Abstract
Objective:
This pilot study was performed to test the hypothesis that an orthodontic oral appliance (OA) that is designed to work against the backwardly directed forces on the upper incisors may counteract the reduction in overjet from these devices.
Materials and Methods:
Thirty patients with normal bites, good oral health, and milder sleep apnea were randomized to treatment with either OAs or orthodontic OAs. Bite changes were evaluated on plaster casts and radiographs and by questionnaires after a mean of 2.4 years in 19 frequent users.
Results:
Four of nine patients in the orthodontic OA group increased their overjet by ≥0.4 mm, while none of the 10 patients in the OA group experienced that effect.
Conclusion:
Only the orthodontic OA increases the overjet; this design may therefore be beneficial to patients at risk of negative effects on their bite during OA treatment.
Keywords: Adverse effects, Obstructive Sleep apnea, Oral appliances, Orthodontic appliances, Snoring
INTRODUCTION
Side effects are common and constitute an important reason for many patients with obstructive sleep apnea (OSA) to comply poorly or to stop using an oral appliance (OA).1–7 Bite changes become increasingly frequent in the longer term. These are mainly recognized by a reduction in overjet when the upper incisors tip backward and the lower incisors move forward8–16 (Figures 1 and 2). After up to 5 years, between 14% and 35% of patients have been reported to experience overjet reductions of more than 1 mm.15–17 Patients with small overjet and overbite run the greatest risk of experiencing unfavorable changes in their bites,8,17 while patients with a deep bite have been found to develop smaller changes in overjet.8,17 The aim of the present pilot study was to test the hypothesis that a new type of OA that was designed to reduce the backward tipping forces on the upper front teeth could counteract the reduction in dental overjet that often occurs during the treatment of patients with snoring and OSA. A second aim was to evaluate whether other side effects were produced by this device.
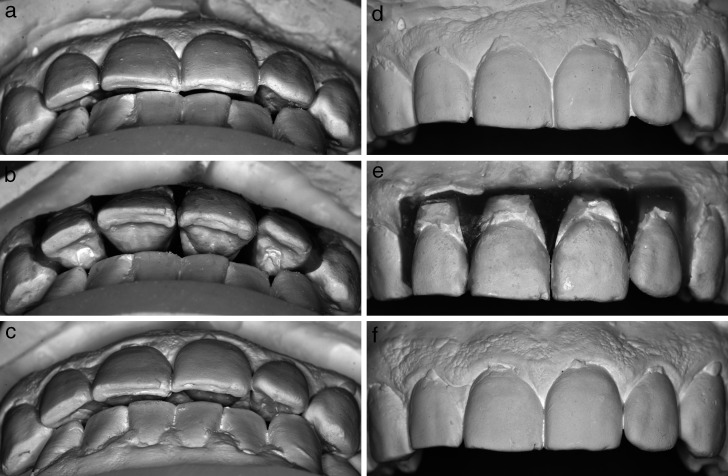
Figure 1.
Measurement of angles and distances on lateral cephalograms. S indicates center of sella turcica; N, nasion, extreme anterior point of the frontonasal suture; Spp, posterior nasal spine; Spa, anterior nasal spine; A, extreme posterior point on the anterior curvature of the maxillary alveolar area in the midsagittal plane; B, extreme posterior point on the anterior curvature of the mandibular alveolar area in the midsagittal plane; Pg, pogonion, extreme anterior point on the bone of the chin; Gn, gnathion, extreme inferior point on the mandibular symphysis; and Go, gonion, extreme inferior point on the mandibular angle at the intersection between the mandibular line and the ramus line. Arrows indicate the forces exerted by the device on the front teeth.
Figure 2.
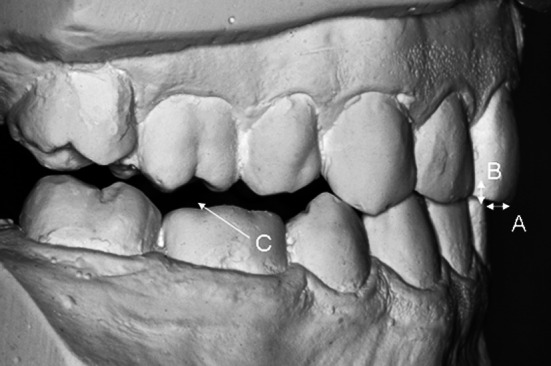
A indicates overjet; B, overbite; and C, posterior bite opening.
