Abstract
The aim of this study was to explore the overlapping key genes, pathway networks and transcription factors (TFs) related to the pathogenesis of rheumatoid arthritis (RA) and atherosclerosis. The gene expression profiles of RA and atherosclerosis were downloaded from the Gene Expression Omnibus database. Differentially expressed genes (DEGs) between RA and atherosclerosis were identified. The biological roles of common DEGs were explored through enrichment analysis. Hub genes were identified using protein–protein interaction networks. TFs were predicted using Transcriptional Regulatory Relationships Unraveled by Sentence Based Text Mining (TRRUST) database. The hub genes and TFs were validated with other datasets. The networks between TFs and hub genes were constructed by CytoScape software. A total of 131 DEGs (all upregulated) were identified. Functional enrichment analyses indicated that DEGs were mostly enriched in leukocyte migration, neutrophil activation, and phagocytosis. CytoScape demonstrated 12 hub genes and one gene cluster module. Four of the 12 hub genes (CSF1R, CD86, PTPRC, and CD53) were validated by other datasets. TRRUST predicted two TFs, including Spi-1 proto-oncogene (SPI1) and RUNX family transcription factor 1(RUNX1). The expression of RUNX1 was validated with another dataset. Our study explored the common pathogenesis of RA and atherosclerosis. These results may guide future experimental research and clinical transformation.
Subject terms: Rheumatic diseases, Cardiovascular diseases
Introduction
Rheumatoid arthritis (RA), a chronic autoimmune disease of unknown etiology, is characterized by synovitis, pannus formation, and destruction of joints and cartilage. RA-related health complications and long-term comorbidities can markedly decrease life expectancy, and cardiovascular morbidity and mortality are relatively high. Cardiovascular diseases and sudden death are the main reasons of premature mortality in patients with RA1. Approximately 30%–60% increase in risk of cardiovascular events and 50% increase in risk of death due to cardiovascular disease were reported in patients with RA because of accelerated atherosclerosis2.
Evidence supports the hypothesis that the pathology of RA and that of atherosclerosis pathology share many common molecular pathways and exhibit analogous mechanisms3. Atherosclerotic plaque has many similarities to RA synovium, such as recruiting of blood-borne mononuclear cells, upregulation of cytokines, and complex interactions of immune cells with resident cell types3. The common pathophysiological mechanisms may provide insights into the common pathogenesis of RA and atherosclerosis. Therefore, the relationship between these diseases has attracted increasingly interest. Tamami et al. reported RA patients who have visceral adiposity have a specifically high risk for atherosclerosis4. In 2020, a study proposed the use of QRESEARCH risk estimator version 3 and the European League Against Rheumatism mSCORE for identifying patients with RA who are at a high risk of carotid plaques5. In addition, Dessein et al. determined the performance of the Framingham score and the Systematic Coronary Risk Evaluation tool in assessing patients with RA who are at high risk of atherosclerosis6. Furthermore, the development of atherosclerosis in patients with RA seems to be influenced by a genetic component. This topic has been the focus of numerous bioinformatics studies that mostly concentrated on genetic polymorphisms. To be specific, the association of the paraoxonase 1 gene polymorphism with carotid plaques in RA was demonstrated in a series of 168 North American patients 7. Moreover, a Spanish group proved the potential protective effect of the IL33 rs3939286 allele T against the risk of subclinical atherosclerosis in patients with RA. However, a number of studies have also reported negative results on this aspect. One study failed to confirm the association of CRP, HNF1A, LEPR, GCKR, NLRP3, IL1F10, PPP1R3B, ASCL1, HNF4A, and SALL1 with cardiovascular disease in RA8. Another work reported that 15 polymorphisms, including TCF21, LPA, HHIPL1, RASD1-PEMT, MRPS6, CYP17A1-CNNM2-NT5C2, SMG6-SRR, PHACTR1, WDR12, and COL4A1-COL4A2, are not associated with atherosclerosis in RA9. Meanwhile, no relationships among ABO rs579459, PPAP2B rs17114036, ADAMTS7 rs3825807, PIK3CG rs17398575, EDNRA rs1878406, and subclinical atherosclerosis in RA were found10. Therefore, in consideration of previous studies, the molecular mechanism in patients with RA complicated with atherosclerosis is controversial and needs further study.
With the rapid development of microarray techniques, differentially expressed genes (DEGs) among different groups of people can be detected. Microarray techniques can illustrate gene expression and identify special proteins produced by genes11. Therefore, disease-related molecules can be identified by using these tools. Thus, in this study, we aim to explore the potential overlapping key genes, pathway networks, and transcription factors (TFs) related to the pathogenesis of RA and atherosclerosis through a combination of microarray and bioinformatics analyses.
Results
Identification of common DEGs
DEGs were identified after the microarray results were standardized (Supplementary Fig. 1a–d). A total of 2735 DEGs were found in the RA datasets (GSE55235 and GSE55457), and 275 DEGs were found in the atherosclerosis dataset (GSE14905). Supplementary Fig. 1a shows the volcano plot of GSE55235 and GSE55457 (RA). Supplementary Fig. 1b provides the volcano plot of GSE14905 (atherosclerosis). The heatmap of the RA datasets (GSE55235 and GSE55457) is presented in Supplementary Fig. 1c, and the heatmap of the atherosclerosis dataset (GSE14905) is depicted in Supplementary Fig. 1d. A total of 131 common DEGs were found after the integration of the DEGs (Supplementary Fig. 1e).
