Abstract
The use of infant formula is widespread internationally. In Australia, 55% of infants receive formula before 6 months of age, with higher rates among disadvantaged communities. Infant formula use can contribute to childhood overweight and obesity, through formula composition and feeding behaviours, such as adding cereal to bottles and parental feeding style. While information abounds to promote and support breastfeeding, formula‐feeding parents report a paucity of advice and support; many rely on formula packaging for information. This study systematically searched and reviewed online resources for infant formula and bottle feeding from Australian governments, health services, hospitals, and not‐for‐profit parenting organisations. A comprehensive search strategy located 74 current resources, mostly for parents. Researchers evaluated the resources against best practice criteria derived from Australian government and UNICEF guidelines on six topics. They assessed how comprehensively the resources addressed each topic and whether the resources provided all the information necessary for parents to understand each topic. The mean ‘comprehensiveness’ rating for topics across all resources was 54.36%. However, some topics were addressed more fully than others. Information on ‘discussing infant formula with health workers’ and on ‘preparing infant formula’ was more frequently accurate and comprehensive. However, there was much less comprehensive information on ‘using infant formula’, including amounts of formula to feed, use of bottle teats, appropriate bottle‐feeding practice and responsiveness to infant satiety cues. Over half the resources were written at an acceptable reading level.
Keywords: artificial feeding, bottle feeding, childhood obesity, feeding behavior, health information, infant feeding, infant formula, patient education
Key messages
Insufficient formula‐feeding support from health services can lead to parents relying on formula packaging or other commercial information.
Most formula‐feeding resources from Australian healthcare organisations focus on preparing infant formula and using infant formula. However, comprehensiveness of information varies—on average, information on preparing infant formula was more comprehensive than that on using infant formula.
Many resources do not address responsive bottle‐feeding practices, which impacts risk of infant overweight and obesity.
The Australian government infant feeding guidelines should be revised to include more comprehensive best‐practice formula‐feeding recommendations; subsequently, this should be reflected in formula‐feeding information from health organisations.
1. INTRODUCTION
Breastfeeding infants is optimal, with numerous health benefits, including decreasing the risk of overweight and obesity (Victora et al., 2016). If infants are not breastfed, commercial infant formula is the only appropriate food for 6 months until infants start solid foods. Infant formula use should continue until at least 12 months of age, when infants can transition to cow's or other calcium‐rich milks (National Health and Medical Research Council, 2012).
Formula feeding may increase the risk of infant overweight, influenced by formula type, mechanism of delivery and feeding behaviours. Infant formula contains higher protein than breast milk, potentially resulting in increased fat deposition and rapid weight gain in formula‐fed infants (Brands et al., 2014). Using infant formula with lower protein content may reduce obesity risk at 2 years (Koletzko et al., 2009), with sustained benefits reported up to age 6 (Weber et al., 2014). A systematic review identified formula‐feeding practices associated with unhealthy weight gain: using ‘follow‐on’ formula with higher protein content, marketed for infants aged over 6 months; adding cereals into bottles; using formula bottles in bed; using larger bottles; and increasing formula intake (Appleton, Russell, et al., 2018). Similarly, an integrative review indicated that parental feeding style, control over feeding, and responsiveness to infant satiety cues, can influence bottle feeding and subsequently, formula intake (Kotowski et al., 2020). Responding to infant satiety cues may guard against excess weight gain, whereas feeding until the bottle is empty may lead to overfeeding and contribute to weight gain (Li et al., 2008, 2012; Shloim et al., 2017). Cup feeding, which is recommended by the World Health Organization for mothers intending to breastfeed until the successful establishment of breastfeeding, can enable infants to control the pace and volume of expressed breast milk or formula to avoid over‐feeding, and can support subsequent breastfeeding, especially among preterm infants (Baby‐Friendly Health Initiative Australia, 2020; McKinney et al., 2016). However, this practice rarely continues beyond the neonatal phase: once infants require larger volumes of milk, parents use supplemental feeding devices or bottles to supplement with expressed breast milk or formula. In Australia, if the mother's intention is to formula feed rather than breastfeed, cup feeding is not advised; parents are usually provided with information on best practice bottle‐feeding (Baby‐Friendly Health Initiative Australia, 2020).
Despite the evidence on the benefits of breastfeeding, many parents use infant formula for various reasons, including supplementing perceived insufficient breast milk; increasing infant satiety; assisting breastfeeding cessation; supporting maternal return to work; allowing other people to help with infant feeding; increasing infant body weight; and avoiding stigma from public breastfeeding (Brown et al., 2011; Choudhry & Wallace, 2012; Hawley et al., 2015; Hunter‐Adams et al., 2016; Kuswara et al., 2016; Osman & el‐Sabban, 1999; Twamley et al., 2011). Infant formula use is extensive internationally, with only 41% of children younger than 6 months being exclusively breastfed (World Health Organization, 2019). The 2010 Australian National Infant Feeding Survey indicated 55% of infants receive some formula by 6 months (Australian Institute of Health and Welfare, 2011). In a socially and economically disadvantaged area of Sydney, Australia, breastfeeding was less common in mothers who were unmarried, living in disadvantaged accommodation, current smokers and with lower levels of education; and at 2 weeks of age, 40% of infants were not breastfed (Yeoh et al., [Link], 2007). Longitudinal data from this region found that infant formula or solid foods were introduced at average 2 months of age; and that introduction of infant formula or solid foods together with cessation of breastfeeding within 4 months was linked to 2.09 increased odds of child overweight and obesity (Mannan, 2018). It is likely that mothers not breastfeeding young infants are feeding with infant formula or solid food. Infant feeding decisions are impacted by economic, social, and environmental factors—to observe decreased breastfeeding from social disadvantage in a high‐income country such as Australia, it is anticipated that greater barriers to breastfeeding and increased formula feeding will also occur internationally where inadequate healthcare support, aggressive marketing of breast milk substitutes, and decreased maternity workplace support are more prevalent (World Health Organization, 2019).
Healthcare professionals have a responsibility to protect, support and promote breastfeeding as the ‘norm’, and to provide parents with support and education to optimise feeding practices. However, parents whose infants require formula for medical reasons or who make an informed decision to formula feed also need timely, unbiased, and accessible information to support best‐practice formula feeding. It is imperative that these parents adopt safe practices that reduce the risk of excess weight gain. In Australia, the National Breastfeeding Strategy (COAG Health Council, 2019) and the amended Baby‐Friendly Hospital Initiative Australia guidelines (Baby‐Friendly Health Initiative Australia, 2020) acknowledge the need for families who do not breastfeed to feed infants safely. Both address this issue to provide a framework and guidelines for health professionals both to scale up breastfeeding and to ensure that families who use formula have appropriate information and education.
In 2018, the World Health Organization (WHO) Global Criteria for the Baby‐Friendly Hospital Initiative (BFHI) was revised to ensure all mothers were supported to make a fully informed decision about formula feeding, with education for safe formula‐feeding practices, responsive feeding, and bottle and pacifier safety (World Health Organization, 2018). In Australia (Baby‐Friendly Health Initiative Australia, 2020), parents receive information and guidance on: safe preparation, storage, and handling of infant formula; risks to the baby from incorrect preparation and handling; demonstration and supervised practice in making infant formula from powder; support services for infant feeding after discharge; and best‐practice for bottle feeding, including responsive feeding.
However, despite their specific needs for education and guidance from reliable sources, previous research suggests that parents who formula feed receive insufficient support. A survey of Australian formula‐feeding mothers found that more respondents received advice about formula feeding from the formula tin than they did from maternal and child health nurses (90% vs. 66%); further, they considered the advice from a formula tin as helpful as advice from a nurse (98% vs. 92% agreement on the information source being ‘helpful’) (Appleton et al., 2020). These findings align with studies from Ireland and Scotland that reported dissatisfaction by mothers with the amount and range of information available to assist them with formula feeding (Cairney et al., 2006; Tarrant et al., 2013), such as needing information and support about suitability of different formulas; sterilising equipment, preparing formula, and choosing suitable bottle teats; feeding processes, such as volume of formula, preventing under‐ or over‐feeding, and feed timing; and receiving help from midwives with feeding.