MATERIALS AND METHODS
Of 243 consecutively referred patients, all patients with an apnea-hypopnea index of below 20, at least 12 teeth in each jaw, an initial overjet and overbite of ≤4 mm (measured in the mouth with a sliding caliper), and a healthy periodontium (defined as an attachment level that was located <3 mm apical to the cementoenamel junction on the front teeth) were asked to participate. Patients with a clinically visible distance between centric relation and centric occlusion were excluded. Thirty-three patients (25 men) were eligible. Three men refused to take part in the study.
The patients were randomized to treatment with either of two types of OA (Figure 3) in a parallel, double-blind study. Block randomization and stratification with respect to the initial overbite (limit = 2 mm) were used to prevent bias from the protective effect of a deep bite on the overjet changes.8,17 Before treatment, the patients responded to questionnaires and were examined clinically. Plaster casts, wax indices, and radiographs were made. After a habituation period with the OA, we adjusted the degree of mandibular advancement in relation to the symptomatic improvement and the side effects reported by the patients. Six patients received one change of mandibular positioning, and one patient demanded two adjustments. The mean amount of advancement was 5.6 mm (range, 3.0 to 8.0 mm) and the mean opening was 9.6 mm (range, 6.2 to 13 mm) after this titration procedure. At a follow-up after a mean of 2.4 years (range, 2.2 to 2.7 years), all the patients who had used the device for full nights and for more than 50% of the nights were re-evaluated using the same procedures performed before treatment. Approval for the study was obtained from the Medical Ethics Committee at Umeå University. Written informed consent was obtained from all patients.
Figure 3.
Oral appliance.
The orthodontic OA, a monoblock elastomeric appliance (SR-Ivocap Elastomer, Ivoclar, Schaan, Liechtenstein), was designed to redistribute the forces on the upper incisors. The control device looked exactly the same and it was impossible for either the patients or the therapist to recognize the type of device that was being used in individual patients. The orthodontic OA was made on a model in which the four upper incisors had been cut out of the initial casts and repositioned with the incisor edges protruding 1–2 mm and the apical parts retraced at about the same distance compared with their original positions (Figure 4).
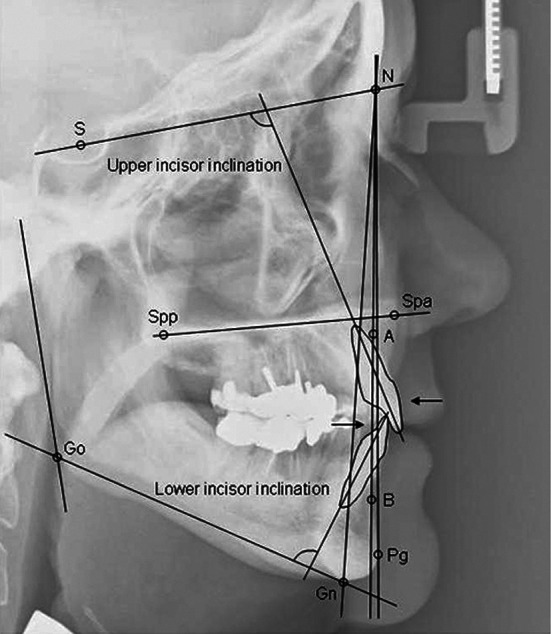
Figure 4.
View of front teeth in one patient who experienced an increase in overjet. (a) Overjet before treatment. (b) Repositioned front teeth. (c) Overjet at longer term follow-up. (d) Front view before treatment. (e) Repositioned teeth. (f) Front view at longer term follow-up.
