Abstract
Smoking is the main risk factor for lung cancer (LC), which is the leading cause of cancer-related death worldwide. Independent randomized controlled trials, governmental and inter-governmental task forces, and meta-analyses established that LC screening (LCS) with chest low dose computed tomography (LDCT) decreases the mortality of LC in smokers and former smokers, compared to no-screening, especially in women. Accordingly, several Italian initiatives are offering LCS by LDCT and smoking cessation to about 10,000 high-risk subjects, supported by Private or Public Health Institutions, envisaging a possible population-based screening program. Because LDCT is the backbone of LCS, Italian radiologists with LCS expertise are presenting this position paper that encompasses recommendations for LDCT scan protocol and its reading. Moreover, fundamentals for classification of lung nodules and other findings at LDCT test are detailed along with international guidelines, from the European Society of Thoracic Imaging, the British Thoracic Society, and the American College of Radiology, for their reporting and management in LCS. The Italian College of Thoracic Radiologists produced this document to provide the basics for radiologists who plan to set up or to be involved in LCS, thus fostering homogenous evidence-based approach to the LDCT test over the Italian territory and warrant comparison and analyses throughout National and International practices.
Keywords: Lung cancer, Lung nodule, Early diagnosis, Screening, Computed tomography, Computer assisted diagnosis
Introduction
Lung cancer (LC) is the leading cause of cancer-related death in Italy and worldwide, with over 2 millions cases in 2018 [1]. LC is associated with smoking, it is usually diagnosed in advanced stage in variable association with clinical symptoms and has 85% five-year mortality [1]. In Italy, LC is the third most common neoplasm (11% of alla cancers in 2018) while ranking first cause of cancer death (20% of all cancer deaths in 2018) [2].
Smoking cessation is the intervention for primary prevention of LC [3]. It is estimated that 85–90% of LC are associated with cigarette smoking in Italy, where prevalence of smoking people is 23% [2]. Smoking cessation decreases LC risk after 10 years since quitting [4]. Age is the second established risk factor for LC, and environmental and professional exposures represent additional risk factors [5–10].
Screening with low-dose computed tomography (LDCT) is the main intervention for secondary prevention of LC and decreases the LC mortality by 20–30%, especially in women [11–17]. A number of Italian trials contributed to the screening literature. In particular, over 8,000 subjects were enrolled in the three randomized controlled trials that took place in Italy since the early 2000S. The Multicentric Italian Lung Detection (MILD, 4,099 participants) showed a statistically significant 39% reduction of lung cancer mortality after 10 years of screening, whereas the ITALUNG Trial (3,206 participants) and the Detection And screening of early lung cancer with Novel imaging Technology (DANTE, 2,450 participants) provided similar results in shorter screening periods and with lower statistical power. Non-randomized trials, including COSMOS and BioMILD in Milan, recruited about 10,000 participants [18, 19], and the bioMILD study (4,119 participants) prospectively investigated the integration of LDCT and blood biomarkers for optimized prolonged screening interval at 3 years [20]. An European Committee for Health Technology Assessment concluded that “screening for lung cancer with LDCT may have a mortality benefit” [21] and the United Stated Preventive Services Task Force (USPSTF) has recently broaden inclusion criteria for LDCT screening [5]. Although COVID-19 infection slowed cancer screening interventions [22], an Italian study demonstrated that LDCT screening can be safely performed during the COVID-19 pandemic [23]. The Cochrane Database of Systematic Reviews is encouraging pilot studies, notably with a short list of necessary outcome measures for continuous quality assurance in data collection and future meta-analyses [24] (Table 1).
Table 1.
Summary list of outcomes reported according to their order of priority by the Cochrane Database of Systematic Reviews
| Summary list of outcomes |
|---|
| Lung cancer related mortality |
| All-cause mortality |
|
Incidence of lung cancer During screening period Post screening period |
| Recall rates |
| Harms of screening including the number of invasive tests performed in those with a false positive diagnosis |
| Impact on smoking behaviour (e.g. cessation, relapse rates, smoking intensity) |
| Health-related quality of life and/or psychosocial consequences |
In 2015, LCS by LDCT started in the USA and is reimbursed by Medicare. In Europe, despite availability of several shared guidelines [25–27], population LCS has not started yet. In Italy, an ongoing discussion is supposed to prepare for inclusion of LCS by LDCT into the governmental healthcare supply (e.g. Livelli Essenziali di Assistenza, LEA), which already includes other population-based cancer screening (e.g. breast, colon-rectum and uterine cervix). These screening interventions are part of the National Prevention Plan, which has purportedly to include high-risk and socially or economically disadvantaged individuals [28].
Several initiatives and studies of LDCT for LCS have been funded and have already started or are next to start in Italy in 2021–2022 (Table 2). They feature some differences in method, thus implying heterogeneity of the proposed screening models, including enrolment criteria and modalities, annual or biennial frequency, strategies to promote smoking cessation, and use of biomarkers. However, taking into account the fundamental role of the radiologist in LCS, we trust sharing fundamentals of radiology practice in LCS is mandatory to warrant quality assurance and allow comparison and/or meta-analyses for informing the next step towards population-based LCS. According to such an objective of harmonization, the Italian College of Thoracic Radiologists discussed and elaborated the present document, which aims to be a practical support for radiologists involved or approaching LCS with LDCT in Italy. The following paragraphs present the current standard of reference for LDCT scan protocol, reading method, classification of findings, reporting and major areas of further management.
Table 2.
Funded studies of lung cancer screening with low-dose CT in Italy until 10 September 2021
| Project | Site(s) | Target sample | Inclusion criteria |
|---|---|---|---|
| Rete Italiana Screening Polmonare (RISP) | Istituto Nazionale Tumori di Milano (and associate centres) | 6,500 |
Age: 55–75 years Smoking history: ≥ 30 pack/years, quit ≤ 10 years |
| Progetto Ministeriale PEOPLHE | University Hospitals of Parma, Pavia, and Catania | 1,500 |
Age: 50–75 years Smoking history: ≥ 15 cig/day for ≥ 25 years ≥ 10 cig/day for ≥ 30 years quit ≤ 10 years |
| Italung 2 | Florence, Pisa, Massa Carrara | 700 |
Age: 55–75 years Smoking history: ≥ 30 pack/years, quit ≤ 10 years |
| CCM | Florence, Pisa, Turin, San Raffaele Hospital in Milan | 570 |
Age: 55–75 years Smoking history: ≥ 30 pack/years, quit ≤ 10 years |
Low-dose CT for lung cancer screening: hardware and scan protocol
The screening LDCT is a simple and fast chest examination, which does not require administration of contrast agent. The technical details about hardware, acquisition, and reconstruction of LDCT for LCS were indicated by an expert panel of chest radiologists from the European Society of Thoracic Imaging (ESTI, link to online resource) [29]. Routine LDCT for LCS is hereafter described.
The acquisition starts with a bidimensional scout scan over the chest and is followed by a volume acquisition from apex to lung bases. Deep inspiratory breathhold is mandatory. Any external object must be removed from the chest to minimize radiation exposure and avoid artefacts that would impair nodule measurements. For the volume acquisition, the tube setting is set at low current (typically below 40 mAs) and 120 kVp (or 140) voltage. It is of paramount importance that the tube voltage (and acquisition and reconstruction parameters) is kept consistent through subsequent LDCT examinations of the same subject to allow reliable evaluation of nodule features, especially for subsolid nodules. The above setting aims to minimize the radiation exposure, while maintaining appropriate image quality for volume segmentation [30]. The reduction of radiation exposure is also available via filtering the X-ray beam by tin filter installed between the tube and the aluminium bowtie filter, his technique was proposed by voltage 100 kVp and current 100 mAs with automatic exposure control [31, 32].
The slice collimation must be thin (≤ 1 mm) to grant optimal data quality for image reconstruction. The number of detector rows of the spiral CT scanner is not per se a limitation for LCS. However, CT scanners with few (e.g. 4–16) rows of detectors are becoming obsolete for the purpose of LCS, since they typically require higher radiation doses owing to lower efficiency of old detector technology. Therefore, although screening LDCT has been performed also with few-row CT scanners, the technological development justifies recommendations for up-to-date (64-row or higher) CT scanners. Software development also assists in dose reduction, namely by controlling the noise: iterative reconstructions or deep learning algorithms outstand the old filtered back projection. Phantom studies indicate that advanced reconstruction algorithms together with careful tube setting allow radiation exposures similar to that of chest X-ray (also known as ultra-low dose CT), while being far more sensitive to lung nodules detection [33].
The radiation dose of a screening chest LDCT varies depending on the biometric features (height and weight) of the subject. The ideal threshold of volume computed tomography (CT) dose index (CTDIvol) is set below 2.0 mGy by the America College of Radiology. It is noteworthy that the Italian law (number 101 released 31 July 2020) requires to report the radiation exposure associated with every examination on each radiology report. While setting an optimized LDCT protocol for LCS, the radiologist should also bear in mind that the image quality should also allow assessment of pulmonary emphysema and coronary artery calcifications [34], which along with pulmonary nodule represent the so-called BIG-3 [35].
LDCT test reading
The time required for reading a screening LDCT examination by an experienced radiologist is generally below 10 min, but it can be less than 5 min in case of a negative test [36]. Usually, the LDCT is read by two independent radiologists. This method is similar to that recommended in breast screening and undoubtedly increases the costs of LC (along with the need of dedicated CT scanner spaces and of acquisition and maintenance of software for volumetric assessment of lung nodules size). Not surprisingly, great attention is paid to the possible implementation of Computer Assisted Diagnosis (CAD) systems. In a study in the Netherlands, LDCT reading performed by a single radiologist supported by CAD system replaced double reading [15]. The time required for LCS test reporting varies according to the use of CAD as support to the reader and type of report (free or structured). Adoption of a certified CAD is suggested to help reducing variability in detection rate between readers, while classification might still vary substantially depending on the manual correction often required for nodule segmentation [37]. Overall, the use of CAD for reading LDCT in LCS can be endorsed, but requires an appropriate education on its function, strength, and limits, that have been outlined in specific recommendations by the ESTI [38]. Webinars on the theoretical backgrounds of CAD and practical hands-on workshops by the same expert panel are available to promote CAD use in LCS with LDCT [39]. Nonetheless, the LDCT for LCS should be read by radiologists educated in lung imaging and with specific skills in LCS. For this purpose, since 2019 the ESTI is providing certification courses for theoretical and practical education of radiologists to the practice of LCS [39].
