Abstract
To enhance mental health care for youth in a midwestern residential treatment facility, Wolverine Human Services partnered with the Beck Institute (an intermediary) and an implementation research team to implement cognitive-behavioral therapy (CBT). CBT has strong evidence supporting effectiveness for treating youth internalizing and externalizing problems, but it is a complex psychosocial intervention that demands a thoughtful implementation approach. This study outlines the implementation phase (2.5 years) of a 5-year collaborative effort. The implementation phase focused on (a) adapting CBT to fit the complex youth needs and the roles of the multidisciplinary team members resulting in a new comprehensive and coordinated care model, and (b) the strategies utilized to support its competent integration by all team members. Six blended implementation strategies were deployed in this phase: forging implementation teams, installing progress monitoring, adapting CBT, training, providing supervision and consultation, and training the trainers. A components-based approach to CBT yielded six core skills: active listening, problem solving, mood monitoring and intervention mapping, activity scheduling, distress tolerance, and cognitive restructuring. By the end of this phase, all staff had robust exposure to and experience with the adapted form of CBT. The work of our academic–community partnership has both research and clinical implications, with respect to integrating an adapted version of CBT for residential environments (CBT-RE).
Keywords: implementation, residential treatment, adaptation, training, cognitive-behavioral therapy
At least 20 evidence-based practices (EBPs) exist with relevance for residential treatment facilities (RTFs; James et al., 2017). Among these is cognitive-behavioral therapy (CBT), which is an approach that has the interplay between thoughts, emotions, and behaviors as its foundation. CBT is skills based, short term, and present focused, which are qualities that align well with the goals of RTFs. Indeed, a recent study found that RTFs participating in the Association of Children’s Residential Centers identified CBT as one of the primary treatments of choice for RTFs (James et al., 2015). This is unsurprising, as CBT has been widely studied and found to be effective for a wide array of mental health concerns in youth (Zhou et al., 2015). However, despite that 66 RTFs recently reported implementing CBT, James and colleagues’ study (2015) revealed that at least two major implementation challenges require significant attention to ensure successful integration: one, addressing the fit of the EBP, in this case CBT, with a teamwide/milieu-based approach; and two, ensuring implementation of the EBP (i.e., CBT) with fidelity.
Implementation science is the study of methods to incorporate EBPs into routine care settings, which offers solutions to address the care gap in RTFs (Bauer et al., 2015). A recent review reported that efforts to implement EBPs into RTFs have grown over the past decade—however, not much is known about what adaptations EBPs need to go through in order to fit the RTF context. James et al. (2017) highlighted the importance of fitting the EBP to the RTF target population (e.g., youth) or only providing certain elements of the EBP (e.g., core skills, such as behavioral activation), which can make the intervention more accessible and easier to train. The broader implementation science literature has recently focused on the elements and processes behind EBP adaptations. A systematic review identified the importance of collaborative adaptation between the organization and the EBP developer, and the need to maintain EBP core components (Escoffery et al., 2018).
However, even though EBP adaptations are often warranted, it remains critical to ensure that the core components are implemented with fidelity (i.e., as intended). Without fidelity to the core components, the desired effect will not likely be achieved. Traditionally, one-time workshops or continuing education sessions were the vehicle to transmit knowledge about an EBP. It is now known that an initial training to impart knowledge is necessary but not sufficient to implement an EBP with fidelity (Lopez et al., 2011). Workshops do not often lead to behavior change and, even if they do, the intervention is rarely delivered with fidelity due to lack of corrective feedback (Beidas et al., 2012; Forsetlund et al., 2009). Instead, ongoing supervision and consultation are needed (Edmunds et al., 2013). Yet, even with ongoing expert consultation, additional strategies, such as the use of implementation teams, are likely needed to address multilevel contextual barriers. Example barriers in RTF’s are negative provider attitudes and insufficient resources (James et al., 2017).
The current paper is Part 2 of a three-paper series describing the process of CBT implementation in a youth RTF across preimplementation/adoption (Scott et al., this issue), implementation (current study), and sustainment (Lewis et al., this issue). This paper outlines the implementation phase, which focuses on the adaptation of CBT to fit a milieu-based mental health setting and the challenges of delivering CBT with fidelity when the goal is for CBT to be delivered by all RTF staff, including paraprofessionals. Specifically, this paper details the implementation phase of a comprehensive CBT implementation effort and will (a) provide an overview of the CBT adaptation process, (b) present the core skills of CBT for an RTF setting, and (c) describe the implementation strategies central to this phase of work.
Setting Overview
Wolverine Human Services (WHS) is a youth RTF located in Michigan. WHS offers services across the state for over 250 male and female youth ages 12–21 in both secure (i.e., locked) and nonsecure facilities. Youth likely struggle with several mental health disorders (e.g., depression, anxiety), behavioral/delinquency problems (e.g., sexual, violent), truancy, or placement failures (e.g., foster care). The programs offer group and individual services, and family therapy, among others across the state. Staff at WHS are divided into two primary types: clinical and operations. Clinical staff consist of therapists, team managers, permanency treatment leaders, permanency planning specialists, clinical managers, and case managers. Therapists generally have a master’s in social work and provide therapeutic support to youth. Team managers typically have a bachelor’s degree and manage the operations within youth units or programs. Permanency treatment leaders have a bachelor’s degree and are responsible for delivery of CBT to youth and their families in support of their transition home. Clinical managers are master’s-level staff who manage operations for units and programs. Case managers are bachelor’s-level staff who ensure that youth are receiving personalized clinical care. Operations staff consist of youth care workers (YCW) and safety and support team coordinators (SSTs). YCW have high school diplomas and help ensure youth safety and security by maintaining line of sight. SSTs are bachelor’s-level staff who aid the YCW by providing guidance and direction, typically during times of crisis.
Implementation Overview
The Framework for Dissemination is an implementation model that highlights distinct implementation phases and provides guidance on the implementation process, as it succinctly delineates the contextual factors that might influence diffusion (Mendel et al., 2008). The model separates EBP diffusion into three stages, which aligns with the three parts of this series: (a) adoption (preimplementation), (b) implementation, and (c) sustainment. It also describes six domains that typically have an influence on implementation, such as the organization’s norms and attitudes, structure and process, resources, policies and incentives, networks and linkages, and media and change agents. This paper focuses on the implementation stage or phase, which includes configuring the EBP, determining how it will be used and adapted, and engaging in various implementation strategies (e.g., training, consultation) to ensure its meaningful integration.
The implementation phase began after CBT had been identified as the EBP to be integrated, completion of a mixed-methods (quantitative and qualitative) needs assessment to identify and prioritize CBT implementation barriers and facilitators, and 8 months of biweekly implementation team meetings to deploy strategies from the preimplementation blueprint (Scott et al., this issue). This 2.5-year implementation phase (of the 5-year partnership) was guided by its own blueprint (see Table 1) and composed of weeklong biannual site visits by the CBT intermediary and implementation research team for an intensive immersion (Lewis et al., 2018). A total of 19 strategies were articulated across the following eight categories for this phase of work: train and educate stakeholders, support clinicians, change infrastructure, develop stakeholder relationships, use evaluative and iterative strategies, provide interactive assistance, adapt and tailor to context, and utilize financial strategies. Ultimately, many of these discrete strategies were blended into multifaceted strategies. This paper elaborates on six key, blended strategies: implementation teams, progress monitoring, adapting CBT, training (which included shadowing experts), supervision and consultation calls (which included reminding clinicians, as well as modifying the context to prompt new behaviors), and train the trainers (which included identifying early adopters, capturing and sharing local knowledge, altering incentives through certification).
Table 1.
