Abstract
OBJECTIVE
To prospectively analyze the association of sedentary behavior time with type 2 diabetes (T2D) risk and perform the isotemporal substitution analyses to estimate the effect of substitution of sedentary behaviors by equal time of different types of daily-life physical activities and structured exercise. We also examined modifications by the genetic predisposition to T2D.
RESEARCH DESIGN AND METHODS
We included 475,502 participants free of T2D in the UK Biobank. Sedentary time was quantified by summing up the time spent on television watching, computer use, and driving.
RESULTS
During a median follow-up of 11 years, we documented 18,169 incident T2D cases. In comparison of the extreme categories (≥6 vs. <2 h/day), the hazard ratio for T2D was 1.58 (95% CI 1.47, 1.71) after adjustment for age, race, sex, lifestyle factors, and other covariates. Replacing 30 min of sedentary behavior per day with an equal amount of time of different types of daily-life activities and structured exercise was significantly associated with a 6–31% risk reduction of T2D, with strenuous sports showing the strongest (31%, 95% CI 24, 37) benefit. Moreover, we found a significant interaction between sedentary behavior and genetic predisposition for the risk of T2D (Pinteraction = 0.0008). The association was more profound among participants with a lower genetic risk of T2D.
CONCLUSIONS
Our study indicates that sedentary behavior time is associated with an increased risk of T2D; replacing sedentary behavior with a short duration (30 min/day) of daily-life physical activities or structured exercise is related to a significant reduction in T2D risk. Furthermore, such association was stronger among those with a lower genetic risk of T2D.
Introduction
The prevalence of type 2 diabetes (T2D) has been increasing and is projected to increase to 7,079 individuals per 100,000 by 2030 worldwide (1,2). Such an escalating trend is partly due to the excessive sedentary behaviors in company with the increasingly popular use of television (TV), computer, and automobile transportation, etc. According to the objectively measured data from the National Health and Nutrition Examination Survey (NHANES), participants on average spent >50% of their monitored time, or 7.7 h/day, engaging in sedentary behaviors (3). In the U.K., ∼30% of the population spend ≥6 h engaging in sedentary behaviors on weekdays, according to the data from the Health Survey for England in 2012. Of note, trends in sedentary behavior time have been increasing significantly in the past decades (4).
Recently, the World Health Organization released new guidelines on physical activity and sedentary behavior (5), which provides new recommendations on reducing sedentary behaviors. In the U.S., sedentary behavior was also introduced as a new topic in the most recent Physical Activity Guidelines for Americans (PAG) (6) and as a new target for T2D prevention and treatment (7). However, there was insufficient evidence for quantification of a sedentary behavior threshold. Epidemiologic evidence has indicated positive associations between sedentary behavior time and T2D (8–12). However, most of the previous studies estimated the effect of sedentary lifestyle while keeping the physical activity constant in the model, i.e., by adjusting for physical activity (13–15). Such models failed to reflect the fact that for a fairly fixed period of total discretionary time, risk reductions from reducing sedentary behaviors depend on the activity that displaces sedentary behaviors (16). An isotemporal substitution paradigm would directly address such questions by theoretically replacing a certain amount of sedentary behavior time with an equal time of physical activity (16,17). In addition, although the new guidelines highlight the importance of reducing sedentary behaviors and increasing physical activity, it is largely unknown which specific types of discretionary activities would be ideal alternatives to sedentary behavior, and little is known about the extent to which substitution of sedentary behaviors by various types of physical activity reduces the risk of T2D (18).
Moreover, it is well accepted that genetic factors contribute to the development of T2D. In recent years, growing studies have shown that genetic susceptibility interacts with lifestyle factors in development of T2D (19); however, few studies have investigated the interaction between a sedentary lifestyle and genetic susceptibility in relation to T2D risk.
In this study, we prospectively analyzed the association between sedentary behavior time and the risk of T2D among participants from the UK Biobank. We particularly investigated the specific types of activity that might be substituted for sedentary behavior time to impart benefit on T2D risk reduction, with the isotemporal substitution analysis. We also examined the interaction between sedentary behavior and genetic predisposition to T2D for the incidence of the disease.
Research Design and Methods
Study Population
The UK Biobank is a large prospective cohort based in the U.K. (20,21). More than half a million participants aged 37–73 years old, living within 25 miles of 1 of the 22 assessment centers across England, Scotland, and Wales, were recruited between 2006 and 2010. Participants provided a wide range of health-related information through touchscreen questionnaires, physical measurements, and biological samples. Detailed information on the study design has previously been described (21). Written informed consent was obtained from all the participants. The study was approved by both the National Health Service National Research Ethics Service (reference no. 11/NW/0382) and the Institutional Review Board of Tulane University (2018-1872).
In the current analysis, we excluded participants with T2D at baseline (n = 13,507) and those with missing information on sedentary behaviors (n = 14,167) at baseline, leaving a total of 475,502 participants for the main analysis. When we examined the interaction between sedentary behavior and genetic susceptibility to T2D, we only included 419,997 European descent participants with complete genotyping data in the analysis.
