ABSTRACT
Purpose
Self-efficacy plays a role in the process of making lifestyle changes. After bariatric surgery, patients must adapt to several lifelong lifestyle changes. The aim of this study was to explore patients’ experiences of recovery after bariatric surgery in those reporting low preoperative self-efficacy.
Methods
This qualitative inductive interview study included 18 participants. Individual interviews were conducted approximately one year after the surgery. Data were analysed using thematic analysis.
Results
The analysis identified one theme, and five subthemes describing recovery after bariatric surgery. Participants described being at a crossroads before surgery and having to make a change. After surgery, they had to learn to handle their new situation, which included getting to know their new body, handling thoughts about themselves, and managing social relations. To enhance their situation, support and information were essential. Social relations, support, successes, and challenges influenced their self-efficacy, and thoughts about adopting lifestyle changes, maintaining motivation, and handling setbacks.
Conclusions
Recovery one year after bariatric surgery is an ongoing process that involves challenges encountered in lifestyle changes and physical and psychological transformations. Self-efficacy is not static and is influenced during the recovery process. Support and information are essential to enhance patient recovery after bariatric surgery.
KEYWORDS: Bariatric surgery, qualitative study, recovery, self-efficacy
Introduction
Obesity is an increasing global health issue, having nearly tripled globally over the last four decades (World Health Organization, 2021). Obesity is associated with health problems such as cardiovascular diseases, diabetes, and higher mortality (Global Burden of Disease (GBD) 2015 Obesity Collaborators 2017). Bariatric surgery is currently the treatment offering the best chance of significant long-term weight loss (Puzziferri et al., 2014; Sjöström et al., 2009), decreased metabolic comorbidities (Colquitt et al., 2014; Sjöström, 2013), and decreased overall mortality (Sjöström et al., 2007). After surgery, patients must commit and adapt to several lifelong lifestyle changes such as learning new eating habits and increasing physical activity (Mechanick et al., 2013). Patients who adopt new eating habits and make multiple changes in behaviours are more successful in their weight loss three years after surgery (Mitchell et al., 2016).
Lifestyle changes are central factors after bariatric surgery. Self-efficacy plays a role in the process of making lifestyle changes, starting from considering adopting a new behaviour to handling setbacks and maintaining motivation to continue with the new behaviour over time. Self-efficacy is described as a person’s beliefs in her/his capacity to organize and execute actions to achieve certain goals (Bandura, 1997). Self-efficacy increases after bariatric surgery and weight loss (Batsis et al., 2009; Nickel et al., 2017). Success in maintaining weight loss further increased patients’ confidence in their ability to maintain healthy lifestyle changes (Liebl et al., 2016).
Self-efficacy can be measured relative to specific tasks and domains or as a general construct. General self-efficacy considers self-efficacy in the broader context of a person’s coping, beliefs, and behaviours in multiple situations (Scholz et al., 2002). General self-efficacy correlates positively with body image (Nickel et al., 2017) and negatively with weight bias internalization in persons undergoing bariatric surgery (Hübner et al., 2015). General self-efficacy also correlates with self-regulation, i.e., a person’s ability to set goals and work towards attaining them (Luszczynska et al., 2005). Patient experiences after bariatric surgery have been described in several studies (Coulman et al., 2017), but we lack knowledge of how people with low self-efficacy experience their recovery after bariatric surgery. The aim of this study is to explore patient experiences of recovery after bariatric surgery in those reporting low preoperative self-efficacy.
Methods
This qualitative inductive interview study is part of a mixed-methods study in which the qualitative study is embedded (Creswell & Plano Clark, 2011) in a prospective longitudinal multicenter trial, whose study protocol has been described in detail by Jaensson et al. (Jaensson, Dahlberg, Nilsson et al., 2019).
Setting and participants
The interviews were conducted approximately one year after the surgery, between December 2019 and November 2020. Inclusion criteria were adults (≥18 years old) scheduled for primary bariatric surgery who understood written and spoken Swedish (Jaensson, Dahlberg, Nilsson et al., 2019). Participants were eligible for this study if reporting a general self-efficacy scale (GSE) score of 27 or below, indicating low preoperative self-efficacy, as guided by a previous Norwegian study (Bonsaksen et al., 2013; Schwarzer, 2014). GSE measures general self-efficacy (Schwarzer & Jerusalem 1995); it has been translated into several languages and adapted for several contexts (Scholz et al., 2002) and has recently been found to be valid and reliable in a population undergoing bariatric surgery in Sweden (Dahlberg et al., 2022, submitted manuscript). GSE was self-assessed. All participants were informed of the study by a research nurse or surgeon at the centre where the surgery had been performed. Eligible participants were purposively selected to include a variety of participants in terms of sex and centre. Based on study aim, theoretical background, sample, and data analysis it was estimated that between 15–25 participants would be sufficient (Braun & Clarke, 2013; Malterud et al., 2016). Forty-two were contacted about the study. Twenty persons agreed to participate. The first or second author contacted eligible participants by phone to provide more information, and schedule interview times. Two declined to participate when they were informed that the interviews would be conducted by phone or videoconference. In total, 18 participants were interviewed, two men and 16 women from three bariatric centres.
Data collection
Due to the Covid 19-pandemic, which started in the beginning of 2020, most interviews were conducted by telephone or videoconference. Two interviews were conducted face to face, two by videoconference, and 14 by telephone. To ensure dependability, a semi-structured interview guide was used (Table I), followed by probing questions such as “tell me more about … ” The first interview was a pilot interview to test the interview guide. During that interview, three questions were identified as missing and were subsequently added to the interview guide: “What were your thoughts before surgery?”; “How have you experienced the support provided by healthcare?”; and “Did the surgery turn out as you expected?” These questions were addressed during the pilot interview, which was therefore included in the analysis.
