Abstract
The novel coronavirus disease 2019 (COVID-19)-related pandemic has been in existence for almost 2 years now after its possible emergence from a wet market in the city of Wuhan of the Chinese mainland. Evidence of the emergence and transmission of this virus was attributed to bats and pangolins. The causative virus, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has rapidly spread globally, affecting humans considerably with its current death toll to be over 4.7 million out of more than 233 confirmed cases as of September 2021. The virus is constantly mutating and continuously trying to establish itself in humans by increasing its transmissibility and virulence through its numerous emerging variants. Several countries have been facing multiple waves of COVID-19 outbreaks one after the other, putting the medical and healthcare establishments under tremendous stress. Although very few drugs and vaccines have been approved for emergency use, their production capabilities need to meet the needs of a huge global population. Currently, not even a quarter of the world population is vaccinated. The situation in India has worsened during the ongoing second wave with the involvement of virus variants with a rapid and huge surge in COVID-19 cases, where the scarcity of hospital infrastructure, antiviral agents, and oxygen has led to increased deaths. Recently, increased surveillance and monitoring, strengthening of medical facilities, campaigns of awareness programs, progressive vaccination drive, and high collaborative efforts have led to limiting the surge of COVID-19 cases in India to a low level. This review outlines the global status of the pandemic with special reference to the Indian scenario.
Keywords: Challenges, COVID-19, COVID-appropriate behavior, Fears of third wave, Pandemic scenario, SARS-CoV-2, Second wave
Context
The advent and vigorous global transmission of the severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2), the cause of coronavirus disease 2019 (COVID-19) pandemic, is a crucial challenge for the governments and the healthcare services and has interrupted various socioeconomic activities worldwide ( 1 - 5 ). In India, the second wave of COVID-19 cases escalated toward the last week of February in 2021 when the average reported cases per day reached over 15,000. The second wave of COVID-19 propagated much more rapidly in India than the first wave (Figure 1). With a rapid and uncontrolled surge in the cases by May 2021, the condition started worsening setting new daily global record cases of infections and deaths ( 6 ). A major public health threat in the form of the second wave of COVID-19 is the result of the mutating SARS-CoV-2 that made it extremely contagious. The nations worldwide undertake extensive measures for expeditious vaccination drive to gain control over the pandemic at the earliest stage ( 7 ).
Figure 1.
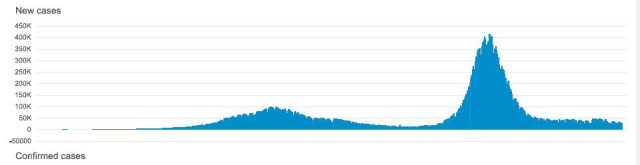
The daily COVID-19 situation report on India reproduced from the World Health Organization (Accessed on 26th September 2021) (15).
2. Evidence Acquisition
The data sources were collected from authentic academic databases, such as PubMed, ScienceDirect, Scopus, and Google Scholar, along with some public and government health organization websites, such as the World Health Organization (WHO), and the Centre for Disease Control and Prevention (CDC) resources. After a literature search covering 2020-2021, the obtained data were carefully examined, and only the relevant studies were considered for critical discussion while excluding the generalized studies.
Several countries have been facing multiple waves, putting the medical and healthcare establishments under tremendous stress. Another big challenge, as observed in the second wave, is the secondary invasive opportunistic infections in the COVID-19 patients during the infection and also during convalescence (8). Such infections are reportedly prominent in the recovered (or recovering) COVID-19 cases with uncontrolled diabetes (high blood sugar), prolonged intensive care units stay, immuno-compromised state (such as human immunodeficiency virus/acquired immunodeficiency syndrome), chronic kidney disease, hematological malignancies, and solid organ transplant (9). The spread of these fungal infections could also be attributed to steroids and antibiotic overdose during COVID-19 treatment (10).
India has the second-largest diabetic population, around 70% of which are uncontrolled (11). The mortality rate of COVID-related fungal infection is reportedly higher (~87%), compared to the earlier cases in non-COVID patients (~50%) (12, 13). Hence, this pandemic is far more threatening for persons with pre-existing comorbidities. Prompt and effective governmental interventions are much needed to seize the vigorous progression of this pandemic (14). The findings reported here and the lessons learned shall enable the healthcare system to counter this ongoing global pandemic.
3. Results
In the initial search, 125 articles/data were found, 76 of which were selected for further analysis based on the specific inclusion and exclusion criteria. The most relevant, and critical literature was given preference and the obtained data were used to develop this specific area review.
3.1. COVID-19 Cases and Death Rate
As of May 3, 2021, there were 1,69,60,172 globally positive COVID-19 cases which increase at a rate of about 400,000 cases per day in India. Moreover, the death toll has risen to 2,22,408 (1.10%) by May 4, 2021, with 3449 daily cases. Owing to the progressing second wave of COVID-19, testing has remarkably increased to cater to the escalating cases at an aggregate of 29,33,10,779 samples tested by May 3, 2021 ( 16 ). India is fighting against the ongoing second wave with an atypical ascent of day-to-day cases and swift infection rates with hospitals flooded with patients, overburdened healthcare workers, and increased oxygen demand.
