Abstract
The Covid‐19 pandemic has led to a substantial increase in remotely provided maternity care services, including breastfeeding support. It is, therefore, important to understand whether breastfeeding support provided remotely is an effective method of support. To determine if breastfeeding support provided remotely is an effective method of support. A systematic review and meta‐analysis were conducted. Twenty‐nine studies were included in the review and 26 contributed data to the meta‐analysis. Remotely provided breastfeeding support significantly reduced the risk of women stopping exclusive breastfeeding at 3 months by 25% (risk ratio [RR]: 0.75, 95% confidence interval [CI]: 0.63, 0.90). There was no significant difference in the number of women stopping any breastfeeding at 4–8 weeks (RR: 1.10, 95% CI: 0.74, 1.64), 3 months (RR: 0.89, 95% CI: 0.71, 1.11), or 6 months (RR: 0.91, 95% CI: 0.81, 1.03) or the number of women stopping exclusive breastfeeding at 4–8 weeks (RR: 0.86, 95% CI: 0.70, 1.07) or 6 months (RR: 0.93, 95% CI: 0.85, 1.0). There was substantial heterogeneity of interventions in terms of mode of delivery, intensity, and providers. This demonstrates that remote interventions can be effective for improving exclusive breastfeeding at 3 months but the certainty of the evidence is low. Improvements in exclusive breastfeeding at 4–8 weeks and 6 months were only found when studies at high risk of bias were excluded. They are also less likely to be effective for improving any breastfeeding. Remote provision of breastfeeding support and education could be provided when it is not possible to provide face‐to‐face care.
Keywords: breast feeding, counselling, lactation, meta‐analysis, online social support, systematic review, telemedicine
Key messages
-
•
This systematic review investigated the effectiveness of breastfeeding support interventions provided remotely.
-
•
There was significant heterogeneity in how support interventions and standard care were provided.
-
•
There is low‐quality evidence that remotely provided breastfeeding support significantly reduced the risk of women stopping exclusive breastfeeding at 3 months but not at 4‐8 weeks or 6 months. There was no significant difference in the number of women stopping any breastfeeding.
-
•
Interventions tended to demonstrate more positive effects when standard care was limited suggesting remote support is preferable to no support.
-
•
There was a lack of evidence exploring women's satisfaction and the impact on maternal mental health. More research is needed to explore this.
This systematic review and meta‐analysis aimed to identify if breastfeeding support provided remotely was effective in improving breastfeeding outcomes. Twenty‐six studies contributed data to the meta‐analysis. Remotely provided breastfeeding support significantly reduced the risk of women stopping exclusive breastfeeding at 3 months by 25%, however, there were no significant differences at any other time points or for any breastfeeding.
1. INTRODUCTION
Breastfeeding is a critical public health measure with fundamental impacts on short‐, medium‐ and long‐term health outcomes for women (Chowdhury et al., 2015; Victora et al., 2016), and health and developmental outcomes for infants (Bowatte et al., 2015; Horta & Victora, 2013; Horta et al., 2015a, 2015b; Peres et al., 2015; Sankar et al., 2015; Tham et al., 2015) and brings societal and economic benefits (Davanzo et al., 2015; Rollins et al., 2016).
Systematic review evidence shows that support interventions are effective in improving breastfeeding rates (Kim et al., 2018; McFadden et al., 2017, 2019; Sinha et al., 2015). However, support tends to have a greater effect in low and middle countries compared to high income countries (Haroon et al., 2013; Jolly et al., 2012). One explanation for this is that within high income countries some form of breastfeeding support is part of routine care and additional support will not confer additional benefits (Jolly et al., 2012).
Despite the evidence of effectiveness for breastfeeding support, response to the COVID‐19 pandemic disrupted daily life for pregnant women, new parents, infants and their families, as well as maternity services and staff. During lockdowns, women and infants are socially isolated, deprived of direct face‐to‐face contact with their social support networks. At the same time, there has been a rapid transition to providing maternity care remotely to comply with social distancing recommendations and minimise the spread of the virus. In the UK, the Royal College of Obstetricians and Gynaecologists (RCOG) and the Royal College of Midwives (RCM) recommend that maternity services should maximise the use of remote consultations (RCM & RCOG, 2020). These social and health system transformations have significant implications for supporting women to breastfeed.
Moreover, breastfeeding during the pandemic is even more important (Renfrew et al., 2020). The World Health Organization (WHO) promotes close contact and breastfeeding for mothers and infants affected by COVID‐19 as long as mothers practice respiratory hygiene (WHO, 2020). To date, there is no evidence that COVID‐19 is transmitted in breastmilk and the public health gains of breastfeeding outweigh any risks, especially for vulnerable infants (Davanzo et al., 2020; Lackey et al., 2020; WHO, 2020). Therefore, safe effective support that enables women to initiate and continue breastfeeding and protects healthcare practitioners and lay breastfeeding supporters is imperative.
In the context of COVID‐19, remote healthcare provision is essential for service users and staff who are shielding because healthcare settings are perceived as high‐risk sources of infection (Greenhalgh et al., 2020). Remote healthcare provision has the added advantage that healthcare staff who are self‐isolating but well, can contribute to service provision without putting themselves or their patients at risk (Greenhalgh et al., 2020). Variously termed telehealth, e‐health and mhealth, remote healthcare provision, including telephone and video consultations, is not new; however, the speed of change during the pandemic is unprecedented (Webster, 2020). While evidence of clinical effectiveness is equivocal, remote healthcare provision does appear to be acceptable to service users (Ignatowicz et al., 2019; Seuren et al., 2020). A Cochrane review of health workers experiences of mobile health technologies in primary healthcare reported that staff views were mixed depending on the efficiency of the technologies used and the health workers confidence (Odendaal et al., 2020). Greenhalgh et al. (2020) suggest that there is considerably more evidence and guidance for telephone consultations.
However, as the aforementioned systematic reviews considered breastfeeding support generally (i.e., peer and professional, face‐to‐face and remote), there is a need to synthesise evidence via systematic review to understand the effectiveness of interventions provided remotely. In addition to examining how remote support impacts breastfeeding rates it is also important to understand how mothers perceive remote support and if it is associated with changes in perinatal mental health indicators. More specifically, we will include maternal satisfaction with breastfeeding which has been defined as the fulfilment of maternal wishes, expectations or needs in providing breastfeeding for her infant and the pleasure derived from this and may hold more importance for women than duration and exclusivity (Edwards, 2018). Maternal self‐efficacy is also positively associated with breastfeeding duration and exclusivity (Meedya et al., 2010), and can be targeted by support interventions. Ensuring these key components are assessed when using remote support strategies serve as a proxy for continued breastfeeding and are important to measure. Perinatal mental health indicators encompass the spectrum of mental health indicators (including and not limited to adjustment disorders and distress, PTSD, mild to moderate depressive illness, severe depressive illness, chronic severe mental illness and postpartum psychosis). Such conditions are associated with adverse breastfeeding outcomes and women could benefit from targeted anticipatory guidance and additional support (Dagla et al., 2021). In addition as evidence demonstrates the benefits of breastfeeding with reduction in hospitalisations and mortality both in the UK and worldwide, it is important to understand if remote support has any impact on these (Payne & Quigley, 2017; Sankar et al., 2015). Finally, we need to understand to what extent remote support can potentially replace face‐to‐face consultations.
The transition to remote breastfeeding support provision is unlikely to be limited to the context of the COVID‐19 pandemic. In the UK, anecdotal evidence before the pandemic, suggested that face‐to‐face breastfeeding support services were being reduced to save money (Better Breastfeeding, 2018). Support provided remotely may be more cost‐effective than face‐to‐face support although there is currently a lack of evidence to support this within healthcare generally (Gonçalves‐Bradley et al., 2020). However, there may be some advantages to remote breastfeeding support such as improved accessibility for those living in remote and rural areas (Kapinos et al., 2019), and improved continuity of care (Friesen et al., 2015). It is therefore important to understand whether breastfeeding support provided remotely is effective.
To inform care during and beyond the COVID‐19 pandemic, we conducted a systematic review and meta‐analysis to determine the most effective methods of providing breastfeeding support and education remotely to pregnant and breastfeeding women. The objectives of the review were to determine the effectiveness of different modes of remote provision of breastfeeding support and education; different providers of remote breastfeeding support and education; and different timings and frequencies of remote breastfeeding support and education on breastfeeding rates and also on the following secondary outcomes: maternal satisfaction; perinatal mental health indicators; maternal self‐efficacy; infant and child morbidity and mortality and number of women requiring additional face‐to‐face support.
2. METHODS
The protocol for this systematic review is registered on PROSPERO (CRD42020176130).
2.1. Search strategy
We searched five electronic databases: MEDLINE, CINAHL, MIDIRS, CENTRAL and EMBASE. Searches were conducted in March 2020 using a combination of index and free‐text terms related to ‘breastfeeding’ AND ‘remote care’ AND trials (for full search strategy see Supporting Information File S1). No language limit was placed on the search, however, only studies reported in English were included. Studies published before 2010 were excluded to ensure the included interventions reflected the most up‐to‐date technologies. We also scanned the reference lists of all included studies and relevant systematic reviews.
2.2. Eligibility criteria
2.2.1. Inclusion criteria
Studies were included if they were individual or cluster‐randomised trials. Studies were eligible for inclusion if they contained the following groups of women: pregnant women intending to breastfeed; mothers who may initiate breastfeeding; mothers who are breastfeeding; mothers who ceased breastfeeding who wished to re‐start. This included women who have specific health problems and mothers of preterm infants or infants requiring additional medical care. Women who gave birth via Caesarean Section or vaginal birth were included. Studies were included if the intervention was also aimed at fathers and/or other caregivers as well as mothers.
Interventions were eligible for inclusion if they involved the provision of breastfeeding support or education provided remotely, defined as where service users and service‐providers are separated by distance, for example, telephone, text messaging, social media, video call and e‐mail (WHO, 2016). Studies were included if the intervention occurred in the antenatal or postnatal periods alone or in both the antenatal and postnatal periods. Interventions that also contained a face‐to‐face element were only included if this was delivered post‐partum and before discharge home and was part of usual care and thus also received by the control group.
Interventions could be offered by health professionals or lay people or both, trained or untrained. It could be offered to groups of women or one‐to‐one and it could be offered proactively by contacting women directly, or reactively, by waiting for women to get in touch.
‘Support’ interventions eligible for this review could include elements such as reassurance, praise, information, and the opportunity to discuss and to respond to the mother's questions. Interventions had to be two‐way interactions between the supporter and participant. It could include discussing the practical management of breastfeeding (e.g., attachment of the infant, identifying an infant's feeding cues). Education interventions eligible for this review had to be provided to the mother and may or may not also have included the father or other caregivers.
The comparator was either standard care, no breastfeeding support, or education or breastfeeding support provided face‐to‐face.
To be included studies had to report one of the following primary outcomes:
-
1.
Number of women who stop exclusive breastfeeding at 4–8 weeks.
-
2.
Number of women who stop any breastfeeding at 4–8 weeks.
-
3.
Number of women who stop exclusive breastfeeding at 3 months.
-
4.
Number of women who stop any breastfeeding at 3 months.
-
5.
Number of women who stop exclusive breastfeeding at 6 months.
-
6.
Number of women who stop any breastfeeding at 6 months.
The outcomes focused on the number of women who stopped breastfeeding to allow for easier comparison with the Cochrane review on Breastfeeding Support (McFadden et al., 2017).
The following secondary outcomes were also included:
-
1.
Maternal satisfaction.
-
2.
Perinatal mental health indicators.
-
3.
Maternal self‐efficacy.
-
4.
Infant and child morbidity and mortality.
-
5.
Number of women requiring additional face‐to‐face support.
2.2.2. Exclusion criteria
Studies were excluded if the intervention was targeted at individuals or organisations providing breastfeeding support or education and did not collect data on maternal or infant outcomes.
Studies that have a face‐to‐face element beyond providing support or education before discharge after birth were excluded. Interventions that provided only one‐way information from a care provider were excluded (e.g., text message reminders).
2.3. Study selection
Titles, abstracts and potentially relevant full texts were screened independently by two authors against the eligibility criteria. Any disagreement was resolved through discussion and consultation with a third author.
