Abstract
Objective:
To identify factors associated with patient satisfaction at least 5 years after orthodontic treatment.
Materials and Methods:
A total of 209 orthodontic patients were included in the study. All subjects were treated with upper and lower fixed orthodontic appliances. Dental casts (n = 627) were examined using the Peer Assessment Rating (PAR) Index pretreatment (T1), at the end of treatment (T2) and at a long-term follow-up (mean, 8.5 years; T3). At T3, a Dental Impact on Daily Living questionnaire was used to assess the long-term effects of orthodontic treatment on daily living and satisfaction with the dentition. Multiple regression analyses were used to quantify associations between patient satisfaction and changes produced by the orthodontic treatment (PAR T2-T1), posttreatment stability (PAR T3), age at the start of treatment (T1), treatment duration (T2-T1), gender, and extraction.
Results:
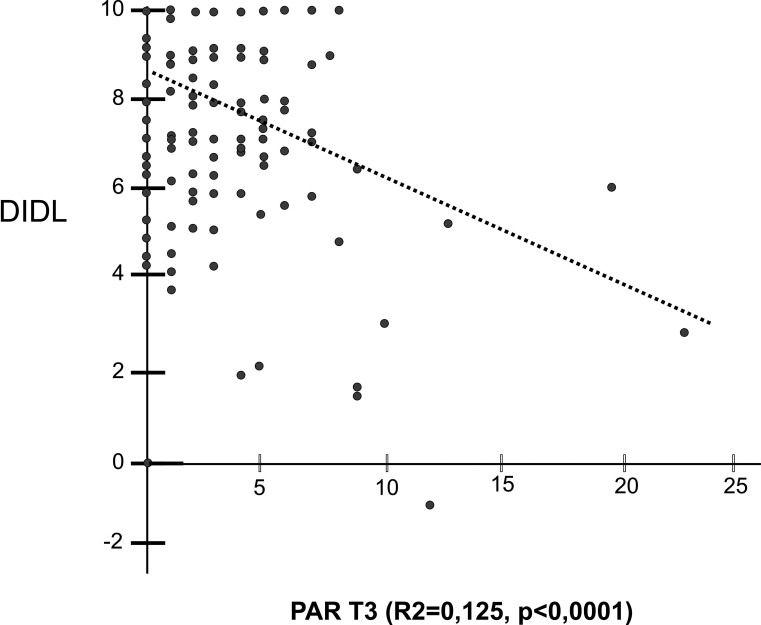
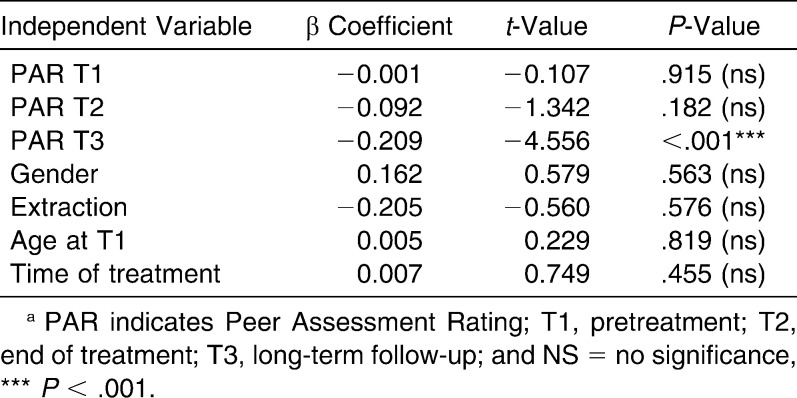
Orthodontic treatment produced a significant improvement of 94.2% in the PAR Index (T2-T1), but this change was not associated with the level of satisfaction when the patient was questioned at least 5 years after treatment. Regression analysis showed that satisfaction was significantly associated only with the long-term posttreatment PAR index (r2 = 0.125, P < .0001). No significant association was observed with the severity of malocclusion at the beginning (PAR-T1) or end of the orthodontic treatment (PAR-T2), age at T1, the amount of time taken during orthodontic treatment, gender, or extraction.
