Abstract
Introduction
Postherpetic neuralgia (PHN) is the most common sequela of herpes zoster, and it is often refractory to guideline-recommended treatments. Acupuncture therapy, a wildly applied complementary-alternative treatment, may help in the management of PHN. Diverse types of acupuncture therapy for PHN have been proposed, however, their comparative efficacies remain unclear. This study protocol plans to compare the efficacy and safety of different acupuncture therapies for PHN.
Methods and analysis
Databases including MEDLINE, Embase, Cochrane Library, Web of Science, Chinese Biomedical Database, China National Knowledge Infrastructure, VIP Database, Wanfang Database, WHO International Clinical Trials Registry Platform, ClinicalTrials.gov, Chinese Clinical Trial Register and OpenGrey will be searched from their inception to January 2022. Randomised controlled trials (RCTs) assessing the effectiveness of acupuncture therapy on the management of PHN will be selected. The primary outcome is pain intensity. Secondary outcomes include negative emotions, sleep condition, quality of life and adverse events. Reviewers will conduct study selection, data extraction and risk of bias assessment procedures. Then, standard pair-wised meta-analysis and Bayesian network meta-analysis will be performed (if applicable). The Confidence in Network Meta-Analysis application will be used to assess the confidence in the evidence for the primary outcome.
Ethics and dissemination
All data used for this study will be extracted from published RCTs, thus, no ethical approval will be required. The results of this systematic review will be disseminated through peer-reviewed journal and conference presentation.
PROSPERO registration number
CRD42020219576.
Keywords: acupuncture therapy, postherpetic neuralgia, systematic review, network meta-analysis
Strengths and limitations of this study.
This study will be the first Bayesian network meta-analysis comparing various acupuncture therapies in the management of postherpetic neuralgia (PHN).
Our study will comprehensively evaluate the effects of acupuncture therapy on pain intensity, emotional symptoms, sleep quality and life quality for patients with PHN.
Our study will focus on the methods of acupuncture treatment, without consideration of acupoints selection or specific details of manual techniques.
We will only search Chinese and English databases, which may result in language bias.
Introduction
Postherpetic neuralgia (PHN) is defined as a neuropathic pain that occurs after an eruptive phase of herpes zoster (HZ), as its most common clinical sequela.1 Definitions of PHN are not consistent across studies, with its occurrence ranging from ≥1 to ≥6 months after the rash.2 Compared with acute HZ-associated pain (pain preceding or accompanying the visible cutaneous manifestation), which resolves within a month, PHN may persist for months, even years.3 4 A systematic review showed that the incidence rate of HZ ranged from 3 to 5/1000 person-years globally, with 5% to more than 30% of patients with HZ progressing to PHN.5 Several risk factors for PHN are commonly reported, including advanced age, female sex, severe immunosuppression, severe rash and pain in acute zoster episode. Physical comorbidities, such as autoimmune conditions and diabetes, may also be associated with an increased risk of PHN.6–8 Patients with PHN prominently report about continuous or intermittent spontaneous pain (eg, aching pain, burning pain, stabbing pain, shooting pain) and may co-present with hyperalgesia, allodynia and other abnormal sensations (eg, anaesthesia, vibration).9 In addition, persistent pain can lead to negative emotions, sleep disorders and lowered quality of life of patients and their families, which causes a heavy burden of healthcare at both the individual and societal levels.10–12
Several systemic and topical treatments are listed in the guidelines for the management of PHN (either exclusive for PHN or specific mention to PHN in neuropathic pain context).13–16 Antiepileptic drugs gabapentin and pregabalin, tricyclic antidepressants (TCAs) and topical lidocaine are recommended as first-line treatments. PHN often requires long-term treatment; thus, side effect profiles of antiepileptic drugs and TCAs may become dangerous, especially for elderly patients who are dealing with other age-related issues.17 Lidocaine patch may only cause mild skin reaction and is well tolerated and safe even in long-term treatment.18 19 Opioids and tramadol are recommended as second-line or third-line options in latest guidelines, with uncertain long-term efficacy and safety.1 Topical use of capsaicin is listed as second-line or third-line therapy, and either capsaicin 0.075% cream or capsaicin 8% patch can be selected. However, its use may be limited by localised pain during the application.20 In general, given the refractory nature of neuropathic pain, conventional medications only provide modest effect on pain relief for PHN.21 Interventional therapy, either involving invasive delivery of drugs or ablation/modulation of related nerves, is proposed in the management of neuropathic pain and often considered after failure of standard pharmacological treatments.22 However, evidence of interventional treatments specific for patients with PHN is generally insufficient, and invasive procedures are often associated with safety concerns.23 24