Protein–protein interaction (PPI) network construction, biological functions analyses, and Molecular Complex Detection (MCODE) cluster modules identification
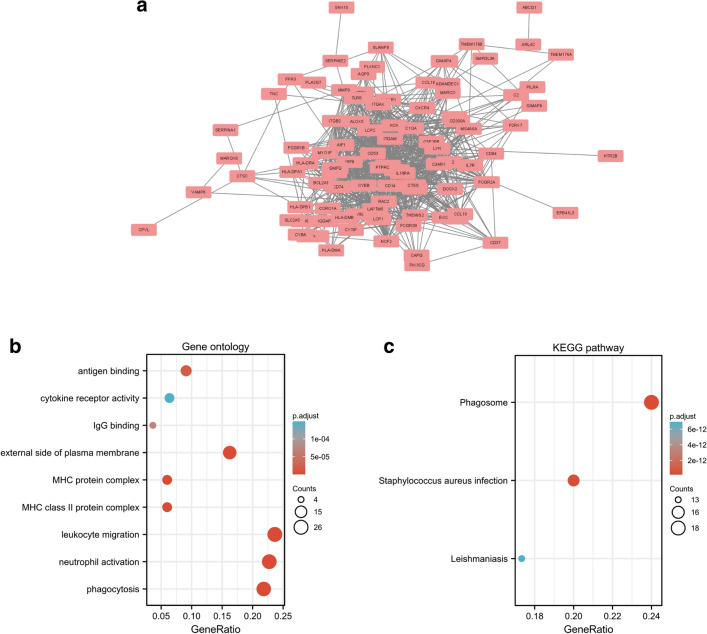
The PPI network for the 131 DEGs was constructed after the common DEGs were imported to STRING (Fig. 1a). Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses were used in analyzing the 131 common DEGs (Fig. 1b,c)12–14. Based on GO enrichment, the biological process acted primarily on phagocytosis, leukocyte migration, and neutrophil activation. These proteins were primarily located in external side of plasma membrane, MHC class II protein complex, and MHC protein complex. With regard to molecular functions, the proteins played roles in antigen binding, IgG binding, and cytokine receptor activity (Fig. 1b). According to KEGG pathway analysis, these proteins were primarily involved in phagosome, staphylococcus aureus infection, and leishmaniasis (Fig. 1c).
Figure 1.
PPI network and functional enrichment of DEGs. (a) The interaction network between proteins coded by DEGs. (b) The enrichment analysis results of GO and (c) KEGG (www.kegg.jp/kegg/kegg1.html) pathway. Adjusted P value < 0.05 was considered significant.
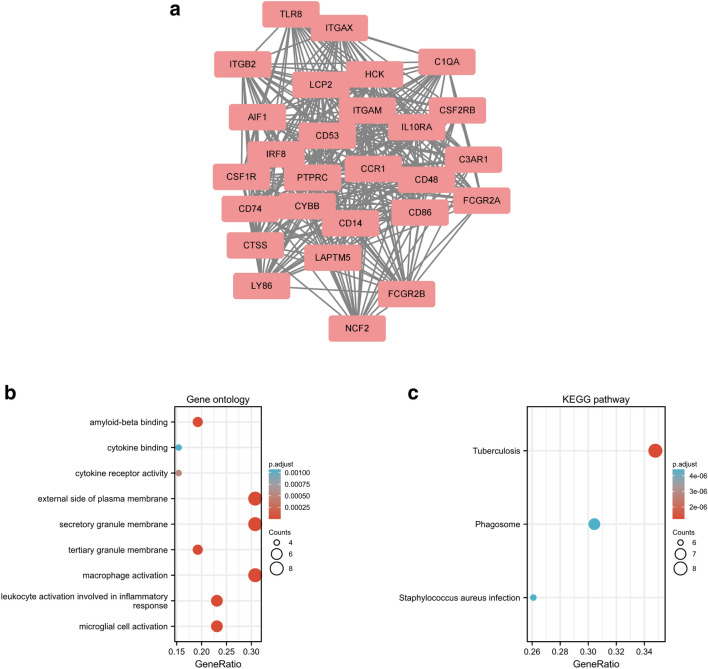
Significant modules of the PPI network were identified by MCODE. MCODE score of 4 was set as a threshold. One module with MCODE score of ≥ 4 is illustrated in Fig. 2a. This cluster (MCODE score = 24.385) had 27 nodes and 317 edges (Fig. 2a). GO analysis showed that the proteins in the cluster were related to macrophage activation, microglial cell activation, and leukocyte activation (Fig. 2b). KEGG pathway analysis showed that these proteins were primarily involved in tuberculosis, phagosome, and staphylococcus aureus infection (Fig. 2c).
Figure 2.
Cluster modules extracted by MCODE and enrichment analysis of the modular genes. (a) One significant gene clustering module. (b) GO and (c) KEGG enrichment analysis of the modular genes. Adjusted P value < 0.05 was considered significant.
