Abstract
Objective:
To evaluate short-term postorthodontic tooth movement without retention.
Materials and Methods:
Thirty consenting patients participated in the study. At the end of active treatment (T1), final archwires were removed while leaving the fixed appliances on, and alginate impressions were taken. Four weeks later (T2) a second set of impressions was taken. A clinical examination performed at T2 determined if the fixed appliances could be removed or if additional treatment was required. Based on the examination, patients were divided into two groups. Patients in group I (n = 13) had their fixed appliances removed, while those in group II (n = 17) required additional treatment. The American Board of Orthodontics' Objective Grading System scores and the following six variables were measured on plaster casts at T1 and T2: maxillary and mandibular crowding or spacing, overbite, overjet, and mandibular intercanine and intermolar widths. Data were analyzed to detect potential changes from T1 to T2 and to evaluate differences between the groups.
Results:
Mandibular crowding, overjet, and interproximal contacts worsened for the entire sample, while marginal ridges, occlusal contacts, and total American Board of Orthodontics scores improved. No statistically significant changes were found within group I from T1 to T2. Mandibular crowding, overbite, overjet, alignment/rotations, and interproximal contacts worsened within group II from T1 to T2, while marginal ridges and occlusal contacts improved. Significant differences were noted between the groups in terms of alignment/rotations, interproximal contacts, and mandibular intercanine width.
Conclusion:
Short-term postorthodontic tooth movement without retainers demonstrated improvement in specific characteristics of the occlusion but negatively affected alignment and interproximal contacts in the sample.
Keywords: Stability, Retention, Relapse
INTRODUCTION
Detrimental postorthodontic tooth movement has challenged orthodontists from time immemorial. In an attempt to prevent such dental changes, orthodontists have developed different philosophies, strategies, and appliances. However, most of these are based on clinical experience that has led to strong convictions rather than compelling scientific evidence. In a recent study1 it was found that fixed retention strategies are gaining in popularity, and no clinician was found to not retain cases. While the first reference to orthodontic treatment was made as early as the beginning of the first millennium by Celsus (25 bc–ad 50), a Roman writer,2 the use of a retention device was not addressed until the early 1800s, when J.M. Alexis Schange outlined the need for a period of stabilization after treatment and used “a rubber band attached to some hooks on the appliance surrounding the molars” as a retention device.2
Since the early days of our specialty, clinicians have agreed on the need for retention, but they have had different opinions regarding the appliances and protocols; Weinberger2 believed a single night was sufficient, and Kingsley3 recommended 3 to 4 months. Hawley4 clearly expressed this nearly 100 years ago when he stated that the mistake had been to apply a “guessed-at” solution to the unsolved and undetermined problem of the instability of treated malocclusions.
In an attempt to understand the causes of relapse, four main schools of thought emerged, beginning in the late 1880s. For Kingsley,3 “the occlusion of the teeth was the most potent factor in determining the stability in a new position.” In 1922, Rogers5 proposed that establishing proper muscle balance was critical in maintaining the corrected malocclusion. Lundstrom6 formed a third school of thought that considered the apical base to be the key to long-term stability, and Tweed7 introduced the theory advocating that mandibular incisors must be upright over the basal bone for optimal stability and esthetics.
During the last century, many factors, such as treatment modalities,8–10 preservation of original mandibular intercanine width,11,12 continued growth,13,14 influence of gingival tissues,15,16 and role of third molars,17,18 were investigated as contributors to relapse. A few studies have attempted to compare different retainers and protocols, ranging from minimal retention19 to permanent retention.20 However, our understanding of this complex and critical area remains poor. The lack of compelling scientific evidence has both allowed and forced clinicians to base their retention appliances and protocols on cost, ease of fabrication, and personal preference.
In attempting to understand postorthodontic tooth movement, as a starting point it would be useful to find out if all patients should indeed be retained, or if a subgroup of patients exists who can benefit from the absence of retention. An extensive review of the literature did not reveal a study that has attempted to answer this fundamental question. The purpose of this descriptive pilot study was to investigate short-term postorthodontic changes in the absence of retention.