Test outcome
Nodule density
The test outcome depends on the presence of non-calcified lung nodules and on their density and size, as well as their possible growth over time. Non-calcified nodules are classified based on their density in solid (homogeneous soft tissue attenuation), non-solid (ground glass opacity: hazy increased attenuation in the lung that does not obliterate the bronchial and vascular margins) or part-solid (mixed non-solid nodule with soft-tissue attenuation components) [40]. Size measurements are meant for solid nodules and solid component of mixed nodules, which substantially drive the test outcome: the greater the size of the solid component, the higher the probability of cancer.
Nodule size
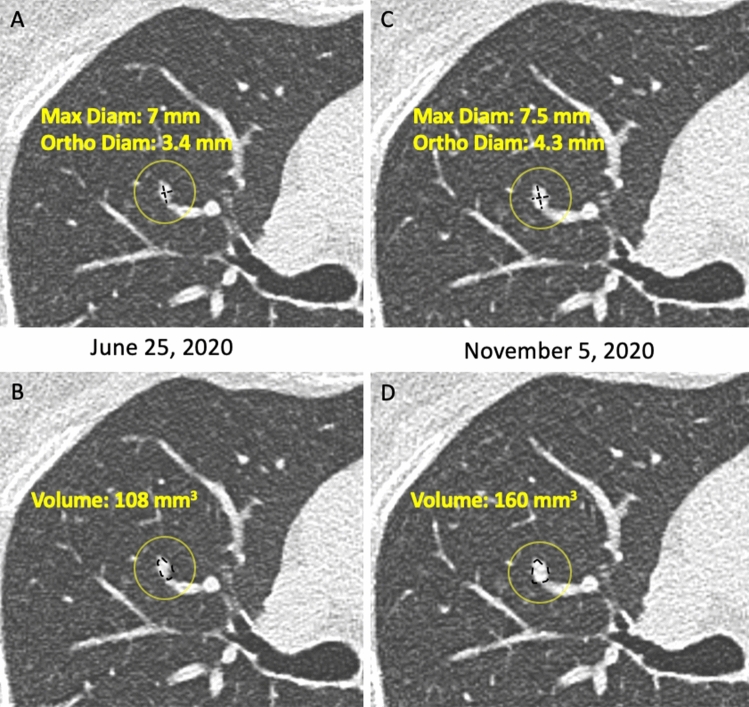
The size of non-calcified solid nodules or of solid component of a mixed nodule can be assessed using bidimensional manual measurement (maximum and orthogonal diameter for calculation of the mean diameter, to one decimal point) [11] or volumetric measurement aided by software [15] (Figs. 1, 2, 3).
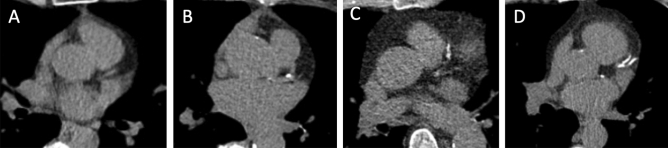
Fig. 1.
A–D. Measurement of a solid nodule with histologic diagnosis of adenocarcinoma in the right upper lobe and its growth. Axial CT image showing a solid nodule in the right upper lobe. Two examples of measurement are displayed: A manual caliper (maximum diameter 7 mm, orthogonal diameter 3.4 mm, mean diameter 5.2 mm) and B semi-automatic volume segmentation (B: 108 mm3). The follow-up scan shows growth of the solid nodule compared to first detection, which is below the minimum threshold of 2 mm by manual caliper (C: 7.5 × 4.3 mm, mean diameter 5.9 mm) and above the minimum threshold of 25% by volume segmentation (160 mm3): such discrepancy reflects into divergent classification as stable by manual caliper and grown by volume segmentation, for this solid nodule that was diagnosed adenocarcinoma. Furthermore, the longitudinal calculation of growth rate shows different estimate of volume doubling time by manual caliper (445 days) or volume segmentation (236 days)
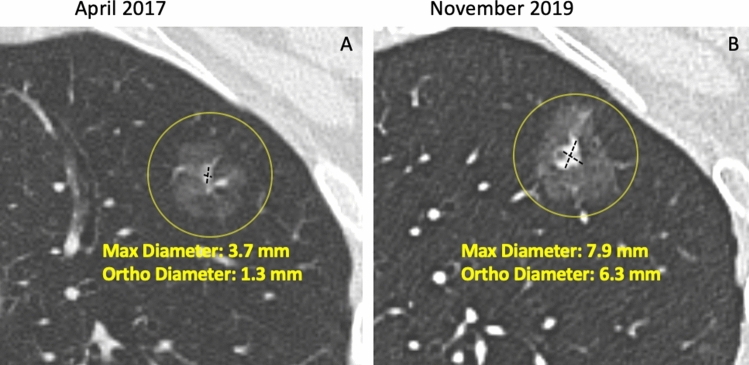
Fig. 2.
A–B. Measurement of a part-solid nodule in the left upper lobe and its growth. Axial CT image showing a part-solid nodule in the left upper lobe. The size of the solid component by manual caliper at first detection (A: maximum diameter 3.7 mm, orthogonal diameter 1.3 mm, mean diameter 2.5 mm) is thereafter confidently increased at follow up scan (B: 7.9 × 6.3 mm, mean diameter 7.1 mm). The variable and limited density difference between solid component and non-solid component represents a factor for variability of semi-automated volume segmentation. Moreover, the figure shows small vessels abutting the surface of the solid component, that is one common factor that further hampers the use of volume segmentation of solid core in part-solid nodules
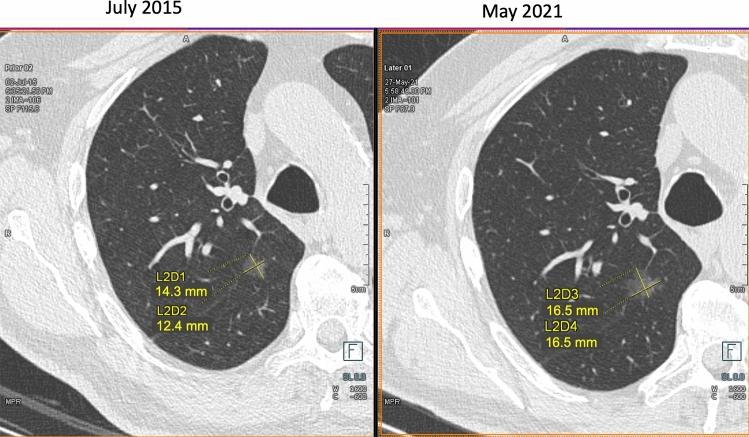
Fig. 3.
A–B. Measurement of a non-solid nodule (ground glass opacity) in the apical segment of the right lower lobe and its growth. Axial CT image showing a non-solid nodule in apical segment of the right lower lobe. The measurement by manual caliper at first detection (maximum diameter 14.3 mm, orthogonal diameter 12.4 mm, mean diameter 13.4 mm) and follow up scan (B: 16.5 × 16.5 mm, mean diameter 16.5 mm). The variable and limited density difference between the non-solid nodule and the surrounding parenchyma represents a factor for variability of semi-automated volume segmentation
Volume measurement of solid nodule is more reproducible and sensitive to nodule growth than manual caliper (Fig. 1). Volumetric software was adopted in the NELSON trial [15] and is strongly recommended in Europe [25]. However, volumetry has a limitations in certain scenarios in which bidimensional (e.g. mean diameter or longest diameter) measurements should be preferred. These scenarios include: (1) solid nodules abutting solid surfaces such as pleura or vessel; (2) solid component of part-solid nodule; (3) non-solid nodules (Fig. 3).
Software for nodule volumetry
Several types of software for nodule segmentation and volume estimation are commercially available. Their performance is much variable with possible over or under-estimation of the nodule size [41]. This variability may impact recall and detection rates even for different releases of the same software. A consistent use of the same software type and release is therefore recommended over time, especially when different software and releases may be available on different CT scanners in the active screening centres.
Classification of the test results
The Lung-RADS 1.1 system is recommended for classification of findings of the chest LDCT for LCS (link to online resource) [42, 43]. It warrants shared lexicon and clear report interpretation. It provides a validated protocol for diagnostic work-up and incorporates the most recent advances in knowledge (e.g. peri-fissural nodules, non-solid nodules, and in the next 2.0 release an update is anticipated dealing with classification and management of cystic lesions [44]. Noteworthy, this reporting system has been adopted in the largest LCS practice, which started in 2015 in the USA and currently involves over a million participants [45]. There is evidence that use of Lung-RADS decreases the rate of false-positive results in lung cancer screening [46].
According to Lung-RADS 1.1 system, lung nodules found on LDCT are divided in 6 categories from 1 to 4X based on density and size characteristics and on the evidence of growth [42]. The higher the category, the higher the risk of malignancy of a given nodule. The category of each LDCT test result should be coded according to the nodule with the highest degree of suspicion, namely the nodule with the highest score (also known as the “dominant nodule”). Lung-RADS 1.1 indicates the size threshold for lung nodule reporting mean diameter:
approximated to one decimal point, and it introduced the use of volume.
Each category has a different management. Nodules belonging to category 1 and 2 correspond to a negative screening test, for which a scheduled annual LDCT is recommended by ACR. Nonetheless, biennial LDCT screening for category 1 and 2 is gaining more and more consensus along with integrated risk models, and this might become the preferred option to optimize cost–benefit ratio of LCS [47, 48]. Differently, category 3 (probably benign), category 4A (suspicious) and category 4B or 4X (very suspicious) nodules qualify for a non-negative screening test. According to Lung-RADS 1.1 system, category 3 lung nodules require 6-month follow-up LDCT, category 4A lung nodules require 3-months follow-up LDCT to ascertain size evolution over time, whereas category 4B and 4X lung nodules require immediate work-up (see below). For new large nodules appearing on a scheduled LDCT screening round and matching 4B category, a 1-month follow-up LDCT is recommended after antibiotic therapy to ascertain potential infectious or inflammatory conditions.
