Abstract
Low- and middle-income countries are home to 80% of older people with HIV (OPWH). Ukrainian OPWH experience higher mortality and decreased antiretroviral therapy (ART) initiation than younger patients, but there is little data examining OPWH’s perspectives around new diagnosis and impact on care. In this study, we examined accounts of 30 newly diagnosed OPWH in Ukraine, exploring challenges faced in the peri-diagnosis period. Themes emerged representing the longitudinal coping process: OPWH (I) viewed themselves as low risk before diagnosis; (2) experienced HIV diagnosis as a traumatic event challenging their self-image; (3) used disclosure to seek support among a small circle of family, friends, or health care providers; (4) avoided disclosure to outsiders including primary care providers for fears of stigma and breaches in confidentiality; (5) viewed age as an asset; and (6) used HIV diagnosis as starting point for growth. These findings highlight the need for age-specific programming to increase HIV knowledge and coping, increase screening, and improve long-term planning.
Keywords: older people with HIV, diagnosis, coping, Ukraine, qualitative
Introduction
Older People With HIV (OPWH) in Ukraine
OPWH, commonly defined as people living with HIV (PLWH) >50 years old, are a growing population that has historically been overlooked by HIV interventions (Kirk & Goetz, 2009; Nachega et al., 2012). It is estimated that 80% of all OPWH live in low- and middle-income countries and that OPWH represent 20% of all PLWH (Autenrieth et al., 2018). In Ukraine, 15% of new HIV diagnoses occur in people over the age of 50, and this percentage is increasing (Rozanova, 2018). Our ongoing research has also shown that OPWH in Ukraine experience delays in antiretroviral therapy (ART) initiation and are over 3 times more likely to be lost to follow-up compared with younger patients (Allen et al., 2020a, 2020b). Despite these figures, there are a lack of targeted prevention or treatment programs for OPWH in Ukraine. HIV Interventions have largely focused on addressing the high-risk subgroups seen as early drivers of the HIV epidemic in Ukraine, such as intravenous drug users (IVDU), prisoners, and sex workers, despite heterosexual sex becoming the most common route of transmission in the early 2000s (“HIV and AIDS in Ukraine,” 2020). OPWH have only recently been identified as a population of interest for public health interventions in the country (Velika et al., 2021).
Coping Among OPWH
The ability to cope with a new diagnosis is influenced by contextual factors, including the age of the individual (Y. Chen et al., 2018; Folkman et al., 1987), disease process (Moskowitz et al., 2009), and cultural context (See & Essau, 2010; Torsch & Ma, 2000). OPWH face a number of challenges with HIV diagnosis compared with other PLWH, including significant delays in diagnosis (Kirk & Goetz, 2009; Longo et al., 2008; Rotily et al., 2000), leading to high incidence of opportunistic infection and immunodeficiency (Girardi et al., 2007; Kirk & Goetz, 2009), delays in ART initiation, increased mortality (Edwards et al., 2015), and increased incidence of physical and psychological comorbidity (Grov et al., 2010; Nachega et al., 2012; Rueda et al., 2014; Vance et al., 2010). They are also at increased risk for social isolation and may be less likely than other PLWH to seek social support, psychological help, or information about their illness (Goodkin et al., 2003). In Ukraine, OPWH may face specific cultural challenges to HIV diagnosis including multigenerational living (Libanova, 2014), which may pose challenges to HIV disclosure, and low pensions that place many older adults in an economically vulnerable position (Blyumina, 2005). New health care reforms in the country aimed at strengthening primary care systems also have important implications for the diagnosis of HIV in OPWH as new incentives become available to transition HIV care from specialty centers to family practitioners (Romaniuk & Semigina, 2018), creating issues surrounding physician rapport and concerns about breaches of confidentiality that may influence coping (Hughes & Lewinson, 2015).
No studies to our knowledge have examined coping with HIV among OPWH immediately after diagnosis in any global context and there are no known studies examining coping with HIV in Ukraine. However, research conducted primarily in the United States examining experiences of individuals aging with HIV or experiences of older individuals several years after HIV diagnosis has found OPWH to be a resilient population, despite the significant challenges they face (Emlet et al., 2011; Fang et al., 2015; Fumaz et al., 2015; Siegel et al., 1998). A recent study by Rosenfeld et al. (2018) examined strategies that OPWH used to improve well-being and identified volunteering, accentuating the positives in life, comparing their health with that of others, and attributing a benign meaning to HIV medication as coping strategies. Notably, the study excluded OPWH diagnosed within the last 12 months, citing a high mental health burden among those newly diagnosed (Rosenfeld et al., 2018). A study conducted by Beuthin et al. (2015) identified the narrative storylines of those aging with HIV theorized to influence how individuals live with HIV, including embodiment of illness, sense making, death and loss, secrets and stigma, identity, and seeking connection. Spirituality has also been identified as a factor in coping for OPWH (Siegel & Schrimshaw, 2002; Slomka et al., 2013). Interventions targeting coping in OPWH have shown promise in reducing depressive symptoms (Heckman et al., 2011) and increasing positive forms of coping (Heckman et al., 2001,2006).
Theoretical Framework
In this study we explore how newly diagnosed (within 6 months) OPWH in Ukraine experience HIV diagnosis and identify coping strategies. Our approach in analyzing the data was guided by the Transactional Model of Stress and Coping (Lazarus & Folkman, 1984), describing both coping strategies and the context surrounding diagnosis. The Lazarus and Folkman model was chosen as the theoretical framework because it is a well-defined model that is widely cited and used in a wide variety of settings (Folkman, 2010), including among patients with HIV (Atkinson et al., 2008; Graham, 2015; Remien et al., 2006). While it has not been used in the Ukrainian context, it has been used in studies of coping in other populations in the wider Eastern Europe and Central Asia (EECA) region, including Russia (Dolgova & Rokitskaya, 2020; Lutsenko, 2020). This model was particularly appealing because of its emphasis on coping as a nonlinear process, which allowed us to explore HIV diagnosis as a participant-defined stressor and examine patient accounts of coping mechanisms and feelings toward diagnosis over time.
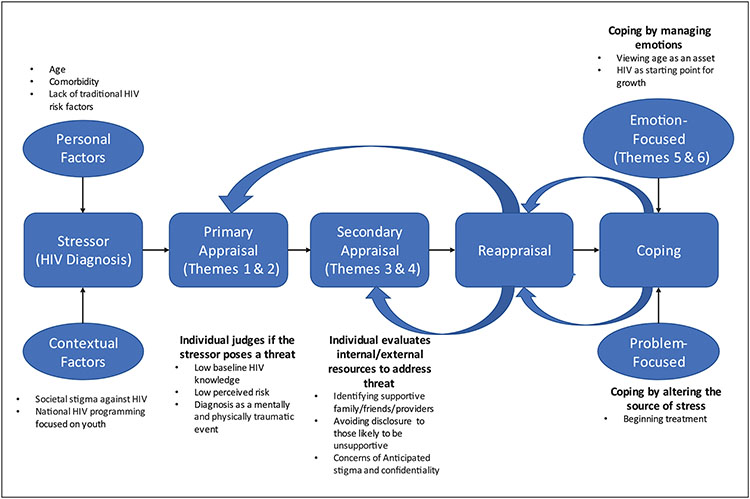
In the Lazarus and Folkman (1984) model, coping is defined as cognitive and behavioral actions to manage stressors that exceed the individual’s ability to handle them. The model, summarized in Figure 1, describes coping as dependent on a series of appraisals of the stressor and is highly dependent on personal and contextual factors that influence how a stressor is perceived. Primary appraisal occurs as an individual judges if the stressor poses a threat, whereas secondary appraisal involves evaluation of resources and coping strategies to address the threat, and reappraisal involves reevaluation of the stressor. Coping strategies then focus on confronting the source of stress (problem-focused coping) or on managing emotions (emotion-focused coping) (Lazarus & Folkman, 1984). While the texts were analyzed inductively, the Lazarus and Folkman model served as the theoretical lens while reading transcripts and interpreting results, with special attention paid to how participants’ appraisal of HIV diagnosis was evolving (in their own words and description) from the time of diagnosis to the time of the interview and what internal and external resources participants utilized.
