Abstract
Alcohol consumption has risen substantially in the United States in the past 2 decades.1,2 Alcohol-associated liver disease (ALD) represents a greater inpatient financial burden than all other etiologies of cirrhosis combined3 and is now the leading indication for liver transplantation.4 A recent study reported that ALD mortality increased between 2006 and 2017.5 Since 2017, alcohol consumption has continued to rise, and more significantly during the COVID-19 pandemic.2 The aim of this research letter is to provide the most updated trends in ALD-related mortality in the United States and to quantify the rate of change of ALD-related mortality over time.
Alcohol consumption has risen substantially in the United States in the past 2 decades.1 , 2 Alcohol-associated liver disease (ALD) represents a greater inpatient financial burden than all other etiologies of cirrhosis combined3 and is now the leading indication for liver transplantation.4 A recent study reported that ALD mortality increased between 2006 and 2017.5 Since 2017, alcohol consumption has continued to rise, and more significantly during the COVID-19 pandemic.2 The aim of this research letter is to provide the most updated trends in ALD-related mortality in the United States and to quantify the rate of change of ALD-related mortality over time.
We extracted data from January 1, 2017, to December 31, 2020, using the Underlying Cause of Death public-use data file from the Centers for Disease Control and Prevention National Center for Health Statistics. This dataset contains mortality data on all US residents. We examined age-adjusted mortality rates per 100,000 (ages 25 years and older) to update previously published data,5 and defined death caused by ALD as the presence of an International Classification of Disease-10 code for ALD (K70) listed as the underlying cause of death on death certificates.5 We report annual age-adjusted mortality rates stratified by sex and race/ethnicity and provide age-specific mortality rates stratified by sex. We further performed a change-point linear regression analysis of crude monthly mortality using the National Cancer Institute’s Joinpoint Regression Program version 4.9.0.0.6 Only crude mortality counts were available on a monthly basis, so we did not use mortality rates in our Joinpoint analysis. From this analysis, we report average monthly percent change in crude mortality from January 1, 2017, through December 31, 2020, estimated months at which any potential change-points occurred, and associated monthly percent change of relevant time subperiods, again stratifying by sex, age, and race/ethnicity.
Age-adjusted ALD-related mortality rates per 100,000 increased each year from 2017 through 2020 for both sexes. Rates rose from 13.1 (95% confidence interval [CI], 12.9–13.3) in 2017 to 16.9 (95% CI, 16.7–17.1) in 2020 among males and from 5.6 (95% CI, 5.4–5.7) in 2017 to 7.7 (95% CI, 7.6–7.9) in 2020 among females. The highest age-adjusted rates were found among American-Indians/Alaska Native, Hispanic, and White individuals. Asian men had the highest relative increase in ALD-related mortality, likely caused by low baseline ALD mortality. Full estimates are available in Supplementary Table 1.
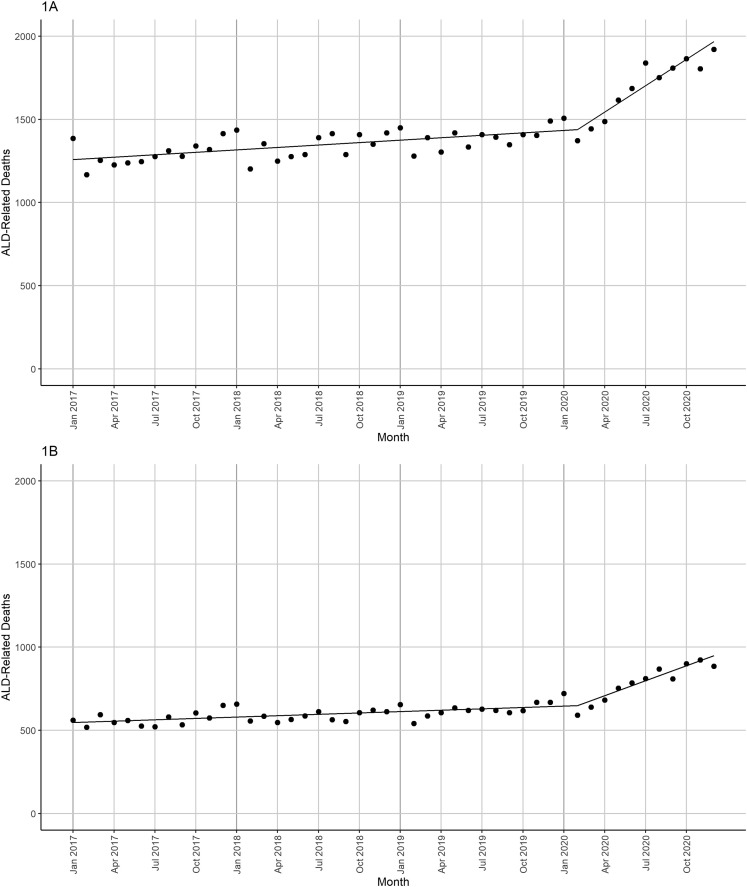
Based on the Joinpoint analysis, we identified strong statistical evidence for a single change-point in February 2020 for both sexes. Among males, the monthly percent change of crude ALD-related mortality counts was 0.36 (95% CI, 0.21–0.51) before February 2020 and 3.18 (95% CI, 2.20–4.17) after February 2020, corresponding to an average monthly percent change from January 2017 through December 2020 of 0.96 (96% CI, 0.73–1.19) (Figure 1 A). Among females, the monthly percent change was 0.46 (95% CI, 0.28–0.64) before February 2020 and 3.8 (95% CI, 2.70–5.07) after February 2020, corresponding to an average of 1.18 (95% CI, 0.90–1.46) from January 2017 