2.4. Data extraction, risk of bias and strength of the evidence assessment
Two authors independently extracted information on participants, intervention, context and outcomes using a specifically designed data extraction form. Any discrepancies were resolved through discussion. When information regarding study methods and results was unclear, we attempted to contact authors to provide further details. Two authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for systematic reviews of Interventions (Higgins et al., 2011). We assessed the quality of the evidence using the GRADE approach (Schünemann et al., 2013), with the GRADEpro online programme (https://gradepro.org/).
2.5. Data analysis and synthesis
Given the pressing need to complete this study in a rapid timeframe to inform how breastfeeding support can be provided in the Covid‐19 situation, primary outcomes were prioritised. Meta‐analysis of the primary outcomes was performed using Review Manager 5 software. The primary outcomes are presented as summary risk ratios with 95% confidence intervals. We anticipated heterogeneity between studies in terms of the interventions and populations, so a random‐effects meta‐analysis was used (Deeks et al., 2011).
Where possible we aimed to include all available data for all randomised patients, in the group to which they were randomised. We contacted authors regarding any missing data. Where data were missing, we assumed that the woman had ceased breastfeeding. Thus the denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
The sample sizes of cluster randomised trials were adjusted using the intracluster correlation coefficient when possible. If these were not presented, we contacted authors for this information. Heterogeneity was quantified using the I 2 statistic.
Secondary outcomes are described narratively and used to aid understanding of the impact of the intervention on primary outcomes.
2.5.1. Cluster randomized trials
Cluster randomized trials were adjusted for clustering using the formula detailed in the Cochrane Handbook (Higgins et al., 2019). First the design effect was calculated using the following formula: 1 + (average cluster size – 1) × intracluster correlation coefficient (ICC). The effective sample size for the intervention and control group was then calculated by dividing the number of participants in each group by the design effect. All studies reported the ICC.
2.5.2. Sensitivity analysis
We carried out sensitivity analyses on missing data and trial quality. For missing data, we excluded studies with high (>20% attrition) or unclear risk of attrition bias. For quality, we excluded all studies with high or unclear risk of bias in the allocation concealment domain of the Cochrane Risk of Bias tool.
2.5.3. Publication bias
We assessed the risk of publication bias through a visual inspection of Funnel Plots for each analysis. To assess whether any asymmetry was a result of publication bias, the effect estimates from the random‐effects model was compared with a fixed‐effects model. If the random effects model was found to increase the effect estimate, one explanation could be the presence of publication bias (Page et al., 2020; Sterne et al., 2011).
3. RESULTS
3.1. Identification of studies
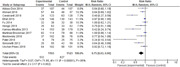
The search identified 3188 original records. One further paper was identified by searching reference lists of included papers and one further paper was published after the search and identified by searching for papers related to relevant protocols. On titles and abstracts screening, 3080 papers were excluded. Following review of 110 full texts articles, 61 were excluded. This left 49 papers reporting 29 studies included in this review (see Figure 1). To facilitate ease of reading we have included only the primary reference from each study within the manuscript text. The additional references are detailed in Table S1. Three studies did not report relevant outcomes or did not present data usable in the meta‐analysis (Demirci et al., 2019; Niela‐Vilen et al., 2016; Reeder et al., 2014) and were therefore not included in the analysis; 26 studies contributed data to the meta‐analysis.
Figure 1.
Preferred reporting items for systematic reviews and meta‐analysis flow diagram detailing study selection
The 29 studies included one cluster randomised trial (Fu et al., 2014), and 28 individually randomised trials. Twenty‐five were 2 arm trials with 4 having 3 arms (Fu et al., 2014; Kamau‐Mbuthia et al., 2013; Reeder et al., 2014; Unger et al., 2018). In 3 of these studies only one intervention arm was relevant and included in this review (Fu et al., 2014; Kamau‐Mbuthia et al., 2013; Unger et al., 2018). In Reeder et al. both intervention arms were relevant, but data were not presented in a form that could be included in a meta‐analysis. Specifically, Fu et al. had one intervention arm with an educational intervention delivered solely in hospital before discharge (excluded) and another with support and education provided by telephone (included); Kamau‐Mbuthia et al. had one arm delivered face‐to‐face peer groups (excluded) and one telephone support (included); and Unger et al. had one intervention weekly one way texts and another weekly two way text messaging (two way only included).
3.2. Description of included studies
Full detail of included studies and description of interventions and comparisons is provided in Table 1.
Table 1.
Characteristics of included studies and description of intervention and comparison
| First author, year published, country | Study design year of study | Participants number randomised intervention/control | Mode, frequency and who provided the intervention | Description of intervention | Description of comparison |
|---|---|---|---|---|---|
|
Abbass‐Dick and Dennis, 2018, Canada |
Parallel RCT 2 arms March–July 2012 |
107/107 | PN in hospital discussion, followed by supportive telephone call at 2 weeks and emails at Week 1 and 3 by lactation specialist | Co‐parenting intervention. Couples provided with BF information via in hospital discussion, booklet, workbook, website and DVD. Couples received a hospital visit; phone call at 2 weeks and emails at 1 and 3 weeks | Standard in‐hospital BF support and any BF assistance that was proactively sought in the community. |
|
Ahmed, 2016, USA |
Parallel RCT 2 arms | 49/57 | PN interactive online web‐based BF monitoring with tailored education on BF outcomes provided by Lactation specialist and research scientists. | Mothers given access to computer application with interactive BF monitoring system before hospital discharge and explained how to use. Mothers asked to enter their BF data, infant's wet and dirty diapers, and any problems for at least 30 days. The system alerted the research team about mothers' problems. | Usual care—BF support and education before discharge, one phone call within the first week after hospital discharge, and a list of community BF resources also encouraged to contact the lactation specialist with any BF problems. |
|
Carlsen, 2013, Denmark |
Parallel RCT 2 arms |
Obese women BMI > 30 108/118 |
PN one‐to‐one, minimum of 9 consultations during the first 6 months (3 in the first month and then every second week until 8 weeks postpartum, monthly thereafter with additional contacts if needed) provided by IBCLCs | Telephone advisory services following a structured design for asking questions about physical and psychological aspects regarding BF and well‐being of mother and child | Standard BF support provided, to women in the control group, by the hospital. All participants had contact with a healthcare visitor or a midwife within the first week postpartum |
|
Cavalcanti, 2018, Brazil |
Parallel RCT 2 arms | 123/128 | PN one to one, educational booklet and closed online social network group. Team updated posts on BF weekly with monthly phone interviews up to 6 months postpartum; provided by academic of nutrition, nursing, social work and psychology courses, nutritionist, paediatricians, and supervising professors. Training was provided by nutritionists | Educational booklet, weekly posts on social network and follow‐up telephone calls. One topic each week included, let down, benefits of exclusive BF, latching, | Routine guidance, about BF and general baby care provided by the care team, with assistance as needed |
|
Di Meglio, 2010, USA |
Parallel RCT 2 arms Not reported |
Adolescent mothers 38/40 |
PN one‐to‐one seven telephone calls every day/2 days provided by peer supporters who undertook La Leche League BF support programme and breastfed more than four weeks | Telephone calls asking about BF experiences. Based on WIC BF promotion peer support effort. | Routine care of having access to other modalities including family, friends, paediatric team and hospital lactation consultants |
|
Efrat, 2015, USA |
Parallel RCT ‐ 2 arms July 2011–July 2012 |
Low income Hispanic mothers 143/146 |
AN and PN one‐to‐one SMS and phone calls, 4 prenatal and 17 PN contacts. Two calls in the first postpartum week, followed by one call from 2‐8 postpartum and one call at 6 months postpartum, provided by lactation consultants who were undergraduate students completed a long semester lactation education course and 10 h training post‐course | Telephone calls for increasing BF motivation and expectation guidance. | Routine BF education and support including prenatal education classes and support about BF, breast pumps, helpline and BF consultation services |
|
Ericson, 2018a, Sweden |
Parallel RCT 2 arms March 2013–Dec 2015 |
Preterm infants 231/262 |
PN one‐to‐one support via daily telephone calls from day one to 14 after discharge provided by NICU staff who were given two days of training | Proactive telephone calls to encourage mothers to talk about whatever important to them | Mothers could phone BF Support Team from day one to day 14 after discharge from 08:00‐16:00 daily and weekend. |
|
Forster, 2019, Australia |
Parallel RCT 2 arms Feb 2013–Dec 2015 |
577/580 | PN one‐to‐one telephone support, 2 calls in the first week post‐charge, then weekly for 12 weeks, then 3‐4 weekly up to 6 months, provided by Lay providers who had breastfed a baby for at least 6 months and had no more than 8 h of professional BF training or counsellor | Proactive telephone calls from peer volunteer focused on BF experiences and well‐being. Referral to existing support services available as required. | One to two PN home visits within the first week of hospital discharge provided by a hospital midwife, after which a Maternal and Child Health Nurse provided services. All women could have access to telephone helpline services staffed by trained volunteer BF counsellors |
|
Fu, Tarrant, 2014, Hong Kong |
Cluster RCT 3 arm Nov 2010–Sept 2011 |
In hospital 191/264 | PN one‐to‐one professional support and education provided for hospital group 2 × 30 min within 24 h and 1 × 30 min in next 24 h. In hospital group, support was provided face‐to‐face through three sessions before discharge. Each session lasted 30–45 min. | In hospital group, information on BF benefits, lactation physiology and problems were provided to participants who also were observed feeding with hands‐on guidance and manual breastfeeding expression. | Routine perinatal care by midwife or lactation consultant. One‐to‐one assistance as needed and time permitted. Information about peer‐support groups after hospital discharge. Follow‐up at the hospital clinics or nearest Maternal and Child Health Centre. |
|
Telephone support 269/264 |
PN one‐to‐one support and education provided for telephone support group within 72 h of discharge. Support was provided weekly for 4 weeks or until BF had stopped | Telephone group, sessions on general information about breastfeeding, assessing feeding patterns, guidance on managing problems and mothers' physical and emotional health and BF discreetly in public. | |||
|
Demirci, 2019, USA |
Parallel RCT 2 arms Not reported |
250 total | AN from 25 weeks and PN to 8 wks, 3–7 times a week one‐to‐one semi‐automated text messages and could text keywords for help from an ‘on‐call’ study lactation consultant (no details of training). | Information on the benefits of exclusive BF, the physiology of lactation, and common early BF problems. Guidance and instruction on BF techniques. During each session, participants were observed positioning, attaching, and feeding the newborn, with appropriate feedback provided and hands‐on guidance only when necessary. | Received general perinatal text‐based support |
|
Gonzalez‐Darias, 2020, Canary Islands, Spain |
Parallel RCT 2 arms April–October 2016 |
76/78 | Website allowed one‐to‐one contact between first‐time mothers and peer‐supporters. Mothers had 24‐h access to information and to contact their named‐supporter. The contact between supporters and new mothers lasted 6 months | Extra support to first‐time mothers wishing to breastfeed, through a website, where mothers had access to the most up‐to‐date information to answer questions regarding BF. Each participant was assigned a named supporter, who could be contacted regarding BF questions. | Routine PN care at both hospital and Health Centres, could attend support groups, midwife care or family planning. |
|
Hagi‐Pedersen, 2020, Denmark |
Parallel RCT 2 arms Nov 2015–Sept 2018 |
Preterm infants 107/110 |
Video consultations 2 to 3 times a week and constant use of application. With responsible nurses with specific interest in‐home care trained in use of the application had access to first author for problems and had regular meetings. | In addition to usual care offer of video consultations from their home. Offered a smartphone with an app and instructions and training on how to use it. App had 3 components (1) advice and recommendations about BF, positions, cues, skin to skin (2) data registration for nutrition vitamins and weight (3) link for video consultations | Pre home care programme included early home care, first aid training, borrowed breast pumps, received a leaflet and information about care of infant and were instructed how to insert the feeding tube. Could call neonatal unit 24 h/day to receive help. Plus 2–3 consultations/wk with nurse at the hospital. |
|
Hoddinott, 2012, Scotland |
Parallel RCT 2 arms (July–Oct 2010) |
Participants from deprived areas 35/34 |
