37% relative increase while white patients experienced a 24% relative increase (data not shown).
Exhibit 2.
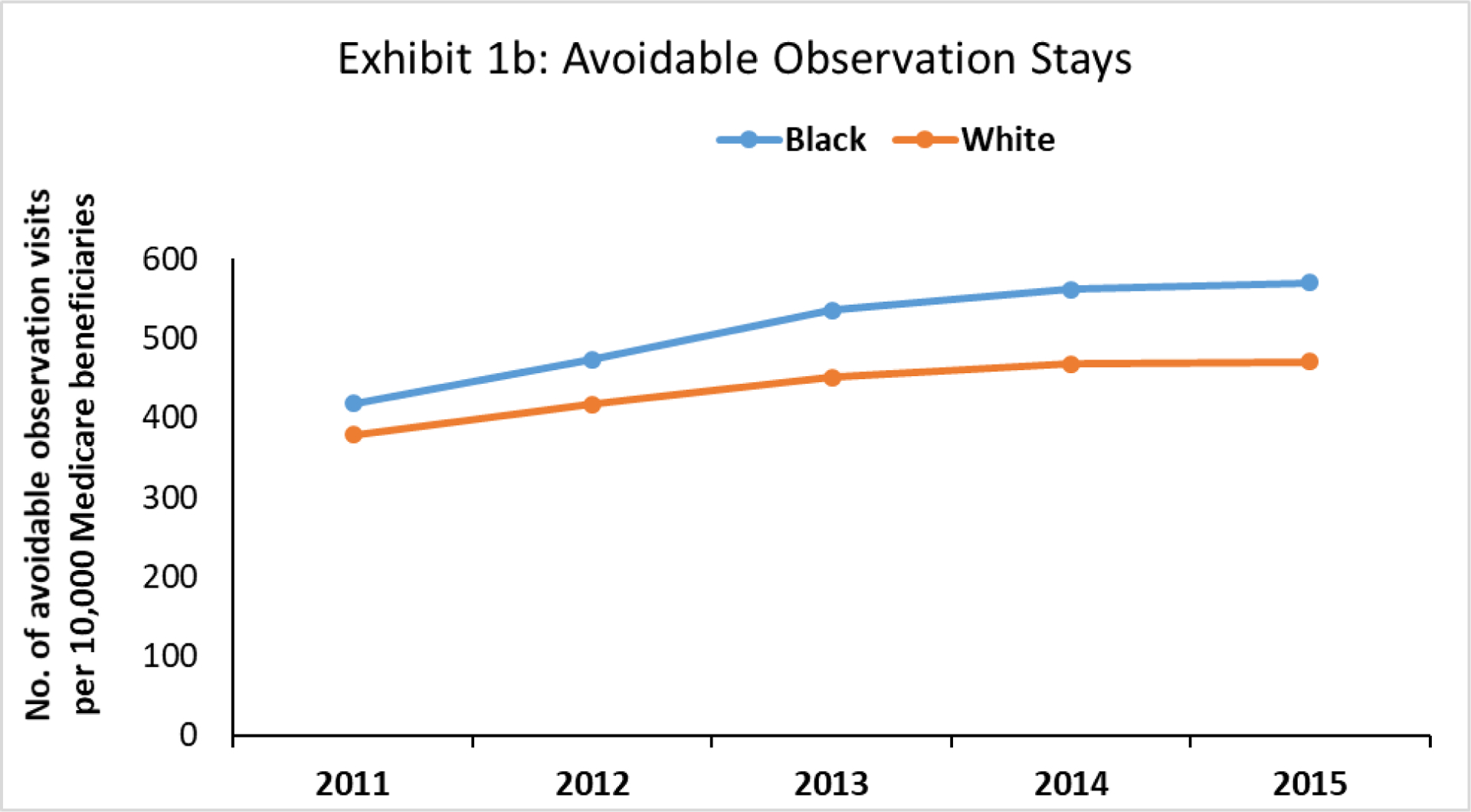
Trends in avoidable observation stays between black and white Medicare beneficiaries for ambulatory care sensitive conditions, 2011–15.
SOURCE: Authors’ analysis of 2011–15 data from 20% Medicare Inpatient and Outpatient Files and Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs) Software
NOTES: Yearly point estimates are based on a risk-adjusted linear regression model where year is included as a categorical predictor.