The patients responded to questionnaires about the frequency of appliance use and whether they had suffered from bite changes, temporomandibular joint (TMJ) sounds, locked jaw, headaches, pain in the teeth or jaws, salivation problems, or headaches. Patients described bite changes using one of the following statements: “The bite has changed in the morning, but this feeling disappears after a short while,” “The bite has changed in the morning, but this feeling disappears after lunch,” “The bite is changed all day,” “The bite is changed all day and this is disturbing,” or “Something else has happened to my teeth.” The patients responded to two questions from the Basic Nordic Sleep Questionnaire about the frequency of nights on which they snored and how often they felt irresistibly sleepy.18 They also reported the degree of disturbing snoring on a 10-point scale.
Overjet, overbite, and degree of mandibular opening were measured by a digital sliding caliper on the upper right central incisor on the study casts. A mark was drawn by a pen on the incisor edge at a defined distance from the midline. This procedure was repeated on the follow-up cast. Another mark was drawn on a lower incisor at the corresponding place with the study casts in central occlusion. The degree of mandibular advancement was measured on a transparent millimeter sheet in the premolar area along the occlusal plane. An increase in lateral bite opening was measured with a transparent millimeter sheet. The measurements were performed blindly with respect to device design by one investigator. The measurements were repeated three times and the average value was reported. A change of more than two standard deviations in the difference between the repeated measurements of the initial overjet was used to identify patients with a decrease or an increase in overjet.
The radiographic examinations comprised bitewing examinations of front teeth, panoramic examinations of jaws and TMJs, and a lateral cephalogram. Analyses of marginal bone level, TMJ condyle position, and selected cephalometric landmarks were performed. The marginal bone level was assessed in relation to the cementoenamel junction of the adjacent teeth and compared between the two evaluations. Images from different TMJ panoramic examinations were superimposed and the condyle positions were evaluated with a subtraction technique. The selected landmarks on the cephalograms were: SNA (sagittal position of the maxilla), SNB (sagittal position of the mandible), N-Gn (face height), SN-Pg (sagittal position of the chin), and angulations of the upper and lower incisors (Figure 1). The radiographic measurements were performed blindly with respect to appliance design by one investigator.
Wilcoxon's matched-pairs signed-rank test was used to evaluate tooth movements on study casts and radiographs. Differences between the appliance groups in terms of patient characteristics and changes in overjet, overbite, and cephalometric variables were analyzed with the Mann-Whitney U-test for independent samples. Calculations were made using the SPSS 16.0 Statistical Package. A P value of less than .05 was considered significant.
RESULTS
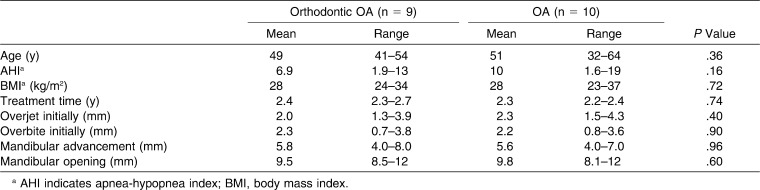
Seven of the 30 patients (23%) had discontinued treatment during the 2.4 years of the study because of insufficient treatment effects (two patients), side effects (two patients), or other reasons (three patients). Three of these patients had been randomized to use the orthodontic OA and four patients had tried the OA. Another four of the 30 patients had used their appliances infrequently; three had been treated with the orthodontic OA and one with the OA. Among the 19 frequent users, 9 used the orthodontic OA and 10 used the OA. There were no differences in age, initial apnea-hypopnea index, body mass index (kg/m2), initial bite characteristics, or any cephalometric variable between the two randomization groups (Table 1).
Table 1.
Patients' Characteristics Among Frequent Users (n = 19)
The mean changes in overjet were 0.1 mm for the orthodontic OA and −0.2 mm for the ordinary OA (Table 2). Four patients who had used the orthodontic OA increased their overjet by ≥0.4 mm, while none of the patients who had been treated with the OA experienced any such effect (Figure 4a,c). Two of the patients who had used the orthodontic OA and three patients treated with the OA decreased their overjet. The remaining nine patients experienced smaller overjet changes. There were no differences in mandibular advancement or opening between the patients who had experienced overjet decreases or increases.
