Abstract
Context.
Expectations about the future (future expectancies) are important determinants of psychological well-being among cancer patients, but the strategies patients use to maintain positive and cope with negative expectancies are incompletely understood.
Objectives.
To obtain preliminary evidence on the potential role of one strategy for managing future expectancies: the adoption of “epistemic beliefs” in fundamental limits to medical knowledge.
Methods.
A sample of 1307 primarily advanced-stage cancer patients participating in a genomic tumor testing study in community oncology practices completed measures of epistemic beliefs, positive future expectancies, and mental and physical health-related quality of life (HRQOL). Descriptive and linear regression analyses were conducted to assess the relationships between these factors and test two hypotheses: 1) epistemic beliefs affirming fundamental limits to medical knowledge (“fallibilistic epistemic beliefs”) are associated with positive future expectancies and mental HRQOL, and 2) positive future expectancies mediate this association.
Results.
Participants reported relatively high beliefs in limits to medical knowledge (M = 2.94, s.d.=.67) and positive future expectancies (M = 3.01, s.d.=.62) (range 0–4), and relatively low mental and physical HRQOL. Consistent with hypotheses, fallibilistic epistemic beliefs were associated with positive future expectancies (b = 0.11, SE=.03, P< 0.001) and greater mental HRQOL (b = 0.99, SE=.34, P = 0.004); positive expectancies also mediated the association between epistemic beliefs and mental HRQOL (Sobel Z=4.27, P<0.001).
Conclusions.
Epistemic beliefs in limits to medical knowledge are associated with positive future expectancies and greater mental HRQOL; positive expectancies mediate the association between epistemic beliefs and HRQOL. More research is needed to confirm these relationships and elucidate their causal mechanisms.
Keywords: Epistemic beliefs, prognosis, positive expectancies, quality of life, coping, well-being
Background
Expectations about the future are important determinants of psychological well-being. A large body of empirical research has shown that positive expectations about the future are associated with higher levels of positive emotions, self-reported mental health, and subjective well-being, while negative expectations are associated with lower levels of these states.1–9 These associations, furthermore, hold across a wide range of different types of expectations—from generalized expectancies that the future will be positive (optimism) or negative (pessimism),3,10 to more specific expectations about the occurrence of particular events (outcome expectancies).11,12 Hope, a variably defined phenomenon encompassing positive expectancies about both future outcomes and one’s ability to achieve them,13–23 has also been associated with greater psychological well-being in numerous studies.18,24–29
For patients with cancer and other serious illnesses that pose significant threats of suffering and death, it stands to reason that these various types of future expectations should be particularly important determinants of psychological well-being. Observational studies of advanced cancer patients have shown that both optimism and hope are associated with lower emotional distress and higher health-related quality of life (HRQOL)—a broader construct than well-being, representing both self-rated physical and mental health and functioning30—while pessimism is associated with higher emotional distress and lower HRQOL.31–37 More specific expectancies about one’s future survival or length of life (life expectancies) have shown similar relationships.38–40 In both observational and interventional studies of advanced cancer patients, unfavorable prognostic perceptions (negative life expectancies) have been associated with anxiety, depression, and hopelessness,41–45 while favorable prognostic perceptions (positive life expectancies) have been associated with positive emotional states.17,37,46–48 A longitudinal study of advanced cancer patients by George and colleagues has further demonstrated that changes in prognostic perceptions are associated with changes in psychological well-being, supporting a causal relationship between these phenomena.49 In this study, worsening prognostic perceptions were associated with an initial short-term increase in fear, sadness, worry, and depressed mood, followed by a recovery to baseline emotional states.49
If expectations about the future—hereafter referred to as future expectancies—are important determinants of psychological well-being for patients with cancer and other life-limiting illnesses, then a critical question is how patients maintain positive expectancies or mitigate the adverse effects of negative ones. Past studies have identified several coping strategies that have been well-described in the broader psychological literature.50–53 These include both adaptive strategies (e.g., acceptance, cognitive reframing, problem solving, emotional or social support), as well as potentially maladaptive ones (e.g., denial, information avoidance, mental or behavioral disengagement).54–56 Among these various strategies, cognitive reframing—i.e., reconceptualizing a problem by seeing it from a different perspective57—appears to be especially important. Use of cognitive reframing has been associated with higher HRQOL and lower depression among advanced cancer patients who acknowledge a poor prognosis,51 and studies of early-stage cancer patients have shown similar associations.53,54
The specific ways patients positively reframe a poor prognosis have not been well-defined; however, Folkman has identified one potential strategy that she has termed “personalizing the odds.”58 This reframing strategy consists of two main actions: 1) identifying reasons why the odds do not apply due to attributes of the individual or situation, and 2) formulating alternative interpretations of prognostic information that highlights its limitations. The psychological importance of this reframing strategy for patients with serious life-limiting illness is supported by several qualitative studies.59–61 One study of patients with advanced ovarian cancer described how some individuals construct and maintain beliefs in both the indeterminacy of future outcomes and the inadequacy of medical evidence as a means of preserving hope in the possibility of a positive future outcome.62 In this way, beliefs in fundamental limits to medical knowledge may ultimately promote greater psychological well-being for some patients with life-limiting illness.
Beliefs in limits to medical knowledge are specific instances of a more general class of epistemic beliefs—that is, beliefs regarding the nature, justification, and certainty of human knowledge. Such beliefs, which educational psychologists have also termed “epistemological beliefs” and “personal epistemologies,”63–66 are important determinants of critical thinking and reasoning skills.67,68 Epistemic beliefs are thought to evolve over time from a relatively naïve view of knowledge as certain (absolute, definitive, and stable), to a more advanced view of knowledge as inherently uncertain (contingent, tentative, and mutable).65,67–71 For medical problems such as the prognosis of seriously ill patients, epistemic beliefs in fundamental limits to knowledge—hereafter referred to as “fallibilistic” epistemic beliefs—are logically justifiable due to the many theoretical and empirical factors that make an individual’s prognosis unknowable.72,73 The additional possibility raised by qualitative studies of how patients cope with life-limiting illness is whether fallibilistic epistemic beliefs may also be psychologically adaptive—increasing well-being by promoting positive future expectancies.