The inclusion of a “S” label to nodule categories allows to indicate other clinically significant or potentially clinically significant findings different from lung cancer [49, 50].
For category 3 (probably benign) nodules Lung-RADS 1.1 recommends a 6 month follow-up LDCT. This 6-month interval is a matter of debate, since other guidelines suggest a shorter 3-month control for the management of the so-called indeterminate nodule [25, 51]. A 3-month follow-up might help contain anxiety for indeterminate results and be more conservative. However, a shorter interval is associated with higher risk that bidimensional but also volume size changes are small and inconclusive. This concept was recently forced and stretched further by the need of delaying LCS screening activity during the pandemic from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). LCS participants with longer follow-up LDCT for “indeterminate nodule” did not incur in stage shift at the time of lung cancer diagnosis [52].
The size threshold for category 4A (suspicious) solid nodules is 8 mm in mean diameter and 268 mm3 in volume on baseline LDCT and 6 mm and 113 mm3 for new nodules appearing at annual repeat LDCT. For category 4B (very suspicious) nodules it is encouraged to use the Brock algorithm that incorporates non-radiological features to predict nodule malignancy [53].
In case of non-solid nodules, Lung-RADS 1.1 recommends follow-up LDCT or interventions only for nodules with a mean diameter ≥ 3 cm, but also in this case the debate is still open [54].
The 4X (very suspicious) category that requires immediate diagnostic work-up can be assigned to small nodules based on special suspicious features as evidence of nodular spiculations or associated mediastinal lymphoadenomegaly [55]. Also a non-solid nodule below 3 cm in size (category 2) should be upgraded to 4X if any interval growth is measured.
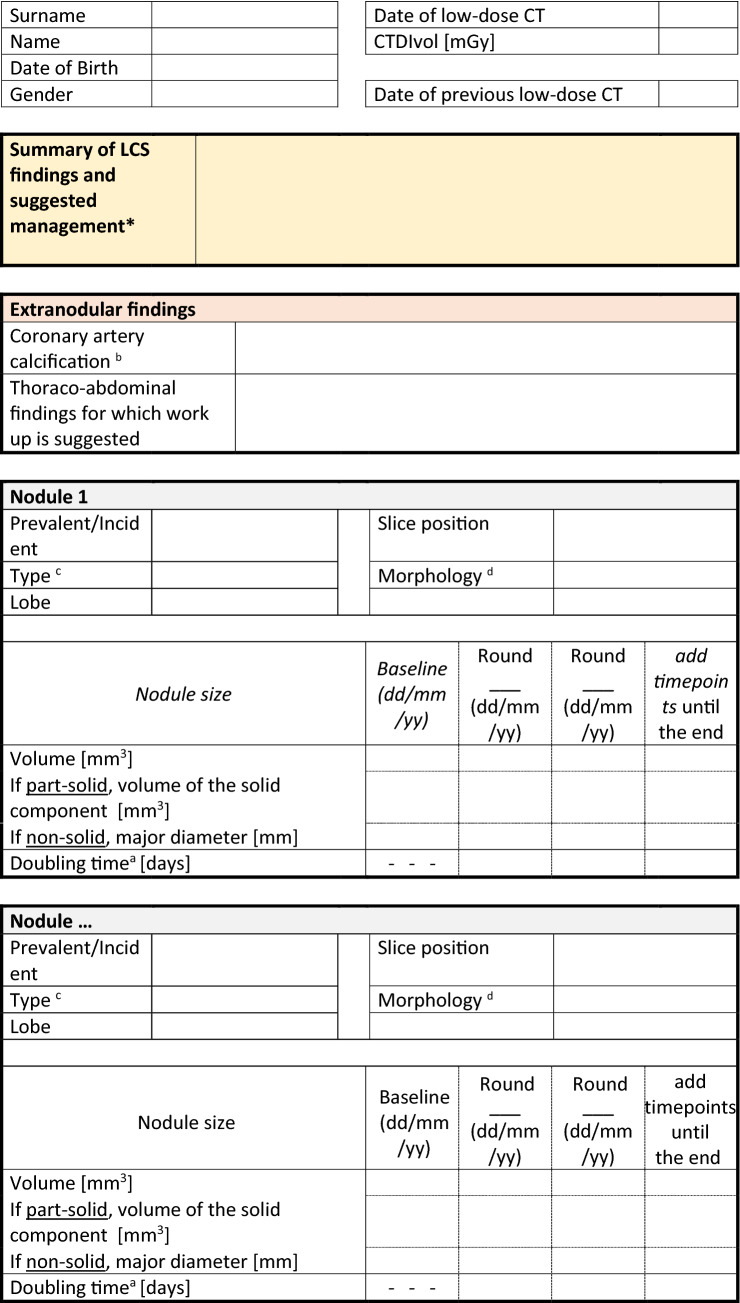
Structured report
Structured report is encouraged to standardize and make LCS with LDCT consistent at large. The ESTI proposed a simplified model for structured report of LDCT [56], which includes the necessary features for nodule descriptions in the LCS setting (Table 3).
Table 3.
Structured report for LDCT in LCS (
modified from www.esti.org) with links for computation of the risk of malignancy of a nodule at baseline (Brock methods)* and of the growth at subsequent low-dose CT examinationsa
*The Brock model calculator is available online from several certified resources, for instance the “PN Risk Calculator” form the British Thoracic Society, either diameter or volume can be used (https://www.brit-thoracic.org.uk/quality-improvement/guidelines/pulmonary-nodules/pn-risk-calculator/)
aThe volume doubling time (VDT) can be calculated with measurement of nodule volume or bit is also accepted by geometric translation of mean diameter. Noteworthy, the VDT is accepted for the specific characterization of solid nodule. The VDT is currently provided by most CADe/CADx software, moreover it is also found online, for instance the “PN Risk Calculator” della British Thoracic Society.
bCoronary artery calcifications can be assessed by semi-quantitative method (0 = absent; 1 = mild; 2 = moderate; 3 = severe) or more complex (from 0 to 12 score) visual scales (see https://doi.org/10.1148/radiol.15142062 and https://doi.org/10.1148/radiol.10100383)
cThe type of nodule is defined according to its: solid/part-solid/non-solid/calcified
dThe morphology of nodule is found in the literature and is usually aimed to stratify risk: spiculation, perifissural nodule
The non-negative LDCT test, namely lung nodules matching Lung-RADS 1.1 categories from 2 to 4X, should be discussed in multidisciplinary teams. To contain costs associated with this procedure, it has been suggested to restrict the multidisciplinary team discussion to lung nodules ≥ 200 mm3 [57].
Diagnostic work-up in positive tests
The work-up of suspicious or highly suspicious (Lung-RADS 1.1 categories 4A-4X) nodules with a solid component exceeding 8 mm can be performed with 18F-fluoro-2-deoxy-glucose -positron emission tomography (FDG-PET)/CT, CT-guided fine needle aspiration or core biopsy, and Video Assisted Thoracic Surgery (VATS). The choice of work-up strategy usually reflects local availability and expertise and is usually accompanied by a staging contrast enhanced CT at standard dose.
Differently, follow-up LDCT is the management tool for indeterminate (Lung-RADS 1.1 category 3) nodules at baseline or annual repeat LDCT with the goal to ascertain possible nodule growth. The latter is trusted at ≥ 25% increase of lesion volume [26], or an increase of the mean diameter > 1.5 mm (Fig. 1). Integrated description of growth dynamics is anticipated for the next Lung-RADS 2.0 release [43, 44]. The dynamics of growth in solid lesion can be estimated by serial LDCT and calculation of the Volume Doubling Time (VDT) (Fig. 1). Notably, the VDT can be calculated based on either mean diameter or segmented volume: a VDT ≤ 400 days is associated with a malignant nodules [25] (Fig. 1). So far, the VDT was validated for solid lung nodules, but not for part-solid or non-solid nodules. For the latter two types of nodules, increase of a solid component in mixed nodules or appearance of new solid component in a former non-solid nodule is considered a sign of significant growth and potential malignancy [58] (Fig. 2, 3).
Collateral and incidental findings
Additional findings in screening LDCT are common, being observed in 4.4 to 40.7% cases. They are more frequent with increasing participants age and can imply further evaluations. The wide variability reflects inconsistent definition of such findings and especially their clinical relevance [59].
Recommendations about reporting of additional findings have evolved [60–62]. To date, the growing experience and advances in knowledge on LDCT screening suggest a “granular interpretation”. The reference guidelines for such a critical interpretation are provided both by the American College of Radiology [50] and the National Health System England [63]. Findings unrelated to LC and pulmonary nodules can be distinguished in smoking-related and non-smoking-related. We shall label smoking-related findings as “collateral findings” which include calcifications of coronary arteries (CAC), pulmonary emphysema and interstitial pulmonary abnormality/disease. The remainder, namely the wide array of non-smoking-related findings will be interpreted as the true “incidental” findings (Table 4).
Table 4.