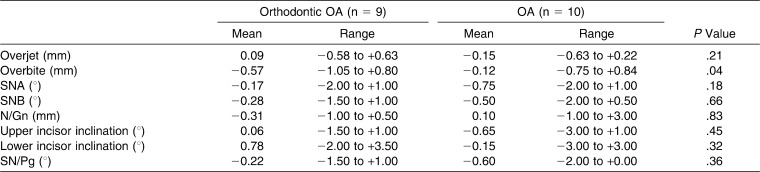
Table 2.
Change in Overjet, Overbite, and Cephalometric Variables in the Two Appliance Groups
The overbite decreased with the orthodontic OA (P = .02) but not with the OA (Table 2). The decrease was significantly larger in the patients who had used the orthodontic OA compared with those who had been treated with the OA (P = .04).
Posterior bite openings increased by a median of 1 mm for both devices and there was no difference between them. There were no visual changes in the lower or upper incisor positions on the study casts from any patient (Figure 4d,f).
The SNA angle decreased in the OA group (P < .05) but was unchanged in the orthodontic OA group (Figure 1, Table 2). The incisors' inclinations were unchanged. The marginal bone level was similar and the TMJ condyle position was unchanged between the radiographic examinations.
Seventeen of the 19 patients experienced no or only minor bite changes. None of the four patients who developed an increased overjet felt any changes in their bites. There were no differences in any reported type of side effect between the two appliance groups.
The 19 frequent users reported that snoring decreased from a median frequency of “Every night or almost every night” to “Less than weekly” (P < .001). The degree of disturbance of the snoring was reported to diminish from 8.2 (range, 4.7 to 10) to 1.7 (range, 0.3 to 7.6) on the 10-point scale (P < .001). The tendency to fall asleep during the daytime decreased from occurring 1–2 times a week to less than once a month (P < .003).
Headaches before the start of the study were reported by four of the patients who were treated with the orthodontic OA and by five who used the OA. None of the patients in the orthodontic OA group and two of the patients in the OA group reported headaches at follow-up.
DISCUSSION
The orthodontic OA produced an increase in overjet in four patients, while the OA generated no such change. Other side effects were mild and similar with both types of device.
Decreases in overjet and overbite are the most common dental side effects to occur during the longer-term treatment of patients with snoring and sleep apnea. Almeida et al8 defined favorable and unfavorable bite changes. Patients with distal occlusion usually benefit from the OA, since a reduction in overjet and overbite increases the occlusal contact area.19 In contrast, patients with a normal bite or mesial occlusion may experience unfavorable changes in their dental occlusion. In the present study, we aimed to avoid the expected decrease in overjet during treatment. In fact, four of the nine patients with normal bites who used the orthodontic OA experienced an increase in their overjet. No patient using the ordinary OA experienced this effect. A reduction in overjet could not be avoided in two of the nine patients treated with the orthodontic OA. In spite of this, the present findings indicate a possible method for protecting patients from a decrease in overjet during longer-term treatment with OAs. Although the aim of the present study was not to produce an increased overjet, such an effect may prolong the time it takes for negative bite changes to develop. This mechanism of the orthodontic OA may be of help in treating patients with normal incisor relationships or mesial occlusion who risk developing unfavorable bite changes during longer-term treatment for snoring and sleep apnea.
Previous studies have shown mean changes in overjet of −1.2 to −0.2 mm and in overbite of −1.9 to −0.1 mm after a mean of 14 months to 7.4 years.9–13,20,21 These changes have been related to the treatment time, the degree of mandibular repositioning, the type of device, initial bite, and age.14,15,17 A larger degree of mandibular advancement will result in a higher risk of a decrease in overjet,9,14,17 and a larger mandibular opening will be related to a higher risk of reduced overbite.17,21 The mean overjet change of 0.1 mm for the orthodontic OA was smaller than that previously reported. The change in overbite was, however, a little larger in the patients using the orthodontic OA. It is possible that this decrease in overbite occurred as a result of the intended forward tipping of the upper front teeth by the orthodontic OA.
