Abstract
Background
Inhaled corticosteroids (ICS) are an integral part of asthma management, and act as an anti‐inflammatory agent in the airways of the lung. These agents confer both significant benefit in terms of symptom management and improvement in lung function, but may also cause harm in terms of local and systemic side‐effects. Ciclesonide is a novel steroid that is metabolised to its active component in the lung, making it a potentially useful for reducing local side effects.
Objectives
To assess the efficacy and adverse effects of ciclesonide relative to those of other inhaled corticosteroids in the management of chronic asthma.
Search methods
We searched the Cochrane Airways Group register of trials with pre‐defined terms. Additional searches of PubMed and Clinicalstudyresults.org were undertaken. The literature searches for this review are current up to June 2007.
Selection criteria
Randomised parallel or crossover studies were eligible for the review. We included studies comparing ciclesonide with other steroids both at nominally equivalent dose or lower doses of ciclesonide.
Data collection and analysis
Two review authors independently assessed trial quality and extracted data. Study authors were contacted for additional information. Adverse effects information was collected from the trials.
Main results
Twenty one trials involving 7243 participants were included. Equal daily doses of ciclesonide and beclomethasone (BDP) or budesonide (BUD) gave similar results for peak expiratory flow rates (PEF), although forced vital capacity (FVC) was higher with ciclesonide. Data on forced expired volume in one second (FEV1) were inconsistent. Withdrawal data and symptoms were similar between treatments. Compared with the same dose of fluticasone (FP), data on lung function parameters (FEV1, FVC and PEF) did not differ significantly. Paediatric quality of life score favoured ciclesonide. Candidiasis was less frequent with ciclesonide, although other side‐effect outcomes did not give significant differences in favour of either treatment. When lower doses of ciclesonide were compared to BDP or BUD, the difference in FEV1 did not reach significance but we cannot exclude a significant effect in favour of BDP/BUD. Other lung function outcomes did not give significant differences between treatments. Paediatric quality of life scores did not differ between treatments. Adverse events occurred with similar frequency between ciclesonide and BDP/BUD. Comparison with FP at half the nominal dose was undertaken in three studies, which indicated that FEV1 was not significantly different, but was not equivalent between the treatments (per protocol: ‐0.05 L 95% confidence intervals ‐0.11 to 0.01).
Authors' conclusions
The results of this review give some support to ciclesonide as an equivalent therapy to other ICS at similar nominal doses. The studies assessed low doses of steroids, in patients whose asthma required treatment with low doses of steroids. At half the dose of FP and BDP/BUD, the effects of ciclesonide were more inconsistent The effect on candidiasis may be of importance to people who find this to be problematic. The role of ciclesonide in the management of asthma requires further study, especially in paediatric patients. Further assessment against FP at a dose ratio of 1:2 is a priority.
Keywords: Adult; Child; Humans; Administration, Inhalation; Androstadienes; Androstadienes/therapeutic use; Anti-Asthmatic Agents; Anti-Asthmatic Agents/therapeutic use; Asthma; Asthma/drug therapy; Beclomethasone; Beclomethasone/therapeutic use; Budesonide; Budesonide/therapeutic use; Chronic Disease; Fluticasone; Pregnenediones; Pregnenediones/therapeutic use; Randomized Controlled Trials as Topic
Plain language summary
Ciclesonide versus other inhaled steroids for chronic asthma in children and adults
Inhaled corticosteroids, such as budesonide, beclomethasone or fluticasone, which have been available for many years, have proven to be an important therapy for controlling the inflammation caused by asthma. They are given usually twice daily, and are recommended therapy in international guidelines for most asthmatics. However, the currently available inhaled corticosteroids can be associated with significant side‐effects, including local effects in the upper airways such as hoarseness and oral candida (thrush infection). Ciclesonide is a new steroid which is reported to make less of the active steroid available until the drug reaches the lung on inhalation, which could reduce the likelihood of throat symptoms. This findings of this review of 21 trials (7243 participants) do not allow certainty about the relative efficacy of ciclesonide compared to older inhaled corticosteroids, especially at higher doses. The results of the review to date do not indicate whether ciclesonide provides a significantly more useful safety profile that other inhaled corticosteroids at similar equivalent doses. However, the finding of lower oral candidiasis in patients treated with ciclesonide compared to fluticasone may be important for those patients who experience oral thrush with their current ICS. In addition, further studies in children are required to obtain data on the side‐effect profile of ciclesonide in this population.
Background
On a worldwide basis asthma is a common chronic disease in clinical practice affecting over 300 million people. It is responsible for one in 250 deaths per year and 15 million disability adjusted life years (DALYs) lost worldwide (GBA 2004). It is a condition which develops in early childhood and generally persists into adulthood (Gerritsen 1989; Martin 1982; Williams 1969). Asthma is a chronic inflammatory disease of the airways involving a complex interaction between airway structural cells and specific allergic inflammatory cells including mast cells, eosinophils and T‐lymphocytes, and the release of specific cytokines and mediators of inflammation. This inflammatory response is associated with airway narrowing, especially in smaller airways, which cause patients to complain of symptoms such as cough and wheeze (GINA 1998; Tattersfield 2002). The anti‐inflammatory corticosteroids have been an effective therapy for asthma for over 30 years and are now the main therapy for asthma control currently for those with persistent asthma (Adams 2005; BGAM 1997; BTS/SIGN 2003; Consensus 1999; Consensus 2005; GINA 1998; Powell 2003).
Corticosteroids deal effectively with the asthma inflammatory process through interaction with the glucocorticoid receptor, thus leading to the amelioration in asthma symptoms and control of the disease (Adams 2005; Adams 2005a; Adams 2007). The main advantage of the inhaled route is to bring the therapy directly to the disease location and at a reduced dose and hence less systemic side‐effects compared to higher dose oral steroid therapy (Mash 2001). There are different types of inhaled corticosteroids available on the market given either by multi‐dose dry powder or aerosol inhaler devices (e.g. beclomethasone, fluticasone, budesonide, and mometasone). Inhaled corticosteroids significantly reduce the hospitalisation rate for asthma (and hence reduce cost associated with the disease) and the mortality from the condition (Suissa 2000; Suissa 2002) when taken on a regular basis. Non‐compliance is a significant problem with inhaled corticosteroid therapy due to a number of factors including increased dosing frequency and may occur due to recurrent local and also systemic side effects (Buston 2000). This has led to the development of more potent formulations with the aim of reducing daily steroid load without compromising disease control (Lasserson 2006). However, while inhaled steroids may be more effective when used four times per day, reducing dosing to twice daily or even once daily dosing can give effective control (Malo 1989; Toogood 1982). However, compliance with increased dosing frequency of inhaled steroids in asthmatics especially four times daily can be poor (Coutts 1992; Eisen 1990). The novel inhaled corticosteroid ciclesonide has recently been approved in Europe. This therapy has novel release and distribution properties, reported to result in better targeting of the anti‐inflammatory effects in the airways especially to the small airways. It is inhaled as a pro‐drug, which is converted to an active metabolite (des CIC) in the airways reportedly with reduced systemic and local (e.g. oropharyngeal) side effects. In addition, ciclesonide is given as a once daily therapy, and may lead to better compliance with inhaled corticosteroids.
This review considers the evidence comparing ciclesonide with other inhaled steroid therapies at nominal 1:1 and 1:2 dose ratios.
Objectives
To assess the efficacy and adverse effects of ciclesonide relative to those of other inhaled corticosteroids in the management of chronic asthma. The review assesses ciclesonide against fluticasone, beclomethasone or budesonide at equivalent dose and lower doses of ciclesonide.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCT) comparing the inhaled corticosteroid ciclesonide with another inhaled corticosteroid were considered for inclusion. Trials that use parallel group designs or cross‐over design with a wash out period of two weeks or more were eligible. Studies published in abstract form will be included. Unpublished data, if available, will be considered.
Types of participants
Adults (aged 18 years and older) and children (less than 18 years) will be eligible for inclusion. All study participants must have a diagnosis of chronic asthma, including those with intermittent and chronic symptoms. Studies that base the diagnosis of asthma on physician opinion or on objective criteria related to symptoms, airway reversibility to an inhaled short‐acting 2‐agonist or airway hyper‐responsiveness in keeping with international asthma guidelines such as GINA 1998 (Global Initiative for Asthma)/National Institutes of Health (NIH) or BTS/SIGN 2003) or evidenced based guidelines will be included. Studies that deliver interventions to patients in the community/family practice setting or hospital‐based settings will be included. Studies with participants with pulmonary diagnosis other than asthma (for example, chronic obstructive pulmonary disease (COPD)) will be excluded.
Types of interventions
This review includes studies that have compared ciclesonide with other inhaled corticosteroids. Two comparator steroids are assessed in this review, each at dose ratios of 1:1 and 1:2: ciclesonide (CIC) versus BDP/budesonide (BDP/BUD) 1:1; CIC versus BDP/BUD 1:2 ; CIC versus fluticasone propionate (FP): 1:1; CIC versus FP 1:2. Study duration was set at a minimum of four weeks. Concomitant therapies for asthma, such as short‐acting 2‐agonists (rescue therapy), theophyllines, long‐acting 2‐agonists (Serevent or formoterol), inhaled anti‐cholinergics were permitted provided that the dose and type of drug remained stable, and was not introduced at the start of the trial as part of the study protocol. Studies involving anti‐leukotrienes (e.g. Singular, Accolate), combination inhalers (fluticasone‐salmeterol and budesonide‐formoterol) or other airway anti‐inflammatory asthma therapy (e.g. cromones) were excluded. Studies were included if they were conducted in an outpatient setting.
Types of outcome measures
Primary outcomes
Asthma exacerbations requiring use of systemic steroids.
Measures of lung function, forced expired volume in one second (FEV1) and or peak expiratory flow rates (PEF)
Secondary outcomes
Measures of healthcare utilisation: doctor visits, emergency visits and or hospital admissions for asthma.
Measures of morbidity: days of school absences, days of restricted activities, nights disturbed by asthma symptoms, health‐related quality of life, asthma severity, asthma‐free days,
Measures of compliance. As a surrogate to include study withdrawal or patient preference in crossover studies.
Asthma symptoms
Rescue beta‐2 agonists use
Measures of adverse effects including oropharyngeal (candidiasis, sore throat, hoarseness), and systemic (osteopenia, adrenal suppression, growth rate) side‐effects and withdrawal rate due to side‐effects will be included.
Search methods for identification of studies
Electronic searches
Trials were identified using the Cochrane Airways Group (CAG) Specialised Register of trials, which is derived from systematic searches of bibliographic databases including the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and CINAHL, and handsearching of respiratory journals and meeting abstracts. All records in the Specialised Register coded as 'asthma' were searched using the following terms:
ciclesonide* or Alveso* or pregnenedione* or CIC
We searched the CAG trials register up to June 2007. Additional searches on PubMed were undertaken with the term 'ciclesonide' for articles published more recently than the last register search (October 2007).
Searching other resources
Reference lists of all primary studies and review articles were reviewed for additional references. Authors of identified trials were contacted and asked to identify other published and unpublished studies. Pharmaceutical manufacturers (Altana) was also contacted for information on any unpublished trials. We undertook additional searches of www.clinicalstudyresults.org for trial reports of ciclesonide (November 2007).
Data collection and analysis
Selection of studies
Two authors (PM and TL) screened the title and abstract of each citation identified for eligibility. Articles that appeared to fulfil the inclusion criteria were retrieved in full text. PM and TL then independently established, from the full text of the articles, whether each study met the inclusion criteria of the review. Translation into English was not necessary. Disagreement was settled by consensus.
Data extraction and management
We independently extracted data from included trials and TL entered this into RevMan 4.2. We attempted to contact study authors to identify additional papers, confirm data for accuracy and completeness.
We extracted the following characteristics of each study. Methods Design, randomisation method, blinding, follow‐up procedures and withdrawals. Population Sample size, age, gender, inclusion and exclusion criteria (including asthma therapy), asthma diagnosis and severity, pulmonary function, other medical diagnoses and therapies. Intervention Type and dose of comparator inhaled steroid, dose of ciclesonide, timing and duration of therapy, method of delivery, co‐intervention medications. Outcomes Reported outcomes
We extracted numerical outcome data independently.
Assessment of risk of bias in included studies
Study quality was assessed using the Jadad scale and the Cochrane approach to assessment of allocation concealment. All trials were scored and entered using the following principals.
Grade A: adequate concealment Grade B: uncertain Grade C: clearly inadequate concealment
Measures of treatment effect
A mean difference (MD) and 95% continuous interval (CI) was calculated for continuous variables measured on identical metrics. SMD (standardised mean difference) was used for the same continuous variables measured with different metrics. Generic inverse variance was used to pool data derived from the same scale if they were only available as mean differences with 95% CIs or standard errors.
For dichotomous outcomes, we calculated a Risk Ratio (RR) based upon the number of participants with an event versus the number of participants without an event.
Assessment of heterogeneity
We assessed statistical heterogeneity using the I square measurement, with a cut‐off of 20% prompting additional analysis.
Data synthesis
Trial data was combined using RevMan 4.2. Data and pooled using a fixed‐effect model. If heterogeneity was observed I2 ≥ 20% (Higgins 2003), a sensitivity analysis using a random‐effects model was applied, to determine whether variation between the studies affected the pooled estimate.
The treatments compared were considered to be equivalent according to whether the 95% CI of the pooled estimates excluded a clinically meaningful benefit. We considered a difference of ≥100 ml in FEV1, ≥ 25 L/min for PEF and RR outside of 0.9 to 1.1 for exacerbations to be clinically meaningful differences. We assessed the pooled estimates for FEV1, am and pm PEF as intention to treat and per protocol populations, if these were available.
Subgroup analysis and investigation of heterogeneity
We subgrouped studies according to the age of the participants (adults versus children).
Results
Description of studies
Results of the search
Literature searches identified a total of 146 citations, and following the exclusion of irrelevant studies and identification of multiple citations, 21 studies (contributing 22 treatment‐control comparisons) derived from 57 citations met the review entry criteria (seeFigure 1). For full descriptions of each study see Characteristics of included studies.
1.
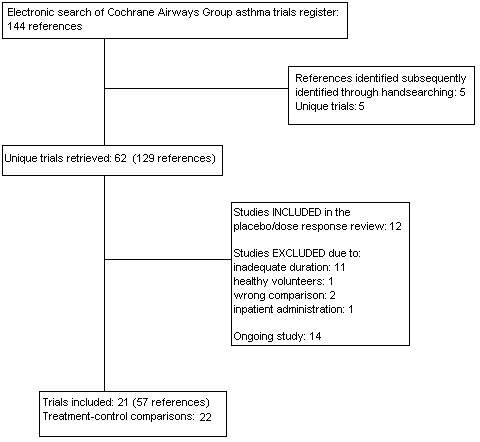
Flow diagram of studies in the review.
Included studies
Study design
All studies were described as randomised.
Participants
A total of 1664 children were recruited to studies with age limits up to 17 years (Pedersen 2006; Vermeulen 2007; von Berg 2007), and 5367 participants were adolescent/adult populations.
Baseline FEV1 predicted varied between the studies, as did the requirement for pre‐treatment with maintenance inhaled steroids. If reported, mean FEV1 predicted suggested that the study populations had moderate airway obstruction, with three reporting FEV1 below 80% in Adachi 2007; Buhl 2006; Hansel 2006; Ukena 2006, and a number with baseline predicted FEV1 at or above 80% in Bateman 2007; Boulet 2006; Boulet 2007; Lipworth 2005; Niphadkar 2005a; Niphadkar 2005b; Pedersen 2006 In the remaining studies baseline means were not presented. In Bernstein 2004 and Vermeulen 2007, entry criteria stipulated predicted FEV1 below 80%. Pre‐treatment with an inhaled steroid was an entry criterion in Boulet 2006; Buhl 2006 and Zietkowski 2006, was cited as an exclusion criterion in Lipworth 2005. In the remaining studies participants whose maintenance dose of inhaled steroids was in excess of a specified level were excluded.
Run‐in periods were performed in the majority of the trials, with Buhl 2006; Hansel 2006; Magnussen 2007; Pedersen 2006; Ukena 2006; von Berg 2007 and Zietkowski 2006 performing run‐in periods where participants could use only as needed rescue medication. In the remaining studies if run‐in periods were reported, participants continued their usual dose of inhaled steroids, or were given a stable dose of a specific steroid.
Intervention
We assessed four comparisons represented by the following studies. 1. Ciclesonide versus BDP or BUD (nominal BDP equivalent dose ratio 1:1): Three studies (Adachi 2007; Boulet 2006; Hansel 2006; Ukena 2006). 2. Ciclesonide versus BDP or BUD (nominal BDP equivalent dose ratio 1:2): Five studies (Adachi 2007; Hansel 2006; Niphadkar 2005a; Niphadkar 2005b; Vermeulen 2007; von Berg 2007). 3. Ciclesonide versus FP (nominal FP dose ratio: 1:1): Eight studies (Bateman 2007; Bernstein 2004; ;Boulet 2006; Buhl 2006; Boulet 2007; Lipworth 2005; Magnussen 2007; Pedersen 2006; Zietkowski 2006). 4. Ciclesonide versus FP (nominal FP dose ratio: 1:2): Four studies (Bernstein 2004; Lipworth 2005; Magnussen 2007; Zietkowski 2006).
Delivery of drug, dosage & duration of studies
Ciclesonide was delivered via metered dose inhalers in all the trials. Open label assessment with budesonide was undertaken in two studies (Adachi 2007; Hansel 2006), and with fluticasone in one other study (Bateman 2007). The remaining comparisons were double‐blind.
Dosing regimens varied, with ciclesonide given once daily in all studies with the exception of Bernstein 2004 and Pedersen 2006 if it was administered twice daily. Conversely the comparator inhaled steroid was administered twice daily in all studies with the exception of Boulet 2006; Ukena 2006; Vermeulen 2007 and von Berg 2007, where it was administered once daily.
One study was 12 months in duration (Adler 2006) and another was six months (Bateman 2007). The remaining studies were 12 weeks long.
Outcomes assessed
Adler 2006; Lipworth 2005 were the only two studies where lung function outcome data were not reported. Symptoms or rescue medication use were assessed in all studies except for Lipworth 2005 and Vermeulen 2007.
Excluded studies
The reasons for the exclusion of studies are listed in Characteristics of excluded studies. Fourteen studies were excluded, the most common reason for exclusion was inadequate follow‐up period. A further fourteen studies were identified as ongoing. We report data from 15 parallel group trials, since these were the primary source of evidence for the review.
Risk of bias in included studies
All trials except three were described as randomised and double‐blind. However, the method of blinding was available in only four studies. Methodological quality, as assessed by the Jadad scoring system, was variable. Five of the studies achieved a score of 5 (high quality), three studies a score of 4 (good quality), three a score of 3 (fair quality) and the remaining three studies a score of 2 or 1(poor quality). The studies with low (i.e. 2 or 1) Jadad scores were published in abstract form for presentation at conferences and we had only limited details about patient withdrawals from study, methods of randomisation and blinding. It is therefore possible that these scores may change upon availability of more information. Allocation concealment scores were graded A for six studies and B for the remainder.
Effects of interventions
A number of the studies identified did not provide sufficient information to contribute data to the findings of this review (Adler 2006, N = 111; Bernstein 2004, N = 531). We describe the pooled findings from 20 study comparisons recruiting 7243 participants. The data available represent 91% of participants randomised to the studies. We report data with the direction of effect indicating a difference in favour of ciclesonide.
1. Ciclesonide versus BDP or BUD (1:1 dose ratio)
Primary outcomes
Exacerbations requiring oral steroids
No studies reported data for this outcome.
Change from baseline in spirometry & clinic measured peak flow
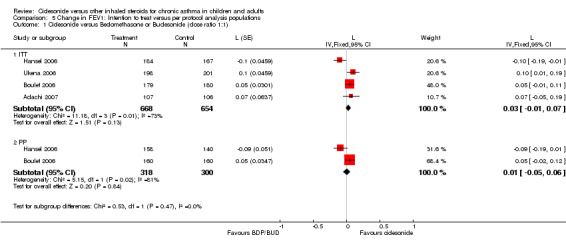
FEV1: 0.03 L; 95% confidence interval ‐0.06 to 0.11 (four studies, N = 1322) FVC: 0.06 L; 95% confidence interval 0.01 to 0.11(three studies, N = 970)
Given the different directions, and the statistical significance of two studies favouring BDP/BUD over ciclesonide, the disagreement between the study findings for change in FEV1 warrants some comment. Of the three studies Boulet 2006 administered a high dose treatment period prior to randomisation of 1280 μg/d of budesonide. This pretreatment of study participants may have led to a 'jump' in FEV1, making the comparison of ciclesonide to budesonide closer to a steroid withdrawal study. Therefore, rather than leading to an improvement in FEV1, Boulet 2006 showed that ciclesonide led to a smaller decline in FEV1 than budesonide. The high degree of statistical heterogeneity meant that our test for equivalence was not reliable.
Change in diary card peak flow
am PEF: 5.37 L/min; 95% confidence interval 0.12 to 10.61(four studies, N = 1329) pm PEF: 3.95 L/min; 95% confidence interval ‐2.89 to 10.80 (two studies, N = 758)
These results exclude a clinically meaningful difference between these treatments and are suggestive of equivalence at CIC and BDP/BUD at 1:1 for this outcome..
Secondary outcomes
Symptoms, rescue medication use & non‐specific exacerbations of asthma
Ukena 2006 and Hansel 2006 were the only studies reporting data for symptom scores, neither of which reported a statistically significant difference between treatments. Rescue medication use was reported as medians in Hansel 2006 with no statistically significant difference between treatments. Boulet 2006 reported no statistically significant difference in exacerbations of asthma between treatments.
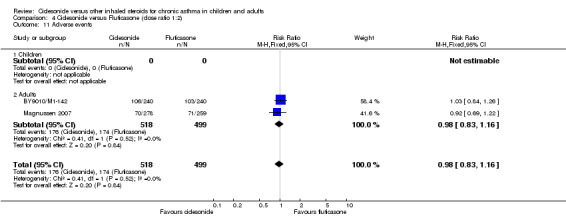
Study withdrawal & adverse event data
Pooled effects did not indicate a significant difference in the frequency of withdrawals when considered as total number (relative risk 0.75; 95% confidence interval 0.47 to 1.19) or as withdrawal due to lack of efficacy (relative risk 1.33; 95% confidence interval 0.88 to 2.01). There was no statistically significant difference in the risk of any adverse event (relative risk 0.99; 95% confidence interval 0.85 to 1.15).
