Abstract
Background
psychotropic medication use has been shown to increase with age and has been associated with increased risk of falls, strokes and mortality. Various guidelines, regulations and tools have been developed to reduce inappropriate prescribing, but this remains high. In order to understand the reasons for this, we aimed to systematically review healthcare professionals’, patients’ and family caregivers’ attitudes towards the use of psychotropic medication in older people.
Methods
a systematic literature search was carried out from inception to September 2020 using PUBMED, EMBASE, PsycINFO and CINAHL and hand-searching of reference lists. Included studies investigated stakeholder views on psychotropic in adults over the age of 65. Findings were thematically synthesised.
Results
overall, there was an acceptance of long-term psychotropic medication for older people both living in the community and in residential care. While healthcare professionals were aware of guidelines for the use of benzodiazepines and psychotropic medicines, they identified barriers to following them on individual, team and organisational levels. Alternative non-pharmacological approaches were not always available or accepted by patients.
Conclusion
psychotropic medicine use in older adults remains a complex issue, which needs to be addressed on a broad level. Attitudes of older people and healthcare professionals encourage long-term use. Meanwhile, various internal and external factors act as barriers to the use of non-drug alternatives in this population. In order to reduce overprescribing of psychotropics, there is a need to increase the acceptability and accessibility of alternative interventions in both care homes and the community.
Keywords: psychotropic medication, professional and patient/lay perspectives, qualitative
Key points
Psychotropic use has been shown to increase with age and has been associated with increased morbidity and mortality.
There is an acceptance of long-term psychotropic use in older people by older people themselves and healthcare professionals.
There are currently many barriers to following guidelines that need to be addressed to reduce inappropriate psychotropic use.
Introduction
Psychotropic medications are commonly used for treating mental illnesses, such as depression and anxiety, where non-pharmacological approaches have failed [1]. In some cases, psychotropic medicines are also used to manage challenging behaviours, such as the behavioural and psychological symptoms of dementia (BPSD) [2].
Psychotropic use has been shown to increase with age [3, 4]. Rates of prescribing are particularly high across care homes, where studies in the Western Europe have shown that up to 63% of residents are prescribed at least one psychotropic drug [5–8]. However, high psychotropic usage has also been noted with older adults in the community [9, 10]. Older adults show greater sensitivity to drugs acting upon the central nervous system and their side effects [11, 12]. In older adults, psychotropic use has been associated with the risk of severe adverse effects such as falls [13–18], stroke [17, 19–22] and mortality [13, 23–25].
A vast number of guidelines and regulations to reduce inappropriate prescribing in older patients have been developed [26–28]. Despite this, some psychotropics are used far longer than recommended or without appropriate, documented reasons [29–31]. Various tools such as screening tool of older people's prescriptions (STOPP)/screening tool to alert to right treatment (START) criteria [32], CQUIN fall prevention resource [33], Beers criteria [34] and psychotropic deprescribing guides [35] have been introduced to tackle some of the associated issues. Education programmes are also a common intervention to reduce inappropriate geriatric prescribing. Examples include the Halting Antipsychotic Use in Long-Term (HALT) study [36], Eliminating Medications Through Patient Ownership of End Results (EMPOWER) study [37] or Reducing Use of Sedatives (RedUSe) project [38]. Despite national policies such as the UK National Dementia Strategy having some effect on antipsychotic prescribing, prescribing of other psychotropics is still relatively common in dementia and other older people [39, 40]. In order to understand the reasons for this, this systematic review aimed to explore stakeholder views and perspectives on the use and issues regarding psychotropic medication use in older adults.
Methods
This systematic review is a synthesis of qualitative and descriptive evidence written following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guidelines [41].
Definitions
For this review, the term older people is defined as adults ≥65 years as in line with NICE guidance [42]. The term ‘doctor’ is the general term used throughout the review for GPs, primary care physicians, psychiatrists and all other physicians. The term ‘family caregiver’ is used throughout to refer to unpaid individuals such as family members providing care for an older person, in comparison with the term ‘carer’ which refers to a paid carers. Stakeholders include older people currently or previously receiving psychotropic treatment, family caregivers, doctors, nursing staff and pharmacists. The term ‘stakeholder’ does not include the public in this review as they are not directly involved or affected by the care of the individual. Psychotropic medications included antidepressants, antipsychotics and anxiolytics.
Search strategy
A comprehensive search strategy was constructed using the population, exposure and outcome framework [43] (Table 1). The electronic databases EMBASE, MEDLINE, CINAHL plus and PsycINFO (via Ovid) were searched from inception to September 2020. Uniform free text terms for each aspect of the research question such as ‘elderly’, ‘opinion’ and ‘psychotropic’ were used and relevant Medical Subject Heading (MeSH) terms were adapted for each database (example in Appendix S1, Supplementary data are available in Age and Ageing online). Reference lists of eligible studies were hand-searched to identify further studies for inclusion.
Table 1.
Summary of population, exposure, outcome (PEO) framework
| Population | Elderly, patient, carer, caregiver, doctor, physician, nurse, family, pharmacist |
| Exposure | Psychotropic medication |
| Outcome | Views |
Inclusion and exclusion criteria
Studies were considered for inclusion if attitudes of stakeholders regarding psychotropic use were specific to the older population (>65 years of age); studies utilised a qualitative, quantitative or mixed-method study design; and full text was available in English. Studies were excluded if they discussed views on the use of psychotropic drugs in people under 65 or across all age groups, focused on attitudes towards psychiatric disorders rather than psychotropic drug treatment or focused on non-pharmacological interventions alone. Studies on non-psychotropic drugs or cholinesterase inhibitors were excluded. Although cholinesterase inhibitors show some psychotropic properties, they are not considered true psychotropic drugs [44]. Studies where views of the public could not be separated from views of the defined stakeholders were excluded; studies not presenting primary data were also excluded.
Selection of studies
All studies were imported into EndNote X9 citation manager and duplicates removed. Titles and abstracts were screened by EB and a 10% sample was screened by SG (Agreement rate 91%). Discrepancies were resolved through discussion. The full texts of all remaining studies were then screened independently by SG and EB and all discrepancies were resolved through discussion.
Quality assessment
The 16-item Quality Assessment Tool for Studies with Diverse Designs (QATSDD) tool was used to appraise the studies, as it could uniformly assess and compare the included studies irrespective of their study design [45]. Higher scores indicated higher quality. Scores were then converted into percentages to allow clear comparison. EB and SG carried out the quality assessment for half the studies each with a 10% overlap as a reliability check (agreement rate was 93%). Studies were not excluded due to their quality, rather, they were used to show how the studies compare to each other in terms of risk of bias, consistency, transparency and organised reporting.
