Abstract
In recent years, there has been growing interest in “moving beyond the individual” to measure area-level racism as a social determinant of health. Much of this work has aggregated racial prejudice data collected at the individual-level to the area-level. As this is a rapidly emerging area of research, we conducted a systematic literature review to describe evidence of the relationship between area-level racial prejudice and health, whether associations differed by race/ethnicity, and to characterize key conceptual and methodological considerations to guide future research. We searched four interdisciplinary databases for US-based, peer-reviewed articles measuring area-level racial prejudice by aggregating individual-level indicators of racial prejudice and examining associations with mental or physical health outcome(s). Data extraction followed PRISMA guidelines and also included theory and conceptualization, pathways to health, and strengths and limitations. Fourteen of 14,632 identified articles met inclusion criteria and were included in the review. Health outcomes spanned all-cause (n=4) and cause-specific (n=4) mortality, birth outcomes (n=4), cardiovascular outcomes (n=2), mental health (n=1), and self-rated health (n=1). All studies found a positive association between area-level racial prejudice and adverse health outcomes among racial/ethnic minoritized groups, with four studies also showing a similar association among Whites. Engagement with formal theory was limited and exposure conceptualization was mixed. Methodological considerations included unmeasured confounding and trade-offs between generalizability, self-censorship, and specificity of measurement. We suggest directions for future research to further develop the conceptual and methodological rigor of this work and inform evidence-based interventions to advance population health and reduce racial health inequities.
Keywords: Systematic review, racism, area-level, racial prejudice, health disparities
Racism is a fundamental driver of health inequities (Feagin, 2013; Gee & Ford, 2011; Harrell, 2000; Jones, 2000; Phelan & Link, 2015; Williams et al., 2019). Racism manifests in various forms, including, but not limited to, structural (i.e., institutional laws, policies, and practices), cultural (i.e., dominant ideological attitudes and beliefs about the relative value of different social groups) and personally-mediated (i.e., racial discrimination occurring in a variety of settings); each of which independently and interactively shape the distribution of societal risks, resources, and opportunities by race (Jones, 2000; Williams et al., 2019).
While the majority of research to-date has focused on self-reported experiences of racial discrimination, there has been growing interest in “moving beyond the individual” to measure community-level racial prejudice as a social determinant of health (Blair & Brondolo, 2017). One increasingly popular method involves measuring individual-level racial prejudice, aggregating to the area-level to capture the variation in racial prejudice across geographies, and examining associations with health outcomes and inequities (Chae et al., 2015; Chae et al., 2018; Hehman et al., 2018; Huang et al., 2020; Kennedy et al., 1997; Lee et al., 2015; Leitner et al., 2016a, 2016b; McKetta et al., 2017; Morey et al., 2018; Nguyen et al., 2018; Orchard & Price, 2017).
The rising popularity of this approach may be attributed to several factors, including: limitations of self-report for measuring exposure to racial discrimination, which can result in nonlinear and heterogeneous findings of associations with health outcomes (Allen et al., 2019; Paradies, 2006); a growing recognition of the role of structural and cultural racism in the production of health inequities (Bailey et al., 2017; Gee & Ford, 2011; Geronimus et al., 2016; Williams et al., 2019); interest in place-based determinants of racial differences in health (Chetty & Hendren, 2018); and the rise of big data in social science and health research (Mooney et al., 2015; Stephens-Davidowitz & Pabon, 2017). As this rapidly emerging area of research develops, a systematic and critical review of the evidence-to-date including an examination of the conceptual foundations and methodological considerations can help guide future research.
The purpose of this study was to systematically review all United States (US)-based, empirical, peer-reviewed studies examining the association between aggregated measures of area-level racial prejudice and health. Our primary research question was: what is the association between area-level racial prejudice and health outcomes in the US, and are associations differential by race/ethnicity? Secondary research questions were: (1) what theories or conceptual models frame the research?; (2) what are the hypothesized and empirically tested mediating and moderating pathways to health?; and (3) what are the primary measurement and other methodological challenges of this developing body of work?
Data and Methods
All study procedures follow Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009) and were preregistered: https://osf.io/vsze4/.
Search Strategy
We conducted an interdisciplinary search across the following electronic databases: (1) PubMed, (2) SCOPUS, (3) PsycInfo, and (4) Sociological Abstracts. Search terms were developed iteratively based on a preliminary review of the literature, research team expertise, and consultation with a public health research librarian.
Inclusion criteria were: (a) peer-reviewed journal article; (b) quantitative empirical study; (c) US-based; (d) English language; (e) study exposure is an indicator of bias, prejudice, animus, attitudes, sentiment, or beliefs toward or about a particular racial, ethnic, or immigrant group(s) that is measured at the individual-level and aggregated to the area-level; (f) study exposure is assessed using data from (1) surveys, questionnaires, or assessment tools, (2) social media, or (3) Google searches; and (g) study outcome is a mental or physical health outcome or health behavior. We utilized Covidence (Innovation, 2016) for managing references.
For the purpose of this review, racial prejudice was defined as “differential assumptions about the abilities, motives, and intentions of others according to their race” (Jones, 2000, p. 1212). While the terminology used differs across the literature, we considered any measure of sentiment, attitude, belief, animus, prejudice, or cognitive (but not behavioral) bias toward or about specific racial, ethnic, and immigrant group(s) under the construct of “racial prejudice” when measured at the individual-level, and “area-level racial prejudice” when aggregated to the area-level. Note that prejudice is distinct from discrimination in that the former pertains to cognitive and affective aspects of racism whereas the latter describes its behavioral manifestation (Jones, 2000). We excluded studies aggregating instances of interpersonal or institutional discrimination (e.g., hate crimes, housing or workplace discrimination) to keep the scope of the review narrowly focused on the cognitive and affective (i.e., prejudice) rather than the behavioral (i.e., discrimination) dimensions of racism. While much of the research in this area has focused on anti-Black racism, there is evidence documenting the unique manifestations, and harmful effects, of prejudice against various racial and ethnic groups in the US (Gee et al., 2009; Novak et al., 2017). Therefore, we included studies of aggregated prejudice against, and potential health consequences among, multiple racial/ethnic groups. We also included measures of anti-immigrant prejudice because people often conflate race/ethnicity with immigration status and immigrants often experience racism (Viruell-Fuentes et al., 2012).
We performed our database search on April 5, 2020. After removal of duplicates, 14,632 records proceeded to title and abstract screening, of which 32 advanced to full-text review, and 14 met inclusion criteria. Figure 1 shows the results of these exclusions.
Figure 1.
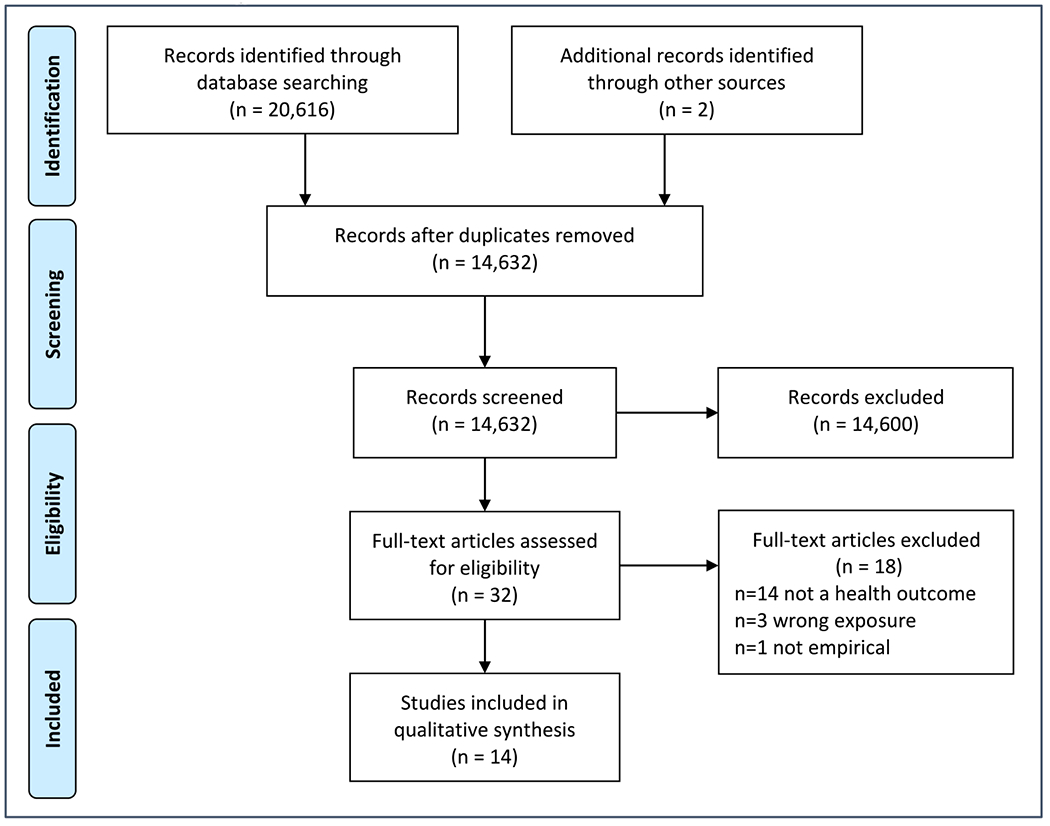
Prisma Flow Diagram
Data Extraction
Using MaxQDA (Software, 2019), we extracted data in accordance with PRISMA guidelines (Moher et al., 2009). We also extracted data for our specific research questions. First, we were interested in conceptualization and framing: how were investigators thinking about area-level racial prejudice in relation to existing conceptual models for racism and health? Second, we extracted data on empirically tested mediation and moderation of the association between area-level racial prejudice and health outcomes. We were particularly interested in whether any association between area-level racial prejudice and health differed by race/ethnicity. Finally, we extracted data on key measurement and other methodological considerations.