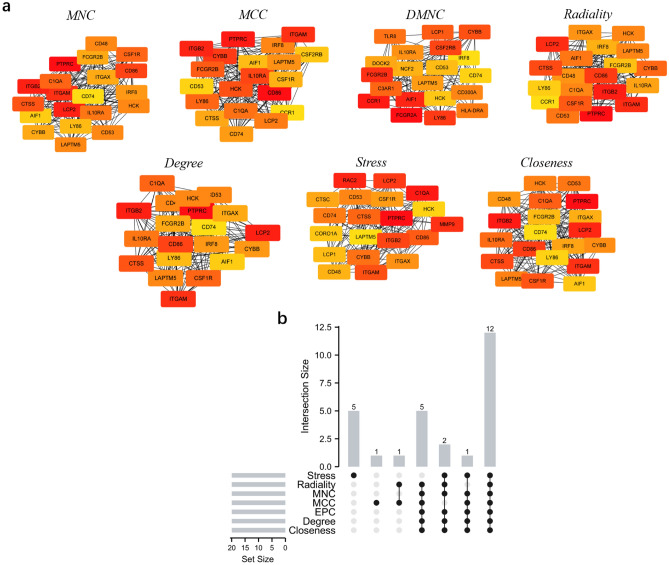
Selection and analysis of hub genes
The top 20 hub genes were calculated using the seven algorithms of the plug-in CytoHubba (Fig. 3a). After the intersection of the UpSet diagram was determined, 12 common hub genes were discovered, namely, cytochrome b-245 beta chain (CYBB), lysosomal protein transmembrane 5 (LAPTM5), colony stimulating factor 1 receptor (CSF1R), Src family tyrosine kinase (HCK), integrin subunit alpha M (ITGAM), CD86 molecule (CD86), complement C1q A chain (C1QA), integrin subunit beta 2 (ITGB2), protein tyrosine phosphatase receptor type C (PTPRC), cathepsin S (CTSS), lymphocyte cytosolic protein 2 (LCP2), and CD53 molecule (CD53; Fig. 3b). Table 1 shows their full names and related functions. GO analysis showed that the genes were mainly involved in amyloid-beta binding, opsonin binding, and complement binding. KEGG pathway analysis revealed that the hub genes were primarily involved in cell adhesion molecules, phagosome, and pertussis (Fig.4a,b).
Figure 3.
Hub genes identified by different algorithms and UpSet diagram. (a) Hub gene identified by seven different algorithms. (b) The UpSet diagram showed that the seven algorithms screened 12 overlapping hub genes.
Table 1.
The details of the hub genes.
| Gene symbol | Full name | Function |
|---|---|---|
| CYBB | cytochrome b-245 beta chain | CYBB is an important composition of cytochrome b (−245), which has been proposed as a primary component of the microbicidal oxidase system of phagocytes45 |
| LAPTM5 | lysosomal protein transmembrane 5 | LAPTM5, encoding a lysosome-associated protein, E3 protein. This protein may play a role in hematopoiesis46 |
| CSF1R | colony stimulating factor 1 receptor | CSF1R encoded protein is the receptor for colony stimulating factor 1, which is a kind of cytokines controls the production, differentiation, and function of macrophages21 |
| HCK | Src family tyrosine kinase | The protein encoded by HCK is a member of the Src family of tyrosine kinases, which play a role in neutrophil migration and in the degranulation of neutrophils47 |
| ITGAM | integrin subunit alpha M | This gene encodes the integrin alpha M chain, which is important in the adherence of neutrophils and monocytes to stimulated endothelium, and also in the phagocytosis of complement coated particles48 |
| CD86 | CD86 molecule | CD86 encodes a type I membrane protein. CD28 antigen binds to this protein to generate a costimulatory signal for activation of the T-cell. Cytotoxic T-lymphocyte-associated protein 4 binds to this protein to negatively regulate T-cell activation and diminishes the immune response49 |
| C1QA | complement C1q A chain | C1QA encodes C1r and C1s associated proteins to yield the first component of the serum complement system. The deficiency is related to lupus erythematosus and glomerulonephritis50 |
| ITGB2 | integrin subunit beta 2 | This gene encodes an integrin beta chain. The encoded protein mainly affects immune response. The deficiency of ITGB2 cause leukocyte adhesion deficiency51 |
| PTPRC | protein tyrosine phosphatase receptor type C | The protein encoded by this gene is a member of the protein tyrosine phosphatase family. The family is known to be signaling molecules that regulates a variety of cellular processes including cell growth, differentiation, mitosis, and oncogenic transformation52 |
| CTSS | cathepsin S | The preproprotein encoded by this gene is a lysosomal cysteine proteinase that participates in the degradation of antigenic proteins to peptides for presentation on MHC class II molecules53 |
| LCP2 | lymphocyte cytosolic protein 2 | This gene encodes an adapter protein,which is thought to play a role in TCR-mediated intracellular signal transduction54 |
| CD53 | CD53 molecule | The encoded protein contributes to the transduction of CD2-generated signals in T cells and natural killer cells and has been suggested to play a role in growth regulation55 |
Figure 4.
GO and KEGG enrichment analysis of the hub genes.
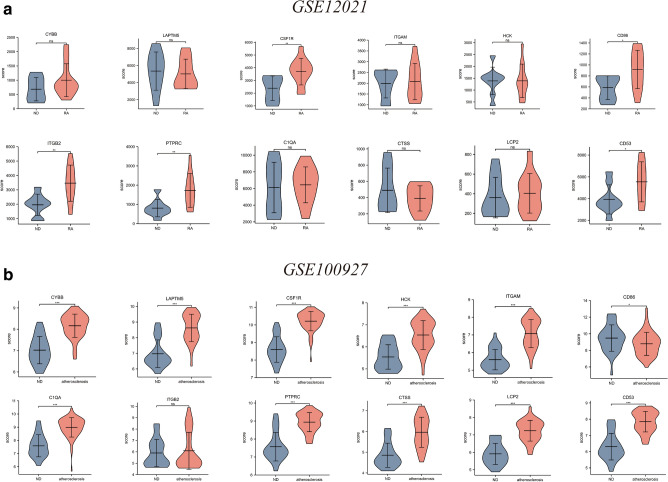
Validation of hub genes expression
The GSE12021 and GSE100927 datasets were used in verifying the expression of the identified hub genes. The mRNA expression levels of CSF1R, CD86, ITGB2, PTPRC, and CD53 were significantly increased in the RA samples compared with the ND samples (P < 0.05, Fig. 5a). In addition, the mRNA expression levels of CYBB, LAPTM5, CSF1R, HCK, ITGAM, CD86, C1QA, PTPRC, CTSS, LCP2, and CD53 were significantly increased in the atherosclerotic plaque samples (P < 0.05, Fig. 5b).
Figure 5.
