Abstract
Oropouche virus (OROV) is an arthropod-borne orthobunyavirus found in South America and causes Oropouche fever, a febrile infection similar to dengue. It is the second most prevalent arthropod-borne viral disease in South America after dengue. Over 500,000 cases have been diagnosed since the virus was first discovered in 1955; however, this is likely a significant underestimate given the limited availability of diagnostics. No fatalities have been reported to date, however, up to 60% of cases have a recurrent phase of disease within one month of recovery from the primary disease course. The main arthropod vector is the biting midge Culicoides paraensis, which has a geographic range as far north as the United States and demonstrates the potential for OROV to geographically expand. The transmission cycle is incompletely understood and vertebrate hosts include both non-human primates and birds further supporting the potential ability of the virus to spread. A number of candidate antivirals have been evaluated against OROV in vitro but none showed antiviral activity. Surprisingly, there is only one report in the literature on candidate vaccines. We suggest that OROV is an undervalued pathogen much like chikungunya, Schmallenberg, and Zika viruses were before they emerged. Overall, OROV is an important emerging disease that has been under-investigated and has the potential to cause large epidemics in the future. Further research, in particular candidate vaccines, is needed for this important pathogen.
Subject terms: Policy and public health in microbiology, Viral infection
Discovery and classification
Oropouche virus (OROV), the causative agent of Oropouche fever (OROF), was first identified in 1955 from the blood of a febrile forest worker in Trinidad and Tobago1. It is a member of the Simbu serogroup of viruses (which also includes Akabane, Manzanilla, Sathuperi, Shamonda, Shuni, and Simbu viruses) within the Orthobunyavirus genus of the family Peribunyaviridae2–4. It is considered a biosafety level 2 (BSL-2) or 3 agent, depending on the specific country. For example, it is BSL-2 in the United States but BSL-3 in Australia. OROV is an arthropod-borne virus (or arbovirus), which has transmission cycles that involve both midges and mosquitoes as the arthropod hosts, and primates and birds as the vertebrate hosts3–5.
Structure and genome organization
OROV is an enveloped virus with a tripartite genome composed of three single-stranded, negative-sense RNA segments5. The small (S) segment contains two overlapping open reading frames (ORFs), which encode the nucleocapsid protein N and the nonstructural (NS) protein NSs, a type I interferon inhibitor6. The medium (M) segment encodes a polyprotein that is post-translationally cleaved into the structural glycoproteins Gn and Gc, and the NSm protein3,4, whose function has not been determined6. Gc is a 939 amino acid class II membrane fusion protein with 3–4 putative N-linked glycosylation sites, and Gn is 290 amino acids with one putative N-linked glycosylation site. There is surprisingly little structural data available for Gc and Gn in members of the Orthobunyavirus genus. To date, there is only a low-resolution cryo-EM structure for Bunyamwera (BUNV) and a high-resolution crystallographic structure for the N-terminal half of Schmallenberg (SBV) Gc7,8. showing an elongated multi-domain protein composed of an α-helical head domain connected to a stalk region composed of two β-sheet subdomains7. In comparison, the structures of only the Gc a-helical head domains from BUNV, OROV, and La Crosse virus (LACV) are available, which indicate that the a-domain appears conserved by these four viruses7. Each has one N-linked glycosylation site that is thought to be solvent exposed. From the available data, it is believed that Gc and Gn form a trimeric spike complex protruding from the viral envelope8. However, no monoclonal antibodies have been generated against OROV so the location of epitopes involved in neutralization and protective immunity is unknown although the epitopes involved in protective immunity have been mapped to Gn for SBV7. No cell receptors have been identified for OROV.
The large (L) segment encodes the L protein and an RNA-dependent RNA polymerase4,9. Flanking the coding regions on each segment are untranslated regions (UTRs) important for replication, transcription, and packaging10,11. Although high-resolution structural studies have not been undertaken with OROV, studies with other orthobunyaviruses suggest that the enveloped OROV virion is about 90 nm in diameter, displaying Gc and Gn on the surface and containing three ribonucleoprotein (RNP) complexes—the RNA segments each complexed with many copies of N and L proteins12.
Phylogeny
Orthobunyaviruses have traditionally been classified by serologic methods, such as plaque reduction neutralization test (PRNT), complement fixation, and hemagglutination inhibition (HI)5. However, serological approaches have gradually given way to nucleotide sequence-based approaches. Genetic studies have characterized the phylogenetic relationships of available sequences of OROV and related Simbu serogroup viruses2–4,10,13,14. OROV has been subdivided into four genotypes (I, II, III, and IV) based on analysis of the N gene, with the mean nucleotide difference among genotypes being around 5%15. However, more recent classification schemes, based on the sequences of all three RNA segments, suggest two clades or lineages within the M or L segment phylogenies3,10,15. The standardized use of four genotypes or two lineages has yet to be agreed upon. Although the first isolation of OROV occurred in Trinidad and Tobago1, analysis of S- and L-segment mutation rates suggests OROV may have originated in the early twentieth century in northern Brazil and has since spread northward into Trinidad and Tobago, and Panama, southward to central Brazil, and westward into Peru and Ecuador3,15.
Reassortment
As the OROV genome comprises three RNA segments, reassortment among OROV genotypes or between OROV and other Simbu serogroup viruses is theoretically possible. The latter scenario poses a risk for the emergence of novel Simbu serogroup viruses. In vitro studies with a virus-like particle (VLP) system, showed OROV glycoproteins packaged the RNP of a fellow Simbu serogroup member SBV16, which is itself considered a reassortant of Shamonda and Sathuperi viruses17. Moreover, SBV N and L proteins were able to promote transcription of an OROV M-segment minigenome, demonstrating cross-recognition among viral components within members of the serogroup, and providing experimental evidence of the viability of reassortant viruses. Since the M segment encodes the envelope glycoproteins, which are major antigenic determinants, selective pressure could result in a higher degree of divergence and reassortment in the M segment among Simbu serogroup members10. Indeed, sites of positive selection are found within Gc, as well as motifs denoting N-linked glycosylation sites that are distinct for different OROV lineages3.
Importantly, there is also evidence that reassortment between Simbu serogroup viruses occurs naturally, with the S and L segments of one virus tending to reassort together with the M segment of another. Iquitos virus, isolated from a febrile patient in 1999 in the northeastern Amazon region of Peru, shares similarity to OROV in the S and L segments but contains a novel Simbu serogroup M segment, and is serologically distinct from OROV18. Similarly, Madre de Dios virus, isolated from a febrile patient in Peru in 2007 and from a monkey in Venezuela in 20104,19, contains an M segment similar to Iquitos virus2, suggesting a currently unidentified Simbu serogroup virus exists in South America. While it remains to be seen whether OROV reassortants will pose a significant public health threat, the clinical importance of reassortants of other orthobunyaviruses has been established. For example, Ngari virus, a reassortant of Bunyamwera and Batai viruses, has been associated with hemorrhagic fever in East Africa in 1997–199820. It seems highly likely that additional OROV reassortants of clinical importance will be identified in the future.
Pathophysiology and clinical disease
Following the bite of an OROV-infected midge or mosquito21–23, there is a 3–8-day incubation period before disease onset23–25. The patient from whom the virus was first isolated (Melajo Forest, Trinidad, 1955) reported symptoms that included fever, backache, and cough without a sore throat in an illness that lasted three days with no recurring symptoms1. In subsequent documented cases, the symptom most commonly reported during acute disease is fever (~39 °C), which is frequently accompanied by headache/retro-orbital pain, malaise, myalgia, arthralgia, nausea, vomiting, and photo-phobia2,26. Less frequent symptoms include a rubella-like rash, meningitis, encephalitis, dizziness, anorexia, and other systemic manifestations2,25,27–30. Hemorrhagic phenomena such as epistaxis, gingival bleeding, and petechiae, or gastrointestinal manifestations such as diarrhea are even more infrequent30.