When combining observation visits and avoidable hospitalization visits, we did not find a significant difference in the slopes of black patients compared to white patients. For all conditions, the slope of improvement for black patients was −6.3 per 10,000/year compared to −3.0 per 10,000/year for white patients (Exhibit 3). The difference in slopes was −3.2 per 10,000/year (95% CI: −8.6 to 2.1, p=0.24).
Exhibit 3.
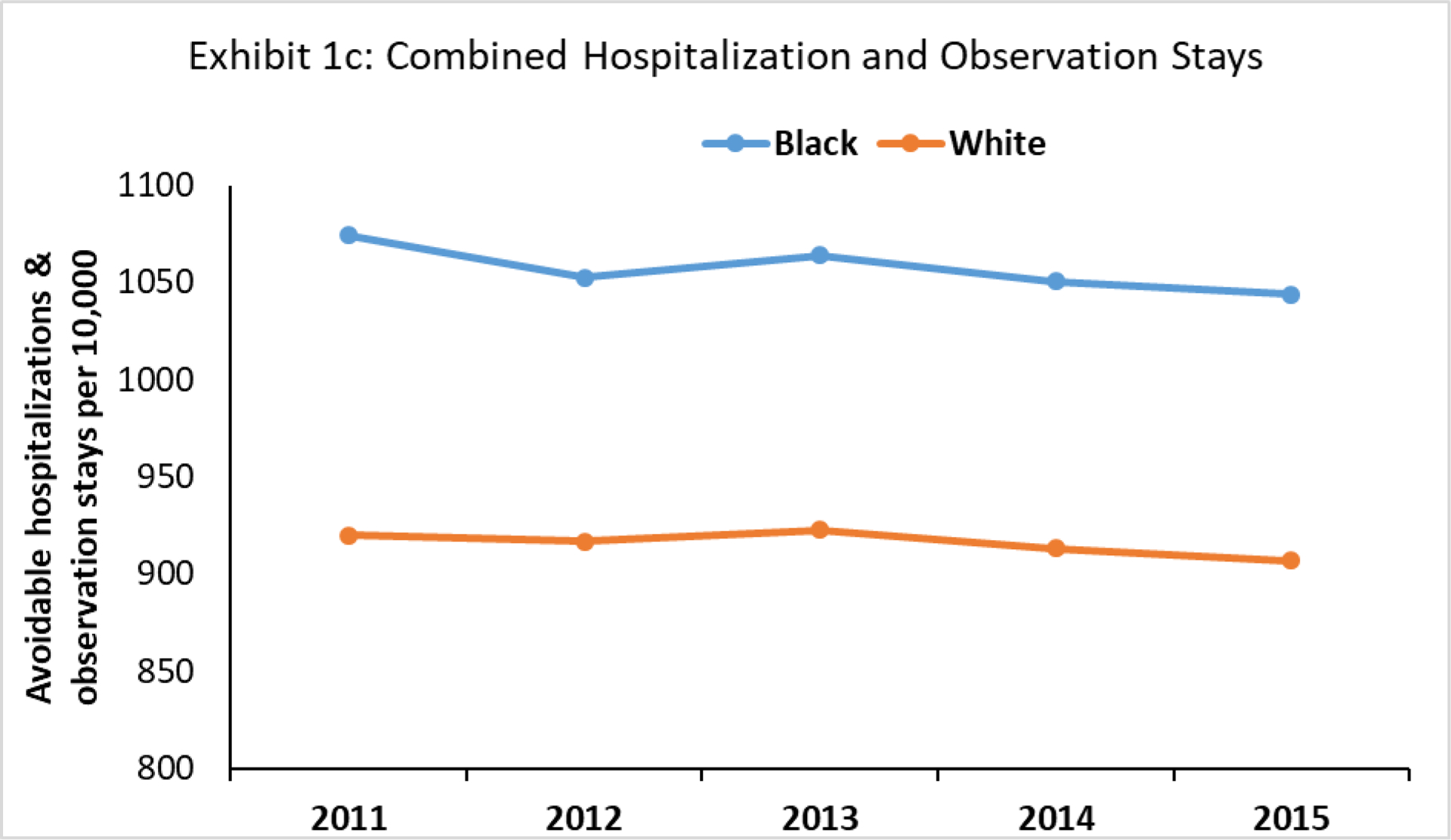
Trends in combined avoidable hospitalization and observation stays between black and white Medicare beneficiaries for ambulatory care sensitive conditions, 2011–15.