To our knowledge, however, the relationships between epistemic beliefs, future expectancies, and psychological well-being have not been investigated quantitatively. The purpose of this cross-sectional study was to measure epistemic beliefs and to evaluate the extent to which fallibilistic epistemic beliefs are associated with both positive future expectancies and greater psychological well-being among a sample of predominantly advanced-stage cancer patients receiving care in community oncology settings. We hypothesized that: 1) Fallibilistic epistemic beliefs (acknowledging the limits of medical knowledge) would be associated with both positive future expectancies and greater HRQOL, and 2) The association between fallibilistic epistemic beliefs and HRQOL would be mediated by positive future expectancies. The study’s overarching objective was to generate proof-of-concept evidence for a potential causal role of epistemic beliefs in helping patients cope with cancer and other life-limiting illnesses, which might inform more definitive future studies.
Methods
Sample population and recruitment.
The sample population consisted of a convenience sample of cancer patients receiving care at community oncology practices in a predominantly rural Northeastern US state. Participants were recruited through the Maine Cancer Genomics Initiative, a statewide program aimed at advancing precision oncology by providing patients with free access to large-panel genomic tumor testing (GTT) performed by the Jackson Laboratory. Eligible participants consisted of patients of 68 participating medical, gynecologic, and neuro-oncologists. Physicians offered GTT to patients at their own discretion, without pre-specified exclusion criteria, although it was anticipated that they would primarily enroll patients with advanced cancer who had exhausted conventional treatment options. The determinants of oncologists’ decisions to offer GTT to patients are currently being investigated; however, available evidence suggests that greater availability of testing and advanced cancer stage are critical factors, along with greater knowledge and favorable attitudes among physicians.74–76 Patients who agreed to receive GTT were invited to participate in a study of their knowledge, attitudes, and experiences regarding GTT, of which the current study was a part. After providing written informed consent, study participants then completed repeated questionnaires administered either by paper or online through a REDCap Cloud® survey data platform. The study protocol was reviewed and approved by the Western IRB (WIRB), Tracking Number 20170880.
The sample for the current study consisted of participants who consented, registered and enrolled in MCGI as of Dec. 31, 2020, and completed a 30-minute baseline questionnaire assessing their knowledge, attitudes, and expectations regarding GTT, as well as sociodemographic and other psychosocial factors; this questionnaire contained all measures used in the current study. Patients completed the questionnaire after their initial consult with their clinician about GTT, but before receiving test results.
Measures.
Epistemic beliefs were assessed using a new 5-item measure (α = 0.62) that our group developed by adapting questions from various existing measures of individual differences in epistemic beliefs or personal epistemologies.67,69,77,78 These measures ascertain the extent to which individuals believe that knowledge is inherently contingent, tentative, and mutable, as opposed to absolute, definitive, and stable.65,67,69,70 We modified individual items from various existing measures to be specific to the medical domain and to assess beliefs in two aspects of medical knowledge—indeterminacy and ambiguity—of potential importance to patients’ responses to prognostic uncertainty.62 Three items assessed indeterminacy: 1) “Sometimes there are no right answers to medical problems,” 2) “There are no absolute truths in medicine,” and 3) “There are many things in medicine that doctors and medical researchers will never know.” Two items assessed ambiguity, focusing on the mutability or instability of information: 1) “The results of medical research change constantly,” and 2) “Medical information that seems correct today can be proven false in the future.” Items measured participants’ level of agreement using a 5-point Likert response scale with end-point anchors “Strongly Disagree” and “Strongly Agree.” Items were averaged to produce a summary score, with higher values indicating more fallibilistic epistemic beliefs in the limits of medical knowledge. An exploratory factor analysis (maximum likelihood, Oblimin rotation) suggested a two-component structure consistent with the a priori constructs of indeterminacy and ambiguity, which accounted for 28% and 10% of the variance, respectively. All individual survey items within each component demonstrated factor loadings ≥0.50, and no item demonstrated high loadings on more than one component.
Positive future expectancies were assessed using a subset of items from the Herth Hope Index (HHI), a 12-item measure designed to assess hope in people with chronic illness, and used in numerous studies of hope and coping.47,79 Individual items of the HHI assess three main factors: “inner sense of temporality and future,” “inner positive readiness and expectancy,” and “interconnectedness with self and others.”41 We administered the 4 items (α = 0.58) that in our judgment focus most precisely on future expectancies: 1) “I have a positive outlook toward life,” 2) “I can see possibilities in the midst of difficulties,” 3) “I feel scared about my future,” 4) “I feel life has value and worth.”79 Items used a 5-point Likert response scale with end-point anchors “Strongly Disagree” and “Strongly Agree,” and were averaged to produce a summary score with higher values indicating more positive expectancies (item 3 was reverse-coded).
Health-related quality of life was assessed using the 10-item PROMIS Short-Form Global Health measure (V.1.2).80–82 This validated measure ascertains self-rated physical and mental health; summary scores are computed and standardized to the general population using a T-score metric (mean = 50, standard deviation = 10), with respect to age, sex, education, and race/ethnicity based on US Census data. Items are scored on a Likert scale from 1 to 5, with 5 representing higher levels of health. The measure produces 2 component scores: global physical health and global mental health; the physical component scale (PCS) comprises 4 items on physical health, physical functioning, pain intensity, and fatigue, whereas the mental component scale (MCS) includes 4 items on overall quality of life, mental health, satisfaction with social activities and relationships, and emotional problems. Two items (general health and social roles) are not used to calculate PCS and MCS scores.
Sociodemographic and clinical characteristics included age, gender, education level (assessed using five response categories: “Less than high school,” “High School Graduate/GED,” “Some college/Trade School,” “Bachelor’s Degree” and “Graduate Degree), household income (assessed by self-reported income categories); and rurality of participants’ primary residence was classified using USDA Rural-Urban Commuting Area codes based on patient Zip codes. Clinical characteristics included cancer type (five categories: breast, colon, lung, prostate, and all other types) and stage (I-IV).
Data analysis.