Assessment of Sedentary Behaviors
According to the World Health Organization guideline, sedentary behavior refers to any waking behavior characterized by a low level of energy expenditure (≤1.5 METs) while sitting, reclining, or lying (22). In the current analysis, sedentary behavior time was quantified at baseline by summing up of the hours spent on TV watching, computer use (not at work), and driving. At the baseline assessment, participants were asked, “In a typical day, how many hours do you spend on watching TV?”, “In a typical day, how many hours do you spend using a computer? (Do not include using a computer at work),” and “In a typical day, how many hours do you spend driving?” We excluded extreme screen hours (TV plus personal computer use ≥12 h and driving time ≥8 h). We also categorized sedentary behavior time into four groups: <2 h/day, 2–3 h/day, 4–5 h/day, and ≥6 h/day.
Assessment of Outcomes
Prevalent T2D was identified based on the UK Biobank algorithms for the diagnosis of T2D, via self-reported medical history and medication (23). Information on incident T2D was collected through 8 February 2020. Incident T2D was defined by ICD-10 code E11 (non-insulin-dependent diabetes mellitus), ascertained according to hospital inpatient records containing data on admissions and diagnoses from the Hospital Episode Statistics for England, Scottish Morbidity Record for Scotland, and the Patients Episode Database for Wales (23,24).
Discretionary Physical Activity
Discretionary physical activity was assessed by the touchscreen questionnaire at baseline. Participants were asked about participation in five different types of activities during the prior 4 weeks. Types of activities included walking for pleasure (not as a means of transport), light do-it-yourself activity (DIY) (i.e., pruning, watering the lawn), heavy DIY (e.g., weeding, lawn mowing, carpentry, digging, chopping wood, home or car maintenance, lifting heavy objects, or using heavy tools), strenuous sports (including those that make one sweat or breathe hard), and other exercises (e.g., swimming, cycling, Keep Fit, and bowling). The average time (minutes per day) spent on each of the five different types of activities was calculated by multiplying the reported frequency by the average duration. Walking for pleasure, light DIY, and heavy DIY were combined into the category daily-life activities, and strenuous sports and other exercises were combined into an indicator of structured exercise according to the methodology of a previous study (25). Total time spent on activities was calculated by summing the average time spent on the five types of activities.
Genotype Data
Genotyping, imputation, and quality control of the genetic data were performed by the UK Biobank team. The detailed information is available from https://www.ukbiobank.ac.uk/scientists-3/genetic-data/ (26). We created a genetic risk score (GRS) for T2D using the 112 single nucleotide polymorphisms (SNPs) that passed quality control out of the 128 SNPs recently identified to be associated with T2D at genome-wide significance (27,28) (Supplementary Table 1). We applied the widely used weight method with use of the following equation: T2D GRS = (β1 × SNP1 + β2 × SNP2 + … + β112 × SNP112) × (112/sum of the β-coefficients), in which SNP was the number of the risk allele of each SNP. The T2D GRS ranged from 81.0 to 136.9. A higher GRS indicates a higher genetic predisposition to T2D.
Assessment of Other Covariates
Information on age, sex, ethnicity, average household income, education, and Townsend deprivation index (based on the participant’s postcode; higher scores indicate a higher degree of deprivation) was obtained from local National Health Service Primary Care Trust registries along with the name of the recruitment center before arrival at the assessment center. Weight and height were measured at baseline during the initial assessment center visit. BMI was calculated as weight divided by the square of height in meters during the initial assessment center visit. Alcohol intake was assessed with the touchscreen questionnaire and reported as “never,” “special occasions only,” “1–3 times per month,” “once or twice a week,” “3 or 4 times a week,” and “daily or almost daily.” Smoking status was obtained with use of the touchscreen questionnaire and reported as “never,” “previous,” or “current.” A healthy diet score was adapted from the American Heart Association guidelines and defined as adherence to four or five components of the following: 1) total fruit intake ≥4.5 pieces/week, 2) total vegetable intake ≥4.5 servings/week (3 tablespoons of vegetables considered as 1 serving), 3) total fish intake ≥2 servings/week, 4) processed meat intake less often than twice per week, and 5) red meat intake five or fewer times per week (29).
Statistical Analysis
Baseline characteristics of the study population were summarized across the categories of sedentary behavior time as n (%) for categorical variables and means (SDs) for continuous variables. Follow-up time was calculated from the recruitment date to the date of the first diagnosis of T2D, death, or end of the follow-up—whichever came first. We conducted the restricted cubic spline regression to assess the dose-response association between sedentary behavior time and T2D incidence. The reference was set at the 5th percentile of sedentary behavior time. Cox proportional hazards models were used to estimate the hazard ratios (HRs) and 95% CI for the associations between sedentary behavior time and risk of T2D. The proportional hazards assumption was tested by inclusion of an interaction term between sedentary behavior time and the time variable. No evidence of violations of the assumption was found. In model 1, we adjusted for age, sex, and ethnicity. In the multivariable-adjusted model 2, we additionally controlled for smoking status, alcohol intake, healthy diet score, education, average household income, total time spent on physical activity, Townsend deprivation index, hypertension, cholesterol-lowering medications, antihypertensive medications, T2D GRS, and the first 10 genetic principal components. Since obesity is a strong mediator for the association between sedentary behavior time and T2D, adjustment for BMI in the model constitutes statistical overcorrection and results in underestimation of the true effect of sedentary behavior, so we did not adjust for BMI in the main analyses.
