Abstract
Objective:
To evaluate impulse debonding compared to three conventional methods for bracket removal in relation to the damage caused to the enamel surface.
Materials and Methods:
Ninety-six osteotomed third molars were randomly assigned to two study groups (n = 48) for bracket bonding with either a composite adhesive system (CAS) or a glass-ionomeric cement (GIC). These two groups were then each randomly divided into four subgroups (n = 12) according to the method of debonding using (1) bracket removal pliers, (2) a side-cutter, (3) a lift-off debracketing instrument, or (4) an air pressure pulse device. Following debonding and corresponding postprocessing with either a finishing bur (CAS) or ultrasound (GIC), the enamel surfaces were assessed for damage, adhesive residues, and the need for postprocessing using scanning electron microscopy and the Adhesive Remnant Index, and the surfaces were compared in terms of mode of removal and type of adhesive using Fisher's exact test (α = 5%).
Results:
No significant differences were found between the two different types of adhesives (CAS, GIC) in terms of the amount of damage to the enamel. Portions of enamel damage were found for impulse debonding/0%<bracket removal pliers/4%<lift-off debracketing instrument/17%<side-cutter/21%. The highest Adhesive Remnant Index grades were seen for impulse debonding. GIC residues after postprocessing using ultrasound were seen in 79%, compared to 48% after rotational postprocessing of CAS residues.
Conclusions:
Impulse debonding provides a good alternative to conventional debonding methods, as the adhesion is usually separated at the bracket-adhesive interface, thereby avoiding enamel damage, independent of the adhesive used.
Keywords: Impulse debracketing, Conventional debonding, Enamel surface alteration, CoronaFlex
INTRODUCTION
Small-scale enamel damage following debonding, such as that associated with ruptures, cracks, or avulsion fractures, is considered to be crucial in the context of the etiology of caries.1 Irreversible loss of enamel should be minimized, as the outermost enamel layer contains a higher concentration of fluoride ions and is considered to be essential for protection against caries.2
A variety of factors (eg, the choice of adhesive used for bracket bonding, the particular type of enamel etching, and postprocessing after debonding, as well as the method used for debonding) have been considered to contribute to a potential loss of enamel and the amount of adhesive residue.3
Composite adhesive systems (CAS) are usually used for orthodontic bonding purposes,4 and to a large extent their bonding strength derives from enamel conditioning by etching and subsequent mechanical retention to microporosities.5 The duration and concentration of acid conditioning influences both the bond strength and enamel loss6 and can cause enamel loss of, on average, about 10 µm when using 37% phosphoric acid.7 However, mechanical adhesive/enamel retention has been measured up to a depth of 100 µm.8
Another negative side-effect of strong mechanical retention is that CAS debonding and the corresponding postprocessing of enamel surfaces using different rotary finishing instruments3,8,9 are laborious and are associated with subsequent enamel damage and a loss of up to 19.2 µm of enamel.7
Apart from CAS, glass-ionomeric cement (GIC) represents an alternative for orthodontic bonding.4,10 In contrast to the mechanical retention produced by CAS, GIC achieves enamel adhesion by bringing about an acid-base reaction that is characterized by significantly reduced bond strength.10 That is why GIC is commonly considered to yield better enamel preservation during debonding. Therefore, GIC residues are easily removed using ultrasonic probes instead of rotary instruments.11
Various methods have been proposed8,11,12 to provide adequate control of pull-off forces and line of breakage during debonding, such as bracket removal pliers (BRP), ligature cutters, or specific lift-off debracketing instruments (LODIs). Alternatively, debonding can also be achieved using air pressure impulse devices, as is common for crown removal in prosthodontics.13
Study Aims
Since a variation in the amount of damage to the enamel and adhesive residues on enamel surfaces following debonding and postprocessing may be expected, depending on the adhesive system and the debonding technique used, the aim of this study was to determine the bonding/debonding procedure that maximally preserves enamel surfaces by evaluating enamel damage and adhesive residues after debonding of CAS- or GIC-bonded brackets with one of four different instruments (BRP, side-cutter [SC], LODI, and an air pressure impulse device).