Conclusions:
Over the long term, patient satisfaction is slightly associated with the stability of the orthodontic treatment regardless of the initial occlusal condition or the final result of the orthodontic treatment.
Keywords: Long-term stability, Patient satisfaction, Orthodontic treatment
INTRODUCTION
The final goal of orthodontic treatment is to obtain normal or ideal occlusion. Follow-up studies of treated cases have shown that although “ideal” occlusion and dental alignment have been achieved, there is a tendency for posttreatment relapse toward the original malocclusion.1–5 The quality and stability of orthodontic treatment outcomes have traditionally been assessed by established metrics or categorical scales. As health services exist primarily to benefit the patient, an important variable for measuring outcome should be overall patient satisfaction with the care provided. Patient satisfaction with orthodontic treatment is poorly covered in the literature.
Satisfaction with dental appearance has been correlated with age and sex in individuals who have not received orthodontic treatment. It has been reported that satisfaction with dentofacial appearance decreases with age.6,7 Therefore, adults are expected to be less satisfied with their dentofacial appearance than are adolescents. Females are more dissatisfied with the appearance of their dentition than are males.8–10
Investigations of patient satisfaction after orthodontic treatment have shown a wide range of satisfaction levels, ranging from 34%11 to 74–75%.12,13 Birkeland et al.14 recorded a high degree of satisfaction (95.4%) with orthodontic treatment results among children. In addition to the countless variables that could interfere with patient satisfaction, the use of different questionnaires to assess satisfaction after orthodontic treatment makes comparison difficult.11 The level of satisfaction of orthodontic patients has been examined just after the end of treatment. Some factors have been reported as predictors of patient satisfaction at this time. Personality traits were found to be correlated with patients' satisfaction with their dentition after orthodontic treatment. In orthodontically treated patients, higher neuroticism scores were associated with lower levels of satisfaction with the dentition.11 Patients treated with nonextraction showed more dissatisfaction with their dentition, while age, sex, and pretreatment orthodontic treatment need had no relationship to patient satisfaction.11
A systematic review15 regarding the long-term stability of orthodontic treatment and patient satisfaction concluded that only a few studies have been conducted on long-term patient satisfaction; furthermore, most of these studies showed little scientific evidence, and no conclusions could be drawn. This review concluded that there is a great need for studies in this area.
MATERIALS AND METHODS
The sample (n = 209) was selected from a total of 4102 Angle Class I or II patients treated in a private clinic with more than 5 years of postorthodontic treatment. Posttreatment time ranged from 5 years to 25 years, with a mean of 8.5 years (standard deviation [SD] = 3.4 years). Subjects with facial anomalies and mental disorders, Class III patients, and those submitted to orthognathic surgery were excluded. The research protocol was submitted to the research ethics committee of the Federal University of Rio Grande do Norte and was approved under No. 110/2005.
Sample size was calculated from a pilot study involving the first 20 consecutive cases. The minimum regression coefficient (r2) was found to be 0.2, having a SD of 2 and an α level of 5% in a two-tailed model with a power of 80%. The estimated sample size was 194 individuals. Initially, 400 patients who still lived in town and who met the inclusion criteria were randomly called by phone. The response rate and attendance at the clinic was 62% (n = 248). Thirty-nine patients refused to make new orthodontic records.
A total of 88 Class I and 121 Class II malocclusions were examined (n = 209); these numbers included 70 males and 139 females. All of these patients were treated with straight-wire full appliances. Thirty patients (14.4%) had undergone tooth extractions for orthodontic reasons. Class II molar relationships were corrected through headgear or functional appliances, according to the mandibular deficiency. The mean ages were 14.3 years (range, 8.6–42.9 years) at pretreatment (T1), 16.2 years (range, 10.8–44.1 years) at the end of treatment (T2), and 24.9 years (range, 17.9–59.2 years) at long-term follow-up (T3).