To further explore whether the discretionary physical activity may shift the risk of T2D induced by sedentary behaviors, and to what extent the risk could be reduced, we performed isotemporal substitution analyses to estimate the effect of substitution of sedentary behaviors by equal time of different types of daily-life physical activities and structured exercise (16). The isotemporal substitution model estimates the effect of replacing sedentary behavior with each type of physical activity for the same amount of time (16). The isotemporal substitution model could be expressed as a basic proportional hazards model as follows:
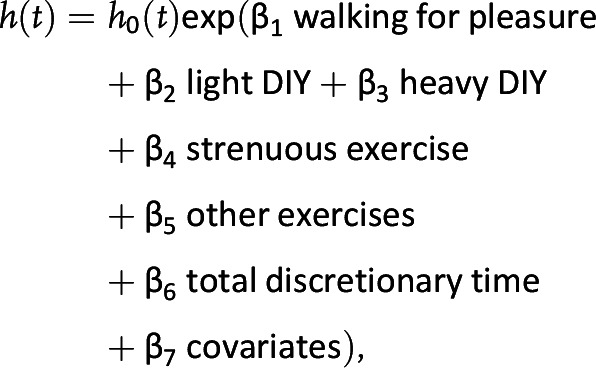 |
where the total discretionary time = sedentary behavior time + total physical activity time. By virtue of eliminating the sedentary behavior time, the coefficient (β1) represents the effect of substituting 30 min/day sedentary behavior with 30 min/day walking for pleasure, the coefficient (β2) represents the effect of substituting 30 min/day sedentary behavior with 30 min/day light DIY, and so on (30).
For investigation of whether the association between the sedentary behavior time and T2D incidence was modified by the genetic predisposition to T2D, an interaction term between sedentary behavior time and T2D GRS was included in the above model. Furthermore, we also tested the potential modification by age or sex.
In the sensitivity analysis, to avoid reverse causation, we excluded the participant who developed T2D within the 2 years of follow-up. Statistical analyses were performed with SAS, version 9.4 (SAS Institute, Cary, NC). All P values were two sided, and P < 0.05 was considered statistically significant.
Results
Among the 475,502 study participants, a total of 18,695 incident T2D cases were documented during a median follow-up of 11 years. Baseline characteristics of the participants according to the categories of sedentary behavior time are presented in Table 1. Participants with excessive sedentary behavior time were older and had higher BMI, higher blood pressure, and less physical activity. They were also more likely to be male and previous or current smokers.
Table 1.
Baseline characteristics of UK Biobank participants according to hours of sedentary behavior (N = 475,502)
| Sedentary behavior, h/day | ||||
|---|---|---|---|---|
| <2 | 2–3 | 4–5 | ≥6 | |
| n | 37,855 | 140,604 | 165,409 | 131,634 |
| Age, years | 55.2 (8.1) | 55.9 (8.1) | 57.1 (8.0) | 56.9 (8.0) |
| Men | 12,544 (33.1) | 51,326 (36.5) | 74,179 (44.9) | 75,646 (57.5) |
| BMI, kg/m2 | 25.4 (4.3) | 26.3 (4.3) | 27.4 (4.5) | 28.6 (4.9) |
| SBP, mmHg | 133.8 (19.0) | 136.5 (18.8) | 138.5 (18.6) | 139.1 (18.3) |
| DBP, mmHg | 80.1 (10.3) | 81.4 (10.1) | 82.4 (10.0) | 83.4 (10.1) |
| Townsend deprivation index | −1.0 (3.2) | −1.5 (3.0) | −1.6 (3.0) | −1.1 (3.2) |
| METs | 2,729.9 (2,612.2) | 2,729.1 (2,652.9) | 2,706.6 (2,744.5) | 2,535.7 (2,765.2) |
| Healthy diet score | 2.2 (0.9) | 2.2 (0.9) | 2.1 (0.9) | 2.0 (0.9) |
| Sedentary time | ||||
| TV time, h/day | 0.4 (0.5) | 1.8 (0.9) | 2.9 (1.1) | 4.0 (1.7) |
| PC time, h/day | 0.2 (0.4) | 0.4 (0.6) | 0.8 (0.9) | 2.0 (1.9) |
| Driving time, h/day | 0.1 (0.3) | 0.3 (0.6) | 0.7 (0.8) | 1.5 (1.6) |
| Daily-life activities, min/day | 15.0 [32.0] | 15.0 [31.9] | 15.0 [32.1] | 11.3 [28.1] |
| Walking for pleasure, min/day | 6.3 [14.2] | 6.3 [14.3] | 6.0 [15.0] | 3.8 [15.0] |
| Light DIY, min/day | 0.7 [7.7] | 0.8 [7.7] | 0.0 [7.7] | 0.0 [6.0] |
| Heavy DIY, min/day | 0.0 [3.8] | 0.0 [3.8] | 0.0 [3.8] | 0.0 [3.5] |
| Structured exercise, min/day | 3.1 [15.0] | 1.9 [15.0] | 0.0 [14.0] | 0.0 [10.0] |
| Strenuous sports, min/day | 0.0 [0.0] | 0.0 [0.0] | 0.0 [0.0] | 0.0 [0.0] |
| Other exercises, min/day | 1.9 [15.0] | 1.5 [14.0] | 0.0 [10.0] | 0.0 [7.7] |
| Total physical activity, min/day | 27.0 [44.1] | 26.3 [43.3] | 24.5 [43.3] | 18.8 [39.0] |
| Smoking | ||||