MATERIALS AND METHODS
Teeth
Ninety-six third molars that were freshly osteotomed (because of a lack of space) and preserved in physiological saline at 20°C were used in the study. Excluded from the study were third molars with enamel damage (fractures, demineralization, or decay), as assessed by visual inspection using a 2× magnifier. The patients or their guardians gave informed consent for donation of the extracted third molars for study purposes. For better handling and to simulate visco-elastic cushioning and elastic fiber suspension, each of the cleaned teeth was embedded in a small block of silicone (Silaplast; Detax, Ettlingen, Germany).
Bonding
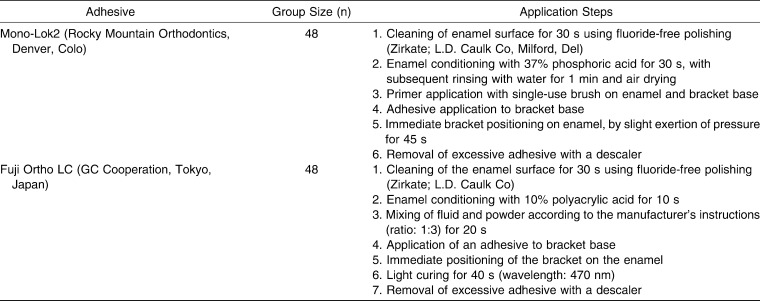
Bonding was achieved using upper premolar metal brackets with a mesh-like base to enable better adhesive retention (Ormesh; Ormco, Orange, Calif), as these fitted neatly to the buccal surface of the third molars. Teeth were randomly assigned to one of two study groups (n = 48) for bonding with either CAS or GIC. For CAS bonding, the hybrid composite Mono-Lok2 (Rocky Mountain Orthodontics, Denver, Colo) was used in accordance with the manufacturer's instructions for application; this step was preceded by enamel etching using 37% phosphoric acid. For GIC bonding, Fuji Ortho LC (GC Co-operation, Tokyo, Japan) was used, which is a light-cured, resin-modified glass-ionomere. Prior enamel conditioning was carried out by conditioning with 10% polyacrylic acid. The application steps for both adhesives are shown in Table 1.
Table 1.
Application Steps for Both the Composite Adhesive Mono-Lok2 and the Glass-Ionomere Cement Fuji Ortho LC
Debonding
The two adhesive groups were randomly assigned to four subgroups (n = 12), and following interim storage in physiological saline, debonding was carried out 24 hours after bonding using the following four debonding methods: (1) BRP (Dentaurum; Ispringen, Germany); (2) a medium-sized SC (Dentaurum); (3) a LODI (3M Unitek; Monrovia, Calif), or (4) an air pressure pulse device (CoronaFlex, Kavo, Biberach; Germany [www.kavo.com]), which is used in prosthodontics for the removal of crowns and bridges (Figure 1). All debondings were carried out by the same operator.
Figure 1.