PN, one to one support by research team. Daily for 1 week following hospital discharge. Offered further daily calls for next week or could choose different frequency or cease calls. | Proactive telephone support. Daily proactive and reactive telephone calls for < or on 14 days. Women could telephone the feeding team at any point over the 2 weeks following discharge. Text and answer phone messaging was available. | Reactive telephone calls < or on day 14. Women could call the feeding teams at any time throughout the two weeks following discharge from hospital. Text and answerphone messaging available. |
|
Hongo, 2019, Japan |
Parallel RCT 2 arms |
63/62 | From hospital discharge to 4 months. Frequency not specified. Contact intervals times to coincide with frequent days | Peer support by telephone. Listened to participants concerns, acknowledged them and provided information and/or referrals to LLL or health professionals if required. Encouraged to call peer supporter if they had concerns. | Conventional care included BF support in hospital and a home visit by a health worker. |
|
Howell, 2014, USA |
Parallel RCT 2 arms |
African American & Hispanic mothers 270/270 |
PN education pamphlet reviewed in hospital plus partner summary sheet and 1 phone call at 2 weeks after birth by social worker. |
Education pamphlet included information on BF, breast/nipple pain, delivery issues, infant colic, depressive symptoms and sources of social support. Partner summary sheet ‐ typical pattern of experience for mothers to normalize the experience. 2‐week call, assessed patients' symptoms, skills in symptom management, and other needs. Created action plans to address current needs that included assessment of community resources. |
Enhanced usual care participants received a list of community resources and received a 2‐week control call. |
| Kamau ‐Mbuthia, 2013 |
Parallel RCT Arms (2 relevant for this review) |
153/179 | AN and PN one‐to‐one telephone support | Trained peer leaders supported both pregnant and post‐partum women with continuous cell phone‐based peer support | Standard of care of existing facility‐based support. |
|
Lewkowitz, 2020, USA |
Parallel RCT 2 arms Not reported |
Low income 84/85 |
PN on demand videos‐Android phone by healthcare workers with certified specialist lactation training. BF application was designed by BF consultants and refined by focus group of pregnant. | BF Friendly application by smartphone with internet contained technology‐based BF education and postpartum support. | Skeleton application provided digital BF handout |
|
Lucas, 2019, USA |
Parallel RCT 2 arms Apr–Nov 2017 |
33/32 | 12 PN one to one bi‐weekly texts via SMS for 6 weeks by healthcare workers without certified specialist lactation training. Nurse‐led team, used IBCLC scripts. | The BF self‐management included nurse‐led instrumental support texting, emailed study measures, hyperlinks to educational modules addressing breast and nipple pain, a daily BF journal, and reminders to complete study documents. All activities were targeted to support women to increase their knowledge and skills regarding breast and nipple pain, as well as their ability to manage BF challenges. | Women in the control group were contacted by text at 1, 2 and 6 weeks to check their email to complete their data measures via a REDCap link. Up to three text and email reminders were sent to the women to complete the data measures. |
|
Maslowsky, 2016, Ecuador |
Parallel RCT 2 arms June–Aug 2012 |
102/76 | PN telephone‐delivered educational session within 48 h of hospital discharge. Then the nurse available by mobile phone for first 30 days | Telephone delivered educational session based on semi‐structure guide. Access to a nurse on‐call during the first 30 days. Could call the nurse to ask questions regarding their own or their newborn's health and care. Nurse provided medical advice, information, and support, and triaged patients to determine whether a clinic visit was needed. Nurse was available via phone from 8 am to 5 pm, Monday to Friday. | Treatment as usual, consisting of brief discharge instructions delivered by a nurse at the time of hospital or clinic discharge. These instructions typically include a newborn check‐up within 1 week, a maternal follow‐up visit within 6 weeks, and initiation of a family planning regimen. |
|
Martinez, 2018, USA |
Parallel RCT 2 arms Aug 2014– Jan 2016 |
114/98 | AN and PN one‐to‐one, text messages by lay provider, peer supporters 4/7 in part‐time employment and three IBCLC. IBCLCs seem to supervise the peer supporters. The researchers initiated text messaging. | Text messages were sent with increasing frequency prenatally and decreasing frequency postpartum. Message content covered the benefits of BF for mothers and children, showed examples of proper positioning, explained how to tell whether the baby was getting enough milk, debunked BF myths, and reinforced the BFPC's supportive role. | The standard care of WIC Loving Support BF peer counselling program. Control group participants did not exchange text messages with their peer counsellors and were instructed not to text their BFPCs via their personal cell phones. Mothers were still able to make contact. |
|
Niela‐Vielen, 2016, Finland |
Parallel RCT 2 arms 2011–2015 |
Preterm infants 60/64 |
PN internet‐based peer support—peer support by untrained peer supporters who had breastfed preterm babies via closed Facebook group. Midwife was available for answering questions. | Closed BF Facebook Support group. Mothers could join after they were discharged or at a later date (e.g. when their infant was discharged). Peer support was provided by three voluntary mothers with previous experience on BF their own preterm infants. Special education for peer supporters was not organized; they were asked to be supportive and respective of the mothers' choices and decisions. The participating mothers were also peer supporters of each other. | Routine NICU care. Mothers were asked to initiate hand expression with 6 h post‐partum, 8 times daily after that, and once at night. Oral feeding (nasogastric tube) in initiated o the day of birth. Bottle feeding and BF are initiated at a mean post‐conceptual age of 33–34 weeks |
|
Palacios, 2018, Hawai'i and Puerto Rico |
A multi‐site parallel RCT 2 arms 2017 |
Low income 102/100 |
PN one‐to‐one, 18 texts over 4 months (1/week) BF certified healthcare workers |
SMS‐Web‐based for BF benefits and BF practical suggestions such as position and attachment; more feeding means more milk | For general infants' health issues and care for common infant illnesses |
|
Patel, 2018, India |
Parallel RCT 2 arms Aug 2010–July 2012 |
Participants resided in slums 518/518 |
AN and PN one‐to‐one, weekly phone counselling and daily text messages by certified auxiliary nurse midwives with counselling training. Starting in the third trimester to 6 months. | Women received cell phone, seven free charges voucher and prepaid cards for speed dial facilities. Content of counselling ‐ appropriate young child feeding practices, avoidance of pre‐lacteal feeds and how to deal with BF problems and immunizations. Texts in own language to augment appropriate feeding practices. | Routine healthcare facilities |
|
Reeder, 2014, USA |
Parallel RCT 3 arms: July 2005‐ July2007 |
Low income 646/657 |
AN and PN one‐to‐one, 4 telephone contacts and 8 telephone contacts Lay person |
4 planned calls for low‐frequency peer counselling group:1st after initial prenatal assignment, 2nd 2 weeks before the expected due date, 3rd & 4th at 1 and 2 weeks PN. | Only standard WIC BF promotion and support. No contact with peer counsellor. |
|
Low income 645/657 |
AN and PN one‐to‐one, 8 telephone contacts with lay person | 8 planned calls for high‐frequency peer counselling group: 4 calls were the same calls for the low‐frequency group, and 4 calls at 1st, 2nd, 3rd and 4th month | |||
|
Seguranyes, 2014, Spain |
Multicentre, parallel RCT Nov 2018–Dec 2019 | 798/800 | PN video conferences and consultation, Skype, calls, from discharged day up to six weeks postpartum. By certified midwives | Videoconferences, video calls, Skype and calls with midwives from 8 am to 8 pm from the discharged day up to 6 weeks. | Standard PN care at centres or home, and one scheduled visit at centre after 6th week postpartum and could attend BF groups |
|
Simonetti, 2012, Italy |
Parallel RCT 2 arms Feb–March 2009 |
55/59 | PN one to one telephone calls at least once a week during the first 6 weeks after birth. Weekly or more often if required by a midwife. | Received telephone calls during the first 6 weeks. The phone call timing was planned in accord by both the mother and Licensed midwife. During every phone call, the midwife gave support and all information on fully BF. | Received a standard counselling program, consisting of programmed periodical visits with the physician at 1, 3 and 5 months after delivery. They were also invited, like the women of the experimental group, to call the Licensed Midwife in case of BF problems |
|
Tahir, 2013, Malaysia |
Parallel RCT 2 arms 2010 |
179/178 | 12 PN by telephone—2× monthly to 6 months by trained certified lactation counsellor. | Lactation counselling by telephone in addition to standard care (no further details provided). | Standard care—BF talks during immunisation, communication and BF advice with lactation counsellors or other health professionals during AN or PN follow‐ups. |
|
Unger, 2018, Kenya |
Parallel RCT 3 arms Aug 2013–Apr 2014 |
One way messaging 99/100 |
Women randomised to the one‐way group received weekly ‘push’ educational and motivational SMS. | Automated personalised messages provided gestational age‐appropriate educational and counselling. Content tailored for maternal characteristics and pregnancy or postpartum timing. Classified into tracks (routine, adolescents, first‐time mothers, women with a previous CS, and multiple gestations). Received routine messages unless in a track. Messages included name, clinic and nurse name, an educational message, and actionable advice targeting one of the main study outcomes. | Routine clinic‐based counselling and care. |
|
Two way 99/100 |
24 AN and PN weekly one‐to‐one two‐way personalised text messaging by nurse (training not reported). | The two‐way group received the same weekly SMS; however, each SMS contained a question related to the content. During enrolment, the study nurse explained that replies to SMS questions were voluntary. Women were also encouraged to send SMS with concerns or questions. | |||
|
Uscher‐Pines, 2019, Pennsylvania USA |
Parallel RCT 2 arms Oct 2016–May 2018 |
102/101 | PN unlimited, on‐demand video calls with IBCLCs through phone application for as long as desired. | Telelactation involved orientation to application by hospital nurses—how to download the app on a personal device (smartphone or tablet), a coupon code for free, unlimited video calls, and encouraged participants to conduct a test call. After orientation, participants could request unlimited, on‐demand video calls with IBCLCs through the app for as long as they desired. | Usual care—support offered by various healthcare professionals during hospital stay. After discharge, support from paediatricians and their staff as a component of routine, outpatient paediatric health maintenance visits, and women enrolled in WIC could access WIC BF services. |
|
Webb, Kamau, Sellens 2013–2015 Kenya |
Parallel RCT Arms (2 relevant for this review) |
153/179 | AN and PN one‐to‐one telephone support | Trained peer leaders supported both pregnant and post‐partum women with continuous cell phone based peer support | Standard of care of existing facility‐based support. |
Abbreviations: AN, antenatal; BF, breastfeeding; BMI, body mass index; IBCLC, International Board Certified Lactation Consultant; PN, postnatal; RCT, randomised controlled trial; WIC, Supplemental Nutrition Programme for Women Infants and Children.
3.2.1. Participants and settings
A total of 11,470 women from 29 trials (sample sizes ranged from 65 to 1948) and their infants from 17 countries were randomised. Twenty‐three studies were conducted in 12 high‐income countries accounting for 79% of participants (9117 participants). Three studies were conducted in upper‐ and 3 in lower‐middle income countries accounting for 6.8% (786) and 13.6% (1567) participants, respectively. No studies were identified that had been conducted in low‐income countries.
Characteristics of participants varied across the studies both for mothers and infants. Some studies recruited from specific populations groups, such as adolescent mothers (Di Meglio et al., 2010), obese mothers (Carlsen et al., 2013), or low income mothers (Efrat et al., 2015; Hoddinott et al., 2012; Kamau‐Mbuthia et al., 2013; Lewkowitz et al., 2020; Palacios et al., 2018; Patel et al., 2018; Reeder et al., 2014), or mothers from specific ethnic backgrounds (Efrat et al., 2015; Howell et al., 2014) and 3 studies recruited only mothers of preterm infants (Ericson et al., 2018; Hagi‐Pedersen et al., 2017; Niela‐Vilen et al., 2016). However, most studies recruited women without medical conditions who gave birth to healthy term infants, with no congenital abnormalities. The mean age of mothers included in 14 trials was in the 20–30 years age range (Cavalcanti et al., 2019; Efrat et al., 2015; Gonzalez‐Darias et al., 2020; Hoddinott et al., 2012; Howell et al., 2014; Martinez‐Brockman et al., 2018; Maslowsky et al., 2016; Niela‐Vilen et al., 2016; Palacios et al., 2018; Patel et al., 2018; Reeder et al., 2014; Tahir & Al‐Sadat, 2013; Unger et al., 2018; Uscher‐Pines et al., 2019) and over 30 years in 9 studies (Abbass‐Dick et al., 2015; Ahmed et al., 2016; Carlsen et al., 2013; Ericson et al., 2018; Forster et al., 2019; Fu et al., 2014; Hagi‐Pedersen et al., 2017; Hongo et al., 2020; Lucas et al., 2019), with only one study with a mean age under 20 years (Di Meglio et al., 2010). In other studies age was not reported. In studies which were not targeting a specific group of women, participants tended to be more highly educated and from higher socioeconomic groups. Twenty‐two studies included both multiparous and primiparous women and seven recruited only primiparous women (Abbass‐Dick et al., 2015; Demirci et al., 2019; Forster et al., 2019; Fu et al., 2014; Gonzalez‐Darias et al., 2020; Lewkowitz et al., 2020; Simonetti et al., 2012). Where mode of birth was reported women were not excluded if they had a Caesarean birth; mode of birth was not reported in 11 studies.
