SUMMARY
The SARS-CoV-2 pandemic has affected in the last two years a large number of subjects, with a high cost in terms of morbidity and mortality. The scientific community made progress in understanding risk factors, pathophysiology, clinical manifestations, diagnosis and treatment of acute SARS-CoV-2 infection. In the last months, another condition has become evident and caught the attention of the scientific community: the so-called long COVID syndrome. The pathophysiology of this condition is not known, even if some hypothesis have been made but not demonstrated yet. Long COVID is characterized by a very heterogeneous group of subacute and/or chronic symptoms and signs that follow the acute phase of SARS-CoV-2 infection and have a very variable duration. The presence of this syndrome in an individual is not dependent from the severity of the acute SARS-CoV-2 infection. Because of the extreme clinical heterogeneity, and also due to the lack of a shared and specific definition of the disease, it is very difficult to know the real prevalence and incidence of this condition. Some risk factors for the development of the disease have been identified: advanced age, elevated body mass index, comorbidities, specific symptoms of acute COVID-19 (in particular dyspnea), number of symptoms in the acute phase and female sex.
The number of individuals affected by long COVID is high, even if it occurs only in a part of the subjects who had COVID-19. Therefore, long COVID constitutes now a major health issue and has to be managed in order to ensure an adequate access to care for all the people that need it.
“Post COVID” clinics have been created in various countries, especially in Europe, for the management of people affected by long COVID syndrome. Guidelines have been written to help clinicians. An important role in the management of long COVID patients is played by the general practitioner, directly or indirectly linked to post COVID hospital clinics. The extreme heterogeneity of clinical presentation needs a patient-tailored, multidisciplinary approach. As NHS guidelines say, the three principal of care for long COVID patients are personalized care, multidisciplinary support and rehabilitation.
More studies are needed in order to know better the pathophysiology of the disease. It is also necessary to create standardized and shared definitions of the disease, in order to better understand the epidemiology, the diagnostic criteria and to offer the right treatment to all the individuals who need it, without social or economic diffeences.
Keywords: Long COVID, post COVID, follow up, COVID-19, SARS-CoV-2
INTRODUCTION
The mechanisms leading to the persistence of symptoms in the absence of chronicization of the infection, in COVID-19, have not been clarified yet. From a pathogenetic point of view, it has not been convincingly demonstrated that SARS-CoV-2 infection can become chronic. The set of symptoms reported by numerous patients with previous COVID-19, at a variable distance from the acute infection and when the virus is no longer found in respiratory secretions, fall within the scope of post-viral syndromes. These type of syndromes have been studied in the infectious field especially months after Epstein Barr Virus and Cytomegalo virus infections, viruses which however integrate into the genetic heritage of target cells.
Another debated issue is the classification of “long COVID”. This definition has been used in multiple ways across the literature. Greenhalgh et al. use the terms ‘post-acute COVID-19’ (from 3 to 12 weeks) and ‘chronic COVID-19’ for symptoms extending beyond 12 weeks [1]. NICE elaborated a case definition at three levels [2]:
Acute COVID-19: signs and symptoms of COVID-19 for up to 4 weeks.
Ongoing symptomatic COVID-19: signs and symptoms of COVID-19 from 4 weeks up to 12 weeks.
Post COVID-19 syndrome: signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis.
In addition to the clinical case definitions, the term ‘long COVID’ is commonly used to describe signs and symptoms that continue or develop after acute COVID-19. It includes both ongoing symptomatic COVID-19 (from 4 to 12 weeks) and post COVID-19 syndrome (12 weeks or more) of the NICE classification [2].
We conducted a narrative review with the help of the literature regarding the essential aspects of the problem, with particular reference to the epidemiological, clinical and therapeutic data currently available. For this purpose, we analyzed the available papers in PubMed and the principal Guidelines written about these topics.