Acupuncture therapy, based on stimulation to acupoints (specific locations on the body), not only is favourable in Asia–Pacific but also gains increasing popularity in Europe and America.25–27 It is one of the major components of traditional Chinese medicine (TCM), which has been used in the management of various pain conditions, including PHN, as a complementary alternative treatment.28–31 With a substantial number of clinical trials conducted in China, diverse acupuncture approaches have been reported either singly or in combination when treating PHN, such as manual acupuncture, moxibustion, electroacupuncture, firing needling and bloodletting.31 These methods most likely have different effects on pain reduction, given their distinct mechanisms in both TCM theory and neurophysiological processes.32 33 In recent years, systematic reviews and meta-analyses have shown a potential positive effect of acupuncture therapy for patients with PHN on pain relief with few reported adverse events.34–36 However, these studies either combined all relative methods as acupuncture therapy when conducting data syntheses or evaluated the effect of only a single type of acupuncture therapy. Thus, their results may not be sufficient to reflect the distinct effects of diverse acupuncture methods. With the majority of existing studies focusing on the comparison between acupuncture therapy and conventional pharmacological treatment, the relative treatment effects of different acupuncture therapies for PHN are poorly understood, which may cause confusion for clinical practitioners. To this end, it is necessary to further explore the relative effectiveness of different acupuncture therapies for PHN.
Network meta-analysis (NMA), as an extension of standard pairwise meta-analysis, compares multiple interventions simultaneously, which can be used to obtain the potential optimal option among different treatments.37 Therefore, we plan to perform NMA to evaluate the effectiveness and safety of different acupuncture therapies (and their combinations) for PHN.
Objective
The overall purpose of this study is to assess the effectiveness and safety of different acupuncture therapies in the treatment of PHN based on existing clinical trials. Using systematic review and NMA methods, we will primarily focus on the efficacy of acupuncture therapies for pain relief when treating PHN. We will also compare their effect on negative emotions, sleep condition and quality of life and evaluate treatment safety to provide a comprehensive view for clinical practice.
Methods
We will perform a systematic review and NMA guided by the Checklist of Items to Include When Reporting a Systematic Review Involving a Network Meta-analysis.38 This study protocol will be presented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement.39 The protocol has been registered on PROSPERO.
Eligibility criteria
Types of studies
This review will only include randomised controlled trials (RCTs) reported in English or Chinese with a parallel-group design. Cross-over trials, quasi-RCTs, cluster RCTs or any other types of non-RCTs will be excluded.
Types of participants
Participants will include patients who meet the diagnostic criteria of PHN according to the definition by the American Academy of Family Physicians,40 which is pain persisting from 30 days to more than 6 months after the HZ lesions have healed, or any other accepted diagnostic guidelines. There will be no restrictions on age, sex or nationality of the participants.
Types of interventions
In this review, we define acupuncture therapy as an acupoint-stimulated technique guided by the TCM theory. Therefore, we will include any of the following treatments: manual acupuncture, electroacupuncture, warm needling, fire needling, pressing needling, transcutaneous electrical acupoint stimulation, moxibustion, bloodletting, cupping, acupoint catgut embedding, acupoint injection or a combination of any two or three of these methods. Therapies related to acupoints defined in a non-traditional way, such as auricular acupuncture and wrist–ankle acupuncture, will be excluded.
Types of control groups
Studies using either conventional medication or placebo in the control groups and studies comparing different types of acupuncture therapies will be included. However, studies comparing different acupoint prescriptions or different manual needling techniques with the same type of acupuncture method will be excluded. We will also exclude studies using sham acupuncture in the control groups, as sham acupuncture is widely considered not inert, which may cause confusion when compared with various types of acupuncture therapies.41
Types of outcome measurements
Primary outcome(s)
Our primary aim is to evaluate pain control efficacy. According to preliminary searches of relevant articles, measurements of pain intensity have been reported in most cases. Other profiles of pain control, such as onset of pain relief time, are not frequently reported.35 Therefore, we will select pain intensity as the main outcome of interest. Pain intensity is usually presented by a score on a range between no pain to maximum pain, with higher number indicating more severe pain, using the Visual Analogue Scale, Numerical Rating Scale, Verbal Rating Scale, Average Daily Pain Score or other validated scales.