Examples of incidental (non-smoking related) extra-thoracic findings in LDCT for LCS,
| Incidental findings | Not Actionable | Actionable |
|---|---|---|
| Thyroid |
< 1.5 cm and lack of suspicious features RECOMMENDATION: No further evaluation |
≥ 1.5 cm and/or suspicious findings (Abnormal lymph node (calcifications, cystic components) and/or invasion of local tissues by thyroid nodule) RECOMMENDATION: Thyroid Ultrasound |
| Ascending aorta dilatation |
Ascending aorta diameter 4.0–4.5 cm RECOMMENDATION: report measure in body of text and remeasure on annual screening CT |
Ascending aorta diameter ≥ 4.5–4.9 cm RECOMMENDATION: Echocardiogram and consider referral to cardiology or cardiac surgery Ascending aorta diameter ≥ 5.0 cm RECOMMENDATION: Echocardiogram and refer to cardiac surgery |
| Breast nodule or asymmetry | Definitely benign nodules (e.g. lipoma, densely calcified nodules, etc.) RECOMMENDATION: No further evaluation |
Indeterminate breast findings (e.g. non-calcified nodules, asymmetries, etc.) RECOMMENDATION: Mammogram |
| Indeterminate renal nodule or mass |
Simple renal cysts (− 10 to 20 HU), cysts > 70 HU, and nodules too small to characterize. Fatty nodules without calcification (angiomyolipomas) RECOMMENDATION: No further evaluation |
All other lesions: Defer to judgement of reading radiologist RECOMMENDATION: Ultrasound or additional imaging as per institutional practice |
| Indeterminate hepatic nodule(s) or mass |
Too small to characterize or with benign features (sharply marginated, homogeneous, ≤ 20 HU) RECOMMENDATION: No further evaluation |
Suspicious features (ill-defined margins, heterogeneous density, mural thickening or nodularity, thick septa) or with cirrhosis RECOMMENDATION: Ultrasound or additional imaging as per institutional practice |
Collateral findings
Calcifications of coronary arteries, pulmonary emphysema and interstitial pulmonary abnormalities/disease (Figs. 4, 5, 6) have definite importance having a prognostic value in high-risk smokers and former smokers undergoing LCS with LDCT. In fact, they are associated with increased risk of morbidity and mortality [34], being cardiovascular (CV) disease and respiratory diseases the main non-neoplastic causes of death in LCS participants [11, 12].
Fig. 4.
A–D. Collateral (smoking-related) findings in screening LDCT. Calcifications of the coronary arteries. Axial CT images at the level of the left main coronary artery showing different degrees of coronary artery calcification (CAC): absent = 0 (A), mild = 1 (B), moderate = 2 (C) and severe = 3 (D). According to the scale proposed by Chiles et al. [67], isolated flecks correspond to a mild degree (B), continuous calcification along the vessel correspond a severe degree (D)
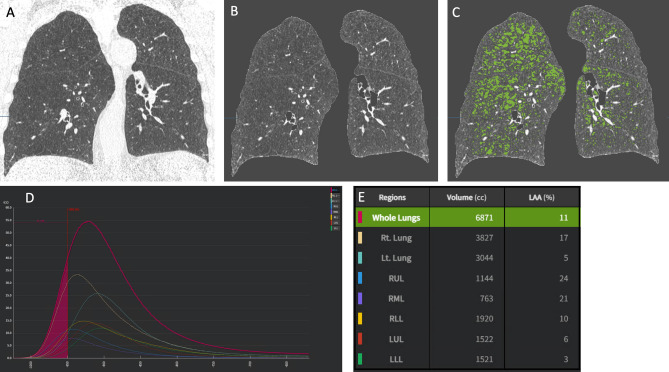
Fig. 5.
A–D. Collateral (smoking-related) findings in screening LDCT. Quantification of pulmonary emphysema with application of the 950HU density mask. Pulmonary emphysema quantified by density mask with segmentation of lung areas with density lower than − 950 HU. The example shows the step-wise process of segmentation of lung parenchyma (A: native image; B: extraction of lung volume) and subsequent quantitation of emphysema extent represented as low attenuation area (LAA) with density below − 950 HU, as represented by green overlay (C). The density histogram (D) shows the distribution of density across the lung volume, and allows to quantify the proportion of LAA below -950 HU as relative extent compared to the overall lung volume (E), namely 11% in this example (specific lobar quantitation is also provided)
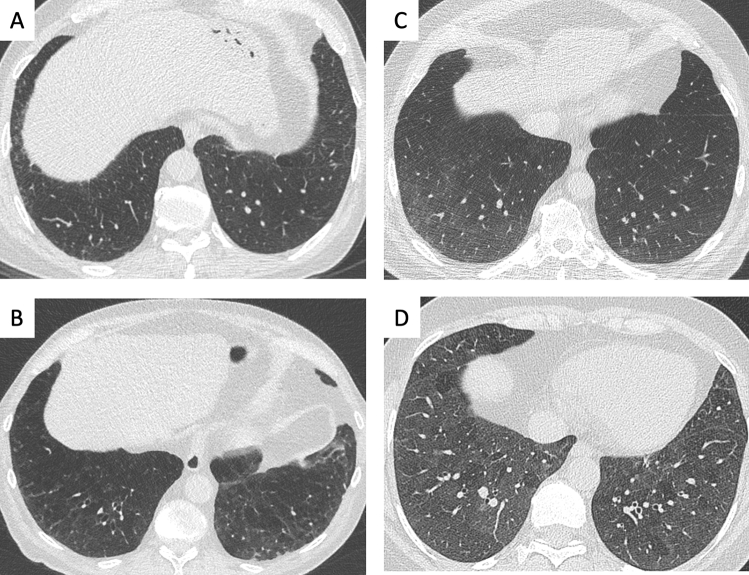
Fig. 6.
A–D. Collateral (smoking-related) findings in screening LDCT:interstitial lung abnormalities with varying extent and morphology.Axial CT image at the level of mid-lower chest showing different patterns of interstitial lung abnormalities with varying severity: A minor reticulation in right lateral sulcus; B reticulation with signs of bronchiolar traction in the lower lobes; C ground-glass opacity with mild extent in the lower lobes; D ground-glass opacity with extensive distribution in the lower lobes, associated with minimal areas of parenchymal sparing with lobular distribution. These findings variably represent smoking related disease, with either reversible or irreversible behaviour worth of multidisciplinary discussion
Calcifications of coronary arteries
CAC are recognized as an independent “risk-enhancing factor” for CV disease [64], because their severity is associated with an increased risk of CV events and mortality, both in smokers and former smokers [65–68]. CAC can be assessed by LDCT using visual score of varying complexity or using software [67]. For screening practice, a swift visual score is emerging [68–71]: 0 = absent; 1 = mild; 2 = moderate; 3 = severe (Fig. 4) [67]. When combined with calcification of the aortic valve, severe CAC is associated with further increase of CV death [72].
Pulmonary emphysema
Densitometry is more reproducible than visual rating for assessment of pulmonary emphysema and must be preferred also in LCS participants [73]. The assessment of lung density in LDCT examinations for LCS (Fig. 5) is valuable since emphysema severity is correlated with either LC incidence, and hence it adds to the post-test risk of LC [74, 75]. Moreover, lung density is correlated with pulmonary function test, smoking history and smoking-cessation [76], and the overall prognosis [77]. Several densitometric measurements can be used for the definition of emphysema presence and severity [78]. Usually “significant” emphysema is assigned when the Relative Area (RA) or Low Attenuation Area (LAA) ≤ 950 Hounsfield Units exceeds 6% of lung parenchyma [79, 80] (Fig. 5).
Interstitial lung disease
Evidence of interstitial lung abnormalities (ILA) or disease (ILD) (Fig. 6) can be particularly relevant in subjects undergoing LCS with LDCT [81]. In fact, ILA can be seen on LDCT in completely asymptomatics subjects [82]. Detection of ILA and its inclusion in the LDCT report with possible discussion in a dedicated multidisciplinary team can add to functional profiling. Identification of ILA should be a strong motivation for quit smoking, whereas the pharmaceutical treatment should be reserved to subjects with established ILD. Moreover, ILA/ILD is a risk factor for also severe complications of LC treatment, including surgery, medical, and radiation therapy.
Admittedly, the ultimate impact of reporting collateral findings in LDCT for LCS and their cost/benefit ratio are hard to define, because the downstream consultation, intervention of primary and secondary prevention and pharmacological treatment have not yet been established. However, certainly, their identification must be used to support smoking quit through access to smoking cessation programs in current smokers who represent the majority of LCS participants. Smoking cessation is offered altogether with LDCT examinations in most LCS initiatives in Italy.
Incidental findings
Screening LDCT can reveal thoracic and extra-thoracic findings which are unrelated to smoking, and represent true “incidental” findings. A Canadian working group classified incidental findings into non-actionable and actionable (Table 4). Benign non-actionable conditions should not be reported. On the other hand, attention must be paid to detection and reporting of actionable findings as dilatation of the ascending aorta or, especially, those potentially associated with malignant lesions of lymphnodes, thyroid gland, thymus, breast, hepato-pacreatic region, adrenal glands, and the kidneys [83]. Extra-pulmonary cancers were diagnosed in 0.5% of subjects participating to the COSMOS observational study in Milan, Italy and in 0.39% of subjects randomized to LDCT in the NLST trial in US [83, 84]. The American College of Radiology Committee on management of incidental findings in chest CT recommends reporting of mediastinal lymphoadenopathy, mediastinal masses, pericardial abnormalities, dilation of the thoracic aorta and of the pulmonary artery [49].
LDCT screening interval, duration and personalization
The recommended interval for LDCT screening is once a year [5]. However, several studies demonstrated that two-year interval allows efficient surveillance while reducing radiation exposure and costs [85–87], whereas longer interval is associated with increased number of advanced LC [85]. The possibility of biennial LDCT screening test should be reserved to subjects with negative baseline by LungRADS 1.1, which represent over 70% of LDCT [47].
Screening should start at age 50 and interrupted at 80 [5]. Moreover, LDCT screening is not recommended for former smokers who quit smoking > 15 years or for people not eligible for or not willing to undergo LC surgery.
So far, the selection of subjects at risk of LC has been mainly based on age and smoking history measured by pack-years. However, the yield of these selection criteria seems relatively low compared to multifactorial profiling [19, 88] including pre-test (before LDCT) findings related to personal and family history [53, 89]. Moreover, several multifactorial risk models aim also to post-test risk refinement by inclusion of findings from LDCT [77, 90]. These factors contribute to stratification of LC risk, as well as of CV and respiratory morbidity and mortality that can ultimately hinder possibility of surgical treatment [5].
The above two general considerations underly the quest of LCS personalization [88, 91, 92] both for LDCT interval [75, 93] and LCS duration in the individual lifetime, also considering the theoretical risk from ionizing radiations [94].
