Abstract
Although many clinically significant strains belonging to the family Enterobacteriaceae fall into a restricted number of genera and species, there is still a substantial number of isolates that elude this classification and for which proper identification remains challenging. With the current improvements in the field of genomics, it is not only possible to generate high-quality data to accurately identify individual nosocomial isolates at the species level and understand their pathogenic potential but also to analyse retrospectively the genome sequence databases to identify past recurrences of a specific organism, particularly those originally published under an incorrect or outdated taxonomy. We propose a general use of this approach to classify further clinically relevant taxa, i.e., Phytobacter spp., that have so far gone unrecognised due to unsatisfactory identification procedures in clinical diagnostics. Here, we present a genomics and literature-based approach to establish the importance of the genus Phytobacter as a clinically relevant member of the Enterobacteriaceae family.
Keywords: Phytobacter diazotrophicus, Phytobacter ursingii, Phytobacter palmae, Genomics, Identification, Taxonomy
Introduction
The taxonomy of Enterobacteriaceae, since its establishment and valid publication in the Approved Lists of Bacterial Names in 1980 [1], has been prone to constant updates, revisions and corrections [2, 3]. Over the years, many novel genus and species names have been validly published. Since about 1985, the use of improved molecular tools such as PCR, 16S rRNA gene and multi-locus sequence analysis (MLSA) has led to a more stable taxonomy [4]. It has been only in the last 10 years that genome-based taxonomic studies and the use of average nucleotide identities (ANI) [5] and digital DNA-DNA hybridization (dDDH) [6] have enabled reliable delineation and detailed analysis of the different taxa, at the species-level, and giving rise in 2016 to the revision of the Enterobacteriaceae, with the creation of several sister families, like the Erwiniaceae or Pectobacteriaceae [2]. A more detailed analysis has shown six distinct phylogenomic-based clades within the family Enterobacteriaceae sensu strictu [3]. Still, some Enterobacteriaceae incertae sedis persist, which cannot be classified in the current taxonomy of the family, while others are not included in such studies.
Even though some medical journals, such as the Journal of Clinical Microbiology and Diagnostic Microbiology and Infectious Diseases, publish regular “taxonomic updates” for their readers [7–12], it may not be so easy for clinical microbiologists to follow all updates systematically. Genome sequencing has greatly accelerated the discovery of new taxa and the need for rearranging old taxonomic relationships [13]. A problem in this perspective is to extract the relevance of the taxonomic changes for clinical microbiologists. A taxonomic change may not be immediately recognised as therapeutically relevant if, due to that taxonomic change, the treatment administered to the patient must not be adapted [14]. On the other hand, the use of outdated taxonomy and misidentification of clinical isolates could prevent the recognition of novel emerging pathogens, cause outbreaks to be overseen or species to be incorrectly held responsible for infections [15]. Furthermore, the deposit of misidentified sequences in the database may, in turn, serve as a seed to propagate errors, causing a cascade effect involving future studies [16].
Most taxonomic confusion can be avoided by critically interpreting the data in nucleotide databases. This requires, however, an additional effort that is often not provided in clinical papers and case reports. Here, we present the case of the genus Phytobacter [17, 18] that has emerged from the disentanglement of the former Erwinia herbicola – Enterobacter agglomerans complex (EEC) [19, 20] and was increasingly detected in clinical settings over the last few years, although many of its isolates are still incorrectly assigned to Pantoea spp., Kluyvera intermedia or Metakosakonia spp. [15, 18, 21–25].
Genome-based resolution of the genus Phytobacter
Clinical isolates belonging to Brenner’s biotype XII had been assigned to the E. agglomerans complex [19] after their first detection [26] but were erroneously transferred to Pantoea agglomerans, when this species was split off from the E. agglomerans clade [27]. They were later recognised to be distinct from P. agglomerans after phenotypic and genotypic analyses of that species [16, 28] but remained without a reliable taxonomic identification. Only in 2018, these strains were included in the genus Phytobacter [17, 18], when the isolates associated with a multistate outbreak in Brazil, caused by contaminated total parenteral nutrition [29], were found to cluster with isolates of Brenner’s biotype XII [19]. This biotype was one of the last biotypes yet to be assigned to a distinct taxonomic rank among those that were reclassified from the E. agglomerans complex [28]. Based on the 16S rRNA gene and MLSA sequence data, the taxonomic positions of earlier clinical isolates belonging to biotype XII [30–32] could thus be revised and assigned to two distinct species: Phytobacter diazotrophicus and Phytobacter ursingii [24].
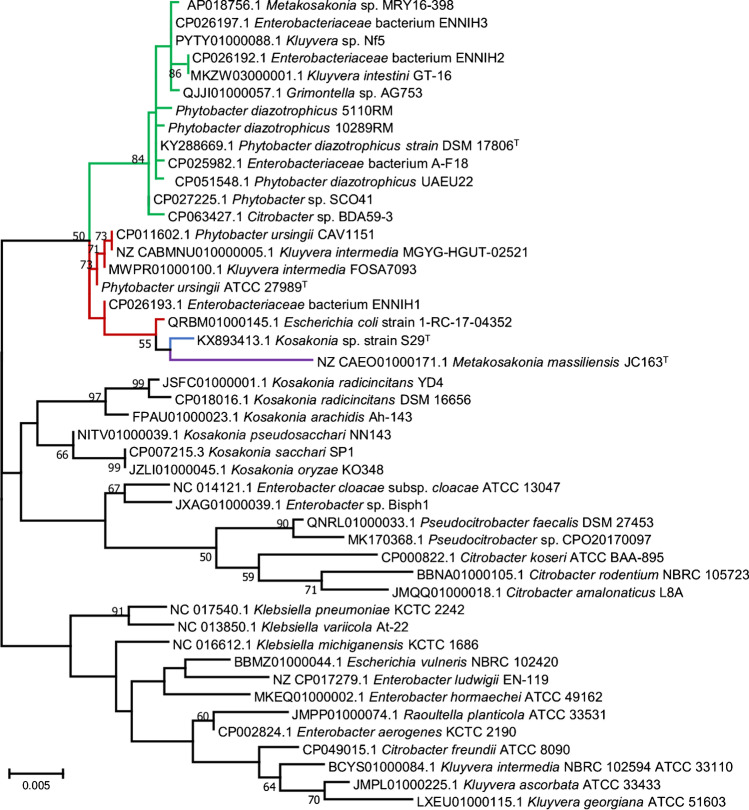
Using modern tools based on whole-genome sequencing (WGS), analysis with digital DNA-DNA-hybridization (dDDH) and average nucleotide identities (ANI), the phylogeny of the genus Phytobacter has been resolved (Fig. 1, created with EDGAR v. 3.0 [33]). Some of the isolates of a US outbreak involving infusion fluids, initially described as Pantoea (Enterobacter) agglomerans during the early 1970s, could be identified as P. diazotrophicus (ATCC 27981 and ATCC 27990) and P. ursingii (ATCC 27982 and ATCC 27989 T) [24, 30–32] within the framework of the investigation of the 2013 Brazilian outbreak. A third species of the genus, Phytobacter palmae, was then identified from oil palm (Elaeis guineensis) in Malaysia [34], while a fourth species, also isolated from the bloodstream of Brazilian patients, will soon be described (M. Pillonetto, unpublished results).
