Abstract
Background:
The influence of shared genetic vulnerability is well-known in the development of alcohol use disorder. However, there is a dearth of studies on shared environments. Hence, the present study aimed to ascertain the influence of shared environments in the development of alcohol use disorder.
Aim:
To examine the influence of adverse childhood experiences, parental bonding, and temperament in the development of alcohol use disorder.
Methods:
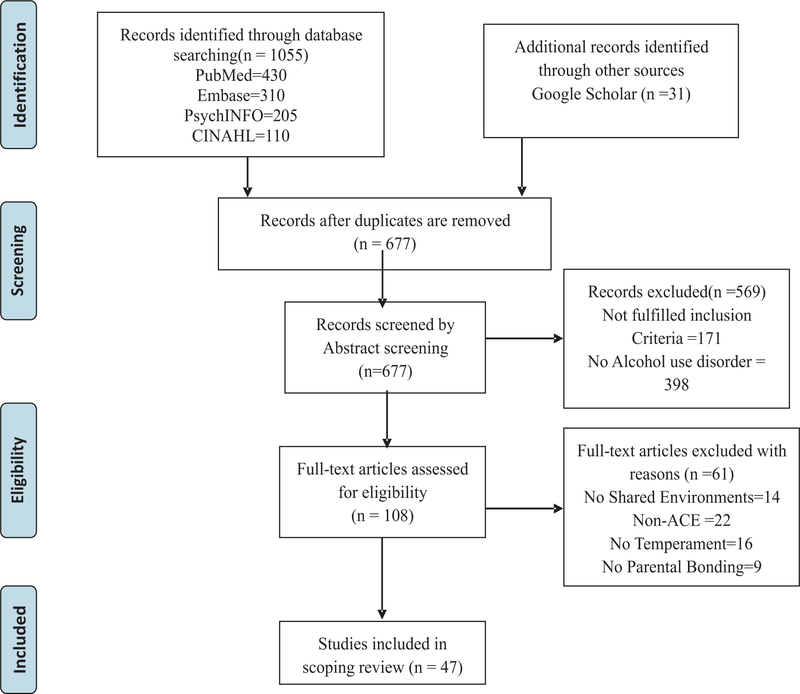
Preferred Reporting Items for Systematic reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) guidelines were followed. Studies were identified through search engines such as PubMed, Embase, and PsychInfo, CINAHL databases. Peer-reviewed articles in English published during 2000 - 2021 were included for the review.
Results:
About 47 articles were considered for the scoping review. Shared environmental factors such as adverse childhood experiences or childhood trauma within 18 years of life, novelty, adventure-seeking, cyclothymia, and immediate need for gratification contribute to alcohol use disorder development. Positive parenting is associated with a lower incidence of AUD.
Conclusion:
Understanding the influence of shared environments and providing tailor-made psycho-social interventions would reduce the risk and prevent alcohol use disorder development..
Keywords: Temperament, parental bonding, adverse childhood consequences
Introduction
Alcohol consumption is the third leading cause of disease and disability. It contributes to traumatic outcomes at a relatively young age, resulting in many years of life to death and disability. The global burden of disease and injury attributable to alcohol consumption is approximately 4.5%. Alcohol consumption is estimated to cause 20–50% of liver cirrhosis, epilepsy, road traffic accidents, violence, and several cancers. Globally, 3.8% of all global deaths were attributable to alcohol, 6.2% for men and 1.1% for women (WHO, 2014).
In India, nearly (one third) 30–35% of adult males and 5% of adult females are regular alcohol users (Gururaj et al., 2011). Alcohol use is considerably higher among men as compared to women, Men (27.3%), Women (1.6%), Children (1.3%). The prevalence of dependent pattern of alcohol use in the general population (10–75 years) is estimated to be 2.7% (Ambekar et al., 2019). There is a significant gender difference in alcohol use in India, wherein men account for 9.1%, whereas women account for 0.5% of use (Gururaj, 2016). The unique environment plays a crucial role in developing alcohol use disorder.
