Abstract
Background
The consequences of the COVID-19 pandemic on physical and mental health in addition to the global economy are huge. Vaccination is a pivotal measure to decrease COVID-19 morbidity and mortality and to help bring the pandemic under control. Yet, success of the vaccination process depends on the population’s willingness to be vaccinated which may be determined by their level of knowledge about and trust in currently available COVID-19 vaccines. Therefore, this study aims to assess the knowledge, attitude, and acceptance of Palestinians towards COVID-19 vaccines.
Methods
A national cross-sectional study was distributed in different Palestinian regions to assess the knowledge and attitude of Palestinians toward COVID-19 vaccines using an online questionnaire, it included three sections; sociodemographic characteristics, knowledge assessment questions, and attitude assessment questions.
Results
A total of 6226 participants completed the questionnaire; among them, 41.36% believed that vaccines are safe, 69.02% agreed that vaccines are vital to protect from COVID-19; in addition, 55.1% approve administering the vaccine once available, and 37.86% do not believe their benefits outweigh the risks. The Source of information for 22.07% of participants in social media, while 11.92% rely on health care providers. Participants’ attitudes and knowledge were significantly affected by gender, governorate, age, education level, and marital status (P <0.001).
Conclusion
The findings suggest that there is good knowledge and attitude toward the vaccination process against COVID-19 in Palestine, although low acceptance was detected. Awareness campaigns are required to spread reliable knowledge about COVID-19 vaccines.
Keywords: COVID-19, Pandemic, Vaccine, Knowledge, Attitude, Acceptance, Palestine
Introduction
The coronavirus disease of 2019 (COVID-19) is a disease first triggered at the end of 2019 in Wuhan (Hubei, China) caused by a virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1–3]. The World Health Organization (WHO) declared on March 2020 a pandemic after deciphering the SARS-CoV-2 genomic sequence earlier in the same year [2, 3]. This pandemic has forced governments and policymakers to impose decisions of national lockdowns partially or completely and put billions of people in quarantine, which severely affected various aspects of life including psychological and economic impact [4, 5]. In addition to lockdowns, governments focused on other non-pharmaceutical interventions (NPIs) strategies to diminish the virus transmissibility including masks wearing, hand sterilizing, social distancing, schools, online education, and transfers restrictions [6].
By the end of May 2021, the WHO has registered more than 168 million confirmed cases of COVID-19 infection globally and more than 3.5 million deaths [7]. Concurrently, the scientific community has made unprecedented efforts to counteract the health crisis by conducting research projects on SARS-CoV-2 to understand its behavior, presenting the clinical image of COVID-19, and developing vaccine candidates [8–10]. The scientific community believes that vaccines are key strategy to stop the spread of the SARS-CoV-2 virus and end the pandemic. Accordingly, many pharmaceutical companies’ labs and research institutes have been working on the virus vectors including mRNA, DNA, subunit, and virus-like particles to develop a vaccine for COVID-19 [11, 12].
Over the past decades, vaccinations have been known to be an effective strategy in preventing the spread of certain viral infections [13]. Since vaccines are considered the most cost-effective and reliable public health interventions, which have been implemented over the past century and saved millions of lives each year [13–15]. Individual vaccination is considered an effective preventive measure as it provides direct immunity for the vaccinated individuals and prevents the spread of the disease among them. Also, vaccines have been proved to shrink the virus spread even among non-vaccinated individuals through herd immunity when sufficient immune proportions are available in the population [16].
Many countries have focused on accelerating the process of vaccine development, therefore, by the end of May 2021, more than 102 vaccines were in the clinical stage and more than 184 vaccines in the pre-clinical stage [17]. Despite the rapid progress of COVID-19 vaccine development, the public attitude toward vaccine acceptance is still challenging which affects the complete mitigation of the pandemic [18]. A study from Kuwait revealed that only 53.1% of participants were willing to receive COVID-19 vaccines once available and those who consider vaccines to have health related risks were less willing to accept vaccination [19]. For instance, 15.6% of people in Saudi Arabia would definitely not administer COVID-19 vaccine, while 26.8% of them would probably not accept the administration of the COVID-19 vaccine [20], while only 7% of people in Bangladesh would definitely not administer the COVID-19 vaccine and 24% of them probably won’t accept administering it [21]. Therefore, the readiness of people to accept the COVID-19 vaccine is vital to succeeding in the vaccination programs [22]. Hence, this national cross-sectional survey aims to measure the knowledge, attitude, and acceptance of the public population in Palestine toward COVID-19 vaccines.
Methods
The study was conducted following the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines [23].
Study design and participants
This is a national, cross-sectional study to assess the knowledge, attitude, and acceptance toward COVID-19 vaccines in the different Palestinian regions using an online self-administered survey pre-piloted and pre-validated during the period 7 May to 6 June 2021. Palestinian who are currently living in Palestine and aged > 18 years were included, while participants age < 18 years old or who did not complete the questionnaire or refused to participate were excluded.
