Abstract
Objective:
To compare the effects of extraction vs nonextraction orthodontic treatments on oropharyngeal airway volume.
Materials and Methods:
An existing patient database was screened for pretreatment (T0) and posttreatment (T1) cone beam computed tomography (CBCT) scans and complete medical histories. Twenty patients treated with removal of four premolars (ExtG) and 20 controls (NExtG), were matched for age, gender, ethnicity, height, weight, body mass index, and oropharyngeal (OP) volumes, among other variables. Constructed lateral cephalograms (three skeletal and four dental variables) and OP volumes were measured at T0 and T1 using Dolphin Imaging 11.0. Independent sample t-tests were used to compare the groups at T0 and the outcome variables at T1. Paired sample t-tests were used to compare the mean changes from T0 to T1. Statistical significance was set at P ≤ .05.
Results:
Changes from T0 to T1 were found to be significant in both groups for CoA, CoGn, U1-FH, and IMPA. In the ExtG alone, U1-Na Perp and L1-Na Perp were also significantly different from T0 to T1. Despite the observed differences, no significant differences were found at the end of treatment between the mean OP volumes for either group (12,675.6 ± 4483.6 for ExtG; 12,002.7 ± 2857.0 for NExtG, P > .05). Similarly, the mean changes in OP volume (1082.6 mm3 and 1701.1 mm3 for ExtG and NExtG, respectively) and increase in mean minimal constricted axial areas (17.4 mm2 and 1.9 mm2 for ExtG and NExtG, respectively, P > .05) from T0 to T1 were not significant for the two groups.
Conclusion:
Extraction of four premolars with retraction of incisors does not affect OP airway volume.
Keywords: Airway, Extraction, Outcomes, CBCT
INTRODUCTION
Traditional radiographic cephalometrics, magnetic resonance imaging (MRI), and computed tomography (CT) are widely used static imaging modalities for the assessment of airway anatomy and volume.1 The ability to perform precise measurements of various cross-sectional areas, three-dimensional (3D) reconstructions, and volumetric measurements of the upper airway are some of the advantages of CT technology when compared with cephalometric techniques. Following the introduction of cone beam CT (CBCT), the main disadvantages of conventional CT devices, such as high radiation dose and longer exposure times, were eliminated.2,3 Although MRIs operate without the need for ionizing radiation, an MRI requires significantly longer operating time that results in decreased airway image quality due to motion artifacts.4 In other words, CBCTs have led to a better understanding of upper airway anatomy and physiology.5
The upper airway has always been an area of interest because the oropharyngeal and nasopharyngeal structures play important roles in the growth and development of the craniofacial and orodental complex.6–8 Various DICOM (digital imaging and communications in medicine) viewer programs have enabled researchers to focus on the airway, specifically, airway volume. A variety of studies that evaluate the airway volume in symptomatic and nonsymptomatic patients have been published.9–14 Most of these studies focused on the possible associations between airway and skeletal structures, soft tissues, and musculature. However, the effects of orthodontic treatment, specifically the effects of four premolar extractions vs nonextraction treatment approaches on airway volume, have never been discussed in the literature. It is well documented that differences exist in the two treatment approaches when it comes to changes in the soft tissue profile, incisor angulations, vertical facial height, and mandibular plane angle, among other differences.15–19 It would be worthwhile therefore, to investigate the effects of extraction vs nonextraction care because an alteration of the incisor and soft tissue position could potentially affect tongue position and affect the upper airway volume, especially the oropharyngeal airway.
The aim of this retrospective, analytical study was to evaluate and compare the effects of extraction and nonextraction treatment modalities on the oropharyngeal airway volume. Specifically, the hypothesis tested was that the extraction of four premolars for orthodontic purposes would not affect the oropharyngeal airway volume compared to a matched, nonextraction group. Additionally, we attempted to determine if the location of minimal constricted axial area (minAx), relative to the occlusal plane, was affected at the end of treatment in both groups.