3.2.2. Interventions
Varied modes of remote interventions were apparent with most involving the telephone. Telephone calls as all or part of the intervention from either peer/lay supporters (Di Meglio et al., 2010; Efrat et al., 2015; Forster et al., 2019; Hongo et al., 2020; Kamau‐Mbuthia et al., 2013; Reeder et al., 2014), or health professionals (Abbass‐Dick et al., 2015; Carlsen et al., 2013; Ericson et al., 2018; Fu et al., 2014; Hoddinott et al., 2012; Howell et al., 2014; Maslowsky et al., 2016; Patel et al., 2018; Seguranyes et al., 2014; Simonetti et al., 2012; Tahir & Al‐Sadat, 2013), were the most common intervention. Telephone calls alone were used in 10 studies (Carlsen et al., 2013; Ericson et al., 2018; Forster et al., 2019; Fu et al., 2014; Hoddinott et al., 2012; Hongo et al., 2020; Kamau‐Mbuthia et al., 2013; Reeder et al., 2014; Simonetti et al., 2012; Tahir & Al‐Sadat, 2013) and in five studies were combined with other components, such as emails (Abbass‐Dick et al., 2015), text messages (Efrat et al., 2015; Patel et al., 2018), education using telephone (Maslowsky et al., 2016) or pamphlets (Howell et al., 2014). Text messaging was a component of the intervention in seven studies (Demirci et al., 2019; Efrat et al., 2015; Lucas et al., 2019; Martinez‐Brockman et al., 2018; Palacios et al., 2018; Patel et al., 2018; Unger et al., 2018). Interactive text messaging alone was used in four studies (Demirci et al., 2019; Efrat et al., 2015; Lucas et al., 2019; Martinez‐Brockman et al., 2018; Palacios et al., 2018; Unger et al., 2018) and with hyperlinks to an educational module in one study (Lucas et al., 2019). A phone App was used in four studies (Ahmed et al., 2016; Hagi‐Pedersen et al., 2017; Lewkowitz et al., 2020; Uscher‐Pines et al., 2019). Other interventions included: peer support via social media (e.g., Facebook) either in response to mothers concerns (Niela‐Vilen et al., 2016), or structured by use of an educational booklet (Cavalcanti et al., 2019); video calls or Skype (Seguranyes et al., 2014); support via a website alone (Gonzalez‐Darias et al., 2020) or via a website combined with other interventions such as a workbook, and a DVD with telephone calls (Abbass‐Dick et al., 2015).
All interventions were provided after birth but in seven studies there was also an antenatal component (Demirci et al., 2019; Efrat et al., 2015; Kamau‐Mbuthia et al., 2013; Martinez‐Brockman et al., 2018; Patel et al., 2018; Reeder et al., 2014; Unger et al., 2018). The frequency of interventions was variable with nine being open access and/or whenever needed by the mother (Ahmed et al., 2016; Gonzalez‐Darias et al., 2020; Kamau‐Mbuthia et al., 2013; Lewkowitz et al., 2020; Maslowsky et al., 2016; Niela‐Vilen et al., 2016; Seguranyes et al., 2014; Simonetti et al., 2012; Uscher‐Pines et al., 2019). In seven studies interventions were provided weekly (Abbass‐Dick et al., 2015; Cavalcanti et al., 2019; Forster et al., 2019; Fu et al., 2014; Palacios et al., 2018; Reeder et al., 2014; Unger et al., 2018) and six were every 1–2 days (Demirci et al., 2019; Ericson et al., 2018; Hagi‐Pedersen et al., 2017; Hoddinott et al., 2012; Lucas et al., 2019; Patel et al., 2018). Six varied in frequency (Carlsen et al., 2013; Di Meglio et al., 2010; Efrat et al., 2015; Martinez‐Brockman et al., 2018; Reeder et al., 2014; Simonetti et al., 2012), one was twice monthly (Tahir & Al‐Sadat, 2013), one was only provided once (Howell et al., 2014), and in one study frequency was not specified (Hongo et al., 2020). A range of personnel provided the interventions. In 11 studies interventions were provided by health care professionals, either nurses or midwives with or without specialist training (Cavalcanti et al., 2019; Ericson et al., 2018; Hagi‐Pedersen et al., 2017; Hoddinott et al., 2012; Lucas et al., 2019; Maslowsky et al., 2016; Palacios et al., 2018; Patel et al., 2018; Seguranyes et al., 2014; Simonetti et al., 2012; Unger et al., 2018) and in one study by social workers (Howell et al., 2014). In eight studies interventions were provided by lactation consultants, although it was not always clear what specialist training had been completed (Abbass‐Dick et al., 2015; Ahmed et al., 2016; Carlsen et al., 2013; Demirci et al., 2019; Fu et al., 2014; Lewkowitz et al., 2020; Tahir & Al‐Sadat, 2013; Uscher‐Pines et al., 2019). In a further nine studies interventions were provided by lay or peer supporters (Di Meglio et al., 2010; Efrat et al., 2015; Forster et al., 2019; Gonzalez‐Darias et al., 2020; Hongo et al., 2020; Kamau‐Mbuthia et al., 2013; Martinez‐Brockman et al., 2018; Niela‐Vilen et al., 2016; Reeder et al., 2014) and a midwife was also available in one study (Niela‐Vilen et al., 2016).
3.2.3. Comparisons
Most comparisons were described as standard or usual care and details were not always provided. Where described, this varied and nine comparisons included face‐to‐face breastfeeding support and/or consultations (Abbass‐Dick et al., 2015; Carlsen et al., 2013; Cavalcanti et al., 2019; Efrat et al., 2015; Hongo et al., 2020; Martinez‐Brockman et al., 2018; Reeder et al., 2014; Tahir & Al‐Sadat, 2013; Uscher‐Pines et al., 2019), two included the option to call the healthcare provider for advice (Ericson et al., 2018; Hoddinott et al., 2012) and three included both (Ahmed et al., 2016; Forster et al., 2019; Simonetti et al., 2012). In six studies the comparison was described as routine postnatal care with no information about breastfeeding support (Gonzalez‐Darias et al., 2020; Maslowsky et al., 2016; Niela‐Vilen et al., 2016; Patel et al., 2018; Seguranyes et al., 2014; Unger et al., 2018). Three studies described combined support and breastfeeding education (Ahmed et al., 2016; Cavalcanti et al., 2019; Efrat et al., 2015). The length of time standard care was provided was reported in 12 studies and varied. It could be as needed (Abbass‐Dick et al., 2015; Cavalcanti et al., 2019), last several weeks (Ahmed et al., 2016; Carlsen et al., 2013; Ericson et al., 2018; Forster et al., 2019; Hoddinott et al., 2012; Howell et al., 2014; Lucas et al., 2019; Maslowsky et al., 2016; Seguranyes et al., 2014) or months after discharge (Simonetti et al., 2012).
3.2.4. Outcomes
For primary outcomes, 14 studies reported exclusive breastfeeding at 4–8 weeks, 12 studies reported any breastfeeding at 4–8 weeks, 12 studies reported exclusive breastfeeding at 3 months, 9 studies reported any breastfeeding at 3 months, 11 studies reported exclusive breastfeeding at 6 months and 6 reported stopping any breastfeeding at 6 months. No studies with an antenatal component measured breastfeeding initiation, thus data were not available for this outcome. Very few studies reported secondary outcomes and there was heterogeneity in terms of outcomes and measures. More specifically four studies measured maternal satisfaction, one study measured perinatal mental health and one study measured maternal self‐efficacy. Five studies only measured breastfeeding rates at 3 months and a post‐hoc decision was made to include this as an outcome to allow these studies to contribute data to the meta‐analyses.
3.2.5. Risk of bias
The risk of bias varied across the domains. More specifically, 75% of studies were judged as low risk of bias for random sequence generation; 48% were low risk of bias for allocation concealment; 59% were low risk of bias for incomplete outcome data; 55% were low risk of bias for selective outcome reporting and 83% were low risk for any other forms of bias. Reasons for high risk of bias in the ‘other’ domain was generally due to significant baseline imbalances. All studies were judged to be at high or unclear risk of performance bias due to the difficulties in blinding participants and personnel to the interventions. Except for Patel et al. (2018), all studies were judged to be either high or unclear risk of bias for blinding of outcome assessment. This was a consequence of most studies collecting self‐report data from the women who were not blinded. See Figures S1,2 for further details.
3.2.6. Effects of interventions
3.2.6.1. Primary outcomes
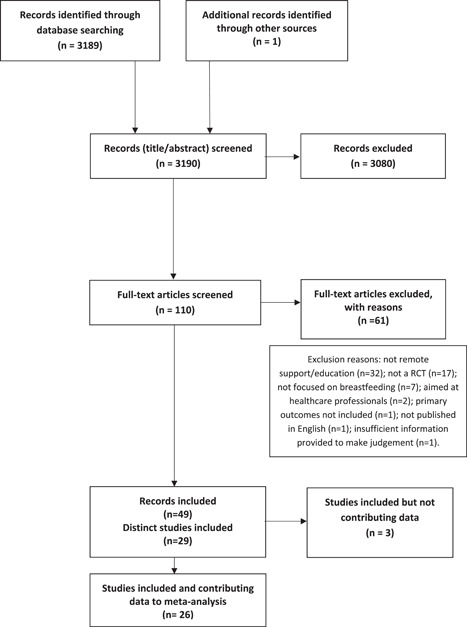
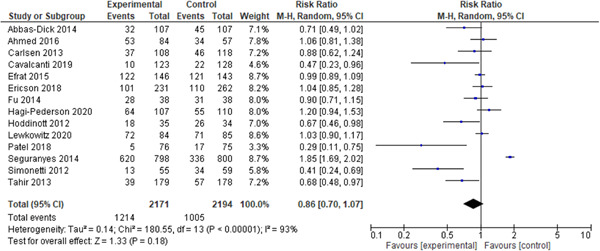
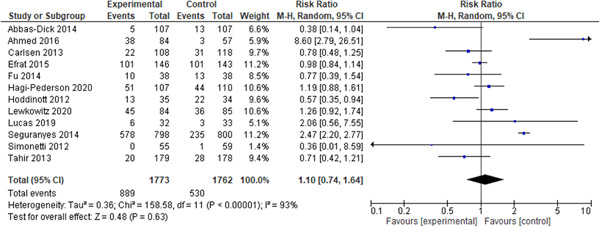
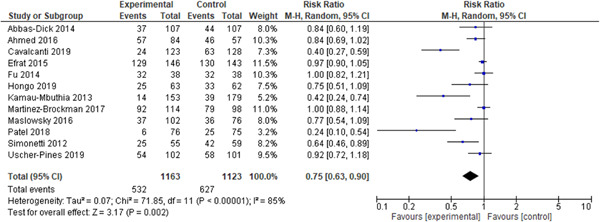
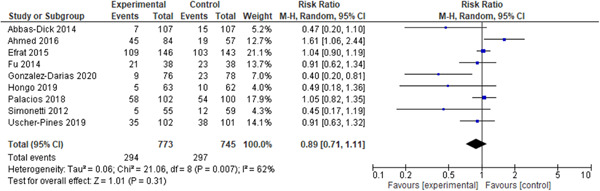
Figures 2, 3, 4, 5, 6, 7 show the pooled effects of remotely provided breastfeeding support on the six primary outcomes included in this review. Remotely provided breastfeeding support significantly reduced the risk of women stopping exclusive breastfeeding at 3 months by 25% (risk ratio [RR]: 0.75, 95% confidence interval [CI]: 0.63, 0.90) (see Figure 4). At 6 months there was a 7% reduction in women ceasing exclusive breastfeeding, however, this did not reach significance (RR: 0.93, 95% CI: 0.85, 1.00) (see Figure 6). There was no significant difference in the number of women stopping any breastfeeding at 4–8 weeks (RR: 1.10, 95% CI 0.74, 1.64), 3 months (RR: 0.89, 95% CI: 0.71,1.11) or 6 months (RR: 0.91, 95% CI: 0.81, 1.03) or the number of women stopping exclusive breastfeeding at 4–8 weeks (RR: 0.86, 95% CI: 0.70, 1.07) (see Figures 2, 3, 5, 7).