Sampling
We used Epi info sample size calculator software to calculate the sample size, which is 384 by power 80% and confidence interval of 95%. To increase the validity of the study and decrease the standard error of a convenient sample approach, and to have more representative sample, a larger number of participants were recruited. Therefore, a total of 5979 participants were included in this study.
Questionnaire development
The study questionnaire was developed and structured into three sections (sociodemographic, knowledge, and attitude) followed by validation and translation into Arabic. The first section consists of demographic characteristics including age, gender, residence, marital status, education, chronic diseases, previous COVID-19 infection, vaccine administration, source of vaccines information, and fears faced during the COVID-19 pandemic. The second section aims to assess the knowledge of people towards COVID-19 vaccines by 18 questions with a 3-Likert scale; Yes/ No /I don't know, we referenced knowledge questions according to El-Elimat et al. [24], while the third part aims to measure the attitudes of people towards COVID-19 vaccines through 9 questions with a 3-Likert scale, Agree/ Disagree /I don't know. Questions used to assess attitude are referenced according to Abdul et al. [25]. A pilot sample (n=30) was used to measure internal consistency and improve the clarity of the questionnaire items. The questionnaire showed strong internal consistency with Cronbach's alpha value (0.75).
Data collection and handling
We recruited collaborators from different locations of Palestine to collect the data in a snowball fashion. The form was sent to social media platforms including Facebook, Instagram, Twitter, and WhatsApp. All collected data were stored confidentially on the author's laptop.
Statistical analysis
IBM's Statistical Package for Social Sciences SPSS version 25 was used to analyze the data. Descriptive analysis (percentage and frequency) was used to describe demographic characteristics and the prevalence of answers for each question in the questionnaire. Furthermore, Mann-Whitney was used to compare the knowledge score and Gender, Governorate, Chronic disease, Previous coronavirus infection, and vaccine administration, while the Kruskal-Wallis test was used to compare Age group, Education level, and Marital status with knowledge score. P-values of less than 0.05 were considered statistically significant.
Results
Socio-demographic characteristics of participants