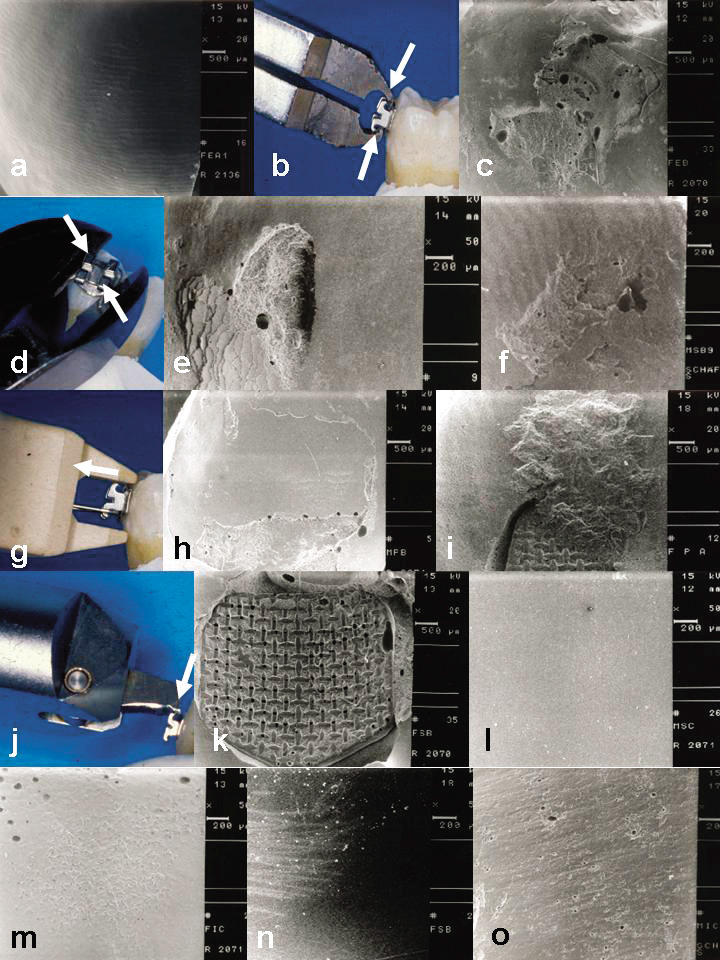
(a) Enamel damage (ED) and ARI Grade 0; (b) BRP debonding; (c) adhesive residues after CAS/BRP debonding; (d) SC debonding; (e) terrace-shaped enamel disaggregation following GIC/SC debonding; (f) ED Grade 3 after CAS/SC debonding; (g) LODI debonding and subsequent (h) ARI Grade 1 after CAS/LODI debonding; (i) larger ED Grade 3, which exceeds the former bracket base area; (j) impulse debracketing; (k) ARI Grade 3; (l) smooth enamel surface following rotary postprocessing; (m) adhesive residues following ultrasonic treatment; (n) ultrasonic-induced enamel traces; and (o) enamel traces and adhesive residues following rotary postprocessing.
Although variations in the use of the debonding instruments are possible, debracketing was performed in the conventional, standardized manner, as follows:
The SC was orientated such that it was inserted diagonally at the bracket base, at the cervical and incisal parts, respectively. The bracket was removed by gentle squeezing of the pliers and an additional clockwise rotational movement.
The BRP was applied by gripping below the bracket wings. By closing and downward tipping of the pliers, a rotational axis was created at the apical bracket margin, thereby releasing the bracket.
The LODI was positioned by linking its hanger to the upper left bracket wing and simultaneously resting the instrument on the tooth. Compression of the pliers caused the bracket to come off on application of a pulling force.
The CoronaFlex was used by positioning its toggle parallel to the adhesive-enamel interface. By pulling the trigger, a piston with a weight of 2.5 g was impelled by an air pressure of 2.2 bar along the shaft on the toggle, thereby releasing a short impact pulse of 3000 N for 10 milliseconds, which removed the adhesion.
Postprocessing was carried by guiding the respective instruments in a direction parallel to the enamel surface for 30 seconds with water cooling. Modes of postprocessing were adhesive specific: namely, a rotary finishing bur for the CAS group (Ortho-bur H23R204 016, Brasseler, Germany) and an ultrasonic probe (No. 1005715832, Siemens, Germany) at a frequency of 50,000 Hz for removing the GIC residues.
Scanning Electron Microscopy Analysis
Scanning electron microscopy (SEM) evaluation (DSM 960; Zeiss; Germany) of enamel surface-negative replicas (President Light/Heavy Body, Coltène Whaledent, Germany) was carried out prior to bonding (T0), after debonding (T1), and after corresponding postprocessing (T2) at an observation angle of 90° and at 20× and 50× magnification. All 96 enamel surfaces appeared intact at baseline (T0).
