Abstract
Introduction:
Anterior fractures of the tibial plateau are either compression or avulsion injuries. Anterior compression fractures of the tibial plateau (ACFT) are rare being traditionally described as involving the rim and often associated with ligament injuries. We have presented 7seven cases of the “large’’ type of ACFT, an uncommon pattern of ACFT.
Materials and Methods:
7Seven cases of large type ACFTs were identified on retrospectively analyzing the institutional database from 2014 to 2019. The bony and ligamentous injury patterns, fixation, and functional outcomes of these cases have been analyzed.
Results:
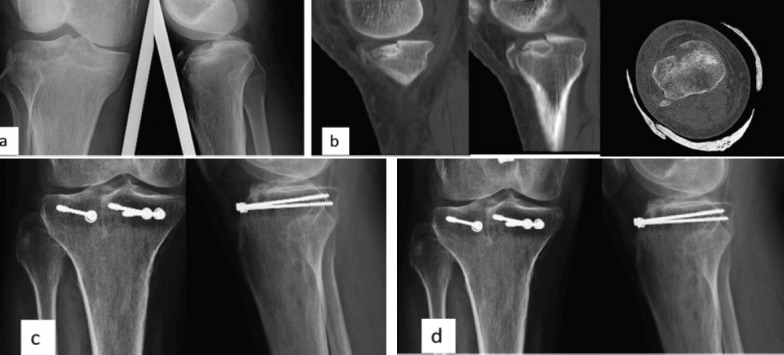
All were males with a mean age of 40 years. Along with the bony injury, we had posterior cruciate ligament (PCL) injuries in three cases and anterior cruciate ligament ACL with medial collateral ligament (MCL) injury in two cases. Our protocol was bony fixation first and later ligament reconstruction based upon knee instability pattern. The locking plates were used in 4 cases and screw fixation in three cases. One patient underwent PCL and MCL reconstruction and another patient underwent PCL reconstruction. The mean union time was 13 weeks. The mean ROM was 128° degrees. Rasmussen’s clinical and radiological scores showed good to an excellent outcome (Mean scores: 28.42, 8.7). No patients had apparent instability at follow-up on clinical examination and stress X-rays.
Conclusion:
Large ACFTs are rare and associated with anterior joint depression and ligament injuries. Their management significantly differs from that of small type ACFTs (Rim compression injuries) where only ligament reconstruction is needed. Recognition of this pattern is essential for the appropriate management and good functional outcome.
Keywords: Tibial plateau fracture, anterior compression fracture, knee ligament injury, rim compression injury, staged protocol
Learning Point of the Article:
Large Anterior compression fractures of the tibial plateau are rare and associated with anterior joint depression and ligament injuries. Prompt recognition is necessary for appropriate management.
Introduction
The understanding of tibial plateau fractures and the principles and techniques of treating them have been continuously evolving over the years. The tendency of these fractures to be associated with ligament injuries, vascular compromise, compartment syndrome, and secondary knee osteoarthritis has attracted a lot of research interest on the personality of fractures over the years [1, 2, 3].
The well-recognized patterns involve the saggital components of the tibial plateau the medial and lateral condyles [2]. The most commonly used Schatzker classification system is based on these saggital components. The description of the posterior coronal component and its significance in affecting the final functional outcome of tibial plateau fractures have been of recent interest which led to the acceptance of column-based classification systems [4]. However, the anterior coronal components of tibial plateau fractures remain less explored.
The anterior tibia is mainly involved in hyperextension injuries [5]. Anterior rim compression fractures described by Moore, are relatively rare and associated with ligament injuries [6]. Chiba et al. classified the Anterior Compression Fractures of the Tibial Plateau (ACFT) into two types - large and small fractures based on the amount of involvement of the tibial plateau [7]. We have presented seven large types of ACFT, which are rare types of anterior compression fractures. We have analyzed the pattern of bony and ligament injury, the line of management that we followed, and the functional outcomes in these cases along with the review of the literature.
Materials and Methods
After institutional ethical committee approval, our hospital data from Picture Archiving and Communication System and Healthlink™ database between January 2014 and January 2019 were analyzed. In the axial cut of Computed Tomography (CT), those fractures involved the anterior half of the proximal tibia - either medial or the lateral column without the involvement of the posterior column according to Luo’s three-column concept [8], were taken into account. Patients more than 18 years and <60 years of age were considered. Open knee injuries and polytrauma cases were excluded from the study. The bony and ligamentous injury patterns, fixation, and functional outcomes of these cases were analyzed.
