PURPOSE
The aim of this study is to determine the pathway that women follow for Breast Cancer Care (BCC) and the time intervals from symptom discovery to treatment initiation and to develop a quality matrix framework.
METHODS
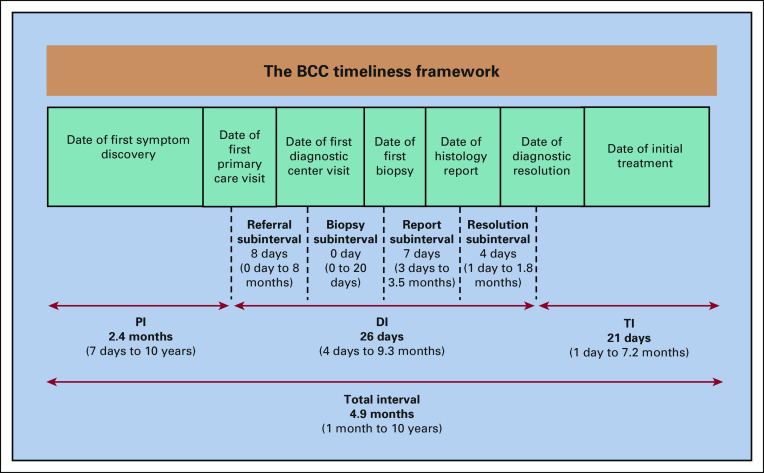
A retrospective cohort study was conducted at six tertiary centers in Malaysia. All women with newly diagnosed breast cancer were interviewed, and a medical records review was conducted using a structured questionnaire. The BCC timeliness framework showed that the total time between a woman discovering their first breast changes and the date of initial treatment was divided into three distinct intervals: presentation interval, diagnostic interval, and treatment interval. Four diagnosis subintervals, referral, biopsy, report, and diagnosis resolution intervals, were also looked into.
RESULTS
The BCC timeliness framework was used to capture important time points. The median total time, presentation interval, diagnostic interval, and treatment interval were 4.9 months (range, 1 month to 10 years), 2.4 months (range, 7 days to 10 years), 26 days (range, 4 days to 9.3 months), and 21 days (range, 1 day to 7.2 months), respectively. Meanwhile, the median time for the diagnosis subinterval of referral, biopsy, report, and diagnosis resolution was 8 days (range, 0 day to 8 months), 0 day (range, 0 day to 20 days), 7 days (range, 3 days to 3.5 months), and 4 days (range, 1 day to 1.8 months), respectively.
CONCLUSION
The BCC timeliness framework is based on the current sequenced trajectory of the BCC journey. Clarity in the measurement of timeliness provides a standardized language for monitoring and outcome research. It can serve as a quality indicator for community and hospital-based breast cancer programs.
INTRODUCTION
Breast cancer is the most common cancer worldwide. In 2020, Asia accounted for 45.4% of the global incident cases and 50.5% of the mortality rate, and the incidence is predicted to climb significantly.1 Similarly, breast cancer is the most frequent cancer in Malaysia,2 and the incidence is expected to escalate because of increasing life expectancy, better socioeconomic status, and changes in lifestyle.3 A high proportion of advanced stage with limited access to timely diagnosis and treatments puts Asian women, especially those living in low-middle–income countries, at a high cancer mortality risk.4 The Malaysian study on cancer survival (MyScan) has reported a lower 5-year relative survival rate of 66.8% compared with Japan (88.9%), United States (88.8%), and Singapore (80.3%).5 Women with breast cancer in Malaysia often delay in seeking medical care and present with more advanced stages of disease.6 Besides the sociodemographic7 and sociocultural8 factors, delays are also associated with health care systems,9 symptom interpretation,10 and type of treatment.11
CONTEXT
Key Objective
This study establishes a framework for the care of breast cancer that can be quickly adopted by nonexperts. The quality matrices for breast cancer quality care are based on the framework data on timeliness.
Knowledge Generated
The Breast Cancer Care (BCC) timeliness framework is based on three (3) sequential episodes of presentation, diagnosis, and treatment. Four (4) diagnosis subintervals of referral, biopsy, report, and diagnosis resolution were examined. The optimal time or the acceptable duration of women's pathway to BCC can be recommended to patients for self-regulation and a guide for seeking BCC.
Relevance
The BCC timeliness framework is useful to study the patients' journey and identify the barriers to early presentation, diagnosis, and treatment, which can be adapted into cancer control programs.
Timely access to health care services has become a priority in public health policies.12,13 The time interval not only is an indicator of the accessibility of health care but also aids in identifying inequalities of care in patient management.14-16 Therefore, appropriate assessment from the primary health care level, timely access to breast cancer diagnosis, and treatment initiation are required, but there is a scarcity of data that measure the timeliness of access to diagnosis and treatments. Only two timeframe studies were conducted in Malaysia. First, the study was conducted on private and tertiary hospitals in a well-resourced urban setting concentrated with cancer specialists, manpower, and physical infrastructure.17 Another study was on the feasibility of patient navigation on breast cancer care (BCC) but limited to a historical comparison without full follow-up data.18
The Clinical Practice Guidelines (CPG) for breast cancer management in Malaysia recommended a 2-month interval from presentation at diagnostic centers to initial treatment,19 and the latest CPG clinical audit indicator targets 80% of women to be referred to the breast clinic within 2 weeks of presenting to primary care services.20 Nevertheless, there has not been a national audit exercise to document timeliness in access to presentation, diagnosis, and treatments in Malaysia. The lack of contextual knowledge among policy makers necessitates that the quality cancer care includes process matrices that nontechnical experts may easily adopt. The framework could identify health system or patient barriers to early presentation, diagnosis, and treatment for timely interventions.