Implementation Blueprint (Reproduced From Lewis et al., 2018)
| Implementation category | Implementation strategy |
|---|---|
| Train and educate stakeholders/provide interactive assistance | Beck/IU training/supervision |
| Develop stakeholder interrelationships | Hold cross-staff clinical meetings |
| Adapt and tailor to context | Facilitate, structure, and promote adaptability (Beck to work with IT to modify CBT to fit the sites) |
| Train and educate stakeholders | Conduct educational outreach visits |
| Utilize financial strategies | Shift resources (ensure strategy for monitoring outcomes) |
| Develop stakeholder interrelationships | Identify early adopters (have person shadowed, talk in clinical meetings about overcoming barriers) |
| Provide interactive assistance | Provide clinical supervision—include IT on calls |
| Train and educate stakeholders | Use train-the-trainers strategies |
| Change infrastructure | Increase demand—present data to courts and state level |
| Support clinicians | Change performance evaluations, change professional roles |
| Use evaluative and iterative strategies | Develop and institute self-assessment of competency |
| Develop stakeholder interrelationships | Capture and share local knowledge |
| Support clinicians | Remind clinicians |
| Train and educate stakeholders | Prep CBT client handouts (Beck to provide examples) |
| Utilize financial strategies | Alter incentives (certification, vacation, salary) |
| Support clinicians | Facilitate relay of clinical data to providers (data parties) |
| Support clinicians | Modify context to prompt new behaviors |
| Train and educate stakeholders | Shadow other experts |
| Use evaluative and iterative strategies | Obtain and use consumer and family feedback (exit interviews and surveys) |
Note. IU = Indiana University; IT = implementation team; CBT = cognitive-behavioral therapy.
Six Blended Implementation Strategies: Process and Outcomes
Implementation Teams
The implementation teams consisted of clinician and operations staff champions and opinion leaders who had the primary goal of improving CBT barriers and preparing the RTF sites for CBT implementation. Between the biannual site visits, the implementation teams continued to have biweekly meetings, alternating between meetings with the intermediary to grow their CBT competency, and the lead implementation research team member to discuss strategy development and deployment. Implementation teams also aided in the development of materials, such as CBT handouts for staff, youth, and family handbooks. Ultimately, the implementation teams deployed 12 of the 19 implementation strategies from the blueprint during this 2.5-year phase of work (Lewis et al., 2018); 3 were not conducted at all (present data to courts, obtain and use consumer feedback, facilitate relay of clinical data to providers via data parties), whereas 4 were shifted to the sustainment phase (change performance evaluations, change professional roles, develop and institute assessment of competency, alter incentives). The six key implementation strategies appeared to have a major impact on WHS’s ability to integrate CBT, each of which are described in greater detail below.
Progress Monitoring
Progress monitoring was implemented very early in this phase to document the subsequent impact of CBT on youth outcomes throughout the implementation process and because it is a core component of CBT. To ensure progress monitoring was feasible and sustainable for the RTF, we reviewed free, brief, and psychometrically sound measures for implementation. Based on this review and in collaboration with the RTF, we decided to implement the Brief Problem Checklist (BPC; Chorpita et al., 2010), a standardized measure of internalizing and externalizing symptoms, and the Top Problems Assessment (TPA; Weisz et al., 2012), an individualized measure to complement the BPC. The progress monitoring system entailed a Microsoft Excel workbook, progress monitoring manual, and a tablet. Although we explored health information technologies in the form of measurement feedback systems to implement, we did not find one that would fit the needs and resources of the RTF. As such, we decided to create a Microsoft Excel workbook that would automatically calculate and graph the youth scores for the therapist in lieu of an established measurement feedback system.
During the first training visit (March, 2015), a 4-hour progress monitoring workshop informed by the theory of planned behavior (TPB; Ajzen, 1991) was conducted with 17 therapists. Prior to the workshop, a pretraining elicitation exercise was conducted via a web-based survey that sought to evaluate therapists’ current attitudes, subjective norms, and perceived behavioral control regarding progress monitoring (Casper, 2007; Francis et al., 2004). The elicitation exercise data informed the topics discussed and emphasized in the training, with therapists’ attitudes, subjective norms, and perceived behavioral control targeted to ultimately increase therapists’ intention to use progress monitoring. In addition, based on procedures used by Casper (2007), the workshop included a group consensus-building exercise focused on using progress monitoring through small-group discussion. Following the workshop, therapists were provided with a tablet with the Microsoft Excel workbook and progress monitoring manual, which had directions on how to use the Excel workbook and the two measures, already uploaded. Therapists saved a unique Excel workbook for each youth and, prior to the start of each therapy session, youth were provided with the tablet to fill out the progress monitoring forms. This allowed a systematic way for therapists and youth to fill out forms and keep track of outcomes over the course of therapy.
Within 1 month (and sustained thereafter), WHS achieved >90% penetration of progress monitoring—that is, all therapists were administering the BPC and TPA to youth before each session. However, there was some minimal user error in the data, such as forgetting to add specific session dates. It became an organizationwide expectation to have progress monitoring be the foundation of treatment. Therefore, progress monitoring was again the focus of an in-person training session during the next site visit, primarily to discuss standardization of data collection and entry, but also to collaboratively design how to utilize the data across providers and teams. There was some concern that sharing the youth’s individual goals beyond the therapist was inappropriate. This strategy was deprioritized and instead of sharing these potentially sensitive details with operations staff, the implementation teams decided to prioritize skills tracking, which appropriately could be shared with both clinical and operations staff working with the youth.
Adaptation of CBT
WHS as an organization decided to implement CBT into their setting (Scott et al., this issue). Prior to the implementation of CBT, approaches to treatment at WHS included behavior modification strategies, such as usage of a points system for managing undesirable behaviors, as well as the Therapeutic Crisis Intervention System, which focuses on de-escalating crisis situations (Residential Child Care Project, 2016). Despite dozens of protocols of CBT, none fit the needs of WHS in their current form. First, all staff needed to be able to deploy skills on the unit—that is, both clinical staff (e.g., therapists, case managers) and operations staff (e.g., YCW) would be delivering services, thus requiring that it be accessible to those who have no formal clinical training (i.e., paraprofessionals). Second, CBT needed to be transdiagnostic given that most youth at WHS had multiple diagnoses, including anxiety, mood disorders, oppositional defiant and conduct disorders, reactive attachment and intermittent explosive disorders, bipolar disorder, posttraumatic stress disorder, and borderline personality traits. The majority of youth at WHS struggled with externalizing problems and comorbid disorders. Third, treatment needed to enable coordination across team members (YCW, family workers, therapists) and settings (e.g., on the unit, at school, in home visits). Fourth, treatment needed to be accessible, engaging, and relevant to youth and their caregivers. Fifth, it needed to be freely available to limit financial burden—that is, WHS would not have to pay for outside training for their staff in perpetuity. Finally, specific interventions, techniques, or skills needed to be designed for deployment both within and outside of traditional one-on-one or group therapy sessions. To meet these parameters, a modular-based approach was prioritized. Although several modular youth-focused versions of CBT exist, such as Practice Wise Managing and Adapting Practice (Chorpita et al., 2014) and CBT+ (Dorsey et al., 2016), none met all of these parameters. Because of this, a core implementation strategy was a collaborative adaptation of CBT to best fit the context at WHS.