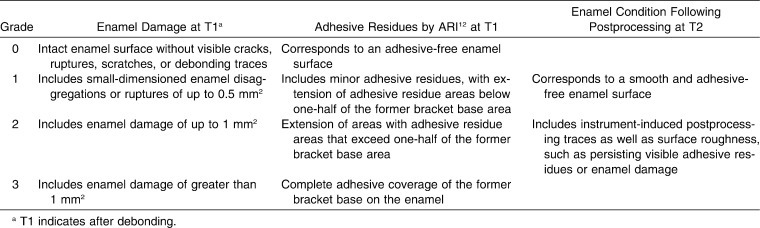
Standardization of SEM recordings and reproducibility of observations were assured by a pretrial series of debonding and subsequent SEM analysis. Enamel damage and adhesive residues at T1 were assessed with four grades (0–3), as were the adhesive residues using the Adhesive Remnant Index (ARI).12 Assessment of enamel surfaces at T2 was made using two grades, applied separately for adhesive residues and enamel traces induced by debonding. Please refer to Table 2 for a summary of all assessment criteria.
Table 2.
Standard of Scanning Electron Microscopy (SEM) Evaluation for Enamel Damage, Adhesive Residues by the Adhesive Remnant Index (ARI; Arthun and Bergland12), and Enamel Condition Following Postprocessing. The assessment of adhesive residues or damage after postprocessing (T2) was a “yes/no” decision made independently by two orthodontists at the Dentistry Center at the University of Göttingen, Germany. In cases of disagreement, the enamel surfaces in question were assigned Grade 2
Statistical Analyses
A comparison was made of the proportions of enamel damage, postprocessing residues, and enamel traces at specific times between the two adhesives and the four instruments, at specific times, using the Fisher's exact test with R (v2.8, www.r-project.de). Adhesive residue grades were compared using the Kruskal-Wallis test. In the case of a significant effect of the method used, subsequent pairwise comparisons were carried out using adjusted significance levels according to Holm. Significance levels for all global tests were set to α = 5%.
RESULTS
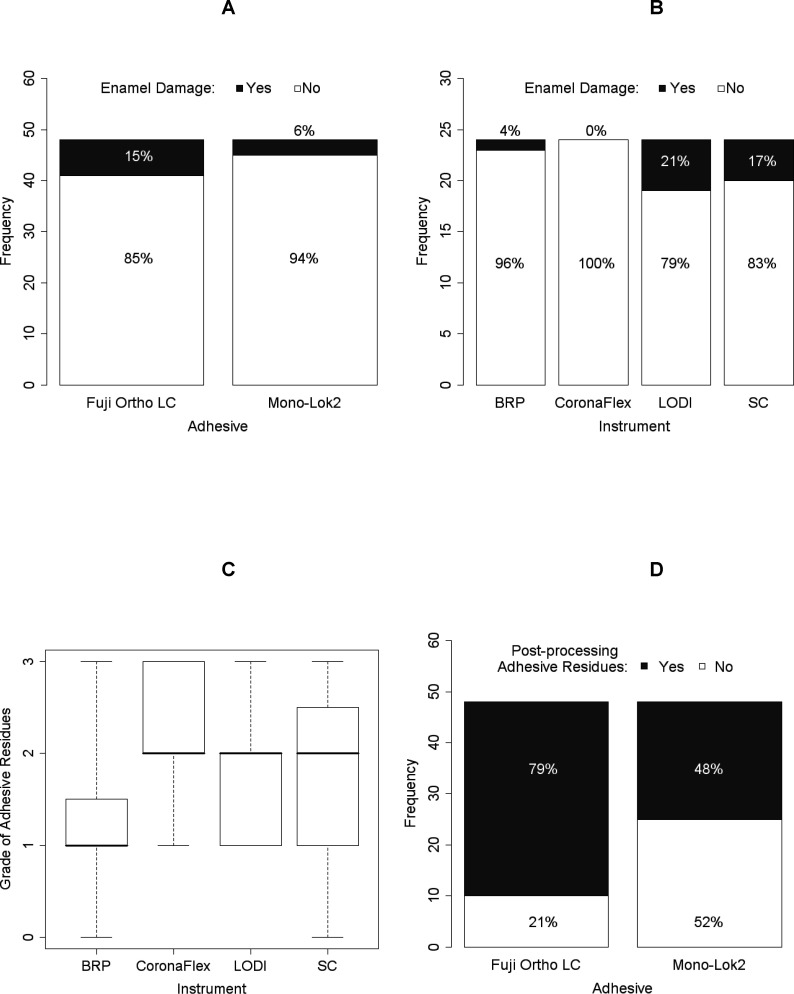
Enamel Condition at T1
Enamel damage was detected in 10 of 96 teeth: four teeth had enamel ruptures, three had less enamel damage, and three had greater enamel damage, according to our assessment criteria (Figure 2a,b, Table 3). Those teeth with enamel ruptures were pervaded by cracks and enamel disaggregations at the area of rupture. Ruptures had a crater shape and a corrugated and terrace-shaped appearance. Enamel ruptures were seen in adhesive-free areas and at the margins between enamel and adhesive (Figure 1c–i).