through December 2020 (Figure 1 B). Hypothesis tests comparing estimated regression slopes before and after the identified change-points were significant (P < .001 for both sexes). Subgroup analyses suggested significant pre-to-post change-point monthly percent change differences for most subgroups and particularly among young adults. Among males aged 25–34, the average monthly percent changes in crude mortality were 1.29 (95% CI, 0.81–1.78) and 5.37 (95% CI, 3.28–7.50) before and after February 2020, respectively. Among females aged 25–34, the monthly percent changes were 0.92 (95% CI, 0.33–1.51) and 5.12 (95% CI, 1.39–8.98) before and after February 2020. Similar increases in the average monthly percent changes in crude mortality were seen after February 2020 in all age and race/ethnicity subgroups with the exception of males >85 years old. Full estimates are available in Supplementary Table 2.
Figure 1.
Monthly crude ALD-related mortality for January 2017 to December 2020 for (A) males and (B) females. Figures depict crude monthly mortality counts.
Using US mortality data from the Centers for Disease Control and Prevention, we found that mortality from ALD increased in most demographic groups and accelerated during the COVID-19 pandemic. These represent the first population-level data describing trends in mortality from ALD from 2017 to 2020. Females and younger adults experienced the highest relative increase in ALD-related mortality.
One underlying explanation for these trends is the rise in alcohol consumption and alcohol-related complications before and during the pandemic.7 The pandemic may have also compromised appropriate health care for patients with ALD. Other potential contributors include rising obesity/metabolic syndrome and comorbid nonalcoholic fatty liver disease, which can increase risk for the development of ALD.8 Adults ages 85 years and older had smaller total increases in ALD mortality (females) and even decreases (males) over the study period. This trend likely reflects that mortality from other causes becomes more common in this age group, and that adults with higher-risk alcohol consumption may be less likely to live beyond 84 years.
Although the pandemic likely contributed to this trend, our analysis indicates that some increases in ALD mortality, both in rate and absolute count, were seen before the pandemic. Policies to reduce alcohol consumption could include changes in taxation, which have been successful in reducing alcohol consumption in other countries.9 Screening for high-risk alcohol use could be improved. Although recommended by the US Preventive Services Task Force, validated screening tools and referral to evidence-based treatment are underused by primary care physicians.10
Although these national data provide important insight into rising ALD burden, our study has limitations. Estimates of mortality based on death certificates can be inaccurate. Because we used the Primary Underlying Cause of Death database, this data reflects a conservative estimate of ALD-related mortality. Furthermore, we did not have reliable monthly population denominator estimates, thus precluding the use of rate estimates for change-point analyses.
ALD mortality is increasing among males and females in almost every age and racial/ethnic demographic in the United States. These troubling trends call for a nationwide effort to reduce national alcohol consumption, improve alcohol use disorder screening, and optimize early treatment. Other countries have demonstrated success with broad policy change,9 and the United States is in urgent need of analogous efforts to curtail rising ALD disease burden and mortality.
Footnotes
Conflicts of interest These authors disclose the following: Alfred S. Barritt serves as a consultant for TARGET RWE; and has consulted for Pfizer and Novo Nordisk. Andrew M. Moon serves as consultant for TARGET RWE. The remaining authors disclose no conflicts.