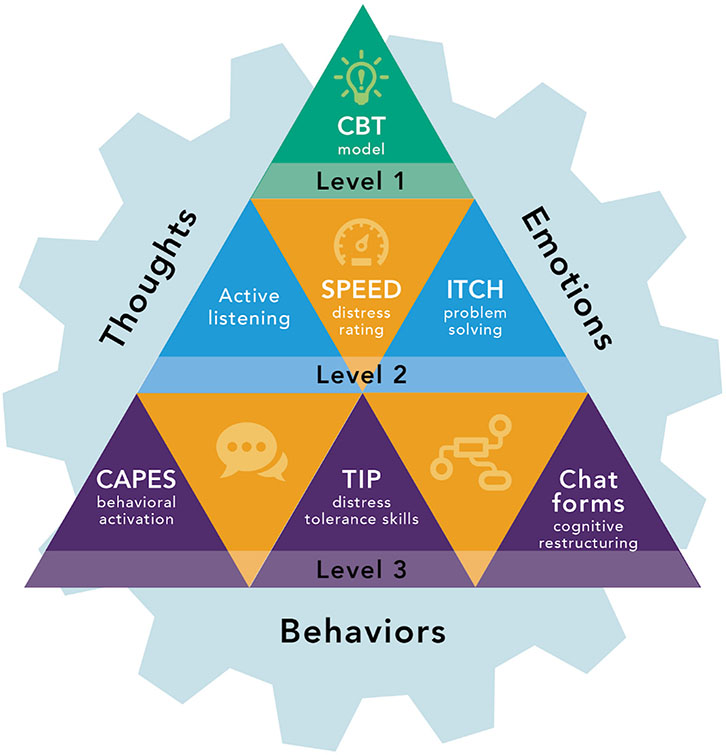
After identifying deficits among staff and carefully considering which minimal set of components of CBT could address the problems most often observed among youth in RTFs, the team prioritized six core skills for CBT for residential environments (CBT-RE) that were organized into three levels (see Figure 1). Level 1 included the CBT model and principles of behaviorism. Level 2 included active listening, mood identification and intervention mapping, and problem solving. Active listening was articulated as the first core CBT skill given its potential for relationship building and crisis diffusion; it would serve as a foundational skill for all youth and staff to use across situations. Mood monitoring and intervention mapping would ensure that youth and staff had a common language for discussing emotions and skills tailored to each youth. Problem solving was prioritized to address a clear deficit in youth and staff in terms of possible solutions to a specific problem that youth were facing, as well as promoting a level of control in youth. Level 3 included activity scheduling, distress tolerance, and cognitive restructuring skills. Activity scheduling would be particularly useful with depressed youth but would present all youth with a way to learn about what activities impact their mood and build resilience by ensuring each day was filled with antidepressant behaviors. Distress tolerance would ensure that all staff and youth could handle high-emotion/stressful situations. Finally, cognitive restructuring would diversify their skill sets and became accessible through CBT Chat Forms. The core CBT skills are detailed below—see Table 3 for the critical elements of each CBT core skill that forms CBT-RE. Core skills were chosen based on the main care gaps faced by the organization, examples of which are detailed below.
Figure 1.
CBT-RE model. Note. CBT = cognitive-behavioral therapy; SPEED = self-perceived excess energy and distress; ITCH = identify a problem, think of solutions, choose a solution, and how did it work?; CAPES = closeness, accomplishment, physical activity, enjoyment, sleep; TIP = toward engaging the senses, intense physical activity, and paced breathing.
Table 3.
Critical Elements of the CBT Core Skills
| Core skill | Critical elements |
|---|---|
| ITCH | Provide rationale Explain the acronym (i.e., What do the letters stand for?) Generate example of a common ITCH at WHS Describe when it is best to engage in problem solving (i.e., What SPEED?) |
| Active listening | Define emotion and thought empathy Provide three example reflection sentence stems Give two examples of thought and feeling empathy Explain why empathy is so important in a population of clients like this Engage in a 2-minute conversation without providing advice or asking a question |
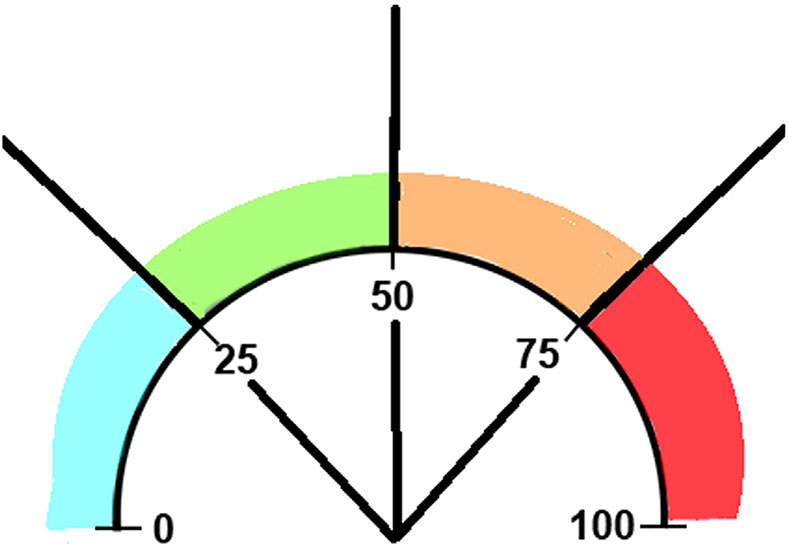
| SPEED maps | Draw SPEEDometer and describe each of the color zones on the map Blue = “cool” 0–25 Green = “go” 26–50 Orange = “warning” 51–75 Red = “danger” 76–100 Provide rationale for using SPEED maps Describe SPEEDometer metaphor Explain the importance of SPEED checks |
| CAPES | Closeness, accomplishment, physical activity, enjoyment, sleep Sleep routine Provide rationale for CAPES Generate at least five examples of each category that can be done on the unit Articulate the importance of scheduling CAPES in detail (what, when, where, who, how often, for how long, barriers) |
| TIP | Locate SPEED at which TIP is best used Provide rationale for TIP skills Explain the acronym Describe/do one guided activity for each letter/skill domain |
| CBT chat forms | Provide rationale Explain the purpose of the three Cs Generate a template + appropriate example Describe what “counts” as a situation Generate at least two questions that would help identify a teen’s thought, two for checking the thought, two for changing the thought Generate a list of at least 10 feeling words Describe three options for responding to thoughts |
Note. ITCH = identify a problem, think of solutions, choose a solution, and how did it work?; WHS = Wolverine Human Services; SPEED = self-perceived excess energy and distress; TIP = toward engaging the senses, intense physical activity, and paced breathing; CBT = cognitive-behavioral therapy.
Behaviorism and the CBT model.
Behaviorism offers a conceptualization of human behavior that focuses on how individuals respond to stimuli from the environment and how such responses are shaped through positive or negative reinforcement (Skinner, 1938). In the context of our work with WHS, it was quickly apparent that staff were inadvertently reinforcing undesirable behaviors. For instance, one youth received news that he could not attend his planned home visit, so he responded aggressively by flipping tables. This type of youth behavior often led to the use of physical restraint to prevent property damage or harm to others. However, even negative attention from multiple staff through physical restraint may reinforce aggression, increasing the likelihood that this youth will respond similarly in the future (Gallimore et al., 1969). Accordingly, principles of behaviorism, including punishment, reinforcement, shaping, and extinction, offered foundational strategies for staff working with youth. The CBT model was also prioritized, as it would provide staff and youth with a complementary lens through which they could better understand the connection among thoughts, behaviors, and emotions. The CBT model was introduced during training using various examples (e.g., text messaging1) and both staff and youth were encouraged to notice mood shifts and consider the model to more rapidly identify automatic thoughts and inform behavioral responses. Staff struggled most with applying principles of behaviorism, particularly when it related to the provision of negative attention to youth, as in the case of physical restraints mentioned above. Staff became proficient primarily through role plays with feedback during training site visits, where we re-created “scenes” on the unit to practice reinforcement of positive behavior among some youth while still maintaining line of sight for the safety of a youth engaging in undesirable behaviors, for example.
Active listening.
Active listening is considered a basic skill and common element of many psychotherapies, including CBT (Levitt, 2002). Active listening is a communication skill that involves one individual offering feedback that conveys attunement to the other individual’s feelings and emotions. Active listening demonstrates that you are listening and validating that it makes sense that they would feel a certain way. We prioritized active listening as a core skill because it is crucial in forming relationships, which are challenging for many youth in RTFs (Payton et al., 2000). Moreover, youth often enter RTFs like WHS with deficits in emotion regulation skills, and active listening helps them learn to identify and begin to regulate emotions more effectively (Linehan et al., 2015). Moreover, youth in crisis often respond with unsafe, aggressive behaviors (e.g., property destruction, yelling at staff) that can be dampened or resolved through staff validation. With active listening, staff were trained to discern between thought empathy and feeling empathy and how these two types of empathy can make youth feel that staff are actively engaged and understand the situation from the youth’s perspective. Active listening is particularly useful in times of crisis, but we emphasized that its relevance cuts across levels of youth distress and can be combined with all other skills. Two primary challenges emerged in trying to support staff to use active listening. First, staff immediately launched into problem solving with youth or intervening in some other way. Second, staff believed they were doing active listening well, which to them meant they asked a lot of good questions. To overcome these challenges, trainings centered on one-to-one practice with a trained observer offering constructive feedback.