Figure 2.
Portions of enamel damage at T1 (A, B) and postprocessing adhesive residues at T1 (boxplot, C) and T2 (D), with respect to the different adhesives and instruments.
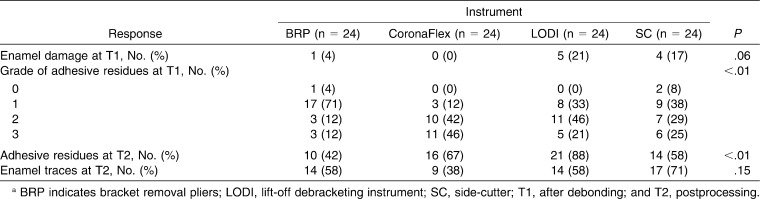
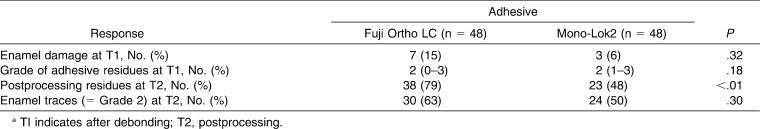
Table 3.
Comparison of Responses (Absolute, [Relative] Frequency) Among the Four Instrumentsa
Although GIC-bonded brackets were subjectively easier to remove compared to those bonded with Mono-Lok2, overall and regardless of the method used for bracket removal there was more enamel damage seen after GIC debonding (15%). However, compared with CAS debonding, the difference (6%) was not significant (Table 4).
Table 4.
Comparison of Responses Between the Two Adhesives. Descriptive values are either the absolute (relative) frequency or the median (range)a
According to Figure 2b, the use of CoronaFlex and, with the exception of a single instance of minor enamel damage, the use of the BRP did not result in visible enamel damage in either of the adhesive groups. The majority of enamel damage resulted from LODI (n = 5) and SC debonding (n = 4) (Table 3).
The proportions of adhesive residues following debonding were significantly influenced by the mode of removal, whereas the adhesive system had no significant influence on the ARI results at T1 (Tables 3 through 5).
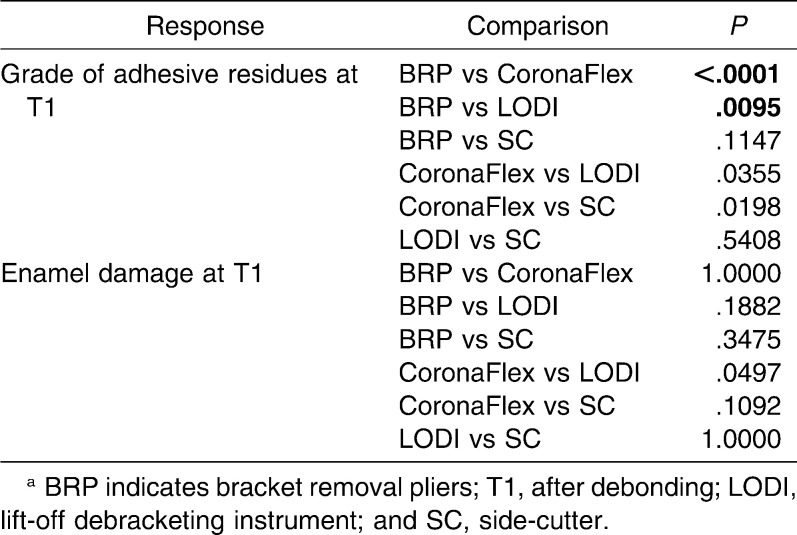
Table 5.