Table I.
Interview guide
| What were your thoughts before the surgery? |
| How did you feel after your surgery? |
| What has been hard to handle after the surgery? |
| What has been easy to handle after your surgery? |
| What has affected your ability to handle the time after the surgery? |
| How have you experienced the support provided by healthcare? |
| How have you adapted your life situation after the surgery? |
| Did the surgery turn out as you expected? |
All interviews were conducted by the first or second author and lasted 21–95 minutes (mean 50 minutes) each. The interviews were audio recorded and transcribed verbatim; before analysis, the transcripts were checked against the audio-recording for accuracy. Altogether, the dataset to be analysed consisted of 223 single-spaced pages.
Data analysis
The transcribed interviews were subjected to inductive thematic analysis (Braun & Clarke, 2006) to provide in-depth analyses of patients’ experiences of recovery after bariatric surgery. The first and last authors had no clinical experience working with patients undergoing bariatric surgery, but the second and third authors did. The analysis was performed by the first and last authors who, after closely reading the transcribed interviews, conducted the coding. Both authors coded all interviews. The codes were searched for patterns and were gathered into subthemes and themes. To ensure credibility, this first step was conducted individually, after which the results were discussed by the first and last authors. The second and third authors then read six interviews each and all authors jointly reviewed and refined the themes and subthemes and discussed the interpretation and latent meaning of the findings. Throughout the analysis, the researchers ensured that codes, subthemes, and theme corresponded to the original dataset.
Ethical considerations
This study followed the ethical principles of the 1964 Helsinki Declaration and its later amendments and was approved by the regional ethical review board in Uppsala, Sweden (number 2018/256). All participants received written and oral information about the study and gave their written informed consent at trial inclusion. None of the authors conducting the interviews worked in the included centres at the time of the interviews.
Results
The point of departure for the results is one year after surgery, when participants were looking back on a year of recovery and lifestyle changes after bariatric surgery. The findings gave rise to one overarching theme with five subthemes (Table II).
Table II.
Overview of theme and subthemes
| The endeavour for change: self-efficacy in transition | ||||
|---|---|---|---|---|
| Making a change | A body in transformation | A self-image in transition | Managing social relations and external expectations | A need for individualized information and support |
The endeavour for change: self-efficacy in transition
Participants described being at a crossroads before surgery and having to make a change. There was a definite before and after the surgery, i.e., there was no turning back. After surgery, patients had to get to know their body, manage social relations, and handle their new situation and thoughts about themselves. To improve their situation, support and information were essential. Social relations, support, successes, and challenges (or failures, as some described them) all influenced the participants’ self-efficacy, which in turn influenced their thoughts about adopting lifestyle changes, maintaining motivation, and handling setbacks.
Making a change
Before surgery, the participants had reached a breaking point with poor physical health and poor social functioning. Understanding and preparing for how their life would be affected after surgery was essential for coping and recovery after surgery.
Before deciding to undergo surgery, many had tried everything in their power to lose weight. Their decision-making process had often taken several years: some waited to feel mentally prepared, whereas others waited to feel fully committed and motivated. Fears of letting oneself down or disappointing one’s next of kin (ie. person or group of people you are most closely related to) or healthcare providers also affected the decision making. All described being the one to decide to undergo surgery, although some felt a certain persuasion from their next of kin. For some, this last chance was empowering to them.
Now damn it, I’m going to take this chance, and do everything in my power, I’m not going to mess it up.Like, that was my thought. And that also means that you have … raised those expectations in your head, that now, now it’s like,don’t mess this up now.(Interview no. 1)
The main reason to undergo surgery was to lose weight and regain one’s health and physical ability. Some described wanting to become slim and to look better. Participants prepared themselves before the surgery to cope with the time after surgery. Some prepared themselves by seeking different sources of information (e.g., friends, family, literature, media, social media, and healthcare), including risks of alcohol problems, divorce, and eating disorders. All participants had to commit to preoperative diet instructions, and some found this commitment highly stressful and the diet difficult to adhere to.
During their preparation, participants predicted their capacity to undergo surgery, recovery, possible complications, and lifestyle changes by observing and comparing how others had handled their recovery and lifestyle changes. This comparison presupposed that other people were somewhat representative of the participants in terms of preoperative weight and life situation. Using other people’s experiences could have two effects, engendering a sense of security or creating fear of the surgery and recovery. Participants described a lingering thought that was verbally reinforced by others: “Is it considered cheating to lose weight through surgery?”
A body in transformation
After surgery, participants had to get to know their physical body again. This was a time-consuming process of learning a new way of living. One year after surgery, some felt that the journey had just begun and that they were just getting used to their new habits. Others had reached a point where their new habits were a natural part of everyday life that they no longer had to think about.
Life situation affected the initiation and maintenance of lifestyle changes. Some had a newborn child, suffered from pre-existing mental illness, or experienced other events that caused lifestyle changes to be especially challenging, meaning that they were still struggling with old behaviour patterns one year after surgery. Others who were more mentally and socially prepared prioritized their time and were determined to make the necessary lifestyle changes.
