Abstract
Background
The aim of this study was to analyse changes in influenza detection rates of the influenza seasons 2017/2018, 2018/2019, 2019/2020, and 2020/2021 and the changes in personal awareness of protection during the COVID-19 pandemic.
Methods
This retrospective study included patients tested for influenza virus A and B from November 2017 to March 2021 at the Affiliated People’s Hospital of Ningbo University (Ningbo, China). Influenza virus A and B tested by direct RT-PCR. A small group of 100 regular participants in influenza virus detection were surveyed on the use of protective measures in four different influenza seasons.
Results
There were 14,902, 14,762, 25,070, and 1107 tests of influenza virus A and B in the four influenza periods, for total positive rates of 32.45%, 35.77%, 29.40%, and 0.54%, respectively. In the two periods of four influenza seasons, from November to January, the total number of influenza samples was 8530, 4980, 22,925, 868; from February to March, the number of tests was 6372, 9782, 2145, 239. Total number of tests and positive rate decreased significantly from February/March onwards of the 2019/2020 season, coinciding with the beginning of COVID-19. The proportion of people taking protective measures also increased during the 2019/20 and 2020/21 flu seasons.
Conclusion
The influenza virus has a high incidence in this area. The diagnosis rate of influenza decreased after the start of the COVID-19 pandemic. The COVID-19 pandemic had an important impact on the detection rates for influenza virus.
Keywords: influenza, COVID-19, pandemic
Introduction
Influenza continues to affect millions of individuals of all age groups, with enormous public health and socioeconomic burdens.1,2 Influenza is considered a self-limiting disease, and most adults present with uncomplicated influenza, a mild-to-moderate, self-limited illness with symptoms including high fever, chills, myalgias, and malaise.3 Still, it can cause serious complications (3–5 million people each year) like pneumonia, myositis, myocarditis, and central nervous system diseases. About 500,000 individuals die from influenza each year worldwide.3 Influenza viruses can cause serious health issues in certain populations, such as pregnant women, the elderly, and infants.4 Influenza infection is seasonal in temperate countries, with peaks during the winter months, but has sustained activity throughout the year in tropical climates.5
Supportive care is the mainstay of treatment for most patients. Antiviral treatment is recommended for patients with confirmed or suspected influenza who have severe, complicated, or progressive illness, require hospitalization.6,7 Still, antivirals are expensive, have significant side effects, and are not widely available.6 Vaccination represents the cornerstone public health intervention, most able to reduce the burden of seasonal influenza disease.2,5
In terms of the overall public awareness of COVID-19, the public has paid close attention to the spread of the disease and has a high awareness of it.8 So a lot of behavior has changed significantly during the COVID-19 pandemic.9 The higher the public’s awareness is of infectious diseases, the higher the correctness and timeliness of adopting healthy behaviors.10 Influenza virus epidemics are also a major public event worldwide.
Since the transmission modes of COVID-19 and influenza are similar (physical contact, fomites, droplets, and aerosols), it is unclear that the prevention methods for COVID-19 also impacted the incidence of influenza.11,12
The interesting phenomenon was observed that during the flu season in the past 2 years, the number of influenza cases displayed a significant decline, coinciding with the COVID-19 pandemic. Through extensive publicity by experts and the media, during the COVID-19 pandemic period, ordinary people actively stepped up their personal protection and maintained social distance.
Therefore, this study aimed to analyze the epidemiologic data of the influenza seasons 2017/2018, 2018/2019, 2019/2020, and 2020/2021 and the changes in personal awareness of protection during the COVID-19 pandemic.
Materials and Methods
Study Design and Data
This retrospective study used the patients’ data tested for influenza from November 2017 to March 2021 at the Affiliated People’s Hospital of Ningbo University (Ningbo, China), Grade III, Class A general hospital with more 1054 beds. The inclusion criterion was being tested for influenza virus in the flu season. Patients with repeated tests within two weeks after the diagnosis of influenza were excluded. These patients tested for influenza viruses generally have associated respiratory and febrile symptoms. This study was approved by the Ethics Committee of the Affiliated People’s Hospital of Ningbo University (Scientific Research No. 2021-025).
