ABSTRACTS
Indian Society of Gastroenterology
Plenary Session
001
Soluble factors and suppressive monocytes can predict early the development of sepsis in acute-on-chronic liver failure
Pushpa Yadav1, Nirupama Trehanpati1, Rakhi Maiwall2, Rashi Sehgal1, Ravinder Singh1, Mojahidul Islam1, Rakesh Kumar Jagdish2, V Rajan2, Deepanshu Maheshwari1, Sadam Bhat1, Pratibha Kale3, Anupam Kumar1, Sukriti Sukriti1, Guresh Kumar1, Gayatri Ramakrishna1, Shiv K Sarin2
Correspondence – Shiv K Sarin – shivsarin@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Hepatology, and 3Microbiology, Institute of Liver and Biliary Sciences, D1, Vasant Kunj, New Delhi 110 070, India
Background and Aim Acute-on-chronic liver failure (ACLF) patients have a high probability to develop systemic inflammatory response syndrome (SIRS) and sepsis due to immune dysregulation. We investigated serial changes in the immune system during sepsis development and the role of potential biomarkers in ACLF patients.
Methods Fifty-nine ACLF patients; 12 with no-SIRS, 19 with-SIRS, and 28 with sepsis were serially monitored for clinical and immunological changes at baseline, 6 hours, day-1, day-3 and day-7 following hospitalization. Ten healthy controls were also included.
Results ACLF patients with-SIRS showed higher vascular endothelial growth factor-a (VEGF-a), monocyte chemoattractant protein-1 (MCP-1) and macrophage inflammatory protein (MIP1β), than no-SIRS patients at admission and all time points (p<0.01). ACLF patients with sepsis had raised (p<0.001) levels of Interleukin-(IL-)1Ra and IL-18 and triggering receptor expressed on myeloid cells (TREM1) compared to patients with-SIRS. Five of 19 (26.3%) patients with-SIRS showed a rise within 24 hours in levels of IL-1Ra (1,203 to 35,000 pg/mL), IL-18 (48 to 114 pg/mL) and TREM1 (1,273 to 4,865 pg/mL) and developed sepsis within 48 hours. Monocytes of ACLF patients with-SIRS and with sepsis showed reduced HLA-DR expression, oxidative burst activity and low mRNA for hypoxia induced factor-1α. On co-culture with T cells from healthy controls, monocytes of ACLF patients showed increased programmed death ligand-1 (PDL1) and T-cell immunoglobulin and mucin domain-containing protein-3 (Tim3) (p<0.04) expression and extracellular traps at baseline and till day-7.
Conclusions High and rising levels of plasma IL-1Ra, IL-18, TREM1 and increased PDL1 and TIM3+ve suppressive monocytes can stratify ACLF patients who are at a higher risk of developing sepsis within 48-72 hours. These cytokines and cellular markers could serve as important biomarkers for early identification of sepsis development.
Keywords Liver Failure, Cirrhosis, Sepsis
002
Impact of transmural plastic stent on recurrence of pancreatic fluid collection after metal stent removal in walled off necrosis with disconnected pancreatic duct: A randomized controlled trial
Radhika Chavan , Sundeep Lakhtakia, Zaheer Nabi, Rajesh Gupta, Jahangeer Basha, Rupjyoti Talukdar, D. Nageshwar Reddy
Correspondence – Sundeep Lakhtakia – drsundeeplakhtakia@gmail.com
Department of Medical Gastroenterology, Asian institute of Gastroenterology, 6-3-661, Somajiguda, Hyderabad 500 082, India
Background and Aim Disconnected pancreatic duct (DPD) after development of walled off necrosis (WON) predisposes to recurrent (peri)pancreatic fluid collection (PFC). In this randomized controlled trial, we aimed to compare the role of plastic stent vs. no plastic stent after removal of LCMS on the incidence of recurrent PFC in cases with DPD.
Methods Consecutive cases with WON who underwent endoscopic ultrasound (EUS)-guided drainage with LCMS from September 2017 till March 2020 were screened for eligibility. At the time of LCMS removal (4 weeks after drainage) cases with DPD documented on magnetic resonance cholangiopancreatography (MRCP) as well as on endoscopic retrograde cholangiopancreatography (ERCP) were randomized to either plastic stent or no stent groups. Primary outcome of the study was incidence of recurrent PFC at 3-months. Secondary outcomes were technical success of plastic stent deployment, adverse events, stent migration and recurrence of PFC at 6 and 12-months.
Results Total 236 cases with WON underwent EUS-guided drainage using LCMS during the study period. 104 (males 94, mean age 35.96±12.47 years) cases with DPD were randomized into stenting (n=52) and no stenting (n=52) groups. Plastic stent deployment was successful in 88%. Migration occurred in 19% cases at a median follow-up of 8 (1-24) months. Overall, recurrent PFC were detected in 20 cases (stent-7, no stent-13, p=0.213). There was no significant difference in the recurrence of PFC between the two groups at 3, 6 and 12-months (p=0.114). Re-intervention was required in 7 cases (Stent group-3, no stent group-4, p= 0.617) with recurrent PFC with no significant difference between the two groups.
Conclusion In cases with WON and DPD, deployment of plastic stents after LCMS removal does not reduce recurrence of PFC. (Clinicaltrials.gov number: NCT03436043)
Keywords Necrotizing pancreatitis, Walled off necrosis, Disconnected pancreatic duct syndrome
003
Integrated bile lipidome and meta-proteome analysis classifies lipid species and microbial peptides predictive of carcinoma of gallbladder
Nupur Sharma, Manisha Yadav, Gaurav Tripathi, Babu Mathew, Vasundhra Bindal, Sadam Bhat, Jaswinder Maras, Shiv Sarin
Correspondence – Jaswinder Maras – jassi2param@gmail.com
Department of Molecular and Cellular Medicine, Institute of Liver and Biliary Science, D1 Vasant Kunj, New Delhi 110 070, India
Histopathological examination is gold standard for detection of gallstone (GS) or gallbladder carcinoma (CAGB). Bile concentrated in the gallbladder, is expected to recapitulate metagenomics/molecular changes associated to development of CAGB. Bile samples were screened for lipidomics and metaproteome (microbiome) signatures capable of early detection of cancer. Analysis of training cohort (n=87) showed that meta-stability of bile was reduced in CAGB patients (p<0.05). Our results showed that CAGB was associated with the alteration of bile lipidome and microbiome as indicated by multivariate PLS-regression analysis and alpha, beta diversity indexes. Significant reduction of lipid species and increase in bacterial taxa were found associated to development of CAGB with gallstone and without gallstone (p<0.05, Log FC>1.5). Multimodular correlation network (MMCN) created using weighted lipid. Meta-proteomic correlation network analysis (W [L/MP] ©) showed striking associations between lipid modules and meta-proteomic functionality. A significant and direct correlation of Meta-proteomic modules functionality and inversely correlation of lipid modules and species with the clinical parameters and bile acid profile was observed in CAGB patients (p<0.05). 5atient5d5s increase in bacterial taxa; Leptospira, Salmonella enterica, Mycoplasma gallisepticum and their functionality showed direct correlation with lipid classes; Glycophosphatidylinositol, Ceramide 1-phosphates, Lysophosphatidylethanolamine, others and development of CAGB (r2>0.85). Lipid/metaproteomic signature-based probability for CAGB was >90% whereas probability for gallstone was >80% (p<0.05). Finally, we identified 8 lipid species of diagnostic capability for CAGB and cross-validated, using 4 machine learning approaches in two separate test cohorts (n=38; bile (T1) and paired plasma (T2) cohort, which jointly showed highest accuracy (99%), sensitivity (98%) and specificity (100%) with random forest model for CAGB detection. We are first to characterize the lipidome and metaproteome of bile and identify a panel of lipid species /bacterial peptides capable of segregating patients predisposed to carcinogenesis of the gallbladder.
Keywords Gallbladder carcinoma, Bile lipidome, Bile microbiome, Machine learning
004
Mycobial (fungal) dysbiosis within walled off necrosis in patients with acute necrotizing pancreatitis
Ila Srnivas 1 , Prianka Sarkar 2 , Ambika Prasanna 1 , Aparna Jakkampudi 2 , Sreelekha Chintaluri 2 , Misbah Unnisa 1 , Subhaleena Sarkar 2 , D Nageshwar Reddy 3 , Rupjyoti Talukdar 1
Correspondence – Rupjyoti Talukdar - rup_talukdar@yahoo.com
1Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs. Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India, 2Welcome DBT Indian Alliance Labs. Institute of Basic and Translational Research, Asian Healthcare Foundation, Mindspace Road, Gachibowli, Hyderabad 500 032, India, 3Medical Gastroenterology, Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Background Infected pancreatic necrosis (IPN) portends a dismal prognosis in patients with acute necrotizing pancreatitis (ANP). Despite use of higher generation pancreas penetrating antibiotics, a substantial proportion of patients continue to deteriorate clinically and require WON drainage procedures. We hypothesize that prolonged use of prophylactic antibiotics could result in mycobial (fungal) dysbiosis within the WON.
Methods In this ongoing study, we have recruited 74 subjects who underwent EUS guided drainage of WON. Apart from the recording clinical and biochemical parameters, we collected WON fluid during drainage, stool and blood samples. This was followed by metagenomic DNA extraction and ITS1 based next generation sequencing in the Illumina MiSeq platform. Following this, fungal annotation using UNITE database in QIIME was performed. We further evaluated the fecal and circulating (blood) mycobial profiles of healthy volunteers to compare with that of the WON fluid in patients with ANP.
Results All patients required EUS guided cystogastrostomy. The mean (SD) metagenomic DNA concentration in WON fluid was 295.9 (555.9) ng/mcl, and the A260:A280 was 1.88 (0.08). There was a high abundance of the Ascomycota and Basidiomycota phyla. In the WON fluid, 36 fungal species which includes Aspergillus penicillioides, Malassezia globose, Aspergillus niger, Aspergillus flavus were observed. Even in the stool and blood samples, Aspergillus penicilloides turned out to be the most abundant species.
Conclusion This study for the first time demonstrates NGS-based fungal dysbiosis in WON fluid in patients who require drainage. The data confirms fungal dysbiosis in the intestine, with translocation into the circulation and finally colonization of the WON. Early initiation of antifungals could ameliorate this poor prognostic determinant which need to be studied further.
Keywords Necrotizing pancreatitis, Mycobiome, NGS-ITS, Illumina Miseq, QIIME, UNITE database
005
Luminal and mucosal gut microbial and metabolomic profiles of patients with ulcerative colitis in response to fecal microbiota transplantation
Manasvini Markandey1, Aditya Bajaj1, Mukesh Singh1, Shubi Virmani1, Sudheer K.Vuyyuru1, Bhaskar Kante1, Peeyush Kumar1, Mahak Verma1, RamasamyThirunavukkarasu2, Pallavi Kshetrapal2 Govind Makharia1, Dinesh Gupta3, Saurabh Kedia1, Vineet Ahuja1
Correspondence – Vineet Ahuja –vineet.aiims@gmail.com
1Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110029, India,2Translational Health Science and Technology Institute, NCR Biotech Science Cluster, Faridabad 121 001, India. 3International Centre for Genetic Engineering and Biotechnology (ICGEB), Aruna Asaf Ali Marg, New Delhi 110 067, India
Background Gut microbiota modulation via fecal microbiota transplantation (FMT) induces long lasting clinical as well as endoscopic remission in patients with UC. The present study aims to identify microbial and metabolomic changes in the faecal as well mucosal niches, in response to FMT in patients with UC.
Methods Twenty-eight patients with mild-moderate UC and 16 non-IBD controls were enrolled. Patients received weekly infusion of pooled-multidonor-FMT, for 8 weeks, while maintaining a uniform diet. We collected paired stool and rectosigmoidal biopsy samples from patients with UC pre-FMT (n=28), post-FMT (n=10) and controls (n=16). 16S-rRNA sequencing and LC-MS based untargeted-metabolomics was performed. α and β diversity analysis and DeSeq2 based differential abundance analysis (DAA) of microbiota was performed. Differential metabolite peaks between the three groups were identified via volcano plot and annotated using LipidMaps, HMDB, Kegg and Metlin.
Results Fecal post-FMT α-diversity differed significantly from pre-FMT group, however in mucosal tissue, the difference was non-significant. β-diversity indices were significant in UC pre-FMT vs. post-FMT populations for both matrices. DAA identified fecal and mucosal controls and UC post-FMT samples to be significantly similar (ANOSIM R=0.07; p=0.1 [fecal] and R=0.02; p=0.315 [mucosal]). UC pre-FMT samples displayed increased abundance Firmicutes (Megasphaera, Limosilactobacillus, Lactobacillus, Veilonella and Sphingomonas, etc.) and Proteobacteria (Methylobacterium) in fecal samples, while mucosa-associated microbiota displayed increased abundances of Firmicutes (Streptococcus, Ligilactobacillus, Eubacterium, Enterococcus, etc.), Bacteroidetes (Parabacteroides and Alistipes) and Proteobacteria (Burkholderia sp.) (Fig.1).
Distinct classes of metabolites, including bacterial cell wall and QS molecules, membrane lipids, vitamin metabolism, long and medium chain fatty acids, bile acids, and tryptophan etc., were also found to be altered between the three groups in both sample matrices (Fig. 2).
Conclusion FMT efficiently restores beneficial bacterial populations and related metabolic pathways in faecal and relatively reserved mucosal niches, which may pave way for induction of remission in patients with UC.
Keywords Gut microbiome, Ulcerative colitis, Fecal microbiota transplantation
006
Genomic variations in ATP7B gene in Indian patients with Wilson disease
Aabha Nagral1,2, Snehal Mallakmir,3Nikita Garg,2 Kritika Tiwari,4Suzena Masih,5Nishtha
Nagral,6Ojas Unavane,7 Ajay Jhaveri,2 Shubha Phadke,5 Rakesh Aggarwal 8,9
Correspondence – AabhaNagral–aabhanagral@gmail.com
1Department of Gastroenterology, 3Department of Pediatrics,Apollo Hospitals, Navi Mumbai, India, and 2Department of Gastroenterology, Jaslok Hospital and Research Centre, 15, Pedder Road, IT Colony, Mumbai 400 026, India,4Department of Pediatrics, Matushree Gomati Hospital, Mumbai, India, 5Department of Medical Genetics,8Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India, 6Department of General Medicine, Fortis Hospital, Mulund, Mumbai, India, 7Seth G S Medical College and KEM hospital, Mumbai 400 012, India, 9Department of Gastroenterology, Jawaharlal Institute of Postgraduate Medical Education and Research, Gorimedu, Priyadarshini Nagar, Puducherry 605 006, India
Objectives Molecular diagnosis of Wilson disease (WD) is important not only for confirmation of diagnosis in individual cases suspected to have this condition, but also because it allows early diagnosis and institution of treatment in asymptomatic family members and prenatal diagnosis for prevention. However, data from the Indian population are limited and our study cohort is the first large cohort of patients of different ethnicities from India.
Methods We sequenced entire ATP7B gene in 58 patients with WD and also did additional testing by multiplex ligation-dependent probe amplification (MLPA) to look for intragenic deletions duplications and exome sequencing to rule out genetic variations with similar phenotypic overlap.
Results Of all patients, 37 patients had a total of 33 distinct pathogenic variations, including 29 in the exonic regions and 4 at intronic splice sites. Of the variations identified, six were novel. We could identify the underlying genomic variations in nearly two-thirds of our patients by sequencing the entire gene.
Conclusions We report here genotype phenotype data to add to the available spectrum of causative variants in ATP7B gene. The inability to detect a pathogenic variation in some patients and existence of phenotypic variations in persons with the same variation suggests that additional factors or genes may play a role in causation of the disease. Further, we found a marked genetic heterogeneity in our patients indicating ethnic diversity of the Indian population.
Keywords ATP7B, Genotype-phenotype, Metabolic liver disease, Wilson disease, WD
Young Investigator Award Session
007
Gut lymphangiogenesis modulates gut immunity and attenuates systemic inflammation in decompensated cirrhosis
Pinky Juneja 1 , Dinesh Tripathi 1 , Impreet Kaur 1 , Sumati Rohilla 1 , Subham Banerjee 2 , Shiv Sarin 3 , Savneet Kaur 1
Correspondence – Savneet Kaur – savykaur@gmail.com
Departments of 1MCM, and 3Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India, and 2Department of Pharmaceutics, NIPER-Guwahati, Changsari 781 101, Assam, India
Introduction Gut lymphatic vessels are crucial in maintaining gut immunity and abdominal fluid homeostasis. In liver cirrhosis, gut lymphatics vessels were dilated causing lymphangiectasia. We thus explored the therapeutic effects of gut-targeted delivery of a pro-lymphangiogenic factor, VEGF-C in decompensated cirrhosis.
Methods A nano-formulation of VEGF-C molecule (E-VEGF-C) for its targeted delivery in gut lymphatic endothelial cells (LyECs) was prepared. In vitro characterization, cytotoxicity, and in vivo biodistribution of E-VEGF-C were performed. In vivo, E-VEGF-C was given orally in CCL4-induced cirrhotic rat models of decompensated cirrhosis. Mesenteric lymphatic vessels and drainage were analyzed. Molecular and histological studies of the mesentery were performed. Gene expression analysis of sorted mesenteric LyECs was evaluated. LyECs were isolated and gene expression profiling was done. Systemic inflammation and immunity were studied.
Results In vitro and in vivo, E-VEGF-C was efficiently taken up by mesenteric LyECs. E-VEGF-C treated rats displayed an increase in numbers and drainage of mesenteric lymphatic vessels and a reduction in vessels diameter and ascites as compared to CCl4-vehicle. Gene expression analysis of LyECs showed increased expression for LyECs identity, permeability, antigen presentation, and chemokine in the E-VEGFC group. Immune-cells quantification showed an increased percentage of activated T cytotoxic cells in MLNs of E-VEGFC rats with a significant reduction in systemic inflammation.
Conclusion Targeted gut and mesenteric lymphangiogenesis leading to an improved functional lymphatic drainage and gut immunity may serve as an emerging therapy for patients with decompensated cirrhosis.
Keywords Cirrhosis, Gut lymphatic vessels, Lymphangiogenesis, Targeted drug delivery
008
Identification of molecular characteristics of infected necrosis in patients with acute pancreatitis: Implications for targeted prophylactic interventions
Aparna Jakkampudi1, Aashish Patel2, K Chandrakanth2, Misbah Unnisa1, Ambika Prasanna1, D Nageshwar Reddy2, Rupjyoti Talukdar3
Correspondence - Rupjyoti Talukdar – rup_talukdar@yahoo.com
1Department of Welcome DBT Indian Alliance Labs., Institute of Basic and Translayional Research, Asian Healthcare Foundation. Mindspace Road, Gachibowli, Hyderabad 500 032, India, 2Department of Medical Gastroenterology. Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India, 3Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs., Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Introduction Earlier we reported that persistent downregulation of HLA-DR increases risk of developing Infected pancreatic necrosis (IPN) in acute pancreatitis (AP). Kynurenine monooxygenase had a protective role In AP-MODS. This study evaluated the association of HLA-DR, KMO and plasma metabolites in IPN development.
Methods Patients with ANP were enrolled based on the presence or absence of IPN. Demographic and clinical parameters were recorded. Plasma procalcitonin, endotoxin, tryptophan, kynurenine and cytokines (IL-8, IL-6, IL-10, TNFα) were quantified by performing ELISA, FACS respectively. Plasma metabolites were quantified using GC-MS/MS. mRNA expression of HLA-DR, IL-10, TLR4, KMO genes were measured by qRT-PCR studies. Mann-Whitney U, Fischer’s exact test was performed for clinical parameters significance. Metaboanalyst was used for metabolite analysis and correlations were expressed by Spearman’s correlation.
Results In total, 99 (67.3%) patients were IPN, 48 (32.6%) were without IPN. The concentrations of plasma procalcitonin, endotoxin, IL-6, IL-10 were significantly high in IPN. HLA-DR expression was significantly down regulated while IL-10, KMO was significantly up regulated in IPN. HLA-DR expression was negatively correlated with plasma IL-6 levels, endotoxin. KMO expression was positively correlated with endotoxin and IL-6. Metabolome analysis resulted in distinct clustering of metabolites between controls and AP. 41 significantly altered metabolites were observed in AP. Hexadecane was significantly high with maximum VIP score. Metabolomic, ELISA results showed significant down regulation of plasma tryptophan.
Conclusion Association of HLA-DR, KMO with plasma metabolites revealed that patients with significant HLADR downregulation can develop IPN, electing appropriate antibiotics prophylaxis in these patients would potentially prevent development of IPN.
Keywords Acute pancreatitis, Infected pancreatic necrosis, HLA downregulation, Metabolomic alteration, Kynurenine
009
Stringent screening strategy significantly reduces reactivation rate of tuberculosis (TB) in patients with inflammatory bowel disease on anti-TNF therapy in a TB endemic region
Peeyush Kumar 1 , Sudheer Kumar Vuyyuru 1 , Bhaskar Kante 1 , Pabitra Sahu 1 , Sandeep Goyal 1 , Deepak Madhu 1 , Saransh Jain 1 , Mukesh Ranjan 1 , Sandeep Mundhra 1 , Rithvik Gola 1 , Mukesh Singh 1 , Shubi Vermani 1 , Anvita Gupta 1 , Nidhi Yadav 1 , Mani Kalaivani 2 , Raju Sharma 3 , Prasenjit Das 4 , Govind Makharia 1 , Saurabh Kedia 1 , Vineet Ahuja 1
Correspondence – Vineet Ahuja – vineet.aiims@gmail.com
1Department of Gastroenterology,2Department of Biostatistics, 3Department of Radiodiagnosis, 4Department of Pathology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Anti-tumor necrosis factor (anti-TNF) therapy use in patients with inflammatory bowel disease (IBD) leads to increased risk of tuberculosis (TB) reactivation despite LTB screening, especially in TB endemic regions. We evaluated the effect of stringent screening strategy and latent tuberculosis (LTB) prophylaxis on TB reactivation.
Methods We performed an ambispective comparison between patients who were started on anti-TNF therapy after January 2019 (Cohort A) and between January 2005-January 2019 (Cohort B). Cohort A patients were subjected to stringent screening criteria which included all: history of past TB/recent contact with active TB, CT chest, IGRA (interferon gamma release assay), TST (tuberculin skin test) and if any positive were given chemoprophylaxis. A cohort comparison was done to evaluate for risk reduction of TB following the stringent screening strategy.
Results One hundred seventy-one patients (63-ulcerative colitis/108-Crohn’s disease; mean age diagnosis-28.5±13.4 years; 60% males; median follow-up duration after anti-TNF:33 months (interquartile range, 23–57 months) were included. Among 112 in Cohort B 22 (19.6%) had LTB and 19 (17%) developed TB. In comparison, 26 (44%) had LTB and only 1 (1.7%) developed TB in Cohort A (p<0.01). On survival analysis, patients in Cohort B had a higher probability of TB reactivation compared to Cohort A at 5 years of follow-up, HR-14.39 (95% CI,1.88-109.81 (p=0.010) after adjusting for gender, age at anti-TNF therapy initiation, concomitant immunosuppression, total number of anti-TNF doses and therapy escalation.
Conclusion The high risk of TB reactivation with anti-TNF therapy in TB endemic regions can be significantly mitigated with stringent LTB screening and chemoprophylaxis.
Keywords TB reactivation, anti-TNF, LTB Screening
010
Duodenal dysbiosis and reduced duodenal oxygenation in patients with Type-2 diabetes mellitus: A prospective study
Aarti Darra 1 , Vandana Singh 1 , Mohd Ahmad 1 , Sanjay Bhadada 2 , Priyanka Popli 3 , Anuraag Jena 3 , Anupam Kumar Singh 3 , Vishal Sharma 3 , Anurag Agrawal 1 , Usha Dutta 3
Correspondence – Usha Dutta – ushadutta@gmail.com
1Molecular Immunogenetics, CSIR-IGIB, North Campus, Near Jubilee Hall, Delhi 110 007, India, Departments of 2Endocrinology, and 3Gastroenterology, Post Graduate Institute of Medical Education and Research, Sector-12, Chandigarh 160 012, India
Introduction Duodenum plays an important role in digestion, entero-insular signalling, and glucose homeostasis. However, the nature and quantity of duodenal flora, permeability, perfusion, and inflammation have not been assessed in patients with type-2 diabetes mellitus. The aim is to study the quantitative and qualitative aspect of duodenal and fecal bacterial flora in patients with hyperglycemia in comparison to normoglycemic subjects along with measurement of duodenal perfusion, permeability and inflammation.
Method A study cohort of 33 hyperglycemic (HbA1c >5.6 % and fasting plasma glucose >110 mg/dL) and 21 normoglycemic subjects was recruited as per protocol approved by institutional ethics committee after informed consent. The paired sampling of endoscopic duodenal biopsy and stool were obtained and analyzed. Microbial analysis was performed using 16S rRNA sequencing with both qualitative and quantitative PCR. Duodenal tissue oxygen saturation was measured using an FDA approved tissue oximeter (T-Stat, Spectros). Serum zonulin was measured using ELISA. The Luminex assay was performed to assess IFN-γ, IL-1β, TNF-α, IL-8, IL-4, IL-5 and IL-10 as markers for inflammation.
Results Bacterial counts normalized to biopsy DNA content were almost three-fold higher in the hyperglycemic group (1100) compared to the normoglycemic group (p=0.04). Increasing duodenal bacterial load was associated with increased zonulin levels. The qualitative microbial analysis using 16S rRNA sequencing showed enrichment of pathogenic flora such as Proteobacteria with reduction of probiotic bacteria like Akkermansia muciniphilia. Hyperglycemic subjects showed reduced mucosal tissue oxygen saturation, increased total leukocyte count and reduced IL-10 levels. Duodenal microbiome showed greater inter-individual variability than the faecal microbiome and was better associated with glycemic status.
Conclusion Hyperglycemia was associated with duodenal dysbiosis with increased bacterial load, increased Proteobacteria, decreased Akkermansia, less perfused gut and reduced anti-inflammatory response. Higher bacterial load was associated with elevated zonulin levels. Obese hyperglycemia was associated with poor duodenal perfusion.
Keywords Duodenum, Type-2 diabetes, Dysbiosis
011
Fluorine18-Fluorodeoxyglucose labeled autologous leukocytes positron emission tomography-computed tomography enterography: A novel non-invasive method for evaluating the extent and activity of Crohn’s disease
Pankaj Kumar1, Anish Bhattacharya2, Jayanta Samanta1, Kaushal K Prasad1, Saroj K Sinha 1 Sarika Sharma2, Rakesh Kochhar1,
Correspondence - Pankaj Kumar - pankdoct2@gmail.com
1Department of Gastroenterology, 2Department of Nuclear Medicine, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Introduction Extent and activity of Crohn’s disease (CD) is best evaluated by ileocolonoscopy. Fluorine 18-Fluorodeoxyglucose labeled autologous leucocytes (18F-FDG-LAL) positron emission tomography-computed tomography enterography (PET-CTE) is a newer and non-invasive imaging modality for the evaluation of inflammation but has not been studied in CD. The aim of this study was to assess the disease extent and activity of CD with 18F-FDG-LAL PET-CTE and to correlate it with clinical criteria, endoscopic findings, and serum and fecal biomarkers.
Methods Consecutive patients of CD between January 2019 to June 2020 were enrolled. Each patient underwent 18F-FDG-LAL PET-CTE followed by ileocolonoscopy within 72 hours and total number of segments involved on both modalities were calculated. Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and fecal calprotectin levels were determined for all patients.
Results A total of 42 patients of CD were evaluated with18F-FDG-LAL PET-CTE of which 32 had lesions within ileocolonoscopy reach. PET activity showed significant correlation with Crohn’s disease activity index (r=0.594, p=0.031), fecal calprotectin (r=0.483, p=0.001) and simple endoscopic score for Crohn’s disease (r=0.366, p=0.018). Number of segments involved on ileocolonoscopy and 18F-FDG-LAL PET-CTE were 94 and 88 respectively with a significant correlation between the two modalities for extent evaluation (r=0.738, p<0.001).
Conclusions 18F-FDG-LAL PET-CTE is a novel, reliable, non-invasive modality for the evaluation of disease extent and activity in CD and shows good correlation with clinical activity, endoscopic score and fecal biomarkers.
Keywords Crohn’s disease; 18F-FDG; Labeled autologous leukocytes, Positron emission tomography
012
Role of artificial intelligence guided esophagogastroduodenoscopy in assessing the procedural completeness and quality
Mahesh Goenka, Shivaraj Afzalpurkar, Gajanan Rodge, Awanish Tewari, Saurabh Jejurikar1
Correspondence – Shivaraj Afzalpurkar – drshivaraj62@gmail.com
Department of Gastroenterology, Day Care Building, Fourth Floor, Institute of Gastrosciences and Liver, Apollo Gleneagles Hospital, EM Bypass Road, 58 Canal Circular Road, Kolkata 700 054, India, and 1Endovision, Founder, Room 1006, 10/F, Haleson Building, 1 Jubilee Street, Central, Hong Kong 999 077.
Introduction The quality of esophagogastroduodenoscopy (EGD) has great impact on the detection of oesophageal and gastric malignancies. An AI system, Cerebro, has been developed as a real-time recognition of a pre-defined 29 locations. This system would alert the endoscopist if the sites were not inspected with adequate time. The aim of the study is to investigate the use of AI in endoscopists-in-training during OGD to provide real-time feedback for ensuring completeness of examination.
Methods This is an observational pilot study. The videos of the EGD procedure performed in last 3 months (July 1, 2021 to September 30, 2021) were prospectively analyzed using AI system. The assessment of completeness of the procedure was done based on the visualization of pre-defined 29 locations. Endoscopists were divided into 2 categories whether they are in the training period (category A) or competed their endoscopy training (category B).
Results A total of 277 procedures were included in the analysis of the study. Category A and B included 114 and 163 endoscopists respectively. The areas which are most commonly covered by all the endoscopists are greater curvature of antrum (97.47%), second part of duodenum (96.75%), other parts of antrum like anterior, lesser curvature and the posterior aspect (96.75%, 94.95% and 94.22% respectively). The areas which were most commonly missed or inadequately seen are vocal cords (99.28%), epiglottis (93.14%), posterior, anterior and lateral incisura (78.70%, 73.65 and 73.53 respectively). The good quality procedures were done predominantly by category B (88.68%) in comparison to only 11.32% by category A endoscopists.
Conclusion AI plays an important role in assessing the quality and completeness of EGD. Large prospective multicentre study is the need of the hour to validate on a large scale. This is the first study form our country to assess the role of AI in EGD.
Keywords Artificial intelligence, Esophagogastroduodenoscopy, Procedural quality
Presidential Posters
013
Low levels of sphingosine-1-phosphate predict severe intrapulmonary shunting and fingolimod represents a novel therapy for hepatopulmonary syndrome
Sukriti Baweja 1 , Anupama Parasa 1 r, Preeti Negi 1 , Arvind Tomar 3 , Aayushi Rastogi 4 , Jitendra Kumar 1 , Arun Sood 5 , Chitranshu Vashistha 2 , Chhagan Bihari 6 , Rakhi Maiwall 2 , Shiv Sarin 1,2
Correspondence – Shiv Sarin – shivsarin@gmail.com
1Department of Molecular and Cellular Medicine, 2Department of Hepatology, 3Department of Pulmonary Medicine, 4Department of Epidemiology, 5Department of Cardiology, 6Department of Pathology, Institute of Liver and Biliary Sciences, D 1, Vasant Kunj, New Delhi 110 070, India
Background The hepatopulmonary syndrome (HPS) results from a defect in arterial oxygenation induced by pulmonary vascular dilatation in liver disease patients. Fingolimod, sphingosine-1-phosphate (S1P) receptor modulator, suppresses vasodilation by reducing nitric oxide (NO) production. We investigated the role of S1P in HPS patients and Fingolimod, in an experimental model of HPS.
Methods Cirrhosis patients with HPS (n=42), without HPS (n=35), and 10 healthy controls were included. Plasma levels of S1P, nitric oxide (NO), systemic inflammation, microvesicles (MV) levels and immune profile was performed. Variations in pulmonary vasculature, arterial oxygenation, liver fibrosis and inflammation in murine model of common bile duct ligation (CBDL) before and after administration of S1P and Fingolimod was investigated.
Results The plasma S1P levels were significantly lower in cirrhosis with HPS than without (p=0.012). The levels progressively decreased from mild to severe intrapulmonary shunting (p=0.002) and S1P <16.1 ng/mL predicted severe HPS (AUROC of 0.72; p=0.03), with low intra-MV S1P levels in HPS patients than without HPS (p<0.001). Plasma TNF-α (p=0.003) and NO (p=0.003) levels were higher in HPS patients than without HPS. Th17 (p<0.001) and T-regulatory cells (p=0.007) were significantly increased; the later inversely correlating with S1P levels. In the CBDL-HPS mouse model, 2 weeks of Fingolimod, restored the vascular integrity by increasing the arterial blood gas exchange (p=0.042), a reduced systemic and pulmonary inflammation in CBDL animals compared to controls, with improved survival (p=0.04). A significant reduction in hemosiderin laden macrophages and F4/80+ cells were seen with Fingolimod (p=0.002) and S1P treated CBDL (p=0.032) animals in bronchoalveolar lavage.
Conclusion Low S1P levels in HPS patients predict increased intrapulmonary shunting. Fingolimod improves the vascular tone, oxygenation and survival in experimental HPS model.
Keywords Heptopulmonary syndrome, Cirrhosis, Sphingosine-1-phosphate, Vasodilation
014
Distinct pattern of gut microbial dysbiosis in Crohn’s disease and intestinal tuberculosis – A machine learning-based classification model
Aditya Bajaj1†, Manasvini Markandey1†, Sudheer K. Vuyyuru1, Srikant Mohta1, Sambudhha Kumar,1Mahak Verma1, Mukesh Singh1, Bhaskar Kante1, Peeyush Kumar1, Govind Makharia1, Saurabh Kedia1, Vineet Ahuja1
Correspondence – Vineet Ahuja - vineet.aiims@gmail.com
1Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi, Delhi 110 029, India
† Equal contribution
Background Crohn’s disease (CD) and intestinal tuberculosis (ITB) are chronic granulomatous inflammatory disorders characterized by a compromised mucosal immunity. Even with diverging etiologies, CD and ITB presents an uncanny resemblance in clinical manifestation resulting in diagnostic dilemma. The gut microbiota regulates myriad of gut mucosal immunological processes. Present study aims to decipher gut microbial dysbiosis in the two disorders and utilize the CD and ITB-specific gut dysbiosis to construct a machine learning (ML)-based predictive model, which can aid in their differential diagnosis.
Methods Fecal samples from healthy controls (n=12) and from patients with CD (n=23) and ITB (n=25) were subjected to 16S-amplicon sequencing. Processing of raw reads, construction of ASV feature tables, diversity, core microbiome analysis and ML classifier construction was done using QIIME2-2021.4. Differential abundance analysis (DAA) between the groups was carried out using Deseq2.
Results The α and β-diversity indices in CD and ITB groups were significantly reduced than HC group (p=0.011 and 0.012 resp.), with no significant differences between the two diseases (Fig.1A, 1B). On comparison with HC, CD and ITB groups showed reduction in members of Firmicutes and Bacteroidetes, with enhancement of Actinobacteria and Proteobacteria (Fig.1C and 1D). DAA (FDR q<0.1, FC>2.5) between CD and ITB groups revealed expansion of Succinivibrio dextrinisolvens, Odoribacter splanchnicus, Megasphaera massiliensis, Bacteroides uniformis and B.xylanisolvens in CD group, while Clostridium sp., Hemophilus parainfluenzae and Bifidobacterium sp. were elevated in ITB (Fig.2A). Random-Forest-based ML model using 80% of the samples to train the model, showed predictive accuracy of 0.78 (AUC=93%). (Fig.2B)
Conclusions Our study shows that CD and ITB witnesses significant changes in gut microbial structure. With no significant differences in microbial diversity between two diseases, the signature of gut dysbiosis is distinct between CD and ITB. Exploitation of these differences to construct ML models can potentiate differential diagnosis of CD and ITB.
Keywords Gut microbiome, Random Forest Machine learning model, Crohn's disease, ITB
015
Plasma exchange to rescue children with rodenticidal hepatotoxicity who met listing criteria for urgent liver transplantation
T V Leenath 1 A Goel 1 , J Chandran 2 , E Jacob 2 , B Chacko 2 , K Subramani 2 , I Agarwal 3 , S Varughese 4 , VG David 4 , D Daniel 5 , J Mammen 5 , B Vijayalekshmi 6 , AP Lionel 7 , U Zachariah 1 , ChundamannilE Eapen 1
Correspondence –Chundamannil E Eapen–eapen@cmcvellore.ac.in
Department of Hepatology1, Critical Care2, Pediatric Nephrology3, Nephrology4, Transfusion Medicine5, Wellcome Trust Research Lab6 and Child Health7, Christian Medical College, Vellore 632 004, India
Background We describe our experience with low-volume plasma exchange (PLEX-LV) to treat rodenticidal hepatotoxicity in children.
Methods From prospectively collected database of 110 rodenticidal hepatotoxicity patients admitted in our department from December 2017 to August 2021, we retrospectively analyzed outcomes in children (≤18 years). Patients were characterized as acute liver injury (ALI, coagulopathy alone) or acute liver failure (ALF, encephalopathy). King’s college criteria and Kochi criteria (model for end-stage liver disease [MELD] score ≥36 or baseline international normalized ratio [INR] ≥ 6 with hepatic encephalopathy) (Saraf et al. PMID: 26310868) were used to assess need for urgent liver transplantation. In-hospital outcome was recorded.
Results Thirty-two children (females: 56%; age: 15.5±2.9 years) with rodenticidal hepatotoxicity presented 4 (2,5) days after consumption (suicidal intent:31, accidental:1) Twenty patients (62%) had ALI (MELD: 20.1±8.0) and 12 (36%) had ALF (MELD: 35.8±5.7). Nine patients with ALF fulfilled King’s college and Kochi criteria for urgent liver transplantation. All patient families opted against liver transplantation. All children received standard management, including N-acetyl cysteine; ALF patients also received anti-cerebral edema measures. In addition, 17 patients (ALI: 6, ALF: 11) were treated with PLEX-LV (3.5±1.1 sessions, volume: 28±7 ml/Kg body weight) and peri-procedure low dose prednisolone. Hospital stay was 10.5±5 days for those who underwent PLEX and 7.7±2.9 days for other patients. Twenty-eight patients (87.5%) were discharged in stable state, while 4 died in-hospital. Of 9 patients who met King’s college criteria for liver transplantation (15.4±2.9 years old, females: 67%, MELD: 39.1±4.5), 5 (63%) survived with PLEX-LV (n=8). Of 10 patients who met Kochi criteria, 6 (67 %) survived with PLEX-LV (n=9). Among the 78 patients >18 years old, 19 patients met the King’s college criteria and 30 met Kochi criteria. The survival in those who underwent LV-PLEX was 50% and 55.6% respectively.