All data extraction variables and the data extraction codebook were determined a-priori based on PRISMA guidelines and research questions. Two independent reviewers performed all screening and data-extraction, meeting regularly to build consensus. Any disagreements were resolved via consult with a third investigator. Our detailed methodology, including search strings and data extraction codebook, are shown in Appendix A.
Results
Characteristics of Included Studies
Table 1 displays the characteristics of studies included in the review; detailed results are presented in Appendix B. Across studies, area-level racial prejudice was examined using one of four data sources: the General Social Survey (GSS) (n=3) (Kennedy et al., 1997; Lee et al., 2015; Morey et al., 2018), Project Implicit (n=4) (Hehman et al., 2018; Leitner et al., 2016a, 2016b; Orchard & Price, 2017), Google Trends (n=3) (Chae et al., 2015; Chae et al., 2018; McKetta et al., 2017), and Twitter (n=4) (Hswen, 2020; Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018). Studies examined a variety of health outcomes, including birth outcomes (n=4) (Chae et al., 2018; Nguyen et al., 2020; Nguyen et al., 2018; Orchard & Price, 2017), all-cause mortality (n=4) (Chae et al., 2015; Kennedy et al., 1997; Lee et al., 2015; Morey et al., 2018), cause-specific mortality (n=4) (Chae et al., 2015; Hehman et al., 2018; Leitner et al., 2016a, 2016b), cardiovascular disease (CVD) and related risk factors (n=2) (Huang et al., 2020; Leitner et al., 2016a), mental health outcomes (n=1) (Hswen, 2020), and self-rated health (n=1) (McKetta et al., 2017). Ten of the fourteen studies explored whether associations between area-level racial prejudice and health were differential by racial/ethnic group, either by comparing race/ethnicity-specific rates (Kennedy et al., 1997; Nguyen et al., 2020; Nguyen et al., 2018) or by testing for statistical interaction between area-level racial prejudice and race/ethnicity (Huang et al., 2020; Lee et al., 2015; Leitner et al., 2016a, 2016b; McKetta et al., 2017; Morey et al., 2018; Orchard & Price, 2017). The remaining four studies were restricted to one racial/ethnic group (Chae et al., 2015; Chae et al., 2018; Hehman et al., 2018; Hswen, 2020). Two studies explored mediators on the pathway to health (Lee et al., 2015; Leitner et al., 2016a).
Table 1.
Characteristics of Included Studies (N=14)
Note: DMA = designated market area (geographic area receiving similar media and news), CBSA = core-based statistical area (similar to metropolitan statistical area), PSU = primary sampling unit (comprised of metropolitan statistical areas and non-metropolitan counties) (Morey et al., 2018).
Cross-sectional: exposure and outcome examined at one time-point only, even if the exposure preceded the outcome; Prospective: exposure precedes outcome and there are multiple outcome assessments on each study participant; Time-series analysis: changes in group-level rates (not necessarily the same study participants) over time.
Multilevel: area-level exposure and individual-level outcomes, analyzed using analytic methods that account for clustered data; Individual: exposure and outcome analyzed at individual-level and methods do not account for clustering (i.e., exposure is measured at the area-level but the unit of analysis is the individual); Ecologic: exposure and outcome analyzed at area-level. Individual-level variables may be used in creation of area-level outcome (e.g., age-standardized death rates), but the unit of analysis is the area (e.g., state, county).
Sum is >100% because categories are not mutually exclusive.
Reflects number of individuals included in outcome assessment. NAs are for studies where outcome was expressed as area-level rates and no individual-level sample sizes were provided. Sample sizes and number aggregated in exposure assessments are shown Appendix B.
Includes any study that examined whether the association between area-level racial prejudice was differential or non-differential by racial/ethnic/immigrant group. This included formal tests of interaction with or without simple slopes or stratified subgroup analysis, stratified subgroup analyses without a formal test of interaction, or examining race-specific rates at the area-level.
Overview of Data Sources Used to Measure Area-Level Racial Prejudice
See Appendix C for more details of these data sources:
General Social Survey
The General Social Survey (GSS) is a nationally representative survey of social and political attitudes among non-institutionalized English-speaking adults living in the US, conducted on a random sample of the eligible population at each wave (Davis & Schwartzman, 1973) (years available: 1972-2018). Examples of racial prejudice questions include: “Do Blacks tend to be unintelligent or tend to be intelligent?”, and “Do Blacks tend to be hard working or lazy?” (Lee et al., 2015). Anti-immigrant prejudice is assessed based on agreement with statements like “America should take stronger measures to exclude illegal immigrants,” and “Immigrants increase crime rates” (Morey et al., 2018). These questions are used to create composite measures of racial prejudice (Kennedy et al., 1997; Lee et al., 2015) or anti-immigrant prejudice (Morey et al., 2018), which are then aggregated to the area-level.
Project Implicit
Project Implicit provides a free, online tool for assessing implicit and explicit biases toward various social groups (e.g., Black vs. White or gay vs. straight people) (years available: 2002-present) (Nosek et al., 2010). Implicit racial bias is assessed via the “Implicit Association Test” (IAT), a timed dual-categorization task which measures the speed of keyboard associations between images of Black versus White faces and positive versus negative words. Faster reaction time matching positive words with White and negative words with Black faces indicates cognitive dissonance between Black people and positive emotions, which is interpreted as an anti-Black and/or pro-White implicit bias (Hehman et al., 2018). Explicit bias is assessed via self-reported feelings of warmth or coldness toward Black/African American versus White/European American persons, and relative preference for the two groups (Hehman et al., 2018). Studies using Project Implicit data aggregate implicit and explicit biases separately to the area-level, either for all respondents (Orchard & Price, 2017) or for subgroups of respondents (e.g., Whites’ racial bias) (Hehman et al., 2018; Leitner et al., 2016a, 2016b).
Google Trends
Google search data come from Google Trends (2020), a publicly available dashboard where users can query the relative popularity of various search terms in specific geographic areas and time periods (years available: 2004-present). The data used in the included studies describe the popularity of Google searches for the “n-word” (ending in “-er(s)” but not “-a(s)”) across 196 designated market areas (DMAs) from 2004-2007 (pooled). DMAs are geographic areas receiving similar media from television, radio, newspapers, and Internet sources.
Twitter data can be collected prospectively (Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018) or retrospectively (Hswen, 2020) (years available: 2006-present). Investigators can filter results to include Tweets that reference particular racial/ethnic groups and use a combination of hand-coding, natural language processing, and machine learning to characterize the sentiment (positive, negative, neutral) of Tweets referencing each group (Hswen, 2020; Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018). Using the latitude and longitude coordinates or other “place” information (e.g., city and state), investigators can geocode tweets to the area where they originated.