MATERIALS AND METHODS
The experimental protocol used in this study was approved by the institutional review board of an established university located in midwestern United States. All participants were obtained from the existing patient database of the Department of Orthodontics and were treated in the same facility using the Ortho II ViewPoint software (Ortho II Computers Systems, Ames, Iowa). All patients had pretreatment (T0) and posttreatment (T1) CBCT images and complete medical records were inspected for all patients. The age of patients used in this study ranged from 12.1 years to 15.5 years for boys and 11.3 years to 15.6 years for girls. The mean ages for ExtG were 13.8 ± 1.3 years for boys and 13.5 ± 1.6 years for girls. The mean ages for NExtG were 13.8 ± 1.2 years for boys and 13.5 ± 1.6 years for girls. Patients with medical histories of craniofacial deformities, pharyngeal pathology and/or nasal obstruction, snoring, obstructive sleep apnea, adenoidectomy, and tonsillectomy were excluded.
All of the CBCT images were acquired using a Hitachi CB MercuRay Scanner (Hitachi Medical Systems America Inc, Twinsburg, Ohio) and were taken as part of the routine initial diagnostic records for orthodontic patients. All images were taken at 2Ma, 120kV, and a 12-inch field of view (F mode) setting. Each patient's image data consisted of 512 slices, with a slice thickness of 0.377 mm, a resolution of 1024 × 1024 pixels, and 12 bits per pixel (4096 gray scale). The images were taken in natural head posture and in maximum intercuspation. Additionally, any CBCT scans in which the airway was not clear, not fully contained in the volume, or contained artifacts, were excluded.
From the selected records, 20 white patients treated with the removal of four premolars (ExtG; 10 female, 10 male), and 20 controls (NExtG), matched for age, gender, height, weight, body mass index (BMI), and skeletal features, were identified. The groups were matched one to one, and t-tests were performed at T0 to ensure the groups were not statistically different for the variables tested. All 40 participants had a Class I malocclusion, were treated with fixed edgewise appliances, and had good occlusion at the end of treatment.
The lateral cephalograms of the patients were obtained from the 3D CBCT data using the InVivoDental 4.0 software (Anatomage Inc, San Jose, Calif) and digitized using the Dolphin Imaging 11.0 software (Dolphin Imaging & Management Solutions, Chatsworth, Calif) for T0 and T1 time intervals. Cephalometric measurements consisted of three skeletal and four dental measurements and were completed by one experienced operator (Figure 1). All of the cephalometric data obtained from lateral cephalograms were organized using Microsoft Excel (Microsoft Corp, Redmond, Wash).
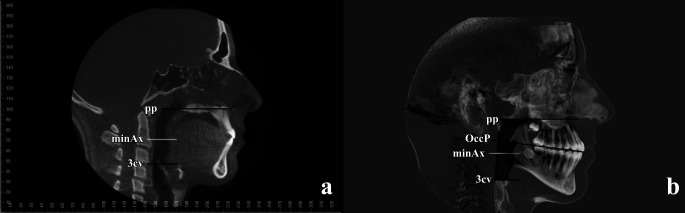
Figure 1.
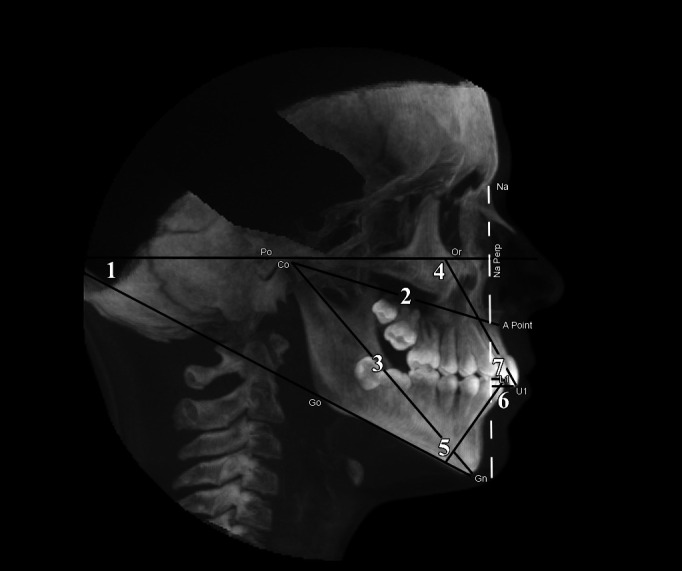
Cephalometric measurements. (1) FMA angle. (2) CoA (midface length). (3) CoGn (effective mandibular length). (4) U1-FH (upper incisor inclination). (5) IMPA (lower incisor inclination). (6) U1-Na Perp (upper incisor tip to a line drawn perpendicular to Frankfort horizontal from nasion). (7) L1-Na Perp (lower incisor tip to a line drawn perpendicular to Frankfort horizontal from nasion).