Although there are guidelines on time frames provided by western countries that can be used as a reference, the time points being used in scientific papers21,22 and policy documents20 vary causing difficulties in selecting the most appropriate intervals that may be suitable for adoption in national cancer control programs. Hence, this study aims to identify the time point intervals of patients' presentation, diagnosis, and treatment in public tertiary centers in Malaysia to precisely define a framework for future audits and studies.
METHODS
Study Design and Study Population
The researchers developed a structured study questionnaire from literature review, expert panel discussion, and pilot testing. The questionnaires were in both Malay and English languages and pretested for content validity among breast surgeons and face validity among breast cancer survivors to meet the study objectives. This retrospective cohort study was conducted at six tertiary public centers in Malaysia between June 2015 and June 2017. These hospitals are the main public tertiary centers located in different regions and act as referral centers for breast cancer cases in Malaysia. Each hospital has an open-access diagnostic center where women may be consulted. The study population consisted of 870 universally sampled patients with newly diagnosed breast cancer that was confirmed through histopathology examination. Cases were identified through breast cancer records at surgery outpatient department and breast clinics in each hospital. After medical records review, exclusions, and missing data, 340 patients were included in the study (Appendix 1). The median follow-up was 14 months (range, 12-18 months) from diagnosis.
Data Collection
All patients with breast cancer consented through phone call before data collection. The sociodemographic data and all important dates of their BCC journey were captured from both medical record reviews and interviews using the structured questionnaire. Phone interviews with the aid of a calendar view helped women remember important dates and events. Relevant clinical information was retrieved from the medical records. All data were then cross-validated between patient medical records and interviews by researchers to ensure accuracy.
The sociodemographic profile included age, ethnicity, marital status, educational level, employment status, household income, and lifestyle. Medical details included the method of cancer detection (eg, self-detected and screen-detected), type of symptom, symptom interpretation, practice of breast self-examination, type of primary care facility (eg, clinic and hospital), type of biopsy, number of biopsies, histologic diagnosis, stage at diagnosis (American Joint Committee on Cancer seventh edition), treatment details, and the all important time points.
Important Time Points for the Breast Cancer Care Pathway
The important time points for the BCC pathway includes the symptom duration, date of symptom discovery, date of first primary care visit, date of first diagnostic center visit, date of the first biopsy, date of histology report that confirmed malignancy, date of diagnostic resolution or completion and communication, and date of initial treatment. Initial treatment is defined as the recommended primary treatment. The total time between a woman discovering symptoms and the date of initial treatment was then divided into three intervals: presentation interval (PI), diagnostic interval (DI), and treatment interval (TI). PI was defined as the time from women discovering the first symptom to presentation at a primary care facility. DI was defined as the time from the first presentation at a primary care facility to a diagnosis resolution. Meanwhile, TI was defined as the time from a diagnosis resolution to initial treatment. In addition, we also explored four other subintervals, which are referral (time taken from referral to a diagnostic center), biopsy (time taken to perform a biopsy), report (time taken to obtain a histologic report of confirmed malignancy), and diagnosis resolution (time taken to diagnosis resolution) intervals. Delay was determined if the PI was more than 3 months,23,24 the DI was more than 1 month,22-24 and the TI was more than 1 month.25,26
Data Analysis
All analyses were performed using SPSS version 20.0 (SPSS Inc, Chicago, IL). Descriptive statistical analysis was used to determine the patterns of presentation and details of diagnosis and treatment, along the median time of women's pathways to BCC. Delay was divided into dichotomous outcomes: nondelay and delay. Important variables and variables with P < .25 in the univariable analysis were selected for multivariable analysis to identify factors associated with delays in presentation, diagnosis, and treatment. Results were presented as adjusted odds ratio, 95% CI with a significant P value < .05.
Ethical approvals were obtained from the University Malaya Medical Centre Ethics Committee (PPUM/MDU/300/04/03) and National Medical Research Registry, Medical Research and Ethics Committee ((2)dlm.KKM/NIHSEC/08/0804/P12-824).
RESULTS
The median age for all patients was 53 years (23-74 years). Most of the patients (45.3%) were Malays, 76.2% were married, and 75.9% have at least a secondary education level. For economic status, 67.9% of the patients were unemployed with a median household income of RM 2,900 (∼US dollars 694) per month. Only a small portion of patients have a family history of breast cancer (18.3%), consumed alcohol (12.1%), ever-smoked (15.9%), and used contraception (26.2%). All the sociodemographic characteristics of women with breast cancer can be found in Table 1.
TABLE 1.
Sociodemographic Characteristics of Women With Breast Cancer (N = 340)

Presentation, Diagnosis, and Treatment Details
The appearance of a breast lump (88.2%) was the most common main symptom, followed by breast pain (3.8%), changes in breast shape (2.9%), nipple discharge (2.6%), and weight loss (2.3%), none were screen-detected. More than half appraised their symptom as cancerous (63.2%). Approximately, 65.3% performed regular breast self-examination before the diagnosis. All patients presented to a primary health care clinic (86.2%) or directly to a hospital (13.8%) through outpatient departments and accident and emergency.