Summary of Study Findings
Measures of area-level racism across multiple data sources were associated with a range of health outcomes, including CVD and related risk factors (Huang et al., 2020; Leitner et al., 2016a), adverse birth outcomes (Chae et al., 2018; Nguyen et al., 2020; Nguyen et al., 2018; Orchard & Price, 2017), increased mortality (Chae et al., 2015; Hehman et al., 2018; Kennedy et al., 1997; Lee et al., 2015; Leitner et al., 2016a, 2016b; Morey et al., 2018), and poor self-reported mental (Hswen, 2020) and physical health (McKetta et al., 2017). Although the overall pattern of results consistently showed a positive relationship between area-level racial prejudice and adverse health, the magnitude of association varied across studies (see Appendix B3). A direct comparison of effect sizes across studies is hindered by different exposure specifications (e.g., continuous vs categorical), measures of association estimated (e.g., beta coefficients vs odds ratios vs prevalence ratios, etc.), and other design features.
Evidence of differential health effects of racial prejudice by race/ethnicity was mixed: some studies found effects that were unique to, or more pronounced among, racial/ethnic minoritized groups; others showed no distinctions between racial/ethnic minoritized groups compared to Whites. In this review, we define the effects of area-level racial prejudice on health to be differential by race/ethnicity if the p-value on the test for multiplicative interaction (i.e., race*area-level racial prejudice) was <0.05, following the threshold used in the reviewed studies and authors’ interpretations of their results. If no test for interaction was performed, we considered the effects to be differential if the race/ethnicity-specific measure of association differed by >10%, a rule-of-thumb for a meaningful difference in epidemiologic quantities (Jewell, 2003).
Evidence of Differential Effects by Race/Ethnicity
Among the ten studies that explored whether effects were differential by race/ethnicity, six found evidence of effect modification.
Of these, two showed harmful but less pronounced effects among Whites compared to racial/ethnic minoritized groups (Kennedy et al., 1997; Leitner et al., 2016a). First, Kennedy et al. (1997) found that states with higher versus lower “collective disrespect” (based on GSS data) had higher Black and White mortality rates; however, these relationships were stronger for Black compared to White rates. Second, using data from White Project Implicit respondents aggregated to the county-level, Leitner and colleagues (2016a) found a positive association between Whites’ explicit pro-White/anti-Black bias and circulatory disease death rates among Black and White residents, with stronger associations for Black rates.
One study showed that area-level racial prejudice may be protective for Whites. Using Project Implicit data, Orchard & Price (2017) found that the Black-White gap in preterm birth and low birthweight was positively associated with county-level racial prejudice. Most of the racial difference in this association was driven by poorer outcomes among Black birthing persons; however, White birthing persons showed slightly better outcomes in counties with higher levels of explicit anti-Black/pro-White racial prejudice.
Using data from the GSS, Morey et al. (2018) constructed a measure of anti-immigrant “community-level prejudice” within metropolitan statistical areas and non-metropolitan counties (Morey et al., 2018). Authors found that area-level anti-immigrant prejudice was not associated with mortality for study respondents overall, nor for White or Black respondents, regardless of whether they were US- or foreign-born. However, US-born “other race” respondents (mostly Hispanics and Asians) living in areas with higher levels of anti-immigrant prejudice had increased mortality rates compared to foreign-born respondents of those ethnicities.
Leitner et al. (2016b) found evidence of race differences that depended on the specification of the study exposure. Authors examined county-level “ingroup” racial bias (i.e., preference for one’s own racial group over the other group based on data from Project Implicit) in relation to circulatory disease mortality among Black and White persons. In counties where Black respondents from Project Implicit harbored more implicit ingroup bias (i.e., pro-Black/anti-White), Black residents died from circulatory disease at a higher rate; whereas in counties where White respondents harbored more explicit ingroup bias (i.e., pro-White/anti-Black), White residents died from circulatory disease at a higher rate.
Using Twitter-characterized measures of racial sentiment, Huang et al. (2020) found race-differential associations that depended on the cardiovascular outcome under consideration. Among non-Hispanic White and Black respondents, Twitter-characterized negative sentiment toward racial/ethnic minoritized groups was most strongly associated with hypertension, myocardial infarction, and CVD. In contrast, among Hispanic respondents, Twitter-characterized negative sentiment toward racial/ethnic minoritized groups was most strongly associated with diabetes, obesity, and stroke.
Findings of Non-Differential Effects by Race/Ethnicity
The remaining four studies that explored effect modification by race/ethnicity showed associations between area-level prejudice and health outcomes that were similar in direction and magnitude (i.e., non-differential) for White as compared with racial/ethnic minoritized groups (Lee et al., 2015; McKetta et al., 2017; Nguyen et al., 2020; Nguyen et al., 2018). Lee et al. (2015) found that area-level prejudice, assessed as a composite measure from the GSS racial attitudes questions, was associated with increased mortality risk among both Black and White GSS respondents. McKetta et al. (2017) found that the state-level popularity of Google searches containing the “n-word” was associated with poor self-rated health among both White and Black Panel Study of Income Dynamics respondents, and no statistically significant interaction with race was observed. Using Twitter data, Nguyen and colleagues found that birthing persons living in states with higher levels of negative (Nguyen et al., 2020), or lower levels of positive (Nguyen et al., 2020; Nguyen et al., 2018), racial sentiment had more adverse birth outcomes, with similarly harmful effects observed among racially minoritized and White persons.
Within-Group Studies
The remaining studies examined outcomes among one racial/ethnic group only, precluding an examination of differential effects (Chae et al., 2015; Chae et al., 2018; Hehman et al., 2018; Hswen, 2020). Chae and colleagues found that in DMAs with a greater popularity of Google searches for “n-word,” Black residents experienced higher rates of all-cause and cause specific mortality (2015) and adverse birth outcomes (2018). Hehman et al. (2018) found that Black residents were killed by police at disproportionate rates relative to their population shares in metropolitan areas where White Project Implicit respondents demonstrated greater implicit and explicit pro-White/anti-Black racial bias. Finally, using Twitter data at the national level, Hswen et al. (2020) found that the percent of negative sentiment tweets mentioning Mexicans and Hispanics was associated with increased daily worry among those identifying as Hispanic during the 20-week period surrounding the 2016 US presidential election.
Theory, Conceptualization, and Proposed Pathways to Health
Several studies referenced theories in their introduction or discussion sections, including “structural stigma” (Morey et al., 2018, p. 56) and “fundamental causes” (Huang et al., 2020, p. 888); however, there was minimal incorporation of the theories and their constructs in the interpretation of the study findings. Few studies formally defined area-level racial prejudice or how it was understood in relation to existing models of racism (Huang et al., 2020; McKetta et al., 2017; Morey et al., 2018). However, the general framing and stated motivation for the studies provided insight into authors’ conceptualization of the exposure.
This conceptualization fell into two categories: (1) area-level racial prejudice as a proxy for the attitudes and actions of prejudiced individuals, with pathways to health occurring via personally-mediated racial discrimination and its consequences or (2) area-level racial prejudice as a broader measure of prejudiced social contexts, with pathways to health occurring at multiple social-ecologic levels. These two conceptualizations were not mutually-exclusive (i.e., some studies described both) and were not specific to the data source or indicator used (i.e., identical measures of area-level racial prejudice were described as measures of prejudiced individuals or prejudiced contexts depending on the study). Pathways were generally explicated in hypothetical terms either in the introduction to provide social and/or biological plausibility for justifying the research question, or in the discussion to explain findings and make recommendations for future work. These pathways are synthesized in Figure 2.
Figure 2.