Risk factors
Family history of alcohol use disorder is considered a significant vulnerability factor for genetic and environmental contributions to Alcohol Use Disorders (WHO, 2014).Genetic risk factors account for a significant variation in alcohol dependence. Multiple genes influence alcohol use initiation, metabolism and reinforcing properties in different ways contributing to the susceptibility to psychoactive and dependence-producing properties of alcohol, particularly in few vulnerable groups and individuals. Alcohol dependence is a complex disease influenced by genetic and environmental factors. Alcohol use disorder is approximately 50% heritable. Studies have also found evidence from modest shared environmental effects suggesting that environmental factors also contribute to the familial aggregation of AUDs (Verhulst et al., 2015).
Parental alcohol use disorders are negatively affect the family situation during childhood. Parental heavy drinking affects family functioning, the parent-child relationship and parenting practices, affecting child development adversely (Latendrese et al., 2008). Child maltreatment, including sexual abuse, physical abuse, and neglect, may lead to childhood psychopathology and, later, problem drinking (Shin et al., 2010).
Core risk factors are attitudes, beliefs, or environmental circumstances that put an individual in jeopardy (danger/harm) of developing a mental and substance use disorder (Moe et al., 2007). Risk factors may include individual, family and community risk factors. Individual risk factors include temperament related to an internal and external locus of control, poor self-control, negative emotionality, immediate gratification, and physical activity level (Wills, 2004).
Environmental risks include limited resources, low socio-economic status, lack of knowledge, skills, and programming necessary to reach out for assistance (Kumpfer, 2004). These include parental and sibling drug use, poor child rearing and socialization practices, ineffective parental supervision, parental discipline skills, negative parent-child relationships, family conflict, marital discord, violence at home, adverse experiences and neglect, disorganization in the family, and social isolation of the family (Kumpfer, 2004).
Rationale for the study
Most studies focused on shared genetic vulnerability; family history of alcohol use disorder is a significant risk factor to develop alcohol use disorder as genetic vulnerability. Very few studies examined shared environments in alcohol use disorder. There is a need to study extensively on shared environmental influences on alcohol use disorders.
Methods
Preferred Reporting Items for Systematic Review and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) guidelines was used to achieve the study objective of examining the influence of shared environments that influence the development of alcohol use disorder. Scoping reviews provide an overview of the existing literature to address broad research questions related to complex and heterogeneous bodies of literature. Eligibility Criteria: Peer-reviewed articles on the shared environment such as parental bonding and adverse childhood experiences published in English between 2000–2021, with a study population of alcohol use disorder. Eligibility criteria: The study title, keywords, MeSH terms included the term shared environments, adverse childhood experiences, parental bonding, and temperament among persons with alcohol use disorder, the abstract listed shared environments in alcohol use disorder as one of the objectives, the list of keywords included term similar environments. The review also included conf studies that have examined shared environments in alcohol and substance use disorders. Search Strategy: Evidence evaluated for this report was obtained from a search of the PubMed, EMBASE, PsychINFO, CINAHL database of scoping reviews, systematic reviews and meta-analyses, and conducted reference searches of relevant reviews and articles. The present study aimed to answer the following question: Do shared environments such as adverse childhood experiences, parental bonding, and temperament influence the development of alcohol use disorder?
Shared environment in Alcohol use disorder
A shared environment pertains to the experiences familiar to the individuals brought up within the same family, which produce within-family familiarities. Behaviour genetic twin studies partition a behaviour's variance into genetic and environmental influences. Environmental influences can be divided into shared environments and non-shared (or unique) environments when behaviour geneticists explain the influence of shared environments that make siblings alike. Examples of shared environmental influences could include growing up in the same home, shared parental rules and upbringing, shared family experiences, the same school and community, and peers familiar to both siblings (Mc Gue., 1998). Studies of children and adolescents have found more consistent evidence of shared environmental effects, as one might expect when children are still living together at home. A shared environment is a critical influence on conduct problems and delinquency in children and IQ in childhood(Mc Gue,1998; Waldman,1992).
Shared environmental effects can be everything from parents and neighbourhood, school and society influences. Most individuals share the community, school, and classroom. Hence, a similar environment component may be separated into family and school/neighbourhood environments. Early-onset smoking and drinking were significant correlations for both control-twin and control-control dyads. The shared environment demonstrates significant contributions from non-familial environments-schools, neighbourhoods and communities for these behaviours' (Rose, 2003).