Results showed that most (68.6%) patients underwent one biopsy to confirm malignancy and 16.8% had a surgical biopsy. The majority were confirmed through needle biopsy, via free-hand core needle (50%), fine needle aspiration cytology (16.5%), or image-guided core (16.7%) biopsies. The majority were diagnosed at the treating hospitals (83.5%), with 45% diagnosed at late-stage cancer (stage III and IV). Surgery (77.6%) was performed in the majority of women as the initial treatment with a high adherence rate of 86%. All the details on the presentation, diagnosis, and treatment of breast cancer can be found in Table 2.
TABLE 2.
Presentation, Diagnosis, and Treatment Details of Women With Breast Cancer (N = 340)

BCC Timeliness Framework
The median total time for BCC pathway from first symptom discovery to initial treatment was 4.9 months (range, 1 month to 10 years), which was then divided into three sequential episodes of PI, DI, and TI.
The median time for PI, DI, and TI was 2.4 months (range, 7 days to 10 years), 26 days (range, 4 days to 9.3 months), and 21 days (range, 1 day to 7.2 months), respectively. Referral interval was the longest duration of diagnostic subinterval with a median time of 8 days (range, 0 days to 8 months). A minimum of 0 days indicated that patients were referred within the same day of the first primary care visit, whereas a maximum of the 8 months was due to patient delay. The interval for a referral from community clinics was shorter than within hospitals, with the median of 7 days (range, 0 day to 5.7 months) and 9 days (range, 0 days to 8 months), respectively. Within the hospital referral included from primary care, gynecology, and emergency department to the surgical outpatient department.
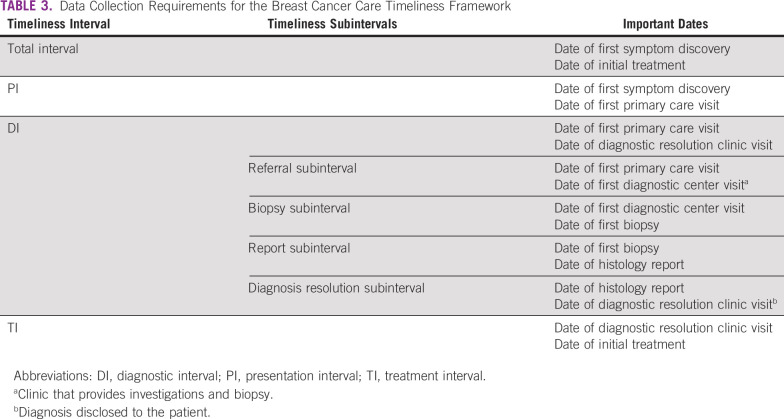
The median time for biopsy interval or getting the first biopsy was 0 days (range, 0 days to 20 days), indicating that the majority of patients (89.0%) undergo biopsy at the first visit or the same day to the diagnostic center. Meanwhile, the pathology report interval took a median time of 7 days (range, 3 days to 3.5 months), and the median time for diagnostic resolution or result disclosure in the clinic was 4 days (range, 1 day to 1.8 months). Figure 1 illustrates the median (range) time intervals of women's pathways to BCC in Malaysia. Table 3 lists the all important data collection requirements for the BCC timeliness Framework.
FIG 1.
Important time points and intervals in the timeliness framework and the median (range) time intervals in Malaysia. BCC, Breast Cancer Care; DI, diagnostic interval; PI, presentation interval; TI, treatment interval.
TABLE 3.
Data Collection Requirements for the Breast Cancer Care Timeliness Framework
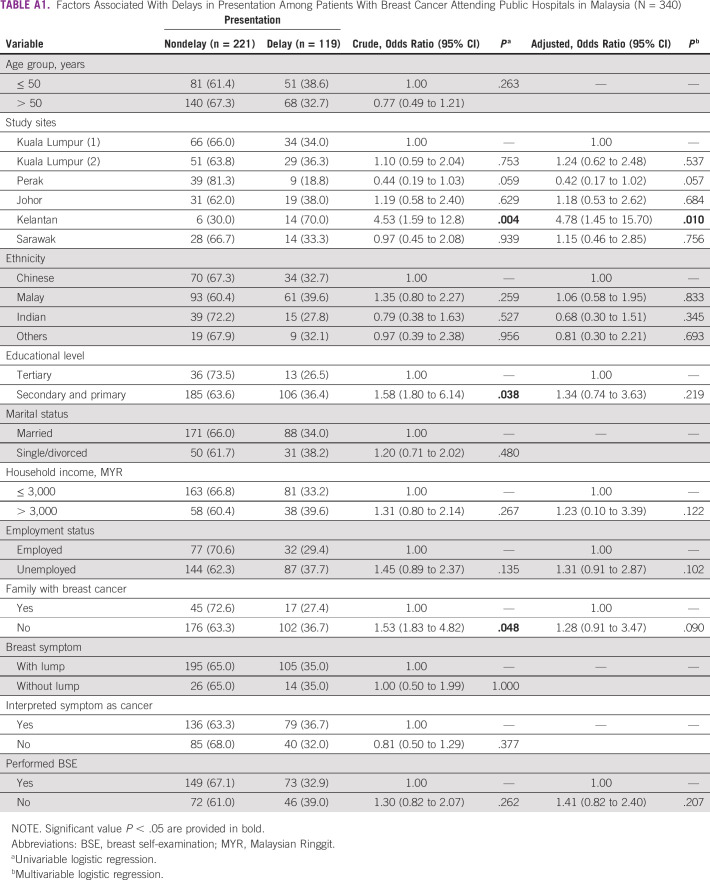