The Dental Impact on Daily Living (DIDL) Index was used to assess the degree of satisfaction. The DIDL questionnaire comprises five major categories and tackles five major dimensions of dental satisfaction, namely appearance, pain, oral comfort, general performance, and chewing and eating. The DIDL scale measures the effect and the proportional importance of each dimension to the patient. The scale yields a score ranging from 0 to 10 to show the relative importance of each dimension to the patient. The DIDL questionnaire is a reliable, valid, and comprehensive test for measuring patient satisfaction and the effects of dental disease on patient daily life.16 Orthodontic problems can affect many aspects of dental esthetics and function, and these aspects are well covered by the DIDL Index.11 The DIDL was collected using a questionnaire at T3 (at least 5 years posttreatment).
To determine occlusal changes during and after orthodontic treatment, the Peer Assessment Rating (PAR) Index17 was used. This index was developed to provide a single score for all of the occlusal changes. Morphologic occlusion examinations were performed on the dental casts (n = 627) of 209 subjects at three periods in time: T1, T2, and T3 (mean 8.5 years).
Multiple regression analysis (at P < .05) was used to assess the association between the primary variable, satisfaction, and the following independent variables: PAR Index at T1, T2, and T3; age at the start of treatment (T1); gender; orthodontic extraction; and duration of treatment (T2 − T1).
The dental cast examination to collect PAR Index data was performed by one previously calibrated orthodontist. Intraexaminer reliability was assessed using the Intraclass Correlation Coefficient at P < .05.
RESULTS
The intraclass coefficient for the intraexaminer was 0.91. This result indicates an excellent reproducibility of the method. By considering the initial PAR Index at T1 to be 100% (median = 17), the changes produced after orthodontic treatment led to a mean improvement of 94.2% in this index (T2). Detailed information about the PAR findings can be obtained in a previous article.5
Patient satisfaction regarding dental occlusion at least 5 years posttreatment (T3) was examined by the DIDL Index with regard to the five major dimensions of dental satisfaction, namely appearance, pain, oral comfort, general performance, and chewing and eating. This revealed that 162 subjects (77.5%) reported being satisfied with their dentition, while 46 individuals (22%) were relatively satisfied. Only one individual (0.5%) reported being unsatisfied with his occlusion. The value of the level of satisfaction reported by this individual was −1.05, while the PAR Index at T1 was 17, and at T2 the level of satisfaction was reduced to 12. Nine years after treatment (T3) the PAR Index remained at 12.
With regard to predictive variables, only the PAR Index at T3 showed a significant relationship with patient satisfaction (P < .001). Figure 1 shows that the higher the PAR Index at T3, the lower the patient's satisfaction. However, the PAR Index at T3 only explained 12.5% of the variation in the DIDL Index (r2 = 0.125). The other variables, such as PAR at T1 (P = .91), PAR at T2 (P = .18), age at beginning of treatment (P = .86), duration of treatment (P = .41), extraction (P = .58), and gender (P = .56), showed no significant association with the dependent variable satisfaction (Table 1).
Figure 1.
T3 PAR Index correlation with DIDL Index.
Table 1.
Multiple Regression Analysis: Dependent Variable, Satisfaction—Dental Impact on Daily Living (DIDL) Index, F = 5.267 (P = .0001)a
DISCUSSION
This study showed that patients reported a high degree of satisfaction with their dentition in a long-term follow-up after orthodontic treatment. Around 77% of the patients reported being satisfied with their dentition when they were questioned at least 5 years after the end of treatment. Orthodontically treated patients demonstrated high levels of satisfaction with their teeth in general. This might be due to the fact that orthodontic treatment can affect dental performance positively, which can lead to higher levels of satisfaction. The changes produced after orthodontic treatment in this sample led to a mean improvement of 94.2% (PAR T2 − T1). Compared to previous studies,18,19 this finding can be considered a high standard of excellence in orthodontic finishing. There is a possibility that although some degree of dissatisfaction may be reported years after orthodontic treatment this level may be considerably more than it was at the beginning of treatment and less than at the end of the treatment. This cannot be determined from the collected data, and a longitudinal evaluation of patient satisfaction should be performed.
