Abstract
Background:
Peripheral arterial disease (PAD) remains underdiagnosed, partly because of the limitations of the Doppler ankle-brachial index (ABI) with regards to equipment, training, and time constraints.
Aims:
To compare the accuracy and validity of automated oscillometric ABI measurement in detecting PAD in primary care settings against a gold standard Doppler device.
Settings and Design:
A cross-sectional observational study was conducted at the physiology department, Dr. Ram Manohar Lohia Institute of Medical Sciences (DrRMLIMS), Lucknow.
Methods and Material:
A total of 200 male building construction workers of all types of age groups between 20 and 40 years were recruited. The ABI measurement was performed using the Watch BP Office and hand-held HI.dop, BT-200 Vascular Doppler device.
Statistical Analysis Used:
The Bland-Altman plot and receiver operator characteristics (ROC) curve were determined to analyze the agreement between the two methods. For the reliability of the test, Pearson’s correlation with linear regression was done and the intraclass correlation (ICC) coefficient was calculated.
Results:
The mean ABI (Osc) and ABI (Dop) were 1.13 ± 0.09 and 1.06 ± 0.08, respectively. The ABI (Dop) and ABI (Osc) methods were highly correlated Pearson’s correlation coefficient of 0.96 with 95% confidence interval (CI) ranges between 0.985 and 1.066 (P < 0.001). On linear regression analysis, the ABI (Dop) predicted ABI (Osc) 92.6% correctly. The paired mean difference between the two measuring devices was 0.07 (95% CI = −0.03 to −0.12). At 0.90 cut-off value of diagnosing PAD, the sensitivity is 50%, specificity 100%, positive predictive value 100%, and negative predictive value 97% by an oscillometric automated device.
Conclusion:
Our finding suggested that ABI measurement by the automated oscillometric device is reliable, free of examiner bias, and less time-consuming.
Keywords: Ankle-brachial index, automated oscillometric device, peripheral arterial disease
Introduction
Atherosclerosis is the major reason for cardiovascular-related deaths in today’s community. The disease is usually asymptomatic in an early stage. Screening for peripheral artery disease (PAD) is usually made by non-invasive measurement of the ankle-brachial index (ABI).[1,2] The ABI is the ratio of the systolic blood pressure at the ankle compared with the brachial artery pressure. When the ABI is ≤0.9, a diagnosis of PAD is made up of 90% accuracy.[3] Doppler-assisted measurement of ABI is the accepted non-invasive gold standard for diagnosing PAD, and therefore, the assessment of disease severity. However, the ABI measurement should require a degree of experience that has precluded its widespread adoption in medical care so far. Moreover, the amount of time required to perform Doppler-assisted ABI measurements was found to be a drawback for widespread office-based applications.[4,5] The ABI measured by the automated oscillometric device is a simple and reproducible method that has become popular since it surpasses the limitations of the Doppler with regard to equipment, training, and time constraints.[6] The purpose of the present study is to validate oscillometric ABI measurement by assessing and comparing the results with the current gold standard of Doppler-assisted measurement of ABI in a high-risk population such as building construction workers.
Material and Methods
Study design: This was a cross-sectional observational study conducted in the Department of Physiology of our institute, Lucknow, Uttar Pradesh, India. The approval of the Institute Ethics Committee for human studies was obtained before the commencement of the work.
Participants: A total of 200 male building construction workers of all types (cement masons, concrete finishers, segmental pavers, brick masons, stonemasons, tapers, tile installers) of age group between 20 and 40 years were recruited from an ongoing academic building construction of DrRMLIMS, Lucknow. The participants with major amputation in the upper and lower limbs, open wounds or ulcerations in the lower limbs, and marked edema of one and both feet were excluded from the study. We obtained informed written consent from each participant who agreed to participate in the study. By using a suitable sample estimation formula, 200 building construction workers were enrolled for the present study.
Parameters measured: All the participants were asked to report in the clinical lab, Department of Physiology, DrRMLIMS, and the following parameters were recorded. The anthropometric parameters such as height (cm) and weight (kg) were measured, and body mass index was calculated as the ratio of weight (kg) to height squared (m2). A history of tobacco chewing and smoking was also taken.