Fig. 1.
Core-genome tree, generated using EDGAR 3.0, with all available genomes of Phytobacter spp. (December 2021). Original descriptions as currently present in GenBank are indicated. Approximately maximum-likelihood phylogenetic trees were generated by aligning all core genes with MUSCLE, concatenation and tree generation with FastTree. The most optimal tree, based on 1424 genes per genome (476,326 amino acids per genome), is shown. Values at the branches are local support values computed by FastTree, using the Shimodaira–Hasegawa test. Line colours represent the different species: green: P. diazotrophicus, red: P. ursingii, blue: P. palmae, yellow: new Phytobacter sp.; purple: P. massiliensis. Type strains are indicated in bold. The origin of each strain is indicated as a dot: red, clinical; green, environmental; yellow, MAG sequence
Additionally, strain JC163T, originally isolated as Enterobacter massiliensis [35] and later renamed Metakosakonia massiliensis [3], was recently proposed as Phytobacter massiliensis based on genomic comparisons [18]. Rule 38 of the International Code of Nomenclature of Prokaryotes [36] recalls the priority of publication, which gives, in this case, the genus name Phytobacter priority over the genus name Metakosakonia [37]. A metagenome-assembled genome (MAG) currently assigned as Enterobacteriaceae bacterium UBA3516 may belong to another novel species of the genus Phytobacter [38] (Fig. 1). However, both genomes of P. massiliensis and that of Enterobacteriaceae bacterium UBA3516 branch deeper in the core-genome tree and do not contain the nitrogen fixation gene cluster (nif-genes), which are described as a key feature of the genus Phytobacter.
Even though the taxonomy of the genus Phytobacter has been well defined in the last few years, many genomes that can be retrieved from GenBank and can unambiguously be assigned to the genus Phytobacter based on the ANI analysis [24] (Table 1), are deposited therein under different names (Fig. 1). The range of potential genus names that may hide misidentified Phytobacter isolates include Metakosakonia, Kluyvera, Enterobacter, Pantoea, Citrobacter, Enterobacteriaceae bacterium, or “Grimontella”. The genus “Grimontella” was never validly published, although a 16S rRNA gene sequence of “Grimontella senegalensis” strain C1p was deposited at NCBI (accession number AY217653). As the name is not validly published, it has no standing in taxonomy. The other names were based on the misidentification of “Kluyvera intermedia” CAV1151 (now P. ursingii CAV1151) [24, 39] and the genome-based phylogenetic analysis of “E. massiliensis” JC163 [35]. This species was, meanwhile, renamed “M. massiliensis” [3]. In the same publication, the strain “Kluyvera intestini” GT-16 was discussed to be a Metakosakonia sp. as well [3]. The strain GT-16 is here included within P. diazotrophicus (Table 1; Fig. 1)[40], whereas M. massiliensis was, based on ANI values, included in the genus Phytobacter as P. massiliensis [18].
Table 1.
Currently available genomes of Phytobacter strains (December 2021) as extracted from NCBI GenBank. The whole-genome-based core phylogeny of these strains is shown in Fig. 1. The name under which the strain was originally or intermediary described is given between double quotation marks in the second column
| Strain | Former/Misidentified name | Source | Source type1 | Origin | Year | MDR genes2 | Reference |
|---|---|---|---|---|---|---|---|
| Phytobacter diazotrophicus | |||||||
| DSM 17806 T | Wild rice (Oryza rufipogon) | E | People’s Republic of China, Lingshui | 2004 | None | [17] | |
| 5110RM | Total parenteral nutrition | H | Brazil, Curitiba | 2013 | None | [24] | |
| 5020RM | Human, blood | H | Brazil, Curitiba | 2013 | None | [24] | |
| 10289RM | Human, rectal swab | H | Brazil, Curitiba | 2015 | bla KPC | [24] | |
| Bisph2 | “Enterobacter” sp. | Sandy soil | E | Algeria, Biskra | 2012 | ND2 | [41] |
| ENNIH2 | “Enterobacteriaceae” bacterium | Hospital wastewater | H | USA, MD | 2012–2016 | bla KPC | [42] |
| ENNIH3 | “Enterobacteriaceae” bacterium | Hospital wastewater | H | USA, MD | 2012–2016 | bla KPC | [42] |
| GT-16 | “Kluyvera intestini” | Human, stomach | H | USA | 2015 | bla | [21, 43] |
| SCO41 | Phytobacter sp. | Gut of C. elegans | E | People’s Republic of China | 2013 | ND | [44] |
| MRY16-398 | “Metakosakonia” sp. | Human, sigmoid colon diverticulitis | H | Japan | 2015 | bla IMP—6 | [23] |
| AG753 | “Grimontella” sp. | Rice bacterial endophyte | E | Italy | 2011 | ND | Unpublished |
| Nf5 (SCK5) | “Kluyvera” sp. | Plant growth promoting bacterium from sugarcane | E | Colombia, Valle del Cauca | 2014 | ND | [45] |
| NFR05 | “Enterobacter” sp. | Bacterial root endophyte of switchgrass | E | USA | NI2 | ND | Unpublished |
| AF18 | Bile sample, coinfection with K. pneumoniae | H | People’s Republic of China, Peking | 2020 | bla CTX-M3 | [46] | |
| UAEU22 | Rhizosphere of date palm | E | Ras Al Khaimah, United Arab Emirates | 2019 | ND | [47] | |
| BDA59-3 | “Citrobacter” sp. | Rice leaves | E | Italy | 2019 | ND | [48] |
| CCUG 74074 | Blood | H | Sweden | 2019 | ND | Unpublished | |
| UBA869 | “Enterobacteriaceae” bacterium | MAG2, terrestrial metagenome | E | USA, New York City | NI | ND | [38] |
| UBA2606 | “Enterobacteriaceae” bacterium | MAG, terrestrial metagenome | E | USA, New York City | NI | ND | [38] |
| UBA4747 | “Enterobacteriaceae” bacterium | MAG, terrestrial metagenome | E | USA, New York City | NI | ND | [38] |
| L1-008-030G1 | “Enterobacteriaceae” bacterium | MAG, infant faeces, human gut metagenome | H | USA, Pittsburgh | 2016/2019 | ND | Unpublished |
| CP_BM_RX_33 | “Metakosakonia” sp. | MAG, rhizosphere of Barbacenia macrantha | E | Brazil, Minas Gerais | 2017 | ND | Unpublished |
| Phytobacter ursingii | |||||||
| ATCC 27989 T |
“Enterobacter agglomerans” “Pantoea agglomerans” |
Human, sputum | H | USA, SC | 1974 | None | [24, 30] |
| CAV1151 | “Kluyvera intermedia” | Human, perirectal | H | USA, VA | 2009 | bla KPC | [39] |
| ENNIH1 | “Enterobacteriaceae” bacterium | Hospital wastewater | H | USA, MD | 2012–2016 | bla KPC | [42] |
| FOSA7093 | “Kluyvera intermedia” | Intraabdominal pancreas cyst | H | Denmark, Copenhagen | 2016 | bla CTX-M-type | [22] |
| 1-RC-17–04352 | “Escherichia coli” | Sink | H | USA, Milwaukee | 2017 | ND | Unpublished |
| UBA3136 |
“Enterobacteriaceae” bacterium “Stenotrophomonas maltophilia” |
MAG, terrestrial metagenome | E | USA, New York City | NI | ND | [38] |
| UHGG_MGYG-HGUT-02521 | “Kluyvera intermedia” | Human gut | H | NI | NI | bla KPC | [49] |
| Phytobacter palmae | |||||||
| S29T | “Kosakonia” sp. | Oil palm | E | Malaysia | 2012 | ND | [34] |
| Phytobacter massiliensis | |||||||
| JC163T | “Enterobacter massiliensis””Metakosakonia massiliensis” | Human, stool sample | H | Senegal | 2011 | ND | [2, 18, 35] |
| MGYG-HGUT-01426 | “Metakosakonia massiliensis” | Human gut | H | NI | NI | ND | [49] |
| Novel MAG species | |||||||
| UBA3516 | “Enterobacteriaceae” bacterium | MAG, terrestrial metagenome | E | USA, New York City | NI | ND | [38] |
1E: environmental isolate; H: hospital-associated isolate
2Abbreviations: MDR, multidrug resistance; ND, not determined; NI, no indications; MAG, metagenome-assembled genome
The emergence of members of the genus Phytobacter under contradicting names in different publications over the past years [18, 24, 25] creates additional problems in handling the genome sequence database (Fig. 1), as NCBI refuses to rename the organisms and/or the phylogenetic assignment without the formal approval of the original submitters. Therefore, improving genomic-based taxonomy will remain a challenge that can currently be tackled only by submitting a sufficient number of genomes with the correct genus and species names.