Secondary outcome(s)
To comprehensively assess the effect of acupuncture therapies for PHN, the following outcomes will be analysed in our study:
Negative emotions, such as anxiety and depression, measured using the Hamilton Anxiety Scale, Self-Rating Anxiety Scale, Self-Rating Depression Scale or other validated scales.
Sleep quality measured using the Pittsburgh Sleep Quality Index or other validated scales.
Quality of life measured using the Quality of Life scale or other validated scales.
Adverse events occurring during the treatment period.
Data sources and search strategy
We will identify clinical studies by searching the following databases: MEDLINE (via PubMed), Embase, Cochrane Library, Web of Science, Chinese Biomedical Database, China National Knowledge Infrastructure, VIP Database, Wanfang Database, WHO International Clinical Trials Registry Platform, ClinicalTrials.gov and Chinese Clinical Trial Register. We will also search for grey literature in the OpenGrey database. Search dates will be from the inception of these databases to 31 January 2022 with the search languages limited to either English or Chinese. Search terms used in our review will be a combination of medical subject headings terms and free-text terms, which can be categorised into three groups: clinical condition (eg, ‘postherpetic neuralgia’, ‘zoster herpes’, ‘shingles’), interventions (eg, ‘acupuncture’, ‘moxibustion’, ‘electroacupuncture’, ‘fire needling’) and study design (eg, ‘randomised controlled trial’, ‘RCT’, ‘clinical trial’). We adjusted the search terms for each database. The search strategy for PubMed is presented in table 1. In addition, reference lists of the included studies will be examined to identify potentially eligible studies.
Table 1.
Search strategy in PubMed
| Order | Search items |
| #1 | MeSH terms: “Neuralgia, Postherpetic” |
| #2 | Title/abstract: “postherpetic neuralgia” OR “post-herpetic neuralgia” OR “PHN” OR “herpes zoster” OR “shingles” |
| #3 | #1 OR #2 |
| #4 | MeSH terms: “Acupuncture Therapy” OR “Acupuncture” OR “Cupping Therapy” OR “Bloodletting” |
| #5 | Title/abstract: “acupuncture” OR “electroacupuncture” OR “moxibustion” OR “moxa” OR “cupping” OR “bloodletting” OR “blood-letting” OR “pricking blood” OR “pyonex” OR “acupressure” OR “needle” OR “needles” OR “needling” OR “acupoint” OR “acupoints” OR “meridian” OR “meridians” |
| #6 | #4 OR #5 |
| #7 | Publication type: “Randomized Controlled Trial” |
| #8 | MeSH terms: “Randomized Controlled Trials as Topic” |
| #9 | Title/abstract: “randomized” OR “randomly” OR “RCT” OR “trial” |
| #10 | #7 OR #8 OR #9 |
| #11 | #3 AND #6 AND #10 |
MeSH, Medical Subject Headings.
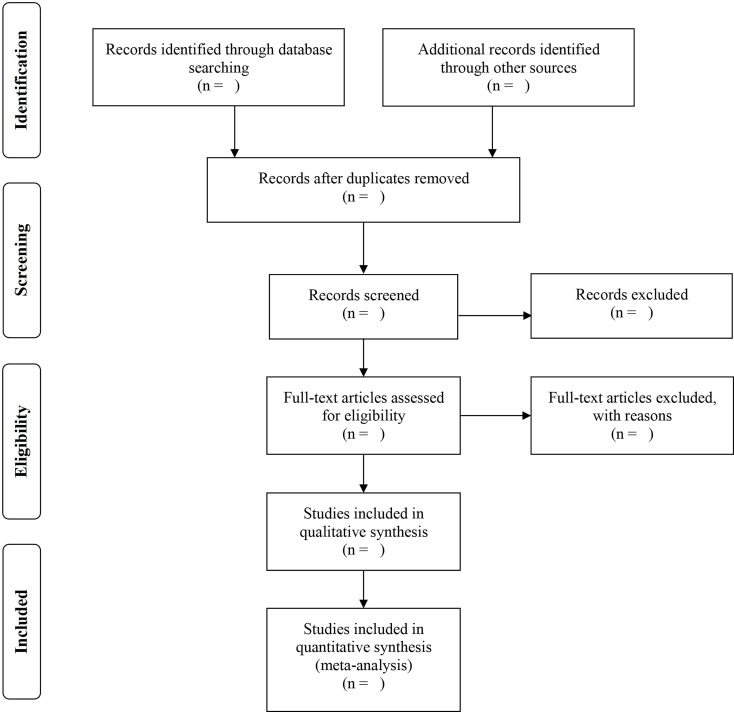
Study selection
The bibliographic information of search results in each database and additional records will be combined and imported into NoteExpress V.3.2.0. After deduplication, two independent reviewers (ZB and JY) will screen the titles and abstracts of the identified studies to remove irrelevant ones. Full texts of the remaining studies will be downloaded for further assessment according to the inclusion criteria. Reviewers will try to identify duplicate data from the same trials from different publications and contact study authors for clarification when needed. Discrepancies in study selection will be resolved by discussion, or when no consensus is reached, a third reviewer (JF) will be consulted for arbitration. Excluded studies will be recorded for reasons of exclusion. The PRISMA flowchart of the study selection process is shown in figure 1.42
Figure 1.