| Never | 23,545 (62.4) | 83,495 (59.6) | 90,142 (54.7) | 64,085 (48.9) |
| Previous | 10,938 (29.0) | 44,627 (31.8) | 58,077 (35.2) | 49,592 (37.8) |
| Current | 3,234 (8.6) | 12,050 (8.6) | 16,649 (10.1) | 17,469 (13.3) |
| Alcohol intake | ||||
| Daily or almost daily | 8,049 (21.3) | 29,655 (21.1) | 34,198 (20.7) | 26,455 (20.1) |
| 3–4 times/week | 8,910 (23.6) | 34,579 (24.6) | 39,291 (23.8) | 28,844 (21.9) |
| 1–2 times/week | 8,743 (23.1) | 35,733 (25.4) | 43,854 (26.5) | 34,739 (26.4) |
| 1–3 times/month | 3,910 (10.4) | 15,353 (10.9) | 18,490 (11.2) | 15,036 (11.4) |
| Special occasions only | 4,352 (11.5) | 14,798 (10.5) | 18,017 (10.9) | 15,986 (12.2) |
| Never | 3,827 (10.1) | 10,392 (7.4) | 11,467 (6.9) | 10,464 (8.0) |
| Household income | ||||
| <£18,000 | 5,936 (15.7) | 21,938 (15.6) | 31,656 (19.1) | 29,928 (22.7) |
| £18,000–£30,999 | 6,722 (17.8) | 29,278 (20.8) | 36,877 (22.3) | 29,966 (22.8) |
| £31,000–£51,999 | 8,031 (21.2) | 32,676 (23.2) | 37,689 (22.8) | 28,735 (21.8) |
| £52,000–£100,000 | 7,966 (21.0) | 28,218 (20.1) | 28,124 (17.0) | 20,148 (15.3) |
| >£100,000 | 3,324 (8.8) | 8,204 (5.8) | 6,687 (4.0) | 4,358 (3.3) |
| Hypertension | 14,871 (39.3) | 64,402 (45.8) | 86,341 (52.2) | 73,810 (56.1) |
| Antihypertension medications | 4,952 (13.2) | 22,243 (15.9) | 33,378 (20.3) | 31,267 (24.0) |
| Cholesterol-lowering medications | 3,664 (9.8) | 16,825 (12.0) | 27,222 (16.6) | 26,359 (20.2) |
Data are mean (SD), median [interquartile range], or N (%). DBP, diastolic blood pressure; PC, personal computer; SBP, systolic blood pressure.
We found a linear dose-responsive relationship between sedentary behavior time and the risk of T2D, with no threshold effect (Supplementary Fig. 1 [Plinearity < 0.0001]). More sedentary behavior time of participants was consistently associated with a higher risk of T2D across the models (Table 2). Each SD (1 SD = 2.4 h) increase in sedentary behavior time was associated with a T2D HR of 1.18 (95% CI 1.16, 1.19) after adjustment for age, race, sex, assessment center, Townsend deprivation index, smoking status, alcohol intake, education, average household income, healthy diet score, hypertension, total METs, cholesterol-lowering medications, antihypertensive medications, the first 10 genetic principal components, and T2D GRS. In comparisons with participants in the lowest category (<2 h/day), the HRs of T2D were 1.09 (95% CI 1.01, 1.18) for 2–3 h/day, 1.29 (1.19, 1.39) for 4–5 h/day, and 1.58 (1.47, 1.71) for ≥6 h/day, respectively (Table 2 [model 2, Ptrend < 0.001]). Further adjustment for BMI attenuated the HRs to 1.03 (0.95, 1.12), 1.11 (1.03, 1.20), and 1.20 (1.11, 1.29) (data not shown). A similar association of sedentary behavior time with the risk of T2D was observed after exclusion of participants who developed T2D within the first 2 years of follow-up (Supplementary Table 2).
Table 2.
HRs of T2D incidence according to categories of hours of sedentary behavior in the UK Biobank
| Sedentary time (h/day) | n cases/n total | Model 1 | Model 2 | ||
|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | ||
| <2 | 908/37,855 | 1 (reference) | 1 (reference) | ||
| 2–3 | 3,749/140,604 | 1.08 (1.01, 1.17) | 0.02 | 1.09 (1.01, 1.18) | 0.02 |
| 4–5 | 6,374/165,409 | 1.46 (1.36, 1.56) | <0.001 | 1.29 (1.19, 1.39) | <0.001 |
| ≥6 | 7,664/131,634 | 2.08 (1.94, 2.23) | <0.001 | 1.58 (1.47, 1.71) | <0.001 |
| Per SD increase | 1.31 (1.30, 1.33) | <0.001 | 1.18 (1.16, 1.19) | <0.001 | |
| P trend | <0.001 | <0.001 | |||
1 SD of sedentary behavior time = 2.4 h/day. Model 1: adjustment for age, race, sex. Model 2: model 1 adjustments plus smoking status, alcohol intake, healthy diet score, education, average household income, total METs, Townsend deprivation index, assessment center, hypertension, cholesterol-lowering medication, antihypertensive medication, T2D GRS, and the first 10 genetic principal components.