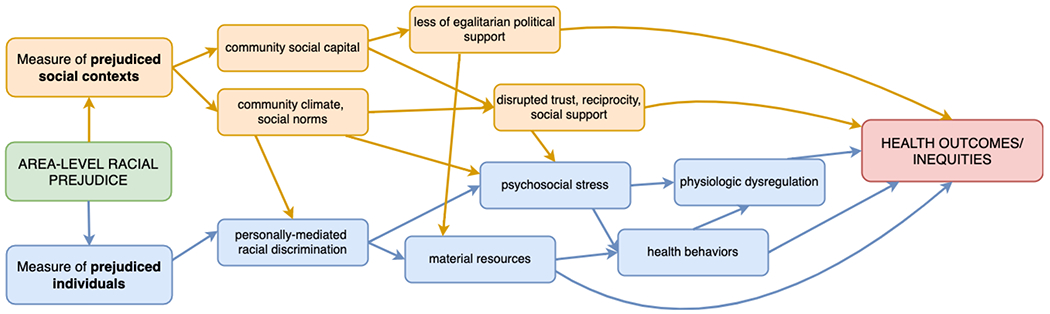
Proposed Pathways Linking Area-Level Racial Prejudice with Health
Measuring Prejudiced Individuals
Many authors described racial discrimination as a key determinant of health but noted limitations of traditional survey instruments which ask individuals to recall past experiences of racially motivated discrimination in various settings. These experiences may be underreported on surveys due to the subtlety of contemporary racism, attributional ambiguity, internalized racism, and the influence of coping style on reporting (Chae et al., 2015; Chae et al., 2018; Hswen, 2020; Leitner et al., 2016a; Morey et al., 2018; Nguyen et al., 2020), which may result in inconsistent or under-estimated effects of racial discrimination on health (Chae et al., 2015; Chae et al., 2018; Hswen, 2020; Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018).
The use of data from the GSS, Project Implicit, Google Trends, and Twitter was described as a strategy to directly assess the racial prejudice of individuals in a defined geographic area, which may serve as a proxy for exposure to racial discrimination, without relying on study respondents to self-report those experiences (Chae et al., 2015; Chae et al., 2018; Leitner et al., 2016a, 2016b). An added benefit of the IAT, Google Trends, and Twitter (as opposed to the explicit measures of racial prejudice from the GSS and Project Implicit) is they do not require prejudiced individuals to openly disclose prejudiced attitudes, which may also be underreported due to self-censorship and social desirability bias (Chae et al., 2018; Hswen, 2020; Huang et al., 2020; McKetta et al., 2017; Nguyen et al., 2020).
The stated or unstated assumption of these studies was that racial/ethnic minoritized groups living in areas where a greater proportion of individuals harbored racial prejudice would be at increased risk of experiencing racial discrimination. For example, Chae and colleagues (2015, p. 3) noted: “an Internet search-based measure of area racism may serve as a more direct indicator of racial attitudes and the extent of discrimination and prejudice towards Blacks in a geographic area, including those experiences of racially motivated bias that are subtle or not observable, and which are not necessarily reported in survey instruments.”
Racial discrimination, in turn, was posited to harm health via biopsychosocial, behavioral, and material mechanisms, as shown in Figure 2. Authors described racial discrimination and intergroup tension as psychosocial stressors that cause increased anger, anxiety, and chronic physiological stress adaption, all of which disrupt key regulatory systems and undermine health (Chae et al., 2015; Chae et al., 2018; Huang et al., 2020; Lee et al., 2015; Leitner et al., 2016a, 2016b; McKetta et al., 2017; Nguyen et al., 2020; Nguyen et al., 2018; Orchard & Price, 2017). They also described how this stress can lead to maladaptive coping behaviors, such as poor diet and exercise (Chae et al., 2015; Chae et al., 2018; Huang et al., 2020; Lee et al., 2015; Leitner et al., 2016a; Nguyen et al., 2020; Orchard & Price, 2017). Lastly, authors described how racial discrimination in institutional settings (e.g., employment and housing) limits economic opportunities and material resources needed to achieve optimal health (Chae et al., 2015; Chae et al., 2018; Leitner et al., 2016a; McKetta et al., 2017; Nguyen et al., 2020; Nguyen et al., 2018), or harms health directly in the case of healthcare discrimination (Chae et al., 2018; Leitner et al., 2016a; Nguyen et al., 2020; Orchard & Price, 2017).
Pathways were described in hypothetical terms but remained largely unexamined, with a few exceptions (Leitner et al., 2016a; Orchard & Price, 2017). Orchard & Price (2017) found that birth outcomes were more strongly associated with the racial prejudice in the county of birth compared to the county of residence, hypothesizing that racial bias in county of birth may proxy healthcare discrimination. Leitner et al. (2016a) found that the association between Whites’ racial prejudice and circulatory disease inequities was not mediated by Black-White differences in smoking, drinking, and exercise, suggesting non-behavioral factors must be considered.
Measuring Prejudiced Social Contexts
Others argued that the self-reported measures of racial discrimination commonly used in the literature may fail to account for macro-level manifestations of racism (Hehman et al., 2018; Huang et al., 2020; Kennedy et al., 1997; Lee et al., 2015; McKetta et al., 2017; Morey et al., 2018; Nguyen et al., 2020), and therefore may under-estimate the total effects of racism on health (Huang et al., 2020; Morey et al., 2018; Nguyen et al., 2020). In these studies, measuring area-level racial prejudice was motivated by a desire to rise above the level of the individual (Blair & Brondolo, 2017) and capture the broader social context (Hehman et al., 2018; Hswen, 2020; Huang et al., 2020; Kennedy et al., 1997; Lee et al., 2015; McKetta et al., 2017; Morey et al., 2018; Nguyen et al., 2020; Nguyen et al., 2018) in which prejudiced attitudes and discriminatory behaviors occur (Hehman et al., 2018; Huang et al., 2020; Nguyen et al., 2018). Authors described area-level racial prejudice as capturing “ambient social attitudes” (McKetta et al., 2017, p. 9), “macropsychological characteristics of residents” (Hehman et al., 2018, p. 5), or a “temperature of the social environment” (Nguyen et al., 2018, p. 309). Some conceptualized area-level racial prejudice as a direct manifestation of structural (McKetta et al., 2017; Morey et al., 2018) or cultural (Huang et al., 2020) racism or stigma, the measurement of which could be used to inform structural interventions.
Authors described multiple pathways through which prejudiced social contexts could undermine health. At the community-level, it was hypothesized that area-level racial prejudice would erode community social capital (Kennedy et al., 1997; Lee et al., 2015; Leitner et al., 2016a; Morey et al., 2018; Nguyen et al., 2020; Nguyen et al., 2018; Orchard & Price, 2017), defined as “the norms of reciprocity, trust and social obligation that are essential for minimizing the risks of poor physical, psychological, or social health” (Kennedy et al., 1997, p. 466). An erosion of community social capital may undermine health through (a) reduced trust, bonding, and norms of mutual reciprocity (Kennedy et al., 1997; Lee et al., 2015; Leitner et al., 2016a; Orchard & Price, 2017), (b) less social and emotional support to buffer stressful life events (Nguyen et al., 2018), and (c) less egalitarian political support and commitment to shared resources, resulting in a lack of investment in policies and programs that could enhance the welfare of community members (Kennedy et al., 1997; Leitner et al., 2016a; Nguyen et al., 2020). Indeed, Lee et al. (2015) found that community social capital mediated the association between community-level racial prejudice and mortality.
Prejudiced social contexts were also hypothesized to maintain social norms that are permissive of racial discrimination, which harms health by increasing stress and material deprivation (Huang et al., 2020; Leitner et al., 2016a; Morey et al., 2018; Nguyen et al., 2020). However, authors also described direct effects on health, independent of personally-mediated discrimination; as Nguyen et al. (2020, p. 2) explained: “the social climate of a place represents a complimentary aspect of racial bias and discrimination that may have its own influence on health, independent of individual-level experiences.” Similarly, Morey et al. (2018) described the harms of living in prejudiced communities based not only on cumulative exposure to, but also increased awareness of, racialized attitudes; and Leitner et al. (2016a, p. 2) emphasized how “hostile community environments” could directly evoke stress and harm health.
Measurement and Other Methodological Considerations
Stated limitations noted across multiple studies, regardless of data source, included: unmeasured confounding (Chae et al., 2015; Chae et al., 2018; Lee et al., 2015; Leitner et al., 2016a; McKetta et al., 2017; Orchard & Price, 2017), self-selection into more or less prejudiced environments based on underlying health status (Chae et al., 2015; Chae et al., 2018; Leitner et al., 2016a, 2016b; McKetta et al., 2017; Morey et al., 2018), the inability to establish temporality (Chae et al., 2015; Chae et al., 2018; Hehman et al., 2018; Kennedy et al., 1997; Lee et al., 2015; Leitner et al., 2016b; Nguyen et al., 2018; Orchard & Price, 2017), and unknown mechanisms linking area-level racial prejudice with health outcomes (Chae et al., 2018; Hehman et al., 2018; Huang et al., 2020; Kennedy et al., 1997; Leitner et al., 2016a, 2016b; McKetta et al., 2017; Morey et al., 2018; Nguyen et al., 2018). In addition, the GSS, Project Implicit, Google Trends, and Twitter each presented a unique set of strengths and limitations, which are summarized below and described in more detail in Appendix D.