2. Ciclesonide versus BDP or BUD (1:2 ratio)
Primary outcomes
Exacerbations requiring oral steroids
No studies reported data for this outcome.
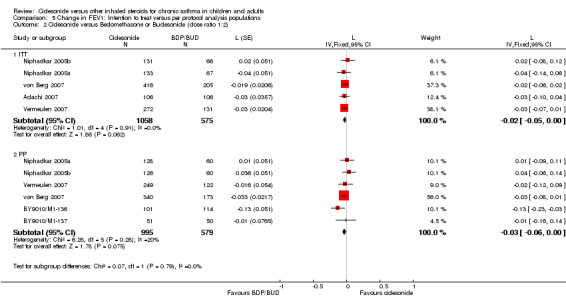
Change from baseline in spirometry & clinic measured peak flow
Intention to treat FEV1: ‐0.02 L; 95% confidence interval ‐0.05 to 0 (five studies, N = 1633); Per protocol FEV1: ‐0.03 L; 95% CI ‐0.06 to 0 (six studies, N = 1574) FVC: ‐0.01 L; 95% confidence interval ‐0.04 to 0.03 (five studies, N = 1633)
Both the ITT and PP population estimates indicate that BDP/BUD is statistically superior to ciclesonide at twice the dose, although the lower limit of the 95% confidence interval is within the threshold value of 0.1 L of FEV1.
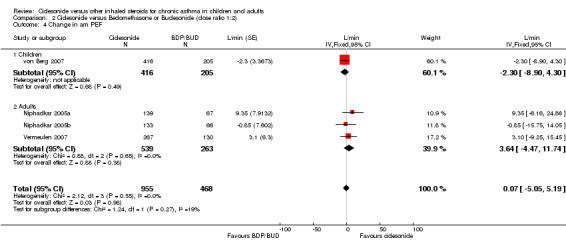
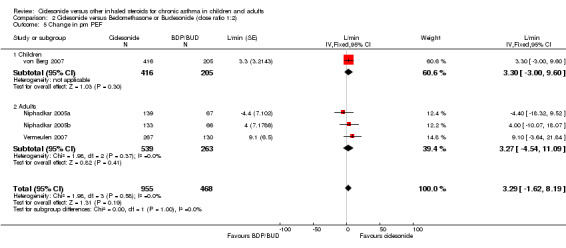
Change in diary card peak flow
am PEF: 0.07 L/min; 95% confidence interval ‐5.05 to 5.19 (four studies, N = 1423) pm PEF: 3.29 L/min; 95% confidence interval ‐1.62 to 8.19 (four studies, N = 1423)
The ITT and PP population estimates for am PEF were similar, and the difference between ciclesonide and BDP/BUD was within the predefined limit of equivalence of 25 L/min.
Secondary outcomes
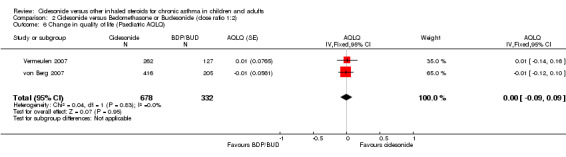
Quality of life, symptoms, rescue medication use & non‐specific exacerbations of asthma
There was no significant difference between treatments in Paediatric AQLQ data (0; 95% confidence interval ‐0.09 to 0.09, two studies). Symptom score and rescue medication use data were only available as medians across the studies, and where available no statistically significant difference was reported.
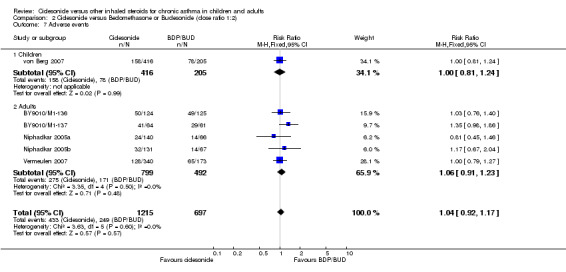
Study withdrawal & adverse event data
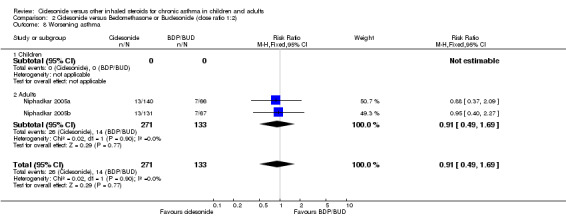
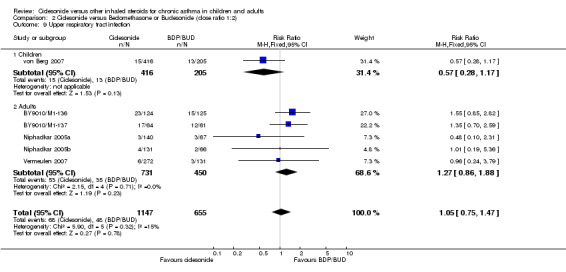
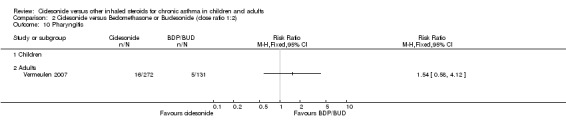
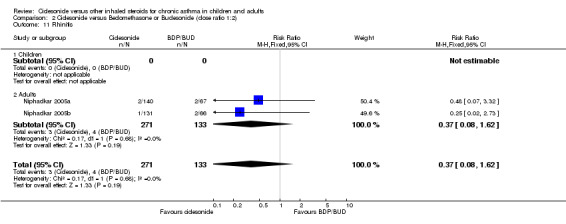
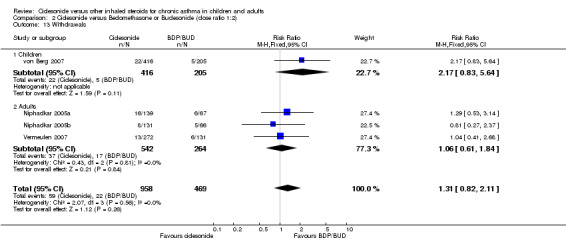
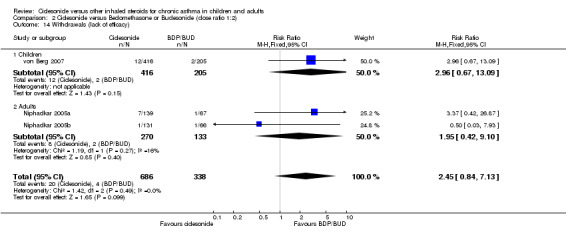
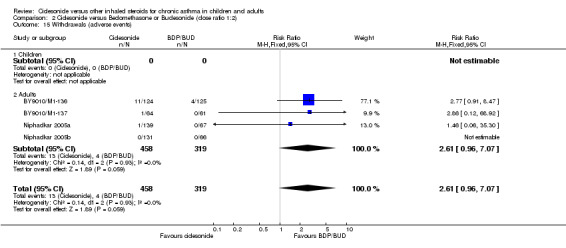
There was no significant difference in the frequency of withdrawals (RR 1.31; 95% confidence interval 0.82 to 2.11) or as withdrawal due to lack of efficacy (RR 2.45; 95% confidence interval 0.84 to 7.13). There was no difference in the risk of any adverse event occurring (RR 1.04; 95% confidence interval 0.92 to 1.17), or specific events such as rhinitis (RR 0.37; 95% confidence interval 0.08 to 1.62, two studies), or upper respiratory tract infection (RR 1.05; 95% confidence interval 0.75 to 1.47).
3. Ciclesonide versus FP (1:1 dose ratio)
Primary outcomes
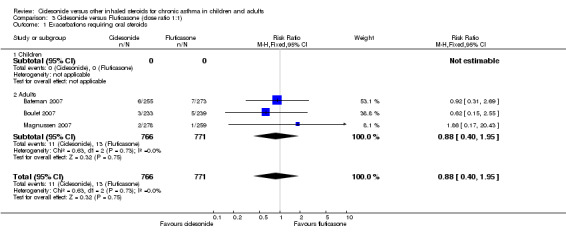
Exacerbations requiring oral steroids
There was no difference in the risk of an exacerbation requiring oral steroids between FP and CIC (0.88; 95% confidence interval 0.4 to 1.95, three studies, N = 1537).
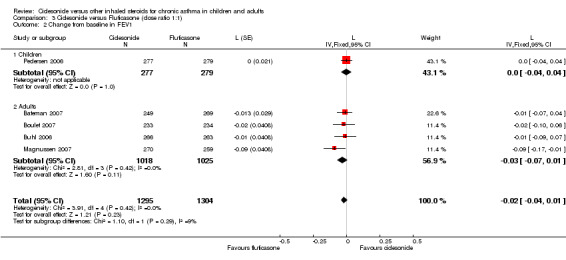
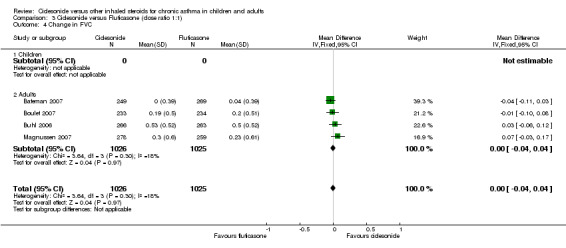
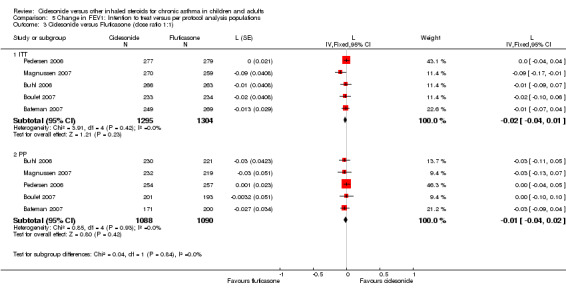
Change from baseline in spirometry & clinic measured peak flow
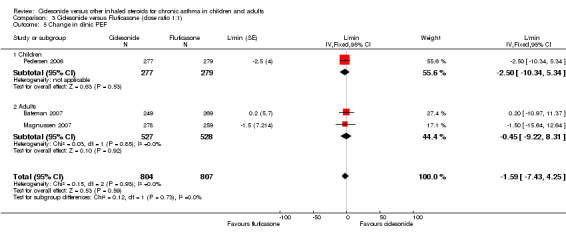
FEV1: ‐0.02 L; 95% confidence interval ‐0.04 to 0.01(five studies, N = 2607) FVC: 0; 95% confidence interval ‐0.04 to 0.04 (four studies, N = 2051) PEF: L/min ‐1.59; 95% confidence interval ‐7.43 to 4.25 (three studies, N = 1611)
The ITT and PP population estimates for FEV1 were similar and were within predefined limits of equivalence.
Change in diary card peak flow
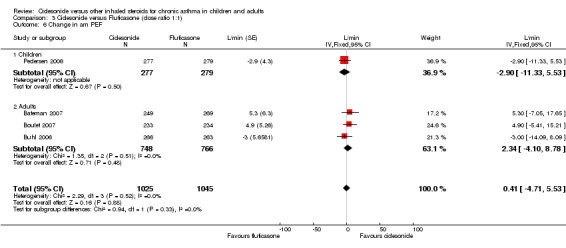
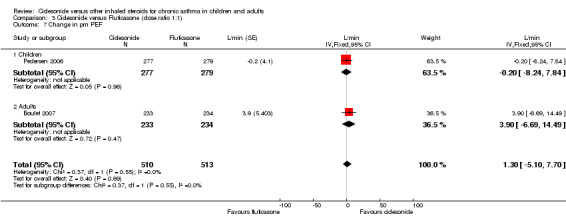
am PEF: 0.41 L/min; 95% confidence interval ‐4.71 to 5.53 (four studies, N = 2070) pm PEF 1.3 L/min; 95% confidence interval ‐5.1 to 7.7 (two studies, N = 1043).
The ITT and PP population estimates for am PEF were similar and were within predefined limits of equivalence.
Secondary outcomes
Quality of life, symptoms, rescue medication use & non‐specific exacerbations of asthma
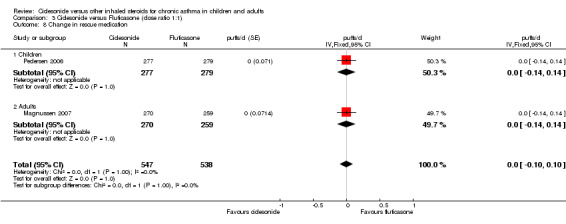
Ciclesonide led to a significantly greater improvement in AQLQ scores compared with FP (0.17 units; 95% confidence interval 0.04 to 0.30, two studies). No significant differences between treatments was reported for asthma worsening when considered as total number (relative risk 1.1; 95% confidence interval 0.61 to 1.97). In Buhl 2006, both CIC and FP produced similar significant decreases in median asthma symptom scores after 12 weeks therapy. In addition, the analysis of asthma symptom scores and use of rescue medication revealed that the onset of treatment effects occurred within 24 hours for both treatments. This was associated with reduced rescue medication use for CIC and FP from baseline. In children (Pedersen 2006) both CIC and FP improved total asthma symptoms scores, nocturnal awakening days and rescue free days to a similar degree at 12 weeks. This result was seen in older and younger children alike independent of disease severity. In Zietkowski 2006, there was a reported reduction in asthma symptoms (day and night), and rescue use which was similar for CIC and FP. In Lipworth 2005, one patient each in the CIC (combined CIC 320 and CIC 640) and FP groups had a worsening of asthma. Rescue use and asthma symptoms were not reported in this study.
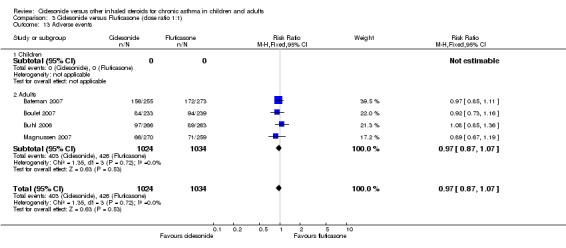
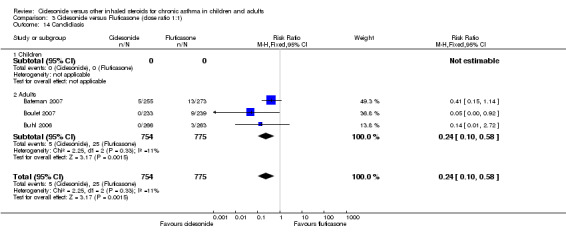
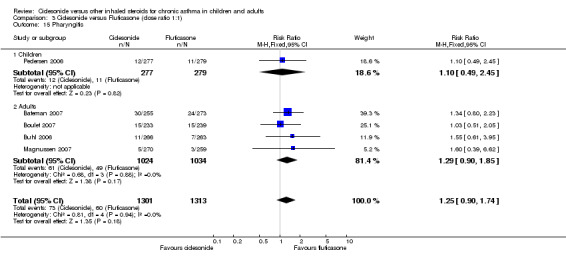
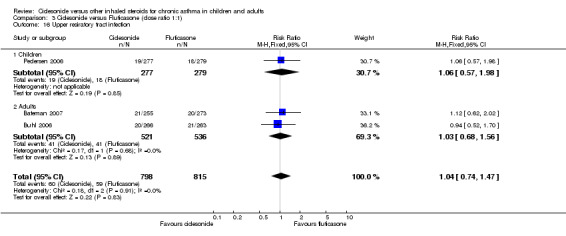
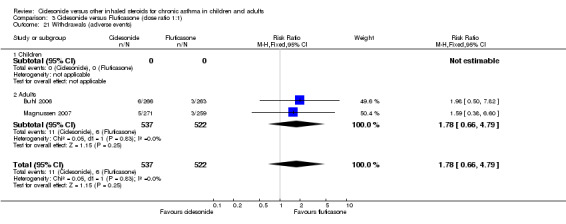
Study withdrawal & adverse event data
There was no significant difference in the frequency of withdrawals between treatments (RR 1.01; 95% confidence interval 0.79 to 1.28). Lack of efficacy leading to withdrawal was available for two studies which did not indicate that there was a significant difference between treatments, although the finding was of only marginal non‐significance (RR 2.55; 95% CI 0.86 to 7.53). There was no difference in the risk of adverse events overall. Candidiasis occurred more frequently with FP than CIC (RR 0.24 (95% CI 0.1 to 0.58). Upper respiratory tract infection, pharyngitis or headache did not differ significantly between the treatments.
4. Ciclesonide versus FP (1:2 dose ratio)
Primary outcomes
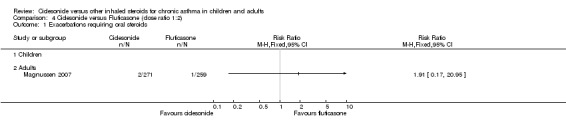
Exacerbations requiring oral steroids
Magnussen 2007 reported a low number of events for this outcome (three participants in total).
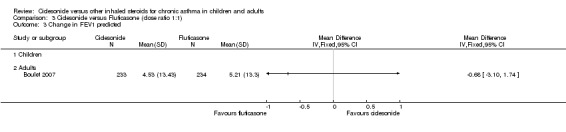
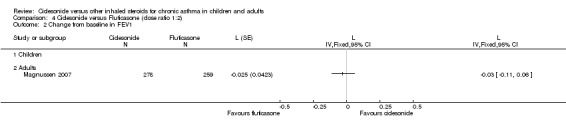
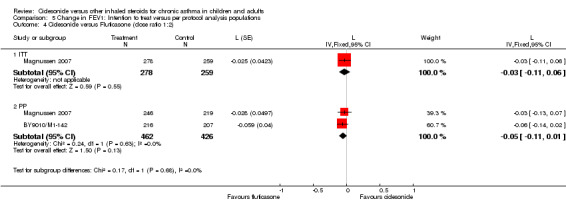
Lung function
Pooled analysis was only possible for per protocol populations from Magnussen 2007 and BY9010/M1‐142, which gave a mean difference of ‐0.05 L; 95% confidence interval ‐0.11 to 0.1). Zietkowski 2006 reported that CIC at half the daily dose equivalent of FP improved FEV1 to a similar degree with no significant differences found between treatments as regards the end study FEV1 (WMD 0.08 L; 95% confidence interval ‐0.52 to 0.68) but the number of participants was low (N = 12). Other lung function parameters (FVC, am and pm PEF) were not reported. All studies reporting these data were conducted in adults (Zietkowski 2006; Lipworth 2005).
Secondary outcomes
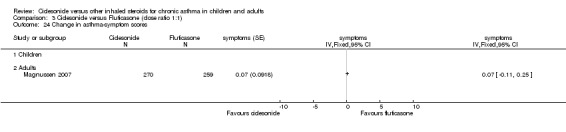
Symptoms, rescue medications use & non‐specific exacerbations of asthma
In Lipworth 2005, one patient each on CIC (combined results of CIC 320 and CIC 640 arms) and FP had a worsening of asthma but rescue use and asthma symptoms were not reported. Zietkowski 2006 reported significant clinical improvement, reduction in asthma symptoms with a reduction in rescue use were observed (P<0.05) in all treatment groups.
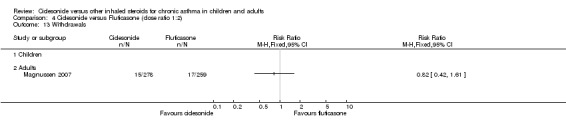
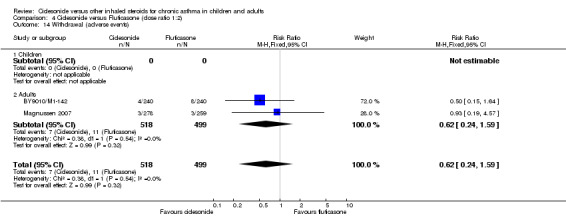
Study withdrawal & adverse event data
Pooled data for withdrawals due to adverse events was not significantly different (RR 0.62; 95% confidence interval 0.24 to 1.59).
Discussion
This review assesses the relative efficacy and safety of ciclesonide at nominal equivalent one to one and nominal doubling doses of BDP/BUD and FP. We included 21 trials which assessed the effects of these drugs in 7243 participants.
Given the apparent similarity of effect between ciclesonide and FP/BDP/BUD at a dose ratio of 1:2, a logical expectation is that ciclesonide demonstrates superior efficacy to BDP/BUD or FP when compared at a dose ratio of 1:1. Pooled analysis of both intention to treat and per protocol populations from the studies fails to demonstrate this. However, consideration of study design may explain this phenomenon. The studies which assessed the effects of ciclesonide and FP/BDP/BUD at 1:1 ratios primarily recruited participants whose asthma was treated with a ceiling dose of steroid indicative of mild to moderate asthma. Where this criterion for study entry exceeded 500 μg BDP equivalent (Bateman 2007; Boulet 2006), FEV1 predicted indicated that their asthma was well‐controlled at baseline.
When the comparator steroid doses assessed in the trials are considered, it is clear that the study populations were exposed to low doses of steroids in the 1:1 dose comparison studies. Of the 10 studies which contribute data to these analyses, only Adachi 2007 and Bateman 2007 compared ciclesonide to total daily doses of steroids higher than 500 μg/d BDP equivalent (BDP 800 μg/d and FP 660 μg/d respectively, seeTable 1). In the remainder of the trials, ciclesonide and its comparator were given at doses of 400 μg BDP equivalent or lower. Thus, the range of doses of the comparator steroid in the 1:1 ratio analyses, combined with the stipulation for low dose maintenance steroid therapy prior to study entry, suggest that the studies may only have shown successful continuation of asthma control with ciclesonide that was evident prior to study entry. The lack of an effect between the study drugs in a population of generally mild to moderate asthma patients may reflect the requirement for low levels of anti‐inflammatory preparations, and as such does not provide a reliable basis for extrapolating the findings to more severe patients, or to comparison between higher dose ranges. Studies which recruit asthma patients whose pre‐study maintenance steroid regimens are high, or who exhibit the requirement for increasing steroid load during a run‐in phase are required.