SOURCE: Authors’ analysis of 2011–15 data from 20% Medicare Inpatient and Outpatient Files and Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs) Software
NOTES: Yearly point estimates are based on a risk-adjusted linear regression model where year is included as a categorical predictor.
Next, we examined rates among high-risk and low-risk patients. We found much greater declines in hospitalizations among high-risk black patients relative to white patients (Appendix Exhibit A3).19 However, we also saw much greater increases in observation stays among high-risk black patients relative to white patients.
Finally, we also examined trends in avoidable hospitalizations and observation visits by type of condition. We found that changes in the rates of avoidable hospitalizations and observation visits for chronic conditions were the primary driver of our findings. For chronic conditions, the slope of avoidable hospitalizations for black patients was −27.6 per 10,000/year while it was −17.0 per 10,000/year for white patients, for a difference in slopes of −10.6 per 10,000/year (95% CI: −12.5 to −8.6, p<0.001) (Exhibit 4). The slope of avoidable observations for chronic conditions was 33.0 per 10,000/year for black patients and 17.5 per 10,000/year for white patients, for a difference in slopes of 15.4 per 10,000/year (95% CI: 11.6 to 19.3, p<0.001). This substitution effect appeared to be predominantly driven by the following ACSCs: diabetes long-term complications, COPD/asthma, hypertension, and heart failure (Appendix Exhibit A4).19 For acute conditions, white patients on average had higher rates of avoidable hospitalizations and observation visits, which were predominantly driven by visits for bacterial pneumonia.
Exhibit 4.
Differences in the yearly change of avoidable hospitalizations and observation visits by condition and race, 2011–15
| Conditions | Baseline Year (2011)a | Latest Year (2015)a | Yearly Change (Slope)b | Difference-in-slopesc | P Value |
|---|---|---|---|---|---|
| Overall | |||||
| Hospitalizations per 10,000 people | |||||
| Black | 674.8 | 483.9 | −46.2 | −13.1 | <0.001 |
| White | 546.7 | 407.8 | −33.2 | ||
| Observations per 10,000 people | |||||
| Black | 417.9 | 570.6 | 39.2 | 16.0 | <0.001 |
| White | 378.8 | 470.6 | 23.2 | ||
| Combined hospitalizations and observations per 10,000 people | |||||
| Black | 1074.1 | 1043.7 | −6.3 | −3.2 | p=0.24 |
| White | 920.0 | 906.8 | −3.0 | ||
| Chronic Conditions | |||||
| Hospitalizations per 10,000 people | |||||
| Black | 446.3 | 328.8 | −27.6 | −10.6 | p<0.001 |
| White | 294.6 | 221.5 | −17.0 | ||
| Observations per 10,000 people | |||||
| Black | 331.7 | 461.4 | 33.0 | 15.4 | p<0.001 |
| White | 260.0 | 327.7 | 17.5 | ||
| Combined hospitalizations and observations per 10,000 people | |||||
| Black | 744.8 | 756.4 | 4.8 | −0.9 | p=0.68 |
| White | 553.2 | 573.5 | 5.7 | ||
| Acute Conditions | |||||
| Hospitalizations per 10,000 people | |||||
| Black | 228.5 | 155.1 | −18.6 | −2.5 | p=0.001 |
| White | 252.1 | 186.3 | −16.1 | ||
| Observations per 10,000 people | |||||
| Black | 86.2 | 109.2 | 6.2 | 0.5 | p=0.61 |
| White | 118.8 | 142.9 | 5.7 | ||
| Combined hospitalizations and observations per 10,000 people | |||||
| Black | 329.3 | 286.3 | −11.1 | −2.3 | p=0.08 |
| White | 366.7 | 333.3 | −8.8 | ||
Source/Notes: SOURCE: Authors’ analysis of 2011–15 data from 20% Medicare Inpatient and Outpatient Files and Agency for Healthcare Research and Quality’s Prevention Quality Indicators (PQIs) Software
NOTES: These results are from linear regression models and the estimated changes are adjusted for covariates.