Misidentifications in clinical laboratories
Unfortunately, isolates belonging to the various Brenner’s biotypes were probably among those used to generate the phenotypic profiles that are the basis for identification of P. agglomerans, by the BD Phoenix™ diagnostic system, thus leading to erroneous results when performing routine identifications, using the corresponding biochemical panels [16]. The same results (i.e., Phytobacter spp., misidentified as Pantoea sp. or P. agglomerans) were obtained when other automated systems, such as Vitek® 2 (bioMérieux) or Microscan® (Beckman Coulter) or manual methods, such as API 20E® (bioMérieux), were used in the laboratories [29]. This indicates that the common phenotypic identification methods in clinical laboratories cannot distinguish Phytobacter isolates from Pantoea spp., without additional effort.
Based on the data available in the literature, we have identified more instances in which Phytobacter may have been potentially misidentified as P. agglomerans (Table 2) and that resulted in the overestimation of the role of the latter species as an opportunistic human pathogen [15, 50]. The case of Boszczowski et al. [51] is emblematic of how erroneously assigned sequences in databases or misnamed catalogue entries can be detrimental for future identifications if they are not carried out with proper diligence. Using the gyrB sequence of their isolate, the authors identified it as P. agglomerans, based on the 100% BLASTN match with strain ATCC 27990, which was then still listed as P. agglomerans in the ATCC catalogue. Strain ATCC 27990, however, had been already excluded from P. agglomerans by previous taxonomic studies [15, 28], and the corresponding gyrB sequence in NCBI was, at that time, tentatively listed as Enterobacter spp. The proper line of action by the authors would have been a comparison of their sequence, not simply with just the first BLAST match, but with a number of the type strains of potential matching species, using clustering analysis. Only later, strain ATCC 27990 was unequivocally identified as a member of the species P. diazotrophicus [24], a fact that was confirmed by genome sequencing. Meanwhile, the name of the strain was also corrected on the ATCC website and in the corresponding NCBI entries, together with the name of three further strains assigned initially to Brenner’s biotype XII, i.e. ATCC 27981 (P. diazotrophicus) and ATCC 27982 and ATCC 27989 (P. ursingii).
Table 2.
Misidentification of cases and outbreaks potentially including Phytobacter spp
| Case study1 | Number of cases | Identification method | Supposed species | Status2 | Reference |
|---|---|---|---|---|---|
| Clinical | 6 | Biochemical | Enterobacter spp. | Some ATCC-deposited strains confirmed P. diazotrophicus or P. ursingii | [30] |
| NICU, TPN | 8 | API-20E | Pantoea spp. | Open | [52] |
| Nosocomial sepsis | 6 | Vitek-2, GNI card | P. agglomerans | Open | [53] |
| Nosocomial sepsis | 6 | Vitek, GN card | P. agglomerans3 | Open | [54] |
| Contaminated TPN | 8 | Vitek-2, API-20E, gyrB | P. agglomerans | Confirmed P. diazotrophicus | [51] |
| Neonatal sepsis | 1 | Vitek-2, GN25 card | Pantoea spp. | Open | [55] |
| NICU, septicaemia | 14 | API-20E | P. agglomerans | Open | [56] |
| Bloodstream infection | 12 | Vitek-2, PFGE | P. agglomerans | Open | [57] |
| Clinical samples | 40 | Biochemical, Vitek-2 | P. agglomerans | Open | [58] |
| Paediatric patients | 14 | BD Crystal, MALDI-TOF MS | P. agglomerans | Open | [59] |
1Abbreviations: NICU, neonatal intensive care unit; TPN, total parenteral nutrition; PFGE, pulsed-field gel electrophoresis; MALDI-TOF MS, matrix-assisted laser desorption-ionisation time-of-flight mass spectrometry
2Interpretation of the data by the authors of this manuscript
3Rahnella aquatilis and Candida famata co-isolated in one sample
Useful microbiological features for the correct identification of Phytobacter spp.
Phytobacter spp. should be suspected when a strong lactose-fermenting Gram-negative colony is isolated from human samples on MacConkey Agar. The colony morphology on this medium resembles that of E. coli and/or Citrobacter, having a variable phenotype [60]. Sometimes strains will show the classic bile salt halo-surrounding colonies. Some strains of P. diazotrophicus and P. ursingii are variably strong lactose-fermenters. Additionally, it can yield lactose-negative or even weak lactose-positive colonies, the latter having a colony morphology that resembles strains belonging to the Enterobacter cloacae complex. Differently from most true P. agglomerans isolates and related species [27, 61, 62], Phytobacter strains do not produce a yellow pigment [24].
Biochemical tests with Phytobacter spp. display a typical profile (Table 3) giving triple-negative results for lysine decarboxylase, arginine dihydrolase, and ornithine decarboxylase [24]. These features generally rule out E. coli and C. amalonaticus (Table 3). In the commercial identification tables and systems, this may lead to confusion with Pantoea spp. [16], but Phytobacter is using citrate as a carbon source (Table 3). Furthermore, Phytobacter spp. can ferment most of the sugars commonly used in manual and automated systems for bacterial identification, except for inositol and melibiose.