3.2. Possible Reasons behind COVID-19 Surge in India
Indian COVID-19 cases flared up sharply during the second wave with the country recording more than 300,000-400,000 cases daily. As genome sequencing seems to be crucial in managing the pandemic, Indian labs need to be well equipped with regard to the necessary funds and facilities for additional human and infrastructural resources for this catering only to 5% of all the detected cases at present. Although the second wave is spreading everywhere, the genome sequence is analyzed barely in 1% of the cases ( 17 ).
At present, India spends less than 1% of its gross domestic product on research and development. An in-depth understanding of the pathological and epidemiological mechanisms seems to be lacking possibly due to the less available data. The Indian R0 (1.37) was high during the second wave, compared to other countries having an R0 value less than 1 to 0.5. It seems that India needs to have timely learned much from the first wave as it witnessed the highest daily COVID-19 death toll amid the deadly second wave.
3.3. Role of SARS-CoV-2 Mutant Strains
Mutations can escalate the capability of viruses to infect humans depending on the type, site, or nature. The RNA viruses mutate relatively rapidly with a rapidly evolving propensity. A novel variant of a virus generates after several cycles of viral mutation. One such SARS-CoV-2 variant is B.1.617 (delta variant), a double SARS-CoV-2 mutant preserving two mutations, namely L452R and E484Q ( 17 , 18 ); L452R is a Californian strain that is also found in India. This variant was first identified in India by the end of March and was also simultaneously reported in the US, the UK, and Australia. The daily tally rising to about 400,000 cases by May 03, 2021, has been attributed to this novel double-mutated strain. Another depiction of a novel variant called ‘triple mutant’ has recently been reported with an additional mutation, namely V383L, recently noticed in SARS-CoV-2 spike protein alongside the double mutation that was earlier reported in the samples sequenced in the state of Maharashtra, India ( 17 , 18 ).
The UK variant B.1.1.7, mutated from B.1.167, has also been reported in some Indian states. The N440K variant has been reported in the Indian states, viz., Kerala, Andhra Pradesh, Telangana. Another highly contagious variant E484Q was reported in Maharashtra, with rapid lung infections, faster pulmonary changes, and a high risk of reinfection. As variants, like B.1.1.7 (UK), B.1.351 (USA), B.1.1.28.1 (Japan/Brazil), and other mutants, are reported, understanding their genome sequences is highly recommended. As per reports, the virus infects the upper and lower respiratory tract, heart, kidney, liver, gut, and nervous system, causing multi-organ damage ( 19 ). It also causes severe complications in pregnant women, elderly people, and persons with pre-existing comorbidities, such as diabetes, obesity, cardiovascular disorders, and hypertension ( 20 ) as mentioned earlier.
3.4. Role of the Government and the Public
The citizens lowering the guard down and ignoring COVID-19 appropriate behavior protocols was certainly a valid reason for the recently observed huge surge in SARS-CoV-2 cases in India ( 18 ). All the major public places, including the malls, movie theatres, parks, schools, bars, restaurants, and stadiums, were opened in full capacity in early 2021 with the COVID-19 surveillance and control taking a backseat. People got frustrated following the COVID-19 precautions after months of canceled activities, economic challenges, and stress. Whatever feeble warning signals of the second wave were shunned down by the public as ‘negative sentiments’ while premature euphoria over herd immunity continued.
The Kumbh Mela, an annual religious event organized with over 3.5 million people taking a dip in the holy Ganges, has been implicated in turning into a super-spreader ( 21 ). It led to an increase in active cases in the state of Uttarakhand from 30-40 cases per day in February to around 2000-2500 cases by the end of April. However, it is under debate of spreading issues whether massive gatherings during any pandemic results in a super spreading event. Furthermore, the elections conducted in India during April might have been a smoldering fire owing to huge gathering events in a few states of the country ( 18 , 21 ). What precede elections in India as also anywhere in a democracy are rallies and massive meetings, which put a massive additional number of people at risk during the ongoing pandemic waves.
A couple of weeks before the second wave, it was assumed that the country has successfully tackled the COVD-19 pandemic along with necessary justification to export vaccines, Remdesivir, and oxygen supplies to the needy based on International policies of collaborative efforts to limit the spread of the pandemic. As a result, the country witnessed a 73.4% whopping increase in the global export of oxygen and 60 million doses of vaccine around January 2021.
When India began recording a dramatic rise in new COVID-19 cases in the second wave and the government allowed registration of citizens within the age group of 18-45 years for vaccination, a shortage of vaccines was felt. Additionally, some rumors about the COVID-19 vaccine made the eligible age group hesitant to take it in many localities, making double-dose vaccination possible only in 0.7% of Indians while the cases were surging. Only 5% of the population received a single (the first) dose at that time when cases were surging; therefore, the impact has not been enough ( 22 ).