Resources provided by wider health services may also be insufficient to meet the needs of parents who use formula. A survey of health services in regional New South Wales, Australia, identified more education resources about breastfeeding than formula feeding, and more services providing breastfeeding support (via group, individual and telephone) than formula‐feeding support (Hegedus & Mullan, 2015). A New South Wales study of nurses in early parenting residential units reported the need for resources aligned with current bottle‐feeding education, as bottle‐feeding handouts were unavailable; parents experienced conflicting information or lack of adequate education on formula preparation and equipment sterilisation; and limited practical bottle‐feeding information was available for parents (Kotowski et al., 2021). A study of United Kingdom (UK) midwives identified gaps in how they supported formula feeding mothers: information was focused on formula preparation, with follow‐up only if problems occurred; few midwives demonstrated feeding, equipment sterilisation or formula preparation in antenatal classes or postnatal ward education; written information was limited to leaflets (Battersby, 2010). Before development of national health department and UNICEF UK resources on formula feeding from 2007 onwards, these midwives reported that formula companies and representatives were their main source of formula information.
These findings highlight the need for unbiased information sources. In accordance with The WHO International Code of Marketing of Breast‐Milk Substitutes (WHO Code), information provided by companies to health professionals should be restricted to scientific and factual information (World Health Organization, 1981). The WHO Code intends to protect pregnant women, mothers, and families from practices and materials that may impact negatively on breastfeeding establishment and continuation (Baby‐Friendly Health Initiative Australia, 2020). Guides further support health professionals to use the WHO Code in daily practice and recognise where and how advertising and marketing can undermine infant feeding recommendations (UNICEF United Kingdom, 2019).
In Australia, the WHO Code principles are enacted by the Marketing in Australia of Infant Formulas: Manufacturers and Importers Agreement (MAIF Agreement) (Infant Nutrition Council, 1992), a voluntary code of conduct for industry. Violations to the MAIF Agreement are addressed through a public complaints process with the federal government health body and reported online (Australian Department of Health, 2021). Inevitably, industry resources will be used as part of education, that is, reconstituting infant formula following the powder‐to‐water ratio individualised for each brand—by referring and recommending parents follow the manufacturer's instructions, health professionals may indirectly be acknowledging manufacturers as the experts on formula. The MAIF Agreement in Australia is important as it aims to contribute to adequate and safe nutrition for infants by promoting and protecting breastfeeding, through ensuring the proper use of breast milk substitutes and adequate information through appropriate marketing and distribution. However, for countries who are not signatories to the WHO Code, it is anticipated that formula advertising and marketing are more prevalent; and even in countries which are signatories or partial signatories to the WHO Code, violations—such as free samples of infant formula received from health professionals—are observed (Hernández‐Cordero et al., 2019; Hidayana et al., 2017; Liu et al., 2014).
This study explores the resources to support formula feeding currently available from Australian health and parenting organisations. It focuses on both the accessibility and the content of resources, specifically how effectively they promote formula feeding practices that are safe and likely to minimise excess weight gain.
Insufficient support may result in parents failing to understand safe formula preparation. Analysis of 2005–2007 longitudinal data from the US Infant Feeding Practices II study found that of mothers who fed their infants formula at age 2 months, 88% did not receive instruction on formula preparation and 82% did not receive instruction on formula storage (Labiner‐Wolfe et al., 2008). At 5 months, 77% and 73% still had not received appropriate instructions, respectively. This may lead to gaps in knowledge about safe preparation and risk of microbial contamination: of mothers who fed their infants formula at age 2 months, 55% did not always wash their hands with soap before formula preparation, 33% did not always wash and sterilise bottle teats between use, and 35% heated formula bottles in a microwave oven (Labiner‐Wolfe et al., 2008). Similarly, a survey with 417 Italian parents with children under 3 years found that 73% believed that infant formula did not contain bacteria and 35% believed microwaves were appropriate for reheating formula bottles (Calamusa et al., 2009).
Parent information on formula feeding should adhere to the WHO Code by addressing social and financial implications of formula use, health hazards of inappropriate foods, feeding methods and unnecessary or improper formula use (World Health Organization, 1981). Moreover, it is equally important that education materials are comprehensible to parents. Several studies evaluating paediatric health information for parents show that the reading level of resources are typically above the average American adult 8th grade reading level (Australian Government, 2020). Across three studies on health‐related resources for parents (Arnold et al., 2006; Oermann et al., 2003; Rothrock et al., 2019), written resources had an average reading level of 9th grade and above, and only 42%, 8% and 29% respectively were written at an 8th grade reading level or below. Some exceptions exist: an evaluation of paediatric dental education materials from government, industry and commercial sources had an average reading grade level of 4.7, 7.4, and 8.1, respectively (Hendrickson et al., 2006). One study on readability of American infant formula instructions found that instructions on step‐by‐step preparation, warnings about formula safety and hygienic handling were written at an 8th grade reading level, but directions for preparing and using infant formula and storing formula tins were at a college reading level (Wallace et al., 2016).
These gaps in appropriate and accessible education resources to support formula feeding indicate the need for comprehensive and consumer‐friendly resources. In the absence of appropriate support, parents may turn to less reliable or more biased information sources. Given that over half of Australian infants receive some formula before 6 months of age, this study aimed to identify and evaluate the information provided in infant formula‐feeding resources currently available online from Australian healthcare organisations. It assessed their readability and evaluated the content against national guidelines on infant feeding and aimed to examine gaps in information on formula feeding in regard to infant overweight and obesity risk, safe formula preparation practices, and best‐practice and responsive feeding processes.
2. METHODS
2.1. Search engine strategy
Using the Google Chrome browser during March and April 2020, we searched for websites or other online resources on infant or baby formula feeding, produced by Australian state or territory governments, public and private hospitals, or established not‐for‐profit or non‐government parenting organisations. Online resources could be for parents (consumers) or for health professionals working with infants. Searches were undertaken without login to a Google Account, to avoid previous search history and cookies affecting the search results. This study reviewed existing and publicly available resources, and did not require ethics approval.
Table 1 presents an abbreviated table of search terms and strategy, with a full list in Appendix 1.
Table 1.
Infant formula or bottle‐feeding resource search strategy, using Google search engine
| Infant or baby formula search terms | Support search terms | State or territory search terms | State or territory health service search terms | Private hospital search terms | Domain specifiers |
|---|---|---|---|---|---|
| Infant OR baby milk | support | .act | “ACT Health” | Epworth | .org |
| Infant OR baby formula preparation | how to formula OR bottle feed | .nsw | “Northern Territory” “Department of Health” | “Calvary Hospital” | .gov |
| Infant OR baby formula milk | .qld | “Northern Territory” “health service” | “Sydney Adventist Hospital” | .edu | |
| Infant OR baby formula feeding | .sa | “NSW Health” | “St John of God” | .net | |
| Infant OR baby formula | .tas | “Queensland Health” | “Ramsay Health Care” | .au | |
| Infant OR baby feeding milk | .vic | “SA Health” | “Mater Health” | ||
| Infant OR baby bottle feeding | .nt | NSW Health | “HealthE Care” | ||
| Formula feeding | .wa | NSW or “New South Wales” “Local Health District” | “Cabrini Health” | ||
| Bottle feeding | “ACT” | Queensland “Hospital and Health Service” | Healthscope | ||
| Baby formula | “Australian Capital Territory” | “South Australia” “local health network” | |||
| “New South Wales” | Tasmania “Department of Health and Human Services” | ||||
| “Northern Territory” | Tasmania “health organisation” | ||||
| “South Australia” | Victoria “Department of Health” | ||||
| “Western Australia” | Victoria “health service” | ||||
| Australia | Victoria Department of Health and Human Services | ||||
| Canberra | “Western Australia” “Department of Health” | ||||
| NSW | “Western Australia” “health service” | ||||
| QLD | |||||
| Queensland | |||||
| Tasmania | |||||
| VIC | |||||
| Victoria |
Search strategy: (one infant or baby formula search term) AND (optional one support search term) AND [(one state or territory search term) OR (one state or territory health service search term) OR (one private hospital search term)] AND (any domain specifier).