Conclusion PLEX-LV shows promise as an effective non-liver transplant treatment in children with rodenticidal hepatotoxicity.
Keywords Acute liver failure, Kochi criteria, Phosphorus, Rat killer
016
Tracing the roots to celiac disease in IgA nephropathy by IgA/anti-tissue transglutaminase 2 antibody deposits in archived tissues
Rimlee Dutta 1 , Ramakant Rawat 2 , Prasenjit Das 1 , Geetika Singh 1 , Alka Singh 2 , Ashish Chauhan 2 , Vineet Ahuja 2 , Sanjay Agarwal 3 , Govind Makharia 2
Correspondence - Rimlee Dutta - rimdutt369@gmail.com
Departments of 1Pathology, 2Gastroenterology and Human Nutrition, and 3Nephrology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction While an association is described between IgA nephropathy (IgAN) and celiac disease (CeD), it is still not known whether this association is casual or causal. Definite pathogenetic evidence linking IgAN and CeD remains to be established.
Methods Biopsy proven patients of IgAN were screened for serum IgA anti-tissue transglutaminase antibody (IgA anti-tTG Ab) titer. Patients with high anti-tTG Ab titer, were invited to undergo endoscopic duodenal biopsy and modified Marsh grading was done on their biopsies. The corresponding duodenal and kidney biopsies were then subjected to CeD-specific IgA/anti-tTG2 antibody colocalization using the dual immunohistochemistry and immunofluorescence techniques. Additionally, kidney biopsies from 105 patients with IgAN, 30 non-IgA nephropathies, and 10 normal kidney tissues were also subjected to IgA/anti-tTG2 antibody colocalization. Dual-IHC stained slides were interpreted based on stain distribution and intensity scores and for dual-IF stained slides, Pearson’s index >0.3 to 1 on confocal imaging was considered significant.
Results Of a cohort of 151 patients with IgAN, 32 consented to undergo CeD sero-screening and 5 of them had high serum anti-tTG Ab titer. Two out of the latter consented for endoscopic duodenal biopsies, which on histological examination showed modified Marsh grade 3b changes. Strong IgA/anti-tTG2 antibody deposits were noted in the kidney and duodenal biopsies. One patient out of non-consenting 105 patients with IgAN and 3 out of 30 patients with other non-IgA nephropathies also showed IgA/anti-tTG2 deposits with dual-IF staining, but not with dual-IHC staining. None of the normal kidney tissues showed IgA/anti-tTG Ab deposits.
Conclusions A small proportion of patients with IgAN have associated CeD. The presence of co-localized IgA/anti-tTG2 deposits in the kidney biopsies of patients with IgAN having co-existent CeD envisages pathogenic link between these two diseases and may serve as evidence for the same. This further aids optimum management of these patients.
Keywords Celiac disease, IgA nephropathy, IgA/anti TG2
017
Development of a software to assess the disease activity in ulcerative colitis
Amey Desai1, Devendra Desai2
Correspondence – Devendra Desai - devendracdesai@gmail.com
1Lifespark Technologies, Kanwal Rekhi Building, IIT Mumbai, Mumbai 400 076, India, and 2Department of Medicine-Gastroenterology, P D Hinduja Hospital, Veer Savarkar Marg, Mahim, Mumbai 400 016, India
Introduction AI offers several benefits to the field of medicine such as more accurate diagnosis, speed, scalability and better insights into available data. However, the use of AI in medicine is limited by the fact that these advanced algorithms produce decisions in a manner that is not interpretable by humans. In a critical field such as medicine, any diagnostic or therapeutic method should be verifiable and interpretable to human experts. We present Assess UC, a method to assess the Ulcerative Colitis Endoscopic Index of Severity or UCEIS score using AI.
Methods We used the open-source KVASIR dataset to obtain 863 usable images. These images were manually scored according to the UCEIS scale and areas of the images relevant to decision making, such as those with bleeding, erosions or ulcers were highlighted. We trained an ensemble model composed of convolutional neural networks and U-Net models to output UCEIS scores and areas of interest that were used to make the scoring decision. The model was tested on a separate set of data.
Results
| Vascular pattern | Bleeding | Erosions and ulceration | |
| Accuracy | 76% | 75% | 87.5% |
| Mean Intersection over Union | NA | 0.62 | 0.58 |
Our model achieved accuracies of 76% for vascular pattern scores, 75% for bleeding scores and 87.5% for erosions and ulcers scores.
Conclusion The presented method is comparable to the current state-of-the-art. We make an important addition that provides transparency into the decision-making process of the algorithm. Our method outputs it’s evaluation as well as the rationale in a simple visual manner. Through this paper, we aim to provide a method to automatically, and accurately score ulcerative colitis disease activity in a way that is verifiable by the physician. We also hope to lay the foundational framework for the development of future systems that provide interpretability and verifiability.
Keywords Machine learning, Ulcerative colitis, Convoluted neural network, Artificial intelligence, Inflammatory
018
Norfloxacin prophylaxis for prevention of bacterial infections in acute-on-chronic liver failure patients- A placebo-controlled double-blind randomized trial
Anand Kulkarni1, Sowmya Tirumalle1, Syeda Fatima1, Bindu Rapole1, Venu Simgadri2, Sasikala Mitnala2, Deepika Gujapalli3, Mithun Sharma1, Rajesh Gupta1, P N Rao1, D Nageshwar Reddy1
Correspondence – Anand Kulkarni –anandvk90@gmail.com
1Department of Hepatology,2Department of Research Asian Healthcare Foundation,3Department of Biochemistry, Asian Institute of Gastroenterology, Cluster M, AIG Hospitals, Hyderabad 500 032, India
Background Bacterial infections (Bis) are frequent in patients with acute-on-chronic liver failure (ACLF) and strongly impact the survival. Norfloxacin prophylaxis is approved for the prevention of spontaneous bacterial peritonitis (SBP). Here we aimed to assess the efficacy of primary NFX prophylaxis for the prevention of Bis in patients with ACLF.
Methods In this double-blind, randomized study, ACLF patients without sepsis, hepatic encephalopathy, or SBP were randomly assigned to either receive oral NFX 400 mg (NFX) or matched placebo (PBO) once daily for 30 days. The primary objective was to assess the incidence of Bis at days 30, 90, and the secondary was to evaluate the transplant-free survival (TFS) at days 30, 90.
Results Seventy-two were randomized to NFX and 71 to PBO. Alcohol was the most common precipitant of ACLF (73.42%). Baseline characteristics, including severity scores, were similar in both groups. Twenty-six percent (37/143) at day 30 developed Bis. The incidence of Bis was lower with NFX than PBO (NFX- 18.1% vs. PBO-33.8%; p=0.03). The incidence of BI at day 90 was 54% (77/143). The incidence of Bis at day-90 was lower with NFX than placebo (NFX-46% vs. PBO- 62%; p=0.052). (Fig.: Kaplan-Meier Analysis of Bis). The most common source of infection was the urinary tract (29%) and peritoneal cavity (14.51%). Sixty-three percent of infections in NFX and 55.3% in PBO group resolved (p=0.57). TFS at day 30 was higher with NFX than PBO (NFX-77.8% vs. PBO- 64.8%; p=0.086). TFS at day 90 was higher with NFX (58.3%) than PBO (43.7%; p=0.079). Sepsis was the commonest cause of mortality. Only 32% (23/72) in NFX group developed hepatic encephalopathy (HE), while 52.1% (37/71) in the PBO group developed HE (p=0.01).
Conclusions Primary NFX prophylaxis is safe and effective in preventing Bis in patients with ACLF.
Keywords Infections, ACLF, Antibiotics, Encephalopathy
019
Intrahepatic transplantation of biliary organoids induces differentiation into functional hepatocytes in chronic liver injury
Savneet Kaur , Impreet Kaur, Ashwini Vasudevan, Sumati Rohilla, Natalia Sanchezromero 1 , Pedro M Baptista 1 , Dinesh M Tripathi, Shiv K Sarin 2
Correspondence – Savneet Kaur – savykaur@gmail.com
Departments of Molecular and Cellular Medicine, and 2Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India, 1Department of abo Laboratory of Organ Bioengineering and Regenerative Medicine, Instituto de Investigación, Sanitária de Aragón Instituto de Investigación, Sanitária de Aragón, Zaragoza 50009, Spain
Introduction Limited replicative potential of hepatocytes (Hep) is a major limitation of cell therapy in patients with liver failure. Biliary organoids (BO) derived from intrahepatic bile ducts differentiate into both hepatocyte and cholangiocytes in vitro. We studied the effects of intrahepatic transplantation of BO and Hep in CCl4-induced liver injury mice models by histology and RNA sequencing of the transplanted liver lobes.
Methods Mice Hep were isolated by collagenase perfusion. Intrahepatic mice bile ducts were used to isolate and culture BO on 19atient19. Rat livers were decellularized and solubilized to make DCL. Mice models of 3-week liver injury were prepared by CCl4. Well-characterized BO and Hep mixed with DCL were transplanted into subcapsular left lateral mice liver lobes. CCl4 mice given DCL alone were sham group. 2-week post-transplantation, transplanted liver lobes were collected from all the study groups and studied by histology and RNA-seq on Illumina Hiseq 2500 with 2X150 paired-end chemistry.
Results Cultured Hep were positive for Alb while BO showed positivity for Krt19 in vitro. Post 3-week CCl4 injections, mice developed a grade 2 fibrosis. After 2-weeks of cell transplantation in CCl4 mice, BO livers had increased PCNA-positive cells as compared to both sham and Hep groups (p< 0.0001). Among the top 20 differentially expressed genes in RNA seq, an upregulation of genes involved in cell cycle progression was observed in BO livers as compared to sham. Hepatocyte differentiation genes, Hnf4a, Bmp4, Foxa3 etc were upregulated in both Hep and BO livers than sham. Serum albumin was significantly increased in both Hep and BO mice and these groups also showed a significant resolution of fibrosis as compared to sham.
Conclusion During chronic liver injury, transplanted BO are differentiated into functional hepatocytes in vivo, indicating that they may serve as an efficient cell therapy for restoring hepatic insufficiency.
Keywords Biliary organoids, Cell therapy, Hepatocytes, Chronic liver injury
020
GMCSF modulates myeloid derived suppressor cells and Tregs activity in decompensated cirrhotic patients with sepsis
Rashi Sehgal 1 , Rakhi Maiwall 2 , Vijayraghavan Rajan 2 , Mojahidul Islam 1 , Sukriti Baweja 1 , Navkiran Kaur 3 , Guresh Kumar 4 , Gayatri Ramakrishna 1 , Shiv Kumar Sarin 1 , Nirupma Trehanpati 1
Correspondence – Nirupma Trehanpati – trehanpati@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Hepatology, 4Clinical Research and Biostatistics, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India, 3Amity Institute of Biotechnology, Amity University, Amity Road, Sector 125, Noida 201 301, India
Background Decompensated cirrhosis patients are more prone to bacterial infections. Myeloid derived suppressor cells (MDSCs) expand in sepsis patients and disrupt immune cell functions. GM-CSF therapy helps in restoring immune cell functions and resolve infections. Its role in MDSCs modulation in cirrhotic with sepsis is not well understood.
Methods One hundred and sixty-four decompensated cirrhotic; 62 without (w/o), 72 with sepsis and 30 with sepsis treated with GM-CSF, and 15 healthy were studied. High-dimensional flow cytometry was performed to analyze MDSCs, monocytes, neutrophils, CD4 T-cells, and Tregs at admission, day3 and 7. Ex-vivo co-cultured MDSCs with T-cells were assessed for proliferation and apoptosis of T-cells, differentiation to T-regs. Plasma factors and mRNA levels were analyzed by cytokine-bead assay and qRT-PCR.
Results Frequency of MDSCs and T-regs were significantly increased (p=0.011, and p=0.02) with decreased CD4 T-cells (p=0.01) in sepsis than without sepsis and HC (p=0.000, p=0.07 and p=0.01) at day 0, and day 7. In sepsis patients, MDSCs had increased IL-10, Arg1 and iNOS mRNA levels (p=0.016, p=0.049 and p=0.06). Ex-vivo co-cultured MDSCs with T-cells drove T-cell apoptosis (p=0.03, p=0.03) with decreased T-cell proliferation and enhanced FOXP3+ expression (p=0.05 and p=0.05) in sepsis compared to no sepsis at day 0. Moreover, blocking the MDSCs with inhibitors suppressed FOXP3 expression. GM-CSF treatment in sepsis patients significantly decreased MDSCs and FOXP3+Tregs but increased CD4 T-cell functionality and improved survival.
Conclusion MDSCs have immunosuppressive function by expanding FOXP3+ Tregs and inhibiting CD4+ T-cell proliferation in sepsis. GM-CSF treatment suppressed MDSCs, improved T-cell functionality, and reduced Tregs in circulation.
Keywords Myeloid derived suppressor cells, Sepsis, GM-CSF, Tregs
021
A novel diagnostic model for advanced fibrosis in an Indian cohort with non-alcoholic fatty liver disease
H Vijay Narayanan , Jijo Varghese, Krishnadas Devadas
Correspondence – Vijay Narayanan H – vijaynh@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background and Aims The spectrum of non-alcoholic fatty liver disease (NAFLD) encompasses simple steatosis, steatohepatitis, advanced fibrosis, and cirrhosis. Progression to advanced fibrosis, the forerunner of cirrhosis, portends a poor outcome. Most of the existing scoring systems for advanced fibrosis are based on Western data. We sought to propose a new diagnostic model for advanced fibrosis in an Asian (Indian) cohort with NAFLD.
Methods This was a cross-sectional study conducted in the Department of Gastroenterology, Government Medical College, Trivandrum over 2 years. After excluding secondary causes of steatosis, patients were subjected to vibration-controlled transient elastography (VCTE) as a measure of hepatic fibrosis. Subjects were grouped into those with advanced fibrosis (TE>10 Kpa) and those without advanced fibrosis (TE<10 Kpa). Based on independent predictors for advanced fibrosis, a new scoring system was derived. Since liver biopsy is the gold standard for advanced fibrosis, we validated the new score in another cohort of biopsyproven NAFLD patients
Results 1617 NAFLD patients were included in the study. 225 had advanced fibrosis and 1392 had non-advanced fibrosis. Independent predictors of advanced fibrosis were Hip circumference, triglycerides, aspartate aminotransferase (AST), and diabetes mellitus (duration > 10 years).
T-HAD score = (Hip circumference x 0.044 + AST x 0.028+ diabetes mellitus x3.7) – (0.03 x triglycerides).
At a cut-off of >2, the T-HAD score had a sensitivity of 90% and specificity of 77% for advanced fibrosis. We validated this score in another cohort of liver biopsy-proven 84 NAFLD patients in whom there were no competing etiologies. In the validation cohort, T-HAD score had an AUROC of 0.926 in diagnosing advanced fibrosis (Sensitivity of 89% and specificity of 71%).
Conclusion T-HAD score is a new diagnostic model based on simple clinical and biochemical variables, which could be used to detect advanced fibrosis in the Asian (Indian) NAFLD patient population.
Keywords T-HAD score, Advanced fibrosis, Non-alcoholic fatty liver disease
022
MicroRNAs in serum can differentiate periampullary carcinoma patients from healthy individuals
Imteyaz Ahmad Khan1 Nidhi Singh1, Deepak Gunjan1, Nihar Ranjan Dash2, Sujoy Pal2, Neelam Lohani1, Surabhi Gupta3, Anoop Saraya1
Correspondence – Anoop Saraya–ansaraya@yahoo.com
1Department of Gastroenterology and Human Nutrition Unit, 2Department of Gastroenterology Surgery, 3Department of Reproductive Biology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background In recent years, accumulating evidence has revealed that circulating microRNAs (miRNAs) can serve as non-invasive biomarkers for cancer diagnosis. The aim of this study was to identify differentially expressed miRNAs in the serum of periampullary carcinoma (PAC) patients and investigate the potential of serum miRNA as a biomarker for non-invasive diagnosis of periampullary carcinoma.
Methods The serum levels of 11 miRNAs (miR-215-5p, miR-122-5p, miR-192-5p, miR-181a-2-3p, miR-30b-5p, miR-216b-5p, miR-320b, miR-214-5p, miR-203a-5p, miR-194-3p and miR-378a-5p) were measured by qRT-PCR. This study recruited 68 PAC patients and 50 healthy controls (HC). The diagnostic values of miRNAs were evaluated by receiver operating characteristic (ROC) analysis.
Results Three miRNAs (miR-215-5p, miR-192-5p, and miR-378a-5p) in serum were significantly up-regulated in PAC patients compared with HC. ROC analysis showed that these three miRNAs can distinguish PAC from HC.
Conclusion We identify a three-miRNA panel in serum which might serve as a promising non-invasive biomarker for PAC diagnosis.
Keywords miRNA, Biomarkers, Periampullary carcinoma
023
Multivariable liver fibrosis staging prediction using machine learning in non-alcoholic fatty liver disease
Mahesh Goenka1, Gajanan Rodge1, Enam Khan2, Raj Shukla3, Bharath Potla4, Usha Goenka5, Sujoy Kar4
Correspondence – Mahesh Goenka – mkgkolkata@gmail.com
1Institute of Gastrosciences and Liver, 2Department of Lab Services and Pathology, 5Department of Interventional Radiology and Clinical Imaging, Apollo Multi-Speciality Hospitals, 58, Canal Circular Road, Kolkata 700 054, India, 3Apollo 24/7 Apollo Hospitals, Jubilee Hills, Hyderabad 500 033, India, 4Corporate IT, Apollo Hospitals, Jubilee Hills, Hyderabad 500 033, India
Introduction Non-alcoholic fatty liver disease (NAFLD) has emerged to be a global epidemic and ranges from isolated steatosis to steatosis plus inflammation with or without fibrosis. The objective of this study is developed and validate a Machine Learning Model to identify and distinguish advanced fibrosis using elastography and liver biopsy.
Methods Data of 5150 NAFLD patients (Advanced Fibrosis F2-4 – 30.34%) was collected from Apollo Hospitals, Kolkata period 2011 to 2017 using standardized template and electronic medical records (ICD 10 codes). Twenty-five clinical and laboratory parameters were studied along with patients’ Elastography reports and ARFI values. The Machine Learning (ML) modelling was performed using eXtreme Gradient Boosting (XGB) algorithm. The prospective validation cohort was selected of 1261 patients (F2-4 – 31.24%) from 2018 to 2020 and compared with Fib4 Score. This was further validated with 98 Liver Biopsies from validation cohort.
Results Out of the 25 clinical and laboratory parameters, 11 variables including Age (Multivariate Odds Ratio [OR]– 3.39; 95% CI 2.99 – 3.84), history of diabetes mellitus (OR – 6.80, 95% CI 5.92 – 7.81), albumin (OR– 3.70, 95% CI 3.25 – 4.20), aspartate aminotransferase (AST) (OR- 3.65, 95% CI – 3.21 – 4.16), total bilirubin (OR–3.13, 95% CI 2.76 – 3.56) and platelet count (OR–2.74, 95%CI 2.40 – 3.13) were found to be significant. The performance parameters of the development model is AUC ROC score of 0.94 and validation cohort had the AUC and accuracy of 0.88. The AUC for 98 liver biopsy validation cohort was 0.83. The model performed better than Fib4 Score with Net Reclassification Improvement (NRI) at 0.499.
Conclusion The model comparing advanced liver fibrosis (F2-4) from no or low fibrosis (F0/F1) provides insights into the clinical and laboratory parameters and accurately predicts onset of liver fibrosis in NAFLD which could be useful as clinical decision support in low-cost settings.
Keywords NAFLD, Artificial intelligence, Advanced liver fibrosis, Machine learning
024
Correlation between magnetic resonance enterography and ileo-colonoscopy for assessment of disease activity in terminal ileal Crohn’s disease
Arshdeep Singh 1 , Chandan Kakkar 2 , Ramit Mahajan 1 , Vandana Medha 3 , Shriya Goyal 1 , Namita Bansal 4
Correspondence – Ajit Sood – ajitsood10@gmail.com
1Departments of Gastroenterology, 2Radiology, 3Medicine, and 4Research and Development, Dayanand Medical College and Hospital Tagore Nagar Civil Lines, Ludhiana 141 001, India
Background Magnetic resonance enterography (MRE) has emerged as a novel tool for assessment of disease activity in Crohn’s disease (CD). Real world data on performance of MRE in terminal ileal CD are lacking.
Methods Retrospective analysis of patients with terminal ileal CD who underwent both ileo-colonoscopy and MRE was performed. Ileo-colonoscopy was considered as gold standard for assessment of disease activity. On ileo-colonoscopy, a simple endoscopic score for Crohn’s disease (SES-CD) ≥2 was considered as active disease; presence of ulcers indicated severe disease. MRE scoring of the disease activity was performed using magnetic resonance index of activity (MARIA) and simplified MARIA (MARIAs). The measure of agreement between ileo-colonoscopy and MRE, comparison of MARIA and MARIAs for assessment of disease activity and sensitivity of MRE to detect mucosal ulcerations were calculated.
Results Seventy patients with terminal ileal CD (mean age 40.74±15.56 years; 71.4% males [n=50]) were evaluated. The sensitivities of MARIA and MARIAs scores to detect active disease were 0.76 and 0.84 respectively. The AUROC for detecting severe disease was 0.836 (p<0.0001) for MARIA and 0.861 (p<0.0001) for MARIAs. For mild active disease, there was no agreement between SES-CD and MARIA or MARIAs, however for severe disease, the agreement was fair and moderate for MARIA and MARIAs respectively. MARIA and MARIAs were comparable for identification of active and severe disease (κ 0.759, p<0.0001 and κ 0.840, p<0.0001 respectively). MRE was 68.18% sensitive to detect mucosal ulcers.
Conclusion MRE is a reliable and sensitive tool for detection of endoscopically severe, but not
mild, terminal ileal CD.
Keywords Colonoscopy, Crohn’s disease, Magnetic resonance imaging
025
Ethanol induced stage specific alteration in gut microbiome and hepatic proteomic signatures in animal model of advanced liver damage
Sudrishti Chaudhary1, Adil Bhat1, Anupama Kumari1, Archana Rastogi2, Guresh Kumar3, Jasvinder Singh Maras1, Shiv Kumar Sarin4, Shvetank Sharma1
Correspondence – Sudrishti Chaudhary – sudrishti.chaudhary@gmail.com
Departments of 1Molecular and Cellular Medicine, 1Pathology, 3Biostatistics, 4Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Introduction Alcohol associated liver disease (ALD) is a major global clinical problem with high morbidity and mortality. The aims of the study were to identify the liver proteome and fecal microbiome at peak injury and during disease progression at early and late stages of ALD and second to correlate these interactions in order to better understand the pathogenesis of ALD.
Methods Male C57BL/6N mice were fed with the control or ethanol Lieber-DeCarli diets for 12 weeks to induce ALD. To capture the events occurring during early and late disease progression, mice were sacrificed after 4, 8 and 12-weeks, respectively. Moreover, peak injury was achieved by a combination of alcohol and thioacetamide-(TAA), which resulted in more severe liver damage. Fecal microbiota was assessed using 16s rRNA. Proteome linked to liver steatosis, injury and intestinal barrier integrity were evaluated by LC-MS.
Results Histology of liver sections revealed wide regions of necrosis and liver damage by 12 weeks, with loss of normal villus structure in the ileal epithelium of intestine. Mice exposed to alcohol and given TAA displayed a pericellular pattern of liver fibrosis, enhanced steatosis, and neutrophil infiltration, comparable to human alcoholic hepatitis. At peak liver injury after 12-weeks, the gram-positive phyla Turicibacteraceae, Paenibacillaceae and Bifidobacteriacea were the most significantly increased, whereas the gram-negative Lachnospiraceae phylum was decreased. The hepatic proteome in the combined treatment group was significantly different from EtOH alone proteins Kif5c, Nod2, Hnf4a, Fxr1 were upregulated (FC>1.5; p <0.05), Whereas proteins Tmsb4x, Cd14, Anxa6, Acot9 (FC<1.5; p<0.05) show downregulation at peak injury.
Conclusion Alcohol exposure induces changes in the fecal microbiome and liver proteome in a stage-specific manner with significant change observed at peak injury in combined treatment group. Modulating the identified bacterial and liver-protein signatures, may pave the way for ALD treatment.
Keywords Mice model, Alcoholic hepatitis, Liver fibrosis, Hepatic proteome, Gut microbiome
026
Human small intestine: A reservoir of gluten degradation bacteria
Sahabram Dewala1, Yogesh Nimonkar1, Om Prakash1, Vineet Ahuja2, Govind K Makharia2 Yogesh Shouche1
Correspondence – Yogesh Shouche–yogesh@nccs.res.in
1National Centre for Microbial Resource, Lab-3, Central Tower, Sai Trinity Complex, National centre for cell science, Pashan–Sus Road, Pashan, Pune 411 021, India, 2Department of Gastroenterology and Human Nutrition Units, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India,
Background Gluten intolerance or celiac disease (CeD) is the most common genetically related food intolerance, worldwide. CeD is T-cells mediated small intestinal inflammation triggered by wheat gluten protein in genetically susceptible individuals who carry HLA-DQ2/8 positive haplotypes. Gluten is one of the major triggering factors known for immunogenic response in CeD patients. The only known cure for gluten intolerance is the lifelong elimination of gluten from the diet. However, sustaining a strict gluten-free diet is very challenging for many reasons. The gluten and immunogenic peptides degradation approach is considered to be a novel therapy for CeD. Thus, we have isolated various aerobic bacteria with gluten and gliadin degradation potential.
Methods In this study, duodenal biopsies were taken from four different categories of patients including treated (6 months on GFD) and untreated CeD, their first-degree relative (FDRs), and disease controls. Colony screening approach was used to screen the gluten degrading bacteria from different CeD groups. Extracellular protease enzymes, which may be responsible for gluten degradation, were partially purified by ammonium sulfate precipitation, dialysis, and then concentrated the enzymes. Degraded immunogenic gliadin were recognized by western blot and quantified by enzyme-linked immunosorbent assays (ELISA).
Results 16S rRNA gene sequencing identified 70 bacterial isolates of 18 distinct bacterial genera of 35 bacterial species from four different CeD groups, only 8 were showed extracellular proteolytic activity against gluten on synthetic gluten agar plates. Isolated bacteria efficiently hydrolyze synthetic Z-PPF-pNA, the most notable T-cell epitope found in gliadin. Moreover, the study found that bacteria and their enzyme can survive at pH 3-7 range.
Conclusion This study identified new gluten-degrading microorganisms from duodenum biopsy of various CeD groups that hold the future therapeutic hopes in CeD treatment. A cocktail of these bacteria, or enzymes, may likely be more effective for achieving maximum gluten detoxification.
Keywords Celiac disease, Z-PPF-pNa, HLA-DQ2/8, ELISA, Antibody, Epitopes
027
Risk alleles of HLA-G exon 8 single nucleotide polymorphisms for hepatocellular carcinoma and its effect on the microRNAs targeting 3’-UTR regulating expression
Baibaswata Nayak1, Neeti Nadda1, Renu Yadav1, Nelanjana Roy1, Sonu Kumar1, Shashi Paul2, Anoop Saraya1, Shalimar1
Correspondence –Baibaswata Nayak –baibaswat@gmail.com
1Departments of Gastroenterology,2Radiodiagnosis, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Human leukocyte antigen-G (HLA-G) expression in cancer is related to tumor-driven immune escape mechanisms. Several polymorphic sites are present in the exon 8 or 3’ untranslated region (UTR) region of HLA-G. Any association these SNPs with HCC and treatment response in Indian patients is not known. How these SNPs influence HLA-G expression is not clear.
Objectives Genetic associations of HLA-G exon 8 polymorphisms with HCC, treatment response and its influence on HLA-G expression by altering miRNA sites.
Methods Twelve SNPs of HLA-G 3’ UTR flanking Exon 8 region (nt8790-9144) were analyzed for case (HCC, n=100)-control (n=110) association study. All these SNPs: were genotyped by sequencing of PCR amplified product and chromatograph reading. Frequency and distribution of Genotype/ Allele in case and control were determined. Hardy-Weinberg equilibrium (HWE) testing and Odds ratio for genetic association were determined. HLA-G expression in HCC patients and influence of different miRNAs on HLA-G expression by targeting polymorphic site were determined.
Result and Discussion We have observed significantly (p = 0.027) higher level of sHLA-G in the serum of HCC patient (61.8±1.8 ng/mL) as compared to healthy (54.2±2.8 ng/mL) controls by ELISA and confirmed in western blot. Out of 12 SNPs, genetic association with HCC and response to locoregional therapy was observed for 5 SNPs: rs1707, rs1710, rs17179108, rs138249160 and rs1063320. Allele with OR>1 are determined as risk and OR<1 determined as protective allele. We have identified several novel miRNAs: miR-5196, miR-4747, miR-3158, miR-8071, miR-3619 and miR-4800 which can target protective allele. The miRNA targeting HLA-G UTR was evaluated by reporter-based assays. Linkage disequilibrium analysis revealed that significantly associated SNPs can form LD blocks.
Conclusion HLA-G SNPs are genetically associated with HCC and treatment response. The miRNAs targeting polymorphic site of 3’UTR can influence HLA-G expressions.
Keywords OncomiR, HCC, Tumor response, Locoregional therapy, HLA-G.
028
Baseline plasma metabolic phenotype in patients with severe alcoholic hepatitis and its association with outcome
Manisha Yadav, Nupur Sharma, Babu Mathew, Gaurav Tripathi, Vasundhra Bindal, Shiv Sarin1, Jaswinder Maras
Correspondence – Jaswinder Maras – jassi2param@gmail.com
Departments of Molecular and Cellular Medicine, and 1Hepatology, Institute of Liver and Biliary Science, D1 Vasant Kunj, New Delhi 110070, India
Severe alcoholic hepatitis (SAH) has high mortality, and corticosteroid therapy is effective in reducing 28 day mortality in about 60% patients. This study was aimed to investigate baseline plasma metabolic phenotype capable of stratifying patients unlikely to respond to corticosteroid therapy and have unfavourable outcome. Plasma metabolomics was performed at baseline, day3 and day7 of corticosteroid therapy in SAH patients using ultra-high performance liquid chromatography and high-resolution mass spectrometry. Patients were categorized as responders (Rs, n=50) and non-responders (NRs, n=20) at day 7 on basis of Lille’s score. Multivariate projection analysis identified metabolites in the derivative cohort (n =70) and were assessed in validation cohort of 153 patients (136 Rs, 17 NRs). Temporal change in the metabolic profile along with Weighted Metabolome Correlation Network Analysis (WMCNA) was performed and correlated to severity. A total of 713 features were annotated (metabolomic/biochemical/spectral databases). After a stringent selection procedure, a total of 8 plasma metabolites significantly discriminated non-responders, most importantly by increased urobilinogen (13-fold), cholesterol sulfate (6.9-fold), AMP (4.7-fold), N-Formimino-L-glutamate (4.3-fold), tryptophan (4.7 folds) levels and decreased 4-Imidazoleacetate (10 fold), urocanic acid (2.2 fold) and thymine (2.4 fold) levels. Additionally, plasma level of urobilinogen, AMP and cholesterol sulfate discriminated non-survivors (p<0.01). Temporal expression of metabolites was higher in Rs (p<0.05). WMCNA identified RED module pathways specific to NRs. Further BLUE and TURQUOISE module pathways were found to be essential for corticosteroid response and correlated with severity in SAH (r>0.7; p<0.01). On validation, baseline plasma urobilinogen (C05791) documented AUC=0.94 (0.91-0.97) for non-response prediction with hazard-ratio of 1.5 (1.2-1.6) for mortality prediction. C05791 at log10 cut-off reliably segregated non-survivors (p-value<0.01, log-rank test) and showed accuracy 98% sensitivity 99% and specificity 98% using random forest-based Machine-Learning.
Conclusion Plasma metabolome signatures can predict pre-therapy steroid response and disease outcome in patients with SAH.
Keywords Nonresponse to steroid, Severe alcoholic hepatitis, Metabolomics, Plasma, Machine learning
029
Clinical utility of transient elastography in the management of patients with Budd-chiari syndrome undergoing endovascular intervention
AbhinavAnand, Sagnik Biswas, ManasVaishnav, Shivanand Gamanagatti1, Anshuman Elhence, Vikas Jindal, Vikas Banyal, Vishwajeet Singh2, Ramesh Kumar3, Shalimar
Correspondence – Shalimar – drshalimar@gmail.com
Departments of Gastroenterology and Human Nutrition, 1Radiodiagnosis, 2Biostatistics, and All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India, 3Department of Gastroenterology, All India Institute of Medical Sciences, Patna - Aurangabad Road, Phulwari Sharif, Patna 801 507, India
Introduction Endovascular interventions for Budd-Chiari syndrome (BCS) have gradually come to the forefront of management of this rare disease. However, such procedures carry the risk of restenosis which is difficult to diagnose clinically. Our aim was to quantify liver stiffness measure (LSM) changes after endovascular intervention for BCS and evaluate whether liver LSM changes predict restenosis after endovascular intervention.
Methods BCS patients who underwent endovascular intervention and had at least two LSM values available after intervention were included. DLSM was the difference between LSM estimated at the last and second last hospital visit. In patients with restenosis, two LSM values before restenosis were included. DLSM% was calculated as the ratio of DLSM to the LSM at second last visit and expressed as a percentage. Odds ratio (OR) with confidence interval (CI) and area under the receiver operating curves (AUROC) were calculated for the predictors of restenosis.
Results The median baseline and post-intervention 1-week, 3-months, 6-months, and 12- months LSM were 47.2 (33.8-68.4) kPa, 29.2 (24.5-43.0) kPa, 26.2 (18.6-38.9) kPa, 20.9 (13.3- 29.8) kPa, and 17.3 (11.8-25.4) kPa, respectively. Of 118 patients, including 67 males, 10 developed restenosis after a median (interquartile range) duration of 19 (11 – 46) months. DLSM% was higher (more positive) in patients with restenosis (44.7 [8.3 – 134.3] vs. -6.6 [- 19.4 to 14.9], p=0.001). DLSM% was a significant predictor of restenosis with an OR of 1.032 (95% CI 1.015 – 1.050, p<0.001). The AUROC for DLSM% was 0.831 (95% CI: 0.750 – 0.893, p=0.001), and a DLSM% increment of 13.2% predicted restenosis with a sensitivity and specificity of 80.0% and 74.1%, respectively.
Conclusion LSM gradually decreases after endovascular intervention and transient elastography is a promising test for detecting restenosis after endovascular treatment of patients with BCS.
Keywords Portal hypertension, Vascular, Fibroscan
030
Ethanol induced alterations in intestinal microbiota correlate with decreased intestinal nuclear receptors (PXR) pathway related proteins
Sudrishti Chaudhary1, Adil Bhat1, Anupama Kumari1, Archana Rastogi2, Guresh Kumar3. Jasvinder Singh Maras1, Shiv Kumar Sarin4, Shvetank Sharma1
Correspondence – Sudrishti Chaudhary – sudrishti.chaudhary@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Pathology, 3Biostatistics, and 4Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Introduction Alcohol liver disease (ALD) is associated with gut bacterial dysbiosis and increased gut permeability. Pregnane X receptor (PXR), a ligand activated nuclear receptor has been implicated in transcriptional regulation of intestinal barrier integrity and inflammation. We investigated whether intestinal PXR expression plays a role in gut microbiota homeostasis affecting hepatic function in a mouse model of ALD.
Methods Male C57BL/6N mice were fed with the ethanol Lieber-DeCarli diet for 12 weeks to induce ALD. Fecal microbiota was assessed using 16s rRNA followed by fecal metabolome analysis. Intestine and liver tissue proteome analysis were evaluated by LC-MS/MS.
Results Chronic ethanol feeding in mice changes the gut microbiota composition and promotes microbial dysbiosis with altered fecal metabolites associated to fatty acid amides. Long-term ethanol exposure resulted in loss of normal villus structure of the ileac epithelium and proteomic analysis of intestinal tissue revealed decrease in anti-oxidative, tight junction proteins and increase in inflammation/injury linked proteins (FC<1.5, p<0.05). Chronic EtOH feeding increased ALT/AST and liver injury in mice. Moreover, EtOH-exposure in mice showed downregulation of proteins such as Cyp3a11 (FC<1.5, p<0.05) important for xenobiotic/bile acid detoxification linked to PXR. Short chain fatty acid producing bacteria such as Chlorobaculum and Lachnospira were decreased in EtOH and positively correlated (r>0.7, p<0.05) with the PXR proteins involved in tight junctions and PPAR signaling. Coriobacterium and Galenea, the secondary bile acid-producing bacteria correlated negatively with the downregulated protein Apoa1 and Cyp1a2 involved in drug metabolism and AMPK signaling pathway (r<0.7, p<0.05) in EtOH fed mice.
Conclusion Long-term EtOH consumption promotes disruption in intestinal PXR expression. The identified bacterial families correlate with PXR linked proteins and pathways suggesting an important role of nuclear receptors in tissue injury which could be explored as therapeutic targets to prevent dysbiosis leading to advance stage of alcoholic liver diseases.
Keywords Gut microbiome, Liver injury, Nuclear receptor, Hepatic proteome, Intestinal proteome
031
Prolonged detection of SARS CoV2 RNA in extracellular vesicles in nasal swab RT-PCR negative with liver disease patients
P Debishree Subudhi , Sheetalnath Rooge, Swati Thangariyal, Ekta Gupta, Shiv Sarin, Sukriti Baweja
Correspondence – Sukriti Baweja – sukritibiochem@gmail.com
Department of Molecular and Cellular Medicine, Institute of Liver and Biliary Sciences, D1 Vasant Kunj, New Delhi 110 070, India
Background There is a prolonged reverse transcription–polymerase chain reaction (RT-PCR) positivity seen in corona virus disease 2019 (COVID-19) infected patients up to 2-3 months. We aim to investigate the presence of viral particles inside extracellular vesicles (EV) and its role in underlying liver disease patients.
Methods SARS CoV2 nasal RT-PCR positive n=78 (n=24 [66.6%] chronic liver disease [CLD]; n=52 [81.3%] non-liver disease) were studied. SARS CoV2 patients were also followed up for day (d) 7, 14 and 28. Extracellular vesicles were isolated using differential ultracentrifugation. SARS CoV2 RNA was measured using qRT-PCR by Altona Real Star kit.