The study included 5979 Palestinians from various governorates in the Gaza Strip and the West Bank, 15.1% of participants were from Gaza and 84.9% were from the West Bank, 73.8% of participants were female, and most participants’ age was between 20 and 24 (47.7%). More than 75% of participants had a university education (92.9%), and single participants account for 78% of the study population. 96% of the participants did not have any chronic diseases. Approximately half (56.1%) of participants reported that they had previously been infected with COVID-19. Additionally, (85.3%) of the participants did not receive the vaccine (See Table 1).
Table 1.
Socio-Demographic characteristics of participants included in the study
| Variable | N (%)(N=5979) |
|---|---|
| Gender | |
| Male | 1564 (26.2%) |
| Female | 4415 (73.8%) |
| The Governorate | |
| Gaza strip | 903 (15.1%) |
| West Bank | 5076 (84.9%) |
| Age group | |
| 18 – 19 | 2064 (34.5%) |
| 20 – 24 | 2854 (47.7%) |
| 25 – 29 | 348 (5.8%) |
| > 29 | 713 (11.9%) |
| Education level | |
| Non-educated | 23 (0.4%) |
| Primary school | 13 (0.2%) |
| Elementary school | 38 (0.6%) |
| Secondary school | 353 (5.9%) |
| University | 5552 (92.9%) |
| Marital status | |
| Single | 4662 (78%) |
| Married | 1253 (21%) |
| Divorced | 39 (0.7%) |
| Widower | 25 (0.4%) |
| Chronic disease | |
| Yes | 237 (4%) |
| No | 5742 (96%) |
| Previously infected with coronavirus | |
| Yes | 3357 (56.1%) |
| No | 2622 (43.9%) |
| Administered a COVID-19 vaccine | |
| Yes | 879 (14.7%) |
| No | 5100 (85.3%) |
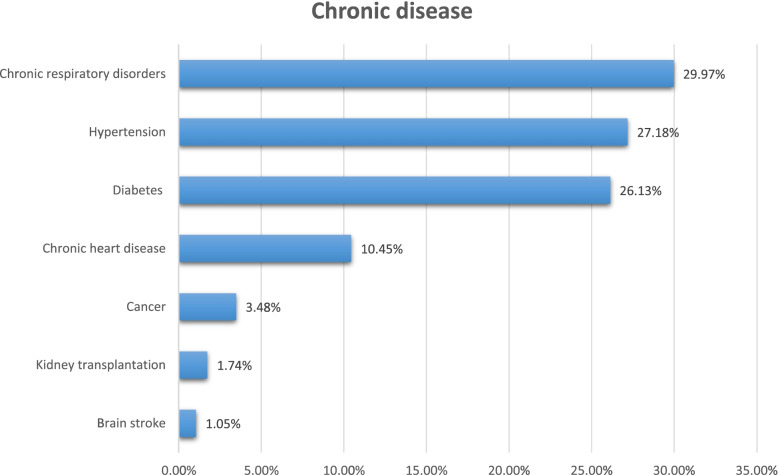
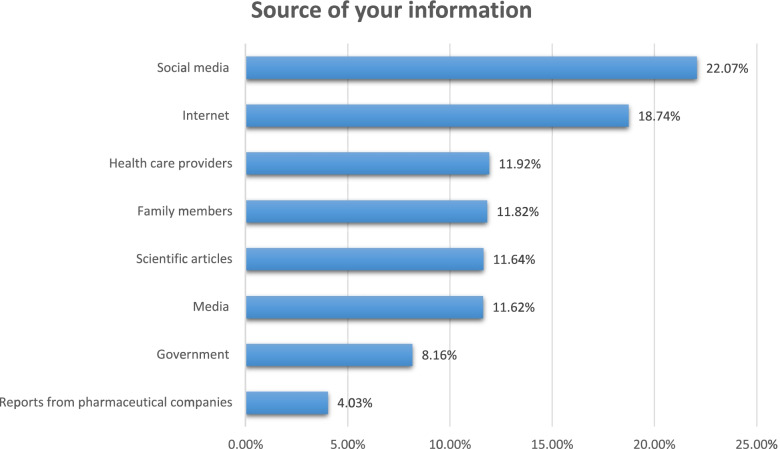
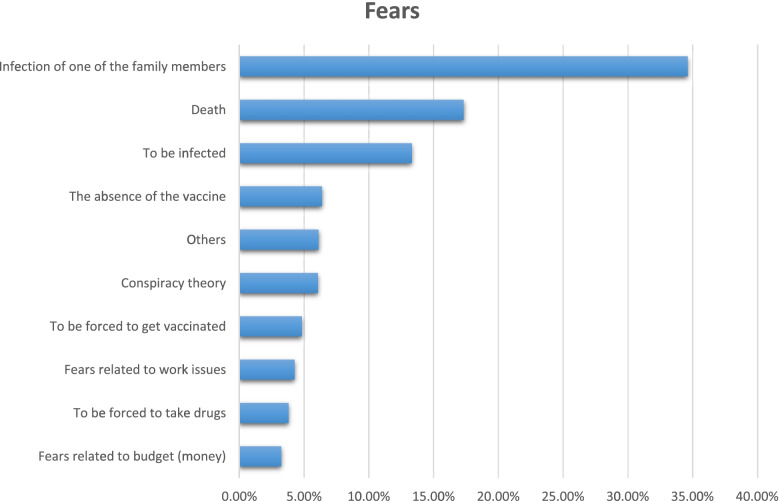
Among 237 participants who were reported with chronic diseases, more than 50% have chronic respiratory disorders and hypertension (29.97%) (27.18%), respectively (See Fig. 1). Regarding the source of information about COVID-19, social media, the internet, and health care providers were the primary source of information for the participants (22.07%), (18.74%), and (11.92%) respectively (See Fig. 2). Most of the participants' fears are related to death and family members’ infection (17.33%) and (34.62%), respectively (See Fig. 3).
Fig. 1.
The distribution of the chronic disease among participants
Fig. 2.
The most reliable sources of information about COVID-19 vaccines in Palestine
Fig. 3.
Palestinian fears during the COVID-19 pandemic
Knowledge of participants towards Covid-19 vaccinations
Frequencies of participants’ answers for each question regarding the knowledge about the COVID-19 vaccine is presented in Table 2. Gender, Governorate, Age group, Education level, Marital status, Previous COVID-19 Infection, and Vaccine administration were statistically significant (P-values<0.05). On the other hand, a history of chronic diseases showed no statistical difference in terms of the knowledge score (Table 3).
Table 2.