Expression level of hub gene in GSE12021 and GSE100927. (a) The verification of hub genes in GSE12021. (b) The verification of hub genes in GSE100927 The comparison between the two sets of data with the mean T test. RStudio (https://www.R-project.org) was used in statistical analysis. P value < 0.05 was considered statistically significant. *P < 0.05; ***P < 0.001.
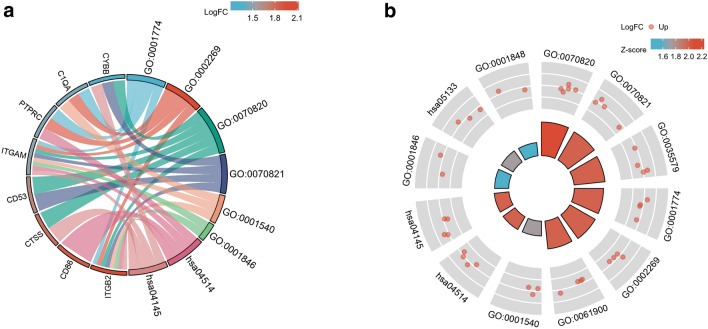
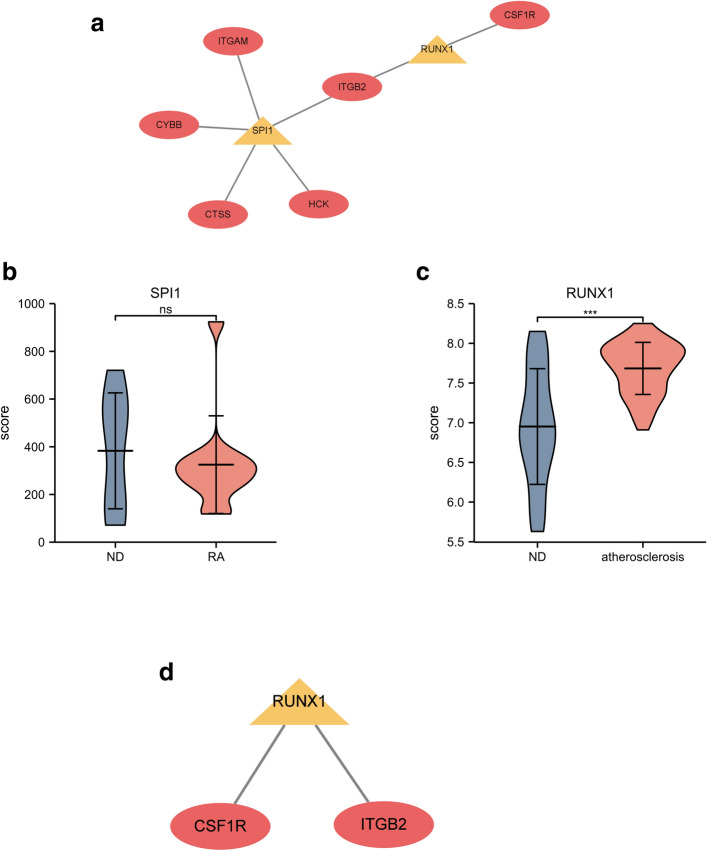
Prediction and verification of TFs
Two TFs that may regulate the expression of the hub genes were identified on the basis of the Transcriptional Regulatory Relationships Unraveled by Sentence Based Text Mining (TRRUST) database (Fig. 6a and Table 2). Spi-1 proto-oncogene (SPI1) and RUNX family transcription factor 1 (RUNX1) were predicted to have the capability to regulate six hub genes (including ITGAM, CYBB, CTSS, HCK, ITGB2, and CSF1R) by acting as TFs. During further verification, we found that one of the TFs, RUNX1, had low expression in the synovial samples of patients with RA in the GSE12021 dataset, whereas the expression of SPI1 was not significantly changed (P < 0.05, Fig. 6b,c). RUNX1, which may function as an important TF in the pathogenesis of patients with RA complicated with atherosclerosis, was predicted to participate in the regulation of the two hub genes CSF1R and ITGB2 (Fig. 6d).
Figure 6.
TFs regulatory network and its expression in GSE12021. (a) TFs regulatory network. (b,c) The expression level of TFs in GSE12021. *P < 0.05. (d) TF regulatory network that has been verified. TFs were marked in yellow, and the hub genes were marked in red.
Table 2.
Key transcriptional factors (TFs) of hub genes.
| Key TFs | Description | P-value | genes |
|---|---|---|---|
| SPI1 | spleen focus forming virus (SFFV) proviral integration oncogene spi1 | 2.52E-10 | CTSS, CYBB, HCK, ITGAM, ITGB2 |
| RUNX1 | runt-related transcription factor 1 | 0.000285 | CSF1R, ITGB2 |
Discussion
The main purpose of our study is to identify the common DEGs in RA and atherosclerosis for the prediction of RA complicated with atherosclerosis and the revelation of potential mechanisms. In this study, 131 overlapping DEGs (all upregulated), of which 12 were hub genes, were detected in both diseases. Among those of the 12 hub genes, the expression levels of CSF1R, CD86, PTPRC, and CD53 were verified by using synovial and atherosclerotic plaque samples. GO and KEGG pathway enrichment analyses revealed that the genes were significantly enriched in phagocytosis, leukocyte migration, and neutrophil activation. In addition, two TFs, RUNX1 and SPI1, were predicted to play roles in the pathogenesis process. One of the TFs, RUNX1, was verified to have low expression in the synovial samples of patients with RA.