Several studies have examined environmental risks for substance initiation, use, and other externalizing behaviours in adolescence and childhood from a phenotypic perspective. The most consistent finding is the influence of peer groups in initiation (Daniels, 1985; Heath, 1988). However, recent research shows the causal influence of peers may be overestimated and due to assortative friendship (Bauman, 1996; Hops et al., 2000; Kendler, 1996). Certain family environments such as low levels of parental bonding and low parental supervision predict initiation, while proactive parents and clear parental communications discourage use and decrease the likelihood of initiation. (Chilcoat et al., 1996; Kosterman, 2000; Sargent, 2001; Stice, 1995).
However, few behaviour genetic studies have identified the sources of shared environmental variance on substance use. Breaking up this aspect into specifics is essential into specifics is essential to genetic behaviour research and is often carried out when specific genes are examined to account for the hereditary phenotype. One critical study examined that 77% of the similar environmental variance in early substance use was considered peer deviance and parent-child relationship problems (Walden, 2004).
Family factors accounted for a large proportion of the shared environmental effects of illicit drug use. While the influence of shared environment on adult substance use was significant the contribution to parental perspectives was moderate and nonsignificant after accounting for age. This may likely reflect that likely reflect the fact that siblings will not always see the same parenting behaviour, nor will the parental attitudes be expressed in the same way in different offspring. (Baker et al., 2012).
Adverse Childhood Experiences
Adverse childhood experience (ACEs) is common in all populations. Two-thirds of the population report at least one ACE, and more than one in five reported three or more ACEs in their lifetime. Few populations are more vulnerable to ACEs because of their social and economic conditions, living, learning, working, and playing. The number of ACEs increases the risk for adverse outcome.
ACEs are strongly related to disease or well-being throughout life (Larkin & Records, 2007). It can have lasting, adverse effects on health. ACEs and associated conditions, such as living in under-resourced or racially segregated neighbourhoods, frequently moving, and experiencing food insecurity, can cause prolonged stress. ACEs can change brain development and affect attention, decision-making, learning, and response to stress. Many children with prolonged stress have difficulty forming healthy and stable relationships. Exposure to traumatic experiences in childhood increases the risks for post-traumatic stress disorder, major depressive disorder, substance abuse or dependence. Longitudinal studies suggest that these psychiatric disorders persist for many years after trauma exposure and are less likely to respond to treatment. Childhood abuse can negatively influence sensitive developmental periods for emotional, behavioural, cognitive, and social domains, interrupting healthy development and increasing the risk for psychopathology.
Adverse Childhood Experiences and Alcohol use disorder
Substance abuse or dependence is one of the most common psychological sequelae of childhood abuse(Bennett & Kemper, 1994; Down & Harrison, 1998). Childhood trauma, particularly in the first few years of life, is associated with psychopathology, including early onset of problem drinking in adolescence, alcohol use disorders (AUD), and substance use disorders (SUD) in early adulthood. The risk-resilience balance for addiction may be due to the interaction between environmental stressors and stress variation. Substance use problems are common psychological sequelae of childhood abuse or other traumatic experiences(Larkin & Records, 2007; Adriana et al., 2010). Smoking, alcohol, and other drug use might manage the expected anxiety anger associated with ACEs (Larkin & Records, 2007; Melanie et al., 2013).
Significant levels of emotional, physical, and sexual abuse were found in alcohol and other drug-dependent women than men (Cavanaugh et al., 2015). Childhood trauma was significantly more prevalent and severe in persons with alcohol dependence, mediated by neuroticism. Emotional abuse is a primary predictor of alcohol dependence severity. Physical abuse had a moderate direct effect on alcohol dependence severity (Rehan et al., 2017). Compared to the low ACEs, higher ACEs' profiles had 4–90 times higher odds of being in the higher mental and substance use disorders profiles(MSUD). However, more than one-third of participants of high multiple ACE's were also lower in MSUD profiles (Engels et al., 2015).
Higher emotional abuse was associated with alcohol abuse in men. In women, severe physical abuse emerged as a forecast for problematic alcohol use. Compared to those in the low ACEs class, young adults in the high multiple ACEs class reported more alcohol-related problems and psychological symptoms (Gracia et al., 2015).