Data extraction
Data extracted included key aspects of the study including study design, aims, treatment class, indication, participating stakeholders, patient group (older or mean age where stated), setting, method, analysis and main findings. EB and SG extracted data for half of the studies each with a 10% overlap as a reliability check. SG suggested some minor changes that EB then applied to the full data set. Data extracted included first-order interpretations (direct participant quotes and quantitative data) and second-order interpretations (the authors’ interpretations), both of which were considered primary data. Further care was taken to ensure quotations were not taken out of context. This was done by keeping in mind the authors’ interpretations to avoid drawing conclusions from incomplete sets of interview data.
Data synthesis
Thematic synthesis was used to synthesise new findings beyond the existing literature in the included studies, as per Cochrane recommendation for qualitative evidence synthesis [46]. Firstly, all transcripts were re-read to fully immerse in the data as recommended [47]. EB carried out inductive line-by-line coding for each study, where the meaning of the text was simply summarised. Duplicate or similar codes were merged, and related codes grouped to form descriptive themes. Descriptive themes summarised first-level codes by looking at similarities and differences between them. These descriptive themes remained close to primary studies [48]. In the third stage, higher-order analytical themes were developed by EB to answer the review question. This was done by interpreting, examining relationships between and extrapolating descriptive themes into ‘third-order interpretations’ to synthesise new findings. This was done iteratively until no new themes were identified while consistently looking back at the original data and its’ context. Coding for 10% of the studies was assessed by a second reviewer and any discrepancies resolved through discussion (S.G.).
Due to the diverse nature of this review, heterogenicity of the data and study designs, meta-analyses were not carried out [41].
Results
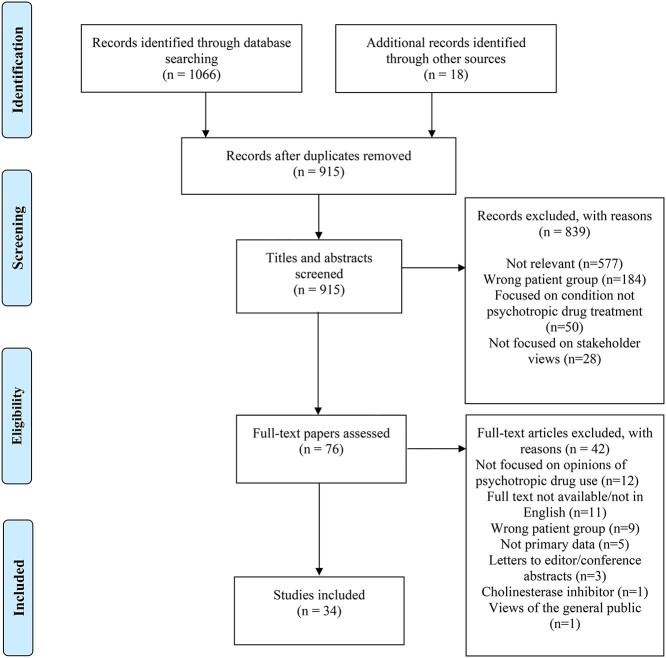
In total, 34 studies were included in this review (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram [41].
Study characteristics
Overall, the review included 3,398 stakeholders: 2,712 healthcare and care home staff, 631 older people and 55 family caregivers. Eighteen quantitative studies, 16 qualitative studies and 2 mixed-method studies were included in this review. The summary of study characteristics of included studies is presented in Table 2 and the full data extraction table in Appendix S2, Supplementary data are available in Age and Ageing online. The most frequent indications for psychotropic prescribing were depression in nine studies [50, 51, 55, 56, 60, 62, 73, 74, 82], sleeping disorders in seven [54–56, 59, 63, 74, 82] and anxiety in six [54–56, 73, 74, 82]. In seven studies, psychotropic medication was used to manage behaviours and BPSD [49, 53, 57, 63, 65, 80, 81].
Table 2.
Overview of summary characteristics of included studies
| Study and country | Study design | Participants | Setting | Treatment class |
|---|---|---|---|---|
| Aerts et al. [49], Australia | Mixed-methods | 27 nursing staff, 22 GPs, 21 family caregivers | Residential care | Antipsychotics |
| Bogner et al. [50], United States | Interviews | 102 older primary care patients | Community | Antidepressants |
| Boyle and Chambers [51], Ireland | Focus groups | 7 family caregivers | Antidepressants | |
| Bourgeois et al [52], Belgium | CS survey | 25 GPs and 16 nurses | Residential care | Benzodiazepines |
| Cohen-Mansfield et al. [53], United States | Interviews | 7 long term-care physicians, 1 nurse | Residential care | Antipsychotics |
| Cook et al. [54], United States | Interviews | 33 primary care physicians | Community | Benzodiazepines |
| Cook et al. [55], United States | Interviews | 50 older benzodiazepine users | Community | Benzodiazepines |
| Damestoy et al. [54], Canada | Interviews | 9 primary care physicians | Community | Benzodiazepines, antidepressants anxiolytics |
| Dickinson et al. [56], England | Interviews | 36 long-term depressed patients, 10 GPs | Community | Antidepressants |
| Ervin et al. [57], Australia | Mixed-methods | 130 nurses | Residential care | Antipsychotics |
| Fitch et al. [58], Canada | CS survey | 487 general practitioners | Community | Antidepressants |
| Flick et al. [59], Germany | Interviews | 20 nursing home doctors | Residential care | Benzodiazepines |
| Givens et al. [60], United States | Interviews | 68 geriatric patients | Community | Antidepressants |
| Glasspoole and Aman [61], New Zealand | CS survey | 44 nurses, 29 administrators | Hospital and residential care | Psychotropics, not further defined |
| Iden et al. [62], Norway | Focus groups, interviews | 16 GPs working in nursing homes, 8 nurses | Residential care | Antidepressants |
| Jacobson and Winograd [63], United States | Interviews | 6 physicians, 14 nursing staff, 14 patients | Residential care | Antipsychotics, anxiolytics, antidepressants |
| Janus et al. [64], Netherlands | CS survey | 81 nurses and nursing assistants | Residential care | Antipsychotics |
| Kerns et al. [65], United States | Interviews | 12 nurses, 20 family caregivers | Community and residential care | Antipsychotics |
| Kuruvilla et al. [66], United States | Interviews | 100 patients | Hospital and community | Antidepressants |
| Kwasny [67], Canada | CS survey | 140 nurses | Acute inpatient | Major and minor tranquilisers |
| Lemay et al. [68], United States | CS survey | 138 nursing home leaders and 779 direct care staff | Residential care | Antipsychotics |
| Lesen et al. [69], Sweden | Interviews | 44 patients who had attempted suicide | Acute inpatient | Antidepressants |
| Lu et al. [70], Australia | CS survey | 135 patients with depression | Outpatients | Antidepressants |
| Lyndon and Russell [71], Australia | Interviews | 45 patients | Benzodiazepines, antidepressants | |
| Mort et al. [72], United States | CS survey | 314 nurses | Residential care | Psychotropics |