Our results from GO and KEGG pathway enrichment analyses indicated that phagocytosis seemed to be activated in RA complicated with atherosclerosis. Prior studies have revealed that the key role of macrophages in atherosclerosis is the phagocytosis of apoptotic and necrotic cells and cell debris; such a role may help reverse plaque vulnerability15. Phagocytosis is impaired in human atherosclerotic plaques, and CD47-blocking antibodies can restore phagocytosis to prevent atherosclerosis16. However, in our study, phagocytosis appeared to be activated. This result may indicate that the mechanism of atherosclerosis complicated with autoimmune diseases, such as RA, may be different. In the disease state, chronic inflammation can lead to the aberrant remodeling of macrophage responses and cause a shift in macrophage phenotypes17. In RA, proinflammatory macrophages are extremely upregulated, which may induce the activation of phagocytosis. Given that this process is always highly activated, phagocytosis may not be a protective factor in patients with RA complicated with atherosclerosis. The exact role of phagocytosis is an interesting study direction and may need further investigation. In addition, our study showed that leukocyte migration and neutrophil activation were also vital in the pathogenesis process. The vasculature is important in inflammation, angiogenesis, and atherosclerosis associated with the pathogenesis of RA18. Vascular injury is caused primarily by activated neutrophils and inflammatory mediators released by neutrophils19. In RA, leukocytes can migrate into the synovium and cause subsequent inflammation processes20. Therefore, the inhibition of phagocytosis, leukocyte migration, and neutrophil activation may offer potential treatment options for patients with RA complicated with atherosclerosis.
Furthermore, our study identified hub genes by using seven common algorithms. Among those of the 12 identified hub genes, the expression levels of CSF1R, CD86, PTPRC, and CD53 were verified. CSF1 is a cytokine that controls the production, differentiation, and function of macrophages21. Although CSF1R is a target in RA and atherosclerosis treatment, studies directly analyzing its role in the concomitant two diseases are limited. Our study demonstrated that CSF1R had remarkably increased expression and served as one of the hub genes. Therefore, drugs targeting CSF1R may have great potential in controlling both diseases simultaneously. CD86 is a type I membrane protein. The CD28 antigen binds to CD86 and generates a co-stimulatory signal for T-cell activation. Abatacept, one of the treatment drugs for RA, can modulate the CD80/CD86–CD28 co-stimulatory signal required for T-cell activation. Although many studies have reported improvement in lipid profiles after abatacept treatment, most of these studies attributed this effect to the reduction in general inflammation and disease activity22,23. Our study showed that CD86 played a vital role in the pathogenesis of RA with atherosclerosis. This role may be another reason for the improvement in lipid profiles after abatacept treatment. PTPRC, also known as CD45, regulates a variety of cellular processes24. Patients with RA who harbor a particular mutation at the PTPRC gene s10919563 locus have better responses to antitumor necrosis factor therapy than individuals who lack it25,26. Meanwhile, PTPRC acts as a regulatory T cell (Treg)-related gene in the deterioration of atherosclerosis27. The upregulation of PTPRC is associated with the progression of atherosclerosis27. Therefore, considering its role in RA and atherosclerosis, PTPRC is a possible treatment target. CD53 regulates the growth of T cells and natural killer cells and has been extensively studied in RA28. CD53 was elevated significantly on leukocytes from patients with RA compared with leukocytes from controls29. Meanwhile, CD53 curbs inflammatory cytokine secretion and is regarded as immune-responsive hub genes related to advanced plaques30. Therefore,drugs targeting CD53 are able to control both dieases at the same time, which emphasizes its importance in future research.
Our study also predicted the TFs of identified hub genes. RUNX1, which was significantly downregulated in RA synovium samples, regulated two hub genes, namely, CSF1R and ITGB2. A previous study discovered that the enhancer of zeste homolog 2 in CD4+ T cells from patients with RA was attenuated, downregulated RUNX1, and ultimately suppressed Treg differentiation31. Treg plays a pivotal role in maintaining immune homeostasis, and Treg deficiency is implicated in the pathogenesis of RA32,33. In addition, Treg is highly involved in atherogenesis. Treg plays a key atheroprotective role by limiting inflammation and counterbalancing plaque formation34.Therefore, the downregulated of RUNX1 may cause Treg suppression, which may aggravate the atherogenesis in RA patinets. Meanwhile, SPI1 was also predicted to be a vital TF in patients with RA complicated with atherosclerosis. However, its expression did not change dramatically likely because of the small smple size of GSE12021. The expression of the SPI1 gene is upregulated during the differentiation of myeloid cells35. In 2020, Pan et al. demonstrated that the expression of SPI1 is significantly increased after a high-fat/cholesterol diet; this result implied that the activation of myeloid cells is critical for atherosclerosis development36. A previous study proved that the inhibition of the complex formed by SPI1 led to the reduction in atherosclerotic lesions37,38. Our study predicted that SPI1 can regulate five hub genes. However, GSE12021 failed to verify the expression level of the five hub genes and SPI1. Hence, the role of SPI1 may need further assessment in a study with a precise design and large population.
In conclusion, our study aimed to identify and verify possible hub genes and TFs, which may serve as promising treatment targets for patients with RA complicated with atherosclerosis. CSF1R, CD86, PTPRC, and CD53 were identified and verified as hub genes. GO and KEGG pathway enrichment analyses revealed that these genes were significantly enriched in phagocytosis, leukocyte migration, and neutrophil activation. In addition, RUNX1 was predicted to participates in the regulation of hub genes as a TF, indicating the role of Treg in this process.
Materials and methods
Data collection
‘‘Rheumatoid arthritis’’ or “atherosclerosis” were used as key words for the expression profiling of RA or atherosclerosis in the GEO database, which is a public repository database39. Datasets, including synovial biopsies from RA or plaque biopsies from atherosclerosis, were used. Finally, three datasets, namely, GSE55235 (GPL96), GSE55457 (GPL96), and GSE28829 (GPL570), were selected as test sets. GSE55235 (GPL96) and GSE55457 (GPL96) included synovial biopsies from 23 patients with RA and 20 normal donors (NDs). GSE28829(GPL570) included plaque biopsies from 13 intimal thickening and 16 thick fibrous cap atheroma lesions. Two datasets, namely, GSE12021 (GPL96) and GSE100927 (GPL17077), were selected as validation sets for RA and atherosclerosis, respectively. The overall flowchart of this research is shown in Supplementary Fig. 2.