During the acute disease, patients experience viremia that peaks on day 2 after the onset of clinical symptoms and decreases over the next several days31. Elevated liver enzymes and leukopenia (values as low as 2000 leukocytes/mL) also occur23,25. In most people, the acute disease is relatively short, lasting from 2 to 7 days but in some, particularly those who experience central nervous system involvement (meningitis and encephalitis), the disease can last for 2–4 weeks and may include loss of strength (asthenia)25.
In approximately 60% of clinical cases, the disease recurs after the patient becomes afebrile (normally within 2-10 days but occasionally up to a month). Recurrence is associated with a range of symptoms including fever, headache, myalgia, asthenia, dizziness, and meningitis32. The mechanisms responsible for the recurring disease remain undefined. Once the patient finally recovers, there are no reported long-term sequelae or reports of additional recurrence events at a later date and, although the disease can be severe, no cases of human fatality have been reported2,23,28,33. Currently, it is unclear whether certain OROV genotypes are more likely to produce more severe or unusual symptoms23,28.
Diagnostics and surveillance
The similarity of OROF to the infections caused by other arboviruses, such as chikungunya and dengue, which often circulate in the same areas24, makes the clinical diagnosis of OROV infection by symptomology or on the basis of clinical laboratory tests problematic. Therefore, the disease is sometimes misdiagnosed and consequently under-reported33.
Multiple diagnostic techniques are available for OROV. Because peak viremia tends to coincide with the onset of acute febrile illness24,31, during this time, it is possible to measure viral RNA and antigen in the blood. Additionally, patients begin to generate IgM and IgG antibodies 1 day to 2 weeks after disease onset allowing serologic testing34.
Historically, HI and enzyme-linked immunosorbent assays (ELISAs) have been used to measure human OROV-specific antibodies24,25. IgM and IgG ELISAs have been used to distinguish OROV from other arboviruses (Venezuelan equine encephalitis and dengue viruses) in febrile and afebrile Peruvian soldiers35. PRNTs, HI, and ELISAs have been used as surveillance tools and for epidemiological studies to determine OROV seroprevalence in livestock and wild animals36,37. Many serological assays require virus or virus-infected cells as a source of antigen27,30, necessitating appropriate biosafety facilities. Thus, the development of an immunoassay utilizing bacterially expressed recombinant N protein, (highly conserved among OROV strains), able to detect both OROV-specific IgG and IgM antibodies with a sensitivity of 95% and a specificity of 99.5% represents an important advance38.
A variety of reverse transcriptase–polymerase chain reaction (RT-PCR)-based diagnostic tools have been developed for OROV. The S segment has been used in several PCR-based diagnostics because it is the least variable among the Simbu serogroup31,39. However, because the S segment is so highly conserved40 between OROV strains and OROV-like reassortants, many RT-PCR methods cannot be considered OROV-specific31,39,41,42.
Some studies have used a one-step RT-PCR method in a multiplex RT-qPCR platform to detect OROV, Mayaro (MAYV), and OROV-like reassortants. The primer design for MAYV, a co-circulating alphavirus, targets the NSP1 coding region, while the OROV primers target conserved sequences of the S segment. The multiplex RT-qPCR platform is highly sensitive and can detect as few as 2–20 genome copies/mL, but the design detects both OROV and S segment-containing reassortant viruses43.
Rapid detection of OROV is a priority during outbreaks in isolated or rural regions. Thus, a one-step RT-qPCR method was developed to test for orthobunyaviruses using a mobile SmartCyclerTM44. The primer design was based on the S segment of the prototype OROV strain TrVL 9760. The limit of detection of this diagnostic tool was determined to be 102 copies/mL with a 93.3% detection rate during the first 5 days of symptoms and appears superior to the previously developed nested RT-PCR method44,45. In an attempt to resolve the issue of detecting both OROV and reassorted strains, RT-qPCR, RT-PCR, and nested RT-PCR methods were developed to target the M segment. These methods of quantifying OROV require further validation before they are used widely in clinical studies13.
Although OROV RNA has been detected in bodily fluids other than blood, there has been little systematic assessment of the efficacy of testing for the presence of OROV in bodily fluids such as cerebral spinal fluid33, urine, and saliva41,46. Detection of OROV RNA in urine and saliva may allow for the development of safe, non-invasive, simple, and effective diagnostics. Further studies are necessary to determine the limits of detection of such assays.
RT-PCR-based diagnostic platforms are best used as part of an orthogonal testing approach, in conjunction with serological testing or viral antigen detection in cases where RT-PCR methods fail or are unable to detect divergent OROV strains due to the high specificity to the target sequence47,48. Metagenomic analysis of patient samples has been used as a means to detect and identify divergent, reassorted, or previously unknown viral strains, where other RT-qPCR systems may fail to detect viral RNA47, and can further inform the optimized design of diagnostic tools13,48. However, metagenomic analysis is not widely available in clinical laboratories in arbovirus-endemic regions. In light of the many circulating arboviruses in South America, a comprehensive one-step multiplex RT-PCR-based diagnostic would be desirable to differentiate between OROV and other common viral illnesses endemic to the area. However, this type of assay requires specialized equipment and reagents, as well as appropriate storage of samples. Other methods, such as the ELISA to detect antibodies against recombinant OROV nucleocapsid38, maybe more easily adopted. Regardless of the method, there is currently no diagnostic standard for OROV, and the field would benefit from standardization to assist in the development and validation of more reliable and readily available diagnostic tools.
Epidemiology
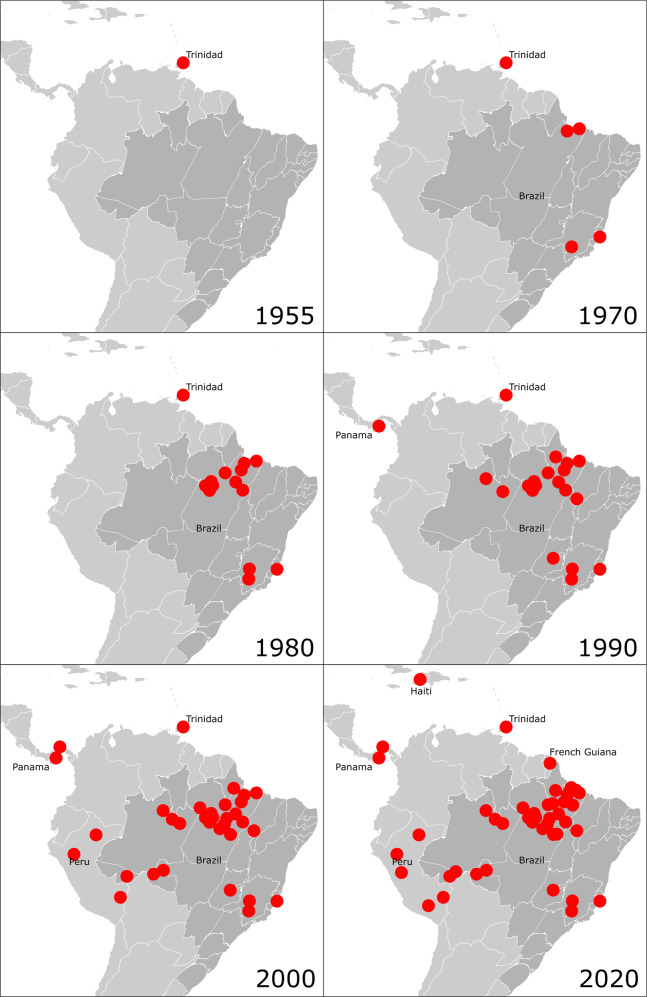
Following its isolation in Trinidad in 19551, OROV was next seen clinically in 1961, in an epidemic in Belém, Brazil that involved an estimated 11,000 people. Peru experienced its first epidemic in the city of Iquitos in 19922. The virus has also been found in Central America where it was first isolated in 1989 from febrile patients in Panama during a dengue surveillance program2. Subsequently, epidemiologic surveillance has shown OROV circulation in other South American countries, including Bolivia, Ecuador, Colombia, and Venezuela19,49–51, and more recently in Haiti in 201452 and French Guiana in 202053. A description of OROF outbreaks by location has been published elsewhere54. and is shown pictorially over time in Fig. 1. The majority of reported cases continue to occur in the Amazon region of Brazil and Peru. Since 1961 there have been over 30 epidemics of OROF in Brazil, all in the Amazon region55,56. The largest epidemic to date occurred in Manaus, Brazil in 1980 resulting in an estimated 97,000 cases (approximately 15% of the population)57. Seven urban epidemics between 1961 and 1978 in Pará, Brazil were analyzed and found to have a common attack rate of approximately 30%56. More than half a million people residing in the Amazon region of Brazil alone are estimated to have been infected with OROV56. It is suspected that the incidence and disease burden of OROV is underestimated due to the similarity of its clinical presentation to febrile illnesses caused by other arboviruses, such as dengue, Zika, chikungunya, and yellow fever. Current surveillance for OROV is limited and the majority of surveillance methods focus on serological testing in humans and animals25,56,58.