Harms of screening
As for every screening intervention, chest LDCT has its harms [95, 96]. In this manuscript we will mention harms directly related to the radiological practice. They include false-positive results with downstream unnecessary (or even harmful) investigations and invasive work-up, overdiagnosis, distress and anxiety due to indetermined test results, and radiation-induced cancer [97]. In particular, overdiagnosis is a topic of active debate in LCS. Subsolid nodule is probably the most prominent finding associated with slow and potentially clinically indolent growth [58, 98], whose progrostic weight may ultimately be overcome by competing causes of death in heavy smokers or former smokers [77].
On the other hand, also false-negative findings are to be accounted for in LCS practice and this is prone to different interpretations [99]. However, estimate of false-negative rates in an important metric for quality assurance in LCS. False-negative can derive from different moments of the LCS practice, including reading of the LDCT test and definition of nodule management protocols. Accordingly, in the NELSON trial the majority of false-negatives could be attributed to detection or interpretation error [100], whereas the risk of missed cancers increased significantly if screening interval was prolonged at 2.5 years [85].
Psychological distress related to LDCT findings is a further potential harm, which is directly linked to the radiology report [97]. The Danish Lung Cancer Screening Trial investigated the psychological distress in LCS and found that data so far available might be biased by selection of a more robust population [101]. This is probably due to the more favourable socio-demographic profile of people participating in the early LCS trials. Looking towards LCS implementation in the general population, the radiologist should strain towards improved communication of the findings to the screening participant, and this might include accounting for person-hours dedicated to the verbal communication of the report.
Conclusions
In conclusion, LDCT represents the standard of reference for LCS. The use of LDCT as preferred test in LCS is intended as optimal practice, yet not perfect. The Italian College of Thoracic Radiologists is convinced that the use of quality assurance references is mandatory to make population practice as accurate as LCS trial results. Technology update is mandatory to maintain appropriate quality of LCS practice, while continuous education is warranted to follow the most appropriate evidence, similarly to what was already witnessed in mammography screening. The near future of LDCT for LCS calls for preparedness in technology and medical skills, the next step is eventually foreseen in continuous optimization of resources [102].
Funding
Open access funding provided by Università degli Studi di Parma within the CRUI-CARE Agreement.
Declarations
Conflict of interest
The author declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Human or animals rights
No involvement of Participants or Animals.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Passiglia F, Calandri M, Guerrera F, Malapelle U, Mangone L, Ramella S, Trisolini R, Novello S. Lung Cancer in Italy. J Thorac Oncol Offic Publ Int Assoc Study Lung Cancer. 2019;14(12):2046–2052. doi: 10.1016/j.jtho.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 3.Pastorino U, Boffi R, Marchiano A, Sestini S, Munarini E, Calareso G, Boeri M, Pelosi G, Sozzi G, Silva M, Sverzellati N, Galeone C, La Vecchia C, Ghirardi A, Corrao G. Stopping smoking reduces mortality in low-dose computed tomography screening participants. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2016;11(5):693–699. doi: 10.1016/j.jtho.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Tyczynski JE, Bray F, Parkin DM. Lung cancer in Europe in 2000: epidemiology, prevention, and early detection. Lancet Oncol. 2003;4(1):45–55. doi: 10.1016/s1470-2045(03)00960-4. [DOI] [PubMed] [Google Scholar]
- 5.Force USPST, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, Davis EM, Donahue KE, Doubeni CA, Kubik M, Landefeld CS, Li L, Ogedegbe G, Owens DK, Pbert L, Silverstein M, Stevermer J, Tseng CW, Wong JB. Screening for lung cancer: US preventive services task force recommendation statement. JAMA. 2021;325(10):962–970. doi: 10.1001/jama.2021.1117. [DOI] [PubMed] [Google Scholar]
- 6.Su SY, Liaw YP, Jhuang JR, Hsu SY, Chiang CJ, Yang YW, Lee WC. Associations between ambient air pollution and cancer incidence in Taiwan: an ecological study of geographical variations. BMC Public Health. 2019;19(1):1496. doi: 10.1186/s12889-019-7849-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipfert FW, Wyzga RE. Longitudinal relationships between lung cancer mortality rates, smoking, and ambient air quality: a comprehensive review and analysis. Crit Rev Toxicol. 2019;49(9):790–818. doi: 10.1080/10408444.2019.1700210. [DOI] [PubMed] [Google Scholar]
- 8.Lopatin S, Tsay JC, Addrizzo-Harris D, Munger JS, Pass H, Rom WN. Reduced lung function in smokers in a lung cancer screening cohort with asbestos exposure and pleural plaques. Am J Ind Med. 2016;59(3):178–185. doi: 10.1002/ajim.22571. [DOI] [PubMed] [Google Scholar]
- 9.Silva M, Sverzellati N, Colombi D, Milanese G, La Vecchia C, Galeone C, Marchiano A, Pastorino U. Pleural plaques in lung cancer screening by low-dose computed tomography: prevalence, association with lung cancer and mortality. BMC Pulm Med. 2017;17(1):155. doi: 10.1186/s12890-017-0506-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mastrangelo G, Marangi G, Ballarin MN, Fadda E, Scoizzato L, Fedeli U, Marchiori L, Valentini F. Lung cancer risk in past asbestos workers a few decades after exposure cessation and prospects for screening. Arch Environ Occup Health. 2016;71(4):237–244. doi: 10.1080/19338244.2015.1134423. [DOI] [PubMed] [Google Scholar]
- 11.National Lung Screening Trial Research T. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paci E, Puliti D, Lopes Pegna A, Carrozzi L, Picozzi G, Falaschi F, Pistelli F, Aquilini F, Ocello C, Zappa M, Carozzi FM, Mascalchi M, the IWG, Mortality, survival and incidence rates in the ITALUNG randomised lung cancer screening trial. Thorax. 2017 doi: 10.1136/thoraxjnl-2016-209825. [DOI] [PubMed] [Google Scholar]
- 13.Pastorino U, Silva M, Sestini S, Sabia F, Boeri M, Cantarutti A, Sverzellati N, Sozzi G, Corrao G, Marchiano A. Prolonged lung cancer screening reduced 10-year mortality in the MILD trial: new confirmation of lung cancer screening efficacy. Ann Oncol Off J Eur Soc Med Oncol ESMO. 2019;30(7):1162–1169. doi: 10.1093/annonc/mdz117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becker N, Motsch E, Trotter A, Heussel CP, Dienemann H, Schnabel PA, Kauczor HU, Maldonado SG, Miller AB, Kaaks R, Delorme S. Lung cancer mortality reduction by LDCT screening-results from the randomized German LUSI trial. Int J Cancer J Int du Cancer. 2020;146(6):1503–1513. doi: 10.1002/ijc.32486. [DOI] [PubMed] [Google Scholar]
- 15.de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, Lammers JJ, Weenink C, Yousaf-Khan U, Horeweg N, van’t Westeinde S, Prokop M, Mali WP, Mohamed Hoesein FAA, van Ooijen PMA, Aerts J, den Bakker MA, Thunnissen E, Verschakelen J, Vliegenthart R, Walter JE, Ten Haaf K, Groen HJM, Oudkerk M. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–513. doi: 10.1056/NEJMoa1911793. [DOI] [PubMed] [Google Scholar]
- 16.Passiglia F, Cinquini M, Bertolaccini L, Del Re M, Facchinetti F, Ferrara R, Franchina T, Larici AR, Malapelle U, Menis J, Passaro A, Pilotto S, Ramella S, Rossi G, Trisolini R, Novello S. Benefits and harms of lung cancer screening by chest computed tomography: a systematic review and meta-analysis. J Clin Oncol Off J Am Soc Clin Oncol. 2021;39(23):2574–2585. doi: 10.1200/JCO.20.02574. [DOI] [PubMed] [Google Scholar]
- 17.Puliti D, Picozzi G, Gorini G, Carrozzi L, Mascalchi M Gender effect in the ITALUNG screening trial. A comparison with UKLS and other trials. Lancet Reg Health Eur [DOI] [PMC free article] [PubMed]
- 18.Veronesi G, Maisonneuve P, Rampinelli C, Bertolotti R, Petrella F, Spaggiari L, Bellomi M. Computed tomography screening for lung cancer: results of ten years of annual screening and validation of cosmos prediction model. Lung Cancer. 2013;82(3):426–430. doi: 10.1016/j.lungcan.2013.08.026. [DOI] [PubMed] [Google Scholar]
- 19.Pastorino U, Boeri M, Sestini S, Sabia F, Silva M, Suatoni P, Verri C, Cantarutti A, Sverzellati N, Corrao G, Marchiano A, Sozzi G (2019) Blood MicroRNA and LDCT Reduce Unnecessary LDCT Repeats in Lung Cancer Sreening: Results of Prospective bioMILD Trial. Paper presented at the World Congress of Lung Cancer, Barcelona (Spain), September 9, 2019
- 20.Pastorino U, Boeri M, Sestini S, Sabia F, Milanese G, Silva M, Suatoni P, Verri C, Cantarutti A, Sverzellati N, Corrao G, Marchianò A, Sozzi G (Accepted 2022) Blood microRNA and computed tomography predict lung cancer risk and define adequate screening intervals in the BioMILD trial. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO [DOI] [PubMed]
- 21.OTCA28 – ‘Lung cancer screening in risk groups’ (https://www.eunethta.eu/otca28/) (2020).