Data Collection
The data of the patients with influenza (including influenza A and B) for the 2017/2018, 2018/2019, 2019/2020, and 2020/2021 influenza seasons were obtained, from our hospital’s electronic medical history system database. Influenza virus detection was performed using a commercial influenza detection test kit (Daan gene, China) based on the real-time PCR method.
As per routine practice, 100 of the same people were randomly selected and asked to answer a short questionnaire about their attitudes towards influenza viruses and influenza vaccination, as well as information on changes in influenza prevention behaviors were collected, such as wearing face masks, keeping a social distance, and avoiding crowded places in four flu seasons. These 100 people are fixed, that is, the 100 people inquired in the four flu seasons are the same from patients tested for influenza. The aim is to understand how these aspects of protection awareness change in the population during the COVID-19 pandemic.
Definition
The influenza season was from November to March. COVID-19 was taken seriously and became popular in late January and early February 2020. Therefore, the non-epidemic period of COVID-19 was defined as before February 2020. The prevalence period of COVID-19 was defined as after February 2020 based on the epidemic time of COVID-19 in the region. In order to investigate the possible impact of the changes in individual awareness on the outcomes during the epidemics and non-epidemics periods of COVID-19, the influenza season was divided into two periods: the first was November to January, and the second was February to March.
Statistical Analysis
Statistical analyses were done using SPSS 17.0 (IBM, Armonk, NY, USA). Continuous variables with a normal distribution were presented as means ± standard (SD) and analyzed by the t-test between groups. For not normally distributed variables, the data were expressed as median (interquartile range, IQR), and non-parametric tests were used. Categorical variables were expressed as number (%) and compared between groups by the Chi-square test of independence. P-values <0.05 were recognized as statistically significant.
Results
Characteristics of the Patients
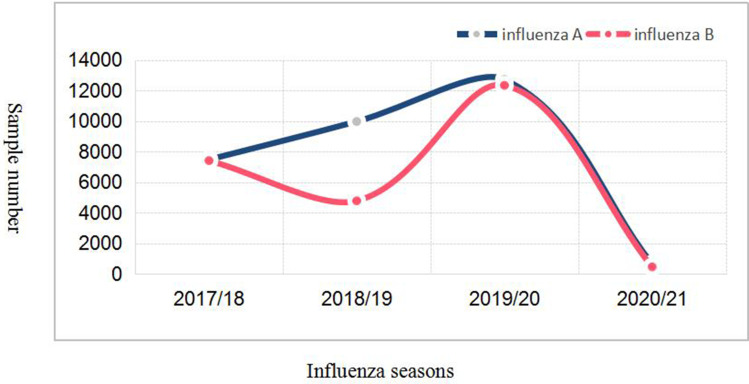
As showed as Table 1, in four different influenza seasons, 14,902, 14,762, 25,070, and 1107 individuals were tested, respectively. The influenza-positive rates were 32.45% in 2017/2018, 35.77% in 2018/2019, 29.40% in 2019/2020, and 0.54% in 2020/2021 (P<0.01). There was no significant difference between the total age group and the number of men and women tested for influenza in each influenza season. More people were tested in 2019/2020 compared with the three other periods, while the smallest number was in 2020/2021 (P<0.01). But from February 2020, there was a sharp drop in the number of tests, from 25,070 in 2019/20 to 1107 in 2020/21 (Figure 1).
Table 1.
Trends in Influenza Virus Testing Across Different Influenza Seasons
| Characteristics | 2017/2018 (n=14,902) | 2018/2019 (n=14,762) | 2019/2020 (n=25,070) | 2020/2021 (n=1107) | P |
|---|---|---|---|---|---|
| Age (years) | 27.1±26.9 | 30.0±25.8 | 22.0±21.3 | 40.0±27.2 | 0.889 |
| ≤16 year | 8038 (53.94%) | 7913 (53.60%) | 15,569 (62.10%) | 325 (29.36%) | <0.01 |
| >16 year | 6864 (46.06%) | 6849 (46.40%) | 9501 (37.90%) | 782 (70.64%) | |
| Sex | 0.991 | ||||
| Male | 7087 (47.56%) | 6942 (47.03%) | 12,312 (49.11%) | 549 (49.59%) | |
| Female | 7815 (52.44%) | 7820 (52.97%) | 12,758 (50.89%) | 558 (50.41%) | |
| Total positive rate | <0.01 | ||||
| Positive | 4836 (32.45%) | 5290 (35.84%) | 7515 (29.98%) | 6 (0.54%) | |
| Negative | 10,066 (67.55%) | 9472 (64.16%) | 17,555 (70.02%) | 1101 (99.46%) | |
| Type of influenza virus | <0.01 | ||||
| A | 7484 | 9977 | 12,729 | 650 | |
| Positive rate | 2630 (35.14%) | 5006 (50.18%) | 4159 (32.67%) | 3 (0.46%) | |
| B | 7418 | 4785 | 12,341 | 457 | |
| Positive rate | 2206 (29.74%) | 274 (5.73%) | 3212 (26.03%) | 3 (0.66%) |
Figure 1.