Fig. 1. Timeline of Oropouche fever outbreaks.
Red dots indicate outbreaks with serological evidence and/or confirmatory viral nucleic acid detection. Data were taken from refs. 1–3,52,54,94. Map graphics adapted from ref. 95.
OROV is maintained in nature through two transmission cycles: an urban cycle and a sylvatic cycle. The urban cycle, which is generally associated with explosive outbreaks of disease, is believed to primarily involve the biting midge Culicoides paraensis25,59. Moreover, epidemics of OROF in Brazil have a seasonal pattern and have predominantly occurred during the rainy season (January to June) which is associated temporally with the highest density of C. paraensis populations56,60. Humans are believed to be the only vertebrate host in the urban cycle since OROV infection has not been detected in domestic animals, except birds. Known arthropod vectors for OROV besides C. paraensis are the mosquito species Culex quinquefasciatus, Coquillettidia venezuelensis, Mansonia venezuelensis, and Aedes serratus1,25,56. C. paraensis is the main vector in Brazil but has a wide geographic range that extends from Argentina and Chile to include large areas in the United States (see Fig. 2)61. A recent study evaluated vector competence of the prototype OROV strain TrVL 9760 in three North American vector species: Cx. tarsalis, Cx. quinquefasciatus, and the midge C. sonorensis62. Both mosquito species were relatively poor vectors whereas C. sonorensis showed high infection and dissemination, and good transmission potential. Thus, there is potential for OROV to emerge across a wide geographic area. Precedence for emergence can be seen with the related orthobunyavirus, SBV, an important veterinary pathogen in ruminants such as sheep and cattle that is also spread by Culicoides midges63. SBV emerged in Germany, the Netherlands, and Belgium in 2011 and has since spread through much of Europe64.
Fig. 2. Distribution of Culicoides paraensis in the Americas.
Dark gray indicates countries and states where C. paraensis has been reported61,96–101. Map template modified from ref. 102.
The main vertebrate hosts involved in the sylvatic cycle have not been fully identified, but there is evidence that wild birds, the three-toed sloth (Bradypus tridactylus), and certain species of New World non-human primates (NHP)—principally capuchin and howler monkeys—are involved10,25,50. Among wild birds, HI antibodies were detected in members of the families Formicariidae, Troglodytidae, Cuculidae, Fringillidae, Dendrocolaptidae, Tyrannidae, Vireonidae, Thraupidae, and Pipridae65. Additionally, HI antibodies to OROV have been found in domestic chickens and one duck65. A variety of domestic vertebrates were tested for the presence of antibodies to OROV during five epidemics in Brazil. No OROV-specific antibodies were detected in cats, dogs, or pigs25,56.
All four of the OROV genotypes have been detected in Brazil. OROV isolates recovered from outbreaks in Brazil revealed that genotype I is more prevalent in the eastern Amazon region and genotype II is more prevalent in the western Amazon region15,40,51. Genotype III was originally thought to be restricted to Panama, but was detected in Minas Gerais State, southeastern Brazil in 200015,50. Genotype IV appears to be restricted to Amazonas State, Brazil15.
Environmental and climate changes, as well as deforestation for agriculture and urbanization are predicted to be drivers for the emergence of arboviral epidemics and re-emergence of yellow fever, Mayaro, and OROV10,60,66,67. In Cusco, Peru, areas with vegetation loss were common locations for recent outbreaks of OROF68. However, ecological niche models suggested this observation could also be due to favorable transmission conditions coinciding in neighboring areas68. One study from Brazil examined the effects of construction and flooding on the transmission of sylvatic arboviruses. The construction of a dam in the 1980s flooded large areas in the Tucuruí area of Pará State for a three-month period. Over one million mosquitoes were captured, and a significant number of new viruses were isolated. While only one strain of OROV was isolated, there were high annual rates of OROV antibody-positive birds and NHPs during the flooding period, creating suitable ecological conditions for transmission. Prevalence rates were between 2 and 7.1% for birds, and 8.5% for monkeys69. More research is urgently needed to assess the relationship between landscape changes, the emergence of OROV, and other arboviral epidemics.
OROV has spread from the Amazon and is making its way into urban areas of endemic South American countries. Current prevention strategies focus on the control and reduction of arthropod vectors mainly by the elimination of vector breeding sites with chemical insecticides. Education efforts emphasizing the importance of topical insecticides and having personal protective products such as bug nets are also being employed56. However, the effectiveness of this individual approach may be limited by a lack of financial resources and access to these materials. Further investigation is needed to fully comprehend the epidemiology of OROV. Additionally, better surveillance methods and determination of incidence are needed to understand the exact burden OROV has on Central and South American countries.
Animal models
OROV infection has been examined in a number of small animal models. Suckling and adult white Swiss mice inoculated intracranially (IC) with a high dose of the virus were highly susceptible to disease and all animals succumbed within 3 days. Lower doses also produced uniform lethality but with an extended incubation period. Intraperitoneal (IP) inoculation with the high dose of virus was lethal to infant mice but induced no clinical signs in adult mice1.
Although immunocompetent adult mice have proven resistant to disease following peripheral OROV challenge, more recent studies using adult animals of a number of immune gene knockout (KO) strains have produced lethality. The most thoroughly studied are strains involving KOs in innate immune sensing mediators associated with the RIG-I-like receptors. Specifically, the importance of innate immune sensing is suggested by hepatic injury and reduced survival of mitochondrial antiviral signaling protein knockout (MAVS−/−) mice compared to wild types (~40% compared to 0% mortality, respectively)70. On examination of downstream signaling events, interferon (IFN) regulatory factor 3 and IFN regulatory factor 7 (IRF3−/− IRF7−/−) double knockout (DKO) mice experienced lethal infection; whereas, individually, the IRF3 and IRF7 KO models showed >90% survival. Interestingly, OROV-infected IFN regulatory factor 5 KO (IRF5−/−) mice exhibited signs of hepatic injury early in the infection, increased viral titers in the spinal cord, and delayed death relative to IRF3−/− IRF7−/− DKO mice71. OROV-infected IFN-β−/− mice lost weight and exhibited a lethality rate of 17%, suggesting that IFN-β plays some role in protection against OROV infection in mice. However, the lower rates of lethality in IFN-β−/− mice and IRF3−/− IRF7−/− DKO mice (~50%) in comparison to IFN-α/β receptor KO (IFNAR−/−) mice (100% lethality) suggest that IFN-β alone is not solely responsible for the protection and that IFN-α may be critical in controlling OROV infection70. In mice that lacked intact type I IFN signaling (IFNAR KO, MAVS KO, IRF3 KO, IRF7 KO), OROV titer was highest in the liver, spleen, and blood and caused extensive liver damage (dead cells, hemorrhages, tissue discoloration)70,71.