Pairwise Comparisons of Enamel Damage, Grade of Adhesive Residues, and Postprocessing Adhesive Residues Among the Four Instruments. Bold-type P-values indicate a significant difference according to Holm-adjusted significance levelsa
Enamel Condition at T2
Upon inspection with the naked eye, all enamel surfaces appeared clean and smooth after postprocessing. Adhesive residues found at T2 were not large laminary remnants but were very small ones that were only visible with SEM.
Both the choice of the debonding mode and the choice of the adhesive system with corresponding postprocessing had a significant effect on residues of adhesives after postprocessing at T2, with greater efficiency of the CAS being revealed with rotational finishing. After use of ultrasonic, roughness sites and treatment traces were seen in 63% of the GIC group teeth compared to 50% of the CAS group (Table 4; Figures 1l–o and 2d).
Neither ultrasonic nor finishing bur treatment produced enamel plate dissolving or fractures that were visible with SEM. Fractures induced by debonding were leveled by both postprocessing regimes.
DISCUSSION
Although both the adhesive system used for orthodontic bonding and the duration, type, and concentration of the etching agent6 are considered to be relevant when evaluating bonding efficacy and impact on enamel damage,14 the results of our study do not support the assumption that there is a significant impact on the reduction in the amount of enamel damage when using GIC instead of CAS. In agreement with previous findings8 regarding enamel damage following debonding, 89% of teeth appeared intact after bracket removal. Despite the use of osteotomed molars, in which reduced microretention could be expected as a result of the impeded acid penetration of the aprismatic enamel layer, the findings of enamel damage were similar to those obtained in corresponding studies3,8 of erupted teeth.
Another aspect to consider is the nature of enamel damage. In addition to regularly occurring enamel loss of up to 41.2 µm caused by etching, bonding, and debonding,7 enamel avulsion is often accompanied by the tearing off of enamel discs, which may have a thickness of up to 100 µm.8 Consequently, those debonding procedures that result in less preservation of enamel damage may amount to more than 140 µm in some areas, which would represent approximately 10% of the facial enamel surface.8 This signals a need for debonding methods that preserve the enamel surface to the greatest extent possible and that at least minimize the tearing off of large enamel discs.
One attempt at reducing enamel damage during debonding entails damaging the bracket more than the enamel structures. It has been suggested15 that debonding methods accompanying the squeezing of bracket wings result in less frequent enamel damage because excessive forces are transferred in such a way that deformation of the bracket results, as opposed to avulsion breaks to the enamel. Moreover, brackets are destroyed in the process, thereby making these methods unsuitable if brackets are to be utilized for rebonding (eg, for correction of malpositions).13
When considering methods for reducing damage to enamel, a crucial point is the line of breakage during bracket loosening. Protection of the enamel could to some extent be ensured if the breakage line was relocated exclusively within the adhesive layer,12 thus maintaining a thin but complete adhesive cover on the enamel (instead of having a breakage at the enamel-adhesive interface). The key to preserving the enamel during debonding may therefore be the amount of adhesive residues remaining after debonding:
In the CAS group, the line of breakage was mainly at the bracket-adhesive interface, whereas in the GIC-bonded teeth it was more likely to be seen at the adhesive-enamel interface, regardless of the debonding mode, a finding that is in agreement with those of previous research.10,14 This typical GIC breakage line may also be responsible for an insignificant tendency to produce greater enamel damage in this group, despite the assumption that more severe enamel damage is caused by CAS microretentive adhesion. In contrast, the greater bonding strength of the CAS seems to provide some protection against the tearing off of enamel discs by maintaining a thin adhesive layer following debonding.