EPIDEMIOLOGY
The lack of a shared and specific definition of long COVID syndrome makes it difficult to estimate its incidence and prevalence; according to some studies, the development of long COVID does not depend on the severity of the disease and the duration of symptoms COVID-related [3].
The onset of the syndrome is independent from hospitalization for COVID-19, although it is more frequent in the court of hospitalized patents. The studies show variable results. According to some authors, in the non-hospitalized population, 1 in 5 subjects reports symptoms compatible with long COVID (eg. asthenia, cough and headache) 5 weeks after the initial infection [4]. For other studies, the percentage of subjects not hospitalized for COVID19 reporting symptoms compatible with Long-COVID syndrome is variable: from 2% of patients 12 weeks after symptoms onset, to 35% 3 weeks after testing and 52% 10 weeks after the onset of symptoms [3–8]. Regarding the patients hospitalized for COVID-19, a percentage varying between 32,6% and 87% reports persistence of symptoms for 60 days after discharge [9–11]. The symptoms most frequently described, in order of frequency, are asthenia, dyspnea, arthralgia and chest pain. Long COVID symptoms seems particularly frequent in patients admitted in intensive care unit. Also the paediatric population can develop long COVID syndrome. According to the scientific literature, a percentage between 4% and 66% has persistence of symptoms between 4 and 20 weeks after acute infection [12]. In conclusion, it is currently very difficult to estimate the population affected by long COVID syndrome, both in the court of patients hospitalized for COVID-19 and in the court of patients not hospitalized. The studies conducted are very heterogeneous in terms of diagnostic definition, population, timing and type of follow-up.
PHYSIOPATHOLOGY
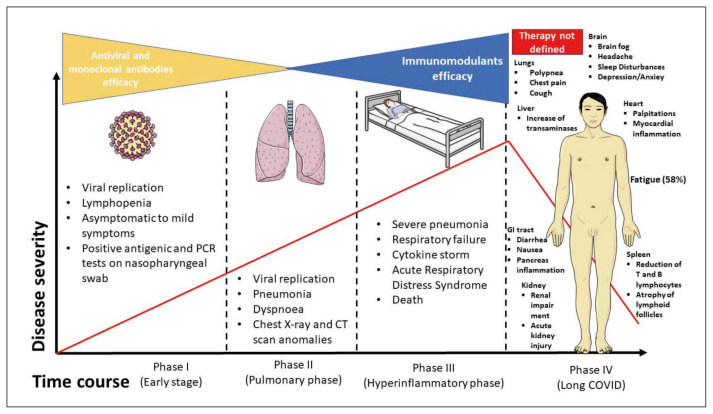
The physiopathology of acute SARS-CoV2 has been studied and identified, but the exact reasons that lead to the persistence of symptoms has to be known yet (Figure 1). Some mechanisms have been proposed:
Figure 1.
COVID-19 phases. Three phases has been described in COVID-19 pathophysiology. Phase 1, called “early stage”, which has a predominant viral replication; it is typically asymptomatic or paucysymptomatic and is highly contagious. Phase 2, called “pulmonary” phase, characterized by lung viral replication and beginning of possible radiological findings; phase 3 or “hyperinflammatory phase” in which prevails the action of immune system ruled by the “cytokine storm”. Recently a fourth phase is being described namely “long COVID” depicted by subacute to chronic conditions and multiorgan involvement.
Sequelae of organ damage, extent of injury and time to recovery of each organ system [13].
Persistence of chronic inflammation or autoantibody generation [14, 15].
Persistence of virus into the body in people with altered immunity, re-infection or relapse [16].
Effect of hospitalization, complications related to SARS-Cov2 infection or complications related to co-morbidities or adverse effects of medications used [17, 18].
Deconditioning, psychological issues like post-traumatic stress [19, 20].
The social and financial impact of COVID-19 also contributes to post COVID issues including psychological ones [7].
Persistently elevated inflammatory markers could indicate chronic persistence of inflammation [7]. However, multiple mechanisms may contribute to the onset of long COVID [7].