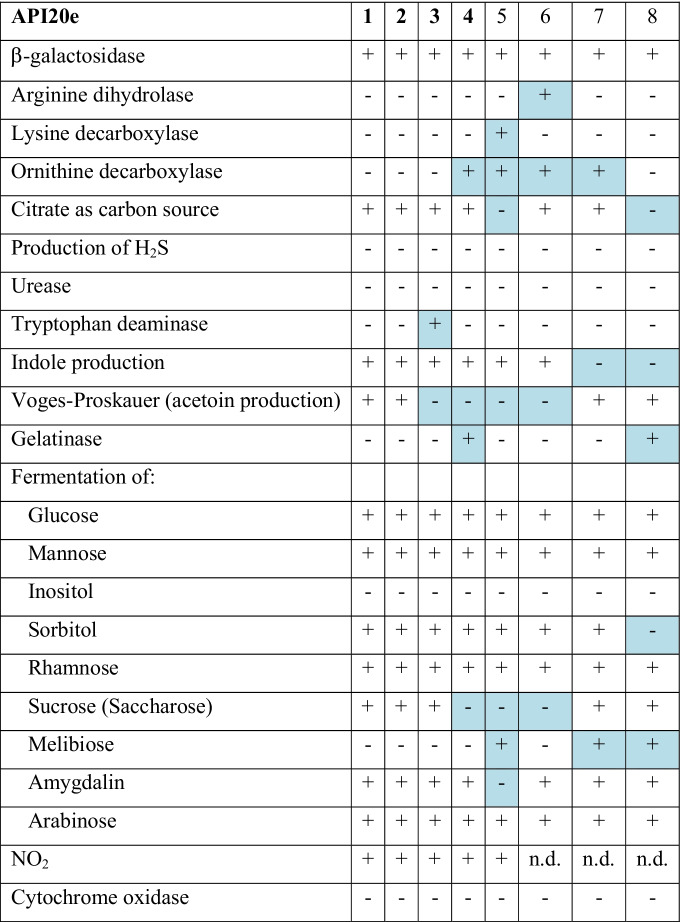
Table 3.
Phenotypic characterization of Phytobacter spp. (columns 1-4, bold) and related organisms as reported by API20e test strips. 1: Phytobacter diazotrophicus (n = 14); 2: Phytobacter ursingii (n = 6); 3: Phytobacter palmae (n = 1); 4: Phytobacter massiliensis JC163T; 5: Escherichia coli DSM 30083 T; 6: Citrobacter amalonaticus CCUG 4860 T 7: Kluyvera intermedia DSM 4581 T; 8: Pantoea agglomerans ATCC 27155 T. Data from own experiments (1–3) or from BacDive (https://bacdive.dsmz.de/) (4–8)). Differences from the majority are highlighted in blue
Clinical microbiologists should be aware that, in the absence of a regularly updated reference database, mass spectrometry systems (MALDI-TOF MS, Vitek-MS, and MALDI Biotyper-Bruker Microflex) can generate a wide choice of false identifications for strains of Phytobacter spp. The erroneous output can include different Pantoea spp., Leclercia adecarboxylata, Pseudescherichia vulneris, Klebsiella ozaenae, Klebsiella oxytoca, Enterobacter cloacae, Salmonella spp., or even indicate as “unidentified species”. Such outputs are not convincing and may further add to the discrepancies already found in the literature [63]. An alternative used in our labs is to implement an in-house SuperSpectrum for the MALDI-TOF MS identification of Phytobacter spp. (M. Pillonetto, unpublished results). Following this strategy, sixteen suspicious strains were identified in Brazil between 2016 and March 2021 as Phytobacter spp. and ultimately confirmed by WGS (Table 4).
Table 4.
Recently isolated clinical strains of Phytobacter spp. not yet published
| Country | City, state | Species | Number of isolates | Isolation period | Sample(s), (number of isolates) | MDR1-positive | MDR-negative |
|---|---|---|---|---|---|---|---|
| Switzerland | Zürich2 | P. diazotrophicus | 2 | 2013–2014 | Blood (2) | 0 | 2 |
| Sweden | Gothenburg, Kalmar, Uppsala | P. diazotrophicus | 5 | 2008–2020 | Urine (1), blood (2), CAPD-fluid (1), sputum (1) | NA1 | NA |
| Gothenburg | P. ursingii | 1 | 2015 | Blood (1) | NA | NA | |
| Brazil | Curitiba-PR, São Paulo-SP, Cuiabá-MT | P. diazotrophicus | 9 | 2016–2021 | Urine (1), blood (4), rectal swab (2), eye infection (1), tracheal aspirate (1) | 3 | 6 |
| Curitiba-PR, São Paulo-SP | P. ursingii | 5 | 2016–2020 | Urine (1), blood (2), catheter (1), rectal swab (1) | 1 | 4 | |
| Curitiba-PR | Novel species | 2 | 2020 | Blood (2) | 0 | 2 |
1Abbreviations: MDR, multidrug-resistant; NA: not analysed
2Source: Dr. Frank Imkamp University of Zürich, Institute of Medical Microbiology, Molecular Diagnostics group, Zürich, Switzerland
The most optimal solution to avoid this problem is for uncertain isolates to be further identified, using sequencing of the 16S rRNA gene (Fig. 2) or, preferably, the gyrB gene, as the housekeeping gene is known to enable good resolution within the Enterobacteriaceae [15, 28]. If the investigation is relevant (as in an outbreak) and access to the technology is available, whole-genome next-generation sequencing (NGS) is the most reliable approach to identify the suspect isolates to the species level, using ANI or dDDH or core-genome phylogeny.
Fig. 2.
Phylogenetic tree showing the evolutionary relationship among Phytobacter species and other type species of the family Enterobacteriaceae based on 16S rRNA gene sequences (1457 bp). The tree was constructed by using the maximum likelihood method and the most optimal tree is shown. Line colours represent the different species: green: P. diazotrophicus, red: P. ursingii, blue: P. palmae, purple: P. massiliensis. Numbers at branching points are bootstrap percentage values (> 50%) based on 1000 replications. GenBank accession numbers are shown before the strain name. Bar, 0.005% nucleotide sequence difference
The clinically oriented Culture Collection University of Gothenburg (CCUG) in Sweden has archived six isolates of P. diazotrophicus and two isolates of P. ursingii in its collection, all isolated in clinical samples in Sweden since 2012. These are presently identified based on 16S rRNA gene sequence and dnaJ gene sequence [64], which also work well for Enterobacteriaceae. The gene sequence allows for clear discrimination from other species and genera. The whole-genome sequence of isolate P. diazotrophicus strain CCUG 74074 corresponded well within the core-genome phylogeny of the genus (Fig. 1). Therefore, the dnaJ gene may be well-suited for fast and concise identifications of the members of the genus, as well.
Clinical relevance
Although Phytobacter has been described in human samples only recently [24], it has unequivocally been proved by WGS that it has previously been misidentified as other species, such as Pantoea or Kluyvera, since the 1970s [18, 24, 25, 46]. In the last 5 years, Phytobacter has been described in important clinical samples such as blood, sputum, digestive tract, and bile (Table 1). We reported 24 human isolates in a 5-year period (2016–2021), including thirteen from the bloodstream and one from a catheter, reinforcing the concept that the genera Phytobacter is clinically relevant (Table 4). Another indirect support is the large number of publications referring to outbreaks or case reports of Pantoea agglomerans and Pantoea spp. infection (Table 2), wherein the organisms in question were poorly identified by manual or automated tests only, which could easily lead to the misidentification of isolates potentially belonging to the genus Phytobacter, as already observed by our research groups [16, 24].