General Social Survey
Primary advantages of the GSS include national representativeness (Lee et al., 2015; Morey et al., 2018), specificity of racial/anti-immigrant prejudice measures, and detailed information on respondent characteristics which could be used for weighting or assessing the prejudices of specific respondents (although none of the reviewed studies did this). Primary disadvantages of the GSS include self-censorship of socially undesirable attitudes (Lee et al., 2015), subnational non-representativeness (Kennedy et al., 1997), and relatively lower temporal and geographic coverage compared to the other data sources due to not all questions being asked on all survey years (Lee et al., 2015).
Project Implicit
Strengths of Project Implicit include the large amount of data and the ability to measure implicit bias without relying on self-report (Leitner et al., 2016a; Orchard & Price, 2017). Additional advantages include the option to explore or adjust for multiple social biases (weapons stereotype, age, race, or gender bias, etc.) (Hehman et al., 2018; Leitner et al., 2016a; Orchard & Price, 2017), examine characteristics of the test-taker for descriptive, weighting, or stratification purposes (Hehman et al., 2018; Leitner et al., 2016a, 2016b; Orchard & Price, 2017), and compare implicit versus explicit biases (Hehman et al., 2018; Leitner et al., 2016a, 2016b; Orchard & Price, 2017). A major limitation of Project Implicit data is that study respondents are self-selected and may not represent the racial bias in their geographic area of residence (Hehman et al., 2018; Leitner et al., 2016a, 2016b; Orchard & Price, 2017). Several studies used post-stratification weights to increase representativeness with respect age and/or sex, reporting similar results with weighted and unweighted data (Leitner et al., 2016a, 2016b; Orchard & Price, 2017). Finally, using the conventional method of scoring the Project Implicit tests, it is not possible to discern whether a higher implicit bias score is driven by greater pro-White or higher anti-Black bias (Leitner et al., 2016b).
Google Trends
A major strength of Google Trends is that search data do not rely on self-report and therefore may capture more private curiosities and socially undesirable attitudes with more authenticity compared to traditional survey instruments (Chae et al., 2015; Chae et al., 2018; McKetta et al., 2017). Studies using Google data described prior validation work, linking area-level rates of searches for the “n-word” with conceptually related constructs, such as voting (McKetta et al., 2017) and other area-based measures of racial bias (Chae et al., 2015). Authors also cited work linking other search queries to real-world outcomes, such as infectious diseases, religiosity, and gun ownership (Chae et al., 2018; McKetta et al., 2017). The primary limitation of Google Trends is a low degree of measurement specificity. The demographic makeup of users and context of the search is unknown; searches for the “n-word” may not be motivated by racism (Chae et al., 2015; Chae et al., 2018; McKetta et al., 2017). Despite this potential for measurement error, Google Trends provides a high “signal-to-noise ratio” based on the sheer volume of data available (Chae et al., 2015; Chae et al., 2018).
The reach of Twitter was described as a major strength: millions of tweets are sent daily, and a large proportion of users make their profiles public (Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018). Authors also noted that the impersonal nature of Twitter may embolden users to speak more freely about racist attitudes than they may otherwise express during in-person interactions or on a survey (Hswen, 2020; Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018). Other benefits of the platform include the range of individuals, groups, and businesses represented (Nguyen et al., 2018), predictive validity across a number of health topics and outcomes (Hswen, 2020; Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018), and the ability to capture racial sentiment in real-time (Hswen, 2020). Finally, sentiment analysis allows investigators to determine the overall tone of the Tweets referencing racial groups (Hswen, 2020; Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018), offering a major strength over Google Trends data where the context or motivation of the search is entirely unknown (Chae et al., 2015; Chae et al., 2018; McKetta et al., 2017). However, misclassification may occur because sentiment analysis cannot capture sarcasm or humor (Huang et al., 2020; Nguyen et al., 2020; Nguyen et al., 2018). Despite the anonymity of Twitter, self-censorship may still influence what users are willing to post (Nguyen et al., 2020; Nguyen et al., 2018). Finally, demographic makeup of Twitter users is unknown (Huang et al., 2020).
Discussion
To our knowledge, this is the first systematic literature review of studies measuring area-level racial prejudice and examining associations with health outcomes in the United States. Collectively, the fourteen studies reviewed contribute to our growing understanding of racism as a multilevel determinant of health, while also illuminating the need for conceptual development and continued methodological rigor.
Is Area-Level Racial Prejudice Harmful to Health, and for Whom?
This systematic review revealed that area-level racial prejudice, measured using several data sources, was associated with adverse health outcomes—ranging from preterm birth to premature mortality. The magnitude of these associations ranged from subtle to more pronounced; differences in effect sizes could be due to exposure and outcome measurement and specification, estimation procedures, or other study distinctions. More work using standardized measures will be necessary to compare findings across studies. It is also important to note that even small effects, when measured at the structural level, can be societally quite meaningful because they are scaled over large populations.
Evidence of differential associations by race/ethnicity was mixed. Some studies found the health harms of area-level racial prejudice to be unique to, or more pronounced among, minoritized racial/ethnic groups compared to Whites (Kennedy et al., 1997; Leitner et al., 2016a; Morey et al., 2018; Orchard & Price, 2017), whereas others found associations of similar magnitude among racial/ethnic minoritized groups and Whites (Lee et al., 2015; McKetta et al., 2017; Nguyen et al., 2020; Nguyen et al., 2018). Among studies that explored race-specific effects, evidence of racial differences did not depend on study outcome or mode of assessment, sample, geographic scale, or other design features. The extent to which these findings are driven by exposure data source is not clear. For example, the three studies that used Project Implicit data and examined differential effects by race found that White people’s pro-White/anti-Black racial bias was disproportionately associated with adverse health among Black as compared to White residents (Leitner et al., 2016a, 2016b; Orchard & Price, 2017). In contrast, studies using GSS data showed both differential (Kennedy et al., 1997; Morey et al., 2018) and non-differential (Lee et al., 2015) effects by race. Further research is needed to illuminate the conditions underlying whether and to what extent associations between area-level racial prejudice and health differ between racial/ethnic groups.
Findings of differential effects by race/ethnicity are consistent with an understanding of racism as a system of power and oppression that maintains white supremacy and advances the economic, social, and physical wellbeing of Whites through the subordination of racial/ethnic minoritized groups (Feagin, 2013; Harrell, 2000; Phelan & Link, 2015). Findings of non-differential effects by race/ethnicity, in contrast, align with an understanding of inequality and white supremacy as harmful to the health of everyone in society (Malat et al., 2018; Wilkinson, 2001). Another plausible explanation for the lack of race-specificity could be unmeasured confounding driving spurious associations of similar magnitude between area-level racial prejudice and health among all racial and ethnic groups. Resolving this mixed evidence is an important avenue for future research and can inform the development of interventions to improve population health and reduce health inequities.
What is Area-level Racial Prejudice Capturing in Relation to Existing Understandings of Racism, and What are the Pathways to Health?
The reviewed studies framed the exposure as either a proxy for the prevalence of prejudiced individuals in a geographic area, or as a macro-level construct, capturing the broader social context over and above the prejudice of individual actors. This latter conceptualization is consistent with Payne et al.’s (2017) “Bias of Crowds” model, which posits that “implicit bias is best understood as a social phenomenon that passes through the minds of individuals, but exists with greater stability in the situations they inhabit” (p. 236). Building consensus around the conceptualization of this exposure is of top priority for grounding future work in this area.