Results
Three thousand and fifty-eighty proximal tibia cases operated at our institute during the study period of which seven cases of ACFT were identified. These injuries accounted for only 0.2% of the total tibial plateau fractures presented at our institute in 6 years.
Demographic data
All were male patients. The mean age of our cases was 40 years (range from 28 to 56 years). The mode of injury was the Road Traffic Accident (RTA) in six cases and fall while running in one case. Among the RTA victims, five cases had motor vehicle crash against another vehicle. One patient had a history of falls from the two-wheeler. The mean time of presentation at the hospital was 50 h (Range 4-96 h). Patients had no neuro-vascular injury at the time of the presentation. After a radiographic initial assessment, patients underwent CT of the affected knee joint. Magnetic Resonance Imaging (MRI) was taken at initial assessment only for the last four of the seven patients. All patients had primary bony stabilization. The internal fixation was done after the subsidence of the swelling to an extent. The mean day of internal fixation was the 4th day after injury; (Range 2-7 days). During follow-up, clinical assessments for instability were routinely done and stress X-rays were taken for unstable knees. Persistent residual instability was addressed surgically. Functional outcome at follow-up was graded using clinical Rasmussen’s score [9]. Radiological parameters were assessed using the radiological Rasmussen’s score. Our patients had a variable pattern of ligament injuries (Table 1).
Table 1.
Fracture pattern, fixation method used, associated ligament injuries, and outcome scores in our patients
Methods of fixation
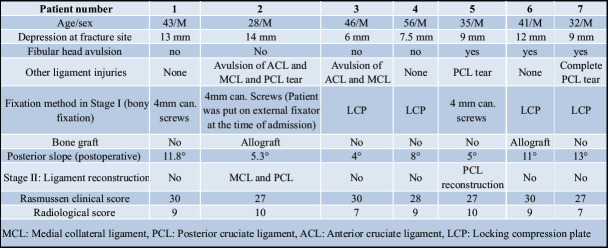
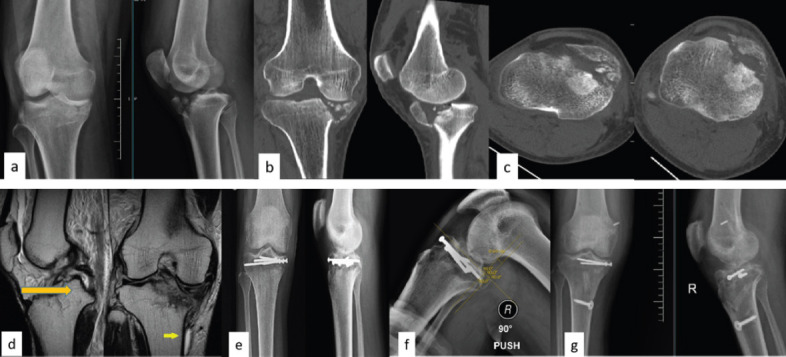
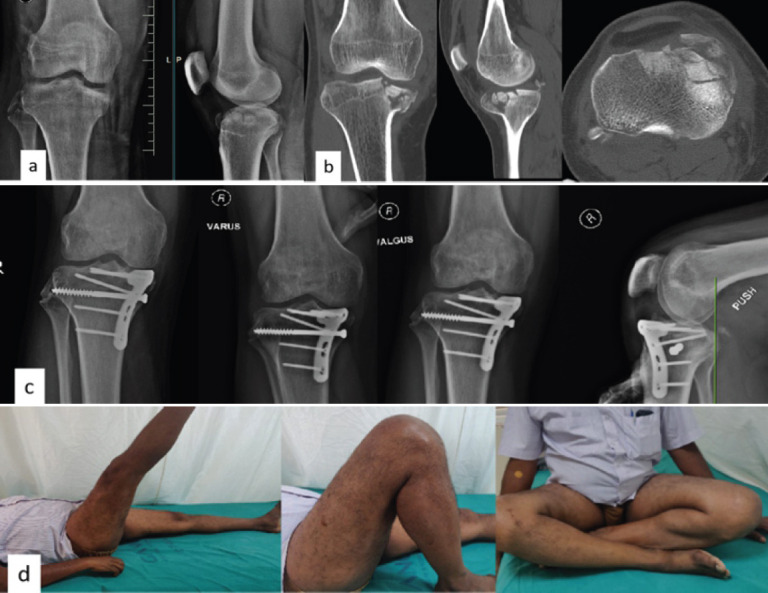
One case (Patient number 2 Table 1) had a high-velocity injury and presented as a subluxated knee. The subluxation was corrected and a knee spanning external fixator was applied in stage 1 followed by internal fixation in Stage 2 and posterior cruciate ligament (PCL) and medial collateral ligament (MCL) reconstruction because of persistent instability in Stage 3 (Fig. 1). All other cases underwent direct internal fixation as Stage 1. All cases had anterior joint depression with a mean depression of 10.1 mm as calculated on coronal CT at the point of maximum joint depression. Elevation of joint depression was done in all cases. Comminution was seen in three cases. In these cases, the elevation of joint depression was done through the fracture site, and locking compression plate (LCP) was used for fixation (Fig. 2). Allograft was used to fill the void in two of those cases. In one case where the fracture fragment was large, LCP was used for fixation. The other three cases were with minimal or no comminution. The anatomical posterior slope was achieved by reducing the anterior fracture fragments and fixing them with cancellous screws (Fig. 1 and 3). Anterior cruciate ligament (ACL) and MCL avulsions were addressed at the time of bony fixation. Fibular head avulsions were undisplaced and hence treated conservatively. Stainless steel implants were used in four cases and titanium implants were used in the other three cases.