The search strategy combined: an infant formula search term; an optional support search term; a search term on Australian state and territories, Australian government health services, or Australian private hospital networks; and a domain specifier for Australian organisations, networks, educational facilities, or government websites.
Two reviewers then assessed each identified resource, using a purpose‐built data extraction form, constructed with REDCap electronic data capture tools (Harris et al., 2009), including availability, scope, readability, and an instrument for evaluating formula‐feeding information (Appendix 2).
2.2. Evaluation criteria
To assess their quality, resources were evaluated against pertinent information about formula feeding for infants, extracted from the Australian National Health and Medical Research Council Infant Feeding Guidelines for Health Workers (National Health and Medical Research Council, 2012), hereafter referred to as Infant Feeding Guidelines. These guidelines, published in 2012 and drawing on the WHO Code, focused on using infant feeding as an opportunity for parent–infant bonding, preventing air swallowing during feeding, and bottle feeding according to infant appetite and need. However, the Infant Feeding Guidelines do not address cues to identify infant appetite and need; we therefore used the UNICEF UK resources on responsive feeding, published from 2015 to 2020 (National Health Service & UNICEF United Kingdom, 2015; UNICEF United Kingdom & First Steps Nutrition Trust, 2019; UNICEF United Kingdom, 2016a, 2016b) for data evaluation, adding criteria to the ‘using infant formula’ topic: holding the infant comfortably upright, stimulating the infant rooting reflex to start feeding, mimicking the stop‐start motion of breastfeeding, and identifying infant cues that signal pauses in feeding.
We developed the evaluation instrument to assess whether and how well the resources addressed each item specified in the Infant Feeding Guidelines and the UNICEF UK documents. Evaluation criteria were compiled into six topics (Appendix 2):
-
(1)
Composition of infant formula (3 items).
-
(2)
Information that health workers should discuss with parents regarding infant feeding, such as hazards of improper formula preparation and storage and suitable duration of formula feeding (5 items).
-
(3)
Preparing infant formula (49 items), with subtopics:
-
I.
Risk of bacterial contamination (1 item),
-
II.
Formula preparation from powder (25 items) and transporting (6 items), and
-
III.
Equipment sterilisation (17 items).
-
I.
-
(4)
Using infant formula (23 items), with subtopics:
-
I.
Use of bottle teats (4 items),
-
II.
Appropriate bottle‐feeding practice (11 items),
-
III.
Amount of formula to feed infants (8 items), and
-
IV.
Use of feeding cups (2 items).
-
I.
-
(5)
Special infant formula (9 items).
-
(6)
Fluoride in infant feeding (2 items).
Two items were included in more than one subtopic but only counted once in analysis: ‘bottle feed according to infant appetite and need’ and ‘do not add cereal or any other foods to infant formula’ appear across the ‘preparing formula from powder’, ‘appropriate bottle‐feeding practice’ and ‘amount of formula to feed infants’ subtopics.
For every resource, we judged whether each topic or subtopic was relevant or not. Relevant items within these topics or subtopics were scored on the evaluation instrument as: Correctly addressed (+1), Not addressed (0), Not relevant, or Incorrectly addressed (−1). Each resource received a percentage score for each topic (referred to as ‘comprehensiveness’): the number of items correctly addressed, divided by the number of relevant items in that resource. To be ‘comprehensive’, a resource should provide accurate information on all the items necessary to fully understand that topic. A resource could theoretically address one topic with a high level of comprehensiveness and another topic less comprehensively. A total percentage score was also calculated, combining the total scores for all topics addressed by the resource.
2.3. Readability
Readability assessment was undertaken for consumer resources only, as health professionals would require higher literacy to understand more complex technical or health‐related information.
Readability, or grade level of written text, was measured using the Flesch–Kincaid (F–K) (Kincaid et al., 1975) and Simple Measure of Gobbledygook (SMOG) (McLaughlin, 1969) tools. A section of text was applied through an online readability calculator (ReadabilityFormulas.com, undated) (F–K, online score; SMOG) or Microsoft Word software (2010 and later; Microsoft Corporation) (Microsoft Word Help Center, 2019) (F‐K, Microsoft score). Each reviewer selected the section of text they assessed using these measures.
F–K and SMOG scores are reported as American reading grades. The Australian writing guide for government content (Australian Government, 2020) advises writing for a reading level of Australian school years 7 and 8, respectively, which correspond to the equivalent American reading grades (Cheng & Dunn, 2015). Resources at the 8th grade or below reading grade were deemed to be an ‘acceptable’ reading level for consumer education material.
2.4. Inter‐rater reliability
2.4.1. Evaluation scores
Resources were evaluated by two authors CR and HC from May 2020 to March 2021. Any disagreements between the two authors were resolved with a consensus discussion.
The degree of agreement between raters on the six topics addressed or not addressed by the resource was calculated.
Rater agreement was calculated using intraclass correlation (ICC), using the two‐way random model, or Krippendorff's α. The authors sometimes disagreed on whether or not topics were addressed by resources, leading to some missing data for total percentage score by topic. Where there was missing paired data, indicated by a negative Cronbach's α score, Krippendorff's α was calculated for rater agreement in paired total percentage scores. Where there was no missing paired data, ICC was calculated for rater agreement in paired total percentage scores.
2.4.2. Readability
Inter‐rater reliability was calculated for readability scores using Pearson's correlation.
2.5. Statistical analysis
Statistical analysis was undertaken in IBM SPSS Statistics for Windows (IBM Corp, Version 25.0.). Significance was indicated at p < 0.05.
2.6. Resource selection
All relevant resources identified from the Google search strategy were downloaded between March and April 2020, and screened for inclusion.
Exclusion criteria were resources no longer in use, for example, superseded by newer resources by the same developers, and pictorial resources or those with very limited text, as the evaluation criteria focused on the written information contained in resources. Consequently, several resources targeted towards Australian Aboriginal and Torres Strait Islander communities were excluded from analysis. A review of literature on health education with Australian Indigenous communities demonstrated that face‐to‐face oral education and verbal explanation, supported by interactive or visual aids, pictures, and short and straightforward language, are more culturally appropriate (Australian Commission on Safety and Quality in Health Care, 2020; Charles, 2016; Davies et al., 2014; Peake et al., 2019; Schoen et al., 2010; Vass et al., 2011). Therefore, resources targeted for Indigenous Australian populations ideally have less written text. With evaluation criteria based on written content, our evaluation tool would artificially create a lower score for pictorial resources with minimal written information.
3. RESULTS
A total of 115 resources were identified through the Google search strategy and 16 resources through hand searching (Figure 1). After removal of duplicates and excluded resources, 74 resources were evaluated, comprising 14 handouts, 3 brochures, 10 booklets, 3 videos, 31 web pages, and 13 clinical guidelines, manuals, or local policies. Most resources were targeted towards consumers (57 resources), followed by early childcare centre staff (9) and health professionals (8). Resources were developed or last updated between 2011 and 2020, with 15 resources undated.
Figure 1.
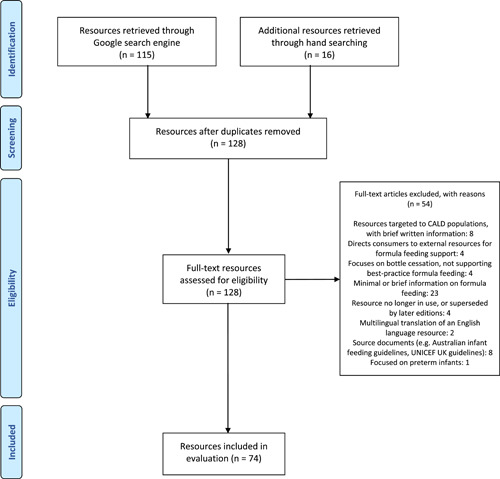
Preferred reporting items for systematic reviews and meta‐analyses flow diagram of resources included
3.1. Topics of resources
The most commonly addressed topics/subtopics were ‘preparing infant formula’ and ‘using infant formula’; the least often addressed were cup feeding, part of ‘using infant formula’ and ‘fluoride in infant feeding’ (Table 2).
Table 2.