Measurement of Blood Pressure: The subjects sat quietly with their backs supported without crossing their legs and with both arms supported at the heart level for 5 min. The brachial blood pressure was measured for both the arms using an automated oscillometric device (Watch BP Office, Widnau, Switzerland) equipped with two cuffs for simultaneous double arm measurements, the cuff size was tailored to the arm of an individual according to their mid-arm circumference.[7] The cuffs were then comfortably set in place, adjusted to the arms at the same distance above the cubital malleolus with the cuffs directed toward the brachial artery trajectory on each side. The systolic and diastolic blood pressure (BP) was repeatedly measured after every 1 min interval. The average of the three measurements was used in the analysis.
Measurement of ABI: The ABI measurements were first performed by using an automated oscillometric device (Watch BP Office, Microlife, Widnau, Switzerland), and then, by a vascular Doppler device (HI.dop, BT-200 Vascular Doppler, Bistos Co. Ltd. Korea). All the participants were rested for 5 min before the measurement. Both Doppler measurements and automated oscillometric recordings were performed using appropriately sized cuffs. In the first procedure, the blood pressure was measured simultaneously on both arms followed by both ankles. The arm with the higher systolic blood pressure was selected for the ABI measurement. If both the arms had equal systolic blood pressure readings, then the right arm reading was chosen for ABI measurement.[8] Similarly, the ankle with a higher systolic blood pressure was selected for ABI measurement. The ABI was calculated by dividing the highest value obtained at each ankle by the highest of arm values. The brachial and posterior tibial systolic pressures were measured using appropriately sized blood pressure cuffs linked to a mercury sphygmomanometer placed successively on the upper arms and just above the ankles. Using a hand-held continuous wave Doppler probe (8 MHz, HI.dop, BT-200 Vascular Doppler, Bistos Co. Ltd. Korea), the systolic pressure in each artery was measured by inflating the cuffs 30 mmHg above the systolic blood pressure and deflated slowly until a flow signal was detected over the brachial and posterior tibial artery.[9] The ABI was calculated similarly to the first method. An index of less than or equal to 0.90 was regarded as being pathological.
Statistical Analysis: All the statistical analyses were performed using the statistical package for social sciences (SPSS) 20.0 and Medcalc 19.4 softwares. The continuous variables are expressed as mean ± standard deviation (SD). The association between ABI <=0.90 and various continuous parameters was done using the unpaired t-test for continuous variable and Fisher exact Chi-square was done for the qualitative variable. The Bland-Altman plot and receiver operator characteristics (ROC) curve were determined to analyze the agreement between the two methods. For reliability of the test, Pearson’s correlation with linear regression was done and intraclass correlation (ICC) coefficient was calculated. The diagnostic accuracy was assessed via sensitivity, specificity, positive productive value, and negative productive value with the ABI readings dichotomized (ABI ≤0 9). The P value <0.05 was considered significant.
Results
The participants’ characteristics are shown in Table 1. The mean age and BMI of the participants were 27.53 ± 4.06 years and 23.46 ± 2.04 kg/m2, respectively. Their mean right and left arm systolic and diastolic blood pressure was 130.13 ± 8.34, 79.30 ± 8.37 mmHg and 128.01 ± 8.23, 78.20 ± 8.32 mmHg, respectively. The mean interarm systolic blood pressure difference was 3.67 ± 2.56 mmHg and out of the 200 participants, 9 subjects were inter-arm difference in systolic blood pressure (IDSBP) >10 mmHg. The mean ABI (Osc) and ABI (Dop) were 1.13 ± 0.09 and 1.06 ± 0.08, respectively.
Table 1.