Figure 1.
Case 1: Preoperative X-ray (a) and CT images (b and c) showing large anterior compression fracture of tibia, MRI images showing PCL and MCL tear (d), Postoperative X-ray (e) PCL stress X-ray showing posterior subluxation (f), and Post PCL and MCL reconstruction X-ray (g). PCL: Posterior cruciate ligament, MCL: Medial collateral ligament
Figure 2.
Case 3: Pre-operative X-ray (a) and CT (b) showing large anterior compression fracture of the tibia and fibular head fracture, Post-operative X-rays showing fracture union and stable joint on valgus, varus, and posterior stress ©, Follow-up pictures showing good knee ROM (d).
Figure 3.
Case 2: Preoperative X-ray (a) and CT images (b) showing large anterior compression fracture of the tibia. Immediate postoperative (c) and 2 years follow-up X-ray (d).
Patients were put on a knee brace fixed in 0° flexion and advised non-weight bearing walking for 4 weeks. Knee mobilization and partial weight-bearing walking were advised from the 5th week. Full weight-bearing walking was advised after 8 weeks from the time of surgery.
During each follow-up, patients were assessed clinically and radiologically using stress X-rays for knee instability. Two patients (patient number 2, 5 - Table 1) had posterior instability at follow-up - on posterior drawer test. They were initially started on quadriceps exercises. Full weight-bearing walking on a knee brace was advised. Because of persistent instability, later they underwent ligament reconstruction. The patient (Patient number 2 Table 1) with grade III posterior instability also had a grade II medial opening on valgus stress. Posterolateral corner instability was not present clinically. That Patient underwent PCL and MCL reconstruction 5 months after the index procedure (Fig. 1). The patient with isolated posterior instability underwent PCL reconstruction 4 months after the index procedure. The average duration of follow-up was 31 months (Range 12-60 months). Restoration of the anatomical tibial posterior slope had been achieved in all cases [10]. The mean anatomical posterior slope on the post-operative radiograph was 8.3° (Range 4-13° - Table 1). The patients were followed up at 2, 4, 8, 12, 16, and 20 weeks postoperatively, then once in 3 months. The mean union time was 13 weeks (range 8–20 weeks). The mean knee range of flexion was 128° (range 110–140°). We had no neurovascular injury or infection in the post-operative period in any of our patients. Rasmussen’s clinical and radiological scores showed good to an excellent outcome (Table 1). The mean clinical Rasmussen score was 28.42 (range 27–30). The mean radiological Rasmussen score was 8.7 (range 7–10). None of our cases had significant secondary arthritic changes at the final follow-up (i.e., progression by grade 1 or no progression in radiological Rasmussen score).
Discussion
All our cases involved more than one-fourth of the anterior diameter of the tibial plateau. In 2001 Chiba et al. [7], in their article classified the compression fractures involving the anterior part of the tibial plateau into two groups small involving less than a quarter of the anteroposterior diameter of the tibial plateau and large, involving more than a quarter of the anteroposterior diameter of the tibial plateau. They concluded that a small compression fracture of the medial tibial plateau was more often associated with postero-lateral corner and PCL injuries. In their series of twelve patients, they had four large anteromedial fractures. Of those, one patient had no ligament injury; two patients had an ACL injury and one patient had both ACL and PCL injuries. Management of such large fractures was however not discussed by Chiba et al.