Influenza virus A and B detected in different influenza seasons.
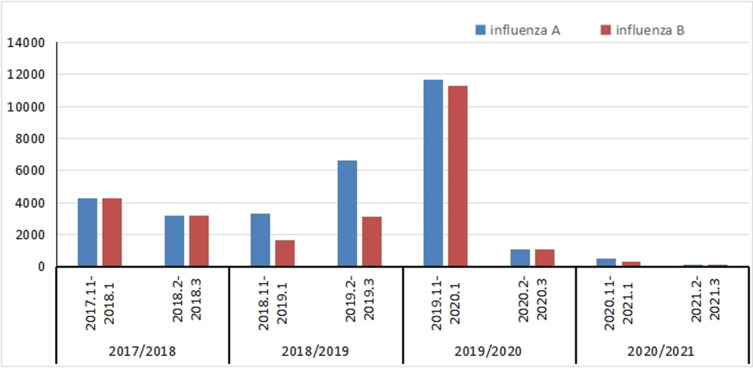
Influenza According to the Two Periods of the Influenza Seasons
In order to better understand the difference in influenza sample data between the epidemic and non-epidemic periods of COVID-19, each influenza season was divided into two periods: November to January and February to March (COVID-19 became widespread at the end of January 2020). Coincident with the beginning of the COVID-19 epidemic, the total number of samples tested of influenza A and B decreased significantly during the same period. The proportion of influenza A samples submitted for testing in the different periods of the 2017/2018 and 2018/2019 seasons was 42.97% (3216/7484) and 66.69% (6654/9977), respectively. Meanwhile, the number of influenza B samples submitted for examination in different periods of the two influenza seasons in 2017/2018 and 2018/2019 accounted for 42.55% (3156/7418) and 65.37% (3128/4785), respectively. However, by the second half of the 2019/2020 flu season, only 8.56% and 8.56% (1089/12,729 and 1056/12,341) of the samples were sent for influenza A and B (Table 2). The number of samples tested increased by nearly 30% during the 2017/2018 and 2018/2019 seasons and the first half of the 2019/2020 season, but the number of samples tested dropped sharply in February-March 2019/2020 (P<0.01), coinciding with the start of COVID-19 (Figure 2).
Table 2.
Numbers of Samples Tested During Different Periods of the Influenza Seasons
| Influenza Type | 2017/2018 | 2018/2019 | 2019/2020 | 2020/2021 | ||||
|---|---|---|---|---|---|---|---|---|
| 2017.11–2018.1 | 2018.2–2018.3 | 2018.11–2019.1 | 2019.2–2019.3 | 2019.11–2020.1 | 2020.2–2020.3 | 2020.11–2021.1 | 2021.2–2021.3 | |
| A | 4268 | 3216(42.97%) | 3323 | 6654(66.69%) | 11,640 | 1089(8.56%) | 526 | 124(19.07%) |
| B | 4262 | 3156(42.55%) | 1657 | 3128(65.37%) | 11,285 | 1056(8.56%) | 342 | 115(25.16%) |
Figure 2.
Influenza virus A and B detected in different periods of the influenza seasons.
Changes in Influenza-Related Behavior
As shown in Table 3, the proportions of individuals washing hands, wearing masks, willing to be vaccinated, and keeping social distance increased in 2019/2020 and 2020/2021 compared with 2017/2018 and 2018/2019 (all P<0.01).
Table 3.