Learning new habits required the participants’ complete attention, particularly concerning food, drinking, and eating: “I think more about food now [than before the surgery]” (Interview no. 1). Some expressed doubt that they would have to change their eating habits and considered to continue eating as before the surgery. The participants described “learning by doing” (i.e., experience-based learning) concerning how the body reacted to different types of food, portion sizes, and the optimal timing of eating. Some always ate too fast or suffered from constant nausea and vomiting. Many described failing to make the expected changes, such as not drinking enough water, not eating enough times per day, and not eating enough protein.
Because you sometimes happily put more on the plate, you think “Yeah, but this doesn’t seem to be too much.” But when you sit down and eat, then it is too much all the same … It’s like eating Christmas dinner [i.e. Swedish julbord], it’s always too much. (Interview no. 5)
The risk of dumping was constantly present and was experienced as frightening. When it happened, the participants often knew what the cause was, but it was challenging to adopt an eating behaviour that minimized the risk of dumping. In other cases, dumping was a part of life that sometimes occurred without any obvious reason.
[It’s] just that I was so scared of dumping. And I think that before you are discharged you should … experience it, when you are still there [i.e., in the hospital], so you don’t feel shocked when you get home. Because I thought that I was going to die when I first experienced it. (Interview no. 3)
It was a pleasant surprise that it was so easy to lose weight after surgery—this was a new experience for many. Weight loss also resulted in excess skin, which participants found embarrassing, and for some causing constant thoughts about corrective surgery. As the participants lost weight, they gained physical capacity, experiencing new energy and capacity for exercise. Physical improvements occurred in terms of lower blood pressure and reduced or eliminated need for blood-pressure or diabetes medications. Normal breathing and improved sleep quality were both pleasant health effects that participants experienced. Participants described this as feeling healthier and getting a new life, saying that this was the best thing that had happened to them. Some described the transformation as one of regaining independence, which was a big step for those who had been desiring greater autonomy.
I weighed 160 kilos when I started and it was a struggle to shower, it was a struggle to dry myself off, everything was a struggle—you sort of hesitated. And just to be able to shower without it being a problem and to put on my socks, cut my toenails—those important little things that all of a sudden I just was able to do … the joy in that is incredible. (Interview no. 2)
Reduced body weight led to a need for smaller-sized clothes. It was considered both fantastic and challenging to have new opportunities to buy clothes. The participants could now enjoy shopping, from a much larger variety of clothes, which was a new experience. It was financially challenging, and some could not afford new clothes to keep up with their weight loss. One solution was to alter clothes so that they could last through several changes in size.
A self-image in transition
Some participants described feeling more confident and developing a stronger sense of self-worth; others said that old habits of negative thoughts about the self were difficult to change.
Participants expressed their weight loss as finally transitioning them to being what they perceived as a “normal person” who have value in society, in contrast to the experiences many had before weight loss. The ability to cope with surgery and weight loss engendered new feelings of mental strength: the participants now knew what they wanted in life and could prioritize themselves and stand up for their opinions and rights.
The weight loss slowly changed the participants’ self-image. Feeling attractive meant being able to look at oneself in a mirror or being perceived as attractive by others. It made them less dismissive of their partners and more willing to receive compliments, be photographed, and wear swimwear.
You go past a shop window and you can look a bit closer because you feel pretty and have permission to feel pretty … Or to start believing what people say … because, of course, you also heard it before [the surgery] when you put on a pretty dress and went to a party and people said, “Oh, you look pretty,” and you hear it but it fades just as fast because, “No I’m not pretty, there is nothing pretty about me. The dress is pretty, so I sort of understand that you’re giving a compliment to the dress, but not to me. But to begin to believe them … it’s incredibly fun and nice. (Interview no. 2)
Altogether this resulted in feeling happier, laughing more, and feeling less worried, all of which improved the quality of life. The regained energy and improved self-image resulted in a desire to socialize with friends and family, in feeling more open to spontaneous activities and social events.
Despite weight loss, some participants described ongoing feelings of stigma and an inability to acknowledge that they had lost weight: they still considered themselves overweight and acted as if they were overweight. Some described a lingering shame at excess skin.
that It’s a bit like … in my head … that when I lost weight I would be super skinny right away, and all the skin would be gone. And now I sit here and see that I have gotten—I know deep down inside that it is excess skin, but I don’t see it as excess skin, I see it as fat, sort of. I continue to drop weight, even though it would stabilize if I held back a little, because I think it is fat and not excess skin that I have. My belly is not flat like I have dreamt of, dreamt of since … well, many, many years ago. (Interview no. 10)
For others there was shame at not being able to lose weight and a feeling of failure. Living with the fear of failing to lose weight or maintain one’s weight loss was a constant: “Who will I be, a success or a failure?” This fear and stress made the participants preoccupied with their weight, and some weighed themselves both morning and evening. Some seemed to undertake extreme training for hours; for others, the opposite occurred, and the fear and stress made them eat too much, too fast or make unhealthy food choices.
Oh God, nothing is happening, no, oh God, it’s been two weeks and … I have only lost one kilo. No, it [i.e., the surgery] is surely a failure.” You know, these thoughts haunted me again and again—“Oh, I’ve undergone this surgery and nothing is happening.” (Interview no. 14)
Managing social relations and external expectations
Participants had to adapt to a new social situation regardless of whether the outcome of the surgery was “successful”, and they had lost weight, or “unsuccessful” and they were struggling to lose weight. They felt that they were constantly being judged, receiving both positive and negative comments from others during their recovery.
It was considered important to be transparent with others about their situation, what it meant, and how it affected their life. This gave a better understanding of their situation when they were eating less or experiencing dumping during social events.