Yearly point estimates are based on a risk-adjusted linear regression model where year is included as a categorical predictor.
The yearly change in each subgroup was estimated from a separate risk-adjusted linear regression model where year was treated as a continuous predictor.
The difference in slopes and its p-value are calculated from the same model as one that determined the yearly change, and it represents the slope in black patients minus the slope in white patients.
Discussion
Using national Medicare data, we examined whether racial disparities in avoidable hospitalizations, a frequently-used metric used to assess the accessibility of quality primary care, have narrowed over time. Although we initially found that the gaps have indeed narrowed, upon further examination, we find that this narrowing appears to be entirely related to differential changes in shifting to observation status – with black patients being coded as admitted to observation status at a higher rate over time than white patients. This substitution effect is primarily driven by shifts in heart failure and diabetes-related complications. It also appears that the substitution affect is primary driven by changes occurring among high-risk Medicare patients with the highest HCC risk scores. Therefore, our findings suggest that much of the progress we are making in improving disparities in potentially avoidable hospitalizations may be mostly explained by the increased use of observation status and not changes in other factors, like the quality of care in the ambulatory setting.
It is unclear why black patients are much more likely to experience shifting from inpatient to observation status. Prior work has suggested that that physicians’ diagnostic and treatment choices differ depending on the patient’s race. For example, physicians were less likely to prescribe black patients pain medications relative to white patients.20, 21 Another study by found that black patients were less likely to be referred for cardiac catheterization than white patients.22 However, the degree to which differential decision-making is influencing physicians to be less likely to admit black patients – perhaps because they are categorically seen as being less sick, or admission is seen as less unnecessary – is unclear.
However, what is known is that the designation of observation status for patients has major financial implications given that patients tend to incur higher out-of-pocket expenses than when admitted to a hospital.23 In addition, observation patients may not qualify for Medicare coverage for subsequent skilled nursing facility care.24 Therefore, this disproportionate substitution effect observed in black patients raises concern that minority patients are facing increased financial burden due to differential decision-making by physicians and hospitals. As providers take on more risk in alternative payment models that increase pressure to reduce hospital admissions, it will be important to ensure that these new incentives to lower costs do not lead to harm for minority patients and all patients in general, especially given that the substitution effect seems to be occurring mostly among high-risk patients. This is also pertinent given recent work showing a possible association with increased mortality for patients admitted with heart failure after the HRRP policy was introduced.25
Though it is possible that patient preference may be playing a role, where white patients may more often request a hospital admission or black patients may be less likely to want admission, it is unlikely that this is a major contributor. Past research has found differences in preferences between racial groups that may help explain some of the disparities in receipt of surgical interventions, renal transplantation, or post-acute care use.26–28 However, to our knowledge, there is no strong empirical evidence to suggest that minority patients have a stronger preference for avoiding a hospitalization compared to whites. In fact, patients may be unaware of whether they are admitted to a hospital under observation vs. inpatient status.29
Our findings have important policy implications. At first glance, the reduction in avoidable hospitalizations among black patients seems to potentially indicate that care in the ambulatory setting, including primary care and preventive care, may have improved for this group. However, when accounting for changes in observation visits, our results suggest that this reduction may instead be explained by changes in disposition practice by hospitals and emergency rooms rather than possible changes in the quality of ambulatory care for black patients. Such a practice may reflect efforts by hospitals trying to avoid hospital penalties levied by the HRRP policy14 or health systems participating in ACOs trying to improve their rates for avoidable hospitalizations. It will be important for policymakers to consider updating the quality measures in existing value-based programs to limit any potential gaming by health care providers. One way to do so is by including observation rates, and also potentially ED visits, related to ASCSs and not just inpatient admissions in the metric. In addition, to the extent that better primary care leads to improvements in disparities in avoidable acute care use, policymakers may need to reconsider new approaches that can improve care delivered to vulnerable populations.