Results In baseline RT-PCR positive patients, SARS-CoV2 RNA inside the EV was present in 64/74 (82%) patients with comparable viral load between VTM and EV (mean 1CT – 0.033±0.005 vs. 1CT– 0.029±0.014, p=ns). On follow-up at day 7, of the 24 patients negative for COVID-19, 10 (41%) had persistence of virus in the EV (1CT – 0.028±0.004) and on day 14, 14 of 40 (35%) negative RT-PCR had Evs with SARS CoV2 RNA (1CT – 0.028±0.06). The mean viral load decreased at day7 and day14 in nasal swab from baseline (p=0.001) but not in EV. SARS-CoV2 RNA otherwise undetectable in plasma, was found to be positive in EV in 12.5% of COVID-19 positive patients. Interestingly, significantly prolonged, and high viral load was found in EV at day 14 in CLD-COVID-19 patients compared to COVID-19 alone (p=0.002). The high cellular injury was seen in CLD-COVID-19 infected patients with significant high levels of EV associated with endothelial cells and hepatocytes than COVID-19 alone (p=0.004; 0.001).
Conclusion Identification of SARS-CoV2 RNA in EV, in RT-PCR negative patients indicates persistence of infection for and likely recurrence of the infection. EV associated RNA may determine the clinical course of subjects with undetectable SARS-CoV2 virus and this may also have relevance in management of chronic liver disease patients.
Keywords SARS CoV2, Chronic liver disease, Extracellular vesicles, RT-PCR
032
Early fecal microbiome transfer after donor defecation determines response in patients with moderate to severe ulcerative colitis
Arshdeep Singh, Ramit Mahajan, Bhavjeet Kaur Kahlon, Ashvin Singh Dhaliwal, Vandana Midha1, Ajit Sood
Correspondence – Ajit Sood – ajitsood10@gmail.com
Department of Gastroenterology, and 1Medicine, Dayanand Medical College and Hospital Tagore Nagar, Civil Lines, Ludhiana 141 001, India
Background Fecal microbiome transfer (FMT) targeting gut microbiome dysbiosis is an emerging therapy for ulcerative colitis (UC). There is however no consensus on protocols for performing FMT in UC, especially in relation to time after donor feces defecation.
Methods This is a single-center retrospective analysis of patients with moderate-severe UC (total Mayo clinic score ≥6 and endoscopic Mayo clinic sub score of ≥2) treated with FMT between September 2017 and December 2019 at Dayanand Medical College and Hospital, India. Fresh fecal samples from unrelated healthy voluntary donors were administered through colonoscopy at weeks 0, 2, 6, 10, 14, 18, and 22. Time interval between donor feces defecation and FMT procedure was recorded for each FMT session and the mean time of seven sessions was designated aika. Impact of aika on clinical response and safety of FMT was evaluated.
Results During the study period, 123 adult patients (mean age 33.75±11.97 years, 61.8% [n=76] males) with moderate-severe UC (mean total Mayo clinic and endoscopic Mayo clinic scores 7.49±1.60 and 2.50±0.50, respectively) were treated with FMT. The mean aika was 2.29±0.75 hours. The aika was smaller in patients who responded to FMT as compared to non-responders (2.09±0.60 vs. 2.32±0.75 hours, p<0.0001) as well as in patients achieving clinical remission (2.09±0.58 hours vs. 2.43±0.81 hours, p=0.05). There was no significant impact of aika on adverse effects except the incidence of borborygmi after FMT, which was higher in patients with aika ≤2 hours.
Conclusion Early FMT after donor feces defecation favorably impacts the clinical response rates in patients with active UC.
Keywords Gastrointestinal microbiome, Fecal microbiota transplantation, Ulcerative colitis
033
Transcription factor Runx1 regulates lecithin retinol acyltransferase during activation of hepatic stellate cells in non-alcoholic fatty liver disease
Sumati Rohilla 1 , Indu Sharma 2 , Pretty Rawal 1 , Impreet Kaur 2 , Dinesh Tripathi 2 , Rekha Puria 1 , Savneet Kaur 2
Correspondence – Savneet Kaur – savykaur@gmail.com
1School of Biotechnology, Gautam Buddha University, Greater Noida 201 312, India, and 2Department of Molecular and Cellular Medicine, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Introduction A runt-related transcription factor (Runx1) is a key transcription factors affecting hepatic stellate cell (HSC) activation in NAFLD. Here, we investigated expression of RUNX1 in hepatocytes and HSCs in the in vitro and in vivo models of NAFLD and studied RUNX1 mediated HSC activation in vitro.
Methods Palmitate-treated primary hepatocytes and HSCs were used for in vitro models of NAFLD. In vivo models of NAFLD were developed by feeding rats with high fat high carbohydrate. Expression of Runx1 and other lipid metabolism genes were studied. The effects of Runx1 silencing on lipid metabolism and HSC activation were analyzed
Results We observed increased number of lipid droplets in hepatocytes and while they were reduced in activated HSCs in steatotic conditions both in vitro and in vivo. Among all studied genes, we observed a significant increase in lecithin retinol acyltransferase (LRAT), a vitamin A storage gene, hepatocytes while its expression was significantly downregulated in comparison to the controls under steatotic conditions. Expression of LRAT in HSCs inversely correlated with expression of alpha-SMA. Runx1 was increased in steatotic HSCs as compared to controls. In silico analysis showed that LRAT interacts with Runx1 at -250 and -198 bp on plus strand. Upon silencing Runx1 in HSCs, expression of LRAT was enhanced with reduced expression of alpha-SMA.
Conclusion In NAFLD, there is a redistribution of LRAT from activated HSCs to the hepatocytes. In activated HSCs, Runx1 negatively regulates expression of LRAT, which may be thus a key mediator of Runx1-induced activation of HSCs.
Keywords Hepatic stellate cell, LRAT, Runx1
034
Better survival with centrifugal plasma exchange compared to membrane plasma exchange in severe alcoholic hepatitis and acute on chronic liver failure patients
Santhosh Kumar 1 , Snehil Kumar 2 , Vinoi David 3 , Santosh Varughese 3 , Dolly Daniel 2 , Joy Mammen 2 , Sukesh Nair 2 , Sushovan Baidya 1 , Vijayalekshmi Balakrishnan 4 , Ashish Goel 1 , Uday Zachariah 1 , Elwyn Elias 5 , C E Eapen 1
Correspondence – C E Eapen – eapen@cmcvellore.ac.in
Departments of 1Hepatology, 2Transfusion Medicine and Immunohematology, 3Nephrology, and 4Wellcome Research Unit, Christian Medical College, Vellore 632 001, India, and 5Department of Hepatology QE Hospital, Birmingham, 35020, United Kingdom
Background Plasma exchange (PLEX) improves survival in patients with severe alcoholic hepatitis (SAH) and acute on chronic liver failure (ACLF), it is not known if centrifugal or membrane PLEX is preferable.
Methods We retrospectively studied SAH and ACLF (APASL) patients treated with PLEX between November 2017 to June 2021 in our department. Patients had low volume PLEX and low dose steroid. PLEX technique (centrifugal or membrane) was decided based on availability of PLEX machine. Primary outcome was survival till September 30th, 2021 or up to 1 year after PLEX.
Results Fifty-one patients with SAH and ACLF (all men, mean age 42.6 [±9.7] years) had PLEX (centrifugal – 25, membrane – 26). Both groups had comparable liver disease severity scores: centrifugal PLEX; MELD 28 (20-46), mDF 90 (50-262.7), AARC score 9 (6-15) and membrane PLEX; MELD 30.5 (22-49), mDF 84.7 (48-192), AARC score 10 (8-13). EASL-CLIF ACLF criteria were fulfilled by 40% and 69% patients in centrifugal and membrane groups respectively (p-0.05). Median number of PLEX sessions (3) and plasma volume exchanged (1.4 liters) were similar between the two groups. Centrifugal PLEX patients had higher plasma removal efficiency (55% vs. 20%) and slower flow rate (35 mL/min vs. 125 mL/min). Significantly better survival was noted in centrifugal PLEX patients compared to membrane PLEX (adjusted [for EASL ACLF] hazard’s ratio 0.21 (0.09-0.47) (p value <0.0001). Survival estimate (standard error) are as follows: Centrifugal; 1 month 88% (6.5), 3 months 79.6% (8.1), 6 months 68.2 % (10.2) and 1 year 62% (11), Membrane; 1 month 61.5% (9.5), 3 months 23.1% (8.3), 6 months 9.2% (6) and 1 year 4.6% (4.4) (p value < 0.0001).
Conclusion SAH and ACLF patients treated with centrifugal PLEX had better survival compared to membrane PLEX. The mechanism of survival benefit by centrifugal PLEX needs to be investigated.
Keywords Centrifugal plasma exchange, Alcoholic hepatitis, Acute on chronic liver failure
035
Intravenous branched chain amino acids for the treatment of hepatic encephalopathy in acute-on-chronic liver failure – Interim analysis of the BCAA-ACLF trial
Rohit Mehtani 1 , Madhumita Premkumar 1 , Kajal Kalal 2 , Shankey Garg 2 , Shiv Soni 2 , Radha K Dhiman 1 , Nipun Verma 1 , Sunil Taneja 1 , Arka De 1 , Ajay Duseja 1 , Virendra Singh 1
Correspondence – Madhumita Premkumar - drmadhumitap@gmail.com
Departments of 1Hepatology, 2Anesthesiology and Critical Care, Post Graduate Institute of Medical Education and Research, Nehru Hospital Extension Block, Sector-12, Chandigarh 160 012, India
Objectives A prospective, randomized controlled clinical trial was conducted to study efficacy of intravenous branched chain amino acids (BCAA) with lactulose vs. lactulose alone in treatment of hepatic encephalopathy (HE) in acute on chronic liver failure (ACLF). Improvement in encephalopathy at 72-hours and survival at day 7 and 28 was measured.
Methods CANONIC ACLF patients with HE grades ≥ 2 received IV BCAA (500 mL/day for 3 days) + Lactulose (treatment arm; n=34) or Lactulose alone (control arm; n=34). Six patients developed corona virus disease 2019 (COVID-19) and were excluded after enrolment (4-treatment arm and 2-control arm). Grade of HE was assessed by West Haven Classification and Hepatic Encephalopathy Scoring Algorithm (HESA). ACLF severity was determined by CLIF-C ACLF, MELD and Child-Pugh’s score. All patients received standard of care for HE and ACLF management.
Results Both groups were similar in baseline characteristics including grade of HE (2.9 ± 0.7 vs. 2.8 ± 0.6; p=0.613) and CLIF-C ACLF score (54 ± 5.9 vs. 55.34 ± 5.4; p=0.383). Overall survival was 40% at 28 days (50% vs. 31.2%; HR – 1.7 [0.88-3.28]; p=0.113). Significant improvement in HESA score by ≥1 grade at 24 hours was seen in 14 patients (46.7%) in treatment group and 6 patients (18.7%) in control group (p=0.029). Median change in HESA score at 24 hours was significantly more in treatment group than control group (p=0.003) however, this was not sustained at day 3 or 7.
Conclusion Intravenous BCAA leads to short-term but ill-sustained improvement in grade of HE and survival in ACLF.
Keywords Acute-on-chronic liver failure, Branched chain amino acids, Hepatic encephalopathy
036
Malnutrition by GLIM criteria in chronic pancreatitis: Prevalence, predictors, and its impact on quality of life
Srikanth Gopi , Sumaira Qamar, Namrata Singh, Samagra Agarwal, Jatin Yegurla, Atul Rana, Deepak Gunjan. Anoop Saraya
Correspondence – Anoop Saraya – ansaraya@yahoo.com
Department of Gastroenterology and Human Nutrition Unit, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Malnutrition in chronic pancreatitis (CP) has prognostic value and there is limited data on the prevalence, predictors of malnutrition in CP and its effect on Quality of life (QoL).
Methods A retrospective study was conducted in patients with CP to assess the prevalence of malnutrition as per the Global Leadership Initiative on Malnutrition (GLIM) criteria. Multivariable-adjusted regression was used to identify independent predictors of both malnutrition and global QoL.
Results A total of 297 patients were included and the most common etiology of CP was idiopathic (75%) and alcohol (25%). The prevalence of malnutrition was 46.4% as per GLIM criteria. On univariate analysis, the risk of malnutrition was significantly higher in alcoholic etiology (p=0.001), current alcohol consumption (p=0.001), smokers (p<0.001), those having higher cumulative days of pain in last 6 months (p<0.001) and lower daily calorie intake (p =0.019). On multivariate analysis, malnutrition was independently associated with current alcohol consumption (Odds ratio: 3.22, p=0.017), current smokers (OR: 2.23, p=0.042) and those having higher cumulative days of abdominal pain (OR: 1.01, p<0.001), while higher daily calorie intake (OR:0.99, p=0.023) has reduced risk of malnutrition. Malnutrition (p=0.015) and higher cumulative days of abdominal pain (p<0.001) were independently associated with lower global QoL in patients with CP.
Conclusion Malnutrition is frequent in patients with CP; and current alcohol consumption, smoking and higher cumulative days of abdominal pain independently predicts risk of developing malnutrition. Patients with malnutrition and higher cumulative days of pain has poorer quality of life.
Keywords Chronic pancreatitis, Diet, Malnutrition, Quality of life
Esophagus
037
Dysphagia as a late complication of endoscopic variceal ligation
C K Adarsh, Jairaj Bomman, Bhuvan Shetty, B S Puneet, Vamshi, A Vamshi, Pooja Krishnappan
Correspondence - Jairaj Bomman - jrajbomman.333@gmail.com
Department of Medical Gastroenterology, BGS Global Hospital, 67, Uttarahalli Main Road, Sunkalpalya, Bengaluru 560 060, India
Introduction Endoscopic variceal ligation (EVL) is the most common therapeutic procedure as primary and prophylactic treatment for EVH. Dysphagia in the early period after EVL is well-known common complication. Here we present a rare cause of dysphagia occurring as a late complication following EVL.
Case Report An elderly male aged 74 years, K/C/O DM, IHD and Myasthenia Gravis, diagnosed to have D.CLD with ascites at index presentation for abdominal distention. Esophagogastroduodenoscopy (EGD) done for EV assessment showed Grade III EV for which EVL was done. Patient underwent 5 sessions of EVL over 1 year to achieve complete eradication. After 3 months of last EVL, he developed dysphagia for solid foods, EGD done after ruling out neurological cause demonstrated, Grade II Varices with a superficial longitudinal ulcer extending 1.5 cms from the gastroesophageal (GE) junction, dysphagia progressed over next 3 months and repeat EGD revealed, lower end esophageal narrowing beyond which scope couldn’t be negotiated, biopsies obtained for HPE were unremarkable. Further evaluation with contrast-enhanced computed tomography (CECT) abdomen showed asymmetric circumferential thickening of lower 1/3 esophagus with enlarged perigastric, celiac and aortic LN likely metastatic. CT guided LN biopsy done, showed ‘metastatic keratinizing squamous cell carcinoma’, and was treated with chemoradiotherapy. Symptoms improved and was tolerating semi solid food. A year later he again developed dysphagia, and EGD showed circumferential lower end esophageal narrowing for which 15 x 120 cms, Niti-S esophageal covered stent was placed.
Conclusion The known immediate and early complications of EVL includes pain, dysphagia, EVL ulcer/bleeding. The late complication like in our case, post EVL ulcer in lower esophagus transforming into SCC causing significant dysphagia is not known or reported in literature and hence should always be considered. Tough has been reported following esophageal injection sclerotherapy (EIS) in the past but none with EVL.
Keywords Dysphagia, Endoscopic variceal ligation complication, Squamous cell carcinoma
038
A case of esophageal tuberculosis- Rare entity
Srinith Patil, Manoj Kumar Sahu, Girish Kumar Pati, Jimmy Narayan, Debakanta Mishra, G Vybhav Venkatesh, Radhika Nittala, Swarup Patnaik, K Ramgopal Teja
Correspondence – Srinith Patil - srinithpatil@yahoo.com
Department of Medical Gastroenterology, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India
Introduction Gastrointestinal (GI) tuberculosis can involve any site in GI tract, with terminal ileum, cecum, and peritoneum being the usual sites. Esophageal TB (ET) is a rare condition, accounts for only 2.8% of all cases of GI TB. Esophageal involvement from Mycobacterium tuberculosis is rare even in patients of pulmonary and extrapulmonary disease because of various protective mechanisms such as esophageal motility, lower esophageal sphincter, and the covering of squamous epithelium.
Case description A 24-year-old male presented to hospital with complaints of dyspepsia and dry cough for the past 2 months. The patient had history of loss of appetite, loss of weight for the past 2 months. On examination, patient heart rate was 80 bpm, respiratory rate 16 cpm, blood pressure- 110/70 mmHg. Routine blood investigations done were within normal limits, tested negative for HIV, HCV, and hepatitis B. The patient’s sputum examination for AFB came out to be negative. HRCT thorax showed fibrocavitary lesions in left upper lobe and few enlarged mediastinal lymph nodes. UGI scopy revealed mid esophageal diverticulum and ulcerated lesion. Histopathological examination revealed ill-defined epithelioid granulomas with giant cells and caseating necrosis. DOTS regimen was started with isoniazid, rifampicin, pyrazinamide, and ethambutol. The patient was advised to continue anti-TB treatment (ATT) for 6 months as prescribed. Patient was under regular follow-up. Repeat UGI scopy done after 6 months of ATT revealed mid esophageal scar and patient was symptomatically better.
Conclusion In patients with risk factor for TB, ET should be included in the differential diagnosis despite its rarity. Histopathology and TB-PCR are the key to confirm the diagnosis. Delay in diagnosis can lead to complications, which might require surgical intervention; otherwise, this condition is effectively treated with ATT.
Keywords Esophageal tuberculosis, Anti-tuberculosis treatment, Giant cells and caseating necrosis
039
Nursing care practice and documentation of care followed by nursing personnel among patients undergoing endoscopy, with a view to develop a protocol-based flow chart
T S Rican, Mini George, Ashok Chaudhary
Correspondence – Mini George - minniegeorge1@gmail.com
College of Nursing, Department of Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Introduction Endoscopy is an invasive procedure used for diagnosis and treatment of gastrointestinal disease. Nursing Care Practice and Documentation of those activities is necessary to provide quality care and evaluate the patient progress to ensure patient safety during endoscopy.
Methods A descriptive study was conducted after formal approval and ethics clearance at Endoscopy Unit of Institute of Liver and Biliary Sciences. Prospectively, 240 events of Nursing Care Practice was observed using Observation Checklist. Retrospectively, from Nursing Records of the period January 2019 to December 2019, documentation (n=717) followed by nursing personnel, was retrieved using Data Abstraction Form, with the help of Abstraction Manual.
Results At the end triangulation is done for both the studies, the researcher discovered the similar findings which had not practice and documented are past medical/surgical history (65.4%, 97.6%), Procedure explanation (98.8%, 97.4%) during pre-procedure care. Level of consciousness (55%, 96%), skin assessment (99.6%, 99.6%) and adverse events (92.9%, 97.8%) during intra-procedure care. In post-procedure care, RAS (99.2%, 99.2%), intake/output (98.3%, 80.2%) and discharge instructions (87.5%, 99.2%).
Conclusion The study findings shows that majority of Nurses did not practice as well as documentation of care is not done related to endoscopy patient care. A Protocol Based Documentation Chart was developed for Endoscopy Nurses, which is expected to improve the Nursing Care as well as its documentation in future.
Keywords Nursing Care, Documentation of care, Endoscopy
040
Outcome of per oral endoscopic myotomy in advanced achalasia cardia with sigmoid esophagus at a median follow-up of 17 months
Harshal Mandavdhare , Jayanta Samanta, Anudeep Jafra, Rajeev Chauhan, Harjeet Singh, Pankaj Gupta, Usha Dutta
Correspondence - Harshal Mandavdhare - hmandavdhare760@gmail.com
Department of Gastroenterology, Post Graduate Institute of Medical Education and Research, Ground Floor, F Block, Nehru Hospital, Sector 12, Chandigarh 160 012, India
Background Advanced achalasia cardia represents the end stage in the natural history of achalasia cardia with anatomical distortion in the form of sigmoid morphology and/or excessive dilatation of the esophagus. Role of per oral endoscopic myotomy (POEM) in this technically difficult subset is emerging.
Methods We did a retrospective review of consecutive patients who underwent POEM for advanced achalasia cardia with sigmoid esophagus. The definition of the sigmoid morphology was adapted as per the Japanese Esophageal Society descriptive rules of achalasia as sigmoid (Sg) (αangle)-<135o) or advanced sigmoid (aSg) (αangle-<90o). We assessed the technical success, clinical success and adverse event rate. Pre and post POEM Eckardt score (ES), Integrated relaxation pressure-4sec (IRP-4), lower esophageal sphincter pressure (LESP) and height and width of barium column at 5 minutes were noted.
Results Ten patients underwent POEM for advanced achalasia cardia with sigmoid esophagus of which 8 were Sg and 2 were aSg. The clinical and technical success was 100% with significant reduction of ES, IRP-4, LESP and height and width of barium column at 5 minutes. One patient had a minor adverse event in the form of mucosal injury that was closed with hemoclips. At a median follow-up of 17 months there was no recurrence.
Conclusion Our study demonstrates POEM to be a safe and effective modality of treatment in this technically difficult subset of achalasia cardia with sigmoid morphology.
Keywords Achalasia cardia, Sigmoid esophagus, POEM, Efficacy
041
A study of clinical, endoscopic and manometric profile of patients with refractory gastroesophageal reflux disease in a tertiary care hospital
Sreeram Vemparala, M S Revathy
Correspondence - M S Revathy - drrevathy2010@gmail.com
Department o, Medical Gastroenterology, Stanley Government College. George Town Road, Chennai 600 001, India
Background Abnormal esophageal motility and low lower esophageal pressure (LES) play an integral role among various etiologies implicated in pathogenesis and severity of gastroesophageal reflux disease (GERD). Delayed clearance of refluxate leads to prolonged mucosal exposure to gastroduodenal contents which promotes esophagitis and its complications. To find out the association of ineffective esophageal motility (IEM) and low LES pressure with endoscopic esophagitis in patients presenting with refractory GERD.
Settings and designs Prospective cross-sectional study done in a tertiary medical care centre from March 2021 to September 2021.
Methods This cross-sectional study was carried out among patients presenting with refractory GERD (heart burn and regurgitation, with partial or no response to 6 weeks of medical management. GERD patients are grouped into erosive and nonerosive reflux disease. After general and systemic clinical examination, high resolution manometry was performed, and data was analyzed using Trace 1.2.3a V software.
Statistical Methods Data was analysed using SPSS version 21. Chi-square test was used to analyse categorical variables and independent ’t’ test was used for continuous variables.
Results A total of 36 patients with refractory GERD symptoms were subjected to esophageal manometry. Out of these 36 patients 17 were males and 19 were females with their mean age 41.278 years. Seven patients were found to have ineffective esophageal motility (1 failed, 6 weak peristalsis) and 11 had low LES pressure (<40 mmHg). Endoscopic finding in these 7 patients with ineffective motility are 1 grade-D, 5 grade-C, 1 grade-B, Ineffective esophageal motility was also found to be more common among older age group individuals with their mean age being 43.54.
Conclusions This study concludes that ineffective motility was commonly seen among Grade-C distal esophagitis in patients with refractory GERD.
Keywords Refractory GERD, High resolution manometry, Hypotensive sphincter, Ineffective peristalsis
042
Outcome of corrosive esophageal stricture in our tertiary care centre
Swarna Anupama, A Chezhian, A Aravind, Caroline Selvi, K Prem Kumar, R Murali, Muthu Kumaran, L Shubha
Correspondence - Swarna Anupama - anupama.swarna92@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Outcome of endoscopic dilatation in corrosive esophageal stricture is less known. This study aims to determine the outcome of dilatation in patients with corrosive esophageal stricture.
Methods All the patients who attended to our hospital with corrosive esophageal stricture from 2019-2021 were included in the study. Endoscopic dilatation with graded Savary-Gilliard dilator was performed as the first line treatment. Outcome of dilatation was considered favorable when patients were able to swallow solid without intervention at least six months after successful dilatation. Failure of dilatation was defined as one of the following: complete luminal stenosis, inability to perform safe dilatation, perforation, and inability to maintain adequate luminal patency. Surgery or repeated dilatation was indicated in failed dilatations.
Results Of 43 patients, 4 lost follow-up, 31 (72%) had failed dilatation (4 having esophageal replacement procedure, 22 continue repeated dilatation, and 5 unfit for surgery). Of 118 sessions of dilatations, eight out of 43 patients (18.6%) had perforations. There was no dilatation-related mortality. All the 4 patients with surgery had good swallow outcome at 6 months post-surgery.
Conclusion Majority of patients with corrosive esophageal stricture were refractory to dilatation. Esophageal dilatations were ultimately failed in about three-fourth of the patients.
Keywords Corrosive stricture, Esophageal dilatation, Refractory strictures
043
Influence of gastroesophageal flap valve on esophageal variceal bleeding in chronic liver disease patients
Jay Chudasama, Pravin Rathi, Shubham Jain, Sanjay Chandnani, Harsh Gandhi, Rishikesh Malokar, Sneha Gupta
Correspondence - Jay Chudasama - Jaychudasama84@yahoo.com
Department of Gastroenterology, Topiwala National Medical College and B Y L Nair Hospital, Mumbai Central, Mumbai 400 008, India
Methods It is interim analysis of cross-sectional study involving 57 adult subjects with esophageal varices of any grade and Flap valve of any grade enrolled. Patients are assessed with esophagogastroduodenoscopy and incidence of variceal bleeding is compared with grade of flap valve.
Results Out of 57 patients, 22 patients had small varices (<5 mm) and 35 had large varices (>5 mm).from those 91.2 % patients (52) had flap valve of hill’s grade 1/2 (p= 0.085). There was no association between grade of varices and Hill’s grade of flap valve. From all the patients, 9 patients presented with hematemesis and 48 had not. From those 9 patients, 8 (88.88%) patients had Hill’s grade 1/2 flap valve (p=0.982). So there was no correlation between incidence of hematemesis and grade oof flap valve.
Conclusion Our study did not confirm the association between Grade of esophageal varices and hematemesis incidence with Hill’s grade of flap valve.
Keywords Hill’s grade, Flap valve, Esophageal varices
044
Role of per oral endoscopic myotomy in advanced achalasia cardia with sigmoid and/or megaesophagus - A systematic review and metanalysis
Harshal Mandavdhare , Praveen M Kumar 1 , Jayendra Shukla, Antriksh Kumar, Vishal Sharma
Correspondence - Harshal Mandavdhare - hmandavdhare760@gmail.com
Departments of Gastroenterology, and 1Pharmacology, Post Graduate Institute of Medical Education and Research, Nehru Hospital, Sector 12, Chandigarh 160 012, India
Background Sigmoid esophagus and/or megaesophagus are considered as an advanced stage in the natural history of achalasia cardia. The role of per oral endoscopic myotomy (POEM) in these subset of patients is emerging.
Methods We performed a systematic review and metanalysis to study the efficacy of POEM in advanced achalasia cardia with sigmoid and megaesophagus. A literature search in PubMed and Embase was done from inception till 03/08/2021 to look for studies reporting exclusively on the role of POEM in advanced achalasia cardia with sigmoid and/or megaesophagus. The random effect method with inverse variance approach was used for the computation of pooled prevalence. For two groups' analysis of continuous outcome standardized mean difference was used as the summary measure.
Results Eleven studies with 428 patients were included for analysis. The pooled technical and clinical success was 98.27% (95% CI; 96.19-99.22; I2=0%) and 89.38% (95% CI; 84.49-92.86; I2=26%) respectively. On subgroup analysis into sigmoid and megaesophagus the technical and clinical success was (98.06% [95% CI; 95.41-99.19; I2=0%], 98.47% [95% CI; 9272-99.69; I2=0%] and 87.92% [95% CI; 80.68-92.70; I2=37%], 88.36% [95% CI; 62.62-97.17; I2=77%]) respectively. The clinical success at < 1year and 1-3 year follow-up was 89.37% (95% CI; 82.82-93.61; I2=0%) and 88.66% (95% CI; 81.65-91.22; I2=46%) respectively. There was a significant reduction in the post POEM scores with standardized mean difference for Eckardt score-4.81, for integrated relaxation pressure at 4 seconds-1.93 and for lower esophageal sphincter pressure-2.06.
Conclusion POEM is an effective modality of treatment even in the subset of patients of advanced achalasia cardia with sigmoid and/or megaesophagus.
Keywords Achalasia cardia, Sigmoid esophagus, Megaesophagus, POEM
045
Effect of lifestyle factors and gastrointestinal disease, among the north Indian patients
Prisha Warikoo , Prateek Sharma, Shweta Mahant, Kunal Das 1 , Rajashree Das
Correspondence – Rajashree Das - rdas@amity.edu
Amity Institute of Biotechnology, Amity University Noida, Amity Road, Sector 125, Noida, 201 301, India, and 1Department of Gastroenterology, Manipal Hospital, Palam Vihar, Sector 6, Dwarka, New Delhi 110 075, India
Introduction Various lifestyle factors, including diet, age, alcohol and gastrointestinal diseases status have individually been proven to alter the host’s gut microbial, in an increasing number of studies, and have been separately linked to various diseases. However, studies examining the influence of the microbiome of patients in North India considering multiple factors, are scarce. Hence this research effort is directed towards lessening that gap, by examining, on the basis of diet, the overlap of age, alcohol, and gastrointestinal disease.
Methodology Human tissue biopsy samples of 19 individuals were collected in which 13 were non- vegetarian, 6 vegetarian, three alcoholic, 16 non-alcoholic, 8 with GERD, 5 DU patients and 5 with gastritis. 16s rRNA was then used to analyse the samples as well as library quality and sequencing.
Results It was found that, across all lifestyle factors, Prevotella Melaninogenica, belonging to the phylum Proteobacteria was present in the top 10 species in omnivores, barring those that drank alcohol. In vegetarians, Corynebacterium sp., was highly abundant across all factors, with its phylum Actinobacteria being in the top three, except for in DU samples, and Haemophilus parainfluenzae (Proteobacteria), also one of the ten most abundant species. The only time there was an obvious similarity in the microbial composition of the two diets was in the alcoholics, where Streptococcus sp. was found to be most abundant in omnivores (18.10%), and second most abundant in vegetarians (14.01%). (Add percentages and phylum)
Conclusions Streptococcus sp. also causes gastric degradation, indicating that despite diet influencing the health of the host, an alcoholic host will majorly face the same repercussions. Prevotella Melaninogenica was also mainly high in omnivores, and has been linked to an increase in gastric cancer risk.
Keywords Gastrointestinal disease, Dietary status, Gut microbiome
046
Quality of life changes in patients of achalasia cardia undergoing pneumatic dilatation versus laparoscopic Heller’s cardiomyotomy
Hemant Purohit , M A Ansari, Vivek Srivastava
Correspondence - Hemant Purohit - drhemant313@gmail.com
Department of General Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221 005, India
Aim To compare quality of life changes in patients of achalasia cardia undergoing pneumatic dilatation vs. laparoscopic Heller’s cardiomyotomy carried out in Department of General Surgery and Department of Gastroenterology, Institute of Medical Science, Banaras Hindu University, Varanasi between July 2017 to July 2019.
Methods Forty manometric confirmed achalasia cardia patients were included in this study. Patients underwent pneumatic dilatation (Group 1) and laparoscopic Heller’s myotomy (Group 2). Patients were followed up post treatment at 1 week and 3 months for symptoms assessment. High resolution manometry was done in patients at 3 months for assessment of short-term therapeutic outcome. Quality of life assessment was done using the SF36 questionnaire prior to intervention, at 1 week and 3-month post intervention.
Results Median of dysphagia score was higher compared to other sub scores of Eckardt in both the groups. Eckardt score decreased significantly in LH group (0.50±0.761) as compared to PD group (1.10±0.852) at 3 months of follow-up. The median post treatment physical summated score at 1week was (38.12 [34.37-41.87]) and (42.50 [38.44-48.59]) in PD and LH group (p value <0.001) median mental summated score at 1 week was (19.06 [17.38-21.75]) and (23.50 [22.25-26.62]) in PD and LH group (p<0.001). Median post treatment physical summated score at 3 month was (65.00 [59.37-66.87]) and (63.75 [63.12-71.38]) in PD and LH group respectively (p=0.157).
Conclusion Surgical treatment (LH) and pneumatic dilatation (PD), both are effective treatment modalities for achalasia even after a short-term follow-up. Patients of LH group had a significant improvement both in the subjective as well as the objective parameters of the disease along with significant improvement in the quality-of-life scores as well, as assessed by SF-36 questionnaire.
Keywords LH-Laparoscopic Heller’s cardiomyotomy, PD- Pneumatic dilatation
047
Indications, safety profile and efficacy of 265 Savary-Gilliard dilatations at a tertiary care centre
Lavanya Narayanan , Kani Shaikh Mohamed, A R Akilandeswari, A Anand
Correspondence - Lavanya Narayanan - lavanya12@gmail.com
Department of Digestive Health and Diseases, Kilpauk Medical College, Chennai 600 010, India
Introduction Esophageal strictures can present with dysphagia, hold-up sensation, weight loss. Etiologies include benign causes like peptic stricture, post corrosive stricture, post radiation stricture, eosinophilic esophagitis, post anastomotic stricture and malignancies. Savary-Gillard dilatations are a commonly used treatment modality for strictures in resource poor settings. This study aims to assess the efficacy and safety of Savary-Gilliard dilatations.
Methods The medical records of patients who underwent Savary-Gilliard dilatation at our hospital between September 2018 to August 2020 were analyzed .The indication for dilatation, grade of dysphagia prior to and after the procedure, post procedural events like significant pain causing prolonged observation, bleeding or perforation were analyzed.
Results A total of 265 Savary-Gilliard dilatations were done in over a period of 2 years. The indication for dilatation in 125 cases was a malignant growth which were excluded from the study. Among the benign 140 cases, the most common indication for SG dilatation was post-radiotherapy stricture which was seen in 63 patients. This was followed by post cricoid web in 38 patients, corrosive stricture in 17 patients, peptic stricture in 15 cases, anastomotic site stricture seen in 7 cases. 90% of patients had an improvement in dysphagia over 2 grades. In the 14 patients who did not improve- the etiology of stricture was corrosive stricture in 8 patients, anastomotic stricture and post radiation stricture in 3 patients each. The complications noted in our study included-post procedural pain in 8 % patients. No significant bleeding or perforation was observed.
Conclusion Savary-Gilliard dilatation is an effective technique for the management of benign esophageal strictures with very low complication rates. Outcomes are better in patients with simple strictures when compared to complex strictures.
Keywords Savary-Gilliard, Stricture, Dysphagia
048
Prospective study evaluating factors associated with occurrence of gastroesophageal reflux disease post peroral endoscopic myotomy in patients with achalasia cardia
Amit Maydeo, Poorva Haridas, Prabha Sawant, Gaurav Patil
Correspondence - Poorva Haridas - prh2091@gmail.com
Department of Gastroenterology, Global Hospitals, Dr E Borges Road, Opp Shirodkar School, Parel 400 012, India
Background Gastroesophageal reflux disease (GER) is commonly seen in patients post peroral endoscopic myotomy (POEM) for achalasia. But the factors associated with the development of GER are explored to a lesser extent.
Methods Consecutive patients of either sex aged ≥18 years, diagnosed to have achalasia cardia who underwent POEM over 18-month period were included. All patients underwent 24-h esophageal pH monitoring, high-resolution manometry and esophagogastroduodenoscopy at baseline and 3 months in addition to filling a GERDQ questionnaire. The pre and post and intra operative parameters were noted. Post POEM GER was defined as per Lyon Consensus.
Results A total of 51 patients (58.8% males) with a mean (SD) age of 40.5 (13.7) years, underwent POEM during the study period out of which 41 (80.4%) completed the 3-month follow-up. At baseline, the mean Eckardt score was 7.2 (1.2), 80 % had type 2 achalasia. Post POEM, mean Eckardt score was 1.48 (0.96), (p<0.05). Post POEM, abnormal AET was seen in 8/41 (20%) as per Lyon. Six (14.6%) had LA grade C esophagitis and 5 (12.1%) were symptomatic i.e. GERDQ score ≥8. On univariate analysis: Fall in IRP >/=20 mmHg from baseline (at 3 months), manometric length of LES segment </=2.5 cm post POEM, length of gastric myotomy (>2cm) and sling fiber involvement during POEM were predictors of GER, while on multivariate analysis only manometric length of LES, long gastric myotomy, sling fiber involvement were independent predictors of GER.
Conclusion Post POEM GER was seen in 17(41.4%) patients at 3 months. Multivariate analysis reveals length of LES, long gastric myotomy and sling fiber involvement to be independent associated with GER.
Keywords POEM, GER, IRP
049
A retrospective study of esophageal self-expandable metallic stent placement for fistulae, perforations and leaks in patients with esophageal cancer at a tertiary cancer centre
Unique Tyagi , Prachi Patil, Sridhar Sundaram, Shaesta Mehta, Aadish Jain, Kiran Mane
Correspondence – Prachi Patil - prachipatil@gmail.com
Department of Gastroenterology, Tata Memorial Hospital, Dr. E Borges Road, Parel, Mumbai 400 012, India
Introduction Esophageal fistulae, perforations and leaks are potentially life-threatening conditions with significant risk of morbidity and mortality. Stent placement and clips are the most commonly used endoscopic treatments.
Methods We did a retrospective analysis of all patients who underwent endoscopic esophageal self-expandable metallic stent (SEMS) placement for leaks, perforations and fistulae at Tata Memorial Hospital, Mumbai. We assessed the technical success, functional success, adverse events and reinterventions.
Result Ninety-four patients (74% male) with esophageal cancer (EC) underwent esophageal SEMS placement between February 2010 till August 2021 for leaks, perforations and fistulae. Mean age was 59.5 years (range 24-85 years). Of these 53 had tracheoesophageal fistulae, 15 had esophago-pleural fistulae and 4 had esophago-bronchial fistulae related to EC. Fourteen patients hada leak after transthoracic total esophagectomy, 3 patients had a spontaneous tumor perforation and 3 had perforation while dilating a post treatment stricture.
Technical success was achieved in 93 patients (98.9%). 25 patients had to undergo a reintervention after the SEMS placement (median reintervention interval- 2.5 months; 24-endoscopic reintervention, 1–surgery). Indications for reintervention were persistent dysphagia (n=2), stent migration (n=10), tissue hyperplasia within SEMS (n=8), non-closure of fistula (n=3), para-stent leak (n=1) and recurrence (n=1). Amongst those who underwent endoscopic intervention, 3 underwent re-stenting while 20 had a nasogastric/nasojejunal feeding tube placed through the stent.
Functional success achieved in 79 patients (84%). Fourteen patients died within 30 days of intervention and 55 patients died within 12 months, mainly related to the underlying EC. There was one post stenting mortality within 24 hrs, rest there were no other adverse events related to the procedure.
Conclusion Esophageal SEMS placement is an effective way to manage esophageal leaks and fistulae with good technical and functional success rates obviating the need for surgery. Upto 27% patients may however need re-intervention.