Funding Sasha Deutsch-Link was supported in part by National Institutes of Health, United States grant T32 DK007634. Andrew M. Moon was supported by an Advanced/Transplant Hepatology Award (AASLD Foundation), United States.
Note: To access the supplementary material accompanying this article, visit the online version of Clinical Gastroenterology and Hepatology at www.cghjournal.org, and at http://doi.org/10.1016/j.cgh.2022.03.017.
Supplementary Material
Supplementary Table 1.
ALD-Related Mortality Rates Per 100,000, January 2017–December 2020
| 2017 | 2018 | 2019 | 2020 | AAPC 2017–2020 | APC 2019–2020 | |
|---|---|---|---|---|---|---|
| Males overalla | 13.09 (12.88 to 13.30) | 13.47 (13.26 to 13.69) | 13.93 (13.71 to 14.15) | 16.91 (16.67 to 17.15) | 9.23 (9.16 to 9.31) | 21.39 (21.22 to 21.55) |
| 25 to 34 | 2.00 (1.82 to 2.18) | 2.15 (1.96 to 2.34) | 2.47 (2.26 to 2.67) | 3.74 (3.49 to 3.98) | 24.56 (23.5 to 25.8) | 51.54 (49.38 to 54.11) |
| 35 to 44 | 7.05 (6.68 to 7.41) | 7.33 (6.96 to 7.69) | 8.09 (7.70 to 8.48) | 11.69 (11.23 to 12.16) | 19.66 (19.14 to 20.23) | 44.55 (43.42 to 45.81) |
| 45 to 54 | 18.23 (17.76 to 18.81) | 18.08 (17.49 to 18.66) | 18.52 (17.92 to 19.11) | 22.17 (21.52 to 22.82) | 7.11 (7.02 to 7.20) | 19.72 (19.42 to 20.05) |
| 55 to 64 | 28.38 (27.65 to 29.12) | 29.56 (28.81 to 30.30) | 30.11 (29.36 to 30.87) | 34.60 (33.80 to 35.41) | 6.97 (6.88 to 7.07) | 14.91 (14.72 to 15.11) |
| 65 to 74 | 21.63 (20.86 to 22.41) | 22.93 (22.15 to 23.72) | 22.65 (21.88 to 23.42) | 26.54 (25.72 to 27.36) | 7.31 (7.13-7.50) | 17.13 (16.79 to 17.51) |
| 75 to 84 | 13.12 (12.24 to 14.01) | 13.54 (12.66 to 14.42) | 13.76 (12.89 to 14.63) | 14.92 (14.03 to 15.82) | 4.42 (4.16 to 4.71) | 8.45 (8.10 to 8.85) |
| 85+ | 6.98 (5.89 to 8.06) | 6.54 (5.50 to 7.58) | 7.20 (6.12 to 8.27) | 6.34 (5.33 to 7.34) | -2.72 (-2.69 to -2.75) | -11.94 (-11.29 to -12.83) |
| White | 13.19 (12.93 to 13.45) | 13.54 (13.27 to 13.80) | 14.08 (13.81 to 14.53) | 17.36 (17.06 to 17.67) | 9.98 (9.90 to 10.08) | 23.33 (23.12 to 23.54) |
| Black | 8.29 (7.78 to 8.80) | 8.52 (8.01 to 9.03) | 8.73 (8.22 to 9.24) | 10.36 (9.80 to 10.91) | 7.94 (7.68 to 8.24) | 18.60 (18.07 to 19.21) |
| Hispanic | 19.04 (18.30 to 19.78) | 19.19 (18.47 to 19.92) | 20.00 (19.27 to 20.73) | 22.27 (21.53 to 23.02) | 5.45 (5.26 to 5.65) | 11.37 (11.05 to 11.71) |
| American Indian | 34.11 (31.02 to 37.21) | 36.72 (33.46 to 39.99) | 32.81 (29.81 to 35.82) | 45.64 (42.11 to 49.17) | 12.03 (11.43 to 12.74) | 39.09 (37.26 to 41.28) |