Formula‐feeding topics addressed across resources (N = 74), by frequency
| Topic addressed | Items/subtopics addresseda | n (%) |
|---|---|---|
| Preparing infant formula | Formula preparation from powder and transport | 52 (70.3) |
| Preparing infant formula | Equipment sterilisation | 41 (55.4) |
| Using infant formula | Appropriate bottle‐feeding practice | 39 (52.7) |
| Using infant formula | Amount of formula to feed infants | 26 (35.1) |
| Discussion of infant formula with health workers | Discussion of infant formula with health workers | 24 (32.4) |
| Using infant formula | Use of bottle teats | 23 (31.1) |
| Special infant formula | Special infant formula | 22 (29.7) |
| Composition of infant formula | Composition of infant formula | 17 (23.0) |
| Preparing infant formula | Risk of bacterial contamination | 15 (20.3) |
| Using infant formula | Use of feeding cups | 5 (6.8) |
| Fluoride in infant feeding | Fluoride in infant feeding | 3 (4.1) |
aSee Section 2; the topics ‘Preparing infant formula’ and ‘Using infant formula’ were broad, which necessitated subtopics.
3.2. Scoring of resources
3.2.1. Comprehensiveness
The distribution of comprehensiveness scores was analysed with histograms (Appendix 3). Three topics demonstrated skewed distribution: ‘composition of infant formula’, ‘discussion of infant formula with health workers’ and ‘special infant formulas’. Other topics had normal distribution: ‘preparing infant formula’, ‘using infant formula’, and the combined comprehensiveness of all resources. Distribution cannot be adequately described for ‘fluoride in infant feeding’, as only three resources were presented.
The mean overall comprehensiveness of topics across all resources was 54.36% (n = 91 topics across 74 resources, SD = 22.47%; range = 0%–95.83%). For skewed data, the topic of ‘discussion of infant formula with health workers’ had the highest median comprehensiveness; for normally distributed data, the topic of ‘preparing infant formula’ had the highest mean comprehensiveness (Table 3 and Figure 2).
Table 3.
Comprehensiveness of formula‐feeding topics addressed across resources (N = 91 topics across 74 resources), percentages
| Topic addressed | n resources | Mean | SD | Median | IQR |
|---|---|---|---|---|---|
| Composition of infant formula | 17 | 49.02 | 29.15 | 66.67 | 33.33–66.67 |
| Discussion of infant formula with health worker | 24 | 75.83 | 28.66 | 100.0 | 50.0–100.0 |
| Preparing infant formula | 61 | 62.41 | 24.27 | 68.29 | 40.91–81.84 |
| Using infant formula | 49 | 37.41 | 26.16 | 34.78 | 20.0–54.76 |
| Special infant formula | 22 | 52.42 | 30.27 | 49.21 | 27.68–69.45 |
| Fluoride in infant feeding | 3 | 66.67 | 28.87 | 50.0 | 50–no upper range |
| Overall comprehensiveness of resource | 74 | 54.36 | 22.47 | 57.51 | 34.78–72.93 |
Note: Scores are reported out of 100%.
Abbreviations: IQR, interquartile range; SD, standard deviation.
Figure 2.
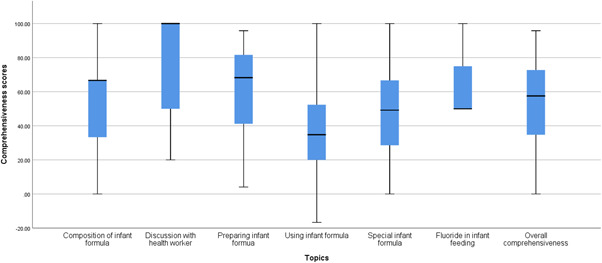
Box and whisker plot (median and IQR) of comprehensiveness of topics addressed in formula feeding resources (N = 74)
Item scoring within each topic is reported in full in Appendix 4. Comprehensiveness scores for each topic across all resources are reported in full in Appendix 5.
3.3. Items addressed
Items that were most frequently correctly addressed in resources were mostly in the topics ‘preparing infant formula’ or ‘using infant formula’: hand washing (42 of 50 resources); sterilising equipment before preparing formula (34 of 42 resources); following formula tin instructions for the correct water‐to‐formula powder ratio (42 of 47 resources); adding water to formula bottles before powder (38 of 46 resources); storing scoop in formula tin when not in use (37 of 45 resources); testing formula temperature before feeding (47 of 52 resources); not heating formula bottles in microwaves due to risk of burns (42 of 50 resources); sterilising equipment by boiling, including washing equipment with a brush and boiling in a saucepan for 5 min (35–38 of 39–41 resources); and not leaving infants unattended to drink from a propped formula bottle (32 of 38 resources).
3.4. Items not addressed
Items that were most often left unaddressed in resources tended to be in the ‘using infant formula’ topic: preferable use of faster bottle teats (unaddressed in 19 of 22 resources); checking for cracks and bacteria risk, and replacing teats regularly (21 of 22 resources); not dipping bottle teats in sugary substances (19 of 20 resources); mimicking the stop‐start motion of breastfeeding in responsive feeding (32 of 37 resources); identifying and providing examples of cues for responsive feeding, such as breaks in feeding (31 of 37 resources); and indicating constipation may occur after introducing infant formula (18 of 22 resources).
3.5. Items incorrectly addressed
Items that were most frequently incorrectly addressed were: discarding formula kept at room temperature for over 1 h (incorrectly addressed in 8 of 50 resources); bottle feeding according to infant appetite and need (3 of 41 resources); approximate formula requirements from birth to 12 months (2–4 of 12–13 resources); not using the microwave to heat infant formula (2 of 50 resources); and preferable use of faster bottle teats (2 of 22 resources).
3.5.1. Ceiling effect
A ceiling effect was observed for ‘discussion of infant formula with health worker’: 24 resources addressed this topic, with comprehensiveness ranging from 20.0% (1 resource) to 100% (13 resources).
The topic ‘discussion of infant formula with health worker’ contained five items (Appendix 6)—the ceiling effect of 13 resources achieving 100.0% comprehensiveness was due to resources only being scored for ‘correctly addressed’ (+1 score) and ‘not applicable’ (no quantitative score given and item removed from the denominator). In these resources, only one addressed all five items of the topic correctly; the other 12 resources addressed one to four items correctly with the remaining items being considered ‘not applicable’. This demonstrates methodological limitations: while many of the five items in this topic were appropriately not the focus of the resource, the method of scoring overestimates the comprehensiveness of information for the topic.
3.5.2. Comprehensiveness of ‘using infant formula’ resources by year of publication
Responsive feeding items were most frequently left unaddressed in the ‘appropriate bottle‐feeding practices’ subtopic (Appendix 4), which were evaluated using different criteria (see Section 2). A scatter plot of comprehensiveness scores for the ‘using infant formula’ resources that addressed the ‘appropriate bottle‐feeding practices’ subtopic denotes a positive trend with year of publication (Appendix 7), with a more pronounced trend for resources published after publication of UNICEF responsive feeding resources in 2015.
3.6. Readability
The 54 text resources for consumers were evaluated for readability. Three video resources were not evaluated.
Readability of written resources are reported in Table 4, which show consistency in reading grade across each of the readability measures for the 108 passages assessed by the two reviewers. Nearly half the consumer resources were at acceptable reading grade level, using the F–K online score, with higher proportions from other readability measurements (Table 4); overall, just over half of all consumer resources were at an acceptable reading level (Figure 3).
Table 4.
Readability of formula‐feeding resources for consumers (N = 54, 108 passages)
| F–K score, online | F–K score, Microsoft | SMOG score | |
|---|---|---|---|
| Readability | |||
| Median | 9th grade or above | 8th grade | 8th grade |
| IQR | 7th grade – 9th grade or above | 6th grade – 9th grade or above | 6th grade – 9th grade or above |
| Reading level (n resources, %) | |||
| Acceptable | 53 (49) | 68 (63) | 61 (57) |
| Higher than acceptable | 55 (51) | 40 (37) | 47 (43) |
Note: Acceptable: ≤8th grade reading level. Higher than acceptable: ≥9th grade reading level.
Abbreviations: F–K, Flesch–Kincaid; IQR, interquartile range; SMOG, simple measure of Gobbledygook.
Figure 3.