Figure I.
The evolution of coping among Ukrainian OPWH.
Source. Adapted from Lazarus and Folkman (1984).
Note. OPWH = older people with HIV.
Study Focus Inspired by Gaps in Extant Knowledge
In this study, we drew inspiration from several gaps in the literature and from themes that were conspicuous in their absence. No studies to our knowledge have examined coping strategies among newly diagnosed OPWH (within 6 months of their diagnosis) in any setting, as extant published studies either excluded OPWH who were newly diagnosed (Rosenfeld et al., 2018), examined OPWH diagnosed many years prior (Beuthin et al., 2015; Fumaz et al., 2015; Solomon et al., 2014), or included a mix of newly diagnosed OPWH and those who had learned about their status long ago (Emlet et al., 2011; Siegel et al., 1998; Siegel & Schrimshaw, 2002). In the Ukrainian context, this early period after diagnosis is of particular concern given ongoing work demonstrating significantly higher rates of loss to follow-up after diagnosis among OPWH compared with younger patients, highlighting the need for intervention during this critical time (Allen et al., 2020b). Furthermore, research on coping in OPWH has primarily been conducted in the United States or Western Europe (Emlet et al., 2011; Fumaz et al., 2015). Studies in Eastern Europe or Central Asia are critically lacking, despite a high prevalence of HIV in the region (UNAIDS, 2020). To our knowledge, this is the first study to examine coping with a new HIV diagnosis among OPWH in Ukraine or the EECA region more broadly.
Finally, research on HIV in Ukraine has traditionally followed the epidemiology of the HIV epidemic, with a heavy focus on the intersection of HIV with intravenous (IV) drug use or comorbidities like hepatitis C (Mazhnaya et al., 2017; Ranjit et al., 2019; Tan et al., 2020). With emerging recognition of the increasing proportion of incident HIV cases among older people, research and programmatic HIV care in Ukraine must also shift to include the aging population (Rozanova, 2018). Using qualitative interviews of OPWH soon after diagnosis, we expand existing knowledge about how members of this understudied population understand HIV and find a way to live with it.
Method
Participant Recruitment
In-depth interviews (IDIs) were conducted with 30 OPWH who met inclusion criteria: aged 50 years and older, diagnosed with HIV within the last 6 months, and receiving care at the Kyiv AIDS Center. The Kyiv AIDS Center is the flagship state institution for HIV care that consists of three clinical facilities and is the main center for HIV-related clinical care in Kyiv and the surrounding region (Kyivska Oblast), providing care for approximately 14,000 patients. Kyiv, Ukraine’s capital, is the epicenter of the HIV epidemic with 23,000 diagnosed PLWH, placing it in the top 30 most profoundly impacted cities globally (“How Kyiv Fights the HIV/AIDS Epidemic,” 2017). The AIDS Center in Kyiv was chosen for our study due to the centralized HIV care, minimizing selection bias, as well as the large volume of patients to facilitate enrollment. HIV testing and treatment in Ukraine is free of charge for all registered patients, as are basic lab tests and doctors’ appointments. Patients must pay out of pocket for any additional tests or medications for comorbid conditions. Since 2016, Ukraine has employed the “Test and Treat” approach, with HIV providers prescribing and dispensing ART to patients as soon as possible after diagnosis, without restrictions based on CD4 count. About 300 OPWH are diagnosed at the AIDS Center per year.
Potential participants were identified by the Center’s psychologist, who meets with every new patient entering care. The psychologist offered eligible patients a description of the study; if interested, the potential participant then met with the interviewer who explained the study, and if a patient was willing to participate in IDI, written informed consent was obtained including for audio recording. Approval of the protocol was obtained from the Human Investigation Committee at Yale University and the Institutional Review Board (IRB) at the Ukrainian Institute of Public Health Policy in Kyiv, Ukraine.
Data Collection
We developed the interview guide for newly diagnosed OPWH based on the domains emerging from interviews we had conducted previously with HIV care providers and the literature (Chiao et al., 1999; Martin et al., 2008; Rubtsova et al., 2017; Sankar et al., 2011). Interview questions focused on the circumstances of participants’ HIV diagnosis, reaction and attitude toward diagnosis, knowledge about HIV, health and treatment history, risk behaviors, disclosure of HIV status or intent of disclosure, and attitude toward the future.
After informed consent, interviews were conducted in a private location in the clinic for 30 to 60 minutes and were audio recorded. Participants were advised that they could skip any question they did not wish to answer, and that they could terminate the interview at any time. Participants received 200 UAH (~US$7) for participating in the IDI. As the interviewer was fluent in both Russian and Ukrainian, participants could choose the language to be interviewed in, and all participants completed the interview in Russian. The sampling was purposive, as we strove to ensure the participants’ diversity including both men and women of a variety of ages over 50, as well as those with different comorbidities. We ceased interviews when thematic saturation was reached. In total, 30 participants completed IDIs.
Data Analysis
Audio files were transcribed verbatim and analysis of texts was conducted in Russian. Transcripts were coded using the latent content analysis method described by Graneheim and Lundman (2004) and Lindbom et al. (2017; Graneheim & Lundman, 2004; Lindbom et al., 2017). Transcripts from the same five interviews were closely read with personal notes to attain a general overview of the material. The ideas from the notes were then discussed and summarized into condensed meaning units, each of which was given a succinct name, or code. This list of inductively created codes formed a codebook that was iteratively refined through team discussion and then applied to code all 30 interview transcripts (including the initially read five). To ensure rigor, we held biweekly team meetings to review coding and made collective decisions about any excerpts that were hard to interpret and code. The coding process took 5 months. During the coding of the data, new codes could be added if new ideas were identified that had not been captured by the existing codes, and previously coded interview transcripts were then reread to ensure ideas captured by the newly created code had not been missed there. At the final stages of the analysis, categories were also aggregated into larger, more general themes that described their collective meaning. Regular meetings were held throughout the process. Reflexivity was practiced during meetings, and alternative interpretation of text was considered prior to making final decisions. Although we did not initially agree, consensus was reached through discussion. MaxQDA software was used for organizing qualitative data analysis.
Overview of Results
This study examined the HIV diagnosis accounts of newly diagnosed OPWH in Ukraine with the goal of understanding the specific challenges that OPWH face in the peri-diagnosis period. We found that OPWH perception of HIV diagnosis evolved quickly in this period, with many describing these changes as a longitudinal process beginning before diagnosis and ongoing at the time of interview. As OPWH reflected on this process, several common themes emerged. OPWH (1) viewed themselves as low risk for HIV; (2) experienced diagnosis as a traumatic event that challenged self-image; (3) disclosed and sought support among a small circle of family, friends, and/or health care providers; (4) avoided disclosure for fears of anticipated stigma and involuntary disclosure; (5) viewed age as an asset; and (6) used HIV diagnosis as starting point for growth. Overall, OPWH generally reported negative attitudes toward their HIV status at the time of diagnosis but could view their diagnosis more optimistically over time.