1. Ciclesonide & comparator dose.
| Study ID | ICS criterion (BDP) | Dose of CIC | Comparator |
| Adachi 2007 | >800mcg | i) 400 ii) 800 | BDP800 |
| Adler 2006 | Not reported | 200 | FP500 |
| Bateman 2007 | 1000‐2000 | 800 | FP660 |
| Bernstein 2004 | Not reported | i) 400 ii) 800 | FP1000 |
| Boulet 2006 | 320‐640 | 400 | BUD400 |
| Boulet 2007 | <1000 | 400 | FP400 |
| Buhl 2006 | <500 | 200 | FP200 |
| BY9010/M1‐136 | <500 | 200 | BUD400 |
| BY9010/M1‐137 | <500 | 200 | BUD400 |
| BY9010/M1‐142 | <500 | 100 | FP200 |
| Hansel 2006 | <500 | i) 100 ii) 200 | BUD200 |
| Lipworth 2005 | 0 | i) 400 ii) 800 | FP1000 |
| Magnussen 2007 | <500 | i) 100 ii) 200 | FP200 |
| Niphadkar 2005 | <500 | 200 | BUD200 |
| Pedersen 2006 | <400 | 200 | FP200 |
| Ukena 2006 | <500 | 400 | BUD400 |
| Vermeulen 2007 | 400‐800 | 400 | BUD800 |
| von Berg 2007 | <400 | 200 | BUD400 |
| Zietkowski 2006 | 500 | i) 100 ii) 200 | FP200 |
The limits of equivalence we have used may not be stable across the age groups assessed in the studies, and the limit of 100 ml for FEV1 was chosen conservatively since in paediatric populations where lung capacity is lower than in adults or adolescents, a clinically meaningful difference is likely to be lower. To date only two studies have been conducted in children under the age of 12 years (Pedersen 2006; von Berg 2007), and further trials in this population are a priority.
The relative effects of these drugs on safety outcomes should also be considered in assessing suitability of these therapies in chronic application. The main advantage of ciclesonide compared to other ICS such as BUD, BDP, and FP is that it is enzymatically converted in the lung to the principal active metabolite C21‐des‐methylpropionaql‐ciclesonide (des‐CIC), reducing the potential for local side effects in the mouth and throat. The pharmacology of the active compound (des‐CIC) shows that it not only exhibits a high receptor binding activity (Lipworth 2005a) at a level between BUD and FP, but it has a high level of protein binding compared to FP (99% plasma protein bound compared to 90%) resulting in a lower free unbound ciclesonide steroid in the systemic circulation.
Ciclesonide should, therefore, lead to fewer systemic adverse events, but the only finding of note for adverse events was the significant reduction in oral candidiasis by 75% when compared with FP at a dose ratio of 1:1. The impact of reduced oral candidiasis may be significant for patients who find this particular side‐effect an impediment to adherence with their ICS, although the way in which these data were obtained in the studies may overestimate the effect of ciclesonide. The monitoring of adverse events in studies primarily interested in efficacy can yield inconsistent results (Adams 2005b). The way in which candidiasis was measured and reported in the studies leaves the validity of this effect in doubt. Since prolonged ciclesonide use may have systemic effects, the monitoring of oral candida in a systematic way with fungal throat cultures should be the standard way of confirming this. Gelfand 2006, a study included in the placebo/dose response review of ciclesonide (Manning 2008), took steps to provide confirmation of candida and reported a low event rate. The data on comparative tolerability and safety of ciclesonide with other ICS are imprecise (compared to BDP/BUD or FP). Data on longer term safety of ciclesonide in children, with particular consideration of the suppression of hypothalamic‐pituitary‐adrenal (HPA) axis and growth in children are required.
There are a number of limitations highlighted in this review. In particular, the characteristics of the studies and their populations are generally unsuitable to conclude equivalence across a range of doses of ciclesonide, and across different severities of asthma. Data on exacerbations defined by oral steroid treatment are lacking and further research in this area is necessary. Symptoms and quality of life were not reported consistently across the studies, and more data for these endpoints would be of value. These issues are important as they are the main purported advantages associated with ciclesonide in comparison to the other inhaled corticosteroids for asthma. Data on several key outcomes are incomplete in our analyses. This is primarily due to the lack of complete availability of data from the available studies, although analysis of three as yet unpublished studies has been possible (BY9010/M1‐136; BY9010/M1‐137; BY9010/M1‐142).
Authors' conclusions
Implications for practice.
The results of this review provide evidence that ciclesonide is equivalent to BDP/BUD in terms of peak flow at dose ratios of 1:1, but the effect in terms of FEV1 was more inconsistent. When compared with FP, ciclesonide demonstrated equivalence in FEV1 and peak flow at dose ratios of 1:1. The patients recruited to the studies of this review were generally mild to moderate as measured by the stipulation for low doses of maintenance treatment and moderate airway obstruction. We could not establish that the use of ciclesonide provided equivalent or superior tolerability at the same doses since the confidence intervals indicated imprecise findings. The finding of lower oral candidiasis with ciclesonide compared to FP may be important for those who find this side effect troublesome. How confirmation of oral thrush was obtained was not reported across the studies, and future studies should provide better descriptions as to how and whether such procedures were undertaken.
Implications for research.
Studies in children are required, and in particular the collection of data on side effects in this population. The findings in this review generally lack precision and more trials would help to establish the relative efficacy of ciclesonide and other ICS agents, before clinically meaningful effects can be ruled out. This is particularly the case in comparison with FP at half the dose. The updated GINA guidelines recommend the early addition of long‐acting ß2‐agonists therapy to ICS to gain control of asthma symptoms. It would be useful to determine whether the addition of LABAs to ciclesonide proves beneficial in future trials of this therapy.
What's new
| Date | Event | Description |
|---|---|---|
| 22 July 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 2, 2008
| Date | Event | Description |
|---|---|---|
| 17 January 2008 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We are grateful to the staff of the editorial base of the Cochrane Airways Group for providing assistance in running searches and obtaining papers. The contact author received a Cochrane Fellowship from the Health Research Board, for the island of Ireland.
Data and analyses
Comparison 1. Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change from baseline in FEV1 | 4 | 1322 | L (Random, 95% CI) | 0.03 [‐0.06, 0.11] |
| 1.1 Children | 0 | 0 | L (Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Adults | 4 | 1322 | L (Random, 95% CI) | 0.03 [‐0.06, 0.11] |
| 2 Change from baseline in FVC | 3 | 970 | L (Fixed, 95% CI) | 0.06 [0.01, 0.11] |
| 2.1 Children | 1 | 399 | L (Fixed, 95% CI) | 0.11 [0.00, 0.22] |
| 2.2 Adults | 2 | 571 | L (Fixed, 95% CI) | 0.05 [‐0.00, 0.10] |
| 3 Change from baseline in clinic PEF (L/min) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Children | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Adults | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Change from baseline in am PEF | 4 | 1329 | L/min (Fixed, 95% CI) | 5.37 [0.12, 10.61] |
| 4.1 Children | 0 | 0 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Adults | 4 | 1329 | L/min (Fixed, 95% CI) | 5.37 [0.12, 10.61] |
| 5 Change from baseline in pm PEF | 2 | 758 | L/min (Fixed, 95% CI) | 3.95 [‐2.89, 10.80] |
| 5.1 Children | 0 | 0 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Adults | 2 | 758 | L/min (Fixed, 95% CI) | 3.95 [‐2.89, 10.80] |
| 6 Change in asthma symptom score | 1 | Symptom score units (Random, 95% CI) | Totals not selected | |
| 6.1 Children | 0 | Symptom score units (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Adults | 1 | Symptom score units (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Withdrawals (total) | 2 | 771 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.47, 1.19] |
| 7.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Adults | 2 | 771 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.47, 1.19] |
| 8 Withdrawals (lack of efficacy) | 3 | 1130 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.88, 2.01] |
| 8.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Adults | 3 | 1130 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.88, 2.01] |
| 9 Adverse events | 3 | 1131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.85, 1.15] |
| 9.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Adults | 3 | 1131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.85, 1.15] |
| 10 Candidiasis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11 Pharyngitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13 Exacerbations of asthma | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Sore throat | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15 Voice alteration | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 16 Changes in cortisol levels (urinary) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Asthma (not otherwsie specified) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 Children | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Adults | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Upper respiratory tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Headache | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Rhinitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Withdrawals (adverse events) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 22.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Cough | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 23.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Data not suitable for meta‐analysis (medians) | Other data | No numeric data | ||
| 25.1 Symptoms | Other data | No numeric data | ||
| 25.2 Rescue medication use | Other data | No numeric data |
1.1. Analysis.
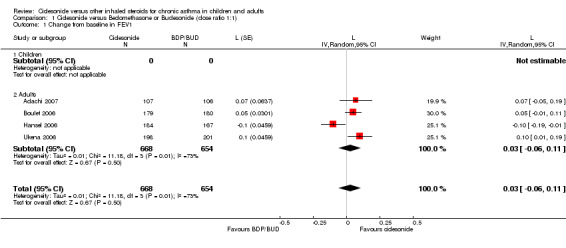
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 1 Change from baseline in FEV1.
1.2. Analysis.
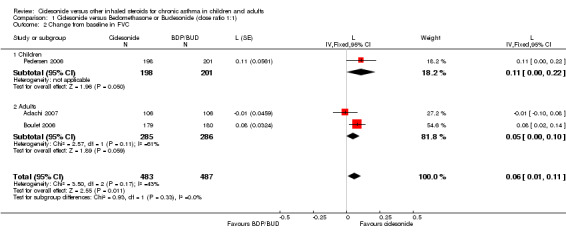
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 2 Change from baseline in FVC.
1.3. Analysis.
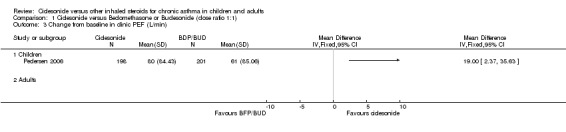
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 3 Change from baseline in clinic PEF (L/min).
1.4. Analysis.
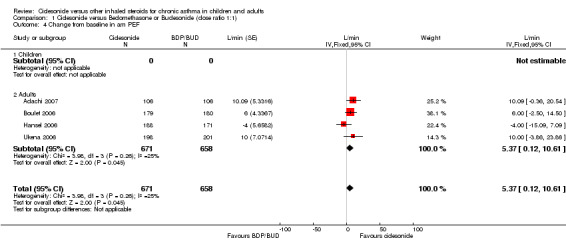
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 4 Change from baseline in am PEF.
1.5. Analysis.
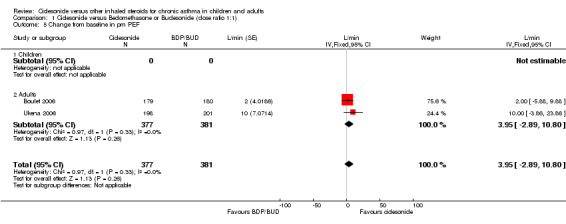
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 5 Change from baseline in pm PEF.
1.6. Analysis.
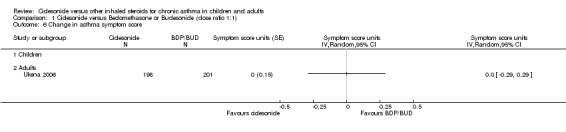
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 6 Change in asthma symptom score.
1.7. Analysis.
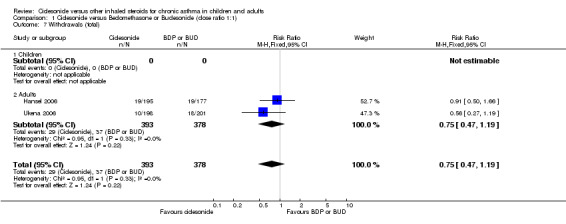
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 7 Withdrawals (total).
1.8. Analysis.
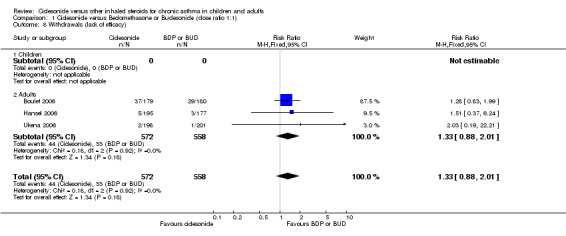
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 8 Withdrawals (lack of efficacy).
1.9. Analysis.
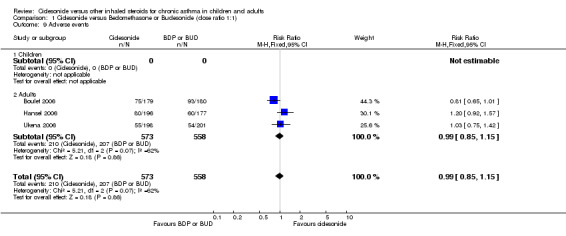
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 9 Adverse events.
1.10. Analysis.
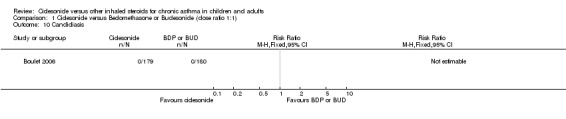
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 10 Candidiasis.
1.11. Analysis.

Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 11 Pharyngitis.
1.13. Analysis.
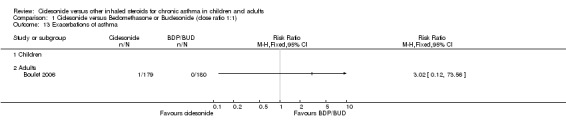
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 13 Exacerbations of asthma.
1.14. Analysis.
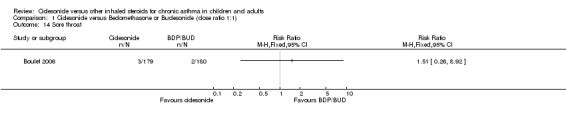
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 14 Sore throat.
1.15. Analysis.
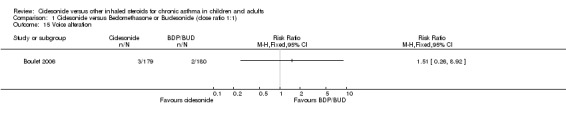
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 15 Voice alteration.
1.16. Analysis.
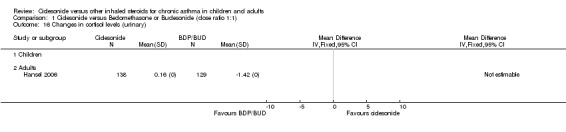
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 16 Changes in cortisol levels (urinary).
1.17. Analysis.
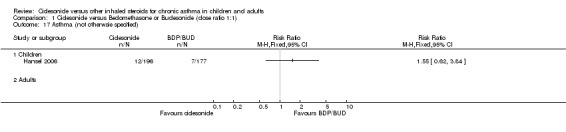
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 17 Asthma (not otherwsie specified).
1.18. Analysis.
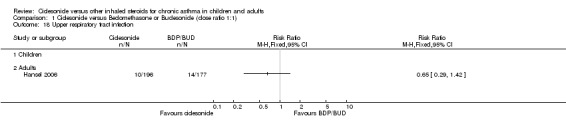
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 18 Upper respiratory tract infection.
1.19. Analysis.
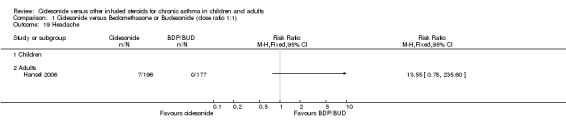
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 19 Headache.
1.21. Analysis.
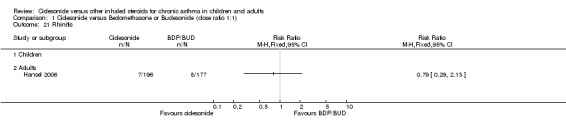
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 21 Rhinitis.
1.22. Analysis.
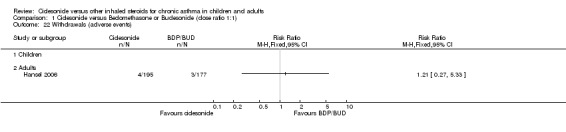
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 22 Withdrawals (adverse events).
1.23. Analysis.
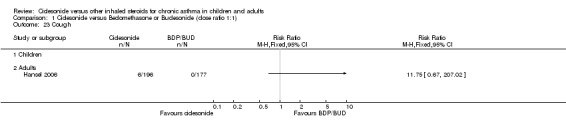
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 23 Cough.
1.25. Analysis.
Comparison 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1), Outcome 25 Data not suitable for meta‐analysis (medians).
| Data not suitable for meta‐analysis (medians) | |
|---|---|
| Study | |
| Symptoms | |
| Hansel 2006 | 0.05 |
| Rescue medication use | |
| Hansel 2006 | 0.05puffs/d |
Comparison 2. Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change from baseline in FEV1 | 5 | 1633 | L (Fixed, 95% CI) | ‐0.02 [‐0.05, 0.00] |
| 1.1 Children | 1 | 621 | L (Fixed, 95% CI) | ‐0.02 [‐0.06, 0.02] |
| 1.2 Adults | 4 | 1012 | L (Fixed, 95% CI) | ‐0.03 [‐0.06, 0.01] |
| 2 Change from baseline in FVC | 5 | 1637 | L (Fixed, 95% CI) | ‐0.01 [‐0.04, 0.03] |
| 2.1 Children | 1 | 621 | L (Fixed, 95% CI) | ‐0.02 [‐0.07, 0.02] |
| 2.2 Adults | 4 | 1016 | L (Fixed, 95% CI) | 0.02 [‐0.03, 0.07] |
| 3 Change in clinic PEF | 1 | L/min (Fixed, 95% CI) | Totals not selected | |
| 3.1 Children | 0 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Adults | 1 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Change in am PEF | 4 | 1423 | L/min (Fixed, 95% CI) | 0.07 [‐5.05, 5.19] |
| 4.1 Children | 1 | 621 | L/min (Fixed, 95% CI) | ‐2.3 [‐8.90, 4.30] |
| 4.2 Adults | 3 | 802 | L/min (Fixed, 95% CI) | 3.64 [‐4.47, 11.74] |
| 5 Change in pm PEF | 4 | 1423 | L/min (Fixed, 95% CI) | 3.29 [‐1.62, 8.19] |
| 5.1 Children | 1 | 621 | L/min (Fixed, 95% CI) | 3.3 [‐1.00, 9.60] |
| 5.2 Adults | 3 | 802 | L/min (Fixed, 95% CI) | 3.27 [‐4.54, 11.09] |
| 6 Change in quality of life (Paediatric AQLQ) | 2 | 1010 | AQLQ (Fixed, 95% CI) | ‐0.00 [‐0.09, 0.09] |
| 7 Adverse events | 6 | 1912 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.17] |
| 7.1 Children | 1 | 621 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.81, 1.24] |
| 7.2 Adults | 5 | 1291 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.91, 1.23] |
| 8 Worsening asthma | 2 | 404 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.49, 1.69] |
| 8.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Adults | 2 | 404 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.49, 1.69] |
| 9 Upper respiratory tract infection | 6 | 1802 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.75, 1.47] |
| 9.1 Children | 1 | 621 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.28, 1.17] |
| 9.2 Adults | 5 | 1181 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.86, 1.88] |
| 10 Pharyngitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Rhinitis | 2 | 404 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.08, 1.62] |
| 11.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Adults | 2 | 404 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.08, 1.62] |
| 12 Oral candidiasis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 12.1 Children | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Adults | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
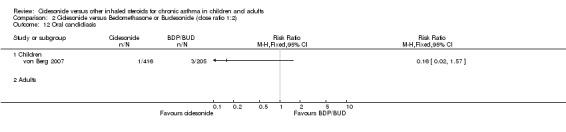
| 13 Withdrawals | 4 | 1427 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.82, 2.11] |
| 13.1 Children | 1 | 621 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.17 [0.83, 5.64] |
| 13.2 Adults | 3 | 806 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.61, 1.84] |
| 14 Withdrawals (lack of efficacy) | 3 | 1024 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.84, 7.13] |
| 14.1 Children | 1 | 621 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.96 [0.67, 13.09] |
| 14.2 Adults | 2 | 403 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.42, 9.10] |
| 15 Withdrawals (adverse events) | 4 | 777 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [0.96, 7.07] |
| 15.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Adults | 4 | 777 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [0.96, 7.07] |
2.1. Analysis.
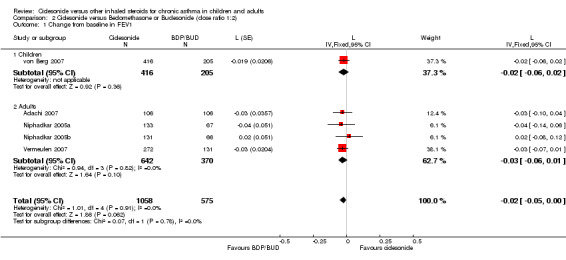
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 1 Change from baseline in FEV1.
2.2. Analysis.
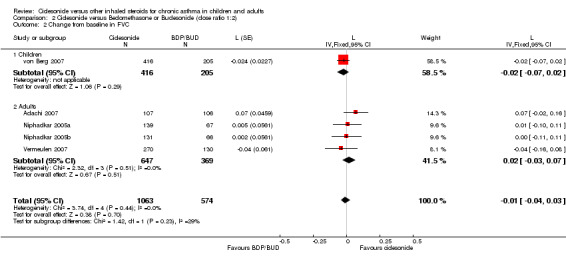
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 2 Change from baseline in FVC.
2.3. Analysis.
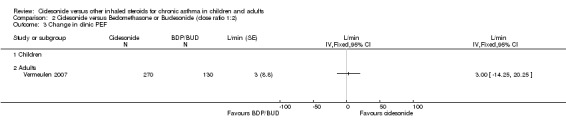
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 3 Change in clinic PEF.
2.4. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 4 Change in am PEF.
2.5. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 5 Change in pm PEF.
2.6. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 6 Change in quality of life (Paediatric AQLQ).
2.7. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 7 Adverse events.
2.8. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 8 Worsening asthma.
2.9. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 9 Upper respiratory tract infection.
2.10. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 10 Pharyngitis.
2.11. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 11 Rhinitis.
2.12. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 12 Oral candidiasis.
2.13. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 13 Withdrawals.
2.14. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 14 Withdrawals (lack of efficacy).
2.15. Analysis.
Comparison 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2), Outcome 15 Withdrawals (adverse events).