Many participants found that others were impressed and curious, gave compliments, and wanted to know what they had done to be so successful at losing weight. Some had changed their appearance so much that they were not recognized. A challenging, puzzling experience was that they were treated differently by others. After their weight loss, the participants felt that they got more positive attention, were noticed more by the opposite sex, got better service, were treated more nicely by others, and had an advantage in discussion with others—all new experiences to them.
All the comments about the amount (i.e., how little) or type of food the participants were eating, or that they had gotten too thin and wrinkled, could also be overwhelming. Those who struggled to lose weight also had to respond to questions about their actual weight and whether the surgery was a failure.
Working life was a challenge because individualized breaks were not always possible. Eating slowly and at specific times was almost impossible during short, prescheduled breaks. These breaks were not as often as required, and it was impossible to eat a whole meal in the break. Sometimes the participants ate too fast, leading to abdominal pain or dumping. On the other hand, if they ate too little, they got tired and unfocused and might experience abdominal pain.
But I try to … when I eat I try to eat slowly, but it is impossible at work now, we have such a short lunch break. (Interview no. 5)
A need for individualized information and support
Receiving sufficient and understandable information and social support was described as essential for coping with their new situation.
For some, information given during patient education sessions was difficult to understand. Identified information barriers were the lack of plain language in written and spoken information, also the content was presented on group level which made it challenging for participants to transfer the information to their own situations. Feelings of anxiety or difficulty concentrating during patient education were personal barriers. Bringing next of kin to patient education was described as support, helping the participants recall and understand information.
No, but I think that, well maybe you should get better information—you do get good information, but … you don’t know what all the words mean … No, that’s why I bring my husband to the hospital and so on, because I hear what they’re saying but I don’t always understand the words. (Interview no. 4)
Those who had difficulty understanding the information felt that they were poorly prepared for the recovery and the radical lifestyle changes that the surgery required. They did not know what to expect after surgery and some even regretted undergoing the surgery.
Next of kin provided the participants with emotional support and motivation to continue with their new lifestyle habits. The joy at every achievement and weight loss milestone was shared, and the progress was considered a joint achievement. Next of kin also helped with practical matters such as heavy lifting, encouraging exercising, sewing clothes, cooking healthy food, arranging appropriate portion sizes, and changing eating habits together. Those who did not have any support from next of kin had difficulties understanding and implementing lifestyle changes. They expressed that support from healthcare providers was especially important. Wanting to be involved in group activities, to learn from others about, for example, what to eat, cooking, and exercise, or to get motivation.
Accessible healthcare provided support, helping participants feel safe and manage their situation. Information folders helped them address various obstacles and maintain the required lifestyle changes. Although complications occurred, those who received accessible support could manage their situation and felt that everything would ultimately be resolved.
I think that it has worked out very well. We got very good information after the surgery, about what is recommended and so on … it was very, very good, it really helped me a lot. (Interview no. 9)
Lack of support and negative attitudes were also mentioned. Some were surprised that they did not receive more followup after the surgery: they wanted and expected a holistic approach to their situation, including feedback on how to lose weight and follow recommendations. The participants perceived that it was difficult to contact healthcare providers with questions or concerns. This difficulty contributed to uncertainty and doubt regarding their capacity to cope with the situation, even to feeling that they should not have undergone the surgery.
And I just felt, no but I … I don’t know where to go, I’m not getting the help that I want. Soon I will go to XX [i.e. another hospital to get a second opinion], because I read about a man who had … who worked with this and who wrote an article specifically about … we who go through this gastric bypass and sleeve, that we get sort of sidelined, that we have problems because people in healthcare don’t … really know how to handle it when there are problems, because it is not very common, but it does happen. (Interview no. 15)
Another concern was the transition of followup from the bariatric centre to primary care two years after surgery (this is a common Swedish practice). Participants described a lack of trust in primary healthcare providers, because they had experienced knowledge gaps about bariatric surgery during followup. Some said that they had full responsibility for their continued recovery, that they had to provide reminders about sampling blood and conducting tests. The participants described this as stressful, because they lacked the appropriate knowledge and competence to keep track of the types of followups needed.
Overall, our findings suggest that information and long-term support from both healthcare providers and next of kin are important for recovery, lifestyle changes, and self-efficacy in patients undergoing bariatric surgery (Figure 1).
Figure 1.
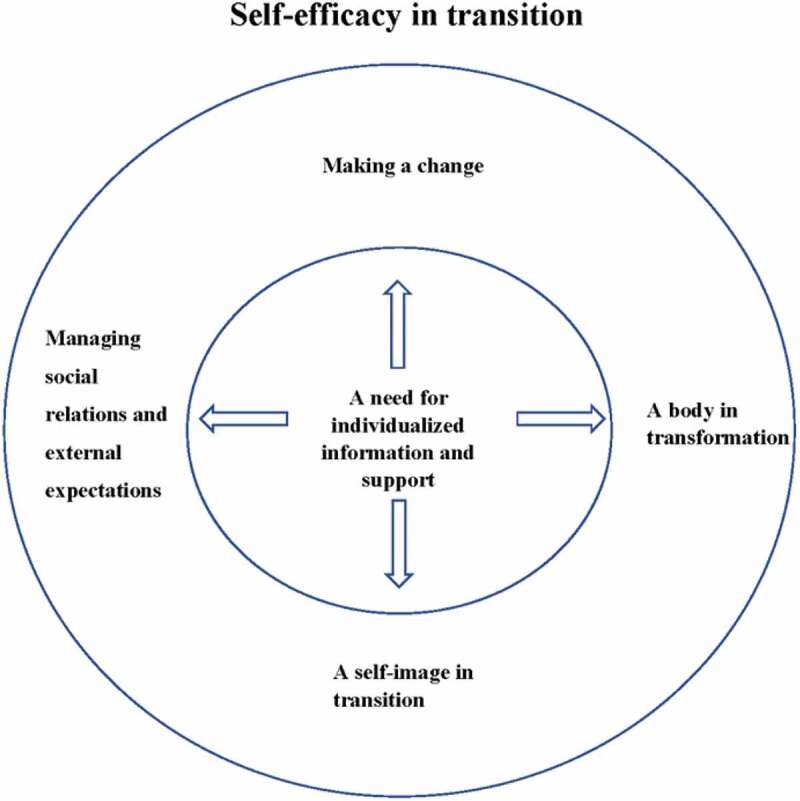
Overview of the theme and subthemes.