SYMPTOMS
Researchers identified two main patterns of symptoms in people with long COVID. The first pattern includes symptoms like fatigue, headache and upper respiratory complaints (shortness of breath, sore throat, persistent cough and loss of smell). The second one includes systemic manifestations like fever and gastroenterological symptoms [7].
Generalized symptoms
The most common symptom is severe fatigue. This can be associated to other manifestations like cervical and axillary lymphadenomegaly, headache, myalgia and arthromyalgia, sore throat, hoarseness and unrefreshing sleep. Raman et al. reported a fatigue frequency of 55% using the Fatigue Severity Scale [21]. Other commonly reported problems are worsened quality of life (44.1%), chest pain (21.7%), skin rashes, alopecia, palpitations, loss of smell and taste, anorexia, abdominal pain and diarrhea [7].
Respiratory system
The two most common symptoms are shortness of breath and dyspnea. In the study of Weerahandi et al. 74.3% of patients undergoing mechanical ventilation manifest this type of symptoms. In this population, pulmonary fibrosis sequelae (PFS) are also common due to the parenchymal stress produced by mechanical ventilation [22]. Other radiological abnormalities like bronchiectasis, pulmonary micronodules and pulmonary vascular disease are still evident at radiological instrumental exams performed 2 to 3 month post-discharge [7].
Nervous system
The emergence of the COVID-19 pandemic has raised many questions around the effects of SARS-CoV-2 on mental health [23]. The increase in incidence of COVID-19 has been associated with an increase in prevalence of major depressive disorder and anxiety disorder. For both disorders, females are affected more than males, and younger age groups are affected more than older ones. In addition, in patients that have been affected by COVID the prevalence of fatigue and generalized symptoms are higher than in the healthy population [7]. Patel V. et al. found that during the COVID-19 pandemic the suicide rate increased [23]. The researchers report other nervous symptoms such as post-traumatic stress disorder following severe illness, difficulty concentrating, worsening of cognitive decline and insomnia/sleep disturbance. Other symptoms like headache, “brain fog”, vertigo, tremor and paraesthesia are also described. Some authors even report the Guillain-Barré syndrome as a rare but possible complication of long COVID [24].
Cardiovascular system
The postural orthostatic tachycardia syndrome (POTS) is the most common manifestation [25]. POTS is an autonomic disorder lasting for 6 months or more, diagnosed by an increased heart rate of > 30 beats per minute within 5–10 min of standing or upright tilt without orthostatic hypotension. This increase in heart rate can cause dizziness, palpitations, blurred vision, headache, generalized weakness, exercise intolerance, etc. [25]. The possible etiologies include dysautonomia, hypovolemia, hyperadrenergic stimulation, even psychological stress. Most of these clinical manifestations involve female subjects and are not associated with the severity of acute SARS-CoV2 infection [25]. Less common cardiovascular manifestations (usually related to already present comorbidities) are myocardial infarction, myocarditis, pericarditis, arrhythmias, cardiac failure and venous thromboembolism.
DIAGNOSIS
The diagnosis of long COVID is clinical and requires a holistic and person-centered approach, as well as multidisciplinary care [3, 26, 27]. Some authors have identified risk factors that can lead to the persistence of symptoms after acute infection, like older age, severity of acute phase (keeping in mind that “long COVID” is different from “post-ICU syndrome”), obesity, female sex, comorbidities, asthma and more than five symptoms in acute phase [3, 28, 29]. Even subjects without these risk factors, however, can develop long COVID, and long COVID isn’t always related to the severity of acute illness [3]. Long COVID symptoms overlap with symptoms of other diseases. To date, long COVID is therefore diagnosed when the symptoms presented do not have other medical explanations [2, 3, 26].