Comparison 3. Ciclesonide versus Fluticasone (dose ratio 1:1).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Exacerbations requiring oral steroids | 3 | 1537 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.40, 1.95] |
| 1.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Adults | 3 | 1537 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.40, 1.95] |
| 2 Change from baseline in FEV1 | 5 | 2599 | L (Fixed, 95% CI) | ‐0.02 [‐0.04, 0.01] |
| 2.1 Children | 1 | 556 | L (Fixed, 95% CI) | 0.0 [‐0.04, 0.04] |
| 2.2 Adults | 4 | 2043 | L (Fixed, 95% CI) | ‐0.03 [‐0.07, 0.01] |
| 3 Change in FEV1 predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Change in FVC | 4 | 2051 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.04, 0.04] |
| 4.1 Children | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Adults | 4 | 2051 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.04, 0.04] |
| 5 Change in clinic PEF | 3 | 1611 | L/min (Fixed, 95% CI) | ‐1.59 [‐7.43, 4.25] |
| 5.1 Children | 1 | 556 | L/min (Fixed, 95% CI) | ‐2.5 [‐10.34, 5.34] |
| 5.2 Adults | 2 | 1055 | L/min (Fixed, 95% CI) | ‐0.45 [‐9.22, 8.31] |
| 6 Change in am PEF | 4 | 2070 | L/min (Fixed, 95% CI) | 0.41 [‐4.71, 5.53] |
| 6.1 Children | 1 | 556 | L/min (Fixed, 95% CI) | ‐2.9 [‐11.33, 5.53] |
| 6.2 Adults | 3 | 1514 | L/min (Fixed, 95% CI) | 2.34 [‐4.10, 8.78] |
| 7 Change in pm PEF | 2 | 1023 | L/min (Fixed, 95% CI) | 1.30 [‐5.10, 7.70] |
| 7.1 Children | 1 | 556 | L/min (Fixed, 95% CI) | ‐0.2 [‐8.24, 7.84] |
| 7.2 Adults | 1 | 467 | L/min (Fixed, 95% CI) | 3.9 [‐6.69, 14.49] |
| 8 Change in rescue medication | 2 | 1085 | puffs/d (Fixed, 95% CI) | 0.0 [‐0.10, 0.10] |
| 8.1 Children | 1 | 556 | puffs/d (Fixed, 95% CI) | 0.0 [‐0.14, 0.14] |
| 8.2 Adults | 1 | 529 | puffs/d (Fixed, 95% CI) | 0.0 [‐0.14, 0.14] |
| 9 Lack of efficacy (exacerbation requiring change in medication) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Children | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Adults | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Worsening asthma | 3 | 1552 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.61, 1.97] |
| 10.1 Children | 1 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.50, 3.14] |
| 10.2 Adults | 2 | 996 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.47, 2.14] |
| 11 Change in asthma‐symptom free days | 1 | % (Fixed, 95% CI) | Totals not selected | |
| 11.1 Children | 1 | % (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Adults | 0 | % (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Change in quality of life (AQLQ) | 2 | 967 | AQLQ (Fixed, 95% CI) | 0.17 [0.04, 0.30] |
| 12.1 Children | 0 | 0 | AQLQ (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Adults | 2 | 967 | AQLQ (Fixed, 95% CI) | 0.17 [0.04, 0.30] |
| 13 Adverse events | 4 | 2058 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.87, 1.07] |
| 13.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Adults | 4 | 2058 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.87, 1.07] |
| 14 Candidiasis | 3 | 1529 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.10, 0.58] |
| 14.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Adults | 3 | 1529 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.10, 0.58] |
| 15 Pharyngitis | 5 | 2614 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.90, 1.74] |
| 15.1 Children | 1 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.49, 2.45] |
| 15.2 Adults | 4 | 2058 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.90, 1.85] |
| 16 Upper resiratory tract infection | 3 | 1613 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.74, 1.47] |
| 16.1 Children | 1 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.57, 1.98] |
| 16.2 Adults | 2 | 1057 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.68, 1.56] |
| 17 Headache | 3 | 1613 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.52, 1.49] |
| 17.1 Children | 1 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [0.56, 3.73] |
| 17.2 Adults | 2 | 1057 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.37, 1.34] |
| 18 Rhinitis | 2 | 1084 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.61, 1.61] |
| 18.1 Children | 1 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.55, 1.69] |
| 18.2 Adults | 1 | 528 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.41, 2.81] |
| 19 Sinusitis | 2 | 1084 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.41, 1.61] |
| 19.1 Children | 1 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.19, 1.65] |
| 19.2 Adults | 1 | 528 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.43, 2.65] |
| 20 Withdrawals | 5 | 2570 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.79, 1.28] |
| 20.1 Children | 1 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.70, 3.11] |
| 20.2 Adults | 4 | 2059 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.74, 1.24] |
| 21 Withdrawals (adverse events) | 2 | 1059 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [0.66, 4.79] |
| 21.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Adults | 2 | 1059 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [0.66, 4.79] |
| 22 Withdrawals (lack of efficacy) | 3 | 1570 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.55 [0.86, 7.53] |
| 22.1 Children | 1 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.51, 8.00] |
| 22.2 Adults | 2 | 1059 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.57 [0.59, 21.51] |
| 23 Data not suitable for meta‐analysis (medians) | Other data | No numeric data | ||
| 24 Change in asthma‐symptom scores | 1 | symptoms (Fixed, 95% CI) | Totals not selected | |
| 24.1 Children | 0 | symptoms (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Adults | 1 | symptoms (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 1 Exacerbations requiring oral steroids.
3.2. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 2 Change from baseline in FEV1.
3.3. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 3 Change in FEV1 predicted.
3.4. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 4 Change in FVC.
3.5. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 5 Change in clinic PEF.
3.6. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 6 Change in am PEF.
3.7. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 7 Change in pm PEF.
3.8. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 8 Change in rescue medication.
3.9. Analysis.
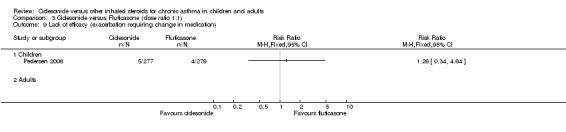
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 9 Lack of efficacy (exacerbation requiring change in medication).
3.10. Analysis.
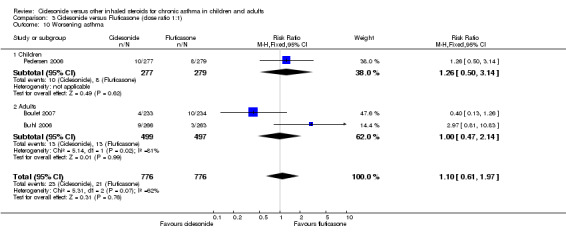
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 10 Worsening asthma.
3.11. Analysis.
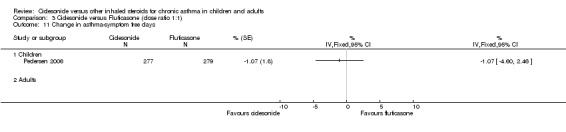
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 11 Change in asthma‐symptom free days.
3.12. Analysis.
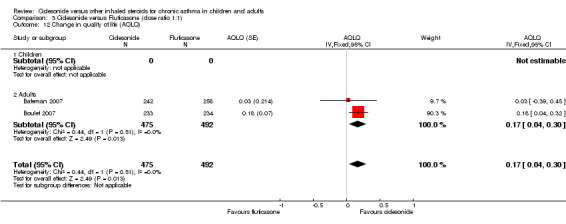
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 12 Change in quality of life (AQLQ).
3.13. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 13 Adverse events.
3.14. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 14 Candidiasis.
3.15. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 15 Pharyngitis.
3.16. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 16 Upper resiratory tract infection.
3.17. Analysis.
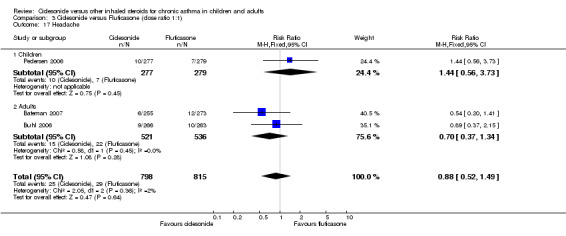
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 17 Headache.
3.18. Analysis.
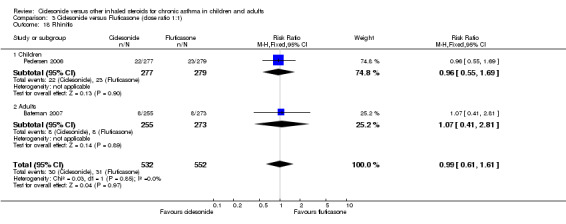
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 18 Rhinitis.
3.19. Analysis.
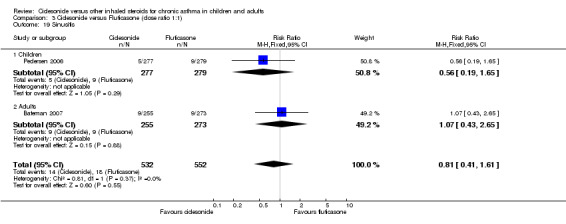
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 19 Sinusitis.
3.20. Analysis.
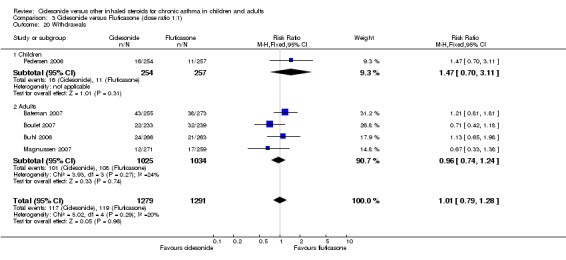
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 20 Withdrawals.
3.21. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 21 Withdrawals (adverse events).
3.22. Analysis.

Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 22 Withdrawals (lack of efficacy).
3.23. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 23 Data not suitable for meta‐analysis (medians).
| Data not suitable for meta‐analysis (medians) | ||
|---|---|---|
| Study | Outcome | Effect size (median) |
| Bateman 2007 | Rescue medication use; symptoms | ‐0.07 puffs/d; 0 |
| Boulet 2007 | Symptoms | 0 |
| Buhl 2006 | Rescue medication use | ‐0.21 puff/s |
3.24. Analysis.
Comparison 3 Ciclesonide versus Fluticasone (dose ratio 1:1), Outcome 24 Change in asthma‐symptom scores.
Comparison 4. Ciclesonide versus Fluticasone (dose ratio 1:2).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Exacerbations requiring oral steroids | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Change from baseline in FEV1 | 1 | L (Fixed, 95% CI) | Totals not selected | |
| 2.1 Children | 0 | L (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Adults | 1 | L (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Endpoint FEV1 (Litres) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Endpoint FEV1 predicted (%) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Change in FVC | 1 | L (Fixed, 95% CI) | Totals not selected | |
| 5.1 Children | 0 | L (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Adults | 1 | L (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Endpoint day symptoms | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Endpoint night symptoms | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Rescue medication use (puffs/d) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Children | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Adults | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Change in clinic PEF | 1 | L/min (Fixed, 95% CI) | Totals not selected | |
| 9.1 Children | 0 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Adults | 1 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Change in rescue medication | 1 | puffs/d (Fixed, 95% CI) | Totals not selected | |
| 10.1 Children | 0 | puffs/d (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Adults | 1 | puffs/d (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Adverse events | 2 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.83, 1.16] |
| 11.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Adults | 2 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.83, 1.16] |
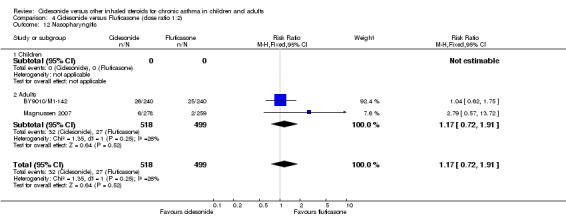
| 12 Nasopharyngitis | 2 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.72, 1.91] |
| 12.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Adults | 2 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.72, 1.91] |
| 13 Withdrawals | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13.1 Children | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Adults | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Withdrawal (adverse events) | 2 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.24, 1.59] |
| 14.1 Children | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Adults | 2 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.24, 1.59] |
4.1. Analysis.
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 1 Exacerbations requiring oral steroids.
4.2. Analysis.
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 2 Change from baseline in FEV1.
4.3. Analysis.
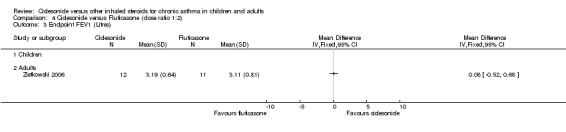
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 3 Endpoint FEV1 (Litres).
4.4. Analysis.
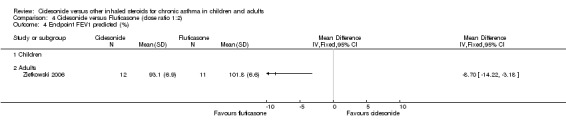
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 4 Endpoint FEV1 predicted (%).
4.5. Analysis.
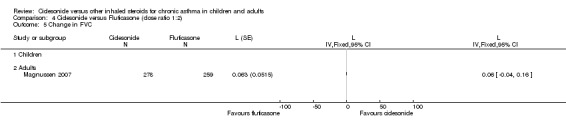
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 5 Change in FVC.
4.6. Analysis.
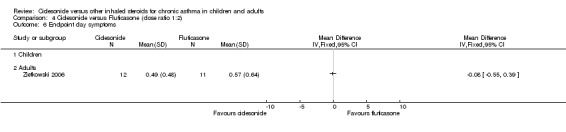
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 6 Endpoint day symptoms.
4.7. Analysis.
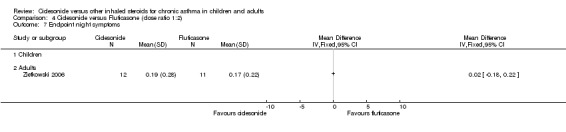
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 7 Endpoint night symptoms.
4.8. Analysis.
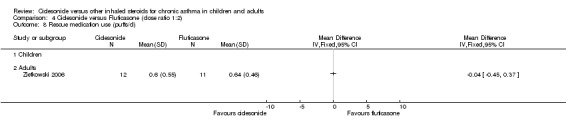
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 8 Rescue medication use (puffs/d).
4.9. Analysis.
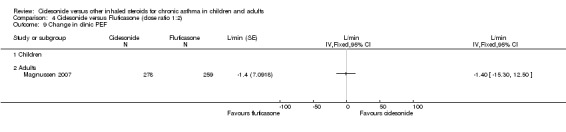
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 9 Change in clinic PEF.
4.10. Analysis.
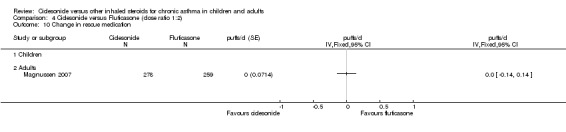
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 10 Change in rescue medication.
4.11. Analysis.
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 11 Adverse events.
4.12. Analysis.
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 12 Nasopharyngitis.
4.13. Analysis.
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 13 Withdrawals.
4.14. Analysis.
Comparison 4 Ciclesonide versus Fluticasone (dose ratio 1:2), Outcome 14 Withdrawal (adverse events).
Comparison 5. Change in FEV1: Intention to treat versus per protocol analysis populations.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1) | 4 | L (Fixed, 95% CI) | Subtotals only | |
| 1.1 ITT | 4 | 1322 | L (Fixed, 95% CI) | 0.03 [‐0.01, 0.07] |
| 1.2 PP | 2 | 618 | L (Fixed, 95% CI) | 0.01 [‐0.05, 0.06] |
| 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2) | 7 | L (Fixed, 95% CI) | Subtotals only | |
| 2.1 ITT | 5 | 1633 | L (Fixed, 95% CI) | ‐0.02 [‐0.05, 0.00] |
| 2.2 PP | 6 | 1574 | L (Fixed, 95% CI) | ‐0.03 [‐0.06, 0.00] |
| 3 Ciclesonide versus Fluticasone (dose ratio 1:1) | 5 | L (Fixed, 95% CI) | Subtotals only | |
| 3.1 ITT | 5 | 2599 | L (Fixed, 95% CI) | ‐0.02 [‐0.04, 0.01] |
| 3.2 PP | 5 | 2178 | L (Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Ciclesonide versus Fluticasone (dose ratio 1:2) | 2 | L (Fixed, 95% CI) | Subtotals only | |
| 4.1 ITT | 1 | 537 | L (Fixed, 95% CI) | ‐0.03 [‐0.11, 0.06] |
| 4.2 PP | 2 | 888 | L (Fixed, 95% CI) | ‐0.05 [‐0.11, 0.01] |
5.1. Analysis.
Comparison 5 Change in FEV1: Intention to treat versus per protocol analysis populations, Outcome 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1).
5.2. Analysis.
Comparison 5 Change in FEV1: Intention to treat versus per protocol analysis populations, Outcome 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2).
5.3. Analysis.
Comparison 5 Change in FEV1: Intention to treat versus per protocol analysis populations, Outcome 3 Ciclesonide versus Fluticasone (dose ratio 1:1).
5.4. Analysis.
Comparison 5 Change in FEV1: Intention to treat versus per protocol analysis populations, Outcome 4 Ciclesonide versus Fluticasone (dose ratio 1:2).
Comparison 6. Change in PEF: Intention to treat versus per protocol analysis populations.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1) | 4 | L/min (Fixed, 95% CI) | Subtotals only | |
| 1.1 ITT | 4 | 1329 | L/min (Fixed, 95% CI) | 5.37 [0.12, 10.61] |
| 1.2 PP | 2 | 629 | L/min (Fixed, 95% CI) | 4.24 [‐3.87, 12.34] |
| 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2) | 4 | L/min (Fixed, 95% CI) | Subtotals only | |
| 2.1 ITT | 4 | 1423 | L/min (Fixed, 95% CI) | 0.07 [‐5.05, 5.19] |
| 2.2 PP | 4 | 1258 | L/min (Fixed, 95% CI) | ‐0.62 [‐5.96, 4.73] |
| 3 Ciclesonide versus Fluticasone (dose ratio 1:1) | 4 | L/min (Fixed, 95% CI) | Subtotals only | |
| 3.1 ITT | 4 | 2070 | L/min (Fixed, 95% CI) | 0.41 [‐4.71, 5.53] |
| 3.2 PP | 4 | 1741 | L/min (Fixed, 95% CI) | ‐0.31 [‐5.75, 5.13] |
| 4 Ciclesonide versus Fluticasone (dose ratio 1:2) | 0 | L/min (Fixed, 95% CI) | Totals not selected | |
| 4.1 ITT | 0 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 PP | 0 | L/min (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.
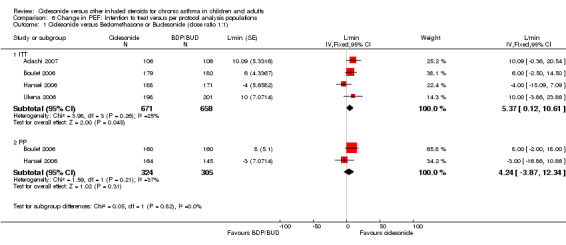
Comparison 6 Change in PEF: Intention to treat versus per protocol analysis populations, Outcome 1 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1).
6.2. Analysis.
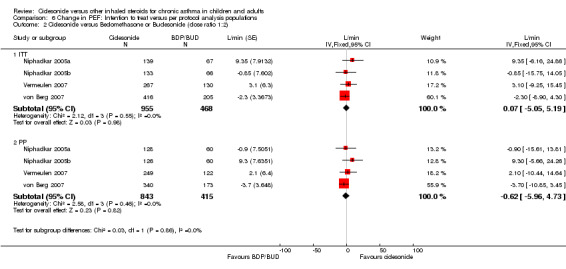
Comparison 6 Change in PEF: Intention to treat versus per protocol analysis populations, Outcome 2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2).
6.3. Analysis.
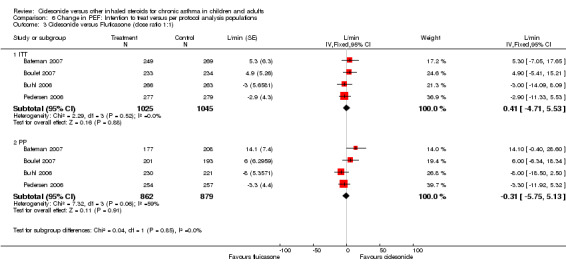
Comparison 6 Change in PEF: Intention to treat versus per protocol analysis populations, Outcome 3 Ciclesonide versus Fluticasone (dose ratio 1:1).