3.5. Challenges and Failure of the Indian Healthcare System
With about 8.5 hospital beds and 8 physicians per 10,000 people, the healthcare system in India got stretched to its breaking point amid the second wave of COVID-19. As many hospitals were extended to work beyond their capacities in handling this highly infectious disease, particularly during the ongoing second wave, patients were worried about the availability of hospital beds, ventilators (oxygen supply), and drugs, like remdesivir and tocilizumab ( 14 , 17 , 18 ). The inefficiency and shortage of healthcare delivery systems did not match the growing need during this crisis ( 23 ).
The lesser public spending on healthcare could be accountable for less equipped infrastructure and limited reach of healthcare services as was needed during the surging second wave of the COVID-19 pandemic. The private healthcare industry of the country, estimated to be around 280 billion dollars, was primarily busy in providing five-star hospitalization and catering to the need for lifestyle diseases with huge insurance coverage.
Doubling the percent gross domestic product expenditure on healthcare from the existing 1.3% to 2.5% could improve the figure of hospital beds per 10,000 populations from 8.5 to 100 as stated by the ambitious national health policy. With more than 80% of the population not having health insurance coverage, WHO revealed that an average Indian spends close to two-thirds from his own pocket towards healthcare expenses compared to the world average of 18.2%. Such exorbitant healthcare expenses push 63 million people into poverty every year. Overall, the pandemic has somehow undermined India’s resilience and reflected underfunding and considerably dysfunctioning the healthcare system amid surging cases ( 14 ).
3.6. Insights into the First wave Vs. the Second Wave in India
Almost after 6 months of its peak in the first wave during September 2020, India witnessed another surge in COVID-19 cases from March 2021. Besides SARS-CoV-2 variants, the possible reason for the second wave could be the overwhelmed euphoria on herd immunity. Moreover, the public ignored the real value of COVID-appropriate behavior (such as, wearing a face mask and following social distancing norms) set by the government to avoid risking SARS-CoV-2 infection. People completely ignored these norms still in vogue, including participation in the Kumbh Mela (a super-spreader event). Additionally, many political rallies with huge gatherings continued during elections in April 2021 ( 24 - 26 ).
Based on an analysis performed on patients from 2020 to 2021, the Indian Council for Medical Research suggested that the difference between the behaviors of the age groups that got infected in both waves was not much. Based on a study performed on 1885 patients in the second wave and 7.600 patients in the first wave, more than 70% of patients in both waves were above 40 years of age. Around 5.8% of the hospitalized patients were of 0-19 years of age in the second wave, compared to 4.2% in the earlier one. Similarly, the patients between 20-39 years of age increased to 25.5% from 23.7%. However, the symptoms in hospitalized cases in both the waves differed, with the higher number of asymptomatic patients being reported in the second wave. More cases of dry cough, joint pains, and headache in the previous wave were replaced by more patients with breathlessness during the second wave.
The need for medical oxygen spiked to an unthinkable level in the second wave, and the request for oxygen support was flooded on social media day in and day out. While about 41.5% of the patients required oxygen in the first wave, the figure increased to 54.5% of the patients in the second wave. Similarly, the ventilator support requirement was 37.3% in the second wave, compared to 27.8% in the first one. Two vaccines were approved for emergency use in India, Covishield (an Oxford-AstraZeneca vaccine version manufactured by the Serum Institute of India, Pune) and Covaxin (developed indigenously by Bharat Biotech, Hyderabad).
The Russian Sputnik V has been approved as a third vaccine in April 2021, and a few more are in pipeline. With vaccination made available to all above 18 years of age, the Institute for Health Metrics and Evaluation predicts that many lives could be saved by first August 2021 ( 17 , 26 , 27 ). However, a total of 160,418,105 vaccine doses were administered in such a highly populated country as of May 3, 2021.
It was also predicted that the daily deaths will rise to 5,600 on May 10. However, Institute for Health Metrics and Evaluation suggested that India may save thousands of more lives if it was able to achieve universal mask coverage in the next week. During the massive surge in COVID-19 cases amid the flaring up of the second wave, foreign aids to India were also pouring in continuously from several countries, including the US, the UK, France, and a few others. This was with regards to the provision of necessary emergency support in the form of ventilators, oxygen concentrators, cryogenic oxygen containers, remdesivir, and other necessary medical facilities to strengthen the country for countering severe COVID-19 surge in India by the timely meeting of the medical needs of SARS-CoV-2 hospitalized patients.
3.7. Travel-to-India Advisory
The CDC has advised against travel to India even for fully (two doses) vaccinated people amid the surging second wave. It issued a Level 4 travel health notice for people traveling to India ( 28 ). Travel restrictions could be a major strategy to break the spread of the virus across a larger geographical region ( 29 , 30 ). Several countries banned flights to and from India and advised travelers not to travel to India due to the rapid COVID-19 upsurge, deadly SARS-CoV-2 variants, and the poor healthcare system. As a result, strict rules and regulations and mandatory quarantine of passengers arriving from India have been imposed by several countries, like the UK, Canada, and Australia.