All our patients fit into a large ACTF group. There were associated ligament injuries in 5 out of our 7 cases. In addition to ligament injuries, there was the involvement of a larger portion of the tibial plateau in these fractures with articular depression. Such a pattern necessitated elevation, accurate reduction, and fixation of bony parts with or without bone graft followed by the management of ligament injuries. In small anteromedial rim compression fractures, however, the management of ligament injuries is crucial. Reports on small anterior rim compression fractures are relatively abundant [7, 11, 12, 13] when compared to those on large anterior compression fractures [7, 14].
Tomás-Hernández et al. [14] in their series of three large anterior compression fractures reported good functional outcomes after single-stage bony and ligament reconstruction. This study, to our best knowledge, is the only study that has classified and described the anterior tibial plateau fracture after Chiba et al. All three cases were associated with postero-lateral corner injuries without cruciate ligament injuries. They noted hyper-extension varus injuries in all their cases. Maheshwari et al. [15] described a series of eight cases which they referred to as anterior tibial condyle fractures. They operated upon four cases that had associated PCL injuries. They, however, did not classify them as small or large fractures.
The primary mechanism of injury in our series was hyperextension. Based on the radiological features and ligament involvement two cases seemed to be of pure hyperextension type injuries (Fig. 3). One patient had MCL avulsion. Mechanism of injury in those cases should have been hyper-extension and valgus. This is similar to that in reverse second fractures [16, 17]. Three of our cases had fibular head avulsion where the mechanism must have been hyper-extension and varus force [18]. The exact sequence of various forces on the tibia at the time of injury could not be postulated in our series as six out of these seven cases were road traffic accidents.
One notable finding in our study is the level of fibular head avulsion. The fibular head avulsion generally involves the fibular styloid with the resulting avulsion of the arcuate complex comprising of the popliteo-fibular ligament, arcuate ligament, and the Fabello-fibular ligament known as arcuate sign [19, 20, 21]. Avulsion of the head of the fibula at a lower level is seen in our cases. This involves avulsion of the lateral collateral ligament and the biceps femoris tendon rather than the arcuate complex [18, 22]. The association between arcuate sign and postero-lateral corner and PCL injuries has been widely described, the mechanism of injury being the hyperextension and varus type [18, 23]. However, the ligament injuries associated with the fibular head avulsion at a slightly lower level have not been clearly described in literature [22, 24]. Association between such LCL avulsion fractures and common peroneal nerve palsy has been described as ligamentous peroneal nerve syndrome or the lateral compartment syndrome of the knee [22, 25]. In our series, two of three cases with fibular head avulsion had PCL injuries. Common peroneal nerve was not involved in our cases. There was no involvement of the posterolateral corner in these fractures. Avulsion at a level lower than the attachment of the arcuate complex could have taken the force off the arcuate complex thus preserving the posterolateral corner structures. Such displaced fibula head fractures have been fixed surgically, while conservative management also has yielded good results in undisplaced fractures [24, 26, 27, 28]. In our cases, all fibula head fractures united at follow-up without any varus laxity.
Reports on the single-stage treatment of associated ligament injuries and tibial plateau fractures are very few [14, 29]. Difficulty in implant positioning and complications such as soft tissue insult and compartment syndrome have been described while adopting such strategies [29, 30, 31]. In line with these recommendations, we followed staged management. Bony injuries were addressed first. We followed an expectant conservative line of management as the ligament injuries are concerned. If instability is persistent we surgically intervened. There was no significant difference in mobilization protocols between our group and that of Tomás-Hernández et al. where primary surgical management of ligament injuries has been done. A good personalized rehabilitation program has resulted in a good range of movements in follow-up in all our patients. One patient had only 110° ROM in our study because of improper adherence to physiotherapy.
The role of MRI in routine preoperative evaluation of ligament injuries in tibial plateau fractures is doubtful [32, 33]. However, in compression fractures where chances of associated ligament injuries are high, MRI would help us document and manage the associated ligament injuries. Hence, we adopted preoperative MRI as a routine practice for the last four of our cases.
A low number of cases in our study can be explained by the rarity of such fractures. We believe our study will add up to available scientific knowledge and will help in better understanding and management of these injuries.
Conclusion
Large anterior compression fractures of the tibial plateau are rare and often associated with anterior joint depression and associated ligament injuries. Their management significantly differs from that of small type anterior rim compression fractures where only ligament reconstruction is needed. Primary bony stabilization for the fracture is a priority and staged management is essential for a good outcome.