The diagnostic workout of the patient suffering from long COVID includes a thorough clinical history: information about acute COVID-19 (suspected or confirmed), the nature and severity of previous and current symptoms, timing and duration of symptoms since the start of acute COVID-19, history of other health conditions, exacerbation of pre-existing conditions [2, 28]. It is important to discriminate which symptoms really need more diagnostic studies, remembering that some patients can develop psychological problems caused by unnecessary investigations. It is useful to refer to specialized centers patients with suspicion of specific diseases or with disabling symptoms, especially psychiatric ones. It is important to consider possible overlapping with post-traumatic stress syndrome.
We report below the diagnostic exams suggested by the majority of studies and guidelines, that should be carried out in the post COVID clinics and services [2, 26, 27, 29]:
– blood exams (full blood count, kidney and liver function tests, C-reactive protein, ferritin, BNP, HbA1c and thyroid function tests);
– exercise tolerance tests: evaluate case-by-case risk benefit ratio (e.g. patients with already known cardio-pulmonary disease);
– lying and standing blood pressure recording;
– Chest X-ray by 12 weeks after acute COVID-19 if the person has continuing respiratory symptoms. Normal plain chest X-ray does not rule out lung disease.
Specific diagnostic tools or scores have not be assessed yet.
Physicians should be aware that symptoms are relapsing-remitting and can be absent at the moment of medical examination.
TREATMENT AND PATIENT MANAGEMENT
The long COVID and the nature of its symptoms, except the management of urgent conditions, lead to the need of a holistic assessment with an approach focused on self-management and rehabilitation (in NHS guidelines, the three principal of care for long COVID patients are personalized care, multidisciplinary support and rehabilitation, supporting and enabling self care) [2]. In the last year, post COVID dedicated clinics and outpatient services have been created, especially in Europe, in order to take care of individuals affected by long COVID. The clinician leading the long COVID dedicated services should be a medical doctor with relevant skills and experience, in order to deliver personalized care and ways to self-manage the symptoms and collaborate with the appropriate specialist support [30]. Beside these services, Authors consider the self-management care an important issue. A possible start point for the patient is keeping a record of his goals, setting on realistic ones, and of any recovery and changes in symptoms to plan a patient-based rehabilitation [2].
A multidisciplinary team should tailor support and rehabilitation for the specific patient, including physical, psychological and psychiatric aspects of management, and plan how often follow up and monitoring are needed, which healthcare professionals should be involved and whether appointments should be carried out in person or remotely [2, 30]. The team should include experts in treating fatigue, respiratory and other symptoms (breathlessness, de-conditioning, dizziness), in occupational therapy and physiotherapy, in clinical psychology and psychiatry and rehabilitation medicine [2]. Speech and language therapists should support the rehabilitation of individuals who manifested common clinical presentations of post COVID syndrome, including cognitive disorders (for example brain fog), swallowing, voice (included muscle tension dysphonia) and respiratory difficulties. It is important to give the chance to re-enter rehabilitation services after being discharged if symptoms worsen [2].
In post COVID clinics, the same healthcare professional or team should provide continuity of care, as much as possible. Support groups, social prescribing, online forums and apps, as the reference clinician, could offer a source of advice and support. Support should be offered to people about the return to education or work, suggesting for example a phased return. For older people or people with complex needs, additional support should be considered [2, 30].
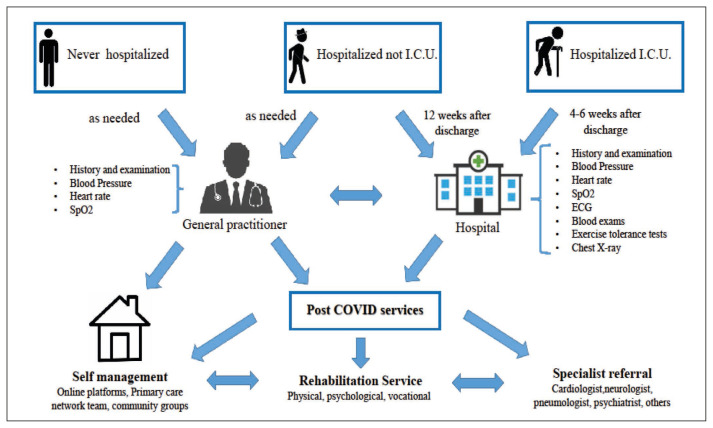
NHS guidelines propose 3 pathways for the management of long COVID patients, depending on the severity of the acute infection and on whether the patient has been hospitalized [31]:
– People never admitted to hospital with their acute illness, but managed independently or in the community: in this case, the general practitioner is the figure who conducts the holistic assessment of the patient and plays a connection role between the patient and the post COVID services if there is the need of further evaluation. This group of patients should have the possibility to access the post COVID services like hospitalized ones, if needed [31].