We computed descriptive statistics for all study variables (sociodemographic and clinical characteristics, epistemic beliefs, positive future expectancies, and HRQOL), and used ANOVA to explore between-group differences in epistemic beliefs by sociodemographic and clinical characteristics. To test study Hypothesis 1, we conducted separate linear regression analyses with epistemic beliefs as the independent variable and both positive future expectancies and HRQOL (both physical and mental component subscores) as the dependent variables. To test study Hypothesis 2, we conducted additional linear regression analyses with positive expectancies as the independent variable and both physical and mental HRQOL subscores as the dependent variables, and then assessed the potential mediational effect of positive future expectancies by fitting a multivariable linear regression model with epistemic beliefs as the independent variable and HRQOL as the dependent variable, adjusting for positive expectancies (following the method of Baron and Kenny).83 We conducted all analyses using SPSS (Version 27), and further assessed mediation with the PROCESS macro (Model 4),84 which uses ordinary least squares regression and boot-strapping to estimate indirect (mediational) effects. Data were assumed to be missing at random; thus, we used a listwise deletion strategy for participants with missing data on any of the outcome measures.
Results
Table 1 summarizes sociodemographic and clinical characteristics of the study population. Of the 1605 participants enrolled in the MCGI study, 1307 (81%) completed the survey items used in this analysis. The sample had an average age of 64.2 years (range 19 to 97) and contained slightly more female participants (58%); 98% of participants reported white race and non-Hispanic ethnicity. A majority had not completed a college degree (69%), came from households with less than $50,000 annual household income (54%) and lived in a rural setting (70%). Most participants (89%) had advanced (Stage III or IV) cancer.
Table 1.
Sociodemographic and Clinical Characteristics of Study Population
| N (%)a | |
|---|---|
| Age | |
| <30 | 7 (0.5%) |
| 30–39 | 26 (2%) |
| 40–49 | 93 (7.1%) |
| 50–59 | 274 (21%) |
| 60–69 | 464 (35.5%) |
| ≥70 | 434 (33.2%) |
| Unknown/Missing | 9 (0.7%) |
| Gender | |
| Female | 760 (58.2%) |
| Male | 536 (41%) |
| Unknown/Missing | 11 (0.8%) |
| Race | |
| White | 1276 (97.6%) |
| Black | 6 (0.5%) |
| Asian | 7 (0.5%) |
| American Indian/Alaska Native | 5 (0.4%) |
| Other | 8 (0.6%) |
| Unknown/Missing | 5 (0.4%) |
| Ethnicity | |
| Not Hispanic or Latino | 1285 (98.3%) |
| Hispanic or Latino | 13 (1%) |
| Unknown/Missing | 9 (0.7%) |
| Education | |
| Less than high school | 83 (6.4%) |
| High school graduate | 402 (30.8%) |
| Some college/Trade school | 413 (31.6%) |
| Bachelor’s degree or higher | 363 (27.7%) |
| Unknown/missing | 46 (3.5%) |
| Household income | |
| Less than $25,000 | 342 (26.2%) |
| $25,000 – $49,999 | 361 (27.6%) |
| $50,000 – $74,999 | 226 (17.3%) |
| $75,000 – $100,000 | 118 (9%) |
| >$100,000 | 110 (8.4%) |
| Unknown/missing | 150 (11.5%) |
| Rurality | |
| Metropolitan area | 328 (25.1%) |
| Large rural | 455 (34.8%) |
| Small or isolated rural | 457 (35%) |
| Unknown/missing | 67 (5.1%) |
| Cancer stage | |
| Stage I | 53 (4.1%) |
| Stage II | 46 (3.5%) |
| Stage III | 190 (14.5%) |
| Stage IV | 967 (74%) |
| Unknown/Missing | 50 (3.9%) |
| Cancer type | |
| Breast | 128 (9.8%) |
| Colon | 133 (10.2%) |
| Lung | 187 (14.3%) |
| Prostate | 83 (6.3%) |
| Other | 776 (59.4%) |
Total N = 1307; not all rows for each variable sum to 1307 due to missing data.
The overall mean score on the epistemic beliefs measure was 2.94 (s.d.=.67) on a scale from 0–4, indicating a relatively high level of fallibilistic epistemic beliefs. There were significant between-group differences in epistemic beliefs by education (F3, 1247 = 4.35, η2 = 0.01, P = 0.005) and household income (F5, 1220 = 4.14, η2=.02, P<0.001). Subgroup differences for each of these sociodemographic variables showed no consistent “dose-response” pattern (Appendix). However, post-hoc analyses demonstrated that participants with some college or trade school education had less fallibilistic epistemic beliefs (M = 2.84, s.d.=.68) than participants with either high school education or less (M = 2.99, s.d. =.66, P = 0.02), or bachelor’s degree or higher (M = 2.98, s.d.=.66, P = 0.01); furthermore, participants reporting household income >$100,000 had more fallibilistic epistemic beliefs (M = 3.05, s.d.=.61) than participants reporting income of $75,000-$100,000 (M = 2.79, s.d.=.70, P = 0.04). There were no significant between-group differences in epistemic beliefs by any other sociodemographic or clinical characteristics.
The mean score on the abbreviated Herth Hope Index was 3.01 (s.d.=.62) on a scale from 0–4, indicating relatively positive general future expectancies. Mental health (MCS) scores on the PROMIS Short-Form Global Health measure (M=46.88, s.d. =8.16) were lower than normed scores for the general population (M = 50), as were physical health (PCS) scores (M=43.99, s.d.=8.46).40
Relationship between epistemic beliefs, positive future expectancies, and HRQOL.
Consistent with Hypothesis 1, more fallibilistic epistemic beliefs were significantly associated with both 1) more positive future expectancies (b = 0.11, SE=.03, P<0.001), and 2) higher mental HRQOL as assessed by PROMIS MCS scores (b=.99, SE=.34, P = 0.004). More fallibilistic epistemic beliefs were not associated with physical HRQOL as assessed by PROMIS PCS scores (b = 0.36, SE = 0.35, P = 0.30). Consistent with predictions, more positive future expectancies were also significantly associated with higher mental HRQOL (b = 6.90, SE = 0.31, P< 0.001).
Mediational analysis.
Consistent with Hypothesis 2, the relationship between fallibilistic epistemic beliefs and higher mental HRQOL was mediated by positive future expectancies (Fig. 1): the significant positive association between these variables (path c: b = 0.99, SE = 0.33, P = 0.004) became non-significant when positive expectancies were added to the regression model (path c’: b = 0.21, SE = 0.29, P = 0.47), and a Sobel test was consistent with full mediation (Sobel Z = 4.27, P<0.001). The indirect effect estimated using the PROCESS macro,84 furthermore, was significant, (b = 0.77, SE = 0.19, 95% CI: 0.40–1.15), supporting the robustness of the mediating effect of positive future expectancies in the relationship between epistemic beliefs and mental HRQOL.