Sample Characteristics
Patient demographic and HIV treatment characteristics are shown in Supplemental Table I. Among 30 OPWH, the mean age was 58 years, and 53.3% were female. The mean time since diagnosis was 2.1 months with 22/30 (73.3%) participants currently taking ART and 13/30 (43%) reporting a history of opportunistic infection. Heterosexual sex was the most commonly reported risk factor for HIV transmission (18/30, 60%), followed by injection drug use (5/30, 16.7%) and being men who have sex with men (MSM; 1/30, 3.3%), though 20% declined to identify a risk factor. Location and circumstance of HIV diagnosis is summarized in Supplemental Table II. Diagnosis most commonly occurred in the outpatient setting during routine screening (12/30, 40%) or during hospitalization with an infectious process (11/30, 36%).
Low self-perceived HIV risk.
Before diagnosis, most OPWH viewed HIV as a stigmatized condition primarily affecting drug users or sex workers, leading many patients to view HIV as a disease of others that could not affect them. Participants often made a clear distinction between “ordinary people” (in reference to themselves) and people who met their expectations of a person with HIV. This sentiment is illustrated by one male participant who spoke about how his understanding of HIV from the media led him to believe that he was not a person who could be affected. Describing his understanding of HIV at the time of diagnosis, he made a clear distinction between himself and those who he believed were at risk:
I figured that [people with HIV] are drug users … needles and so on. Therefore, I did not communicate with drug users and I am myself not a drug user. Homosexuals—this is the same, and I am also not one.
Participants often struggled to reconcile their diagnosis with their view that they were not at risk for the disease in the first place.
Many had little awareness about HIV and equated risk of HIV with not living a “healthy lifestyle,” believing that HIV and a healthy lifestyle were incongruent. As a female participant stated, “all that I knew [of HIV] was what was advertised on television” and as another pointedly stated, “I knew that this virus was a dangerous disease but it happened that it didn’t concern me as I lead a regular lifestyle, well I didn’t think that I would get it so I was not worried about it.”
While participants used the phrase “healthy lifestyle” regarding the absence of drug use or high-risk sexual practices, it was also closely tied to their identity as older adults and how participants viewed themselves in a broader sense. As one female participant expressed, “I never thought that [HIV] would someday touch me … I am a family person … I’m 60 years old, I never did bad things, in this sense—a healthy lifestyle.” For her, “healthy lifestyle” was a reflection of her identity as an older woman who lived a morally acceptable life. Four participants who were diagnosed as a result of their heterosexual partner being diagnosed with HIV similarly expressed shock at their diagnosis and struggled to identify themselves as being at risk prior to learning about their partner’s status.
A notable exception to viewing themselves as low risk for HIV were participants who were either currently using IV drugs or had a history of drug use in the past. These patients had a higher awareness of HIV at baseline and of their susceptibility to HIV. As one male participant with a history of IV drug use stated, “I have scolded myself my whole life for the diagnosis of HIV. I repeatedly jumped from drug to abstinence, I forced myself and then again relapsed. Well psychologically I long ago set myself up for this.” While these participants recognized their HIV risk, they also believed that their history of drug use meant that they had not led a “healthy lifestyle.”
HIV diagnosis as a traumatic event.
Participants described their HIV diagnosis as an emotionally and physically traumatic event. Their most common reactions toward diagnosis were “shock,” “fear,” and “shame.” Emotional reactions to diagnosis could be extreme. As one male participant described, after his diagnosis he felt like he no longer wanted to live: “I for the whole week walked like a zombie. I even, honestly, wanted … to die.” Some patients described lasting psychological consequences of diagnosis with one participant even quitting her job over fears of her coworkers finding out about her HIV. Another male participant, a widower in his 60s, remembered how HIV had worsened his existing feelings of isolation and made him feel “humiliated.” For him, HIV was a condition in which “you are not whole … You have an illness in which you are not a whole person.” A female participant compared the fear in receiving HIV diagnosis with someone learning they have cancer: “Who knows what is better, cancer or HIV.”
These feelings were exacerbated in those who viewed diagnosis as challenging their self-image. Having received HIV diagnosis, participants were forced to reconcile their view of themselves with their negative associations surrounding HIV. For one female participant, HIV diagnosis challenged her view of herself as an “ordinary,” older person.
It is hard for me, because there is this stereotype that this is a disease of a certain segment of the population, some garbage of society … You don’t want to associate yourself with that group, so that you are then abnormal … But you find yourself in this environment, this is very uncomfortable, you know, it is very depressing.
This participant also compared her experience of HIV diagnosis with her previous diagnosis of cancer, saying that her diagnosis of HIV was more difficult because she was fighting feelings of guilt: “The worst thing is that you blame yourself … you did something wrong … The guilty feeling eats you up.”
Many patients described their HIV diagnosis as a physically traumatic process, as the road to diagnosis was often long and arduous. This was especially true for the one third of patients diagnosed while hospitalized with an infectious process in the setting of acute and serious illnesses. Many of them described extensive hospitalizations, often seeing multiple specialists before being tested for HIV. One male participant recalled being evaluated by five different specialists over two hospitalizations before he was tested for HIV, while another described over a year of being in a “terrible state of health” with multiple illnesses, viral lung conditions, and a 15-kg weight loss before physicians tested him for HIV. Others were diagnosed in the setting of severe illness like one female participant, who had presented to her primary care doctor for a runny nose but soon ended up unconscious for 4 days with meningoencephalitis. A late diagnosis led directly to physical disability in three participants, impacting their ability to work or creating difficulty returning to their normal life.
Serious illness contributed to the difficulty of receiving an HIV diagnosis. For one male participant, HIV diagnosis challenged his view of his own health as he had considered himself healthier than many people of similar age: “I am a healthy man! … I know that many do not live to my age! … Where is this from? It was an enormous shock!” These participants commonly viewed their physical recovery as the most difficult part of life. As one participant stated, “the hardest thing is to recover,” while another participant stated, “to be treated to live even a little more … we must pull ourselves together, as they say, to not lose heart.”
Use disclosure to seek support among a small circle of family, friends, and/or health care providers.
The majority of OPWH had chosen to disclose to at least one close family member or friend, with children and partners being the most common. Participants overall received positive responses, with many confidantes becoming actively involved in their treatment. One female participant described how her daughter helped her learn more about HIV: “My daughter was in shock for two days. Then I went to her and we searched the internet together, to learn everything. We learned, and now everything is well.” The son of another female participant encouraged her to accept her diagnosis: “As my son says, you simply have to be confident in yourself, love yourself. Well you got this [HIV] but no one is to blame, and you have to love yourself so that you can care for yourself.”
Others described their disclosure as changing their relationship with the person they disclosed to, often for the better. For the same participant, her diagnosis became easier to handle when she “stopped hiding in herself’ and told her children about it. Her relationships with children became the best part of her life.
The best is that I have children, loved ones who understand me, grandchildren who make me happy, and relationships which became much better between me and my children. They became more caring towards me.
Another participant said her son became much more supportive since she disclosed her diagnosis: “He began to treat me better. Earlier he didn’t call … and now he comes running every day and brings me something to eat.”
Health care professionals were cited as a large source of support for the participants as they learned of their diagnosis. One female participant spoke about her communication with a social worker:
Especially at the first stage, when you get there, it is like ice water is poured on you, you are in shock. Then, of course, when there is a social worker, a girl that calmly explained to me that I should not be afraid, it is very important. It’s very important that you are not alone with this problem. I can always call her, she told me to call at any time, if there is any problem—this is very important.
Another participant described how her social worker was instrumental immediately after she was diagnosed, and connected her to care.
It’s good that the social worker came and I didn’t have to go to the AIDS Center on my own, that the girl came and took me by the hand. It is good that they called her from the hospital because I would not have come on my own in my life, to be honest … You can talk to the social worker about everything, because she knows everything.
Selective disclosure and anticipated stigma.