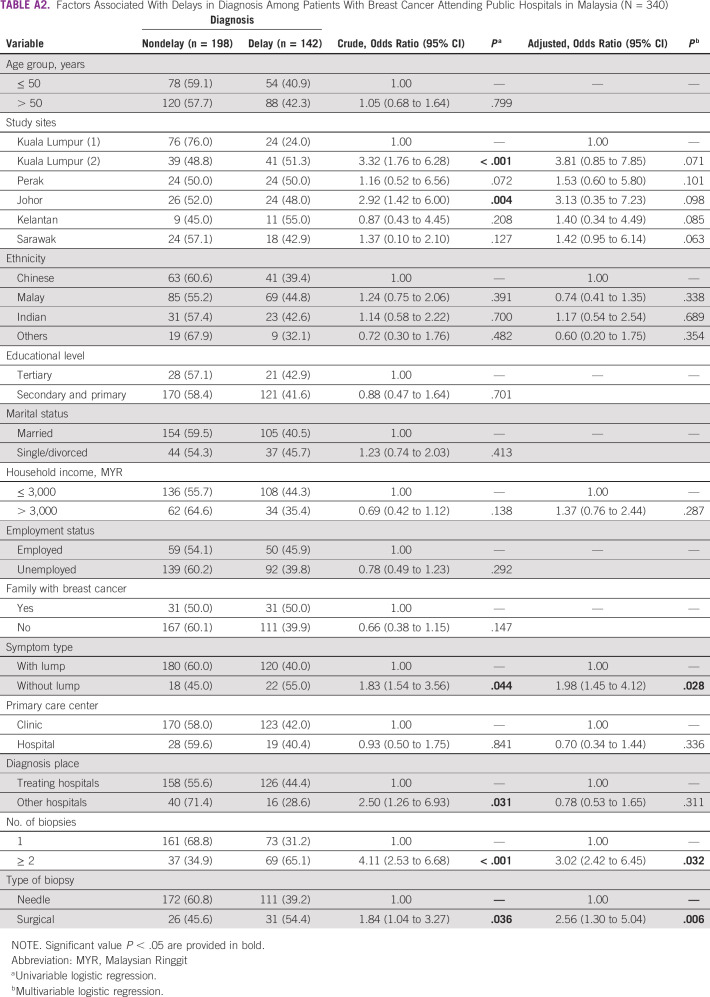
The proportions for presentation, diagnosis, and treatment delays in our study were 35%, 41.8%, and 36.2%, respectively. The multivariable analysis did not find any sociodemographic characteristic linked with these delays. However, the study location showed a significant association with presentation delay. Diagnosis delay was associated with symptoms without lumps, having two or more biopsies, and undergoing surgical excision biopsy. Treatment delay was associated with the study site. The analyses are not shown here; refer to Appendix Tables A1, A2, and A3 in the Appendix.
DISCUSSION
A timeliness framework for the BCC pathways was developed. A PI of 2.4 months was the most extended interval in this study compared with the DI and TI. The range of 7 days to 10 years illustrates the delayed help-seeking process and possibly the natural history of low-grade cancer. Other local studies similarly report a median of 2-4 months after symptoms discovery,6,17,18 indicating that time taken to present for seeking medical care among patients with breast cancer is delayed and differs between institutions and Malaysia locations. We found that the Kelantan site was most likely to delay the presentation. Kelantan located on the East Coast is more rural and less developed than the West Coast.10 Rural and suburban Asian women are private and less receptive to revealing their private parts even to health care providers.10,27,28 Previous studies conducted in Kelantan reported that poor knowledge, fear of consequences of cancer, beliefs in complementary alternative medicine, needing support from others, competing priorities, denial, wait and see attitude, and perceptions of a weak health care system were reasons for delay.29,30 In addition, there were lack of self-management skills, lack of family support, especially husbands, and a firm reliance on family to make medical decisions.31-33 The Malaysian and specifically Kelantan community would require a strategic and culturally sensitive health education.
Notably, we uncovered delays in this study where all the patients were symptomatic. Malaysia does not have a population-based mammogram screening program. Screening is performed opportunistically with a low uptake of 6.8% to 25.5%.34,35 However, there are opportunities to improve breast cancer outcomes by downstaging clinically apparent breast cancer.8 Given that 47.9% of cases were diagnosed with advanced disease2 with low survival rates in Malaysia,5 the priority for cancer control is not only to intensify health promotion but also to strengthen timely diagnostic services in the public sector, which remain the safety net of many underprivileged citizens as Malaysia has universal health coverage before implementing screening programs.