MATERIALS AND METHODS
All patients treated with fixed edgewise appliances in the “core” orthodontic clinic who were nearing the end of their orthodontic treatment at an established graduate orthodontic department located in the Midwest were requested to participate in the study. The “core” orthodontic graduate clinic consists of patients who are in the permanent dentition, under the age of 18 years, and are not in need of additional specialty services. Patients are treated by graduate students under the direct supervision of the orthodontic faculty. The recruitment of participants lasted for 6 months. Out of 56 potential participants, 36 individuals consented to participate. Four patients, eager to have their braces removed, withdrew from the study, and two were still in active treatment when data collection for this stage of the study ended. The final sample consisted of 30 patients. The procedures and protocol were approved by the institutional review board at the university.
When the end of treatment (T1) was approved by the faculty member overseeing the case, final archwires were removed and a set of alginate impressions was taken. Four weeks later (T2), a second set of alginate impressions was taken. The patient's occlusion was then compared to the set of models taken 4 weeks earlier (at T1). In the absence of undesirable changes, braces were removed and retainers delivered. If undesirable changes were detected by the supervising orthodontic faculty member, additional treatment was rendered. The faculty member's decision was purely based on his/her clinical assessment. Thus, two groups were formed based on the results of the clinical examination performed at T2. Group I consisted of the 13 individuals who had their braces removed at the recall appointment, and group II consisted of 17 individuals who required additional treatment.
Measurements
All data were collected by a single operator. The following six measurements were made with a digital caliper to the nearest hundredth of a millimeter on plaster models at pretreatment (T0), T1 (post–active treatment), and T2 (4-week recall): Maxillary crowding: the difference between space available (from first molar to first molar) and space necessary (sum of the mesio-distal dimension of each tooth anterior to the first molar); Mandibular crowding: the difference between space available (from first molar to first molar) and space necessary (sum of the mesio-distal dimension of each tooth anterior to the first molar); Overbite: the vertical overlap of maxillary and mandibular incisors; Overjet: distance from the facial surface of the mandibular central incisors to the facial surface of the maxillary central incisors; Mandibular intercanine width: distance between cusp tips; and Mandibular intermolar width: distance between the mesio-buccal cusp tips.
In addition, the American Board of Orthodontics' Objective Grading System21 (ABO-OGS) was used to score the plaster models both at T1 and T2 in order to detect potential changes in the posterior occlusion. In an effort to minimize examiner bias, casts were numbered 1 through 60 at random, and the examiner was unaware of the grouping of individual casts. Using a table of random numbers, they were randomly selected for scoring with the gauge provided by the ABO. A change of either 0.5 mm or 1 point over 4 weeks for the continuous and categorical data, respectively, was deemed clinically significant. There were no statistical differences between the measurements done initially and the ones made at least 2 weeks later on the 10 randomly selected casts; thus, intraoperator reliability was established.
Data Analyses
Data from the plaster casts were entered into the statistical program Minitab®, Release 14 (Minitab Inc, State College, Penn). In order to detect potential changes between T1 and T2, for the two groups paired t-tests and Wilcoxon signed rank tests were performed on the six continuous variables and the ABO scores (ordinal data), respectively. To test for differences between the groups, independent sample t-tests and Wilcoxon rank sum tests were used for the continuous and categorical data, respectively. Intraexaminer reliability was determined by computing t-tests as well as Wilcoxon signed rank tests with the data from 10 randomly selected casts 2 weeks after the first round of data collection. The level of significance, alpha, for all of the inferential statistical tests was set at ≤.05.
RESULTS
The final sample consisted of 14 males and 16 females, with an average age of 15.2 and 16.4 years, respectively. Twenty of the participants were white, five were African-Americans, three were Hispanic, and two belonged to other ethnic backgrounds. Six individuals had extractions, and five had a rapid palatal expander prior to fixed treatment.