| Oehlberg et al. [73], United States | Interviews | Older patients with depression | Community | Antidepressants |
| Perodeau et al. [74], Canada | Interviews | 21 frail older women, 14 female family caregivers | Community | Antipsychotics, benzodiazepines |
| Prabhakaran and Butler [75], United Kingdom | Interviews | 118 patients | Hospital in/outpatients | Antidepressants |
| Rej et al. [76], Netherlands | CS survey | 68 patients with bipolar disorder | Community | Psychotropics |
| Shaw [77], United Kingdom | Interviews | 49 nursing home staff and 8 GPs | Residential care | ‘Psychoactive medicines’ |
| Svarstad et al. [78], United States | L survey | 191 nurses | Residential care | Antipsychotics, |
| Tiller et al. [79], Australia | CS survey | 57 psychiatric doctors | Inpatients | Antipsychotics |
| Walsh et al. [80], Canada | Interviews | 8 nurses | Inpatient acute | Antipsychotics |
| Walsh et al. [81], England | Interviews | 8 nurses, 5 GPs, 5 healthcare assistants, 4 geriatricians,3 family caregivers, 2 pharmacists | Residential care | Antipsychotics |
CS, cross sectional, L, longitudinal.
Quality assessment
The quality assessment scores of studies ranged between 31 and 100%. A full breakdown of the quality assessment of included studies is available (Appendix S3, Supplementary data are available in Age and Ageing online).
Thematic synthesis
Four themes were identified from the primary studies: acceptance of long-term psychotropic medication, risk benefit assessment, best practice versus actual practice and organisational factors. All these overall themes were relevant in both community and residential settings. However, some of the specific examples and subthemes were more relevant to the residential setting. In addition, the class of medicines discussed varied between setting with antipsychotics being more commonly researched in residential settings and benzodiazepines and antidepressants being more commonly researched in the community.
Acceptance of long-term use of psychotropic medication in older people
Ageing was seen as a negative experience by many participants; being commonly associated with social, physical and emotional decline such as ill-health, loss of autonomy and bereavement [50, 56, 74, 82]. Both doctors and patients shared the belief that older people were largely ‘set in their ways’ [55, 56, 82]. Doctors anticipated resistance to discontinuation of psychotropic medication or introduction of non-pharmacological interventions and older patients expressed the view that they did not wish to ‘experiment’ at their age by tapering or discontinuing their psychotropic medication [54–56, 59]. Doctors indicated that they did not necessarily agree with or promote long-term use in; however, they discussed being more tolerant of long-term use in older people [54, 56, 59]. Both doctors and older people expressed the view that psychotropic medication was at times used as a ‘crutch’, where taking the medication, even at a very low dose, provided emotional comfort and helped keep the patient on an ‘even keel’ [56, 74]. Family caregivers, nursing staff and doctors all expressed fear of threatening older people’s stable condition. Negative effects experienced by patients during prior attempts to discontinue were also reported to discourage further attempts [54–56, 74]. Doctors expressed being much more careful initiating psychotropic treatment compared to providing repeats for long-term use [59, 81, 82]. Meanwhile, patients were of the view that they trusted prescribers and had confidence in them that if they prescribed medication it was appropriate for them [55, 56, 74]. However, family caregivers had a differing view to other stakeholders in this area and did not always feel that their concerns were listened to by healthcare professionals [51, 65].
Risk benefit assessment
A range of benefits of psychotropic medicines were identified by patients, family caregivers and healthcare professionals including enabling normal functioning of patients [55, 56], allowing family caregivers and healthcare professionals to feel that they were doing something to help [51, 74], treating sleep disorders [49, 53, 55, 56, 59, 63, 80], managing aggressive and agitated behaviour and maintaining health and safety [49, 53, 57, 65, 80, 81]. Findings suggested that there was variation with medication class with antipsychotics being seen by healthcare professionals as a last resort, but benzodiazepines being prescribed more freely [59]. Findings also suggested differences between healthcare professional groups with nurses seeming more likely than doctors to encourage use of psychotropic medicines in some situations [62, 81]. Some doctors expressed the view that prescribing medication to aid sleep helped care home staff more than care home residents and preferred alternative approaches such as giving space to residents to wander safely at night [53, 59, 63, 80]. They reported being in a challenging situation trying to minimise inappropriate prescribing while having to stay conscious of the risk to and safety of nursing home staff, carers and other residents [53, 81].
Older people, family caregivers and healthcare professionals also expressed concerns about psychotropic medication including side effects [49, 53, 55, 59, 60, 65, 81], potential for addiction [60, 73] and stigma [73]. One study found that nurses reported side effects more frequently than both older people and doctors [63]. Some older people felt medication did not address the root of their problem and was only a ‘partial fix’ [50, 51, 56, 60, 74]. However, side effects associated with psychotropic medication were also minimised by some older people, doctors and family members [54–56, 59, 63, 65, 74, 81, 82]. Some older people referred to their psychotropic medication as a stable, low dose or a ‘small pill’ [55]. Some doctors were also of the view that older people had a low potential for abuse and minimised or accepted the risks of addiction [54, 59, 74, 82]. However, in the study, comprising views of psychiatrists’ adverse events in older people were frequently reported as a barrier to prescribing [79].