Parental Bonding
Another crucial shared environment is parental bonding among persons with alcohol use disorder. Research studies have investigated the interplay between child characteristics lack of self-control, aggression and parenting on problematic alcohol use in young adulthood. A longitudinal study showed strong effects of childhood aggression and poor parenting on enhanced levels of problem drinking in young adulthood. Further, the combination of high levels of aggression and low levels of parenting were related to problem drinking in men, whereas the combination of low parental control and low levels of affection were related to problem drinking in women (Schneider et al., 2015). Affectionless control is the most frequent parental bonding style among drug and alcohol abusers. Maternal/paternal care and overprotection have shown an association with the onset and the use of specific substances (Vyssoki et al., 2011). Higher levels of positive parenting are related to a lower incidence of AUD (Boden et al., 2021). Drug dependent individuals perceive their parenting was characterised by affection less control, higher protection and low care (Jacob Johney 1990).
Temperament
Novelty seeking was most associated with increased alcohol, cannabis, and cocaine involvement. Harm avoidance and benzodiazepine use are interrelated. Abstinence was lower in cannabis, benzodiazepine, cocaine-dependents, and hallucinogen users with such characteristics (Polderman et al., 2015). In temperament, cyclothymic scores have significantly influenced the age at onset of alcohol abuse and alcohol dependence (Ward et al., 2014). So-called additive genetic cause accounted for 61% of the difference in attention deficit hyperactivity disorder (ADHD), and 28% in substance abuse. Shared environmental factors accounted for 34% of the variance in ODD. The genetic causes of difficult temperament were highly associated with preschool ADHD, and Substance use disorders. Shared family factors accounted for the temperamental trait of resistance to control (Silberg et al., 2015; Clifford et al., 2015).
How can the risk for alcohol use be reduced?
Twin and family studies have found critical genetic and environmental components in the inheritance of substance use disorders, and modern advances in genetics are making it possible to find out specific causes that may prejudice an individual to these disorders. Adolescence is a crucial period for initiation, experimentation, and establishing more regular patterns of use of alcohol and other drugs. Adolescence substance use is a known risk factor for developing later alcohol and substance use problems. Understanding the early risk factors and process that makes these adolescents vulnerable to substance use disorders is crucial to developing effective strategies for prevention with relevant psycho-social interventions (Centers for Disease Control and Prevention, 2019).
Prevention of Adverse Childhood Experiences
Adverse Childhood Experiences and their associated harms are preventable. Providing and maintaining safe, stable, nurturing relationships and environments for all children and the families can be prevented ACE and help children acquire their optimal health and life potential (Kendler et al., 2003).
Risk of shared environments in Alcohol use disorder
The elementary structure of the gene and environmental risk factors for alcohol and drug use disorders and other psychiatric disorders in men and women is very similar. Genetic risk factors predispose to two broad groups of internalizing and externalizing disorders. Substance use disorders have disorder-specific genetic risks. The shared environment significantly influences conduct disorder and adult antisocial behaviour (Peay & Austin, 2011).
Environmental factors include anything outside of the genome that can affect the expression of a gene, including the in-utero environment, shared home environments, type and quality of social interactions and experiences. Environmental factors act on gene expression throughout the lifetime, from preconception until death. Based on an individual's genes, he or she might not react to a particular environmental factor at all, or the environmental factor might be beneficial or protective, or the environmental factor might be harmful. These effects might be different at different times in a person's life-that is, something that is harmful in infancy might be neutral in later childhood and protective as an adult.
Many families have an intuitive understanding that personal experiences or environment can contribute to psychiatric disorders. For example, a stressful event of some kind often precedes an episode of anxiety, depression, mania, or psychosis, and affected individuals and their families frequently notice this temporal connection. Other families may note the association between substance use and the onset of psychiatric symptoms or perceive a complex home environment in the onset of psychiatric disorder. Families and clinicians naturally and correctly have a high level of interest in environmental risk factors for psychiatric disorders. In theory, few environmental factors are controllable and modifiable, and there are both risk-increasing and protective environmental factors. If we can identify and modify risk factors, it would be possible to reduce the risk for psychiatric illness and substance use disorders in individuals at-risk. For schizophrenia, stress, life events such as the death of a loved one, a relationship breakup, traumatic experiences such as accidents, financial or work-related crises certainly contribute to the development of psychiatric illness, drug use, parental age, obstetric complications, birth season, head injury, urban upbringing, immigration, maternal famine, infection(Keyes et al., 2014).