Hamsters have also been used to model OROV pathogenesis. Anderson et al.1 showed that OROV caused disease in adult Syrian golden hamsters (Mesocrisetus auratus) after either IC or IP inoculation. Signs of disease using either route of inoculation included loss of appetite, coat ruffling, and difficulty walking, with some animals showing complete hind limb paralysis. Virus titers in the brain at death (105 units/0.02 mL) were similar using either route of inoculation1. Subsequently, a subcutaneous (SC) challenge model was developed in 3-week-old hamsters that resulted in over 50% of the animals developing the severe disease (lethargy, ruffled fur, weight loss, shivering, walking difficulty, paralysis) and approximately one-third succumbed. High titers of OROV were present in the blood, liver, and brain (102–107 TCID50/mL or /g). Notably, viral antigen was strongly associated with neurons. This was accompanied by histopathological signs of meningoencephalitis (microglial nodules, infiltrating mononuclear cells, perivascular cuffs with leukocytes) and hepatitis (infiltrating mononuclear cells, eosinophils, necrosis, Kupffer cell activation). In the liver, the viral titer remained higher than 104 TCID50/g of tissue from day 3 until day 11 post-infection, suggesting highly efficient replication of the virus in this organ72. Overall, following infection by the SC route, hamsters show systemic infection, neurological motor impairment, paralysis, and virus accumulation in the brain and liver. They also develop fatal hepatitis, necrosis of hepatocytes, and Kupffer cell hyperplasia. It has been hypothesized that macrophages capture OROV and transfer it to hepatocytes72. Hepatic lesions were seen 6 h post-inoculation73. The fact that the virus caused these liver manifestations even after only being introduced via the IC route signifies that this virus may have very specific tissue tropism for the liver1.
To date, there are no reports of well-characterized NHP models of OROV infection. Serological surveys show that multiple New World NHPs, including capuchin and howler monkeys, have OROV antibodies suggesting they are susceptible to infection1. However, there are no reports of overt clinical signs of illness in New World NHPs infected with OROV experimentally and there have been no investigations of the use of Old World NHPs (baboons and macaques).
Immunology
OROV infection results in the production of type I IFN in multiple mouse strains70,71,74. The high mortality in IFNAR KO mice demonstrates that protection against lethal infection in mice is dependent on appropriate IFNAR signaling. When IFNAR signaling was selectively knocked out in granulocytes and dendritic cells, infection was not lethal, suggesting that subsets of non-myeloid cells are predominantly responsible for producing protective IFN. In fact, in mice where IFNAR signaling was ablated in granulocytes, there was an improved survival rate, suggesting that perhaps IFN signaling in granulocytes may play a role in OROV pathogenesis70.
In one of the few immunological studies in humans, IFN-α was shown to be a universal biomarker of OROV infection evidenced by high levels of expression regardless of OROV antibody titer34. This study also showed that the cytokine profiles exhibited by early and late seroconverters were highly divergent. Early seroconverters were defined as patients with high titers of IgM and IgG 1–7 days after disease onset while late seroconverters developed high titers ≥8 days after disease onset. Early seroconverters expressed high levels of interleukin (IL)-5, presumably resulting in the differentiation of antibody-producing plasma cells earlier in infection. Early seroconverters also expressed high levels of C-X-C motif chemokine ligand (CXCL) 8, known to recruit neutrophils and other granulocytes; however, the role of neutrophilic activity in OROV pathogenesis has yet to be characterized. Late seroconverters expressed high levels of IL-17 and CXCL10 (also known as IP-10). All patients demonstrated increased levels of IFN-α and CXCL8, and decreased levels of tumor necrosis factor (TNF) and IL-10. Regardless of the association between seroconversion and cytokine profile, there was no correlation between time of seroconversion and viremia or symptomology34.
While type I IFN responses appear essential to combat OROV infection, the IFN-stimulated genes responsible for the restriction of OROV replication remain to be fully elucidated. There are few studies that explore the host response to OROV infection, and even fewer that utilize patient samples. There are currently no studies following patients who have cleared OROV infection, thus the adaptive immune response to OROV infection is poorly understood. Furthermore, questions regarding the role of T cells in the pathogenesis or control of OROV and the kinetics of B cell activation, differentiation, and OROV-specific antibody production remain unanswered.
Antivirals
Currently, there is no specific antiviral therapy for OROV infection, and existing literature describing possible treatments for OROF is limited. Ribavirin (RBV), mycophenolic acid (MPA), and IFN-α have been investigated for OROV treatment. In in vitro studies, RBV showed no antiviral activity against OROV infection but was active against two other orthobunyaviruses (Tacaiuma virus (TCMV) and Guama virus (GMAV))75. RBV had no antiviral activity against OROV or any of the other orthobunyaviruses tested in newborn Swiss mice75. Similarly, in vitro administration of MPA had no antiviral activity against OROV but was active against GMAV and TCMV76. IFN-α showed limited activity in vitro that was dependent on the dose and timing of treatment77. In vivo, mice dosed IP route with 30 μL of IFN-α-2a per day for 10 days beginning 1 day before infection survived a lethal OROV challenge. When treatment was initiated 3 or 24 h after infection the protective effect on mortality was lost and viral replication in the brain was not prevented77.
The drug favipiravir, a nucleoside analog, has not been tested against OROV, but shows promising activity against multiple viruses belonging to the family Peribunyaviridae suggesting such studies are warrented78,79.
Vaccines
To date, there has been only one published preclinical or clinical study on candidate OROF vaccines, other than an immunoinformatic analysis that identified a number of putative T and B cell epitopes within the OROV M-segment polyprotein80. Recently, a candidate vaccine based on replication-competent vesicular stomatitis virus (VSV) expressing the OROV glycoproteins was shown to protect mice from wild-type challenge. Briefly, C57BL/6 mice were given two doses of 106 focus forming units (ffu) of rVSV-OROV by the SC route, 28 days apart, and challenged 7 days later with 106 TCID50 OROV strain BeAn19991 by the SC route. Protection was shown by no loss of body weight or increase in body temperature, and reduced viral loads in vaccinated mice compared to control mice81.
The recent development of a reverse genetics system for OROV should prove beneficial to vaccine development6. Vaccine development efforts for OROF are likely to be guided by approaches taken with other orthobunyaviruses of clinical and veterinary interest where live attenuated, chemically inactivated, DNA-vectored, and protein-subunit immunization strategies have been employed. Attenuation strategies include deletion of the nonstructural proteins82,83 or parts of the UTRs11, swapping of UTRs between segments84, swapping of the M segment coding regions of related orthobunyaviruses85, and mutation of N86.
OROF vaccine development may also be informed by attempts to develop vaccines against other members of the Simbu serogroup87–89. A number of these viruses, particularly SBV, Aino, and Akabane (AKAV) viruses are important veterinary pathogens. A binary ethylenimine (BEI)-inactivated SBV vaccine containing a pre-inactivation titer of about 106 TCID50/mL is approved in the European Union for IM administration to cattle and SC administration to sheep. Two immunizations with this vaccine reduced (in cattle) or prevented (in sheep) viremia when animals were challenged with infectious serum 2 weeks after the second immunization90.