Volumetric measurements were performed separately for T0 and T1 time intervals using the 3D airway module of Dolphin Imaging 11.0 program following the recommendations of the manufacturer. The limits of the oropharyngeal (OP) volume were defined on the midsagittal slice, anteriorly by the incisive canal and the midline of the upper incisors.20 The superior border of the OP volume was defined by the palatal plane (ANS-PNS) line extending to the posterior wall of the pharynx, and the inferior border was defined by the line passing from the most inferoanterior point on the body of the third cervical vertebra and the base of the epiglottis (Figure 2). In addition to volumetric measurements, the surface area of the most constricted area between the previously mentioned limits was recorded in relation to the occlusal plane as above the occlusal plane (AOP), below the occlusal plane (BOP), or on the occlusal plane (OccP). The volumes and area data were also imported into Excel for comparisons.
Figure 2.
Two-dimensional (a) and three-dimensional (b) representations of superior and inferior borders of the OP airway. pp indicates line passing from ANS and PNS points extending to the posterior wall of the pharynx; minAx, minimal constricted axial area; 3cv, line passing from the most inferoanterior point on the body of the third cervical vertebra and the base of the epiglottis; OccP, occlusal plane.
Thirty randomly selected records were reevaluated after a week of preliminary data collection to estimate operator reliability. Intraclass correlation coefficients were calculated to estimate reliability for the volumetric measurements. The error for linear and angular measurements of cephalometric analysis was measured using the Dahlberg formula ( ).21 To validate the consistency of both groups at T0 in terms of age, height, weight, and BMI and to compare the outcome variables at the T1 time interval, independent sample t-tests were used. Paired sample t-tests were used to compare the mean changes from T0 to T1. Similarly, the mean difference in airway variables between T0 and T1 time intervals were compared for both groups. For all statistical analyses, SPSS Statistics 17.0 (SPSS Inc, Chicago, Ill) was used, and the statistical significance was set at ≤ .05.
).21 To validate the consistency of both groups at T0 in terms of age, height, weight, and BMI and to compare the outcome variables at the T1 time interval, independent sample t-tests were used. Paired sample t-tests were used to compare the mean changes from T0 to T1. Similarly, the mean difference in airway variables between T0 and T1 time intervals were compared for both groups. For all statistical analyses, SPSS Statistics 17.0 (SPSS Inc, Chicago, Ill) was used, and the statistical significance was set at ≤ .05.
RESULTS
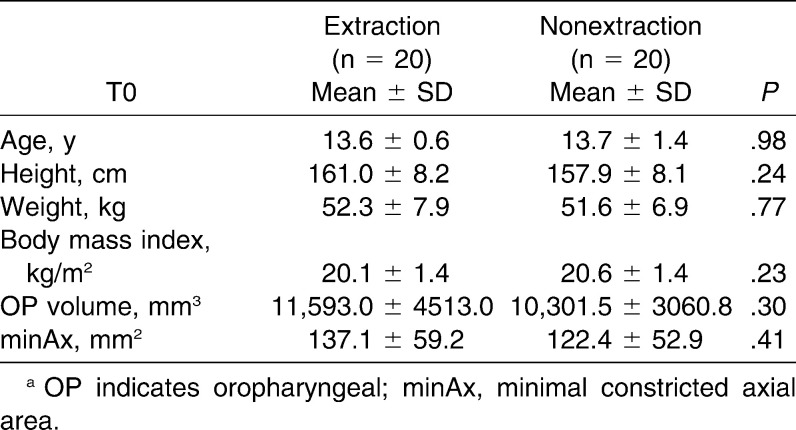
The differences in demographic and airway variables between the ExtG and NExtG at T0 are provided in Table 1. No statistical differences were noted at T0 when the two groups were compared (age, height, weight, and BMI). Although the mean OP volume (11,593.0 ± 4513.0 mm3) and minAx (137.1 ± 59.2) of ExtG at T0 were slightly larger than the nonextraction group (10,301.5 ± 3060.8 and 122.4 ± 52.9, respectively), there was no statistically significant difference.