Strengths:
The study reviewed shared environments in persons with alcohol and other substance use disorders and co-morbidities, which would help the mental health professionals to understand the influence of shared environments while providing clinical care for vulnerable populations.
Conclusion
Shared environmental factors such as adverse childhood experiences or childhood trauma within 18 years of life, novelty and adventurous seeking, cyclothymia, immediate need gratification contribute to alcohol use disorder development. Positive parenting is associated with a lower incidence of AUD. Understanding the influence of shared environments and providing tailor-made psycho-social interventions would reduce the risk and prevent alcohol use disorder development.
PRISMA Flow Diagram.
(Moher et al.,2009).
Acknowledgement
Dr. Sanjeev Jain, Senior Professor & Dean (Behavioural Sciences), Department of Psychiatry, NIMHANS, Bangalore. Principal Investigator, Accelerator program for discovering in Brain Disorders using stem cells (ADBS), Department of Biotechnology, Government of India.
Funding Source: First author received funding support from the project titled "Accelerated program for discovery in brain disorders using stem cells (ADBS) Department of Bio-Technology, Government of India by grant number: BT/PR17316/MED/31/326/2015.
Footnotes
Conflict of Interest: Nil
References
- Adriana MT, Florence KC, Maria LSF (2010). Childhood trauma in substance use disorder and depression: An analysis by gender among a Brazilian clinical sample. Child Abuse & Neglect, (34), 95–104. [DOI] [PubMed] [Google Scholar]
- Ambekar A, Agrawal A, Rao R, Mishra AK, Khandelwal SK, Chadda RK on behalf of the group of investigators for the National Survey on Extent and Pattern of Substance Use in India (2019). Magnitude of Substance Use in India. New Delhi: Ministry of Social Justice and Empowerment, Government of India [Google Scholar]
- Baker H, Maes H, Kendler S, Gue M. (2012). Shared Environmental contributions to substance use. Behavior Genetics, 42 (3), 345–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman KE, Ennett ST (1996). On the importance of peer influence for adolescent drug use: Commonly neglected considerations. Addiction, 91(2), 185–198. [PubMed] [Google Scholar]
- Bennett & Kemper, (1994). Is Abuse during Childhood a Risk Factor for Developing Substance Abuse Problems as an Adult? Journal of Developmental and Behavioral Practice, 15 (6), 426–9. [PubMed] [Google Scholar]
- Boden Joseph & Crossin Rose & Susan Cook & Greg Martin & James Foulds & Giles Newton-Howes (2021). Parenting and Home Environment in Childhood and Adolescence and Alcohol Use Disorder in Adulthood. Journal of Adolescent Health. 69 (10), 1016. [DOI] [PubMed] [Google Scholar]
- Cavanaugh E, Petras H, Martins S. (2015). Gender-specific profiles of Adverse childhood experiences, Past year Mental and Substance use Disorders, and their Associations among a National Sample of Adults in the United States. Social Psychiatry Epidemiology, 50(8), 1257–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2019). Preventing Adverse Childhood Experiences: Leveraging the Best Available Evidence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Chilcoat HD,Anthony JC. (1996). Impact of parent monitoring on initiation of drug use through late childhood. J Am Acad Child Adolesc Psychiatry, 35(1), 91–100. [DOI] [PubMed] [Google Scholar]
- Clifford S, Chalfant LK, Goldsmith H (2015). The Unique and Shared Genetic and Environmental Contributions to Fear, Anger, and Sadness in Childhood; Child Dev, 86(5), 1538–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels. D, Plomin R (1985). Differential experience of siblings in the same family. Developmental Psychology, 21(5), 747–760. [Google Scholar]
- Down WR, Harrison L (1998). Childhood maltreatment and the risk of substance problems in later life. Health Soc Care community, 6, 35–46. [DOI] [PubMed] [Google Scholar]