Participants’ knowledge toward COVID-19
| Statement | Yes N (%) |
No N (%) |
I don’t Know |
|---|---|---|---|
| There is an effective drug available to treat COVID-19. | 1211 (20.3%) | 2990 (50%) | 1778 (29.7%) |
| Vaccines are safe. | 2498 (41.8%) | 1211 (20.3%) | 2270 (38%) |
| There are ways to help slow the spread of the Coronavirus. | 5100 (85.3%) | 348 (5.8%) | 531 (8.9%) |
| There is currently a vaccine to protect against Coronavirus infection. | 4034 (67.5%) | 921 (15.4%) | 1024 (17.1%) |
| Regular flu vaccine will protect me from COVID-19. | 284 (4.7%) | 4034 (67.5%) | 1661 (27.8%) |
| Antibiotics are an effective treatment for COVID-19 | 936 (16.7%) | 3296 (55.1%) | 1747 (29.2%) |
| Taking vitamin C or other vitamins will protect you from Coronavirus infection. | 2802 (46.9%) | 1867 (31.2%) | 1310 (21.9%) |
| Wearing a mask helps reduce the spread of the Coronavirus. | 5331 (89.2%) | 411 (6.9%) | 237 (4.0%) |
| Hand washing helps reduce the spread of the Coronavirus. | 5481 (91.7%) | 280 (4.7%) | 218 (3.6%) |
| Cleaning surfaces helps reduce the spread of the Coronavirus. | 5109 (85.4%) | 513 (8.6%) | 357 (6.0%) |
| Vaccines against pneumonia will protect you from the Coronavirus. | 1016 (17%) | 2059 (34.4%) | 2904 (48.6%) |
| Regularly rinsing your nose with a saline solution will protect you from Coronavirus infection. | 2021 (33.8%) | 1602 (26.8%) | 2357 (39.4%) |
| So far, no one in your country has died from the Coronavirus infection. | 514 (8.6%) | 5130 (85.8%) | 336 (5.6%) |
| Eating garlic will protect you from the Coronavirus infection | 1173 (19.6%) | 2503 (41.9%) | 2303 (38.5%) |
| COVID-19 health complications are more severe on people who already have a serious medical condition. | 5016 (83.9%) | 309 (5.2%) | 654 (10.9%) |
| Other strains of Coronavirus can infect humans, including those that cause the common cold. | 4230 (70.7%) | 329 (5.5%) | 1420 (23.7%) |
| The virus has been genetically modified as part of a biological weapons program | 1547 (25.9%) | 1037 (17.3%) | 3395 (56.8%) |
| The virus is originally man-made and was spread intentionally | 1665 (27.8%) | 1272 (21.3%) | 3042 (50.9%) |
Table 3.
Influence of Palestinian participants Socio-Demographic and professional characteristics on knowledge
| Characteristic | Mean ± SD (out of 18) |
P-value |
|---|---|---|
| Gender | ||
| Male | 10.23 ± 3.7 | 0.007 |
| Female | 10.55 ± 3.26 | |
| The Governorate | ||
| Gaza strip | 10.98 ± 2.94 | <0.001 |
| West Bank | 10.37 ± 3.45 | |
| Age group | ||
| 18 – 19 | 10.21 ± 3.21 | <0.001 |
| 20 – 24 | 10.88 ± 3.35 | |
| 25 – 29 | 10.16 ± 3.68 | |
| > 29 | 9.67 ± 3.63 | |
| Education level | ||
| Non-educated | 7.39 ± 3.27 | <0.001 |
| Primary school | 8.84 ± 3.21 | |
| Elementary school | 7.21 ± 3.92 | |
| Secondary school | 9.3 ± 3.55 | |
| University | 10.58 ± 3.34 | |
| Marital status | ||
| Single | 10.69 ± 3.32 | <0.001 |
| Married | 9.72 ± 3.42 | |
| Divorced | 9.66 ± 4.73 | |
| Widower | 7.2 ± 4.15 | |
| Chronic disease | ||
| Yes | 10.1 ± 3.67 | 0.076 |
| No | 10.48 ± 3.37 | |
| Previous infected with the corona virus | ||
| Yes | 10.72 ± 3.27 | <0.001 |
| No | 10.14 ± 3.51 | |
| COVID-19 vaccinated | ||
| Yes | 11.2 ± 3.5 | <0.001 |
| No | 10.34 ± 3.55 | |
The attitude of participants towards Covid-19 vaccinations
Participants’ answers for the attitude towards the vaccine questions were reported in Table 4. Among participants, 55.1% agreed that they would administer the vaccine once available.
Table 4.
Participants’ Attitude toward COVID-19
| Statement | Agree N (%) |
Disagree N (%) | Don’t know (Neutral) N (%) |
|---|---|---|---|
| It is important to get vaccinated to protect people from coronavirus infection. | 4130 (69.1%) | 561 (9.4%) | 1288 (21.5%) |
| I have concerns about the unexpected effects of the vaccine. | 3780 (63.2%) | 1251 (20.9%) | 948 (15.9%) |
| Pharmaceutical companies are developing safe and effective vaccines against coronavirus. | 3304 (55.3%) | 527 (8.8%) | 2148 (35.9%) |
| I don't generally trust the benefits of the vaccine. | 2232 (37.3%) | 2593 (43.4%) | 1154 (19.3%) |
| Coronavirus vaccines developed in Europe or the United States are much safer than those made in other countries of the world. | 1547 (25.9%) | 1623 (27.1%) | 2809 (47%) |
| I have concerns regarding the commercial profitability of the pharmaceutical companies | 2567 (42.9%) | 1827 (30.6%) | 1585 (26.5%) |
| Possible side effects are considered barriers for me to administer the COVID-19 vaccine. | 1908 (31.9%) | 2603 (43.5%) | 1468 (24.6%) |
| Natural immunity is better than the immunity obtained by the COVID-19 vaccine. | 3484 (58.3%) | 1623 (27.1%) | 872 (14.6%) |
| If you were offered the vaccine, would you accept it? | 3295 (55.1%) | 1668 (27.9%) | 1016 (17%) |
Discussion
This is a cross-sectional study that was conducted among Palestinians in different areas, it has revealed that the general populations in the different areas of Palestine have good knowledge towards the preventive measures against the new coronavirus, which positively affects their attitudes to avoid spreading of infection. Regarding the attitudes and acceptance of COVID-19 vaccines among Palestinians; they have a low acceptance rate despite their knowledge that the vaccine can protect against COVID-19 infection.