Fig. 1.
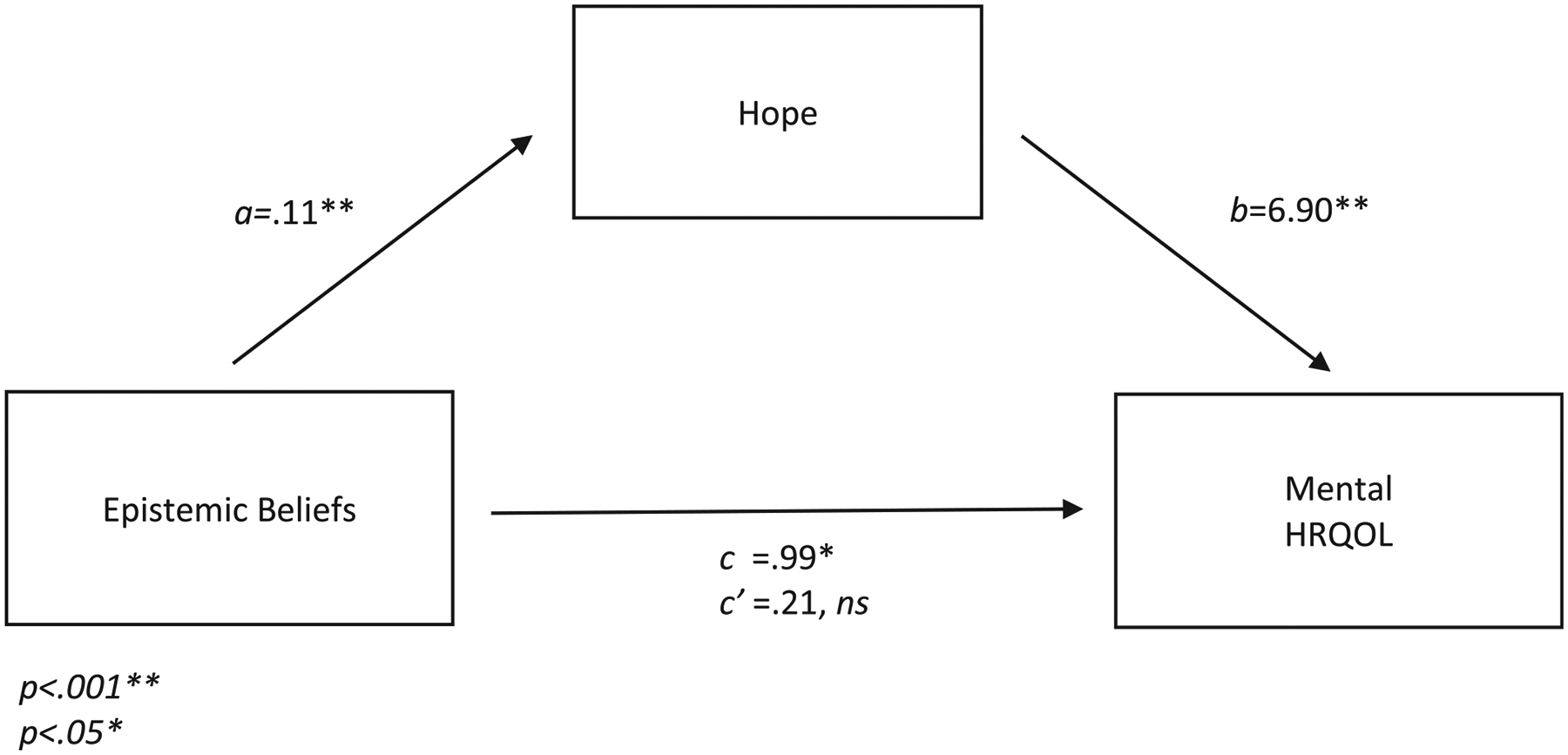
Associations between epistemic beliefs, hope, and mental health-related quality of life (HRQOL).
a, b, and c represent regression coefficients for the associations between epistemic beliefs, hope, and mental health-related quality of life (HRQOL); c’ represents the regression coefficient for the association between epistemic beliefs and mental HRQOL, adjusting for hope (total effect).
ns = non-significant.
Discussion
In this study we investigated the prevalence and psychological significance of epistemic beliefs among mostly advanced-stage cancer patients receiving care in community oncology settings. We found that these patients had a fairly high level of fallibilistic epistemic beliefs acknowledging fundamental limits to medical knowledge, and that epistemic beliefs differed by education and income level. Most importantly, we also found that fallibilistic epistemic beliefs were associated with both more positive general future expectancies and higher levels of mental HRQOL, and that positive future expectancies also mediated the relationship between epistemic beliefs and mental HRQOL. Fallibilistic epistemic beliefs were not associated with physical HRQOL; however, this finding is expected given that physical HRQOL encompasses physical rather than emotional functioning, and symptoms of pain and fatigue rather than anxiety or depressed mood. Although the cross-sectional nature of this study restricts causal inferences, our findings support our study hypotheses and raise the possibility that epistemic beliefs in limits to medical knowledge may increase mental HRQOL, and primarily by increasing positive future expectancies.