Our work adds to a body of literature examining disparities in the acute care setting.30–33 A prior study found that disparities in hospital readmissions following admissions for medical conditions have been narrowing over time.32 Given these findings, it will be important to investigate whether changes in observation rates partially contributed to this improvement. Notably, Rachael Zuckerman et al. did not find that observation changes over time explained the drop in readmission rates.34 In other work, Kathryn Fingar et al. found that rates for emergency department visits that are treated and released from the ED have also been going up over time.35 It is possible that increases in these direct ED discharges may also be partially explaining changes in avoidable hospitalizations over time. However, observations are a more likely substitute than direct ED discharges. Further work is needed to examine how changes in avoidable acute care disposition may be affecting patient outcomes.
Conclusion
In conclusion, disparities in preventable acute care use for ambulatory care sensitive conditions, a frequently-used metric for assessing quality of care in the ambulatory setting, have not narrowed over time. While the initial results seem to show that the gaps in avoidable hospitalizations were closing, closer examination of the observation status data suggests otherwise. Therefore, new efforts are needed to truly close the gap and ensure that all Americans get high-quality ambulatory care, irrespective of their race.
Supplementary Material
REFERENCES
- 1.Fiscella K Health care reform and equity: promise, pitfalls, and prescriptions. Ann Fam Med. 2011;9(1):78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aysola J, Bitton A, Zaslavsky AM, Ayanian JZ. Quality and equity of primary care with patient-centered medical homes: results from a national survey. Med Care. 2013;51(1):68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care — the growing importance of the community health center. N Engl J Med. 2010;362(22):2047–50. [DOI] [PubMed] [Google Scholar]
- 4.Moy E, Chang E, Barrett M, Control CfD, Prevention. Potentially preventable hospitalizations—United States, 2001–2009. MMWR Surveill Summ. 2013;62(Suppl 3):139–43. [PubMed] [Google Scholar]
- 5.Gao J, Moran E, Li YF, Almenoff PL. Predicting potentially avoidable hospitalizations. Med Care. 2014;52(2):164–71. [DOI] [PubMed] [Google Scholar]
- 6.Feng C, Paasche-Orlow MK, Kressin NR, Rosen JE, Lopez L, Kim EJ, et al. Disparities in potentially preventable hospitalizations: near-national estimates for Hispanics. Health Serv Res. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doshi RP, Aseltine RH Jr., Sabina AB, Graham GN Racial and ethnic disparities in preventable hospitalizations for chronic disease: prevalence and risk factors. J Racial Ethn Health Disparities. 2017;4(6):1100–6. [DOI] [PubMed] [Google Scholar]
- 8.Parchman ML, Culler SD. Preventable hospitalizations in primary care shortage areas: an analysis of vulnerable Medicare beneficiaries. Arch Fam Med. 1999;8(6):487–91. [DOI] [PubMed] [Google Scholar]
- 9.Phillips RL Jr., Bazemore AW Primary care and why it matters for U.S. health system reform. Health Aff (Millwood). 2010;29(5):806–10. [DOI] [PubMed] [Google Scholar]
- 10.Arnett MJ, Thorpe RJ Jr., Gaskin DJ, Bowie JV, LaVeist TA Race, medical mistrust, and segregation in primary care as usual source of care: findings from the Exploring Health Disparities in Integrated Communities Study. J Urban Health. 2016;93(3):456–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gaskin DJ, Arbelaez JJ, Brown JR, Petras H, Wagner FA, Cooper LA. Examining racial and ethnic disparities in site of usual source of care. J Natl Med Assoc. 2007;99(1):22–30. [PMC free article] [PubMed] [Google Scholar]
- 12.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of coded severity with readmission reduction after the hospital readmissions reduction program. JAMA Intern Med. 2018;178(2):290–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ody C, Msall L, Dafny LS, Grabowski DC, Cutler DM. Decreases in readmissions credited to Medicare’s program to reduce hospital readmissions have been overstated. Health Aff (Millwood). 2019;38(1):36–43. [DOI] [PubMed] [Google Scholar]