Various splints have been used for orthodontic reasons to achieve smaller or larger tooth movements.22 These splints are made from plaster casts on which the teeth have been repositioned in the desired positions. Our orthodontic OA was designed in accordance with that methodology. We planned to avoid the backward tipping of the upper front teeth by repositioning these teeth in a more proclined position in the appliance. The radiographs did not, however, show any change of the incisors as a result of any type of device.
Only two nonrandomized studies have compared the dental side effects of devices.14,17 The OA that was used in these studies, which featured extensions over the alveolar processes, was shown to produce fewer bite changes compared with a device that only covered the teeth. Many factors may influence the risk of bite changes in the individual patient. The relationship between older age and a higher risk of overjet changes may indicate that dental conditions influence the degree of bite changes.14 We only included milder sleep apnea patients with normal bite, good periodontal health, and at least 12 teeth in each jaw to produce similar randomization groups. There were few patients who fulfilled these criteria, since only 33 of 243 referred patients could be considered. Our present aim was to test the new device design in a well-defined group of patients regarding effects and side effects as baseline data for future studies in other populations. It is possible that the bite changes would have been larger in patients with reduced periodontal support or fewer teeth and that these patients might benefit more from an orthodontic OA.
Nineteen of 30 patients (63%) completed the entire study protocol; seven patients discontinued the study and four patients used the appliance infrequently. This compliance rate is comparable to previous findings, where about 55% to 70% of patients continued using an OA on a regular basis after similar treatment times.6,7
An elastomeric, monoblock OA was used in the present study. Adjustable dual-block devices are more commonly used today. It is possible that appliances of this kind with a thicker soft inner lining might be adapted according to the same principle as that used for the orthodontic OA in the present study. Because no unforeseen side effects in terms of pain or deterioration in appearance were found in the present study, we intend to further evaluate whether this appliance could be of benefit to patients who are doubtful about starting OA treatment because of the risk of a change in bite. In fact, the lack of negative effects from the new orthodontic OA indicates that this design could already be used in the clinic.
CONCLUSION
An orthodontic OA that is designed to counteract the backward tipping forces of the upper incisors may increase dental overjet during the longer-term treatment of patients with milder sleep apnea and good oral health.
There were no differences in subjective side effects between the orthodontic OA and an ordinary OA. The orthodontic OA may therefore be beneficial to patients at risk of negative effects on the bite during OA treatment.
REFERENCES
- 1.Chan A. S, Cistulli P. A. Oral appliance treatment of obstructive sleep apnea: an update. Curr Opin Pulm Med. 2009 Aug 25 doi: 10.1097/MCP.0b013e3283319b12. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Cistulli P. A, Gotsopoulos H, Marklund M, Lowe A. A. Treatment of snoring and obstructive sleep apnea with mandibular repositioning appliances. Sleep Med Rev. 2004;8:443–457. doi: 10.1016/j.smrv.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson K. A, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29:244–262. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 4.Hoekema A, Stegenga B, De Bont L. G. Efficacy and co-morbidity of oral appliances in the treatment of obstructive sleep apnea-hypopnea: a systematic review. Crit Rev Oral Biol Med. 2004;15:137–155. doi: 10.1177/154411130401500303. [DOI] [PubMed] [Google Scholar]