Table 1.
Differences in Demographic and Airway Variables Between the Extraction and Nonextraction Groups at T0a
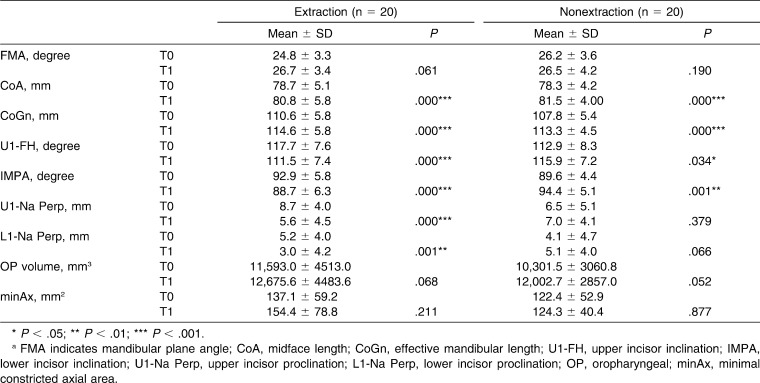
Differences in skeletal, dental, and airway variables at T0 and T1 among ExtG and NExtG are presented in Table 2. There was a significant increase in midface length and effective mandibular length for both groups. For the ExtG, U1-FH, and IMPA angles decreased significantly, whereas a significant increase was observed for the respective angles for the nonextraction group. The position of the upper and lower incisors for ExtG relative to Na-Perp decreased significantly. Although there was an increase in upper and lower incisor positions with respect to Na-Perp, the difference was not significant. The mean increases in OP volume, and the increases in mean minAx, were not statistically significant in either group.
Table 2.
Differences in Skeletal, Dental, and Airway Variables at T0 and T1 Between the Extraction and Nonextraction Groupsa
Table 3 shows differences in skeletal, dental, and airway variables between the ExtG and NExtG at T1. The treatment time for the extraction group was significantly longer than the time for the nonextraction group. The lower incisors were significantly more labially inclined at the end of treatment for the nonextraction group when compared with the extraction group. No statistically significant changes were observed for OP volume and minAx between the groups at the end of treatment.
Table 3.