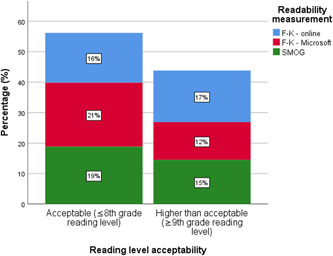
Reading level acceptability of formula feeding resources for consumers (N = 54, 108 passages)
There was a good correlation among reading grade scores across the readability measures (p < 0.001, Table 5).
Table 5.
Correlation of readability scores of formula‐feeding resources for consumers (N = 54, 108 passages)
| F–K score, online | F–K score, Microsoft | SMOG score | |
|---|---|---|---|
| F–K score, online | – | – | – |
| F–K score, Microsoft | 0.704a | – | – |
| SMOG score | 0.868a | 0.711a | – |
Abbreviations: F–K, Flesch–Kincaid; SMOG, simple measure of Gobbledygook.
Correlation is significant at the p < 0.001 level, two‐tailed.
3.7. Inter‐rater reliability
Inter‐rater reliability in evaluation of resources and readability is reported in Appendix 8.
4. DISCUSSION
This desk review identified 74 infant formula‐feeding resources available online from Australian health organisations, predominantly as web pages and handouts. It then evaluated the comprehensiveness of content and their readability. We argue that the limited scope of many of these resources and their complexity mean that parents who use infant formula may lack access to adequate material to support best‐practice formula feeding. While the resources generally provide accurate information about safe preparation, storage and administration of formula, fewer provide guidance to parents about infant feeding practices that reduce the risk of excess weight gain and later risk of overweight and obesity. Moreover, the higher than recommended reading grade of many resources makes them inaccessible to some parents, especially those with limited education and literacy or whose first language is not English.
The most commonly addressed topics focused on preparing infant formula (61 resources)—particularly preparing infant formula from powder and transporting (52), sterilising equipment (41) and using infant formula (49)—particularly appropriate bottle‐feeding practice (39 resources). Few resources focused on fluoride in infant feeding (3 resources) and cup feeding when using infant formula (5 resources).
Topics within the resources were assessed for quality in terms of their comprehensiveness against criteria extracted from the Australian Infant Feeding Guidelines (National Health and Medical Research Council, 2012) and UNICEF UK publications (National Health Service & UNICEF United Kingdom, 2015; UNICEF United Kingdom & First Steps Nutrition Trust, 2019; UNICEF United Kingdom, 2016a, 2016b) on responsive formula feeding. Overall, the comprehensiveness of formula‐feeding topics across all resources was moderate, with mean comprehensiveness of 54.36%. Certain topics were more comprehensively addressed: resources on ‘preparing infant formula’, ‘discussion of infant formula with health workers’ and ‘composition of infant formula’. Conversely, the topics ‘using infant formula’ and ‘special infant formula’ were addressed less comprehensively (37.4% and 52.4%, respectively). Further, few resources offered guidance on responsive feeding practices, a critical oversight given the complex association between responsive formula feeding and healthy infant weight gain (R. Li et al., 2008, 2012; Shloim et al., 2017). Similarly, there is limited information to help parents assess the claimed efficacy of special infant formula, which is crucial as formula marketing claims can distort parental beliefs on health benefits of breastfeeding compared to formula feeding (Parry et al., 2013; Richter et al., 2021). Consumers need accurate information on these topics, yet the available resources remain evasive and unhelpful.
This distribution of comprehensiveness scores reflects item scoring (Appendix 4): topics on preparing infant formula were frequently addressed correctly, and topics on using infant formula were often unaddressed or addressed incorrectly, again highlighting the paucity of accurate information on how parents should use bottles to feed their infants. Although evaluation criteria were modelled directly using the Infant Feeding Guidelines (National Health and Medical Research Council, 2012), any future replication of this evaluation method should move three items on formula preparation risks (on incorrect storage and incorrect preparation methods) and using infant formula up to 12 months to different topics, that is ‘preparing infant formula’ and ‘using infant formula’ to mitigate any ceiling effect.
As a national reference document, it can be expected that health organisations would first refer to the Australian guidelines when developing resources. Thirty‐nine resources addressed the topic ‘using infant formula’—of these, over half (21) were developed between 2016 and 2020, after the first UNICEF responsive feeding publication in 2015 (National Health Service & UNICEF United Kingdom, 2015). Many items in the ‘using infant formula’ topic were not addressed, particularly regarding responsive feeding; there was a positive trend between resource comprehensiveness and year of publication (Appendix 7), with a more pronounced trend for resources published since 2015.
The BFHI was expanded in 2018 to include education for safe formula‐feeding practices, responsive bottle feeding, and bottle and pacifier safety (World Health Organization, 2018). Appropriate provision of formula‐feeding information and resources in Australian maternity facilities is also required for BFHI accreditation (Baby‐Friendly Health Initiative Australia, 2020). The Australian dietary guidelines have been slated for update in 2024 (National Health and Medical Research Council, 2021); accordingly, the infant feeding guidelines should be concomitantly updated to include responsive feeding practices (UNICEF United Kingdom & First Steps Nutrition Trust, 2019). Uptake of best‐practice formula‐feeding practices into national guidelines should improve availability of responsive feeding information from Australian healthcare organisations; however, this information must be available in more Australian consumer resources earlier than 2024.
The consumer resources demonstrated varied readability. Just over half of the passages reviewed (56%) were at an acceptable reading level. This is concerning for parents with low literacy levels or whose first language is not English, who may struggle to understand the complex information in many of the resources. Yet, these groups may be more likely to formula feed their infants (Kuswara et al., 2016; Twamley et al., 2011; Wandel et al., 2016), placing them at greater disadvantage. However, this result varied depending on the measurement: despite good correlation in readability scores (Table 5), there were more acceptable scores (8th grade reading level or below) for resources assessed with the F–K, Microsoft and SMOG tools than the F–K, online tool (Figure 3). This finding contrasts with previous studies of paediatric education resources (D'Alessandro et al., 2001; Freda, 2005), which found higher readability scores using the SMOG measure. More than one readability measurement tool should be used when assessing resources; moreover, it remains concerning that nearly half of consumer resources (44%) were at a higher than acceptable recommended reading level.
Readability is only one indicator of accessibility. Availability and searchability of resources are also important for consumer access. This relies on webpages remaining current and search engines directing users to appropriate webpages. Effective search engine optimisation (SEO) (Bernhardt et al., 2011) is essential for consumers to find correct and relevant results on infant formula or bottle‐feeding resources.
Of the 74 resources downloaded in March and April 2020, seven were no longer available online 1 year later and one had been updated with newer content. This currency of resources can be significant: one resource that was removed focused on cup feeding with infant formula, a topic rarely addressed by other resources. Furthermore, SEO could be extremely limiting: resources from private hospital networks or non‐government organisations, were only located using private hospital search terms and were not linked to state and territory health services. To ensure resources developed by healthcare organisations reach consumers, resource designers should consider SEO and other dissemination technologies (Bernhardt et al., 2011).
Our search focused on resources produced by government health services, hospitals and not‐for‐profit parenting organisations. It intentionally did not include information from infant formula manufacturers. Under the WHO Code on breast milk substitutes, commercial literature can only provide scientific and factual information (World Health Organization, 1981). In Australia, this is supported by the Infant Feeding Guidelines, which stipulate all health workers should promote breastfeeding, ‘provide information about infant formula when required’, ‘support families who are using infant formula’ and ‘limit the marketing of infant formula’ (National Health and Medical Research Council, 2012); Baby‐Friendly Health Initiative Australia's accreditation guidelines for maternity centres, which comply with the WHO Code (Baby‐Friendly Health Initiative Australia, 2020); and the MAIF Agreement (Infant Nutrition Council, 1992), a voluntary code of conduct that enacts the principles of the WHO Code. Many of the resources contained text that came directly from the Australian Infant Feeding Guidelines as well as academic journal articles.