Mood monitoring and intervention mapping.
Self-perceived excess energy and distress (SPEED) maps are a tool for monitoring mood and mapping effective techniques (i.e., adaptive coping skills) to different levels of distress. SPEED is based on the subjective units of distress scale (SUDS) that is often used in CBT for youth (Kendall et al., 2005). This skill was selected because youth were having difficulty understanding their levels of distress and they did not know which interventions to use when. The SPEED acronym enabled staff to enhance youth understanding of their emotions by comparing them to the speed of a car. Youth could be taught to monitor their speedometer, notice that they are in better control at lower speeds, and realize that higher speeds make it hard to respond effectively (see Figure 2). We prioritized SPEED maps as a core skill because it would help youth notice their emotions and quickly identify the most appropriate intervention in that moment. Staff could also use SPEED to quickly check in with youth about their level of distress and recommend interventions depending on distress level. Youth were encouraged to monitor their mood at least hourly via “SPEED checks” prompted by staff, and to employ interventions throughout the day to prevent high SPEED or to regulate emotions once their SPEED was high. Youth first completed a personalized SPEED map with individualized skills and interventions with their therapist. These personalized SPEED maps were then shared with YCW on the unit and were modified as needed based on skill effectiveness in the moment. The biggest challenge for this core skill was access to personalized SPEED maps for youth in the unit. To overcome this challenge, staff decided to put hard copies of each youth’s SPEED map in his or her daily log book, which allowed youth to access them in the moment and refine them in real time. Another challenge with SPEED maps was assigning appropriate interventions to various SPEEDs. We addressed this challenge through team-based games where staff submitted challenging youth scenarios and associated youth SPEEDs and they were asked to generate appropriate interventions within 30 seconds. Trainers assessed suggestions and offered points to teams for selecting appropriate interventions for the SPEED zone under consideration.
Figure 2.
SPEED map. Note. SPEED = self-perceived excess energy and distress. Blue = cool zone. At 0, the teen is totally relaxed and completely calm. As he or she approaches 25, there is an experience of mild distress and his or her energy levels are low. There is no interference with the teen’s ability to engage in activities. Green = go zone. As the teen moves away from 25 and toward 50, the distress becomes uncomfortable and/or energy levels are somewhat disruptive. Concentration is affected, but the teen is able to continue on. Orange = warning zone. As the teen moves from 50 toward 75, the distress is increasingly uncomfortable and/or excess energy is observable. The teen is preoccupied with the symptoms of distress and finds it very difficult to concentrate. The teen is considering escaping from the situation. Red = danger zone. At 100, the distress is at the highest the teen has ever experienced and/or he or she appears to be out of control. The teen is unable to concentrate or think rationally.
Problem solving.
Identify a problem, think of solutions, choose a solution, and how did it work? (ITCH) is a problem-solving technique that allows youth to cope with stressors (Creed et al., 2011; Muñoz et al., 2000). This core skill was selected due to an empirically established relation among aggressive behavior, emotional impulsivity, and dysfunctional decision making (Kuin, Masthoff, Kramer, & Scherder, 2015). We included ITCH so that youth would have step-by-step guidelines for effective problem solving, to aid them in identifying alternatives to impulsive and aggressive behaviors, and to increase their sense of control over their environment, a critical component for youth mandated into RTF. Youth used ITCH to constructively identify a problem, brainstorm possible solutions, and evaluate the outcomes of that solution. Staff, notably YCW, provided suggestions and guided youth’s ITCH problem-solving efforts. The challenges observed during ITCH implementation were similar to its use in other settings, notably that staff and youth had difficulty identifying the specific problem and brainstorming without immediately/simultaneously evaluating the choices. These challenges were overcome with focused practice and feedback.
Activity scheduling.
Activity scheduling reflects five antidepressant activity domains that informed tailored behavioral activation for youth: closeness, accomplishment, physical activity, enjoyment, and sleep (CAPES). We selected activity scheduling due to behavioral activation’s efficacy in treating depression (Cuijpers et al., 2007), which is very common among youth in RTFs. Youth were taught that intentionally striving for these types of activities each day can make it easier to handle challenging situations and prevent prolonged distress. Each morning, youth filled out a CAPES form with intended activities to complete throughout the day with a focus on activities that were specific, concrete, and achievable (i.e., able to do within the setting). Staff encouraged youth to engage in their CAPES activities and to review CAPES sheets during evening reflection (i.e., time spent with a YCW to review outcomes from the day) to consider the impact of the activities on their mood and overall well-being. The biggest challenges when implementing activity scheduling included the intentionally structured day that WHS imposed on youth combined with their limited access to resources (e.g., especially in the secure site many activities, like jump rope, were considered dangerous) and behavioral restrictions (e.g., no leaving the unit). This took immense creativity to clarify the universe of possibilities within the structured and restricted setting, but also invited some loosening of the otherwise risk-averse culture.
Distress tolerance.
Distress tolerance is a set of techniques from dialectical behavior therapy (Linehan et al., 2015) that help youth regulate their emotions when they are in the most intense end of their spectrum of distress, or SPEED. Like Linehan, we used the acronym TIP, which was slightly modified and represents activities that are geared toward engaging the senses, intense physical activity, and paced breathing. These skills were meant to provide youth with a distraction from their intense distress until arousal began to reduce, at which time youth were encouraged to employ other skills. TIP interventions also calm physiological symptoms of distress. Staff coached youth to use TIP to reduce their SPEED in the moment by offering stimuli for activities that would engage the senses or encouraging intense physical activity, for instance. The biggest challenge in integrating TIP into this residential setting was the intentional limited access to materials to engage in the skill (e.g., ice, cold water, self-soothing lotions). Early on in implementation, WHS invested in solutions, such as having a “self-care kit” in translucent plastic backpacks, but they ultimately removed these due to safety concerns (e.g., youth used elements of the backpack as weapons). To overcome this challenge, youth were encouraged to prioritize intensive exercise and paced breathing, and when possible, regulate their temperature.
Cognitive restructuring.
CBT chat forms are cognitive restructuring worksheets (i.e., a thought record) that were named by WHS and used to explore youth’s distressing reactions to situations. This strategy helped youth identify automatic thoughts and correct maladaptive interpretations that occur across emotional disorders (Koster et al., 2009). Staff (clinical and operations) could guide youth through a CBT chat form, thereby helping both staff and youth understand the youth’s emotional reactions and patterns in thinking. Youth also gained skills in evaluating thoughts on their own with the goal of eventually using the skill without the aid of the chat form. See Figure 3 for an example chat form. Cognitive restructuring is perhaps the most challenging skill for both staff and youth given the complexities and nuances in terms of differentiating thoughts and feelings, catching automatic thoughts in an unfiltered way, identifying hot thoughts, articulating evidence for and against thoughts, and generating balanced/alternative ways of thinking. To simplify the process, WHS came up with the CBT chat forms, which allowed for integration of various cognitive skills in a streamlined, accessible format.
Figure 3.
