Summary:
Glomus tumors are painful, benign tumors that develop from the glomus bodies. They account for less than 1% of tumors in hand, and less than 10% present in the pulp of the digits. Cold hypersensitivity, increased pinprick sensitivity, and paroxysmal pain are common glomus tumor symptoms. We describe a 27-year-old man who came with pain in the right little digit, confined to the pulp for 10 years. The tip of the finger was extremely sensitive to touch, and the pain worsened in a cold atmosphere. Upon palpation, no mass was recognized. There was pinpoint tenderness within the distal volar pulp of the little finger. MRI with a contrast of the right little digit showed a 2-mm enhancing lesion in the tip of the little finger. An incision was done over the volar plane of the little finger, removing the tumor bluntly. The tumor was found to be a glomus tumor after histologic evaluation. Glomus tumors of the volar pulp are notoriously hard to detect. Hence, the presence of localized pain in the volar tip for the finger should raise suspicion of the diagnosis of a glomus tumor, and surgical removal should be offered to relieve symptoms and avoid recurrence.
Glomus tumors are benign, vascular neoplasms that make about 1%–5% of all soft tissue tumors in the hand.1 Studies have reported glomus tumors on the digit in different locations such as subungual, paraungual, palmar-radial, palmar-ulnar, and pulp.1 There is no difference in the incidence of glomus tumors between women and men. However, subungual glomus tumors are most seen in women.2 Cold hypersensitivity, paroxysmal pain, and localized discomfort are the