Details of the participants
| Parameter | Mean | ±SD |
|---|---|---|
| Age (years) | 27.53 | 4.06 |
| BMI (kg/m2) | 23.46 | 2.04 |
| Right arm systolic blood pressure | 130.13 | 8.34 |
| Right arm diastolic blood pressure | 79.30 | 8.37 |
| Left arm systolic blood pressure | 128.01 | 8.23 |
| Left arm diastolic blood pressure | 78.20 | 8.32 |
| Interarm systolic BP difference (IDSBP) | 3.67 | 2.56 |
| ABI (Osc) | 1.13 | 0.09 |
| ABI (Dop) | 1.06 | 0.08 |
Reliability between Doppler ABI and Oscillometric ABI: The ABI (Dop) and ABI (Osc) methods were highly correlated Pearson’s correlation coefficient of 0.96 with 95% CI ranges between 0.985 and 1.066 (P < 0.001). On linear regression analysis, the ABI (Dop) predicted ABI (Osc) 92.6% correctly [Figure. 1] The reliability of ABI (Osc) was measured by intraclass correlation by average measure, the agreement between both the measures was extremely high with ICC of 0.98 with 95% CI ranges between 0.973 and.985 and it was statistically significant (P < 0.001).
Figure 1.
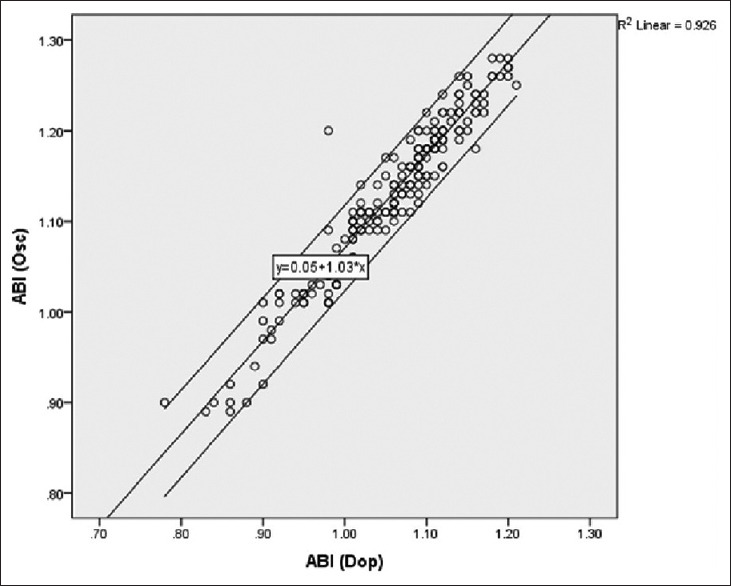
A scattered plot illustrate high correlation with R = 0.92 between oscillometric and Doppler determination of ABI
Level of agreement between the two methods: The Bland-Altman plot for assessing the agreement of the two methods for all 200 participants is shown in Figure 2. The paired mean difference between the two measuring devices was 0.07 (95% CI = −0.03 to 0.12). The comparison showed a good level of agreement between the two methods.
Figure 2.
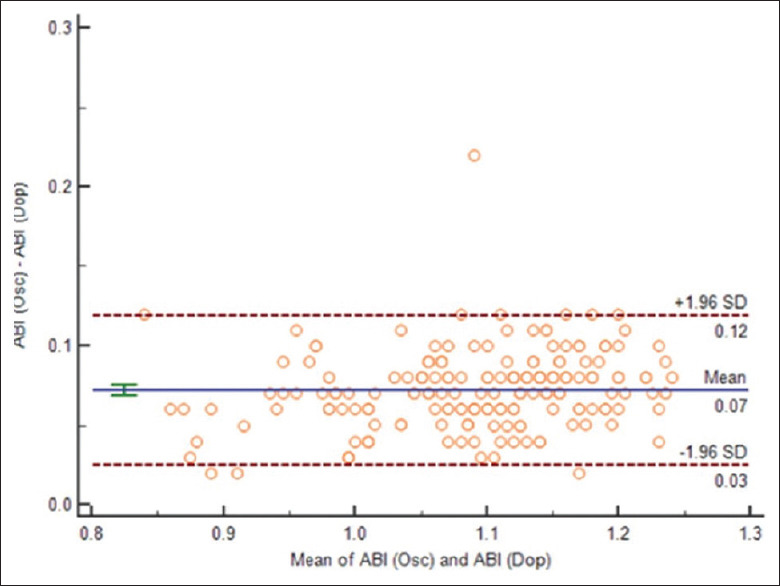
Bland-Altman plot reveals high level of agreement between average and difference of the means of Doppler ABI and Oscillometric ABI measurements
Diagnostic Accuracy: Considering the Doppler method of ABI calculation as the gold standard, there were 188 true negatives, 6 true positives, 6 false negatives, and 0 false positive in 200 participants. At 0.90 cut-off value of diagnosing PAD, the sensitivity was 50%, specificity 100%, positive predictive value 100%, and negative predictive value 97% by the oscillometric automated device. The area under the ROC curve was 0.98 (95% CI = 0.96–1.0) [Figure 3].