Subjective clinical exams performed at the recall appointment revealed that 13 patients showed no change or an improvement in their occlusion after 4 weeks without archwires. Their appliances were therefore removed during the follow-up appointment. Seventeen patients required additional treatment, and maxillary, mandibular, or maxillary and mandibular archwires were reinserted for an average of 62 days. One patient received a mandibular spring aligner, and another was given a custom-made positioner.
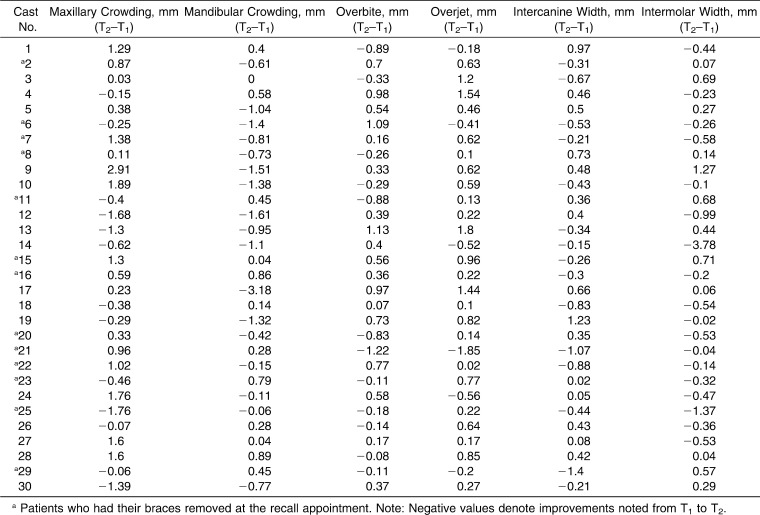
Table 1 outlines the changes in the six continuous variables between the time the archwires were removed and the recall visit (4 weeks later) for all subjects. Across the entire sample, mandibular crowding (0.4 ± 0.8; P = .03) and overjet (0.4 ± 0.7; P = .01) were found to be statistically significant. No significant changes were observed in mandibular intercanine width, mandibular intermolar width, maxillary crowding, or overbite.
Table 1.
Changes in Values for Continuous Variables from the End of Active Treatment (T1) to 4 Weeks Later (T2)
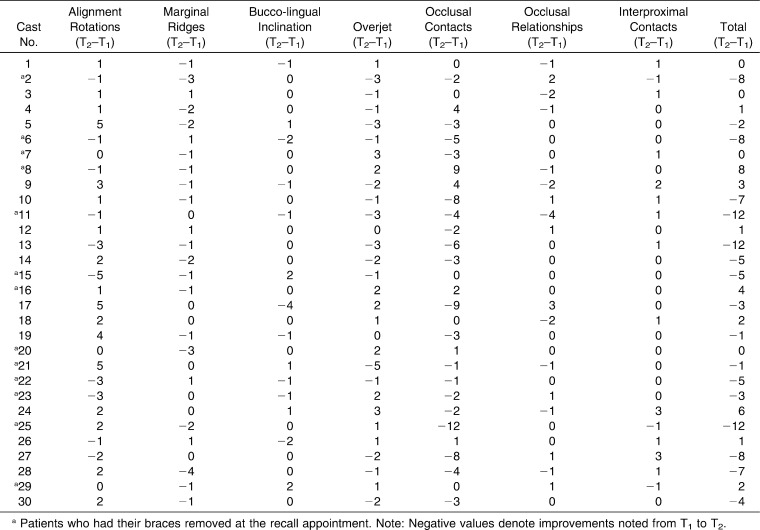
Table 2 shows the changes in ABO scores between the time the archwires were removed (T1) and the recall visit 4 weeks later (T2) for all subjects. Marginal ridges, occlusal contacts, interproximal contacts, and the total scores were statistically significant (P < .05).