To our knowledge, epistemic beliefs among cancer patients have not been previously measured, nor have their relationships with HRQOL and other outcomes related to psychological well-being been investigated. Our findings must thus be interpreted with caution, particularly given the novel nature of our measure of epistemic beliefs, and its somewhat low internal consistency reliability. Reliable and valid measures of this construct need to be developed, and our findings need to be replicated before any definitive conclusions can be drawn about the causal relationships between epistemic beliefs, future expectancies, and psychological well-being. In the meantime, however, we believe our preliminary findings endorse further investigation of these relationships. The factor structure of our new epistemic beliefs measure supports its construct validity. Furthermore, although the observed between-group differences between epistemic beliefs by both education and income levels showed no clear “dose-response” pattern, they provide initial support for the measure’s construct validity given the potential influence of sociodemographic factors on the development of epistemic beliefs.69–71
Above all, our findings are consistent with both psychological theory and emerging empirical evidence suggesting a potential causal relationship between epistemic beliefs, positive future expectancies, and psychological well-being among patients with life-limiting illness.58–62,85 Believing that one’s own future lies beyond the ken of medical knowledge may be a critical factor that enables some patients to maintain hope in the possibility of beating the odds.86 The extent of this potential effect likely depends on numerous factors, including individual characteristics (e.g., health literacy and numeracy, dispositional optimism or other personality characteristics) and clinical circumstances (e.g., diagnosis, prognosis, availability of alternative treatment options). More research is needed to evaluate the potential moderating role of these and other factors. In the meantime, our data suggest that for at least some patients, the adoption of fallibilistic epistemic beliefs may ultimately be a strategy that promotes “tolerance” of uncertainty about their prognosis—that is, the capacity to achieve an adaptive balance in one’s negative and positive psychological responses to this uncertainty.87,88 Research investigating the relationship between epistemic beliefs and patients’ uncertainty tolerance is an important future need.
If confirmed by future research, the observed relationship between epistemic beliefs, positive future expectancies, and psychological well-being has important implications for clinical practice and research. It suggests that prognostic uncertainty—the end-product of fallibilistic epistemic beliefs—may sometimes be psychologically adaptive. Patients with serious life-limiting illnesses may not always avoid, respond negatively to, or reduce prognostic uncertainty; rather, they may sometimes seek, respond positively to, and maintain it as a way of coping with the threat of death. Prognostic uncertainty and psychological well-being may thus have a more complicated relationship than prior studies would suggest,89–92 and more research is needed to better understand this relationship.
These findings also raise deeper normative questions about whether and how clinicians should attempt to mitigate the adverse psychological effects of unfavorable prognostic perceptions on patients with cancer and other life-limiting illnesses. On the one hand, the positive relationships between epistemic beliefs, positive future expectancies, and psychological well-being suggest that reinforcing patients’ beliefs in fundamental limits to medical knowledge—thereby maintaining their prognostic uncertainty—may be an appropriate strategy for some patients. Clearly, however, this approach may also have undesirable effects. It may lead patients to discount evidence-based prognostic estimates, and promote “false hope”—that is, unrealistically positive life expectancies—which may prevent patients from acknowledging and preparing for the possibility of death.15,18,58,93,94 It should be noted, however, that the generic, positive future expectancies we measured, using items from the Herth Hope Index, are not logically incompatible with more specific, negative life expectancies that acknowledge the possibility of death. Furthermore, reinforcing epistemic beliefs that maintain prognostic uncertainty is not the only way to promote psychological well-being among patients with life-limiting illnesses, given that survival is not the only positively valued future outcome. Other outcomes—e. g., meaning, purpose, connectedness with loved ones —may be equally valued and more achievable, and shifting attention to these or other important expectancies may be a more morally appropriate way to achieve psychological well-being.93,95–97 More research is needed to understand how and to what extent patients shift between different types of expectancies when confronting life-limiting illness, and what other coping strategies are most effective and appropriate for mitigating the adverse psychological effects of unfavorable prognostic perceptions.
Our study had several limitations that qualify its findings. The sample population consisted of predominantly White residents of a largely rural state; more research is needed to replicate our findings in more diverse populations. Participants were also enrolled in a larger observational study examining the use of genomic tumor testing, which may have influenced their responses to the survey measures. Participants completed all measures before receiving their GTT results; therefore, these results cannot have affected their responses. Nevertheless, the novel nature of GTT and the opportunity to engage in research may have engendered heightened participants’ expectations of therapeutic benefit, or favored recruitment of patients with more positive views of medical knowledge. More work is thus needed to replicate our findings in patient populations receiving usual care only. More research is also needed to improve the measurement of epistemic beliefs and to evaluate how they relate to similar constructs—e.g., belief in science,98 perceived credibility of science,99 trust in the medical profession.100 Furthermore, we measured future expectancies only in a general sense, using select items from a widely used measure of hope; we did not measure participants’ specific life expectancies, or personal perceptions of prognosis. Further work is needed to understand how epistemic beliefs influence patients’ specific prognostic expectancies, and how these expectancies relate to not only HRQOL, but more specific related outcomes—e.g., hope, positive emotions, life satisfaction.2,24,25,101 Finally, the cross-sectional nature of our study limits inferences about the causal relationships between different variables, and more studies utilizing longitudinal and interventional designs are needed to confirm these relationships.
In spite of these limitations, our study provides initial evidence that epistemic beliefs may play an important role in helping cancer patients cope with an unfavorable prognosis. The study endorses the value of further research to confirm our findings, understand their mechanisms, and develop interventions that can improve the psychological well-being of patients with advanced cancer and other life-limiting illnesses.
Supplementary Material
Key Message.
This cross-sectional study explored whether “epistemic” beliefs that acknowledge fundamental limits to medical knowledge might help cancer patients maintain positive future expectancies that, in turn, promote psychological well-being. Supporting this possibility, these beliefs were associated with greater mental quality of life, and this association was mediated by positive future expectancies.
Acknowledgments
We thank the many patients who generously gave their time to participate in the Maine Cancer Genomics Initiative, and Leo B. Waterston, MS, Petra Helbig, MSc, and Kate Reed, MPH, ScM, for their assistance with the conduct of the study.
Disclosures
The authors have no conflicts of interest to declare. This study was supported by funding from the Harold Alfond Foundation.
Footnotes
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jpainsymman.2021.12.017.