Doctors and nurses were of the view that assessing whether psychotropic medication was appropriate in older people was challenging [49, 53–56, 62, 65, 80–82]. Difficulties that were identified included: establishing a clear diagnosis [56, 62], communication difficulties [56, 80] and the increased sensitivity to the side effects of psychotropic medication in older people. Doctors and nurses were of the view that greater vigilance was necessary for this population. Prescribing seemed to occur where doctors believed the overall benefits of initiating or maintaining use outweighed the harms. Many doctors referred to the process of a risk–benefit analysis [53–56, 59, 65, 82]. The importance of a holistic assessment of any underlying needs such as pain or constipation which may be causing distress was also highlighted by healthcare professionals [49, 53, 57, 80, 81]. However, nurses and doctors’ opinions to treat differed at times. Nurses sometimes expressed frustration with the fact that prescribers were not always present when residents were most agitated [63, 65]. Nurses were identified as the main driver of prescribing [49, 62, 81]. Nurses’ knowledge of their patients seemed to both promote and prevent psychotropic use. Knowing the residents helped nurses understand behaviours and provide individualised non-drug interventions which better addressed the patients’ needs [53]. However, anticipating resident’s behaviour also sometimes led to pre-emptively treating behaviours with less assessment of underlying needs [81]. Glasspoole and Aman found that the majority of nurses wanted to be more involved in decisions regarding antipsychotic medicines and weighted nursing notes and observations more highly than standardised assessments [61].
Best practice versus actual practice
Doctors seemed to generally express awareness and agreement with current guidelines for psychotropic use, such as prescribing benzodiazepines for short-term treatment of specific indications only. However, some doctors criticized guidelines as being ‘out of touch’ with real-world problems and practice and discussed how over-regulation of psychotropic medication did not necessarily improve care [53, 54, 81]. Other prescribers and nursing staff believed regulation and guidelines helped inform and evaluate their decision-making [81]. However, they also identified that they did not always follow them in practice. Some were of the view that medication reviews could help identify inappropriate use while acknowledging that these were not always carried out [49, 55, 56, 62].
Stakeholders suggested that further education regarding psychotropic medicines was needed to increase their appropriate use, discontinuation and the uptake of non-pharmacological interventions [52]. Doctors believed that nurses with a better understanding of BPSD, non-drug interventions and the risks and benefits of psychotropic medication may be less likely to request drug treatment [53, 62, 80, 81]. In addition, some doctors expressed feeling out of their comfort zone, particularly when persuading older people to discontinue their psychotropic medication [56, 81].
Organisational factors
Time and staff constraints
A recurring theme across studies was that lack of time was a barrier to deprescribing. Addressing psychotropic use was considered difficult and time-consuming by doctors, with psychotropic discontinuation requiring more time than other medication [54, 56, 57, 59]. Doctors believed older people discontinuing psychotropic medication were likely to require more support, which may not always be easily available. In addition, nurses stated that the time needed to complete day-to-day tasks left them with little time to interact with residents or provide them with recreational activities for example involving arts and crafts, pets and home activities [53, 81]. Prescribing for staff-orientated needs was not considered good practice. However, doctors and nurses acknowledged the use of psychotropics such as antipsychotics or benzodiazepines helped manage nurse workload by managing the resident’s BPSD or insomnia [59, 80, 81].
Treatment culture and hierarchies
Treatment culture and hierarchy was particularly relevant in residential care home settings. Pharmacists and nursing assistants in one study described a perceived hierarchy in nursing home environments, with decision-making largely between doctors and nurses [81]. Some stakeholders stated that doctors often relied on nurses’ judgement to inform decision-making, with little mention of other staff involved in the older people’s care [62, 80, 81]. Doctors believed treatment cultures could impact prescribing. If nursing home environments were more suited for the needs of the residents and less task orientated, there may be less of a need to prescribe [53, 81]. In a longitudinal study, greater reductions in the use of antipsychotic drugs over time were found in facilities with a resident-centred culture, a less severe case mix and a higher nurse-to-resident staffing ratio [76].
Barriers to non-pharmacological treatments
While recognising non-pharmacological alternatives as the gold standard, barriers to their use were identified by doctors and nurses. These included lack of time, training, funding, accessibility, volunteers or other resources [53, 54, 56, 59, 65, 81], and older people not wishing to try psychological interventions [54–56]. However, older people expressed being more open to social interventions [53, 56, 59]. Where older people rejected interventions such as bereavement counselling, doctors expressed a lack of alternatives [54–56, 80]. Doctors also acknowledged difficulty treating social and emotional causes of depression, anxiety or insomnia. Family events, loneliness, ill health or bereavement were commonly at the root of these issues [56, 74]. Doctors felt psychotropic medications could help alleviate some symptoms; however, addressing psychosocial problems required non-drug interventions. Doctors however reported not always being able to provide these due to time, structural and other factors. Some doctors felt unease prescribing psychotropic medication solely for older peoples’ social issues, such as loneliness from the loss of a spouse or isolation, and some nurses also agreed that taking time to explore social aspects of older people’s lives and employ non-drug interventions could reduce the need for medication.
Discussion
There are several personal and external factors influencing the use of psychotropic drugs in older people. The acceptance of long-term use in this population is a prominent theme of this review. Many older people possess negative beliefs regarding their ability to get better and their suitability for non-drug approaches. Older people, healthcare professionals and family caregivers express fear of negative consequences of discontinuation, which often leads to prolonged use of psychotropic medication, despite no longer being clinically appropriate or necessary. Side effects and addiction in this population are commonly minimised by stakeholders. This may partly be due to some groups of patients being unable to express the side effects that they are experiencing. Nurses appear to have a large influence on prescribing of psychotropics in residential care. Nonetheless, psychotropic drugs, antipsychotics in particular, are highlighted to be the last resort showing awareness of the need for appropriate use. Although many doctors feel unease prescribing for social issues of older people, they often feel they have little choice due to situatedness pressures, including patient, environmental and organisational factors. These factors led to a discordance between best and actual practice and the medicalisation of conditions that may not have needed drug treatment if tailored non-pharmacological interventions were available.
There is a distinction in views regarding prescribing antipsychotic agents in comparison with other psychotropic medication. The initiation and long-term use of antidepressants, hypnotics and anxiolytics seem to be more accepted by staff, family caregivers and patients in comparison with the initiation of antipsychotic agents. In addition, psychiatrists showed preference for atypical antipsychotics over typical antipsychotic drugs in terms of safety and clinical usefulness.