Differences in Skeletal, Dental, and Airway Variables Between the Extraction and Nonextraction Groups at T1a
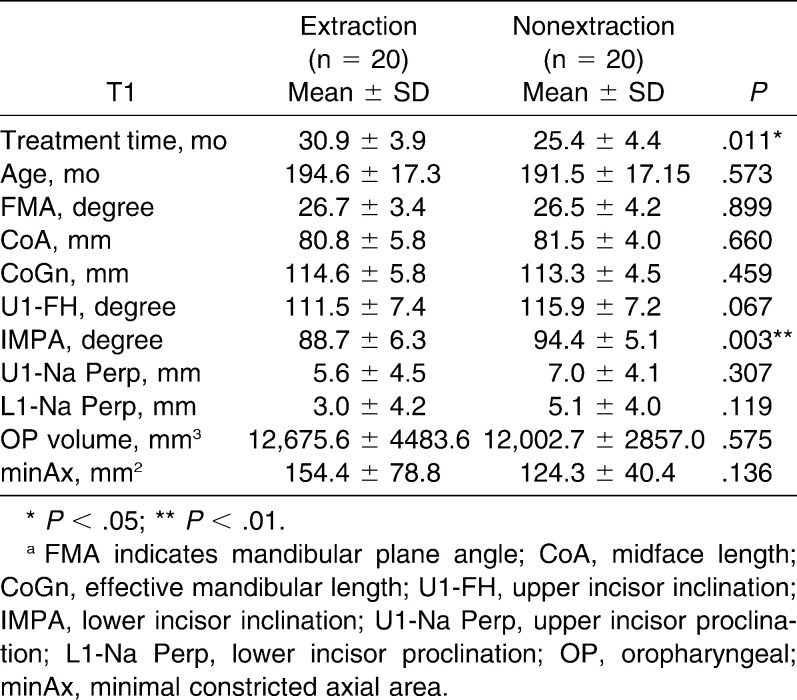
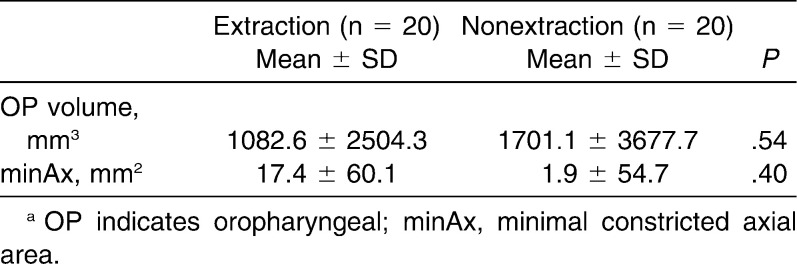
Mean differences for OP airway volume and minAx between T0 and T1 time intervals are given in Table 4. No statistically significant differences were observed for the mean differences between T0 and T1 for the two groups.
Table 4.
Mean Differences for OP Airway Volume and Minimal Constricted Axial Area Between T0 and T1 Time Intervalsa
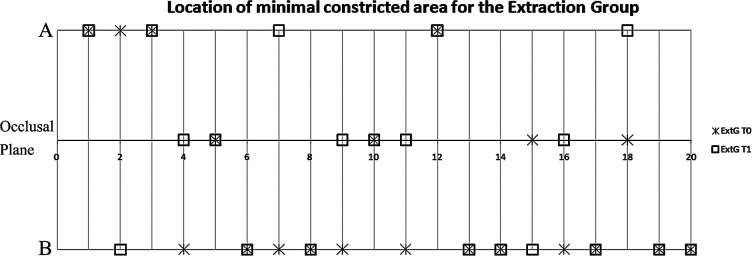
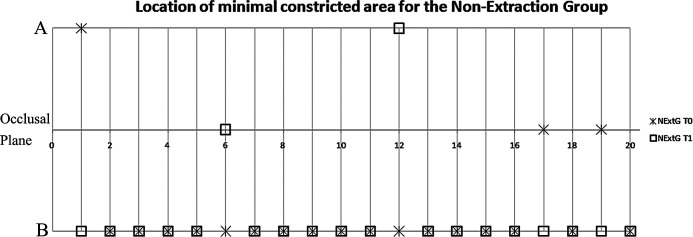
The location of the minAx at T0 for ExtG was AOP for 4 patients, BOP for 12 patients and at the OccP for 4 patients. In the ExtG, the minAx moved downwards for 2 patients, moved upwards for 6 patients, and stayed at the same level for 12 patients (Figure 3). The location of minAx at T0 for NExtG was AOP for 1 patient, BOP for 17 patients, and at the OccP for 2 patients. In the NExtG, the minAx moved downwards for 3 patients, moved upwards for 2 patients, and stayed at the same level for 15 patients (Figure 4).
Figure 3.
Location of the minimal constricted axial area for the extraction group at T0 and T1 time intervals.
Figure 4.
Location of the minimal constricted axial area for the nonextraction group at T0 and T1 time intervals.
DISCUSSION
The effects of extraction and nonextraction treatment modalities over the dentofacial complex have been researched intensively throughout the orthodontic literature. To the best of the authors' knowledge, the current study is the first study evaluating the effects of extraction and nonextraction treatments on OP airway volume.