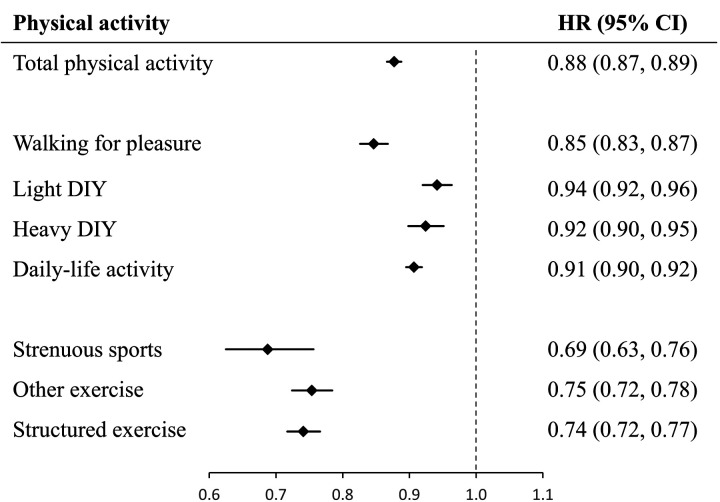
In the isotemporal substitution analyses, replacing 30 min/day sedentary behaviors with an equal amount of time of different types of activities was associated with significantly lower risks of T2D (Fig. 1). Replacing 30 min/day sedentary behaviors with an equal amount of time of daily-life activity and structured exercise was associated with 9% (HR 0.91 [95% CI 0.90, 0.92]) and 26% (0.74 [0.72, 0.77]) reductions of T2D risk, respectively. In assessment of the specific types of physical activity, the greatest risk reduction was found in modeling 30 min/day reallocations from sedentary behaviors into strenuous sports (0.69 [0.63, 0.76]). Even replacing 30 min/day sedentary behaviors with an equal amount of time of light DIY (such as pruning and watering the lawn) was associated with a 6% lower risk of T2D (0.94 [0.92, 0.96]). Further stratified analyses in women and men separately showed stronger benefits among women (Supplementary Fig. 2).
Figure 1.
HRs for T2D according to isotemporal substitution of 30 min/day sedentary time with equivalent durations of each different type of physical activity. Models have the sedentary behavior component omitted and are adjusted for total discretionary time, time of each type of physical activity, age, race, sex, smoking status, alcohol intake, education, average household income, healthy diet score, Townsend deprivation index, assessment center, hypertension, cholesterol-lowering medication, antihypertensive medication, T2D GRS, and the first 10 genetic principal components.
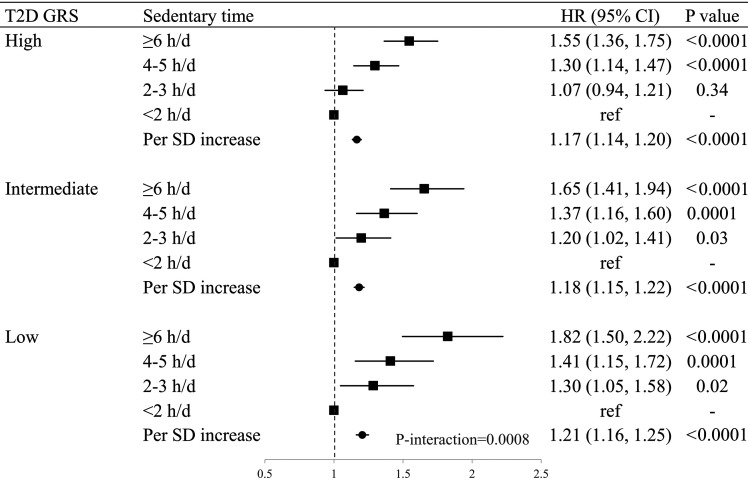
In addition, we found significant interactions between sedentary behavior time and genetic predisposition to T2D (Fig. 2 [Pinteraction = 0.0008]). For participants within the lowest tertile of T2D GRS, the HR for T2D was 1.21 (95% CI 1.16, 1.25) per SD (2.4 h/day) increase in the sedentary behavior time, while among those with the highest tertile of T2D GRS, the HR for T2D was 1.17 (1.14, 1.20) after adjustment for age, race, sex, assessment center, Townsend deprivation index, smoking, alcohol intake, total METs, education, average household income, healthy diet score, hypertension, cholesterol-lowering medications, antihypertensive medications, and the first 10 genetic principal components. We did not observe significant modification by age or sex (data not shown).
Figure 2.
Multivariate-adjusted HRs for T2D according to T2D GRS. Models were adjusted for age, race, sex, assessment center, Townsend deprivation index, smoking, alcohol intake, education, average household income, healthy diet score, hypertension, total METs, cholesterol-lowering medication, antihypertensive medication, and the first 10 genetic principal components, according to tertile categories of T2D GRS. h/d, hours per day.