Figure 2.
Forest plot of comparison: Remote support versus standard care/control, outcome: Stopping exclusive breastfeeding at 4–8 weeks
Figure 3.
Forest plot of comparison: Remote support versus standard care/control, outcome: Stopping any breastfeeding at 4–8 weeks
Figure 4.
Forest plot of comparison: Remote support versus standard care/control, outcome: Stopping exclusive breastfeeding at 3 months
Figure 5.
Forest plot of comparison: Remote support versus standard care/control, outcome: Stopping any breastfeeding at 3 months
Figure 6.
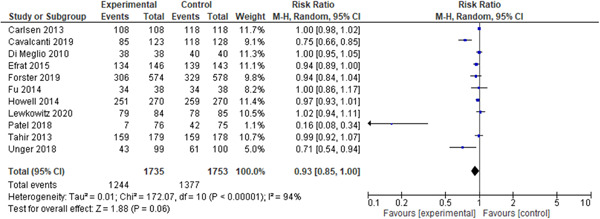
Forest plot of comparison: Remote support versus standard care/control, outcome: Stopping exclusive breastfeeding at 6 months
Figure 7.
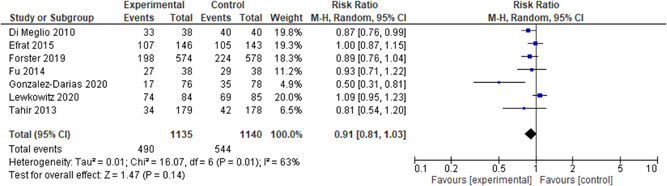
Forest plot of comparison: Remote support versus standard care/control, outcome: Stopping exclusive breastfeeding at 6 months
Statistical heterogeneity was high for all outcomes: exclusive breastfeeding at 4–8 weeks (Tau2 = 0.14, I 2 = 93%, Chi2 = 180.55, p < 0.00001); any breastfeeding at 4–8 weeks (Tau2 = 0.36, I 2 = 93%, Chi2 =158.58, p < 0.00001); exclusive breastfeeding at 3 months (Tau2 = 0.0.07, I 2 = 85%, Chi2 = 43.39, p < 0.0001); any breastfeeding at 3 months (Tau2 = 0.06, I 2 = 62%, Chi2 = 21.06, p = 0.007); exclusive breastfeeding at 6 months (Tau2 = 0.02, I 2 = 94%, Chi2 = 172.07, p < 0.00001); and any breastfeeding at 6 months (Tau2 = 0.01, I 2 = 63%, Chi2 = 16.07, p = 0.01).
Sensitivity analyses which removed the 13 studies at high or unclear risk of bias for allocation concealment found similar effects (see Table S2), except for exclusive breastfeeding at 6 months which became significant (RR: 0.85, 95% CI: 0.73, 0.99) and 3 months which changed to be nonsignificant (RR: 0.76, 95% CI: 0.56, 1.04). However, a sensitivity analysis whereby the 12 studies at high or unclear risk of bias for incomplete outcome data (see Table S2), found that exclusive breastfeeding at 4–8 weeks became significant with a 24% reduction in risk of stopping breastfeeding (RR: 0.76, 95% CI: 0.61, 0.96). Similarly, any breastfeeding at 3 and 6 months just reached statistical significance with a reduced risk in stopping breastfeeding of 26% (RR: 0.74, 95% CI: 0.55, 1.00) and 18% (RR: 0.82, 95% CI: 0.67, 1.00), respectively.
Inspection of funnel plots did identify some asymmetry with smaller studies tending to show more positive effects (see Figures S1‐S6). However, there is also evidence of substantial heterogeneity which may contribute to this. To further explore the risk of publication bias, the fixed and random effect sizes were compared. The random effects model did not shift the effect estimates towards the results of the smaller studies which suggests an absence of any small study effects (Page et al., 2020; Sterne et al., 2011).
3.2.6.2. Additional outcomes
Three of the four studies measuring maternal satisfaction reported no differences between the study groups. Ericson et al. (2018) reported no significant difference in maternal satisfaction at 8 weeks in the intervention group (mean [M]: 113.7, standard deviation [SD]: 19.2) versus the control group (M: 113.6, SD: 19.3, p = 0.97). Similarly no significant difference in maternal satisfaction was reported by Hoddinott et al. (2012) in the intervention group (M: 8.7, SD: 1.7) compared to the control group (M: 81, SD: 2.8, p = 0.23) and no significant difference was reported by Seguranyes et al. (2014) in the intervention group (M: 4.77, SD: 0.5) compared to the control group (M: 4.76, SD: 0.56, p = 0.105). However Patel et al. (2018), reported that 92.3% of the intervention group were satisfied versus 36% of the control group.
Only one study reported measures relating to perinatal mental health (Ericson et al., 2018). There was a small but significant improvement in perinatal mental health measured by the Swedish parental stress scale in the intervention group (M: 2.35, SD: 0.5) compared to the control group (M: 2.48, SD: 0.51, p = 0.015). Only one study measured maternal self‐efficacy. Hagi‐Pedersen et al. (2017) reported no significant difference in maternal self‐efficacy in the intervention group (median: 43, interquartile range [IR]: 41–45) compared to the control group (median: 43, IR: 40–44).
3.2.7. Certainty of the evidence
The six primary outcomes were assessed with the GRADE criteria (see Table 2). All outcomes were graded low or very low. Outcomes were not downgraded for lack of blinding. Although Funnel Plot asymmetry was identified we did not downgrade for this as a comparison with a fixed effects model did not reveal that the random effects estimate was more beneficial.
Table 2.
Summary of findings table
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | |
|---|---|---|---|---|---|
| Risk with standard care/control | Risk with Remote support | ||||
| Stopping exclusive breastfeeding at 4–8 weeks | 458 per 1000 | 394 per 1000 (321–490) | RR 0.86 (0.70–1.07) | 4365 (14 RCTs) | ⊕〇〇〇 VERY LOWa, b, c |
| Stopping any breastfeeding at 4–8 weeks | 314 per 1000 | 345 per 1000 (226–468) | RR 1.10 (0.74–1.64) | 3535 (12 RCTs) | ⊕⊕〇〇 LOWb, c |
| Stopping exclusive breastfeeding at 3 months | 558 per 1000 | 435 per 1000 (336–474) | RR 0.5 (0.63–0.90) | 2286 (12 RCTs) | ⊕⊕〇〇 LOWb, d |
| Stopping any breastfeeding at 3 months | 415 per 1000 | 370 per 1000 (229–434) | RR 0.89 (0.71–1.11) | 1518 (9 RCTs) | ⊕⊕〇〇 LOWb, c |
| Stopping exclusive breastfeeding at 6 months | 786 per 1000 | 715 per 1000 (691–746) | RR 0.93 (0.88–0.1.00) | 3488 (11 RCTs) | ⊕⊕〇〇 LOWb, d |
| Stopping any breastfeeding at 6 months | 477 per 1000 | 434 per 1000 (387–492) | RR 0.91 (0.81–1.03) | 2275 (7 RCTs) | ⊕⊕〇〇 LOWa, b |
High or unclear risk of bias for incomplete outcomes. Sensitivity analyses restricted to trials of low risk of bias showed a change in significant of findings. Downgraded 1 level.
Substantial unexplained heterogeneity (>60%). Downgraded 1 level.
Wide confidence interval crossing line of no effect (RR < 0.75 or >1.25).
High or unclear risk of bias for allocation concealment. Sensitivity analyses restricted to trials of low risk of bias showed a change in significant of findings. Downgraded 1 level.
4. DISCUSSION
This systematic review found that remotely provided breastfeeding support and education combined with support in hospital is an effective intervention to increase the rates of exclusive breastfeeding at 3 months. However, for other outcomes the results are less clear. Exclusive breastfeeding at 6 months was only significant when studies at high risk of allocation concealment were excluded. Exclusive breastfeeding at 4–8 weeks was only significant once studies with loss to follow‐up greater than 20% were excluded. There was little evidence of any impact on any breastfeeding. However, when studies with loss to follow‐up greater than 20% were excluded, any breastfeeding at 3 and 6 months did become significant. The certainty of the evidence was judged to be low or very low for all outcomes.
While this may suggest that remote breastfeeding support and education had little effect on duration of any breastfeeding, it is important to consider what the interventions were being compared to, with the majority of studies providing some form of breastfeeding support as part of their routine care. There was considerable heterogeneity in how routine care was offered (e.g., lactation consultants, peer support, in‐hospital, outpatient clinics, reactive or proactive), which makes comparisons difficult. Moreover, in the studies reporting statistically significant benefits, the control group appeared to have more limited support, e.g. offered reactively or only limited details provided (Abbass‐Dick et al., 2015; Cavalcanti et al., 2019; Gonzalez‐Darias et al., 2020; Hoddinott et al., 2012; Kamau‐Mbuthia et al., 2013; Simonetti et al., 2012; Tahir & Al‐Sadat, 2013). It therefore could be argued that if remote provision is the only type of provision available (as would be the case in the Covid‐19 pandemic), then this may have been more effective than the comparator. Alternatively, if remote provision in addition to existing services including face‐to‐face support is synergistic then inability to provide these may reduce the effectiveness of the remote provision.
Given the low number of studies and high heterogeneity, it is difficult to extrapolate from our review, why remote support has a greater effect for exclusive breastfeeding compared to any breastfeeding and why this occurs only at certain timepoints. One reason could be that mothers who are highly motivated to breastfeed exclusively benefited most from support to achieve their goals. This explanation is supported by a realist review of breastfeeding peer support (Trickey et al., 2018) Other systematic reviews have also found that breastfeeding support has a greater effect on exclusive compared to any breastfeeding outcomes (McFadden et al., 2017; McFadden et al., 2019). In addition, McFadden et al. (2017) found that support was more effective in settings where background rates of breastfeeding initiation were high. This suggests that continued efforts are needed to promote breastfeeding to increase motivation.
Explanations for why support interventions were effective for exclusive breastfeeding at 3 but not 6 months are probably multi‐faceted. Overall, the breastfeeding interventions tended to have higher intensity in the first 6 weeks following birth, with frequency of contact reducing or ceasing beyond this timepoint. Reasons why mothers cease breastfeeding in the first 6 weeks such as fatigue, inconvenience and concerns about milk supply (C. R. L. Brown et al., 2014; McAndrew et al., 2012), may be more amenable to the support interventions There are additional contextual challenges to exclusive breastfeeding beyond 3 months, for example mothers returning to paid employment, cultural practices of introducing solids before 6 months and societal attitudes towards breastfeeding public in some settings (Alianmoghaddam et al., 2018; Burns & Triandafilidis, 2019). These challenges may impact on the effectiveness of support interventions.
In addition, we cannot extrapolate whether any specific participant characteristics such as age, level of education or parity impacted on the effectiveness of interventions. These characteristics are not consistently reported in trials and their association with breastfeeding varies in different settings.
As expected, statistical heterogeneity was high for all primary outcomes. Due to the relatively small number of studies and unequal distribution of the co‐variates, formal sub‐group analysis was not undertaken. However, a qualitative examination of the characteristics of the interventions indicated that the studies which reported positive intervention effects did not differ greatly from those that reported no significant differences or negative effects in terms of who provided the intervention, whether it was provided one‐to‐one or to groups or whether it was provided postnatally only or antenatally and postnatally. However, it is worth noting that only nine studies reported a positive effect on at least one breastfeeding outcome and of these seven used the telephone as a mode of support (Cavalcanti et al., 2019; Di Meglio et al., 2010; Hoddinott et al., 2012; Kamau‐Mbuthia et al., 2013; Patel et al., 2018; Simonetti et al., 2012; Tahir & Al‐Sadat, 2013). This may suggest that telephone is a more effective way of providing support, however, results should be interpreted with caution due to the risk of bias in these studies and the lack of formal sub‐group analysis.