Comparison with existing literature
The findings of this review help explain the findings of previous studies that have shown high rates of inappropriate psychotropic prescribing in older people both in care homes [4–7] and wider settings [83]. While some studies have shown a decrease in the prescribing of some drug classes, such as benzodiazepines over time [83, 84], these decreases have been small and inconsistent across different countries [85, 86]. Various guidelines have been developed to support appropriate psychotropic use, barriers exist in practice. However, more focus on increasing accessibility and acceptability of alternative non-pharmacological treatments is necessary to reduce inappropriate prescribing of psychotropic medication. Previous research has also shown that country of residence is more important than clinical factors in determining psychotropic use and this also suggests that prescribing habits, social, cultural, behavioural and regulatory factors play an important role [8, 87]. Many of our findings are also consistent with general themes relating to medication use in older people found in previous studies. They include negative self-perceptions of ageing with declining health, more perceived barriers to care [88–90] and high levels of general inappropriate prescribing in residential homes [91].
Strengths and limitations
The number of studies included in this review covered the views of an overall large number of participants, giving a good insight into a range of stakeholder views. However, excluding papers not available in English may have excluded useful studies. Evidence on the effects of language bias is inconclusive [92–95], but it is of note that all the included studies were from North America, Australia and Europe. Current tools for studies with diverse designs such as QATSDD can be difficult to apply, with some indicators being rather subjective. While thematic synthesis can be used with both ‘thick’ and ‘thin’ data, it is the ‘thicker’ data with higher levels of conceptual detail, which develop descriptive themes into more in-depth analytic themes [46]. Some of the included studies provided more conceptually poor or ‘thin’ data, which resulted in less contribution to the final analysis in comparison with studies which had richer results. This may have limited some of the findings of the thematic synthesis. In addition, the studies varied greatly in quality. However, the consistency of themes identified across studies suggests cumulative validity of the findings.
Implications for research and practice
Time constraints are a clear barrier to addressing long-term use of psychotropic medication in older adults. Where utilised, psychotropic reviews have been useful, reducing prescribing rates by 28–82% [36, 96, 97]. The implementation of pharmacist-led psychotropic reviews could be a suitable intervention to ensure older people taking these medicines are regularly reviewed. Utilising general practice and care home pharmacists could address psychotropic use and discontinuation. Family caregivers should be involved in shared decision-making about psychotropic medication where appropriate as our findings show that they did not always feel that their concerns are addressed adequately. Further research quantifying the health and patient need, as well as the effectiveness of the service on improving patient outcomes is necessary. However, without non-pharmacological support, discontinuation can be detrimental to older people’s quality of life [96]. To help ease the fear of discontinuation and perceived necessity for psychotropics, there is a clear need for further research into tailoring psychosocial supportive approaches to older people, encouraging participation and implementing individualised care in care homes by educating nursing staff. Taking into account the various barriers to non-pharmacological interventions, more needs to change on a systemic level to reduce the need for psychotropic medication. With loneliness, negative life events and losses commonly at the root of psychotropic prescribing, research into how to best provide non-drug interventions tailored to older peoples’ needs is necessary to reduce patient and staff reliance on psychotropic medication.
There is less research on the views and experiences of family caregivers compared to other groups and future research should focus more on this group. In addition, only one study included psychiatrists, and this was limited to the inpatient setting. No studies compared the opinions of psychiatrists with general practitioners and other healthcare professionals. This is an important area for future research due to psychiatrists’ expertise and possibly different levels of situational pressures to general practitioners. Such research should focus on the role of psychiatrists in both inpatient and outpatient settings and incorporate their views on time and resources available. The interactions between psychiatrists and other members of the healthcare team regarding psychotropic use in older adults should also be explored.
Conclusion
Psychotropic use in older adults remains a complex issue which requires addressing on a wider level. Attitudes of patients and other stakeholders encourage long-term use as well as organisational factors. Findings of this study provide the groundwork to support the development of alternative interventions, improving care in both care homes and the community.
Supplementary Material
Acknowledgements
This work was supported by the National Institute for Health Research (NIHR) Imperial Patient Safety Translational Research Centre. This report presents independent research. The views expressed in this publication are those of the authors, not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
None.
References
- 1. National Institute for Health and Care Excellence (NICE) . First-Choice Antidepressant Use in Adults with Depression or Generalised Anxiety Disorder Key Therapeutic Topic [KTT8]. nice.org.uk/guidance/ktt8(2 January 2021, date last accessed).
- 2. National Institute for Health and Care Excellence (NICE) . Antipsychotics in People Living with Dementia [KTT7]. https://www.nice.org.uk/advice/ktt7(2 January 2021, date last accessed).
- 3. Brett J, Pearson S-A, Daniels B, Wylie CE, Buckley NA. A cross sectional study of psychotropic medicine use in Australia in 2018: a focus on polypharmacy. Br J Clin Pharmacol 2021; 87: 1369–77. [DOI] [PubMed] [Google Scholar]
- 4. Percudani M, Barbui C, Fortino I, Petrovich L. Antidepressant drug prescribing among elderly subjects: a population-based study. Int J Geriatr Psychiatry 2005; 20: 113–8. [DOI] [PubMed] [Google Scholar]
- 5. Dempsey O, Moore H. Psychotropic prescribing for older people in residential care in the UK, are guidelines being followed? Prim Care Community Psychiatry 2005; 10: 13–8. [Google Scholar]
- 6. Grill P, Marwick C, de Souza N, Burton JK, Hughes C, Guthrie B. The burden of psychotropic and anticholinergic medicines use in care homes: population-based analysis in 147 care homes. Age Ageing 2021; 50: 183–9. [DOI] [PubMed] [Google Scholar]
- 7. Smeets CHW, Gerritsen DL, Zuidema SUet al. Psychotropic drug prescription for nursing home residents with dementia: prevalence and associations with non-resident-related factors. Aging Ment Health 2018; 22: 1239–46. [DOI] [PubMed] [Google Scholar]