A live attenuated SBV candidate vaccine lacking both NSs and NSm, when administered SC in a single 106 TCID50/mL dose (volume unspecified), was protective in cattle, preventing clinical signs and detectable viral load in the serum of previously SBV-naive calves after either immunization or challenge with infectious cattle serum, and by neutralizing antibody titers of at least 5 by 7 days post-challenge83. A bivalent SBV-AKAV protein-subunit candidate vaccine consisting of the N-termini of the Gc proteins from both SBV and AKAV, expressed in HEK-293T cells and covalently-linked has also been developed. When this vaccine was administered SC in two 50 μg doses three weeks apart, it was found to protect against challenge with a cattle-passaged field strain of SBV. Animals showed no clinical signs or detectable viral RNA in the blood or organs and neutralizing antibody titers were at least 20 at the time of challenge91. Two candidate DNA-vectored vaccines, encoding either N or the ectodomain of Gc, were protective in IFNAR−/− mice preventing weight loss and reducing viremia compared to mock-vaccinated controls92. While neither vaccine candidate induced detectable neutralizing antibody, the N vaccine induced high levels of SBV-specific binding antibody and the Gc vaccine-induced proliferation of SBV-specific CD8+ T cells.
Conclusions
OROV is a significant public health problem producing ongoing endemic disease and periodic outbreaks in substantial areas of South America. Further, there is clear potential for the virus to emerge or undergo reassortment in new geographic areas, increasing the population at risk for infection. Despite this, it is clear that comparatively little is known about the virus and there are at present no candidate medical countermeasures, other than one study of a candidate vaccine in a mouse model. This may in part be because virus infection is not lethal. There are comparatively large, active vaccine and drug research programs for Crimean-Congo hemorrhagic fever, Powassan, Nipah, and Middle Eastern respiratory syndrome (MERS) viruses—all of which cause fewer clinical cases than OROV but which are responsible for fatal infections. Nonetheless, it should be remembered that three other arboviruses have emerged to cause high morbidity with little mortality. Mosquito-borne Zika virus is associated with permanently disabling illness and some mortality in neonates, while mosquito-borne chikungunya virus is another example of a debilitating but non-lethal arboviral disease that has emerged globally in the recent past92. Both viruses rapidly emerged into global public health problems. Similarly, Culicoides midge-borne SBV rapidly emerged in Europe to become a major veterinary problem64. Of particular note is that the transmission cycle of OROV is incompletely understood and that the geographic range of the arthropod vectors C. paraensis and C. sonorensis includes North America. Additionally, the potential of birds as vertebrate hosts, raise concerns for the potential emergence of OROV in different geographic locations. Further, the proven ability of OROV and closely related viruses to produce reassortants represents a poorly defined public health threat.
The lack of publications on the evaluation of candidate antivirals against OROV is a concern as is only one report on candidate vaccines. Other bunyaviruses have had their envelope glycoproteins expressed using different vaccine platform technologies; thus, such platforms should be able to be translated to candidate OROV vaccines with relatively little effort. There is insufficient information to justify a preventative vaccine program, although this may change with improved diagnostics. Thus, a reactive vaccine program is considered more applicable.
Perhaps the most significant deficiency at this time is the lack of a characterized NHP model to evaluate candidate antivirals and vaccines for efficacy. The fact that serologic surveys indicate that multiple New World primate species are susceptible to infection provides evidence that the development of such models is possible. To date, the clinical impact of OROV has not driven the development of such models. However, this would appear warranted with the potential for OROV to become a significant public health pathogen.
Overall, OROV has the potential to become a major public health problem in an expanded geographic area, and there is an urgent need to evaluate medical countermeasures in case the virus emerges as Zika virus did a few years ago93.
Author contributions
All authors reviewed the literature, provided substantial input, and reviewed the paper; contributed equally to the critical revisions of the manuscript; approved the final article; and are accountable for all aspects of the work.
Competing interests
A.D.T.B is the editor-in-Chief of npj Vaccines. The remaining authors declare no competing financial and non-financial interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Megan A. Files, Clairissa A. Hansen, Vanessa C. Herrera, Craig Schindewolf.
References
- 1.Anderson CR, Spence L, Downs WG, Aitken TH. Oropouche virus: a new human disease agent from Trinidad, West Indies. Am. J. Trop. Med. Hyg. 1961;10:574–578. doi: 10.4269/ajtmh.1961.10.574. [DOI] [PubMed] [Google Scholar]
- 2.Travassos da Rosa JF, et al. Oropouche virus: clinical, epidemiological, and molecular aspects of a neglected orthobunyavirus. Am. J. Trop. Med. Hyg. 2017;96:1019–1030. doi: 10.4269/ajtmh.16-0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gutierrez, B. et al. Evolutionary dynamics of Oropouche virus in South America. J. Virol. 10.1128/jvi.01127-19 (2020). [DOI] [PMC free article] [PubMed]
- 4.Ladner JT, et al. Genomic and phylogenetic characterization of viruses included in the Manzanilla and Oropouche species complexes of the genus Orthobunyavirus, family Bunyaviridae. J. Gen. Virol. 2014;95:1055–1066. doi: 10.1099/vir.0.061309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elliott RM. Orthobunyaviruses: recent genetic and structural insights. Nat. Rev. Microbiol. 2014;12:673–685. doi: 10.1038/nrmicro3332. [DOI] [PubMed] [Google Scholar]
- 6.Tilston-Lunel NL, Acrani GO, Randall RE, Elliott RM. Generation of recombinant Oropouche viruses lacking the nonstructural protein NSm or NSs. J. Virol. 2015;90:2616–2627. doi: 10.1128/JVI.02849-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hellert J, et al. Orthobunyavirus spike architecture and recognition by neutralizing antibodies. Nat. Commun. 2019;10:879. doi: 10.1038/s41467-019-08832-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowden TA, et al. Orthobunyavirus ultrastructure and the curious tripodal glycoprotein spike. PLoS Pathog. 2013;9:e1003374. doi: 10.1371/journal.ppat.1003374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aquino VH, Moreli ML, Moraes Figueiredo LT. Analysis of Oropouche virus L protein amino acid sequence showed the presence of an additional conserved region that could harbour an important role for the polymerase activity. Arch. Virol. 2003;148:19–28. doi: 10.1007/s00705-002-0913-4. [DOI] [PubMed] [Google Scholar]