Participants used discretion about disclosure to avoid disclosing to people they felt would react poorly. In some cases, the choice to not disclose was to protect their relationships due to high anticipated stigma. One female participant explained her reasoning for disclosing to her son but not to her daughter, as her daughter had once tried to get her coworker fired for being HIV-positive. Another refused to tell her children for fear they would not let her see her grandchildren:
I will never tell [my children] about [HIV]. I do not know their reaction. I have a granddaughter, who is one year old, and there should soon be another one from [my son], well from my son, next year. I can’t tell them. What if they would not want me to visit.
Other participants framed their decision to not disclose as a means to protect loved ones from the emotional difficultly they had experienced themselves in receiving their diagnosis. One woman was afraid to disclose to her mother and children for fear that the news would cause them too much stress:
They will be scared, I’m more afraid for my mother so that she doesn’t have a heart attack, she’s already older. All these explanations about modern drugs and other things will not have an effect on her and especially on the children.
None of the employed participants had chosen to disclose their status to colleagues out of fear that “they would not understand [me]” or fear of being fired. As one participant explained,
Many simply don’t want to lose their jobs because, as far as I know, they can’t officially fire me because I have HIV but they can persistently ask me and create conditions so that I leave.
OPWH were wary about disclosing to certain health care professionals and sought treatment environments where their condition would be understood. Most participants would rather not disclose their HIV status to physicians outside of the AIDS Center unless they were directly asked, and almost all indicated that they were resistant to changing care from the AIDS Center to a family physician. Participants strongly associated their primary care clinics with their communities; they feared that they would lose confidentiality, and news of their diagnosis would spread in the community. One woman reacted to news that ART treatment could be moved to community clinics saying, “Believe me, then the whole clinic and everyone on earth will know about this [HIV diagnosis]. I do not agree with this, completely disagree.” Another preferred to continue treatment at the AIDS Center because she felt it preserved her anonymity:
I don’t know how they [family doctors] would react to this, let’s say, if I [disclosed] in the clinic near my residence. I don’t know. Here, simply, they have specialists and everything is the same. No one advertises anything here. Here no one knows anything about you. No one asks anything. They only know your name and that’s it. But there—no, I would not want to talk to anyone about it.
Beyond fear of involuntary disclosure, participants like this woman anticipated stigma from non-HIV health care professionals and did not know how to disclose HIV to other clinicians/providers. As another stated,
[At the AIDS Center] the attitude is good. The nurses are caring, the staff, the doctors good, here—yes, but to strangers it is … I don’t even know how to admit to someone if I was staying in a hospital somewhere, I don’t know at all.
Overall, participants at this early stage after diagnosis expressed a strong preference for preserving their confidentiality, seeking care at specialized AIDS clinics, and eschewed care in primary care settings.
View age as an asset.
Age was invoked as a positive in participants’ ability to embrace uncertainty of life and to cope with their diagnosis. As one male participant said of his diagnosis,
It made me nervous, but … in the end, I am [more than 50] years old, not 20 [laughs], and life … I would, of course, like to live another 30 years … but what will happen—will happen.
Her age allowed a female participant to focus on living: “What can be good at this age—good weather, yes. As they say, a good mood in the morning. It is necessary that we don’t get fixated on all of this. And live further.” Another female participant expressed a similar sentiment: “I’m 60 years old, I understand honestly that there is nothing to be done but live.” She also felt that being diagnosed at this age had allowed her to live the majority of her life without the burden of HIV:
It is good that I am not young anymore, that I am not with anyone and I do not need men … If I were young and I would have spread [HIV], everything would have been mined, it would have been tough.
She also described feeling that being diagnosed at an older age put her in a better position than younger people:
… by this age, you know, I’m not scared anymore. When I see pregnant girls in the hallway, I’m scared for them, I feel sorry for them. I think—God they are young, they give birth, but I already lived and everything was fine, okay … Of course, it’s scary … but looking at the youth, it’s a little for me, well, you can’t say it’s calming … it’s really scary for them. I think how they will live, because they have everything ahead.
As evident in both participants’ statements, participants appreciated that being diagnosed at an older age had allowed them to live most of their life as a “normal person” and allowed them to navigate major life events without HIV.
By drawing on past experiences and age as an asset, OPWH could reframe the unexpected HIV diagnosis as another life event that they were capable of overcoming. One male participant described his outlook on the future by comparing it to his past struggles with finances, deaths of loved ones, and other health issues, while another said he was able to begin to view HIV as something that he must actively fight against: “I had this in my life, not only ups, but also downs. I understood that if a person does not pull himself together and does not begin to do something to be good, then it will not be good.” For others, comparisons of HIV with other chronic diseases helped frame the diagnosis as a familiar condition that could be managed. As one stated,
And here I think, that there should be information about HIV—that it is not fatal, that this is a state which cannot fully be cured, but … that you need to live with it … like diabetes or hepatitis—you live and you live.
HIV diagnosis as a foundation for personal growth.
Despite all the difficulties experienced through HIV diagnosis, many identified that knowledge had empowered them to make changes. One female participant described a day where she could feel positive about her diagnosis as it was something that she was actively treating: “I am happy because I know of my illness.” Another echoed her:
[what is] good—probably that, at the end of the day, I knew that I was sick. And now I will fight with this illness, infection. I will be careful and not infect anyone … Well, now I know, at least, about it, about the problem and I will try to resolve, to treat. That is it. It is good that I found out.
Participants described their diagnosis as an opportunity to reconsider their priorities. They spoke about three (often interconnected) ways in which their diagnosis had impacted their view of the future: (a) embracing life, (b) focusing on relationships, and (c) prioritizing health.
One woman described how being diagnosed with HIV forced her to consider her mortality and embrace living in the moment: “The main thing is quality of life, and not who is sick with what. The quality of life, and how much you will live. That’s all. You need to understand that you can die from the flu tomorrow.”
Others used diagnosis as an opportunity to begin prioritizing their health. For another participant, being “as healthy as possible” was what allowed her to look to the future with optimism. For participants who reported current or past drug use as a route of transmission, this was especially apparent. Two participants who were actively using drugs at the time of diagnosis cited their diagnosis as an incentive to make changes in their lifestyle by quitting drugs or starting drug treatment. One woman, who had since quit using drugs, explained that her diagnosis gave her relief as it was an opportunity for her to confront an issue [HIV infection] that she had suspected but not confirmed: “I knew it. I knew it. Therefore, I embraced it. Honestly, the kind of certainty at last, I am dealing with this issue already.”
HIV diagnosis made another participant focus on her relationships, both with her children and those around her:
You know, psychologically, I rejoice every day. I try to share more of my attention with my children. I became calmer, surprisingly. It would seem I would worry but it is the opposite, I became calmer. Calmer in my relation to people, towards their moods, towards their flaws, I try to smooth sharp comers because who knows what will happen in a month, in two months …
For many, living in the moment meant refocusing on relationships. One participant said that the biggest change in her life was “my relationship to life … You know I started to live more, well as they say, I do not need money, money, money, not money but relationships. Relationships with family, relationships with loved ones.”
Discussion
Mapping patients’ accounts of HIV diagnosis to Lazarus and Folkman’s model provides a framework for understanding how OPWH experience HIV diagnosis and find a way to move forward. Understanding this adjustment process is essential for informing the development of strategies to improve rapid engagement of OPWH in HIV care. Figure 1 provides a graphical representation of the Lazarus and Folkman transactional model of stress and coping adapted for Ukrainian OPWH. HIV diagnosis represented a significant stressor, Themes 1 and 2 exemplified primary appraisal, Themes 3 and 4 exemplified secondary appraisal, and Themes 5 and 6 exemplified early emotion-based coping mechanisms. As participants began primary appraisal, several factors appeared to influence how OPWH experienced HIV diagnosis as a stressful event. These included a low level of baseline HIV knowledge, harmful stereotypes about people with HIV, conception of self as an “ordinary” older person, and lack of recognition of personal risk (Theme 1). HIV diagnosis was characterized as both a psychologically and physically traumatic event that often challenged self-image and identity, contributing to the stress of diagnosis (Theme 2). Participants sought assistance addressing HIV diagnosis through the process of secondary appraisal, confiding in the family, friends, and health care workers who were likely to be supportive (Theme 3), and avoiding disclosure to those who would not, including primary care providers (Theme 4). Anticipated stigma and fears of breaches in confidentiality were the biggest barriers to secondary appraisal. Participants also demonstrated early use of emotion-focused coping mechanisms, including positive interpretation and growth by viewing age as a strength (Theme 5) and HIV diagnosis as a starting point for personal development (Theme 6).