Theories of cultural racism (Cogburn, 2019; Hicken, 2019; Williams et al., 2019) may advance our understanding of area-level racial prejudice and how it undermines health. Defined as “the instillation of the ideology of inferiority in the values, language, imagery, symbols, and unstated assumptions of the larger society” (Wiliams et al., 2019, p. 110), cultural racism provides a shared framework through which members of society value different racial/ethnic groups. Cultural racism reflects and reinforces structural racism, including institutional practices and policy regimes, which together shape the distribution of resources by race/ethnicity. At the same time, cultural racism creates the prejudice and stereotypes that undergird racial discrimination, a primary source of psychosocial stress and related health outcomes (Williams et al., 2019). Cultural racism may also directly impact health through other forms of racism-related stress, such as vicarious racism (e.g., witnessing or hearing about discrimination against family or friends), vigilance (e.g., bracing oneself in anticipation of experiencing discrimination) and collective experiences (e.g., awareness of discrimination against one’s racial/ethnic group, exposure to harmful media representations) (Harrell, 2000; Hicken, 2019).
Previous research provides insights into the social antecedents and consequences of area-level racial prejudice. For example, evidence suggests that racial prejudice has historical roots in slavery and subsequent structural inequities (e.g., racial residential segregation and Black-White gaps in poverty and social mobility) (Payne et al., 2019), as well as acute racialized social shocks, such as media coverage of the Black Lives Matter movement (Sawyer & Gampa, 2018) and the COVID-19 pandemic (Darling-Hammond et al., 2020). Documented social consequences of areal-level racial prejudice include racial inequities in access to healthcare (Leitner et al., 2016a), self-employment (Kopkin, 2017), and income (Connor et al., 2019). Together, this evidence can be used to inform testable mechanistic hypotheses and deepen the conceptual rigor of future work.
What are the Primary Measurement and Other Methodological Considerations in this Area of Work?
There were several important limitations that prevent drawing causal conclusions from the evidence reviewed. The majority of studies were cross-sectional, examining exposures and outcomes each at one time point only (Chae et al., 2015; Chae et al., 2018; Hehman et al., 2018; Huang et al., 2020; Kennedy et al., 1997; Leitner et al., 2016a, 2016b; Nguyen et al., 2020; Nguyen et al., 2018; Orchard & Price, 2017). Given existing theory and evidence to suggest that higher rates of disease can drive up collective biases (O’Shea et al., 2020), reverse-causation may pose a threat to validity (Hehman et al., 2018). Of note, the few studies that measured health outcomes prospectively provided evidence to support to the hypothesis that living in an area with high levels of racial prejudice may be associated with incident morbidity and premature mortality (Lee et al., 2015; McKetta et al., 2017; Morey et al., 2018).
A related concern is residual confounding, or a “mixing of effects” (Rothman et al., 2008) of area-level racial prejudice with unmeasured macro-level factors that may also influence health (Glymour, 2006). While studies controlled for a variety of population-level sociodemographic variables, it is not possible to measure all of the complex structural and historical processes that likely shape collective prejudice, and drive health outcomes. Last, how do we define “area-level” (neighborhood, school district, city, county, MSA, state), and might higher levels of aggregation beyond neighborhoods obscure heterogeneity in prejudice across places? Future work could compare effects of prejudice at different geographic scales or examine cross-level interactions (e.g., county*state) to inform mechanistic hypotheses and multi-level policy interventions.
Across the four data sources used to measure area-level racial prejudice, there were important trade-offs between (1) representativeness, (2) self-censorship, and (3) specificity of measurement. First, the value of aggregating data from multiple individuals to characterize the racial prejudice in a defined geographic area relies on the assumption that those individuals are representative of the populations in the areas where they reside. The Google and Twitter measures have been described as highly representative, given the broad accessibility of internet access today (Nguyen et al., 2020; Stephens-Davidowitz, 2014). However, according to the Pew Research Center, only about 22% of adults use Twitter (Perrin & Anderson, 2019), and users tend to be younger, more educated, and more progressive than the general population (Wojcik & Hughes, 2019). In addition, Twitter data are restricted to the 83% of users who make their profiles public (Huang et al., 2020; Nguyen et al., 2020; Remy, 2019). It is possible that public users and the content of their tweets differ systematically from other users, which poses a threat to validity. Moreover, while almost all (99%) of public tweets can be geotagged at the state-level, only about 3-4% provide latitude and longitude information needed to examine sentiment at smaller geographic scales.
Project Implicit data are the least representative because respondents are self-selected, with reasons for participation ranging from class assignments and racial bias trainings or pure curiosity (Sakong, 2018). On average, Project Implicit respondents tend to be younger and comprised of more women than the general population (Xu, 2014). To mitigate this concern, some studies implemented post-stratification weights to make county averages more representative based on age and/or sex (Leitner et al., 2016a, 2016b; Orchard & Price, 2017); however, this strategy does not address self-selection based on unmeasured factors, including amount of racial bias (Blair & Brondolo, 2017; Hoover & Dehghani, 2019; Leitner et al., 2016a). Somewhat reassuringly, validation work by Hehman et al. (2019) demonstrated a high degree of convergent validity of unweighted area-level implicit and explicit racial bias data from Project Implicit with racially charged Google searches and nationally representative racial attitude data from the Pew Research Center. The GSS is a nationally-representative survey, but may not be completely representative at smaller geographic scales (Kennedy et al., 1997).
A second consideration is self-censorship of racial prejudice due to social desirability bias, or individuals’ reluctance to report social attitudes they perceive to be unacceptable (Krumpal, 2013). The survey-based measures of explicit racial attitudes from Project Implicit and the GSS are highly subject to self-censorship because they are self-reported. A benefit of the IAT from Project Implicit is that it assesses racial prejudice based on unconscious cognitive associations rather than self-report, thereby mitigating this concern. A major draw of Google and Twitter is that these measures do not rely on self-reported racist attitudes; they discern this information based on the content of people’s tweets and search queries.
Third, specificity of measurement refers to whether the instrument is actually measuring racial prejudice. The IAT from Project Implicit is highly specific: it is a validated measure of racial prejudice and is shown to reliably predict discriminatory behavior across a number of settings (Greenwald et al., 2009; Jost et al., 2009; Nosek et al., 2010); although there is some measurement ambiguity between pro-White from anti-Black bias (Leitner et al., 2016b). The explicit measure of racial bias from Project Implicit and GSS also offer high specificity because they directly ask respondents’ attitudes about race-related topics, but as discussed, are threatened by self-censorship.
While Google and Twitter have high generalizability and low self-censorship compared to the survey-based measures, their validity relies on the assumption that searches and tweets actually reflect racial prejudice. The sentiment analysis used to classify Twitter data may help to evaluate this assumption by enabling the researcher to discern the tone (e.g., positive, negative, or neutral) of the tweets, with the caveat that these algorithms are unable to detect humor, sarcasm, or colloquialisms, potentially resulting in residual misclassification (Huang et al., 2020; Nguyen et al., 2018). With Google, the content and context of the search query is entirely unknown, and it is plausible that the “n-word” is searched for reasons unrelated to racism. A final threat to measurement specificity, shared by Google and Twitter, is the inability to ascertain the racial identity of the user. Whereas Project Implicit and GSS data allow the researcher to perform stratified aggregation capturing area-level prejudice specifically among Whites (i.e., the racial/ethnic group with the most wealth and decision-making power), Google and Twitter data combine the internet activity of all users. To the extent that racially-charged searching and tweeting means something qualitatively different when performed by a White versus racially minoritized individual, the validity of the exposure will be compromised.
No single data source offered superior representativeness, specificity of measurement, and self-censorship. For example, Project Implicit data are the least representative but the most specific. Google and Twitter minimize self-censorship but in doing so, compromise specificity of measurement. These and other trade-offs are summarized in Appendix D. An outstanding question is whether aggregated data from various sources measure the same or different exposures. Factor analysis would be one way to evaluate this question, and if an underlying factor is found, a composite score combining data from multiple sources may be useful for more holistically capturing area-level racial prejudice.
Recommendations for Future Research
This critical review contributes to the growing understanding of racism as a social determinant of health and highlights important directions for future research.
First, there is a pressing need to deepen the conceptual and theoretical rigor of this work. What are these aggregated measures of racial prejudice capturing in relation to the field’s current understanding of racism? Might they be conceptualized as a component or bi-product of cultural racism (Cogburn, 2019; Hicken, 2019; Williams et al., 2019)? Evaluating associations between area-level racial prejudice and other manifestations of cultural racism (e.g., media representations, language and symbols, social norms) would provide useful insight. At the same time, researchers may examine how area-level racial prejudice relates to various dimensions of structural racism (e.g., institutional policies and practices, racial residential segregation), and whether these cultural and structural forces interact to shape social and health inequities.