typical triad of symptoms associated with glomus tumors.1 A previous case study of a volar pulp location of a glomus tumor in an elderly patient has been mentioned in the literature.3 Hence, this case report describes an unusual, but not unique, location of the pulp glomus tumor of the little finger and a review of the literature.
CASE PRESENTATION
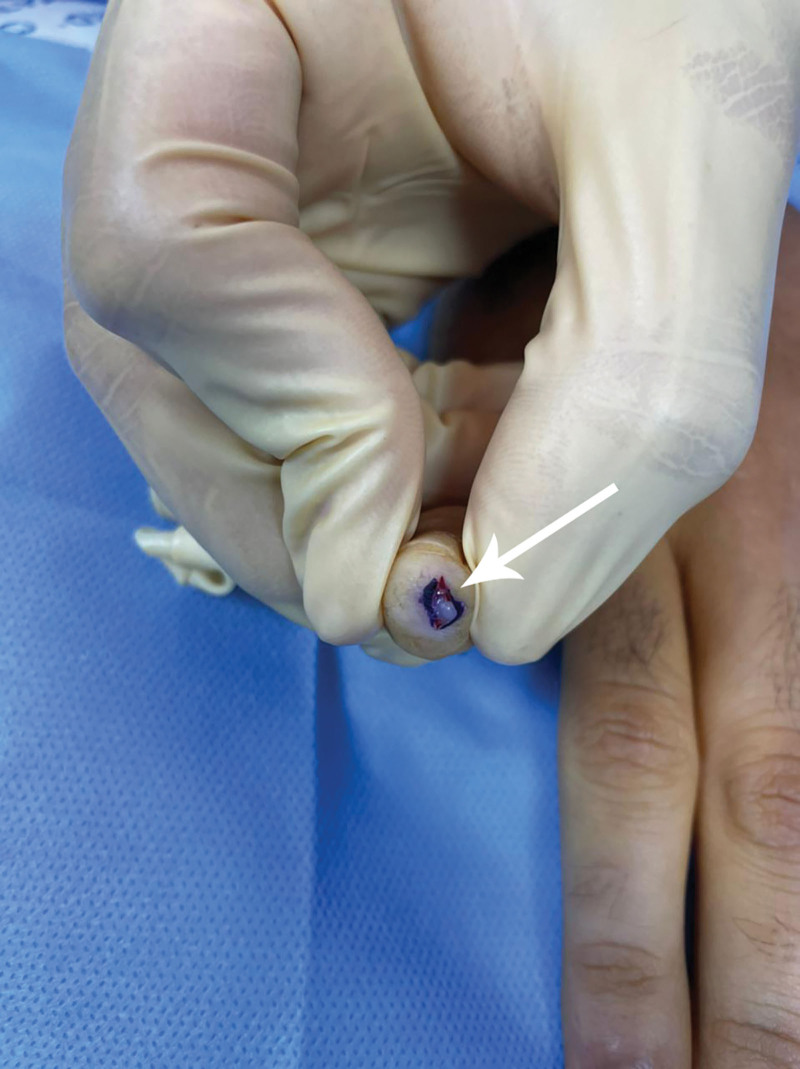
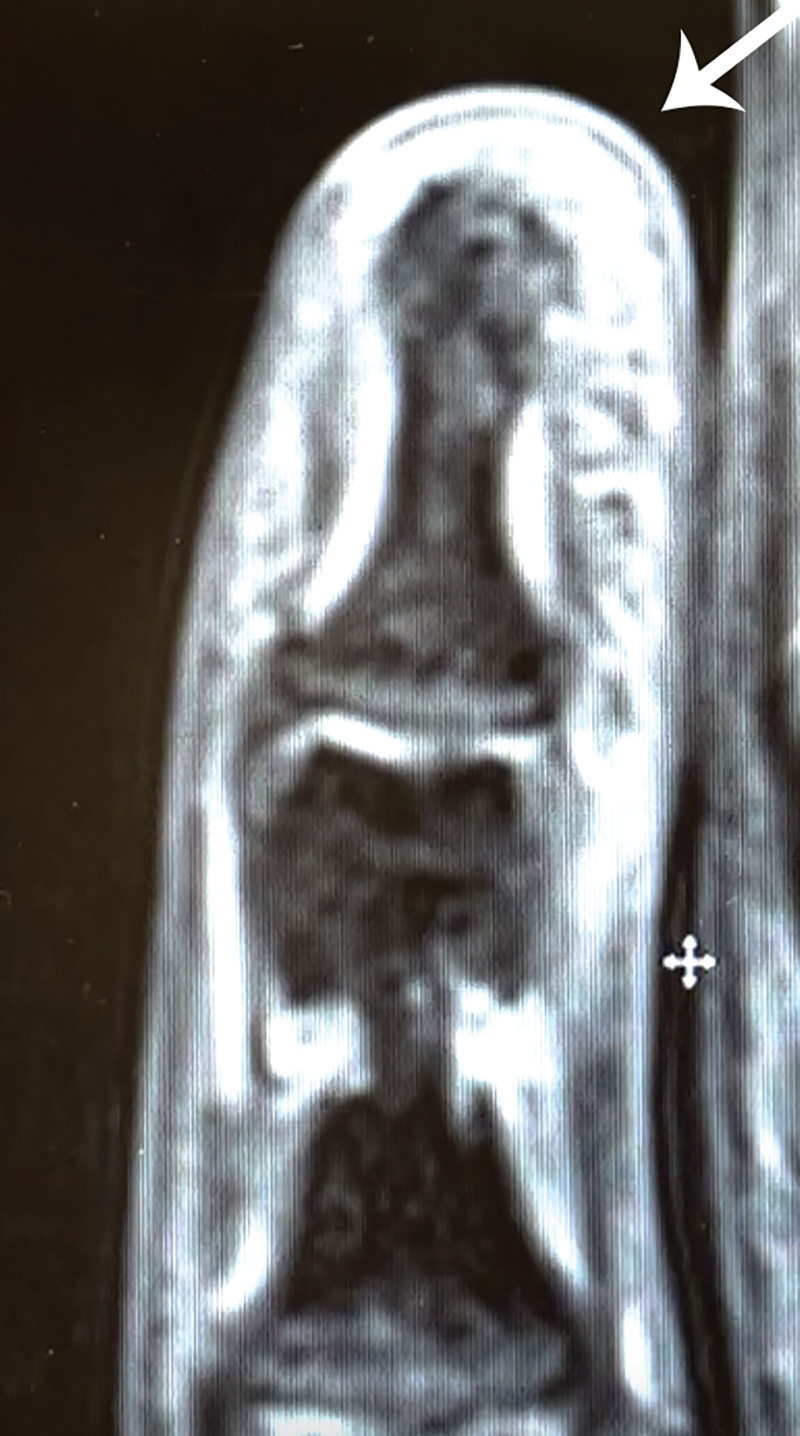
We describe a 27-year-old, right-handed man, not known to have any chronic medical conditions. He complained of recurrent, on and off discomfort on the ulnar aspect of the pulp of the right little finger, for 10 years. The patient also complained of cold hypersensitivity and that direct pressure causes severe pain in the same region. He denied any pertinent medical or family history. There was no history of trauma or injury. During the physical examination, a normal-appearing little finger with a complete range of motion and no neurological abnormalities was discovered. There were no physical findings (no visible masses or skin changes). There was pinpoint tenderness over the painful digit. No mass was palpable. Magnetic resonance imaging (MRI) with contrast showed a lesion within the tip of the little finger measuring 2 mm, showing T1 low signal, T2 high signal with postcontrast enhancement (Fig. 1). The mass was excised through a 1 cm volar incision centered over the maximum tenderness point (Fig. 2). A small lesion was noticed volar to the distal part of the little finger. After meticulous dissection to avoid causing harm to the nearby structures, complete removal was accomplished.