Discussion
This study explored experiences of recovery after bariatric surgery in patients reporting low preoperative self-efficacy. Social relations, support, accomplishments, and challenges (or failures, as some described them) all influenced their self-efficacy. Altogether, these factors influenced the participants’ thoughts, lifestyle changes, motivation, and handling of setbacks. Our interpretation of the findings is that most participants experienced a transition in their self-efficacy during recovery and that weight loss was the outcome they regarded as representing success. Those who did not lose weight as expected felt like failures and had difficulties maintaining the required lifestyle changes.
Our results concerning recovery confirm earlier qualitative research (Coulman et al., 2017), although previous research was not conducted from the perspective of low self-efficacy. There are four influential sources of self-efficacy, according to Bandura (1997): enactive mastery experience (i.e., success or failure in performing a task or behaviour), vicarious experience (i.e., judging our own ability by watching others’ performance), verbal persuasion (i.e., others express faith that you can perform a task), and physiological and affective states (i.e., physical status and psychological factors that influence the judging of capabilities; Bandura, 1997). Our interpretation from the interviews were that many described themselves and their postoperative experiences in terms of strengthened self-efficacy, which is important for implementing and maintaining sustainable lifestyle changes. In our findings, we could identify all four of these sources and how they might exert positive influence.
Enactive mastery experience: It was clear that accomplishments and failures (as described by participants) in making lifestyle changes increased or decreased the participants’ self-efficacy. Participants described an experience-based learning process during recovery. When they succeeded in losing weight, eating proper food, and exercising, participants gained confidence, becoming more motivated to maintain the new behaviours.
Vicarious experience: Seeing how others succeeded and failed guided how participants judged their capacity to undergo bariatric surgery. It also guided them after surgery in making lifestyle changes and in responding when they faced challenges.
Verbal persuasion: Participants received persuasive input from society, healthcare providers, and next of kin. This motivated them to undergo surgery and maintain the motivation after surgery. It was also important to receive support and feedback on how they were doing from both next of kin and healthcare providers.
Physical and affective states: The participants’ physical and affective states greatly influenced their self-efficacy. As participants regained energy and strength, they felt stronger and better able to manage various situations, which also affected their mental state and self-image. Feeling that they had support and sufficient information influenced their feelings of security and their ability to handle the situation.
Self-efficacy and its four sources have also been studied in patients undergoing heart transplant surgery in Sweden. Similar to our study, accomplishments and performance were found to be linked to self-efficacy, whereas setbacks and unfulfilled expectations led to less confidence in one’s ability to succeed and therefore to lower self-efficacy; balanced expectations were seen as a way to prevent perceived setbacks (Almgren et al., 2017). Realistic expectations were also mentioned by patients who had undergone bariatric surgery (Coblijn et al., 2018). Patients can find it challenging to balance expectations in the case of bariatric surgery, as the very nature of the surgery leads to the outcome of weight loss. Although a 10% loss of total weight is associated with significant reduction in several risk factors and comorbidities (Aminian et al., 2020), an inability to lose more weight is considered a failure by patients, society, and healthcare providers. It is also a failure that patients have experienced earlier in their lives.
Enactive mastery experience is considered the strongest of the four sources of self-efficacy (Bandura, 1997). Self-efficacy has been found to correlate with postoperative recovery (Magklara et al., 2014) and to increase after bariatric surgery and weight loss (Batsis et al., 2009; Nickel et al., 2017). Success in maintaining weight loss after bariatric surgery increased patients’ confidence in their ability to maintain healthy lifestyle changes (Liebl et al., 2016). The outcome and path of recovery both influence self-efficacy, and measures to strengthen self-efficacy should be addressed by healthcare both before and after surgery.
Almgren et al. described how verbal persuasion often emphasizes adherence to recommendations, whereas it should instead focus on offering support and creating a partnership that helps patients through the emotional transitions involved in recovery after surgery (Almgren et al., 2017). Lifelong support and better followup and support for bariatric patients have been proposed by Coulman et al., to sustain positive changes and postoperative outcomes (Coulman et al., 2017). The participants in our study also mentioned access to healthcare and support as strengthening a sense of security and helping them cope with successes and failures. Support from next of kin, as highlighted here, has been identified as a factor that positively influences the maintenance of weight loss (Liebl et al., 2016).