Currently, formula‐feeding resources do not adequately address the risk of excess weight gain. Babies are at risk of rapid weight gain and childhood overweight and obesity via the mechanism of bottle feeding and the composition of infant formula. If resources are unavailable from professional sources, there is evidence that the parents will rely on information from the formula packaging (Appleton et al., 2020). An Irish study found a majority of formula‐feeding mothers using non‐professional sources for information (Tarrant et al., 2013). Adherence to industry information can be important: following information on correct powder‐to‐water preparation ratios on formula tins is essential for safe formula preparation. However, adherence to formula tin guides for feeding to volume of formula per feed and number of feeds per day—instead of feeding responsively to infant hunger and satiety cues—may potentially lead to overfeeding and excess weight gain (Appleton, Laws, et al., 2018). Nurses in an Australian focus group study reported that parents' reliance on the formula tin for amount of formula to feed resulted in overfeeding (Kotowski et al., 2021). This paradox can make consumer education by healthcare workers more complex: to advise adherence to formula preparation instructions from the formula tin, while concomitantly advising deviation from formula tin suggestions for feeding volumes, to promote responsive feeding to infant appetite and cues instead.
Furthermore, the information on formula tins can be complex and in small typeface; this may impact adherence to instructions. Readability of USA formula tin instructions can range from 8th grade to college reading level (Wallace et al., 2016), undermining correct preparation by caregivers with limited health literacy. A study of modifying formula instructions to increase comprehension (Gilmore et al., 2020) found improved accuracy in formula powder dispensing and caloric density of prepared formula. Reliance on formula packaging for nutrition information can unintentionally support misleading or deceptive marketing practices: three studies found that without up‐to‐date, noncommercial information about infant formula, health professionals may believe there are significant differences between infant formula products (Berry et al., 2011); parents believed toddler formula was indistinguishable from infant formula (Berry et al., 2010); and after reviewing infant formula advertisements, parents doubted the nutritional equivalence of breast milk against infant formula (Parry et al., 2013).
This evaluation had some limitations. Importantly, it did not review resources developed for Australian Aboriginal and Torres Strait Islander groups or resources in languages other than English; this is notable, as culturally and linguistically diverse groups can have high rates of formula feeding use and would benefit from culturally appropriate and targeted resources (Cheng et al., 2020). This exclusion was based on previous research indicating written resources should supplement oral or spoken education; therefore, including these resources with minimal written information would create a floor effect for comprehensiveness scores. Further, we only investigated whether resources were accessible in terms of their readability. We did not identify or rate how readily searchable the resources were, although our complex search process suggests that some were difficult to locate. Data on web traffic to explore the uptake of the available resources, such as number of visitors to webpages, is not publicly available.
5. CONCLUSION
This study has highlighted the limitations of formal resources available online to support formula‐feeding parents in Australia. It argues that many existing resources do not provide sufficient information on practices to reduce the risk of unhealthy weight gain and that resources are often hard to understand, making them inaccessible to parents who may need them most. Accordingly, we propose the following recommendations:
-
1)
Australian infant formula resources should include best‐practice bottle feeding and responsive feeding strategies in accordance with UNICEF UK, ahead of anticipated review of the Australian infant feeding guidelines in 2024.
-
2)
Healthcare organisations should consider SEO to increase accessibility and searchability, such as using common keywords, when creating and disseminating infant formula resources.
-
3)
Infant formula resources should include topics that are infrequently addressed, such as fluoride in infant feeding and risk of unhealthy weight gain through formula use.
-
4)
Infant formula resources should be prepared at an 8th grade reading level or below, and be available in multilingual translations.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Elizabeth Denney‐Wilson devised the project and main conceptual ideas. Heilok Cheng developed the data collection instruments. Chris Rossiter and Heilok Cheng undertook the evaluation of resources. Heilok Cheng undertook statistical analysis. Donna Size provided expert clinical advice throughout. All authors wrote the manuscript, and read and approved the final manuscript.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGEMENTS
The authors would like to thank Judith Fethney, biostatistician, for SPSS support; Alison Tutt, Catherine Llewellyn and Jessica Appleton, child and family health nurses, who helped in the development of the resource evaluation criteria.
Cheng, H. , Rossiter, C. , Size, D. , & Denney‐Wilson, E. (2022). Comprehensiveness of infant formula and bottle feeding resources: A review of information from Australian healthcare organisations. Maternal & Child Nutrition, 18, e13309. 10.1111/mcn.13309
DATA AVAILABILITY STATEMENT
As this reviews publicly‐available resources, data sharing is not applicable to this article.
REFERENCES
- Appleton, J. , Fowler, C. , Laws, R. , Russell, C. G. , Campbell, K. J. , & Denney‐Wilson, E. (2020). Professional and non‐professional sources of formula feeding advice for parents in the first six months. Maternal & Child Nutrition, 16, e12942. 10.1111/mcn.12942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton, J. , Laws, R. , Russell, C. G. , Fowler, C. , Campbell, K. J. , & Denney‐Wilson, E. (2018). Infant formula feeding practices and the role of advice and support: An exploratory qualitative study. BMC Pediatrics, 18, 12. 10.1186/s12887-017-0977-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton, J. , Russell, C. G. , Laws, R. , Fowler, C. , Campbell, K. , & Denney‐Wilson, E. (2018). Infant formula feeding practices associated with rapid weight gain: A systematic review. Maternal & Child Nutrition, 14, e12602. 10.1111/mcn.12602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold, C. L. , Davis, T. C. , Frempong, J. O. , Humiston, S. G. , Bocchini, A. , Kennen, E. M. , et al. (2006). Assessment of newborn screening parent education materials. Pediatrics, 117, S320–S325. 10.1542/peds.2005-2633L [DOI] [PubMed] [Google Scholar]
- Australian Commission on Safety and Quality in Health Care . (2020). Nationwide stocktake of Aboriginal and Torres Strait Islander health resources. https://www.safetyandquality.gov.au/sites/default/files/2020-03/acsqhc_and_circa_-_nationwide_stocktake_of_aboriginal_torres_strait_islander_health_resources_-_report_-_march_2020.pdf
- Australian Department of Health . (2021). Marketing in Australia of infant formulas: Manufacturers and importers agreement. https://www1.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-foodpolicy-apmaif.htm
- Australian Government . (2020). Literacy and access. Style manual. https://www.stylemanual.gov.au/user-needs/understanding-needs/literacy-and-access
- Australian Institute of Health and Welfare . (2011). 2010 Australian National Infant Feeding Survey: Indicator results. https://www.aihw.gov.au/getmedia/af2fe025-637e-4c09-ba03-33e69f49aba7/13632.pdf.aspx?inline=true
- Baby‐Friendly Health Initiative Australia . (2020). BFHI Australia: Maternity facility handbook. https://bfhi.org.au/wp-content/uploads/2020/03/BFHI-Handbook-Maternity-Facilities-2020.pdf
- Battersby, S. (2010). An evaluation of midwives' knowledge of formula feeding and their role in supporting mothers who formula feed their infants. Journal of Family Health Care, 20, 192–197. [PubMed] [Google Scholar]