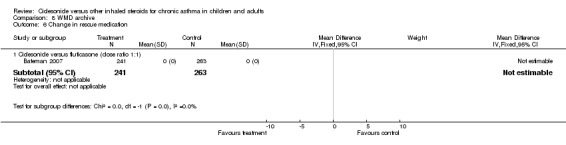
Comparison 8. WMD archive.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
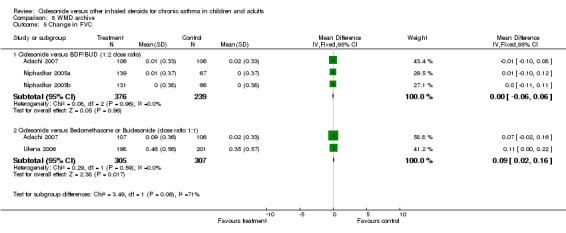
| 1 Change in FEV1 | 11 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Ciclesonide versus BDP or BUD | 3 | 963 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 1.2 Ciclesonide versus BDP or BUD per protocol | 1 | 298 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.19, 0.01] |
| 1.3 Ciclesonide versus BDP or BUD (dose ratio 1:2) | 4 | 1130 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.01] |
| 1.4 Ciclesonide versus BDP or BUD pre protocol (dose ratio 1:2) | 4 | 702 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.08, 0.03] |
| 1.5 Ciclesonide versus fluticasone (dose ratio 1:1) | 3 | 1530 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.09, 0.01] |
| 1.6 Ciclesonide versus fluticasone per protocol (dose ratio 1:1) | 2 | 845 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.08, 0.05] |
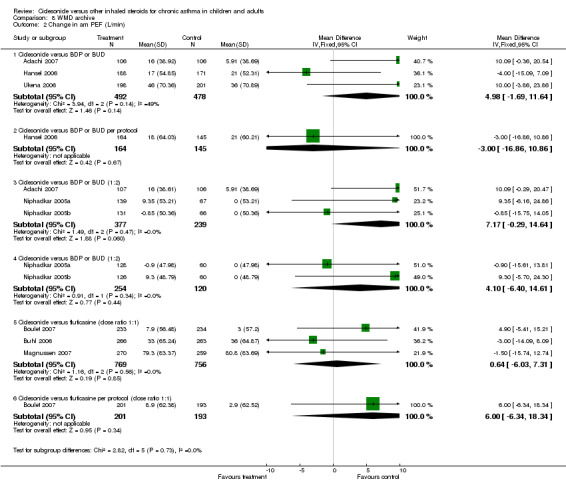
| 2 Change in am PEF (L/min) | 8 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Ciclesonide versus BDP or BUD | 3 | 970 | Mean Difference (IV, Fixed, 95% CI) | 4.98 [‐1.69, 11.64] |
| 2.2 Ciclesonide versus BDP or BUD per protocol | 1 | 309 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐16.86, 10.86] |
| 2.3 Ciclesonide versus BDP or BUD (1:2) | 3 | 616 | Mean Difference (IV, Fixed, 95% CI) | 7.17 [‐0.29, 14.64] |
| 2.4 Ciclesonide versus BDP or BUD (1:2) | 2 | 374 | Mean Difference (IV, Fixed, 95% CI) | 4.10 [‐6.40, 14.61] |
| 2.5 Ciclesonide versus fluticasine (dose ratio 1:1) | 3 | 1525 | Mean Difference (IV, Fixed, 95% CI) | 0.64 [‐6.03, 7.31] |
| 2.6 Ciclesonide versus fluticasine per protocol (dose ratio 1:1) | 1 | 394 | Mean Difference (IV, Fixed, 95% CI) | 6.00 [‐6.34, 18.34] |
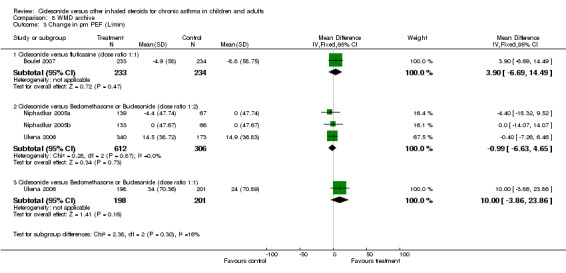
| 3 Change in pm PEF (L/min) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Ciclesonide versus fluticasine (dose ratio 1:1) | 1 | 467 | Mean Difference (IV, Fixed, 95% CI) | 3.90 [‐6.69, 14.49] |
| 3.2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2) | 3 | 918 | Mean Difference (IV, Fixed, 95% CI) | ‐0.99 [‐6.63, 4.65] |
| 3.3 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1) | 1 | 399 | Mean Difference (IV, Fixed, 95% CI) | 10.0 [‐3.86, 23.86] |
| 4 Change in quality of life (AQLQ) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Ciclesonide versus fluticasone (dose ratio 1:1) | 1 | 500 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.39, 0.45] |
| 4.2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:2) | 1 | 389 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.14, 0.16] |
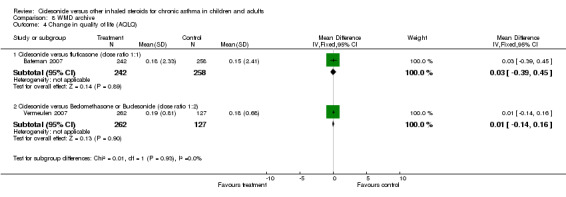
| 5 Change in FVC | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Ciclesonide versus BDP/BUD (1:2 dose ratio) | 3 | 615 | Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.06, 0.06] |
| 5.2 Ciclesonide versus Beclomethasone or Budesonide (dose ratio 1:1) | 2 | 612 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [0.02, 0.16] |
| 6 Change in rescue medication | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Ciclesonide versus fluticasone (dose ratio 1:1) | 1 | 504 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
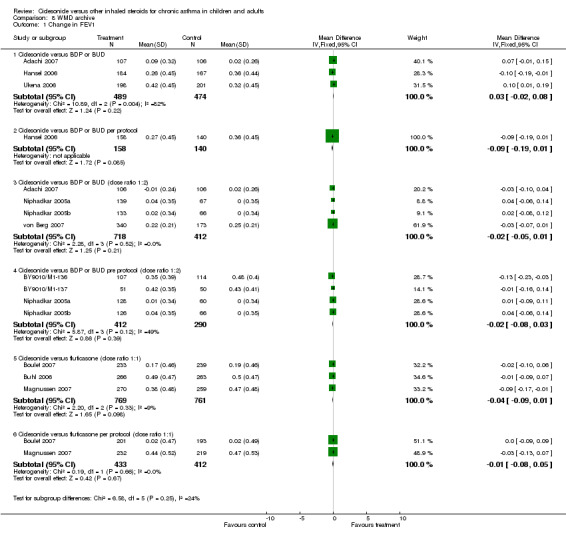
Comparison 8 WMD archive, Outcome 1 Change in FEV1.
8.2. Analysis.
Comparison 8 WMD archive, Outcome 2 Change in am PEF (L/min).
8.3. Analysis.
Comparison 8 WMD archive, Outcome 3 Change in pm PEF (L/min).
8.4. Analysis.
Comparison 8 WMD archive, Outcome 4 Change in quality of life (AQLQ).
8.5. Analysis.
Comparison 8 WMD archive, Outcome 5 Change in FVC.
8.6. Analysis.
Comparison 8 WMD archive, Outcome 6 Change in rescue medication.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adachi 2007.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 59 centres in Japan DURATION OF STUDY: 8 weeks (4 week run‐in period CFC‐BDP 800 mcg/day). CONCEALMENT OF ALLOCATION: Unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: No METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not stated METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Open label DESCRIPTION OF WITHDRAWALS/DROPOUTS: Not stated JADAD SCORE (5‐1): 1 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Not clear COMPLIANCE: Not reported CONFOUNDERS: Balanced groups at baseline | |
| Participants | N SCREENED: 478 N RANDOMISED: 316 (213 to groups of interest to this review) N COMPLETED: Not clear M = 105; F = 108 MEAN AGE: 52.3 years BASELINE DETAILS: FEV1 69% predicted; FVC: 2.76 L INCLUSION CRITERIA: 16‐75 years; moderate to severe asthma according to the Japanese Guidelines; treated with >800 mg/day CFC‐BDP or > 400 mg/day of FP for more than four weeks; mean morning PEF during last week of run‐in of <80% predicted PEF; reversibility of airflow limitation of >15%. EXCLUSION: Significant coexisting respiratory disease; hospitalization, emergency room care for asthma or treatment with systemic steroids < 4 weeks before run‐in. | |
| Interventions | 1. Ciclesonide 200 mcg BID (400 mcg/d) 2. Ciclesonide 400 mcg BID (800 mcg/d) 3. Beclomethasone 400 mcg BID (800 mcg/d) DELIVERY: CIC: HFA‐MDI; BDP: CFC‐MDI + spacer TREATMENT PERIOD: 8 weeks RESCUE: SABA CO‐INTERVENTIONS PERMITTED: Not stated % on ICS baseline: 100 | |
| Outcomes | am PEF; pm PEF; FEV1; FVC; symptoms; use of rescue medication | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Adler 2006.
| Methods | STUDY DESIGN: Parallel group ‐ pilot study LOCATION, NUMBER OF CENTRES: Multicentre DURATION OF STUDY: 12 months (2 week run‐in on FP 250 mcg/d) CONCEALMENT OF ALLOCATION: Unknown COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Not reported DESCRIPTION OF WITHDRAWALS/DROPOUTS: No JADAD SCORE (5‐1): 2 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT (presumed as most likely) COMPLIANCE: Not reported CONFOUNDERS: Not reported | |
| Participants | N SCREENED: Unknown N RANDOMISED: 111 N COMPLETED: Unknown M = unknown; F = unknown MEDIAN AGE: Range 17‐75 years BASELINE DETAILS: Not reported INCLUSION CRITERIA: Stable asthma; FEV1 >= 90% EXCLUSION: Not reported | |
| Interventions | 1. Ciclesonide 200 mcg OD (CIC 200)
2. Fluticasone 250 mcg BID (FP 500) DELIVERY: CIC: HFA‐MDI; FP MDI TREATMENT PERIOD: 12 weeks RESCUE: Not reported CO‐INTERVENTIONS PERMITTED: Not reported CO‐INTERVENTIONS: Not reported % on ICS baseline: Not reported |
|
| Outcomes | % days without asthma symptoms; % days without asthma symptoms or rescue | |
| Notes | Unpublished conference abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Bateman 2007.
| Methods | STUDY DESIGN: Randomised parallel group trial LOCATION, NUMBER OF CENTRES: 100 centres in North America and Europe DURATION OF STUDY: Six months CONCEALMENT OF ALLOCATION: A DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: No METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Centralised, automated facsimile system (Fisher Automated Clinical Trial Service [FACTS]. METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Open label DESCRIPTION OF WITHDRAWALS/DROPOUTS: Stated TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT | |
| Participants | N SCREENED: 658 N RANDOMISED: 528 (CIC: 255; FP: 273) N COMPLETED: 447 M = 206 F = 322 MEAN AGE: 43 BASELINE DETAILS: FEV1 predicted: 93%; Baseline AQLQ score: 5.79 INCLUSION CRITERIA: 12‐75 years; 6 month history of ATS defined asthma; FP 500‐1000 mg/day or equivalent; FEV1 greater than 80% predicted, measured 4h post‐SABA and 24 h post‐other asthma medication. Post‐run in: FEV1 greater than 80% predicted; reversibility of greater than 12% (and greater than 0.200 L), or diurnal PEF greater than 15% during 3 or more days within the last week of run‐in. At least 1 day without any asthma symptoms during the last 7 days prior to baseline. EXCLUSION CRITERIA: Coexisting severe diseases; COPD and/or other relevant lung diseases other than asthma; use of systemic steroids within 4 weeks (injectable depot steroids, 6 weeks) prior study or more than three times during previous 6 months; use of non‐allowed drugs, including corticosteroids other than specified in the inclusion criteria, ketotifen, inhaled anticholinergics, disodium cromoglycate and nedocromil, and bronchoconstrictive agents, including ß‐blockers. Patients with more than 10 cigarette pack‐years (ex‐smokers or current smokers). | |
| Interventions | 1. Ciclesonide 400 mcg BID (800 mcg/d)
2. Fluticasone 330 mcg BID (660 mcg/d) DELIVERY: HFA‐metered dose inhalers RUN‐IN PERIOD: Two weeks on current ICS therapy (500‐1000 mcg/d FP equivalent) TREATMENT PERIOD: Six months RESCUE: Salbutamol CO‐INTERVENTIONS: Usual pre‐study interventions permitted (LABAs, oral ß2‐agonists, theophylline, leukotriene antagonists or lipoxygenase inhibitors). |
|
| Outcomes | FEV1; am PEF; symptoms; quality of life (AQLQ); exacerbations; withdrawal | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Bernstein 2004.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: Multicentre DURATION OF STUDY: 12 weeks (run‐in unclear) CONCEALMENT OF ALLOCATION: Not reported COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Not reported DESCRIPTION OF WITHDRAWALS/DROPOUTS: Not reported JADAD SCORE (5‐1): 2 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT(presumed) COMPLIANCE: Not reported CONFOUNDERS: Not reported. | |
| Participants | N SCREENED: Not reported
N RANDOMISED: 531
N COMPLETED: Not reported
M = unknown; F = unknown
MEDIAN AGE: Not reported
BASELINE DETAILS: Not reported
INCLUSION CRITERIA: Moderate‐severe asthma for 6 months or more; FEV1 of 40‐65%; age >= 12 years. EXCLUSION: unknown |
|
| Interventions | 1. Ciclesonide 200 mcg BID (CIC400)
2. Ciclesonide 400 mcg BID (CIC800)
3. Fluticasone 500 mcg BID (FP1000)
4. Placebo DELIVERY: CIC: MDI; FP CFC‐MDI TREATMENT PERIOD: 12 weeks RESCUE: unknown CO‐INTERVENTIONS PERMITTED: Not reported CO‐INTERVENTIONS: Not reported % on ICS baseline: Not reported |
|
| Outcomes | FEV1; am PEF; AQLQ symptom score; adverse events | |
| Notes | Unpublished conference abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Boulet 2006.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: Europe and Canada, 64 centres. DURATION OF STUDY: 12 weeks (2 week run‐in on usual dose of ICS, with high dose ICS during a post‐run in baseline period prior to study entry) CONCEALMENT OF ALLOCATION: Adequate COCHRANE QUALITY SCORE: DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Yes (computer generated list) METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: yes (double dummy) DESCRIPTION OF WITHDRAWALS/DROPOUTS: Yes JADAD SCORE (5‐1): 5 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not reported CONFOUNDERS: Baseline values showed older, more females, fewer non‐smokers, higher baseline dose of ICS, lower FEV1, and greater reversibility in BUD group | |
| Participants | N SCREENED: 688 N RANDOMISED: 359 N COMPLETED: 320 (PP) and 359 (ITT analysis) M = 148; F = 211 MEDIAN AGE (range): CIC320 39 years (12‐72); BUD320 42 (12‐71) BASELINE DETAILS: FEV1 (% Pred): CIC320 2.60 (81%); BUD320 2.43 (79%) INCLUSION CRITERIA: Aged 12‐75 years; persistent asthma for 6 months ATS definition; FEV1 of 65‐95% depending on ICS pretreatment at baseline of 320‐640 ug BUD and the addition of other controller meds (LABA, LTAs or equivalent). To enter treatment period patients had to also demonstrate improvement in FEV1 during pretreatment period of >= 7% or 150 mls following the increase in their daily ICS dose of 320‐640 ug BUD (or the equivalent) to 1280 mcg BUD. EXCLUSION: Concomitant severe diseases or contraindications to ICS use; abnormal lab tests suggesting disease; Use of systemic steroids within 4 weeks or injectable steroids within 6 weeks of baseline or more than 3 times within last 6 months or had an asthma exacerbation, LRTI or asthma hospitalisation within 4 weeks of baseline. Had other lung disease or COPD, or heavy smokers or ex‐smokers with smoking history >= 10 cigs per day or two pipes per day; suspected noncompliance; drug abuse;or pregnancy. | |
| Interventions | 1. Ciclesonide 400 mcg OD
2. Budesonide 400 mcg OD DELIVERY: CIC: HFA‐MDI (no spacer), BUD: Turbohaler in morning TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol MDI CO‐INTERVENTIONS PERMITTED: None % on ICS baseline: not indicated (but it would appear to be all patients) |
|
| Outcomes | FEV1; FVC; am PEF; pm PEF; clinic PEF; adverse events; exacerbations; withdrawals | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Boulet 2007.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 59 centres in North America, Europe, South Africa DURATION OF STUDY: 12 weeks (1‐4 week run in on usual steroid; non‐steroidal preventer medication was ceased) CONCEALMENT OF ALLOCATION: Adequate COCHRANE QUALITY SCORE: A DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Centralised, automated randomisation programme. METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double‐dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: Stated JADAD SCORE (5‐1): 5 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not reported CONFOUNDERS: Baseline values comparable. | |
| Participants | N SCREENED: Not clear (637 enrolled in run‐in period) N RANDOMISED: 474 (CIC: 234; FP: 240) N COMPLETED: 420 M = 182 F = 290 MEAN AGE: 39 years BASELINE DETAILS: Duration of symptoms: 15 years; allergic rhinitis: 23/35 participants INCLUSION CRITERIA: 12‐75 years; ATS defined asthma (6 months); constant dose and type of asthma medication in 4 weeks prior to run‐in; moderate asthma based on GINA 2002 classifications; FEV1 60‐80% predicted if managed with bronchodilators or non‐steroidal preventer medication; FEV1 > 80% predicted if treated with FP </= 250 mg/day or equivalent; FEV1 > 80% predicted and asthma symptoms in previous 7 days if treated with FP > 250 and <500 mg/day or equivalent; FEV1 > 85% predicted and asthma symptoms in previous 7 days if treated with FP </= 250 mg/day or equivalent in combination with LABA or theophylline treatment. Post‐run in criteria: Patients previously using bronchodilators or non‐steroidal preventer medication without concomitant ICS use had to have FEV1 60‐80% predicted and symptoms (total and nocturnal symptoms) during last 7 days of run‐in period; Patients previously using ICS had to have an FEV1 >80% predicted and nocturnal symptoms, asthma symptoms more than once but not daily, not used rescue medication daily; Reversibility demonstrated during the run‐in period (if not achieved then historical reversibility accepted). EXCLUSION: Clinically relevant abnormal laboratory values; use of systemic steroids in previous 4 weeks; pregnancy, breast feeding or not using reliable contraception; current/former smoking status of 10 or more cigarette pack years. | |
| Interventions | 1. Ciclesonide OD 400 mcg in evening (+ dummy DPI)
2. Fluticasone BID 200 mcg (+ dummy MDI) DELIVERY: CIC: MDI; FP: DPI TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: Not reported. CO‐INTERVENTIONS: Not listed. % on ICS pre‐baseline: 70 |
|
| Outcomes | FEV1 L; FEV1 predicted; FVC; am PEF; pm PEF; AQLQ; symptoms; adverse events; withdrawals | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Buhl 2006.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: Europe and South Africa, 57 centres. DURATION OF STUDY: 12 weeks (1‐4 week run‐in with suspension of usual ICS) CONCEALMENT OF ALLOCATION: Unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: yes appropriate (double dummy) DESCRIPTION OF WITHDRAWALS/DROPOUTS: Yes JADAD SCORE (5‐1): 4 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not reported CONFOUNDERS: Baseline values comparable. Note: Patients in two treatment groups were balanced with regard to prior use of ICS and other treatment medications (unclear how this was done). | |
| Participants | N SCREENED: 644 N RANDOMISED: 529 N COMPLETED: 451 (PP) but with 529 (ITT analysis) M = 224; F = 305 MEDIAN AGE (range): CIC160 41 years (12‐74); FP88 38 (12‐74) BASELINE DETAILS: FEV1 (% Pred): CIC160 2.383 (75%); FP88 2.440 (75%) INCLUSION CRITERIA: Aged 12‐75 years; persistent asthma for 6 months ATS definition; previous use of ICS for 6 months (constant dose up to 500 ug/day BDP or equivalent for 4 weeks and an FEV1 of 80‐100% pred. At randomisation patients were required to have FEV1 50‐90% after rescue was withheld for 4 hours and a decrease in FEV1 >= 10% after ICS withdrawal and a reversibility of FEV1 >= 15% after 2‐4 puffs salbutamol or a diurnal variation in PEF of 15% during baseline period. EXCLUSION: Use of systemic steroids within 4 weeks of baseline or more than 3 times within last 6 months or had an asthma exacerbation, LRTI or asthma hospitalisation within 4 weeks. Had other lung disease such as COPD, or significant smoking history >= 10 pack years. " | |
| Interventions | 1. Ciclesonide 200 mcg OD in evening (double dummy placebo)
2. Fluticasone 100 mcg BID DELIVERY: CIC: MDI, FP: HFA MDI TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol MDI CO‐INTERVENTIONS PERMITTED: None % on ICS baseline: 0 |
|
| Outcomes | FEV1; am PEF; rescue medication use; adverse events; withdrawals | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
BY9010/M1‐136.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: Korea, 16 centres DURATION OF STUDY: 12 weeks (4 weeks run‐in, prn SABA) CONCEALMENT OF ALLOCATION: unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: yes DESCRIBED AS DOUBLE BLIND: yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: not described METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: double dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: not stated JADAD SCORE (5‐1): 3 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Per protocol COMPLIANCE: not assessedCONFOUNDERS: not clear | |
| Participants | N SCREENED: Not reported N RANDOMISED: 249 N COMPLETED: not clear M = 39%; F = 61% MEDIAN AGE: 42 years BASELINE DETAILS: FEV1 79% predicted INCLUSION CRITERIA: 18‐75 years; ATS defined asthma; Korean descent; treatment with ICS (maximum FP250 mcg/d); FEV1 80‐105% predicted prior to run‐in (60‐90% post run‐in) EXCLUSION: not stated | |
| Interventions | 1. Ciclesonide 200 mcg OD 2. Budesonide 400 mcg OD DELIVERY: Ciclesonide: MDI; Budesonide: Turbohaler TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: prn SABA CO‐INTERVENTIONS: Not stated % on ICS at baseline: 100 | |
| Outcomes | FEV1; am & pm PEF; safety | |
| Notes | Unpublished data set available from http://www.clinicalstudyresults.org | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
BY9010/M1‐137.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 9 centres in Taiwan and Malaysia DURATION OF STUDY: 12 weeks (prn SABA) CONCEALMENT OF ALLOCATION: Not clear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double‐dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: Not reported JADAD SCORE (5‐1): 3 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Per protocol and ITT COMPLIANCE: Not assessed CONFOUNDERS: Groups balanced at baseline | |
| Participants | N SCREENED: Not reported N RANDOMISED: 125 N COMPLETED: Not reported M = not reported F = not reported MEAN AGE: 48 BASELINE DETAILS: FEV1 72% predicted INCLUSION CRITERIA: 18‐ 75 years; ATS defined asthma for at least 6 months; treatment with ICS for 4 weeks (maximum 250mcg fluticasone propionate or equivalent); FEV1 80‐105% of predicted. | |
| Interventions | 1. Ciclesonide 200 mcg OD
2. Budesonide 400 mcg OD DELIVERY: Ciclesonide: MDI; Budesonide: Turbohaler TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: prn SABA CO‐INTERVENTIONS: Not reported % on ICS at baseline: 100 |
|
| Outcomes | FEV1; FVC; symptoms; adverse events | |
| Notes | Unpublished data set available from http://www.clinicalstudyresults.org | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
BY9010/M1‐142.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 48 centres in Europe and Canada DURATION OF STUDY: 24 weeks CONCEALMENT OF ALLOCATION: Not clear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not clear METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: Not stated JADAD SCORE (5‐1): 3 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Per protocol and ITT COMPLIANCE: Not assessed CONFOUNDERS: Groups balanced at baseline | |
| Participants | N SCREENED: Not reported N RANDOMISED: 480 N COMPLETED: Not reported M = 190 F = 290 MEDIAN AGE: 42 years BASELINE DETAILS: 76% predicted INCLUSION CRITERIA: 12‐75 years; history of asthma for 6 months; treatment with ICS for 4 weeks (maximum daily dose of 250 mcg fluticasone propionate); FEV1: 80‐105% predicted EXCLUSION CRITERIA: Not reported | |
| Interventions | 1. Ciclesonide 100 mcg OD
2. Fluticasone 100 mcg BID DELIVERY: Ciclesonide: MDI; TREATMENT PERIOD: 24 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: prn SABA % on ICS at baseline: 100 |
|
| Outcomes | FEV1; FVC; am PEF; pm PEF; symptoms; adverse events | |
| Notes | Unpublished data set available from http://www.clinicalstudyresults.org | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Hansel 2006.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: Europe, 62 centres. DURATION OF STUDY: 12 weeks (1‐4 week run‐in on prn SABA) CONCEALMENT OF ALLOCATION: Not reported COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes to ciclesonide dose but open label for BUD (no BUD placebo available) METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Yes (computer generated randomisation list) METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Appropriate for CIC arms DESCRIPTION OF WITHDRAWALS/DROPOUTS: yes JADAD SCORE (5‐1): 5 (CIC v CIC); 3 (CIC v BUD) TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not reported CONFOUNDERS: Baseline values comparable | |
| Participants | N SCREENED: 684 N RANDOMISED: 554 N COMPLETED: 490 (64 withdrawn). 49 excluded from PP analysis (protocol violations) M = 301; F = 253 MEDIAN AGE (range): CIC80 38 years (12‐73); CIC320 41 (14‐74); BUD 45 (13‐73) BASELINE DETAILS: FEV1 (% Pred): CIC80 2.48 (73%); CIC320 2.46 (72%); BUD 2.42 (72%) INCLUSION CRITERIA: Aged 12‐75 years; mild to moderate persistent asthma of over 6 months duration according to ATS criteria including asthma symptoms and spontaneous fluctuations in obstruction. EXCLUSION: Oral or systemic steroid use within 4 weeks of screening or more than 3 times during preceding 6 months; inhaled daily dose of BDP > 500 ug or equivalent steroids within 4 weeks of screening, contraindication to inhaled corticosteroids use, hypersensitivity to study meds, asthma exacerbation or LRTI within 4 weeks of screening, COPD or other relevant respiratory disease, pregnancy, breast feeding, lack of contraceptive in women of child bearing potential, inability to follow study procedures, with clinically relevant lab values suggestive of disease. | |
| Interventions | 1. Ciclesonide 100 mcg OD
2. Ciclesonide 400 mcg OD
3. BUD 200 mcg BD (open labelled) DELIVERY: HFA‐MDI (CIC) and Turbohaler (BUD) TREATMENT PERIOD: 12 weeks RESCUE: SABA salbutamol or terbutaline CO‐INTERVENTIONS PERMITTED: rescue only (withdrawal if asthma exacerbation needing oral or systemic steroids, other ICS) % on ICS (pre‐run in): 0 |
|
| Outcomes | FEV1; am PEF; asthma symptom score, rescue medication use; adverse events; 24‐hour urinary cortisols (HPA‐axis) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Lee 2004.