This study highlights that information is essential for patients undergoing bariatric surgery. Several barriers are described in our results. Insufficient information or an inability to recall information can negatively affect recovery, as reported in research on day surgery and bariatric surgery (Berg et al., 2013; Dahlberg et al., 2018; Jaensson, Dahlberg, Nilsson et al., 2019; Madan & Tichansky, 2005; Wongkietkachorn et al., 2018). Patients have cited the importance of clinicians summarizing and verifying that they have understood the information provided (Coblijn et al., 2018). Other proposed clinical improvements are repetition of information (Madan & Tichansky, 2005), use of multimedia to enhance information presentation after surgery (Ronco et al., 2012), and use of multimedia to increase self-efficacy in patients undergoing hip replacement surgery (Yeh et al., 2005). Another clinical implication is that need-based information has been shown to decrease anxiety and increase satisfaction in patients undergoing day surgery (Wongkietkachorn et al., 2018). In cases of bariatric surgery, individualized patient education has been proposed (Groller, 2017). When investigating patient preferences regarding information one of the most important factors raised was to be considered as an individual person (Coblijn et al., 2018).
Methodological considerations
This study has both strengths and limitations. To ensure dependability a semi-structured interview guide was used and a detailed description of how the interviews were collected and analysed. Interviews were recorded and transcribed verbatim by a professional transcriber to ensure that the informants experiences were captured to ensure confirmability. All transcripts were audio-checked for accuracy. Analyses were conducted individually before a mutual discussion. Further, a strength in this study was the multidisciplinary research team that had different pre-understandings and competences that contributed to exploring different aspects of the analysis. In combination with an ongoing reflective discussion of the analysis until consensus was achieved and ensured credibility.
To ensure confidentiality of the participants, age and date of surgery were not collected. This is a limitation of the study since it affects the transferability of the results. A strength is that participants were included from three centres located in different parts of Sweden. Our study included more women than men. This reflects the studied population, higher proportion of people with obesity are women (Global Burden of Disease (GBD) 2015 Obesity Collaborators 2017) and more women than men undergo bariatric surgery (Stenberg et al., 2019). Moreover, women report lower GSE scores than do men (Bonsaksen et al., 2019; Löve et al., 2012).
Conducting most interviews over telephone or videoconference may be a limitation of the study since it may be more challenging to build personal trust. Also, it affects dependability since data were collected in different ways. Two participants declined to participate when it was decided not to conduct interviews face to face. The interviews that were conducted were rich in their descriptions, which indicates that participants could speak freely about their experiences irrespective if it were conducted over phone or face to face.
Clinical implications
Patients do not seem to be amenable to receiving all relevant information preoperatively, so it is important to repeat information after the surgery, perhaps using different presentation formats, such as multimedia approaches. Taking account of the experiences and opinions of patients who have undergone bariatric surgery when designing pre- and postoperative information presentations may increase the chances of creating useful information accessible to most future patients. The information should preferably be individualized, with support adapted to the individual patient’s situation. A patient’s information needs could be identified during preoperative planning and preparation to assess the patient’s personal situation. How to identify patients who need tailored individualized information and support merits further research, however.
Conclusion
Recovery one year after bariatric surgery in those reporting low preoperative self-efficacy is an ongoing process that involves challenges in making lifestyle changes and in negotiating physical and psychological transformations. Social relations, support, accomplishments, and challenges all influence patient’s self-efficacy. Weight loss was the outcome regarded as representing success. Altogether, these factors influenced the participants’ thoughts, lifestyle changes, motivation, and handling of setbacks. Self-efficacy is not static but is influenced during the recovery process. Support and information are essential in order to enhance patient recovery, lifestyle changes, and self-efficacy.
Biographies
Karuna Dahlberg is a specialist nurse, PhD. She works as an associate senior lecturer at the School of Health Sciences, Örebro University, Sweden. Her research area is in postoperative recovery. It includes research about nurse competence, the concept of postoperative recovery, follow up after surgery as well as how health literacy and self-efficacy can impact recovery after surgery.
Ami Bylund is a registered nurse, PhD. She has a postdoctoral position at the department of learning, informatics, management, and ethics – LIME, Karolinska institutet, Sweden. Her research involves family functioning after obesity surgery and family system nursing. Her present research is part of a research program that study how new models of self-care and co-care are implemented in health care practice and patients’ lives.
Erik Stenberg is a consultant surgeon working at the Department of Surgery at Örebro University Hospital and Lindesberg Hospital, Sweden. He is also appointed associate professor at Örebro University. His research area mainly involves metabolic and bariatric surgery.
Maria Jaensson is a registered nurse anesthetist, PhD, associate professor and excellent teaching practitioner. She works as a senior lecturer at the School of Health Sciences, Örebro University, Sweden. Her research area includes quantitative and qualitative research about postoperative recovery, health literacy and self-efficacy and professional development for nurses.
Funding Statement
This work was supported by Örebro University (grant numbers 2018/00376 and ORU 2018/01219); ALF funding, Region Örebro County (grant numbers OLL-886141, OLL-935386, and OLL-939106); and the Bengt Ihre Foundation.