- 22.Mazzone PJ, Gould MK, Arenberg DA, Chen AC, Choi HK, Detterbeck FC, Farjah F, Fong KM, Iaccarino JM, Janes SM, Kanne JP, Kazerooni EA, MacMahon H, Naidich DP, Powell CA, Raoof S, Rivera MP, Tanner NT, Tanoue LK, Tremblay A, Vachani A, White CS, Wiener RS, Silvestri GA. Management of lung nodules and lung cancer screening during the COVID-19 pandemic: CHEST expert panel report. Chest. 2020 doi: 10.1016/j.chest.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Milanese G, Sabia F, Sestini S, Ledda RE, Rolli L, Suatoni P, Sverzellati N, Sozzi G, Apolone G, Marchiano AV, Pastorino U. Feasibility and safety of lung cancer screening and prevention program during the COVID-19 pandemic. Chest. 2021;160(1):e5–e7. doi: 10.1016/j.chest.2021.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bonney A, Malouf R, Marchal C, Manners D, Fong KM, Marshall HM, Irving LB, Manser R. Low-dose computed tomography (LDCT) screening for lung cancer—related mortality (Protocol) Cochrane Datab Syst Rev. 2021 doi: 10.1002/14651858.CD013829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oudkerk M, Devaraj A, Vliegenthart R, Henzler T, Prosch H, Heussel CP, Bastarrika G, Sverzellati N, Mascalchi M, Delorme S, Baldwin DR, Callister ME, Becker N, Heuvelmans MA, Rzyman W, Infante MV, Pastorino U, Pedersen JH, Paci E, Duffy SW, de Koning H, Field JK. European position statement on lung cancer screening. Lancet Oncol. 2017;18(12):e754–e766. doi: 10.1016/S1470-2045(17)30861-6. [DOI] [PubMed] [Google Scholar]
- 26.Kauczor H-U, Baird A-M, Blum TG, Bonomo L, Bostantzoglou C, Burghuber O, Čepická B, Comanescu A, Couraud S, Devaraj A, Jespersen V, Morozov S, Agmon IN, Peled N, Powell P, Prosch H, Ravara S, Rawlinson J, Revel M-P, Silva M, Snoeckx A, van Ginneken B, van Meerbeeck JP, Vardavas C, von Stackelberg O, Gaga M. ESR/ERS statement paper on lung cancer screening. Eur Radiol. 2020 doi: 10.1007/s00330-020-06727-7. [DOI] [PubMed] [Google Scholar]
- 27.Veronesi G, Baldwin DR, Henschke CI, Ghislandi S, Iavicoli S, Oudkerk M, De Koning HJ, Shemesh J, Field JK, Zulueta JJ, Horgan D, Fiestas Navarrete L, Infante MV, Novellis P, Murray RL, Peled N, Rampinelli C, Rocco G, Rzyman W, Scagliotti GV, Tammemagi MC, Bertolaccini L, Triphuridet N, Yip R, Rossi A, Senan S, Ferrante G, Brain K, van der Aalst C, Bonomo L, Consonni D, Van Meerbeeck JP, Maisonneuve P, Novello S, Devaraj A, Saghir Z, Pelosi G. Recommendations for implementing lung cancer screening with low-dose computed tomography in Europe. Cancers (Basel) 2020 doi: 10.3390/cancers12061672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Definizione e aggiornamento dei livelli essenziali di assistenza, di cui all'articolo 1, comma 7, del decreto legislativo 30 dicembre 1992, n. 502. (17A02015) (2017)
- 29.(ESTI) ESoTI (2019) Chest CT for Lung Cancer Screening: Technical Standards [ https://www.myesti.org/content-esti/uploads/ESTI-LCS-technical-standards_2019-06-14.pdf ].
- 30.(QIBA) QIBA (2018) QIBA Profile: Small Lung Nodule Volume Assessment and Monitoring in Low Dose CT Screening
- 31.Messerli M, Kluckert T, Knitel M, Walti S, Desbiolles L, Rengier F, Warschkow R, Bauer RW, Alkadhi H, Leschka S, Wildermuth S. Ultralow dose CT for pulmonary nodule detection with chest x-ray equivalent dose—a prospective intra-individual comparative study. Eur Radiol. 2017;27(8):3290–3299. doi: 10.1007/s00330-017-4739-6. [DOI] [PubMed] [Google Scholar]
- 32.Milanese G, Silva M, Frauenfelder T, Eberhard M, Sabia F, Martini C, Marchiano A, Prokop M, Sverzellati N, Pastorino U. Comparison of ultra-low dose chest CT scanning protocols for the detection of pulmonary nodules: a phantom study. Tumori. 2019 doi: 10.1177/0300891619847271. [DOI] [PubMed] [Google Scholar]
- 33.Huber A, Landau J, Ebner L, Butikofer Y, Leidolt L, Brela B, May M, Heverhagen J, Christe A. Performance of ultralow-dose CT with iterative reconstruction in lung cancer screening: limiting radiation exposure to the equivalent of conventional chest X-ray imaging. Eur Radiol. 2016;26(10):3643–3652. doi: 10.1007/s00330-015-4192-3. [DOI] [PubMed] [Google Scholar]
- 34.Schreuder A, Jacobs C, Lessmann N, Broeders MJ, Silva M, Isgum I, de Jong PA, Sverzellati N, Prokop M, Pastorino U, Schaefer-Prokop CM, van Ginneken B. Combining pulmonary and cardiac computed tomography biomarkers for disease-specific risk modelling in lung cancer screening. Eur Respir J. 2021 doi: 10.1183/13993003.03386-2020. [DOI] [PubMed] [Google Scholar]
- 35.Heuvelmans MA, Vonder M, Rook M, Groen HJM, De Bock GH, Xie X, Ijzerman MJ, Vliegenthart R, Oudkerk M. Screening for early lung cancer, chronic obstructive pulmonary disease, and cardiovascular disease (the big-3) using low-dose chest computed tomography: current evidence and technical considerations. J Thorac Imaging. 2019;34(3):160–169. doi: 10.1097/RTI.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 36.Bartlett EC, Desai SR, Padley S, Ridge C, Silva M, Milanese G, Ruggirello M, Pastorino U, Darby MJ, Devaraj A (2019) Lung cancer screening reporting feasibility and capacity: what is the current status? Paper presented at the British Society of Thoracic Imaging 2019, Edinburgh, United Kingdom, Nov 7, 2019
- 37.Hwang EJ, Goo JM, Kim HY, Yoon SH, Jin GY, Yi J, Kim Y. Variability in interpretation of low-dose chest CT using computerized assessment in a nationwide lung cancer screening program: comparison of prospective reading at individual institutions and retrospective central reading. Eur Radiol. 2021;31(5):2845–2855. doi: 10.1007/s00330-020-07424-1. [DOI] [PubMed] [Google Scholar]
- 38.Devaraj A, van Ginneken B, Nair A, Baldwin D. Use of volumetry for lung nodule management: theory and practice. Radiology. 2017;284(3):630–644. doi: 10.1148/radiol.2017151022. [DOI] [PubMed] [Google Scholar]
- 39.ESTI Lung Cancer Screening Certification Project. (2019). https://www.myesti.org/lungcancerscreeningcertificationproject/. Accessed December 1 2021
- 40.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Muller NL, Remy J. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 41.Soo E, Edey AJ, Mak SM, Moser J, Mohammadi S, Rodrigues T, Duffy SW, Field JK, Baldwin DR, Nair A, Devaraj A. Impact of choice of volumetry software and nodule management guidelines on recall rates in lung cancer screening. Eur J Radiol. 2019;120:108646. doi: 10.1016/j.ejrad.2019.108646. [DOI] [PubMed] [Google Scholar]
- 42.(ACR) ACoR (2019) Lung-screening reporting and data system (LungRADS) Version 1.1 [ https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads ]. https://www.acr.org/-/media/ACR/Files/RADS/Lung-RADS/LungRADSAssessmentCategoriesv1-1.pdf?la=en. Accessed July 5 2019
- 43.Chelala L, Hossain R, Kazerooni EA, Christensen JD, Dyer DS, White CS. Lung-RADS version 1.1: challenges and a look ahead, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol. 2021;216(6):1411–1422. doi: 10.2214/AJR.20.24807. [DOI] [PubMed] [Google Scholar]
- 44.Christensen JD (2021) Tools for Tracking Nodule Follow-up in Lung Cancer Screening. Paper presented at the Radiology Society of North America (RSNA) Meeting, Chicago (IL), November 29, 2021
- 45.Okereke IC, Nishi S, Zhou J, Goodwin JS. Trends in lung cancer screening in the United States, 2016–2017. J Thorac Dis. 2019;11(3):873–881. doi: 10.21037/jtd.2019.01.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pinsky PF, Gierada DS, Black W, Munden R, Nath H, Aberle D, Kazerooni E. Performance of lung-RADS in the national lung screening trial: a retrospective assessment. Ann Intern Med. 2015;162(7):485–491. doi: 10.7326/M14-2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silva M, Milanese G, Sestini S, Sabia F, Jacobs C, van Ginneken B, Prokop M, Schaefer-Prokop CM, Marchiano A, Sverzellati N, Pastorino U. Lung cancer screening by nodule volume in Lung-RADS v1.1: negative baseline CT yields potential for increased screening interval. Eur Radiol. 2021;31(4):1956–1968. doi: 10.1007/s00330-020-07275-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Myers R, Mayo J, Atkar-Khattra S, Yuan R, Yee J, English J, Mcguire A, Grant K, Dewar L, Tammemagi M, Lam S (2021) Prospective Evaluation of the International Lung Screening Trial (ILST) Protocol for Management of First Screening LDCT. Paper presented at the World Conference on Lung Cancer (WCLC) 2021, Worldwide Virtual Event, September 12, 2021
- 49.Munden RF, Carter BW, Chiles C, MacMahon H, Black WC, Ko JP, McAdams HP, Rossi SE, Leung AN, Boiselle PM, Kent MS, Brown K, Dyer DS, Hartman TE, Goodman EM, Naidich DP, Kazerooni EA, Berland LL, Pandharipande PV. Managing incidental findings on Thoracic CT: mediastinal and cardiovascular findings. A white paper of the ACR incidental findings committee. J Am Coll Radiol. 2018;15(8):1087–1096. doi: 10.1016/j.jacr.2018.04.029. [DOI] [PubMed] [Google Scholar]