In line with the observations of genetic modifications, we found that the benefit of replacing 30 min sedentary behavior per day with an equal amount of time of different types of activities was stronger among those with a lower genetic predisposition to T2D (Supplementary Table 3). For example, replacing 30 min sedentary behavior with an equal amount of time of walking for pleasure was associated with a 19% (95% CI 15, 24) risk reduction among participants with the lowest tertile of T2D-GRS, while among those with the highest tertile of T2D-GRS there was a 13% (95% CI 10, 16) risk reduction for the same type of replacement.
Conclusions
In this large prospective cohort of middle-aged participants, we found a positive linear dose-responsive association between sedentary behavior time and the risk of T2D, with no threshold effect. We found that replacing 30 min/day sedentary behavior with an amount of equal time of different types of physical activities was associated with a 6–31% lower risk of T2D, with strenuous sports showing the strongest benefit. In addition, we found that genetic predisposition to T2D significantly modified the above relationship; a stronger association was observed among those with lower T2D GRS.
Our findings extend the literature showing that sedentary behavior time is associated with an increased risk of T2D in a linear fashion (13–15) and add evidence regarding the newly released guidelines on reducing sedentary behavior (5,6). A previous cross-sectional study with objectively measured sedentary behavior showed that excessive sedentary behavior time was independently associated with higher fasting insulin, HOMA of insulin resistance, and prevalent diabetes (31). Results from a comparably large cohort among a Chinese population, the China Kadoorie Biobank (CKB), also showed a significant positive association between sedentary behavior time and T2D (10). However, an approximate log-linear relationship was reported between sedentary behavior time and T2D risk in CKB. Of note, in CKB, the sedentary behavior time was calculated based on time spend on TV watching, reading, or playing card games and did not include personal computer use time outside of work or driving time. Differences in the lifestyle between the developed and developing countries, as well as the source of the population, may also explain the disparity.
Interestingly, our isotemporal substitution analyses showed that replacing sedentary behaviors with both daily-life physical activities (including walking for pleasure, light DIY, and heavy DIY) and structured exercises (including strenuous sports and other exercises) could significantly reduce T2D risk, with light DIY showing the minimal (6%) and strenuous sports showing the maximal (31%) risk reduction. Most of the previous studies failed to reflect the competing nature of different activities within a fairly constant amount of leisure time (10,11,14). Indeed, the limited studies that used the substitutional analyses were cross-sectional, with small sample sizes and without considering different types of physical activities (7,8,32). It was previously reported that replacing sedentary time (accelerometer-measured) with moderate-to-vigorous physical activity was associated with lower diabetes risk among older women (33). In comparison with previous studies without consideration of the competing nature, evidence from the isotemporal substitution models provides more realistic estimates of the potential public health impact of behavioral changes, as it includes a finite amount of time in a day taken into account (17). The prior evidence was extremely limited regarding the beneficial effect of gardening and housework with regard to T2D risk reduction (34). Our results from a large cohort provide supporting evidence that replacing sedentary behavior even by light DIY, such as pruning, watering the lawn, gardening, and housework, could also significantly reduce the risk of T2D. Strenuous sports include sports that make people sweat or breathe hard, i.e., basketball, football, badminton, hiking, and folk dancing. Previous studies have also shown that moderate- to high-intensity physical activities were associated with protective effects for T2D (35). However, most of them used METs as a measure of physical activity, which is difficult for the general population to estimate and may hinder the application in daily life. Of note, using easily understood types of daily-life activities and structured exercises are likely to be more practicable and feasible alternatives for replacing sedentary behavior time among the general population compared with physical activities reflected by METs.
Multiple mechanisms may account for the benefits of replacing sedentary behavior time with different types of physical activities for T2D risk. It is well documented that sedentary behaviors are associated with obesity, dyslipidemia, and decreased insulin sensitivity, which may contribute to the development of T2D. On the other hand, previous studies have shown that increasing physical activity could reduce blood glucose by increasing GLUT-4–mediated uptake of glucose into muscle, reducing insulin resistance, and also stimulate fat oxidation and storage in muscle (36,37). Particularly, a recent study comprehensively meta-analyzed 37 controlled trials and showed that physical activity breaks in sitting time could lead to significant benefits in postprandial glucose and insulin metabolism (38), which are closely related to T2D. Furthermore, several other metabolic responses to physical activity may also explain the underlying mechanisms, including reduction of C-peptide, lipoproteins, adipose tissue gene expression, and molecular signaling that modulates glucose metabolism (38). Our findings suggest that substituting sedentary behavior with structured exercise might confer stronger effects in reducing T2D risk. Such observations are supported by prior evidence that high-intensity activities are in general related to greater improvement of cardiometabolic factors, such as adiposity and lipid, than low-intensity activities (39).
For the first time, we observed a significant interaction between sedentary behavior time and T2D GRS for the risk of T2D. The relationship between sedentary behavior time and the risk of T2D was weaker in those with higher T2D genetic risk than those with lower T2D genetic risk. This finding is in line with results from other studies such as the Atherosclerosis Risk in Communities (ARIC) study, in which the association between physical activity and risk of T2D was found to be weaker in those with higher T2D genetic risk (40). Taken together, we speculate that although both genetic risk and sedentary behavior are associated with increased risk of T2D, risk for individuals who are already at a higher genetic predisposition to T2D might be less affected by behavior changes. Our substitution analyses according to the genetic risk of T2D showed greater benefits of replacing sedentary behaviors with daily-life activities and structured exercise among those with a lower genetic predisposition to T2D, and such observations also supported our speculation. However, such results do not support that genetic effect is stronger and cannot be offset. As shown in Fig. 2 and Supplementary Table 3, although the magnitudes were slightly smaller, there were still substantial benefits among individuals with high genetic risks of T2D.