- Engels E, Vermulst A, Dubas S, Bot M, Gerris J. (2005). Long-Term Effects of Family Functioning and Child Characteristics on Drinking in Young Adulthood. European Addiction Research, 11, 32–37. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH &Bihun JT (1997). Conceptualizing genetic influences on early behavior development, Acta paediatrica 422, 54–59. [DOI] [PubMed] [Google Scholar]
- Gracia S, Raina M, Aloi M, Palmieri A, Pellegrino A, Manfrida P, Montesano F, Grade B, Fazio D S, Fazio D P. (2015). Parental Bonding in substance and alcohol abusers. Heroin Addiction and Related Clinical Problems. [Google Scholar]
- Gururaj G, Murthy P, Girish N, Benegal V. (2011). Alcohol-related harm: Implications for public health and policy in India, Bengaluru, India, (73). NIMHANS. [Google Scholar]
- Gururaj G, Varghese M, Benegal V, Rao GN, Pathak K, Singh LK, et al. (2016). National Mental Health Survey of India, 2015–16. Collaborators group. Summary. National Institute of Mental Health and Neuro Sciences. NIMHANS Publication No. 128, Bengaluru. [Google Scholar]
- Heath AC, Martin NG (1988). Teenage alcohol use in the Australian twin register: genetic and social determinants of starting to drink. Alcohol Clin Exp Res, 12(6),735–741. [DOI] [PubMed] [Google Scholar]
- Hill J, Emery JH, Harden KP, Mendle J, Turkheimer E (2008). Alcohol use in adolescent twins and affiliation with substance-using peers. J Abnorm Child Psychol, 36(1), 81–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hops H, Andrews JA, Duncan SC, Duncan TE, Tildesley E (2000). Adolescent drug use development: a social interactional and contextual perspective. In: Sameroff AJ., Lewis M, Miller SM,(Eds). Handbook of developmental psychopathology. Kluwer Academic/Plenum Publishers, New York, 589–605. [Google Scholar]
- Howkins DJ, Catalano RF, Miller YJ (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull, 112, 64–105. [DOI] [PubMed] [Google Scholar]
- Johney Jacob (1990). Parent-child relationship in families of male drug dependents and normals. NIMHANS, Bengaluru. [Google Scholar]
- Kendler KS (1996). Parenting: a genetic-epidemiologic perspective. Am J Psychiatry, 153, 11–20. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC (2003). The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry,60 (9), 929–37. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, & Shear MK (2014). The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. The American journal of psychiatry, 171(8), 864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosterman R, Hawkins JD, Guo J, Catalano RF, Abbott RD (2000). The dynamics of alcohol and marijuana initiation: patterns and predictors of first use in adolescence.Am J Public Health, 90 (3), 360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumpfer K L, & Bluth B. (2004). Parent/child transactional processes predictive of resilience or vulnerability to substance use disorders. Substance Use & Misuse, 39 (5), 671–698. [DOI] [PubMed] [Google Scholar]
- Larkin H, & Records J (2007). Adverse childhood experiences: Overview, response strategies, and Integral Theory. Journal of Integral Theory and Practice, 2(3), 1–25. [Google Scholar]
- Latendrese J, Rose J, Viken, Pulkkin L, Kaprio J, Dick M (2008). Parenting mechanisms in links between parents and Adolescents, Alcohol Use Behaviors. Alcohol Clin Exp Res, 32 (2), 322–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mary-Anne E & Bernard J A (2007). Genetic and Environmental Risk Factors for Alcohol Use Disorders in American Indians and Alaskan Natives, Am J Addict, 26, (5)461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mc Gue M & Bouchard TJ (1998). Genetic and environmental influences on human behavioural differences, Annual Review of Neuroscience, 21, 1–24. [DOI] [PubMed] [Google Scholar]
- Schwandt Melanie L., Heilig Markus, Hommer Daniel W., George David T., Ramchandani Vijaya A.. (2013). Laboratory of Clinical and Translational Studies, National Institute on Alcohol Abuse and Alcoholism, Alcohol Clin Exp Res, 37 (6), 984–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moe J, Johnson J L, & Wade W. (2007). Resilience in children of substance users: In their own words. Substance Use & Misuse, 42 (2–3), 391–398. [DOI] [PubMed] [Google Scholar]