Figure 3.
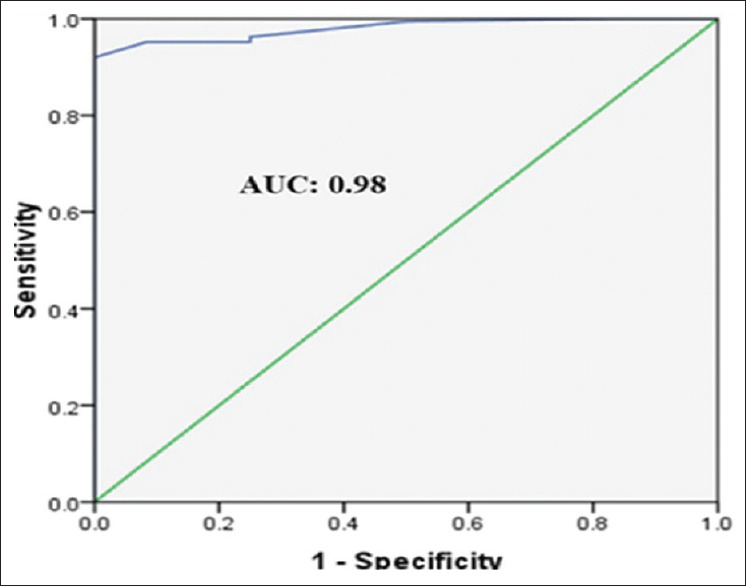
Receiver operating characteristic (ROC) curve analysis of diagnosing of Normal blood flow in arteries and ABI (Osc)
There was a statistically significant correlation between BMI >25 kg/m2, IDSBP >10 mmHg, and smoking habit with ABI value <0.9 in both the ABI (Osc) and ABI (Dop) methods. In our study, age was not significantly associated with ABI value <0.9 [Tables 2 and 3].
Table 2.
Association of smoking habit with ABI<=0.9 with both methods of ABI calculation
| ABI (OSC) | P | ABI (DOP) | P | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| <=0.90 | >.90 | <=0.90 | >.90 | |||
| Smoking | ||||||
| Yes | 6 | 94 | <0.03 | 11 | 89 | <0.006 |
| No | 0 | 100 | 1 | 99 | ||
Table 3.
Association of different variables with ABI<=0.9 with both methods of ABI calculation
| Variables | ABI (OSC) | P | ABI (DOP) | P | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| <=0.90 | >.90 | <=0.90 | >.90 | |||
| Age Mean (SD) | 29.16 (3.31) | 27.47 (4.08) | 0.316 | 28.50 (3.14) | 27.46 (4.11) | 0.39 |
| BMI Mean (SD) | 26.44 (0.68) | 23.36 (2.00) | <0.001 | 25.78 (1.11) | 23.30 (1.99) | <0.001 |
| IDSBP Mean (SD) | 10.83 (2.04) | 3.44 (2.23) | <0.001 | 10.167 (1.99) | 3.250 (1.96) | <0.001 |
Discussion
The recognition of PAD is the most common factor in reducing the burden of cardiovascular disease because it requires specialized equipment, training, and time. These constraints limit the use of Doppler ABI measurement in general outpatient departments and offices. So, a simple, faster, and accurate method is the need of the hour to facilitate the diagnosis and screening of PAD in the outpatient departments (OPDs) and office settings.[3] We suggest and validate the use of an automated oscillometric blood pressure monitoring device in the practice of primary care physicians for the measurement of ABI for screening as well as diagnosing PAD in the general population. The diagnosis of PAD is often missed during routine physical examination. Automated oscillometric devices are compatible with daily activities. They require the same amount of time as blood pressure measurements, and they can detect PAD in a percentage of patients who otherwise would have not been diagnosed. The systematic use of the automated oscillometric device in routine OPDs would even reduce the cost of the National Health Service, waiting lists, and inconvenience to the patients. The main findings of our study were that the correlation between the oscillometric and Doppler-assisted measurements was considerably good for all the subjects as these participants were not diagnosed cases of any cardiovascular disease. However, the sensitivity and specificity of our study were only 50 and 100% at ABI = 0.9 for the detection of PAD, respectively. This finding was due to the limited number of PAD cases detected in our study (12 by Doppler and 6 by the oscillometric method). If we consider a cut-off value of ABI = 0.89 and ABI = 0.91 for the detection of PAD, the sensitivity and specificity of our study improve to 100, 83.3%, and 75, 96.8%, respectively. In our study, the mean oscillometric value (1.13) was higher than the mean Doppler ABI value (1.06), which is consistent with various other studies. This difference might be explained due to the intrinsic differences in the blood pressure measurements between the two methods and also by the variation in the Doppler measurement due to the interexaminer differences.