- Bernhardt, J. M. , Mays, D. , & Kreuter, M. W. (2011). Dissemination 2.0: Closing the gap between knowledge and practice with new media and marketing. Journal of Health Communication, 16, 32–44. 10.1080/10810730.2011.593608 [DOI] [PubMed] [Google Scholar]
- Berry, N. J. , Jones, S. , & Iverson, D. (2010). It's all formula to me: Women's understandings of toddler milk ads. Breastfeeding Review, 18, 21–30. [PubMed] [Google Scholar]
- Berry, N. J. , Jones, S. C. , & Iverson, D. (2011). Relax, you're soaking in it: Sources of information about infant formula. Breastfeeding Review, 19, 9–18. [PubMed] [Google Scholar]
- Brands, B. , Demmelmair, H. , & Koletzko, B. (2014). How growth due to infant nutrition influences obesity and later disease risk. Acta Paediatrica, 103, 578–585. 10.1111/apa.12593 [DOI] [PubMed] [Google Scholar]
- Brown, A. , Raynor, P. , & Lee, M. (2011). Healthcare professionals' and mothers' perceptions of factors that influence decisions to breastfeed or formula feed infants: A comparative study. Journal of Advanced Nursing, 67, 1993–2003. 10.1111/j.1365-2648.2011.05647.x [DOI] [PubMed] [Google Scholar]
- Cairney, P. A. , Alder, E. M. , & Barbour, R. S. (2006). Support for infant feeding: Mothers' perceptions. British Journal of Midwifery, 14(694), 696–700. 10.12968/bjom.2006.14.12.22505 [DOI] [Google Scholar]
- Calamusa, G. , Valenti, R. M. , Guida, I. , & Mammina, C. (2009). A survey on knowledge and self‐reported formula handling practices of parents and child care workers in Palermo, Italy. BMC Pediatrics, 9, 9. 10.1186/1471-2431-9-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles, J. (2016). An evaluation and comprehensive guide to successful Aboriginal health promotion. Australian Indigenous Health Bulletin, 16, 1–8. http://healthbulletin.org.au/articles/an-evaluation-and-comprehensive-guide-to-successful-aboriginal-health-promotion/ [Google Scholar]
- Cheng, C. , & Dunn, M. (2015). Health literacy and the Internet: A study on the readability of Australian online health information. Australian and New Zealand Journal of Public Health, 39, 309–314. 10.1111/1753-6405.12341 [DOI] [PubMed] [Google Scholar]
- Cheng, H. , Eames‐Brown, R. , Tutt, A. , Laws, R. , Blight, V. , McKenzie, A. , Rossiter, C. , Campbell, K. , Sim, K. , Fowler, C. , Seabury, R. , & Denney‐Wilson, E. (2020). Promoting healthy weight for all young children: A mixed methods study of child and family health nurses' perceptions of barriers and how to overcome them. BMC Nursing, 19, 84. 10.1186/s12912-020-00477-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhry, K. , & Wallace, L. M. (2012). ‘Breast is not always best’: South Asian women's experiences of infant feeding in the UK within an acculturation framework. Maternal & Child Nutrition, 8, 72–87. 10.1111/j.1740-8709.2010.00253.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- COAG Health Council . (2019). Australian National Breastfeeding Strategy: 2019 and beyond. https://www.coaghealthcouncil.gov.au/Portals/0/Australian%20National%20Breastfeeding%20Strategy%20-%20Final.pdf
- D'Alessandro, D. M. , Kingsley, P. , & Johnson‐West, J. (2001). The readability of pediatric patient education materials on the world wide web. Archives of Pediatrics & Adolescent Medicine, 155, 807–812. 10.1001/archpedi.155.7.807 [DOI] [PubMed] [Google Scholar]
- Davies, J. , Bukulatjpi, S. , Sharma, S. , Davis, J. , & Johnston, V. (2014). “Only your blood can tell the story”—A qualitative research study using semi‐structured interviews to explore the hepatitis B related knowledge, perceptions and experiences of remote dwelling Indigenous Australians and their health care providers in northern Australia. BMC Public Health, 14, 1233. 10.1186/1471-2458-14-1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freda, M. C. (2005). The readability of American Academy of Pediatrics patient education brochures. Journal of Pediatric Health Care, 19, 151–156. 10.1016/j.pedhc.2005.01.013 [DOI] [PubMed] [Google Scholar]
- Gilmore, L. A. , Altazan, A. D. , Flanagan, E. W. , Beyer, A. G. , Olson, K. N. , O'Connell, A. A. , Nguyen, T. H. , Beyl, R. A. , & Redman, L. M. (2020). Modifications to infant formula instructions improve the accuracy of formula dispensing. Nutrients, 12, 1150. 10.3390/nu12041150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley, N. L. , Rosen, R. K. , Strait, E. A. , Raffucci, G. , Holmdahl, I. , Freeman, J. R. , et al. (2015). Mothers' attitudes and beliefs about infant feeding highlight barriers to exclusive breastfeeding in American Samoa. Women and Birth, 28, e80–e86. 10.1016/j.wombi.2015.04.002 [DOI] [PubMed] [Google Scholar]
- Hegedus, J. , & Mullan, J. (2015). Are we adequately providing support services for optimal infant nutrition in Australia? A study in regional NSW. Australian Journal of Primary Health, 21, 293–298. 10.1071/PY14044 [DOI] [PubMed] [Google Scholar]
- Hendrickson, R. L. , Huebner, C. E. , & Riedy, C. A. (2006). Readability of pediatric health materials for preventive dental care. BMC Oral Health, 6, 14. 10.1186/1472-6831-6-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández‐Cordero, S. , Lozada‐Tequeanes, A. L. , Shamah‐Levy, T. , Lutter, C. , González de Cosío, T. , Saturno‐Hernández, P. , et al. (2019). Violations of the international code of marketing of breast‐milk substitutes in Mexico. Maternal & Child Nutrition, 15, e12682. 10.1111/mcn.12682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidayana, I. , Februhartanty, J. , & Parady, V. A. (2017). Violations of the international code of marketing of breast‐milk substitutes: Indonesia context. Public Health Nutrition, 20, 165–173. 10.1017/S1368980016001567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter‐Adams, J. , Myer, L. , & Rother, H.‐A. (2016). Perceptions related to breastfeeding and the early introduction of complementary foods amongst migrants in Cape Town, South Africa. International Breastfeeding Journal, 11, 29. 10.1186/s13006-016-0088-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infant Nutrition Council . (1992). Marketing in Australia of Infant Formulas (MAIF) agreement. https://www.infantnutritioncouncil.com/wp-content/uploads/2016/10/MAIF-Agreement-2015.pdf
- Kincaid, P. J. , Fishbourne, R. P. J. , Rogers, R. L. , & Chissom, B. S. (1975). Derivation of new readability formulas (automated readability index, fog count and flesch reading ease formula) for navy enlisted personnel. https://stars.library.ucf.edu/cgi/viewcontent.cgi?article=1055%26context=istlibrary
- Koletzko, B. , von Kries, R. , Closa, R. , Escribano, J. , Scaglioni, S. , Giovannini, M. , et al. (2009). Lower protein in infant formula is associated with lower weight up to age 2 y: A randomized clinical trial. The American Journal of Clinical Nutrition, 89, 1836–1845. 10.3945/ajcn.2008.27091 [DOI] [PubMed] [Google Scholar]
- Kotowski, J. , Fowler, C. , Hourigan, C. , & Orr, F. (2020). Bottle‐feeding an infant feeding modality: An integrative literature review. Maternal & Child Nutrition, 16, e12939. 10.1111/mcn.12939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotowski, J. , Fowler, C. , & Orr, F. (2021). Bottle‐feeding, a neglected area of learning and support for nurses working in child health: An exploratory qualitative study. Journal of Child Health Care, 136749352110073. 10.1177/13674935211007321 [DOI] [PubMed] [Google Scholar]
- Kuswara, K. , Laws, R. , Kremer, P. , Hesketh, K. D. , & Campbell, K. J. (2016). The infant feeding practices of Chinese immigrant mothers in Australia: A qualitative exploration. Appetite, 105, 375–384. 10.1016/j.appet.2016.06.008 [DOI] [PubMed] [Google Scholar]
- Labiner‐Wolfe, J. , Fein, S. B. , & Shealy, K. R. (2008). Infant formula‐handling education and safety. Pediatrics, 122, S85–S90. 10.1542/peds.2008-1315k [DOI] [PubMed] [Google Scholar]
- Li, R. , Fein, S. B. , & Grummer‐Strawn, L. M. (2008). Association of breastfeeding intensity and bottle‐emptying behaviors at early infancy with infants' risk for excess weight at late infancy. Pediatrics, 122, S77–S84. 10.1542/peds.2008-1315j [DOI] [PubMed] [Google Scholar]
- Li, R. , Magadia, J. , Fein, S. B. , & Grummer‐Strawn, L. M. (2012). Risk of bottle‐feeding for rapid weight gain during the first year of life. Archives of Pediatrics & Adolescent Medicine, 166, 431–436. 10.1001/archpediatrics.2011.1665 [DOI] [PubMed] [Google Scholar]