- 8. Janus SI, Manen JG, IJzerman MJ, Zuidema SU. Psychotropic drug prescriptions in western European nursing homes. Int Psychogeriatr 2016; 28: 1775–90. [DOI] [PubMed] [Google Scholar]
- 9. Voyer P, Martin LS. Improving geriatric mental health nursing care: making a case for going beyond psychotropic medications. Int J Ment Health Nurs 2003; 12: 11–21. [DOI] [PubMed] [Google Scholar]
- 10. Bajracharya R, Qato DM. Patterns of psychoactive medication use in community-dwelling older adults in the US in 2016: a descriptive cross-sectional study. J Aging Health 2021; 33: 86–100. [DOI] [PubMed] [Google Scholar]
- 11. Shi S, Mörike K, Klotz U. The clinical implications of ageing for rational drug therapy. Eur J Clin Pharmacol 2008; 64: 183–99. [DOI] [PubMed] [Google Scholar]
- 12. Varma S, Sareen H, Trivedi JK. The geriatric population and psychiatric medication. Mens Sana Monogr 2010; 8: 30–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnell K, Jonasdottir Bergman G, Fastbom Jet al. Psychotropic drugs and the risk of fall injuries, hospitalisations and mortality among older adults. Int J Geriatr Psychiatry 2017; 32: 414–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Izza MAD, Lunt E, Gordon AL, Gladman JRF, Armstrong S, Logan P. Polypharmacy, benzodiazepines, and antidepressants, but not antipsychotics, are associated with increased falls risk in UK care home residents: a prospective multi-Centre study. Eur Geriatr Med 2020; 11: 1043–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Seppala LJ, Wermelink AMAT, Vries Met al. Fall-risk-increasing drugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc 2018; 19: 371.e11–7. [DOI] [PubMed] [Google Scholar]
- 16. Janus SIM, Reinders GH, Manen JGet al. Psychotropic drug-related fall incidents in nursing home residents living in the eastern part of the Netherlands. Drugs R&D 2017; 17: 321–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Richardson K, Loke YK, Fox Cet al. Adverse effects of Z-drugs for sleep disturbance in people living with dementia: a population-based cohort study. BMC Med 2020; 18: 351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Díaz-Gutiérrez MJ, Martínez-Cengotitabengoa M, Sáez de Adana Eet al. Relationship between the use of benzodiazepines and falls in older adults: a systematic review. Maturitas 2017; 101: 17–22. [DOI] [PubMed] [Google Scholar]
- 19. Hsu WT, Esmaily-Fard A, Lai CCet al. Antipsychotics and the risk of cerebrovascular accident: a systematic review and meta-analysis of observational studies. J Am Med Dir Assoc 2017; 18: 692–9. [DOI] [PubMed] [Google Scholar]
- 20. Gill SS, Rochon PA, Herrmann Net al. Atypical antipsychotic drugs and risk of ischaemic stroke: population based retrospective cohort study. BMJ 2005; 330: 445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zivkovic S, Koh CH, Kaza N, Jackson CA. Antipsychotic drug use and risk of stroke and myocardial infarction: a systematic review and meta-analysis. BMC Psychiatry 2019; 19: 189–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Szmulewicz AG, Angriman F, Pedroso FE, Vazquez C, Martino DJ. Long-term antipsychotic use and major cardiovascular events: a retrospective cohort study. J Clin Psychiatry 2017; 78: e905–12. [DOI] [PubMed] [Google Scholar]
- 23. Maust DT, Kim HM, Seyfried LSet al. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiat 2015; 72: 438–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA 2005; 294: 1934–43. [DOI] [PubMed] [Google Scholar]
- 25. Jennum P, Baandrup L, Iversen HK, Ibsen R, Kjellberg J. Mortality and use of psychotropic medication in patients with stroke: a population-wide, register-based study. BMJ Open 2016; 6: e010662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. National Institute for Health and Care Excellence (NICE) . Dementia: Assessment, Management and Support for People Living with Dementia and Their Carers NICE Guidance [NG97]. https://www.nice.org.uk/guidance/ng97(2 January 2021, date last accessed). [PubMed]
- 27. Reus VI, Fochtmann LJ, Eyler AEet al. The American Psychiatric Association practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia. Am J Psychiatry 2016; 173: 543–6. [DOI] [PubMed] [Google Scholar]
- 28. Keltner NL, Folks DG. The omnibus budget reconciliation act: impact on psychotropic drug use in long-term care facilities. Perspect Psychiatr Care 1995; 31: 30–3. [DOI] [PubMed] [Google Scholar]
- 29. Lornstad MT, Aarøen M, Bergh S, Benth JŠ, Helvik AS. Prevalence and persistent use of psychotropic drugs in older adults receiving domiciliary care at baseline. BMC Geriatr 2019; 19: 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Royal College of Psychiatrists . National Audit of Dementia: Prescription of Psychotropic Medication Initiated in Hospital for Behavioural and Psychological Symptoms of Dementia. https://www.rcpsych.ac.uk/docs/default-source/improving-care/ccqi/national-clinical-audits/national-audit-of-dementia/r4-resources/spotlight/nad-spotlight-report-feb2020.pdf?sfvrsn=6a86cfbd_2(2 January 2021, date last accessed).
- 31. Sgnaolin V, Engroff P, Andrade CPet al. Patterns of chronic benzodiazepine use in the elderly. Arch Clin Psychiatr 2016; 43: 79–82. [Google Scholar]
- 32. O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 2015; 44: 213–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Commissioning for Quality and Innovation (CQUIN) . CCG7: Three High Impact Actions to Prevent Hospital Falls. https://improvement.nhs.uk/documents/5335/Falls_CQUIN_FAQ_Final.pdf(02 January 2021, date last accessed).
- 34. American Geriatrics Society . American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019; 67: 674–94. [DOI] [PubMed] [Google Scholar]
- 35. New South Wales Therapeutic Advisory Group . DeprescribingTools. https://www.nswtag.org.au/deprescribing-tools/(2 January 2021, date last accessed).
- 36. Brodaty H, Aerts L, Harrison Fet al. Antipsychotic deprescription for older adults in long-term care: the HALT study. J Am Med Dir Assoc 2018; 19: 592–600.e7. [DOI] [PubMed] [Google Scholar]
- 37. Tannenbaum C, Martin P, Tamblyn Ret al. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med 2014; 174: 890–8. [DOI] [PubMed] [Google Scholar]
- 38. Breen J, Jackson S, Gee Pet al. An effective approach to decrease antipsychotic and benzodiazepine use in nursing homes: the RedUSe project. Int Psychogeriatr/IPA 2009; 22: 26–36. [DOI] [PubMed] [Google Scholar]
- 39. Szczepura A, Wild D, Khan AJet al. Antipsychotic prescribing in care homes before and after launch of a national dementia strategy: an observational study in English institutions over a 4-year period. BMJ Open 2016; 6: e009882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kales HC, Gitlin LN, Lyketsos CG. When less is more, but still not enough: why focusing on limiting antipsychotics in people with dementia is the wrong policy imperative. J Am Med Dir Assoc 2019; 20: 1074–9. [DOI] [PubMed] [Google Scholar]
- 41. Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. National Institute for Health and Care Excellence (NICE) . Older People: Independence and Mental Wellbeing NICE Guideline [NG32] https://www.nice.org.uk/guidance/ng32(2 January 2021, date last accessed).