Identification of DEGs
The row expression data of GSE55235, GSE55457, and GSE28829 were analyzed. DEGs between the disease and ND groups were obtained using the online web-based tool GEO2R. |Log2 fold change|> 1 and adjusted P value < 0.05 were considered statistically significant. Overlapping DEGs were detected with the online tool Draw Venn Diagram (http://bioinformatics.psb.ugent.be/webtools/Venn/).
Functional and pathway enrichment analyses
GO enrichment and KEGG pathway analyses were performed for the identification of DEGs. R packages (clusterProfile, ggplot2 and GOplot) were used 40. ClusterProfile package was used in analyzing the DEGs. Ggplot2 (https://ggplot2.tidyverse.org) and GOplot packages were used for the visualization of the results.
Construction of a PPI network
The common DEGs were analyzed by the online tool STRING (https:// string-db.org) for the construction of a PPI network. The cut-off standard was set as a combined score > 0.441. Then, the results were visualized with CytoScape software. MCODE V1.5.1, which is a plug-in of CytoScape, was used in identifying significant modules (MCODE score ≥ 4)42. Moreover, the hub genes were selected using CytoHubba, which is another plug-in of CytoScape, according to the number of associations with other genes in the PPI network43. Seven common algorithms (MCC, MNC, Degree, Closeness, Radiality, Stress, and EPC) were used in evaluating and selecting hub genes.
Prediction of TFs
TRRUST, a database for the prediction of transcriptional regulatory networks, was used in predicting TFs that regulate hub genes, and an adjusted P value of < 0.05 was considered significant44.
Statistical analysis
RStudio (https://www.R-project.org) was used in statistical analysis. GSE12021 and GSE100927 were used in validating the expression levels of the identified hub genes and TFs. Wilcoxon rank sum test was used as the statistical method when the data was not normally distributed, and T- test was used as the statistical method when the dada was normally distributed. P value < 0.05 was considered significant.
Supplementary Information
Acknowledgements
The authors are very thankful to all participants for their cooperation in this study. They thank all the staff for their dedication.
Author contributions
L.X. designed the study. L.X. and Z.Y. wrote the manuscript. S.L. revised the manuscript. All authors read and approved the final manuscript.
Funding
This research was supported by Hainan Provincial Natural Science Foundation of China (820QN386). This project is supported by Hainan Province Clinical Medical Center.
Data availability
The datasets generated and/or analyzed during the current study are available in the GEO repository. It is a public free repository database, which stores a large number of gene functions and expressions. The working links are as following, GSE55235(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE55235), GSE55457(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE55457), GSE12021(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE12021), GSE28829(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc = GSE28829), and GSE100927(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc = GSE100927).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-08274-1.
References:
- 1.Gonzalez-Gay MA, Gonzalez-Juanatey C, Martin J. Rheumatoid arthritis: A disease associated with accelerated atherogenesis. Semin. Arthritis Rheum. 2005;35:8–17. doi: 10.1016/j.semarthrit.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Myasoedova E, et al. The role of rheumatoid arthritis (RA) flare and cumulative burden of RA severity in the risk of cardiovascular disease. Ann. Rheum. Dis. 2016;75:560–565. doi: 10.1136/annrheumdis-2014-206411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Full LE, Ruisanchez C, Monaco C. The inextricable link between atherosclerosis and prototypical inflammatory diseases rheumatoid arthritis and systemic lupus erythematosus. Arthritis Res. Ther. 2009;11:217. doi: 10.1186/ar2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoshida T, et al. Non-obese visceral adiposity is associated with the risk of atherosclerosis in Japanese patients with rheumatoid arthritis: A cross-sectional study. Rheumatol. Int. 2018;38:1679–1689. doi: 10.1007/s00296-018-4095-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corrales A, et al. Combined use of QRISK3 and SCORE as predictors of carotid plaques in patients with rheumatoid arthritis. Rheumatology (Oxford) 2021;60:2801–2807. doi: 10.1093/rheumatology/keaa718. [DOI] [PubMed] [Google Scholar]
- 6.Dessein PH, et al. The Framingham Score and the Systematic Coronary Risk Evaluation at Low Cutoff Values Are Useful Surrogate Markers of High-risk Subclinical Atherosclerosis in Patients with Rheumatoid Arthritis. J. Rheumatol. 2016;43:486–494. doi: 10.3899/jrheum.150510. [DOI] [PubMed] [Google Scholar]