– People who needed hospitalization for COVID-19 should undergo a 12-week post discharge assessment, which include a chest X-ray, review of symptoms and consideration of further investigations and rehabilitation requirements, if the X-ray chest results abnormal or other medical invalidating issues continue. If the chest X-ray is normal and there are no more symptoms, the patient can be discharged with follow up in community as needed. Some people may need clinical evaluation before the scheduled 12 weeks. The timing is based on individual needs and is at the discretion of the assessing clinician. However, although recovery time is different for everyone, for many people symptoms will resolve by 12 weeks [31].
– The individuals cared for in an Intensive Care Unit (ICU) or High Dependency Unit setting should undergo a post ICU multidisciplinary clinic reassessment at 4–6 weeks post discharge. If continuing to improve, they should be followed as the other hospitalized ones [31] (Figure 2).
Figure 2.
Long COVID management. Patients affected by long COVID can be managed through three pathways, depending on the severity of the acute SARS-CoV-2 infection. The main figures that lead the management of the patients are the general practitioner and the leading physician belonging to the health care centres where the patient has been hospitalized. If needed (abnormal radiological exams or persistence of symptoms after acute infections), the patient accesses the post COVID services where a specific patient-tailored treatment is offered.
The frequency and duration of follow up is currently not defined [2].
There is paucity of evidence about when to return to normal activities. This decision should be patient-tailored, according to the subject occupation and activities [24]. Some potential risks, including cardiac, pulmonary, and psychiatric, along with the patient’s pre-illness baseline physical status and activities, have to be considered. Salman et al recommended waiting at least a week after being asymptomatic to resume exercise. Moreover, the first 2 weeks of exercise should be minimal exertion, with gradual progression. The self-monitoring of the signs/symptoms and mood using a diary is highly recommended in all steps [32].
Specific conditions: Pharmacological and rehabilitation treatment
Minor symptoms (cough, pain, myalgia): symptomatic treatment with paracetamol, cough suppressants and oral antibiotics (if secondary bacterial infection is suspected). Kratum (Mytragina speciosa) has been proposed for patients with contraindications for non-steroidal anti-inflammatory drugs [24]. Chest physiotherapy and neuro rehabilitation are important in patients with pulmonary and neuromuscular sequelae. Worsening of underlying co-morbidities like diabetes, hypertension and cardiovascular illness may occur in people after SARS-CoV-2 infection, requiring optimization of treatment [29].
Pulmonary symptoms: NICE recommends a multidisciplinary approach [2]. Breathlessness can be investigated with an exercise tolerance test (oneminute sit and stand test or 6 minutes walking test). If patient has respiratory symptoms after 12 weeks from acute infections, a chest x ray can be useful [2]. Mayo clinic suggest the elimination of factors that can exacerbate dyspnea (smoking, pollutants, extreme temperatures, exercise) [33]. Non-pharmacological strategies include also breathing exercises, pulmonary rehabilitation, and postural relief [29].
Cardiovascular symptoms: Exercise tolerance tests for heart rate measuring, while blood pressure and heart rate while standing and lying can be measured if POTS is suspected [2]. ESC recommends beta-blockers for tachycardia, others suggest ivabradin for cardiovascular manifestation of long COVID [2, 34]. Myocarditis usually resolves over time, but supportive or immunomodulating drugs can accelerate recovery in some cases [33]. Some authors have also suggested the use of anticoagulants to face the risk connected to the ongoing inflammation [35].