- 43. City University of London . Doing Postgraduate Research. https://libguides.city.ac.uk/postgraduate_research(02 January 2021, date last accessed).
- 44. Cummings JL. Cholinesterase inhibitors: a new class of psychotropic compounds. Am J Psychiatry 2000; 157: 4–15. [DOI] [PubMed] [Google Scholar]
- 45. Sirriyeh R, Lawton R, Gardner Pet al. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract 2012; 18: 746–52. [DOI] [PubMed] [Google Scholar]
- 46. Noyes J BA, Cargo M, Flemming K, Harden A, Harris J, Garside R, Hannes K, Pantoja T, Thomas J. Chapter 21: Qualitative Evidence. https://training.cochrane.org/cochrane-handbook-systematic-reviews-interventions(2 January 2021, date last accessed).
- 47. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 48. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Aerts L, Cations M, Harrison Fet al. Why deprescribing antipsychotics in older people with dementia in long-term care is not always successful: insights from the HALT study. Int J Geriatr Psychiatry 2019; 34: 1572–81. [DOI] [PubMed] [Google Scholar]
- 50. Bogner HR, Cahill E, Frauenhoffer C, Barg FK. Older primary care patient views regarding antidepressants: a mixed methods approach. J Ment Health 2009; 18: 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Boyle E, Chambers M. Medication compliance in older individuals with depression: gaining the views of family carers. J Psychiatr Ment Health Nurs (Wiley-Blackwell) 2000; 7: 515. [DOI] [PubMed] [Google Scholar]
- 52. Bourgeois J, Elseviers MM, Azermai Met al. Barriers to discontinuation of chronic benzodiazepine use in nursing home residents: perceptions of general practitioners and nurses. Eur Geriatr Med 2014; 5: 181–7. [Google Scholar]
- 53. Cohen-Mansfield J, Lipson S, Patel Jet al. Wisdom from the front lines: clinicians’ descriptions of treating agitation in the nursing home, a pilot study. J Am Med Dir Assoc 2005; 6: 257–64. [DOI] [PubMed] [Google Scholar]
- 54. Cook JM, Marshall R, Masci C, Coyne J. Physicians’ perspectives on prescribing benzodiazepines for older adults: a qualitative study. Soc Gen Intern Med 2007; 22: 303–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cook JM, Biyanova T, Masci C, Coyne J. Older patient perspectives on long-term anxiolytic benzodiazepine use and discontinuation: a qualitative study. Soc Gen Intern Med 2007; 22: 1094–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Dickinson R, Knapp P, House AOet al. Long-term prescribing of antidepressants in the older population: a qualitative study. Br J Gen Pract 2010; 60: e144–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ervin K, Finlayson S, Cross M. The management of behavioural problems associated with dementia in rural aged care. Collegian 2012; 19: 85–95. [DOI] [PubMed] [Google Scholar]
- 58. Fitch K, Molnar FJ, Power Bet al. Antidepressant use in older people: family physicians' knowledge, attitudes, and practices. Can Fam Physician 2005; 51: 81–1. [PMC free article] [PubMed] [Google Scholar]
- 59. Flick U, Garms-Homolová V, Röhnsch G. “And mostly they have a need for sleeping pills”: Physicians' views on treatment of sleep disorders with drugs in nursing homes. J Aging Stud 2012; 26: 484–94. [DOI] [PubMed] [Google Scholar]
- 60. Givens JL, Datto CJ, Ruckdeschel Ket al. Older Patients' aversion to antidepressants: a qualitative study. J Gen Intern Med 2006; 21: 146–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Glasspoole LA, Aman MG. Attitudes and knowledge of gerontological nurses toward psychotropic drugs. Gerontologist 1988; 28: 667–71. [DOI] [PubMed] [Google Scholar]
- 62. Iden KR, Hjørleifsson S, Ruths S. Treatment decisions on antidepressants in nursing homes: a qualitative study. Scand J Prim Health Care 2011; 29: 252–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Jacobson DH, Winograd CH. Psychoactive medications in the long-term care setting: differing perspectives among physicians, nursing staff, and patients. J Geriatr Psychiatry Neurol 1994; 7: 176–83. [DOI] [PubMed] [Google Scholar]
- 64. Janus SI, Manen JG, IJzerman MJ, Bisseling M, Drossaert CHC, Zuidema SU. Determinants of the nurses' and nursing assistants' request for antipsychotics for people with dementia. Int Psychogeriatr 2017; 29: 475–84. [DOI] [PubMed] [Google Scholar]
- 65. Kerns JW, Winter JD, Winter KM, Kerns CC, Etz RS. Caregiver perspectives about using antipsychotics and other medications for symptoms of dementia. Gerontologist 2018; 58: e35–45. [DOI] [PubMed] [Google Scholar]
- 66. Kuruvilla T, Fenwick CD, Haque MSet al. Elderly depressed patients: what are their views on treatment options? Aging Ment Health 2006; 10: 204–6. [DOI] [PubMed] [Google Scholar]
- 67. Kwasny P, Hagen B, Armstrong-Esther C. Use of major and minor tranquilizers with older patients in an acute care hospital: an exploratory study. J Adv Nurs 2006; 55: 135–41. [DOI] [PubMed] [Google Scholar]
- 68. Lemay CA, Mazor KM, Field TSet al. Knowledge of and perceived need for evidence-based education about antipsychotic medications among nursing home leadership and staff. J Am Med Dir Assoc 2013; 14: 895–900. [DOI] [PubMed] [Google Scholar]
- 69. Lesén E, Wiktorsson S, Carlsten A, Waern M, Hedenrud T. Beliefs about antidepressants among persons aged 70 years and older in treatment after a suicide attempt. Int Psychogeriatr 2015; 27: 1795–803. [DOI] [PubMed] [Google Scholar]
- 70. Lu Y, Arthur D, Hu Let al. Beliefs about antidepressant medication and associated adherence among older Chinese patients with major depression: a cross-sectional survey. Int J Ment Health Nurs 2016; 25: 71–9. [DOI] [PubMed] [Google Scholar]
- 71. Lyndon RW, Russell JD. Can overuse of psychotropic drugs by the elderly be prevented? Aust N Z J Psychiatry 1990; 24: 77–81. [DOI] [PubMed] [Google Scholar]
- 72. Mort JR, Singh YN, Gaspar PM, Adams PL, Singh NN. Attitudes and knowledge of long term care nurses toward psychotropic medication for the elderly. Clin Gerontol 1993; 13: 13–31. [Google Scholar]