In the current study, the images were acquired with the patient in an upright position (which is typical for most of the CBCT machines). It has been documented that the upper airway size and shape are prone to change depending upon the body position.22,23 While some may argue that this introduces a systematic error, studies have documented that images recorded in the upright position are adequate to evaluate the airway.24 Additionally, all images were taken under the same conditions and positions. Besides, this was not an obstructive sleep apnea study, but rather a study designed to evaluate the OP volumes for normal breathing adolescent patients.
A change in dimensions is expected in the pharyngeal soft tissue between the ages of 12 and 15 years.25 There was an increase in OP volume for both groups, but this increase was not significant. This observed difference when compared with 2D linear measurement studies is likely the result of our outcomes being recorded as volumes. However, a high variability for OP airway volume was observed for the evaluated patients in both groups, which was in concordance with the findings of Peters-Schuster et al.26 It should be noted that airway size and shape is extremely variable depending on the head posture and the breathing stage,23,27 and there are no norms or studies at this point to compare with our results.
In general, four premolar extraction treatments do not cause significant bony changes. In our sample there was a slight increase in mandibular plane angle for both of the groups (P = .061). Midface length (CoA) (P < .001) and effective mandibular length (CoGn) (P < .001) increased significantly, which was expected as a result of normal growth.28 The statistically nonsignificant increases in the OP airway volume also likely occurred as a result of normal growth process. There is a positive correlation between the OP airway and the length and position of the mandible.29,30 Therefore, to be more specific, most of the changes that occurred in the OP volume may be attributed to mandibular growth.
On the other hand, dental outcomes exhibited statistically significant differences for most of the measured variables between the groups. The only nonsignificant change was the position of the upper and lower incisors relative to the Na-Perp plane for the NExtG. All of the dental changes were in line with expectations in each of the groups. However, our hypothesis that a change in incisor angulation and position for patients who underwent extractions for orthodontic purposes would not cause a significant difference in the OP airway volume (secondary to a reduced size oral cavity and a change in tongue position) was not rejected. This could be the result of a type II error (false-negative caused by lack of sensitivity) and could be addressed, in part, by further increasing the sample size in future studies. The OP airway volumes of the NExtG displayed a slightly bigger but nonsignificant increase (P = .052). In fact, the mean difference in OP airway volume between the two groups was only 700 mm.3 It is interesting to note that the average volume of a standard-sized sugar cube is 5000 mm.3 In other words, the mean volume difference between the groups at T1 was approximately one seventh of the volume of a standard sugar cube. It is noteworthy that the total size of the mean OP airway volume was less than the volume of three sugar cubes.
One of the most common measurements used to evaluate the static morphology of the upper airway is to determine the area and location of a minimally constricted axial slice.12,31–33 The size and shape of this area are prone to change with positional changes of the mandible, tongue, or soft palate.34 The magnitude of these positional changes that are created with intraoral appliances cannot be compared to those obtained with extraction or nonextraction treatments. However, it was interesting to observe that the location of minAx was more prone to change for the ExtG. For both groups, there was an increase in minAx between T0 and T1. We speculate this increase occurred as a result of growth.
A major strength of our study is the groups were matched for age, gender, body mass index, height, weight, OP volume, and minimally constricted axial areas at T0. However, further investigations in this emerging area would be required to validate the observations and trends noted in this study.
CONCLUSION
No statistically significant OP airway volume changes were found between cases treated with the extraction of four premolars and nonextraction groups, despite expected changes in incisor angulations and position.
Acknowledgments
This study was partially funded by the Scientific and Technological Research Council of Turkey (TUBITAK) and the Alumni of the Orthodontic Department of Case Western Reserve University.