In contrast to BRP or the SC, the use of CoronaFlex and LODI in no case resulted in an adhesive-free surface after debonding, independent of the adhesive used. Using impulse debonding, 46% of enamel surfaces were covered completely, and 42% were more than half covered with adhesive (ie, the line of breakage was mostly located at the interface between the bracket base and the adhesive), which provides an explanation for the absence of enamel damage following impulse debonding in both of the adhesive groups. This functional principle entails the creation of large forces and moments parallel to the enamel surface, but these only last for 10 milliseconds rather than a number of seconds; details on respective force systems have been published previously.13 Also, when BRP was used, we only found a small amount of damage to the enamel in both adhesive groups. However, according to previous research,13 and in contrast to SC and BRP debonding, it was found that impulse debonding results in brackets that can be reused, as is also the case following LODI debonding. However, there is no damage to the enamel surface. On the other hand, adhesive residues were largest after impulse debonding.
Debonding forces are generated by the SC insert at the adhesive layer and below the bracket base, and they are known to transmit large forces to the underlying enamel,15 thereby producing quite significant enamel damage. We found these forces were quantitatively not significantly different compared to results obtained with the other methods investigated in our study. In some cases, even traces left by the SC itself were also seen in the enamel. Therefore, the SC is not recommended for debonding purposes.
Beneath small-dimensioned damage and ruptures, larger enamel disaggregations were also seen following LODI debonding. It may be assumed that the pull-off forces transmitted perpendicular to the bracket-adhesive-enamel interface—with the proviso of good microretentive anchorage—may provide an explanation for these disaggregations. In some teeth, we even found enamel disaggregations that exceeded the adhesive area of the former bracket base (Figure 1).
Adhesive Residues at T2
Rotary postprocessing in the CAS group produced noticeably better removal of adhesive residues (52%) compared to ultrasonic postprocessing in the GIC group (21%; Figure 2). This is in line with the findings of previous research.8,11 Ultrasound-induced traces or disaggregations were found in two-thirds of the GIC group. However, these disaggregations were more superficial compared to those left behind by rotary CAS, which finished more superficially. Wave-like postprocessing traces and coincident enamel loss were found in 50% of the CAS-bonded teeth following rotary finishing, a phenomenon that has been explained8 by the inevitable variations in the contact pressure of the instrument during postprocessing. After rubber polishing, postprocessing traces were never seen. Final polishing is therefore recommended for both adhesives.9
In general, as phosphoric acid conditioning may result in adhesive residues up to a depth of 100 µm,8 the complete removal of CAS adhesive residues is not possible.16 Also, in our study, it is likely that only superficial residues were removed.
Clinical Implications
Despite the great forces applied to the teeth, impulse debonding is a method that is considered to be more enamel preserving than are LODI and SC debonding, but impulse bonding performs only slightly better when compared to BRP debonding, in terms of the amount of enamel damage. However, one fact that has to be considered is that brackets debonded with BRP are not suitable for reuse.13,15
Despite the assumption that enamel damage might be greater as a result of microretentive adhesion when bonding with CAS, this technique seems to provide some enamel protection by preventing the tearing off of enamel discs by maintaining a thin adhesive layer on the enamel. The effect of GIC is more to produce a breakage line at the adhesive-enamel interface. However, the two requirements of an enamel-preserving debonding procedure, on the one hand, and a minimized/reduced postprocessing, on the other, are somewhat controversial. Enamel preservation during debonding appears to coincide with greater amounts of adhesive residues.
CONCLUSIONS
No significant differences were seen for the two different types of adhesives (CAS, GIC) in terms of the amount of enamel damage.
The lowest proportions of enamel damage were seen for impulse (0%) and BRP (4%) debonding.
Low proportions of enamel damage during BRP debonding are likely to be due to destructive bracket squeezing.
When assessed in terms of enamel damage, the SC and the LODI cannot be recommended for debonding brackets.