Clinical Message.
1. The large anterior rim compression fractures are a rare type of tibial plateau fractures
2. These anterior rim compression fractures involve a larger part of the anterior tibia when compared to the more common small anterior rim compression fractures; These are also associated with a range of ligament injuries.
3. Management involves bony reconstruction followed by ligament reconstruction.
4. Recognition of this pattern is essential for appropriate staged management and good functional outcome.
Declaration of patient consent : The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s parents have given their consent for patient images and other clinical information to be reported in the journal. The patient’s parents understand that his names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of interest:Nil Source of support:None
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Shepherd L, Abdollahi K, Lee J, Vangsness CT., Jr The prevalence of soft tissue injuries in nonoperative tibial plateau fractures as determined by magnetic resonance imaging. J Orthop Trauma. 2002;16:628–31. doi: 10.1097/00005131-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Cole P, Levy B, Schatzker J, Watson JT. Tibial plateau fractures. In: Browner B, Levine A, Jupiter J, Trafton P, Krettek C, editors. Skeletal Trauma:Basic Science Management and Reconstruction. Philadelphia, PA: WB Saunders Co; 2009. pp. 2201–87. [Google Scholar]
- 3.The Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures:Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006;88:2613–23. doi: 10.2106/JBJS.E.01416. [DOI] [PubMed] [Google Scholar]
- 4.Zhang BB, Sun H, Zhan Y, He QF, Zhu Y, Wang YK, et al. Reliability and repeatability of tibial plateau fracture assessment with an injury mechanism-based concept. Bone Joint Res. 2019;8:357–66. doi: 10.1302/2046-3758.88.BJR-2018-0331.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzalez LJ, Lott A, Konda S, Egol KA. The hyper-extension tibial plateau fracture pattern:A predictor of poor outcome. J Orthop Trauma. 2017;31:e369–74. doi: 10.1097/BOT.0000000000000930. [DOI] [PubMed] [Google Scholar]
- 6.Moore TM. Fracture-dislocation of the knee. Clin Orthop Relat Res. 1981;156:128–40. [PubMed] [Google Scholar]
- 7.Chiba T, Sugita T, Onuma M, Kawamata T, Umehara J. Injuries to the posterolateral aspect of the knee accompanied by a compression fracture of the anterior part of the medial tibial plateau. Arthroscopy. 2001;17:642–7. doi: 10.1053/jars.2001.22362. [DOI] [PubMed] [Google Scholar]
- 8.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–92. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen PS. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–50. [PubMed] [Google Scholar]
- 10.Nekkanti S, Patted P, Nair LM, Chandru V, Shashank G. The variation of the posterior tibial slope in South Indians:A hospital-based study of 290 cases. Niger J Orthop Trauma. 2018;17:17–21. [Google Scholar]
- 11.Bennett DL, George MJ, El-Khoury GY, Stanley MD, Sundaram M. Anterior rim tibial plateau fractures and posterolateral corner knee injury. Emerg Radiol. 2003;10:76–83. doi: 10.1007/s10140-003-0298-z. [DOI] [PubMed] [Google Scholar]
- 12.Cohen AP, King D, Gibbon AJ. Impingement fracture of the anteromedial tibial margin:A radiographic sign of combined posterolateral complex and posterior cruciate ligament disruption. Skeletal Radiol. 2001;30:114–6. doi: 10.1007/s002560000309. [DOI] [PubMed] [Google Scholar]
- 13.Yoo JH, Kim EH, Yim SJ, Lee BI. A case of compression fracture of the medial tibial plateau and medial femoral condyle combined with posterior cruciate ligament and posterolateral corner injury. Knee. 2009;16:83–6. doi: 10.1016/j.knee.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 14.Tomás-Hernández J, Monyart JM, Serra JT, Vinaixa MR, Farfan EG, García VM, et al. Large fracture of the anteromedial tibial plateau with isolated posterolateral knee corner injury:Case series of an often missed unusual injury pattern. Injury. 2016;47(Suppl 3):S35–40. doi: 10.1016/S0020-1383(16)30604-0. [DOI] [PubMed] [Google Scholar]