Second, rooted in theory, future research could incorporate additional data to explore mediation and moderation by community-level demographic, economic, environmental, institutional, and political forces, as well as by individual-level identities, socioeconomic characteristics, and psychosocial, behavioral, and biologic processes.
Third, many of the threats to causal inference identified in this review (e.g., unmeasured confounding, temporality issues) could be mitigated by the use of natural experiments and econometric methods. These approaches leverage the timing and/or location of “social shocks” to understand how exogenous changes in the social environment cause changes in health outcomes (Glymour, 2006). For example, research examining the relationship between acute or ongoing racially salient events, changes in area-level racial prejudice, and changes in health outcomes among different racial/ethnic groups can advance our understanding of the causal mechanisms at play, while strengthening the conceptualization of the exposure by identifying its antecedents. In tandem, research linking area-level racial prejudice measures with data from longitudinal cohort studies with multiple prospective outcome assessments across the life course could identify developmental windows of vulnerability and inform targeted interventions.
Lastly, as the use of big data in public health and social science increases, innovations in the data sources used to measure area-level racial prejudice are likely (e.g., prejudice expressed on Facebook, Instagram, TikTok, Craigslist). When evaluating the utility of various data sources, researchers can seek to maximize representativeness and specificity of measurement while minimizing self-censorship. Researchers may also consider validation and factor analysis to strengthen measurement. We caution, however, that rigor and innovation in measurement must be accompanied by equally rigorous theoretical work, as specified in the first recommendation for future research. Additional sources of data will not overcome the need for a clearly defined exposure with solid theoretical grounding.
Strengths and Limitations of the Systematic Review
This preregistered systematic literature review had several notable strengths. Developing comprehensive search strings with consultation from a research librarian and searching across four multidisciplinary databases increased the breadth and depth of our search and the likelihood of identifying eligible articles from across academic disciplines. Two independent investigators performed all screening and data extraction, and met regularly to build consensus, strengthening the quality of our data.
There were also important limitations. Despite a comprehensive search strategy which yielded over 14,000 unique articles, it is possible we did not identify all eligible studies. In addition, publication and reporting bias pose a threat to validity in systematic literature reviews; null or counterintuitive findings may be omitted or unpublished, which would over-estimate the effects of area-level racial prejudice on health (Dwan et al., 2008). Our working definition of area-level racial prejudice focused on aggregated indicators of cognitive but not behavioral manifestations of racism. This choice was made strategically to manage the conceptual specificity and scope of the study. A future systematic review examining health consequences of aggregated measures of racial discrimination (e.g., home mortgage discrimination (Beyer et al., 2016), racist policing (Sewell & Jefferson, 2016), or hate crimes (Duncan & Hatzenbuehler, 2014)) could complement this study.
Conclusions
The measurement of area-level racial prejudice based on aggregated individual-level data, and estimation of associations with key health outcomes, is a promising area of inquiry. Future studies can deepen the theoretical rigor of this work while advancing innovations in measurement, strengthening causal inference, and exploring social and biologic mechanisms. Findings from this emerging body of literature can be used to inform public health policymakers and practitioners in developing evidence-based interventions to reduce the harm caused by ambient racial prejudice in society.
Supplementary Material
Footnotes
We have no known conflict of interest to disclose.
REFERENCES:
Note: references marked with an asterisk indicate studies included in the systematic review
- Allen AM, Thomas MD, Michaels EK, Reeves AN, Okoye U, Price MM, Hasson RE, Syme SL, & Chae DH (2019). Racial discrimination, educational attainment, and biological dysregulation among midlife African American women. Psychoneuroendocrinology, 99, 225–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, & Bassett MT (2017, Apr 08). Structural racism and health inequities in the USA: evidence and interventions. Lancet, 389(10077), 1453–1463. 10.1016/s0140-6736(17)30569-x [DOI] [PubMed] [Google Scholar]
- Beyer KM, Zhou Y, Matthews K, Bemanian A, Laud PW, & Nattinger AB (2016, Jul). New spatially continuous indices of redlining and racial bias in mortgage lending: links to survival after breast cancer diagnosis and implications for health disparities research. Health Place, 40, 34–43. 10.1016/j.healthplace.2016.04.014 [DOI] [PubMed] [Google Scholar]
- Blair IV, & Brondolo E (2017). Moving beyond the individual: Community-level prejudice and health. Social Science & Medicine(183), 169–172. [DOI] [PubMed] [Google Scholar]
- * Chae DH, Clouston S, Hatzenbuehler ML, Kramer MR, Cooper HL, Wilson SM, Stephens-Davidowitz SI, Gold RS, & Link BG (2015). Association between an internet-based measure of area racism and Black mortality. PLoS ONE, 10(4), e0122963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Chae DH, Clouston S, Martz CD, Hatzenbuehler ML, Cooper HL, Turpin R, Stephens-Davidowitz S, & Kramer MR (2018). Area racism and birth outcomes among Blacks in the United States. Social Science & Medicine, 199, 49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R, & Hendren N (2018). The impacts of neighborhoods on intergenerational mobility I: Childhood exposure effects. The quarterly journal of economics, 133(3), 1107–1162. [Google Scholar]
- Cogburn CD (2019). Culture, race, and health: implications for racial inequities and population health. The Milbank Quarterly, 97(3), 736–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor P, Sarafidis V, Zyphur MJ, Keltner D, & Chen S (2019). Income inequality and White-on-Black racial bias in the United States: Evidence from project implicit and Google Trends. Psychological Science, 30(2), 205–222. [DOI] [PubMed] [Google Scholar]
- Darling-Hammond S, Michaels EK, Allen AM, Chae DH, Thomas MD, Nguyen TT, Mujahid ΜM, & Johnson RC (2020). After “The China Virus” Went Viral: Racially Charged Coronavirus Coverage and Trends in Bias Against Asian Americans. Health Education & Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JA, & Schwartzman K (1973). General Social Survey: March 1975 (Vol. 4). Inter-University Consortium for Political Research. [Google Scholar]
- Duncan DT, & Hatzenbuehler ML (2014). Lesbian, gay, bisexual, and transgender hate crimes and suicidality among a population-based sample of sexual-minority adolescents in Boston. American Journal of Public Health, 104(2), 272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan A-W, Cronin E, Decullier E, Easterbrook PJ, Von Elm E, & Gamble C (2008). Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS ONE, 3(8), e3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feagin J (2013). Systemic racism: A theory of oppression. Routledge. [Google Scholar]
- Gee GC, & Ford CL (2011). Structural racism and health inequities: old issues, new directions. Du Bois Review: Social Science Research on Race, 8(1), 115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Ro A, Shariff-Marco S, & Chae D (2009). Racial discrimination and health among Asian Americans: evidence, assessment, and directions for future research. Epidemiologic Reviews, 31(1), 130–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, James SA, Destin M, Graham LF, Hatzenbuehler ML, Murphy MC, Pearson JA, Omari A, & Thompson JP (2016). Jedi public health: Co-creating an identity-safe culture to promote health equity. SSM-population health, 2, 105–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour ΜM (2006). Natural experiments and instrumental variable analyses in social epidemiology. Methods in social epidemiology, 1, 429. [Google Scholar]
- Google. (2020). Google Trends. https://trends.google.com/trends/?geo=US
- Greenwald AG, Poehlman TA, Uhlmann EL, & Banaji MR (2009). Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of personality and social psychology, 97(1), 17. [DOI] [PubMed] [Google Scholar]
- Harrell SP (2000, Jan). A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry, 70(1), 42–57. [DOI] [PubMed] [Google Scholar]
- Hehman E, Calanchini J, Flake JK, & Leitner JB (2019, Jun 2019 2019-06-10). Establishing construct validity evidence for regional measures of explicit and implicit racial bias. Journal of Experimental Psychology: General, 148(6), 1022–1040. 10.1037/xge0000623 [DOI] [PubMed] [Google Scholar]