The importance of knowledge and education about HIV was repeatedly emphasized by OPWH. In the process of primary appraisal, previous education about HIV (or lack thereof) played a large role in how OPWH evaluated and experienced HIV diagnosis as a stressor. Stereotypes about those with HIV as drug users or sex workers were often cited as the only source of baseline HIV knowledge among participants, with many citing these stereotypes as a major factor in their lack of self-perceived risk (Theme 1) and contributing to the identity crisis that participants described upon diagnosis (Theme 2). These findings also reveal that OPWH strongly associate HIV as a disease of a very specific population (i.e., substance users, MSM, sex work). This conception of HIV is likely closely connected to the epidemiology of HIV in Ukraine and the efforts undertaken to control the epidemic. According to major international reports (UNAIDS, 2020; WHO Regional Office for Europe, European Centre for Disease Prevention and Control, 2017), Ukraine had one of the fastest growing HIV epidemics in the world, largely fueled by IV drug use in the setting of stark economic and health care collapse coinciding with the fall of the Soviet Union. Early large-scale prevention efforts to combat the epidemic focused heavily on addressing key populations, such as IV drug user and sex workers, and were overall successful in expanding HIV testing, ART availability, and opioid treatment programs. Education surrounding HIV followed suit, largely focused on addressing the epidemic in key populations (Colborne, 2017; Ministry of Health of Ukraine, 2015). These aggressive efforts led to a slowing of new cases, and in 2008, heterosexual sex appeared to become the most commonly reported route of transmission in Ukraine (Vitek et al., 2014; WHO Regional Office for Europe, European Centre for Disease Prevention and Control, 2017).
While the epidemiology of the HIV epidemic has shifted, our research reveals that the stereotypes of HIV among older adults in Ukraine have not. While no studies in Ukraine have assessed HIV knowledge specifically among older adults, a study conducted in Ukraine among PLWH of all ages identified a lack of knowledge about HIV as a major barrier to linkage to care (Kiriazova et al., 2018). The results of this study, as well as findings globally in other settings showing that OPWH possess low levels of knowledge about HIV (Henderson et al., 2004) and do not perceive themselves to be at risk for HIV (Altschuler et al., 2008; Jackson et al., 2005; Maes & Louis, 2003), suggest that HIV knowledge and risk perception may be lower in Ukrainian OPWH compared with younger patients and may contribute to the low linkage to care seen in Ukraine (Allen et al., 2020b). In general, increased awareness of HIV in older adults and the variety of mechanisms by which HIV is transmitted is needed among the general population, providers, and at the institutional level in Ukraine. Frameworks for HIV educational campaigns aimed at older people in the United States have been developed (Orel et al., 2005), well received (Altschuler et al., 2004), and shown to decrease unprotected sex (Illa et al., 2010). Informal surveillance in Kyiv revealed that there are currently no organizations that offer formal age-specific programming. Age-inclusive educational interventions in the Ukrainian context are needed to address stereotypes, stigma, and perceptions of risk among both the public and older adults.
In secondary appraisal, as participants began to evaluate the support available to them, they turned to close contacts or health care professionals (Theme 3). Disclosure to a confidante among people with HIV of all ages has been shown to play an important role in HIV acceptance and treatment (Horter et al., 2017; Nam et al., 2008) and in mental health and wellness (Rosenfeld et al., 2018). While disclosure patterns among OPWH are understudied, one study conducted by Emlet et al. (2011) in the United States found that OPWH were less likely than younger patients to disclose HIV status and that disclosure was associated with increasing time since diagnosis and having a close confidante (Emlet, 2006a). Our findings suggest that the majority of OPWH in Ukraine had disclosed to at least one family member or friend within 6 months of diagnosis. Health care workers, especially social workers, were noted by participants to be particularly important immediately after diagnosis before OPWH were able to involve close confidantes. Older people in Ukraine face specific challenges engaging in dialogue about issues of sexual wellness, including with their providers. This is likely related to views of older adults as moral authorities in society and stereotypes about the asexuality of older adults. This may be especially true of older women, who are more likely to be scrutinized or have their sexual or substance use behavior equated to moral failings. These views of older people contribute to the lack of perceived risk and difficulties accepting the diagnosis. From ongoing work among HIV providers, many of whom are also older, discomfort speaking to older patients regarding sexuality or substance use behaviors is common. Many cited a fear of offending the older person, believing in the wake of such questions older patients would feel targeted as a “type” of person that engaged in promiscuous or addictive behavior.
Secondary appraisal was complicated by anticipated stigma and fear of confidentiality violations contributing to hesitancy around disclosure (Theme 4). The finding that the majority of OPWH would not want to transfer HIV care or disclose about HIV to a primary care physician is of particular significance in the Ukrainian setting, as ongoing health reform efforts in the country aim to incentivize the development of a comprehensive primary care system. Our study highlights that the major resistance toward this transfer was concern for breach of confidentiality and fears of judgment from providers, who patients viewed to be within their immediate community, similar to findings of another study of Russian PLWH published recently (Dudina et al., 2020). For some, the AIDS center provided an anonymity that their primary clinics could not and OPWH feared that discussing their diagnosis in the same physical location that they, their family, and friends received care posed a risk of involuntary disclosure. Almost paradoxically, OPWH in our study who said they had good relationships and long-term established trust with their family provider were hesitant about disclosing their HIV status to them for fear of how the disclosure could affect their relationship. Notably, while literature from the United States suggests that OPWH do experience ageism (Emlet, 2006b), HIV-related stigma (Emlet, 2007), and significant breaches in confidentiality (Emlet, 2008), our study did not identify these challenges among OPWH, potentially attributable to relatively short time since diagnosis. Given these findings, there is a need for additional training for medical providers to institute nonjudgmental care, tackle issues of confidentiality, as well as develop training tools to improve engagement among older patients about sexual health and substance use in the primary care setting, and increased emphasis on routine screening (Leblanc et al., 2016).
Early emotion-focused coping mechanisms included seeing age as a strength and using HIV as a starting point for growth (Themes 5 and 6). Considering age as a strength, OPWH often applied the coping mechanisms they employed for other hardships to their experience of HIV diagnosis. Previous studies have shown that OPWH were able to view their age as an advantage in line with what our participants expressed (Emlet et al., 2011; Fumaz et al., 2015; Siegel & Schrimshaw, 2002; Vance & Woodley, 2005). Participants also used positive reinterpretation and growth by viewing their HIV diagnosis as an opportunity to redefine their priorities, a coping technique that has also been described in OPWH (Fumaz et al., 2015). These results suggest that interventions aimed at promoting the use of social support and focusing on the opportunity for growth may be particularly useful for newly diagnosed OPWH in Ukraine. Social support among OPWH in Ukraine has also been linked to retention in care during the COVID pandemic, emphasizing the need for innovative interventions to promote social support at a time when physical interaction may be limited (Rozanova et al., 2020).