The median DI of 26 days in this study was similar to other studies in Asia36,37 and high-income countries38,39 where the reported intervals were 7-45 days. Moreover, these intervals are within the recent Breast Health Global Initiative recommendations that health systems should strive to complete a diagnostic examination within 60 days.12 This finding illustrates that the time interval to a diagnosis of breast cancer in Malaysia is acceptable, but the 9.3 months upper range begs for improvement. Between the diagnosis subintervals, the referral interval showed the longest duration. No time frame was recommended for a referral from a primary care facility to a diagnostic center in Malaysia at the time of the study, but 2 weeks is suggested for referral time in the United Kingdom and Ireland,15,40 and recently, this has been incorporated into the updated Malaysian Management of Breast Cancer CPG.20 Meanwhile, the short median time for the biopsy in this study indicated that many patients underwent biopsy during their first visit to the diagnostic center. However, the upper range of the biopsy interval was 20 days, indicating that there could be a health system or help-seeking barrier that the study could not capture.
This study showed that symptoms without a breast lump were significantly associated with diagnosis delay, similarly seen in other studies.26,41,42 This finding illustrates incorporation of breast cancer lump and nonlump symptoms education. A systematic review has reported that false attribution of breast lumps as benign, lack of proficient clinical breast examination, and nonreferral for further investigation among primary health care workers also cause diagnostic delays,8,33,43 necessitating comprehensive education to health care providers.8,41,44,45
In our study, 31.2% of the patients had two or more biopsies to resolve the diagnosis, indicating the issues with the quality of biopsy technique, and poor clinical decision making or lack of image-guided biopsies in public hospital settings, indicating the urgent need to support training and diagnostic equipment for the workforce. Some 18% of diagnosis was resolved beyond a month, indicating that timely scheduling or pathology reporting is still a major barrier. The practice of multidisciplinary team (MDT) meetings in all the studied hospitals was beyond the scope of the study, and only the academic center had routine weekly multidisciplinary team meetings.46 The availability of diagnostic MDTs can reduce the rate of institutional procedure sampling errors and errors in pathology laboratory interpretation.47
The median TI in this study was consistent with other studies.48-51 We found that treatment delay was primarily influenced by the type of hospital. Although all study sites were tertiary referral centers, the public hospitals in this study did not have the whole range of in-house cancer services, compared with the university hospital comparator, which had the full range of disciplines. Furthermore, longer TI was associated with scheduling issues, high caseloads, and the need for cross-referrals to other centers in general hospitals compared with university hospitals.52 Besides health system delays, patient delays may also influence delays in treatments because of the holdups in making treatment decisions as illustrated in the total breast cancer delay model.53 Moreover, treatment decisions are left to family members on the basis of the family-oriented culture in Asia.56-56
Our study like other studies57,58 indicated that those who were diagnosed at other hospitals than treating hospitals had a higher risk of treatment delay. Unfortunately, limitations of navigating patients between hospitals are unavoidable because of issues of availability, accessibility, affordability, timely care, and need for second opinion necessitating attending multiple hospitals.14,42,59-61 Therefore, navigating patients to reduce logistical barriers is vital in timely treatment. Our study similar to others showed that TI did not differ according to the cancer stage.62,63 Another study has found that the advanced stages of cancer were associated with a shorter time to treatment.48 Hence, prioritizing according to advanced disease may help in providing safer timely access to those who need urgent treatments.
This study provides a framework that details the BCC pathway that is divided into three sequential episodes of care that can be adopted easily by nontechnical experts. This pathway is based on the current sequential breast cancer presentation, diagnosis, and treatment care pathways that are required in all resource settings, similar to that proposed in the recent Breast Health Global Initiative summit.12 Our timeliness framework includes the critical dates that need to be recorded, thus making this concept easy to implement (Table 3). The data on timeliness intervals provide the quality matrices for breast cancer quality care. Furthermore, the publication language for these time points and intervals is not standardized, making comparisons in research and monitoring challenging. To ensure data quality, cost efficiency, and time-saving, electronic medical record–enabled hospitals can be designed to digitalize the timepoints.64 Our study illustrates that these timepoints data have been tested and are available in all hospitals. The prospective collection of these dates is also feasible. Hence, the BCC timeliness framework may be a useful outcome measurement tool for community-based interventions in shortening PIs and in hospital-based quality indicators for ensuring timely diagnosis and treatment initiation. Although not mentioned in this study, other treatment dates can be recorded to measure other treatment subintervals.56
Although our results may be affected by the small sample size and attrition of the sample, every precaution and resource were used. Furthermore, all data obtained through medical record review and interviews were cross-validated to ensure accuracy. Hence, a retrieval rate of 54% in busy public tertiary hospitals with limitations in manual record keeping would provide a good representation. In addition, this study is a multicenter retrospective cohort study conducted at six public tertiary hospitals that act as referral centers for patients with breast cancer representing all regions in Malaysia, making this study relevant for policy makers in cancer control planning.
In conclusion, the BCC timeliness framework is based on the current sequential trajectory of breast cancer presentation, diagnosis, and treatment. This framework provides clarity in the measurement of timeliness even for nonexperts. It provides a standardized language for monitoring and outcome research. It can serve as a quality indicator for community and hospital-based breast cancer programs.
ACKNOWLEDGMENT
We would like to thank the Director General of Health Malaysia for permission to publish this article. Sincere appreciation is also due for all patients with breast cancer and enumerators involved in this research.
APPENDIX 1
Number of Samples
A total of 870 patients with breast cancer were provided by the six hospitals from their hospital registries. A review of the medical records excluded those with recurrent cancer and secondary cancer, thus excluding 86 patients. The remaining 784 patients who were newly diagnosed during that period were contacted through a telephone call, whereby only 426 (54%) agreed to participate. Those with incomplete data (n = 86) were excluded, leaving a total of 340 patients.