Fig. 1.
A contrast enhanced MRI revealed a round 2-mm soft tissue lesion in the volar ulnar aspect of the distal little finger. There was no bone invasion, and the rest of the soft tissue was normal.
Fig. 2.
An intraoperative image of the lesion after the 1-cm incision.
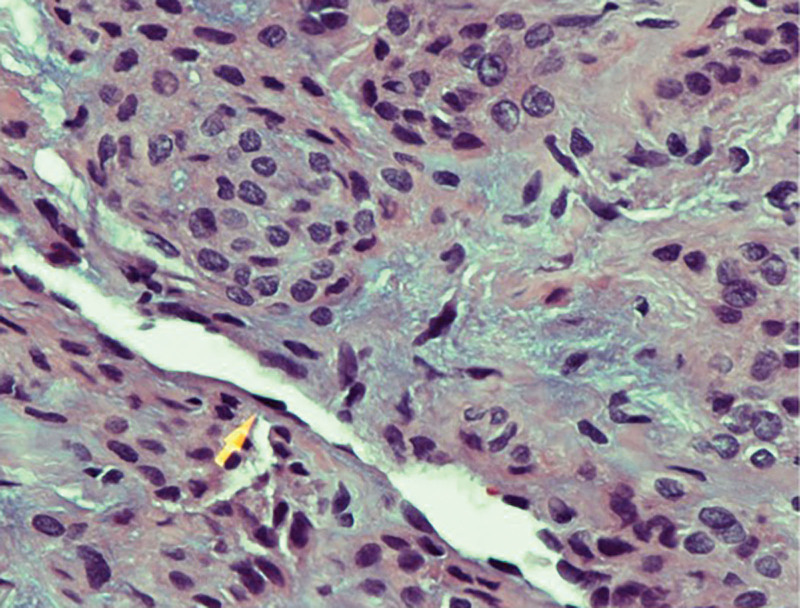
After the surgery, the pain was entirely resolved, and the pain was absent at the 6-month follow-up. The tumor was well-circumscribed, yellowish, and 2 mm in diameter. The discrete, pseudo-encapsulated lesion consisted of a sheet of homogenous, relatively small, round to ovoid cells (Fig. 3). The presence of tumoral smooth muscle actin in immunohistochemistry confirmed the diagnosis of a glomus tumor.
Fig. 3.
Histology findings. Photomicrograph showing clusters of oval-shaped perivascular glomus cells surrounding blood vessels (arrow). H/E stain X400. Photomicrograph showing clusters of oval-shaped perivascular glomus cells surrounding blood vessels. H/E stain X600.
DISCUSSION
Glomus tumors arise from the glomus body, a contractile neuromyoarterial that controls peripheral blood flow and temperature.1 The location of the glomus tumors can widely vary. The subungual region contains more glomus bodies; therefore, 75%–90% of glomus tumors arise there.1 In our case, the tumor’s location was on the distal pulp of the right little finger, which is an uncommon location of glomus tumors on the digits.
Table 1 summarizes the literature review on glomus tumors of the digits. Glomus tumors were most seen in middle-aged women. Moreover, Saaiq et al reported the largest size range of 2–11 mm.9 In our case, the tumor’s size was 2 mm. Glomus tumors of the digits tend to be smaller in diameter, rendering the diagnosis upon palpation only and resulting in symptoms and pain out of proportion. MRI is the most used modality due to its sensitivity in detecting glomus tumors. Therefore, when glomus tumors are suspected, MRI with contrast is encouraged.
Table 1.