Notes on contributions
Conception and design: KD, ES, MJ; Data analysis: All authors; Interpretation of data: All authors; Drafting the work and approving the final manuscript: All authors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Almgren, M., Lennerling, A., Lundmark, M., & Forsberg, A. (2017). Self‐efficacy in the context of heart transplantation–a new perspective. Journal of Clinical Nursing, 26(19–20), 3007–10. 10.1111/jocn.13647 [DOI] [PubMed] [Google Scholar]
- Aminian, A., Zajichek, A., Tu, C., Wolski, K. E., Brethauer, S. A., Schauer, P. R., … Nissen, S. E. (2020). How much weight loss is required for cardiovascular benefits? Insights from a metabolic surgery matched-cohort study. Annals of Surgery, 272(4), 639–645. 10.1097/SLA.0000000000004369 [DOI] [PubMed] [Google Scholar]
- Bandura, A. (1997). Self-efficacy The exercise of control. W.H. Freeman and Company. [Google Scholar]
- Batsis, J. A., Clark, M. M., Grothe, K., Lopez-Jimenez, F., Collazo-Clavell, M. L., Somers, V. K., & Sarr, M. G. (2009). Self-efficacy after bariatric surgery for obesity. A population-based cohort study. Appetite, 52(3), 637–645. 10.1016/j.appet.2009.02.017 [DOI] [PubMed] [Google Scholar]
- Berg, K., Årestedt, K., & Kjellgren, K. (2013). Postoperative recovery from the perspective of day surgery patients: A phenomenographic study. International Journal of Nursing Studies, 50(12), 1630–1638. 10.1016/j.ijnurstu.2013.05.002 [DOI] [PubMed] [Google Scholar]
- Bonsaksen, T., Kottorp, A., Gay, C., Fagermoen, M. S., & Lerdal, A. (2013). Rasch analysis of the General self-efficacy scale in a sample of persons with morbid obesity. Health and Quality of Life Outcomes, 11(1), 1–11. 10.1186/1477-7525-11-202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonsaksen, T., Lerdal, A., Heir, T., Ekeberg, Ø., Skogstad, L., Grimholt, T. K., & Schou-Bredal, I. (2019). General self-efficacy in the norwegian population: Differences and similarities between sociodemographic groups. Scandinavian Journal of Public Health, 47(7), 695–704. 10.1177/1403494818756701 [DOI] [PubMed] [Google Scholar]
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Braun, V., & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. SAGE. [Google Scholar]
- Coblijn, U. K., Lagarde, S. M., de Raaff, C. A., van Wagensveld, B. A., & Smets, E. M. (2018). Patients’ preferences for information in bariatric surgery. Surgery for Obesity and Related Diseases, 14(5), 665–673. 10.1016/j.soard.2018.01.029 [DOI] [PubMed] [Google Scholar]
- Colquitt, J. L., Pickett, K., Loveman, E., & Frampton, G. K. (2014). Surgery for weight loss in adults. Cochrane Database of Systematic Reviews(8). 10.1002/14651858.CD003641.pub4. Art. No.: CD003641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulman, K. D., MacKichan, F., Blazeby, J. M., & Owen‐Smith, A. (2017). Patient experiences of outcomes of bariatric surgery: A systematic review and qualitative synthesis. Obesity Reviews, 18(5), 547–559. 10.1111/obr.12518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell, J. W., & Plano Clark, V. L. (2011). Designing and conducting mixed methods research (2. ed.). SAGE Publications. [Google Scholar]
- Dahlberg, K., Jaensson, M., Nilsson, U., Eriksson, M., & Odencrants, S. (2018). Holding it together—patients’ perspectives on postoperative recovery when using an e-assessed follow-up: Qualitative STUDy. JMIR mHealth and uHealth, 6(5), e10387. 10.2196/10387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg, K., Stenberg, E., Liang, Y., Nilsson, U., & Jaensson, M. (2022). The general self-efficacy scale in a population planned for bariatric surgery in Sweden: A prospective psychometric evaluation study. Submitted Manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Burden of Disease (GBD) 2015 Obesity Collaborators . (2017). Global Burden of Disease (GBD) 2015 Obesity Collaborators . Health effects of overweight and obesity in 195 countries over 25 years. New England Journal of Medicine, 377(1), 13–27 doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groller, K. D. (2017). Systematic review of patient education practices in weight loss surgery. Surgery for Obesity and Related Diseases, 13(6), 1072–1085. 10.1016/j.soard.2017.01.008 [DOI] [PubMed] [Google Scholar]
- Hübner, C., Baldofski, S., Zenger, M., Tigges, W., Herbig, B., Jurowich, C., … Hilbert, A. (2015). Influences of general self-efficacy and weight bias internalization on physical activity in bariatric surgery candidates. Surgery for Obesity and Related Diseases, 11(6), 1371–1376. 10.1016/j.soard.2014.11.013 [DOI] [PubMed] [Google Scholar]
- Jaensson, M., Dahlberg, K., & Nilsson, U. (2019). Factors influencing day surgery patients’ quality of postoperative recovery and satisfaction with recovery: A narrative review. Perioperative Medicine, 8(1), 1–7. 10.1186/s13741-019-0115-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaensson, M., Dahlberg, K., Nilsson, U., & Stenberg, E. (2019). The impact of self-efficacy and health literacy on outcome after bariatric surgery in Sweden: A protocol for a prospective, longitudinal mixed-methods study. BMJ Open Science, 9(5), e027272. 10.1136/bmjopen-2018-027272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebl, L., Barnason, S., & Brage Hudson, D. (2016). Awakening: A qualitative study on maintaining weight loss after bariatric surgery. Journal of Clinical Nursing, 25(7–8), 951–961. 10.1111/jocn.13129 [DOI] [PubMed] [Google Scholar]