REFERENCES
- 1.Walker B. N, Makinson O. F, Peters M. C. Enamel cracks. The role of enamel lamellae in caries initiation. Aust Dent J. 1998;43:110–116. doi: 10.1111/j.1834-7819.1998.tb06099.x. [DOI] [PubMed] [Google Scholar]
- 2.Arends J, Christoffersen J. The nature of early caries lesions in enamel. J Dent Res. 1986;65:2–11. doi: 10.1177/00220345860650010201. [DOI] [PubMed] [Google Scholar]
- 3.Sandison R. M. Tooth surface appearance after debonding. Brit J Orthod. 1981;8:199–201. doi: 10.1179/bjo.8.4.199. [DOI] [PubMed] [Google Scholar]
- 4.Summers A, Kao E, Gilmore J, Gunel E, Ngan P. Comparison of bond strength between a conventional resin adhesive and a resin-modified glass-ionomer adhesive: an in vitro and in vivo study. Am J Orthod Dentofacial Orthop. 2004;126:200–206. doi: 10.1016/j.ajodo.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Bishara S. E, Gordon V. V, Von Wald L, Jakobsen J. R. Shear bond strength of composite, glass-ionomer and acid primer adhesive systems. Am J Orthod Dentofacial Orthop. 1999;115:24–28. doi: 10.1016/s0889-5406(99)70312-4. [DOI] [PubMed] [Google Scholar]
- 6.Sadowsky P. L, Retief D. H, Cox P. R, Newcombe R. G. Effect of etching concentration and duration on the retention of orthodontic brackets: an in vivo study. Am J Orthod Dentofacial Orthop. 1990;98:417–421. doi: 10.1016/S0889-5406(05)81650-6. [DOI] [PubMed] [Google Scholar]
- 7.Pus M. D, Way D. C. Enamel loss due to orthodontic bonding with filled and unfilled resins using various clean-up techniques. Am J Orthod. 1980;77:269–283. doi: 10.1016/0002-9416(80)90082-2. [DOI] [PubMed] [Google Scholar]
- 8.Diedrich P. Enamel alterations from bracket bonding and debonding. A study with the scanning electron microscope. Am J Orthod. 1981;79:500–522. doi: 10.1016/s0002-9416(81)90462-0. [DOI] [PubMed] [Google Scholar]
- 9.Campbell P. M. Enamel surfaces after orthodontic bracket debonding. Angle Orthod. 1995;65:103–110. doi: 10.1043/0003-3219(1995)065<0103:ESAOBD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Cook P. Direct bonding with glass-ionomer cement. J Clin Orthod. 1990;8:509–511. [PubMed] [Google Scholar]
- 11.Krell K. V, Courey J. M, Bishara S. E. Orthodontic bracket removal using conventional and ultrasonic debonding techniques, enamel loss and time requirements. Am J Orthod Dentofacial Orthop. 1993;103:258–266. doi: 10.1016/0889-5406(93)70007-B. [DOI] [PubMed] [Google Scholar]
- 12.Arthun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etching enamel pretreatment. Am J Orthod. 1984;85:333–340. doi: 10.1016/0002-9416(84)90190-8. [DOI] [PubMed] [Google Scholar]
- 13.Knösel M, Mattysek S, Jung K, Kubein-Meesenburg D, Sadat-Khonsari R, Ziebolz D. Suitability of orthodontic brackets for rebonding and reworking following removal by air pressure pulses and conventional debracketing techniques. Angle Orthod. 2010;80:461–467. doi: 10.2319/102809-605.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toledano M, Osorio R, Osorio E, Romeo A, de la Higuera B, Garcia-Godoy F. Bond strength of orthodontic brackets using different light and self-curing cements. Angle Orthod. 2003;73:56–63. doi: 10.1043/0003-3219(2003)073<0056:BSOOBU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Bennett C. G, Shen C, Waldron J. H. The effects of debonding on the enamel surface. J Clin Orthod. 1984;18:330–334. [PubMed] [Google Scholar]
- 16.Osorio R, Toledano M, Garcia-Godoy F. Bracket bonding with 15- or 60-second etching and adhesive remaining on enamel after debonding. Angle Orthod. 1999;69:45–49. doi: 10.1043/0003-3219(1999)069<0045:BBWOSE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]