Abstract
Posterior wall fractures are the most common type of acetabular fractures. Treatment can be conservative or surgical. Operative treatment is indicated for acetabular fractures that result in hip joint instability and/or incongruity, as well injuries with incarceration of fragments of bone or soft tissue within the hip joint. Surgical treatment can range from open reduction and osteosynthesis to hip arthroplasty. Arthroscopy has recently been used as the main surgical technique or as a reduction aid. In this case a 26-year-old male with a fracture of the posterior wall who underwent a posterior miniinvasive approach, followed by hip arthroscopy. This allowed joint wash, removal of the loose body, confirmation of reduction and absence of intra-articular hardware. Excellent clinical and radiological results were obtained. This case demonstrates the advantage of using hip arthroscopy in assessment of fracture reduction, the absence of intra-articular hardware or fragments, as well as a less invasive approach.
Keywords: Acetabulum, Arthroscopy, Fracture fixation, Hip joint
Fractures of the posterior wall of the acetabulum are of the elementary type, which is the most frequent type, accounting for approximately 25%1,2). In this type of fracture, an osteochondral fragment is detected in more than 46% of cases2). Operative treatment is indicated for acetabular fractures that result in hip joint instability and/or incongruity, as well in injuries with incarceration of fragments of bone or soft tissue within the hip joint, regardless of classification type1).
Treatment can be conservative or surgical, with the last one ranging from open reduction and osteosynthesis to hip arthroplasty.
Hip arthroscopy was first described in cadaveric studies conducted in the 1930s3). Its use was significantly increased, particularly in the setting of femoroacetabular impingement and osteoarthritis4,5). In trauma, use of hip arthroscopy was described in cases of bullet extraction, femoral head fixation, loose body removal, acetabular fracture fixation, labral injury, and debridement of a ligamentum teres avulsion6). Use of hip arthroscopy was described as safe, and largely successful (96%) and associated with limited risks, regardless of indication6).
We report a case of posterior wall acetabular fracture treated using a posterior mini-invasive approach with aid of hip arthroscopy.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
CASE REPORT
A 26-year-old male was a victim of high kinetic energy trauma (collision between motorcycle and car) which resulted in posterior dislocation of the femur and posterior fracture of the acetabulum (Fig. 1). In the initial evaluation, closed reduction of dislocation and placement of supracondylar skeletal traction was performed. He was hemodynamically stable, with no objective neurovascular deficits, and no other concomitant musculoskeletal injuries.
Fig. 1. Preoperative pelvic radiography: arrow pointing to the fracture line.

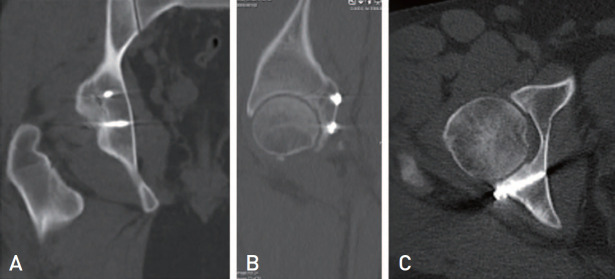
Computed tomography (CT) was performed, which confirmed a fracture of the posterior wall of the acetabulum with relevant displacement and the presence of intra-articular fragments, corresponding to an elementary fracture of the posterior wall according to Letournel’s anatomical classification (Fig. 2).
Fig. 2. Computed tomography characterization of the fracture showing intraarticular loose bodies (A, B) and a displaced posterior wall fracture (A, C). (A) Axial view. (B) Coronal view. (C) Sagittal view.
A skeletal traction of 7 kg was applied, and the patient underwent surgical treatment five days after admission.
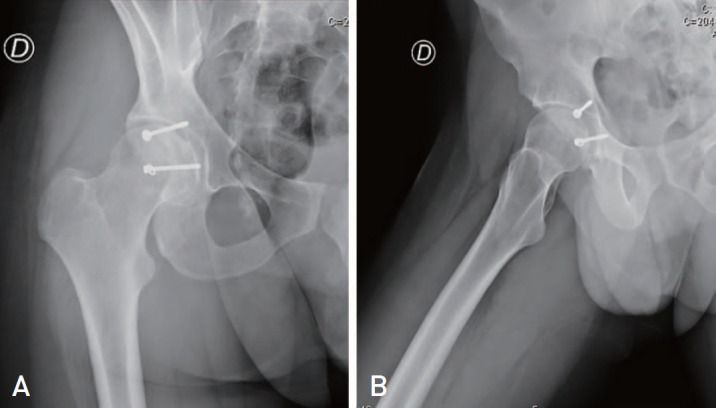
A mini-open and arthroscopy-assisted internal fixation was planned. The procedure was performed with the patient in lateral decubitus position. A posterior mini-invasive approach of the right hip of four inches was performed with preservation of the external rotators and identification of the capsule and the displaced bone fragment. Two hip arthroscopy portals (anterolateral and midanterior) were made for an initial dry arthroscopy with examination of the joint space using a 70° arthroscope. A posterior wall fracture and loose bodies at the cotyloid fossa were confirmed. Provisional reduction with Kirschner wires was performed. Adequate fracture reduction was arthroscopically confirmed. A small vertical capsulotomy was performed for removal of intra-articular and unstable fragments using a grasper followed by joint irrigation (Fig. 3). Definitive fixation was achieved using two 4 mm cannulated screws with a washer (Fig. 4).