3.8. Fears of the Third Wave of COVID-19 Pandemic
The people of India have just been presently experiencing a sign of relief from the second wave of the COVID-19 pandemic as a massive surge in cases has come down to only nearly 20,000 cases per day as of September 30, 2021. By this time, around 880,000,000 people (65%) have been vaccinated (with at least one single dose of COVID-19 vaccine) out of 1,350,000,000 population of India by follow up of massive vaccination drive (https://covid19.who.int/region/searo/country/in). Medical facilities and infrastructures have been strengthened in recent times with increasing the production capacity of vaccines in the country.
Except for the educational institutions, most of the social, and commercial establishments, including the holy worshipping places are now open for unrestricted human movements but following the COVID-19 appropriate behavior and recommended protocols to control the spread. More recently, educational institutes and schools are also being opened up gradually. Nevertheless, the majority of people have been following the anti-infection practices, like wearing the mask, using hand sanitizers, and maintaining social distancing.
However, due to the incumbent season of festivals and religious ceremonies combined with long-due marriage ceremonies, there is an increased possibility for large-scale gatherings in the future. This may precipitate the situation, increase the transmissibility of the virus, and initiate the third wave of the COVID-19 pandemic. Interestingly, the second wave of the COVID-19 pandemic in India was due to the Delta variant of the novel SARS-CoV-2 ( 31 ). The Delta variant and the Delta plus variant (B. 1. 617. 3) variant had further spread to several parts of the world including the USA, UK, Japan, Indonesia, and several other European and developed countries ( 32 - 34 ).
The Delta variant continues to be responsible for multiple fresh waves of infections throughout the world and raising the concerns for medical emergencies and deteriorating the public health situations. The Indian scenario is unique, where the second wave appears to have now been stabilized with only 2-3 states of the country accounting for more than 80% of the daily total infections and deaths. However, the concern of a third wave remains owing to the fact that a genetic variant of the Delta strain which is now called Delta plus is potentially circulating and may in the future become responsible for the third wave of the pandemic (Figure 2).
Figure 2.
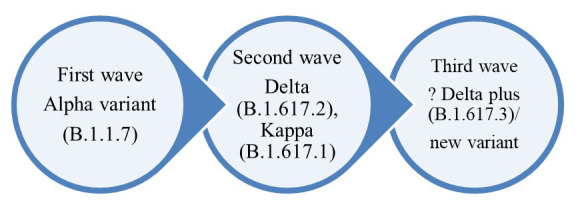
Variants of SARS-CoV-2 responsible for consecutive hits in the Indian scenario.
The Delta variants of the novel SARS-CoV-2 virus have been labeled as variants of concern, and there is emerging evidence about their increased transmissibility, resistance to monoclonal antibodies, and convalescent sera ( 35 , 36 ). Moreover, the Delta variants appear to also infect the vaccinated population which further raises the associated concerns ( 37 ). However, the availability of vaccination is instrumental in minimizing the morbidity associated with the infection and reducing the stress on the healthcare systems, especially in the developing and third world countries that lack adequate infrastructures ( 38 ).
Recent studies have also noted that the seropositivity against the novel SARS-CoV-2 among the selected population groups improved through the first (<5%) and second waves (up to 20%) of the pandemic. In addition, a reduction was noted in the occurrences of milder infections, rates of hospitalizations, and intensive care admissions along with reduced fatalities ( 39 , 40 ).
3.9. Blood Scarcity During COVID-19
Like other sectors, the COVID-19 outbreak has posed a very negative impact on blood donation campaigns worldwide. The imposed lockdowns in several countries led to severe blood scarcity in the blood banks as the blood donation programs are halted worldwide ( 41 ). In several countries, blood donations have been decreased over time ( 42 ). The spread of SARS-CoV-2 via blood transfusion has not been detected yet; however, the increasing fear and anxiety may be the possible reason for a substantial decrease in blood donations ( 43 - 45 ). For this reason, people would not participate in various blood donation programs. The blood collecting agencies have also pointed a significant rise in donor cancellations, which resulted in a remarkable reduction in blood availability and raised serious concerns among the hospitals ( 46 , 47 ). A number of research groups have pointed out several consequences related to the scarcity of blood in the blood banks. Hence, the strategies to promote blood donations with appropriate safety measures during the COVID-19 pandemic are highly recommended ( 48 - 52 ).
3.10. Challenges Ahead to be Addressed
The ongoing COVID-19 pandemic is still haunting around with its devastating health effects and severe adverse impacts on economies worldwide. As of September 30, 2021, more than 233 million confirmed cases have been reported with over 4.7 million deaths ( 53 ). Few of the challenges are required to be handled, like developing more efficacious and protective vaccines, vaccine safety issues, breaking vaccine hesitancy, and affordable equitable access of vaccines at global level, ramping up of bulk production of
vaccines, dangers of emerging SARS-CoV-2 variants, and mutants, checking breakthrough of vaccine-induced protective levels, immunized people being infected with the virus/variants, vaccination drive to be scaled up and obtaining herd immunity. Moreover, the recommended prevention and control strategies are warranted to be strictly implemented, altogether aiding to tackle the COVID-19 pandemic ( 54 - 66 ).