The studies that did not use telephone calls used other delivery methods including video conferencing, SMS and/or platforms to facilitate online text‐based interventions. Current evidence for health interventions delivered using these platforms have only shown effectiveness in specific groups of participants, for example, those with stable chronic illnesses (Free et al., 2013; Greenhalgh et al., 2020), and therefore may not be applicable to breastfeeding women. Nevertheless in Seguranyes et al. (2014), 90% of women chose videoconferencing over telephone calls, although only 40% of the intervention group made use of any form of teleconsultation. Over 80% of women who did not use services said they had no reason to do so, which suggests it is not the mode of the delivery that impacted on uptake of the intervention and for those seeking help, videoconferencing was the preferred option.
Four studies measured the secondary outcome of maternal satisfaction, with only one of these reporting significantly higher scores in women receiving remote support (Patel et al., 2018). This could be explained by the fact that, in the three studies where no significant difference was identified, women in the control group were provided either with reactive breastfeeding support (Ericson et al., 2018; Hoddinott et al., 2012) or face‐to‐face support (Seguranyes et al., 2014). Whereas women in the control group in the study by Patel et al. (2018), were not provided breastfeeding support. This may therefore suggest that any form of breastfeeding support is perceived positively by women. This is consistent with findings from an integrative review on telehealth and breastfeeding (Ferraz dos Santos et al., 2020). There was insufficient information to draw conclusions about the other secondary outcomes of perinatal mental health and maternal self‐efficacy as few studies measured these outcomes.
Overall, this review found less evidence of positive intervention effects than existing reviews which considered on support more generally (Haroon et al., 2013; McFadden et al., 2017; McFadden et al., 2019; Olufunlayo et al., 2018; Shakya et al., 2017). Furthermore, reviews that have specifically assessed the effect of telephone in relation to face‐to‐face support via sub‐group analysis have identified that face‐to‐face support appears to be more effective than telephone support alone, although caution of interpretation is advised due to high within‐group heterogeneity (McFadden et al., 2017). Olufunlayo et al. (2018) studied the effectiveness of a range of interventions on exclusive breastfeeding in LMICs and concluded that all were effective except telephone support alone and evidence for this was insufficient.
There are several reasons why this review found less evidence of effectiveness. As noted previously, breastfeeding support interventions tend to be more effective in LMICs (Haroon et al., 2013; Jolly et al., 2012) and where background breastfeeding initiation rates are high (McFadden et al., 2017). However, this review only identified studies in HICs with low background breastfeeding initiation rates. Additionally, there are components of the interventions included in the remote review which may make them less effective. For instance, peer support has been found to be associated with more positive effects (McFadden et al., 2017), however only 6 of the studies included in the meta‐analysis utilised this. Moreover, there was insufficient detail provided to ascertain whether the interventions aligned with the characteristics of successful peer support identified by Trickey et al. (2018). The interventions identified in this review were generally of a lower intensity in terms of numbers of contacts and the web‐based ones required the mother to reactively access it. Previous evidence suggests that generally higher intensity delivered proactively may be more successful (McFadden et al., 2017; Trickey et al., 2018). Moreover, a more nuanced approach whereby a schedule of contacts is agreed between the mother and supporter may better meet the needs of women (Trickey et al., 2018).
Breastfeeding support is complex and there may be important elements that are not easily addressed remotely. In addition to practical and informational elements, support incorporates emotional support and esteem‐building as well as social support, such as signposting women to support groups and helping to build their social networks. Although it is possible to offer emotional support via telephone or using other remote technologies this may be more challenging and may require specific training for supporters (Penny et al., 2018). A recently published study of over 1200 women in the UK reported that 72.6% of women who stopped breastfeeding during Covid‐19 attributed this to a lack of face‐to‐face support, compared to 42.9% of women before Covid‐19 (A. Brown & Shenker, 2021). While previous studies have shown high satisfaction levels with remotely provided support (e.g., voluntary sector breastfeeding helplines; Kam & Haines, 2021; Thomson et al., 2012) these studies were conducted pre Covid‐19 and provided additional support in addition to routine face‐to‐face care. Such helplines helped women feel more confident and reassured. It could therefore be argued that remotely provided support can be a beneficial addition to face‐to‐face care, continuing beyond the early weeks. Similarly, qualitative studies with midwives and women receiving maternity care via videoconferencing, suggested that it was not a replacement for face‐to‐face contact (Lindberg et al., 2009; Penny et al., 2018).
An important consideration is changes in mode of delivery and women and providers’ abilities to use different technologies that occur over time. For instance, most studies included in this review used the telephone. However, later studies used a range of different modalities including video chat, webchat and social media and these tended to be less effective than telephone‐based interventions. Whilst previous studies have suggested that digital approaches may be limited by technical problems and staff capabilities (Penny et al., 2018), more recent research has demonstrated an improvement in the capacity of staff to provide digital support (Fortuna et al., 2020). It is therefore plausible, that remotely provided interventions provided in a post‐Covid context, may be more effectively implemented due to higher skill levels of providers. Such interventions offer greater flexibility for the user, allowing for choice, and individual preference (e.g., a text‐based intervention may be more useful if a mother is caring for a crying infant). Given the increasing range of digital platforms, there is a need for qualitative work to explore women's experiences with them and that could provide more insights into why such interventions succeed or fail.
There is a lack of evidence relating to low‐ and middle‐income countries. No studies from low‐income countries were included in this review and only 6 from middle‐income countries (20% of participants). Most interventions in this review involved the use of a telephone (e.g., calls, texts) or smartphone (e.g., websites, Facebook, apps) and while ownership may be affected by poverty, surveys have shown that phone ownership is relatively high in some low‐income countries, although this varies greatly (Taylor & Silver, 2019). Additionally, there is also inequity in access within high‐income countries, with families on a lower income and those with lower educational attainment less likely to have access to a smartphone and home broadband (Katzow et al., 2020). It may be that the provision of remote support increases accessibility for some mothers (e.g., remote and rural) and can be offered out of regular office hours covering evening, weekends and holidays but some mothers may be excluded by lack of access to technologies or by costs of phone and/or internet access.
Finally, there was a lack of evidence on support for women with preterm infants. As additional considerations are needed for preterm infants, for example kangaroo care (Charpak et al., 2021) responsive versus scheduled feeding (Watson & McGuire, 2016), the use of milk banks (Quigley et al., 2019), use of bottles or cups (Collins et al., 2016), and therefore the evidence from studies with term babies may not be applicable.
4.1. Strengths and limitations of this review
A key strength of this systematic review was that it followed the methodology outlined in the Cochrane Handbook (Higgins et al., 2019) and the GRADE approach was used to help judge the certainty of the evidence (Schünemann et al., 2013). This review had some important limitations. Standard care for those in the control groups was not well‐described or when described it was variable. In many studies face‐to‐face provision was part of standard care and this may not have been possible during lockdowns.
A second limitation of this review is the high drop‐out rate, with 11 studies being rated as high risk of bias and 2 as unclear risk of bias for this domain. In our intention‐to‐treat analysis we assumed all women did not complete follow‐up had stopped breastfeeding. However, this potentially leads to an underestimation of effect size as a sensitivity analysis identified that differences in exclusive breastfeeding at 4–8 weeks and any at 6 months became significant when studies at high or unclear risk of bias in this domain were excluded. A qualitative examination of the studies did not identify any clear differences in attrition rates based on mode of delivery.
Third, a post‐hoc decision was made to include any or exclusive breastfeeding at 3 months as an outcome. This decision was made because several studies otherwise meeting the eligibility criteria only measured breastfeeding rates at this time point. Fourth, statistical heterogeneity was high for all outcomes and is likely a manifestation of heterogeneity in participants and interventions. Fifth, there was some evidence of funnel plot asymmetry, however, due to high levels of heterogeneity we cannot be certain that this was due to publication bias. Finally, only studies published in English were eligible for inclusion. One full‐text paper which may have potentially met the inclusion criteria was excluded for this reason (Araque García et al., 2018), and others may have been excluded at the title and abstract screening stage.
5. CONCLUSION
The findings of this systematic review and meta‐analysis demonstrate that remote interventions can be effective for improving exclusive breastfeeding but only at specific time frames. Remote interventions were effective at increasing exclusive breastfeeding at 3 months but at 4–8 weeks and 6 months they were effective only when studies at high risk of bias were removed in a sensitivity analysis. However, remotely provided breastfeeding support was less likely to be effective for improving any breastfeeding and only reached significance at 3 and 6 months when studies with rates of attrition were excluded. Moreover, the certainty of the evidence was judged to be low or very low due to risk of bias, substantial heterogeneity and imprecision in some outcomes. High levels of attrition were an issue in 11 of 26 studies and when these studies were removed differences in any breastfeeding at 4–8 weeks and 6 months became significant. There was significant heterogeneity in terms of interventions and routine care making comparisons difficult, however, interventions tended to show more positive effects when only limited routine care was provided. Given that the need for breastfeeding support is highlighted in the wider literature, this review suggests that remote provision of breastfeeding support and education should be provided when it is unsafe or not possible to provide face‐to‐face care. Beyond the Covid‐19 pandemic, remote support could be offered as part of a support package that could supplement face‐to‐face provision. This would offer women more flexibility to access help when needed to meet individual needs and changing circumstances. To inform policy and longer‐term provision globally there is a need to further understand the use of contemporary technologies and women's and care providers’ experiences of using these.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
AG, AM, JM and SR designed the research study. All authors were involved in at least one stage of the research process (i.e., study selection, data extraction, risk of bias assessment, meta‐analysis). AG, AM and JM wrote the manuscript. PB and SR helped with re‐drafting the manuscript. All authors have read and approved the final manuscript.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Gavine, A. , Marshall, J. , Buchanan, P. , Cameron, J. , Leger, A. , Ross, S. , Murad, A. , & McFadden, A. (2022). Remote provision of breastfeeding support and education: Systematic review and meta‐analysis. Maternal & Child Nutrition, 18, e13296. 10.1111/mcn.13296
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Abbass‐Dick, J. , & Dennis, C. L. (2018). Maternal and paternal experiences and satisfaction with a co‐parenting breastfeeding support intervention in Canada. Midwifery, 56, 135–141. [DOI] [PubMed] [Google Scholar]
- Abbass‐Dick, J. , Stern, S. B. , Nelson, L. E. , Watson, W. , & Dennis, C. L. (2015). Coparenting breastfeeding support and exclusive breastfeeding: A randomized controlled trial. Pediatrics, 135(1), 102–110. [DOI] [PubMed] [Google Scholar]
- Ahmed, A. H. , Roumani, A. M. , Szucs, K. , Zhang, L. , & King, D. (2016). The effect of interactive web‐based monitoring on breastfeeding exclusivity, intensity, and duration in healthy, term infants after hospital discharge. Journal of ObstetricGynecologic & Neonatal Nursing, 45(2), 143–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alianmoghaddam, N. , Phibbs, S. , & Benn, C. (2018). Reasons for stopping exclusive breastfeeding between three and six months: A qualitative study. Journal of Pediatric Nursing, 39, 37–43. [DOI] [PubMed] [Google Scholar]
- Araque García, J. , García Perea, E. , Pedraz Marcos, A. , & Alba Diego, R. M. (2018). Efectividad de una consulta online de Enfermería en el seguimiento e instauración de la lactancia materna. Nure Investigación, 15(96), 1–9. [Google Scholar]
- Better Breastfeeding . (2018). Cuts to breastfeeding support in England. https://betterbreastfeeding.files.wordpress.com/2018/07/cuts-in-england-20182.pdf