Keywords Esopheal cancer, Leaks, Fistulae, Esophageal SEMS, Technical success, Functional success
050
Esophageal melanosis – A case report
Matta Rakesh , Lokesh Locheruvapalli, Avinash Balekuduru
Correspondence – Locheruvapalli Lokesh - rakeshkumar.matta@gmail.com
Department of Gastroenterology, M S Ramaiah Medical College, B E L M S Ramaiah Nagar, RIT Post, M S Ramaiah Nagar, Mathikere, Bengaluru 560 054, India
Introduction Esophageal melanosis is a rare benign entity characterized by an increase amount of melanin in esophageal mucosa and increase in the number of melanocytes in basal layer of epithelium. In India, its incidence is 2.1%.
Case Report A 60-year-old male, a known case of type 2 DM/HTN was referred to us from outside hospital in view of evaluation of iron deficiency anemia. On diagnostic endoscopy the patient found to have black pigmented esophageal mucosa. On retrospective history -no h/o of coal dust exposure, smoking, tobacco intake, skin lesions. Biopsy was sent for HPE. HPE revealed subepithelial aggregates of melanophages and diagnosed as esophageal melanosis and advised for follow-up.
Conclusion Esophageal melanosis is a rare benign condition with unknown etiopathogenesis and no specific treatment is available. It is a precursor of malignant melanoma, so patients require follow-up for surveillance of malignancy.
Keywords Pigmented esophageal mucosa, Melanosis
051
Study of esophageal abnormalities in patients with noncardiac chest pain: An observational study
Awadhesh Narayan, Piyush Ranjan, Mandhir Kumar, Shrihari Anikhindi, Rajneesh Jain1
Correspondence – Piyush Ranjan- piyushranjan70@gmail.com
Departments of Gastroenterology, and 1Cardiology, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Noncardiac chest pain (NCCP) is defined as recurrent episodes of retrosternal pain or discomfort that is diagnosed after excluding nonesophageal causes such as cardiac, musculoskeletal, pleural and pulmonary disorders. Aim of this study was to evaluate the various esophageal abnormalities in NCCP.
Methods This was a prospective observational study which included adults (18-65 years) with NCCP. Known cases of pulmonary or pleural diseases, on NSAIDs, history of chest trauma, esophageal or gastric surgery were excluded. All patients underwent UGI endoscopy and esophageal biopsy to rule out eosinophilic esophagitis (EE) . If both endoscopy and biopsy were normal these patients underwent high resolution esophageal manometry (HRM) and those with normal HRM underwent 24-hour Impedance pH monitoring.
Result Sixty patients were included (33 [55%] male and 27 [45%] females) in this study with mean age of 41.8 +/- 13.38 years. Twelve (20%) patients were diagnosed as EE, 16 patients (26.6 %) had esophageal motility disorders (8 ineffective motility, 4 achalasia cardia, 2 small hiatus hernia with EGJ outflow obstruction and one each of Jackhammer esophagus and DES). Fourteen (23.3%) patients were of gastroesophageal reflux disease (GERD), eleven patients (18.3%) were having esophageal hypersensitivity and remaining 7 (11.6%) were diagnosed as functional chest pain.
Conclusion HRM and Impedance pH metry are important diagnostic tools for accurate diagnosis of NCCP in patients with normal endoscopic and esophageal biopsy findings. GERD were present in 23.3% and 26.6% had esophageal motility disorder. After this step-up approach only 30% were found to have esophageal hypersensitivity and functional chest pain, who will be requiring different modalities of treatment.
Keywords Non cardiac chest pain, HRM, 24-hour Impedance pH monitoring
052
Eosinophilic esophagitis
Hima Bindu Panta, Jagadeeshwara Reddy, N Kayal Vizhi. B M Raghu, Amit Yelsingakar, Anupama Nagar, Naresh Bhat
Correspondence - Hima Bindu Panta - bindu60579@gmail.com
Department of Gastroenterology, Aster CMI Hospital, No. 43/2, New Airport Road, NH.7, Hebbal, Sahakara Nagar, Bengaluru 560 092, India
Introduction Eosinophilic esophagitis (EoE) has evolved over the last 3 decades. Incidence of 2.1 to 12.8/100,000/year is described in western literature. There is no data from India.
Methods This is a descriptive study in a tertiary hospital in Bangalore from 2019 -2021. Patients with symptoms suggestive of EoE with or without atopy underwent esophagogastroduodenoscopy and biopsies were obtained from mid and upper esophagus. Demographic and clinical characteristics, endoscopic and histopathologic findings were documented.
Results Out of 114 suspected cases, 14 patients were diagnosed with EoE. Majority of them were males (M:F - 10:4 ) Median age of presentation was 40 years (7 years to 72 years). Median follow-up was up to 3 months (Range: 1 month to 2 years). Atopy was present in 60% of patients (8/14) and peripheral eosinophilia in 20% (2/14) only. Clinical presentation varied from heartburn and regurgitation in 35% (5/14), atypical chest pain in 21% (3/14), dysphagia in 42% (6/14), food bolus obstruction 28% (4/14) and pharyngeal symptoms (dry cough, throat discomfort, globus) 28% (4/14). Endoscopic findings were normal in 28% (2/14). Abnormal findings including feline rings 50% (7/14), linear furrows 35% (5/14), pinpoint exudates (14%) 2/14, fixed rings 35% (5/14) and stenosis 14% (2/14) were seen as well. Most of the patients responded to SFED and PPI. 1 patient required systematic steroids and 2 patients required esophageal dilatation.
Conclusion Incidence of EoE is increasing in our country and high index of clinical suspicion is necessary for diagnosis.
Keywords Six food elimination diet, Budesonide, Incidence
053
Rare case of ectopic sebaceous gland in the esophagus
Arun Patted, Jagadeeshswara Reddy, B M Raghu, N Kayal Vizhi, Amit Yelsangikar. N K Anupama
Correspondence - Arun Patted - arun.medico135@gmail.com
Department of Gastroenterology, Aster CMI Hospital, No. 43/2, New Airport Road, NH.7, Hebbal, Sahakara Nagar, Bengaluru 560 092, India
Introduction Sebaceous glands are derived from the ectoderm. Ectopic sebaceous glands (ESG) have been reported in various other ectopic sites including lips and mouth, eyes, orbits, palms and soles, salivary glands, tongue, and larynx. Esophagus is derived from the endoderm and presence of ectopic sebaceous gland is very rare. We report a case of ESG in the esophagus.
Case Report A 38-year-old gentleman, presented with history of heartburn, regurgitation and abdominal bloating of 8 months duration. There is no history of smoking or alcohol intake. He has no prior comorbid illness and is not on any medications. Clinical examination was unremarkable. BMI was 23. He has been on intermittent empirical proton pump inhibitors despite which he has not had any clinical improvement. Upper GI endoscopy done revealed presence of multiple yellowish-white plaques measuring 5 mm each and was resistant to flushing. Possibility of candida esophagitis or eosinophilic esophagitis was considered, and biopsies were taken. Microscopic examination revealed presence of fragments of hyperplastic stratified squamous epithelium with sub-mucosa showing mature sebaceous glands arranged in lobules. There were no features of fungal organisms, eosinophilic esophagitis, dysplasia or malignancy. There are only 52 case reports of ESG described in the English literature and its clinical significance is not known.
Conclusion ESG in the esophagus is a benign lesion and is very rare. It has to be considered as a differential diagnosis in patients with yellowish-white plaques in the esophagus.
Keywords ESG - ectopic sebaceous glands
054
Study of endoscopic prevalence, clinical, demographic and histological characteristics of heterotopic gastric mucosa in the cervical esophagus and its association with Barrett’s esophagus and hiatus hernia
Cyril Alex, Benoy Sebastian, Anil Jose
Correspondence - Cyril Alex - cyril_alex@yahoo.com
Department of Gastroenterology, Medical Trust Hospital, Mahatma Gandhi Road, Pallimukku, Kochi 682 016, India
Heterotopic gastric mucosa of proximal esophagus (HGMPE) or inlet patch is the presence of gastric columnar mucosa in the upper esophagus. Until recently these lesions were mostly considered non-pathogenic and were usually neglected. Of late the role of inlet patch in various disorders like globus, chronic cough, dysphagia etc are increasingly being noted. Dramatic resolution of troublesome symptoms like chronic globus sensation and cough following ablation of these lesions albeit in small studies, points to a need to study them more closely. The study was undertaken in a tertiary care centre in Kerala over a 1-year period. A total of 2791 patients were enrolled in this study who met the inclusion criteria. The demographic data and the clinical profile were documented, and an upper GI endoscopy was performed and a dedicated effort to look for inlet patches were made using narrow band imaging (NBI) and slow withdrawal in all patients. Paired antral and inlet patch biopsies were taken to analyse the histological type of inlet patch, presence of dysplasia and H. pylori. The study detected 66 cases of inlet patch with a prevalence rate of 2.36%. Laryngopharyngeal reflux symptoms were the predominant symptom found in 54.54%. Globus sensation had a positive association with the presence of inlet patch while dyspepsia and dysphagia failed to show significant correlation. The histopathological analysis showed cardia type mucosa as the predominant type of inlet patch and there was no dysplasia or malignancy detected. There was a positive correlation between the presence of H. pylori in inlet patch and antral biopsy. Taken together a recommendation for avoiding routine biopsies of inlet patches detected during endoscopy is suggested. The presence of inlet patch also had statistically significant association with the presence of endoscopic GERD, Barrett’s esophagus and hiatus hernia.
Keywords Inlet patch, Barrett's esophagus, Helicobacter pylori
055
Comparative efficacy of octreotide and terlipressin along with endoscopic variceal band ligation in the treatment of esophageal variceal bleeding
Krishna Chaitanya Reddy Ramireddy
Correspondence - Krishna Chaitanya Reddy Ramireddy - rchaitanya13@yahoo.com
Department of Medical Gastroenterology, Thoothukudi Government Medical College Hospital, Kamaraj Nagar, Thoothukudi 628 008, India
Introduction Variceal bleeding is a medical emergency that carries a high mortality rate despite timely and appropriate management. Octreotide and Terlipressin are two common agents used as adjuvant agents in the management of variceal bleeding. The objective of this study is to compare the effectiveness of Terlipressin with Octreotide along with endoscopic band ligation in the management of esophageal variceal bleeding in cirrhotic patients.
Methods This randomized control study was carried out at the Department of Medical Gastroenterology, Thoothukudi Government Medical College Hospital, Thoothukudi, for eight months extending from September 2020 to April 2021. A total of 60 cirrhotic patients were selected based on predetermined inclusion and exclusion criteria. The patients were randomly divided into two groups of equal strength. Thirty patients were included in Group A and 30 patients were included in Group B along with banding. Group A received Terlipressin whereas Group B received Octreotide. The two groups were monitored for variceal bleeding for 72 hours.
Results In Group A, 21 (70%) male and 9 (30%) female patients were included. In Group B, there were 18 (60%) male and 12 (40%) female patients. In Group A, the treatment was effective for 27 (90.0%) patients and in Group B, 21 (70.0%) patients had an effective treatment.
Conclusion It is concluded from this study that Terlipressin is statistically more effective than Octreotide in terms of preventing esophageal variceal bleeding.
Keywords Octreotide, Terlipressin, Esophageal varices, Endoscopic band ligation
056
Single center prospective study of Post Cricoid Web
Pavan Thondapu 1 , L R S Girinadh 2
Correspondence – Pavan Thondapu - pavanreddy.1857@gmail.com
1Department of Medical Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014. India, and 2Department of Gastroenterology and Hepatology, Andhra Medical College, Jagadamba Junction, Visakhapatnam 530 002, India
Dysphagia or difficulty in swallowing is a common symptom. Esophageal webs are uncommon causes of dysphagia.
Aims To study the clinical characteristics of patients with post cricoid oesophageal webs. To see the response in those who underwent dilatation procedure. The study was cross sectional study with a population of 111 patients. Dysphagia was graded according to Atkinson grade. The mean age of the population was 45.4±7.66 year. Females 83.8% are more common than males. The mean duration of the disease was 2.5±1.54 years and with 43.2% Grade II and 30% Grade III dysphagia. Duration of Grade III dysphagia (3.62±1.69) was significantly longer (p<0.001) than Grade II dysphagia. The mean hemoglobin was significantly lower in Grade II (9.25±1.32, p<0.001) and Grade III (8.29±1.32, p<0.001) dysphagia compared to Grade 1 dysphagia (10.71±1.65, p<0.001). A significant negative correlation was found (r= -0.73, p<0.0001), which implies that, longer the duration severe the anemia. The mean duration of dysphagia was significantly higher in Grade III dysphagia (3.62±1.69, p<0.001) and Grade II dysphagia (2.35±0.92, p<0.001) compared to Grade I dysphagia. Follow-up of the patients at 3rd and 6th month after dilatation showed Grade 1 and Grade 2 dysphagia has better symptoms resolution with improvement of Hb than Grade 3 dysphagia. Endoscopic intervention (Savary-Gilliards dilatation) along with correction of anemia, achieves remarkable symptomatic improvement in dysphagia and resolution of webs. Post Cricoid web is predominantly seen in middle-aged females. IDA is the most common of anemia in patients with Post Cricoid Web. Our study confirms the safety and efficacy of dilatation of post cricoid web with Savary-Gilliards dilators. The risk of associated carcinoma with long duration disease justifies the need for regular endoscopic surveillance.
Keywords Post cricoid web, Iron deficiency anemia, Endoscopy
057
Comparison of 24-hour pH-metry and impedance monitoring for diagnosis of gastroesophageal reflux disease: A retrospective analysis
Sugata Narayan Biswas, Anshuman Elehence, Anand Agrahari, Bushra Fatima, Uday Ghoshal
Correspondence – Uday Ghoshal - udayghoshal@gmail.com
Department of Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow 226 014, India
Introduction Current gold standard for the diagnosis of gastroesophageal reflux disease (GERD) is 24-h pH-metry. However, 24-h pH-metry fails to detect non-acidic reflux. There has been concern on sensitivity of 24-h pH-metry monitoring alone (both catheter-based and BRAVO capsule) compared to 24-h impedance monitoring, especially, if gastric acid secretion is low due to reduced parietal cell mass, Helicobacter pylori induced gastric atrophy and antisecretory therapy. Accordingly, we aimed to analyse the diagnostic ability of 24-h pH-metry as compared to 24-h impedance monitoring in relation to gastric acid levels for patients off-antisecretory therapy.
Methods A retrospective analysis of prospectively collected data of 91 patients with suspected GERD referred to the GI Pathophysiology and Motility Laboratory for 24-h pH impedance study was done.
Results Among 91 patients (56 [61.5%] males), 73 (80.2%) had confirmed GERD either by pH-metry alone (10 [11%.0]), impedance monitoring alone (25 [27.5%]) or both (38 [41.8%]). Reflux of gastric contents was detected by pH-metry and impedance monitoring in 48 (52.7%) and 63 (69.2%) of patients respectively (p=0.022). Among 48 patients, who were diagnosed with GERD by pH-metry, 12 (13.2%) had reflux in supine posture, 4 (4.4%) had reflux in upright posture while 32 (35.1%) had reflux in both positions. Among 63 patients diagnosed with GERD by impedance monitoring, 5 (5.5%) had reflux in supine posture, 13 (14.3%) had reflux in upright posture, while 45 (49.5%) had reflux in both positions. The mean gastric pH in patients of GERD detected by pH-metry alone (2.34±1.36), impedance monitoring alone (2.02±1.59) and both (1.57±0.91) were comparable (p=0.247). The percentage time of gastric pH <4 in patients of GERD detected by pH-metry alone (82.47±22.30), impedance monitoring alone (82.62± 27.23) and both (91.42±11.68) were also comparable (p=0.228).
Conclusion 24-h impedance monitoring picks up GERD more often than 24-h pH-metry with comparable gastric acid levels in patients who are not on antisecretory therapy.
Keywords Gastroesophageal reflux disease, 24-h pH impedance metry, Reflux
058
Predictors of severity of corrosive injury, can it be predicted?
Neeraj Nagaich 1 , Radha Sharma 2
Correspondence – Neeraj Nagaich - drneerajn@gmail.com
1Department of Gastroenterology, Fortis Escorts, Jaipur 302 020, India, and 2Department of Pathology, RUHS CMS Medical College, Jaipur 302 020, India
Objective To evaluate clinical and biochemical predictor and role of a 6-point EGD classification system of injury in predicting outcomes in patients diagnosed with caustic agent ingestion.
Methods One hundred and six patients with definite caustic ingestion between 2010-2021 were evaluated prospectively and retrospectively Detailed history, physical examination, biochemical, radiological, and endoscopic evaluation was done in all patients at the time of admission and during a follow-up period of 6 month minimum for all patients. Patients were given standard care treatment during this period depending on severity of disease.
Results Endoscopic grading wast most accurate predictor. Voluntary ingestion, vomiting, drooling, stridor and abdominal tenderness were associated with the severity of injury. Leucocytosis, low pH, low phosphorus and alkaline phosphatase level, and high uric acid were significantly associated with severe injury.
Conclusions Serious signs and symptoms (vomiting, drooling, and stridor) had serious esophageal injury. Leucocytosis, low pH, low phosphorus and alkaline phosphatase level, and high uric acid also predict severity of injury. Best predictor of injury is endoscopic grading.
Keywords Corrosive injury, endoscopy, Predictors.
059
Iatrogenic tracheoesophageal fistula: Gargiling Ryle’s tube
Amogh Chandrashekar, Praveen Mathew
Correspondence – Praveen Mathew - drpraveenmathew@yahoo.com
Department of Medical Gastroenterology, Vydehi Institute of Medical Science and Research Centre, Vydehi Hospital, Bangalore 560 076, India
Esophageotracheal fistula is a rare condition, and in most cases such fistulas are caused by malignant disease or emergency endotracheal intubation. approximately 50% of acquired TOFs are secondary to mediastinal malignancy.
Iatrogenic tracheoesophageal (TE) fistula is a rare diagnosis that has high morbidity and mortality and requires a high index of suspicion.
In our case, patient is a 26-year-old male, with no premorbid illness presented with a history of fever and headache since 2 months, altered sensorium since 10 days. There was no history of trauma, chest pain, palpitations, breathlessness, sore throat. No history of foreign body aspiration, ingestion of toxic substances or any surgical procedure in the past. On CNS examination, patient was drowsy but arousal, moving all four limbs. Patient was started on anti-tubercular drugs. Post insertion of nasogastric tube, bubble were seen coming out from the Ryle’s tube. CT thorax done showed tracheoesophageal fistula. OGD confirmed tracheoesophageal fistula. Metallic stent was placed. Feeding jejunostomy was done. Patient improved symptomatically. Metallic stent was removed after 3 months. Patient is tolerating orally.
Keywords Tracheoesophageal fistula, Iatrogenic, Ryle’s tube, Tubercular meningitis
Stomach
060
Clinical and endoscopic characterization of patients with functional dyspepsia
Mayank Jain
Correspondence – Mayank Jain - mayank4670@rediffmail.com
Department of Gastroenterology, Arihant Hospital and Research Centre, 283- A, Gumasta Nagar, Scheme 71, Indore 452 009, India
Background Functional dyspepsia is an umbrella term referring to patients with postprandial distress syndrome (PDS) and epigastric pain syndrome (EPS).
Aim To study the clinical and endoscopic characteristics of patients with dyspepsia who underwent upper gastrointestinal endoscopy at our centre.
Methods This is a retrospective analysis of prospectively maintained database of patients who underwent upper gastrointestinal endoscopy between May 2019 and April 2021. We included all patients >18 years who underwent endoscopic evaluation for dyspeptic symptoms for >4 weeks duration as per Rome IV criteria. We excluded patients with alarm symptoms, antibiotic use, use of proton pump inhibitors or H2 receptor antagonists and upper gastrointestinal malignancy. Data recorded were age, sex, use of alcohol or tobacco, co-morbid diseases, clinical diagnosis with duration and endoscopic findings. Statistical analysis-Chi square test, Student’s t test, Kruskal-Wallis test. A p-value of < 0.05 was considered significant.
Results Two hundred thirty-four patients satisfied the study criteria. They were sub-classified as-EPS (18, 7.7%); PDS (116, 49.6%) and overlap of EPS + PDS (100, 42.7%). Organic dyspepsia (duodenal erosions, duodenal ulcer, erosive esophagitis) were noted in 15% cases. H. pylori infection was detected in 114 cases (48.7%). Prevalence of organic dyspepsia was statistically significant in EPS subgroup (p 0.001).
Conclusion PDS is the commonest presentation of dyspepsia, followed by EPS+PDS overlap. Organic dyspepsia is noted in 15% of cases with dyspepsia and is significantly more common in those with EPS. Rapid urease test for H. pylori infection is positive in 48.7% of cases with dyspepsia.
Keywords Stomach, Dyspepsia, Rome, Epigastric pain, Bloating
061
Gastric xanthelasma: A case report
Shruti Verma, Arshdeep Singh, Ajit Sood
Correspondence – Arshdeep Singh - drarshdeepsingh@gmail.com
Departments of Gastroenterology, Dayanand Medical College and Hospital, Tagore Nagar Civil Lines, Ludhiana 141 001, India
Gastric xanthelasma (GX) are benign clusters of lipid-laden macrophages present in lamina propria. Though the pathogenesis of GX is not known, it is associated with dyslipidemia, Helicobacter pylori infection-related chronic gastritis, hyperplastic gastric polyps, intestinal metaplasia, diabetes mellitus and synchronous or metachronous gastric cancer. We present a case of a 44-year-old female who presented GX without concomitant Helicobacter pylori infection.
Keywords Xanthelasma, Gastric Xanthoma, Helicobacter pylori
062
Comparative study of non-invasive C12 urea breath test with histopathology for diagnosis of Helicobacter pylori
Swati Rajput 1 , Prashant Chauhan 1 , Rohit Gupta 2 , Itish Patnaik 2 , Devna Chaudhary 1 , Kiran Meena 1 ,
Anissa Atif Mirza 1 , Satyavati Rana 1
Correspondence - Satyavati Rana - svrana25@hotmail.com
1Department of Biochemistry, and 2Gastroenterology, All India Institute of Medical Sciences, Rishikesh, Virbhadra Road Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Background and Aim More than 20 million Indians are estimated to suffer from peptic ulcer disease and H pylori infection. Though endoscopic biopsy with histopathological diagnosis of H pylori is the gold standard but remains an invasive cumbersome procedure. Radiolabeled C14- urea breath test is invasive and C13 urea breath test needs a costly instrument. Hence, this study is planned to compare and validate sensitivity and specificity of a non-invasive C12 urea breath test with gold standard detection of H pylori by histopathology in endoscopic gastric biopsies which is an invasive method.
Methods Ninety-seven adult patients with gastritis were enrolled. They were advised to stop proton pump inhibitors 2 weeks and antibiotics 4 weeks before the test. The non-invasive urea breath test was done using HELIC ABT Reader and reagent kits. On the same day, the gastric biopsy was taken during endoscopy for detection of H. pylori by histopathology. Special Warthin’s stain specific for H pylori detection was done. The sensitivity and specificity of the urea C12 breath test was calculated against Histopathology. Results were analyzed using SPSS version 22.
Results Out of 97 patients, 58 were males and 39 were females. Out of 97 patients, 27 patients were positive in both urea breath test and histopathology, 23 positives only in the urea breath test. Thus, 27 patients were true positive, 23 false positives, 47 true negatives, and 0 false negatives. The sensitivity and specificity of the urea breath test is 100% and 67.14% respectively with a positive predictive value of 54%, a negative predictive value of 100%, and an accuracy of 76.29%. This is interim data of an ongoing study.
Conclusion This study shows that a non-invasive urea breath test is 100% sensitive to detect H pylori. Therefore, it can replace invasive endoscopic histopathology for the detection of H pylori.
Keywords Urea breath test, H pylori, Histopathology
063
Low FODMAP diet versus traditional dietary advice for functional dyspepsia: A randomized controlled trial
Omesh Goyal1, Prerna Goyal2, Sahil Nohria1, Shveta Batta3, Ajit Sood1
Correspondence – Omesh Goyal - goyalomesh@yahoo.co.in
1Department of Gastroenterology and 3Dietetics, Dayanand Medical College and Hospital, Udham Singh Nagar, Civil Lines, Ludhiana 141 001, India, 2Department of Medicine, Baba Jaswant Singh College, 155, Bharat Nagar. Ludhiana 141 001, India
Introduction Functional dyspepsia (FD) is common worldwide. Prospective trials evaluating the efficacy of specific diet restrictions in FD are scarce. We aimed to assess the efficacy of low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) diet in FD, compared with traditional dietary advice (TDA).
Methods In this prospective, single-blind trial, patients with FD (Rome IV) were randomized into low FODMAP diet (LFD) and TDA groups, for 4 weeks (phase I). In phase II (4-12 weeks), the LFD group was advised systematic re-introduction of FODMAPs. Symptom severity and quality of life were assessed using ‘Short-Form Nepean Dyspepsia Index (SF-NDI)’. Primary outcome was the symptomatic response (symptom score reduction of ≥ 50%), at four weeks. The study was registered with CTRI (2019/06/019852).
Results Of 184 patients screened, 105 were randomized to LFD (n=54) and TDA (n=51) groups. At four weeks, both groups showed a significant reduction in SF-NDI symptom scores compared to baseline, with no significant difference in inter-group response rates (LFD- 66.7% [36/54], TDA - 56.9% [29/51]; p=0.32). On subgroup analysis, patients with postprandial distress syndrome or bloating had significantly better symptomatic response with LFD (p=0.04). SF-NDI quality of life scores improved significantly in both groups. On multivariate analysis, factors predicting response to LFD were bloating and male gender. Incidences of adverse events (minor) were similar in both groups.
Conclusions In patients with FD, both LFD and TDA lead to significant symptomatic and quality of life improvement. Patients with postprandial distress syndrome and/or bloating respond significantly better to LFD. Therefore, dietary advice for FD should be individualized according to the FD subtype.
Keywords Bloating, Epigastric pain syndrome, Functional
064
Quality of life in Indian patients with functional dyspepsia: translation and validation of the Hindi-version of Short-Form Nepean Dyspepsia Index
Prerna Goyal1, Omesh Goyal, Harsh Kishore, Jaskirat Kaul, Sahil Nohria, Ajit Sood
Correspondence – Omesh Goyal - goyalomesh@yahoo.co.in
1Department of Gastroenterology, Baba Jaswant Singh College, 155, Bharat Nagar, Ludhiana 141 001, India, and Department of Gastroenterology, Dayanand Medical College and Hospital, Tagore Nagar, Ludhiana 141 001, India
Introduction Patients with functional dyspepsia (FD) have poor health-related quality of life (HRQOL). Indian data on this subject is lacking. Also, there is non-availability of a validated disease-specific questionnaire to assess HRQOL in Hindi speaking dyspeptics. We aimed to develop and validate a reliable translation of the Short-Form Nepean Dyspepsia Index (SF-NDI) in Hindi and assess the impact of FD on HRQOL in Indian patients.
Methods Cross-cultural adaptation of English version of SF-NDI, translation to Hindi, and adaptation of Hindi version was performed using standard procedures. English and Hindi versions were assessed against SF-36, examining for internal consistency, test-retest reliability, and validity.
Results Total 211 FD patients (144 Hindi speaking, 67 English speaking) were enrolled (mean age 40.8 ±11.7 years; male: female=115:96). Median total SF-NDI scores for both languages were 38.75 and 40.0 respectively. Test-retest reliability intraclass correlation coefficients were 0.85 (Hindi) and 0.89 (English). Internal consistency evaluation revealed Cronbach’s α coefficient of 0.79- 0.86 (Hindi) and 0.78- 0.89 (English). SF-NDI sub-scales showed moderate to good correlation with various domains of SF-36 (content validity). There was a significant (p<0.001) decline of HRQOL for patients with severe dyspepsia relative to those with mild dyspepsia (construct validity). On multivariate analysis, factors independently associated with HRQOL were duration of symptoms and dyspepsia severity.
Conclusion Both English and Hindi versions of SF-NDI are reliable and valid for HRQOL assessment in Indian FD patients and will be useful in future epidemiological and clinical studies. Indian FD patients have poor HRQOL, being worse in those with severe dyspepsia and a longer duration of symptoms.
Keywords Epigastric pain syndrome, nausea, post-prandial distress syndrome
065
Gastric mucormycosis in post corona virus disease patients
Kamlesh Kumar Pravin Kumar, Ritesh Prajapati, Mayank Kabrawala, Raj Tandel
Correspondence - Kamlesh Kumar Pravin Kumar - kamlesh.magnani1234@gmail.com
Department of Gastroenterology, Surat Institute of Digestive Sciences, Vijay Nagar Gate No-3, Besides Nirman Bhavan, Majura Gate, Ring Road, Surat 395 002, India
Background Mucormycosis is a life-threatening disease. Rhinocerebral involvement is most common. Gastrointestinal (GI) involvement is uncommon of which stomach involvement is most common. We encountered 2 patients with post corona virus disease (COVID) gastric mucormycosis.
Case 1 A 73-year-old male presented with massive upper gastrointestinal bleed and shock. Patient was admitted 20 days back for COVID pneumonia and was treated with remdesivir, steroid and anticoagulants. During day 10 of COVID illness patient developed anterior wall myocardial infarction for which PTCA with drug eluting stent was placed and Aspirin, ticagrelor and dabigatran started. After hemodynamic stabilization, upper GI endoscopy was done which revealed large necrotic gastric ulcer, biopsy suggestive of mucormycosis. Patient was treated with liposomal amphotericin B. On day 6 patient rebled, repeat upper GI endoscopy revealed large gastric ulcer with visible vessels, hemostasis was achieved by hemoclip application. Reevaluation after 5 weeks showed clean based ulcer with granulation. Patient developed acute myocardial infarction on day 56 of GI bleed and succumbed to it.
Case 2 A 56-year-old male presented with massive upper gastrointestinal bleed and shock. Patient was admitted 1 month back for COVID pneumonia and was treated with remdesivir, steroid and anticoagulants. After hemodynamic stabilization, upper GI endoscopy was done which revealed large necrotic gastric ulcer, biopsy suggestive of mucormycosis. Patient was treated with Amphotericin B deoxycholate. On day 12 patient had large volume hemetmesis with hypotension, upper GI endoscopy showed active bleed from ulcer base and a visible vessel, was controlled with difficulty by injection adrenaline, gold probe coagulation, hemoclip application and coagulation of vessel head by coag-grasper. Follow-up upper GI endoscopy done after 1.5 months showed healing of ulcer, with healthy granulation tissue.
Conclusion Gastric mucormycosis can occur in post COVID setting if patients have received immunosuppressants. Early diagnosis and treatment may avoid surgery.
Keywords Post Covid gastric mucormycosis
066
A case of small vessel vasculitis (HSP) presenting with recurrent abdominal pain
Sandeep Kumar Reddy G
Correspondence - Sandeep Kumar G - sandeepgaddam02@gmail.com
Department of Gastroenterology, Madras Medical College, Near Park Town Station, Park Town, Chennai 600 003, India
Henoch–Schönlein purpura (HSP), also known as immunoglobulin A vasculitis (IgA) vasculitis, is a systemic vasculitis which is the most common vasculitis in children.
IgA vasculitis formerly called Henoch-Schönlein purpura (HSP) is the most common form of systemic vasculitis in children.
Ninety percent of cases occur in the pediatric age group.
In contrast to many other forms of systemic vasculitis, IgA V is self-limited in the great majority of cases. The disease is characterized by a tetrad of clinical manifestations:
? Palpable purpura in patients with neither thrombocytopenia nor coagulopathy
? Arthritis/arthralgia
? Abdominal pain
? Renal disease
The incidence in adults varies from 3.4 to 14.3 cases per million.
The classic triad of symptoms include purpuric rash, arthritis and abdominal pain.
First Description
Dr. William Heberden, a London physician, described the first cases of Henoch-Schönlein purpura (HSP) in 1801. In describing HSP, Heberden wrote of a 5-year-old boy who “…was seized with pains and swellings in various parts…He sometimes had pains in his belly with vomiting’s and the urine was tinged with blood. Presently, the skin of his leg was all over full of bloody points” (purpura). The young boy suffered all four disease hallmarks of HSP: arthritis, gastrointestinal involvement, kidney inflammation, and purpura. Johann Schönlein (1837) and Edouard Henoch (1874) reported additional cases decades after Heberden. They recognized that the disorder often followed upper respiratory tract infections and was not always self-limited, sometimes progressing to serious kidney involvement.
We present a case of a 45-year-old female with small vessel vasculitis (HSP) who presented with recurrent episodes of abdominal pain, followed by classical symptoms with an identified post-infectious etiology.
Keywords HSP; RASH; Abdominal pain
067
Comparative study of non-invasive C12 urea breath test with stool antigen test and histopathology for diagnosis of Helicobacter pylori
Swati Rajput1, Prashant Chauhan1, Rohit Gupta2, Itish Patnaik2, Devna Chaudhary1, Kiran Meena1, Anissa Atif Mirza1, Satyavati Rana1
Correspondence - Satyavati Rana - svrana25@hotmail.com
Departments of 1Biochemistry, and 2Gastroenterology, All India Institute of Medical Sciences, Virbhadra Road, Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Background and Aim Endoscopic biopsy with histopathological diagnosis of H. pylori is gold standard but remains an invasive procedure. Radiolabeled C14 urea breath test is invasive, and C13 urea breath test needs costly instrument. Hence, this study was planned to compare and validate sensitivity and specificity of non-invasive C12 urea breath test with stool antigen test and histopathology for H. pylori detection in endoscopic gastric biopsies which is an invasive method.
Methods Ninety-seven adult patients with gastritis were enrolled. They were advised to stop proton pump inhibitors 2 weeks and antibiotics 6 weeks before test. Non-invasive C12 urea breath test was done using HELIC ABT Reader. On same day, stool for antigen test by ELISA and gastric biopsy for H. pylori detection by histopathology were taken. Special Warthin’s stain specific for H. pylori detection was done. Sensitivity and specificity of C12 urea breath test was calculated against stool antigen test and histopathology of H. pylori. Results were analyzed using SPSS version 22.
Results Out of 97 patients, 58 were males. Twenty-seven patients out of 97 were positive in both urea breath test and histopathology, 23 positives only in urea breath test. Thus, 27 patients were true positive, 23 false positive, 47 true negative and 0 false negative. Sensitivity and specificity of urea breath test against histopathology is 100% and 67.14% with positive predictive value 54%, negative predictive value 100% and accuracy 76.29%. Sensitivity and specificity of urea breath test against stool antigen test is 100%. This is interim data of an ongoing study.
Conclusion This study shows that non-invasive urea breath test is 100% sensitive and specific to stool antigen test and 100% sensitive to detect H. pylori by histopathology. Therefore, it can replace invasive endoscopic histopathology and unpleasant stool antigen tests for detection of H. pylori.
Keywords Urea breath test, H. pylori, Histopathology
068
Efficacy and safety of levofloxacin based triple therapy as first line regimen to eradicate Helicobacter pylori infection: A single-center, prospective, open-labeled study
Saumyaleen Roy, Sanjeev Kumar Jha, Ravikant Kumar, Manjinder Singh
Correspondence - Sanjeev Kumar Jha - saumyaleenroy1987@gmail.com
Department of Gastroenterology, Indira Gandhi Institute of Medical Sciences, Bailey Road, Sheikhpura, Patna 800 014, India
Background Eradicating Helicobacter pylori (H. pylori) infection is challenging because of increasing prevalence of antibiotic-resistant H. pylori infection. There is scanty data in India that assessed the efficacy of levofloxacin containing regimen as first line therapy against H. pylori infection.
Aim of this study was to evaluate the efficacy and tolerability of a 2-week course of levofloxacin, amoxicillin and proton pump inhibitor (PAL regimen) as first-line treatment against H pylori infection.
Methods This was an open-label, prospective study. Patients with H. pylori infection were treated with amoxicillin (1000 mg twice daily), levofloxacin (500 mg once daily) and esomeprazole (40 mg twice daily) for 14 days. Eradication of H. pylori infection was assessed 4 - 6 weeks after completion of therapy. H. pylori eradication was assessed by either gastric biopsy or stool antigen assay. Treatment compliance and adverse effects were also evaluated.
Results Out of 131 patients who entered into study for final analysis, H. pylori eradication was achieved in 83.97%; 95% CI:78–90 (110 out of 131) patients in per protocol analysis and 81.48%; 95% CI:75-88 (110 out of 135) patients in intention to treat analysis. 98.5% patients were compliant to therapy. Adverse effects were reported in 18 %, mostly were mild in nature.
Conclusion PAL regimen as first-line therapy to eradicate H. pylori infection is found to be effective, compliant, and well tolerated. It could be used as alternative first line regimen especially in area of high dual clarithromycin and metronidazole resistance.
Keywords Helicobacter pylori, Levofloxacin, PAL Regimen, Eradication, First line therapy
069
Helicobacter pylori serology in patients of dyspepsia attending super speciality hospital
Arun Sharma, Vishal Sharma, Kaushal Kishore Prasad, Anupam Singh
Correspondence - Arun Sharma - arunsharma792001@yahoo.co.in
Department of Gastroenterology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Background Patients of dyspepsia may or may not be associated with Helicobacter pylori (H pylori) infection. H. pylori serology can be an important tool in screening patients of dyspepsia for H. pylori infection.
Method Seventy-five patients of dyspepsia and reflux attending Nehru Hospital, PGIMER, Chandigarh between December 1999 to March 2021 were included in the study. Three mL of their blood was collected, and serum stored at -20°C. All samples were tested uniformly for anti H. pylori IgG (Calbiotech, USA), anti H. pylori IgM (Eurofinns), anti H. pylori IgA (Eurofinns) and anti H. pylori cagA IgA (Dia. Pro, Italy) by ELISA.
Results Out of 75 patients of dyspepsia with reflux symptoms 38 (50.66%, 38/75) were reactive for anti H. pylori IgG. 21 (28%, 21/75) out of 75 dyspeptic patients were reactive for anti H. pylori IgM. These patients of dyspepsia were also reactive for anti H. pylori IgA in 14 patients (18.66%, 14/75). However, only 5 patients (6.66%, 5/75) of dyspepsia were reactive for anti H. pylori cagA IgA by ELISA.
Conclusion 50.77% patients of dyspepsia with reflux are associated with H. pylori infection by detecting anti H. pylori IgG by serology. Detection of anti H. pylori IgM and anti H. pylori IgA were less relevant compared to detection by anti H. pylori IgG for association of H. pylori infection in dyspeptic patients.