The first published isolates of Phytobacter were sensitive to common antibiotics [24, 31]. However, in recent years, the number of multidrug-resistant Phytobacter isolates has increased. Several isolates for which genomes are available (Table 1, Table 4) show that multidrug resistance is present, including critical antimicrobial resistance genes such as blaKPC, blaIMP6, and blaCTX-M [18, 23, 29, 39, 43, 46]. Genomic analysis has revealed that in many cases, resistance is encoded on plasmids [42], thus potentially transferred from other hospital-related pathogens. It may be possible that Phytobacter spp. have adapted from their natural ecological niches as soil or plant-associated bacteria to the hospital environment and can easily exchange resistance plasmids or other mobile genetic elements, potentially becoming a new, emerging threat as a multidrug-resistant microorganism.
Future directions
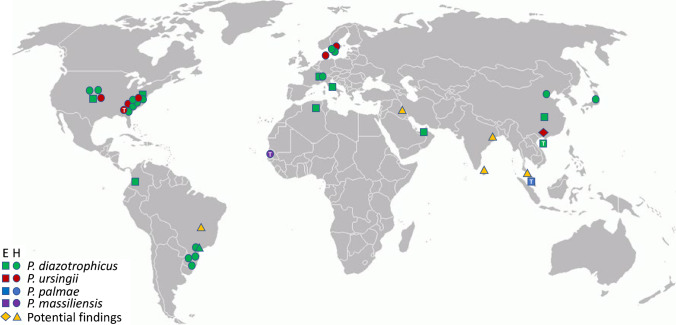
The clinical history of Phytobacter, with outbreaks mainly on the US East Coast and in Brazil [29, 31, 51] but also with individual cases at other locations worldwide (Fig. 3), shows us that clinicians should be(-come) aware of the importance of this genus as a recurring opportunistic pathogen. The clinical relevance has increased over the last few years, although it is not clear from the literature whether more cases could have been ascribed to this organism. Many of the current papers about clinical infections in humans caused by emerging and/or opportunistic Enterobacterales, such as Pantoea spp., Kluyvera spp., Raoultella spp., and L. adecarboxylata are attributing the identifications of the pathogen to the species-level, using only intrinsically inaccurate phenotypic-based methods, such as manual (API-20E) or automated biochemical profiling (Vitek-2, Phoenix, or Walkaway systems). However, the major problem is that the databases on which these commercial platforms rely are commonly outdated. Their updates involve prolonged and complex verification and certification processes, which does not keep up with the pace of developments in bacterial taxonomy. Erroneous designations can impair outbreak investigation and compromise epidemiological studies of etiological agents, especially in hospital-acquired infections. In this sense, correct identifications of Phytobacter remain challenging for routine clinical laboratories. Clinical microbiologists need to be aware of this and other new species that are becoming increasingly relevant to infectious diseases [11].
Fig. 3.
Geographic overview of Phytobacter spp. distribution. Coloured squares and circles represent the different species for which genomes are available (Table 1): green: P. diazotrophicus, red: P. ursingii, blue: P. palmae, violet: P. massiliensis. A white “T” in the symbol represents the location of the type strain. Diamonds and triangles (orange) indicate the origins of potential findings as reported in Table 2. E: environmental isolate; H: hospital-associated isolate
Many of the cases identified as Phytobacter spp. infection consisted of sepsis after receiving intravenous fluids or the use of medical devices, often in neonatal intensive care units (Table 2). Neonates may not yet be able to deal with this organism due to a still-developing immune system, whereas infants and adults respond better to infection. Outbreaks of Phytobacter spp. have already been shown to be able to lead to high mortality of mainly young and immunocompromised patients [32, 51, 52]. The coinfection of Phytobacter spp. with other potential pathogens can result in clinical situations that are even more complicated [29, 46]. In our previous study, combinations of three bacteria (P. diazotrophicus, Acinetobacter baumannii, and Rhizobium radiobacter) were often found in clinical outbreak samples, while one sample contained all three species at once [29]. A recent study showed coinfection of P. diazotrophicus with Klebsiella pneumoniae with the latter bacterium acting as the major pathogen but being protected against antibiotics by a resistant strain of P. diazotrophicus [46]. These examples of bacterial coexistence should be followed in more detail in clinical diagnostics, as they appear to be more common than expected.
Conclusion
Although the currently reported number of Phytobacter infections is not very high, the clinical relevance of this organism may actually be masked by inadequate identification procedures. We understand the impracticality of integrating additional steps in routine clinical diagnostics, but in order to preserve scientific integrity and avoid detrimental taxonomic confusion, it is critical for the most accurate available identification approach to be applied at least in those cases that are to be published in the scientific literature. This is especially important because clinical samples are rarely retained for subsequent independent verification after initial analysis [50]. Based on our investigations, Phytobacter potentially may have the same (or even a greater) clinical relevance as Kluyvera spp. or Pantoea spp., especially since isolates are often confused with species of those genera [24, 42, 43] (Tables 1 and 2). An appropriate identification protocol that targets a reference gene or the genome sequence would be required to better understand the occurrence of Phytobacter in clinical samples. Comparison of generated sequences to curated databases such as the Type Strain Genome Server (https://tygs.dsmz.de/), which contains the verified genomes of bacterial type species (including Phytobacter), rather than to NCBI, further can contribute to enhancing identification accuracy. On the other hand, the improvement of current biochemical and mass spectrometry methods to include Phytobacter spp. in their list of reference organisms is critical for all situations in which sequencing approaches might not be available. Additionally, it is essential to perform proper monitoring of antimicrobial resistance in members of this genus, as the number of cases of multidrug resistant Phytobacter is already increasing now.
With the current improvements in the field of genomics [18, 40], it is possible to generate high-quality data to help understand the pathogenic potential of individual nosocomial Phytobacter isolates in comparison to that of environmental isolates. Further work will focus on developing molecular diagnostic procedures for field and clinical studies and improving the current databases to resolve the taxonomic confusion so that new isolates can immediately be assigned to the correct genus.
Acknowledgements
The authors thank Dr. Frank Imkamp (Institute of Medical Microbiology, University of Zürich, Switzerland) and Prof. Dr. Henrik Westh (Department of Clinical Microbiology, Hvidovre Hospital, Denmark) for sharing information on the occurrence of Phytobacter in their institution.
Author contribution
Initial idea: Theo H. M. Smits, Fabio Rezzonico, and Marcelo Pillonetto; literature research and data analysis: Theo H. M. Smits, Lavinia N. V. S. Arend, Sofia Cardew, Erika Tång Hallbäck, Edward R.B. Moore, Fabio Rezzonico, and Marcelo Pillonetto; manuscript draft: Theo H. M. Smits, Fabio Rezzonico, and Marcelo Pillonetto; critical revision: Theo H. M. Smits, Marcelo T. Mira, Edward R. B. Moore, Jorge L. M. Sampaio, Fabio Rezzonico, and Marcelo Pillonetto. All authors read and approved the final manuscript.