- Bowatte, G. , Tham, R. , Allen, K. , Tan, D. , Lau, M. , Dai, X. , & Lodge, C. (2015). Breastfeeding and childhood acute otitis media: A systematic review and meta‐analysis. Acta Paediatrica, 104, 85–95. [DOI] [PubMed] [Google Scholar]
- Brown, A. , & Shenker, N. (2021). Experiences of breastfeeding during COVID‐19: Lessons for future practical and emotional support. Maternal & Child Nutrition, 17(1), e13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, C. R. L. , Dodds, L. , Legge, A. , Bryanton, J. , & Semenic, S. (2014). Factors influencing the reasons why mothers stop breastfeeding. Canadian Journal of Public Health, 105(3), e179–e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns, E. , & Triandafilidis, Z. (2019). Taking the path of least resistance: A qualitative analysis of return to work or study while breastfeeding. International Breastfeeding Journal, 14(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsen, E. M. , Kyhnaeb, A. , Renault, K. M. , Cortes, D. , Michaelsen, K. F. , & Pryds, O. (2013). Telephone‐based support prolongs breastfeeding duration in obese women: A randomized trial. American Journal of Clinical Nutrition, 98(5), 1226–1232. 10.3945/ajcn.113.059600 [DOI] [PubMed] [Google Scholar]
- Cavalcanti, D. S. , Cabral, C. S. , de Toledo Vianna, R. P. , & Osorio, M. M. (2019). Online participatory intervention to promote and support exclusive breastfeeding: Randomized clinical trial. Maternal & Child Nutrition, 15(3), e12806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charpak, N. , Montealegre‐Pomar, A. , & Bohorquez, A. (2021). Systematic review and meta‐analysis suggest that the duration of Kangaroo mother care has a direct impact on neonatal growth. Acta Paediatrica, 110(1), 45–59. [DOI] [PubMed] [Google Scholar]
- Chowdhury, R. , Sinha, B. , Sankar, M. J. , Taneja, S. , Bhandari, N. , Rollins, N. , Bahl, R. , & Martines, J. (2015). Breastfeeding and maternal health outcomes: A systematic review and meta‐analysis. Acta Paediatrica, 104, 96–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, C. T. , Gillis, J. , McPhee, A. J. , Suganuma, H. , & Makrides, M. (2016). Avoidance of bottles during the establishment of breast feeds in preterm infants. Cochrane Database of Systematic Reviews, 9(9), CD005252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dagla, M. , Mrvoljak‐Theodoropoulou, I. , Karagianni, D. , Dagla, C. , Sotiropoulou, D. , Kontiza, E. , Kavakou, A. T. , & Antoniou, E. (2021). Women's mental health as a factor associated with exclusive breastfeeding and breastfeeding duration: Data from a longitudinal study in Greece. Children, 8(2), 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davanzo, R. , Moro, G. , Sandri, F. , Agosti, M. , Moretti, C. , & Mosca, F. (2020). Breastfeeding and coronavirus disease‐2019: Ad interim indications of the Italian Society of Neonatology endorsed by the Union of European Neonatal & Perinatal Societies. Maternal & Child Nutrition, 16, e13010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davanzo, R. , Romagnoli, C. , & Corsello, G. (2015). Position statement on breastfeeding from the Italian pediatric societies. Italian Journal of Pediatrics, 41(1), 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks, J. J. , Higgins, J. P. T. , & Altman, D. G. (2011). Chapter 9: Analysing data and undertaking meta‐analyses. In Higgins J. P. T., & Green S. (Eds.), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. [Google Scholar]
- Demirci, J. , Glasser, M. , Bogen, D. , & Chang, J. (2019). Design, implementation, and feasibility–acceptability of a text message–based intervention to prevent perceived insufficient milk supply. Paper presented at the AWHONN Convention, Philadelphia, Pennsylvania. https://search.ebscohost.com/login.aspx?direct=true%26AuthType=ip,athens,cookie,url,uid%26db=cin20%26AN=137209854%26site=ehost-live
- Di Meglio, G. , McDermott, M. P. , & Klein, J. D. (2010). A randomized controlled trial of telephone peer support's influence on breastfeeding duration in adolescent mothers. Breastfeeding Medicine, 5(1), 41–47. [DOI] [PubMed] [Google Scholar]
- Edwards, R. (2018). An exploration of maternal satisfaction with breastfeeding as a clinically relevant measure of breastfeeding success. Journal of Human Lactation, 34(1), 93–96. [DOI] [PubMed] [Google Scholar]
- Efrat, M. W. , Esparza, S. , Mendelson, S. G. , & Lane, C. J. (2015). The effect of lactation educators implementing a telephone‐based intervention among low‐income Hispanics: A randomised trial. Health Education Journal, 74(4), 424–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ericson, J. , Eriksson, M. , Hoddinott, P. , Hellström‐Westas, L. , & Flacking, R. (2018). Breastfeeding and risk for ceasing in mothers of preterm infants: Long‐term follow‐up. Maternal & Child Nutrition, 14(4), e12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraz dos Santos, L. , Borges, R. F. , & de Azambuja, D. A. (2020). Telehealth and breastfeeding: An integrative review. Telemedicine and e‐Health, 26(7), 837–846. [DOI] [PubMed] [Google Scholar]
- Forster, D. A. , McLardie‐Hore, F. E. , McLachlan, H. L. , Davey, M. ‐A. , Grimes, H. A. , Dennis, C.‐L. , Mortensen, K. , Moorhead, A. M. , Tawia, S. , Gold, L. , Shafiei, T. , Small, R. , East, C. E. , & Amir, L. H. (2019). Proactive peer (mother‐to‐mother) breastfeeding support by telephone (ringing up about breastfeeding early [RUBY]): A multicentre, unblinded, randomised controlled trial. EClinicalMedicine, 8, 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuna, K. L. , Myers, A. L. , Walsh, D. , Walker, R. , Mois, G. , & Brooks, J. M. (2020). Strategies to increase peer support specialists’ capacity to use digital technology in the era of COVID‐19: Pre‐post study. JMIR Mental Health, 7(7), e20429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free, C. , Phillips, G. , Galli, L. , Watson, L. , Felix, L. , Edwards, P. , Patel, V. , & Haines, A. (2013). The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: A systematic review. PLOS Medicine, 10(1), e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friesen, C. A. , Hormuth, L. J. , Petersen, D. , & Babbitt, T. (2015). Using videoconferencing technology to provide breastfeeding support to low‐income women: Connecting hospital‐based lactation consultants with clients receiving care at a community health center. Journal of Human Lactation, 31(4), 595–599. [DOI] [PubMed] [Google Scholar]
- Fu, I. C. , Fong, D. Y. , Heys, M. , Lee, I. L. , Sham, A. , & Tarrant, M. (2014). Professional breastfeeding support for first‐time mothers: A multicentre cluster randomised controlled trial. BJOG: An International Journal of Obstetrics and Gynaecology, 121(13), 1673–1683. [DOI] [PubMed] [Google Scholar]
- Gonçalves‐Bradley, D. C. , Maria, A. R. J. , Ricci‐Cabello, I. , Villanueva, G. , Fønhus, M. S. , Glenton, C. , & Mehl, G. L. (2020). Mobile technologies to support healthcare provider to healthcare provider communication and management of care. Cochrane Database of Systematic Reviews, 8(8), CD012927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez‐Darias, A. , Diaz‐Gomez, N. M. , Rodriguez‐Martin, S. , Hernandez‐Perez, C. , & Aguirre‐Jaime, A. (2020). 'Supporting a first‐time mother': Assessment of success of a breastfeeding promotion programme. Midwifery, 85, 102687. [DOI] [PubMed] [Google Scholar]
- Greenhalgh, T. , Wherton, J. , Shaw, S. , & Morrison, C. (2020). Video consultations for covid‐19: An opportunity in a crisis. BMJ, 368, m998. [DOI] [PubMed] [Google Scholar]
- Hagi‐Pedersen, M. B. , Norlyk, A. , Dessau, R. , Stanchev, H. , & Kronborg, H. (2017). Multicentre randomised study of the effect and experience of an early inhome programme (PreHomeCare) for preterm infants using video consultation and smartphone applications compared with inhospital consultations: Protocol of the PreHomeCare study. BMJ Open, 7(3), e013024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haroon, S. , Das, J. K. , Salam, R. A. , Imdad, A. , & Bhutta, Z. A. (2013). Breastfeeding promotion interventions and breastfeeding practices: A systematic review. BMC Public Health, 13(3), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Altman, D. G. , & Sterne, J. A. C. (2011). Chapter 8: Assessing risk of bias in included studies. In Higgins J., & Green S. (Eds.), Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration. [Google Scholar]
- Higgins, J. P. T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. J. , & Welch, V. A. (2019). Cochrane handbook for systematic reviews of interventions (2nd ed.). The Cochrane Collaboration. [Google Scholar]
- Hoddinott, P. , Craig, L. , MacLennan, G. , Boyers, D. , & Vale, L. (2012). The FEeding Support Team (FEST) randomised, controlled feasibility trial of proactive and reactive telephone support for breastfeeding women living in disadvantaged areas. BMJ Open, 2(2), e000652. 10.1136/bmjopen-2011-000652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hongo, H. , Green, J. , Shibanuma, A. , Nanishi, K. , & Jimba, M. (2020). The influence of breastfeeding peer support on breastfeeding satisfaction among Japanese mothers: A randomized controlled trial. Journal of Human Lactation, 36(2), 337–347. [DOI] [PubMed] [Google Scholar]
- Horta, B. L. , Loret de Mola, C. , & Victora, C. G. (2015a). Breastfeeding and intelligence: A systematic review and meta‐analysis. Acta Paediatrica, 104, 14–19. [DOI] [PubMed] [Google Scholar]
- Horta, B. L. , Loret de Mola, C. , & Victora, C. G. (2015b). Long‐term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta‐analysis. Acta Paediatrica, 104, 30–37. [DOI] [PubMed] [Google Scholar]
- Horta, B. L. , & Victora, C. G. (2013). Short‐term effects of breastfeeding: A systematic review on the benefits of breastfeeding on diarrhoea and pneumonia mortality (9241506121). Geneva.
- Howell, E. A. , Bodnar‐Deren, S. , Balbierz, A. , Parides, M. , & Bickell, N. (2014). An intervention to extend breastfeeding among black and Latina mothers after delivery. American Journal of Obstetrics and Gynecology, 210(3), 239–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignatowicz, A. , Atherton, H. , Bernstein, C. J. , Bryce, C. , Court, R. , Sturt, J. , & Griffiths, F. (2019). Internet videoconferencing for patient–clinician consultations in long‐term conditions: A review of reviews and applications in line with guidelines and recommendations. Digital Health, 5, 2055207619845831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolly, K. , Ingram, L. , Freemantle, N. , Khan, K. , Chambers, J. , Hamburger, R. , Brown, J. , Dennis, C. L. , & Macarthur, C. (2012). Effect of a peer support service on breast‐feeding continuation in the UK: A randomised controlled trial. Midwifery, 28(6), 740–745. [DOI] [PubMed] [Google Scholar]
- Jolly, K. , Ingram, L. , Khan, K. S. , Deeks, J. J. , Freemantle, N. , & MacArthur, C. (2012). Systematic review of peer support for breastfeeding continuation: Metaregression analysis of the effect of setting, intensity, and timing. BMJ, 344, 8287. [DOI] [PubMed] [Google Scholar]
- Kam, R. L. , & Haines, N. (2021). The Australian Breastfeeding Association's national breastfeeding helpline: A report of the experiences of callers and volunteers in 2019. Breastfeeding Review, 29(1), 15–30. [Google Scholar]
- Kamau‐Mbuthia, E. , Mbugua, S. , Webb Girard, A. , Kalungu, S. , Sarange, C. , Lou, W. , & Sellen, D. (2013). Cell phone based peer counseling to support exclusive breastfeeding is associated with more frequent help and decreased breastfeeding problems: O079. Annals of Nutrition and Metabolism, 63, 196–197. [Google Scholar]
- Kapinos, K. , Kotzias, V. , Bogen, D. , Ray, K. , Demirci, J. , Rigas, M. A. , & Uscher‐Pines, L. (2019). The use of and experiences with telelactation among rural breastfeeding mothers: Secondary analysis of a randomized controlled trial. Journal of Medical Internet Research, 21(9), e13967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzow, M. W. , Steinway, C. , & Jan, S. (2020). Telemedicine and health disparities during COVID‐19. Pediatrics, 146(2), e20201586. [DOI] [PubMed] [Google Scholar]
- Kim, S. K. , Park, S. , Oh, J. , Kim, J. , & Ahn, S. (2018). Interventions promoting exclusive breastfeeding up to six months after birth: A systematic review and meta‐analysis of randomized controlled trials. International Journal of Nursing Studies, 80, 94–105. [DOI] [PubMed] [Google Scholar]
- Lackey, K. A. , Pace, R. M. , Williams, J. E. , Bode, L. , Donovan, S. M. , Järvinen, K. M. , Seppo, A. E. , Raiten, D. J. , Meehan, C. L. , McGuire, M. A. , & McGuire, M. K. (2020). SARS‐CoV‐2 and human milk: What is the evidence? Maternal & Child Nutrition, 16, e13032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewkowitz, A. K. , Lopez, J. D. , Carter, E. B. , Duckham, H. , Strickland, T. , Macones, G. A. , & Cahill, A. G. (2020). Impact of a novel smartphone application on low‐income women's breastfeeding rates: A randomized controlled trial. American Journal of Obstetrics & Gynecology, 222(1), S38–S39. 10.1016/j.ajog.2019.11.061 [DOI] [PubMed] [Google Scholar]
- Lindberg, I. , Christensson, K. , & Öhrling, K. (2009). Parents’ experiences of using videoconferencing as a support in early discharge after childbirth. Midwifery, 25(4), 357–365. [DOI] [PubMed] [Google Scholar]
- Lucas, R. , Zhang, Y. , Walsh, S. J. , Evans, H. , Young, E. , & Starkweather, A. (2019). Efficacy of a breastfeeding pain self‐management intervention: A pilot randomized controlled trial. Nursing Research, 68(2), E1–E10. 10.1097/NNR.0000000000000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez‐Brockman, J. L. , Harari, N. , Segura‐Perez, S. , Goeschel, L. , Bozzi, V. , & Perez‐Escamilla, R. (2018). Impact of the lactation advice through texting can help (LATCH) trial on time to first contact and exclusive breastfeeding among WIC participants. Journal of Nutrition Education & Behavior, 50(1), 33–42. [DOI] [PubMed] [Google Scholar]
- Maslowsky, J. , Frost, S. , Hendrick, C. E. , Trujillo Cruz, F. O. , & Merajver, S. D. (2016). Effects of postpartum mobile phone‐based education on maternal and infant health in Ecuador. International Journal of Gynaecology & Obstetrics, 134(1), 93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAndrew, F. , Thompson, J. , Fellows, L. , Large, A. , Speed, M. , & Renfrew, M. J. (2012). Infant feeding survey 2010. Leeds.