- Peay H, Austin J. (2011). How to talk with the families about genetics and psychiatric illness. W.W. Norton & Company, New York. [Google Scholar]
- Polderman TJ, Benyamin B, de Leeuw CA, Sullivan PF, van Bochoven A, Visscher PM, et al. , (2015). Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nature genetics, 1, 47(7), 702–9. [DOI] [PubMed] [Google Scholar]
- Rehan W, Antflok J, Johansson A, Jern P, Santtila P. (2017). Experiences of Severe childhood maltreatment, Depression, Anxiety and Alcohol abuse among adults in Finland. PLoSONE (12)5, e0177252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose RJ, Dick DM, Viken RJ, Pulkkinen L, Nurnberger JI Jr & Kaprio J (2004). Genetic and environmental effects on conduct disorder, alcohol dependence symptoms, and their covariation at age 14, Alcoholism: Clinical and Experimental Research 28, 1541–1548. [DOI] [PubMed] [Google Scholar]
- Rose RJ, Viken RJ, Dick DM, Bates J, Pulkkinen L & Kaprio J (2003). It does take a village: non-familial environments and children's behavior, Psychological Science 14, 273–277. [DOI] [PubMed] [Google Scholar]
- Rutter M, Silgerg J, O'Connor T & Simonoff E (1999). Genetics and child psychiatry: II. Empirical research findings, Journal of Child Psychology and Psychiatry 40. 19–55. [PubMed] [Google Scholar]
- Sargent JD, Dalton M (2001). Does parental disapproval of smoking prevent adolescents from becoming established smokers? Pediatrics, 108, (6),1256–1262. [DOI] [PubMed] [Google Scholar]
- Schneider R, Ottoni L, Carvalho H, Elisabetsky E, Lara D. (2015). Temperament and character traits associated with the use of alcohol, cannabis, cocaine, benzodiazepines, and hallucinogens: evidence from a large Brazilian web survey. Revista Brasileira de Psiquiatria, 37, 31–39. [DOI] [PubMed] [Google Scholar]
- Shin H, Edwards E, Heeren T, Amodeo M. (2010). Relation between Multiple Factors of Maltreatment by a Parent or Guardian and Adolescent Alcohol Use. The American Journal onAddictions. [DOI] [PubMed] [Google Scholar]
- Silberg LJ, Gillespie N, Moore A, Eaves JL (2015). Shared Genetic and Environmental Influences on Early Temperament and Preschool Psychiatric Disorders in Hispanic Twins; Twin Research and Human Genetics; 18(2), 171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Barrera M Jr. (1995). A longitudinal examination of the reciprocal relations between perceived parenting and adolescents' substance use and externalizing behaviors. Dev Psychol 31(2), 322–334. [Google Scholar]
- Verhulst B, Neale M, Kendler K. (2015). The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med: 45 (5), 1061–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyssoki B, Bluml V, Gleiss A, Friedrich F, Kogoj D, Walter H, Zeiler J, Hofer P, Lesch OM, Erfurth A. (2011). The impact of temperament in the course of alcohol dependence: Journal of Affective Disorders, 135, 177–183. [DOI] [PubMed] [Google Scholar]
- Walden B, McGue M, Iacono W, Burt SA, Elkins I. (2004). Identifying shared environmental contributions to early substance use: the respective roles of peers and parents. J Abnorm Psychology. 113(3), 440–450. [DOI] [PubMed] [Google Scholar]
- Waldman ID, DeFries JC &Fulker DW (1992). Quantitative genetic analysis of IQ development in young children: multivariate multiple regression with orthogonal polynomials, Behavior Genetics 22, 229–238. [DOI] [PubMed] [Google Scholar]
- Ward B, Snow P, James. P, Griffith J (2014). The influence of parents and siblings on children's and adolescents' attitudes and behaviors towards alcohol: A critical review of the literature: DrinkwiseAustralia [Google Scholar]
- WHO. (2014). Global status report on alcohol and health. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Wills T A, & Dishion T J. (2004). Temperament and adolescent substance use: A transactional analysis of emerging self-control. Journal of Clinical Child and Adolescent Psychology, 33,69–81. [DOI] [PubMed] [Google Scholar]