Apart from these, animal spillover events, cross-species jumping, and zooanthroponotic transmission of SARS-CoV-2 along with zoonotic implications and concerns need to be taken into account by strengthening the surveillance and monitoring of animals for the presence of SARS-CoV-2, adopting one health strategy to a wider level, and developing vaccines for companion and captive animals, vaccinating few animal species to check the circulation of SARS-CoV-2 in animal population and subsequently, limiting human-to-animal or any possibility of animal-to-human transmission as was seen in minks. Such strategies would help restrain the ongoing COVID-19 pandemic waves as well as facilitate the design of appropriate preparedness plans to mitigate the fears of future pandemics ( 67 - 76 ).
4. Conclusion
In view of the fact that the virus has been undergoing mutations, increased surveillance of the SARS-CoV-2 mutations based on genomic sequence studies could help to understand the course of the second COVID-19 wave in the country and facilitate the preparation of plans to tackle feasible third wave of the pandemic. It is important to restrict the movements of people both locally and globally. Besides, there is a public need to follow appropriate COVID-19 guidelines as well as prevention and control strategies.
Other measures include strengthening of the healthcare systems and medical facilities, increasing the containment zones, extending the currently imposed partial and complete lockdowns implemented in a few states, and going further for more lockdowns, strictly ‘breaking the chain’ of the rapid virus spread to effectively control the ongoing second wave of the pandemic, and counter the possible incidence of the 3rd wave. Governments are working proactively to boost the vaccine drive and ensure complete vaccination of people at the earliest time possible. Major efforts are going on currently to contain and limit the second wave of COVID-19 in India and hopefully, it will be controlled soon.
Authors' Contribution
All the authors substantially contributed to the conception, design, analysis, and interpretation of data, and approving the final version of the manuscript.
Conflict of Interest
All authors declare that there exist no commercial or financial relationships that could, in any way, lead to potential conflicts of interest.
Grant Support
There is no substantial funding to declare.
Acknowledgement
All the authors acknowledge and thank their respective institutes and universities of affiliation.
References
- 1.Gupta M, Mohanta SS, Rao A, et al. Transmission dynamics of the COVID-19 epidemic in India and modeling optimal lockdown exit strategies. Int J Infect Dis. 2021;103:579–89. doi: 10.1016/j.ijid.2020.11.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohapatra RK, Pintilie L, Kandi V, et al. The recent challenges of highly contagious COVID-19; causing respiratory infections: symptoms, diagnosis, transmission, possible vaccines, animal models and immunotherapy. Chem Biol Drug Des. 2020;96:1187–1208. doi: 10.1111/cbdd.13761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohapatra RK, Mishra S, Azam M, et al. COVID-19, WHO guidelines, pedagogy, and respite. Open Med. 2021;16:491–493. doi: 10.1515/med-2021-0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohapatra RK, Das PK, Pintilie L, et al. Infection capability of SARS-CoV-2 on different surfaces. Egypt. J Basic Appl Sci. 2021;8(1):75–80. [Google Scholar]
- 5.Mohapatra RK, Perekhoda L, Azam M, et al. Computational investigations of three main drugs and their comparison with synthesized compounds as potent inhibitors of SARS-CoV-2 main protease (Mpro): DFT, QSAR, molecular docking, and in silico toxicity analysis. J King Saud Univ Sci. 2021;33(2):101315. doi: 10.1016/j.jksus.2020.101315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mukherjee A, Anand T, Agarwal A, et al. SARS-CoV-2 re-infection: development of an epidemiological definition from India. Epidemiol Infect. 2021;149:e82. doi: 10.1017/S0950268821000662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menon V, Kar SK, Ransing R, et al. Impending Second Wave of COVID-19 Infections: What India Needs to Do? . Asia Pac J Public Health. 2021;33(4):456–457. doi: 10.1177/1010539521998862. [DOI] [PubMed] [Google Scholar]
- 8.Szarpak L, Chirico F, Pruc M, et al. Mucormycosis-a serious threat in the COVID-19 pandemic? . J Infect. 2021;83(2):237–279. doi: 10.1016/j.jinf.2021.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Claustre J, Larcher R, Jouve T, et al. Mucormycosis in intensive care unit: surgery is a major prognostic factor in patients with hematological malignancy. Ann Intensive Care. 2020;10:74. doi: 10.1186/s13613-020-00673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehta S, Pandey A. Rhino-Orbital Mucormycosis Associated With COVID-19. Cureus. 2020; 12(9):e10726. doi: 10.7759/cureus.10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suvvari TK, Arigapudi N, Kandi V, et al. Mucormycosis: A Killer in the Shadow of COVID-19. J Mycol Med. 2021;31(3):101161. doi: 10.1016/j.mycmed.2021.101161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garg D, Muthu V, Sehgal IS, et al. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia. 2021;186(2):289–298. doi: 10.1007/s11046-021-00528-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verma DK, Bali RK. COVID-19 and Mucormycosis of the Craniofacial skeleton: Causal, Contributory or Coincidental? . J Maxillofac Oral Surg. 2021;20(2):165–166. doi: 10.1007/s12663-021-01547-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The L. India's COVID-19 emergency. The Lancet. 2021;397(10286):1683. doi: 10.1016/S0140-6736(21)01052-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. situation report on India: who; [cited 2021 [Google Scholar]
- 16.COVID-19 Dashboard. Government of India. 2021. Available from: https://www.mygov.in/covid-19.