Keywords H. pylori, Anti H. pylori IgG, Anti H. pylori IgM, Anti H. pylori IgA
070
First case report of combination of gastric xanthelasma, Helicobacter pylori gastritis with pernicious anemia
Apurva Shah, Maitrey Patel, Aastha Jha, Shravan Bohra
Correspondence – Apurva Shah - apurvashah411@gmail.com
Department of Medical Gastroenterology, Apollo Hospital International Limited, Plot No. 1A, Gandhinagar, Ahmedabad Road, GIDC Bhat, Ahmedabad 382 428, India
Gastric Xanthelasma (GX) is an incidentally diagnosed yellowish whitish plaque like lesion during endoscopy and microscopically formed by clusters of foamy macrophages in lamina propria. Etiology of GX is unclear, but it has been suggested to be involved in chronic gastritis, infection with Helicobacter pylori (H. pylori), diabetes mellitus, and hyperlipidemia. Xanthelasmas are associated with chronic gastritis, gastrointestinal anastomosis, intestinal metaplasia, and H. pylori infection and these lesions predispose to gastric cancer. We report a case of 49-year-old male patient who was presented with severe anemia . Investigations (Table 1) showed severe macrocytic anemia, thrombocytopenia, and indirect hyperbilirubinemia along with very low B12 levels with normal lipid profile. Anti-parietal cell antibody was strongly positive. He was diagnosed as pernicious anemia and on evaluation found to have GX, chronic atrophic gastritis and rapid urease test for H. pylori positive during upper GI endoscopy (Fig.1). Patient was given IM Vitamin B12 (1000 microgm daily for 5 days followed by weekly 1000 microgm) for 1 month with H. pylori eradication treatment for 2 weeks. On follow-up after one month patient improved symptomatically and reports (Table 1) showed Hb 12.9 gm/dL, WBC count 7611/cumm, platelet 2.7 x 106/cumm and bilirubin 0.6 mg/dL. GX is a novel predictive marker for early gastric cancer detected after H. pylori eradication. In literature direct correlation between pernicious anemia and GX is not mentioned. Even though GX being benign condition once detected; it is necessary to search for accompanying premalignant conditions, histological confirmation and regular follow-up is advised if high risk for malignancy.
Keywords Gastric Xanthelasma, Pre malignant, Pernicious anemia, H. pylori
071
Relation between gut microbiota and Helicobacter pylori status in gastroduodenal diseases
Shravani M Phatak , Prateek Sharma, Shweta Mahant, Kunak Das1, Rajashree Das
Correspondence – Rajashree Das - rdas@amity.edu
Amity Institute of Biotechnology, Amity University, Noida Amity Road, Sector 125, Noida, 201 301, India, and 1Department of Gastroenterology, Manipal Hospital, Palam Vihar, Sector 6, Dwarka, New Delhi 110 075, India
Introduction Microbiomes have been known to inhabit the human gut since time immemorial. While some are beneficial for us, others may in turn cause gastroduodenal diseases. The aim of this study was to find out abundance of gut microbiota in various gastroduodenal diseases in accordance with HP (Helicobacter pylori) status.
Methods In this study, raw data from 15 participants which underwent proper physical examination, was obtained having GERD, gastritis and duodenal ulcer (DU). Using urease PCR test, the data was categorized as HP (+ and -) and 16S rRNA gene sequencing was done for meta-analysis. Finally, library preparation and quality purified read was obtained data was analyzed for results.
Results At phylum level, for HP (+) among DU and gastritis patients, proteobacteria (87.2 % and 72.6 %, respectively) had highest abundance followed by firmicutes (6.7% and 14.2 %, respectively), whereas, in GERD, firmicutes (41.01%) had a dominance followed by proteobacteria (23.6%). On the other hand, in HP (-) category, Proteobacteria was dominant in all three diseases i.e. GERD, DU, gastritis (94.2%, 46.8% and 63.25%, respectively) trailed by firmicutes in GERD, DU, gastritis participants (2.68%, 21.03%, 24.94% respectively). Thermi (0.85%) phyla were abundant only in DU participants having HP (+). At species level, H. pylori was the most abundant in all categories (GERD= 32.31%; DU= 89.44% and gastritis= 86.54%), whereas in HP (-), Helicobacter pullorum was dominantly abundant in GERD and gastritis (44.9% and 23.9% respectively) and Corynebacterium sp. (24.5%) had higher rate in DU.
Conclusion As clearly evident, there exists a symbiotic relation between gut microbiota and HP status in the host. According to the analyses, proteobacteria has the most abundance in the diseases considered, regardless of HP status.
Keywords Microbiome, Gastro duodenal diseases, Helicobacter pylori
072
White light endoscopic findings of gastric and duodenal mucosa in Helicobacter pylori infected patients: Cross sectional observational study in a tertiary hospital of south India
Debapratim Routh , A Chezhian
Correspondence - Debapratim Routh - debapratimraja@gmail.com
Institute of Medical Gastroenterology, Madras Medical College, Near Park Town Station, Park Town, Chennai 600 003, India
Background and Aims Helicobacter pylori (H. pylori) infection causes variety of upper gastrointestinal tract diseases. Successful eradication can prevent H. pylori associated diseases. H. pylori infection can be diagnosed by various non-invasive tests, but they have some limitations including high false negative results. Now a days endoscopy plays an important role for diagnosis of various gastric and duodenal lesions. This paper provides preliminary study on endoscopic features associated with H. pylori infection in gastric and duodenal mucosa.
Methods It is a cross sectional observational study carried out from April 2021 to September 2021 at Medical Gastroenterology Department of Madras Medical College. Total, 200 biopsy proven for H. pylori, patients were enrolled for endoscopic correlation. Endoscopic images of stomach and duodenum were recorded and biopsy specimens were collected as per Sydney protocol, stained by H-E staining and examined using a light microscope.
Results After proper evaluation as per inclusion and exclusion criteria total 100 patients (55 male and 45 female, 40 patients above 40 year of age and 60 patients were below 40 years) were diagnosed H. pylori by biopsy and were correlated with endoscopic findings. Most common endoscopic finding was spotty redness (38.5%) followed by enlarged gastric mucosal fold (20.5%), least common findings are erosions (2%) and multiple dots (1%).
Conclusion This finding may aid cost effective management of H. pylori infection. But additional studies with larger sample sizes and more diverse populations are required to establish the association of endoscopic features with H. pylori infection.
Keywords Helicobacter pylori, Endoscopy, Biopsy
073
Effect on gut microbiota due to lifestyle factors and gastrointestinal disease, among the north Indian patients
Prateek Sharma, Prisha Warikoo, Shweta Mahant, Kunal Das1, Rajashree Das
Correspondence – Rajashree Das - rdas@amity.edu
Amity Institute of Biotechnology, Amity University, Noida Amity Road, Sector 125, Noida 201 301, India, and 1Department of Gastroenterology, Manipal Hospital, Palam Vihar, Sector 6, Dwarka, New Delhi 110 075, India
Introduction Various lifestyle factors, including diet, age, alcohol and gastrointestinal diseases status have individually been proven to alter the host’s gut microbial, in an increasing number of studies, and have been separately linked to various diseases. However, studies examining the influence of the microbiome of patients in North India considering multiple factors, are scarce. Hence this research effort is directed towards lessening that gap, by examining on the basis of diet, the overlap of age, alcohol, and gastrointestinal disease.
Methodology Human tissue biopsy samples of 19 individuals were collected in which 13 were non-vegetarian, 6 vegetarian, three alcoholic, 16 non-alcoholic, 8 with gastroesophageal reflux disease (GERD), 5 duodenal ulcer (DU) patients and 5 with gastritis. 16s rRNA was then used to analyze the samples as well as library quality and sequencing.
Results It was found that, across all lifestyle factors, Prevotella Melaninogenica, belonging to the phylum Proteobacteria was present in the top 10 species in omnivores, barring those that drank alcohol. In vegetarians, Corynebacterium sp., was highly abundant across all factors, with its phylum Actinobacteria being in the top three, except for in DU samples, and Hemophilus parainfluenzae (Proteobacteria), also one of the ten most abundant species. The only time there was an obvious similarity in the microbial composition of the two diets was in the alcoholics, where Streptococcus sp. was found to be most abundant in omnivores (18.10%), and second most abundant in vegetarians (14.01%).
Conclusions Streptococcus sp. also causes gastric degradation, indicating that despite diet influencing the health of the host, an alcoholic host will majorly face the same repercussions. Prevotella Melaninogenica was also mainly high in omnivores and has been linked to an increase in gastric cancer risk.
Keywords Gastrointestinal disease, Dietary status, Gut microbiome
074
Isolated gastric Crohn’s disease with pyloric stenosis – An unusual initial presentation
Shanky Koul , V Arul Selvan, P Senthil Kumar, A Senthil Vadivu, T Ravishankar
Correspondence - Shanky Koul - shanky.doctor2006@gmail.com
Department of Medical Gastroenterology, Coimbatore Medical College Hospital, Avinashi Road, Peelamedu, Civil Aerodrome Post, Coimbatore 641 018. India
Introduction Crohn’s disease (CD) is a heterogeneous disorder with multifactorial etiology, including genetic factors, environmental insults, and intestinal microbiota, characterized by chronic, segmental and trans mural inflammation that affects the gastrointestinal tract and may involve any segment of the oral cavity up to anus. Isolated stomach involvement is very unusual presentation accounting for less than 0.7% of all gastrointestinal Crohn's disease.
Case A 17-year-old male presented to our department with recurrent postprandial vomiting, epigastric discomfort, and unintentional weight loss over 3 months. No history of any bleed, fever, loose stools, cough, or jaundice.
Per abdomen – mild epigastric tenderness. Per rectal examination – normal.
Investigations CBC – microcytic hypochromic anemia, RFT, LFT, S. amylase, viral markers, Erect AXR, CXR – normal.
CECT abdomen – no abnormality detected.
UGI endoscopy – Circumferential nodulo-ulcerative mass seen in antro-pyloric region with narrowing of pyloro-duodenal opening. Histopathological examination of biopsy from the lesion revealed non-caseating granuloma with superficial ulceration.
Colonoscopy revealed normal colon up to 15 cms of terminal ileum. CT enterography was normal tuberculosis, H. pylori and sarcoidoses were excluded by appropriate investigations, and a diagnosis of gastric Crohn’s disease was made.
Patient underwent CRE balloon dilation of the pylorus and was put on oral steroids and azathioprine for maintenance. Patient showed remarkable response at 8-week follow-up with complete resolution of symptoms and started to gain weight as well.
Conclusion Symptoms of pyloric obstruction as a manifestation of isolated gastric Crohn’s disease are extremely unusual in clinical practice, awareness of which would facilitate early appropriate investigations and treatment. Balloon dilatation followed by oral steroids and immunomodulators is an effective way to manage such cases.
Keywords Gastric Crohn’s, Balloon dilatation, Steroids
075
High prevalence of virulent Helicobacter pylori with low clarithromycin resistance in patients with dyspepsia from Odisha
Vinaykumar Hallur1, Manas Panigrahi2, Mukund Sable3, Manaswini Ghosh1, Srujana Mohanty1, Suvendu Purkait2, Ashok Praharaj1
Correspondence - Vinaykumar Hallur - vinay118@gmail.com
Departments of 1Microbiology, 2Gastroenterology, and 3Pathology, All India Institute of Medical Sciences, Sijua, Patrapada, Bhubaneswar 751 019, India
Background The outcome of Helicobacter pylori (HP) infection depends at least partly virulence factors and its eradication as preventive measure against gastric cancer has been advocated by some guidelines. Universal eradication or use of failing antibiotic can add fuel to the antimicrobial resistance pandemic. Hence, there is need to identify candidates at risk for gastric cancer and antimicrobial resistance in HP for rational management. Such candidates could be identified by studying the association of virulence factors with clinical outcome. As this data is lacking from Odisha, India this study was undertaken.
Methods One hundred and thirteen consecutive dyspeptic patients attending our centre were subjected to endoscopy to obtain tissue which was subjected to culture and antibiotic susceptibility, histological examination, molecular detection of HP, virulence typing (cagA, EPIYA typing, vacA, vacA s1/s2, vacA m1/m2 and babA2) by conventional PCR and identification of clarithromycin resistance by real time PCR. Cultures isolates were subjected to antibiotic sensitivity using e strips as per EUCAST guidelines.
Results Ninety-three (83%) dyspeptic patients were infected by HP by histology and PCR. Sixty-two (66.7%), 87 (93.5%) and 43 (46.2%) of these patients harboured HP with CagA, VacA and babA2 genes. The western cagA found in 33 (53.2%) samples and vacA s1m1 in 50 (53.8%) samples were the commonest virulence subtypes. No association was found between virulence factors and outcome except vacA S2M2 which was significantly associated with peptic ulcer. Eleven (11.8%) of the 93 samples with HP were resistant to clarithromycin by real time PCR. HP was isolated from 32 (34.4%) of these patients. Phenotypically 11 (36.7%), 1 (3.3%), 21 (70%) and 26 (86.7%) isolates were resistant to clarithromycin, amoxicillin, levofloxacin, and metronidazole.
Conclusions This is the first study that explored the antibiotic resistance of HP, its virulence factors, and in dyspeptic patients from this region of India.
Keywords Helicobacter pylori, Dyspepsia, Antimicrobial resistance, Clarithromycin resistance, PCR
076
A gastric strongyloidiasis an unusual cause presenting with weight loss
Amol Vadgaonkar, Gaurav Patil, Amit Maydeo
Correspondence - Amol Vadgaonkar - vadu169@gmail.com
Department of Gastroenterology, Baldota Institute of Digestive Sciences, Global Hospital, Opposite Shirodkar High School, Ernest Borges Road, Lower Parel, Mumbai 400 012, India
Introduction Eosinophilia can arise due to numerous conditions including allergy and infections. It can also be an incidental finding; but identification and assessment of associated organ is essential.
The case A 55-year-old male presented with loss of appetite, vomiting, heartburn and unexplained weight loss since two months. His laboratory parameters for blood counts, renal function test and liver parameters were normal except for low albumin (1.9 g/dL) and eosinophilia (900/μL). His stool occult blood was positive. Esophagogastroduodenoscopy (EGD) showed mild erythema (antrum), pyloroduodenal ulceration with exudates. Rapid urease test for H. pylori was positive. Colonoscopy showed diverticuli in sigmoid and descending colon with inflammatory patches in terminal ileum, cecum and descending colon. Biopsy showed moderate ileitis and nonspecific colitis. Gene expert was negative for mycobacterium tuberculosis. Biopsy specimen of pylorus epithelial lining showed few parasites of Strongyloides stercoralis. He was initially prescribed anti-H pylori therapy, fexofenadine, esomeprazole, probiotics, multivitamin, and advised to consume protein rich diet. At follow-up (2 weeks), patient was treated with Ivermectin 12 mg once a week for 2 weeks. Patient was advised to wear shoes to avoid contact with infected soil in endemic areas. The patient responded well to treatment, a follow up EGD (4 months) revealed no significant ulcers in the stomach, and stool culture was negative.
Discussion Strongyloidiasis is a parasitic infection that can present with nonspecific symptoms and is difficult to eradicate. Definitive therapy is possible when infection is established. Clinicians should carefully consider the possibility of such infection in stomach.
Keywords Strongyloides stercoralis, Stomach, Eosinophilia, Weight loss
077
Comparison of the efficacies of standard triple, sequential and quadruple antibiotic therapy in eradicating Helicobacter pylori infection: A randomized controlled trial
Mohd Imran Chouhan 1 , Manas Kumar Panigrahi 1 , Vinay Hallur 2 , Chandan Kumar 1 , Subash Chandra Samal 1 , Biswa Mohan Padhy 3
Correspondence - Manas Kumar Panigrahi - manaskumarpanigrahi@gmail.com
Departments of 1Gastroenterology, 2Microbiology, and 3Pharmacology, All India Institute of Medical Sciences, Sijua, Patrapada, Bhubaneswar 751 019, India
Introduction There is regional variation in the eradication rates of Helicobacter pylori (H. pylori) regimens depending on the local antibiotic resistance patterns. Data from Odisha, where prevalence of H. pylori and peptic ulcer disease is still high is lacking. The aim of this study was to compare the efficacies of standard triple therapy, sequential therapy, and quadruple therapy in eradicating Helicobacter pylori infection in this region.
Methods A total of 304 H. pylori positive patients were randomized to receive one of the three regimens (standard triple therapy [n=102], sequential therapy [n=101] or quadruple therapy [n=101]). Eradication rate was assessed by H. pylori stool antigen test.
Results Seventy-one, seventy-one and sixty-nine patients completed the follow-up in the standard triple therapy group, sequential therapy group and quadruple therapy group respectively. The eradication rates of standard triple therapy, sequential therapy, and quadruple therapy was 93%, 94.4%, and 97.8%, respectively.
Conclusion Fourteen days of standard triple therapy, ten days of sequential therapy and fourteen days of bismuth-based quadruple therapy are equally efficacious in eradicating H. pylori and all the regimens have optimum H. pylori eradication rates in this part of India.
Keywords H. pylori, Eradication rate, Dyspepsia
078
Redox perturbations of human gastric mucosa influence gastric microbiome in chronic gastritis
Manas Kumar Panigrahi1, Venkatesh Kaliaperumal Kaliaperumal, Abhishek Akella3, Giriprasad Venugopal3, Sudhanshubala Lenka4, Balamurugan Ramadass4
Correspondence - Manas Panigrahi - manaskumarpanigrahi@gmail.com
Departments of 1Gastroenterology, 3CCMR Center of Excellence for Clinical Microbiome Research, 4Biochemistry, All India institute of Medical Sciences, Sijua, Patrapada, Bhubaneswar 751 019, India, 2Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education and Research, Dhanvantri Nagar, Gorimedu, Puducherry 605 006, India
Introduction Gastric microbial composition may be influenced by redox perturbations where microbiome may be a passive bystander or induce oxidative stress and related pathology, like H. pylori. We aim to decipher microbial signatures of redox perturbation for the quantitative assessment of mucosal health.
Methods Gastric mucosal tissue biopsy is obtained from 10 peptic ulcer and 10 non-ulcer dyspepsia patients and subjected to 16s RNA gene sequencing. Using abundance correlation mapping, a microbial redox spectrum is deduced based on oxygen requirement/tolerance and the presence of the enzymes catalase (Cat) and oxidase (Ox). A simple redox index of mucosal health based on top two predominant Ox+, Cat+ aerobes and Ox–, Cat– anaerobes is conceived.
Results The oxidative end of redox spectrum was populated by Ox+, Cat+ aerobes namely, H. pylori, S. mizutaii and T. fusca. These three species had an inverse correlation with the abundance of anaerobes and Ox–, Cat+ aerobes. The abundance of most of the anaerobes was positively correlated with each other except for the aerotolerant Clostridium intestinale. The ratio of the top two Ox+, Cat+ aerobes (H. pylori, S. mizutaii) and top two Ox–, Cat– anaerobes correlated with the tissue oxidation-reduction potential (ORP), Shannon and Species richness indices.
Conclusion This study envisages at-least five discrete categories of bacteria along the redox spectrum. The approach described herein may be useful as a widely applicable quantitative measure of mucosal health with prognostic and therapeutic implications. In addition, a comprehensive understanding of the microbial community from a redox perspective will enable targeted/personalized prebiotic and probiotic interventions.
Keywords Dyspepsia, Gastric microbiome, H. Pylori, Probiotic
079
Gastritis cystic profunda in an unoperated stomach: A malignancy mimicker
Ramya Mamidipalli, R S Arun, Nageswara Rao
Correspondence - Ramya Mamidipalli - ramya.mamidipalli27@gmail.com
Department of Medical Gastroenterology, Madras Medical Mission Hospital, 4-A, Dr, Mogappair, Chennai 600 037, India
Introduction Gastritis cystic profunda (GCP) is a rare condition characterised by presence of cystic dilatation of gastric glands in basal mucosa and submucosa of the stomach. It commonly occurs in patients with history of gastric surgery at gastroenterostomy sites. Few case reports have noted its development in an unoperated stomach as well. Here we report a case of GCP in a patient who had not undergone any gastric surgery.
A78-year-old gentleman presented with complaints of anorexia, weight loss of 4 kgs since 2 weeks and non-bilious vomiting since 10 days. Past medical history was unremarkable. He had no history of gastric surgery. Upper GI endoscopy revealed a thickened nodular lesion with irregular surface 2 x 1.5 cms in the body of the stomach along the greater curvature. Histopathological examination of the lesion revealed multiple dilated cystic gastric glands lying in the deeper mucosa and between distorted muscularis mucosae fibres with no evidence of dysplasia.
Review of literature GCP is considered a benign lesion. GCP may present as elevated lesions in gastroscopy and should be differentiated from early gastric cancers. Most cases of GCP in an unoperated stomach are secondary to changes caused by prolonged chronic inflammation and ischemia. Injury to the muscularis mucosae caused by gastric surgery or suturing material is assumed to trigger the ectopic entrapment of gastric glands in the basal mucosa and submucosa.
Keywords Gastritis cystic profunda, Gastric cancer
080
Comparison of serum lactic acid and urea-creatinine ratio with Rockall, Glasgow-Blatchford and AIMS65 score in risk stratification of patients with acute upper gastrointestinal hemorrhage - Prospective cohort study
Anto Delasalle , Bailuru Vishwanath Tantry, Sandeep Gopal, Suresh Shenoy, Anurag J
Shetty
Correspondence – Anto Delasalle - anto19893@gmail.com
Department of Medical Gastroenterology, Kasturba Medical College Hospital, Manipal Academy of Higher Education, Mangalore 575 001, India
Introduction Upper gastrointestinal (UGI) bleeding is a common emergency requiring admission to the intensive care unit. A number of clinical scores have been developed to aid in the prediction of mortality risk. In this study we evaluated the role of serum lactic acid and urea-creatinine ratio (UCR) in risk stratification of patients.
Methods This was a prospective observational study conducted on 70 patients with UGI bleed over a period of 18 months. At admission, baseline blood investigations included measurement of serum lactate levels, and calculation of UCR, Glasgow-Blatchford Score (GBS), Rockall and AIMS65 scores. These were correlated with the primary (inpatient and thirty-day mortality) and secondary outcomes (need for ICU stay, requirement of blood transfusion, re-bleeding and need for endoscopic/surgical/radiological interventions).
Results In this study the mortality rate was found to be 11.4% (8 patients). Mean lactate levels were significantly higher in the non-survivor group (91.61 mg/dL) in comparison to the survivors (32.96 mg/dL). Elevated lactate levels (>40 mg/dL) was found to be a better predictor of mortality (area under ROC curve 0.85, p<0.0.1), when compared to Rockall, GBS and AIMS65 scores with a sensitivity of 90% and a specificity of 79%. However, UCR was a poor predictor of mortality. On analysis of secondary outcomes, a serum lactate of >40 mg/dL at admission was associated with increased length of ICU stay (3.06 days, p<0.01), increased requirement of blood transfusions (2.63 units, p–0.01), increased requirement of inotropic support and endoscopic interventions. UCR was not found to have any significant association.
Conclusion Our study shows that serum lactate levels is useful in predicting in-hospital and thirty-day mortality in patients with UGI bleed. However, UCR showed no similar benefit. Lactate levels can be incorporated into the existing risk stratification scores for better prediction and timely intervention, in patients with UGI bleed.
Keywords Gastrointestinal hemorrhage, Lactic acid, Urea, Creatinine
081
Primary gastric mucormycosis presenting as post corona virus disease 2019 gastrointestinal bleed: A case report
Sayan Malakar , Anshuman Elehence, Uday C Ghoshal, Gaurav Pande, Srikanth Kothalkar, Samir Mohindra
Correspondence – Samir Mohindra - mohindrasamir@yahoo.com
Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014, India
Corona virus disease 2019 (COVID-19) pandemic has affected more than 2.5 billion people claiming more than 5 million lives worldwide. During the second wave of this pandemic in India nasopharyngeal mucormycosis was found to complicate the disease however mucormycosis of the gut has been rarely reported. We present a case of gastric mucormycosis in an 82-year-old gentleman who presented with a massive post-covid upper gastrointestinal (UGI) bleed. He was initially diagnosed with moderate COVID-19 and was treated with oral prednisolone for 21 days. One month after he recovered from COVID-19 pneumonia he presented to us with a massive UGI bleed. His UGI endoscopy was suggestive 7.8 cm large gastric ulcer extending from the gastroesophageal junction. Biopsy showed largely ulcerated stomach mucosa with necrotic debris containing Periodic Acid Schiff positive fungal hyphae suggestive of mucormycosis. Contrast-enhanced computed tomography of the abdomen was also consistent with the diagnosis. He was planned for surgery but because of his age, he denied surgery and was managed conservatively with intravenous pantoprazole infusion and amphotericin B. After the initial 13 days, because of worsening renal function amphotericin B was stopped and he was started on posaconazole which was continued for 3 months. On follow-up endoscopy, his ulcer healed and subsequently resolved after 3 months. Gastric mucormycosis is a rare but potentially lethal fungal infection with mortality of up to 54% in immunocompromised patients. Most of the literature suggests early anti-fungal with surgical debridement or gastrectomy for gastric mucormycosis with necrosis, angio-invasion, or extensive disease. This is a rare case of mucormycosis. Our patient highlights an unusual cause of post-COVID GI bleed which was successfully managed with antifungal therapy only despite having a large necrotic ulcer. Awareness of this complication is essential for its early diagnosis and appropriate management.
Keywords COVID-19 pandemic, Covid Asscociated Mucormycosis, Upper GI bleed, Gastric mucormycosis
082
Spectrum of primary gastric lymphoma in India: A series of thirty patients
Akash Mathur 1 , Uday C Ghoshal 1 , Sushil Kumar 2 . Neeraj Kumari 2 , Narendra Krishnani 2
Correspondence – Uday C Ghoshal - udayghoshal@gmail.com
Departments of 1Gastroenterology, and 2Pathology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014, India
Primary gastric lymphoma (PGL) is uncommonly reported from India. Since gastric neoplasm (GN) is a relatively less common in northern India, PGL is also considered uncommon. During a 12-y period (2000-2012), data of GN in a teaching institute were retrospectively analyzed to know (i) the frequency of PGL among patients with GN, (ii) its clinical profile, (iii) the diagnostic procedures needed, and (iv) frequency of Helicobacter pylori (H. pylori) among them. 30/324 (9.2%) patients (age 56-y, range 25-72, 73.3% male) with GN had PGL. Forty percent had H. pylori infection (2/3 tests positive). Presentations included dyspepsia (9, 30%), gastric outlet obstruction (n=7, 23.3%), upper gastrointestinal bleeding (n=5, 16.7%), dysphagia (n=4, 13.3%), malignant ascites (n=3, 10%) and other (n=2, 6.7%). H. pylori infection was present in seven (23.3%), twelve (40%), and 21/29 (72.4%) patients by RUT and histopathology, and positive anti-H. pylori IgG serology, respectively. Using any two of three test positive criteria, H. pylori was detected in 12 (40%) patients. Though in 60% PGL was diagnosed on endoscopic biopsy, in 40%, surgical resection was required. The endoscopic and surgical diagnosis groups were comparable in age (53.4-y vs. 52.7-y), sex (male 77.8% vs. 66.7%), H. pylori infection (38.9 vs. 16.7%), presentation with dyspepsia (38.9 vs. 16.7%), organic symptoms (61.1 vs. 83.3%) and need for repeated endoscopic biopsies before diagnosis (12.5 vs. 33.3%). We conclude that PGL is not uncommon (9.2%) in India, often missed on endoscopic biopsy and is associated with H. pylori infection (40%).
Keywords Gastrointestinal lymphoma, Helicobacter pylori, Gastric cancer, Chronic gastritis, Dyspepsia
083
A rare case of primary gastric actinomycosis – Guided by endoscopic ultrasound
Kondal Reddy Mogili 1 , Rakesh Kumar Adi 2 , Jyoti P Dekate 3
Correspondence – Kondal Red dy Mogili – kondal14r@gmail.com
Departments of 1Medical Gastroenterology, and 3Histopathology, Gleneagles Global Hospital, Lakdi-ka-pul, Hyderabad 500 004, India, and 2Department of Medical Gastroenterology, Yashoda Hospital, Alexander Road, Kummari Guda, Shivaji Nagar, Secunderabad 500 003, India
Introduction Primary gastric actinomycosis is a rare, chronic, progressive, suppurative disease characterized by formation of multiple abscesses, draining sinuses, and abundant granulation and dense fibrous tissue [1]. It should be considered in the differential diagnosis of radiologic and gastroscopic diffuse gastric wall thickening and submucosal tumor-like or infiltrative lesions, particularly in patients with history of abdominal surgery or trauma. A high level of suspicion is needed for diagnosis. The presence of sulfur granules strongly suggests a diagnosis but not pathognomonic for the disease [2-4].
Methods A 52-year-old female presented with severe abdominal pain for 5 days with no medical comorbidities. No history of abdominal trauma. History of tubectomy 32 years ago and hysterectomy 17 years ago. Gastroscopy showed antral ulcer with edematous mucosa. Mucosal biopsy suggestive of chronic nonspecific gastritis with focal ulceration. Contrast enhanced computed tomography (CECT) abdomen showed ill-defined heterogeneously enhancing exophytic soft tissue lesion approximately 4.2 x 3.5 x 3.3 cm seen arising from antrum of stomach. Mild circumferential wall thickening seen in involved segment of antrum. Inflammatory changes seen in surrounding fat.
Results On Endoscopic ultrasound (EUS) evaluation there is well defined lesion measuring 2.9 x 2.3 cm in antrum of stomach no active doppler uptake. No lymphadenopathy. Based on radiologic and gastroscopic findings, a non-infectious etiology was suspected. EUS guided fine needle aspiration (FNA) from stomach lesion on Hematoxylin and Eosin-stained slide showing basophilic filamentous organism with adjacent neutrophilic inflammation and Gomori Methenamine silver (GMS) stain showing silver positivity morphologically consistent with Actinomyces. She was treated conservatively with long duration of penicillin antibiotic.
Conclusion EUS can aid in taking biopsies for histological evaluation to avoid morbidity and mortality due to unnecessary surgery, usually as most cases were diagnosed in post-surgical resection specimens.
Keywords Actinomycosis, Endoscopic ultrasound, Primary gastric
Small intestine
084
Prevalence of SIBO in IBS-D patients and role of rifaximin in the management
Rakesh Garlapati , Nirdesh Chauhan, Venkata Ranga Reddy
Correspondence – Nirdesh Chauhan – drnirdesh@live.in
Department of Gastroenterology, Kurnool Medical College, Near, Bhudawarapet Bharath Petroleum, Kisan Ghat Road, Kurnool 518 003, India
Introduction Irritable bowel syndrome (IBS) is characterized by the presence of abdominal pain associated with altered bowel movement. There is a paradigm shift from Brain-Gut axis disorder, as previously thought, to Gut-Brain axis disorder, which has shown increased importance to gut dysbiosis, including small intestinal bacterial overgrowth (SIBO). SIBO can be diagnosed as the presence of excess bacteria (either quantitative [>105 cfu/mL] or qualitative [excess bacteria of colonic origin] in the small intestine accompanied by intestinal or extraintestinal symptoms thought to result from this excess. The gold standard test for SIBO has customarily been considered the quantitative culture of a jejunal aspirate. This, however, is invasive and costly as it generally requires endoscopy for sample collection. Glucose hydrogen breath test (GHBT) is a reliable test to diagnose SIBO with about 80% to 100% specificity and 40% sensitivity.
Method This study was done in the Department of Gastroenterology, Kurnool Medical College, Kurnool, to find the prevalence of SIBO in irritable bowel syndrome with diarrhea (IBS-D) patients by using the GHBT (LactoFAN2*) and response to Rifaximin. Eighty diagnosed cases of IBS-D (using ROME IV criteria) were subjected to GHBT using 100 g of glucose in 250 mL water and breath samples were taken at baseline and at 20 min interval for 2 hours. A hydrogen increase of ≥12 parts per million (ppm) over baseline is considered diagnostic of SIBO.
Results Out of 80 patients, only 18 were positive for SIBO and were treated with rifaximin. After 14 days, out of 18 patients, only 15 showed clinical improvement and repeat GHBT in these 15 patients was also negative.
Conclusion The prevalence of SIBO in IBS-D patients is 22.5% using GHBT and use of rifaximin, was associated with good clinical response in treating SIBO in IBS-D patients.
Keywords IBS, SIBO, Rifaximin, GHBT
085
Correlation between magnetic resonance enterography and ileo-colonoscopy for assessment of disease activity in terminal ileal Crohn’s disease
Arshdeep Singh 1 , Chandan Kakkar 2 , Ramit Mahajan 1 , Vandana Medha 3 , Shriya Goyal 1 , Namita Bansal 4
Correspondence – Ajit Sood – ajitsood10@gmail.com
1Departments of Gastroenterology, 2Radiology, 3Medicine, and 4Research and Development, Dayanand Medical College and Hospital Tagore Nagar Civil Lines, Ludhiana 141 001, India
Background Magnetic resonance enterography (MRE) has emerged as a novel tool for assessment of disease activity in Crohn’s disease (CD). Real world data on performance of MRE in terminal ileal CD are lacking.
Methods Retrospective analysis of patients with terminal ileal CD who underwent both ileo-colonoscopy and MRE was performed. Ileo-colonoscopy was considered as gold standard for assessment of disease activity. On ileo-colonoscopy, a simple endoscopic score for Crohn’s disease (SES-CD) ≥2 was considered as active disease; presence of ulcers indicated severe disease. MRE scoring of the disease activity was performed using magnetic resonance index of activity (MARIA) and simplified MARIA (MARIAs). The measure of agreement between ileo-colonoscopy and MRE, comparison of MARIA and MARIAs for assessment of disease activity and sensitivity of MRE to detect mucosal ulcerations were calculated.
Results Seventy patients with terminal ileal CD (mean age 40.74±15.56 years; 71.4% males [n=50]) were evaluated. The sensitivities of MARIA and MARIAs scores to detect active disease were 0.76 and 0.84 respectively. The AUROC for detecting severe disease was 0.836 (p<0.0001) for MARIA and 0.861 (p<0.0001) for MARIAs. For mild active disease, there was no agreement between SES-CD and MARIA or MARIAs, however for severe disease, the agreement was fair and moderate for MARIA and MARIAs respectively. MARIA and MARIAs were comparable for identification of active and severe disease (κ 0.759, p<0.0001 and κ 0.840, p<0.0001 respectively). MRE was 68.18% sensitive to detect mucosal ulcers.
Conclusion MRE is a reliable and sensitive tool for detection of endoscopically severe, but not mild, terminal ileal CD.
Keywords Colonoscopy, Crohn’s disease, Magnetic resonance imaging
086
Diagnostic yield of routine duodenal biopsy for suspected celiac disease in a tertiary care centre in south India (Tamil Nadu)
Vikranth Chunduri, Ganesh Panchapakesan, Shanmuganathan Subramanyam
Correspondence – Vikranth Chunduri – chvv.vikranth@gmail.com
Department of Medical Gastroenterology, Sri Ramachandra Institute of Higher Education and Research. 1, Mount Poonamallee Road, Ramachandra Nagar, Porur, Chennai 600 116, India
Background The prevalence of celiac disease is estimated to be around 1% in northern India, but it is much lower in southern India. This disparity in prevalence is thought to be due to dietary differences.
Objective To determine the yield of routine duodenal biopsies in patients with suspected celiac disease in tertiary care centre in Tamil Nadu.
Study design Retrospective study, and patients from January 2018 to June 2021 were included.
Methods Patients with Iron deficiency anemia (<12 gm/dL in women and <13 gm/dL in men with low mean corpuscular volume [MCV] and ferritin), chronic diarrhea (>4 weeks) and significant weight loss (>5% in 6 months) or a combination of these symptoms are included.
Results A total of 448 patients are included in the study, 206 (45.9%) males, and 242 (55.1%) females. With mean age was 47.2 years in males, and 44.56 years in females. The predominant symptoms are, only anemia in 383 (85.4%), only diarrhea in 29 (6.4%), anemia + diarrhea in 21 (4.6%), with rest of the combination of symptoms in minority. Scalloping of the duodenal mucosa observed in 15 (3.3%) patients, but none of these patients have features of celiac disease on microscopy.
Biopsy features of celiac disease are seen in four patients, three of them came with only anemia and one with only diarrhea. All the patients had normal duodenal endoscopy, but HPE were suggestive of celiac with Marsh stage 3. The overall yield of duodenal biopsy for all symptoms is 0.89%, patients with only anemia 0.78%, and patients with only diarrhea is 3.44%.
Conclusion Even in a targeted group of patients with celiac disease symptoms, the yield of duodenal biopsy is very low. Patients who have only diarrhea have a better yield than patients who have only anemia.
Keywords Celiac disease, South India, Anemia
087
Selection of the type of enteroscope in management of SI disease
Ravi Shankar Bagepally, Tajuddin Farooqui
Correspondence – Ravi Shankar Bagepally – b_ravishankar@yahoo.com
Department of Gastroenterology, Yashoda Hospitals, Alexander Road, Kummari Guda, Shivaji Nagar, Secunderabad 500 003, India
Introduction Enteroscopy has always been a challenging area in Gastroenterology. Indications can be difficult, and outcomes may be unpredictable. Option of the technique may depend on the operators experience and expertise.
Methods We conducted a total of 92 enteroscopy examinations; Capsule Endoscopy (CE – 64), Balloon Enteroscopy (BE – 13), Power Spirus Enteroscopy (PSE – 15). Gastrointestinal (GI) bleed constituted 63/92 (69%). Capsule endoscopy was commonly performed for bleeding whereas device assisted enteroscopy (DAE) preferred for suspected obstruction, Crohn’s disease or abdominal pain.
Results Eighty percent (51/64) of cases with CE, 42% (12/28) of cases with DAE were conducted for bleeding. In patients with GI bleed (occult, overt or anemia), the positivity rate of CE was 41% and DAE was 75%. In patients with strongly suspected SI obstruction, the obvious choice was DAE. Enteroscopy was complete in most cases with CE and in <10% cases of antegrade DAE. Power Spiral Enteroscope appeared technically difficult initially, but with experience seemed easier to perform.
Conclusions CE was commonly preferred for intestinal bleed. DAE was preferred for suspected obstruction or thickening of the bowel wall on imaging and bleed control. Technical difficulty with PSE seemed easy to overcome with minimal experience. Balloon Enteroscopy seemed to be reserved for thin subjects and resource crunch situation or failed PSE.
Keywords GI bleed, Capsule Endoscopy, Power Spirus Enteroscopy
088
Lupus enteritis as the initial manifestation of systemic lupus 74atient74d74s74i
Antony George , Shimabara Dhal Mohapatra, Ravindra Pal, Krishnadas Devadas
Correspondence – Antony George – anthony00590@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor-Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Systemic lupus 74atient74d74s74i (SLE) is a complex autoimmune disorder with multisystem involvement, with a prevalence of 3.2 per 100,000 in India. Lupus enteritis is a vasculitis of the bowel, a rare manifestation with a reported prevalence of 0.2% to 5.8%. Lupus enteritis as the initial manifestation of SLE is rare in literature.