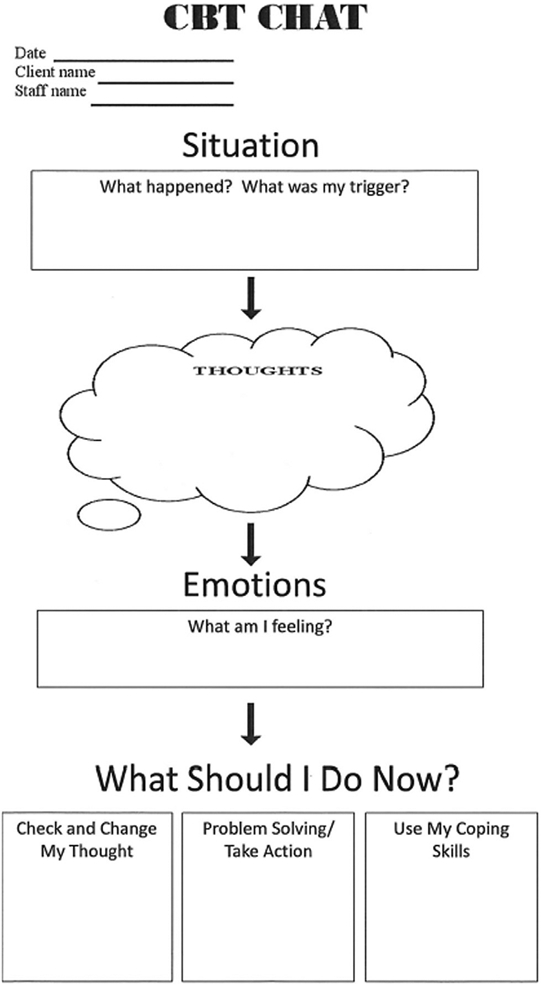
CBT chat form. Note. CBT = cogntive-behavioral therapy.
Training
A total of seven on-site training visits were conducted, the descriptions of which can be found in Table 2. In general, earlier trainings focused on introductory, foundational content (e.g., What is CBT? How do you assess mental health problems?) and then moved into more nuanced, advanced content (e.g., how to differentially integrate CBT into your specific role). Consistent with the literature on active learning, all trainings included only brief didactic elements followed by trainee engagement in interactive activities to maximize knowledge gain and behavior change (Lyon et al., 2016). Activities included demonstration, role play and feedback, games, spontaneous case examples, and competency assessment.
Table 2.
Description of Training Visits
| Training visit | Training/meeting topic | Staff in attendance |
Content | Number of sessions |
Phase of diffusion |
|---|---|---|---|---|---|
| #1 March 2015 | Administration Meeting Introduction to CBT General Competencies Train-the-Trainer Assertiveness Training NSSI and Acting Out Principles of Behaviorism Assessment and Documentation Progress Monitoring |
CLM, RCC, PM All All TT, ST, CD All All All TH, CLM, CA TH, CLM, CA |
Discussing reassessment outcomes Introducing staff to CBT Focused on general treatment competencies (e.g., relationship) Orienting administrative staff around the train-the-trainer model How to effectively be assertive with clients and colleagues Interacting with clients displaying NSSI and behavior disruptions Training on the foundations of behaviorism Informing staff about the importance of treatment assessment Training staff on how to integrate progress monitoring |
14 | Implementation |
| #2 August 2015 | CBT Competencies Specific CBT Techniques Data Collection/Progress Monitoring Implementation Team Meetings |
TH, CM All TH IT |
Articulating core competencies of CBT Introducing specific CBT techniques (e.g., cognitive restructuring) Reintroducing progress monitoring Meeting to coordinate with implementation teams |
14 | Implementation |
| #3 March 2016 | Problem-Solving Treatment Daily CBT Integration Progress Monitoring Follow-Up Core Beliefs and Behavioral Experiments Motivational Interviewing Putting CBT First Expert Cohort Session Implementation Teams |
All All TH TH CT SM CT IT |
Introduction to cognitive model problem-solving techniques Training on using CBT techniques throughout daily care Follow-up on the implementation of progress monitoring Training on techniques to address core beliefs (e.g., experiments) Teaching staff to integrate motivational interviewing into treatment Changing culture to prioritize CBT as a first-line approach Working with clinical staff to understand barriers to change Meeting with the implementation teams to reorient goals |
8 | Implementation |
| #4 November 2016 | Train-the-Trainer, Part 1 CBT in Session Core Skills—Developing Competency Imagery Rehearsal CBT Sustainment Train-the-Trainer, Part 2 |
CC TH All TH IT CC |
Orienting administrative staff around the train-the-trainer model Training therapists on effectively using CBT in therapy session Using CBT core skills competently Using evidence-based technique to reducing recurring nightmares Introducing methods for program sustainment Orienting administrative staff around the train-the-trainer model |
8 | Implementation |
| #5 March 2017 | CBT Endorsement CBT Supervision CBT Endorsement Principles of Behaviorism How to Use Core CBT Skills in Your Role Integrating Core Skills in Session Case Conceptualization |
CC CC CC, IT, PM/PS, TH All All CC, TH |
Introducing the CBT endorsement process to CBT coaches Establishing CBT-oriented supervision sessions Introducing the CBT endorsement process to staff Refreshing the principles of behaviorism Showing all staff how to integrate CBT in their daily roles How to use CBT core skills in therapy sessions Practicing the application of cognitive conceptualization |
7 | Sustainment |
| #6 October 2017 | Endorsement Process Implementation Team Meeting CBT and Family Therapy Using Level 1 CBT Skills Core Skills Refresher Point System Intake Checklist Core Skills Follow-Up |
CC IT FT All All All TH, IT, FT FT, PS |
Laying out the endorsement process to CBT coaches Meeting with the implementation teams regarding endorsement Integrating CBT techniques into family therapy Training on how to use core skills on oneself Training staff over core skills again, led by implementation team Introducing staff to the consequences of giving negative rewards Covering the intake checklist with clinical staff Reviewing core skills with family therapists |
12 | Sustainment |
| #7 July 2018 | Sustainment Meeting Reinforcement System Implementation Teams Family Handbook/CBT Core Skills Bringing CBT to Family Therapy CTRS for Therapists Core Skills Refresh/Incident Reports Intake Checklist Client Skills Tracker CBT Coaches |
AS PM, TH, CT IT FT, PS FT, PS TH AS TH, CM TH, CM, PM CC |
Meeting with vice president covering sustainment needs Introducing the new reinforcement system Meeting covering sustainment tasks and team-building exercise Introducing the family therapy handbook/refresher on core skills Covering how to integrate core skills in family sessions Practice scoring therapy sessions for supervision Refresher on CBT core skills and using CBT in incident reports Covering how to use the intake checklist effectively Practicing use of the CBT skills tracker Exit meeting, sustainment follow-up, Q&A |
14 | Sustainment |
Note. CBT = cognitive-behavioral therapy; NSSI = nonsuicidal self-injury; CTRS = cognitive Therapy Rating Scale; CLM = clinical manager; RCC = residential care coordinator; PM = program manager; All = all staff; TT = transformers team; ST = staff trainer; CD = clinical director; TH = therapist; CA = clinical assistant; CM = case manager; IT = implementation team; SM = site management; CT = clinical team; CC = CBT coach; PS = program supervisor; FT = family therapist; AS = administrative staff.
As trainings and site visits progressed, external intermediaries tapered their involvement to prepare on-site staff to train others. For instance, after the second training visit, WHS staff began leading training sessions focused on CBT “Core Skills Refresh.” This tapering strategy was vital, because having WHS staff who were early CBT adopters lead trainings offered a powerful message of support for CBT across diverse staff roles. WHS staff trainers received ongoing support from the intermediaries and were provided with standardized training slides with associated activities and handouts. The Core Skills Refresh was a 4-hour session hosted at each site at all subsequent visits, allotting 30 minutes to each skill. The 30-minute slot utilized the following structure: two staff jointly present a very brief standardized slide deck (core skill and critical elements defined, examples provided), staff conduct demonstration of the core skill, group discussion reflecting critical elements they observed in the demonstration, and dyadic practice with coaches and trainers floating and providing feedback. The regularity of the booster training sessions ensured that new staff were offered active learning opportunities and staff familiar with the skills were less likely to drift from fidelity in their delivery.