Although the use of different questionnaires to assess satisfaction makes comparisons difficult, investigations of patient satisfaction after orthodontic treatment have shown a wide range of satisfaction levels, ranging from 34%11 to 95%.14 We used the same satisfaction questionnaire employed by Al-Omiri and Alhaija.11 These authors reported 34% satisfied and 62% relatively satisfied patients just after orthodontic treatment, while the percentage of dissatisfied patients was 4%. Given the differences in the timing during which the questionnaires were applied (immediately after treatment and long term) comparisons with previous results are difficult, because countless factors can be associated with these differences.
Predictive factors related to patient satisfaction are controversial in the literature. A small number of studies have examined this issue. Untreated patients have reported that satisfaction with dentofacial appearance decreases with age,6,7 and females are more dissatisfied with the appearance of their dentition than are males.8–10 Our results showed that gender, age, and duration of treatment were not related to patient satisfaction. The lack of a relationship between gender and patient satisfaction seems to be a common outcome for patients who have received orthodontic treatment.11,12 Al-Omiri and Alhaija11 found that satisfaction with the dentition after orthodontic treatment showed no relationship to age.
No association was observed between patient satisfaction and extraction for orthodontic reason in the present study. A previous study11 reported that patients treated with nonextraction showed more dissatisfaction with their dentition when the patient was examined immediately after orthodontic treatment. It is possible that the diagnostic criteria for tooth extraction and its impact on dentofacial morphology are more relevant than the procedure itself.
Among the predictive factors investigated in this study, the only one able to produce any prediction of long-term patient satisfaction was the PAR Index at T3 (Figure 1). However, this variable explains only 12.5% of variations in the DIDL Index. Thus, patient satisfaction is not related to the improvement produced by the orthodontic treatment (PAR T1 and T2) when the patient is asked some years after the orthodontic treatment. A previous investigation14 showed that orthodontic treatment outcome (PAR T2) is related to 20% of the variability of children's opinion of psychosocial benefits. The results of this study show that a few years after orthodontic treatment this feeling of benefit appears to be lost. Thus, for patients, the current status of the dentition is more relevant than the benefits obtained just after orthodontic treatment.
A previous investigation5 examining this sample showed that the use of a lower fixed retainer was one important factor related to treatment stability (PAR T3) as well as the time of use of the Hawley upper retainer. Therefore, the use of orthodontic retention can contribute to a higher level of satisfaction in patients who have undergone orthodontic treatment. Since patient satisfaction were slightly associated with orthodontic variables and higher neuroticism scores were associated with lower levels of satisfaction with the dentition,11 further investigations are necessary in order to meet a wider range of factors able to predict patient satisfaction.
CONCLUSIONS
From a long-term perspective, patient satisfaction is slightly associated with stability of the orthodontic treatment, regardless of the initial occlusal condition or the final result of the orthodontic treatment.
Neither gender, age, extraction for orthodontic reasons, nor the amount of treatment time has a significant relationship with long-term patient satisfaction.