- 73. Oehlberg K, Barg FK, Brown GK, Taraborelli D, Stern MB, Weintraub D. Attitudes regarding the etiology and treatment of depression in Parkinson's disease: a qualitative study. J Geriatr Psychiatry Neurol 2008; 21: 123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Pérodeau G, Paradis I, Grenier S, O'Connor K, Grenon É. Chronic psychotropic drug use among frail elderly women receiving home care services. J Women Aging 2011; 23: 321–41. [DOI] [PubMed] [Google Scholar]
- 75. Prabhakaran P, Butler R. What are older people's experiences of taking antidepressants? J Affect Disord 2002; 70: 319–22. [DOI] [PubMed] [Google Scholar]
- 76. Rej S, Schuurmans J, Elie Det al. Attitudes towards pharmacotherapy in late-life bipolar disorder. Int Psychogeriatr 2016; 28: 945–50. [DOI] [PubMed] [Google Scholar]
- 77. Shaw C, McCormack B, Hughes CM. Prescribing of psychoactive drugs for older people in nursing homes: an analysis of treatment culture. Drugs Real World Outcomes 2016; 3: 121–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Svarstad BL, Mount JK, Bigelow W. Variations in the treatment culture of nursing homes and responses to regulations to reduce drug use. Psychiatr Serv 2001; 52: 666–72. [DOI] [PubMed] [Google Scholar]
- 79. Tiller J, Ames D, Brodaty Het al. Antipsychotic use in the elderly: what doctors say they do, and what they do. Australas J Ageing 2008; 27: 134–42. [DOI] [PubMed] [Google Scholar]
- 80. Walsh B, Dahlke S, O’Rourke H, Hunter KF. Exploring acute care nurses' decision-making in psychotropic PRN use in hospitalised people with dementia. J Clin Nurs 2020; 1–12. 10.1111/jocn.15477. [DOI] [PubMed] [Google Scholar]
- 81. Walsh KA, Sinnott C, Fleming Aet al. Exploring antipsychotic prescribing behaviors for nursing home residents with dementia: a qualitative study. J Am Med Dir Assoc 2018; 19: 948–58.e12. [DOI] [PubMed] [Google Scholar]
- 82. Damestoy N, Collin J, Lalande R. Prescribing psychotropic medication for elderly patients: some physicians' perspectives. CMAJ 1999; 161: 143–5. [PMC free article] [PubMed] [Google Scholar]
- 83. Torres-Bondia F, Batlle J, Galván L, Buti M, Barbé F, Piñol-Ripoll G. Trends in the consumption rates of benzodiazepines and benzodiazepine-related drugs in the health region of Lleida from 2002 to 2015. BMC Public Health 2020; 20: 818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wolf I-K, Du Y, Knopf H. Changes in prevalence of psychotropic drug use and alcohol consumption among the elderly in Germany: results of two National Health Interview and examination surveys 1997–99 and 2008–11. BMC Psychiatry 2017; 17: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Oliveira ALML, Nascimento MMG d, Castro-Costa É, Firmo JOA, Lima-Costa MF, Loyola Filho AI d. Aumento da utilização de benzodiazepínicos entre idosos mais velhos: Projeto Bambuí. Rev Bras Epidemiol 2020; 23: e200029. [DOI] [PubMed] [Google Scholar]
- 86. Maust DT, Blow FC, Wiechers IR, Kales HC, Marcus SC. National trends in antidepressant, benzodiazepine, and other sedative-hypnotic treatment of older adults in psychiatric and primary care. J Clin Psychiatry 2017; 78: e363–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Lukačišinová A, Fialová D, Peel NMet al. The prevalence and prescribing patterns of benzodiazepines and Z-drugs in older nursing home residents in different European countries and Israel: retrospective results from the EU SHELTER study. BMC Geriatr 2021; 21: 277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Sun JK, Smith J. Self-perceptions of aging and perceived barriers to care: reasons for health care delay. Gerontologist 2017; 57: S216–s226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Wolff JK, Schüz B, Ziegelmann JPet al. Short-term buffers, but long-term suffers? Differential effects of negative self-perceptions of aging following serious health events. J Gerontol B Psychol Sci Soc Sci 2017; 72: 408–14. [DOI] [PubMed] [Google Scholar]
- 90. Robertson DA, King-Kallimanis BL, Kenny RA. Negative perceptions of aging predict longitudinal decline in cognitive function. Psychol Aging 2016; 31: 71–81. [DOI] [PubMed] [Google Scholar]
- 91. Halvorsen KH, Selbaek G, Ruths S. Trends in potentially inappropriate medication prescribing to nursing home patients: comparison of three cross-sectional studies. Pharmacoepidemiol Drug Saf 2017; 26: 192–200. [DOI] [PubMed] [Google Scholar]
- 92. Moher D, Fortin P, Jadad ARet al. Completeness of reporting of trials published in languages other than English: implications for conduct and reporting of systematic reviews. Lancet 1996; 347: 363–6. [DOI] [PubMed] [Google Scholar]
- 93. Morrison A, Polisena J, Husereau Det al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care 2012; 28: 138–44. [DOI] [PubMed] [Google Scholar]
- 94. Stern C, Kleijnen J. Language bias in systematic reviews: you only get out what you put in. JBI Evid Synth 2020; 18: 1818–9. [DOI] [PubMed] [Google Scholar]
- 95. Neimann Rasmussen L, Montgomery P. The prevalence of and factors associated with inclusion of non-English language studies in Campbell systematic reviews: a survey and meta-epidemiological study. Syst Rev 2018; 7: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Ballard C, Orrell M, YongZhong Set al. Impact of antipsychotic review and nonpharmacological intervention on antipsychotic use, neuropsychiatric symptoms, and mortality in people with dementia living in nursing homes: a factorial cluster-randomized controlled trial by the well-being and health for people with dementia (WHELD) program. Am J Psychiatry 2016; 173: 252–62. [DOI] [PubMed] [Google Scholar]
- 97. Massot Mesquida M, Tristany Casas M, Franzi Sisó Aet al. Consensus and evidence-based medication review to optimize and potentially reduce psychotropic drug prescription in institutionalized dementia patients. BMC Geriatr 2019; 19: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.