- Liu, A. , Dai, Y. , Xie, X. , & Chen, L. (2014). Implementation of international code of marketing breast‐milk substitutes in China. Breastfeeding Medicine, 9, 467–472. 10.1089/bfm.2014.0053 [DOI] [PubMed] [Google Scholar]
- Mannan, H. (2018). Early infant feeding of formula or solid foods and risk of childhood overweight or obesity in a socioeconomically disadvantaged region of australia: A longitudinal cohort analysis. International Journal of Environmental Research and Public Health, 15, 15. 10.3390/ijerph15081685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney, C. M. , Glass, R. P. , Coffey, P. , Rue, T. , Vaughn, M. G. , & Cunningham, M. (2016). Feeding neonates by cup: A systematic review of the literature. Maternal and Child Health Journal, 20, 1620–1633. 10.1007/s10995-016-1961-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin, H. G. (1969). SMOG grading—A new readability formula. Journal of Reading, 12, 639–646. https://ogg.osu.edu/media/documents/health_lit/WRRSMOG_Readability_Formula_G._Harry_McLaughlin__1969_.pdf [Google Scholar]
- Microsoft Word Help Center . (2019). Test your document's readability. https://support.office.com/en-us/article/test-your-document-s-readability-85b4969e-e80a-4777-8dd3-f7fc3c8b3fd2
- National Health and Medical Research Council . (2012). Infant Feeding Guidelines: Information for health workers. (N56). National Health and Medical Research Council. https://www.nhmrc.gov.au/about-us/publications/infant-feeding-guidelines-information-health-workers [DOI] [PubMed] [Google Scholar]
- National Health and Medical Research Council . (2021). Review of the 2013 Australian Dietary Guidelines. https://www.nhmrc.gov.au/health-advice/nutrition/australian-dietary-guidelines-review
- National Health Service, & UNICEF United Kingdom . (2015). Guide to bottle feeding: how to prepare infant formula and sterilise feeding equipment to minimise the risks to your baby. https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2008/02/start4life_guide_to_bottle_-feeding.pdf
- Oermann, M. H. , Gerich, J. , Ostosh, L. , & Zaleski, S. (2003). Evaluation of asthma websites for patient and parent education. Journal of Pediatric Nursing, 18, 389–396. 10.1016/S0882-5963(03)00161-1 [DOI] [PubMed] [Google Scholar]
- Osman, N. A. , & el‐Sabban, F. F. (1999). Infant‐feeding practices in Al‐Ain, United Arab Emirates. Eastern Mediterranean Health Journal, 5, 103–110. [PubMed] [Google Scholar]
- Parry, K. , Taylor, E. , Hall‐Dardess, P. , Walker, M. , & Labbok, M. (2013). Understanding women's interpretations of infant formula advertising. Birth: Issues in Perinatal Care, 40, 115–124. 10.1111/birt.12044 [DOI] [PubMed] [Google Scholar]
- Peake, R. M. , Jackson, D. , Lea, J. , & Usher, K. (2019). Investigating the processes used to develop and evaluate the effectiveness of health education resources for adult Indigenous people: A literature review. Contemporary Nurse, 55, 421–449. 10.1080/10376178.2019.1633939 [DOI] [PubMed] [Google Scholar]
- Richter, A. P. C. , Duffy, E. W. , Smith Taillie, L. , Harris, J. L. , Pomeranz, J. L. , & Hall, M. G. (2021). The impact of toddler milk claims on beliefs and misperceptions: A randomized experiment with parents of young children. Journal of the Academy of Nutrition and Dietetics, 83, 1067. 10.1016/j.jand.2021.08.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ReadabilityFormulas.com. (undated). Automatic readability checker. http://www.readabilityformulas.com/contactus.php
- Rothrock, S. G. , Rothrock, A. N. , Swetland, S. B. , Pagane, M. , Isaak, S. A. , Romney, J. , et al. (2019). Quality, trustworthiness, readability, and accuracy of medical information regarding common pediatric emergency medicine‐related complaints on the web. The Journal of Emergency Medicine, 57, 469–477. 10.1016/j.jemermed.2019.06.043 [DOI] [PubMed] [Google Scholar]
- Schoen, D. , Balchin, D. , & Thompson, S. (2010). Health promotion resources for Aboriginal people: Lessons learned from consultation and evaluation of diabetes foot care resources. Health Promotion Journal of Australia, 21, 64–69. 10.1071/HE10064 [DOI] [PubMed] [Google Scholar]
- Shloim, N. , Vereijken, C. M. J. L. , Blundell, P. , & Hetherington, M. M. (2017). Looking for cues—infant communication of hunger and satiation during milk feeding. Appetite, 108, 74–82. 10.1016/j.appet.2016.09.020 [DOI] [PubMed] [Google Scholar]
- Tarrant, R. , Sheridan‐Pereira, M. , McCarthy, R. , Younger, R. , & Kearney, J. (2013). Mothers who formula feed: Their practices, support needs and factors influencing their infant feeding decision. Child Care in Practice, 19, 78–94. 10.1080/13575279.2012.737764 [DOI] [Google Scholar]
- Twamley, K. , Puthussery, S. , Harding, S. , Baron, M. , & Macfarlane, A. (2011). UK‐born ethnic minority women and their experiences of feeding their newborn infant. Midwifery, 27, 595–602. 10.1016/j.midw.2010.06.016 [DOI] [PubMed] [Google Scholar]
- UNICEF United Kingdom . (2016a). A guide to infant formula for parents who are bottle feeding. https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2016/12/Parents-guide-to-infant-formula.pdf
- UNICEF United Kingdom . (2016b). A guide to infant formula for parents who are bottle feeding: The health professionals' guide. https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2016/12/Health-professionals-guide-to-infant-formula.pdf
- UNICEF United Kingdom . (2019). Working Within the International Code of Marketing of Breastmilk Substitutes: A guide for health workers. https://www.unicef.org.uk/babyfriendly/baby-friendly-resources/international-code-marketing-breastmilk-substitutes-resources/guide-to-working-within-the-code/
- UNICEF United Kingdom, & First Steps Nutrition Trust . (2019). Responsive bottle feeding. https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2019/04/Infant-formula-and-responsive-bottle-feeding.pdf
- Vass, A. , Mitchell, A. , & Dhurrkay, Y. (2011). Health literacy and Australian Indigenous peoples: An analysis of the role of language and worldview. Health Promotion Journal of Australia, 22, 33–37. 10.1071/he11033 [DOI] [PubMed] [Google Scholar]
- Victora, C. G. P. , Bahl, R. M. D. , Barros, A. J. D. P. , França, G. V. A. P. , Horton, S. P. , Krasevec, J. M. , et al. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387, 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Wallace, L. S. , Rosenstein, P. F. , & Gal, N. (2016). Readability and content characteristics of powdered infant formula instructions in the United States. Maternal & Child Health Journal, 20, 889–894. 10.1007/s10995-015-1877-9 [DOI] [PubMed] [Google Scholar]
- Wandel, M. , Terragni, L. , Nguyen, C. , Lyngstad, J. , Amundsen, M. , & de Paoli, M. (2016). Breastfeeding among Somali mothers living in Norway: Attitudes, practices and challenges. Women and Birth, 29, 487–493. 10.1016/j.wombi.2016.04.006 [DOI] [PubMed] [Google Scholar]
- Weber, M. , Grote, V. , Closa‐Monasterolo, R. , Escribano, J. , Langhendries, J. ‐P. , Dain, E. , et al. (2014). Lower protein content in infant formula reduces BMI and obesity risk at school age: Follow‐up of a randomized trial. The American Journal of Clinical Nutrition, 99, 1041–1051. 10.3945/ajcn.113.064071 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (1981). International code of marketing of breast‐milk substitutes. https://www.who.int/nutrition/publications/code_english.pdf
- World Health Organization . (2018). Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services—The revised Baby‐friendly Hospital Initiative. https://www.who.int/nutrition/publications/infantfeeding/bfhi-implementation-2018.pdf [PubMed]
- World Health Organization . (2019). Global breastfeeding scorecard, 2019: increasing commitment to breastfeeding through funding and improved policies and programmes. https://apps.who.int/iris/bitstream/handle/10665/326049/WHO-NMH-NHD-19.22-eng.pdf?sequence=1%26isAllowed=y
- Yeoh, B. H. , Eastwood, J. , Phung, H. , & Woolfenden, S. (2007). Factors influencing breastfeeding rates in south‐western Sydney. Journal of Paediatrics and Child Health, 43, 249–255. 10.1111/j.1440-1754.2007.01055.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
As this reviews publicly‐available resources, data sharing is not applicable to this article.