Questionnaire on Protective Measures Taken During the Flu Season
| Question | 2017/2018 | 2018/2019 | 2019/2020 | 2020/2021 | P |
|---|---|---|---|---|---|
| n=100 (%) | |||||
| Do you wash your hands regularly? | 75 | 80 | 91 | 100 | <0.01 |
| Whether to wear a mask during flu season? | 21 | 25 | 85 | 98 | <0.01 |
| Willingness to get flu vaccine? | 3 | 5 | 10 | 20 | <0.01 |
| Maintain social distancing during flu season? | 65 | 68 | 80 | 100 | <0.01 |
Note: Data is displayed as count (percentage).
Discussion
This study analyzed the epidemiologic data of the influenza seasons 2017/2018, 2018/2019, 2019/2020, and 2020/2021 and the changes in personal awareness of protection during the COVID-19 pandemic. The results suggest that the diagnosis rate of influenza decreased after the start of the COVID-19 pandemic.
In the present study, a sharp decrease in influenza tests and positivity was observed starting in February 2020, coinciding with the enforcement of sanitary measures in China. Only a small number of individuals were tested in 2020/2021, the specific reason for this may that people’s awareness of dense gatherings has increased due to the COVID-19 pandemic, reducing the spread of influenza to each other. But further research is needed.
Other papers also have showed similar results: Stamm et al showed that not only reduced respiratory syncytial virus cases, but also decreased influenza samples.13 The rate of influenza-positive tests also sharply decreased. Such a decrease was observed in other countries.14–16 Of course, there is a similar reduction trends founded in China.17
Before the COVID-19 epidemic, like everywhere else in the world, Chinese individuals did not take or strengthen certain protective measures during the influenza season. On the other hand, because of COVID-19ʹs highly infectious nature and high fatality rate,18 the government and medical experts urged the populations to take strict precautions, such as wearing a mask, maintaining a social distance, and avoiding crowded places.15,19 Many people were concerned about flu during the COVID-19 epidemic because of the greater difficulty in seeing a physician, the fear of going to the hospital, and the fear of displaying symptoms that might be misconstrued for COVID-19 symptoms.
An international public health crisis such as the COVID-19 pandemic tests a nation’s governance ability to deal with such crises. Public health governance involves many individuals and institutions that sometimes overlap and are redundant, sometimes leaving some governance areas less well covered. The effectiveness of public health governance is determined by its response to a stimulus. A study in China suggested that government should disclose and share information to the public timely and pay more attention to the core value of order in crisis management.20 Such measures should improve public adherence to the safety and protection measures and ensure reduced pressure on the healthcare system. Still, the COVID-19 pandemic highlighted the gaps and deficiencies of the emergency healthcare system in China10 and elsewhere in the world,21–23 and governments should improve their capacity to face emergency situations. Encouraging preventive and protection measures is a first step in protecting public health.
This study had several limitations. First, it was a retrospective study and limited to the available data. Only one screening center covering a single city in China was included, limiting the generalizability of the results. Larger-scale studies are necessary. Secondly, the sample size of the questionnaire was only 100, which limited its representativeness to some extent. Of course, in the 2020/21 influenza season, which is different from the past, the majority of adults will be tested, which warrants further discussion.
Conclusions
During the COVID-19 pandemic, the detection rate of influenza virus in my region, as in most parts of the world, declined significantly. The COVID-19 pandemic is affecting all aspects of society, as well as the way some respiratory epidemics spread.
Ethics and Consent
Institutional review board approval was obtained for this study. Patient informed consent was not required by the institutional review board. The medical records of these patients were screened retrospectively. Because this study is only a retrospective analysis of electronic data, the patient’s personal information will not be included in the article. The guidelines according to the Declaration of Helsinki were followed.
Disclosure
All authors declare that they have no competing interests in this work.