- McFadden, A. , Gavine, A. , Renfrew, M. J. , Wade, A. , Buchanan, P. , Taylor, J. L. , Veitch, E. , Rennie, A. M. , Crowther, S. A. , Neiman, S. , & MacGillivray, S. (2017). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews, 2(2), 001141. 10.1002/14651858.CD001141.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadden, A. , Siebelt, L. , Marshall, J. L. , Gavine, A. , Girard, L.‐C. , Symon, A. , & MacGillivray, S. (2019). Counselling interventions to enable women to initiate and continue breastfeeding: A systematic review and meta‐analysis. International Breastfeeding Journal, 14, 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meedya, S. , Fahy, K. , & Kable, A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women and Birth, 23(4), 135–145. [DOI] [PubMed] [Google Scholar]
- Niela‐Vilen, H. , Axelin, A. , Melender, H. L. , Loyttyniemi, E. , & Salantera, S. (2016). Breastfeeding preterm infants—A randomized controlled trial of the effectiveness of an Internet‐based peer‐support group. Journal of Advanced Nursing, 72(10), 2495–2507. [DOI] [PubMed] [Google Scholar]
- Odendaal, W. A. , Watkins, J. A. , Leon, N. , Goudge, J. , Griffiths, F. , Tomlinson, M. , & Daniels, K. (2020). Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: A qualitative evidence synthesis. Cochrane Database of Systematic Reviews, 3(3), CD011942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olufunlayo, T. F. , Roberts, A. A. , MacArthur, C. , Thomas, N. , Odeyemi, K. A. , Price, M. , & Jolly, K. (2018). Interventions to improve breastfeeding exclusivity in low‐and middle‐income countries: A systematic review and meta‐analysis (August 14, 2018). Available at SSRN: https://ssrn.com/abstract=3234908 or 10.2139/ssrn.3234908 [DOI]
- Page, M. J. , Higgins, J. P. , & Sterne, J. A. (2020). Chapter 13: Assessing risk of bias due to missing results in a synthesis. In Higgins J. P. T., Thomas J., Chandler J., Cumpston M., Li T., Page M. J., & Va W. (Eds.), Cochrane handbook for systematic reviews of intervention (pp. 349–374). Cochrane. [Google Scholar]
- Palacios, C. , Campos, M. , Gibby, C. , Melendez, M. , Lee, J. E. , & Banna, J. (2018). Effect of a multi‐site trial using short message service (SMS) on infant feeding practices and weight gain in low‐income minorities. Journal of the American College of Nutrition, 37(7), 605–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, A. , Kuhite, P. , Puranik, A. , Khan, S. S. , Borkar, J. , & Dhande, L. (2018). Effectiveness of weekly cell phone counselling calls and daily text messages to improve breastfeeding indicators. BMC Pediatrics, 18(1), 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne, S. , & Quigley, M. A. (2017). Breastfeeding and infant hospitalisation: Analysis of the UK 2010 Infant Feeding Survey. Maternal & Child Nutrition, 13(1), e12263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penny, R. A. , Bradford, N. K. , & Langbecker, D. (2018). Registered nurse and midwife experiences of using videoconferencing in practice: A systematic review of qualitative studies. Journal of Clinical Nursing, 27(5–6), e739–e752. [DOI] [PubMed] [Google Scholar]
- Peres, K. G. , Cascaes, A. M. , Nascimento, G. G. , & Victora, C. G. (2015). Effect of breastfeeding on malocclusions: A systematic review and meta‐analysis. Acta Paediatrica, 104, 54–61. [DOI] [PubMed] [Google Scholar]
- Quigley, M. , Embleton, N. D. , & McGuire, W. (2019). Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database of Systematic Reviews, 7(7), CD002971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RCM & RCOG . (2020). Guidance for antenatal and postnatal services in the evolving coronavirus (COVID‐19) pandemic.
- Reeder, J. A. , Joyce, T. , Sibley, K. , Arnold, D. , & Altindag, O. (2014). Telephone peer counseling of breastfeeding among WIC participants: A randomized controlled trial. Pediatrics, 134(3), e700–e709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renfrew, M. J. , Cheyne, H. , Page, L. , Dykes, F. , Downe, S. , Hunter, B. , & Spiby, H. (2020). Optimising mother‐baby contact and infant feeding in a pandemic: Rapid analytic review. Part 1. https://www.rcm.org.uk/media/4096/optimising-infant-feeding-and-contact-rapid-review-19th-may-2020-submitted.pdf
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , Piwoz, E. G. , Richter, L. M. , Victora, C. G. , & Lancet Breastfeeding Series, G. (2016). Why invest, and what it will take to improve breastfeeding practices? The Lancet, 387(10017), 491–504. [DOI] [PubMed] [Google Scholar]
- Sankar, M. J. , Sinha, B. , Chowdhury, R. , Bhandari, N. , Taneja, S. , Martines, J. , & Bahl, R. (2015). Optimal breastfeeding practices and infant and child mortality: A systematic review and meta‐analysis. Acta Paediatrica, 104, 3–13. [DOI] [PubMed] [Google Scholar]
- Schünemann, H. , Brożek, J. , Guyatt, G. , & Oxman, A. (2013). GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. https://gdt.gradepro.org/app/handbook/handbook.html
- Seguranyes, G. , Costa, D. , Fuentelsaz‐Gallego, C. , Beneit, J. V. , Carabantes, D. , Gómez‐Moreno, C. , Pauli, A. , Abella, M. , & Postpartum Telematics Research Group (Grupo de Grupo de Investigación Posparto Telemático . (2014). Efficacy of a videoconferencing intervention compared with standard postnatal care at primary care health centres in Catalonia. Midwifery, 30(6), 764–771. [DOI] [PubMed] [Google Scholar]
- Seuren, L. , Wherton, J. , Cameron, D. , Shaw, S. , & Greenhalgh, T. (2020). Physical examinations via video? Qualitative study of video examinations in heart failure, using conversation analysis. Journal of Medical Internet Research, 22(2), 16694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakya, P. , Kunieda, M. K. , Koyama, M. , Rai, S. S. , Miyaguchi, M. , Dhakal, S. , Sandy, S. , Sunguya, B. F. , & Jimba, M. (2017). Effectiveness of community‐based peer support for mothers to improve their breastfeeding practices: A systematic review and meta‐analysis. PLOS One, 12(5), e0177434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonetti, V. , Palma, E. , Giglio, A. , Mohn, A. , & Cicolini, G. (2012). A structured telephonic counselling to promote the exclusive breastfeeding of healthy babies aged zero to six months: A pilot study. International Journal of Nursing Practice, 18(3), 289–294. [DOI] [PubMed] [Google Scholar]
- Sinha, B. , Chowdhury, R. , Sankar, M. J. , Martines, J. , Taneja, S. , Mazumder, S. , Rollins, N. , Bahl, R. , & Bhandari, N. (2015). Interventions to improve breastfeeding outcomes: A systematic review and meta‐analysis. Acta Paediatrica, 104, 114–134. [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. , Sutton, A. J. , Ioannidis, J. P. , Terrin, N. , Jones, D. R. , Lau, J. , Carpenter, J. , Rücker, G. , Harbord, R. M. , Schmid, C. H. , Tetzlaff, J. , Deeks, J. J. , Peters, J. , Macaskill, P. , Schwarzer, G. , Duval, S. , Altman, D. G. , Moher, D. , & Higgins, J. P. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta‐analyses of randomised controlled trials. BMJ, 343, 4002. [DOI] [PubMed] [Google Scholar]
- Tahir, N. M. , & Al‐Sadat, N. (2013). Does telephone lactation counselling improve breastfeeding practices? A randomised controlled trial. International Journal of Nursing Studies, 50(1), 16–25. [DOI] [PubMed] [Google Scholar]
- Taylor, K. , & Silver, L. (2019). Smartphone ownership is growing rapidly around the World, but not always equally. https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/
- Tham, R. , Bowatte, G. , Dharmage, S. C. , Tan, D. J. , Lau, M. X. , Dai, X. , Allen, K. J. , & Lodge, C. J. (2015). Breastfeeding and the risk of dental caries: A systematic review and meta‐analysis. Acta Paediatrica, 104, 62–84. [DOI] [PubMed] [Google Scholar]
- Thomson, G. , Crossland, N. , Dykes, F. , & Sutton, C. J. (2012). UK Breastfeeding Helpline support: An investigation of influences upon satisfaction. BMC Pregnancy and Childbirth, 12(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trickey, H. , Thomson, G. , Grant, A. , Sanders, J. , Mann, M. , Murphy, S. , & Paranjothy, S. (2018). A realist review of one‐to‐one breastfeeding peer support experiments conducted in developed country settings. Maternal & Child Nutrition, 14(1), e12559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger, J. A. , Ronen, K. , Perrier, T. , DeRenzi, B. , Slyker, J. , Drake, A. L. , Mogaka, D. , Kinuthia, J. , & John‐Stewart, G. (2018). Short message service communication improves exclusive breastfeeding and early postpartum contraception in a low‐ to middle‐income country setting: A randomised trial. BJOG, 125(12), 1620–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uscher‐Pines, L. , Ghosh‐Dastidar, B. , Bogen, D. L. , Ray, K. N. , Demirci, J. R. , Mehrotra, A. , & Kapinos, K. A. (2019). Feasibility and effectiveness of telelactation among rural breastfeeding women. Academic Pediatrics, 16, 16–659. [DOI] [PubMed] [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. , França, G. V. , Horton, S. , Krasevec, J. , Murch, S. , Sankar, M. J. , Walker, N. , Rollins, N. C. , & Lancet Breastfeeding Series Group . (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. [DOI] [PubMed] [Google Scholar]
- Watson, J. , & McGuire, W. (2016). Responsive versus scheduled feeding for preterm infants. Cochrane Database of Systematic Reviews, 8(8), CD005255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster, P. (2020). Virtual health care in the era of COVID‐19. The Lancet, 395(10231), 1180–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2016). Global diffusion of eHealth: Making universal health coverage achievable. Report of the third global survey on eHealth. WHO.
- WHO . (2020). Breastfeeding and Covid‐19. Scientific Brief. WHO.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