Fatigue, cognitive and neuropsychiatric disorders: NICE recommends self management and support to manage chronic fatigue, because no specific pharmacologic treatment exists [2]. Cognitive behavioral treatment and graded exercise treatment have been suggested [36], but evidences are lacking. Another possible treatment strategy for fatigue is pacing (patient manages tasks and activities in order to avoid overexertion and exacerbating fatigue) [37].
Group therapy and supportive listening are other useful strategies. Cognitive impairment can be assessed through screening tools. If present, the patient should be offered services like occupational, speech and language therapist. Medications can be considered (methylphenidate, donepezil, modafinil) [29]. Sleep disturbance, post-traumatic stress disorder, depression, anxiety, and other mental health problems have to be managed according to specific guidelines.
Emerging treatments: some trials are ongoing in order to assess the efficacy of iperbaric oxygen, montelukast, deupirfenidone, breath exercise and singing to treat respiratory symptoms of long COVID. Vitamin C through in vein administration, nicotinamide to treat chronic fatigue, probiotic supplement to treat gastrointestinal symptoms, leronlimab, tocilizumab, melatonin to reduce the proinflammatory trigger, and other adjiuvant therapies are on study [29].
CONCLUSIONS
Long COVID is a relatively new medical condition. More studies are needed in order to better understand the pathophysiology, the symptoms and the correct management of the patients. According to the last two years experience and to the scientific literature, a holistic, multidisciplinary and patient centered approach is the best way to take care of patients affected by this condition.
Footnotes
Conflict of interest
None of the authors have conflict of interest.
Funding
No funding was received for the preparation of the manuscript.
REFERENCES
- 1.Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute COVID-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN), Royal College of General Practitioners (RCGP) COVID-19 rapid guideline: managing the long-term effects of COVID-19. NICE. 2022;1:13. [Google Scholar]
- 3.European Observatory on Health Systems and Policies. Rajan S, Khunti K, et al. In the wake of the pandemic: preparing for Long COVID. World Health Organization Regional Office for Europe. 2021:1997–8073. [PubMed] [Google Scholar]
- 4.Office for National Statistics. Updated estimates of the prevalence of long COVID symptoms. Office for National Statistics; 2021. p. 12788. [Google Scholar]
- 5.Sudre CH, Murray B, Varsavsky T, Graham MS, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the COVID Symptoms Study App. medRxiv. 2020:20214494. [Google Scholar]
- 6.Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network - United States, March–June 2020. Morb Mortal Wkly Rep. 2020;69(30):993–8. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: An overview. Diabetes Metab Syndr. 2021;15(3):869–75. doi: 10.1016/j.dsx.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Townsend L, Dyer AH, Jones K, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One. 2020;15(11):e0240784. doi: 10.1371/journal.pone.0240784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chopra V, Flanders SA, O’Malley M, Malani AN, Prescott HC. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med. 2021;174(4):576–8. doi: 10.7326/M20-5661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carf A, Bernabei R, Landi F Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–5. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmermann P, Pittet LF, Curtis N. How common is long COVID in children and adolescent? Pediatr Infect Dis J. 2021;40(12):e482–e7. doi: 10.1097/INF.0000000000003328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11(1):16144. doi: 10.1038/s41598-021-95565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colafrancesco S, Alessandri C, Conti F, Priori R. COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? Autoimmun Rev. 2020;19(7):102573. doi: 10.1016/j.autrev.2020.102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–74. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biehl M, Sese D. Post-intensive care syndrome and COVID-19 implications post pandemic. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc055. [DOI] [PubMed] [Google Scholar]