- 50.Munden RF, Black WC, Hartman TE, MacMahon H, Ko JP, Dyer DS, Naidich D, Rossi SE, McAdams HP, Goodman EM, Brown K, Kent M, Carter BW, Chiles C, Leung AN, Boiselle PM, Kazerooni EA, Berland LL, Pandharipande PV. Managing incidental findings on thoracic CT: lung findings. A white paper of the ACR incidental findings committee. J Am Coll Radiol. 2021;18(9):1267–1279. doi: 10.1016/j.jacr.2021.04.014. [DOI] [PubMed] [Google Scholar]
- 51.Callister ME, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J, Franks K, Gleeson F, Graham R, Malhotra P, Prokop M, Rodger K, Subesinghe M, Waller D, Woolhouse I, British Thoracic Society Pulmonary Nodule Guideline Development G, British Thoracic Society Standards of Care C (2015) British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax, doi:10.1136/thoraxjnl-2015-207168 [DOI] [PubMed]
- 52.Creamer A, Dickson J, Horst C, Tisi S, Hall H, Verghese P, Mccabe J, Gyertson K, Mullin AM, Farrelly L, Clark C, Hamilton S, Allen B, Hackshaw A, Devaraj A, Nair A, Janes S (2021) Delayed interval scanning is not associated with stage-shift at diagnosis: Preliminary results to support guidelines for lung cancer screening during the COVID-19 pandemic. Paper presented at the European Respiratory Society (ERS) International Congress
- 53.McWilliams A, Tammemagi MC, Mayo JR, Roberts H, Liu G, Soghrati K, Yasufuku K, Martel S, Laberge F, Gingras M, Atkar-Khattra S, Berg CD, Evans K, Finley R, Yee J, English J, Nasute P, Goffin J, Puksa S, Stewart L, Tsai S, Johnston MR, Manos D, Nicholas G, Goss GD, Seely JM, Amjadi K, Tremblay A, Burrowes P, MacEachern P, Bhatia R, Tsao MS, Lam S. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910–919. doi: 10.1056/NEJMoa1214726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kastner J, Hossain R, Jeudy J, Dako F, Mehta V, Dalal S, Dharaiya E, White C. Lung-RADS version 1.0 versus lung-RADS version 1.1: comparison of categories using nodules from the national lung screening trial. Radiology. 2021;300(1):199–206. doi: 10.1148/radiol.2021203704. [DOI] [PubMed] [Google Scholar]
- 55.Chung K, Jacobs C, Scholten ET, Goo JM, Prosch H, Sverzellati N, Ciompi F, Mets OM, Gerke PK, Prokop M, van Ginneken B, Schaefer-Prokop CM. Lung-RADS Category 4X: Does it improve prediction of malignancy in subsolid nodules? Radiology. 2017 doi: 10.1148/radiol.2017161624. [DOI] [PubMed] [Google Scholar]
- 56.(ESTI) ESoTI (2019) Chest CT for Lung cancer screening: structured report basic template
- 57.Horst C, Dickson JL, Tisi S, Ruparel M, Nair A, Devaraj A, Janes SM. Delivering low-dose CT screening for lung cancer: a pragmatic approach. Thorax. 2020;75(10):831–832. doi: 10.1136/thoraxjnl-2020-215131. [DOI] [PubMed] [Google Scholar]
- 58.Silva M, Prokop M, Jacobs C, Capretti G, Sverzellati N, Ciompi F, van Ginneken B, Schaefer-Prokop CM, Galeone C, Marchiano A, Pastorino U. Long-term active surveillance of screening detected subsolid nodules is a safe strategy to reduce overtreatment. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2018 doi: 10.1016/j.jtho.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 59.Jonas DE, Reuland DS, Reddy SM, Nagle M, Clark SD, Weber RP, Enyioha C, Malo TL, Brenner AT, Armstrong C, Coker-Schwimmer M, Middleton JC, Voisin C, Harris RP. Screening for lung cancer with low-dose computed tomography: updated evidence report and systematic review for the US preventive services task force. JAMA. 2021;325(10):971–987. doi: 10.1001/jama.2021.0377. [DOI] [PubMed] [Google Scholar]
- 60.van de Wiel JC, Wang Y, Xu DM, van der Zaag-Loonen HJ, van der Jagt EJ, van Klaveren RJ, Oudkerk M, group Ns, Neglectable benefit of searching for incidental findings in the Dutch-Belgian lung cancer screening trial (NELSON) using low-dose multidetector CT. Eur Radiol. 2007;17(6):1474–1482. doi: 10.1007/s00330-006-0532-7. [DOI] [PubMed] [Google Scholar]
- 61.Kucharczyk MJ, Menezes RJ, McGregor A, Paul NS, Roberts HC. Assessing the impact of incidental findings in a lung cancer screening study by using low-dose computed tomography. Can Assoc Radiol J. 2011;62(2):141–145. doi: 10.1016/j.carj.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 62.Puliti D, Mascalchi M, Carozzi FM, Carrozzi L, Falaschi F, Paci E, Lopes Pegna A, Aquilini F, Barchielli A, Bartolucci M, Grazzini M, Picozzi G, Pistelli F, Rosselli A, Zappa M, Group IW (2019) Decreased cardiovascular mortality in the ITALUNG lung cancer screening trial: Analysis of underlying factors. Lung cancer 138:72-78. doi:10.1016/j.lungcan.2019.10.006 [DOI] [PubMed]
- 63.Quality Assurance Standards prepared for the Targeted Lung Health Checks Programme (2019). https://www.england.nhs.uk/wp-content/uploads/2019/02/targeted-screening-for-lung-cancer-quality-assurance-standard.pdf
- 64.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC, Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 65.Shemesh J, Henschke CI, Shaham D, Yip R, Farooqi AO, Cham MD, McCauley DI, Chen M, Smith JP, Libby DM, Pasmantier MW, Yankelevitz DF. Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology. 2010;257(2):541–548. doi: 10.1148/radiol.10100383. [DOI] [PubMed] [Google Scholar]
- 66.Sverzellati N, Cademartiri F, Bravi F, Martini C, Gira FA, Maffei E, Marchiano A, La Vecchia C, De Filippo M, Kuhnigk JM, Rossi C, Pastorino U. Relationship and prognostic value of modified coronary artery calcium score, FEV1, and emphysema in lung cancer screening population: the MILD trial. Radiology. 2012;262(2):460–467. doi: 10.1148/radiol.11110364. [DOI] [PubMed] [Google Scholar]
- 67.Chiles C, Duan F, Gladish GW, Ravenel JG, Baginski SG, Snyder BS, DeMello S, Desjardins SS, Munden RF, Team NS (2015) Association of coronary artery calcification and mortality in the national lung screening trial: a comparison of three scoring methods. Radiology 276 (1):82-90. 10.1148/radiol.15142062 [DOI] [PMC free article] [PubMed]
- 68.Mascalchi M, Puliti D, Romei C, Picozzi G, De Liperi A, Diciotti S, Bartolucci M, Grazzini M, Vannucchi L, Falaschi F, Pistelli F, Gorini G, Carozzi F, Rosselli A, Carrozzi L, Paci E, Zappa M. Moderate-severe coronary calcification predicts long-term cardiovascular death in CT lung cancer screening: The ITALUNG trial. Eur J Radiol. 2021;145:110040. doi: 10.1016/j.ejrad.2021.110040. [DOI] [PubMed] [Google Scholar]
- 69.Balata H, Blandin Knight S, Barber P, Colligan D, Crosbie EJ, Duerden R, Elton P, Evison M, Greaves M, Howells J, Irion K, Karunaratne D, Kirwan M, Macnab A, Mellor S, Miller C, Newton T, Novasio J, Sawyer R, Sharman A, Slevin K, Smith E, Taylor B, Taylor S, Tonge J, Walsham A, Waplington S, Whittaker J, Booton R, Crosbie PAJ. Targeted lung cancer screening selects individuals at high risk of cardiovascular disease. Lung Cancer. 2018;124:148–153. doi: 10.1016/j.lungcan.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 70.Ruparel M, Quaife SL, Dickson JL, Horst C, Burke S, Taylor M, Ahmed A, Shaw P, Soo MJ, Nair A, Devaraj A, O'Dowd EL, Bhowmik A, Navani N, Sennett K, Duffy SW, Baldwin DR, Sofat R, Patel RS, Hingorani A, Janes SM. Evaluation of cardiovascular risk in a lung cancer screening cohort. Thorax. 2019;74(12):1140–1146. doi: 10.1136/thoraxjnl-2018-212812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tailor TD, Chiles C, Yeboah J, Rivera MP, Tong BC, Schwartz FR, Benefield T, Lane LM, Stashko I, Thomas SM, Henderson LM. Cardiovascular risk in the lung cancer screening population: a multicenter study evaluating the association between coronary artery calcification and preventive statin prescription. J Am Coll Radiol. 2021;18(9):1258–1266. doi: 10.1016/j.jacr.2021.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhu Y, Yip R, Shemesh J, Jirapatnakul AC, Yankelevitz DF, Henschke CI. Combined aortic valve and coronary artery calcifications in lung cancer screening as predictors of death from cardiovascular disease. Eur Radiol. 2020;30(12):6847–6857. doi: 10.1007/s00330-020-07049-4. [DOI] [PubMed] [Google Scholar]
- 73.Cavigli E, Camiciottoli G, Diciotti S, Orlandi I, Spinelli C, Meoni E, Grassi L, Farfalla C, Pistolesi M, Falaschi F, Mascalchi M. Whole-lung densitometry versus visual assessment of emphysema. Eur Radiol. 2009;19(7):1686–1692. doi: 10.1007/s00330-009-1320-y. [DOI] [PubMed] [Google Scholar]
- 74.Labaki WW, Xia M, Murray S, Hatt CR, Al-Abcha A, Ferrera MC, Meldrum CA, Keith LA, Galban CJ, Arenberg DA, Curtis JL, Martinez FJ, Kazerooni EA, Han MK. Quantitative emphysema on low-dose CT imaging of the chest and risk of lung cancer and airflow obstruction: an analysis of the national lung screening trial. Chest. 2021;159(5):1812–1820. doi: 10.1016/j.chest.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Robbins HA, Berg CD, Cheung LC, Chaturvedi AK, Katki HA. Identification of candidates for longer lung cancer screening intervals following a negative low-dose computed tomography result. J Natl Cancer Inst. 2019;111(9):996–999. doi: 10.1093/jnci/djz041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ashraf H, Lo P, Shaker SB, de Bruijne M, Dirksen A, Tonnesen P, Dahlback M, Pedersen JH. Short-term effect of changes in smoking behaviour on emphysema quantification by CT. Thorax. 2011;66(1):55–60. doi: 10.1136/thx.2009.132688. [DOI] [PubMed] [Google Scholar]