Factors Associated With Delays in Presentation, Diagnosis, and Treatment of Patients With Breast Cancer
Details of the factors associated with delays in presentation, diagnosis, and treatment of patients with breast cancer are shown in Appendix Tables A1-A3.
TABLE A1.
Factors Associated With Delays in Presentation Among Patients With Breast Cancer Attending Public Hospitals in Malaysia (N = 340)
TABLE A2.
Factors Associated With Delays in Diagnosis Among Patients With Breast Cancer Attending Public Hospitals in Malaysia (N = 340)
TABLE A3.
Factors Associated With Delays in Treatment Among Patients With Breast Cancer Attending Public Hospitals in Malaysia (N = 340)
Nor Aina Emran
Consulting or Advisory Role: Roche
Nur Aishah Mohd Taib
Consulting or Advisory Role: Roche, AstraZeneca, MSD
No other potential conflicts of interest were reported.
SUPPORT
Supported by the Peruntukan Penyelidikan Pascasiswazah (PPP) Grant (UM.TNC2/IPPP/UPGP/638/PPP) from the Universiti Malaya, Kuala Lumpur, and High Impact Research (HIR) Grant No. (UM.C/HIR/MOHE/06) from the Ministry of Higher Education of Malaysia.
AUTHOR CONTRIBUTIONS
Conception and Design: Noor Mastura Mohd Mujar, Maznah Dahlui, Nur Aishah Mohd Taib
Financial support: Noor Mastura Mohd Mujar, Nor Aina Emran, Yang Wai Yan, Sarojah Arulanantham, Chan Hooi Chea, Nur Aishah Mohd Taib
Provision of study material or patients: All authors
Collection and assembly of data: All authors
Data analysis and interpretation: Noor Mastura Mohd Mujar, Maznah Dahlui, Nur Aishah Mohd Taib
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Nor Aina Emran
Consulting or Advisory Role: Roche
Nur Aishah Mohd Taib
Consulting or Advisory Role: Roche, AstraZeneca, MSD
No other potential conflicts of interest were reported.
REFERENCES
- 1.Globocan : The Global Cancer Observatory; Breast Cancer. Lyon, France, International Agency for Research on Cancer, 2020 [Google Scholar]
- 2.National Cancer Registry : Malaysia National Cancer Registry Report 2012-2016 (ed 5). Azizah A, Hashimah B, Nirmal K, et al. (eds): Putrajaya, Malaysia, Ministry of Health Malaysia, 2019, pp 2-116 [Google Scholar]
- 3.Yip CH, Pathy NB, Teo SH: A review of breast cancer research in Malaysia. Med J Malaysia 69:8-22, 2014. (suppl A) [PubMed] [Google Scholar]
- 4.Rivera-franco MM, Leon-rodriguez E: Delays in breast cancer detection and treatment in developing countries. Breast Cancer (Auckl) 10.1177/1178223417752677 [epub ahead of print on January 8, 2018] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Cancer Registry : Malaysian Study on Cancer Survival (MySCan), Volume 4. National Cancer Institute, Ministry of Health Malaysia, Putrajaya, Malaysia, 2018, pp 1-72 [Google Scholar]
- 6.Yip CH, Mohd Taib NA, Mohamed I: Epidemiology of breast cancer in Malaysia. Asian Pac J Cancer Prev 7:369-374, 2006 [PubMed] [Google Scholar]
- 7.Ibrahim NA, Oludara MA: Socio-demographic factors and reasons associated with delay in breast cancer presentation: A study in Nigerian women. Breast 21:416-418, 2012 [DOI] [PubMed] [Google Scholar]
- 8.Taib NA, Yip CH, Low WY: Recognising symptoms of breast cancer as a reason for delayed presentation in Asian women-the psycho-socio-cultural model for breast symptom appraisal: Opportunities for intervention. Asian Pac J Cancer Prev 12:1601-1608, 2011 [PubMed] [Google Scholar]
- 9.Sharma K, Costas A, Shulman LN, et al. : A systematic review of barriers to breast cancer care in developing countries resulting in delayed patient presentation. J Oncol 2012:121873, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norsa'adah B, Rahmah MA, Rampal KG, et al. : Understanding barriers to Malaysian women with breast cancer seeking help. Asian Pac J Cancer Prev 13:3723-3730, 2012 [DOI] [PubMed] [Google Scholar]
- 11.Arpino G, Pensabene M, Condello C, et al. : Tumor characteristics and prognosis in familial breast cancer. BMC Cancer 16:924, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duggan C, Dvaladze A, Rositch AF, et al. : The Breast Health Global Initiative 2018 global summit on improving breast healthcare through resource‐stratified phased implementation: Methods and overview. Cancer 126:2339-2352, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moodley J, Cairncross L, Naiker T, et al. : Understanding pathways to breast cancer diagnosis among women in the Western Cape Province, South Africa: A qualitative study. BMJ Open 6:1-7, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCutchan GM, Wood F, Edwards A, et al. : Influences of cancer symptom knowledge, beliefs and barriers on cancer symptom presentation in relation to socioeconomic deprivation: A systematic review. BMC Cancer 15:1000, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hiom SC: Diagnosing cancer earlier: Reviewing the evidence for improving cancer survival. Br J Cancer 112:S1-S5, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martins T, Hamilton W, Ukoumunne OC: Ethnic inequalities in time to diagnosis of cancer: A systematic review. BMC Fam Pract 14:197, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim GCC, Aina EN, Cheah SK, et al. : Closing the global cancer divide—Performance of breast cancer care services in a middle income developing country. BMC Cancer 14:212, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeoh Z-Y, Jaganathan M, Rajaram N, et al. : Feasibility of patient navigation to improve breast cancer care in Malaysia. J Glob Oncol 4:1-13, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministry of Health Malaysia : Clinical Practice Guidelines, Management of Breast Cancer (ed 2). Putrajaya, Malaysia, Ministry of Health, 2010 [Google Scholar]