- 10.Tilston-Lunel NL, et al. Genetic analysis of members of the species Oropouche virus and identification of a novel M segment sequence. J. Gen. Virol. 2015;96:1636–1650. doi: 10.1099/vir.0.000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazel-Sanchez, B. & Elliott, R. Attenuation of Bunyamwera orthobunyavirus replication by targeted mutagenesis of genomic untranslated regions and creation of viable viruses with minimal genome segments. J. Virol. 10.1128/JVI.02253-12 (2012). [DOI] [PMC free article] [PubMed]
- 12.Obijeski JF, Bishop DH, Murphy FA, Palmer EL. Structural proteins of La Crosse virus. J. Virol. 1976;19:985–997. doi: 10.1128/jvi.19.3.985-997.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nunes MRT, et al. Oropouche orthobunyavirus: genetic characterization of full-length genomes and development of molecular methods to discriminate natural reassortments. Infect. Genet. Evol. 2019;68:16–22. doi: 10.1016/j.meegid.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, et al. Evolutionary history of Simbu serogroup orthobunyaviruses in the Australian episystem. Virology. 2019;535:32–44. doi: 10.1016/j.virol.2019.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Vasconcelos HB, et al. Molecular epidemiology of Oropouche virus, Brazil. Emerg. Infect. Dis. 2011;17:800–806. doi: 10.3201/eid1705.101333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tilston-Lunel NL, Shi X, Elliott RM, Acrani GO. The potential for reassortment between Oropouche and Schmallenberg orthobunyaviruses. Viruses. 2017;9:220. doi: 10.3390/v9080220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yanase T, et al. Genetic reassortment between Sathuperi and Shamonda viruses of the genus Orthobunyavirus in nature: implications for their genetic relationship to Schmallenberg virus. Arch. Virol. 2012;157:1611–1616. doi: 10.1007/s00705-012-1341-8. [DOI] [PubMed] [Google Scholar]
- 18.Aguilar PV, et al. Iquitos virus: a novel reassortant Orthobunyavirus associated with human illness in Peru. PLoS Negl. Trop. Dis. 2011;5:e1315. doi: 10.1371/journal.pntd.0001315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Navarro J-C, et al. Isolation of Madre de Dios Virus (Orthobunyavirus; Bunyaviridae), an Oropouche virus species reassortant, from a monkey in Venezuela. Am. J. tropical Med. Hyg. 2016;95:328–338. doi: 10.4269/ajtmh.15-0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Briese T, Bird B, Kapoor V, Nichol ST, Lipkin WI. Batai and Ngari viruses: M segment reassortment and association with severe febrile disease outbreaks in East Africa. J. Virol. 2006;80:5627–5630. doi: 10.1128/JVI.02448-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mercer DR, Spinelli GR, Watts DM, Tesh RB. Biting rates and developmental substrates for biting midges (Diptera: Ceratopogonidae) in Iquitos, Peru. J. Med. Entomol. 2003;40:807–812. doi: 10.1603/0022-2585-40.6.807. [DOI] [PubMed] [Google Scholar]
- 22.Pinheiro FP, Travassos da Rosa AP, Gomes ML, LeDuc JW, Hoch AL. Transmission of Oropouche virus from man to hamster by the midge Culicoides paraensis. Science. 1982;215:1251–1253. doi: 10.1126/science.6800036. [DOI] [PubMed] [Google Scholar]
- 23.Pinheiro, F. P. Travossos da Rosa, A. P. A. & Vasconcelos, P. F. D. C. Feigin and Cherry’s textbook of pediatric infectious diseases 7th edn (Saunders, 2014).
- 24.Sakkas H, Bozidis P, Franks A, Papadopoulou C. Oropouche fever: a review. Viruses. 2018;10:175. doi: 10.3390/v10040175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pinheiro FP, et al. Oropouche virus. I. A review of clinical, epidemiological, and ecological findings. Am. J. Trop. Med. Hyg. 1981;30:149–160. [PubMed] [Google Scholar]
- 26.Pinheiro, F. P. & Travossos da Rosa, A. P. A. Arboviral Zoonoses of Central and South America. Handbook of Zoonoses Section B: Viral Zoonoses 2nd edn (CRC Press, 1994).
- 27.Vasconcelos HB, et al. Oropouche fever epidemic in Northern Brazil: epidemiology and molecular characterization of isolates. J. Clin. Virol. 2009;44:129–133. doi: 10.1016/j.jcv.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 28.Alvarez-Falconi PP, R¡os Ruiz BA. [Oropuche fever outbreak in Bagazan, San Martin, Peru: epidemiological evaluation, gastrointestinal and hemorrhagic manifestations] Rev. Gastroenterol. 2020;30:334–340. [PubMed] [Google Scholar]
- 29.Vasconcelos PF, et al. [1st register of an epidemic caused by Oropouche virus in the states of Maranhão and Goiás, Brazil] Rev. Inst. Med. Trop. 1989;31:271–278. doi: 10.1590/s0036-46651989000400011. [DOI] [PubMed] [Google Scholar]
- 30.Mourão, M. P. G. et al. Oropouche fever outbreak, Manaus, Brazil, 2007–2008. Emerg. Infect. Dis. 2063–2064 (2009). [DOI] [PMC free article] [PubMed]
- 31.Cardoso BF, et al. Detection of Oropouche virus segment S in patients and in Culex quinquefasciatus in the state of Mato Grosso, Brazil. Mem. Inst. Oswaldo Cruz. 2015;110:745–754. doi: 10.1590/0074-02760150123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tesh RB. The emerging epidemiology of Venezuelan hemorrhagic fever and Oropouche fever in tropical South America. Ann. NY Acad. Sci. 1994;740:129–137. doi: 10.1111/j.1749-6632.1994.tb19863.x. [DOI] [PubMed] [Google Scholar]
- 33.Bastos MES, et al. Identification of Oropouche Orthobunyavirus in the cerebrospinal fluid of three patients in the Amazonas, Brazil. Am. J. Trop. Med. Hyg. 2012;86:732–735. doi: 10.4269/ajtmh.2012.11-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Oliveira, E. et al. IFN-α as a time-sensitive biomarker during Oropouche virus infection in early and late seroconverters. Sci. Rep. 10.1038/s41598-019-54223-w (2019). [DOI] [PMC free article] [PubMed]
- 35.Watts DM, et al. Venezuelan equine encephalitis and Oropouche virus infections among Peruvian army troops in the Amazon region of Peru. Am. J. Trop. Med. Hyg. 1997;56:661–667. doi: 10.4269/ajtmh.1997.56.661. [DOI] [PubMed] [Google Scholar]
- 36.Gibrail MM, et al. Detection of antibodies to Oropouche virus in non-human primates in Goiânia City, Goiás. Rev. Soc. Bras. Med. Trop. 2016;49:357–360. doi: 10.1590/0037-8682-0425-2015. [DOI] [PubMed] [Google Scholar]
- 37.Pauvolid-Corrêa A, Campos Z, Soares R, Nogueira RMR, Komar N. Neutralizing antibodies for orthobunyaviruses in Pantanal, Brazil. PLOS Negl. Trop. Dis. 2017;11:e0006014–e0006014. doi: 10.1371/journal.pntd.0006014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saeed MF, et al. Diagnosis of Oropouche virus infection using a recombinant nucleocapsid protein-based enzyme immunoassay. J. Clin. Microbiol. 2001;39:2445–2452. doi: 10.1128/JCM.39.7.2445-2452.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Camarão AAR, Swanepoel R, Boinas F, Quan M. Development and analytical validation of a group-specific RT-qPCR assay for the detection of the Simbu serogroup orthobunyaviruses. J. Virol. Methods. 2019;271:113685–113685. doi: 10.1016/j.jviromet.2019.113685. [DOI] [PubMed] [Google Scholar]