PRISMA flow diagram of the study selection process. PRISMA, Preferred Reporting Items for Systematic review and Meta-Analysis.
Data extraction
Two independent reviewers (MT and JH) will use a predesigned data collection form to extract data from the included studies. The following information will be collected: publication information (publication year, first author), characteristics of the study population (sample size, age, sex, duration of PHN), details of intervention (type of acupuncture therapies, acupoint selection, needle retention time, frequency and duration of treatment sessions), details of the comparator (drug names, dosage, frequency, treatment duration) and outcomes (data and time point of outcome measures, adverse events and dropouts). Any disagreement will be solved through discussion or consultation with a third reviewer (JF).
For multiarm studies that report different types of acupuncture interventions (or comparators), data from all relevant arms will be extracted.
Means and SDs of change scores between baseline and after treatment (defined as baseline scores minus outcome scores) will be collected for each outcome. When studies fail to report data on changes from baseline and means and SDs before and after the treatment will be extracted, we will calculate the mean change in each arm and the SD of the changes.43 For studies where outcomes are reported at multiple time points after the treatment, data of outcomes assessed at the first time point after the complete treatment regimen will be used.
For studies where SDs of the outcome are not reported, missing SDs will be calculated from SEs, CIs, t-statistics and p values. Additionally, in studies reporting only the median and IQRs, means and SDs will be calculated using a specific formula.44 If these data are not presented, we will contact the corresponding authors of original studies to obtain the missing data. After these steps, studies with insufficient data for quantitative synthesis will be excluded from the meta-analysis.
Risk of bias assessment
We will assess the risk of bias of included studies using the Cochrane tool risk of bias 2, which identifies bias in the following domains: randomisation process, deviations from intended interventions, missing outcome data, measurement of the outcome and selection of the reported result.45 Pain intensity, as the main outcome of interest, will be selected as the result to assess. The assessment will be performed in relation to the assignment to the intervention (intention-to-treat effect). Two reviewers (BL and RS) will independently answer the signalling questions of each domain. Subsequently, a judgement into ‘low’, ‘some concerns’ or ‘high’ risk of bias will be made depending on the responses to these questions, finally reaching an overall risk-of-bias judgement. Disagreements during the assessment will be resolved by discussion, and a third reviewer (JF) will be consulted where necessary.
Data synthesis
We will perform NMA as the primary method for data synthesis. Additionally, standard pairwise meta-analyses will be performed, and the results will be compared with those from the NMA. For each outcome, the mean difference (MD) of the change score will be considered the measure of relative treatment effects. When trials use different measurement scales for a certain outcome, the standardised MD will be calculated. We will use the OR to investigate adverse event data as a measure of treatment safety.