Table 2.
Change in American Board of Orthodontics (ABO) Scores from the End of Active Treatment (T1) to 4 Weeks Later (T2)
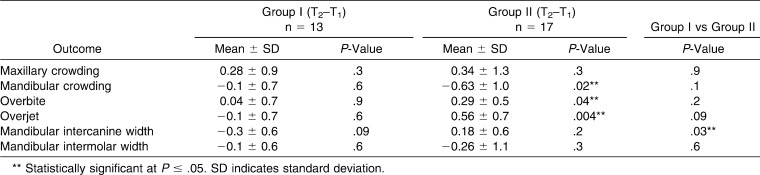
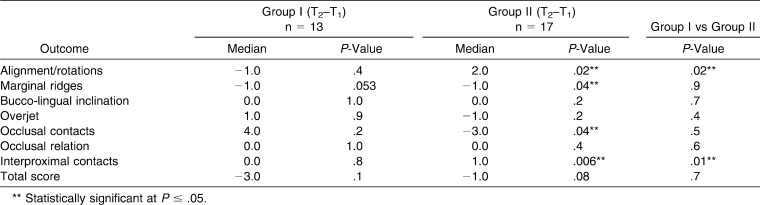
Tables 3 and 4 illustrate the results for the two subgroups. There was no change within group II from T1 to T2, as seen in Table 3. Within group II, mandibular crowding, overbite, overjet, alignment/rotations, and interproximal contacts all showed a significant worsening during the observation period, while marginal ridges and occlusal contacts showed a significant improvement. Differences between the changes for the two groups show significant differences in intercanine width, alignment/rotations, and interproximal contacts.
Table 3.
Mean Differences in Continuous Outcome Variables Within and Between the Two Groups (end of active treatment [T1] to 4 weeks later [T2])
Table 4.
Median Differences in Median American Board of Orthodontics (ABO) Scores Within and Between the Two Groups (end of active treatment [T1] to 4 weeks later [T2])
DISCUSSION
To the best of our knowledge, this appears to be the first study related to postorthodontic tooth movement following active orthodontic treatment without retention; therefore, it is difficult to make comparisons to other studies. The results of this exploratory pilot study raise several important considerations.
Relapse indicates a return to a previous, usually undesirable state. From our preliminary study it is evident that several changes that occur following orthodontic treatment (in the absence of retention) are not undesirable but are in fact welcome and desirable changes. It is interesting to note that seven out of the eight categorical variables (the ABO Index) showed substantial overall improvement in the short run. Marginal ridges and bucco-lingual inclination scores exhibited stability and/or improvement. Additionally, every patient exhibited some change in at least one variable, reminding us that the human dentition is a dynamic entity.
Among the continuous variables, only mandibular crowding and overjet showed a statistically significant change over 4 weeks, a finding that concurs with the literature.22,23 The increases in mandibular crowding and overjet, while statistically significant, were small. Such differences can, however, be clinically relevant. It is important to note that the use of mean values masks the important distinction between recurrence of crowding and reopening of spaces. Indeed, the range revealed clinically significant changes, from −3.18 mm to 0.9 mm, indicating that some patients experienced greater deleterious tooth movement than others over the course of the observation period. Surprisingly, mandibular intercanine width showed the least amount of change in the entire sample, which contradicts the results of most studies11,12 that evaluated the stability of the mandibular canine dimension and concluded that a significant decrease was to be expected regardless of treatment modality. It is likely that the 4-week observation interval was too short to allow for significant changes in the intercanine dimension to be observed. Yet the finding was surprising, as no known attempt was made to maintain the pretreatment mandibular intercanine width in any of the 30 subjects.
The analyses of the ABO-OSG scores showed statistically significant changes in alignment/rotations, marginal ridges, occlusal contacts, and interproximal contacts. An expert orthodontist will agree that forces of mastication help achieve better interdigitation. Similarly, spacing present at the start of treatment typically has a strong tendency to recur: hence, the increase in the interproximal contacts scores. It is valuable to validate these clinical observations by the experts in our field as we confront the challenge of understanding a complex and critical area of orthodontics.