Training visits themselves surfaced several challenges. Given the size of the trainings (e.g., up to 100 people in a given session) and our need to observe staff practice and offer real-time feedback, we prioritized in-person weeklong site visits. Unfortunately, this often meant long days on top of the typical work that many staff still needed to complete. Staff attitudes, particularly from new YCW (new due to constant turnover), were unfortunately poor, which manifested in nonparticipation, walking out of the trainings, and even making disparaging remarks to the trainers about their perceived lack of competence. Our approach to shifting culture and improving attitudes was multifaceted. First, the implementation teams developed a code of conduct that, for example, led to cell phones being put away during meetings and sharing concerns with suggestions for solutions. We also used positive reinforcement (e.g., providing candy for participation), active learning strategies (e.g., demonstrations, role plays tailored to specific problems they were having), and the use of CBT success stories—that is, other staff sharing how CBT has been helpful with their youth. Finally, we selected opinion leaders from typically disengaged staff roles (e.g., YCW) to lead core skills training to model engagement and channel peer respect.
Consultation calls
Consultation calls with the implementation teams occurred on a biweekly basis and alternated between two topics: (a) implementation consultation (once a month) and (b) clinical consultation (once a month). The implementation support calls focused on deploying the strategies from the blueprint to address the barriers identified in the original needs assessment. The meetings were run by the implementation team chair and documented by the secretary to ensure progress month-to-month. When new barriers emerged, such as issues regarding buy-in within specific staff roles, the implementation teams identified them swiftly and took action. For example, early on it was noted that the YCW were not utilizing CBT in response to crises on the unit. To increase their buy-in and competence with distress tolerance skills, YCW team members were selected to train their peers in these skills in the next Core Skills Refresh session.
The clinical consultation calls focused on identifying and discussing challenging clinical cases. The implementation teams would present the case, discuss their CBT efforts to date, and then the intermediary modeled how to apply the skills. The implementation teams felt hopeful about the discussions held during the clinical calls, as they were able to better understand (using cognitive case conceptualization) and select interventions for cases they felt had no “solution.” Eventually the intermediary began using Socratic dialogue to engage the team in self-consultation.
Train the trainers
We used a train-the-trainers approach to identify and grow on-site experts to ensure CBT sustainment (Martino et al., 2011). The train-the-trainer model consists of trainers teaching supervisors, and then supervisors training the front-line staff, an approach that has been shown to aid in the dissemination and implementation of EBPs (Nakamura et al., 2014; Pearce et al., 2012). Train the trainers was a blended, multifaceted implementation strategy that included identifying early adopters, capturing and sharing local knowledge, and altering incentives through certification. Coaches were selected by WHS administrators based on their general therapy skills, aptitude for CBT per early demonstration of skill, leadership potential, and intention to stay at WHS. They received weekly training and group supervision from a faculty member at the Beck Institute. The meetings started off on a weekly basis and focused on reviewing recordings from sessions and discussing clinical cases in which they were experiencing difficulties. The goal of such meetings was for the coaches to learn a flexible CBT approach through the use of the cognitive case conceptualization. In some cases, the skills they learned went beyond the core CBT skills, such as exposure and trauma-based work.
Each week, one of the coaches was tasked with selecting one recording of a session and rating it for competency on the Cognitive Therapy Rating Scale (CTRS; Young & Beck, 1980). Initially, sharing their session recordings was anxiety provoking and providing feedback to peers was difficult. However, the intermediary utilized role-playing strategies to normalize and model such behaviors. Once coaches earned the current gold standard competency rating score of 40+ on the CTRS for two consecutive sessions, they were put forth for certification by the Academy of Cognitive Therapy2 All CBT coaches were successfully certified by the Academy of Cognitive Therapy by the end of the implementation phase. Subsequently, coaches were trained to provide CBT supervision and complete CTRS ratings for other therapists, given that creating a pathway to certification was a prioritized implementation strategy for the sustainment phase (see Part 3 of this special series; Lewis et al., this issue). In this training phase, the CBT coaches provided feedback to one another on the CTRS first, and then received feedback from the Beck Institute intermediary on how they delivered CTRS results. The meetings later moved to review of coach supervision sessions conducted with other staff and clinicians. To assuage concerns about CBT supervision competence, supervision on supervision was slowly phased out by first switching from weekly to biweekly, then to monthly, and then to every 3 months. The booster sessions provided evidence that the coaches were capable of providing CBT without the intermediary.
Discussion
This study offered a detailed account of the implementation phase of a comprehensive CBT implementation effort in an RTF. Specifically, the study focused on detailing the adaptation of CBT to fit the RTF context and core implementation strategies to address multilevel implementation barriers identified in the initial needs assessment to ensure CBT’s delivery with fidelity. The six multifaceted implementation strategies deployed in this phase included developing implementation teams, instituting progress monitoring, adapting CBT, training, providing consultation, and training the trainers. The effects of the strategies deployed in this phase were profound, but the work was not complete until the team moved through a 1-year sustainment phase during which several new strategies were deployed, as is described in the third part of this special series (Lewis et al., this issue).
CBT has been shown to be effective for youth (Zhou et al., 2015). Nonetheless, most efficacy and effectiveness studies do not take place in the settings for which they are intended, which may explain subsequent implementation failures. Mental health needs are alarmingly high in RTFs and remain unaddressed, yet implementation science has only recently started to reveal barriers to implementation and potential implementation strategies for these settings (James, 2017). At the start of this study, no relevant CBT approaches were available for the RTF setting. Consistent with a recent systematic review (Wiltsey Stirman et al., 2017), collaboratively adapting CBT to fit the context was a crucial implementation strategy for this phase. Fortunately, more and more team-based options for delivering CBT are emerging for settings like these, including one from a similar study implementing team-based CBT in a juvenile justice setting (Valentine et al., 2019). Fewer resources are needed to make the minor modifications that will move these novel modular or component-based approaches into new settings.
Indeed, a modularized approach to treatment with youth has been shown to be effective and can be a great starting point for CBT adaptation into various settings (Weisz et al., 2012). Working with modules (i.e., free-standing sessions or topics) allows a nonlinear approach to treatment that can be tailored to an individual youth’s specific needs and provide flexibility to the service provider. Fit of the intervention was not measured quantitatively, but rather iteratively throughout the collaboration process. Although analyses are underway to explore the impact of fidelity to CBT-RE in WHS on youth outcomes as obtained in the progress monitoring, qualitative anecdotal data suggest that important impacts were observed that could be indicative of implementation success. For instance, the WHS clinical director sent this e-mail regarding the decrease in number of physical restraints in the unit: “Exciting new Performance and Quality Indicators data in. Secure site is at the lowest restraint number in years … and at 100% maximum capacity.” Also, a therapist reported, “My ability to use skills went from ‘Sure, I am willing to give this a try’ to ‘Hey, this stuff works,’ and I am now to the point where I am using it daily and having conversations with my staff when I see them miss an opportunity to use a skill.” Another therapist said, “I used to use a ‘talk at them’ approach to clinical work, and I thought I was pretty good at it. Nevertheless, after learning about how to implement true CBT, my clients not only behave better, they report feeling better. I’ve learned that I used to just get compliance and now I am helping clients effect real change in their lives.”