REFERENCES
- 1.Stuck B. A, Maurer J. T. Airway evaluation in obstructive sleep apnea. Sleep Med Rev. 2008;12:411–436. doi: 10.1016/j.smrv.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Kau C. H, Richmond S, Palomo J. M, Hans M. G. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 3.Halazonetis D. J. From 2-dimensional cephalograms to 3-dimensional computed tomography scans. Am J Orthod Dentofacial Orthop. 2005;127:627–637. doi: 10.1016/j.ajodo.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 4.De Backer J. W, Vos W. G, Verhulst S. L, De Backer W. Novel imaging techniques using computer methods for the evaluation of the upper airway in patients with sleep-disordered breathing: a comprehensive review. Sleep Med Rev. 2008;12:437–447. doi: 10.1016/j.smrv.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Osorio F, Perilla M, Doyle D. J, Palomo J. M. Cone beam computed tomography: an innovative tool for airway assessment. Anesth Analg. 2008;106:1803–1807. doi: 10.1213/ane.0b013e318172fd03. [DOI] [PubMed] [Google Scholar]
- 6.McNamara J. A., Jr Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981;51:269–300. doi: 10.1043/0003-3219(1981)051<0269:IORPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Solow B, Siersbaek-Nielsen S, Greve E. Airway adequacy, head posture, and craniofacial morphology. Am J Orthod. 1984;86:214–223. doi: 10.1016/0002-9416(84)90373-7. [DOI] [PubMed] [Google Scholar]
- 8.Tourne L. P. Growth of the pharynx and its physiologic implications. Am J Orthod Dentofacial Orthop. 1991;99:129–139. doi: 10.1016/0889-5406(91)70115-D. [DOI] [PubMed] [Google Scholar]
- 9.Ogawa T, Enciso R, Memon A, Mah J. K, Clark G. T. Evaluation of 3D airway imaging of obstructive sleep apnea with cone-beam computed tomography. Stud Health Technol Inform. 2005;111:365–368. [PubMed] [Google Scholar]
- 10.Kawamata A, Fujishita M, Ariji Y, Ariji E. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular setback osteotomy for prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:278–287. doi: 10.1016/s1079-2104(00)70089-8. [DOI] [PubMed] [Google Scholar]
- 11.Rachmiel A, Aizenbud D, Pillar G, Srouji S, Peled M. Bilateral mandibular distraction for patients with compromised airway analyzed by three-dimensional CT. Int J Oral Maxillofac Surg. 2005;34:9–18. doi: 10.1016/j.ijom.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa T, Enciso R, Shintaku W. H, Clark G. T. Evaluation of cross-section airway configuration of obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:102–108. doi: 10.1016/j.tripleo.2006.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tso H. H, Lee J. S, Huang J. C, Maki K, Hatcher D, Miller A. J. Evaluation of the human airway using cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:768–776. doi: 10.1016/j.tripleo.2009.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Aboudara C. A, Hatcher D, Nielsen I. L, Miller A. A three-dimensional evaluation of the upper airway in adolescents. Orthod Craniofac Res. 2003;6(suppl 1):173–175. doi: 10.1034/j.1600-0544.2003.253.x. [DOI] [PubMed] [Google Scholar]
- 15.Bravo L. A. Soft tissue facial profile changes after orthodontic treatment with four premolars extracted. Angle Orthod. 1994;64:31–42. doi: 10.1043/0003-3219(1994)064<0031:STFPCA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Ismail S. F, Moss J. P, Hennessy R. Three-dimensional assessment of the effects of extraction and nonextraction orthodontic treatment on the face. Am J Orthod Dentofacial Orthop. 2002;121:244–256. doi: 10.1067/mod.2002.121010. [DOI] [PubMed] [Google Scholar]
- 17.Kocadereli I. Changes in soft tissue profile after orthodontic treatment with and without extractions. Am J Orthod Dentofacial Orthop. 2002;122:67–72. doi: 10.1067/mod.2002.125235. [DOI] [PubMed] [Google Scholar]