To the best of our knowledge, this is the first large prospective study to estimate the substitution effects of replacing sedentary behavior with an equal amount of time of different types of daily-life physical activity and structured exercises. The strengths of our study include the large sample size and prospective design. We also considered a wide range of potential confounders and performed the sensitivity analysis by excluding the T2D cases developed in the first 2 years of follow-up. More importantly, we not only applied the isotemporal substitution model, to address the practical question of how much benefit could be gained by replacing sedentary behavior with physical activities (16,17), but also quantified the beneficial effects of the domain-specific physical activities. We specifically focused on five easily understood types of physical activities in the leisure and home domain, which were more feasible and practical alternatives for the general population. We acknowledge that the current study has several potential limitations. First, sedentary behaviors and physical activity types were self-reported and information bias is inevitable. However, the misclassification is more likely to attenuate the association between sedentary behavior and T2D. The self-reported data may not capture the full waking period with use of the isotemporal substitution model. Second, no information was collected on sedentary bout duration or sedentary breaks. Third, a single time measurement for sedentary behavior and physical activity was used in the analysis, which did not include the changes in these behaviors during the follow-up. Fourth, the diagnosis of T2D may not be perfectly accurate, as it was based on self-report and hospital records and death registration, and there was a potential delay in the ascertainment of incident cases (23). Finally, we could not determine causality due to the observational nature of the current study.
In conclusion, our data indicate a positive linear relation between sedentary behavior time and the risk of T2D, with no threshold effect. We also provide novel evidence that replacing sedentary behaviors (i.e., 30 min/day) with short-duration daily-life physical activities or structured exercise is related to 6–31% risk reductions in T2D. In addition, we found that the positive association between sedentary behavior time and risk of T2D was stronger among those with a lower genetic risk of T2D. Substituting sedentary behavior with an equal amount of time of physical activities also showed the largest benefits among those with lower T2D genetic risk. Our results provide the general population a feasible and practical alternative for reduction of sedentary behavior time and lend further support to the newly released guidelines on reducing sedentary behavior time in the prevention of T2D.
Article Information
Acknowledgments. The authors appreciate the participants in UK Biobank for their participation and contribution to the research. This study was conducted using the UK Biobank resource under application no. 29256.
Funding. The study was supported by grants from the National Heart, Lung, and Blood Institute (HL071981, HL034594, HL126024), the National Institute of Diabetes and Digestive and Kidney Diseases (DK115679, DK091718, DK100383), the Fogarty International Center (TW010790), and by Tulane Research Centers of Excellence Awards. X.L. was the recipient of the American Heart Association Predoctoral Fellowship Award (19PRE34380036).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. X.L. and L.Q. conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. T.Z. contributed to statistical analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted. H.M., Z.L., V.A.F., and L.Q. critically reviewed the manuscript and approved the final manuscript as submitted. All authors approved the final manuscript and agreed to be accountable for all aspects of the work. L.Q. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 81st Scientific Sessions of the American Diabetes Association, 25–29 June 2021.
Footnotes
See accompanying article, p. 2194.
This article contains supplementary material online at https://doi.org/10.2337/figshare.14589438.
This article is featured in a podcast available at https://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1. Zimmet P, Alberti KG, Magliano DJ, Bennett PH. Diabetes mellitus statistics on prevalence and mortality: facts and fallacies. Nat Rev Endocrinol 2016;12:616–622 [DOI] [PubMed] [Google Scholar]
- 2. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health 2020;10:107–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr 2012;95:437–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang L, Cao C, Kantor ED, et al. Trends in sedentary behavior among the US population, 2001-2016. JAMA 2019;321:1587–1597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization . WHO guidelines on physical activity and sedentary behaviour. Geneva, World Health Organization, 2020. License: CC BY-NC-SA 3.0 IGO [PubMed] [Google Scholar]
- 6. Piercy KL, Troiano RP. Physical activity guidelines for Americans from the US Department of Health and Human Services. Circ Cardiovasc Qual Outcomes 2018;11:e005263. [DOI] [PubMed] [Google Scholar]
- 7. Henson J, Dunstan DW, Davies MJ, Yates T. Sedentary behaviour as a new behavioural target in the prevention and treatment of type 2 diabetes. Diabetes Metab Res Rev 2016;32(Suppl. 1):213–220 [DOI] [PubMed] [Google Scholar]