- * Hehman E, Flake JK, & Calanchini J (2018). Disproportionate use of lethal force in policing is associated with regional racial biases of residents. Social Psychological and Personality Science, 1948550617711229. [Google Scholar]
- Hicken M, Stanton A, Lee H (2019). The Burden of Cultural Racism: Vigilance and Racial Health Inequalities. In Ford C, Griffith D, Bruce M, Gilbert K (Ed.), Racism: Science & Tools for the Public Health Professional (pp. 583). American Public Health Association. [Google Scholar]
- Hoover J, & Dehghani M (2019). The big, the bad, and the ugly: Geographic estimation with flawed psychological data. Psychological Methods. [DOI] [PubMed] [Google Scholar]
- * Hswen Y (2020). Online negative sentiment towards Mexicans and Hispanics and impact on mental well-being: A time-series analysis of social media data during the 2016 United States presidential election. Heliyon, 6(9). 10.1016/j.heliyon.2020.e04910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Huang D, Huang Y, Adams N, Nguyen TT, & Nguyen QC (2020). Twitter-Characterized Sentiment Towards Racial/Ethnic Minorities and Cardiovascular Disease (CVD) Outcomes. Journal of racial and ethnic health disparities, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Innovation VH (2016). Covidence systematic review software. In www.covidence.org
- Jewell NP (2003). Statistics for epidemiology. Chapman and Hall/CRC. [Google Scholar]
- Jones CP (2000, 2000). Levels of racism: a theoretic framework and a gardener’s tale. American Journal of Public Health, 90(8), 1212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1446334/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jost JT, Rudman LA, Blair IV, Carney DR, Dasgupta N, Glaser J, & Hardin CD (2009). The existence of implicit bias is beyond reasonable doubt: A refutation of ideological and methodological objections and executive summary of ten studies that no manager should ignore. Research in organizational behavior, 29, 39–69. [Google Scholar]
- * Kennedy BP, Kawachi I, Lochner K, Jones C, & Prothrow-Stith D (1997). (Dis) respect and black mortality. Ethnicity & disease, 7(3), 207–214. [PubMed] [Google Scholar]
- Kopkin N (2017). Does racial prejudice affect black entrepreneurship?: evidence exploiting spatial differences in prejudicial attitudes. Applied Economics, 49(31), 3045–3066. [Google Scholar]
- Krumpal I (2013). Determinants of social desirability bias in sensitive surveys: a literature review. Quality & Quantity, 47(4), 2025–2047. [Google Scholar]
- * Lee Y, Muennig P, Kawachi I, & Hatzenbuehler ML (2015). Effects of racial prejudice on the health of communities: a multilevel survival analysis. American Journal of Public Health, 105(11), 2349–2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Leitner JB, Hehman E, Ayduk O, & Mendoza-Denton R (2016a). Blacks’ death rate due to circulatory diseases is positively related to whites’ explicit racial bias: A nationwide investigation using project implicit. Psychological Science, 27(10), 1299–1311. [DOI] [PubMed] [Google Scholar]
- * Leitner JB, Hehman E, Ayduk O, & Mendoza-Denton R (2016b). Racial bias is associated with ingroup death rate for Blacks and Whites: Insights from Project Implicit. Social Science & Medicine, 170, 220–227. [DOI] [PubMed] [Google Scholar]
- Malat J, Mayorga-Gallo S, & Williams DR (2018). The effects of whiteness on the health of whites in the USA. Social Science & Medicine, 199, 148–156. [DOI] [PubMed] [Google Scholar]
- * McKetta S, Hatzenbuehler ML, Pratt C, Bates L, Link BG, & Keyes KM (2017). Does social selection explain the association between state-level racial animus and racial disparities in self-rated health in the United States? Annals of Epidemiology, 27(8), 485–492.e486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group P (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS med, 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney SJ, Westreich DJ, & El-Sayed AM (2015). Epidemiology in the era of big data. Epidemiology (Cambridge, Mass.), 26(3), 390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Morey BN, Gee GC, Muennig P, & Hatzenbuehler ML (2018). Community-level prejudice and mortality among immigrant groups. Social Science & Medicine, 199, 56–66. [DOI] [PubMed] [Google Scholar]
- * Nguyen TT, Adams N, Huang D, Glymour ΜM, Allen AM, & Nguyen QC (2020). The Association Between State-Level Racial Attitudes Assessed From Twitter Data and Adverse Birth Outcomes: Observational Study. JMIR Public Health and Surveillance, 6(3), e17103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Nguyen TT, Meng H-W, Sandeep S, McCullough M, Yu W, Lau Y, Huang D, & Nguyen QC (2018). Twitter-derived measures of sentiment towards minorities (2015–2016) and associations with low birth weight and preterm birth in the United States. Computers in Human Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosek B, Banaji M, & Greenwald A (2010). Project implicit. Project Implicit. [Google Scholar]
- Novak NL, Geronimus AT, & Martinez-Cardoso AM (2017). Change in birth outcomes among infants born to Latina mothers after a major immigration raid. International Journal of Epidemiology, 46(3), 839–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea BA, Watson DG, Brown GD, & Fincher CL (2020). Infectious disease prevalence, not race exposure, predicts both implicit and explicit racial prejudice across the United States. Social Psychological and Personality Science, 11(3), 345–355. [Google Scholar]
- * Orchard J, & Price J (2017). County-level racial prejudice and the black-white gap in infant health outcomes. Social Science & Medicine, 181, 191–198. [DOI] [PubMed] [Google Scholar]
- Paradies Y (2006, Aug). A systematic review of empirical research on self-reported racism and health. Int J Epidemiol, 35(4), 888–901. 10.1093/ije/dyl056 [DOI] [PubMed] [Google Scholar]
- Payne BK, Vuletich HA, & Brown-lannuzzi JL (2019). Historical roots of implicit bias in slavery. Proceedings of the National Academy of Sciences, 116(24), 11693–11698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne BK, Vuletich HA, & Lundberg KB (2017). The bias of crowds: How implicit bias bridges personal and systemic prejudice. Psychological Inquiry, 28(4), 233–248. [Google Scholar]
- Perrin A, & Anderson M (2019). Share of US adults using social media, including Facebook, is mostly unchanged since 2018. Pew Research Center, 10. https://www.pewresearch.org/fact-tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-unchanged-since-2018/ [Google Scholar]
- Phelan JC, & Link BG (2015). Is racism a fundamental cause of inequalities in health? Annual Review of Sociology, 41, 311–330. [Google Scholar]
- Remy E (2019). How public and private Twitter users in the U.S. compare — and why it might matter for your research. Decoded, https://medium.com/pew-research-center-decoded/how-public-and-private-twitter-users-in-the-u-s-d536ce2a41b3 [Google Scholar]
- Rothman KJ, Greenland S, & Lash TL (2008). Modern epidemiology. Lippincott Williams & Wilkins. [Google Scholar]
- Sakong J (2018). The Obama Effect: Effect of Black Electoral Victory on Racial Prejudice and Inequality. [Google Scholar]
- Sawyer J, & Gampa A (2018). Implicit and Explicit Racial Attitudes Changed During Black Lives Matter. Personality and Social Psychology Bulletin, 0146167218757454. [DOI] [PubMed] [Google Scholar]
- Sewell AA, & Jefferson KA (2016). Collateral damage: the health effects of invasive police encounters in New York City. Journal of Urban Health, 93(1), 42–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Software V (2019). MAXQDA 2020. In maxqda.com
- Stephens-Davidowitz S (2014). The cost of racial animus on a black candidate: Evidence using Google search data. Journal of Public Economics, 118, 26–40. [Google Scholar]
- Stephens-Davidowitz S, & Pabon A (2017). Everybody lies: Big data, new data, and what the internet can tell us about who we really are. HarperCollins New York. [Google Scholar]
- Viruell-Fuentes EA, Miranda PY, & Abdulrahim S (2012). More than culture: structural racism, intersectionality theory, and immigrant health. Social Science & Medicine, 75(12), 2099–2106. [DOI] [PubMed] [Google Scholar]
- Wilkinson RG (2001). Mind the gap: hierarchies, health and human evolution. Yale University Press. [Google Scholar]
- Williams DR, Lawrence JA, & Davis BA (2019). Racism and health: evidence and needed research. Annual Review of Public Health, 40, 105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojcik S, & Hughes A (2019). Sizing up Twitter users. Washington, DC: Pew Research Center, https://www.pewresearch.org/internet/wp-content/uploads/sites/9/2019/04/twitter_opinions_4_18_final_clean.pdf [Google Scholar]
- Xu K, Nosek B and Greenwald AG (2014). Psychology data from the Race Implicit Association Test on the Project Implicit Demo website. 10.5334/jopd.ac [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