Review of the Literature on Glomus Tumors on the Digit
| First Author | Study Type | Sample Size | Gender | Age (y) | Size (mm) | Duration of the Symptoms (y) | Location | Diagnosis | Complications | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Man | Woman | Recurrence | Nail Deformity | ||||||||
| Nazerani et al4 | Case series | 8 | 3 | 5 | 38.5 (25–58) | <6 (n = 7) 12 (n = 1) | — | Ulnar side (n = 3) Radial side (n = 5) | MRI and x-ray (n = 8) | n = 2 | n = 3 |
| Hamdi5 | Retrospective cohort | 8 | 3 | 5 | 40 (23–61) | 2–6 | 2.101–7 | Subungual (n = 6) Pulp (n = 2) | MRI and x-ray (n = 8) | n = 0 | n = 0 |
| Tomak et al6 | Case series | 14 | 4 | 10 | 46 (28–65) | 3–4 | 7.4 (0.8–25) | Subungual (n = 14) | X-ray (n = 14) | n = 2 | n = 3 |
| Fujioka et al7 | Case series | 4 | 2 | 2 | 29 (25–31) | — | 4.5 (0.6–10) | Subungual (n = 4) | MRI (n = 4) | n = 0 | n = 0 |
| Takata et al2 | Retrospective cohort | 30 | 7 | 23 | 42 (16–78) | — | 7.8 | Subungual (n = 30) | — | n = 2 | n = 5 |
| Bhaskaranand and Navadgi8 | Case series | 18 | 11 | 7 | 31 (16–51) | — | 1.9 (0.1–5) | Subungual (n = 7)Paraungual (n = 4)Palmar-radial (n = 1) Palmar–ulnar (n = 2) | X-ray (n = 2) MRI (n = 1) | n = 0 | n = 0 |
| Saaiq9 | Case series | 17 | 5 | 12 | 41.17 (27–62) | 2–11 | 1.6 (0.3–3) | Subungual (n = 14) Volar pulp (n = 3) | MRI (n = 17) | n = 0 | n = 0 |
| Lin et al10 | Retrospective cohort | 75 | 17 | 58 | Women 41.2 (15–75) Men 42.7 (26–71) |
2–8 | 3.9 | Nail matrix (n = 20) Nail bed (n = 29)Volar (n = 19) | X-ray (n = 15)US (n = 4)MRI (n = 2) MRI and x-ray (n = 8)US and x-ray (n = 1) | n = 13 | n = 0 |
Furthermore, studies about glomus tumors have noted a long duration of symptoms before the diagnosis is made. Bhaskaranand et al reported the lowest average duration of symptoms (1.9 years),8 and Takata et al reported the highest average duration of symptoms (7.8 years).2 In the case we presented, the patient complained of symptoms for 10 years.
Glomus tumor diagnosis mainly depends on the clinical presentation with the classic triad of symptoms: hypersensitivity to cold, paroxysmal pain, and localized tenderness.1 The classical triad was consistent with our patient, who complained of on and off finger pain, sensitivity to low temperature, and severe pain by direct pressure. Other symptoms may be present such as blue discoloration, nail deformity, and a palpable or visible mass.1,2
There are bedside tests that can help in the diagnosis. The first test is the love pin test, where pressure is applied to the suspected area with a pinhead. The area in which the glomus tumor is located will be in intense pain. The second test, Hildreth’s test, applies a tourniquet on the arm to induce transient ischemia resulting in the withdrawal of pain, attributed to the temporary restriction of the blood supply. The third test is the cold sensitivity test, where an ice cube is placed over the affected area.4 Imaging modalities such as x-ray, ultrasound, and MRI can be used to confirm the diagnosis and identify the anatomical location before surgical excision.10 On examination, our patient’s love test was positive, and MRI showed a 2 mm nodular lesion.