- 8. van der Berg JD, Stehouwer CDA, Bosma H, et al. Associations of total amount and patterns of sedentary behaviour with type 2 diabetes and the metabolic syndrome: The Maastricht Study. Diabetologia 2016;59:709–718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Duvivier BMFM, Schaper NC, Hesselink MKC, et al. Breaking sitting with light activities vs structured exercise: a randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia 2017;60:490–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bennett DA, Du H, Bragg F, et al.; China Kadoorie Biobank Study Collaborative Group . Physical activity, sedentary leisure-time and risk of incident type 2 diabetes: a prospective study of 512 000 Chinese adults. BMJ Open Diabetes Res Care 2019;7:e000835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA 2011;305:2448–2455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. de Rezende LFM, Rodrigues Lopes M, Rey-López JP, Matsudo VKR, Luiz OdoC. Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS One 2014;9:e105620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003;289:1785–1791 [DOI] [PubMed] [Google Scholar]
- 14. Ford ES, Schulze MB, Kröger J, Pischon T, Bergmann MM, Boeing H. Television watching and incident diabetes: findings from the European Prospective Investigation into Cancer and Nutrition-Potsdam Study. J Diabetes 2010;2:23–27 [DOI] [PubMed] [Google Scholar]
- 15. Hu FB, Leitzmann MF, Stampfer MJ, Colditz GA, Willett WC, Rimm EB. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med 2001;161:1542–1548 [DOI] [PubMed] [Google Scholar]
- 16. Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol 2009;170:519–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mekary RA, Ding EL. Isotemporal substitution as the gold standard model for physical activity epidemiology: why it is the most appropriate for activity time research. Int J Environ Res Public Health 2019;16:797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grgic J, Dumuid D, Bengoechea EG, et al. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: a systematic scoping review of isotemporal substitution studies. Int J Behav Nutr Phys Act 2018;15:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dietrich S, Jacobs S, Zheng J-S, Meidtner K, Schwingshackl L, Schulze MB. Gene-lifestyle interaction on risk of type 2 diabetes: a systematic review. Obes Rev 2019;20:1557–1571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Collins R. What makes UK Biobank special? Lancet 2012;379:1173–1174 [DOI] [PubMed] [Google Scholar]
- 21. Sudlow C, Gallacher J, Allen N, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 2015;12:e1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. World Health Organization . WHO Guidelines on Physical Activity and Sedentary Behaviour. Geneva, World Health Org., 2020, p. 104. [PubMed] [Google Scholar]
- 23. Eastwood SV, Mathur R, Atkinson M, et al. Algorithms for the capture and adjudication of prevalent and incident diabetes in UK Biobank. PLoS One 2016;11:e0162388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ma H, Li X, Zhou T, et al. Glucosamine use, inflammation, and genetic susceptibility, and incidence of type 2 diabetes: a prospective study in UK Biobank. Diabetes Care 2020;43:719–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wijndaele K, Brage S, Besson H, et al. Television viewing and incident cardiovascular disease: prospective associations and mediation analysis in the EPIC Norfolk Study. PLoS One 2011;6:e20058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bycroft C, Freeman C, Petkova D, et al. Genome-wide genetic data on ∼enome-wide Biobank participants. 20 July 2017 [preprint]. bioRxiv:166298 [Google Scholar]
- 27. Vetter C, Dashti HS, Lane JM, et al. Night shift work, genetic risk, and type 2 diabetes in the UK biobank. Diabetes Care 2018;41:762–769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Scott RA, Scott LJ, Mägi R, et al.; DIAbetes Genetics Replication And Meta-analysis (DIAGRAM) Consortium . An expanded genome-wide association study of type 2 diabetes in Europeans. Diabetes 2017;66:2888–2902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lloyd-Jones DM, Hong Y, Labarthe D, et al.; American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010;121:586–613 [DOI] [PubMed] [Google Scholar]
- 30. Mekary RA, Lucas M, Pan A, et al. Isotemporal substitution analysis for physical activity, television watching, and risk of depression. Am J Epidemiol 2013;178:474–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barone Gibbs B, Pettee Gabriel K, et al. Cross-sectional and longitudinal associations between objectively measured sedentary time and metabolic disease: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Diabetes Care 2015;38:1835–1843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Edwardson CL, Henson J, Bodicoat DH, et al. Associations of reallocating sitting time into standing or stepping with glucose, insulin and insulin sensitivity: a cross-sectional analysis of adults at risk of type 2 diabetes. BMJ Open 2017;7:e014267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bellettiere J, LaMonte MJ, Healy GN, et al. Sedentary behavior and diabetes risk among women over the age of 65 years: the OPACH Study. Diabetes Care 2021;44:563–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hamasaki H. Daily physical activity and type 2 diabetes: a review. World J Diabetes 2016;7:243–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Smith AD, Crippa A, Woodcock J, Brage S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia 2016;59:2527–2545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Richter EA, Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev 2013;93:993–1017 [DOI] [PubMed] [Google Scholar]
- 37. Duncan GE, Perri MG, Theriaque DW, Hutson AD, Eckel RH, Stacpoole PW. Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care 2003;26:557–562 [DOI] [PubMed] [Google Scholar]
- 38. Loh R, Stamatakis E, Folkerts D, Allgrove JE, Moir HJ. Effects of interrupting prolonged sitting with physical activity breaks on blood glucose, insulin and triacylglycerol measures: a systematic review and meta-analysis. Sports Med 2020;50:295–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Healy GN, Winkler EAH, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J 2015;36:2643–2649 [DOI] [PubMed] [Google Scholar]
- 40. Klimentidis YC, Chen Z, Arora A, Hsu C-H. Association of physical activity with lower type 2 diabetes incidence is weaker among individuals at high genetic risk. Diabetologia 2014;57:2530–2534 [DOI] [PMC free article] [PubMed] [Google Scholar]