Funding
Open access funding provided by ZHAW Zurich University of Applied Sciences. This study was supported by the Central Public Health Laboratory of Paraná (LACEN/PR), the Core for Advanced Molecular Investigation at PUCPR, the FLASH Research Programme Project SAMBA funded by the Swiss State Secretariat for Education, Research and Innovation (SERI), the Leading House for the Latin American Region of the University of St. Gallen, Switzerland, and the Life Science and Facility Management Department at Zurich University for Applied Sciences (ZHAW). None of the funding agencies was involved in the study design, in the collection, analysis, and interpretation of data nor in the writing of the manuscript.
Data availability
Genome data were extracted from GenBank or available from the authors after reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Theo H. M. Smits, Email: theo.smits@zhaw.ch
Marcelo Pillonetto, Email: m.pilonetto@pucpr.br.
References
- 1.Skerman VBD, McGowan V, Sneath PHA. Approved lists of bacterial names. Int J Syst Bacteriol. 1980;30(1):225–420. [PubMed] [Google Scholar]
- 2.Adeolu M, Alnajar S, Naushad S, Gupta RS. Genome-based phylogeny and taxonomy of the ‘Enterobacteriales’: proposal for Enterobacterales ord. nov. divided into the families Enterobacteriaceae, Erwiniaceae fam. nov., Pectobacteriaceae fam. nov., Yersiniaceae fam. nov., Hafniaceae fam. nov., Morganellaceae fam. nov., and Budviciaceae fam. nov. Int J Syst Evol Microbiol. 2016;66:5575–5599. doi: 10.1099/ijsem.0.001485. [DOI] [PubMed] [Google Scholar]
- 3.Alnajar S, Gupta RS. Phylogenomics and comparative genomic studies delineate six main clades within the family Enterobacteriaceae and support the reclassification of several polyphyletic members of the family. Infect Genet Evol. 2017;54:108–127. doi: 10.1016/j.meegid.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 4.Rosselló-Móra R, Amann R. Past and future species definitions for Bacteria and Archaea. Syst Appl Microbiol. 2015;38:209–216. doi: 10.1016/j.syapm.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Konstantinidis KT, Tiedje JM. Towards a genome-based taxonomy for prokaryotes. J Bacteriol. 2005;187(18):6258–6264. doi: 10.1128/JB.187.18.6258-6264.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meier-Kolthoff JP, Auch AF, Klenk H-P, Göker M. Genome sequence-based species delimitation with confidence intervals and improved distance functions. BMC Bioinformatics. 2013;14:60. doi: 10.1186/1471-2105-14-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janda JM. Proposed nomenclature or classification changes for bacteria of medical importance: taxonomic update 5. Diagn Microbiol Inf Dis. 2020;97(3):115047. doi: 10.1016/j.diagmicrobio.2020.115047. [DOI] [PubMed] [Google Scholar]
- 8.Munson E, Carroll KC. An update on the novel genera and species and revised taxonomic status of bacterial organisms described in 2016 and 2017. J Clin Microbiol. 2019;57(2):e01181–01118. doi: 10.1128/JCM.01181-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kraft CS, McAdam AJ, Carroll KC. A rose by any other name: practical updates on microbial nomenclature for clinical microbiology. J Clin Microbiol. 2017;55(1):3–4. doi: 10.1128/JCM.02169-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janda JM. Proposed nomenclature or classification changes for bacteria of medical importance: Taxonomic Update 4. Diagn Microbiol Inf Dis. 2019;94:205–208. doi: 10.1016/j.diagmicrobio.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Munson E. Moving targets of bacterial taxonomy revision: what are they and why should we care? Clin Microbiol Newsletter. 2020;42(14):111–120. [Google Scholar]
- 12.Janda JM, Abbott SL. The changing face of the family Enterobacteriaceae (order: “ Enterobacterales”): new members, taxonomic issues, geographic expansion, and new diseases and disease syndromes. Clin Microbiol Rev. 2021;34(2):e00174-00120. doi: 10.1128/CMR.00174-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parks DH, Chuvochina M, Chaumeil P-A, Rinke C, Mussig AJ, Hugenholtz P. A complete domain-to-species taxonomy for Bacteria and Archaea. Nat Biotechnol. 2020;38:1079–1086. doi: 10.1038/s41587-020-0501-8. [DOI] [PubMed] [Google Scholar]
- 14.Janda JM. Clinical decisions: how relevant is modern bacterial taxonomy for clinical microbiologists? Clin Microbiol Newsletter. 2018;40(7):51–57. [Google Scholar]
- 15.Rezzonico F, Smits THM, Duffy B. Misidentification slanders Pantoea agglomerans as a serial killer. J Hosp Infect. 2012;81(2):137–139. doi: 10.1016/j.jhin.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Rezzonico F, Vogel G, Duffy B, Tonolla M. Whole cell MALDI-TOF mass spectrometry application for rapid identification and clustering analysis of Pantoea species. Appl Environ Microbiol. 2010;76(13):4497–4509. doi: 10.1128/AEM.03112-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang GX, Peng GX, Wang ET, Yan H, Yuan QH, Zhang W, Lou X, Wu H, Tan ZY. Diverse endophytic nitrogen-fixing bacteria isolated from wild rice Oryza rufipogon and description of Phytobacter diazotrophicus gen. nov. sp. nov. Arch Microbiol. 2008;189:431–439. doi: 10.1007/s00203-007-0333-7. [DOI] [PubMed] [Google Scholar]
- 18.Ma Y, Yao R, Li Y, Wu X, Li S, An Q. Proposal for unification of the genus Metakosakonia and the genus Phytobacter to a single genus Phytobacter and reclassification of Metakosakonia massiliensis as Phytobacter massiliensis comb. nov. Curr Microbiol. 2020;77:1945–1954. doi: 10.1007/s00284-020-02004-4. [DOI] [PubMed] [Google Scholar]
- 19.Brenner DJ, Fanning GR, Leete Knutson JK, Steigerwalt AG, Krichevsky MI. Attempts to classify Herbicola group-Enterobacter agglomerans strains by deoxyribonucleic acid hybridization and phenotypic tests. Int J Syst Bacteriol. 1984;34(1):45–55. [Google Scholar]
- 20.Rezzonico F, Smits THM, Pelludat C, Montesinos E, Frey JE, Duffy B. Genotypic comparison of Pantoea agglomerans biocontrol and clinical isolates to address taxonomic and bio-safety questions. IOBC Bull. 2009;43:35–39. [Google Scholar]