References
- 1.Oettingen G, Mayer D. The motivating function of thinking about the future: expectations versus fantasies. J Pers Soc Psychol 2002;83:1198–1212. [PubMed] [Google Scholar]
- 2.Gallagher MW, Lopez SJ. Positive expectancies and mental health: Identifying the unique contributions of hope and optimism. J Positive Psychol 2009;4:548–556. [Google Scholar]
- 3.Scheier M, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 1985;4:219–247. [DOI] [PubMed] [Google Scholar]
- 4.Scheier M, Carver CS. Effects of optimism on psychological and physical well-being: theoretical overview and empirical update. Cog Ther Res 1992;16:201–228. [Google Scholar]
- 5.Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev 2010;30:879–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheier MF, Carver CS. Dispositional optimism and physical well-being: the influence of generalized outcome expectancies on health. J Personality 1987;55:169–210. [DOI] [PubMed] [Google Scholar]
- 7.Scheier MF, Matthews KA, Owens JF, et al. Dispositional optimism and recovery from coronary artery bypass surgery: the beneficial effects on physical and psychological well-being. J Pers Soc Psychol 1989;57:1024–1040. [DOI] [PubMed] [Google Scholar]
- 8.Rief W, Glombiewski J, Gollwitzer M, Schubö A, Schwarting R, Thorwart A. Expectancies as core features of mental disorders. Curr Opin Psychiatry 2015;28:378–385. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher MW, Lopez SJ, Pressman SD. Optimism is Universal: exploring the presence and benefits of optimism in a representative sample of the world. J Personality 2013;5:429–440. [DOI] [PubMed] [Google Scholar]
- 10.Scheier M, Weintraub JK, Carver CS. Coping with stress: divergent strategies of optimists and pessimists. J Pers Soc Psychol 1986;51:1257–1264. [DOI] [PubMed] [Google Scholar]
- 11.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery G, David D, Dilorenzo T, Erblich J. Is hoping the same as expecting? Discrimination between hopes and response expectancies for nonvolitional outcomes. Pers Individ Dif 2003;35:399–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Snyder CR. Conceptualizing, measuring, and nurturing hope. J Counsel Devel 1995;73:355–360. [Google Scholar]
- 14.Snyder CR. Hope theory: rainbows in the mind. Psychol Inq 2002;13:249–275. [Google Scholar]
- 15.Leung KK, Silvius JL, Pimlott N, Dalziel W, Drummond N. Why health expectations and hopes are different: the development of a conceptual model. Health Expect 2009;12:347–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McClement SE, Chochinov HM. Hope in advanced cancer patients. Eur J Cancer 2008;44:1169–1174. [DOI] [PubMed] [Google Scholar]
- 17.DeMartini J, Fenton JJ, Epstein R, et al. Patients’ hopes for advanced cancer treatment. J Pain Symptom Manage 2019;57:57–63. e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corn BW, Feldman DB, Wexler I. The science of hope. Lancet Oncol 2020;21:e452–e459. [DOI] [PubMed] [Google Scholar]
- 19.Feudtner C. Hope and the prospects of healing at the end of life. J Altern Complement Med 2005;11(Suppl 1):S23–S30. [DOI] [PubMed] [Google Scholar]
- 20.Feudtner C. The breadth of hopes. N Engl J Med 2009;361:2306–2307. [DOI] [PubMed] [Google Scholar]
- 21.Feudtner C, Carroll KW, Hexem KR, Silberman J, Kang TI, Kazak AE. Parental hopeful patterns of thinking, emotions, and pediatric palliative care decision making: a prospective cohort study. Arch Pediatr Adolesc Med 2010; 164:831–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bruininks P, Malle BF. Distinguishing hope from optimism and related affective states. Motivation and Emotion 2005;29:327–355. [Google Scholar]
- 23.Krafft AM, Guse T, Maree D. Distinguishing perceived hope and dispositional optimism: theoretical foundations and empirical findings beyond future expectancies and cognition. J Well-Being Assess 2021. [Google Scholar]
- 24.Pleeging E, Burger M, van Exel J. The relations between hope and subjective well-being: a literature overview and empirical analysis. Appl Res Qual Life 2021; 16:1019–1041. [Google Scholar]
- 25.Bailey TC, Eng W, Frisch MB, Snyder CR. Hope and optimism as related to life satisfaction. J Positive Psychol 2007;2:168–175. [Google Scholar]
- 26.Long KNG, Kim ES, Chen Y, Wilson MF, Worthington EL, VanderWeele TJ. The role of Hope in subsequent health and well-being for older adults: an outcome-wide longitudinal approach. Global Epidemiology 2020;2:100018. [Google Scholar]
- 27.Vacek KR, Coyle LD, Vera EM. Stress, self-esteem, hope, optimism, and well-being in urban ethnic minority adolescents. J Multicultural Couns Dev 2010;38:99–111. [Google Scholar]
- 28.Gallagher MW, Long LJ, Phillips CA. Hope, optimism, self-efficacy, and posttraumatic stress disorder: a meta-analytic review of the protective effects of positive expectancies. J Clin Psychol 2020;76:329–355. [DOI] [PubMed] [Google Scholar]
- 29.Alarcon GM, Bowling NA, Khazon S. Great expectations: a meta-analytic examination of optimism and hope. Pers Individ Dif 2013;54:821–827. [Google Scholar]
- 30.Hays RD, Reeve BB. Measurement and modeling of health-related quality of life. Int Encyclopedia Public Health, First Ed 2008;4:241–252. [Google Scholar]
- 31.Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rose-nfeld B, Breitbart W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psychooncology 2014;23:299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller DL, Manne SL, Taylor K, Keates J, Dougherty J. Psychological distress and well-being in advanced cancer: the effects of optimism and coping. J Clin Psychol Med Settings 1996;3:115–130. [DOI] [PubMed] [Google Scholar]
- 33.Petersen LR, Clark MM, Novotny P, et al. Relationship of optimism-pessimism and health-related quality of life in breast cancer survivors. J Psychosoc Oncol 2008;26:15–32. [DOI] [PubMed] [Google Scholar]
- 34.de Moor JS, de Moor CA, Basen-Engquist K, Kudelka A, Bevers MW, Cohen L. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosom Med 2006;68:555–562. [DOI] [PubMed] [Google Scholar]
- 35.Cohen L, de Moor C, Amato RJ. The association between treatment-specific optimism and depressive symptomatology in patients enrolled in a Phase I cancer clinical trial. Cancer 2001;91:1949–1955. [DOI] [PubMed] [Google Scholar]
- 36.Milbury K, Tannir NM, Cohen L. Treatment-related optimism protects quality of life in a phase II clinical trial for metastatic renal cell carcinoma. Ann Behav Med 2011; 42:313–320. [DOI] [PubMed] [Google Scholar]