Contradicting the results of the analyses of the continuous data, the ABO-OSG revealed no significant changes in overjet scores. A possible explanation may be that the changes over a 4-week interval were too small to be detected by the categorical scale adopted in the ABO-OSG, leading one to believe that the actual change from T1 to T2 may have been underestimated by this index. No significant change was noted for any variable within group I from T1 to T2, which supports the clinical decision to remove braces at the recall appointment in these 13 individuals. Further supporting the treatment decision that was made at T2, seven significant differences were found within group II. Both mandibular crowding and the alignment/rotations component of the ABO-OSG indicated significant deleterious changes. The interproximal contacts score increased, showing a reappearance of spaces. These findings are consistent with those of previous studies.9,10 The combined worsening of lower arch crowding and interproximal contacts provides a possible explanation for the fourth and fifth significant differences within group II, namely, the increase in overbite and overjet from T1 to T2. The ABO scores for marginal ridges and occlusal contacts showed significant improvement over the course of 4 weeks, demonstrating that masticatory forces have a positive influence, if only on the posterior dentition, with regard to interdigitation.
Perhaps most noteworthy was that the only significant differences between the two groups are the changes in alignment/rotations, interproximal contacts, and intercanine width. As most orthodontists do not measure intercanine width intraorally, the comprehensive clinical examination performed at the recall appointment likely focused on the alignment of the incisors in deciding whether additional treatment was necessary.
As with any study, let alone a study dealing with complex, multifactorial causes, there are limitations to be acknowledged. No attempt was made to stratify our sample based on initial findings. An attempt to consider admittedly important variables such as pretreatment crowding, type of malocclusion, extraction vs nonextraction, expansion vs no expansion, different bracket designs, use of elastics, duration of treatment, wires used, patient compliance, etc, would have involved a substantially larger sample, raising questions about the very ethics of conducting such a study without pilot data from a smaller sample.
The aim of this descriptive study was to understand changes that occur in the absence of retention over a short period of time. We hope the results of this study assist in future hypothesis-driven, analytical studies. This study does, however, underscore several positive developments that occur immediately following treatment, and it indicates that there exists a subgroup of patients who require less aggressive retention strategies. In other words, adopting identical retention strategies for all patients result in unnecessary treatment for some.
CONCLUSIONS
The results of the study support the practice of removing the archwires from the posterior teeth a few weeks prior to removing archwires from the anterior teeth.
Beneficial postorthodontic tooth movement occurs in the absence of retention, immediately following completion of active treatment. Across the sample, posttreatment improvements occurred in the occlusion, but negative changes were noted in dental alignment.
A good proportion of the participants did not suffer any negative changes during the observation period.