OPWH would also benefit from age-specific and cultural-specific counseling to facilitate disclosure to children, ascertain comorbidities, clarify the role of primary care providers, redefine their priorities, and consider future goals (Theme 6). While health care service utilization is overall similar to those for younger patients, OPWH were more likely to require adjunctive services such as physical therapy, adult day care, home chore services, and home delivered meals (Emlet & Berghuis, 2002). Other concerns of OPWH could be addressed in counseling, such as uncertainty in aging with HIV (Furlotte & Schwartz, 2017; Solomon et al., 2014), disability (Hanass-Hancock et al., 2015), and aging expectations with a chronic illness (Kahana & Kahana, 2001; Pitts et al., 2005).
There appeared to be a great diversity of experiences and life circumstances within the group of OPWH. Those OPWH who were relatively younger were frequently engaged in caregiving to either children, grandchildren, or elderly parents while continuing to work full- or part-time. Older OPWH were more likely to be retired and often relied on financial support from adult children, as pensions for retirees are especially modest. In general, women (both relatively younger and relatively older ones) were more likely to be tested because a partner was diagnosed with HIV and men were more likely than women to have a partner who was HIV negative. Our study is the first foray into exploring the experiences of OPWH in Ukraine; among our next steps will be to further explore gender and the experiences of older and younger OPWH.
More research is needed to examine the relationship between culture and coping among OPWH. Almost all research regarding coping in this population has been conducted in the United States and Western Europe. A minority of studies conducted in China have examined coping strategies (D. Chen et al., 2020) and correlations (Xu et al., 2018) in Chinese OPWH, but the impact of culture remains unclear and inconsistent definitions and methodology make cross-cultural comparison difficult. Although OPWH in Ukraine may face many unique challenges, it is difficult to discern the role of culture in the coping strategies used by Ukrainian OPWH without a better understanding of this population within Ukraine and coping strategies of OPWH globally. Future studies may also examine the impact of gender, caregiving, and sexual identity on the experiences of OPWH in Ukraine.
There were several important limitations to our study. Participants of this study were all 50 years or older and there was no comparison group of younger patients, limiting our ability to differentiate characteristics specific only to OPWH. Furthermore, all participants were engaged in care through the Kyiv AIDS Center and the experiences of the OPWH interviewed in this study may not reflect the experiences of OPWH who are diagnosed and who may not link to care. In addition, all participants were able to visit the center in-person for interview, excluding participants with physical or financial barriers.
Future investigations must explore how Ukrainian and former Soviet culture impacts HIV diagnosis coping mechanisms. Similarly, findings warrant further investigation of gender and sexual identity, as these likely intersect with HIV stigma and ageism, shaping the experiences for Ukrainian older women (but also older men) and influencing disclosure of HIV status and likely engagement in HIV care.
Conclusion
In this study, we explored the accounts of 30 newly diagnosed OPWH in Ukraine, examining their experiences of HIV diagnosis as a dynamic process that challenges identity and self-image for OPWH yet moves toward perceiving age as a strength and HIV diagnosis as a foundation for personal growth. Characterizing this early period after diagnosis through an established framework provides a unique opportunity for developing interventions to improve linkage to care, ART initiation, and reduction of observed high mortality.
Supplementary Material
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental Material for this article is available online at journals.sagepub.com/home/qhr. Please enter the article’s DOI, located at the top right hand corner of this article in the search bar, and click on the file folder icon to view.
References
- Allen AZO, Postnov O, Rozanova J, Litz T, Zaviryukha I, Kiriazova T, & Shenoi S (2020a). Correlates of antiretroviral therapy initiation among newly diagnosed older people with HIV [unpublished abstract]. Ukrainian Institute for Public Health Policy. [Google Scholar]
- Allen AZO, Postnov O, Rozanova J, Litz T, Zaviryukha I, Kiriazova T, & Shenoi S (2020b). Correlates of lost to follow-up among newly diagnosed older people with HIV in Ukraine [unpublished abstract]. Ukrainian Institute of Public Health Policy. [Google Scholar]
- Altschuler J, Katz AD, & Tynan M (2004). Developing and implementing an HIV/AIDS educational curriculum for older adults. The Gerontologist, 44(1), 121–126. 10.1093/geront/44.1.121 [DOI] [PubMed] [Google Scholar]
- Altschuler J, Katz AD, & Tynan MA (2008). Implications for HIV/AIDS research and education among ethnic minority older adults. Journal of HIV/AIDS & Social Services, 7(3), 209–228. 10.1080/15381500802307476 [DOI] [Google Scholar]
- Atkinson J, Nilsson Schönnesson L, Williams M, & Timpson S (2008). Associations among correlates of schedule adherence to antiretroviral therapy (ART): A path analysis of a sample of crack cocaine using sexually active African–Americans with HIV infection. AIDS Care, 20(2), 253–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Autenrieth CS, Beck EJ, Stelzle D, Mallouris C, Mahy M, & Ghys P (2018). Global and regional trends of people living with HIV aged 50 and over: Estimates and projections for 2000-2020. PLOS ONE, 13(11), Article e0207005. 10.1371/journal.pone.0207005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beuthin RE, Bruce A, & Sheilds L (2015). Storylines of aging with HIV: Shifts toward sense making. Qualitative Health Research, 25(5), 612–621. [DOI] [PubMed] [Google Scholar]
- Blyumina A (2005). Population ageing in Ukraine: Some demographic, socioeconomic, and Medicare issues. https://ukraine.unfpa.org/sites/default/files/pub-pdf/Population%20Ageing%20in%20Ukraine%20%282005%29%20%28EN%29.pdf [Google Scholar]
- Chen D, Duan L, Chen X, Zhang Q, Chen Y, Yuan Z, & Li X (2020). Coping strategies and associated factors among older Chinese people living with HIV/AIDS. Psychology, Health & Medicine, 25(7), 898–907. [DOI] [PubMed] [Google Scholar]
- Chen Y, Peng Y, Xu H, & O’Brien WH (2018). Age differences in stress and coping: Problem-focused strategies mediate the relationship between age and positive affect. The International Journal of Aging and Human Development, 86(4), 347–363. [DOI] [PubMed] [Google Scholar]
- Chiao EY, Ries KM, & Sande MA (1999). AIDS and the elderly. Clinical Infectious Diseases, 28(4), 740–745. [DOI] [PubMed] [Google Scholar]
- Colborne M (2017). Ukrainians battle escalating HIV epidemic. Canadian Medical Association Journal, 189(26), E901–E902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolgova V, & Rokitskaya Y (2020). Factor structure of coping behavior of curious elderly people. Advances in Gerontology = Uspekhi Gerontologii, 33(1), 172–178. [PubMed] [Google Scholar]
- Dudina VI, King EJ, & Tsareva AV (2020). Concealing an HIV-positive status in medical settings: Discussions in Russian online forums. Qualitative Health Research, 30(9), 1379–1391. [DOI] [PubMed] [Google Scholar]