Case Summary We report a 28-year-old female, with a history of thrombocytopenia detected during her 2nd pregnancy, for which she was given oral steroids, and a history of cholelithiasis with choledocholithiasis – post cholecystectomy with CBD exploration, who presented to our OPD with complaints of watery diarrhea, colicky abdominal pain, and vomiting since 4 weeks and abdominal distension since 1 week. General examination revealed signs of dehydration, pallor, pedal edema and signs of postural hypotension. Abdominal examination revealed epigastric tenderness and shifting dullness. Investigations showed normocytic normochromic anemia (hemoglobin – 7.2 g/dL), hypoalbuminemia (2.9 g/dL) and proteinuria (24 hour urine albumin – 734 mg/24 hour). Blood and stool studies were negative for infection. Ascitic fluid analysis revealed low SAAG high protein ascites. CECT abdomen revealed diffuse mucosal edema of stomach, small and large intestine, and right mild hydroureteronephrosis. Esophagogastroduodenoscopy and colonoscopy revealed edematous mucosa in the stomach and throughout the colon. Further workup revealed ANA +ve; low complement levels (C3 – 10 and C4 – 20) and anti-dsDNA +ve. Based on the ACR criteria she was diagnosed with SLE. She was treated with Methylprednisolone pulse for 3 days, followed by Cyclophosphamide, because of multisystem involvement. Her symptoms resolved with the treatment. She was asymptomatic during follow-up after 1 month.
Conclusion Lupus enteritis as the presenting feature of SLE is rare and the diagnosis requires a high index of clinical suspicion, combining clinical, biochemical, and imaging features. Though Lupus enteritis is steroid-responsive, our patient required Cyclophosphamide because of multisystem involvement.
Keywords Lupus enteritis, Abdominal pain, Chronic diarrhea, Systemic lupus 75atient75d75s75i, Ascites
089
Eosinophilic enteritis: A rare cause of small bowel obstruction
Amal Velse, R Akhilandeshwari
Correspondence – A R Akhilandeshwari – amalvelse16oct@gmail.com
Department of Medical Gastroenterology, Government Kilpauk Medical College, Chennai 600 010, India
Introduction Eosinophilic enteritis is a rare entity characterized by eosinophilic infiltration of the small intestine. Clinical features of this condition depends on the site of involvement of the intestinal wall and includes malabsorption, failure to thrive, bloody stools and ascites. Rarely it may be severe enough to result in small bowel obstruction.
Case report A 38-year-old female with no significant medical history presented with complaints of periumbilical, episodic, colicky abdominal pain of 5 years duration accompanied by vomiting and weight loss. Her workup included a hemoglobin of 12.2 gm/dL, total counts of 7800 cells/mm3 with eosinophilic predominance. Imaging showed features of acute small bowel obstruction secondary to ileal stricture. Patient underwent an explorative laparotomy. Intraoperative findings included multiple ileal strictures in distal 100 cm with grossly dilated proximal small bowel. Small bowel resection with reanastomosis was done. Histopathology of the resected specimen showed marked transmural eosinophilic infiltrate of the small bowel suggestive of eosinophilic enteritis. Patient was started on low dose steroid along with dietary advice. Patient improved symptomatically and is currently asymptomatic.
Discussion Since its discovery in 1937 by Kaijser et al. approximately 280 cases of eosinophilic gastroenteritis have been reported in literature. Pathogenesis of this condition is not clearly understood. Current theories implicate hypersensitivity reactions in its development. Endoscopic appearance is nonspecific and do not aid in diagnosis. Mild symptoms are managed conservatively. More severe symptoms are managed with a course of corticosteroids. If small bowel obstruction is suspected surgical evaluation should be promptly pursued as was in the case of our patient.
Conclusion With this case, we wish to highlight a rare etiology that should be kept in the differential when evaluating patients with intestinal obstruction and eosinophilia.
Keywords Eosinophilic enteritis, Obstruction, Steroid
090
Duodenal tuberculosis – A rare site of a common disease
Sharathchandra Khanappanavar, Deepak Suvarna, H P Nandeesh, T R Vijaykumar, H V Maj Aradya, Maj Aradya Koppad, M R Hitesh
Correspondence – Sharathchandra Khanappanavar – khanappanavar.sharathchandra@gmail.com
Department of Gastroenterology, J S S Hospital, Mahatma Gandhi Road, Fort Mohalla, Mysuru 570 004, India
Introduction Tuberculosis is a worldwide health problem, with a high incidence in developing countries. Duodenal tuberculosis is very rare, with few cases reported in the literature. We report a case of duodenal tuberculosis in a 29-year-old male patient.
Case Details The patient presented with persistent dyspeptic symptoms, bloating and epigastric discomfort of one week’s duration, following which an upper GI endoscopy was done. A 1 x 0.5 cm nodule was seen in the first Part of duodenum. Histopathologically, epithelioid granulomas with giant cells and necrosis were seen with acid fast bacilli (AFB). Retrospectively, the patient revealed that he had taken anti-tubercular drugs for four months in 2018 for tubercular lymphadenitis.
Discussion The reported incidence of gastroduodenal tuberculosis is 0.5 %. The possible causes of the rareness of duodenal tuberculosis may be gastric acid, rapid transport of micro-organisms, sparse lymphoid follicles in the wall, and integrity of duodenal mucosa. Duodenal involvement may be endogenous, exogenous or both. The exogenous type may cause duodenal involvement due to the compression by enlarged peri-duodenal lymph nodes, while the endogenous type may show ulcerative, hypertrophic or ulcerative-hypertrophic lesions.
Conclusion Duodenal tuberculosis is easy to be misdiagnosed as an ulcer or inflammatory bowel disease. Although the sensitivity of AFB staining is low, it should remain an important part of the diagnostic evaluation of mucosal biopsies. Wrong diagnosis often leads to wrong treatment or serious complications due to delayed treatment. Thus, it is of great significance for patients that diagnosis be made through optimal imaging and histological analysis.
Keywords Tuberculosis, Duodenum, Endoscopy, Biopsy
091
A common disease at an uncommon site-isolated jejunal tuberculosis, a rare presentation
Sanjo John, A R Akhilandeswari
Correspondence – A R Akhilandeswari – sanjojohnmavely@gmail.com
Department of Medical Gastroenterology, Government Peripheral Hospital, 3rd Avenue, Anna Nagar, Chennai 600 102, India
Introduction Tuberculosis (TB) can affect any organ system. Intestinal TB constitutes 1% to 3% of TB worldwide. The most common site of gastrointestinal (GI) involvement are the ileum and ccum. Concomitant jejunal TB is usually seen at the terminal stages of extensive bowel involvement. Isolated jejunal involvement, without bowel involvement elsewhere is rare.
Case Report A 29-year-old male presented with periumbilical abdominal pain since 2 years, bilious vomiting 1 to 2 hours after food intake since 3 weeks. He had loss of appetite and loss of weight. No fever, cough. General examination was normal. ESR- 72. Baseline investigations were normal. Viral markers-negative. Chest X-ray was normal. Barium meal study revealed focal dilatation of distal ileal loops. USG abdomen showed dilated, fluid filled bowel loops in right iliac fossa with sluggish peristalsis. CT enterography showed long segment mild circumferential bowel wall thickening with significant luminal narrowing involving mid/distal jejunal loops and significant dilatation of proximal jejunal loops. Mild adjacent fat stranding and few mesenteric lymph nodes enlarged, largest measuring 12 mm. VOGD was normal. carcinoembryonic antigen (CEA)-negative. Patient underwent diagnostic laparoscopy and resection anastomosis. Histology showed granulomatous inflammation with Langhans giant cells. The possibility of tuberculosis was considered and started on category 1 ATT. Patient improved symptomatically with treatment.
Discussion The normal GIT physiology propels food from small intestine, limiting the contact period of the bacilli with jejunal mucosa. The 77atient77d77s77is7777 of the patient also checks the bacillary invasion. Vague symptoms and nonspecific investigations make the early diagnosis of intestinal TB challenging.
Conclusion Gastrointestinal TB can present at uncommon sites. Isolated jejunal TB is rare and a high degree of suspicion should prompt the clinician to think of TB in jejunal lesions even in immunocompetent individuals.
Keywords Tuberculosis, Granulomas, Jejunum
092
Assessment of intestinal failure and insufficiency in patients with celiac disease
Mahendra S Rajput 1 , Alka Singh 1 , Ashish Chauhan 1 , Shubham Prasad 1 , Vikas Jindal 1 , Sanjay Kumar 2 , Saroj K Sinha 2 , K S Madhusudan 3 , Rajesh Khadgawat 4 , Sanjayn K Agarwal 5 , Vineet Ahuja 1 , Govind K Makharia 1
Correspondence – Govind K Makharia – govindmakharia@gmail.com
1Departments of Gastroenterology and Human Nutrition, 3Radiology, 4Endocrinology, 5Nephrology, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India, and 2Department Gastroenterology, Post Graduate Institute of Medical Education and Research, Chandigarh 160 012, India
Background Intestinal failure/insufficiency has been defined and graded mainly in relation with short bowel syndrome. Diffuse mucosal disease of intestine such as celiac disease (CeD) also leads to intestinal failure/insufficiency which further secondarily leads to other target organ failure. It is also believed that patients with potential CeD have no significant disease.
Patients and Method Fifty-one consecutive treatment naïve patients with CeD and potential CeD underwent intestinal and extraintestinal failure/insufficiency assessment. The severity of clinical manifestations was assessed using Gastrointestinal Symptom Rating Scale (GSRS) and Celiac Symptom Index (CSI). Intestinal mucosal absorption was assessed using d-Xylose and enterocyte mass using plasma citrulline level estimation. Objectively, intestinal insufficiency was defined if d-Xylose excretion was <5 gm/25 gm/5 hr and/or if plasma citrulline was <30 μMol/L. Secondary, five extraintestinal organ insufficiency/failure were defines as follows; short stature (as linear growth failure), BMI (as nutritional status), anemia (hematological failure), osteopenia and osteoporosis (bone health failure) and sarcopenia (muscle mass failure).
Results Intestinal insufficiency/failure was present in 90.7% and 100% patients with CeD and potential CeD respectively. Overall, 39 and 8 patients with CeD and potential CeD had one or more secondary organ failure/insufficiency. Secondary organ failure were present as short stature in 21.6%, anaemia in 78.4%, osteopenia and/or osteoporosis in 54.3%, sarcopenia in 36.4% and low BMI in 43% patients. Amongst patients with CeD, 7.8% had no organ failure, 17.6% had one, 33.3% had two and 42.2% had three or more secondary organ failure. All patients with potential CeD (n=8) had ≥1 organ insufficiency or evidence of primary intestinal failure.
Conclusions In not only patients with CeD, but also those with potential CeD have evidence of intestinal failure/insufficiency, which further leads to secondary target organs failure/insufficiency. It is thus essential to identify these diseases early in course before irreversible changes set in other organs.
Keywords Celiac disease, Intestinal insufficiency, Intestinal failure
093
Gastrointestinal tract involvement in patients of potential celiac disease beyond small intestine – An early proof
Ashish Chauhan 1 , Prasenjit Das 2 , Alka Singh 1 , Madhu Rajeshwari 2 , Mahender Singh
Rajpoot 1 , Ashish Aggarwal 1 , Rimlee Dutta 2 , Vikas Banyal 1 , Shubham Mehta 1 , Wajiha Mehtab 1 , Anam Ahmed 1 , Vineet Ahuja 1 , Govind Makharia 1
Correspondence – Govind Makharia – marquez.dvl@gmail.com
Departments of 1Gastroenterology and Human Nutrition, and 2Pathology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction IgA anti-tissue transglutaminase-2 antibody (anti-TG2 Ab) deposits in the tissue have been used as evidence of involvement of both intestinal and extraintestinal organs in patients with celiac disease (CeD). We have recently shown the involvement of the esophagus, stomach, and colon in a subset of patients with celiac disease using anti-TG2 Ab deposits. Whether extra-small intestinal organs are affected in patients with potential CeD is not known.
Methods Nine patients with potential CeD and 27 age and gender-matched patients with irritable bowel syndrome were recruited as cases and controls, respectively. Mucosal biopsies were collected from the esophagus, stomach, duodenum, and rectosigmoid regions in cases and controls. All biopsies were evaluated for histological changes, and they were subjected to dual-color immunohistochemical staining for identifying IgA anti-TG2 Ab deposits at various sites.
Results IgA anti-TG2 Ab deposits were observed in significantly higher numbers of patients with potential CeD at all sites than in patients with IBS (esophagus 22.2% [2/9] vs. 0%, p=0.012; stomach 66.7% [6/9] vs. 11.5% [3/26], p<0.001; duodenum 57.1% [4/7] vs. 0%, p<0.001; and colon 42.9% [3/7] vs. 0% [0/24], p=0.001).
Conclusion The presence of anti-TG2 Ab deposits in organs other than the small intestine such as the esophagus, stomach, and colon suggests the involvement of these extraintestinal organs even in patients with potential CeD.
Keywords Celiac disease, Potential celiac disease, Immuno-histochemistry, IgA tTG mucosal deposits
094
Prediction of villous atrophy based on anti-tissue transglutaminase antibody titre
Aditya Vikram Pachisia , Nishakar Thakur 1 , Alka Singh, Sachin Rajput, Mahender Singh
Rajput, Varun Teja, Anam Ahmed, Shubham Mehta, Prasenjit Das 2 , Vineet Ahuja, Govind Makharia
Correspondence – Aditya Vikram Pachisia – avpafmc@gmail.com
Departments of Gastroenterology and Human Nutrition Unit, 1Center for Community Medicine, and 2Pathology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, New Delhi 029, India
Introduction The European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) 2020 guidelines proposes that IgA anti tissue transglutaminase (tTG) antibody titre ≥ 10 times the upper limit of normal (ULN) and a positive anti endomysial antibody on second sample is sufficient for diagnosis of celiac disease (CeD ) in children and duodenal biopsy is not warranted. Studies have suggested that anti tTG antibody ≥ 10 times can be applied in symptomatic adult CeD but it has not been widely adopted in standard guidelines. Our aim is to determine the fold rise in anti tTG antibody levels that is predictive of small intestinal villous atrophy (Modified Marsh grade 2 and 3) in adults and to determine the accuracy of anti tTG antibody level ≥10 times ULN in predicting small intestinal villous atrophy (Modified Marsh grade 2 and 3) diagnostic of CeD.
Methods Retrospective analysis of 641 adults with CeD assessed in the specialist CeD clinic at AIIMS, New Delhi from 2009 to 2021 who had a serum IgA anti tTG test and duodenal biopsy within 6 weeks of each other and naivety to a gluten-free diet.
Results Only 42.28% of patients had ≥ 10-fold rise in anti tTG antibody titre. More than equal to 10-fold rise in anti tTG antibody titre predicts villous atrophy Modified Marsh grade 2 and 3 with a specificity of 100% and 94% and positive predictive value of 100% and 98% respectively. Prediction of villous atrophy modified marsh grade 3 has 100% specificity and positive predictive value at ≥ 13-fold rise in anti tTG antibody titre.
Conclusion Biopsy is essential in more than 50% of adults with CeD who have ≤ 10-fold rise in anti tTG antibody titre. However, patients with anti tTG antibody titre ≥ 10 fold have high predictive value for diagnosing CeD.
Keywords Anti tTG antibody, Duodenal biopsy, ESPGHAN
095
Retrospective analysis of diagnostic yield and therapeutic outcomes of double balloon enteroscopy – A single center experience
Pankaj Shrimal , Mukesh Kalla. Ramesh Roop Rai, Nikhil Atolia, Anant Gupta
Correspondence – Pankaj Shrimal – drpankajshrimal@gmail.com
Department of Medical Gastroenterology, S R Kalla Memorial Gastro and General Hospital, 78-79, Dhuleshwar Garden, C Scheme, Jaipur 302 001, India
Introduction Double balloon enteroscopy (DBE) is an effective endoscopic tool for diagnosis and treatment of small bowel diseases. This study is a retrospective analysis of consecutive patients undergoing DBE at our centre.
Methods The data of all patient’s undergoing DBE was retrospectively analysed between April 2019 to August 2021. The indications, diagnostic yield and therapeutic outcomes were analyzed.
Result A total of 118 patients (Mean age 49.46 years, range 18-80 years, 85 males) underwent 130 DBE procedures (63 via antegrade and 67 via retrograde approach) in the study period. Indications for DBE were chronic pain abdomen, obscure GI bleeding, chronic diarrhea and recurrent vomiting in 50.8%, 24.50%, 17.80% and 6.70% respectively. The overall diagnostic yield was 69.7% and the diagnostic yield in indications of chronic pain abdomen, obscure GI bleeding, chronic diarrhea and recurrent vomiting were 75%, 68%, 59 % and 80% respectively. Among therapeutic procedures, 12 patients underwent 16 sessions of argon plasma coagulation for angiodysplasias. Follow-up data was available for 9 patients. Overt bleeding resolved and hemoglobin levels stabilised in 5 patients (42 %) with mean follow-up of 8 months (range 2 to 12 months). One patient with liver cirrhosis had acute bleeding due to mid ileal ectopic varix which was controlled with glue injection. Two patients underwent DBE assisted endoscopic retrograde cholangiopancreatography (ERCP) for hepaticojejunostomy (HJ) stricture, one patient underwent CRE balloon dilatation and biliary stenting for benign HJ stricture, another patient underwent bilateral biliary stenting for malignant HJ stricture.
Conclusion Double balloon enteroscopy is useful tool for diagnosis and treatment of small bowel diseases and provides opportunity for biliary intervention in surgically altered anatomy.
Keywords Balloon assisted enteroscopy, Stricture dilatation, APC
096
Pattern of practice of the diagnosis, dietary counselling and follow-up of patients with celiac disease
Wajiha Mehtab1,2, Tamoghna Ghosh1, Harsh Agarwal1, Alka Singh1, Namrata Singh1, Ashish Chauhan1, Shubham Mehta1, Mahendra Singh Rajput1, Shubham Prasad1, Vineet Ahuja1, Anita Malhotra3, Govind K Makharia1
Correspondence – Wajiha Mehtab – jiya.mehtab12@gmail.com
1Department of Gastroenterology and Human Nutrition, 2Department of Home Science, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India, 2University of Delhi, South Moti Bagh, New Delhi 110 021, India, 3Department of Home Science, Lakshmibai College, University of Delhi, Ashok Vihar III – Ashok Vihar, Delhi 110 052, India
Objective Compliance to guidelines in making of a diagnosis, dietary counselling and follow-up of patients with celiac disease (CeD) varies markedly amongst physicians. We therefore conducted a questionnaire-based survey to assess the pattern of practice of the diagnosis, dietary counselling, and follow-up of patients with CeD in India.
Methods A questionnaire including 30-questions was developed based on review of literature, group discussions and expert group meetings. The web-based questionnaire was administered through social media (WhatsApp) to 18 groups comprising of 2980 adult patients with CeD. Of them, 970 (32.5%) responses were received and responses from 955 patients (females:611 [63.9%], medianage:21years, inter quartile range:12-35years) were finally included.
Results While 679 (71.1%) patients were diagnosed based on a combination of blood tests and upper gastrointestinal endoscopy and biopsy, 214 (22.4%) based on blood test alone and 62 (6.5%) based on endoscopic examination for diagnosis. After diagnosis, 875 (91%) patients were 81atient81d81 initially by the physician and only 585 (61%) were referred to a dietician for dietary counselling. In majority, the time spent by doctors and dietitians during first 81atient81d81s was between 10-20 minutes only. After first 81atient81d81s, 191 (20%) and 355 (37.3%) patients did not visit the doctor and the dietitian, respectively. Only 515 (53.8%) patients were getting their anthropometric parameters checked at every follow-up visit and one-fourth (n=232, 24.3%) of patients were self-monitoring their serological parameters. The adherence to diet was not monitored by the dietitian in 495 (51.8%) patients.
Conclusion The practice of the diagnosis, dietary counselling, and follow-up of patients with CeD in India is not as per the standard guidelines. Most of the patients are not referred to a dietitian. There is a need to reinforce the guidelines for proper care and management of patients with CeD.
Keywords Counselling, Gluten-free diet, Celiac disease, Follow-up
097
Histo morphological study of duodenal nodules in first part of duodenum in 104 patients in a tertiary care center in south India
Vineesha Bontha
Correspondence – Vineesha Bontha – bontha.vineesha@gmail.com
Department of Medical Gastroenterology, Sri Ramachandra Institute, 1, Mount Poonamallee Road, Ramachandra Nagar, Porur, Chennai 600116, India
Introduction Duodenal nodules in first part of duodenum are frequently noted as an incidental finding in many patients undergoing upper gastrointestinal scopy for other indications such as dyspepsia. The aim was to evaluate histology and character of this nodules.
Methods This is a retrospective study of 104 patients who had nodules in first part of duodenum either single or multiple during routine endoscopy procedures done between January 2019 to July 2021 which are biopsied. The morphology and its histopathology was analyzed.
Results The mean age of presentation is 52 years. Out of 104 patients, 64 (61.53%) were males and 40 (38.46%) were females. Single nodule was seen in 41 (39.4%) patients. Multiple nodules were seen in 63 (60.5%) patients. On histological evaluation, Brunner hyperplasia was noted in 46 (44.2%) patients. No significant changes were noted in 43 (41.3%) patients. Neuroendocrine tumor was diagnosed in 15 (14.4%) patients. Fourteen patients of diagnosed neuroendocrine tumor had single 5-10 mm sized nodule in the anterior wall. One patient had multiple nodules in duodenum of size 1-2 mm with one predominant nodule of 8 mm size which was neuroendocrine tumour on biopsy.
Conclusion There is high incidence (34.1%) of neuroendocrine tumor in single nodules. Single nodules are much less likely to represent duodenitis unlike multiple nodules and in fact they have significant neoplastic potential mandating biopsy whenever they are found.
Keywords Duodenal nodule, Neuroendocrine tumor, Endoscopy
098
Etiological spectrum of chronic organic non-bloody diarrhea in northern India
Prachi Daga, Lipika Lipi1, Randhir Sud, Amarender Singh Puri
Correspondence – Amarender Singh Puri – amarender.puri@gmail.com
Departments of Gastroenterology, and 1Pathology, Medanta Medicity, Gurgaon 122 022, India
Introduction Chronic non-bloody diarrhea is attributed to functional or organic disease. The latter category may present with malabsorption syndrome. Indian data largely focussed on the etiological spectrum of MAS in adults. Data from south India suggest tropical sprue (TS) is the commonest cause of MAS, whereas northern India data suggests celiac disease and TS are leading causes.
Aim The aim of the study was to evaluate the etiological spectrum of chronic organic non-bloody diarrhea in northern India.
Methods This prospective observational study was done at a tertiary care corporate hospital in north India. Patients ≥ 18 years presenting with chronic non bloody diarrhea of > 4-week duration, from the period of July 2020 to July 2021 were enrolled for the study. Patients with irritable bowel syndrome (IBS) and other functional disorders were excluded.
Results During the study period, 69 patients presented with chronic non-bloody diarrhea which was organic in nature. The mean age of the patients (56.5% males) was 49 ± 16 years. A definite etiological diagnosis was made in 68 (98.5%) patients. The median duration of diarrhea was 6 months. Inflammatory bowel disease (IBD) (CD-29 and UC-3) accounted for 32 of the 68 (46%) cases making it the predominant cause. Gastrointestinal (GI) infection comprising of giardiasis, human immunodeficiency virus (HIV) and TS accounted for 10 cases (14.5%). Adult celiac disease was diagnosed on the basis of revised European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) criteria seen in 6 patients (9%). Notably, GI malignancies manifesting as chronic non-bloody diarrhea was seen in 4 cases (6%). Pancreatic disease (chronic pancreatitis -3, NET-2) accounted for 5 patients (7%).
Conclusion Our data suggest that IBD (Crohn’s disease) is the predominant cause of chronic organic non-bloody diarrhea in adults, followed by GI infections. Our study differs from previous studies which suggested that celiac disease and TS are the leading causes of chronic diarrhea and malabsorption in India.
Keywords Chronic Diarrhea, Non bloody, IBD
099
An uncommon cause of a chronic diarrhea in a middle-aged male- A case report
K Abhishek , Sunil Kumar, M Goutham, G Sagar
Correspondence – K Abhishek – abhisheksmrt6@gmail.com
Department of Medical Gastroenterology, Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad 500 082, India
Introduction Chronic diarrhea is one of the most common gastrointestinal symptoms and may lead to severe protein energy malnutrition and its attendant complications. We present a case report of a middle aged male presenting with chronic diarrhea and malabsorption secondary to common variable immunodeficiency (CVID). It is a primary immunodeficiency disorder characterized by reduced immunoglobulin serum levels and absent or impaired antibody production with variable involvement of GIT.
Case Report A 46-year- old male presented with small bowel type diarrhea associated with significant weight loss since 1 year. He also had a h/o multiple hospitalization for recurrent pulmonary infections. Primary evaluation revealed iron deficiency anemia and elevated ESR. Celiac serology, hydrogen breath test and stool for ova and cysts were negative. Serum immunoglobulins were low, with significantly reduced levels of IgG (17.2 mg/dL) and IgA (<10 mg/dL). UGIE revealed nodularity in D2 with histopathology suggestive of reactive lymphocytosis and no evidence of atypical cells. Abdominal imaging showed edematous small bowel loops with changes of bronchiectasis on HRCT chest.
Hematology and pulmonology opinion were taken, and he was initiated on antibiotics by pulmonology team for LRTI. He was also initiated on treatment with rifaximin and probiotics, but the response was suboptimal. In view of recurrent pulmonary infections and chronic diarrhea leading to compromised quality of life, he was started on intravenous immunoglobulins once in 2-4 weeks with the aim of maintaining IgG trough levels between 400-500 mg/dL. 1 month after initiation of immunoglobulins there was a significant improvement in his symptoms.
Keywords Chronic diarrhea, CVID, Immunoglobulins
100
Serum concentration of soluble apoptosis-associated molecules in celiac disease
Kaushal Prasad 1 . Arun Kumar Sharma 1 , Uma Debi 2 , Pramod Kumar Gupta 3 . Saroj Kant Sinha 1
Correspondence – Kaushal Prasad – kaushalkp10@hotmail.com
Departments of 1Gastroenterology, 2Radiodiagnosis, and 3Biostatistics, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 -012, India
Aim The exact role of soluble apoptosis-related mediators in celiac disease is still not fully understood. It is possible that serum sFas-sFasL may have a role in the pathogenesis of celiac disease. In this study, we assess the circulating soluble Fas and Fas ligand levels in celiac disease.
Methods The study included 50 newly diagnosed celiac disease adults and 25 non-celiac adults as control. The circulating sFas and sFasL levels were assessed by ELISA kits. All duodenal mucosal histological parameters were evaluated, classified, and graded histological lesions according to the criteria proposed by our group. The serum sFas and sFasL levels and duodenal histological results were then analyzed using appropriate statistical methods.
Results The mean age of 50 adults with celiac disease was 31.28 ± 12.83 (range, 15-62) years, with a M:F :: 1:1. In adult celiac disease mean serum sFas was significantly lower (p <0.001) than non-celiac control. However, mean serum sFasL was significantly higher (p=0.018) than non-celiac control. One way ANOVA indicated no relationship between grade of duodenal mucosal damage and concentration of serum sFas. On the other hand, One way ANOVA indicated a statistically significant relationship between different grades of duodenal mucosal damage and sFasL.
Conclusions The concentration of serum soluble Fas and FasL are significantly altered in celiac disease. Altered serum sFas does not correlate with grades of duodenal mucosal lesions. Further studies are required to see any relation between membrane-bound Fas or FasL and grades of duodenal mucosal lesions which may help to understand pathogenesis of celiac disease.
Keywords Celiac disease, Soluble Fas, Fas ligand, Apoptosis, Serum
101
Combined T cell/B cell defect with recurrent fungal and giardial infections presenting as chronic diarrhea
Pritam Das , Samir Mohindra
Correspondence – Samir Mohindra – mohindrasamir@yahoo.com
Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Rae Bareili Road, Lucknow 226014, India
18 years male presented with large volume, watery diarrhea since 11 months, frequency 3-4/ day, large volume, Bristol 5-6. The patient also had complaints of acute onset flaccid paraparesis for 1 day in February 2021, 2 doses of IVIG administered on 7th June 2021 and 13th July 2021 respectively with minimal response in the clinical course. The patient had exacerbation of loose watery stools since 7th August, similar nature as before. The patient also had complaints of acute onset weakness of bilateral lower limb and upper limb weakness since 1 day. D2 Biopsy 23/02/2021: Lamina showing mild lymphoplasmacytic infiltration, occasional structures resembling Giardia organisms. UGIE: 20/08/2021: Curdy white plaques in esophagus. Decreased duodenal folds with nodular mucosa. sIgs: 25/02/2021: NIH IgG: 1.49 IgA: 0.28 IgM: 0.19 IgE: normal (Low IgG, IgM, IgG levels) Lymphocyte Subset Analysis: 01/03/2021: CD3+/CD19-: 378 (1000-2200), CD3-/CD19+: 103 (110-570), CD3+/CD4+: 182 (530-1300), CD3+/CD8+: 167 (330-920), CD16+/CD56+: 10 (70-480) 28/04/2021: CD3+/CD19-) 883 (1000-2200), CD3-/CD19+: 132 (110-570), CD3+/CD4+: 230 (530-1300), CD3+/CD8+: 415 (330-920), CD16+/CD56+: 35 (70-480).
In case of patients presenting with recurrent fungal, bacterial as well as mycobacterial diseases, T cell defect should also be suspected in addition to B cell defect. In such cases, the option of Bone marrow transplant is a viable option and to an extent curable. However, in cases of non-respondent to IVIG in B cell defect, other viable options including Rituximab may be tried.
In case of this patient, it is very unlikely for combined disorder to present at such age, however X linked disorder may present at adolescent age.
Keywords SCID, Chronic diarrhea, Giardia, Fungal infections
102
Assessment of celiac disease in patient with liver cirrhosis
Shivam Kumar Verma , Gaurav Garg, Manisha Dwivedi, S P Misra
Correspondence – Shivam Verma – verma.shivam1211@gmail.com
Department of Gastroenterology, M L N Medical College, Prayagraj 211 002, India
Introduction Celiac disease is a long-term immune disorder that primarily affects the small intestine. The occurrence of liver impairment in CD is well established and must be regarded as one of the various extra intestinal presentations of gluten-sensitive enteropathy. However data is still insufficient and only a few studies had been done on the evaluation of celiac disease in patients already with liver cirrhosis. Thus, we did performed an observational study to determine the prevalence of celiac disease in patients with liver cirrhosis
Methodology This observational study has been undertaken in the Department of Gastroenterology and Hepatology, Moti Lal Nehru Medical College, Prayagraj. Cases has been selected from the patients who are attending Gastroenterology OPD or admitted in the ward.
Result Total of 134 patients were included in our study. Out of which 89 were male as compared to 45 females. More than 50% were in the age group of 30-50 years. Out of total 4 patients had celiac disease and 6 had non-specific duodenitis consistent with Marsh 1 stage.
Conclusion This study showed that CD was present in 2.9% of cirrhotics which is more than 2 times the prevalence in general population. This study also concluded the presence of nonspecific duodenitis in 4.5% of the study population which frequency was similar to that of general healthy population.
Keywords Cirrhosis, Celiac disease, Non-specific Duod
103
Spectrum of motor dysphagia in the pediatric ulcers in massive, small bowel bleeding
V G Mohan Prasad, Madhura Prasad, K Vamsi Murthy, A Sangameswaran, Sunil Chacko Verghese, Mithra Prasad
Correspondence – Madhura Prasad – mitnmad@yahoo.co.in
Department of Gastroenterology, V G M Hospital, 2100 Trichy Road, Coimbatore 641 005, India
Background Small bowel bleeding poses a diagnostic and therapeutic challenge. With the advent of newer device assisted enteroscope, diagnostic and therapeutic enteroscopy has become easy to perform. Here we present a case of massive, small bowel bleeding where a novel endoscopic collagen spray was used to achieve hemostasis.
Methods Novel motorized spiral enteroscope and endoscopic collagen spray (Hemoseal spray, Shalili) were used.
: Case Report A 26-year-old gentleman, presented with bleeding per rectum on and off. At presentation he was in shock with hemoglobin 0.6.g/dL. He was resuscitated. Endoscopy and colonoscopy were normal. CT visceral angiography showed enhancing wall thickening in distal jejunum/proximal ileal loop, possible Crohn’s disease. Novel motorized spiral enteroscopy showed multiple large ulcers with ooze of blood in distal jejunum and proximal ileum. Hemoclip was applied to a visible vessel and novel endoscopic collagen spray was applied to the entire extent of bleeding. He stabilized and recovered. He is currently on treatment of Crohn’s disease on follow-up.
Conclusion Endoscopic collagen spray can be used as an additional hemostatic agent for diffuse bleeding in extensive ulcers in the small intestine safely.
Keywords Small bowel bleeding, Obscure GI bleeding, Collagen spray
104
An atypical presentation of adenocarcinoma of duodenum: A case report
H N Nithin, Praveen Mathew, Prashant Kanni, Chandrababu Devarapu, Manoj Gowda, Raghuveer Balabhadra
Correspondence – Nithin H N – nithinnagraj08@gmail.com
Department of Medical Gastroenterology, Vydehi Institute of Medical Science and Research Centre, Vydehi Hospital, Bangalore 560 076, India
Small bowel malignancies are relatively rare, accounting for only 2% of all gastrointestinal cancers and 40-60 times less frequent when compared with colon cancer. Among small bowel tumors, most malignancies arise from the ileum, followed by the duodenum and jejunum. Adenocarcinoma of duodenum is an uncommon tumor, which is frequently delayed in diagnosis as its symptoms and signs are non-specific.
Wilkie’s syndrome also known as superior mesenteric artery syndrome (SMAS) is an uncommon cause of upper gastrointestinal tract obstruction due to the compression of the duodenum by the superior mesenteric artery. It is commonly due to loss of fatty tissue as a result of a various debilitating conditions leading to acute angulation between superior mesenteric artery and aorta. The exact prevalence of SMAS remains unclear, however, the rate has been estimated to be 0.013 and 0.3%, based on barium studies.
The present study describes a case of duodenal adenocarcinoma occurring in a 44-year-old man, who presented with features of intestinal obstruction secondary to Wilkie’s syndrome. This is the second case report in the world where a patient of small bowel adenocarcinoma masquerading as Wilkie’s syndrome. This case highlights the importance of considering the possibility of SMAS in patients presenting with upper gastrointestinal obstruction caused by intestinal carcinoma.
Keywords Superior mesenteric artery syndrome, Duodenal adenocarcinoma and small bowel obstruction
105
Capsule endoscopy for obscure gastrointestinal bleed in tropics: A single center experience on 352 patients
Uday C Ghoshal, Piyush Mishra
Correspondence – Uday C Ghoshal - udayghoshal@gmail.com
Department of Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow 226 014, India
Introduction Small bowel bleeding arising distal to ampulla and proximal to ileocecal valve contributes to 5% to 10% of all gastrointestinal (GI) bleed. Capsule endoscopy has enabled the evaluation of previously inaccessible small bowel pushing “true obscure GI bleeding” into oblivion. There are limited data of utility of capsule endoscopy from the tropics.
Methods A retrospective analysis of prospectively collected database from December 2003 to April 2020 of patients presenting to a tertiary care academic medical center with suspected small bowel bleeding was done. Capsule endoscopy was done for 352 patients and descriptive analysis of data was done comparing patients with overt and occult GI bleed.
Results Out of 352 patients, 245 (age 53.7 ± 18.7 years, 73.5% male) had overt and 107 (age 49.3 ± 14.9 years, 65.1% male) had occult GI bleed. Diagnostic yield of capsule endoscopy was similar for occult (68 out of 107; 63.5%) and overt GI bleed (168 out of 243; 69.1%), p=0.22. Lesions identified were ulcers (34.9% in occult and 26.6% in overt GI bleed), strictures (29.9% vs. 12.3% respectively, p<0.01), vascular malformations (14.9% vs. 22.2%, p=0.14), tumors (2.8% vs. 9.9%, p<0.05), hookworms (5.6% vs. 9.9%, p=0.21) and portal hypertensive enteropathy (0.9% vs. 5.8%, p<0.05). Capsule was retained in 10 (2.8%) patients who required surgery for retained capsule and the lesion.
Conclusion Capsule is safe and effective in detection of lesion(s) in suspected small bowel bleeding. Among patients with overt GI bleed (ulcers [26.6%] and vascular malformations [22.2%]), while among patients with occult GI bleed (ulcers [34.9%] and strictures [29.9%]), were the most common causes of small bowel bleed.
Keywords Obscure gastrointestinal bleed, Fecal occult blood, Capsule endoscopy
106
Relevance of examining entire small bowel in terminal ileitis
Isha Pahuja, Ajay Kumar, Neha Berry, Manav Wadhawan, Amrish Sahney
Correspondence – Isha Pahuja – ishapahuja5@gmail.com
Department of Medical Gastroenterology, B L K Super Speciality Hospital, Near Pusa Road, New Delhi 110 005, India
Introduction Terminal ileitis is an important entity in India but its etiology and diagnostic approach is poorly defined. Role of complete small bowel evaluation in these patients is still a dilemma. In this study we evaluate the role of capsule endoscopy in these patients.
Methods All consecutive patients with terminal ileitis were prospectively included in this observational study conducted from November 2019 to August 2021. All symptomatic patients with terminal ileitis underwent both CT enterography and capsule endoscopy.
Results Total 25 patients were included in this study. There were 10 males and 15 females. Most common symptoms were pain abdomen and diarrhea. On evaluation, 2/25 patients (8%) had specific findings on histopathological examination, one had tuberculosis and one had eosinophilic enteritis. Capsule endoscopy showed additional lesions in 4/25 (16%) patients, 2 had deep ileal ulcers and 2 had skip lesions which help in 88atient88d them as IBD- Crohn’s. These patients had long standing non resolving symptoms. Colonoscopic findings and histopathology in these patients were non-contributory. These 4 patients were started on specific treatment of Crohn’s and showed good clinical response. CT enterography showed skip lesions in only one of these four patients and was non-contributory in rest 24 patients.
Conclusion Capsule Endoscopy was helpful in changing the diagnosis in 16% patients of terminal ileitis in our study. Capsule endoscopy findings can help in establishing the etiology of isolated terminal ileal ulcers even when histopathology and CT enterography were non-contributory.
Keywords Terminal ileitis, Capsule endoscopy, Crohn’s disease, CT enterography
107
Impact of delay in the diagnosis on the severity of celiac disease
Shubham Mehta1, Govind Makharia1, Alka Singh1, Ankit Agarwal1, Amit Chavan2, Anam Ahmed1, Vignesh Dwarakanathan3, Wajiha Mehtab1, Mahendra Singh Rajput1, Ashish Chauhan4, Ashish Agarwal4, Varun Teja1, Aditya Vikram Pachisia1, Sachin Rajput1, Randeep Rana1, Prasenjit Das5, Vineet Ahuja1
Correspondence – Govind Makharia – govindmakharia@gmail.com
Department of 1Gastroenterology and Human Nutrition Unit, 2Medicine, 3Center for Community Medicine, 4Gastroenteroloy, and 5Pathology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029. India
Introduction Celiac disease has now become global disease with worldwide prevalence of 0.67%. Despite being a common disease, celiac disease is often not diagnosed and there is a significant delay in the diagnosis. We reviewed the impact of the delay in the diagnosis of celiac disease on the severity of celiac disease.