[10] The automated oscillometric system allows three simultaneous readings of the blood pressure measurement of both arms or both legs and takes an average reading of blood pressure for the calculation of ABI, and so it is free of observer bias. In contrast, Doppler measurements necessitate additional steps such as pulse auscultation, Doppler signal evaluation, and are performed successively and need interpretation by an observer, making them difficult and time-consuming for general practice.[4] The earlier studies have reported various results concerning the reliability of oscillometric ABI measurement over the Doppler ABI measurement method. A study by Kollias A on a total of 93 patients suffering from various cardiovascular diseases found a strong correlation between oscillometric and Doppler ABI with an intraclass correlation coefficient of the agreement as 0.98 and the ROC as 0.981, which is almost similar to the finding in our study. Their sensitivity and specificity were 83 and 97%, respectively, in diagnosing PAD. This difference in the sensitivity and specificity was may be due to the differences in the study group (diabetic and hypertensive vs. building construction workers without any cardiovascular disease).[11] Similarly, a study by Jing Ma on 230 diabetic patients found a good agreement between the two methods by Bland-Altman plot and area under the ROC curve as 0.98 with high sensitivity and specificity.[12] A study by Ichihashi S et al.[13] examining the diagnostic accuracy of oscillometric ABI for detecting PAD using computed tomography angiography (CTA) as a gold standard concludes that the oscillometric device has high diagnostic accuracy. A study by Sessa A et al.[14] in the year 2019 on the determination of ABI in 701 Type 2 diabetic patient with an automated oscillometric device by 24 general practitioners (GPs) and also receive Doppler ultrasound examination. The study concluded that the device was easy to use and it can be a useful instrument for the early diagnosis of PAD in daily practice. In a recent study by Hageman D et al.[15] in the year 2021, it was concluded that oscillometric ABI had excellent diagnostic accuracy with 74% sensitivity and 97% specificity compared with the Doppler ABI equipment. Similarly, other studies also found that oscillometric ABI measurement was a reliable and accurate method for screening and diagnosing PAD[16,17] whereas some other studies suggest that the reliability of oscillometric ABI values for PAD diagnosis is controversial as it is not able to detect PAD in the population at a high risk of cardiovascular disease, but it can be used as a screening tool for PAD with caution.[18,19,20,21] Apart from validation between the two methods of measurement of ABI, we also had seen a correlation between different established risk factors for PAD with ABI value <=0.9. We found a statistically significant correlation between BMI >25 kg/m2, inter-arm difference in systolic blood pressure (IDSBP) >10 mmHg, and smoking with ABI value <=0.9, and this finding is similar in both the methods of ABI measurement. The interarm blood pressure difference of more than 10 mmHg and smoking are regarded as simple markers for coronary artery disease (CAD) and PAD.[22,23] Although age is also an independent risk factor for PAD, in our study, it was significantly not correlated. In our study, we chose the younger age group compared to previous researches. The key points of our study are that automated oscillometric device can be used for screening as well as diagnostic purposes of PAD in the outpatient department for the general population as this method wins over the standard method due to its simplicity, automatic readings, no bias, negligible cost, ease of use, and the speed with which it can be completed (6–8 min), not only by doctors but also by the paramedical staff.