When two or more studies comparing the same pair of interventions exist for an outcome, a standard meta-analysis will be performed. Random-effects models will be fitted using Stata V.15.1. The effect size will be estimated with a 95% CI. We will use the I² statistic to quantify the heterogeneity of the results in the same treatment comparisons.46 If the I² value is greater than 75%, which indicates the existence of high heterogeneity, and no main source of heterogeneity is found, we will provide a narrative summary without conducting data synthesis.47
We will perform network meta-analyses to simultaneously compare multiple interventions. For each outcome, network plot of all included comparisons will be generated using Stata V.15.1, where interventions are represented by nodes, and each line between two nodes means that a direct comparison between two interventions is available. Studies that are not connected to the network will be excluded from network meta-analyses. The sizes of the nodes and lines are proportional to the number of included studies. We will conduct NMA within a Bayesian hierarchical framework in OpenBUGS V.3.2.3. Random-effects models with vague priors will be fitted, and the Markov Chain Monte Carlo (MCMC) method will be employed to obtain the pooled treatment effect, with a 95% credible interval. Three MCMC chains with different sets of initial values will be run simultaneously. For each initial value, 60 000 simulations will be conducted after discarding 10 000 simulations as the burn-in period, and convergence will be assessed visually and using the Gelman-Rubin statistic.48 To assess the model fit, the posterior mean residual deviance will be calculated and compared with the number of data points in the model.49 We will obtain the ranking probabilities of all included interventions using the surface under the cumulative ranking curve analysis in Stata V.15.1.50
Clinical and methodological heterogeneity will be assessed by examining the characteristics and design of the included studies. The transitivity assumption for NMA will be evaluated by reviewing the distribution of potential effect modifiers (participant characteristics: age, pain severity at baseline; interventions: treatment duration; study design: risk of bias) across comparisons. We will also assess statistical heterogeneity by calculating the between-study SD (τ2), with a larger τ2 value indicating a higher level of heterogeneity among studies. We will evaluate the global inconsistency of the treatment network by comparing the consistency model with an inconsistency model; the node-splitting method will be used to assess local inconsistency.51 52
Additional analyses
We will perform network meta-regression using a random-effects model to examine the influence of potential effect modifiers (eg, average age of participants, duration of PHN, pain severity at baseline) on the main outcome. As dose of acupuncture treatment is an important factor that can influence treatment efficacy, a subgroup analysis involving different dosage of the acupuncture therapies on the main outcome will be performed. The concept of adequate acupuncture dose has been introduced in several systematic reviews.53 54 Accordingly, we will define a ‘high dosage’ of acupuncture treatment when both the following criteria are met: (1) the treatment frequency is ≥2 sessions a week, and (2) the total number of treatment sessions is ≥12.55 When only one of (1) or (2) is met, the treatment will be defined as ‘medium dosage’, and when neither of them are met, the treatment will be defined as ‘low dosage’. If sufficient studies are available, we will also perform sensitivity analysis by excluding trials rated as a high risk of bias to ensure the robustness of the primary findings. Furthermore, the presence of potential reporting bias will be inspected using a comparison-adjusted funnel plot.56
Credibility of the evidence
We plan to evaluate credibility of the evidence from NMA using the Confidence in Network Meta-Analysis web application for the primary outcome.57 Two reviewers (GI and YX) will independently assess the following domains: within-study bias, across-study bias, indirectness, imprecision, heterogeneity and incoherence. Disagreements will be solved by discussion or consultation with a third reviewer (JF). Confidence in the results will be graded as ‘high’, ‘moderate’, ‘low’ and ‘very low’.
Patient and public involvement
No patients or public will be involved in this study.
Discussion
Patients with PHN usually experience persistent pain, and many of them report about other clinical symptoms, such as anxiety, depression and sleep disorders, which are frequent in general neuropathic pain.58 Although several recommendations have been made on pharmacological therapy, many patients with PHN do not achieve satisfactory pain relief or discontinue treatment due to adverse effects.59 Acupuncture therapy is proposed as potentially beneficial in the management of neuropathic pain and is generally safe when operated by competent practitioners.60 61 Moreover, acupuncture therapy may help with negative emotions and sleep disorders, which would provide additional benefits for patients in usually long-term treatment.62 63
In clinical practice for PHN, diverse acupuncture methods are available, and in many trials, the integrated use of two or more acupuncture methods have been reported. The existing systematic reviews are generally focusing on comparing a single type of acupuncture therapy with pharmacologic therapy, while the effects of integrated use of different acupuncture methods are poorly investigated. The clinical practice guidelines of acupuncture for HZ, launched by the WHO’s Western Pacific Regional Office, recommended the use of fire needling, electroacupuncture and bloodletting in the PHN phase and suggested that the combined use of two or more methods is more beneficial.64 However, there is still little knowledge on the relative effectiveness of these acupuncture methods and their integrated use, which causes confusion for the selection of these methods. NMA, a technique to integrate direct and indirect comparisons across a set of multiple variables, can be used for comparing efficacies of multiple treatments simultaneously in a single analysis.65 Our NMA will clearly define the types of included acupuncture therapy and their integrated use, to comprehensively evaluate their effects in the management of PHN. In recent years, NMA has been increasingly performed to compare the efficacies of different acupuncture methods for many diseases, such as knee osteoarthritis, myofascial pain syndrome and chronic fatigue syndrome.66–68 To the best of our knowledge, this study will be the first Bayesian NMA of acupuncture therapies for the treatment of PHN. We sincerely hope that our results will offer credible evidence and contribute to the proper use of acupuncture therapy for treating PHN.