Palestinians showed a good knowledge in the measures used in preventing the spread of the new coronavirus, 91.7%, 89.2%, and 85.4% agreed that hand washing, wearing masks, and cleaning surfaces reduce the spread of COVID-19 infection; respectively, participants from Gaza strip showed a better knowledge when being compared to participants from the West bank, and the majority of participants (85.3%) believed that there are ways that help to slow the spreading of the virus, which is consistent with a survey conducted in the United States and the United Kingdom found that respondents understood how COVID-19 is transmitted and disseminated [26], in addition, our results were consistent and similar to a previous study in a neighboring country, Jordan, which revealed that Jordanians had a positive attitude towards COVID-19; about 99.7% of the participants believed that hand washing is essential, 81.8% and 79.5% of participants agreed that smoking and antibiotics could not prevent infection [27].
Palestinians also believed that COVID-19 complications are more severe in patients with previous serious medical conditions (83.9%), about half of the participants believed that vitamin C or garlic could protect them from COVID-19 (46.9%) (19.6%), respectively, while more than half of participants believed that antibiotics won’t be helpful against the new coronavirus. More than half of Palestinians (67.54%) know that there is a vaccine against COVID-19, (41.8%) believe that the COVID-19 vaccine is safe, and (67.5%) and (34.4%) believe that the flu vaccine and the pneumococcal vaccine will not protect against COVID-19. When being compared with other populations, about a quarter of people in Bangladesh believe that the COVID-19 vaccine is safe [21]. In Jordan, 90% of participants clearly understood COVID-19 symptoms, and more than 80% were aware of the lack of vaccination [27]. Knowledge is vital in stopping spreading the coronavirus, a Chinese study has reported that knowledge has a direct impact on attitudes [28].
Palestinians have a good knowledge of preventive measures of COVID-19 which positively affects their attitudes to avoid the spread of infection. however, although (85.3%) of participants did not receive any vaccines, only (55.1%) reported that they would receive the vaccine if they had a chance to. The low percent of Palestinians, as reported in this study, who administered the vaccine can be explained mainly by the low percentage of vaccines acceptance as revealed by our study, also other reasons may contribute like the unavailability of vaccines or weaknesses of healthcare authorities to promote the vaccines availability, although (69.1%) believe that getting the vaccine would protect other people from having COVID-19.
Just like the previous pandemics humanity has faced, the COVID-19 pandemic is accompanied by feelings of fear, anxiety [29, 30]. Our findings agreed with those of Mertens et al., who reported that higher levels of fear during the COVID-19 pandemic were linked to family members getting infected or dead [31]. The self-worry is focused on preventing the disease from spreading to family members, particularly the elderly who have been recognized as vulnerable to bad COVID-19 prognosis [32]. Further widely, surveys that investigated the association between vaccination willingness and fear of the disease, found that individuals who are fearful of the disease are more likely to be vaccinated [33–37].
Studies have found that a people's intention to accept the vaccine is influenced by a variety of variables, including the risk of viral infection, the severity of the viral complications, the vaccine's safety, efficacy, and adverse reactions, misinformation, misconceptions regarding the vaccine, and lack of understanding the nature of diseases which are vaccine-preventable [38, 39].
There are conflicting reports of gender effects in the literature, some reported that males were more acceptable to receiving the vaccine in comparison with females [40, 41], in contrast, other studies indicated that females were more acceptable to receive the vaccine [42, 43]. In this study, the knowledge score for females’ participants was higher than the knowledge score among males’ participants. When being compared to other countries, Palestinians have a lower acceptance rate towards COVID-19 vaccine when being compared to other countries, for instance, Saudi Arabia, recorded a higher acceptance rate of (64.7%) [43], while in China acceptance rate was (88.6%) [44].
We found that younger participants had a better knowledge than older participants, contrary to previous research that found older age groups to be more accepting [41, 43, 44]. Differences in age distribution among some countries can explain those results, while Palestine is considered a country with a predominantly young population. In addition, participants with higher education (bachelor degree or above) are found to have higher knowledge score when compared with participants with lower education., which is consistent with a study conducted among six countries which indicates a relationship between good knowledge and level of education [45].
We stated that (55.3%) of the participants agreed that pharmaceutical companies would develop safe and effective COVID-19 vaccines, however, (63.2%) and (42.9%) reported some concerns about the vaccine side effects and the commercial profitability of the pharmaceutical companies; respectively. This discrepancy could be attributed to a global phenomenon that has contributed to such a low level of trust as various anti-vaccination campaigns fueled by modern technologies of communication; social media with fake, incorrect, and often inaccurate Arabic content and translations feed some people's conspiracy theories. Some factors associated with the country and region may also have a role, for example, Palestinian people can have lower confidence in the Palestinian authorities, some reports indicated that there is a positive correlation between lower acceptance levels of COVID-19 vaccines and lower confidence in the government's ability to handle the pandemic [44, 46].