- 40.Saeed MF, et al. Nucleotide sequences and phylogeny of the nucleocapsid gene of Oropouche virus. J. Gen. Virol. 2000;81:743–748. doi: 10.1099/0022-1317-81-3-743. [DOI] [PubMed] [Google Scholar]
- 41.Fonseca LMDS, Carvalho RH, Bandeira AC, Sardi SI, Campos GS. Oropouche virus detection in febrile patients’ saliva and urine samples in salvador, Bahia, Brazil. Jpn. J. Infect. Dis. 2020;73:164–165. doi: 10.7883/yoken.JJID.2019.296. [DOI] [PubMed] [Google Scholar]
- 42.Moreli ML, Aquino VH, Cruz AC, Figueiredo LT. Diagnosis of Oropouche virus infection by RT-nested-PCR. J. Med. Virol. 2002;66:139–142. doi: 10.1002/jmv.2122. [DOI] [PubMed] [Google Scholar]
- 43.Naveca FG, et al. Multiplexed reverse transcription real-time polymerase chain reaction for simultaneous detection of Mayaro, Oropouche, and oropouche-like viruses. Mem. Inst. Oswaldo Cruz. 2017;112:510–513. doi: 10.1590/0074-02760160062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weidmann M, Rudaz V, Nunes MRT, Vasconcelos PFC, Hufert FT. Rapid detection of human pathogenic orthobunyaviruses. J. Clin. Microbiol. 2003;41:3299–3305. doi: 10.1128/JCM.41.7.3299-3305.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rojas A, et al. Real-time RT-PCR for the detection and quantitation of Oropouche virus. Diagn. Microbiol. Infect. Dis. 2020;96:114894–114894. doi: 10.1016/j.diagmicrobio.2019.114894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Do Nascimento, V. A. et al. Oropouche virus detection in saliva and urine. Mem. Inst. Oswaldo Cruz10.1590/0074-02760190338 (2020). [DOI] [PMC free article] [PubMed]
- 47.Wise EL, et al. Isolation of Oropouche virus from febrile patient, Ecuador. Emerg. Infect. Dis. 2018;24:935–937. doi: 10.3201/eid2405.171569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wise EL, et al. Oropouche virus cases identified in Ecuador using an optimised qRT-PCR informed by metagenomic sequencing. PLoS Negl. Trop. Dis. 2020;14:e0007897. doi: 10.1371/journal.pntd.0007897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Forshey BM, et al. Arboviral etiologies of acute febrile illnesses in Western South America, 2000-2007. PLoS Negl. Trop. Dis. 2010;4:e787–e787. doi: 10.1371/journal.pntd.0000787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nunes MRT, et al. Oropouche virus isolation, southeast Brazil. Emerg. Infect. Dis. 2005;11:1610–1613. doi: 10.3201/eid1110.050464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Azevedo RS, et al. Reemergence of Oropouche fever, northern Brazil. Emerg. Infect. Dis. 2007;13:912–915. doi: 10.3201/eid1306.061114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elbadry, M. A. et al. Orthobunyaviruses in the Caribbean: Melao and Oropouche virus infections in school children in Haiti in 2014. PLoS Negl. Trop. Dis. 10.1371/journal.pntd.0009494 (2021). [DOI] [PMC free article] [PubMed]
- 53.Gaillet M, et al. Outbreak of Oropouche virus in French Guiana. Emerg. Infect. Dis. 2021;27:2711–2714. doi: 10.3201/eid2710.204760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Romero-Alvarez D, Escobar LE. Oropouche fever, an emergent disease from the Americas. Microbes Infect. 2018;20:135–146. doi: 10.1016/j.micinf.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 55.Pinheiro, M., Bensabath, G., Causey, O. R. & Shope, R. E. Epidemia de vírus Oropouche em Belém - Nota prévia(Publicado originalmente em 1962) (Instituto Evandro Chagas, 2002).
- 56.Pinheiro, F., Travassos, D., Rosapedro, A. & Vasconcelos, F. Oropouche fever. Textbook of Pediatric Infectious Diseases. 5th edn (W.B. Saunders, 2004).
- 57.Borborema CA, et al. [1st occurrence of outbreaks caused by Oropouche virus in the State of Amazonas] Rev. Inst. Med Trop. 1982;24:132–139. [PubMed] [Google Scholar]
- 58.Baisley KJ, Watts DM, Munstermann LE, Wilson ML. Epidemiology of endemic Oropouche virus transmission in upper Amazonian Peru. Am. J. Trop. Med. Hyg. 1998;59:710–716. doi: 10.4269/ajtmh.1998.59.710. [DOI] [PubMed] [Google Scholar]
- 59.Dixon KE, Travassos da Rosa AP, Travassos da Rosa JF, Llewellyn CH. Oropouche virus. II. Epidemiological observations during an epidemic in Santarém, Pará, Brazil in 1975. Am. J. Trop. Med. Hyg. 1981;30:161–164. [PubMed] [Google Scholar]
- 60.Pinheiro, F. P., Travassos da Rosa, A. P. A. & Vasconcelos Pedro, F. C. In An Overview of Arbovirology in Brazil and Neighbouring Countries Belém (eds Travassos da Rosa, A. P. A., Vasconcelos, P. F. C. & Travassos da Rosa, J. F. S.) 186–192 (Erandro Chagas Instituto, 1998).
- 61.Wirth W, Felippe-Bauer M. The neotropical biting midges related to Culicoides paraensis (Diptera: Ceratopogonidae) Mem. Inst. Oswaldo Cruz. 1989;84:551–565. [Google Scholar]
- 62.McGregor BL, Connelly CR, Kenney JL. Infection, dissemination, and transmission potential of North American Culex quinquefasciatus, Culex tarsalis, and Culicoides sonorensis for Oropouche virus. Viruses. 2021;13:226. doi: 10.3390/v13020226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wernike, K. & Beer, M. Schmallenberg virus: to vaccinate, or not to vaccinate? Vaccines10.3390/vaccines8020287 (2020). [DOI] [PMC free article] [PubMed]
- 64.Stavrou A, Daly JM, Maddison B, Gough K, Tarlinton R. How is Europe positioned for a re-emergence of Schmallenberg virus? Vet. J. 2017;230:45–51. doi: 10.1016/j.tvjl.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 65.Pinheiro FP, Travassos da Rosa AP, Travassos da Rosa JF, Bensabath G. An outbreak of Oropouche virus diease in the vicinity of santarem, para, barzil. Tropenmed. Parasitol. 1976;27:213–223. [PubMed] [Google Scholar]
- 66.Pinheiro FP, et al. An outbreak of Mayaro virus disease in Belterra, Brazil. I. Clinical and virological findings. Am. J. Trop. Med. Hyg. 1981;30:674–681. doi: 10.4269/ajtmh.1981.30.674. [DOI] [PubMed] [Google Scholar]
- 67.Vasconcelos PF, et al. An epidemic of sylvatic yellow fever in the southeast region of Maranhao State, Brazil, 1993–1994: epidemiologic and entomologic findings. Am. J. Trop. Med. Hyg. 1997;57:132–137. doi: 10.4269/ajtmh.1997.57.132. [DOI] [PubMed] [Google Scholar]
- 68.Romero-Alvarez D, Escobar LE. Vegetation loss and the 2016 Oropouche fever outbreak in Peru. Mem. Inst. Oswaldo Cruz. 2017;112:292–298. doi: 10.1590/0074-02760160415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Degallier, N. et al. Modifications of arbovirus eco-epidemiology in Tucurui, Para, Brazilian Amazonia, related to the construction of a hydroelectric dam. In Arbovirus Research in Australia. pp 124–135. Proceedings of the Fifth Symposium. August 28-September 1, 1989, Brisbane, Australia. (Eds Uren, M. F., Blok, J. & Manderson, L. H.) CSIRO Tropical Animal Science, Brisbane: xviii + 393 p.