- 17.Thiagarajan K. Why is India having a covid-19 surge? . BMJ. 2021;373:n1124. doi: 10.1136/bmj.n1124. [DOI] [PubMed] [Google Scholar]
- 18.Kumar S. Second Wave of COVID-19: Emergency Situation in India. J Travel Med. 2021;28(7) doi: 10.1093/jtm/taab082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dhama K, Patel SK, Pathak M, et al. An update on SARS-CoV-2/COVID-19 with particular reference to its clinical pathology, pathogenesis, immunopathology and mitigation strategies. Travel Med Infect Dis. 2020; 37:101755. doi: 10.1016/j.tmaid.2020.101755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arumugam VA, Thangavelu S, Fathah Z, et al. COVID-19 and the World with Co-Morbidities of Heart Disease, Hypertension and Diabetes. J Pure Appl Microbiol. 2020; 14(3):1623–1638. [Google Scholar]
- 21.Choudhary OP, Priyanka, Singh I, et al. Second wave of COVID-19 in India: Dissection of the causes and lessons learnt. Travel Med Infect Dis. 2021;43: 102126. doi: 10.1016/j.tmaid.2021.102126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suvvari TK, Hegde S, Sreeram S, et al. The COVID-19 vaccine: A race nearing the finish line. Apollo Med. 2021;18:111–121. [Google Scholar]
- 23.Kar SK, Ransing R, Arafat SMY, et al. Second wave of COVID-19 pandemic in India: Barriers to effective governmental response. EClinicalMedicine. 2021;36:100915. doi: 10.1016/j.eclinm.2021.100915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghosh A, Nundy S, Mallick TK. How India is dealing with COVID-19 pandemic. Sen Int. 2020; 1 doi: 10.1016/j.sintl.2020.100021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ranjan R, Sharma A, Verma MK. Characterization of the Second Wave of COVID-19 in India. medRxiv. 2021;121(1):85–93. [Google Scholar]
- 26.Mallapaty S. India’s massive COVID surge puzzles scientists. Nature. 2021;592(7856):667–8. doi: 10.1038/d41586-021-01059-y. [DOI] [PubMed] [Google Scholar]
- 27.Sv P, Lathabhavan R, Ittamalla R. What concerns Indian general public on second wave of COVID-19? A report on social media opinions. Diabetes Metab Syndr. 2021; 15(3):829–830. doi: 10.1016/j.dsx.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC, COVID-19 Travel Information. 2021. Available from: https://wwwnc.cdc.gov/travel/destinations/traveler/none/india.
- 29.Sharun K, Tiwari R, Natesan SK, et al. International travel during the COVID-19 pandemic: implications and risks associated with 'travel bubbles'. J Travel Med. 2020; 27(8) doi: 10.1093/jtm/taaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohapatra RK, Das PK, Kandi V. Challenges in controlling COVID-19 in migrants in Odisha. India. Diabetes Metab Syndr. 2020; 14:1593–1594. doi: 10.1016/j.dsx.2020.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samarasekera UU. India grapples with second wave of COVID-19. Lancet Microbe. 2021;2(6):e238. doi: 10.1016/S2666-5247(21)00123-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kannan SR, Spratt AN, Cohen AR, Naqvi SH, Chand HS, Quinn TP, Lorson CL, Byrareddy SN, Singh K. Evolutionary analysis of the Delta and Delta Plus variants of the SARS-CoV-2 viruses. J Autoimmun. 2021; 124: 102715. doi: 10.1016/j.jaut.2021.102715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mishra S, Mindermann S, Sharma M, Whittaker C, Mellan TA, Wilton T, et al. Changing composition of SARS-CoV-2 lineages and rise of Delta variant in England. EClinicalMedicine. 2021;39:101064. doi: 10.1016/j.eclinm.2021.101064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khan MA, Ullah S, Kumar S. A robust study on 2019-nCOV outbreaks through non-singular derivative. Eur Phys J Plus. 2021;136(2):168. doi: 10.1140/epjp/s13360-021-01159-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kandi V. SARS-CoV-2 Genetic Variations, Immunity, and Efficacy of Vaccines: The Current Perspectives and Future Implications. Am J Infect Dis. 2021;9(3):90–97. [Google Scholar]