REFERENCES
- 1.McNamara J. A, Jr, Baccetti T, Franchi L, Herberger T. A. Rapid maxillary expansion followed by fixed appliances: a long-term evaluation of changes in arch dimensions. Angle Orthod. 2003;73:344–353. doi: 10.1043/0003-3219(2003)073<0344:RMEFBF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Little R. M, Riedel R. A, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–428. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 3.McReynolds D. C, Little R. M. Mandibular second premolar extraction—postretention evaluation of stability and relapse. Angle Orthod. 1991;61:133–144. doi: 10.1043/0003-3219(1991)061<0133:MSPEPE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Al Yami E. A, Kuijpers-Jagtman A. M, van't Hof M. A. Stability of orthodontic treatment outcome: follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999;115:300–304. doi: 10.1016/s0889-5406(99)70333-1. [DOI] [PubMed] [Google Scholar]
- 5.Maia N. G, Normando A. D. C, Feitosa M. S, Ferreira M. A, Maia F. A. Factors associated to orthodontic stability—a longitudinal retrospective study of 209 patients. World J Orthod. 2010;11:61–66. [PubMed] [Google Scholar]
- 6.Shaw W. C. Factors influencing the desire for orthodontic treatment. Eur J Orthod. 1981;3:151–162. doi: 10.1093/ejo/3.3.151. [DOI] [PubMed] [Google Scholar]
- 7.Cunningham S. J, Gilthorpe M. S, Hunt N. P. Are orthognathic patients different? Eur J Orthod. 2000;22:195–202. doi: 10.1093/ejo/22.2.195. [DOI] [PubMed] [Google Scholar]
- 8.Sheats R. D, McGorray S. P, Keeling S. D, Wheeler T. T, King G. J. Occlusal traits and perception of orthodontic need in eighth grade students. Angle Orthod. 1998;68:107–114. doi: 10.1043/0003-3219(1998)068<0107:OTAPOO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Gosney M. B. E. An investigation into some of the factors influencing the desire for orthodontic treatment. Br J Orthod. 1986;13:87–94. doi: 10.1179/bjo.13.2.87. [DOI] [PubMed] [Google Scholar]
- 10.Wheeler T. T, McGorray S. P, Yurkiewicz L, Keeling S. D, King G. J. Orthodontic treatment demand and need in third and fourth grade school children. Am J Orthod Dentofacial Orthop. 1994;106:22–23. doi: 10.1016/S0889-5406(94)70017-6. [DOI] [PubMed] [Google Scholar]
- 11.Al-Omiri M. K, Abu Alhaija E. S. Factors affecting patient satisfaction after orthodontic treatment. Angle Orthod. 2006;76:422–431. doi: 10.1043/0003-3219(2006)076[0422:FAPSAO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Larsson B. W, Bergsröm K. Adolescents' perception of the quality of orthodontic treatment. Scand J Caring Sci. 2005;19:95–101. doi: 10.1111/j.1471-6712.2005.00325.x. [DOI] [PubMed] [Google Scholar]
- 13.Anderson L. E, Arruda A, Inglehart M. R. Adolescent patients' treatment motivation and satisfaction with orthodontic treatment. Do possible selves matter? Angle Orthod. 2009;79:821–827. doi: 10.2319/120708-613.1. [DOI] [PubMed] [Google Scholar]
- 14.Birkeland K, Bøe O. E, Wisth P. J. Relationship between occlusion and satisfaction with dental appearance in orthodontically treated and untreated groups. A longitudinal study. Eur J Orthod. 2000;22:509–518. doi: 10.1093/ejo/22.5.509. [DOI] [PubMed] [Google Scholar]
- 15.Bondemark L, Holm A, Hansen K, Axelsson S, Mohlin B, Brattstrom V, Paulin G, Pietila T. Long-term stability of orthodontic treatment and patient satisfaction. Angle Orthod. 2007;77:181–191. doi: 10.2319/011006-16R.1. [DOI] [PubMed] [Google Scholar]
- 16.Leao A. The Development of Measures of Dental Impacts on Daily Living [PhD thesis] London, UK: London University; 1993. [Google Scholar]
- 17.Richmond S, Shaw W. C, O'Brien K. D, Buchanan I. B, Jones R, Stephens C. D. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 18.Birkeland K, Furevik J, Boe O. E, Wisth P. J. Evaluation of treatment and posttreatment changes by the PAR Index. Eur J Orthod. 1997;19:279–288. doi: 10.1093/ejo/19.3.279. [DOI] [PubMed] [Google Scholar]
- 19.Wood M, Lee D, Crawford E. Finishing occlusion, degree of stability and the PAR Index. Aust Orthod J. 2000;16:9–15. [PubMed] [Google Scholar]