- 18.Saldarriaga J. R. Protocol for the treatment of anterior open bite patients: an evaluation. World J Orthod. 2007;8:285–299. [PubMed] [Google Scholar]
- 19.Bishara S. E, Cummins D. M, Zaher A. R. Treatment and posttreatment changes in patients with Class II, Division 1 malocclusion after extraction and nonextraction treatment. Am J Orthod Dentofacial Orthop. 1997;111:18–27. doi: 10.1016/s0889-5406(97)70297-x. [DOI] [PubMed] [Google Scholar]
- 20.Shigeta Y, Ogawa T, Venturin J, Nguyen M, Clark G. T, Enciso R. Gender- and age-based differences in computerized tomographic measurements of the oropharynx. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:563–570. doi: 10.1016/j.tripleo.2008.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dahlberg G. Statistical Method for Medical and Biological Students. New York, NY: Interscience Publications; 1940. [Google Scholar]
- 22.Pevernagie D. A, Shepard J. W., Jr Effects of body position on upper airway size and shape in patients with obstructive sleep apnea. Acta Psychiatr Belg. 1994;94:101–103. [PubMed] [Google Scholar]
- 23.Yildirim N, Fitzpatrick M. F, Whyte K. F, Jalleh R, Wightman A. J, Douglas N. J. The effect of posture on upper airway dimensions in normal subjects and in patients with the sleep apnea/hypopnea syndrome. Am Rev Respir Dis. 1991;144:845–847. doi: 10.1164/ajrccm/144.4.845. [DOI] [PubMed] [Google Scholar]
- 24.Pracharktam N, Hans M. G, Strohl K. P, Redline S. Upright and supine cephalometric evaluation of obstructive sleep apnea syndrome and snoring subjects. Angle Orthod. 1994;64:63–73. doi: 10.1043/0003-3219(1994)064<0063:UASCEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Taylor M, Hans M. G, Strohl K. P, Nelson S, Broadbent B. H. Soft tissue growth of the oropharynx. Angle Orthod. 1996;66:393–400. doi: 10.1043/0003-3219(1996)066<0393:STGOTO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Peters-Schuster B. R, Hans M. G, Strohl K. P, Palomo J. M. A 3D Airway Assessment of 12–13 Year Old Subjects [master's thesis] Cleveland, Ohio: Case Western Reserve University; 2009. [Google Scholar]
- 27.Muto T, Yamazaki A, Takeda S, Kawakami J, Tsuji Y, Shibata T, Mizoguchi I. Relationship between the pharyngeal airway space and craniofacial morphology, taking into account head posture. Int J Oral Maxillofac Surg. 2006;35:132–136. doi: 10.1016/j.ijom.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 28.Enlow D. H, Hans M. G. Essentials of Facial Growth 2nd ed. Philadelphia, Pa: Saunders; 2008. [Google Scholar]
- 29.Trenouth M. J, Timms D. J. Relationship of the functional oropharynx to craniofacial morphology. Angle Orthod. 1999;69:419–423. doi: 10.1043/0003-3219(1999)069<0419:ROTFOT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Muto T, Yamazaki A, Takeda S. A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int J Oral Maxillofac Surg. 2008;37:228–231. doi: 10.1016/j.ijom.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 31.Cosentini T, Le Donne R, Mancini D, Colavita N. Magnetic resonance imaging of the upper airway in obstructive sleep apnea. Radiol Med. 2004;108:404–416. [PubMed] [Google Scholar]
- 32.Chen N. H, Li K. K, Li S. Y, Wong C. R, Chuang M. L, Hwang C. C, Wu Y. K. Airway assessment by volumetric computed tomography in snorers and subjects with obstructive sleep apnea in a Far-East Asian population (Chinese) Laryngoscope. 2002;112:721–726. doi: 10.1097/00005537-200204000-00023. [DOI] [PubMed] [Google Scholar]
- 33.Schwab R. J, Gefter W. B, Hoffman E. A, Gupta K. B, Pack A. I. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148:1385–1400. doi: 10.1164/ajrccm/148.5.1385. [DOI] [PubMed] [Google Scholar]
- 34.Cozza P, Ballanti F, Castellano M, Fanucci E. Role of computed tomography in the evaluation of orthodontic treatment in adult patients with obstructive sleep apnea syndrome (OSA) Prog Orthod. 2008;9:6–16. [PubMed] [Google Scholar]