- 18.Gemelli Against COVID-19 Post-Acute Care Study Group. Post-COVID-19 global health strategies: the need for an interdisciplinary approach. Aging Clin Exp Res. 2020;32(8):1613–20. doi: 10.1007/s40520-020-01616-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.G, Favieri F, Tambelli R, Casagrande M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Environ Res Public Health. 2020;17(11):4151. doi: 10.3390/ijerph17114151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiang H, Nan J, Lv Z, Yang J. Psychological impacts of the COVID-19 epidemic on Chinese people: exposure, post-traumatic stress symptom, and emotion regulation. Asian Pac J Trop Med. 2020;13:252–9. [Google Scholar]
- 21.Writing Committee for the COMEBAC Study Group. Morin L, Savale L, et al. Four-month clinical status of cohort of patients after hospitalization for COVID-19. JAMA. 2021;325(15):1525–34. doi: 10.1001/jama.2021.3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weerahandi H, Hochman KA, Simon E, et al. Post-discharge health status and symptoms in patients with severe COVID-19. J Gen Intern Med. 2021;36(3):738–45. doi: 10.1007/s11606-020-06338-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel JA, Nielsen FBH, Badiani AA, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020;183:110–1. doi: 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akbarialiabad H, Taghrir MH, Abdollahi A, et al. Long COVID, a comprehensive systematic scoping review. Infection. 2021;49(6):1163–86. doi: 10.1007/s15010-021-01666-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shin JY, Shiliang L. Proposed sybtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev Med Virol. 2021:e2315.. doi: 10.1002/rmv.2315. [DOI] [PubMed] [Google Scholar]
- 26.National Health Service. Guidelines for supporting our NHS people affected by Long COVID. NHS. 2022 Version 1. [Google Scholar]
- 27.Nurek M, Rayner C, Freyer A, et al. Recommendations for the recognition, diagnosis, and management of long COVID: a Delphi study. Br J Gen Pract. 2021;71(712):e815–e25. doi: 10.3399/BJGP.2021.0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The Royal Australian College of General Practitioners. Caring for patients with post-COVID-19 conditions. East Melbourne, Vic: RACGP; 2021. [Google Scholar]
- 29.Crook H, Raza S, Nowell J, Young M, Edison P. Long COVID-mechanisms, risk factors, and management. BMJ. 2021;374:n1648. doi: 10.1136/bmj.n1648. [DOI] [PubMed] [Google Scholar]
- 30.Istituto Superiore di Sanità. Indicazioni ad interim sui principi di gestione del Long-COVID. Rapporto ISS COVID-19. 20212021 [Google Scholar]
- 31.National Health Service. National guidance for post-COVID syndrome assessment clinics. NHS; 2021. Version 2. [Google Scholar]
- 32.Salman D, Vishnubala D, Le Feuvre P, et al. Returning to physical activity after COVID-19. BMJ. 2021;372:m4721. doi: 10.1136/bmj.m4721. [DOI] [PubMed] [Google Scholar]
- 33.Sinagra G, Anzini M, Pereira NL, et al. Myocarditis in clinical practice. Mayo Clin Proc. 2016;91(9):1256–66. doi: 10.1016/j.mayocp.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 34.European Society of Cardiology. ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic. ESC; 2020. [Google Scholar]
- 35.Onishi A, Ange KSt, Dordick JS, Linhardt RJ. Heparin and anticoagulation. Front Biosci (Landmark Ed) 2016;21:1372–92. doi: 10.2741/4462. [DOI] [PubMed] [Google Scholar]
- 36.Adamson J, Ali S, Santhouse A, Wessely S, Chalder T. Cognitive behavioural therapy for chronic fatigue and chronic fatigue syndrome: outcomes from a specialist clinic in the UK. J R Soc Med. 2020;113(10):394–402. doi: 10.1177/0141076820951545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torjesen I. NICE cautions using graded exercise therapy for patients recovering from COVID-19. BMJ. 2020;370:m2912. doi: 10.1136/bmj.m2912. [DOI] [PubMed] [Google Scholar]