Understanding the sources of information about COVID-19 vaccines that people trust the most is critical to future national vaccination programs [47, 48]. When Palestinians were asked which sources of information regarding COVID-19 vaccines they used the most, social media came out on top followed by the internet, while the government and pharmaceutical companies were the least trusted information sources, which is consistent with Malik Sallam et. al. findings that social media is the main source of information among participants who have higher Vaccine Conspiracy Belief Scale (VCBS) scores [49].
Good knowledge about COVID-19 vaccines is vital to increase the rate of acceptance to administer the vaccine, therefore, it is important to provide a reliable and scientific source of information which is evidence-based to be disseminated in the press and media to reach the public. Our study has shown that the largest percentage of knowledge among Palestinians is gained from social media and internet, therefore, attention must be paid to publishing scientific evidence-based content for people on internet and different social media platforms, also, Palestinian authorities should fight rumor mongers and limit their impact on society, as well as educating the media cadre about vaccines in order to involve them in urging people to take the vaccine and reassured public about the vaccine’s effectiveness and side effects. Our study showed that there are many non-vaccinated populations who have intentions to take the vaccine if it was available, we believe that the Palestinian Ministry of Health should target this large segment, and this could be done through the organization of vaccination campaigns.
Our study will help health care providers and policymakers in Palestine to understand public knowledge, attitude and acceptance toward COVID-19 vaccines and to take appropriate procedures and interventions aimed to increase the rate of vaccine acceptance and improving the health sector. It is also useful to carry out longitudinal studies aimed to study the behavior of Palestinians more accurately so that we can take the appropriate and rational action.
Strengths
We collected a large sample size from Palestinian individuals from various academic levels.
The current findings describe the public reactions of Palestinians towards the COVID-19 vaccines.
The results provide a good beginning point for identifying demographics and factors involving in affecting health behaviors.
The pattern of results could be generalized to a larger population.
Self-report measures were primarily employed to optimize convenience sampling to avoid bias effects.
Limitations
Online questionnaire may missed elderly people or people who have no internet access.
Our study is an online cross-sectional, so it is susceptible to participation bias.
Conclusion
Palestinian populations could have good knowledge and attitudes towards COVID-19, although they have low acceptance rate towards COVID-19 vaccines compared to other countries. Public health authorities should promote more research into the core causes of the differences in the acceptance rate towards COVID-19 vaccines worldwide. National health authorities should re-establish trusted sources of information as campaigns to provide more information about the safety, efficacy, and technology used to produce vaccinations.
Acknowledgments
None. Consortium name: IMedRA Collaboration Team: Thara Kh. Hussein AL-Ali1, Haroun Neiroukh2, Falasteen Jameel Almakhtoob1, Sireen Sufian Marabeh2, Malak Y. Badawi1, Anwar Y. Jabari1, Fida Hussien Al-Ali1, Tamer Sami Asafrah1, Yara Safwat Muhanna3.
1- Faculty of Medicine, Palestine Polytechnic University, Hebron, Palestine.
2- Faculty of Medicine, An-Najah National University, Nablus, Palestine.
3- Faculty of Pharmacy, Al-Azhar University - Gaza, Gaza Strip, Palestine.
Authors’ contributions
M.A.: questionnaire development, data collection, writing the manuscript, and supervision. S.G.M.: statistical analysis and manuscript revision. H.W.M.: questionnaire development and writing the manuscript. K.A.: statistical analysis. A.A.E.: statistical analysis. D.S.W., S.D.J., O.H.S., and E.A.I.: data collection and proposal writing. H.Z.A.: manuscript revision and editing. M.S.Z.: supervision. E.A.H: supervision and drafting manuscript. All authors reviewed and approved the final version of the paper.
Funding
This project was not funded.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was ethically approved by the Institutional Review Board of Polytechnic Palestine University (Ref no: KA/41/2021). And all the study methodology was carried out by the relevant ethical guidelines and regulations. The participants were asked to give consent that they agree to fill out the questionnaire for research purposes on the first page of the online form, and informed consent was provided by all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mohammed Al-kafarna, Email: malkafarna99@gmail.com.
Sajeda Ghassan Matar, Email: Sajeda.matar@hotmail.com.
Hossam Waleed Almadhoon, Email: Hossam.madhon@gmail.com.
Bashar Khaled Almaghary, Email: bmaghary@gmail.com.
Mohamed Sayed Zaazouee, Email: mohamedzaazouee@gmail.com.
Asmaa Ahmed Elrashedy, Email: asmaa.ahmed.4999@gmail.com.
Dalia Sami Wafi, Email: daliawafi97@gmail.com.
Sami D. Jabari, Email: samijabari6@gmail.com
Omar H. Salloum, Email: omar.h.h.maree@gmail.com
Eman Ahmed Ibrahim, Email: eman.a.ibrahim.1997@gmail.com.