| Asian | 3.95 (3.46 to 4.44) | 4.22 (3.72 to 4.72) | 3.96 (3.48 to 4.44) | 5.54 (4.98 to 6.10) | 13.49 (12.55 to 14.69) | 39.76 (37.32 to 42.88) |
| Females overalla | 5.58 (5.44 to 5.72) | 5.76 (5.62 to 5.90) | 6.08 (5.93 to 6.22) | 7.72 (7.56 to 7.88) | 11.92 (11.78 to 12.07) | 27.05 (27.38 to 26.72) |
| 25 to 34 | 1.31 (1.16 to 1.46) | 1.48 (1.32 to 1.64) | 1.60 (1.44 to 1.77) | 2.21 (2.01 to 2.40) | 19.59 (18.58 to 20.85) | 37.55 (35.69 to 39.92) |
| 35 to 44 | 4.05 (3.78 to 4.33) | 4.33 (4.05 to 4.61) | 4.65 (4.36 to 4.95) | 6.84 (6.49 to 7.20) | 20.46 (19.76 to 21.23) | 47.04 (45.47 to 48.80) |
| 45 to 54 | 9.20 (8.79 to 9.61) | 9.03 (8.62 to 9.43) | 9.30 (8.89 to 9.72) | 11.59 (11.12 to 12.06) | 8.59 (8.43 to 8.76) | 24.57 (24.05 to 25.15) |
| 55 to 64 | 10.93 (10.49 to 11.37) | 11.42 (10.97 to 11.86) | 11.99 (11.53 to 12.45) | 14.18 (13.68 to 14.68) | 9.25 (9.07 to 9.45) | 18.28 (17.93 to 18.65) |
| 65 to 74 | 6.16 (5.78 to 6.55) | 6.86 (6.46 to 7.27) | 7.19 (6.78 to 7.59) | 8.61 (8.17 to 9.05) | 11.96 (11.53 to 12.45) | 19.82 (19.15 to 20.53) |
| 75 to 84 | 3.09 (2.71 to 3.46) | 3.12 (2.75 to 3.49) | 3.38 (3.00 to 3.76) | 4.27 (3.85 to 4.69) | 11.93 (11.10 to 12.99) | 26.41 (24.83 to 28.40) |
| 85+ | 1.62 (1.26 to 2.06) | 1.30 (0.98 to 1.70) | 1.21 (0.90 to 1.59) | 1.49 (1.14 to 1.90) | -1.35 (-1.45 to -1.21) | 23.13 (19.74 to 27.06) |
| White | 6.34 (6.15 to 6.52) | 6.60 (6.41 to 6.79) | 6.90 (6.71 to 7.10) | 8.81 (8.59 to 9.03) | 12.11 (11.96 to 12.28) | 27.63 (27.28 to 27.99) |
| Black | 3.74 (3.23 to 4.05) | 3.85 (3.53 to 4.16) | 4.15 (3.82 to 4.47) | 5.14 (4.77 to 5.50) | 11.51 (11.03 to 12.06) | 23.84 (22.93 to 24.94) |
| Hispanic | 4.23 (3.91 to 4.55) | 4.13 (3.82 to 4.45) | 4.39 (4.07 to 4.70) | 5.79 (5.43 to 6.16) | 11.96 (11.43 to 12.56) | 32.11 (30.87 to 33.51) |
| American Indian | 24.48 (21.86 to 27.10) | 25.98 (23.32 to 28.64) | 29.23 (26.40 to 32.05) | 38.21 (34.99 to 41.42) | 16.45 (15.60 to 17.48) | 30.72 (29.23 to 32.54) |
| Asian | 0.84 (0.64 to 1.07) | 1.10 (0.88 to 1.36) | 1.03 (0.82 to 1.28) | 1.17 (0.95 to 1.43) | 12.68 (10.80 to 14.97) | 13.18 (11.30 to 15.38) |
AAPC, average annual percent change; ALD, alcohol-associated liver disease; APC, annual percent change.
Overall mortality rates and race/ethnicity-specific rates reported here have been age-adjusted; age-specific rates reported are crude rates.
Supplementary Table 2.