Despite these illustrations of success, it should also be highlighted that training all staff versus just therapists can be a challenge but is important because other staff (e.g., YCW) interact more frequently with youth—that is, therapists typically see the youth 1–3 hours each week, whereas YCW’s maintain 24-hour contact with the youth. Forgoing training with these staff members presents a missed opportunity. Ultimately, the goal of CBT is to train youth to be their own therapist by internalizing the skills. By including them in the CBT implementation process, the YCW may be better able to support the youth in applying the core skills throughout their day and ideally upon their departure back in their communities. Training paraprofessionals in CBT is made easier with a core skills-based approach like that which emerged from our adaptation. However, few RTFs have taken this approach, perhaps because of the daunting training task associated with such a goal (James et al., 2015). For instance, even though WHS prioritized YCW involvement in the CBT training sessions, they struggled to ensure their attendance at the trainings because they still needed to maintain line-of-sight ratios. YCWs who were able to attend often displayed disinterest in the content of the trainings given a common perception that the youth were “bad” and simply needed to be disciplined. These implementation barriers were addressed to the best of WHS’s ability by introducing CBT principles in their orientation for new staff, as well as having safety and support team members cover the units so that YCW could be in attendance of trainings and by having senior YCWs lead training sessions with recent examples. Additionally, over time, staff were able to witness in the units that using the other core skills, such as active listening, prevented escalation. Overall, we believe that the organization experienced a culture shift that was inspired by engaging staff at all levels, intentionally bringing opinion leaders onto the implementation teams, and creating opportunities for them to see how well CBT worked.
Indeed, our training approach was quite comprehensive and included didactic training, group consultation, and training by early (and late) adopters, as well as shadowing. Each component and strategy within the training approach was selected to target known and emergent implementation barriers with an eye toward sustainment. For example, active learning strategies were integrated into every training session throughout implementation. This decision was important given that active learning has been associated with improved skills (Cross et al., 2011). We also used a train-the-trainers approach in which we selected CBT expert cohorts to become coaches that would continue training once the intermediary left the organization. Train-the-trainer approaches have demonstrated improved patient outcomes, improved EBP knowledge, and change in skills (Nakamura et al., 2014). All of these discrete implementation strategies were complementary, yet more work is needed to determine whether all are needed given the resource-intensive nature of this multifaceted approach.
The implementation teams led the deployment of 12 of the 19 planned strategies (Lewis et al., 2018). To be clear, there were several strategies that were deployed but were not a major focus of this paper, such as the preparation of CBT core skill handouts and games, as well as youth, family, and staff CBT core skill handbooks. Although important, these strategies are quite straightforward and warrant less reflection in our detailed account. Four key strategies were moved to the sustainment phase: development of competency assessments, change in the professional role descriptions, change in role evaluations, and altering incentives for achieving competence with CBT (Lewis et al., 2018). Although the implementation teams began work on these strategies in the implementation phase, the primary reason for moving these strategies to sustainment is that the version of CBT continued to be adapted in the implementation phase and these strategies required the CBT to be in its “final” form. Three planned strategies were not deployed at all. The teams did not present data to courts despite the belief that it would be important to influence the courts to make length-of-stay decisions based on skill development or clinical goals. Unfortunately, the teams felt this was a lofty goal and so deprioritized it. The teams did not formally obtain consumer and family feedback, but youth feedback was present in every discussion the teams had. Finally, as noted above, relaying clinical goals in the form of data parties was deprioritized because there was ongoing concern that this type of information was sensitive and private to be held in confidence between the therapist and the youth, in part out of fear that operations staff could misuse the data.
Despite the success of this implementation phase, this study has several limitations. First, given the pragmatic nature of this study, it is unclear the extent to which of the CBT core skills are necessary or translatable. For example, are all components needed? What are the mechanisms of action of these strategies? Would other teams need to make major adaptations to fit their context or could they use CBT-RE in its current form and implement it into their setting? Second, turnover was a big challenge throughout the study, particularly at the YCW level. Third, there were challenges and difficulties in collecting pragmatic objective data on implementation and much of what was gathered was qualitative or collected during pre- and posttrainings. Last, there was no comparison group in this implementation project. Thus, it is unclear how outcomes would have changed over time without the CBT implementation effort. Nonetheless, this study offers an exemplar to the field on how to adapt and implement CBT into a youth residential setting. Future research is needed, notably randomized implementation–effectiveness hybrid trials would significantly advance our understanding of how to improve mental health care for youth in RTFs.
Conclusions
This study described the implementation phase of an academic–community partnership aimed at implementing CBT into an RTF. Details regarding the collaborative adaptation of CBT are provided, resulting in six core skills collectively referenced as CBT-RE that can be used for youth with transdiagnostic disorders in residential environments. Six key multifaceted implementation strategies were deployed and described in detail for ease of replication. This implementation process offers an exemplar for others looking to take a comprehensive and collaborative approach to implementing EBPs into complex team-based care settings for youth.
Acknowledgments
Kelli Scott is funded by a T32 AA 007459; PI: Peter Monti.
Footnotes
Cognitive behavioral therapy (CBT) is based on the idea that situations don’t determine how we react, it’s our interpretation of them. For example, imagine that you sent a text message to a friend and she hasn’t texted you back after three hours. If you have the thought, “She’s ignoring me” you may feel mad and choose to ignore her text when she gets back to you the next day. If you have the thought, “She doesn’t care about me” you may feel rejected and decide not to bother her with your texts in the future. If you have the thought, “She has a lot on her plate right now” you might feel concern for her and send a follow up text the next day to see how she’s doing. As can be seen, it’s how we interpret situations that drives how we feel and what we choose to do in response. In CBT we help teens learn to catch automatic thoughts (interpretations) and replace them with more accurate and helpful ways of making sense of situations so they get to feel better and act in ways consistent with their goals.
The Academy of Cognitive Therapy certification was pursued prior to the creation of the Beck Institute Certification.
Authors have no conflicts of interests.
Contributor Information
Natalie Rodriguez-Quintana, Indiana University.
Cara C. Lewis, Kaiser Permanente Washington Health Research Institute
Kelli Scott, Brown University.
Brigid Marriot, University of Missouri.
Sarah Wahlen, Indiana University.
Robert Hindman, Beck Institute for Cognitive Behavior Therapy.