| Methods | STUDY DESIGN: Crossover LOCATION, NUMBER OF CENTRES: Single centre in Scotland DURATION OF STUDY: 4 weeks CONCEALMENT OF ALLOCATION: Not reported COCHRANE QUALITY SCORE: DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double dummy (identical devices used). DESCRIPTION OF WITHDRAWALS/DROPOUTS: 9/28 JADAD SCORE (5‐1): 4 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Bonferroni correction set at 95% CI in order to obviate pairwise comparisons. COMPLIANCE: Not reported. CONFOUNDERS: Not reported. | |
| Participants | N SCREENED: Not reported. N RANDOMISED: 28 N COMPLETED: 19 M = 9 F = 10 MEAN AGE: 45 years BASELINE DETAILS: FEV1 predicted 84%; am PEF: 470 L/min; rescue medication usage: 0.2 puffs/d; AQLQ: 6.15 INCLUSION CRITERIA: Non‐smokers, mild‐moderate asthma; stable for three months prior to study entry; BDP equivalent 2000mcg/d (half of this if used in conjunction with additional controller therapy). EXCLUSION: Oral steroids or antibiotics in 3 months prior to study entry | |
| Interventions | 1. Ciclesonide 400mcg OD
2. Fluticasone 250mcg BID DELIVERY: CIC: HAD‐MDI; FP: Evohaler TREATMENT PERIOD: 2 x 4 week treatment periods RESCUE: Not clear. CO‐INTERVENTIONS PERMITTED: Montelukast and Salmeterol given during washout phase to prevent withdrawals. CO‐INTERVENTIONS: Montelukast and Serevent. % on ICS baseline: 100 |
|
| Outcomes | Methacholine challenge; FEV1; am PEF; pm PEF; symptoms; rescue medication; AQLQ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Lee 2005.
| Methods | STUDY DESIGN: Crossover. LOCATION, NUMBER OF CENTRES: One centre in Scotland. DURATION OF STUDY: 2 x 4 week treatment periods (2 week washout). CONCEALMENT OF ALLOCATION: Unclear. COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported. METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double dummy. DESCRIPTION OF WITHDRAWALS/DROPOUTS: 6/20 JADAD SCORE (5‐1): 4 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Bonferroni correction set at 95% CI in order to obviate pairwise comparisons. COMPLIANCE: 90% compliance required in order for data to be analysed. CONFOUNDERS: NA | |
| Participants | N SCREENED: Not reported N RANDOMISED: 20 N COMPLETED: 14 M = 9 F = 5 MEAN AGE: 47 BASELINE DETAILS: FEV1 2.44l; FEV1 predicted: 77%. INCLUSION CRITERIA: Non‐smokers with moderate persistent asthma; stable for three months prior to study entry; BDP equivalent 2000mcg/d (half of this if used in conjunction with additional controller therapy); 20% fall in FEV1 following < 0.4 mg/ml EXCLUSION: Oral steroids or antibiotics in 3 months prior to study entry | |
| Interventions | 1. Ciclesonide 800 mcg BID
2. Fluticasone 1000 mcg BID DELIVERY: CIC: HAD‐MDI; FP: Evohaler TREATMENT PERIOD: 2 x 4 week treatment periods RESCUE: Not clear. CO‐INTERVENTIONS PERMITTED: Montelukast and Salmeterol given during washout phase to prevent withdrawals. CO‐INTERVENTIONS: Montelukast and Serevent. % on ICS baseline: 100 |
|
| Outcomes | HPA axis; FEV1; methacholine challenge; am PEF; pm PEF; asthma symptoms; rescue medication puffs/d; AQLQ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Lipworth 2005.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: USA, 20 centres. DURATION OF STUDY: 12 weeks (no run‐in described) CONCEALMENT OF ALLOCATION: Unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Identical inhaler devices DESCRIPTION OF WITHDRAWALS/DROPOUTS: Reported JADAD SCORE (5‐1): 3 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Similar across treatment groups (assessed by canister weight) CONFOUNDERS: Baseline characteristics comparable. | |
| Participants | N SCREENED: Not reported. N RANDOMISED: 164 N COMPLETED: 148 M= 79; F= 85 MEAN AGE: 37 BASELINE DETAILS: FEV1: 3L; FEV1 predicted: 81% INCLUSION CRITERIA: >/‐18 years; mild to moderate persistent asthma; acceptable inhaler technique; SABA only for 6 months (at least 2 x daily); FEV1 >/=70% predicted. Females taking oral contraceptives and HRT were required to have an increase in serum cortisol levels of 7mcg/dL or greater from basal to peak levels. EXCLUSION: Systemic steroid use within 6 months of screening; inhaled steroids within 2 months. | |
| Interventions | 1. Ciclesonide 400mcg OD
2. Ciclesonide 400mcg BID
3. Fluticasone 500mcg BID
4. Placebo DELIVERY: CIC: HFA MDI without a spacer; FP: CFC MDI without a spacer. TREATMENT PERIOD: 12 weeks RESCUE: Not reported CO‐INTERVENTIONS PERMITTED: None permitted % on ICS baseline: 0 |
|
| Outcomes | Hypothalmic pituitary axis function; serum cortisol; safety | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Magnussen 2007.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: Europe, number of centres not reported DURATION OF STUDY: 12 weeks (1‐4 weeks prn SABA) CONCEALMENT OF ALLOCATION: Unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Both treatments given via MDIs DESCRIPTION OF WITHDRAWALS/DROPOUTS: Stated JADAD SCORE (5‐1): 4 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT and PP COMPLIANCE: Not reported CONFOUNDERS: Balanced groups at baseline | |
| Participants | N SCREENED: Not reported N RANDOMISED: 808 N COMPLETED: 764 M = 409; F = 398 MEDIAN AGE: 29‐33 BASELINE DETAILS: FEV1 predicted: 79%; reversibility: 25% INCLUSION CRITERIA: ATS defined asthma; 12‐75 years; 61‐90% predicted (if treated with ICS), or 61‐105% predicted if not treated with ICS; maximum daily dose was FP 250 mcg; post‐run in participants had to demonstrate FEV1 between 60‐90% predicted. EXCLUSION: Concomitant severe disease; smoking history of >10 pack years; LABA or OCS treatment in previous 4 weeks. | |
| Interventions | 1. Ciclesonide 100 mcg OD
2. Ciclesonide 200 mcg OD
3. Fluticasone 100 mcg BID DELIVERY: MDI TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: Not reported CO‐INTERVENTIONS: Not reported % on ICS: Not reported |
|
| Outcomes | FEV1; peak flow; asthma symptoms; asthma exacerbations requiring oral steroids | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Niphadkar 2005a.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: India, 11 centres DURATION OF STUDY: 12 weeks (2 week run‐in on BUD 400 mcg/d) CONCEALMENT OF ALLOCATION: Adequate. COCHRANE QUALITY SCORE: A DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Computer‐generated randomisation schedule. METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double‐dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: Reported JADAD SCORE (5‐1): 5 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not assessed CONFOUNDERS: Baseline characteristics similar. | |
| Participants | N SCREENED: Not reported N RANDOMISED: 473 participants enrolled (405 randomised, 403 received treatment: CIC160 am: 140; CIC160 pm: 131; BUD200: 134) N COMPLETED: 370 M = 213; F = 190 MEDIAN AGE: 31 BASELINE DETAILS: FEV1: 2.2L; FEV1 predicted: 93%; PEF: 320L/min. Concomitant therapy: LABA: 105; Xanthines: 62; ICS and LABA (separate): 54; antihistamine: 37; nasal steroids: 24. INCLUSION CRITERIA: 18‐69 years; diagnosis of persistent asthma (at least 6 months); maintenance ICS (BDP equivalent up to 500mcg/d); FEV1 predicted >/=70%. Post‐run in phase, participants were required to have stable asthma (low variation in PEF; no more than four puffs of rescue medication on more than two consecutive days). EXCLUSION: Use of systemic steroids, asthma exacerbation or hospitalisation with asthma in 4 weeks before study entry; COPD; pregnancy/lactation. | |
| Interventions | 1. Ciclesonide 200 mcg OD (am)
2. Budesonide 200 mcg BID DELIVERY: HFA‐MDI TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: LABAs, oral beta‐agonists, leukotriene agents, theophylline, SCG, nedocromil. CO‐INTERVENTIONS: Not reported % on ICS: 100 |
|
| Outcomes | FEV1; FVC; am PEF; pm PEF; symptoms; rescue medication use; withdrawals; adverse events | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Niphadkar 2005b.
| Methods | See above. | |
| Participants | See above. | |
| Interventions | 1. Ciclesonide 200 mcg OD (pm)
2. Budesonide 200 mcg BID See above |
|
| Outcomes | FEV1; FVC; am PEF; pm PEF; symptoms; rescue medication use; withdrawals; adverse events | |
| Notes | Created as secondary reference to Niphadkar 2005 (am) due to additional treatment arm in this trial (pm administration of ciclesonide) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pedersen 2006.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 51 centres in Europe, South Africa and Canada. DURATION OF STUDY: 12 weeks (2‐4 week run in on prn SABA) CONCEALMENT OF ALLOCATION: Adequate COCHRANE QUALITY SCORE: A DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Computer‐generated randomisation schedule from manufacturer. METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Identical inhaler devices. DESCRIPTION OF WITHDRAWALS/DROPOUTS: Not reported JADAD SCORE (5‐1): 4 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not assessed CONFOUNDERS: Baseline characteristics comparable. | |
| Participants | N SCREENED: Not reported N RANDOMISED: 728 (N meeting post‐run in criteria and subsequently analysed: 556. Baseline details given for per‐protocol set. CIC: 277; FP279) N COMPLETED: Not reported. M = 331; F = 180 MEDIAN AGE: 10 BASELINE DETAILS: Add‐on therapy prior to baseline: 147; ICS therapy prior to baseline: 332; mean ICS dose: 390mcg/d; FEV1: 1.7L; FEV1 predicted: 80%; am PEF: 257L; Mean FEV1 reversibility: 20% INCLUSION CRITERIA: 6‐15 years; persistent asthma for at least six months (ATS criteria); clinically stable for four weeks prior to study entry; FEV1 predicted: 50‐90% rescue medication only, 80‐100% in patients treated with ICS only; symptom score >1 on 6 of last 10 days of run in; adequate MDI inhaler device technique without spacer. EXCLUSION: History of life‐threatening asthma; two or more inpatient hospitalisations in previous year; >60 days of systemic steroids in past year >400mcg BUD or equivalent/d in 30 days prior to baseline; >8 puffs SABA/d for three consecutive days during run‐in." | |
| Interventions | 1. Ciclesonide 100 mcg BID
2. Fluticasone 100 mcg BID DELIVERY: HFA‐MDI TREATMENT PERIOD: 12 weeks (2‐4 week run‐in) RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: Not reported. CO‐INTERVENTIONS: Not listed % on ICS (pre‐baseline): 65% |
|
| Outcomes | FEV1; clinic PEF; am PEF; pm PEF; symptoms; rescue medication usage; adverse events | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Ukena 2006.
| Methods | STUDY DESIGN: Parallel group. LOCATION, NUMBER OF CENTRES: 43 centres in three countries in Western Europe DURATION OF STUDY: 12 weeks (1‐4 weeks run‐in on prn SABA) CONCEALMENT OF ALLOCATION: Unclear. COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported. METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double‐dummy. DESCRIPTION OF WITHDRAWALS/DROPOUTS: Reported JADAD SCORE (5‐1): 4 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT COMPLIANCE: Not assessed. CONFOUNDERS: Baseline characteristics comparable. | |
| Participants | N SCREENED: Not reported. N RANDOMISED: 437 (ITT based on 399 participants: CIC: 198; BUD: 201) N COMPLETED: 371 M = 183; F = 216 MEDIAN AGE: 45 BASELINE DETAILS: FEV1 L: 2.33; FEV1 predicted: 72%; am PEF predicted: 78%; PEF variability: 12% INCLUSION CRITERIA: 12‐75 years; asthma for at least six months (ATS criteria); </= 500 mcg/d BDP equivalent; stable regimen of additional anti‐asthma medication if this was used; participants on prn SABA were allowed to participate. Post‐run in period: FEV1: 50‐90% predicted; Participants treated with ICS had to demonstrate a fall in FEV1 predicted of >/=10%; reversibility if >/= 15% FEV1 post‐SABA. EXCLUSION: Exacerbation/lower RTI in four weeks prior to randomisation. | |
| Interventions | 1. Ciclesonide 400 mcg OD
2. Budesonide 400 mcg OD DELIVERY: CIC: HFA‐MDI; BUD: DPI TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: leukotriene agents, theophyllines CO‐INTERVENTIONS: Not listed % on ICS: 38% pre‐treated with ICS |
|
| Outcomes | FEV1; FVC; clinic PEF; am PEF; pm PEF; symptoms; rescue medication use; adverse events | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Vermeulen 2007.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 31 centres in Europe and South Africa DURATION OF STUDY: 12 weeks (2 week baseline period – BUD 400 mcg/d) CONCEALMENT OF ALLOCATION: Adequate COCHRANE QUALITY SCORE: A DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Computer‐generated randomisation schedule METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: Stated JADAD SCORE (5‐1): 5 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT and per protocol COMPLIANCE: Not reported CONFOUNDERS: Groups balanced at baseline | |
| Participants | N SCREENED: 431 N RANDOMISED: 403 (CIC: 272; BUD: 131) N COMPLETED: 384 M = 272; F = 131 MEDIAN AGE: 14 BASELINE DETAILS: FEV1 73% predicted INCLUSION CRITERIA: 12‐17 years old; FEV1 50‐80% predicted; severe asthma (GINA 2003 definition); Not well controlled after constant treatment with fixed dose BUD 400 mg/day (or equivalent) 4 weeks prior to study entry with FEV1 45% to 80% predicted; Alternatively constant treatment with fixed dose BUD 400 to 800 mg/day (or equivalent) 4 weeks prior to study entry, with FEV1 46% to 85% predicted; Entry into treatment period at randomization (baseline), FEV1 50% to80% predicted, FEV1 reversibility > 15% salbutamol. EXCLUSION: Oral steroids within 4 weeks of study entry; concomitant severe diseases; relevant lung diseases or clinically relevant abnormal laboratory values; > 10 cigarette pack‐year smoking history; females of child‐bearing potential without contraception. | |
| Interventions | 1. Ciclesonide 400 mcg OD
2. Budesonide 800 mcg OD DELIVERY: HFA‐MDI (CIC); DPI (BUD) TREATMENT PERIOD: 12 weeks RESCUE: Not reported CO‐INTERVENTIONS PERMITTED: Not reported CO‐INTERVENTIONS: Not reported % on ICS: 100 |
|
| Outcomes | FEV1; PEF; 24hr urinary free concentrations | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
von Berg 2007.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: 59 centres in Europe and South Africa DURATION OF STUDY: 12 weeks (2‐4 run in period prn SABA only) CONCEALMENT OF ALLOCATION: Unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Not reported DESCRIPTION OF WITHDRAWALS/DROPOUTS: Stated JADAD SCORE (5‐1): 3 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): ITT and per protocol. COMPLIANCE: Not reported. CONFOUNDERS: Not reported. | |
| Participants | N SCREENED: 774 N RANDOMISED: 621 (CIC: 416; BUD: 205) N COMPLETED: M = 395; F = 226 MEAN AGE: 9 years BASELINE DETAILS: FEV1 78% predicted; ICS treatment: 51% INCLUSION CRITERIA: 6‐11 years; diagnosis of persistent asthma for 6 months; FEV1 >50% to 90% predicted if rescue medication only, >50% to 100% predicted if using constant dose of controller medication other than steroids for 1 month; 80% to 105% predicted if using </=400 mcg/d BDP equivalent for 1 month before inclusion. Post‐run‐in: FEV1 50‐90% predicted after withholding SABA for at least four hours; reversibility of FEV1 >12% of initial post‐SABA; asthma symptom scores >1 on at least six of previous 10 days or use of >8 puffs of rescue medication during the previous 10 days. EXCLUSION: History of life‐threatening asthma, concomitant severe diseases; two or more hospitalizations for asthma within previous 12 months; asthma exacerbation during four weeks before baseline; systemic corticosteroids during 30 days before baseline; use of systemic steroids for more than 60 days within the previous 2 years; participation in another study within 30 days before baseline. No other asthma medication permitted during study. | |
| Interventions | 1. Ciclesonide 200 mcg OD
2. Budesonide 400 mcg OD DELIVERY: CIC: HFA‐MDI (+ Aerochamber); BUD: DPI. TREATMENT PERIOD: 12 weeks RESCUE: Not reported CO‐INTERVENTIONS PERMITTED: None CO‐INTERVENTIONS: NA % on ICS: Not reported. 52 |
|
| Outcomes | FEV1; Peak flow; asthma symptoms; rescue medication; bone growth; 24hr urinary cortisol; adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Zietkowski 2006.
| Methods | STUDY DESIGN: Parallel group LOCATION, NUMBER OF CENTRES: One centre in Poland. DURATION OF STUDY: 12 weeks (1‐4 week run in on prn SABA) CONCEALMENT OF ALLOCATION: Unclear COCHRANE QUALITY SCORE: B DESCRIBED AS RANDOMISED: Yes DESCRIBED AS DOUBLE BLIND: Yes METHOD OF RANDOMISATION WELL DESCRIBED/APPROPRIATE: Not reported METHOD OF BLINDING WELL DESCRIBED/APPROPRIATE: Double‐dummy DESCRIPTION OF WITHDRAWALS/DROPOUTS: Not reported JADAD SCORE (5‐1): 3 TYPE OF ANALYSIS (AVAILABLE CASE/TREATMENT RECEIVED/ ITT): Assumed available case. COMPLIANCE: Not reported CONFOUNDERS: Baseline values comparable. | |
| Participants | N SCREENED: Not clear N RANDOMISED: 35 (CIC80: 12; CIC160: 12; FP200: 11) N COMPLETED: 35 M = 19; F = 16 MEAN AGE: 45 years BASELINE DETAILS: Duration of symptoms: 15 years; allergic rhinitis: 23/35 participants INCLUSION CRITERIA: Mild allergic asthma (according to GINA guidelines); free from exacerbations in previous four weeks; non‐smokers; treatment with FP equivalent 250mcg/d. EXCLUSION: Not reported. | |
| Interventions | 1. Ciclesonide 100 mcg OD
2. Ciclesonide 200 mcg OD
3. Fluticasone 100 mcg BID DELIVERY: unclear TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol CO‐INTERVENTIONS PERMITTED: Not reported. CO‐INTERVENTIONS: Not listed. % on ICS pre‐baseline: 100. |
|
| Outcomes | FEV1 L; FEV1 predicted; symptoms; rescue medication use | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
AQLQ: Asthma quality of life questionnaire; ATS: American Thoracic Society; BDP: beclomethasone dipropionate; BID: twice daily; BUD: budesonide; CFC‐MDI: Chlorofluorocarbon metered dose inhaler; CIC: Ciclesonide; COPD: Chronic obstructive pulmonary disease; DPI: Dry powder inhaler device; FEV1: forced expiratory volume in one second; FP: fluticasone propionate; FVC: forced vital capacity; GINA: Global initiative for asthma; HFA‐MDI: Hydro‐fluoroalkane metered dose inhaler; HPA: hypothalamic‐pituitary‐adrenal; ICS: inhaled corticosteroids; ITT: intention‐to‐treat; LABA: Long‐acting beta2‐agonist; MDI: metered dose inhaler; OCS: oral corticosteroids; OD: once daily; PEF: peak expiratory flow; PP: per‐protocol; RTI: respiratory tract‐infection; SABA: short‐acting beta‐agonist; SCG: sodium cromoglycate
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agertoft 2005 | Treatment < 4 weeks |
| Bethke 2002 | Healthy volunteers |
| Dahl 1998 | Treatment < 4 weeks |
| Derom 2005 | Treatment < 4 weeks |
| Drollman 2004 | Treatment < 4 weeks |
| Erin 2005 | Treatment < 4 weeks |
| Gauvreau 2005 | Treatment < 4 weeks |
| Kanniess 2001 | Treatment < 4 weeks |
| Larsen 2003 | Treatment < 4 weeks |
| Postma 2001 | Morning versus evening administration |
| Richter 2005 | Treatment < 4 weeks |
| Subbarao 2006 | Treatment < 4 weeks |
| Szefler 2005 | Inpatient administration |
| Taylor 1999 | Treatment < 4 weeks |
Characteristics of ongoing studies [ordered by study ID]
Arshad.