Limitation
As we are validating a method of measurement of ABI in comparison with the gold standard in apparently normal subjects, we should have taken a larger sample size. We are also not able to repeat the Doppler ABI measurement in participants due to time constraints.
Conclusion
Our finding suggested that ABI measurement by the automated oscillometric device is reliable, free of examiner bias, less time-consuming, and also helps in the simultaneous assessment of interarm systolic blood pressure difference. It can be used in place of the conventional Doppler method for screening and diagnosis of PAD in a larger population, OPDs, and offices.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Massmann A, Stemler J, Fries P, Kubale R, Kraushaar LE, Buecker A, et al. Automated oscillometric blood pressure and pulse-wave acquisition for evaluation of vascular stiffness in atherosclerosis. Clin Res Cardiol. 2017;106:514–24. doi: 10.1007/s00392-017-1080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Song P, Rudan D, Zhu Y, Fowkes FJI, Rahimi K, Fowkes FGR, et al. Global, regional and national prevalence and risk factors for peripheral artery disease in 2015:An updated systematic review and analysis. Lancet Glob Health. 2019;7:e1020–30. doi: 10.1016/S2214-109X(19)30255-4. doi:10.1016/S2214-109X (19) 30255-4. [DOI] [PubMed] [Google Scholar]
- 3.Beckman JA, Higgins CO, Gerhard-Herman M. Automated oscillometric determination of the ankle–brachial index provides accuracy necessary for office practice. Hypertension. 2006;47:35–8. doi: 10.1161/01.HYP.0000196686.85286.9c. [DOI] [PubMed] [Google Scholar]
- 4.Diehm N, Dick F, Czuprin C, Lawall H, Baumgartner I, Diehm C. Oscillometric measurement of ankle-brachial index in patients with suspected peripheral vascular disease:Comparison with Doppler method. Swiss Med Wkly. 2009;139:357–63. doi: 10.4414/smw.2009.12636. [DOI] [PubMed] [Google Scholar]
- 5.Herraxiz-Adillo Ax, Martıxnez-Vizcaıxno V, Cavero-Redondo I, Axlvarez-Bueno C, GarridoMiguel M, Notario-Pacheco B. Diagnostic accuracy study of an oscillometric ankle-brachial index in peripheral arterial disease:The influence of oscillometric errors and calcified legs. PLoS One. 2016;11:e0167408. doi: 10.1371/journal.pone.0167408. doi:10.1371/journal. pone.0167408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herráiz-Adillo A, Cavero-Redondo I, Álvarez-Bueno C, Martínez-Vizcaíno V, Pozuelo-Carrascosa DP, Notario-Pacheco B. The accuracy of an oscillometric ankle- brachial index in the diagnosis of lower limb peripheral arterial disease:A systematic review and meta- analysis. Int J Clin Pract. 2017;71:e12994. doi: 10.1111/ijcp.12994. doi:10.1111/ijcp.12994. [DOI] [PubMed] [Google Scholar]
- 7.Song BM, Kim HC, Shim JS, Lee MH, Choi DP. Inter-arm difference in brachial blood pressure in the general population of Koreans. Korean Circ J. 2016;46:374–83. doi: 10.4070/kcj.2016.46.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kawamura T. Assessing Ankle-Brachial index (ABI) by using automated Oscillometric devices. Arq Bras Cardiol. 2008;90:294–8. doi: 10.1590/s0066-782x2008000500003. [DOI] [PubMed] [Google Scholar]
- 9.Benchimol D, Pillois X, Benchimol A, Houitte A, Sagardiluz P, Tortelier L, et al. Accuracy of ankle-brachial index using an automatic blood pressure device to detect peripheral artery disease in preventive medicine. Arch Cardiovasc Dis. 2009;102:519–24. doi: 10.1016/j.acvd.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Takahashi I, Furukawa K, Ohishi W, Takahashi T, Matsumoto M, Fujiwara S. Comparison between oscillometric- and doppler-ABI in elderly individuals. Vasc Health Risk Manag. 2013;9:89–94. doi: 10.2147/VHRM.S39785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kollias A, Xilomenos A, Protogerou A, Dimakakos E, Stergiou GS. Automated determination of ankle-brachial index using an oscillometric blood pressure monitor:Validation vs Doppler measurement and cardiovascular risk factor profile. Hypertens Res. 2011;34:825–30. doi: 10.1038/hr.2011.53. [DOI] [PubMed] [Google Scholar]