Methods We reviewed records of 409 consecutive patients with celiac disease (January 2012- January 2021) following in Celiac Disease Clinic. In many of patients, the duodenal biopsies had already been done before reporting to us, hence data of 311 patients having complete data set was finally analyzed. We extracted the specific data including the time of onset of symptoms, time to diagnosis from the onset of the symptoms, symptoms, and the fold-rise in anti-tissue transglutaminase antibody (IgA anti-tTG Ab) and severity of villous abnormalities as assessed using modified Marsh classification.
Results The median duration between the onset of symptoms and the diagnosis of celiac disease was 36 months (interquartile range 12-72 months). A longer delay in the diagnosis of celiac disease from the onset of symptoms was associated with lower body mass index, lower hemoglobin, higher fold rise in IgA Anti tTG titres and higher severity of villous abnormalities. There was no significant impact on the levels of serum protein and serum albumin and time since diagnosis.
Conclusions There is a significant delay in the diagnosis of celiac disease since the onset of its symptoms. The severity of celiac disease increases with increasing delay in its diagnosis. There is a need to keep a low threshold for the diagnosis of celiac disease in appropriate clinical setting.
Keywords Celiac disease, Diagnostic delay, Severity
108
Plugging the leak-Endovascular therapy for massive gastrointestinal bleed
Yeruva Deepthi Reddy, Avinash Balekuduru, Lokesh Locheruvapalli
Correspondence – Avinash Balekuduru – avinashbalekuduru@gmail.com
Department of Medical Gastroenterology, M S Ramaiah Medical College and Hospitals, B E L M S Ramaiah Nagar, RIT Post, M S Ramaiah Nagar, Mathikere, Bengaluru 560 054, India
Introduction Acute upper gastrointestinal bleeding is a life-threatening emergency which requires hospitalization, evaluation and endoscopic treatment. In this case report, we present a successful endovascular repair of infra renal aortic aneurysm presenting as hematemesis.
Case Report A 65-year-old female, known case of rheumatic heart disease on oral penicillin prophylaxis presented to emergency department with 4 episodes of hematemesis and melena associated with giddiness. Upon arrival, she was pale and was hemodynamically unstable with hypotension and tachycardia. Fluid resuscitation and blood transfusion was started. After stabilization bed side endoscopy was negative for bleeding source. Colonoscopy was done which revealed multiple non-bleeding colonic diverticula and melenic stools. In view of obscure gastrointestinal bleed, contrast enhanced computed tomography abdomen with angiography which showed infra renal aortic aneurysm of 30 x 37 x 55 mm with partial thrombosis eroding the 2nd part of duodenum. Vascular surgery opinion sought, and endovascular aneurysm repair (EVAR) was planned. ENDERVANT 16 x 16 x 82 cms stent graft deployed in aneurysm under fluoroscopic guidance. She tolerated the procedure well and she had no further episodes of hematemesis / melena at 3 months follow-up.
Conclusion Infrarenal aortic aneurysm presenting as 90atient90d90s is very rare. High degree of clinical suspicion is essential to make a correct diagnosis and early treatment, which is crucial for the prognosis of these patients.
Keywords Abdominal aortic aneurysm (AAA), Endovascular aneurysm repair (EVAR)
109
Unusual case of foreign body in the distal small bowel
Prasanna Gore , Subhash Agal
Correspondence – Prasanna Gore – drprasannagore@gmail.com
Department of Medical Gastroenterology, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Rao Saheb, Achutrao Patwardhan Marg, Four Bungalows, Andheri West, Mumbai 400 053, India
Eighty-year-old female known case of hypertension, hypothyroid, ischemic heart disease. History of cholecystectomy, carcinoma cervix status post radical hysterectomy and recurrence for which she received chemo-radiotherapy. Patient had massive per rectal bleed followed by fall at home. Patient was taken to hospital. On examination had right bruised eye CT brain plain revealed bilateral fronto-temporal subdural hygroma. She received 1-unit PRBC in view of severe anemia. Colonoscopy showed altered blood, small diverticulum in left sided colon and AVM noted in right sided colon APC done along with small internal hemorrhoid. CT abdomen angiography subtle hypodensities in descending colon and terminal ileum. EGD suggestive of small hiatus hernia. She had persistent drop in HB hence relatives brought the patient to our institute. Patient on arrival had history of recurrent anemia with multiple hospital admission. Patient had complaints of abdominal pain, melena with intermittent hematochezia, loss of appetite, weight loss, pedal edema. on examination patient had pallor, pitting pedal edema, cachexia. Patient was then investigated further found to have severe iron deficiency anemia; low hemoglobin hence transfused 2-pint PRBC. Additionally, patient had very low albumin hence albumin was given. Patient was posted for colonoscopy which revealed AVM for which APC was done. Repeat EGD revealed antral gastritis and hiatus hernia. As the bleeding was persistent CT angiography was done which revealed a hyperdense artifact in distal ileum? foreign body. Single balloon enteroscopy was done which revealed video capsule stuck in distal ileum along with local ulceration and stricture, capsule was retrieved. Patients’ symptoms improved and overall general condition improved. Surgery for the distal stricture which was likely post radiotherapy induced was advised. But the relatives gave a negative directive for the surgery.
Keywords Video capsule, Single balloon enterscopy, Recurrent anemia, Post radiotherapy
110
Relapse rates after withdrawal of thiopurines in patients with inflammatory bowel disease
Mukesh Kumar Ranjan, Vineet Ahuja
Correspondence – Vineet Ahuja – vineet.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Withdrawal of thiopurines after remission has been shown to be associated with an increased risk of relapse in patients with inflammatory bowel disease. However, long-term data on thiopurine withdrawal is limited especially from developing countries where the cost of long-term therapy poses a significant burden on patients.
Methods We retrospectively analyzed data of patients with IBD on thiopurine monotherapy who had stopped and were not on any other immunomodulator or biologics at the time of stopping thiopurines. All these were in clinical remission at the time of withdrawal.
Results Among 1264 patients of IBD who were treated with thiopurines, a total of 461 patients had to stop thiopurine because of various reasons. Among these, 218 (UC=179; CD=39) patients were in clinical remission and were continued on mesalamine. Overall, 36.7% (n=80) had relapsed after a median duration of months of 20 months (IQR: 9-49). There is no difference in relapse rate between UC and CD (39.6% vs. 23%). The overall cumulative probabilities of relapse were 17%, 34%, and 44% at the end of 1, 3, and 5 years respectively. The relapse rate was numerically low in patients who had stopped azathioprine after at least 24 months of therapy (31.9% vs. 44.1%, p=0.051). On univariate Cox regression analysis, female sex (HR: 1.6 [1.0-2.6], p=0.02) and short duration of therapy with thiopurines (HR: 1.02 [1.01-1.02], p=0.004) before withdrawal were associated with increase risk of relapse.
Conclusion Though thiopurine withdrawal is associated with an increased risk of relapse, a significant proportion of patients maintain well even after stopping thiopurines. We need further studies to identify this specific group of patients to avoid adverse events associated with long-term thiopurine therapy.
Keywords Inflammatory bowel disease, Azathioprine, Relapse
111
Sweet’s syndrome associated with Crohn’s disease and a dramatic response to steroids
Ashok Kumar , Kshitiz Saran, Itish Patnaik, Anand Sharma, Rohit Gupta
Correspondence – Ashok Kumar – drashok.sgpgims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Virbhadra Road Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Introduction Sweet’s syndrome (SS) is a rare extraintestinal manifestation of Crohn’s disease (CD) with <50 case reports. We describe a case of CD associated SS with a dramatic response to steroids.
Results Thirty-two-year-old housewife, presented with recurrent periumbilical colicky pain and skin lesions for 2 years. Pain was associated with intermittent, non-bilious, large volume vomiting’s but without abdominal distention or obstipation. The skin lesions involved palms and soles, initially macular and erythematous which evolved into elevated pus filled 92atien. There was no history of fever or joint pains. CT abdomen showed thickening, heterogenous enhancement and narrowing of antrum. Endoscopy showed large ulcer along pylorus with evidence of gastric outlet obstruction (GOO). Symptoms were transiently relieved with pantoprazole and domperidone but recurred necessitating gastrojejunostomy (GJ). Three months later, the GOO symptoms recurred, and endoscopy showed stomal ulcers and stenosis with patent GJ loops. Revision Roux-en-Y GJ provided short lasting symptom relief for 4 months. CT showed jejunal stricture, which was resected, and histopathology showed crypt distortion and transmural inflammation. Diagnosis of CD was made, and with prednisolone (40 mg/day), GOO symptoms resolved. After overlap with azathioprine (100 mg/day), steroids were tapered off. Patient discontinued azathioprine and GOO symptoms and skin lesions reappeared (Fig. 1). Skin biopsy showed neutrophilic infiltrate and a diagnosis of SS was made (Fig. 2). A pulse of intravenous hydrocortisone was given, which lead to dramatic resolution of skin lesions over one week (Fig. 1).
Conclusion The Sweet syndrome is characterized by fever, leukocytosis, painful papules or nodules of the skin, and a diffuse neutrophilic infiltrate. It is commonly found in 30–60-year females (women to men ratio 4:1). It recurs in one-third of patients. First-line treatments include systemic corticosteroids, potassium iodide, colchicine, and topical corticosteroids.
Keywords Crohn’s disease, Inflammatory bowel disease, Sweet syndrome
112
Prevalence of anti-tissue transglutaminase serology in community population and patients with irritable bowel syndrome: Two kits comparison
Anam Ahmed , Alka Singh, Ashish Chauhan, Mahendra Singh Rajput, Vikas Jindal, Vineet Ahuja, Govind K Makharia
Correspondence – Govind K Makharia – govindmakharia@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029. India
Background Anti-tissue transglutaminase-2 antibody (TG2) based serology are the cornerstone of diagnosing celiac disease (CeD), with a reported sensitivity of 98%. However, a few small, single-centre studies have questioned their sensitivity in clinical practice. Moreover, there are variation in TG2 antigens in commercial kits, with cut-offs determined by using small, poorly defined populations. We compared the variations in diagnostic performance of two immnunoglobulin IgA-TG2 assays in community population and patients with irritable bowel syndrome (IBS) at two different time periods.
Methods A total of 6210 adults from defined community and 406 patients with IBS from outpatient department of Gastroenterology, AIIMS, New Delhi were enrolled under the study during 2013 and 2019 respectively. Diagnosis of patients with IBS was done on the basis of Rome IV criteria. Serum samples were drawn from all recruited subjects after taking informed consent. For both the cohorts, IgA-TG2 was measured by 2 commercially available ELISA assays i.e. Quanta Lite h-tTG IgA, Inova Diagnostic, USA and Aeskulisa tTG-A New Generation, Germany.
Results For Quanta Lite assay, the seropositivity for patients with IBS and community population were 0.5% (2/400) and 1.5% (92/6210) respectively. However, for Aeskulisa assay, the seropositivity for patients with IBS and community population were 10.2% (41/400) and 8.9% (556/6210) respectively. Out of 556 participants from community, which were positive by Aeskulisa assay, 441 reported as negative serology from Quanta Lite assay.
Conclusion The diagnostic performance of IgA-TG2 varies markedly between 2 different kits. Therefore, a single IgA-TG2 assay may not adequately rule out CeD and further confirmatory tests should strongly be considered.
Keywords Celiac, Aeskulisa, Tissue-transglutaminase, Irritable bowel syndrome
113
Acute mesenteric ischemia in corona virus disease 2019 patients
Sunil Kasturi , Sanjay Kumar, T M U Naveen
Correspondence – Sunil Kasturi – drsunilkasturi@gmail.com
Department of Medical Gastroenterology, Gastrocare Hospital, 120, 121, Link Road, Number 3, Near Personal Branch SBI, E3, Arera Colony, Bhopal 462 016, India
Introduction The novel 2019 corona virus disease (COVID-19), which is caused by infection with the severe acute respiratory syndrome corona-virus 2 (SARS-CoV-2), was first reported in Wuhan, China, in December 2019. Although efforts to recognize and manage SARS-CoV-2 infections have focused primarily on respiratory complications, some patients with COVID-19 infection may experience gastrointestinal manifestation of this disease. Arterial thrombosis, though less common in comparison with venous thrombosis, has also been documented in patients with COVID-19. Arterial thrombotic complications include stroke, acute limb ischemia, renal infarcts, and, rarely, mesenteric ischemia.
Methods This is a retrospective analysis of mesenteric ischemia in COVID-19 patients (April to June 2021). Their clinical parameters, imaging findings and outcome were analyzed.
Results All patients presenting in emergency for mesenteric ischemia were analyzed, and it was noticed that 8 of the 10 patients were males. 9 had SMA thrombosis, 1 IMA thrombosis. Seven were operated. Among them 2 expired. Four (40%) did not have any comorbidities. Mean leukocyte, neutrophil, and platelet levels were within the normal range, while the lymphocyte level was near the lower limit. C-reactive protein and D-dimer was raised in all patients. The mean levels of international normalized ratio, platelet, and activated partial thromboplastin time were above the limits.
Conclusion The presence of hypercoagulation status in critical COVID-19 patients should be observed closely, and anticoagulation therapy to be considered in selected patients. Serious arterial thrombotic events might occur in COVID-19. Clinicians should be aware of the life-threatening situation in COVID-19 patients. For optimal management of these patients, understanding of various systemic manifestations and complications of SARS-CoV2 is vital.
Keywords Acute mesenteric ischemia, SMA thrombosis
114
Efficacy of budesonide in management of functional dyspepsia (defined by Rome IV) associated with duodenal eosinophilia
Adinath Wagh 1 , Chetan Bhatt 2 , Shobna Bhatia 2
Correspondence – Adinath Wagh – Adinath185wagh@gmail.com
1Department of Gastroenterology, and 2Gastroenterology, Hepatology and Pancreatobilliary Sciences, Sir H N Reliance Hospital, Girgaon, Mumbai 400 008, India
Background Duodenal eosinophilia is recognised as an important factor in pathogenesis of functional dyspepsia. Oral budesonide has been used for treatment of eosinophilic esophagitis. Its use in eosinophilic duodenitis has not been evaluated.
Aims To study the efficacy of oral budesonide in functional dyspepsia with duodenal eosinophilia.
Methods This prospective observational study was done in 270 consenting adults with dyspepsia. Seventy-two patients with FD who had >22 eosinophils/hpf on duodenal biopsies (age 39.93+12.8 years; 39 men) were included. Patients received oral budesonide (9 mg/day for 4 weeks, and tapered to 6 mg/day and, then 3 mg/day for 4 weeks each) along with PPI +/- prokinetic. Patients filled out Leeds dyspepsia questionnaire (LDQ), Short form Nepean dyspepsia index (SF-NDI) and 7 point Likert scale/Global Symptom Outcome Score (GOS) at presentation, and at 3 months. Treatment response was defined as 5-point reduction in Leeds questionnaire, 2-point reduction in SF-NDI and drop in GOS score to either no or minimal severity (scores of 1 or 2 at end of 3 months treatment). The protocol was approved by the IRB. Statistical analysis: P value <0.05 was considered significant.
Results Fifty-one patients had epigastric pain (EPS), and 21 had post-prandial distress syndrome (PDS). 59/72 (46/51 EPS and 13/21 PPDS (73.4%) patients responded; median LDQ score improved from 21 (IQR 17-26) to 11 (IQR 5-15) in EPS and 22 (IQR 17-26) to 11 (IQR 9-18) in PPDS subgroup (RR 2.02; p<0.04). Similarly GOS score improved from 5.2/7 to 2/7 in 73.6% patients (p=0.001). QoL improved in 83.3% FD patients. Mean SF-NDI score reduced from 24.5/40 to 15.1/40 (p 0.001). None of the patients reported any adverse event related to budesonide.
Conclusions Amongst patients with FD who had duodenal eosinophilia, budesonide added to standard of care gives symptom relief to >70% patients.
Keywords Functional dyspepsia, Duodenal 94atient94d94s94, Oral budesonide
115
Colonic mucormycosis in fistulising Crohn’s disease: A case report
Akash Mathur , Piyush Mishra, Neha Nigam1, Uday C Ghoshal
Correspondence – Uday C Ghoshal – udayghoshal@gmail.com
Departments of Gastroenterology, and 1Pathology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India
Background Gastrointestinal mucormycosis, a rare fatal fungal infection in an immunocompromised host, commonly affects the stomach.
Case Report A 46-year-old female with long-standing diabetes mellitus, hypothyroidism, and hypertension, presented with a 3-month history of fecal discharge per vagina. She reported having intermittent loose stools, mixed with blood and mucus for 1.5 years. Based on the evaluation and unsuccessful treatment with anti-tubercular drugs elsewhere, Crohn’s disease was diagnosed, and Adalimumab biosimilar started; however, the response was partial. Examination revealed: pallor and large perianal tags. Investigations: Hb 9.4 g/dL, total serum protein, and albumin 5.5 and 2.8 g/dL, respectively. A computerized tomography (CT) scan with rectal contrast showed inflammatory involvement of the rectum and sigmoid along with a rectovaginal fistula. A magnetic resonance (MR) enterography showed a loss of haustrations in the transverse colon with a prominent vasa recta in the sigmoid colon. Colonoscopy showed loss of vascular pattern with pseudopolyps in the terminal ileum, IC valve, cecum, ascending, transverse, descending, sigmoid colon, and rectum; a fistulous opening was seen in the rectum. Descending and sigmoid colon biopsies revealed crypt distortion, mononuclear cell infiltrates in lamina propria, exudate with broad aseptate fungal hyphae suggesting mucormycosis. The serology for the human immunodeficiency virus was negative. With a diagnosis of colonic mucormycosis with fistulising Crohn’s disease, liposomal amphotericin B was started, but the patient succumbed. Conclusion: This rare patient highlights the need for increasing awareness about fungal infestations as a cause of disease flare in patients with inflammatory bowel disease.
Keywords Crohn’s disease, Mucormycosis, Inflammatory bowel disease
116
Small intestinal bacterial overgrowth in chronic pancreatitis: A systematic review and meta-analysis
Anshuman Elehence , Samir Mohindra, Uday C Ghoshal
Correspondence – Uday C Ghoshal – udayghoshal@gmail.com
Department of Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow 226 014, India
Introduction A number of mechanisms predisposes patients with chronic pancreatitis (CP) to small intestinal bacterial overgrowth (SIBO). Frequency of SIBO among patients with CP has been reported to vary between 0% and 92%. However, previous studies had limitations including high heterogeneity, inclusion of post-surgical patients with altered anatomy and inclusion of studies using lactulose hydrogen breath test (LHBT) for diagnosis of SIBO, which as several limitations.
Methodology An extensive literature search of specified databases was performed using a predefined search strategy for studies evaluating the SIBO in patients with CP. After exclusion of studies not fulfilling the predefined inclusion criteria or those meeting the exclusion criteria data were extracted for meta-analysis on prevalence of SIBO in those with and without CP and also among those with CP with or without alcoholic etiology, exocrine insufficiency and diabetes.
Results Among studies shortlisted for the analysis, SIBO was more commonly diagnosed in patients with CP compared to controls (Odds ratio [OR] 5.6; 95% confidence interval [CI] 2.7-11.5). However, there was no difference in frequency of SIBO among alcoholic as compared to non-alcoholic CP (OR 0.90 [95% CI 0.5-1.7]). SIBO was 2.4 (95% CI 1.4-4.2) and 2.7 (95% CI 1.4-4.2) times more common among those with diabetes and pancreatic exocrine insufficiency, respectively.
Conclusions Patients with CP have SIBO more commonly as compared to controls and the risk is more in patients with endocrine and exocrine insufficiency than those without and does not depend on etiology of CP.
Keywords Steatorrhea; Bloating; Bacterial overgrowth
Large intestine
117
Clostridioides difficile infection in patients with Corona Virus Disease-19
Mayank Jain
Correspondence – Mayank Jain- mayank4670@rediffmail.com
Department of Gastroenterology, Arihant Hospital and Research Centre, 283- A, Gumasta Nagar, Scheme 71, Indore 452 009, India
Background Frail individuals with long standing medical diseases are vulnerable to corona virus disease-19 (COVID-19) infection. Use of broad-spectrum antibiotics in these patients may be associated with subsequent increase in Clostridioides difficile infection (CDI)
Methods Retrospective analysis of cases with CDI detected between January and April 2021 in patients with COVID-19
Results Over the period of last 4 months (January 2021 to April 2021), the author encountered eight cases of CDI in patients who underwent treatment for COVID -19. In the previous 2 years (2019-2020), only one case of documented CDI was noted at our centre. A, all patients were above 45 years of age and predominantly females. All patients had one or more comorbid states. All patients had severe COVID-19 infection and required prolonged hospital stay. Broad spectrum antimicrobials, steroids, proton pump inhibitors and remdesivir were used in these patients. Six patients presented within one month of discharge from COVID care facility while two were diagnosed during hospital stay. The symptoms of CDI included-profuse diarrhea (8,100%), abdominal distention (2, 25%), anorexia (2, 25%) and nausea (2, 25%). Diagnosis was confirmed by stool test for C. difficile toxin assay in all cases and sigmoidoscopy showing pseudomembranes in 6 cases. One case had toxic megacolon and another case was on ventilation with inotropic support. All patients were started on antibiotics – metronidazole and vancomycin. Six cases who presented post discharge improved with treatment and were doing well on follow-up at 1 month. Two cases – one with toxic megacolon and other with multiorgan failure- succumbed to their illness.
Conclusion It is highly likely that cases of CDI are being under diagnosed and under-reported among COVID-19 patients. It is important to create an increased awareness regarding this issue and implement effective measures at local level to control this infection.
Keywords COVID, Intestine, Infection, Clostridium
118
A unusual presentation of rare disease as hematochezia
U S Manmohan , R S Arun, Nageswara Rao
Correspondence – Manmohan U S – manmohanus@gmail.com
Department of Medical Gastroenterology, Madras Medical Mission Hospital, 4-A, Dr, Mogappair, J J Nagar, Mogapair, Chennai 600 037, India
Introduction Primary amyloidosis of gastrointestinal (GI) tract is a rare presentation. In the GI tract, amyloidosis affects the duodenum most commonly, followed by the stomach and colorectum. GI bleeding due to AL amyloidosis is a rare phenomenon and has been reported in 10% to 40% of patients with GI involvement. GI amyloidosis presents as abdominal pain, gastroesophageal reflux disease-like symptoms, upper or lower GI bleeding, malabsorption, bacterial overgrowth, and diarrhea.
Case Report We here present a 66-year-old male known case of coronary artery disease (CAD) on antiplatelets presented with intermittent lower abdominal pain and hematochezia for 3 days. Colonoscopy showed multiple colonic ulcers, biopsy of ulcers showed features of amyloidosis. Biopsy reports were suggestive of secondary amyloidosis (AA type). He had significant proteinuria and renal core needle biopsy revealed mild medial hypertrophy of arteries and arterioles with deposition of extracellular eosinophilic material suggestive of amyloidosis. The presence of lambda light chain restriction by direct immunoflourensce studies favored primary amyloidosis. On further evaluation he was found to have plasma cell dyscariasis and was later started on 97atient97d97s97is9797t medications. Amyloidosis of GI tract presenting as lower GI bleed is a rare entity.
Conclusion The clinical presentation and high index of suspicion most essential, when patient has multisystem involvement to detect primary amyloidosis. Biopsy is of utmost importance in guiding the diagnostic evaluation along with other supportive investigations. Though the evaluation with intestinal biopsy alone would have been misleading regarding the type of amyloidosis in our case. On further evaluation, other features suggested towards systemic light chain related amyloidosis such as renal and bone marrow biopsy, guiding appropriate treatment plan. The biopsies of the rectal or small bowel mucosa or renal or biopsy of subcutaneous adipose tissue will help in diagnosis, as it will be positive in many patients with amyloidosis.
Keywords Hematochezia, Amyloidosis, Plasma cell dyscariasis
119
Endoscopic and histological correlation between sigmoidoscopy and colonoscopy in ulcerative colitis patients
Sameet Patel, Prasanta Debnath, Shubham Jain, Saurabh Bansal, Sanjay Chandnani, Qais Contractor, Pravin Rathi
Correspondence – Sameet Patel - sameetpat8@gmail.com
Department of Gastroenterology, T N M C and B Y L Nair Ch. Hospital, Room No 717, Department of Gastroenterology, 7th floor, OPD Building, Dr A Nair Road, Mumbai Central, Mumbai 400 008, India
Introduction Endoscopic remission is the current treatment target in ulcerative colitis (UC) patients. Literature on adequacy of sigmoidoscopy in comparison to pan colonoscopy in UC patients is sparse.
Methods It is an interim analysis of a prospective study of patients diagnosed with UC with disease extent proximal to the sigmoid colon. Twenty adult patients underwent a complete colonoscopy with segmental biopsies. Endoscopic disease activity was graded using Mayo Endoscopic Subscore and the histological grading was done using the Simplified Geboes Score (SGS). The maximum rectosigmoid disease activity was compared with the maximum disease activity in the rest of the colon.
Results Endoscopic Correlation: Sigmoidoscopic examination showed good correlation with pan colonoscopic examination for disease severity with a sensitivity of 87.5% and specificity of 75%. The accuracy of sigmoidoscopic examination for pancolonoscopic disease severity was 80% (95% CI – 57% to 100%).
Histological Correlation Rectosigmoid histological examination for SGS showed good correlation with SGS for biopsies from the proximal colon to diagnose severe pancolonic involvement with a sensitivity of 88.24%, specificity of 33.33% and an accuracy of 80%.
Conclusion In patients diagnosed with UC and having disease extent proximal to the sigmoid colon, sigmoidoscopic examination has good correlation with pan colonic examination for grading endoscopic and histological disease severity. A sigmoidoscopic examination is adequate to assess the disease severity in patients with disease extent proximal to the sigmoid colon.
Keywords Ulcerative colitis, Simplified Geboes score, Mayo endoscopic subscore
120
Intestinal amebiasis: A masquerade
Sameet Patel, Saurabh Bansal, Shubham Jain, Sanjay Chandnani, Sujit Nair, Pravin Rathi
Correspondence – Sameet Patel - sameetpat8@gmail.com
Department of Gastroenterology, T N M C and B Y L Nair Ch. Hospital, Room No 717, Department of Gastroenterology, 7th floor, OPD Building, Dr A Nair Road, Mumbai Central, Mumbai 400 008, India
Introduction Entamoeba Histolytica is a pathogenic protozoan endemic in the Indian subcontinent and can have protean presentation.
Methods We present a case series of 7 patients who presented with isolated bleeding per rectum (PR) in whom intestinal amebiasis was not initially suspected. None of the patients had fever and infectious colitis was not anticipated.
Results First case A 7-year-old male child who presented with bleeding PR and was suspected to have a juvenile rectal polyp.
Second case A 72-year-old female with ischemic heart disease who presented with bleeding PR and was suspected to have diverticular bleed or bleeding from angioectasia or ischemic colitis.
Third case A 69-year-old male who was suffering from COVID-19 infection, was on steroids and developed bleeding PR. Initial diagnosis was ischemic bowel disease.
Fourth case A 39-year-old male who presented with isolated bleeding PR. Imaging was suggestive of ileo-colonic tuberculosis or Crohn’s disease.
Fifth case A 45-year-old male who presented with large quantity bleeding PR. Suspected diagnosis was massive diverticular bleed.
Sixth case A 9-year-old male child who presented with bleeding PR and was suspected to have juvenile rectal polyp.
Seventh case A 85-year-old lady who presented with bleeding PR and initial diagnosis was diverticular bleed.
Diagnosis was established in all 7 cases after ileo-colonoscopy and histopathology.
On colonoscopy, all 7 patients had cecal ulcerations. Three had additional rectal ulcerations, while one had additional terminal ileal ulceration and one had ulcerations throughout the colon including rectum.
Histopathology showed typical amebic ulcers with trophozoites of Entameba histolytica.
All 7 patients recovered with metronidazole therapy.
Conclusions Intestinal amoebiasis can be a great 100atient100d100 and should be considered in the differential diagnosis of patients presenting with isolated bleeding per rectum in endemic countries like India.
Keywords Intestinal Amoebiasis, Bleeding per rectum, Entamoeba Histolytica
121
Management of irritable bowel syndrome in Indian patients with a fixed-dose combination of mebeverine hydrochloride and chlordiazepoxide
Nitesh Pratap1, Omesh Goyal2, Sumeet Jagtap3, Bhabadev Goswami4, Partha Pratim Kalita5
Correspondence – Nitesh Pratap – pratapnitesh@gmail.com
1Department of Gastroenterology, KIMS Hospitals, 1-8-31/1, Minister Road, Krishna Nagar Colony, Begumpet, Secunderabad 500 003, India, 2Department of Gastroenterology, Dayanand Medical College and Hospital, Tagore Nagar, Ludhiana 141 001, India, and 3Department of General Medicine, Sai Sneh Hospital and Diagnostic Centre, Pune-Satara Road, Katraj, Pune 411 046, India, 4Institute of Digestive and Liver Disease, Dispur Hospital Pvt Ltd, Ganeshguri, Guwahati 786 001, India, and 5Department of Internal Medicine, Doctor Chamber, Bamundi, Santipur, Guwahati 781 103, India
Aim To assess the effectiveness and safety of a fixed-dose combination of mebeverine hydrochloride 135 mg and chlordiazepoxide 5 mg in the management of irritable bowel syndrome (IBS) in Indian patients.
Methods This was an 8-week, prospective, open-label, observational study. Patients (n=60, age: 18-60 years), newly diagnosed with IBS and having anxiety symptoms (score =18 on Hamilton anxiety rating scale [HAM-A]), who were prescribed the study drug as a part of routine practice were included. The study drug dosage was thrice daily before food.
Results All 60 patients completed the study. Patients’ mean (SD) age was 37.45 (11.00) years; most were male (73.33%). The mean (SD) irritable bowel syndrome-symptoms severity scores (IBS-SSS) at baseline was 182.72 (84.39). The mean change in IBS-SSS scores from baseline at week 8 (primary endpoint) was -85.50 (82.69), p<0.0001, and at week 4 was -64.70 (58.44), p<0.0001. There was a notable decrease in scores from baseline at week 4 and at week 8 for each of the individual parameters assessed on the IBS-SSS scale (all p<0.0001). The mean (SD) irritable bowel syndrome-36 (IBS-36) score at baseline was 78.33 (41.87) and change from baseline at week 8 was -45.88 (34.92), p<0.0001. At week 8, majority of patients achieved a =50-point improvement in IBS SSS score (73.33%), and a =10-point improvement in IBS-36 score (88.33%). The mean (SD) HAM-A total score was 26.97 (6.72) at baseline and decreased to 10.45 (8.99) at week 8, p<0.0001. Three adverse drug reactions were reported in two patients: nausea in one patient and headache in both patients. All patients and investigators described “good” tolerability to study drug at week 8.
Conclusion The fixed-dose combination of mebeverine hydrochloride 135 mg and chlordiazepoxide 5 mg was well tolerated and effective in the management of symptoms related to IBS.
Keywords Fixed-dose combination, Irritable bowel syndrome, Mebeverine hydrochloride
122
Inflammatory bowel disease: Three decadal status and trends from global burden of disease study 2019
Khushdeep Dharni1, Sonika Sharma2, Arshdeep Singh3, Ramit Mahajan3, Vandana Midha4, Ajit Sood3
Correspondence – Ajit Sood - ajitsood10@gmail.com
1School of Business Studies, 2Department of Food and Nutrition, Punjab Agricultural University, Ludhiana 141 001, India, 3Department of Gastroenterology, and 4Medicine, Dayanand Medical College and Hospital, Tagore Nagar, Civil Lines, Ludhiana 141 001, India
Background Status and trends of disease related burden provide valuable information for effectively handling various dimensions of disease management and carving out suitable policy measures. Present study investigates Global Burden of Disease (GBD) 2019 study database to summarize and critically investigate the global burden of IBD.
Methods Using Log-Linear growth models, we have presented trends for three decadal data (1990-2019) for age standardized prevalence estimates, incidence estimates, disability adjusted life years (DALYs) and its components: years lived with disability (YLDs) and years of life lost (YLLs). We have also reported IBD related burden measures stratified across 15 macrogeographic regions, Socio-Demographic Index (SDI) based quintiles, gender and age.
Results On crude basis, globally the prevalence rate of IBD increased from 62.09 in 1991 to 63.30 in 2019. Age standardized IBD related prevalence and burden measures have shown a significant downward trend over the period of study. There are negative compound annual growth rates of 0.656% and 1.035% for prevalence and burden of disease respectively over the study period. There is a wide variation in burden estimates and their growth rates across regions and SDI based quintiles. Although the contribution of premature mortality to the burden of disease has come down over last 30 years, yet in 2019 it contributed about 56.33% to the disability adjusted life years. Incidence rate of IBD has fallen significantly in the age groups of more than 25 years but the same has remained stable for the age groups of less than 25 years. Australasia and Western Europe have high IBD prevalence and related disease burden, and contrary to global trends, these regions have exhibited significant positive growth trends.
Conclusions The findings highlight widespread variations in all IBD related burden measures across regions. For better management of IBD, there is a need for localized research and policy measures.
Keywords Inflammatory bowel disease, epidemiology, quality adjusted life years
123
A rare cause of bleeding colonic ulcers: Case report
U S Manmohan, R S Arun, Nageswara Rao, Ramya Mamidipalli
Correspondence – Manmohan U S – manmohanus@gmail.com
Department of Medical Gastroenterology, Madras Medical Mission Hospital, 4-A, Mogappair, Chennai 500 037, India
Introduction The common causes of bleeding colonic ulcers includes dieulafoy lesions, solitary rectal ulcer syndrome, stercoral ulcers, ischemic colitis, diversion colitis, inflammatory bowel disease (IBD) and endometriosis. Amyloidosis of gastrointestinal (GI) tract presenting as lower GI bleed is a rare entity. GI bleed4ng due to AL amyloidosis is a rare phenomenon, and has been reported in 10% to 40% of patients with GI involvement.
Case report A 66-year-old gentlemen with previously diagnosed coronary artery disease on antiplatelets presented with intermittent lower abdominal pain and hematochezia for 3 days. Colonoscopy revealed diffuse linear ulceration and a few deep necrotic ulcers throughout the transverse and descending colon; diffuse erythema and erosions in rectum. Biopsy of ulcers revealed amyloidosis. Initially biopsy was reported as secondary amyloidosis (AA type) since submucosal vessel thickening with salmon red colored material and apple green birefringence with congo red stain were noted. He also had significant proteinuria; renal core needle biopsy revealed mild medial hypertrophy of arteries and arterioles with deposition of extracellular eosinophilic material suggestive of amyloidosis. The presence of lambda light chain restriction by direct immunoflourensce studies favored a revised diagnosis of primary amyloidosis. On further systemic evaluation he was found to have plasma cell dyscariasis and was initiated on immunosuppresants. Amyloidosis of GI tract affects the duodenum most commonly, followed by the stomach and colorectum. GI amyloidosis presents as abdominal pain, gastroesophageal reflux disease-like symptoms, upper or lower GI bleeding, malabsorption, bacterial overgrowth, and diarrhea.The mechanism of GI bleed in amyloidosis is believed to be due to thickening and calcification of the mesentry, peritoneum and retroperitoneum causing GI ulcers with bleeding.
Conclusion A high index of suspicion is necessary to diagnose primary amyloidosis. This case report illustrates the importance of obtaining biopsy in the evaluation of bleeding colonic ulcers. Amyloidosis, being a multisystem disease, its detection in the GI tract should prompt one for careful evaluation of other systems as well.
Keywords Hematochezia, Amyloidosis, Colonic ulcers
124
Gaps in optimal use of biologic therapy in inflammatory bowel disease patients at tertiary care centre in developing country- A gap analysis
Aditya Kale, Leela Shinde, Mayur Satai, Sridhar Sundaram, Akash Shukla
Correspondence – Aditya Kale – adityapkale@yahoo.com
Department of Gastroenterology, Seth G S Medical college and KEM Hospital, Multistoried Building, 9th Floor, Acharya Donde Marg, Parel. Mumbai 400 012, India
Background and Aims Inflammatory bowel disease (IBD) is chronic relapsing disease requiring life-long therapy. Biologics are often required for induction and maintenance of remission. Treatment discontinuation often occurs. We decided to analyse gaps in optimal use of biologics.
Methods Patients eligible for biologic therapy were selected from prospectively maintained IBD database. Coverage gap is a gap between number of patients prescribed biological therapy and number of patients eligible for therapy measured by screening rate and 1st dose received rate. Retention gap denotes difference between the number of patients actually on biologic therapy at a given point to number of patients expected to be on biologic therapy measured by medication possession rate, discontinuation rate. Wellness gap is defined as patients on biologic therapy with remission with or without adequate quality of life as per IBDQ-32 questionnaire.
Out of 540 patients, 150 (27.77%) eligible patients with complete record were identified. Screening rate was 100%. First dose received rate was 55.33% (83/150). Sixty-seven (44.66%) cases fall in the coverage gap due to financial constraints (90%), drug non-availability (5%) and 5% selected surgery/clinical trial as option. Out of 83 patients started and maintained on biologics 44 (53.01%) had medication possession rate >80%. Thirty-nine (46.98%) could not be ‘retained’ in maintenance phase due to financial constraints (20, 51.28%), discontinuation due to remission (10, 25.64%), surgery (6, 15.38%), clinical trial (3, 7.6%) suggestive of ‘retention gap’. Out of 44 patients on maintenance, 38 (86.36%) were in clinical remission and 35 (80%) were satisfied and happy as per IBDQ-32 questionnaire. Out of remaining 9 (20%) patients, 6 had response loss and 3 had tuberculosis. Out of 150, 38 (25.33%) were in remission. Thirty-five (23.33%) had good quality of life (QOL).
Conclusion Financial constraints and high cost of biologic therapy are responsible for significant coverage and retention gaps. Low cost effective therapies may help to reduce these gaps.
Keywords Inflammatory bowel disease, Gap analysis, Biologics
125
Endoscopic appearance among patients with chronic diarrhea in a urban tertiary care centre
Chittuluri Jagadeesh
Correspondence – Chittuluri Jagadeesh – doctorjd18@gmail.com
Institute of Medical Gastroenterology, Madras Medical College and Rajiv Gandhi Government General Hospital, Poonamallee High Road, Park Town, Chennai 600 003, India
Backgrounds and Aims Chronic diarrhea is defined as abnormal stool weight, consistency and/or frequency, that last for at least four weeks. There are many possible causes of chronic diarrhea. Chronic diarrhea treatment seeks at eliminating the underlying cause, strengthening bowel movements, and treating any problems associated with diarrhea. Endoscopy plays an important role as a chronic diarrhea diagnostic instrument. This paper provides a preliminary study of chronic diarrhea based on endoscopy appearance in adults.