- 5.Hoffstein V. Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath. 2007;11:1–22. doi: 10.1007/s11325-006-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGown A. D, Makker H. K, Battagel J. M, L'Estrange P. R, Grant H. R, Spiro S. G. Long-term use of mandibular advancement splints for snoring and obstructive sleep apnoea: a questionnaire survey. Eur Respir J. 2001;17:462–466. doi: 10.1183/09031936.01.17304620. [DOI] [PubMed] [Google Scholar]
- 7.Shadaba A, Battagel J. M, Owa A, Croft C. B, Kotecha B. T. Evaluation of the Herbst Mandibular Advancement Splint in the management of patients with sleep-related breathing disorders. Clin Otolaryngol Allied Sci. 2000;25:404–412. doi: 10.1046/j.1365-2273.2000.00411.x. [DOI] [PubMed] [Google Scholar]
- 8.Almeida F. R, Lowe A. A, Otsuka R, Fastlicht S, Farbood M, Tsuiki S. Long-term sequelae of oral appliance therapy in obstructive sleep apnea patients: part 2. Study-model analysis. Am J Orthod Dentofacial Orthop. 2006;129:205–213. doi: 10.1016/j.ajodo.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 9.Battagel J. M, Kotecha B. Dental side-effects of mandibular advancement splint wear in patients who snore. Clin Otolaryngol. 2005;30:149–156. doi: 10.1111/j.1365-2273.2004.00944.x. [DOI] [PubMed] [Google Scholar]
- 10.Bondemark L, Lindman R. Craniomandibular status and function in patients with habitual snoring and obstructive sleep apnoea after nocturnal treatment with a mandibular advancement splint: a 2-year follow-up. Eur J Orthod. 2000;22:53–60. doi: 10.1093/ejo/22.1.53. [DOI] [PubMed] [Google Scholar]
- 11.Fransson A. M, Tegelberg A, Johansson A, Wenneberg B. Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop. 2004;126:687–693. doi: 10.1016/j.ajodo.2003.10.040. [DOI] [PubMed] [Google Scholar]
- 12.Fritsch K. M, Iseli A, Russi E. W, Bloch K. E. Side effects of mandibular advancement devices for sleep apnea treatment. Am J Respir Crit Care Med. 2001;164:813–818. doi: 10.1164/ajrccm.164.5.2003078. [DOI] [PubMed] [Google Scholar]
- 13.Hammond R. J, Gotsopoulos H, Shen G, Petocz P, Cistulli P. A, Darendeliler M. A. A follow-up study of dental and skeletal changes associated with mandibular advancement splint use in obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2007;132:806–814. doi: 10.1016/j.ajodo.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 14.Marklund M, Franklin K. A, Persson M. Orthodontic side-effects of mandibular advancement devices during treatment of snoring and sleep apnoea. Eur J Orthod. 2001;23:135–144. doi: 10.1093/ejo/23.2.135. [DOI] [PubMed] [Google Scholar]
- 15.Pantin C. C, Hillman D. R, Tennant M. Dental side effects of an oral device to treat snoring and obstructive sleep apnea. Sleep. 1999;22:237–240. doi: 10.1093/sleep/22.2.237. [DOI] [PubMed] [Google Scholar]
- 16.Rose E. C, Staats R, Virchow C, Jr, Jonas I. E. Occlusal and skeletal effects of an oral appliance in the treatment of obstructive sleep apnea. Chest. 2002;122:871–877. doi: 10.1378/chest.122.3.871. [DOI] [PubMed] [Google Scholar]
- 17.Marklund M. Predictors of long-term orthodontic side effects from mandibular advancement devices in patients with snoring and obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2006;129:214–221. doi: 10.1016/j.ajodo.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Partinen M, Gislason T. Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res. 1995;4:150–155. doi: 10.1111/j.1365-2869.1995.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 19.Ueda H, Almeida F. R, Lowe A. A, Ruse N. D. Changes in occlusal contact area during oral appliance therapy assessed on study models. Angle Orthod. 2008;78:866–872. doi: 10.2319/100107-470.1. [DOI] [PubMed] [Google Scholar]
- 20.Ghazal A, Jonas I. E, Rose E. C. Dental side effects of mandibular advancement appliances—a 2-year follow-up. J Orofac Orthop. 2008;69:437–447. doi: 10.1007/s00056-008-0811-9. [DOI] [PubMed] [Google Scholar]
- 21.Robertson C, Herbison P, Harkness M. Dental and occlusal changes during mandibular advancement splint therapy in sleep disordered patients. Eur J Orthod. 2003;25:371–376. doi: 10.1093/ejo/25.4.371. [DOI] [PubMed] [Google Scholar]
- 22.Lagravere M. O, Flores-Mir C. The treatment effects of Invisalign orthodontic aligners: a systematic review. J Am Dent Assoc. 2005;136:1724–1729. doi: 10.14219/jada.archive.2005.0117. [DOI] [PubMed] [Google Scholar]