Fig. 3. (A) Joint inspection with inspection of the fracture line. (B-D) Intra-articular fragments. (E, F) Fracture reduction and confirmation of absence of intra-articular hardware.
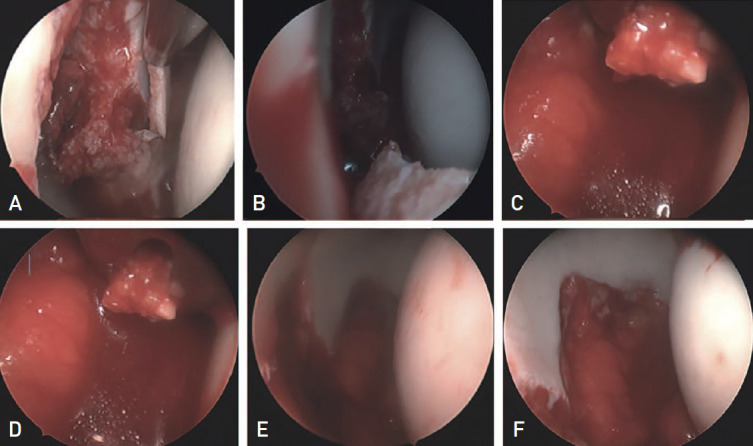
Fig. 4. (A, B) Radiography of the pelvis after surgery showing definitive fixation with two 4 mm cannulated screws with washer.
The patient was clinically stable for discharge four days after surgery.
Immediate follow-up was uneventful and partial weight bearing was recommended for the first six weeks after surgery, followed by a rehabilitation program with a progressive increase in load.
At six months, the patient presented with no pain and he had no functional limitations, with a value of 18/18 in the Modified Score of Merle d’Aubigné (Table 1)7). Excellent results were observed on radiographs, showing a joint with normal appearance. At this point, he was allowed to commence with sports.
Table 1. Modified Score of Merle d’Aubigné.
| Criteria | Score (Points) | |
|---|---|---|
| Prefixes | A) Patient with 1 hip involved* | |
| B) Patient with 2 hips involved | ||
| C) Patient with some factor contributing to failure to achieve normal gait | ||
| Gait | 6) Normal* | |
| 5) Limps, without crutches | ||
| 4) Walks long distance with cane | ||
| 3) Limited with cane, tolerates prolonged orthostatism | ||
| 2) Limited in time and distance with or without cane | ||
| 1) Few meters or bedridden; uses canes or crutches | ||
| Pain | 6) No pain* | |
| 5) Pain when starting deambulation, decreasing with activity | ||
| 4) Pain after activities, disappearing with rest | ||
| 3) Tolerable pain with limited activity | ||
| 2) Intense pain during ambulation | ||
| 1) Intense and spontaneous pain | ||
| Mobility (sum of range of motion) | 6) 211。-260。* | |
| 5) 161。-210。 | ||
| 4) 101。-160。 | ||
| 3) 61。-100。 | ||
| 2) 31。-60。 | ||
| 1) 0。-30。 | ||
| Total score | 18/18 | |
| Range of motion | ||
| Flexion | (10。)* (0。) | |
| Extension | (0。) (10。) (20。) (30。) (40。) (50。) (60。) (70。) (80。) (90。) (100。) (110。) (120。) (130。) (>130。)* | |
| Abduction | (>60。)* (60。) (50。) (40。) (30。) (20。) (10。) (0。) | |
| Adduction | (0。) (10。) (20。) (30。)* (40。) (>40。) | |
| External rotation | (>50。)* (50。) (40。) (30。) (20。) (10。) (0。) | |
| Internal rotation | (0。) (10。) (20。) (30。)* (40。) (50。) (>50。) | |
Revised from the article of Ugino et al. (Acta Ortop Bras. 2012;20:213-7)7) in accordance with the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license.