- Emlet CA (2006a). A comparison of HIV stigma and disclosure patterns between older and younger adults living with HIV/AIDS. AIDS Patient Care STDS, 20(5), 350–358. 10.1089/apc.2006.20.350 [DOI] [PubMed] [Google Scholar]
- Emlet CA (2006b). “You’re awfully old to have this disease”: Experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. The Gerontologist, 46(6), 781–790. 10.1093/geront/46.6.781 [DOI] [PubMed] [Google Scholar]
- Emlet CA (2007). Experiences of stigma in older adults living with HIV/AIDS: A mixed-methods analysis. AIDS Patient Care STDS, 21(10), 740–752. 10.1089/apc.2007.0010 [DOI] [PubMed] [Google Scholar]
- Emlet CA (2008). Truth and consequences: A qualitative exploration of HIV disclosure in older adults. AIDS Care, 20(6), 710–717. 10.1080/09540120701694014 [DOI] [PubMed] [Google Scholar]
- Emlet CA, & Berghuis JP (2002). Service priorities, use, and needs: Views of older and younger consumers living with HIV/AIDS. Journal of Mental Health and Aging, 8, 307–318. [Google Scholar]
- Emlet CA, Tozay S, & Raveis VH (2011). “I’m not going to die from the AIDS”: Resilience in aging with HIV disease. The Gerontologist, 51(1), 101–111. 10.1093/geront/gnq060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang X, Vincent W, Calabrese SK, Heckman TG, Sikkema KJ, Humphries DL, & Hansen NB (2015). Resilience, stress, and life quality in older adults living with HIV/AIDS. Aging & Mental Health, 19(11), 1015–1021. 10.1080/13607863.2014.1003287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S (2010). Stress, health, and coping: Synthesis, commentary, and future directions. In Folkman S (Ed.), The Oxford handbook of stress, health, and coping (pp. 453–462). Oxford University Press. [Google Scholar]
- Folkman S, Lazarus RS, Pimley S, & Novacek J (1987). Age differences in stress and coping processes. Psychology and Aging, 2(2), Article 171. [DOI] [PubMed] [Google Scholar]
- Fumaz CR, Ayestaran A, Perez-Alvarez N, Munoz-Moreno JA, Molto J, Ferrer MJ, & Clotet B (2015). Resilience, ageing, and quality of life in long-term diagnosed HIV-infected patients. AIDS Care, 27(11), 1396–1403. 10.1080/09540121.2015.1114989 [DOI] [PubMed] [Google Scholar]
- Furlotte C, & Schwartz K (2017). Mental health experiences of older adults living with HIV: Uncertainty, stigma, and approaches to resilience. Canadian Journal on Aging/La Revue canadienne du vieillissement, 36(2), 125–140. [DOI] [PubMed] [Google Scholar]
- Girardi E, Sabin CA, & Monforte AD (2007). Late diagnosis of HIV infection: Epidemiological features, consequences and strategies to encourage earlier testing. Journal of Acquired Immune Deficiency Syndromes, 46(Suppl. 1), S3–S8. 10.1097/01.qai.0000286597.57066.2b [DOI] [PubMed] [Google Scholar]
- Goodkin K, Heckman T, Siegel K, Linsk N, Khamis I, Lee D, Lecusay R, Poindexter CC, Mason SJ, & Suarez P (2003). Putting a face” on HIV infection/AIDS in older adults: A psychosocial context. Journal of Acquired Immune Deficiency Syndromes, 33(Suppl. 2), S171–S184. [PubMed] [Google Scholar]
- Graham LJ (2015). Integration of the interaction model of client health behavior and transactional model of stress and coping as a tool for understanding retention in HIV care across the lifespan. Journal of the Association of Nurses in AIDS Care, 26(2), 100–109. [DOI] [PubMed] [Google Scholar]
- Graneheim UH, & Lundman B (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. [DOI] [PubMed] [Google Scholar]
- Hanass-Hancock J, Myezwa H, & Carpenter B (2015). Disability and living with HIV: Baseline from a cohort of people on long term ART in South Africa. PLOS ONE, 10(12), Article e0143936. 10.1371/journal.pone.0143936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman TG, Barcikowski R, Ogles B, Suhr J, Carlson B, Holroyd K, & Garske J (2006). A telephone-delivered coping improvement group intervention for middle-aged and older adults living with HIV/AIDS. Annals of Behavioral Medicine, 32(1), 27–38. [DOI] [PubMed] [Google Scholar]
- Heckman TG, Kochman A, Sikkema K, Kalichman S, Masten J, Bergholte J, & Catz S (2001). A pilot coping improvement intervention for late middle-aged and older adults living with HIV/AIDS in the USA. AIDS Care, 13(1), 129–139. [DOI] [PubMed] [Google Scholar]
- Heckman TG, Sikkema KJ, Hansen N, Kochman A, Heh V, Neufeld S, & The AIDS and Aging Research Group. (2011). A randomized clinical trial of a coping improvement group intervention for HIV-infected older adults. Journal of Behavioral Medicine, 34(2), 102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson SJ, Bernstein LB, George DM, Doyle JP, Paranjape AS, & Corbie-Smith G (2004). Older women and HIV: How much do they know and where are they getting their information? Journal of the American Geriatrics Society, 52(9), 1549–1553. 10.1111/j.1532-5415.2004.52421.x [DOI] [PubMed] [Google Scholar]
- HIV and AIDS in Ukraine. (2020). Avert. https://www.avert.org/printpdf/node/2201 [Google Scholar]
- Horter S, Thabede Z, Dlamini V, Bernays S, Stringer B, Mazibuko S, Dube L, Rusch B, & Jobanputra K (2017). “Life is so easy on ART, once you accept it”: Acceptance, denial and linkage to HIV care in Shiselweni, Swaziland. Social Science & Medicine, 176, 52–59. 10.1016/j.socscimed.2017.01.006 [DOI] [PubMed] [Google Scholar]
- How Kyiv fights the HIV/AIDS epidemic. (2017). AFEW International. [Google Scholar]
- Hughes AK, & Lewinson TD (2015). Facilitating communication about sexual health between aging women and their health care providers. Qualitative Health Research, 25(4), 540–550. [DOI] [PubMed] [Google Scholar]
- Illa L, Echenique M, Jean GS, Bustamante-Avellaneda V, Metsch L, Mendez-Mulet L, Eisdorfer C, & Sanchez-Martinez M (2010). Project ROADMAP: Reeducating older adults in maintaining AIDS prevention: A secondary intervention for older HIV-positive adults. AIDS Education and Prevention, 22(2), 138–147. 10.1521/aeap.2010.22.2.138 [DOI] [PubMed] [Google Scholar]
- Jackson F, Early K, Schim SM, & Penprase B (2005). HIV knowledge, perceived seriousness and susceptibility, and risk behaviors of older African Americans. Journal of Multicultural Nursing & Health, 11(1), Article 56. [Google Scholar]
- Kahana E, & Kahana B (2001). Successful aging among people with HIV/AIDS. Journal of Clinical Epidemiology, 54(Suppl. 1), S53–S56. 10.1016/s0895-4356(01)00447-4 [DOI] [PubMed] [Google Scholar]
- Kiriazova T, Postnov O, Bingham T, Myers J, Flanigan T, Vitek C, & Neduzhko O (2018). Patient and provider perspectives inform an intervention to improve linkage to care for HIV patients in Ukraine. BMC Health Services Research, 18(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk JB, & Goetz MB (2009). Human immunodeficiency virus in an aging population, a complication of success. Journal of the American Geriatrics Society, 57(11), 2129–2138. 10.1111/j.1532-5415.2009.02494.x [DOI] [PubMed] [Google Scholar]
- Lazarus R, & Folkman S (1984). Stress, appraisal, and coping. Springer. [Google Scholar]
- Leblanc NM, Flores DD, & Barroso J (2016). Facilitators and barriers to HIV screening: A qualitative meta-synthesis. Qualitative Health Research, 26(3), 294–306. [DOI] [PubMed] [Google Scholar]
- Libanova E (2014). Situation of older women in Ukraine [Analytical report]. Ukraine Centre for Social Reforms, United Nations Population Fund. [Google Scholar]