- 36.Liu C, Ginn HM, Dejnirattisai W, Supasa P, Wang B, Tuekprakhon A, et al. Reduced neutralization of SARS-CoV-2 B.1.617 by vaccine and convalescent serum. Cell. 2021;184(16):4220–36 e13. doi: 10.1016/j.cell.2021.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med . 2021;385(7):585–94. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nemat A, Asady A. The Third Wave of the COVID-19 in Afghanistan: An Update on Challenges and Recommendations. J Multidiscip Health. 2021;14:2043–2045. doi: 10.2147/JMDH.S325696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soriano V, de Mendoza C, Gómez-Gallego F, Corral O, Barreiro P. Third wave of COVID-19 in Madrid, Spain. Int J Infect Dis. 2021;107:212–214. doi: 10.1016/j.ijid.2021.04.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soriano V, Ganado-Pinilla P, Sanchez-Santos M, Gómez-Gallego F, Barreiro P, de Mendoza C, Corral O. Main differences between the first and second waves of COVID-19 in Madrid, Spain. Int J Infect Dis. 2021;105:374–376. doi: 10.1016/j.ijid.2021.02.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Raturi M, Kusum A. The blood supply management amid the COVID-19 outbreak. Transfus Clin Biol. 2020;27(3):147–151. doi: 10.1016/j.tracli.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Riley W, Love K, McCullough J. Public policy impact of the COVID-19 pandemic on blood supply in the United States. Am J Public Health . 2021;111(5):860–866. doi: 10.2105/AJPH.2021.306157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sah R, Rodriguez-Morales AJ, Fathah Z, Shrestha S, Mehta R, Khatiwada AP, et al. Blood scarcity at the blood banks during COVID-19 pandemic and strategies to promote blood donations: current knowledge and futuristic vision. Egypt J Basic Appl Sci. 2021;8(1):261–8. [Google Scholar]
- 44.Leung JNS, Lee CK. Impact of the COVID-19 - a regional blood centre’s perspective. ISBT Sci Ser. 2020;15(4):362–364. [Google Scholar]
- 45.Wang Y, Han W, Pan L, et al. Impact of COVID-19 on blood centres in Zhejiang province China. Vox Sang. 2020;115(6):502–506. doi: 10.1111/vox.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haw J, Holloway K, Masser BM, et al. Blood donation and the global COVID-19 pandemic: areas for social science research. Vox Sang. 2021;116(4):363–365. doi: 10.1111/vox.12974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sachdev S, Kishore K, Singh L, et al. Exploration of COVID-19 related fears deterring from blood donation in India. ISBT Sci Ser. 2021;16 (2):147–157. doi: 10.1111/voxs.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gammon RR, Prichard AB, Gannett MS, et al. The effect of COVID-19 on blood donation habits. Transfusion. 2021;61(4):1134–1140. doi: 10.1111/trf.16278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumar S, Azim D, Nasim S, et al. Dwindling blood reserves: an ominous downside of COVID-19 pandemic. Transfus Apher Sci. 2020;59(5):102818. doi: 10.1016/j.transci.2020.102818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nieto-Calvache AJ, Quintero-Santacruz M, Macia-Mejía C, et al. Dangerous shortage of blood banks as an indirect effect of SARS-CoV-2: an obstetrics perspective. Int J Gynaecol Obstet. 2020;151(3):424–430. doi: 10.1002/ijgo.13409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Al-Riyami AZ, Abdella YE, Badawi MA, et al. The impact of COVID-19 pandemic on blood supplies and transfusion services in Eastern Mediterranean region. Transfus Clin Biol. 2021;28(1):16–24. doi: 10.1016/j.tracli.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stanworth SJ, New HV, Apelseth TO, et al. Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020;7(10):e756–e764. doi: 10.1016/S2352-3026(20)30186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.WHO. WHO COVID-19 Dashboard - Up to date data on pandemic 2021. Availablefrom: https://covid19.who.int/?gclid=CjwKCAiApNSABhAlEiwANuR9YM0k0JigJ56NivXbxLo_GNuUC2W0j79EBV9ZLho5WBFDR7AO8Bt2ihoCqfoQAvD_BwE.