- 37.Duggleby WD, Degner L, Williams A, et al. Living with hope: initial evaluation of a psychosocial hope intervention for older palliative home care patients. J Pain Symptom Manage 2007;33:247–257. [DOI] [PubMed] [Google Scholar]
- 38.Enzinger AC, Zhang B, Schrag D, Prigerson HG. Outcomes of prognostic disclosure: associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol 2015;33:3809–3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tang ST, Chang WC, Chen JS, Chou WC, Hsieh CH, Chen CH. Associations of prognostic awareness/acceptance with psychological distress, existential suffering, and quality of life in terminally ill cancer patients’ last year of life. Psychooncology 2016;25:455–462. [DOI] [PubMed] [Google Scholar]
- 40.Kang E, Kang JH, Koh SJ, et al. The impacts of prognostic awareness on mood and quality of life among patients with advanced cancer. Am J Hosp Palliat Care 2020;37:904–912. [DOI] [PubMed] [Google Scholar]
- 41.Helft PR, Hlubocky F, Wen M, Daugherty CK. Associations among awareness of prognosis, hopefulness, and coping in patients with advanced cancer participating in phase I clinical trials. Support Care Cancer 2003;11:644–651. [DOI] [PubMed] [Google Scholar]
- 42.El-Jawahri A, Traeger L, Kuzmuk K, et al. Prognostic understanding, quality of life and mood in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 2015;50:1119–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.El-Jawahri A, Traeger L, Park ER, et al. Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer 2014;120:278–285. [DOI] [PubMed] [Google Scholar]
- 44.Hui D, Mo L, Paiva CE. The importance of prognostication: impact of prognostic predictions, disclosures, awareness, and acceptance on patient outcomes. Curr Treat Options Oncol 2021;22:12. [DOI] [PubMed] [Google Scholar]
- 45.Carver CS, Meyer B, Antoni MH. Responsiveness to threats and incentives, expectancy of recurrence, and distress and disengagement: moderator effects in women with early stage breast cancer. J Consult Clin Psychol 2000;68:965–975. [DOI] [PubMed] [Google Scholar]
- 46.Chochinov HM, Wilson KG, Enns M, Lander S. Depression, Hopelessness, and suicidal ideation in the terminally ill. Psychosomatics 1998;39:366–370. [DOI] [PubMed] [Google Scholar]
- 47.Herth KA. The relationship between level of hope and level of coping response and other variables in patients with cancer. Oncol Nurs Forum 1989;16:67–72. [PubMed] [Google Scholar]
- 48.Folkman S, Greer S. Promoting psychological well-being in the face of serious illness: when theory, research and practice inform each other. Psychooncology 2000;9:11–19. [DOI] [PubMed] [Google Scholar]
- 49.George LS, Maciejewski PK, Epstein AS, Shen M, Prigerson HG. Advanced cancer patients’ changes in accurate prognostic understanding and their psychological well-being. J Pain Symptom Manage 2020;59:983–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: hope and coping strategies as predictors of adjustment. Psychooncology 2002;11:93–102. [DOI] [PubMed] [Google Scholar]
- 51.Nipp RD, Greer JA, El-Jawahri A, et al. Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol 2017;35:2551–2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baumstarck K, Chinot O, Tabouret E, et al. Coping strategies and quality of life: a longitudinal study of high-grade glioma patient-caregiver dyads. Health Qual Life Outcomes 2018;16:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brunault P, Champagne AL, Huguet G, et al. Major depressive disorder, personality disorders, and coping strategies are independent risk factors for lower quality of life in non-metastatic breast cancer patients. Psychooncology 2016;25:513–520. [DOI] [PubMed] [Google Scholar]
- 54.Carver CS, Pozo C, Harris SD, et al. How coping mediates the effect of optimism on distress: a study of women with early stage breast cancer. J Pers Soc Psychol 1993;65:375–390. [DOI] [PubMed] [Google Scholar]
- 55.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 1989;56:267–283. [DOI] [PubMed] [Google Scholar]
- 56.Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol 1985;48:150–170. [DOI] [PubMed] [Google Scholar]
- 57.American Psychological Association. Reframing. In: APA dictionary of psychology. Available at: https://dictionary.apa.org/reframing. Accessed November 10, 2021. [Google Scholar]
- 58.Folkman S. Stress, coping, and hope. Psychooncology 2010;19:901–908. [DOI] [PubMed] [Google Scholar]
- 59.Timmermans S. Dying of awareness: the theory of awareness contexts revisited. Sociol Health Illness 1994;16:322–339. [Google Scholar]
- 60.Thorne S, Hislop TG, Kuo M, Armstrong EA. Hope and probability: patient perspectives of the meaning of numerical information in cancer communication. Qual Health Res 2006;16:318–336. [DOI] [PubMed] [Google Scholar]
- 61.Eliott JA, Olver IN. Hope, life, and death: a qualitative analysis of dying cancer patients’ talk about hope. Death Stud 2009;33:609–638. [DOI] [PubMed] [Google Scholar]
- 62.Han PKJ, Gutheil C, Hutchinson RN, LaChance JA. Cause or effect? The role of prognostic uncertainty in the fear of cancer recurrence. Front Psychol 2020;11:626038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hofer BK, Pintrich PR. Personal epistemology: The psychology of beliefs about knowledge and knowing. New York: Routledge; 2002. [Google Scholar]
- 64.King PM, Kitchener KS. The reflective judgment model: twenty years of research on epistemic cognition. In: Hofer BK, Pintrich PR, eds. Personal epistemology: The psychology of beliefs about knowledge and knowing, New York: Routledge; 2002:37–61. [Google Scholar]
- 65.Schommer-Atkins M. An evolving theoretical framework for an epistemological belief system. In: Hofer BK, Pintrich PR, eds. Personal epistemology:The psychology of beliefs about knowledge and knowing, New York: Routledge; 2002:103–118. [Google Scholar]
- 66.Rule DC, Bendixen LD. The integrative model of personal epistemology development: theoretical underpinings and implications for education. In: Bendixen LD, Feucht FC, eds. Personal epistemology in the classroom: Theory, research, and implications for practice, Cambridge: Cambridge University Press; 2010:94–123. [Google Scholar]
- 67.Hofer BK. Dimensionality and Disciplinary Differences in Personal Epistemology. Contemp Educ Psychol 2000;25:378–405. [DOI] [PubMed] [Google Scholar]