- 14.Wadhera RK, Joynt Maddox KE, Kazi DS, Shen C, Yeh RW. Hospital revisits within 30 days after discharge for medical conditions targeted by the Hospital Readmissions Reduction Program in the United States: national retrospective analysis. BMJ. 2019;366:l4563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright B, Zhang X, Rahman M, Abir M, Ayyagari P, Kocher KE. Evidence of racial and geographic disparities in the use of Medicare observation stays and subsequent patient outcomes relative to short-stay hospitalizations. Health Equity. 2018;2(1):45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Figueroa JF, Burke LG, Zheng J, Orav EJ, Jha AK. Trends in hospitalization vs observation stay for ambulatory care-sensitive conditions. JAMA Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality (AHRQ). QI modules [Internet]. Rockville (MD): AHRQ; [cited 2019 March 12]. Available from: https://www.qualityindicators.ahrq.gov/Archive/default.aspx# [Google Scholar]
- 18.Centers for Medicare & Medicaid Services (CMS). Chronic conditions data warehouse: condition categories [Internet]. Baltimore (MD): CMS; 2018. [cited 2019 March 12]. Available from: https://www.ccwdata.org/web/guest/condition-categories [Google Scholar]
- 19.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 20.Shah AA, Zogg CK, Zafar SN, Schneider EB, Cooper LA, Chapital AB, et al. Analgesic access for acute abdominal pain in the emergency department among racial/ethnic minority patients: a nationwide examination. Med Care. 2015;53(12):1000–9. [DOI] [PubMed] [Google Scholar]
- 21.Singhal A, Tien YY, Hsia RY. Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS One. 2016;11(8):e0159224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–26. [DOI] [PubMed] [Google Scholar]
- 23.Baugh CW, Schuur JD. Observation care--high-value care or a cost-shifting loophole? N Engl J Med. 2013;369(4):302–5. [DOI] [PubMed] [Google Scholar]
- 24.Sheehy AM, Courtney J. Medicare and the 3-inpatient midnight requirement: a statute in need of modernization. J Hosp Med. 2017;12(3):199–200. [DOI] [PubMed] [Google Scholar]
- 25.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320(24):2542–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kwoh CK, Vina ER, Cloonan YK, Hannon MJ, Boudreau RM, Ibrahim SA. Determinants of patient preferences for total knee replacement: African-Americans and whites. Arthritis Res Ther. 2015;17:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341(22):1661–9. [DOI] [PubMed] [Google Scholar]
- 28.Cagney KA, Agree EM. Racial differences in skilled nursing care and home health use: the mediating effects of family structure and social class. J Gerontol B Psychol Sci Soc Sci. 1999;54(4):S223–36. [DOI] [PubMed] [Google Scholar]
- 29.Jaffe S Medicare covers less when a hospital stay is an observation, not an admission. The Washington Post [newspaper on the Internet]. 2014. Sept 8 [cited 2019 March 12];Sect. Health & Science. Available from https://www.washingtonpost.com/national/health-science/medicare-covers-less-when-a-hospital-stay-is-an-observation-not-an-admission/2014/09/08/9c609544-2d5c-11e4-9b98-848790384093_story.html [Google Scholar]
- 30.Mehtsun WT, Figueroa JF, Zheng J, Orav EJ, Jha AK. Racial disparities in surgical mortality: the gap appears to have narrowed. Health Aff (Millwood). 2017;36(6):1057–64. [DOI] [PubMed] [Google Scholar]
- 31.Rangrass G, Ghaferi AA, Dimick JB. Explaining racial disparities in outcomes after cardiac surgery: the role of hospital quality. JAMA Surg. 2014;149(3):223–7. [DOI] [PubMed] [Google Scholar]
- 32.Figueroa JF, Zheng J, Orav EJ, Epstein AM, Jha AK. Medicare program associated with narrowing hospital readmission disparities between black and white patients. Health Aff (Millwood). 2018;37(4):654–61. [DOI] [PubMed] [Google Scholar]
- 33.Figueroa JF, Zheng J, Orav EJ, Jha AK. Across US hospitals, black patients report comparable or better experiences than white patients. Health Aff (Millwood). 2016;35(8):1391–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;0:null. [DOI] [PubMed] [Google Scholar]
- 35.Fingar KR, Barrett ML, Elixhauser A, Stocks C, Steiner CA. Trends in potentially preventable inpatient hospital admissions and emergency department visits [Internet]. Rockville (MD): AHRQ; 2015. [cited 2019 March 12]. Report No.: Statistical Brief #195. Available from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb195-Potentially-Preventable-Hospitalizations.pdf [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