- Löve, J., Moore, C. D., & Hensing, G. (2012). Validation of the Swedish translation of the general self-efficacy scale. Quality of Life Research, 21(7), 1249–1253. 10.1007/s11136-011-0030-5 [DOI] [PubMed] [Google Scholar]
- Luszczynska, A., Gutiérrez‐Doña, B., & Schwarzer, R. (2005). General self‐efficacy in various domains of human functioning: Evidence from five countries. International Journal of Psychology, 40(2), 80–89. 10.1080/00207590444000041 [DOI] [Google Scholar]
- Madan, A. K., & Tichansky, D. S. (2005). Patients postoperatively forget aspects of preoperative patient education. Obesity Surgery, 15(7), 1066–1069. 10.1381/0960892054621198 [DOI] [PubMed] [Google Scholar]
- Magklara, E., Burton, C. R., & Morrison, V. (2014). Does self-efficacy influence recovery and well-being in osteoarthritis patients undergoing joint replacement? A systematic review. Clinical Rehabilitation, 28 (9), 835–846. http://journals.sagepub.com/doi/pdf/10.1177/0269215514527843. [DOI] [PubMed] [Google Scholar]
- Malterud, K., Siersma, V. D., & Guassora, A. D. (2016). Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research, 26(13), 1753–1760. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- Mechanick, J. I., Youdim, A., Jones, D. B., Garvey, W. T., Hurley, D. L., McMahon, M. M., … Heinberg, L. J., Kushner, R., Adams, T. D., Shikora, S., Dixon, J. B., Brethauer, S. (2013). Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: Cosponsored by American association of clinical endocrinologists, The obesity society, and American society for metabolic & bariatric surgery. Endocrine Practice, 19(2), 337–372 doi: 10.1002/oby.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell, J. E., Christian, N. J., Flum, D. R., Pomp, A., Pories, W. J., Wolfe, B. M., … Belle, S. H. (2016). Postoperative behavioral variables and weight change 3 years after bariatric surgery. JAMA Surgery, 151(8), 752–757. 10.1001/jamasurg.2016.0395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickel, F., Schmidt, L., Bruckner, T., Büchler, M. W., Müller-Stich, B.-P., & Fischer, L. (2017). Influence of bariatric surgery on quality of life, body image, and general self-efficacy within 6 and 24 months—a prospective cohort study. Surgery for Obesity and Related Diseases, 13(2), 313–319. 10.1016/j.soard.2016.08.017 [DOI] [PubMed] [Google Scholar]
- Puzziferri, N., Roshek, T. B., Mayo, H. G., Gallagher, R., Belle, S. H., & Livingston, E. H. (2014). Long-term follow-up after bariatric surgery: A systematic review. JAMA, 312(9), 934–942. 10.1001/jama.2014.10706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronco, M., Iona, L., Fabbro, C., Bulfone, G., & Palese, A. (2012). Patient education outcomes in surgery: A systematic review from 2004 to 2010. International Journal of Evidence-Based Healthcare, 10(4), 309–323. 10.1111/j.1744-1609.2012.00286.x [DOI] [PubMed] [Google Scholar]
- Scholz, U., Doña, B. G., Sud, S., & Schwarzer, R. (2002). Is general self-efficacy a universal construct? Psychometric findings from 25 countries. European Journal of Psychological Assessment, 18(3), 242. 10.1027//1015-5759.18.3.242 [DOI] [Google Scholar]
- Schwarzer, R. (2014). Everything you wanted to know about the general self-efficacy scale but were afraid to ask. Documentation of the General Self-Efficacy Scale, 1–11. http://www.ralfschwarzer.de/
- Schwarzer, R, Jerusalem, M.. (1995).. Generalized Self-Efficacy scale. Weinman, J., Wright, S., Johnston, M.. Measures in health psychology: A users portfolio. Causal and control beliefs. (Windsor, UK: NFER-NELSON; ) [Google Scholar]
- Sjöström, L. (2013). Review of the key results from the Swedish obese subjects (SOS) trial–a prospective controlled intervention study of bariatric surgery. Journal of Internal Medicine, 273(3), 219–234. 10.1111/joim.12012 [DOI] [PubMed] [Google Scholar]
- Sjöström, L., Gummesson, A., Sjöström, C. D., Narbro, K., Peltonen, M., Wedel, H., Dahlgren, S. (2009). Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish obese subjects study): A prospective, controlled intervention trial. The Lancet Oncology, 10(7), 653–662. 10.1016/S1470-2045(09)70159-7 [DOI] [PubMed] [Google Scholar]
- Sjöström, L., Narbro, K., Sjöström, C. D., Karason, K., Larsson, B., Wedel, H., … Carlsson, B. (2007). Effects of bariatric surgery on mortality in Swedish obese subjects. New England Journal of Medicine, 357(8), 741–752. 10.1056/NEJMoa066254 [DOI] [PubMed] [Google Scholar]
- Stenberg, E., Persson, C., Näslund, E., Ottosson, J., Sundbom, M., Szabo, E., & Näslund, I. (2019). The impact of socioeconomic factors on the early postoperative complication rate after laparoscopic gastric bypass surgery: A register-based cohort study. Surgery for Obesity and Related Diseases, 15(4), 575–581. 10.1016/j.soard.2019.01.025 [DOI] [PubMed] [Google Scholar]
- Wongkietkachorn, A., Wongkietkachorn, N., & Rhunsiri, P. (2018). Preoperative needs-based education to reduce anxiety, increase satisfaction, and decrease time spent in day surgery: A randomized controlled trial. World Journal of Surgery, 42(3), 666–674. 10.1007/s00268-017-4207-0 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2021) . Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweightUpdated9th June 2021
- Yeh, M.-L., Chen, -H.-H., & Liu, P.-H. (2005). Effects of multimedia with printed nursing guide in education on self-efficacy and functional activity and hospitalization in patients with hip replacement. Patient Education and Counseling, 57(2), 217–224. 10.1016/j.pec.2004.06.003 [DOI] [PubMed] [Google Scholar]