- 54.Blasi F, Gramegna A, Sotgiu G, Saderi L, Voza A, Aliberti S, Amati F. SARS-CoV-2 vaccines: A critical perspective through efficacy data and barriers to herd immunity. Respir Med. 2021;180:106355. doi: 10.1016/j.rmed.2021.106355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dhama K, Sharun K, Tiwari R, Dhawan M, Emran TB, Rabaan AA, et al. COVID-19 vaccine hesitancy - reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Hum Vaccin Immunother. 2021;17(10):3495–9. doi: 10.1080/21645515.2021.1926183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Farooqi T, Malik JA, Mulla AH, Al Hagbani T, Almansour K, Ubaid MA, et al. An overview of SARS-COV-2 epidemiology, mutant variants, vaccines, and management strategies. J Infect Public Health. 2021;14(10):1299–312. doi: 10.1016/j.jiph.2021.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lai CC, Chen IT, Chao CM, Lee PI, Ko WC, Hsueh PR. COVID-19 vaccines: concerns beyond protective efficacy and safety. Expert Rev Vaccines. 2021;20(8):1013–1025. doi: 10.1080/14760584.2021.1949293. [DOI] [PubMed] [Google Scholar]
- 58.Raman R, Patel KJ, Ranjan K. COVID-19: Unmasking Emerging SARS-CoV-2 Variants, Vaccines and Therapeutic Strategies. Biomolecules. 2021;11(7):993. doi: 10.3390/biom11070993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sharun K, Tiwari R, Dhama K, Emran TB, Rabaan AA, Al Mutair A. Emerging SARS-CoV-2 variants: impact on vaccine efficacy and neutralizing antibodies. Hum Vaccin Immunother. 2021;23:1–4. doi: 10.1080/21645515.2021.1923350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schlagenhauf P, Patel D, Rodriguez-Morales AJ, Gautret P, Grobusch MP, Leder K. Variants, vaccines and vaccination passports: Challenges and chances for travel medicine in 2021. Travel Med Infect Dis . 2021; 40:101996. doi: 10.1016/j.tmaid.2021.101996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sharun K, Dhama K. COVID-19 Vaccine Diplomacy and Equitable Access to Vaccines Amid Ongoing Pandemic. Arch Med Res. 2021;52(7):761–3. doi: 10.1016/j.arcmed.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sharma N, Vyas S, Mohapatra A, Khanduri R, Roy P, Kumar R. Combating COVID-19 pandemic in India: Demystifying the concept of herd immunity. J Family Med Prim Care. 2021;10(4):1515–1519. doi: 10.4103/jfmpc.jfmpc_1971_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Snehota M, Vlckova J, Cizkova K, Vachutka J, Kolarova H, Klaskova E, Kollarova H. Acceptance of a vaccine against COVID-19 - a systematic review of surveys conducted worldwide. Bratisl Lek Listy. 2021;122(8):538–547. doi: 10.4149/BLL_2021_086. [DOI] [PubMed] [Google Scholar]
- 64.Tareq AM, Emran TB, Dhama K, Dhawan M, Tallei TE. Impact of SARS-CoV-2 delta variant (B.1.617.2) in surging second wave of COVID-19 and efficacy of vaccines in tackling the ongoing pandemic. Hum Vaccin Immunother. 2021;17(11):4126–7. doi: 10.1080/21645515.2021.1963601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397(10278):1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yan ZP, Yang M, Lai CL. COVID-19 Vaccines: A Review of the Safety and Efficacy of Current Clinical Trials. Pharmaceuticals (Basel) 2021;14(5):406. doi: 10.3390/ph14050406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dhama K, Patel SK, Sharun K, Pathak M, Tiwari R, Yatoo MI, et al. SARS-CoV-2 jumping the species barrier: Zoonotic lessons from SARS, MERS and recent advances to combat this pandemic virus. Travel Med Infect Dis. 2020;37:101830. doi: 10.1016/j.tmaid.2020.101830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Malik YS, Sircar S, Bhat S, Sharun K, Dhama K, Dadar M, Tiwari R, Chaicumpa W. Emerging novel coronavirus (2019-nCoV)-current scenario, evolutionary perspective based on genome analysis and recent developments. Vet Q. 2020;40(1):68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tiwari R, Dhama K, Sharun K, Iqbal Yatoo M, Malik YS, Singh R, Michalak I, Sah R, Bonilla-Aldana DK, Rodriguez-Morales AJ. COVID-19: animals, veterinary and zoonotic links. Vet Q. 2020;40:169–182. doi: 10.1080/01652176.2020.1766725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Banerjee A, Mossman K, Baker ML. Zooanthroponotic potential of SARS-CoV-2 and implications of reintroduction into human populations. Cell Host Microbe. 2021;29:160–164. doi: 10.1016/j.chom.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chavda VP, Feehan J, Apostolopoulos V. A Veterinary Vaccine for SARS-CoV-2: The First COVID-19 Vaccine for Animals. Vaccines (Basel) 2021;9(6):631. doi: 10.3390/vaccines9060631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Karikalan M, Chander V, Mahajan S, Deol P, Agrawal RK, Nandi S, et al. Natural infection of Delta mutant of SARS-CoV-2 in Asiatic lions of India. Transbound Emerg Dis. 2021 doi: 10.1111/tbed.14290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Korath ADJ, Janda J, Untersmayr E, Sokolowska M, Feleszko W, Agache I, Adel Seida A, Hartmann K, Jensen-Jarolim E, Pali-Schöll I. One Health: EAACI Position Paper on coronaviruses at the human-animal interface, with a specific focus on comparative and zoonotic aspects of SARS-Cov-2. Allergy Eur J Allergy Clin Immunol. 2021;2021:1–17. doi: 10.1111/all.14991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sharun K, Dhama K, Pawde AM, Gortazar C, Tiwari R, Bonilla-Aldana DK, et al. SARS-CoV-2 in animals: potential for unknown reservoir hosts and public health implications. Vet Q. 2021;41(1):181–201. doi: 10.1080/01652176.2021.1921311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tass. Russia registers world's first anti-coronavirus vaccine for animals [updated March 31, 2021. Available from: https://tass.com/world/1272331.
- 76.Vandeputte J, Van Damme P, Neyts J, Audonnet JC, Baay M, Neels P. Animal experiments show impact of vaccination on reduction of SARS-CoV-2 virus circulation: A model for vaccine development? Biologicals. 2021;73:1–7. doi: 10.1016/j.biologicals.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