- 21.Tetz G, Tetz V. Draft genome sequence of Kluyvera intestini strain GT-16 isolated from the stomach of a patient with gastric cancer. Genome Announc. 2016;4(6):e01432-01416. doi: 10.1128/genomeA.01432-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thele R, Gumpert H, Christensen LB, Worning P, Schønning K, Westh H, Hansen TA. Draft genome sequence of a Kluyvera intermedia isolate from a patient with a pancreatic abscess. J Glob Antimicrob Resist. 2017;10:1–2. doi: 10.1016/j.jgar.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Sekizuka T, Matsui M, Takahashi T, Hayashi M, Suzuki S, Tokaji A, Kuroda M. Complete genome sequence of blaIMP–6-Positive Metakosakonia sp. MRY16–398 isolate from the ascites of a diverticulitis patient. Front Microbiol. 2018;9:2853. doi: 10.3389/fmicb.2018.02853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pillonetto M, Arend L, Faoro H, D’Espindula HRS, Blom J, Smits THM, Mira MT, Rezzonico F. Emended description of the genus Phytobacter, its type species Phytobacter diazotrophicus (Zhang 2008) and description of Phytobacterursingii sp. nov. Int J Syst Evol Microbiol. 2018;68(1):176–184. doi: 10.1099/ijsem.0.002477. [DOI] [PubMed] [Google Scholar]
- 25.Liu L, Feng Y, Wei L, Qiao F, Zong Z. Precise species identification and taxonomy update for the genus Kluyvera with reporting Kluyverasichuanensis sp. nov. Front Microbiol. 2020;2020:579306. doi: 10.3389/fmicb.2020.579306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ewing WH, Fife MA. Enterobacteragglomerans (Beijerinck) comb. nov. (the Herbicola-Lathyri bacteria) Int J Syst Bacteriol. 1972;22(1):4–11. [Google Scholar]
- 27.Gavini F, Mergaert J, Beji A, Mielcarek C, Izard D, Kersters K, De Ley J. Transfer of Enterobacteragglomerans (Beijerinck 1888) Ewing and Fife 1972 to Pantoea gen. nov. as Pantoeaagglomerans comb. nov. and description of Pantoeadispersa sp. nov. Int J Syst Bacteriol. 1989;39(3):337–345. [Google Scholar]
- 28.Rezzonico F, Smits THM, Montesinos E, Frey JE, Duffy B. Genotypic comparison of Pantoea agglomerans plant and clinical strains. BMC Microbiol. 2009;9:204. doi: 10.1186/1471-2180-9-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pillonetto M, Arend L, Gomes SMT, Oliveira MAA, Timm LN, Martins AF, Barth AL, Mazzetti A, Hersemann L, Smits THM, Mira MT, Rezzonico F. Molecular investigation of isolates from a multistate polymicrobial outbreak associated with contaminated total parenteral nutrition in Brazil. BMC Infect Dis. 2018;18:397. doi: 10.1186/s12879-018-3287-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Felts SK, Schaffner W, Melly MA, Koenig MG. Sepsis caused by contaminated intravenous fluids. Ann Intern Med. 1972;77:881–890. doi: 10.7326/0003-4819-77-6-881. [DOI] [PubMed] [Google Scholar]
- 31.Mackel DC, Maki DG, Anderson RL, Rhame FS, Bennett JV. Nationwide epidemic of septicemia caused by contaminated intravenous products: mechanisms of intrinsic contamination. J Clin Microbiol. 1975;2(6):486–497. doi: 10.1128/jcm.2.6.486-497.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maki DG, Martin WT. Nationwide epidemic of septicemia caused by contaminated infusion products. IV. growth of microbial pathogens in fluids for intravenous infusion. J Infect Dis. 1975;131(3):267–272. doi: 10.1093/infdis/131.3.267. [DOI] [PubMed] [Google Scholar]
- 33.Dieckmann MA, Beyvers S, Nkouamedjo-Fankep RC, Hanel PHG, Jelonek L, Blom J, Goesmann A. EDGAR3.0: comparative genomics and phylogenomics on a scalable infrastructure. Nucleic Acids Res. 2021;49(W1):W185–W192. doi: 10.1093/nar/gkab341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madhaiyan M, Saravanan VS, Blom J, Smits THM, Rezzonico F, Kim S-J, Weon H-Y, Kwon S-W, Whitman WB, Ji L. Phytobacterpalmae sp. nov., a novel endophytic, N fixing, plant growth promoting Gammaproteobacterium isolated from oil palm (ElaeisguineensisJacq.) Int J Syst Evol Microbiol. 2020;70(2):841–848. doi: 10.1099/ijsem.0.003834. [DOI] [PubMed] [Google Scholar]
- 35.Lagier J-C, El Karkouri K, Mishra AK, Robert C, Raoult D, Fournier P-E. Non contiguous-finished genome sequence and description of Enterobacter massiliensis sp. nov. Stand Genomic Sci. 2013;7:399–412. doi: 10.4056/sigs.3396830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parker CT, Tindall BJ, Garrity GM. International Code of Nomenclature of Prokaryotes: Prokaryotic Code (2008 Revision) Int J Syst Evol Microbiol. 2019;69(1A):S1–S111. doi: 10.1099/ijsem.0.000778. [DOI] [PubMed] [Google Scholar]
- 37.Oren A, Garrity GM. Notification of changes in taxonomic opinion previously published outside the IJSEM. Int J Syst Evol Microbiol. 2021;71(1):004596. doi: 10.1099/ijsem.0.004596. [DOI] [PubMed] [Google Scholar]
- 38.Parks DH, Rinke C, Chuvochina M, Chaumeil P-A, Woodcroft BJ, Evans PN, Hugenholtz P, Tyson GW. Recovery of nearly 8,000 metagenome-assembled genomes substantially expands the tree of life. Nat Microbiol. 2017;2:1533–1542. doi: 10.1038/s41564-017-0012-7. [DOI] [PubMed] [Google Scholar]
- 39.Sheppard AE, Stoesser N, Wilson DJ, Sebra R, Kasarskis A, Anson LW, Gless A, Pankhurst LJ, Vaughan A, Grim CJ, Cox HL, Yeh AJ, the Modernising Medical Microbiology (MMM) Informatics Group. Sifri CD, Walker AS, Peto TE, Crook DW, Mathers AJ. Nested Russian doll-like genetic mobility drives rapid dissemination of the carbapenem resistance gene blaKPC. Antimicrob Agents Chemother. 2016;60(6):3767–3778. doi: 10.1128/AAC.00464-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smits THM. The importance of genome sequence quality to microbial comparative genomics research. BMC Genomics. 2019;20:662. doi: 10.1186/s12864-019-6014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Benslama O, Boulahrouf A. High-quality draft genome sequence of Enterobacter sp. BISPH2, a glyphosate-degrading bacterium isolated from a sandy soil of Biskra, Algeria. Genomics Data. 2016;8:61–66. doi: 10.1016/j.gdata.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weingarten RA, Johnson RC, Conlan S, Ramsberg AM, Dekker JP, Lau AF, Khil P, Odom RT, Deming C, Park M, Thomas PJ, Comparative Sequencing Program NISC, Henderson DK, Palmore TN, Segre JA, Frank KM. Genomic analysis of hospital plumbing reveals diverse reservoir of bacterial plasmids conferring carbapenem resistance. mBio. 2018;9(1):e02011–02017. doi: 10.1128/mBio.02011-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tetz G, Vecherkovskaya M, Zappile P, Dolgalev I, Tsirigos A, Heguy A, Tetz V. Complete genome sequence of Kluyveraintestini sp. nov., isolated from the stomach of a patient with gastric cancer. Genome Announc. 2017;5(43):e01184–01117. doi: 10.1128/genomeA.01184-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang B, Huang B, Chen J, Li W, Yang L, Yao L, Niu Q. Whole-genome analysis of the colonization-resistant bacterium Phytobacter sp. SCO41T isolated from Bacillusnematocida B16-fed adult Caenorhabditis elegans. Mol Biol Rep. 2019;46(2):1563–1575. doi: 10.1007/s11033-018-04574-w. [DOI] [PubMed] [Google Scholar]