- 77.Schreuder A, Jacobs C, Lessmann N, Broeders M, Silva M, Isgum I, de Jong P, van den Heuvel M, Sverzellati N, Prokop M, Pastorino U, Schaefer-Prokop C, van Ginneken B (In Press) Scan-based competing death risk model for reevaluating lung cancer computed tomography screening eligibility. Eur Respir J [DOI] [PubMed]
- 78.Mascalchi M, Camiciottoli G, Diciotti S. Lung densitometry: why, how and when. J Thorac Dis. 2017;9(9):3319–3345. doi: 10.21037/jtd.2017.08.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gevenois PA, De Vuyst P, de Maertelaer V, Zanen J, Jacobovitz D, Cosio MG, Yernault JC. Comparison of computed density and microscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med. 1996;154(1):187–192. doi: 10.1164/ajrccm.154.1.8680679. [DOI] [PubMed] [Google Scholar]
- 80.Lynch DA, Austin JH, Hogg JC, Grenier PA, Kauczor HU, Bankier AA, Barr RG, Colby TV, Galvin JR, Gevenois PA, Coxson HO, Hoffman EA, Newell JD, Jr, Pistolesi M, Silverman EK, Crapo JD. CT-Definable subtypes of chronic obstructive pulmonary disease: a statement of the fleischner society. Radiology. 2015;277(1):192–205. doi: 10.1148/radiol.2015141579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sverzellati N, Guerci L, Randi G, Calabro E, La Vecchia C, Marchiano A, Pesci A, Zompatori M, Pastorino U. Interstitial lung diseases in a lung cancer screening trial. Eur Respir J. 2011;38(2):392–400. doi: 10.1183/09031936.00201809. [DOI] [PubMed] [Google Scholar]
- 82.Hatabu H, Hunninghake GM, Richeldi L, Brown KK, Wells AU, Remy-Jardin M, Verschakelen J, Nicholson AG, Beasley MB, Christiani DC, San Jose Estepar R, Seo JB, Johkoh T, Sverzellati N, Ryerson CJ, Graham Barr R, Goo JM, Austin JHM, Powell CA, Lee KS, Inoue Y, Lynch DA. Interstitial lung abnormalities detected incidentally on CT: a position paper from the fleischner society. Lancet Respir Med. 2020;8(7):726–737. doi: 10.1016/S2213-2600(20)30168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rampinelli C, Preda L, Maniglio M, Sirica L, Travaini LL, Veronesi G, Bellomi M. Extrapulmonary malignancies detected at lung cancer screening. Radiology. 2011;261(1):293–299. doi: 10.1148/radiol.11102231. [DOI] [PubMed] [Google Scholar]
- 84.Nguyen XV, Davies L, Eastwood JD, Hoang JK. Extrapulmonary findings and malignancies in participants screened with chest CT in the national lung screening trial. J Am Coll Radiol. 2017;14(3):324–330. doi: 10.1016/j.jacr.2016.09.044. [DOI] [PubMed] [Google Scholar]
- 85.Yousaf-Khan U, van der Aalst C, de Jong PA, Heuvelmans M, Scholten E, Lammers JW, van Ooijen P, Nackaerts K, Weenink C, Groen H, Vliegenthart R, Ten Haaf K, Oudkerk M, de Koning H. Final screening round of the NELSON lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax. 2017;72(1):48–56. doi: 10.1136/thoraxjnl-2016-208655. [DOI] [PubMed] [Google Scholar]
- 86.Pastorino U, Sverzellati N, Sestini S, Silva M, Sabia F, Boeri M, Cantarutti A, Sozzi G, Corrao G, Marchiano A. Ten-year results of the multicentric italian lung detection trial demonstrate the safety and efficacy of biennial lung cancer screening. Eur J Cancer. 2019;118:142–148. doi: 10.1016/j.ejca.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sverzellati N, Silva M, Calareso G, Galeone C, Marchiano A, Sestini S, Sozzi G, Pastorino U. Low-dose computed tomography for lung cancer screening: comparison of performance between annual and biennial screen. Eur Radiol. 2016;26(11):3821–3829. doi: 10.1007/s00330-016-4228-3. [DOI] [PubMed] [Google Scholar]
- 88.Ten Haaf K, van der Aalst CM, de Koning HJ, Kaaks R, Tammemagi MC. Personalising lung cancer screening: an overview of risk-stratification opportunities and challenges. Int J Cancer J Int du Cancer. 2021;149(2):250–263. doi: 10.1002/ijc.33578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Raji OY, Duffy SW, Agbaje OF, Baker SG, Christiani DC, Cassidy A, Field JK. Predictive accuracy of the Liverpool Lung Project risk model for stratifying patients for computed tomography screening for lung cancer: a case-control and cohort validation study. Ann Intern Med. 2012;157(4):242–250. doi: 10.7326/0003-4819-157-4-201208210-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lebrett MB, Balata H, Evison M, Colligan D, Duerden R, Elton P, Greaves M, Howells J, Irion K, Karunaratne D, Lyons J, Mellor S, Myerscough A, Newton T, Sharman A, Smith E, Taylor B, Taylor S, Walsham A, Whittaker J, Barber PV, Tonge J, Robbins HA, Booton R, Crosbie PAJ. Analysis of lung cancer risk model (PLCOM2012 and LLPv2) performance in a community-based lung cancer screening programme. Thorax. 2020;75(8):661–668. doi: 10.1136/thoraxjnl-2020-214626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.O'Dowd EL, Ten Haaf K. Lung cancer screening: enhancing risk stratification and minimising harms by incorporating information from screening results. Thorax. 2019;74(9):825–827. doi: 10.1136/thoraxjnl-2019-213156. [DOI] [PubMed] [Google Scholar]
- 92.Baldwin D, O'Dowd E, Ten Haaf K. Targeted screening for lung cancer is here but who do we target and how? Thorax. 2020;75(8):617–618. doi: 10.1136/thoraxjnl-2020-215156. [DOI] [PubMed] [Google Scholar]
- 93.Patz EF, Jr, Greco E, Gatsonis C, Pinsky P, Kramer BS, Aberle DR. Lung cancer incidence and mortality in National Lung Screening Trial participants who underwent low-dose CT prevalence screening: a retrospective cohort analysis of a randomised, multicentre, diagnostic screening trial. Lancet Oncol. 2016;17(5):590–599. doi: 10.1016/S1470-2045(15)00621-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rampinelli C, De Marco P, Origgi D, Maisonneuve P, Casiraghi M, Veronesi G, Spaggiari L, Bellomi M. Exposure to low dose computed tomography for lung cancer screening and risk of cancer: secondary analysis of trial data and risk-benefit analysis. BMJ. 2017;356:j347. doi: 10.1136/bmj.j347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Robbins HA, Callister M, Sasieni P, Quaife SL, Cheung LC, Brennan P, Katki HA, Berg CD, Baldwin D, Johansson M. Benefits and harms in the national lung screening trial: expected outcomes with a modern management protocol. Lancet Respir Med. 2019 doi: 10.1016/S2213-2600(19)30136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.de Koning HJ, Meza R, Plevritis SK, ten Haaf K, Munshi VN, Jeon J, Erdogan SA, Kong CY, Han SS, van Rosmalen J, Choi SE, Pinsky PF, Berrington de Gonzalez A, Berg CD, Black WC, Tammemagi MC, Hazelton WD, Feuer EJ, McMahon PM. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive services task force. Ann Intern Med. 2014;160(5):311–320. doi: 10.7326/M13-2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kauczor H-U, Baird A-M, Blum TG, Bonomo L, Bostantzoglou C, Burghuber O, Čepická B, Comanescu A, Couraud S, Devaraj A, Jespersen V, Morozov S, Nardi Agmon I, Peled N, Powell P, Prosch H, Ravara S, Rawlinson J, Revel M-P, Silva M, Snoeckx A, van Ginneken B, van Meerbeeck JP, Vardavas C, von Stackelberg O, Gaga M. ESR/ERS statement paper on lung cancer screening. Eur Respir J. 2020;55(2):1900506. doi: 10.1183/13993003.00506-2019. [DOI] [PubMed] [Google Scholar]
- 98.Yip R, Li K, Liu L, Xu D, Tam K, Yankelevitz DF, Taioli E, Becker B, Henschke CI. Controversies on lung cancers manifesting as part-solid nodules. Eur Radiol. 2018;28(2):747–759. doi: 10.1007/s00330-017-4975-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bartlett EC, Silva M, Callister ME, Devaraj A. False negative results in lung cancer screening—evidence and controversies. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2021 doi: 10.1016/j.jtho.2021.01.1607. [DOI] [PubMed] [Google Scholar]
- 100.Scholten ET, Horeweg N, de Koning HJ, Vliegenthart R, Oudkerk M, Mali WP, de Jong PA. Computed tomographic characteristics of interval and post screen carcinomas in lung cancer screening. Eur Radiol. 2015;25(1):81–88. doi: 10.1007/s00330-014-3394-4. [DOI] [PubMed] [Google Scholar]
- 101.Hestbech MS, Siersma V, Dirksen A, Pedersen JH, Brodersen J. Participation bias in a randomised trial of screening for lung cancer. Lung Cancer. 2011;73(3):325–331. doi: 10.1016/j.lungcan.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 102.Smith HB, Ward R, Frazier C, Angotti J, Tanner NT. Guideline recommended lung cancer screening adherence is superior with centralized approach. Chest. 2021 doi: 10.1016/j.chest.2021.09.002. [DOI] [PubMed] [Google Scholar]