Hala ZI Alagha, Email: Hala135@yahoo.com.
Elfatih A. Hasabo, Email: elfatih.ahmed.hasabo@gmail.com
IMedRA Collaboration Team:
Thara Kh. Hussein AL-Ali, Haroun Neiroukh, Falasteen Jameel Almakhtoob, Sireen Sufian Marabeh, Malak Y. Badawi, Anwar Y. Jabari, Fida Hussien Al-Ali, Tamer Sami Asafrah, and Yara Safwat Muhanna
References
- 1.Helmy YA, Fawzy M, Elaswad A, Sobieh A, Kenney SP, Shehata AA. The COVID-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J Clin Med. 2020;9(4) [DOI] [PMC free article] [PubMed]
- 2.Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed Atenei Parmensis. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sidor A, Rzymski P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients. 2020 Jun;12(6) [DOI] [PMC free article] [PubMed]
- 5.Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg (London, England). 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. World Health Organization; 2021. [cited 2021, 29 May]. Available from: https://covid19.who.int/
- 8.Nowakowska J, Sobocińska J, Lewicki M, Lemańska Ż, Rzymski P. When science goes viral: The research response during three months of the COVID-19 outbreak. Biomed Pharmacother. 2020;129:110451. doi: 10.1016/j.biopha.2020.110451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rzymski P, Nowicki M, Mullin GE, Abraham A, Rodríguez-Román E, Petzold MB, et al. Quantity does not equal quality: Scientific principles cannot be sacrificed. Int Immunopharmacol. 2020;86:106711. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1567576920319251. [DOI] [PMC free article] [PubMed]
- 10.Gianola S, Jesus TS, Bargeri S, Castellini G. Characteristics of academic publications, preprints, and registered clinical trials on the COVID-19 pandemic. PloS One. 2020;15(10):e0240123. doi: 10.1371/journal.pone.0240123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang J, Xie B, Hashimoto K. Current status of potential therapeutic candidates for the COVID-19 crisis. Brain Behav Immun. 2020;87:59–73. doi: 10.1016/j.bbi.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim E, Erdos G, Huang S, Kenniston TW, Balmert SC, Carey CD, et al. Microneedle array delivered recombinant coronavirus vaccines: Immunogenicity and rapid translational development. EBioMedicine. 2020;55:102743. doi: 10.1016/j.ebiom.2020.102743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hajj Hussein I, Chams N, Chams S, El Sayegh S, Badran R, Raad M, et al. Vaccines Through Centuries: Major Cornerstones of Global Health. Front Public Health. 2015;3:269. doi: 10.3389/fpubh.2015.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodrigues CMC, Plotkin SA. Impact of Vaccines; Health, Economic and Social Perspectives. Front Microbiol. 2020;11:1526. doi: 10.3389/fmicb.2020.01526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ehreth J. The value of vaccination: a global perspective. Vaccine. 2003;21(27–30):4105–4117. doi: 10.1016/S0264-410X(03)00377-3. [DOI] [PubMed] [Google Scholar]
- 16.Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52(7):911–916. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Draft landscape and tracker of COVID-19 candidate vaccines. 2021. Accessed 29 May 2021.
- 18.Coustasse A, Kimble C, Maxik K. COVID-19 and Vaccine Hesitancy: A Challenge the United States Must Overcome. J Ambul Care Manag. 2021;44(1):71–75. doi: 10.1097/JAC.0000000000000360. [DOI] [PubMed] [Google Scholar]
- 19.Alqudeimat Y, Alenezi D, AlHajri B, Alfouzan H, Almokhaizeem Z, Altamimi S, et al. Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Med Princ Pract. 2021;30(3):262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahmud I, Kabir R, Rahman MA, Alradie-Mohamed A, Vinnakota D, Al-Mohaimeed A. The Health Belief Model Predicts Intention to Receive the COVID-19 Vaccine in Saudi Arabia: Results from a Cross-Sectional Survey. Vaccines. 2021;9(8):864. doi: 10.3390/vaccines9080864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Islam MS, Siddique AB, Akter R, Tasnim R, Sujan MSH, Ward PR, et al. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. BMC Public Health. 2021;21(1):1851. doi: 10.1186/s12889-021-11880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12):e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eysenbach G. Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: A cross-sectional study from Jordan. Di Gennaro F, editor. PLoS ONE. 2021;16(4):e0250555. doi: 10.1371/journal.pone.0250555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdul K, Mursheda K. Munich Personal RePEc Archive Knowledge , Attitude and Acceptance of a COVID-19 Vaccine : A Global Cross-Sectional Study. Munich Pers RePEc Arch. 2020;(105236)