References
- 1.Putri W, Muscatelli DJ, Stockwell MS, et al. Economic burden of seasonal influenza in the United States. Vaccine. 2018;36(27):3960–3966. doi: 10.1016/j.vaccine.2018.05.057 [DOI] [PubMed] [Google Scholar]
- 2.Domnich A, Cambiaggi M, Vasco A, et al. Attitudes and beliefs on influenza vaccination during the COVID-19 pandemic: results from a representative Italian survey. Vaccines (Basel). 2020;8(4):711. doi: 10.3390/vaccines8040711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Betancourt-Cravioto M, Falcón-Lezama JA, Saucedo-Martínez R, et al. Public health and economic benefits of influenza vaccination of the population aged 50 to 59 years without risk factors for influenza complications in Mexico: a cross-sectional epidemiological study. Vaccines. 2021;9(3):188. doi: 10.3390/vaccines9030188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yechezkel M, Ndeffo Mbah ML, Yamin D, et al. Optimizing antiviral treatment for seasonal influenza in the USA: a mathematical modeling analysis. BMC Med. 2021;19(1). doi: 10.1186/s12916-021-01926-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices - United States, 2020–21 influenza season. MMWR Recomm Rep. 2020;69(8):1–24. doi: 10.15585/mmwr.rr6908a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin H, Jiang N, Shi WH, et al. Development and effects of influenza antiviral drugs. Molecules. 2021;26(4):810. doi: 10.3390/molecules26040810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Influenza antiviral medications: summary for clinicians. Atlanta: Centers for Disease Control and Prevention; 2021. Available from: https://www-cdc-gov.acces.bibl.ulaval.ca/flu/professionals/antivirals/summary-clinicians.htm. Accessed August 10, 2021. [Google Scholar]
- 8.Sun ZG, Yang BQ, Zhang RL, et al. Influencing factors of understanding COVID-19 risks and coping behaviors among the elderly population. Int J Environ Res Public Health. 2020;17(16):5889. doi: 10.3390/ijerph17165889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xing CH, Zhang RL. COVID-19 in China: responses, challenges and implications for the health system. Healthcare (Basel). 2021;9(1):82. doi: 10.3390/healthcare9010082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qi Y, Chen LH, Zhang L, et al. Study on public cognition, attitude and behavior of COVID-19 pneumonia. J Trop Med. 2020;20:145–149. [Google Scholar]
- 11.Leung NHL. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol. 2021;19(8):528–545. doi: 10.1038/s41579-021-00535-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bazant MZ, Bush JWM. A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci U S A. 2021;118(17):e2018995118. doi: 10.1073/pnas.2018995118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stamm P, Sagoschen I, Weise K, et al. Influenza and RSV incidence during COVID-19 pandemic-an observational study from in-hospital point-of care testing. Med Microbiol Immunol. 2021;210(5–6):277–282. doi: 10.1007/s00430-021-00720-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park KY, Seo S, Han J, et al. Respiratory virus surveillance in Canada during the COVID-19 pandemic: an epidemiological analysis of the effectiveness of pandemic-related public health measures in reducing seasonal respiratory viruses test positivity. PLoS One. 2021;16(6):e0253451. doi: 10.1371/journal.pone.0253451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wan WY, Thoon KC, Loo LH, et al. Trends in respiratory virus infections during the COVID-19 pandemic in Singapore, 2020. JAMA Netw Open. 2021;4(6):e2115973. doi: 10.1001/jamanetworkopen.2021.15973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeoh DK, Foley DA, Minney-Smith CA, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72(12):2199–2202. doi: 10.1093/cid/ciaa1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun J, Shi Z, Xu H, et al. Non-pharmaceutical interventions used for COVID-19 had a major impact on reducing influenza in China in 2020. J Travel Med. 2020;27(8):taaa064. doi: 10.1093/jtm/taaa064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang CL, Wang YM, Li XW, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ayouni I, Maatoug J, Dhouib W, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015. doi: 10.1186/s12889-021-11111-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang JR, Zhang RL. COVID-19 in China: power, transparency and governance in public health crisis. Healthcare. 2020;8(3):288. doi: 10.3390/healthcare8030288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faggioni MP, Gonzalez-Melado FJ, Pietro MLD. National health system cuts and triage decisions during the COVID-19 pandemic in Italy and Spain: ethical implications. J Med Ethics. 2021;47:1–8. doi: 10.1136/medethics-2020-107153 [DOI] [PubMed] [Google Scholar]
- 22.Legido-Quigley H, Mateos-Garcia JT, Campos VR, et al. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. 2020;5(5):e251–e252. doi: 10.1016/S2468-2667(20)30060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blumenthal D, Fowler EJ, Abrams M, et al. Covid-19 - implications for the health care system. N Engl J Med. 2020;383(15):1483–1488. doi: 10.1056/NEJMsb2021088 [DOI] [PubMed] [Google Scholar]