| Trial name or title | An assessment of safety and efficacy in treating moderate to severe asthmatics with inhaled Ciclesonide vs Fluticasone |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Beck.
| Trial name or title | Efficacy and safety of ciclesonide administered with or without different spacers in patients with asthma (12 to 75 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Beckman.
| Trial name or title | Efficacy of ciclesonide inhaled once daily versus other corticosteroids used for treatment of mild asthma in children (4‐11 ys ). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Colatruglio.
| Trial name or title | Effect of ciclesonide on quality of life in patients with moderate persistent asthma (21 to 65 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Dahl.
| Trial name or title | Efficacy of ciclesonide versus fluticasone propionate inpatients with mild to moderate asthma (12 to 75 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Derom.
| Trial name or title | Effect of inhaled ciclesonide versus fluticasone propionate in patients with mild to moderate asthma (18 to 65 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Dusser.
| Trial name or title | Efficacy of ciclesonide and fluticasone propionate in adult patients with moderate and severe persistent asthma (18 to 75 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Engelstätter.
| Trial name or title | Efficacy of ciclesonide inhaled once daily versus fluticasone propionate inhaled twice daily in children with asthma (4 to 15 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Giwa.
| Trial name or title | Comparison of inhaled ciclesonide and fluticasone proprionate in moderate to severe asthma patients, well controlled under high doses of inhaled corticosteroids |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Hansel.
| Trial name or title | A 3‐period double‐blind, cross‐over study on the onset of action of inhaled ciclesonide on airway responsiveness to adenosine monophosphate, sputum eosinophils and exhaled breath NO in patients with asthma |
| Methods | |
| Participants | Outpatients of either sex who are between 18‐45 years with a history of atopic disease, who have a history of perennial bronchial asthma for at least 6 months as defined by ATS criteria (increased responsiveness to a variety of stimuli; symptoms like dyspnoe, wheezing and cough of varying degree; spontaneous fluctuations in the severity of obstruction with substantial improvements following bronchodilators or corticosteroids (American Thoracic Society, 1987) |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
O'Byrne.
| Trial name or title | Efficacy of ciclesonide vs fixed combination of fluticasone propionate/salmeterol vs placebo in patients with mild persistent asthma (12 to 75 y). Clinicaltrials.Gov. 2005. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Park.
| Trial name or title | Effectiveness of ciclesonide versus budesonide in patients with asthma (18 to 75 y). Clinicaltrials.Gov. 2005 |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Sanofi Aventis.
| Trial name or title | Effects of ciclesonide and beclomethasone on lens opacification in adult participants with moderate to severe persistent asthma. Clinicaltrials.Gov . 2005; Efficacy of ciclesonide vs. placebo administered as once daily or twice daily in patients not treated with inhaled corticosteroid. Clinicaltrials.Gov. 2005; Effects of ciclesonide MDI 50 mg/day and 200 mg/day (ex‐value) once‐daily on growth in children with mild persistent asthma. Clinicaltrials.Gov. 2005; Sanofi‐Aventis. Dose response study of inhaled ciclesonide (glucocorticosteroid) to patients with persistent asthma. Clinicaltrials.Gov. 2005. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Stenton.
| Trial name or title | A double‐blind randomised parallel group study comparing the efficacy and safety of 800 and 1000 mcg CIC/day in patients with asthma followed by an open long‐term study to assess the safety of CIC in patients with asthma |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
ATS: vs: versus y: years
Contributions of authors
PM: initiation of protocol; assessment of studies, data extraction, write‐up TL: Assessment of studies, data extraction, data entry & analysis, write‐up PG: Protocol development, write‐up, contact editor
Sources of support
Internal sources
No sources of support supplied
External sources
Cochrane Fellowship from the Health Research Board, Ireland.
Declarations of interest
None declared.
Edited (no change to conclusions)
References
References to studies included in this review
Adachi 2007 {published data only}
- Adachi M, Ishihara K, Inoue H, Kudo K, Takahashi K, Morita Y, et al. Efficacy and safety of once‐daily inhaled ciclesonide in adults with mild to moderate asthma: A double‐blind, placebo‐controlled study. Respirology 2007;12(4):566‐72. [DOI] [PubMed] [Google Scholar]
Adler 2006 {published data only}
- Adler M, Langan J, Martinot JB, Croonenborghs L, Gruss C, Oedekoven C. Ciclesonide 160 mcg once daily compared with fluticasone propionate 250 mcg twice daily in maintenance therapy of patients with stable asthma. European Respiratory Journal 2006;28(Suppl 50):205s. [Google Scholar]
Bateman 2007 {published data only}
- Bateman ED, Langan J, Vereecken G, Smau L, Engelstatter R. Efficacy and tolerability of ciclesonide compared with fluticasone propionate in patients with moderate‐to‐severe asthma. American Thoracic Society Annual Conference, San Francisco, USA. 2006:A103.
- Bateman ED, Linnhof AE, Homik L, Freudensprung U, Smau L, Engelstatter R. Comparison of twice‐daily inhaled ciclesonide and fluticasone propionate in patients with moderate‐to‐severe persistent asthma. Pulmonary Pharmacology & Therapeutics 2007;Epub ahead of print. [doi:10.1016/j.pupt.2007.05.002] [DOI] [PubMed] [Google Scholar]
Bernstein 2004 {unpublished data only}
- Bernstein D, Berger W, Welch M, Kundu S, Banerji D. Once‐daily ciclesonide significantly improves pulmonary function in adults/adolescents with mild‐moderate asthma. American Thoracic Society 2005 International Conference; May 20‐25; San Diego, California. 2005:B35; poster: G27.
- Bernstein D, Nathan R, Ledford D, Ledoux E, Pedinoff A, Crivera C, et al. Ciclesonide, a new inhaled corticosteroid, significantly improves asthma‐related quality of life in patients with severe, persistent asthma. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S210. [Google Scholar]
- Bernstein JA, Noonan MJ, Rim C, Fish J, Kundu S, Williams J, et al. Ciclesonide has minimal oropharyngeal side effects in the treatment of patients with moderate‐to‐severe asthma. Journal of Allergy and Clinical Immunology 2004;113(2 Suppl):S113. [Google Scholar]
- Busse W, Kaliner M, Bernstein D, Nayak A, Kundu S, Williams J. The novel inhaled corticosteroid ciclesonide is effacious and has a favourable safety profile in adults and adolescents with severe persistent asthma. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S213. [Google Scholar]
- Weinstein S, Friedman B, Kundu S, Banerji D. Ciclesonide is effective and well tolerated in adults/adolescents with severe persistent asthma. American Thoracic Society 2005 International Conference; May 20‐25 San Diego, California. 2005.
Boulet 2006 {published and unpublished data}
- Boulet LP, Drollmann A, Magyar P, Timar M, Knight A, Engelstätter R, et al. Comparative efficacy of once‐daily ciclesonide and budesonide in the treatment of persistent asthma. Repiratory Medicine 2006;100(5):785‐94. [DOI] [PubMed] [Google Scholar]
- Boulet LP, Engelstatter R, Magyar P, Timar M, Knight A, Fabbri L. Ciclesonide is at least as effective as budesonide in the treatment of patients with bronchial asthma. American Thoracic Society 99th International Conference. 2003:C105; Poster D63.
Boulet 2007 {published data only}
- Boulet LP, Bateman ED, Voves R, Müller T, Wolf S, Engelstätter R. A randomized study comparing ciclesonide and fluticasone propionate in patients with moderate persistent asthma. Respiratory Medicine 2007;In press. [DOI] [PubMed] [Google Scholar]
Buhl 2006 {published data only}
- Buhl R, Vinkler I, Magyar P, Gyori Z, Rybacki C, Middle MV, et al. Comparable efficacy of ciclesonide once daily versus fluticasone propionate twice daily in asthma. Pulmonology Pharmacology and Therapeutics 2006;19:404‐12. [DOI] [PubMed] [Google Scholar]
- Buhl R, Vinkler I, Magyar P, Rybacki C, Middle MV, Escher A, et al. Once daily ciclesonide is as effective as fluticasone proprionate given twice daily in treating patients with asthma. American Thoracic Society 100th International Conference, May 21‐26, 2004, Orlando. 2004:A37; Poster J111.
- Buhl R, Vinkler I, Magyar P, Rybacki C, Middle V, Wolf S, et al. Once daily ciclesonide and twice daily fluticasone propinate are equally effective in the treatment of patients with asthma. European Respiratory Journal 2004;24(Suppl 48):347s. [Google Scholar]
- Buhl R, Wolf S, Engelstätter R. Once daily ciclesonide is comparable to twice daily fluticasone propionate in the treatment of patients with asthma. Respirology 2005;10(Suppl):A26. [Google Scholar]
- Buhl R, Wolf S, Tiesler C, Escher A, Weber HJ. Once‐daily ciclesonide is as effective as twice‐daily fluticasone propionate in improving lung function in patients with mild‐to‐moderate persistent asthma. American Thoracic Society 2005 International Conference; May 20‐25; San Diego, California. 2005:B35; Poster: G19.
- Buhl R, Wolf S, Tiesler C, Excher A, Engelstatter R. Once daily ciclesonide is as effective as twice daily fluticasone propionate in improving lung function in patients with asthma. Thorax 2004;59(Suppl II):ii71. [Google Scholar]
BY9010/M1‐136 {unpublished data only}
- Altana pharma. A comparative study of inhaled ciclesonide 160 mcg/day versus budesonide 400 mcg/day in patients with asthma. http://www.clinicalstudyresults.org/documents/company‐study_2484_0.pdf Accessed 17 October 2007.
BY9010/M1‐137 {unpublished data only}
- Altana pharma. A comparative study of inhaled ciclesonide 160 mcg/day versus budesonide 400 mcg/day in patients with asthma. http://www.clinicalstudyresults.org/documents/company‐study_2485_0.pdf Accessed 17 October 2007.
BY9010/M1‐142 {unpublished data only}
- Altana Pharma. Comparison of ciclesonide (80 mcg once daily in the evening) and fluticasone propionate (100 mcg twice daily) in patients with mild to moderate asthma. http://www.clinicalstudyresults.org/documents/company‐study_2758_0.pdf issue Accessed 17 October 2007.
Hansel 2006 {published data only}
- Engelstätter R, Benezet O, Kafe H, Ponitz HH, Hansel T, Cheung D, et al. Comparative study in asthma patients treated with inhaled ciclesonide (80 µg or 320 µg once daily) or budesonide (200 µg twice daily) for 12 weeks. American Thoracic Society 99th International Conference. 2003; Vol. C105:D64.
- Hansel T, Biberger C, Engelstätter R. Ciclesonide 80 µg or 320 µg once daily achieves lung function improvement comparable with budesonide 200 µg twice daily in patients with persistent asthma. Thorax 2004;59(Suppl II):ii71. [Google Scholar]
- Hansel T, Engelstatter R, Benezet O, Kafe H, Ponitz HH, Cheung D, et al. Once daily ciclesonide (80 ug or 320 ug) is equally effective as budesonide 200 ug given twice daily: a 12 week study in asthma patients. European Respiratory Journal 2003;22(Suppl 45):Abstract No: P2639. [Google Scholar]
- Hansel TT, Benezet O, Kafe H, Ponitz HH, Cheung D, Engelstatter R, et al. A multinational, 12‐week, randomized study comparing the efficacy and tolerability of ciclesonide and budesonide in patients with asthma. Clinical Therapeutics 2006;28(6):906‐20. [DOI] [PubMed] [Google Scholar]
Lee 2004 {published data only}
- Fardon TC, Lee DK, Gray RD, Currie GP, Haggart K, Bates CE, et al. Effects of hydrofluoralkane formulations of ciclesonide 320µg once daily versus fluticasone propionate 220µg twice daily on methacholine hyperresponsiveness in mild‐to‐moderate persistent asthma. Journal of Allergy and Clinical Immunology 2004;113(2 Suppl):S119. [Google Scholar]
- Lee DK, Haggart K, Currie GP, Bates CE, Lipworth BJ. Effects of hydrofluoroalkane formulations of ciclesonide 400 microg once daily versus fluticasone 250 microg twice daily on methacholine hyper‐responsiveness in mild‐to‐moderate persistent asthma. British Journal of Clinical Pharmacology 2004;58(1):26‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2005 {published data only}
- Lee DK, Fardon TC, Bates CE, Haggart K, McFarlane LC, Lipworth BJ. Airway and systemic effects of hydrofluoroalkane formulations of high‐dose ciclesonide and fluticasone in moderate persistent asthma. Chest 2005;127(3):851‐60. [DOI] [PubMed] [Google Scholar]
- Lee DK, Lipworth BJ. Relative airway and systemic effects of high dose ciclesonide and fluticasone propionate in asthma. Thorax 2004;59(Suppl II):ii11. [Google Scholar]
Lipworth 2005 {published data only}
- LaForce CF, Baker JW, Amin D, Rohatagi S, Mendes P, Williams J, et al. Ciclesonide a novel inhaled steroid has no effect on hypothalamic pituitary adrenal (HPA) ‐ axis function in mild to moderate asthmatics. Journal of Allergy and Clinical Immunology 2003;111(2 Suppl):S218. [Google Scholar]
- Lipworth BJ, Kaliner MA, LaForce CF, Baker JW, Kaiser HB, Amin D, et al. Effect of ciclesonide and fluticasone on hypothalamic‐pituitary‐adrenal axis function in adults with mild‐to‐moderate persistent asthma. Annals of Allergy, Asthma and Immunology 2005;94(4):465‐72. [DOI] [PubMed] [Google Scholar]
Magnussen 2007 {published data only}
- Magnussen H, Hellwig M, Hellbradt S, Josten JP, Engelstätter R. Ciclesonide 80 ug or 160 ug once‐daily and fluticasone propionate 88 ug twice‐daily similarly reduce asthma symptoms and rescue medication use in patients with mild‐to‐moderate asthma. American Thoracic Society 2005 International Conference; May 20‐25; San Diego, California. 2005:B35; Poster: G20.
- Magnussen H, Hofman J, Novakova B, Kaczmarek B, Hellwig M, Engelstätter R. Ciclesonide 80 µg or 160 µg once daily is comparable to fluticasone propionate 88 µg twice daily in the treatment of asthma patients. European Respiratory Journal 2005;26(Suppl 49):255s. [Google Scholar]
- Magnussen H, Hofman J, Novakova B, Kaczmarek B, Hellwig M, Engelstätter R. Ciclesonide decreases exhaled breath nitric oxide and rapidly reduces airway responsiveness to adenosine monophosphate in asthma patients. European Respiratory Journal 2005;26(Suppl 49):Abstract No. 1723. [Google Scholar]
- Magnussen H, Hofman J, Novakova B, Kaczmarek‐Czeczothka B, Koci T, Staneta P, et al. Ciclesonide 80 µg or 160 µg once‐daily is as effective as fluticasone propionate 88 µg twice‐daily in the treatment of persistent asthma. Journal of Allergy and Clinical Immunology 2005;115(2 Suppl):S4. [Google Scholar]
- Magnussen H, Hofman J, Novokova B, Kaczmarek B, Schutze J, Hellwig M. Once daily ciclesonide 80 µg or 160 µg is comparable to twice daily fluticasone propionate 88 µg in the treatment of persistent asthma. XIX World Allergy Organization Congress; Munich, Germany. 2005:Abstract 297.
- Magnussen H, Hofman J, Staneta P, Lawo JP, Hellwig M, Engelstatter R. Similar efficacy of ciclesonide once daily versus fluticasone propionate twice daily in patients with persistent asthma. Journal of Asthma 2007;44(7):555‐63. [DOI] [PubMed] [Google Scholar]
Niphadkar 2005a {published data only}
- Gadgil DA, Niphadkar P, Jagannath KT, Joshi JM, Awad N, Chhabra SK, et al. Once‐daily ciclesonide is as effective as twice‐daily budesonide in maintaining lung function and asthma control in patients with asthma. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S3. [Google Scholar]
- Niphadkar P, Jagannath K, Joshi JM, Awad N, Boss H, Hellbardt S, et al. Comparison of the efficacy of ciclesonide 160 microg QD and budesonide 200 microg BID in adults with persistent asthma: a phase III, randomized, double‐dummy, open‐label study. Clinical Therapeutics 2005;27(11):1752‐63. [DOI] [PubMed] [Google Scholar]
- Niphadkar P, Jagannath KT, Helbardt S, Engelstatter R. Comparable efficacy of ciclesonide 160 µg once daily and budesonide 200 µg twice daily in patients with asthma. European Respiratory Journal. 2005; Vol. 26, issue Suppl 49:Abstract No. 1734.
- Niphadkar P, Jagannath KT, Joshi JM, Eckert J, Hellbardt S. Efficacy of ciclesonide 160 µg once daily is comparable to budesonide 200 µg twice daily in treating patients with asthma. XIX World Allergy Organization Congress; Munich, Germany. 2005.
Niphadkar 2005b {published data only}
- Gadgil DA, Niphadkar P, Jagannath KT, Joshi JM, Awad N, Chhabra SK, et al. Once‐daily ciclesonide is as effective as twice‐daily budesonide in maintaining lung function and asthma control in patients with asthma. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S3. [Google Scholar]
- Niphadkar P, Jagannath K, Joshi JM, Awad N, Boss H, Hellbardt S, et al. Comparison of the efficacy of ciclesonide 160 microg QD and budesonide 200 microg BID in adults with persistent asthma: a phase III, randomized, double‐dummy, open‐label study. Clinical Therapeutics 2005;27(11):1752‐63. [DOI] [PubMed] [Google Scholar]
- Niphadkar P, Jagannath KT, Helbardt S, Engelstatter R. Comparable efficacy of ciclesonide 160 µg once daily and budesonide 200 µg twice daily in patients with asthma. European Respiratory Journal. 2005; Vol. 26, issue Suppl 49:Abstract No. 1734.
- Niphadkar P, Jagannath KT, Joshi JM, Eckert J, Hellbardt S. Efficacy of ciclesonide 160 µg once daily is comparable to budesonide 200 µg twice daily in treating patients with asthma. XIX World Allergy Organization Congress; Munich, Germany. 2005.
Pedersen 2006 {published data only}
- Pedersen S, Garcia‐Garcia ML, Manjra A, Theron I, Engelstätter R. A comparative study of inhaled ciclesonide 160 microg/day and fluticasone propionate 176 microg/day in children with asthma. Pediatric Pulmonology 2006;41(10):954‐61. [DOI] [PubMed] [Google Scholar]
- Pedersen S, Garcia‐Garcia ML, Manjra I, Vermeulen H, Venter L, Engelstätter R. Ciclesonide and fluticasone propionate show comparable efficacy in children and adolescents with asthma. European Respiratory Journal 2004;24(Suppl 48):346s. [Google Scholar]
- Pedersen S, Gyurkovits K, Delft KHE, Boss H, Engelstätter R. Safety profile of ciclesonide as compared with fluticasone propionate in treatment of children and adolescents with asthma. European Respiratory Journal 2004;24(Suppl 48):346s. [Google Scholar]
- Pedersen S, Theron I, Engelstätter R. Ciclesonide is as effective as fluticasone propionate for treatment of children and adolescents with asthma. Respirology 2005;10(Suppl):A25. [Google Scholar]
Ukena 2006 {published and unpublished data}
- Biberger C, Behren V, Malek R, Weber HH, Beck E, Linnhoff A, et al. Efficacy and safety of ciclesonide compared with budesonide in asthma patients: a randomized 12‐week study. American Thoracic Society 99th International Conference. 2003:C105, Poster D62.