- 70.Proenca-Modena JL, et al. Oropouche virus infection and pathogenesis are restricted by MAVS, IRF-3, IRF-7, and type I interferon signaling pathways in nonmyeloid cells. J. Virol. 2015;89:4720–4737. doi: 10.1128/JVI.00077-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Proenca-Modena JL, et al. Interferon-regulatory factor 5-dependent signaling restricts orthobunyavirus dissemination to the central nervous system. J. Virol. 2016;90:189–205. doi: 10.1128/JVI.02276-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rodrigues AH, et al. Oropouche virus experimental infection in the golden hamster (Mesocrisetus auratus) Virus Res. 2011;155:35–41. doi: 10.1016/j.virusres.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 73.Araújo R, Dias LB, Araújo MT, Pinheiro F, Oliva OF. [Ultrastructural changes in the hamster liver after experimental inoculation with Oropouche arbovirus (type BeAn 19991)] Rev. Inst. Med. Trop. 1978;20:45–54. [PubMed] [Google Scholar]
- 74.Pinto AK, et al. Human and murine IFIT1 proteins do not restrict infection of negative-sense RNA viruses of the Orthomyxoviridae, Bunyaviridae, and Filoviridae families. J. Virol. 2015;89:9465–9476. doi: 10.1128/JVI.00996-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Livonesi MC, De Sousa RL, Badra SJ, Figueiredo LT. In vitro and in vivo studies of ribavirin action on Brazilian Orthobunyavirus. Am. J. Trop. Med. Hyg. 2006;75:1011–1016. [PubMed] [Google Scholar]
- 76.Livonesi MC, Moro de Sousa RL, Moraes Figueiredo LT. In vitro study of antiviral activity of mycophenolic acid on Brazilian orthobunyaviruses. Intervirology. 2007;50:204–208. doi: 10.1159/000099219. [DOI] [PubMed] [Google Scholar]
- 77.Livonesi MC, de Sousa RL, Badra SJ, Figueiredo LT. In vitro and in vivo studies of the Interferon-alpha action on distinct Orthobunyavirus. Antivir. Res. 2007;75:121–128. doi: 10.1016/j.antiviral.2007.01.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Furuta Y, Komeno T, Nakamura T. Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2017;93:449–463. doi: 10.2183/pjab.93.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gowen BB, Hickerson BT. Hemorrhagic fever of bunyavirus etiology: disease models and progress towards new therapies. J. Microbiol. 2017;55:183–195. doi: 10.1007/s12275-017-7029-8. [DOI] [PubMed] [Google Scholar]
- 80.Adhikari, U., Tayebi, M. & Rahman, M. Immunoinformatics approach for epitope-based peptide vaccine design and active site prediction against polyprotein of emerging Oropouche virus. J. Immunol. Res. 10.1155/2018/6718083 (2018). [DOI] [PMC free article] [PubMed]
- 81.Stubbs SH, et al. Vesicular stomatitis virus chimeras expressing the Oropouche virus glycoproteins elicit protective immune responses in mice. mBio. 2021;12:e0046321. doi: 10.1128/mBio.00463-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bridgen A, Weber F, Fazakerley J, Elliott R. Bunyamwera bunyavirus nonstructural protein NSs is a nonessential gene product that contributes to viral pathogenesis. Proc. Natl Acad. Sci. USA. 2001;98:664–669. doi: 10.1073/pnas.98.2.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kraatz, F. et al. Deletion mutants of Schmallenberg virus are avirulent and protect from virus challenge. J. Virol. 10.1128/JVI.02729-14 (2015). [DOI] [PMC free article] [PubMed]
- 84.Lowen, A., Boyd, A., Fazakerley, J. & Elliott, R. Attenuation of bunyavirus replication by rearrangement of viral coding and noncoding sequences. J. Virol. 10.1128/JVI.79.11.6940-6946.2005 (2005). [DOI] [PMC free article] [PubMed]
- 85.Bennett RS, Gresko AK, Nelson JT, Murphy BR, Whitehead SS. A recombinant chimeric La Crosse virus expressing the surface glycoproteins of Jamestown Canyon virus is immunogenic and protective against challenge with either parental virus in mice or monkeys. J. Virol. 2012;86:420–426. doi: 10.1128/JVI.02327-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Eifan SA, Elliott RM. Mutational analysis of the Bunyamwera orthobunyavirus nucleocapsid protein gene. J. Virol. 2009;83:11307–11317. doi: 10.1128/JVI.01460-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wernike K, Nikolin V, Hechinger S, Hoffmann B, Beer M. Inactivated Schmallenberg virus prototype vaccines. Vaccine. 2013;31:3558–3563. doi: 10.1016/j.vaccine.2013.05.062. [DOI] [PubMed] [Google Scholar]
- 88.Kim, Y. et al. Development of inactivated trivalent vaccine for the teratogenic Aino, Akabane and Chuzan viruses. Biologicals10.1016/j.biologicals.2011.02.004 (2011). [DOI] [PubMed]
- 89.Kurogi H, et al. Development of inactivated vaccine for Akabane disease. Natl Inst. Anim. Health Q. 1978;18:97–108. [PubMed] [Google Scholar]
- 90.European Medicines Agency Committee for Medicinal Products for Veterinary Use. CVMP assessment report for ZULVAC SBV (EMEA/V/C/002781/0000). https://www.ema.europa.eu/en/documents/assessment-report/zulvac-sbv-epar-public-assessment-report_en.pdf (2020).
- 91.Wernike, K., Aebischer, A., Roman-Sosa, G. & Beer, M. The N-terminal domain of Schmallenberg virus envelope protein Gc is highly immunogenic and can provide protection from infection. Sci. Rep. 10.1038/srep42500 (2017). [DOI] [PMC free article] [PubMed]
- 92.Puntasecca CJ, King CH, LaBeaud AD. Measuring the global burden of chikungunya and Zika viruses: a systematic review. PLoS Negl. Trop. Dis. 2021;15:e0009055. doi: 10.1371/journal.pntd.0009055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Boshra, H. et al. DNA vaccination regimes against Schmallenberg virus infection in IFNAR−/− mice suggest two targets for immunization. Antivir. Res.10.1016/j.antiviral.2017.02.013 (2017). [DOI] [PubMed]
- 94.World Health Organization. Oropouche virus disease - French Guiana. https://www.who.int/emergencies/disease-outbreak-news/item/oropouche-virus-disease---french-guiana-france (2021).
- 95.Menegaz, F. Brazil Blank Map.svg. Wikimedia Commons. Attribution-Share Alike 3.0 Unported license. https://commons.wikimedia.org/wiki/File:Brazil_Blank_Map.svg (2021).
- 96.Smith, K. et al Monitoring of Culicoides spp. at a site enzootic for hemorrhagic disease in white-tailed deer in Georgia, USA. J. Wildlife Dis. 10.7589/0090-3558-32.4.627 (1996). [DOI] [PubMed]
- 97.Brickle D, Hagan D. The Culicoides (Diptera: Ceratopogonidae) of Belize. Cent. Am. Insect. Mundi. 1999;13:39–44. [Google Scholar]
- 98.Martin E, et al. Culicoides species community composition and infection status with parasites in an urban environment of east central Texas, USA. Parasites Vectors. 2019;12:39. doi: 10.1186/s13071-018-3283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Aybar, C., Juri, M., de Grosso, M. & Spinell, G. New records of Culicoides species (Diptera: Ceratopogonidae) for Bolivia. J. Am. Mosq. Control Assoc.10.2987/10-6059.1 (2011). [DOI] [PubMed]
- 100.Pappas L, Moyer S, Pappas C. Tree hole Culicoides (Diptera: Ceratopogonidae) of the Central Plains in the United States. J. Am. Mosq. Control Assoc. 1991;7:624–627. [PubMed] [Google Scholar]
- 101.Lamberson C, Pappas C, Pappas L. Pupal taxonomy of the tree-hole Culicoides (Diptera: Ceratopogonidae) in eastern North America. Ann. Entomol. Soc. Am. 1992;85:111–120. [Google Scholar]
- 102.Commons Wikimedia. File: Spanish speakers in the Americas (orthographic projection).svg. Attribution-Share Alike 3.0 Unported license. https://commons.wikimedia.org/wiki/File:Spanish_speakers_in_the_Americas_(orthographic_projection).svg (2020).