*The corresponding values two years after the surgical procedure.
He had fully recovered at two years after surgery with normal hip function and a CT-scan (Fig. 5) showing a nearly normal joint appearance, without degenerative changes.
Fig. 5. Computed tomography scan of the pelvis two years after surgery showing fracture consolidation, absence of intra-articular hardware and no articular step. (A) Coronal view. (B) Sagittal view. (C) Axial view.
DISCUSSION
The incidence of treating acetabular fractures with hip arthroscopy is low8). Patients who sustain acetabular fractures are often under the care of a traumatologist or an orthopaedist who is providing emergency department coverage. However, contrary to arthroscopy procedures around the knee or shoulder, not all of of these are capable of performing hip arthroscopy8).
Indications for hip arthroscopy after a hip fracture have not yet been clearly defined9). Relative indications for hip arthroscopy after a hip dislocation were reported by Foulk and Mullis10) as follows: as an alternative to an open arthrotomy for a non-concentric reduction; similarly to address a dislocation associated with a stable acetabular fracture not requiring open reduction and internal fixation; to evaluate for residual loose bodies or a labral tear when there is suspicion of these lesions.
Loose bodies are one component of a constellation of hip pathology that can accompany a hip dislocation; in some series loose bodies are diagnosed arthroscopically in 92% of dislocated hips8). Labral tears and cartilage injuries are also commonly seen in cases of high-energy trauma. The anatomy of the ligamentum teres also predisposes it to injury with a hip dislocation8).
Plain radiographs and CT scans appear to underestimate the true incidence of intra-articular pathological findings, therefore the arthroscope is a powerful tool in identifying these injuries11). A prospective cohort study conducted in 2014 by Khanna et al.11) evaluated 29 post-traumatic hips with hip arthroscopy and identified 17 of 29 hips (59%) as having loose bodies, 11 of 29 (38%) hips as having an intra-articular step deformity, 14 of 29 (49%) hips as having an osteochondral lesion, and 27 of 29 (93%) hips as having a labral tear.
Arthroscopic tecniques such as labral and ligamentum teres debridement or reconstruction, removal of microfractures and lose bodies can be usefull treatment options8).
Traditional surgical treatment requires extensive exposure, which may be complicated by infection, blood loss, wound healing problems, abductor weakness, sciatic nerve palsy, and heterotopic ossification12). Periacetabular screws are commonly used and technically demanding, so that joint perforations are described in 0.9% to 7% of cases and can be a severe complication that causes rapid joint wear resulting in hip arthritis12,13). Although the use of hip arthroscopy provides advantages in treatment of acetabular fractures, a 1.5% incidence of complication has been reported14). During hip arthroscopy, irrigation fluid is injected into the hip joint to expand it. A recent study using postoperative ultrasound examination reported that 16% of patients had intraabdominal fluid extravasation after hip arthroscopy; still the incidence of symptomatic intraperitoneal accumulation of fluid is only 0.16%14). It has been reported that in trauma cases peritoneal damage results in communications between the retroperitoneum and the peritoneal cavity, causing the entry of irrigation fluid into the peritoneal cavity14). This can cause an abdominal compartment syndrome, a condition characterized by a sustained increase of abdominal pressure (20 mmHg or higher), leading to new organ dysfunction14). High perfusion pressure is a risk factor for development of this complication15).
Increased surgical time and blood loss could be a potential disadvantage of simultaneous use of hip arthroscopy. A study comparing treatment of acetabular fractures with or without hip arthroscopy reported a mean increase in surgical time of 38.8 minutes and 21.2 mL in intra-operative blood loss. However this difference was not statistically significant9).
In this case a posterior mini-invasive approach was performed followed by hip arthroscopy, which allowed joint wash, removal of loose bodies (usually present in this type of fracture) and confirmation of reduction and absence of intra-articular hardware.
Four studies (three case reports and one series of cases) also demonstrated the value of hip arthroscopy in traumatology, to assist fracture reduction, in six patients. Complete recovery was achieved in five of these cases at the end of the follow-up (mean, 1.75 years), with no occurrence of intra or postoperative complications (intra-articular hardware penetration, nerve damage, avascular necrosis, heterotopic ossification)6).
Park et al.12) described two cases of fractures of the posterior wall of the acetabulum in young patients, one with an isolated fracture and the other with a concomitant femur fracture. In both cases an anatomical reduction of the fracture was performed via arthroscopy and fixation with two cannulated screws; excellent results were obtained in both cases three months after surgery. A case report involving fixation with only one 4.5 mm cannulated screw through the posterolateral portal was also reported with good outcomes16).