- 12.Ma J, Liu M, Chen D, Wang C, Liu G, Ran X. The validity and reliability between automated oscillometric measurement of ankle-brachial index and standard measurement by Eco-doppler in diabetic patients with or without diabetic foot. Int J Endocrinol. 2017;2017:2383651. doi: 10.1155/2017/2383651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ichihashi S, Hashimoto T, Iwakoshi S, Kichikawa K. Validation study of automated oscillometric measurement of the ankle-brachial index for lower arterial occlusive disease by comparison with computed tomography angiography. Hypertens Res. 2014;37:591–4. doi: 10.1038/hr.2014.34. [DOI] [PubMed] [Google Scholar]
- 14.Sessa A, Paolini I, Marulli CF, Di Guardo A, Medea G. Determination of ankle-brachial index in type 2 diabetic patients with an automated oscillometric device. Eur J Clin Biomed Sci. 2019;5:5–8. [Google Scholar]
- 15.Hageman D, van den Houten MML, Pesser N, Gommans LNM, Scheltinga MRM, Teijink JAW. Diagnostic accuracy of automated oscillometric determination of ankle-brachial index in peripheral artery disease. J Vasc Surg. 2021;73:652–60. doi: 10.1016/j.jvs.2020.05.077. [DOI] [PubMed] [Google Scholar]
- 16.Richart T, Kuznetsova T, Wizner B, Struijker-Boudier HA, Staessen JA. Validation of automated oscillometric versus manual measurement of the ankle-brachial index. Hypertens Res. 2009;32:884–8. doi: 10.1038/hr.2009.125. [DOI] [PubMed] [Google Scholar]
- 17.Špan M, Geršak G, Millasseau SC, Meža M, Košir A. Detection of peripheral arterial disease with an improved automated device:comparison of a new oscillometric device and the standard Doppler method. Vasc Health Risk Manag. 2016;12:305–11. doi: 10.2147/VHRM.S106534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinski M, Styczynski G, Szmigielski C. Automated oscillometric measurement of the ankle-brachial index in patients with coronary artery disease. Hypertens Res. 2013;36:25–8. doi: 10.1038/hr.2012.120. [DOI] [PubMed] [Google Scholar]
- 19.Macdougall AM, Tandon V, Wilson MP, Wilson TW. Oscillometric measurement of ankle-brachial index. Can J Cardiol. 2008;24:49–51. doi: 10.1016/s0828-282x(08)70548-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wohlfahrt P, Ingrischova M, Krajcoviechova A, Palous D, Dolejsová M, Seidlerová J, et al. A novel oscillometric device for peripheral arterial disease screening in every day practice. The Czech-post Monica study. Int Angiol. 2011;30:256–61. [PubMed] [Google Scholar]
- 21.Korno M, Eldrup N, Sillesen H. Comparison of ankle-brachial index measured by an Automated Oscillometric Apparatus with that by standard Doppler Technique in vascular patients. Eur J Vasc Endovasc Surg. 2009;38:610–5. doi: 10.1016/j.ejvs.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Igarashi Y, Chikamori T, Tomiyama H, Usui Y, Hida S, Tanaka H, et al. Clinical significance of inter-arm pressure difference and ankle-brachial pressure index in patients with suspected coronary artery disease. J Cardiol. 2007;50:281–9. [PubMed] [Google Scholar]
- 23.Fu S, Wu Q, Luo L, Ye P. Relationships of drinking and smoking with peripheral arterial stiffness in Chinese community-dwelling population without symptomatic peripheral arterial disease. Tob Induc Dis. 2017;15:39. doi: 10.1186/s12971-017-0144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