- 20.Ministry of Health Malaysia : Clinical Practice Guidelines, Management of Breast Cancer (ed 3). Putrajaya, Malaysia, Malaysian Health Technology Assessment Section (MaHTAS), 2020 [Google Scholar]
- 21.Ho PJ, Cook AR, Binte Mohamed Ri NK, et al. : Impact of delayed treatment in women diagnosed with breast cancer: A population-based study. Cancer Med 9:2435-2444, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moodley J, Cairncross L, Naiker T, et al. : From symptom discovery to treatment—Women's pathways to breast cancer care: A cross-sectional study. BMC Cancer 18:312, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim JNW, Potrata B, Simonella L, et al. : Barriers to early presentation of self-discovered breast cancer in Singapore and Malaysia: A qualitative multicentre study. BMJ Open 5:e009863, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghazali SM, Othman Z, Cheong KC, et al. : Non-Practice of breast self examination and marital status are associated with delayed presentation with breast cancer. Asian Pac J Cancer Prev 14:1141-1145, 2013 [DOI] [PubMed] [Google Scholar]
- 25.Huo Q, Cai C, Zhang Y, et al. : Delay in diagnosis and treatment of symptomatic breast cancer in China. Ann Surg Oncol 22:883-888, 2014 [DOI] [PubMed] [Google Scholar]
- 26.Plotogea A, Chiarelli AM, Mirea L, et al. : Clinical and prognostic factors associated with diagnostic wait times by breast cancer detection method. Springerplus 3:125, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pruitt L, Mumuni T, Raikhel E, et al. : Social barriers to diagnosis and treatment of breast cancer in patients presenting at a teaching hospital in Ibadan, Nigeria. Glob Public Health 10:331-344, 2014 [DOI] [PubMed] [Google Scholar]
- 28.Rastad H, Khanjani N, Khandani BK: Causes of delay in seeking treatment in patients with breast cancer in Iran: A qualitative content analysis study. Asian Pac J Cancer Prev 13:4511-4515, 2012 [DOI] [PubMed] [Google Scholar]
- 29.Taib NA, Yip CH, Ibrahim M, et al. : Breast cancer in Malaysia: Are our women getting the right message? 10 Year-experience in a single institution in Malaysia. Asian Pac J Cancer Prev 8:141-145, 2007 [PubMed] [Google Scholar]
- 30.Norsa'adah B, Rahmah MA, Rampal KG: Understanding barriers to Malaysian women with breast cancer seeking help. Asian Pac J Cancer Prev 13:3723-3730, 2012 [DOI] [PubMed] [Google Scholar]
- 31.Taib NA, Akmal MN, Mohamed I, et al. : Improvement in survival of breast cancer patients—Trends in survival over two time periods in a single institution in an Asia Pacific country, Malaysia. Asian Pac J Cancer Prev 12:345-349, 2011 [PubMed] [Google Scholar]
- 32.Mohd Taib NA, Su TT, Al Sadat N, et al. : Malaysian breast cancer survivorship cohort (MYBCC) study. J Univ Malaya Med Cent 16:58, 2013 [Google Scholar]
- 33.Yu FQ, Murugiah MK, Khan AH, et al. : Meta-synthesis exploring barriers to health seeking behaviour among Malaysian breast cancer patients. Asian Pac J Cancer Prev 16:145-152, 2015 [DOI] [PubMed] [Google Scholar]
- 34.Mahmud A, Aljunid SM: The uptake of mammogram screening in Malaysia and its associated factors: A systematic review. Med J Malaysia 73:202-211, 2018 [PubMed] [Google Scholar]
- 35.Institute for Public Health : National Health and Morbidity Survey (NHMS) 2019: Non-communicable Diseases, Healthcare Demand, and Health Literacy—Key Findings. Putrajaya, Malaysia, Ministry of Health, Malaysia, 2019 [Google Scholar]
- 36.Poum A, Promthet S, Duffy SW, et al. : Factors associated with delayed diagnosis of breast cancer in Northeast Thailand. J Epidemiol 24:102-108, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Norsa'adah B, Rampal KG, Rahmah MA, et al. : Diagnosis delay of breast cancer and its associated factors in Malaysian women. BMC Cancer 11:141, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang G, Chan CW, Hartman M: A commentary on delayed presentation of breast cancer in Singapore. Asian Pac J Cancer Prev 12:1635-1639, 2011 [PubMed] [Google Scholar]
- 39.Harirchi I, Ghaemmaghami F, Karbakhsh M, et al. : Patient delay in women presenting with advanced breast cancer: An Iranian study. Public Health 119:885-891, 2005 [DOI] [PubMed] [Google Scholar]
- 40.Mccain S, Newell J, Badger S, et al. : Referral patterns , clinical examination and the two-week-rule for breast cancer : A cohort study. Ulster Med J 80:68-71, 2011 [PMC free article] [PubMed] [Google Scholar]