Supplementary Material
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Footnotes
ZB and JY contributed equally.
Contributors: ZB and JY conceived this study and wrote the manuscript. MT and BL developed the search strategy. JH, GI, RS and YX provided methodological advice. YJ, XH and JF revised the manuscript. All authors have reviewed this protocol and approved the final manuscript.
Funding: This study is supported by Project of Zhejiang Provincial Administration of Traditional Chinese Medicine (NO:2022ZZ029) and Key Plan of Zhejiang Province Traditional Chinese Medicine Prevention and Treatment of Major Disease of the Health and Family Planning Commission of Zhejiang Province (No.2018ZY008). The funders had no role on the design of this study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Johnson RW, Rice ASC. Clinical practice. postherpetic neuralgia. N Engl J Med 2014;371:1526–33. 10.1056/NEJMcp1403062 [DOI] [PubMed] [Google Scholar]
- 2.CDC (Centers for Disease Control and Prevention) . Prevention of herpes zoster: recommendations of the Advisory Committee on immunization practices (ACIP). CDC 2008. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr57e0515a1.htm [PubMed] [Google Scholar]
- 3.Gan EY, Tian EAL, Tey HL. Management of herpes zoster and post-herpetic neuralgia. Am J Clin Dermatol 2013;14:77–85. 10.1007/s40257-013-0011-2 [DOI] [PubMed] [Google Scholar]
- 4.Dworkin RH, Gnann JW, Oaklander AL, et al. Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain 2008;9:37–44. 10.1016/j.jpain.2007.10.008 [DOI] [PubMed] [Google Scholar]
- 5.Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open 2014;4:e004833. 10.1136/bmjopen-2014-004833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choo PW, Galil K, Donahue JG, et al. Risk factors for postherpetic neuralgia. Arch Intern Med 1997;157:1217–24. 10.1001/archinte.1997.00440320117011 [DOI] [PubMed] [Google Scholar]
- 7.Forbes HJ, Thomas SL, Smeeth L, et al. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain 2016;157:30–54. 10.1097/j.pain.0000000000000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forbes HJ, Bhaskaran K, Thomas SL, et al. Quantification of risk factors for postherpetic neuralgia in herpes zoster patients: a cohort study. Neurology 2016;87:94–102. 10.1212/WNL.0000000000002808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schutzer-Weissmann J, Farquhar-Smith P. Post-herpetic neuralgia - a review of current management and future directions. Expert Opin Pharmacother 2017;18:1739–50. 10.1080/14656566.2017.1392508 [DOI] [PubMed] [Google Scholar]
- 10.Oster G, Harding G, Dukes E, et al. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: results from a population-based survey. J Pain 2005;6:356–63. 10.1016/j.jpain.2005.01.359 [DOI] [PubMed] [Google Scholar]
- 11.Mauskopf J, Austin R, Dix L, et al. The Nottingham health profile as a measure of quality of life in zoster patients: convergent and discriminant validity. Qual Life Res 1994;3:431–5. 10.1007/BF00435395 [DOI] [PubMed] [Google Scholar]
- 12.Weinke T, Glogger A, Bertrand I, et al. The societal impact of herpes zoster and postherpetic neuralgia on patients, life partners, and children of patients in Germany. ScientificWorldJournal 2014;2014:749698 10.1155/2014/749698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubinsky RM, Kabbani H, El-Chami Z, et al. Practice parameter: treatment of postherpetic neuralgia: an evidence-based report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2004;63:959–65. 10.1212/01.wnl.0000140708.62856.72 [DOI] [PubMed] [Google Scholar]
- 14.Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol 2010;17:1113–88. 10.1111/j.1468-1331.2010.02999.x [DOI] [PubMed] [Google Scholar]
- 15.Dworkin RH, O'Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 2007;132:237–51. 10.1016/j.pain.2007.08.033 [DOI] [PubMed] [Google Scholar]
- 16.Dworkin RH, O'Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 2010;85:S3–14. 10.4065/mcp.2009.0649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadley GR, Gayle JA, Ripoll J. Post-herpetic Neuralgia: a Review [published correction appears in Curr Pain Headache Rep 2016 Apr;20:28]. Curr Pain Headache Rep;2016:17. [DOI] [PubMed] [Google Scholar]
- 18.Wilhelm IR, Tzabazis A, Likar R, et al. Long-term treatment of neuropathic pain with a 5% lidocaine medicated plaster. Eur J Anaesthesiol 2010;27:169–73. 10.1097/EJA.0b013e328330e989 [DOI] [PubMed] [Google Scholar]