References
- Ajzen I (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- Bauer MS, Damschroder L, Hagedorn H, Smith J, & Kilbourne AM (2015). An introduction to implementation science for the non-specialist. BMC Psychology, 3(1), 32. 10.1186/S40359-015-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidas RS, Edmunds JM, Marcus SC, & Kendall PC (2012). Training and consultation to promote implementation of an empirically supported treatment: A randomized trial. Psychiatric Services, 63(7), 660–665. 10.1176/appi.ps.201100401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casper ES (2007). The theory of planned behavior applied to continuing education for mental health professionals. Psychiatric Services, 58(10), 1324–1329. 10.1176/ps.2007.58.10.1324. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, & Collins KS (2014). Managing and adapting practice: A system for applying evidence in clinical care with youth and families. Clinical Social Work Journal, 42(2), 134–142. 10.1007/s10615-013-0460-3. [DOI] [Google Scholar]
- Chorpita BF, Reise S, Weisz JR, Grubbs K, Becker KD, & Krull JL (2010). Evaluation of the brief problem checklist: Child and caregiver interviews to measure clinical progress. Journal of Consulting and Clinical Psychology, 78(4), 526–536. 10.1037/a0019602. [DOI] [PubMed] [Google Scholar]
- Creed TA, Reisweber J, & Beck AT (2011). Cognitive therapy for adolescents in school settings. Guilford Press. [Google Scholar]
- Cross WF, Seaburn D, Gibbs D, Schmeelk-Cone K, White AM, & Caine ED (2011). Does practice make perfect? A randomized control trial of behavioral rehearsal on suicide prevention gatekeeper skills. Journal of Primary Prevention, 32(3–4), 195–211. 10.1007/s10935-011-0250-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, & Warmerdam L (2007). Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review, 27(3), 318–326. 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Dorsey S, Berliner L, Lyon AR, Pullmann MD, & Murray LK (2016). A statewide common elements initiative for children’s mental health. Journal of Behavioral Health Services and Research, 43(2), 246–261. 10.1007/s11414-014-9430-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmunds JM, Beidas RS, & Kendall PC (2013). Dissemination and implementation of evidence-based practices: Training and consultation as implementation strategies. Clinical Psychology: Science and Practice, 20(2), 152–165. 10.1111/cpsp.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escoffery C, Lebow-Skelley E, Haardoerfer R, Boing E, Udelson H, Wood R, Hartman M, Fernandez ME, & Mullen PD (2018). A systematic review of adaptations of evidence-based public health interventions globally. Implementation Science, 13(1), 125. 10.1186/s13012-018-0815-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsetlund L, Bjørndal A, Rashidian A, Jamtvedt G, O’Brien MA, Wolf F, Davis Dave, Odgaard-Jensen Jan, & Oxman AD (2009). Continuing education meetings and workshops: Effects on professional practice and health care outcomes (review). Cochrane Library, 2(2), 2–4. 10.1002/14651858.CD003030.pub2.Copyright. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis JJ, Eccles MP, Johnston M, Walker A, Grimshaw J, Foy R, Kaner EFS, Smith L, & Bonetti D (2004). Constructing questionnaires based on the theory of planned behaviour: A manual for health services researchers. Newcastle upon Tyne: University of Newcastle. [Google Scholar]
- Gallimore R, Tharp RG, & Kemp B (1969). Positive reinforcing function of “negative attention”. Journal of Experimental Child Psychology, 8(1), 140–146. 10.1016/0022-0965(69)90035-6. [DOI] [Google Scholar]
- James S (2017). Implementing evidence-based practice in residential care: How far have we come? Residential Treatment for Children and Youth, 34(2), 155–175. 10.1080/0886571X.2017.1332330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S, Thompson RW, & Ringle JL (2017). The implementation of evidence-based practices in residential care: Outcomes, processes, and barriers. Journal of Emotional and Behavioral Disorders, 25(1), 4–18. 10.1177/1063426616687083. [DOI] [Google Scholar]
- James S, Thompson RW, Sternberg N, Schnur E, Ross JR, Butler L, Triplett D, Puett L, & Muirhead J (2015). Attitudes, perceptions, and utilization of evidence-based practices in residential care. Residential Treatment for Children and Youth, 32(2), 144–166. 10.1080/0886571X.2015.1046275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Robin JA, Hedtke KA, Suveg C, Flannery-Schroeder E, & Gosch E (2005). Considering CBT with anxious youth? Think exposures. Cognitive and Behavioral Practice, 12(1), 136–148. 10.1016/S1077-7229(05)80048-3. [DOI] [Google Scholar]
- Koster EHW, Fox E, & MacLeod C (2009). Introduction to the special section on cognitive bias modification in emotional disorders. Journal of Abnormal Psychology, 118(1), 1–4. 10.1037/a0014379. [DOI] [PubMed] [Google Scholar]
- Kuin N, Masthoff E, Kramer M, & Scherder E (2015). The role of risky decision-making in aggression: A systematic review. Aggression and Violent Behavior, 25, 159–172. 10.1016/j.avb.2015.07.018. [DOI] [Google Scholar]
- Levitt DH (2002). Active listening and counselor self-efficacy. Clinical Supervisor, 20(2), 101–115. 10.1300/J001v20n02_09. [DOI] [Google Scholar]
- Lewis CC, Scott K, & Marriott BR (2018). A methodology for generating a tailored implementation blueprint: An exemplar from a youth residential setting. Implementation Science, 13(1), 1–13. 10.1186/s13012-018-0761-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CC, Scott K, Rodriguez-Quintana N, Hoffacker C, Boys C, & Hindman R (this issue). Implementation of the Wolverine Mental Health Program, Part 3: Sustainment phase. Cognitive and Behavioral Practice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, McDavid J, Anne Comtois K, & Murray-Gregory AM (2015). Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiatry, 72(5), 475–482. 10.1001/jamapsychiatry.2014.3039. [DOI] [PubMed] [Google Scholar]
- Lopez MA, Osterberg LD,Jensen-Doss A, & Rae WA (2011). Effects of workshop training for providers under mandated use of an evidence-based practice. Administration and Policy in Mental Health and Mental Health Services Research, 38(4), 301–312. 10.1007/s10488-010-0326-8. [DOI] [PubMed] [Google Scholar]
- Lyon AR, Lewis CC, Melvin A, Boyd M, Nicodimos S, Liu FF, & Jungbluth N (2016). Health information technologies—academic and commercial evaluation (HIT-ACE) methodology: Description and application to clinical feedback systems. Implementation Science, 11(1), 128. 10.1186/s13012-016-0495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Ball SA, Nich C, Canning-Ball M, Rounsaville BJ, & Carroll KM (2011). Teaching community program clinicians motivational interviewing using expert and train-the-trainer strategies. Addiction, 106(2), 428–441. 10.1111/j.1360-0443.2010.03135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendel P, Meredith LS, Schoenbaum M, Sherbourne CD, & Wells KB (2008). Interventions in organizational and community context: A framework for building evidence on dissemination and implementation in health services research. Administration and Policy in Mental Health and Mental Health Services Research, 35(1–2), 21–37. 10.1007/s10488-007-0144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz RF, Ippen CG, Rao S, Le H, & Dwyer EV (2000). Manual for group cognitive behavioral therapy of major depression. San Francisco General Hospital Depression Clinic. [Google Scholar]
- Nakamura BJ, Selbo-Bruns A, Okamura KH, Chang J, Slavin L, & Shimabukuro S (2014). Developing a systematic evaluation approach for training programs within a train-the-trainer model for youth cognitive behavior therapy. Behaviour Research and Therapy, 53(1), 10–19. 10.1016/j.brat.2013.12.001. [DOI] [PubMed] [Google Scholar]
- Payton JW, Wardlaw DM, Graczyk PA, Bloodworth MR, Tompsett CJ, & Weissberg RP (2000). Social and emotional learning: A framework for promoting mental health and reducing risk behavior in children and youth. Journal of School Health, 70(5), 179–185. 10.1111/j.1746-1561.2000.tb06468.x. [DOI] [PubMed] [Google Scholar]
- Pearce J, Mann MK, Jones C, van Buschbach S, Olff M, & Bisson JI (2012). The most effective way of delivering a train-the-trainers program: A systematic review. Journal of Continuing Education in the Health Professions, 32, 215–226. 10.1002/chp.21148. [DOI] [PubMed] [Google Scholar]
- Residential Child Care Project (2016). The therapeutic crisis intervention system. Cornell University, 1–14. [Google Scholar]
- Scott K, Lewis CC, Rodriguez-Quintana N, Marriott BR, & Hindman RK (this issue) Implementation of the Wolverine Mental Health Program, Part 1: Adoption phase. Cognitive and Behavioral Practice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner BF (1938). The behavior of organisms. New York: Appleton. [Google Scholar]
- Valentine SE, Ahles EM, Dixon De Silva LE, Patrick KA, Baldwin M, Chablani-Medley A, Shtasel DL, & Marques L (2019). Community-based implementation of a paraprofessional-delivered cognitive behavioral therapy program for youth involved with the criminal justice system. Journal of Health Care for the Poor and Underserved, 30(2), 841–865. 10.1353/hpu.2019.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, Daleiden EL, Ugueto AM, Ho A, Martin J, Gray J, Alleyne A, Langer DA, Southam-Gerow MA, & Gibbons RD Research Network on Youth Mental Health. (2012). Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry, 69(3), 274–282. 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Wiltsey Stirman S, Gamarra JM, Bartlett BA, Calloway A, & Gutner CA (2017). Empirical examinations of modifications and adaptations to evidence-based psychotherapies: Methodologies, impact, and future directions. Clinical Psychology: Science and Practice, 24(4), 396–420. 10.1111/cpsp.12218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young J, & Beck A (1980). Cognitive therapy scale: Rating manual. Unpublished manuscript. Philadelphia: Center for Cognitive Therapy. [Google Scholar]
- Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, Cohen D, Del Giovane C, Liu Y, Michael KD, Zhang Y, Weisz JR, & Xie P (2015). Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: A systematic review and network meta-analysis. World Psychiatry, 14(2), 207–222. 10.1002/wps.20217. [DOI] [PMC free article] [PubMed] [Google Scholar]