- 41.Forbes LJL, Warburton F, Richards MA, et al. : Risk factors for delay in symptomatic presentation: A survey of cancer patients. Br J Cancer 111:1-8, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El Jones C, Maben J, Jack RH, et al. : A systematic review of barriers to early presentation and diagnosis with breast cancer among black women. BMJ Open 4:e004076, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lim JN, Potrata B, Simonella L, et al. : Barriers to early presentation of self-discovered breast cancer in Singapore and Malaysia: A qualitative multicentre study. BMJ Open 5:e009863, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bish A, Ramirez A, Burgess C, et al. : Understanding why women delay in seeking help for breast cancer symptoms. J Psychosom Res 58:321-326, 2005 [DOI] [PubMed] [Google Scholar]
- 45.Burgess CC, Ramirez AJ, Richards MA, et al. : Who and what influences delayed presentation in breast cancer? Br J Cancer 77:1343-1348, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tham TM, Iyengar KR, Taib NA, et al. : Fine needle aspiration biopsy, core needle biopsy or excision biopsy to diagnose breast cancer—Which is the ideal method? Asian Pac J Cancer Prev 10:155-158, 2009 [PubMed] [Google Scholar]
- 47.Bairati I, Jobin E, Fillion L, et al. : Determinants of delay for breast cancer diagnosis. Cancer Detect Prev 31:323-331, 2007 [DOI] [PubMed] [Google Scholar]
- 48.Plotogea A, Chiarelli AM, Mirea L, et al. : Factors associated with wait times across the breast cancer treatment pathway in Ontario. Springerplus 2:388, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shieh S-H, Hsieh VC-R, Liu S-H, et al. : Delayed time from first medical visit to diagnosis for breast cancer patients in Taiwan. J Formos Med Assoc 113:696-703, 2014 [DOI] [PubMed] [Google Scholar]
- 50.Caplan LS, May DS, Richardson LC: Time to diagnosis and treatment of breast cancer: Results from the national breast and cervical cancer early detection program, 1991-1995. Am J Public Health 90:130-134, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruddy KJ, Gelber S, Tamimi RM, et al. : Breast cancer presentation and diagnostic delays in young women. Cancer 120:20-25, 2014 [DOI] [PubMed] [Google Scholar]
- 52.Brazda A, Estroff J, Euhus D, et al. : Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol 17:291-296, 2010. (suppl 3) [DOI] [PubMed] [Google Scholar]
- 53.Taib NA, Yip CH, Low WY: A grounded explanation of why women present with advanced breast cancer. World J Surg 38:1676-1684, 2014 [DOI] [PubMed] [Google Scholar]
- 54.Muhamad M, Merriam S, Suhami N: Why breast cancer patients seek traditional healers. Int J Breast Cancer 2012:689168, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teh Y, Elina N, Shaari N, et al. : Determinants of choice of surgery in Asian patients with early breast cancer in a middle income country. Asian Pac J Cancer Prev 15:3163-3167, 2014 [DOI] [PubMed] [Google Scholar]
- 56.Mujar NM, Dahlui M, Emran NA, et al. : Complementary and alternative medicine (CAM) use and delays in presentation and diagnosis of breast cancer patients in public hospitals in Malaysia. PLoS One 12:e0176394, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yoo T, Kim J, Lee JW, et al. : Delay of treatment initiation does not adversely affect survival outcome in breast cancer. Cancer Res Treat 48:962-969, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen SJ, Kung P-T, Huang KH, et al. : Characteristics of the delayed or refusal therapy in breast cancer patients: A longitudinal population-based study in Taiwan. PLoS One 10:e0131305, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Facione NC, Facione PA: The cognitive structuring of patient delay in breast cancer. Soc Sci Med 63:3137-3149, 2006 [DOI] [PubMed] [Google Scholar]
- 60.Unger-Saldaña K: Challenges to the early diagnosis and treatment of breast cancer in developing countries. World J Clin Oncol 5:465-477, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Landercasper J, Linebarger JH, Ellis RL, et al. : A quality review of the timeliness of breast cancer diagnosis and treatment in an integrated breast center. J Am Coll Surg 210:449-455, 2010 [DOI] [PubMed] [Google Scholar]
- 62.Wagner JL, Warneke CL, Mittendorf EA, et al. : Delays in primary surgical treatment are not associated with significant tumor size progression in breast cancer patients. Ann Surg 254:119-124, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mujar M, Dahlui M, Yip CH, et al. : Delays in time to primary treatment after a diagnosis of breast cancer: Does it impact survival? Prev Med (Baltim) 56:222-224, 2013 [DOI] [PubMed] [Google Scholar]
- 64.Mohd Nor NA, Taib NA, Saad M, et al. : Development of electronic medical records for clinical and research purposes: The breast cancer module using an implementation framework in a middle income country—Malaysia. BMC Bioinformatics 19:402, 2019. (suppl 13) [DOI] [PMC free article] [PubMed] [Google Scholar]