- 26.Geldsetzer P. Use of Rapid Online Surveys to Assess People’s Perceptions During Infectious Disease Outbreaks: A Cross-sectional Survey on COVID-19. J Med Internet Res. 2020;22(4):e18790. doi: 10.2196/18790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alzoubi H, Alnawaiseh N, Al-Mnayyis A, Abu- Lubad M, Aqel A, Al-Shagahin H. COVID-19 - Knowledge, Attitude and Practice among Medical and Non-Medical University Students in Jordan. J Pure Appl Microbiol. 2020;14(1):17–24. doi: 10.22207/JPAM.14.1.04. [DOI] [Google Scholar]
- 28.Moro M, Vigezzi G Pietro, Capraro M, Biancardi A, Nizzero P, Signorelli C, et al. 2019-novel coronavirus survey: knowledge and attitudes of hospital staff of a large Italian teaching hospital. Acta bio-medica : Atenei Parmensis [Internet]. 2020;91(3-S):29–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32275264. [DOI] [PMC free article] [PubMed]
- 29.Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO. Psychological Predictors of Anxiety in Response to the H1N1 (Swine Flu) Pandemic. Cogn Ther Res. 2012;36(3):210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- 30.Blakey SM, Abramowitz JS. Psychological Predictors of Health Anxiety in Response to the Zika Virus. J Clin Psychol Med Settings. 2017;24(3–4):270–278. doi: 10.1007/s10880-017-9514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord. 2020;74:102258. doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicomedes CJC, Avila RMA. An analysis on the panic during COVID-19 pandemic through an online form. J Affect Disord. 2020;276:14–22. doi: 10.1016/j.jad.2020.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kwon Y, Cho H-Y, Lee Y-K, Bae G-R, Lee S-G. Relationship between intention of novel influenza A (H1N1) vaccination and vaccination coverage rate. Vaccine. 2010;29(2):161–165. doi: 10.1016/j.vaccine.2010.10.063. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen TTM, Lafond KE, Nguyen TX, Tran PD, Nguyen HM, Ha VTC, et al. Acceptability of seasonal influenza vaccines among health care workers in Vietnam in 2017. Vaccine. 2020;38(8):2045–2050. doi: 10.1016/j.vaccine.2019.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knowledge and awareness about cervical cancer and human papilloma virus (hpv) vaccine among nursing students. J Crit Rev. 2020;7(12).
- 36.Anraad C, Lehmann BA, Visser O, van Empelen P, Paulussen TGW, Ruiter RAC, et al. Social-psychological determinants of maternal pertussis vaccination acceptance during pregnancy among women in the Netherlands. Vaccine. 2020;38(40):6254–6266. doi: 10.1016/j.vaccine.2020.07.047. [DOI] [PubMed] [Google Scholar]
- 37.Bhanu C, Gopal DP, Walters K, Chaudhry UAR. Vaccination uptake amongst older adults from minority ethnic backgrounds: A systematic review. PLoS Med. 2021;18(11):e1003826. doi: 10.1371/journal.pmed.1003826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilson K, Nguyen HH, Brehaut H. Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist. 2011;197 10.2147/IDR.S23174. [DOI] [PMC free article] [PubMed]
- 39. Al-Mohaithef M, Padhi BK. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J Multidiscip Healthc. 2020;13:1657–63. Available from: https://www.dovepress.com/determinants-of-covid-19-vaccine-acceptance-in-saudi-arabia-a-web-base-peer-reviewed-article-JMDH. [DOI] [PMC free article] [PubMed]
- 40.Abu-Farha RK, Alzoubi KH, Khabour OF. Public Willingness to Participate in COVID-19 Vaccine Clinical Trials: A Study from Jordan. Patient Preference Adherence. 2020;14:2451–2458. doi: 10.2147/PPA.S284385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. Author Correction: A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):354. doi: 10.1038/s41591-020-01226-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Al-Mohaithef M, Padhi BK. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J Multidiscip Healthc. 2020;13:1657–1663. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Opatola Kikelomo O, Olanrewaju MF, Atulomah NO. Knowledge, Attitude, Perception of Covid-19 Prevention Practices Among Residents in Selected Local Government Areas in Lagos State Nigeria. Afr J Biol Med Res. 2021;4(3):17–38. doi: 10.52589/AJBMR-KBTRCCBU. [DOI] [Google Scholar]
- 45.Mangla S, Zohra Makkia FT, Pathak AK, Robinson R, Sultana N, Koonisetty KS, et al. COVID-19 Vaccine Hesitancy and Emerging Variants: Evidence from Six Countries. Behav Sci. 2021;11(11):148. doi: 10.3390/bs11110148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLos One. 2021;16(4):e0250555. doi: 10.1371/journal.pone.0250555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siegrist M, Zingg A. The Role of Public Trust During Pandemics. Eur Psychologist. 2014;19(1):23–32. doi: 10.1027/1016-9040/a000169. [DOI] [Google Scholar]
- 48.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Sources and Perceived Credibility of Vaccine-Safety Information for Parents. Pediatrics. 2011;127(Supplement):S107–S112. doi: 10.1542/peds.2010-1722P. [DOI] [PubMed] [Google Scholar]
- 49.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, et al. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines. 2021;9(1):42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.