- 15.Maheshwari J, Pandey V, Mhaskar V. Anterior tibial plateau fracture:An often missed injury. Indian J Orthop. 2014;48:507. doi: 10.4103/0019-5413.139871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hall FM, Hochman MG. Medial Segond-type fracture:Cortical avulsion off the medial tibial plateau associated with tears of the posterior cruciate ligament and medial meniscus. Skeletal Radiol. 1997;26:553–5. doi: 10.1007/s002560050285. [DOI] [PubMed] [Google Scholar]
- 17.Escobedo EM, Mills WJ, Hunter JC. The reverse Segond fracture:Association with a tear of the posterior cruciate ligament and medial meniscus. AJR Am J Roentgenol. 2002;178:979–83. doi: 10.2214/ajr.178.4.1780979. [DOI] [PubMed] [Google Scholar]
- 18.Huang GS, Yu JS, Munshi M, Chan WP, Lee CH, Chen CY, et al. Avulsion fracture of the head of the fibula:MR imaging findings predictive of injuries to the posterolateral ligaments and posterior cruciate ligament. AJR Am J Roentgenol. 2003;180:381–7. doi: 10.2214/ajr.180.2.1800381. [DOI] [PubMed] [Google Scholar]
- 19.Shindell R, Walsh WM, Connolly JF. Avulsion fracture of the fibula:The “arcuate sign”of posterolateral knee instability. Nebra Med J. 1984;69:369–71. [PubMed] [Google Scholar]
- 20.Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982;64:536–41. [PubMed] [Google Scholar]
- 21.Laprade RF, Bollom TS. Anatomy and biomechanics of the posterolateral aspect of the knee. In: Fanelli GC, editor. Posterior Cruciate Ligament Injuries:A Practical Guide to Management. New York: Springer-Verlag; 2001. pp. 23–46. [Google Scholar]
- 22.Capps GW, Hayes CW. Easily missed injuries around the knee. Radiographics. 1994;14:1191–210. doi: 10.1148/radiographics.14.6.7855335. [DOI] [PubMed] [Google Scholar]
- 23.Juhng SK, Lee JK, Choi SS, Yoon KH, Roh BB, Won JJ. MR evaluation of the “arcuate”sign of posterolateral knee instability. AJR Am J Roentgenol. 2002;178:583–8. doi: 10.2214/ajr.178.3.1780583. [DOI] [PubMed] [Google Scholar]
- 24.Chytas A, Spyridakis A, Gigis J, Beslikas T, Panos N, Christoforidis J. A rare case of traumatic bilateral fibular head fractures. Case Rep Med. 2010;2010:920568. doi: 10.1155/2010/920568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Towne LC, Blazina ME, Marmor L, Lawrence JF. Lateral compartment syndrome of the knee. Chin Orthop. 1971;76:160–1. doi: 10.1097/00003086-197105000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Sharma B, Parmar RS, Kapoor K, Verma R. Presentation and options in the management of avulsion fracture fibular head:A prospective study of a rare entity. Int J Orthop Sci. 2017;3:677–82. [Google Scholar]
- 27.Phadnis A, Johnston P, Glasgow M. Avulsion of the fibular head post-total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1340–2. doi: 10.1007/s00167-007-0309-9. [DOI] [PubMed] [Google Scholar]
- 28.Rawes ML, Roberts J, Dias JJ. Bilateral fibula head fractures complicating an epileptic seizure. Injury. 1995;26:562. doi: 10.1016/0020-1383(95)00086-o. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y, Wang L, Zhu T, Liu Z, Liu G. Open reduction and internal fixation in a one-stage anterior cruciate ligament reconstruction [Google Scholar]
- 30.Caspari RB, Hutton PM, Whipple TL, Meyers JF. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy. 1985;1:76–82. doi: 10.1016/s0749-8063(85)80035-9. [DOI] [PubMed] [Google Scholar]
- 31.Abdel-Hamid MZ, Chang CH, Chan YS, Lo YP, Huang JW, Hsu KY, et al. Arthroscopic evaluation of soft tissue injuries in tibial plateau fractures:Retrospective analysis of 98 cases. Arthroscopy. 2006;22:669–75. doi: 10.1016/j.arthro.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 32.Aurich M, Koenig V, Hofmann G. Comminuted intraarticular fractures of the tibial plateau lead to posttraumatic osteoarthritis of the knee:Current treatment review. Asian J Surg. 2018;41:99–105. doi: 10.1016/j.asjsur.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 33.Warner SJ, Garner MR, Schottel PC, Fabricant PD, Thacher RR, Loftus ML, et al. The effect of soft tissue injuries on clinical outcomes after tibial plateau fracture fixation. J Orthop Trauma. 2018;32:141–7. doi: 10.1097/BOT.0000000000001042. [DOI] [PubMed] [Google Scholar]