- 19.Bursi R, Piana C, Grevel J, et al. Evaluation of the population pharmacokinetic properties of lidocaine and its metabolites after long-term multiple applications of a lidocaine plaster in post-herpetic neuralgia patients. Eur J Drug Metab Pharmacokinet 2017;42:801–14. 10.1007/s13318-017-0400-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Argoff CE. Review of current guidelines on the care of postherpetic neuralgia. Postgrad Med 2011;123:134–42. 10.3810/pgm.2011.09.2469 [DOI] [PubMed] [Google Scholar]
- 21.Wright ME, Rizzolo D. An update on the pharmacologic management and treatment of neuropathic pain. JAAPA 2017;30:13–17. 10.1097/01.JAA.0000512228.23432.f7 [DOI] [PubMed] [Google Scholar]
- 22.Dworkin RH, O'Connor AB, Kent J, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain 2013;154:2249–61. 10.1016/j.pain.2013.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colloca L, Ludman T, Bouhassira D, et al. Neuropathic pain. Nat Rev Dis Primers 2017;3:17002. 10.1038/nrdp.2017.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin C-S, Lin Y-C, Lao H-C, et al. Interventional treatments for postherpetic neuralgia: a systematic review. Pain Physician 2019;22:209–28. [PubMed] [Google Scholar]
- 25.Wiesener S, Falkenberg T, Hegyi G, et al. Legal status and regulation of complementary and alternative medicine in Europe. Forsch Komplementmed 2012;19 Suppl 2:29–36. 10.1159/000343125 [DOI] [PubMed] [Google Scholar]
- 26.Bücker B, Groenewold M, Schoefer Y, et al. The use of complementary alternative medicine (cam) in 1 001 German adults: results of a population-based telephone survey. Gesundheitswesen 2008;70:e29–36. 10.1055/s-2008-1081505 [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y, Lao L, Chen H, et al. Acupuncture use among American adults: what acupuncture practitioners can learn from national health interview survey 2007? Evid Based Complement Alternat Med 2012;2012:1–8. 10.1155/2012/710750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu L-M, Li J-T, Wu W-S. Randomized controlled trials of acupuncture for neck pain: systematic review and meta-analysis. J Altern Complement Med 2009;15:133–45. 10.1089/acm.2008.0135 [DOI] [PubMed] [Google Scholar]
- 29.Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet 2005;366:136–43. 10.1016/S0140-6736(05)66871-7 [DOI] [PubMed] [Google Scholar]
- 30.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444–53. 10.1001/archinternmed.2012.3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen L-K, Arai H, Chen L-Y, et al. Looking back to move forward: a twenty-year audit of herpes zoster in Asia-Pacific. BMC Infect Dis 2017;17:213. 10.1186/s12879-017-2198-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deng H, Shen X. The mechanism of moxibustion: ancient theory and modern research. Evid Based Complement Alternat Med 2013;2013:1–7. 10.1155/2013/379291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Q-Y, Qu Y-Y, Feng C-W, et al. [Analgesic mechanism of acupuncture on neuropathic pain]. Zhongguo Zhen Jiu 2020;40:907–12. 10.13703/j.0255-2930.20190927-k0003 [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Li W, Peng W, et al. Acupuncture for postherpetic neuralgia: systematic review and meta-analysis. Medicine 2018;97:e11986. 10.1097/MD.0000000000011986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pei W, Zeng J, Lu L, et al. Is acupuncture an effective postherpetic neuralgia treatment? A systematic review and meta-analysis. J Pain Res 2019;12:2155–65. 10.2147/JPR.S199950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu YJ, Zhang QA, YY W. Meta-Analysis for efficacy and safety of electroacupuncture in treating postherpetic neuralgia. J Guangzhou Univ Tradit Chin Med 2020;37:2472–80. [Google Scholar]
- 37.Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med 2017;12:103–11. 10.1007/s11739-016-1583-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777–84. 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fashner J, Bell AL. Herpes zoster and postherpetic neuralgia: prevention and management. Am Fam Physician 2011;83:1432–7. [PubMed] [Google Scholar]
- 41.Lund I, Lundeberg T. Are minimal. superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med 2006;24:13–15. [DOI] [PubMed] [Google Scholar]
- 42.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins JPT, Li T, Deeks JJ. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.1. Cochrane 2020. [Epub ahead of print: Available from] www.training.cochrane.org/handbook [Google Scholar]