- 7.Charles-Schoeman C, et al. Association of paraoxonase 1 gene polymorphism and enzyme activity with carotid plaque in rheumatoid arthritis. Arthritis Rheum. 2013;65:2765–2772. doi: 10.1002/art.38118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.López-Mejías R, et al. Influence of elevated-CRP level-related polymorphisms in non-rheumatic Caucasians on the risk of subclinical atherosclerosis and cardiovascular disease in rheumatoid arthritis. Sci. Rep. 2016;6:31979. doi: 10.1038/srep31979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.López-Mejías R, et al. Influence of coronary artery disease and subclinical atherosclerosis related polymorphisms on the risk of atherosclerosis in rheumatoid arthritis. Sci. Rep. 2017;7:40303. doi: 10.1038/srep40303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.López-Mejías R, et al. Lack of association between ABO, PPAP2B, ADAMST7, PIK3CG, and EDNRA and carotid intima-media thickness, carotid plaques, and cardiovascular disease in patients with rheumatoid arthritis. Mediators Inflamm. 2014;2014:756279. doi: 10.1155/2014/756279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang S, Song J. Robust gene selection methods using weighting schemes for microarray data analysis. BMC Bioinf. 2017;18:389. doi: 10.1186/s12859-017-1810-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucl. Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanehisa M. Toward understanding the origin and evolution of cellular organisms. Prot. Sci. Publ. Prot. Soc. 2019;28:1947–1951. doi: 10.1002/pro.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanehisa M, Furumichi M, Sato Y, Ishiguro-Watanabe M, Tanabe M. KEGG: Integrating viruses and cellular organisms. Nucleic Acids Res. 2021;49:D545–d551. doi: 10.1093/nar/gkaa970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamczyk, M. R., Villa-Bellosta, R. & Andrés, V. In Vitro Macrophage Phagocytosis Assay. Methods in molecular biology (Clifton, N.J.)1339, 235–246. 10.1007/978-1-4939-2929-0_16 (2015). [DOI] [PubMed]
- 16.Kojima Y, et al. CD47-blocking antibodies restore phagocytosis and prevent atherosclerosis. Nature. 2016;536:86–90. doi: 10.1038/nature18935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuznetsova T, Prange KHM, Glass CK, de Winther MPJ. Transcriptional and epigenetic regulation of macrophages in atherosclerosis. Nat. Rev. Cardiol. 2020;17:216–228. doi: 10.1038/s41569-019-0265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu S, et al. Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: From mechanism to pharmacotherapies. Pharmacol. Rev. 2021;73:924–967. doi: 10.1124/pharmrev.120.000096. [DOI] [PubMed] [Google Scholar]
- 19.Szekanecz Z, Koch AE. Vascular involvement in rheumatic diseases: 'Vascular rheumatology'. Arthritis Res. Ther. 2008;10:224. doi: 10.1186/ar2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lefevre S, Meier FM, Neumann E, Muller-Ladner U. Role of synovial fibroblasts in rheumatoid arthritis. Curr. Pharm. Des. 2015;21:130–141. doi: 10.2174/1381612820666140825122036. [DOI] [PubMed] [Google Scholar]
- 21.Valero JG, et al. The receptor of the colony-stimulating factor-1 (CSF-1R) is a novel prognostic factor and therapeutic target in follicular lymphoma. Leukemia. 2021;35:2635–2649. doi: 10.1038/s41375-021-01201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benucci M, et al. Factors correlated with the improvement of endothelial dysfunction during Abatacept therapy in patients with rheumatoid arthritis. J. Inflamm. Res. 2018;11:247–252. doi: 10.2147/jir.s156822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Charles-Schoeman C, et al. Remodeling of the HDL proteome with treatment response to abatacept or adalimumab in the AMPLE trial of patients with rheumatoid arthritis. Atherosclerosis. 2018;275:107–114. doi: 10.1016/j.atherosclerosis.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huntington ND, Tarlinton DM. CD45: Direct and indirect government of immune regulation. Immunol. Lett. 2004;94:167–174. doi: 10.1016/j.imlet.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Ferreiro-Iglesias A, et al. Replication of PTPRC as genetic biomarker of response to TNF inhibitors in patients with rheumatoid arthritis. Pharmacogenomics J. 2016;16:137–140. doi: 10.1038/tpj.2015.29. [DOI] [PubMed] [Google Scholar]
- 26.Lee YH, Bae SC. Associations between PTPRC rs10919563 A/G and FCGR2A R131H polymorphisms and responsiveness to TNF blockers in rheumatoid arthritis: A meta-analysis. Rheumatol. Int. 2016;36:837–844. doi: 10.1007/s00296-016-3476-5. [DOI] [PubMed] [Google Scholar]
- 27.Xia M, Wu Q, Chen P, Qian C. Regulatory T cell-related gene biomarkers in the deterioration of atherosclerosis. Front. Cardiovasc. Med. 2021;8:661709. doi: 10.3389/fcvm.2021.661709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pedersen-Lane JH, Zurier RB, Lawrence DA. Analysis of the thiol status of peripheral blood leukocytes in rheumatoid arthritis patients. J. Leukoc. Biol. 2007;81:934–941. doi: 10.1189/jlb.0806533. [DOI] [PubMed] [Google Scholar]
- 29.Lee H, et al. CD53, a suppressor of inflammatory cytokine production, is associated with population asthma risk via the functional promoter polymorphism -1560 C>T. Biochem. Biophys. Acta. 1830;3011–3018:2013. doi: 10.1016/j.bbagen.2012.12.030. [DOI] [PubMed] [Google Scholar]
- 30.Liu C, et al. Identifying RBM47, HCK, CD53, TYROBP, and HAVCR2 as hub genes in advanced atherosclerotic plaques by network-based analysis and validation. Front. Genet. 2020;11:602908. doi: 10.3389/fgene.2020.602908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xiao XY, et al. EZH2 deficiency attenuates Treg differentiation in rheumatoid arthritis. J. Autoimmun. 2020;108:102404. doi: 10.1016/j.jaut.2020.102404. [DOI] [PubMed] [Google Scholar]
- 32.Niu Q, Cai B, Huang ZC, Shi YY, Wang LL. Disturbed Th17/Treg balance in patients with rheumatoid arthritis. Rheumatol. Int. 2012;32:2731–2736. doi: 10.1007/s00296-011-1984-x. [DOI] [PubMed] [Google Scholar]
- 33.Nguyen LT, Jacobs J, Mathis D, Benoist C. Where FoxP3-dependent regulatory T cells impinge on the development of inflammatory arthritis. Arthritis Rheum. 2007;56:509–520. doi: 10.1002/art.22272. [DOI] [PubMed] [Google Scholar]