- 45.Medina-Cordoba LK, Chande AT, Rhishishwar L, Mayer LW, Valderrama-Aguirre LC, Valderrama-Aguirre A, Gaby JC, Kostka JE, Jordan IK. Genomic characterization and computational phenotyping of nitrogen-fixing bacteria isolated from Colombian sugarcane fields. Sci Rep. 2021;11:9187. doi: 10.1038/s41598-021-88380-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Z, Li D, Shi X, Zhai Y, Guo Y, Zheng Y, Zhao L, He Y, Chen Y, Wang Z, Su J, Kang Y, Gao Z. Genomic characterization of an emerging Enterobacteriaceae species: the first case of co-infection with a typical pathogen in a human patient. BMC Genomics. 2020;21:297. doi: 10.1186/s12864-020-6720-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salha Y, Sudalaimuthuasari N, Kundu B, AlMaskari RS, Alkaabi AS, Hazzouri KM, AbuQamar SF, El-Tarabily KA, Amiri KMA. Complete genome sequence of Phytobacter diazotrophicus strain UAEU22, a plant growth-promoting bacterium isolated from the date palm rhizosphere. Microbiol Res Announc. 2020;9:e00499-00420. doi: 10.1128/MRA.00499-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bianco C, Andreozzi A, Romano S, Fagorzi C, Cangioli L, Prieto P, Cisse F, Niangado O, Sidibé A, Pianezze S, Perini M, Mengoni A, Defez R. Endophytes from African rice (Oryza glaberrima L.) efficiently colonize Asian rice (Oryza sativa L.) stimulating the activity of its antioxidant enzymes and increasing the content of nitrogen, carbon, and chlorophyll. Microorganisms. 2021;9:1714. doi: 10.3390/microorganisms9081714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Almeida A, Nayfach S, Boland M, Strozzi F, Beracochea M, Shi ZJ, Pollard KS, Sakharova E, Parks DH, Hugenholtz P, Segata N, Kyrpides NC, Finn RD. A unified catalog of 204,938 reference genomes from the human gut microbiome. Nat Biotechnol. 2021;39:105–114. doi: 10.1038/s41587-020-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rezzonico F, Stockwell VO, Tonolla M, Duffy B, Smits THM. Pantoea clinical isolates cannot be accurately assigned to species based on metabolic profiling. Transpl Infect Dis. 2012;14(2):220–221. doi: 10.1111/j.1399-3062.2011.00684.x. [DOI] [PubMed] [Google Scholar]
- 51.Boszczowski I, de Almeida N, Júnior J, Peixoto de Miranda EJ, Pinheiro Freire M, Guimarães T, Chaves CE, Cais DP, Strabelli TMV, Risek CF, Soares RE, Rossi F, Costa SF, Levin AS. Nosocomial outbreak of Pantoea agglomerans bacteraemia associated with contaminated anticoagulant citrate dextrose solution: new name, old bug? J Hosp Infect. 2012;80(3):255–258. doi: 10.1016/j.jhin.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 52.Habsah H, Zeehaida M, Van Rostenberghe H, Noraida R, Wan Pauzi WI, Fatimah I, Rosliza AR, Nik Sharimah NY, Maimunah H. An outbreak of Pantoea spp. in a neonatal intensive care unit secondary to contaminated parenteral nutrition. J Hosp Infect. 2005;61:213–218. doi: 10.1016/j.jhin.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 53.Bicudo EL, Macedo VO, Carrara MA, Castro FFS, Rage RI. Nosocomial outbreak of Pantoea agglomerans in a pediatric urgent care center. Braz J Infect Dis. 2007;11(2):281–284. doi: 10.1590/s1413-86702007000200023. [DOI] [PubMed] [Google Scholar]
- 54.Liberto MC, Matera G, Puccio R, Lo Russo T, Colosimo E, Focà E. Six cases of sepsis caused by Pantoea agglomerans in a teaching hospital. New Microbiol. 2009;32:119–123. [PubMed] [Google Scholar]
- 55.Tiwari S, Beriha SS. Pantoea species causing early onset neonatal sepsis: a case report. J Med Case Rep. 2015;9:188. doi: 10.1186/s13256-015-0670-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Senanayake NP, Thevanesam V, Karunanayake L. An outbreak of Pantoea agglomerans infection in the neonatal intensive care unit at Teaching Hospital, Kandy, Sri Lanka. Sri Lanka J Child Health. 2016;45(1):32–33. [Google Scholar]
- 57.Yablon BR, Dantes R, Tsai V, Lim R, Moulton-Meissner H, Arduino M, Jensen B, Toth Patel M, Vernon MO, Grant-Greene Y, Christiansen D, Conover C, Kallen A, Guh AY. Outbreak of Pantoea agglomerans bloodstream infections at an oncology clinic—Illinois, 2012–2013. Infect Control Hosp Epidemiol. 2017;38(3):314–319. doi: 10.1017/ice.2016.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.AbdAlhussen LS, Darweesh MF. Prevelance and antibiotic susceptibility patterns of Pantoea spp. isolated form clinical and environmental sources in Iraq. Int J ChemTech Res. 2016;9(8):430–437. [Google Scholar]
- 59.Büyükcam A, Tuncer Ö, Gür D, Sancak B, Ceyhan M, Cengiz AB, Kara A. Clinical and microbiological characteristics of Pantoea agglomerans infection in children. J Infect Public Health. 2018;11(3):304–309. doi: 10.1016/j.jiph.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 60.Procop GW, Church DL, Hall GS, Janda WM, Koneman EW, Schreckenberber PC, Woods GL. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 7. Burlington: Jones & Bartlett Learning; 2020. p. 1830. [Google Scholar]
- 61.Brady CL, Venter SN, Cleenwerck I, Engelbeen K, Vancanneyt M, Swings J, Coutinho TA. Pantoea vagans sp. nov., Pantoea eucalypti sp. nov., Pantoea deleyi sp. nov. and Pantoea anthophila sp. nov. Int J Syst Evol Microbiol. 2009;59(9):2339–2345. doi: 10.1099/ijs.0.009241-0. [DOI] [PubMed] [Google Scholar]
- 62.Smits THM, Rezzonico F, Pelludat C, Goesmann A, Frey JE, Duffy B. Genomic and phenotypic characterization of a non-pigmented variant of Pantoea vagans biocontrol strain C9–1 lacking the 530 kb megaplasmid pPag3. FEMS Microbiol Lett. 2010;308(1):48–54. doi: 10.1111/j.1574-6968.2010.01994.x. [DOI] [PubMed] [Google Scholar]
- 63.Cuénod A, Foucault F, Pflüger V, Egli A. Factors associated with MALDI-TOF mass spectral quality of species identification in clinical routine diagnostics. Front Cell Infect Microbiol. 2021;11:646648. doi: 10.3389/fcimb.2021.646648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nhung PH, Ohkusu K, Mishima N, Noda M, Shah MM, Sun X, Hayashi M, Ezaki T. Phylogeny and species identification of the family Enterobacteriaceae based on dnaJ sequences. Diagn Microbiol Inf Dis. 2007;58:153–161. doi: 10.1016/j.diagmicrobio.2006.12.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Genome data were extracted from GenBank or available from the authors after reasonable request.