- 44.Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 46.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Melsen WG, Bootsma MCJ, Rovers MM, et al. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect 2014;20:123–9. 10.1111/1469-0691.12494 [DOI] [PubMed] [Google Scholar]
- 48.Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Statist. Sci. 1992;7:457–72. 10.1214/ss/1177011136 [DOI] [Google Scholar]
- 49.Dias S, Ades A, Welton N. Network meta-analysis for decision-making. Chichester, UK: John Wiley & Sons, Ltd, 2018. [Google Scholar]
- 50.Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol 2015;15:58. 10.1186/s12874-015-0060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dias S, Welton NJ, Sutton AJ, et al. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Making 2013;33:641–56. 10.1177/0272989X12455847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dias S, Welton NJ, Caldwell DM, et al. Checking consistency in mixed treatment comparison meta-analysis. Stat Med 2010;29:932–44. 10.1002/sim.3767 [DOI] [PubMed] [Google Scholar]
- 53.Sun N, Tu JF, Lin LL, et al. Correlation between acupuncture dose and effectiveness in the treatment of knee osteoarthritis: a systematic review. Acupunct Med 2019;37:261–7. 10.1136/acupmed-2017-011608 [DOI] [PubMed] [Google Scholar]
- 54.Giovanardi CM, Cinquini M, Aguggia M, et al. Acupuncture vs. pharmacological prophylaxis of migraine: a systematic review of randomized controlled trials. Front Neurol 2020;11:576272. 10.3389/fneur.2020.576272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bauer M, McDonald JL, Saunders N. Is acupuncture dose dependent? ramifications of acupuncture treatment dose within clinical practice and trials. Integr Med Res 2020;9:21–7. 10.1016/j.imr.2020.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chaimani A, Higgins JPT, Mavridis D, et al. Graphical tools for network meta-analysis in STATA. PLoS One 2013;8:e76654. 10.1371/journal.pone.0076654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salanti G, Del Giovane C, Chaimani A, et al. Evaluating the quality of evidence from a network meta-analysis. PLoS One 2014;9:e99682. 10.1371/journal.pone.0099682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Colloca L, Ludman T, Bouhassira D, et al. Neuropathic pain. Nat Rev Dis Primers 2017;3:17002. 10.1038/nrdp.2017.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dworkin RH, Panarites CJ, Armstrong EP, et al. Is treatment of postherpetic neuralgia in the community consistent with evidence-based recommendations? Pain 2012;153:869–75. 10.1016/j.pain.2012.01.015 [DOI] [PubMed] [Google Scholar]
- 60.Macone A, Otis JAD. Neuropathic pain. Semin Neurol 2018;38:644–53. 10.1055/s-0038-1673679 [DOI] [PubMed] [Google Scholar]
- 61.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002;136:374–83. 10.7326/0003-4819-136-5-200203050-00010 [DOI] [PubMed] [Google Scholar]
- 62.Goyatá SLT, Avelino CCV, Santos SVMD, et al. Effects from acupuncture in treating anxiety: integrative review. Rev Bras Enferm 2016;69:602–9. 10.1590/0034-7167.2016690325i [DOI] [PubMed] [Google Scholar]
- 63.Shergis JL, Ni X, Jackson ML, et al. A systematic review of acupuncture for sleep quality in people with insomnia. Complement Ther Med 2016;26:11–20. 10.1016/j.ctim.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 64.Liu Z-S, Peng W-N, Liu B-Y, et al. Clinical practice guideline of acupuncture for herpes zoster. Chin J Integr Med 2013;19:58–67. 10.1007/s11655-013-1191-y [DOI] [PubMed] [Google Scholar]
- 65.Caldwell DM, Ades AE, Higgins JPT. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005;331:897–900. 10.1136/bmj.331.7521.897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Corbett MS, Rice SJC, Madurasinghe V, et al. Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta-analysis. Osteoarthritis Cartilage 2013;21:1290–8. 10.1016/j.joca.2013.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li X, Wang R, Xing X, et al. Acupuncture for myofascial pain syndrome: a network meta-analysis of 33 randomized controlled trials. Pain Physician 2017;20:E883–902. [PubMed] [Google Scholar]
- 68.Wang T, Xu C, Pan K, et al. Acupuncture and moxibustion for chronic fatigue syndrome in traditional Chinese medicine: a systematic review and meta-analysis. BMC Complement Altern Med 2017;17:163. 10.1186/s12906-017-1647-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.