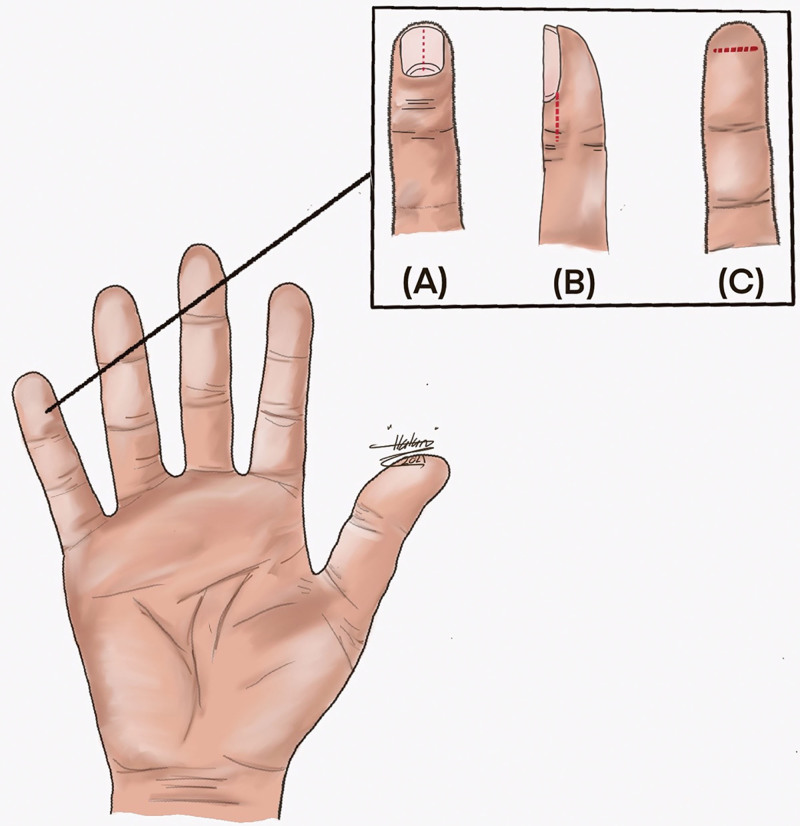
The definitive treatment of a glomus tumor is surgical excision, and the surgical approach depends mainly on the tumor’s location. Figure 4 shows various techniques of surgical approach for glomus tumor excision in the digit. The total excision of the glomus tumor is curative. However, incomplete excision can cause the recurrence of the tumor.10 Apart from recurrence, studies have reported nail deformity as a complication, contributing to the surgical approach chosen and nail bed involvement.2,4,6 Our patient had a complete resection of the tumor, and postoperatively the pain was resolved. At the follow-up, the patient denied any pain, and no deformity was noted. This case report might not be a unique presentation for a glomus tumor. However, we are aiming to add to the current literature regarding this rare condition.
Fig. 4.
Different methods of surgical approach for digital glomus tumor excision. A, Transungal method. B, Lateral subperiosteal method. C, Volar method.
CONCLUSIONS
We describe a glomus tumor that developed in an unusual location on the volar pulp of the little finger, causing long-term pain and sensitivity to touch for 10 years. Because of the ambiguous symptoms, glomus tumors are challenging to identify without precise tests. The deep and peculiar placement of the mass exhibited here rendered the diagnosis of the mass’s identity ambiguous. The existence of localized pain in the fingertip, on the other hand, was a reason to consider a glomus tumor in the differential diagnosis to avoid unnecessary therapeutic delays.
Footnotes
Published online 17 March 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972;54:691–703. [PubMed] [Google Scholar]
- 2.Takata H, Ikuta Y, Ishida O, et al. Treatment of subungual glomus tumour. Hand Surg. 2001;6:25–27. [DOI] [PubMed] [Google Scholar]
- 3.Rosner IA, Argenta AE, Washington KM. Unusual volar pulp location of glomus tumor. Plast Reconstr Surg Glob Open. 2017;5:e1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nazerani S, Motamedi MH, Keramati MR. Diagnosis and management of glomus tumors of the hand. Tech Hand Up Extrem Surg. 2010;14:8–13. [DOI] [PubMed] [Google Scholar]
- 5.Hamdi MF. Glomus tumour of fingertip: report of eight cases and literature review. Musculoskelet Surg. 2011;95:237–240. [DOI] [PubMed] [Google Scholar]
- 6.Tomak Y, Akcay I, Dabak N, et al. Subungual glomus tumours of the hand: diagnosis and treatment of 14 cases. Scand J Plast Reconstr Surg Hand Surg. 2003;37:121–124. [DOI] [PubMed] [Google Scholar]
- 7.Fujioka H, Kokubu T, Akisue T, et al. Treatment of subungual glomus tumor. Kobe J Med Sci. 2009;55:E1–E4. [PubMed] [Google Scholar]
- 8.Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br. 2002;27:229–231. [DOI] [PubMed] [Google Scholar]
- 9.Saaiq M. Presentation and management outcome of glomus tumors of the hand. Arch Bone Jt Surg. 2021;9:312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin YC, Hsiao PF, Wu YH, et al. Recurrent digital glomus tumor: analysis of 75 cases. Dermatol Surg. 2010;36:1396–1400. [DOI] [PubMed] [Google Scholar]