- 34.Huang L, et al. Decreased frequencies and impaired functions of the CD31(+) subpopulation in T(reg) cells associated with decreased FoxP3 expression and enhanced T(reg) cell defects in patients with coronary heart disease. Clin. Exp. Immunol. 2017;187:441–454. doi: 10.1111/cei.12897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wittwer J, Marti-Jaun J, Hersberger M. Functional polymorphism in ALOX15 results in increased allele-specific transcription in macrophages through binding of the transcription factor SPI1. Hum. Mutat. 2006;27:78–87. doi: 10.1002/humu.20273. [DOI] [PubMed] [Google Scholar]
- 36.Pan Y, et al. Bioinformatics analysis of vascular RNA-seq data revealed hub genes and pathways in a novel Tibetan minipig atherosclerosis model induced by a high fat/cholesterol diet. Lipids Health Dis. 2020;19:54. doi: 10.1186/s12944-020-01222-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao L, et al. Selective interleukin-12 synthesis defect in 12/15-lipoxygenase-deficient macrophages associated with reduced atherosclerosis in a mouse model of familial hypercholesterolemia. J. Biol. Chem. 2002;277:35350–35356. doi: 10.1074/jbc.M205738200. [DOI] [PubMed] [Google Scholar]
- 38.Chen H, Wang L, Jiang J. Transcriptome and miRNA network analysis of familial hypercholesterolemia. Int. J. Mol. Med. 2014;33:670–676. doi: 10.3892/ijmm.2013.1610. [DOI] [PubMed] [Google Scholar]
- 39.Clough, E. & Barrett, T. (2016) The Gene Expression Omnibus Database. Methods Mol. Biol. (Clifton, NJ)1418, 93-110. [DOI] [PMC free article] [PubMed]
- 40.Yu G, Wang LG, Han Y, He QY. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16:284–287. doi: 10.1089/omi.2011.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Szklarczyk D, et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucl. Acids Res. 2019;47:D607–d613. doi: 10.1093/nar/gky1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bandettini WP, et al. MultiContrast Delayed Enhancement (MCODE) improves detection of subendocardial myocardial infarction by late gadolinium enhancement cardiovascular magnetic resonance: A clinical validation study. J. Cardiovasc. Magnet. Resonance. 2012;14:83. doi: 10.1186/1532-429x-14-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chin, C. H. et al. cytoHubba: Identifying hub objects and sub-networks from complex interactome. BMC Syst. Biology 8 Suppl 4, S11. 10.1186/1752-0509-8-s4-s11 (2014). [DOI] [PMC free article] [PubMed]
- 44.Han H, et al. TRRUST v2: An expanded reference database of human and mouse transcriptional regulatory interactions. Nucl. Acids Res. 2018;46:D380–d386. doi: 10.1093/nar/gkx1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grauers Wiktorin H, Aydin E, Hellstrand K, Martner A. NOX2-derived reactive oxygen species in cancer. Oxid. Med. Cell. Longev. 2020;2020:7095902. doi: 10.1155/2020/7095902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jun DY, et al. Ectopic overexpression of LAPTM5 results in lysosomal targeting and induces Mcl-1 down-regulation, Bak activation, and mitochondria-dependent apoptosis in human HeLa cells. PLoS ONE. 2017;12:e0176544. doi: 10.1371/journal.pone.0176544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pond MP, et al. Membrane Anchoring of Hck Kinase via the Intrinsically Disordered SH4-U and Length Scale Associated with Subcellular Localization. J. Mol. Biol. 2020;432:2985–2997. doi: 10.1016/j.jmb.2019.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Anaya JM, et al. Evaluation of genetic association between an ITGAM non-synonymous SNP (rs1143679) and multiple autoimmune diseases. Autoimmun. Rev. 2012;11:276–280. doi: 10.1016/j.autrev.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Podojil JR, Sanders VM. CD86 and beta2-adrenergic receptor stimulation regulate B-cell activity cooperatively. Trends Immunol. 2005;26:180–185. doi: 10.1016/j.it.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 50.Chen LH, et al. Complement C1q (C1qA, C1qB, and C1qC) May Be a Potential Prognostic Factor and an Index of Tumor Microenvironment Remodeling in Osteosarcoma. Front. Oncol. 2021;11:642144. doi: 10.3389/fonc.2021.642144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nawaz Tipu H, et al. β2 Integrin Gene (ITGB2) mutation spectra in Pakistani families with leukocyte adhesion deficiency type 1 (LAD1) Immunobiology. 2020;225:151938. doi: 10.1016/j.imbio.2020.151938. [DOI] [PubMed] [Google Scholar]
- 52.Al Barashdi, M. A., Ali, A., McMullin, M. F. & Mills, K. Protein tyrosine phosphatase receptor type C (PTPRC or CD45). J. Clin. Pathol.74, 548–552. 10.1136/jclinpath-2020-206927 (2021). [DOI] [PMC free article] [PubMed]
- 53.Brown R, et al. Cathepsin S: Investigating an old player in lung disease pathogenesis, comorbidities, and potential therapeutics. Respir. Res. 2020;21:111. doi: 10.1186/s12931-020-01381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huo Y, Zhang K, Han S, Feng Y, Bao Y. Lymphocyte cytosolic protein 2 is a novel prognostic marker in lung adenocarcinoma. J. Int. Med. Res. 2021;49:3000605211059681. doi: 10.1177/03000605211059681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dunlock VE. Tetraspanin CD53: an overlooked regulator of immune cell function. Med. Microbiol. Immunol. 2020;209:545–552. doi: 10.1007/s00430-020-00677-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the GEO repository. It is a public free repository database, which stores a large number of gene functions and expressions. The working links are as following, GSE55235(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE55235), GSE55457(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE55457), GSE12021(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE12021), GSE28829(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc = GSE28829), and GSE100927(https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc = GSE100927).