The clinical and radiological results achieved in this case are in concordance and add to those that are published, supporting the potential and usefulness of hip arthroscopy in selected acetabular fractures.
In conclusion, hip arthroscopy is a technique that is used increasingly in orthopedics, with increasing applicability in traumatology. No robust studies to prove its added value have been reported, however the published studies have been consistent in the excellent results obtained with its use. This case demonstrates the value of arthroscopy in treatment of fractures of the posterior wall of the acetabulum, namely in confirming fracture reduction, absence of intra-articular hardware or fragments, as well as a less invasive approach. Its increasing use should be accompanied by conduct of prospective studies in order to prove its effectiveness and define the indications for its use.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Court-Brown CM, Tornetta P, McQueen MM, Ricci WM. Rockwood and Green’s fractures in adults. 9th ed. Philadelphia: Wolters Kluwer Health; 2020. pp. 789–834. [Google Scholar]
- 2.Moed BR, WillsonCarr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84:752–758. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Larson CM, Swaringen J, Morrison G. A review of hip arthroscopy and its role in the management of adult hip pain. Iowa Orthop J. 2005;25:172–179. [PMC free article] [PubMed] [Google Scholar]
- 4.Bozic KJ, Chan V, Valone FH, 3rd, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8 Suppl):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 5.Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:e23. doi: 10.2106/JBJS.J.01886. [DOI] [PubMed] [Google Scholar]
- 6.Niroopan G, de Sa D, MacDonald A, Burrow S, Larson CM, Ayeni OR. Hip arthroscopy in trauma: a systematic review of indications, efficacy, and complications. Arthroscopy. 2016;32:692–703.e1. doi: 10.1016/j.arthro.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 7.Ugino FK, Righetti CM, Alves DP, Guimaraes RP, Honda EK, Ono NK. Evaluation of the reliability of the modified Merle d’Aubigne and Postel Method. Acta Ortop Bras. 2012;20:213–217. doi: 10.1590/S1413-78522012000400004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newman JT, Saroki AJ, Philippon MJ. Hip arthroscopy for the management of trauma: a literature review. J Hip Preserv Surg. 2015;2:242–248. doi: 10.1093/jhps/hnv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim HJ, Kim SS, Jung YH, Lee KH. Effectiveness of hip arthroscopy performed simultaneously before open reduction and internal fixation for acetabular fracture and fracture-dislocation of the hip. Hip Pelvis. 2018;30:92–100. doi: 10.5371/hp.2018.30.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foulk DM, Mullis BH. Hip dislocation: evaluation and management. J Am Acad Orthop Surg. 2010;18:199–209. doi: 10.5435/00124635-201004000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Khanna V, Harris A, Farrokhyar F, Choudur HN, Wong IH. Hip arthroscopy: prevalence of intra-articular pathologic findings after traumatic injury of the hip. Arthroscopy. 2014;30:299–304. doi: 10.1016/j.arthro.2013.11.027. [DOI] [PubMed] [Google Scholar]
- 12.Park JY, Chung WC, Kim CK, Huh SH, Kim SJ, Jung BH. Arthroscopic reduction and transportal screw fixation of acetabular posterior wall fracture: technical note. Hip Pelvis. 2016;28:120–126. doi: 10.5371/hp.2016.28.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jang JH, Moon NH, Park KY. Arthroscopic management of intraarticular screw perforation after surgical treatment of an acetabular posterior wall fracture: a case report. Hip Pelvis. 2018;30:60–64. doi: 10.5371/hp.2018.30.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shakuo T, Bito K, Yasuda S, Asagi C. Abdominal compartment syndrome during hip arthroscopy for an acetabular fracture: a case report. JA Clin Rep. 2017;3:24. doi: 10.1186/s40981-017-0100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kocher MS, Frank JS, Nasreddine AY, Safran MR, Philippon MJ, Sekiya JK, et al. Intra-abdominal fluid extravasation during hip arthroscopy: a survey of the MAHORN group. Arthroscopy. 2012;28:1654–1660.e2. doi: 10.1016/j.arthro.2012.04.151. [DOI] [PubMed] [Google Scholar]
- 16.GürpInar T, Polat B, Kanay E, Polat A, Öztürkmen Y. Arthroscopic fixation of a posterior acetabular wall fracture: a case report. Cureus. 2019;11:e6264. doi: 10.7759/cureus.6264. [DOI] [PMC free article] [PubMed] [Google Scholar]