- 68.Hofer BK. Personal epistemology as a psychological and educational construct: an introduction. In: Hofer BK, Pintrich PR, eds. Personal epistemology: The psychology of beliefs about knowledge and knowing, New York: Routledge; 2002:3–13. [Google Scholar]
- 69.Trautwein U, Lüdtke O. Epistemological beliefs, school achievement, and college major: a large-scale longitudinal study on the impact of certainty beliefs. Contemp Educ Psychol 2007;32:348–366. [Google Scholar]
- 70.Kienhues D, Bromme R, Stahl E. Changing epistemological beliefs: the unexpected impact of a short-term intervention. Br J Educ Psychol 2008;78(Pt 4):545–565. [DOI] [PubMed] [Google Scholar]
- 71.Perry WG. Forms of intellectual and ethical development in the college years. New York: Holt, Rinehart, and Winston; 1970. [Google Scholar]
- 72.Han PK. Conceptual, methodological, and ethical problems in communicating uncertainty in clinical evidence. Med Care Res Rev 2013;70(1 Suppl):14S–36S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gillies D. Philosophical heories of probability. London: Routledge; 2000. [Google Scholar]
- 74.Demeshko A, Pennisi DJ, Narayan S, Gray SW, Brown MA, McInerney-Leo AM. Factors influencing cancer genetic somatic mutation test ordering by cancer physician. J Transl Med 2020;18:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hall MJ, D’Avanzo P, Chertock Y, Brajuha J, Bass SB. Oncologists’ perceptions of tumor genomic profiling and the communication of test results and risks. Public Health Genomics 2021;24:304–309. [DOI] [PubMed] [Google Scholar]
- 76.Anderson EC, Hinton AC, Lary CW, et al. Community oncologists’ perceptions and utilization of large-panel genomic tumor testing. BMC Cancer 2021;21:1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schommer M. Effects of beliefs about the nature of knowledge on comprehension. J Educ Psych 1990;82:498–504. [Google Scholar]
- 78.Schraw G, Bendixen LD, Dunkle ME. Development and validation of the epistemic belief inventory (EBI). In: Hofer BK, Pintrich PR, eds. Personal epistemology: The psychology of beliefs about knowledge and knowing, New York: Routledge; 2002:261–275. [Google Scholar]
- 79.Herth K. Abbreviated instrument to measure hope: development and psychometric evaluation. J Adv Nurs 1992;17:1251–1259. [DOI] [PubMed] [Google Scholar]
- 80.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res 2009;18:873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu H, Cella D, Gershon R, et al. Representativeness of the Patient-reported outcomes measurement information system internet panel. J Clin Epidemiol 2010;63:1169–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.PROMIS Network. Patient-reported outcomes measurement information system (PROMIS). Available at: https://commonfund.nih.gov/promis/index. Accessed April 26, 2021.
- 83.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- 84.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. 2nd Edition New York: Guilford Press; 2017. Vol. [Google Scholar]
- 85.Han PKJ, Strout TD, Gutheil C, et al. How physicians manage medical uncertainty: a qualitative study and conceptual taxonomy. Med Decis Making 2021;41:275–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Han PK. The need for uncertainty: a case for prognostic silence. Perspect Biol Med 2016;59:567–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hillen MA, Gutheil CM, Strout TD, Smets EM, Han PKJ. Tolerance of uncertainty: conceptual analysis, integrative model, and implications for healthcare. Soc Sci Med 2017;180:62–75. [DOI] [PubMed] [Google Scholar]
- 88.Han P. Uncertainty in medicine: A framework for tolerance. New York: Oxford University Press; 2021. [Google Scholar]
- 89.Kurita K, Garon EB, Stanton AL, Meyerowitz BE. Uncertainty and psychological adjustment in patients with lung cancer. Psychooncology 2013;22:1396–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Clayton MF, Mishel MH, Belyea M. Testing a model of symptoms, communication, uncertainty, and well-being, in older breast cancer survivors. Res Nurs Health 2006;29:18–39. [DOI] [PubMed] [Google Scholar]
- 91.Verduzco-Aguirre HC, Babu D, Mohile SG, et al. Associations of uncertainty with psychological health and quality of life in older adults with advanced cancer. J Pain Symptom Manage 2021;61:369–376. e361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gramling R, Stanek S, Han PKJ, et al. Distress due to prognostic uncertainty in palliative care: frequency, distribution, and outcomes among hospitalized patients with advanced cancer. J Palliat Med 2018;21:315–321. [DOI] [PubMed] [Google Scholar]
- 93.Coulehan J. Deep hope: a song without words. Theor Med Bioeth 2011;32:143–160. [DOI] [PubMed] [Google Scholar]
- 94.Gramling R, Epstein R. Optimism amid serious disease: clinical panacea or ethical conundrum?: comment on “Recovery expectations and long-term prognosis of patients with coronary heart disease”. Arch Intern Med 2011;171:935–936. [DOI] [PubMed] [Google Scholar]
- 95.Carver CS, Scheier M. Control theory: a useful conceptual framework for personality, social, clinical and health psychology. Psychol Bull 1982;92:111–135. [PubMed] [Google Scholar]
- 96.Wrosch C, Scheier M, Carver CS, Schulz R. The importance of goal disengagement in adaptive self-regulation: when giving up is beneficial. Self and Identity 2003;2:1–20. [Google Scholar]
- 97.Blumenthal-Barby JS, Ubel PA. In defense of “denial”: difficulty knowing when beliefs are unrealistic and whether unrealistic beliefs are bad. Am J Bioeth 2018;18:4–15. [DOI] [PubMed] [Google Scholar]
- 98.Farias M, Newheiser AK, Kahane G, de Toledo Z. Scientific faith: belief in science increases in the face of stress and existential anxiety. J Exp Soc Psychol 2013;49:1210–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hartman RO, Dieckmann NF, Sprenger AM, Stastny BJ, DeMarree KG. Modeling attitudes toward science: development and validation of the credibility of science scale. Basic Appl Soc Psychol 2017;39:358–371. [Google Scholar]
- 100.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res 2002;37:1419–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Office of Disease Prevention and Health Promotion (ODPHP). Foundation health measure report: health-related quality of life and well-being. Healthy People 2020. Available at: https://www.healthypeople.gov/sites/default/files/HRQoLWBFullReport.pdf. Accessed August 1, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