Monthly Change in Crude ALD-Related Mortality Counts, January 2017–December 2020
| AMPC (All) | AMPC (Pre) | AMPC (Post) | |
|---|---|---|---|
| Males overall | 0.96 (0.73 to 1.19) | 0.36 (0.21 to 0.51) | 3.18 (2.20 to 4.17) |
| 25 to 34 | 2.15 (1.52 to 2.78) | 1.29 (0.81 to 1.78) | 5.37 (3.28 to 7.50) |
| 35 to 44 | 1.79 (1.37 to 2.22) | 1.06 (0.73 to 1.40) | 3.26 (5.84 to 7.25) |
| 45 to 54 | 0.71 (0.32 to 1.10) | -0.03 (-0.27 to 0.21) | 3.50 (1.83 to 5.19) |
| 55 to 64 | 0.78 (0.49 to 1.08) | 0.31 (0.14 to 0.49) | 2.53 (1.29 to 3.80) |
| 65 to 74 | 0.89 (0.60 to 1.17) | 0.55 (0.33 to 0.76) | 2.17 (1.29 to 3.05) |
| 75 to 84 | 0.25 (-0.92 to 1.44) | 0.16 (-1.79 to 2.16) | 0.78 (0.48 to 1.07) |
| 85+ | 0.90 (-2.01 to 3.89) | 1.17 (-2.48 to 4.97) | -0.13 (-0.80 to 0.55) |
| Black | 0.94 (0.47 to 1.41) | 0.24 (-0.07 to 0.54) | 3.58 (1.60 to 5.60) |
| White | 0.84 (0.62 to 1.06) | 0.46 (0.29 to 0.64) | 2.23 (1.60 to 2.86) |
| American Indian | 1.33 (0.47 to 2.19) | 0.30 (-0.28 to 0.88) | 5.23 (1.94 to 8.63) |
| Asian | 1.03 (0.26 to 1.81) | 0.73 (0.06 to 1.40) | 2.17 (0.31 to 4.06) |
| Hispanic | 1.08 (0.66 to 1.51) | 0.44 (0.19 to 0.70) | 3.49 (1.73 to 5.28) |
| Females overall | 1.18 (0.90 to 1.46) | 0.46 (0.28 to 0.64) | 3.88 (2.70 to 5.07) |
| 25 to 34 | 1.80 (0.91 to 2.69) | 0.92 (0.33 to 1.51) | 5.12 (1.39 to 8.98) |
| 35 to 44 | 1.86 (1.32 to 2.40) | 0.91 (0.50 to 1.32) | 5.44 (3.63 to 7.28) |
| 45 to 54 | 0.69 (0.21 to 1.18) | 0.17 (-0.22 to 0.56) | 2.66 (1.27 to 4.07) |
| 55 to 64 | 0.97 (0.62 to 1.33) | 0.42 (0.19 to 0.65) | 3.06 (1.55 to 4.60) |
| 65 to 74 | 1.46 (0.91 to 2.02) | 0.93 (0.63 to 1.23) | 3.47 (1.12 to 5.87) |
| 75 to 84 | 1.01 (0.15 to 1.87) | 0.82 (-0.13 to 1.78) | 1.70 (0.72 to 2.68) |
| 85+ | -0.23 (-2.19 to 1.78) | -0.66 (-2.76 to 1.50) | 1.38 (-1.11 to 3.94) |
| Black | 1.29 (0.63 to 1.95) | 0.62 (0.17 to 1.07) | 3.80 (1.30 to 6.36) |
| White | 0.99 (0.72 to 1.25) | 0.54 (0.33 to 0.75) | 2.65 (1.91 to 3.40) |
| American Indian | 1.89 (1.03 to 2.76) | 0.73 (0.18 to 1.29) | 6.29 (2.70 to 10.02) |
| Asian | 1.62 (-0.83 to 4.13) | 0.63 (-0.42 to 1.70) | 5.37 (-5.27 to 17.21) |
| Hispanic | 1.26 (0.65 to 1.88) | 0.71 (0.20 to 1.21) | 3.35 (1.62 to 5.11) |
NOTE. “All” refers to entire study period; “pre” refers to January 2017 through February 2020; “post” refers to February 2020 through December 2020.
ALD, alcohol-associated liver disease; AMPC, average monthly percent change.
References
- 1.Spillane S., et al. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2019.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pollard M.S., et al. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barritt A.S., et al. Dig Dis Sci. 2019;64:1460–1469. doi: 10.1007/s10620-019-5471-7. [DOI] [PubMed] [Google Scholar]
- 4.Wong R.J., et al. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2019.20294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moon A.M., et al. Am J Gastroenterol. 2020;115:79–87. doi: 10.14309/ajg.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 6.Kim H.J., et al. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 7.Julien J., et al. Hepatology. 2021 Dec 8 doi: 10.1002/hep.32272. [DOI] [Google Scholar]
- 8.Idalsoaga F., et al. Front Med. 2020;7:448. doi: 10.3389/fmed.2020.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson P., et al. Lancet Public Health. 2021;6:e557–e565. doi: 10.1016/S2468-2667(21)00052-9. [DOI] [PubMed] [Google Scholar]
- 10.Friedmann P.D., et al. J Gen Intern Med. 2000;15:84–91. doi: 10.1046/j.1525-1497.2000.03379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]