- Ukena D, Biberger C, Steinijans V, Behren V, Malek R, Weber HH, et al. Ciclesonide is more effective than budesonide in the treatment of persistent asthma. Pulmonary Pharmacology & Therapeutics 2006:Epub ahead of print. [DOI] [PubMed]
- Ukena D, Biberger C, Behren V, Malek R, Weber HH, Beck E, et al. Ciclesonide significantly improves pulmonary function when compared with budesonide: a randomised 12 week study. European Respiratory Journal 2003;22(Suppl 45):Abstract No: P2640. [Google Scholar]
Vermeulen 2007 {published data only}
- Vermeulen JH, Gyurkovits K, Rauer H, Engelstatter R. Randomized comparison of the efficacy and safety of ciclesonide and budesonide in adolescents with severe asthma. Respiratory Medicine 2007;101(10):2182‐91. [DOI] [PubMed] [Google Scholar]
- Vermeulen JH, Kósa L, Villa JR, Rauer H, Wurst W, Engelstätter R. Effects of ciclesonide on lung function and cortisol excretion in adolescent asthma patients – a comparative study with budesonide. European Respiratory Journal 2006;28(Suppl 50):206s. [Google Scholar]
- Vermeulen JH, Minic P, Barkai L, Sreckovic MD, Gyurkovitis K, Rauer H, et al. Ciclesonide 320 mcg once daily is as effective as budesonide 800 mcg once daily and has a favourable safety profile in adolescent patients with persistent asthma. http://www.abstracts2view.com. 2006.
von Berg 2007 {published data only}
- Berg A, Engelstatter R, Minic P, Sreckovic M, Garcia‐Garcia ML, Latos T, et al. Comparison of the efficacy and safety of ciclesonide 160 microg once daily versus budesonide 400 microg once daily in children with asthma. Pediatric Allergy Immunology 2007;18(5):391‐400. [DOI] [PubMed] [Google Scholar]
- Berg A, Garcia‐Garcia ML, Herllbardt S, Bethke TD. Ciclesonide 160 ug once daily is as effective as budesonide 400 ug once daily in pediatric patients with persistent asthma. Journal of Allergy and Clinical Immunology 2006;117(2 Suppl 1):s11. [Google Scholar]
- Berg A, Minic P, Sreckovic M, Bollroth C, Hellbardt S, Engelstätter R. Efficacy and safety of once‐daily ciclesonide 160 µg as compared with once‐daily budesonide 400 µg in paediatric asthma patients. Thorax 2005;2(Suppl II):ii43. [Google Scholar]
- Berg A, Vermeulen J, Manjra A, Weber H, Hellbardt S, Engelstätter R. Once‐daily ciclesonide 160 mcg is as effective as once‐daily budesonide 400 mcg in improving lung function in children with asthma and demonstrates a favorable safety profile. Paediatric Respiratory Reviews 2006;7(s283‐4). [Google Scholar]
- Berg A, Vermeulen JH, Zachgo W, Hellbardt S, Bethke TD, Engelstätter R. Comparison of ciclesonide 160 mcg/d with budesonide 400 mcg/d in a randomised, double‐blind study in children with moderate to severe asthma. European Respiratory Journal 2006;28(Suppl 50):711s. [Google Scholar]
Zietkowski 2006 {published data only}
- Zietkowski Z, Bodzenta‐Lukaszyk A, Tomasiak MM, Szymanski W, Skiepko R. Effect of ciclesonide and fluticasone on exhaled nitric oxide in patients with mild allergic asthma. Respiratory Medicine 2006;100:1651‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agertoft 2005 {published data only}
- Agertoft L, Pedersen S. Inhaled ciclesonide does not effect lower leg growth rate or HPA‐axis function in children with mild asthma. European Respiratory Journal 2004;24(Suppl 48):377s. [Google Scholar]
- Agertoft L, Pedersen S. Short‐term lower‐leg growth rate and urine cortisol excretion in children treated with ciclesonide. Journal Allergy & Clinical Immunology 2005;115(5):940‐5. [DOI] [PubMed] [Google Scholar]
- Agertorft L, Pedersen S. Lower‐leg growth rate and APA‐axis function in children with asthma during treatment with inhaled ciclesonide. Journal of Allergy and Clinical Immunology 2004;113(2 Suppl):S119. [Google Scholar]
Bethke 2002 {published data only}
- Bethke TD, Drollman A, Hauns B, Nave R, Zech K, Seinijans VW, et al. Bioequivalence of two ciclesonide dosing regimen (4 puffs of 200 µg versus 16 puffs of 50 µg using a MDI). European Respiratory Journal 2002;20(Suppl 38):109s. [Google Scholar]
- Drollmann A, Bethke TD, Nave R, Zech K, Hauns B, Steinjans VW, et al. Bioequivalence of two ciclesonide dosing regimen (4 puffs of 200 µg vs. 8 puffs of 100 µg using MDI). European Respiratory Journal 2002;20(Suppl 38):304s. [Google Scholar]
Dahl 1998 {published data only}
- Dahl R, Nielsen LP, Christensen MB, Engelstätter R. Ciclesonide ‐ an inhaled corticosteroid prodrug ‐ inhibits allergen induced early and late phase reactions. European Respiratory Journal 1998;12(Suppl 28):62S. [Google Scholar]
Derom 2005 {published data only}
- Derom E, Velde V, Marissens S, Engelstätter R, Vincken W, Pauwels R. Effects of inhaled ciclesonide and fluticasone propionate on cortisol secretion and airway responsiveness to adenosine 5'monophosphate in asthmatic patients. Pulmonary Pharmacology & Therapeutics 2005;18(5):328‐36. [DOI] [PubMed] [Google Scholar]
- Derom E, Velde V, Marissens S, Vincken W, Pauwels RA. Efficacy and systemic effects of ciclesonide and fluticasone in asthma patients. European Respiratory Journal 2001;18(Suppl 33):147s. [Google Scholar]
- Pauwels RA, Derom E, Velde V, Marissens S, Vincken W. Effects of inhaled ciclesonide and fluticasone propionate on cortisol secretion and PC²° for adenosine in asthma patients. American Journal of Respiratory and Critical Care Medicine 2002;165(Suppl 8):A768. [Google Scholar]
Drollman 2004 {published data only}
- Drollman A, Nave R, Steinijans VW, Bethke TD, Baumgartner E. Equivalent pharmacokinetics of the active metabolite of ciclesonide with and without use of a spacer for inhalation. Journal of Allergy and Clinical Immunology 2004;113(2 Suppl):S120. [DOI] [PubMed] [Google Scholar]
- Nave R, Baumgartner E, Bethkle D, Steinijans W, Drollman A. Equivalent pharmacokinetics of the active metabolite of ciclesonide when using the ciclesonide MDI without a spacer. European Respiratory Journal 2004;24(Suppl 48):583s. [Google Scholar]
Erin 2005 {published data only}
- Erin EM, Engelstätter R, Hellwig M, Hansel TT, Barnes PJ. Ciclesonide decreases exhaled breath nitric oxide and rapidly reduces airway responsiveness to adenosine monophosphate in asthma patients. European Respiratory Journal 2005;26(Suppl 49):1723. [Google Scholar]
- Erin EM, Englestätter R, Hellwig M, Hansel TT, Barnes PJ. Ciclesonide rapidly reduces airway responsiveness to adenosine monophosphate and deceases exhaled breath nitric oxide in patients with asthma. American Thoracic Society 2005 International Conference; May 20‐25; San Diego, California. 2005:D99; Poster: 916.
- Erin EM, Hansel TT, Barnes PJ, Schutze J, Hellwig M, Engelstätter R. Ciclesonide rapidly decreases airway responsiveness to adenosine monophosphate, and reduces exhaled nitric oxide in patients with asthma. XIX World Allergy Organization Congress; Munich, Germany. 2005:Abstract 295.
Gauvreau 2005 {published data only}
- Gauvreau GM, Boulet LP, Postma DS, Kawayama T, Watson RM, Duong M, et al. Effect of low‐dose ciclesonide on allergen‐induced responses in subjects with mild allergic asthma. Journal of Allergy & Clinical Immunology 2005;116(2):285‐91. [DOI] [PubMed] [Google Scholar]
- Gauvreau GM, Watson RM, Postma DS, Monchy GR, Deschesnes F, Boulet L. Effect of ciclesonide 40 µg and 80 µg on early and late asthmatic reactions, and sputum eosinophils after allergen challenge in patients with mild asthma. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S210. [Google Scholar]
- Kawayama T, Gauveau GM, Watson RM, Killian KJ, Duong M. Effects of inhaled ciclesonide on circulating Th1/Th2 cells in atopic asthmatics after allergen challenge. American Thoracic Society 2005 International Conference; May 20‐25; San Diego, California. 2005:B35; Poster: G1.
- O'Byrne PM, Postma DS, Smau L, Widmann A, Gauvreau GM, Monchy J, et al. Once daily ciclesonide reduces allergen‐induced early and late asthmatic reaction, and sputum eosinophils in patients with mild asthma. XIX World Allergy Organization Congress; Munich, Germany 2005:Abstract 296. [Google Scholar]
Kanniess 2001 {published data only}
- Kanniess F, Richter K, Bohme S, Jorres RA, Magnussen H. Effect of inhaled ciclesonide on airway responsiveness to inhaled AMP, the composition of induced sputum and exhaled nitric oxide in patients with mild asthma. Pulmonary Pharmacology & Therapeutics 2001;14(2):141‐7. [DOI] [PubMed] [Google Scholar]
Larsen 2003 {published data only}
- Larsen BB, Nielsen LP, Engelstatter R, Steinijans V, Dahl R. Effect of ciclesonide on allergen challenge in subjects with bronchial asthma. Allergy 2003;58(3):207‐12. [DOI] [PubMed] [Google Scholar]
Postma 2001 {published data only}
- Postma DS, Schlosser N, Sevette C, Martinat Y, Aumann J, Kafe H. Morning and evening administration of inhaled ciclesonide is equally effective in treatment of asthma. European Respiratory Society Annual Congress 2002. 2002:P1913.
- Postma DS, Sevette C, Martinat Y, Schlosser N, Aumann J, Kafe H. Treatment of asthma by the inhaled corticosteroid ciclesonide given either in the morning or evening. European Respiratory Journal 2001;17(6):1083‐8. [DOI] [PubMed] [Google Scholar]
Richter 2005 {published data only}
- Richter K, Kanniess F, Biberger C, Nave R, Magnussen H. Comparison of the oropharyngeal deposition of inhaled ciclesonide and fluticasone propionate in patients with asthma. Journal of Clinical Pharmacology 2005;45(2):146‐52. [DOI] [PubMed] [Google Scholar]
Subbarao 2006 {published data only}
- Duong M, Subbarao P, Otis J, Adelroth E, Inman M, Pedersen S, et al. Relationship between exercise‐induced bronchoconstriction and sputum eosinophillia during ciclesonide treatment in asthmatics. American Thoracic Society 2005 International Conference; May 20‐25; San Diego, California. 2005:B35; Poster: G11.
- Subbarao P, Duong M, Adelroth E, Otis J, Obminski G, Inman M, et al. Effect of ciclesonide dose and duration of therapy on exercise‐induced bronchoconstriction in patients with asthma. Journal of Allergy & Clinical Immunology 2006;117(5):1008‐13. [DOI] [PubMed] [Google Scholar]
- Subbarao P, Duong M, Otis J, Obminski G, Inman M, Alderoith E, et al. Ciclesonide attenuates exercise‐induced bronchoconstriction over time in asthmatic subjects. American Thoracic Society 2005 International conference; May 20‐25; San Diego, California. 2005:B35; Poster: G10.
- Subbarao P, Duong M, Pedersen S, Eckert J, Hellbardt S, Engelstatter R, et al. Once daily ciclesonide protects against exercise‐induced bronchoconstriction. XIX World Allergy Organization Congress; Munich, Germany. 2005:Abstract 298.
- Subbarao PJ, Duong M, Otis J, Obminski G, Adelroth E, Pedersen S, et al. Ciclesonide is effective in protecting against exercise‐induced bronchoconstriction. Journal of Allergy & Clinical Immunology 2005;115(2 Suppl):S1. [DOI] [PubMed] [Google Scholar]
Szefler 2005 {published data only}
- Szefler S, Rohatagi S, Williams J, Lloyd M, Kundu S, et al. Ciclesonide, a novel inhaled steroid, does not affect hypothalamic‐pituitary‐adrenal axis function in patients with moderate‐to‐severe persistent asthma. Chest 2005;128(3):1104‐14. [DOI] [PubMed] [Google Scholar]
- Szefler SJ, Herron J, Lloyd M, Rohatagi S, Williams JE, Kundu S, et al. High doses of the novel inhaled steroid ciclesonide have no effect on HPA‐axis function in patients with moderate to severe persistent asthma. Journal of Allergy and Clinical Immunology 2003;111(2 Suppl):S216. [Google Scholar]
Taylor 1999 {published data only}
- Jensen MW, Taylor DA, Englestätter R, Kanabar V, O'Connor BJ. A novel inhaled steroid, ciclesonide, reduces aiway responsiveness to AMP in a dose‐related manner. American Journal of Respiratory and Critical Care Medicine 1998;157(3 Suppl):A406. [DOI] [PubMed] [Google Scholar]
- Taylor DA, Jensen MW, Kanabar V, Engelstätter R, Steinijans VW, Barnes PJ, et al. A dose‐dependent effect of the novel inhaled corticosteroid ciclesonide on airway responsiveness to adenosine‐5'‐monophosphate in asthmatic patients. American Journal of Respiratory & Critical Care Medicine 1999;160(1):237‐43. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Knox 2007 {published data only}
- Knox A, Langan J, Martinot JB, Gruss C, Hafner D. Comparison of a step‐down dose of once‐daily ciclesonide with a continued dose of twice‐daily fluticasone propionate in maintaining control of asthma. Current Medical Research & Opinion 2007, (E‐pub ahead of print). [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Arshad {published data only}
- An assessment of safety and efficacy in treating moderate to severe asthmatics with inhaled Ciclesonide vs Fluticasone. Ongoing study Starting date of trial not provided. Contact author for more information.
Beck {published data only}
- Efficacy and safety of ciclesonide administered with or without different spacers in patients with asthma (12 to 75 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Beckman {published data only}
- Efficacy of ciclesonide inhaled once daily versus other corticosteroids used for treatment of mild asthma in children (4‐11 ys ). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Colatruglio {published data only}
- Effect of ciclesonide on quality of life in patients with moderate persistent asthma (21 to 65 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Dahl {published data only}
- Efficacy of ciclesonide versus fluticasone propionate inpatients with mild to moderate asthma (12 to 75 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Derom {published data only}
- Effect of inhaled ciclesonide versus fluticasone propionate in patients with mild to moderate asthma (18 to 65 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Dusser {published data only}
- Efficacy of ciclesonide and fluticasone propionate in adult patients with moderate and severe persistent asthma (18 to 75 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Engelstätter {published data only}
- Efficacy of ciclesonide inhaled once daily versus fluticasone propionate inhaled twice daily in children with asthma (4 to 15 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Giwa {published data only}
- Comparison of inhaled ciclesonide and fluticasone proprionate in moderate to severe asthma patients, well controlled under high doses of inhaled corticosteroids. Ongoing study Starting date of trial not provided. Contact author for more information.
Hansel {published data only}
- A 3‐period double‐blind, cross‐over study on the onset of action of inhaled ciclesonide on airway responsiveness to adenosine monophosphate, sputum eosinophils and exhaled breath NO in patients with asthma. Ongoing study Starting date of trial not provided. Contact author for more information.
O'Byrne {published data only}
- Efficacy of ciclesonide vs fixed combination of fluticasone propionate/salmeterol vs placebo in patients with mild persistent asthma (12 to 75 y). Clinicaltrials.Gov. 2005.. Ongoing study Starting date of trial not provided. Contact author for more information.
Park {published data only}
- Effectiveness of ciclesonide versus budesonide in patients with asthma (18 to 75 y). Clinicaltrials.Gov. 2005. Ongoing study Starting date of trial not provided. Contact author for more information.
Sanofi Aventis {published data only}
- Effects of ciclesonide and beclomethasone on lens opacification in adult participants with moderate to severe persistent asthma. Clinicaltrials.Gov . 2005; Efficacy of ciclesonide vs. placebo administered as once daily or twice daily in patients not treated with inhaled corticosteroid. Clinicaltrials.Gov. 2005; Effects of ciclesonide MDI 50 mg/day and 200 mg/day (ex‐value) once‐daily on growth in children with mild persistent asthma. Clinicaltrials.Gov. 2005; Sanofi‐Aventis. Dose response study of inhaled ciclesonide (glucocorticosteroid) to patients with persistent asthma. Clinicaltrials.Gov. 2005.. Ongoing study Starting date of trial not provided. Contact author for more information.
Stenton {published data only}
- A double‐blind randomised parallel group study comparing the efficacy and safety of 800 and 1000 mcg CIC/day in patients with asthma followed by an open long‐term study to assess the safety of CIC in patients with asthma. Ongoing study Starting date of trial not provided. Contact author for more information.
Additional references
Adams 2005
- Adams NP, Bestall JB, Malouf R, Lasserson TJ, Jones PW. Beclomethasone versus placebo for chronic asthma. Cochrane Database of Systematic Reviews 2005, Issue 1. [Art. No.: CD002738. DOI: 10.1002/14651858.CD002738.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Adams 2005a
- Adams NP, Bestall JC, Lasserson TJ, Jones PW, Cates CJ. Fluticasone versus placebo for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2005, Issue 4. [Art. No.: CD003135. DOI: 10.1002/14651858.CD003135.pub3] [DOI] [PubMed] [Google Scholar]
Adams 2005b
- Adams NP, Bestall JC, Jones PW, Lasserson TJ, Griffiths B, Cates CJ. Fluticasone at different doses for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2005, Issue 3. [Art. No.: CD003534. DOI: 10.1002/14651858.CD003534.pub2] [DOI] [PubMed] [Google Scholar]
Adams 2007
- Adams N, Lasserson TJ, Cates CJ, Jones PW. Fluticasone versus beclomethasone or budesonide for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2007, Issue 4. [Art. No.: CD002310. DOI: 10.1002/14651858.CD002310.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
BGAM 1997
- British Thoracic Society, National Asthma Campaign, Royal College of Physicians of London, et al. The British guidelines on asthma management: 1995 review and position statement. Thorax 1997;52(Suppl 1):S1‐21. [Google Scholar]
BTS 1997
- British Thoracic Society, National Asthma Campaign, Royal College of Physicians of London, et al. The British guidelines on asthma management: 1995 review and position statement. Thorax 1997;52(Suppl 1):S1‐21. [Google Scholar]
BTS/SIGN 2003
- British Thoracic Society. British Guideline on the Management of Asthma. Thorax 2003;58:Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buston 2000
- Buston KM, Wood SF. Non‐compliance amongst adolescents with asthma: listening to what they tell us about self‐management. Family Practice 2000;17:134‐8. [DOI] [PubMed] [Google Scholar]
Consensus 1999
- Canadian Asthma Concensus Group. Canadian asthma consensus report. CMAJ 1999;161(11 Suppl). [PMC free article] [PubMed] [Google Scholar]
Consensus 2005
- Summary of recommendations from the Canadian Asthma Consensus Guidelines, 2003 and Canadian Pediatric Asthma Consensus Guidelines, 2003 (updated to December 2004). Canadian Medical Association Journal 2005;173(Suppl):s1‐s156. [PMC free article] [PubMed] [Google Scholar]
Coutts 1992
- Coutts JA, Gibson NA, Paton JY. Measuring compliance with inhaled medication in asthma. Archives of Disease of Childhood 1992;67:332‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eisen 1990
- Eisen SA, Miller DK, Woodward RS, Spitznagel E, Przybeck TR. The effect of prescribed daily dose frequency on patient medication compliance. Archives of Internal Medicine 1990;150:1881‐4. [PubMed] [Google Scholar]
Gelfand 2006
- Gelfand EW, Georgitis JW, Noonan M, Ruff ME. Once‐daily ciclesonide in children: efficacy and safety in asthma. Journal of Pediatrics 2006;148(3):377‐83. [DOI] [PubMed] [Google Scholar]
Gerritsen 1989
- Gerritsen J, Koeter GH, Postma DS, Schouten JP, Krol K. Prognosis of asthma from childhood to adulthood. American Review of Respiratory Disease 1989;140:1325‐30. [DOI] [PubMed] [Google Scholar]
GINA 1998
- National Institutes of Health (NIH), National Heart, Lung and Blood Institute. Global Strategy for Asthma Management and Prevention.. NIH publication No. 96‐36598 (document available at: www.ginasthma.com) 1998.
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lasserson 2006
- Lasserson TJ, Cates CJ, Jones AB, Lasserson EH, White J. Fluticasone versus HFA‐beclomethasone dipropionate for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2006, Issue 2. [Art. No.: CD005309. DOI: 10.1002/14651858.CD005309.pub3] [DOI] [PubMed] [Google Scholar]
Lipworth 2005a
- Lipworth B. Designer inhaled corticosteroids ‐ are they safer?. Chest 2005;128(3):1081‐4. [DOI] [PubMed] [Google Scholar]
Malo 1989
- Malo JL, Cartier A, Merland N, Ghezzo H, Burek A, Morris J, et al. Four‐times‐a‐day dosing frequency is better than twice‐a‐day regimen in subjects requiring a high‐dose inhaled steroid, budesonide, to control moderate to severe asthma. American Review of Respiratory Disease 1989;140:624‐8. [DOI] [PubMed] [Google Scholar]
Manning 2008
- Manning PJ, Gibson PG, Lasserson TJ. Ciclesonide for chronic asthma in adults and children. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 1982
- Martin AJ, Landau LJ, Phelan PD. Asthma from childhood at age 21: the patient and his disease. British Medical Journal 1982;284:380‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mash 2001
- Mash B, Bheekie A, Jones PW. Inhaled versus oral steroids for adults with chronic asthma (Cochrane review). Cochrane Database of Systematic Reviews 2001, Issue 1. [Art. No.: CD002160. DOI: 10.1002/14651858.CD002160] [DOI] [PubMed] [Google Scholar]
Masoli 2004
- Masoli M, Fabian D, Holt S, Beasley R. Developed for Global Initiative for Asthma (GINA). Allergy 2004;59:469‐78. [Full report available on www.ginasthma.com] [DOI] [PubMed] [Google Scholar]
Powell 2003
- Powell H, Gibson PG. High dose versus low dose inhaled corticosteroid as initial starting dose for asthma in adults and children. Cochrane Database of Systematic Reviews 2003, Issue 4. [Art. No.: CD004109. DOI: 10.1002/14651858.CD004109.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Suissa 2000
- Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low‐dose inhaled corticosteroids and the prevention of death from asthma. New England Journal of Medicine 2000;343:332‐6. [DOI] [PubMed] [Google Scholar]
Suissa 2002
- Suissa S, Ernst P, Kezoul A. Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax 2002;57:880‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tattersfield 2002
- Tattersfield AE, Knox AS, Britton JR, Hall IP. Asthma. Lancet 2002;360:1313‐20. [DOI] [PubMed] [Google Scholar]
Toogood 1982
- Toogood JH, Baskerville JC, Jennings B, Lefcoe NM, Johannsson SA. Influence of dosing frequency and schedule on the response of chronic asthmatics to the aerosol steroid, budesonide. Journal Allergy and Clinical Immunology 1982;70:288‐98. [DOI] [PubMed] [Google Scholar]
Williams 1969
- Williams H, McNicol KN. Prevalence, natural history, and relationship of wheezy bronchitis and asthma in children. An epidemiological study. British Medical Journal 1969;4:321‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]