- Lindbom SJ, Larsson M, & Agardh A (2017). The naked truth about HIV and risk taking in Swedish prisons: A qualitative study. PLOS ONE, 12(7), Article e0182237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutsenko AM (2020). Coping strategies and personality profile characteristics of people whose parents were alcohol addicts. Behavioral Sciences, 10(1), Article 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes CA, & Louis M (2003). Knowledge of AIDS, perceived risk of AIDS, and at-risk sexual behaviors among older adults. Journal of the American Academy of Nurse Practitioners, 15(11), 509–516. 10.1111/j.1745-7599.2003.tb00340.x [DOI] [PubMed] [Google Scholar]
- Martin CP, Fain MJ, & Klotz SA (2008). The older HIV-positive adult: A critical review of the medical literature. The American Journal of Medicine, 121(12), 1032–1037. [DOI] [PubMed] [Google Scholar]
- Mazhnaya A, Meteliuk A, Barnard T, Zelenev A, Filippovych S, & Altice FL (2017). Implementing and scaling up HCV treatment services for people who inject drugs and other high risk groups in Ukraine: An evaluation of programmatic and treatment outcomes. International Journal of Drug Policy, 47, 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health of Ukraine. (2015). Ukraine country progress report 2015. https://www.unaids.org/sites/default/files/country/documents/UKR_narrative_report_2015.pdf [Google Scholar]
- Moskowitz JT, Hult JR, Bussolari C, & Acree M (2009). What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin, 135(1), 121–141. 10.1037/a0014210 [DOI] [PubMed] [Google Scholar]
- Nachega JB, Hsu AJ, Uthman OA, Spinewine A, & Pham PA (2012). Antiretroviral therapy adherence and drug-drug interactions in the aging HIV population. AIDS, 26(Suppl. 1), S39–S53. 10.1097/QAD.0b013e32835584ea [DOI] [PubMed] [Google Scholar]
- Nam SL, Fielding K, Avalos A, Dickinson D, Gaolathe T, & Geissler PW (2008). The relationship of acceptance or denial of HIV-status to antiretroviral adherence among adult HIV patients in urban Botswana. Social Science & Medicine, 67(2), 301–310. 10.1016/j.socs-cimed.2008.03.042 [DOI] [PubMed] [Google Scholar]
- Orel N, Spence M, & Steele J (2005). Getting the message out to older adults: Effective HIV health education risk reduction publications. Journal of Applied Gerontology, 24,490–508. 10.1177/0733464805279155 [DOI] [Google Scholar]
- Pitts M, Grierson J, & Misson S (2005). Growing older with HIV: A study of health, social and economic circumstances for people living with HIV in Australia over the age of 50 years. AIDS Patient Care STDs, 19(7), 460–465. 10.1089/apc.2005.19.460 [DOI] [PubMed] [Google Scholar]
- Ranjit YS, Azbel L, Krishnan A, Altice FL, & Meyer JP (2019). Evaluation of HIV risk and outcomes in a nationally representative sample of incarcerated women in Azerbaijan, Kyrgyzstan, and Ukraine. AIDS Care, 31(7), 793–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remien RH, Exner T, Kertzner RM, Ehrhardt AA, Rotheram-Borus MJ, Johnson MO, Weinhardt LS, Kittel LE, Goldstein RB, & Pinto RM (2006). Depressive symptomatology among HIV-positive women in the era of HAART: A stress and coping model. American Journal of Community Psychology, 38(3), 275–285. [DOI] [PubMed] [Google Scholar]
- Romaniuk P, & Semigina T (2018). Ukrainian health care system and its chances for successful transition from Soviet legacies. Globalization and Health, 14(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfeld D, Catalan J, Ridge D, & HIV and Later Life (HALL) Team. (2018). Strategies for improving mental health and wellbeing used by older people living with HIV: A qualitative investigation. AIDS Care, 30(Suppl. 2), 102–107. [DOI] [PubMed] [Google Scholar]
- Rozanova J (2018, July 23–27). Newly increasing HIV incidence among adults aged 50 years or older in Ukraine [Poster, Abstract, Conference session]. International AIDS Conference, Amsterdam, The Netherlands. [Google Scholar]
- Rozanova J, Shenoi S, Zaviryukha I, Zeziulin O, Kiriazova T, Rich K, Mamedova E, & Yariy V (2020). Social support is key to retention in care during COVID-19 pandemic among older people with HIV and substance use disorders in Ukraine. Substance Use & Misuse, 55(11), 1902–1904. 10.1080/10826084.2020.1791183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubtsova AA, Kempf M-C, Taylor TN, Konkle-Parker D, Wingood GM, & Holstad MM (2017). Healthy aging in older women living with HIV infection: A systematic review of psychosocial factors. Current HIV/AIDS Reports, 14(1), 17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar A, Nevedal A, Neufeld S, Berry R, & Luborsky M (2011). What do we know about older adults and HIV? A review of social and behavioral literature. AIDS Care, 23(10), 1187–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- See CM, & Essau CA (2010). Coping strategies in cross-cultural comparison. In Mayer B & Kornadt H-J (Eds.), Psychologie–Kultur–Gesellschaft (pp. 161–173). Springer. [Google Scholar]
- Siegel K, Raveis V, & Karus D (1998). Perceived advantages and disadvantages of age among older HIV-infected adults. Research on Aging, 20(6), 686–711. 10.1177/0164027598206004 [DOI] [Google Scholar]
- Siegel K, & Schrimshaw EW (2002). The perceived benefits of religious and spiritual coping among older adults living with HIV/AIDS. Journal for the Scientific Study of Religion, 41(1), 91–102. [Google Scholar]
- Slomka J, Lim J-W, Gripshover B, & Daly B (2013). How have long-term survivors coped with living with HIV? Journal of the Association of Nurses in AIDS Care, 24(5), 449–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon P, O’Brien K, Wilkins S, & Gervais N (2014). Aging with HIV and disability: The role of uncertainty. AIDS Care, 26(2), 240–245. 10.1080/09540121.2013.811209 [DOI] [PubMed] [Google Scholar]
- Tan J, Altice FL, Madden LM, & Zelenev A (2020). Effect of expanding opioid agonist therapies on the HIV epidemic and mortality in Ukraine: A modelling study. The Lancet HIV, 7(2), e121–e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torsch VL, & Ma GX (2000). Cross-cultural comparison of health perceptions, concerns, and coping strategies among Asian and Pacific Islander American elders. Qualitative Health Research, 10(4), 471–489. [DOI] [PubMed] [Google Scholar]
- UNAIDS. (2020). Eastern Europe and Central Asia, https://www.unaids.org/en/regionscountries/easterneuropeand-centralasia [Google Scholar]
- Vance DE, & Woodley RA (2005). Strengths and distress in adults who are aging with HIV: A pilot study. Psychological Reports, 96(2), 383–386. 10.2466/pr0.96.2.383-386 [DOI] [PubMed] [Google Scholar]
- Velika O, Volosevich I, & Savchyk D (2021). Antiretroviral therapy, comorbidity and quality of life of HIV-infected elderly people: Optimization of treatment and prevention of complications, https://www.phc.org.ua/sites/default/files/users/user90/PHLWH50%2B_report.pdf [Google Scholar]
- Vitek CR, Čakalo J-I, Kruglov YV, Dumchev KV, Salyuk TO, Božičević I, Baughman AL, Spindler HH, Martsynovska VA, & Kobyshcha YV (2014). Slowing of the HIV epidemic in Ukraine: Evidence from case reporting and key population surveys, 2005–2012. PLOS ONE, 9(9), Article e103657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Regional Office for Europe, European Centre for Disease Prevention and Control. (2017). Surveillance report: HIV/AIDS surveillance in Europe 2016. https://www.ecdc.europa.eu/sites/portal/files/documents/20171127-Annual_HIV_Report_Cover+Inner.pdf [Google Scholar]
- Xu Y, Lin X, Chen S, Liu Y, & Liu H (2018). Ageism, resilience, coping, family support, and quality of life among older people living with HIV/AIDS in Nanning, China. Global Public Health, 13(5), 612–625. 10.1080/17441692.2016.1240822 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.