REFERENCES
- 1.Valiathan M, Hughes E. A study of the most common retention protocols prescribed in the United States. Am J Orthod Dentofacial Orthop. 2010;137:170–177. doi: 10.1016/j.ajodo.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 2.Weinberger B. W. Orthodontics A Historical Review of its Origin and Evolution. St Louis, Mo: The CV Mosby Company; 1926. Vols. 1–2. [Google Scholar]
- 3.Kingsley N. Treatise on Oral Deformities. New York, NY: Appleton and Company; 1880. pp. 64–65. [Google Scholar]
- 4.Hawley C. A. A removable retainer. Dental Cosmos. 1919;61:449. [Google Scholar]
- 5.Rogers A. P. Making facial muscles our allies in treatment of retention. Dental Cosmos. 1922;64:711–730. [Google Scholar]
- 6.Lundstrom A. Malocclusion of the teeth regarded as a problem in connection with the apical base. Int J Ortho Oral Surg. 1925;11:1022–1042. [Google Scholar]
- 7.Tweed C. Indications for the extraction of teeth in orthodontic procedure. Am J Orthod. 1944;30:405–428. [PubMed] [Google Scholar]
- 8.Glenn G, Sinclair P, Alexander R. Nonextraction orthodontic therapy: posttreatment dental and skeletal stability. Am J Orthod Dentofacial Orthop. 1987;92:321–328. doi: 10.1016/0889-5406(87)90333-7. [DOI] [PubMed] [Google Scholar]
- 9.Little R, Riedel R, Engst D. Serial extraction of first premolars—postretention evaluation of stability and relapse. Angle Orthod. 1990;60:255–262. doi: 10.1043/0003-3219(1990)060<0255:SEOFPP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Riedel R, Little R, Bui T. Mandibular incisor extraction—postretention evaluation of stability and relapse. Angle Orthod. 1992;62:103–116. doi: 10.1043/0003-3219(1992)062<0103:MIEPEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Burke S. P, Silveira A. M, Goldsmith L. J, Yancey J. M, Van Stewart A, Scarfe W. C. A meta-analysis of mandibular intercanine width in treatment and postretention. Angle Orthod. 1998;68:53–60. doi: 10.1043/0003-3219(1998)068<0053:AMAOMI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Housley J. A, Nanda R. S, Currier G. F, McCune D. E. Stability of transverse expansion in the mandibular arch. Am J Orthod Dentofacial Orthop. 2003;124:288–293. doi: 10.1016/s0889-5406(03)00450-5. [DOI] [PubMed] [Google Scholar]
- 13.Baum A. T. Age and sex differences in the dento-facial changes following orthodontic treatment and the significance in treatment planning. Am J Orthod. 1961;47:355–370. [Google Scholar]
- 14.Baum A. T. Orthodontic treatment and the maturing face. Angle Orthod. 1966;36:121–135. doi: 10.1043/0003-3219(1966)036<0121:OTATMF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Ahrens D, Shapira Y, Kuftinec M. An approach to rotational relapse. Am J Orthod. 1981;80:83–91. doi: 10.1016/0002-9416(81)90198-6. [DOI] [PubMed] [Google Scholar]
- 16.Edwards J. A long-term prospective evaluation of the circumferential supracrestal fiberotomy in alleviating orthodontic relapse. Am J Orthod Dentofacial Orthop. 1988;93:380–387. doi: 10.1016/0889-5406(88)90096-0. [DOI] [PubMed] [Google Scholar]
- 17.Ades A, Joondeph D, Little R, Chapko M. A long-term study of the relationship of third molars to changes in the mandibular dental arch. Am J Orthod Dentofacial Orthop. 1990;97:323–335. doi: 10.1016/0889-5406(90)70105-L. [DOI] [PubMed] [Google Scholar]
- 18.Harradine N, Pearson M, Toth B. The effect of extraction of third molars on late lower incisor crowding: a randomized controlled trial. Br J Orthod. 1998;25:117–122. doi: 10.1093/ortho/25.2.117. [DOI] [PubMed] [Google Scholar]
- 19.Strang R. H. W. Highlights of sixty-four years in orthodontics. Angle Orthod. 1974;44:101–112. doi: 10.1043/0003-3219(1974)044<0101:HOSYIO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Parker W. S. Retention—retainers may be forever. Am J Orthod. 1989;95:505–513. doi: 10.1016/0889-5406(89)90414-9. [DOI] [PubMed] [Google Scholar]
- 21.Casko J. S, Vaden J. L, Kokich V. G, et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am J Orthod Dentofacial Orthop. 1998;114:589–599. doi: 10.1016/s0889-5406(98)70179-9. [DOI] [PubMed] [Google Scholar]
- 22.Little R, Wallen T, Riedel R. Stability and relapse of mandibular anterior alignment—first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:349–365. doi: 10.1016/0002-9416(81)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.Little R, Riedel R, Årtun J. An evaluation of changes in the mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–428. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]