Methods A cross sectional study was conducted at Madras Medical College in Chennai. Data of their demographic profiles and endoscopy were recorded from medical record.
Results Two-hundred and seventy patients were included in this study from January 2021 – September 2021. Median age was 54 years old (range 19 to 84 years old). The amount of male and female patients doesn’t differ. The most common diagnosis of chronic diarrhea is inflammatory bowel disease (67.2%), followed by cancer (22.6%). Among of those patients with cancer, there are 63.6% with rectal cancer and 36.4% with colon cancer. Of those with diarrhea, there are twelve patients with tuberculous colitis who were all patients with human immunodeficiency virus (HIV) infection. The remainder of these patients with chronic diarrhea were radiation colitis with cervical cancer as underlying disease.
Conclusion Chronic diarrhea can affect the quality of life and general health considerably. Chronic diarrhea patients generally require some assessment, but in some cases history and physical examination may be adequate to direct treatment. Diet, medicines, and surgery or radiation therapy can be significant causes of chronic diarrhea that can be suspected from history alone. Endoscopy and biopsy is valuable for the diagnosis of chronic diarrhea.
Keywords Chronic diarrhea, Endoscopy, Biopsy
126
An immunohistochemical study of nerve growth factor in myenteric neurons of colorectal adenocarcinoma tissues in humans
Asha Gupta 1 , Seema Singh 2 , Esha Singh 2 , Prasenjit Das 3 , Sujoy Pal 4 , Gyan Prakash Gupta 5 , Saba Sarwar 2 , Javed A Quadri 2 , A Shariff 2
Correspondence – Asha Gupta – gasha5207@gmail.com
1Department of Anatomy, V M M C and Safdarjung Hospital, New Delhi110 049, India, 2Departments of Anatomy, 3Pathology, and 4Gastrointestinal Surgery, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India, and 5Department of ENT, D D U Hospital, Krishna Vatika, Gautam Nagar, Delhi 110 049, India
Introduction Colorectal carcinoma (CRC) is the third most common cancer of gastrointestinal tract in the world. Ninety percent CRC develops are mainly adenocarcinoma. Nerve growth factor (NGF) is significant for the development and phenotypic maintenance of neurons. There is a major utility of NGF in maintenance of visceral integrity. The function of NGF in gastric cancer and ulcerative colitis have been reported but in colorectal carcinoma is still unidentified.
Aim Immunohistochemical study of nerve growth factor in myenteric neurons of the colorectal adenocarcinomatous tissues in humans.
Methods Thirty specimens collected for this study. 20 specimens from patients undergoing surgery for colorectal adenocarcinoma in department of gastrointestinal surgery and 10 specimens of normal colonic tissues collected from department of forensic medicine, All India Institute of Medical Sciences, New Delhi. It was approved by the Institutional Ethical Clearance Committee of All India Institute of Medical Sciences, New Delhi. Tissues were processed and 3 μm thick sections used for H&E and immunohistochemistry (anti-NGF antibody: neuronal marker used).
Results H&E stained sections showed decrease in the myenteric neurons with increasing grades of colorectal carcinoma and immunohistochemistry showed the increasing expression of anti-NGF antibody with increasing grades of colorectal adenocarcinoma as compared to normal human colonic tissue.
Conclusion NGF may have profound effects on enteric neurophysiology and emphasizes the importance of increasing the current understanding in maintenance of enteric nervous system.
Keywords Myenteric neurons, Nerve growth factor, Colorectal carcinoma
127
Delayed manifestations of colonic mucormycosis in severe corona virus disease 2019
Ravi Shankar Bagepally, Vijay Rampally
Correspondence – Ravi Shankar Bagepally – b_ravishankar@yahoo.com
Department of Gastroenterology, Yashoda Hospitals, Alexander Rd, Kummari Guda, Shivaji Nagar, Secunderabad 500 003, India
Mucormycosis is a rare, devastating fungal infection of humans and usually affects immunosuppressed individuals. The corona virus disease 2019 (COVID-19) pandemic has affected millions of people and caused significant mortality in severely diseased subjects. During the second wave of pandemic in India (2021), Mucormycosis has surfaced as a significant opportunistic infection. Gastrointestinal mucormycosis is rare and the usual presentation is gastrointestinal (GI) bleed. We present two cases of colonic mucormycosis with manifestation of colonic bleed and colonic perforation.
Diagnosis of these cases was made by KOH stain on endoscopic biopsies and histopathology at surgery. Both patients had severe COVID infection. Systemic antifungal therapy did not benefit any of the patients. Both patients underwent surgery at a later stage of disease.
There could be a significant number of patients with COVID in whom GI mucormycosis might have been overlooked.
High suspicious and early endoscopy in COVID patients with bleed, abdominal pain or late onset diarrhea may be helpful in quick diagnosis and probable recovery, if treatment is instituted before it is late.
Keywords GI bleed, Perforation, Colitis
128
Profile of colonic polyps in North Indian population
Anurag Mishra
Correspondence – Anurag Mishra – dr.anuragmishrakgmc@gmail.com
Department of Gastroenterology, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, 1, Jawaharlal Nehru Marg, New Delhi 110 002, India
Introduction Data on the prevalence and distribution of colonic polyps in Indian/Asians is limited. To study this, we conducted a retrospective study on 202 polyps out of 7936 colonoscopies.
Method The objective was to analyse demographic, clinical, endoscopic and histopathological characteristics of polyps in patients undergoing colonoscopy from 2016 to 2019 at GIPMER, New Delhi. All polyps were removed colonoscopically by polypectomy and specimen were sent for histopathological examination. Parameters like age, gender, symptoms, site, gross morphology, and histological subtypes of polyps were assessed.
Result Total 7936 colonoscopies were performed in this period. Polyps were seen in 202 patients. Mean age was 23 years. 72% were males. 82% were below 40 years and 18% were above 40 years of age. 69% polyps were found in rectum. 63% polyps were juvenile, 10% Peutz-Jeghers, 17% adenomatous, 3% inflammatory and 7% others. Mean age of adenomatous polyp was 48 years. 66% polyps were pedunculated. 51% polyps were less than 1 cm. 81% patients presented with bleeding P/R. 78% of adenomatous polyps were dysplastic. Out of adenomatous polyp 44% were tubular, 34% 106atien-villous and 22% villous.
Conclusion Frequency of polyps on colonoscopy at our centre was 2.5%. Most common type was juvenile polyp. Polyps were more common in younger age group. Adenomatous polyps were common in middle to old age group. Most polyps were small, pedunculated, and located in rectum. Tubular was most common type of adenomatous polyp. Dysplasia was more common in villous type.
Keywords Polypectomy, Peutz-Jeghers, Dysplastic polyp
129
Corona virus disease 2019 (COVID-19) pandemic and inflammatory bowel disease from patients’ perspective – A survey from COVID epicenter in India
Aditya Kale , Leela Shinde, Sridhar Sundaram, Biswa Ranjan Patra, Praveen Kumar Rao, Mohd Irtaxa, Akash Shukla
Correspondence – Aditya Kale – adityapkale@yahoo.com
Department of Gastroenterology, Seth G S Medical College and K E M Hospital, Mumbai, Multistoried Building, 9th Floor, Acharya Donde Marg, Parel. Mumbai 400 012, India
Background and Aims The corona virus disease (COVID) pandemic and countrywide lockdown has had significant impact on patients with inflammatory bowel disease (IBD), with delay in diagnosis, difficulty in access to healthcare and unavailability of drugs. We conducted a telephonic survey to assess this impact.
Methods Out of 350, 302 participated in the survey. Demographic data, disease severity at the time of survey, extent of disease, details of therapy and adherence were noted. A validated questionnaire addressing information source, perception of COVID-19 situation, contact with healthcare, adherence to standard precautions was administered telephonically.
Results Out of 350 contacted patients, 302 (86.28%) patients participated in the survey. Median age of cohort was 39 years. Ulcerative colitis (UC) constituted 79%, 16% Crohn’s disease (CD) and 5% IBD-unclassified. At the time of survey, 86.98% patients with UC were in clinical remission and 75.75% of CD patients were generally well. One hundred and fifteen (38%) cases were nonadherent to therapy due to unavailability of medicines (66.38%), financial constraints (25.21%) inability to reach healthcare facility (3.6%). Disease flare was seen in 14.2% correlated well with nonadherence. Existing drug therapy was switched to alternative drug in 70 (23.17%) cases due to unavailability (74%). Social media (52.3%) and television (40.4%) were the common sources of information about the pandemic. Telemedicine platforms (WhatsApp and telephone) were used by 180 (59.6%) patients for consultation with good acceptance (81.6%). Eighty-seven (28.8%) patients failed to contact healthcare. Apprehension regarding severe Covid infection was noted in 80% while 29% thought that IBD therapy could increase infection risk. Adherence to wearing mask, hand washing, and social distancing was 100%.
Conclusion Pandemic resulted in disruption of healthcare visits and medication supply. Majority were concerned about increased risk of COVID-19 infection and adhered to standard precautions. Mobile phone-based formats for patient care may be an alternative due to patient acceptance and convenience.
Keywords COVID-19 pandemic, Inflammatory bowel disease, Adherence, Telemedicine
130
Gastroinestinal mucormycosis in a corona virus disease 2019 patient- A case report
Dhruv Shah, Kaushal Vyas
Correspondence – Kaushal Vyas - gastro.svp@gmail.com
Department of Gastromedicine, NHL Medical College, Pritan Rai Cross Road, Ellise Bridge, Paldi, Ahmedabad 380 006, India
Introduction The novel corona virus disease 2019 (COVID-19) is a potential devastating disease with varying presentation from asymptomatic to critically ill patients. Patients are susceptible to fungal and bacterial infections due to low immunity. Mucormycosis is life threatening fungal disease with propensity to vascular invasion by hyphae, causing ischemic necrosis to tissue it invade.
Case Study A 60-year-old male patient presented to us with c/o fever, abdominal pain, hematochezia from 1 day. Patient was treated at some hospital for breathlessness, fever, sore throat 10 days ago and was found to be COVID-19 positive and treated there with meropenem, oseltemavir and hydrocortisone and discharged. Patient again came to our emergency, was admitted. Repeat throat swab was done, found to be COVID-19 positive. Urgent colonoscopy was done s/o giant ulcer with debris and active bleeding in ascending colon, biopsy examination confirmed mucormycosis after confirmation on biopsy Amphotericin was prescribed as per standard dose with gradual improvement in clinical condition.
Discussion Patients with COVID-19 has higher level of inflammatory markers such as IL-6, IL -10, with impairment in cell mediated immunity. There is current protocol of using steroids to prevent or treat cytokine storm to prevent further complications, but this leads to increased risk of fungal infections. Mucormycosis causes ischemia and necrosis by hyphae invasion. GI involvement from stomach to rectum can be seen in 5% to 8% of cases. Disease has high mortality and diagnosis is based on biopsy confirmation of typical fungal hyphae from specimen obtained during surgery or endoscopy. Treatment consists of early antifungal with surgical resection of involved part.
Conclusion Although GIT Mucormycosis is a rare disease due to decreased immunity. High clinical suspicion with early intervention is required to prevent further complications in COVID-19.
Keywords COVID -19, Overuse of steroids, GI mucomycosis
131
Case of primary signet ring cell carcinoma of rectum with vascular calcifications
Vijaylaxmi Biradar, B Ramesh Kumar, L Sahitya
Correspondence – Vijaylaxmi Biradar – dr.viju21@yahoo.in
Department of Gastroenterology, Osmania General Hospital, Afzalgunj Road, Afzal Gunj, Hyderabad 500 001, India
Primary signet ring cell carcinoma of the rectum (PSRCCR) is a rare variant of colorectal adenocarcinoma (AC) with incidence of less than 1%, containing > 50% of cells with prominent intracytoplasmic mucin with marked nuclear displacement and molding (signet ring cells) and presents at an advanced stage. The tumor has a distinctive molecular pattern and poor prognosis as it presents as diffuse infiltration and circular thickening of the bowel wall, also called “colonic linitis plastica.”
Case Report A 20-year-old female born out of nonconsanguineous marriage with hematochezia, pain abdomen since 3 months, tenesmus and loss of appetite since 3 months. There are no affected relatives due to colonic cancer in family. On examination patient is pale. Per abdomen examination was normal except with mild tenderness in left iliac and lumbar region.
Investigations Laboratory examination shows Hb:9.1g/dL, MCV:82.1fL, TLC:4100/microL, platelet: 2.11Lakhs, ESR: 40 mm/hr, CRP was negative. Contrast CT abdomen shows homogenous smooth circumferential thickening with enhancement of rectum for length of 8 cm with 24 mm thickness causing luminal narrowing with transverse and descending colon dilatation of 5 cm with evidence of hyperdense linear branching foci noted in right pararectal region likely vascular calcifications extending into rectal wall suggestive of phlebosclerosing colitis. Upper GI endoscopy was normal, but sigmoidoscopy shows presence of circumferential edema, erythema, ulceration, wall thickening, friability and spontaneous bleeding from 5 to 10 cm from anal verge, causing luminal narrowing. Biopsy reveals sheets of signet ring cells, infiltrating into lamina propria with extracellular mucinous material suggestive of poorly differentiated adenocarcinoma, signet ring cell type.
Conclusion Primary signet ring cell cancer in young females being rare in rectum with no family history is a distinct entity and imaging evidence of vascular calcifications in mucosal wall with thickening can be a early sign in signet ring cell carcinoma and may indicate poor prognosis
Keywords PSRCCR, Vascular calcifications
132
Colonic polyps and metabolic syndrome: Is there a relation?
Nutan Desai, Hozefa Runderawala, Hardik Shah, Neha Bhave
Correspondence – Nutan Desai – nchopda@yahoo.com
Department of Gastroenterology, Fortis Hospital Mulund, Mulund Goregaon Link Road, Nahur West, Mumbai 400 078, India
Aim To study prevalence of polyps detected during colonoscopy and its association with metabolic syndrome in an urban cohort.
Introduction Recent data has suggested that incidence of colonic polyps has markedly increased in the last 2 decades in Asia- Pacific region and so is metabolic syndrome which is linked to high fat, high protein diet and lack of physical exercise. Colonic polyps are increasingly being detected in Indian population undergoing colonoscopy. The association between colonic polyps and metabolic syndrome is still controversial. We aim to study the prevalence of polyps detected during colonoscopy and its association with metabolic syndrome.
Methods Two hundred consecutive cases of colonoscopy were selected. Patients more than 18 years of age posted for colonoscopy were included and those with history of colonic disease such as inflammatory bowel disease, previously diagnosed adenomas, colorectal cancer, family history of adenomas or colorectal cancer were excluded. The prevalence of polyps detected among colonoscopy was calculated. Polyps were classified according to site, size, number and histopathology.
Results Of 200 cases, polyps were detected in 41 patients and of these 31 pts fulfilled criteria for metabolic syndrome. In remaining 159 patients without colonic polyps 29 had metabolic syndrome. Statistical analysis showed prevalence of colonic polyps in sample population at 20%. Polyps were most commonly found in left colon and were predominantly adenomatous in nature. Prevalence of metabolic syndrome was found to be 30%. Also, upon applying Chi-square test for Yates’s correction the association between the occurrence of polyps and that of metabolic syndrome is found to be statistically significant (p value =0.00001).
Conclusion Our study shows statistically significant association between occurrence of colonic polyps and presence of metabolic syndrome, further multicentric studies are required to validate our finding and to make recommendations for the screening in this population.
Keywords Colonic polyp, Metabolic syndrome.
133
Clinical features and colonoscopic findings in patients with radiation proctitis
Vishnupriya Rajagopal, A R Akilandeshwari, A Anand, N Arun, Kani Shaikh Mohamed
Correspondence – Vishnupriya Rajagopal – drvishnupriyaprashanth@gmail.com
Department of Digestive Health and Diseases, Government Kilpauk Medical College, Royapuram, Chennai 600 013, India
Background and Aims This study aims to assess the clinical features and colonoscopic findings in patients with radiation proctitis after radiotherapy for pelvic malignancy.
Methods This was an observational cross sectional study conducted in Department of Digestive Health and Disease, attached to Kilpauk Medical College over a period of 1 year. A total of 28 patients above the age of 18 years who received radiotherapy for pelvic malignancies were included in this study. Clinical features and colonoscopic findings were assessed in those patients. Vienna Rectoscopy Score (VRS) was used to describe the colonoscopic findings and was compared to the European Organization for Research and Treatment of Cancer (EORTC)/Radiation Therapy Oncology Group (RTOG) morbidity score for clinical features.
Results A total of 28 patients of age ranging (30-55) were included. Mean interval between radiotherapy and presenting symptoms was 15 months. Sixteen patients had carcinoma cervix and rest had carcinoma endometrium, prostate, and rectum. Twenty-two patients received radiation dose of 45-70 Gy,7 above 70 Gy. The most frequent symptom observed was rectal bleeding in 21 patients, bowel habit change in 4 patients and mucous stools in 3 patients. Colonoscopic findings were congested mucosa in 18 patients, telangiectasia in 8 patients. Ulcerations in 2 patients. Eighteen patients (VRS score >grade 2) had morbidity score greater than grade 2. The VRS significantly correlated with EORTC/RTOG score (p = 0.038).
Conclusion In conclusion, rectal bleeding was the most frequent symptom in RT induced proctitis followed by bowel habit change. Congested mucosa and telangiectasias were the most prevalent colonoscopic findings in RT induced proctitis. Vienna rectoscopy scoring significantly correlated with EORTC/RTOG morbidity score.
Keywords Radiation, Proctitis, Rectal bleeding
134
Comparative analysis of gene expression in blood and colonic tissue of ulcerative colitis
Ajay Oli1, Rohit N Maidur2, Anita P Javalgi3, Preetham S Hurakadli2, Palaksha K Javaregowda1, Apoorva Jain1
Correspondence – Ajay Oli – ajay.moli@gmail.com
Departments of 1Biomedical Science, 2Gastroenterology, 3Patholoy, SDM Research Institute for Biomedical Sciences, Shri Dharmasthala Manjunatheshwara University, 5th Floor, Specialty Block, Manjushree Nagar, Sattur- Dharwad 580 009, India
Background Inflammatory bowel disease (IBD) includes Crohn’s disease (CD) and ulcerative colitis (UC) cause gut tissue chronic inflammation, has no cure, and requires life-long therapy. UC is a chronic relapsing-remitting disease of the large intestine that is associated with both genetic and environmental risk factors. UC is characterized by inflammation of the mucosa and sub-mucosa, a loss of epithelial barrier integrity, and dysregulated immune responses.
Aim The aim of this study is to analyze a gene expression level in a blood sample and the colonic mucosa of UC patients.
Methodology We studied a total of 20 patients with a definitive diagnosis of UC and the control group (20 subjects) without endoscopic evidence of intestinal inflammation. Peripheral blood samples and colonic mucosal biopsies were collected by venipuncture and colonoscopy procedures, respectively. Then the total RNA was extracted by using Trizol method and genes, IDO-1, TNFβ, IFNα, IL-6 expression was analyzed by quantitative real-time polymerase chain reaction (qrtPCR).
Results The study demonstrated the significant difference in genes, IDO-1, TNF-β, IFNα, IL-6 expression in both blood and tissue biopsies of UC patients as compared to the control. Furthermore, this preliminary study also demonstrated the importance of sample type, blood vs. tissue in studying the biomarkers for diagnosis of UC.
Conclusion The expression of marker genes is associated with the clinical course and histological deviations and are of relevance since they define the usefulness of markers in diagnosis of UC. The result indicates the possible involvement of genes, IDO-1, TNF-β, IFNα, IL-6 in pathogenesis of UC. The comparative analysis indicates the similarity in marker gene expression in blood and tissue biopsies of UC patients. Hence, the blood sample could be a potential substitute for tissue biopsies for early diagnosis of ulcerative colitis.
Keywords IBD, UC, qRTPCR, Gene expression, mRNA
135
Clostridioides difficile infection in severely ill corona virus disease 2019 patients
Pankaj Nawghare, Shubham Jain, Sanjay Chandnani, Saurabh Bansal, Siddhesh Rane, Prashanta Debnath, Pravin Rathi
Correspondence – Pankaj Nawghare – pankaj9ghare21@gmail.com
Department of Gastroenterology, Topiwala National Medical College, B Y L Nair Ch. Hospital, Mumbai 400 008, India
Introduction Clostridioides difficile infection (CDI) is common with the widespread use of broad-spectrum antibiotics in the corona virus disease 2019 (COVID-19) pandemic. There is an overlap of GI symptoms between these two infections.
Method We have screened severely ill COVID-19 patients with persistent diarrhea for CDI. Stool assay for GDH and stool enzyme immunoassay for toxin were screening and confirmation test respectively.
Results Among, 32 screened patients, we have identified eleven patients with CDI co-infection. All patients had persistent diarrhea as presenting complaints. However, 6 patients complained of bloody diarrhea. Other clinical features include- fever in 4 patients and abdominal pain in 2 patients. The most commonly used antibiotic was ceftriaxone. Severe CDI was noted in 8 patients. All patients with severe CDI were on steroids. Colonoscopy was done in 7 patients, which revealed erythematous mucosa in all patients, focal pseudo-membrane in 3 patients, and diffuse pseudo-membrane in 1 patient. Histology revealed predominant neutrophilic infiltrate in all patients. Computed tomography was done in 4 patients- all patients had diffuse bowel wall thickening. The accordion sign was seen in 2 patients. All patients received the standard medical line of management. Three patients with mild CDI improved with antibiotics. However, 1 patient succumbed to respiratory complications. Five patients with severe infection succumbed- 3 due to C. difficile related complications, one each due to respiratory failure and multi-organ dysfunction.
Conclusion CDI in COVID-19 patient may be challenging, and needs high degree of suspicion. Judicious use of antibiotics is advisable in COVID-19 hospitalized patients.
Keywords COVID-19, Cl. difficile, Antibiotics
136
Vitamin-D level in patients of acute severe ulcerative colitis
Uday Vadicherla, Muthu Kumaran, Prem Kumar, Caroline Selvi, Sir Aravind, I Shubha, R Murali, A Chezhian
Correspondence – Uday Vadicherla – uday.vadicherla@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Near Park Town Station, Park Town, Chennai 600 003, India
Introduction Vitamin D plays a primary role in calcium, phosphorus and bone metabolism. However, the discovery of vitamin D receptors on lymphocytes, monocytes, and dendritic cells initiated various studies which have highlighted the role of vitamin D in regulating gut mucosal immunity and gut barrier. Ulcerative colitis (UC) is characterized by an inappropriate and exaggerated mucosal immune response to gastrointestinal antigens in genetically susceptible individuals. This study done to detect vitamin-D deficiency in severe ulcerative colitis patients and find any relationship with vitamin-D deficiency and severity of ulcerative colitis.
Methods Twenty-five patients of acute severe colitis patients were taken in to study and vitamin-D levels was measured. They were divided in to 4 groups based on vitamin-D level as severe vitamin D deficiency (< 12 ng/mL), mild to moderate deficiency (12 to 19 ng/mL), insufficiency (20 to 29 ng/mL), and suboptimal levels (29 to 40 ng/mL).
Results Out of 25 patients vitamin-D level <12 ng/mL present in 11 (44%) patients, 12-19 ng/mL present in 8 (32%) patients, 20-29 ng/mL present in 5 (20%) patients and 30-40 ng/mL present in 1 (4%) patients.
Conclusion In this study all patients included in the study had vitamin-D deficiency. Further studies required to demonstrate its therapeutic and preventive role in exacerbations of ulcerative colitis.
Keywords Vitamin-D, Ulcerative colitis, Immune response
137
Extensive deep vein thrombosis as the initial presentation of colorectal cancer: A case report
H Vijay Narayanan, David Mathew Thomas, N Premaletha, Krishnadas Devadas
Correspondence – Vijay Narayanan H – vijaynh@gmail.com
Department of Medical Gastroenterology Government Medical College, Super Specialty Block, Trivandrum 695 011, India
Introduction Malignancy is a hypercoagulable state. Carcinoma of pancreas, stomach, and lung are commonly associated with venous thromboembolism (VTE). Colorectal carcinoma (CRC) is a very rare cause of VTE with a two year cumulative incidence of 3%. We present a case of extensive unprovoked DVT as the initial presentation of colonic malignancy.
Case Summary 54-year-old male, farmer, with no prior comorbidities or addictions, presented with insidious onset of dull aching pain in left thigh. He had no upper GI or lower GI symptoms. Examination revealed bilateral calf tenderness. Venous doppler was suggestive of extensive DVT of both lower limbs. He was started on warfarin after bridging with heparin. While on adequate anticoagulation, he developed new onset pain in his right arm and was diagnosed to have cephalic vein thrombosis. He was evaluated in view of extensive unprovoked DVT. Thrombophilia workup was negative. Ultrasound abdomen showed multiple hypoechoic focal lesions in both lobes of liver. Upper GI endoscopy was normal. Tumor markers revealed elevated CEA with normal AFP. CECT abdomen showed multiple liver metastases and a short segment circumferential wall thickening of distal transverse colon. Colonoscopy revealed ulceroproliferative growth in mid-transverse colon with luminal narrowing. Histopathology confirmed a colonic malignancy.
Discussion There is a synergistic relationship between cancer biology and the clotting system. In colorectal carcinoma, there can be upregulation of the clotting system with tissue factor (TF) being abnormally expressed on tumor cells. TF positivity correlates with TNM stage and hepatic metastasis. Clot formation surrounding metastatic cells in the bloodstream may allow them to escape immune surveillance to form distant metastatic deposits. Our patient had CRC with hepatic metastasis presenting as DVT.
Conclusion In extensive unprovoked DVT, in middle aged men, search for underlying malignancy even if patients do not have any symptom to suggest a colorectal carcinoma.
Keywords Colorectal cancer, Deep vein thrombosis, VTE
138
Comparison of Mayo endoscopic score and ulcerative colitis endoscopic Index of severity score with histological activity in ulcerative colitis
Ramalingam Rajendiran , Pazhanivel Mohan
Correspondence – Pazhanivel Mohan – dr.pazhan@gmail.com
Department of Medical Gastroenterolog, Jawaharlal Institute of Postgraduate Medical Education and Research, Dhanvantri Nagar, Gorimedu, JIPMER Campus, Puducherry 605 006, India
Introduction Endoscopic and histological remission are the desirable targets in ulcerative colitis (UC) for achieving better long-term outcomes. The aim of the present study was to compare the correlation of Mayo endoscopic score (MES) and Ulcerative Colitis Endoscopic Index of Severity (UCEIS) score with histological activity in UC.
Methods This is a longitudinal follow-up study conducted between September 2018 and February 2020 including patients with newly diagnosed acute UC or a flare of pre-existing UC. The disease activity was assessed using clinical, colonoscopy (MES and UCEIS) and histopathology (Geboes [GS] and Robarts histopathology index [RHI]) at baseline and at clinical remission. The correlation of MES and UCEIS with histology was done using spearman correlation coefficient at clinical remission.
Results A total of 43 patients were studied. The mean age was 36 ± 10 years with a slight male predominance. At clinical remission, 79% (34/43) achieved endoscopic remission by MES while 56% (24/43) achieved by UCEIS. Histological remission was achieved by 42% (18/43) and 40% (17/43) by GS (≤12) and RHI (≤3) respectively. There was a weak correlation of MES with both GS (rho=0.312, p=0.04) and RHI (rho=0.375, p=0.01). Correlation of UCEIS with GS was weak (rho=0.327, p=0.03), however there was moderate correlation with RHI (rho=0.44, p=0.003).
Conclusion Our study showed that the currently available endoscopic scores (MES and UCEIS) have only a weak to moderate correlation with histological activity. Hence, a biopsy is required to confirm the presence of an underlying inflammation even in those who have endoscopic remission.
Keywords Endoscopic activity, Geboes score, Robarts histopathologic index, Ulcerative Colitis
139
Arteriovenous malformation of rectum-Case report
Paila Ramesh
Correspondence – Paila Ramesh – pailaramesh549@gmail.com
Medical Gastroenterology, Madras Medical College, Near Park Town Station, Park Town, Chennai 600 003, India
Introduction There are many case reports on AV malformations of gastrointestinal (GI) tract. Most of the AVMs of GI tract occur in right side of colon, but it is very rare to observe AVMs in rectum.
Here we report a case of 22-year-old female with past history of pulmonary tuberculosis completed ATT for 6 months presented to our hospital (RGGGH, Chennai) with on and off bleeding per rectum from the age of 11 years, on examination patient had clinical pallor, no other findings, patients’ investigation showed Hb 5.1 gm% (severe anemia), initially treated with 3 units of PRBCs. CECT abdomen showed diffuse circumferential wall thickening with submucosal edema noted in rectum (maximum thickness of 2.1 cm). Multiple prominent vessels noted with in the rectal wall showing enhancement in the arterial phase. The inferior mesenteric artery is mildly dilated. The inferior mesenteric vein is dilated and shows early enhancement in arterial phase. colonoscopy showed submucosal tumor like lesion in distal rectum, but not tumor. Ulcer like erosions were observed on elevated lesion. Biopsy from ulcer like erosions showed colonic mucosa with preserved architecture showing ulceration, fibro muscular hyperplasia in lamina propria and scant inflammation with no evidence of dysplasia or malignancy. DSA showed hypertrophied IMA dividing into right and left branches. Large, hypertrophied vessels are noted in rectum on either side with rapid AV shunting from right side. These vessels selectively catheterised and embolised with coils and gel foam to reduce pressure head and bleeding. Control angiogram revealed complete obliteration of flow. Embolization was performed to control bleeding and to avoid surgery. After embolization she was followed up for 4 months in our hospital without recurrence.
Conclusion Here we seen a rare case of rectal AVM as a cause of bleeding and was cured by trans arterial embolization.
Keywords AV malformations, Rectum, IMA
140
Colonic stricture in ulcerative colitis: Diagnosis out-of-the-way
Rohit Mathur, Neeraj Singla, Arun Karyampudi, Anuradha Sekaran, D N Reddy
Correspondence – Rohit Mathur – rohitmathur2021@gmail.com
Department of Gastroenterology, Asian Institute of Gastroenterology, 6-3-661, Somajiguda, Hyderabad 500 082, India
Background Primary colorectal lymphoma (PCL) occurs more commonly in patients with inflammatory bowel disease who are on long-term immunosuppression. However, PCL occurring de novo in an untreated patient with ulcerative colitis is extremely rare. Histologically, non-Hodgkin’s lymphoma (NHL) is more common than Hodgkin’s lymphoma. The exact etiology is not known, although infection with Epstein-Barr virus may play a role.
Case Presentation A 51-year-old man presented to Gastroenterology Clinic with 8 months history of intermittent abdominal pain, fatigue, feeling of a lump in his abdomen, tenesmus bleeding per rectum associated with diarrhea alternating with constipation and significant weight loss. He was diagnosed with ulcerative colitis 8 years back but was lost to follow-up until recently. He initially took 5-ASA since diagnosis for 5 years and never had immunosuppressant during his treatment. MRI abdomen was suggestive of circumferential enhancing mass lesion in the left colon extending from splenic flexure distally for a length of 24 cm and diffuse thickening of the wall of the colon. Colonoscopy biopsy and IHC marker (pan CK negative, CD 45+, CD 20 +and CD 3 highlights T lymphocytes with Ki67 50%) were suggestive of lymphoproliferative disorder. Further IHC marker BCL 2 CD 20 BCL 6 c MYC (focal) was positive and MUM 1 was negative, suggestive of diffuse B cell lymphoma germinal origin. All these findings were suggestive of NHL DBCL (germinal), fulfilling the Dawson criteria for PCL, and after WHO staging he was started on a CHOP regimen with good nutrition supplementation. The patient was followed for 6 months and showed significant improvement.
Conclusion Primary colorectal lymphomas are associated with poor survival rates as compared to NHL of other gastrointestinal sites. Better imaging and advances in IHC techniques made this diagnosis possible early.
Keywords Primary colorectal lymphoma, Inflammatory bowel disease
141
Cytomegalovirus colitis in a immunecompetent patients – A case series
Muppa Girish , Amol S Dahale, Debabrata Banerjee, Ashok Dalal, Sanjeev Sachdeva
Correspondence – Amol S Dahale – amolsd1986@gmail.com
Department of Medical Gastroenterology, D Y Patil Medical College, Hospital and Research Centre, Pune 411 018, India
Cytomegalovirus (CMV) colitis is a common occurrence in immune-compromised patients but uncommon in immune-competent patients with usual mild and self-limiting symptoms and rarely gives rise to serious complications. CMV infection is often more severe in immunosuppressive diseases such as immunodeficiency syndrome. Furthermore, patients with cancer, and organ- or bone marrow-transplantation and those undergoing treatment with steroids or chemotherapeutics are more susceptible to CMV. Some of the recent literature report that cases of CMV infection are seen in immune-competent individuals. Serious CMV infection occurs commonly in immunocompromised patient as compared to immunocompetent patient. Colitis is a secondary manifestation to CMV infection and less frequently occurs within a clinical setup. The gastrointestinal tract involvement usually results in gastroenteritis, duodenitis, ileitis, proctitis, or exacerbation of inflammatory bowel disease (IBD). Gastrointestinal involvement is very rare in immunocompetent individuals; however, the commonly involved sites are colon and rectum. Immunocompromised state is associated with latent CMV infection that gets reactivated and also occurs as a primary infection in immunocompetent individuals. Many case reports and series document that comorbidities like diabetes and renal failure in immunocompetent individuals are associated with immune dysfunction. CMV colitis association with Crohn’s disease is a very rare occurrence. However, a clear relationship between CMV colitis and ulcerative colitis has been reported in the literature. The chances of morbidity and reported deaths due to CMV in immunocompetent patients were low as compared to immunocompromised patients, but life-threating situations were seen in critically ill and in patients having comorbidities. We aimed to share our experience of CMV colitis in immunocompetent patients. In conclusion, CMV colitis is frequently encountered nowadays even in immunocompetent patients. Colonoscopy findings in our case series showed nonspecific ulcers, so high index of suspicion is required. Histology along with immunohistochemistry and tissue PCR remains the mainstay for diagnosis. Highly effective antiviral treatment has led to improved outcomes over time.
Keywords CMV colitis, Immunecompetent, Histology, Colonoscopy
142
Colonoscopic intralesional injection of Coca-Cola for evacuation of large rectal fecaloma
Avnish Kumar, Rinkesh Kumar Bansal, Avinash Kumar Sudan, Neha Choudhary, Reyaz Ahmed Para, Radha Krishan Verma
Correspondence – Avnish Kumar - 117atien.seth@fortishealthcare.com
Department of Gastroenterology, Fortis Memorial Research Institute, Sector - 44, Opposite HUDA City Centre, Gurugram 122 002, India
Introduction Fecaloma is a large mass of organized hardened feces causing impaction, usually in rectum and sigmoid colon. Management includes digital evacuation, use of clearance enema, oral laxatives or, as described by us, colonoscopic instillation of Coca-Cola. We present use of intralesional injection of Coca-Cola for evacuation of large rectal fecaloma refractory to other treatment modalities.
Case Report Eighty-one-year-old male with long standing constipation, presented with inability to pass stool and severe pain in rectum for one month and difficulty in passing urine for one day. Examination of abdomen was unremarkable. Per-rectal examination revealed rounded 10 cm diameter hard non-pitting fecaloma in rectum that could not be crushed. Abdominal X-ray and NCCT scan confirmed presence of solid stool with distension of rectum and sigmoid colon. Attempts at clearance of stool with conventional methods were unsuccessful. At colonoscopy (Olympus CF-H180AL), large mobile fecaloma was noted in distal rectum with presence of solid fecal matter in proximal rectum and sigmoid colon. Following informed consent, two liters of Coca-Cola was instilled with 50 mL syringe through the working channel of colonoscope into descending and sigmoid colon, leading to evacuation of stool, but the rounded fecaloma was retained in the rectum. 50 mL of Coca-Cola was then injected into the fecaloma with 21-G endoscopic sclerotherapy needle. After 5 minutes, the hard fecaloma could easily be crushed against the sacrum and was successfully evacuated digitally.
Conclusion Colonoscopic intralesional injection of Coca-Cola followed by manual removal is effective for removal of rectal fecaloma refractory to conventional treatment.
Keywords Fecaloma, Colonoscopic removal, Colonoscopic injection Coca-Cola
143
Assessment of thiopurine metabolites 6-MMP and 6-TGN ratio in inflammatory bowel disease patients on thiopurine therapy
Khushboo Upadhyay1, Alpa Dherai1, Devendra Desai2, Prasad Naik1, Sarita Pol1, Mihika Dave1, Dhanashri Shetty1, Satish Kulkarni2, Tester Ashavaid1
Correspondence – Devendra Desai – dr_ddesai@hindujahospital.com
Departments of 1Biochemistry, and 2Gastroenterology, P D Hinduja Hospital and MRC, S V S Marg, Mahim, Mumbai 400 016, India
Introduction The enzyme TPMT methylates 6-Mercaptopurine (6-MP) to 6-Methylmercaptopurine (6-MMP) thereby preventing accumulation of active metabolite 6-Thioguanine (6-TGN). In many individuals there is a preferential conversion to 6-MMP resulting in increased 6-MMP/6-TGN ratio (>11). These individuals are known as shunters who may accumulate hepatotoxic 6-MMP and may exhibit thiopurine resistance.
Aim We reviewed 6-MMP/6-TGN ratio retrospectively in inflammatory bowel disease (IBD) patients undergoing thiopurine metabolite analysis at our center.
Methods The data from July 2015- August 2021 (n=309) was reviewed to identify patients with 6-MMP/6-TGN ratio >11. The patients were then sorted based on therapeutic 6-TGN range of 235-400 pmoles/8x10^8 RBCs and 6-MMP cut off <5700 pmoles/8x10^8 RBCs.
Results A 6-MMP/6-TGN ratio of >11 was obtained in 20 IBD patients wherein 14 had moderate elevation (11-20) and 6 had >20. Nine of these had 6-MMP above the cut off however only 1 patient with 6-MMP level of 3132 pmoles/8x10^8 RBCs had hepatotoxicity. All these patients had active disease and were on thiopurine dose of >1 mg/kg body weight (1.06-3.27 mg/kg) except 1 who was on 0.46 mg/kg. Inspite of the high dose 50% (n=10) had sub therapeutic 6-TGN suggesting preferential formation of 6-MMP. Thiopurine dose was reduced in 7 patients and allopurinol was added in 4 of them. Though subsequent metabolite analysis is not performed in any of them a clinical improvement subsequent to Allopurinol addition was noted in all. Thiopurine was discontinued only in one 64Y/F on a dose of 2.36 mg/kg presenting with leucopenia. She had increased ratio, 6-TGN and 6-MMP. Other patients are being followed up in the OPD.
Conclusion In our study cohort 6.5% of patients have a high 6-MMP/6-TGN ratio. These shunters may not respond to an increase in thiopurine dose. Hence a metabolite level based objective therapeutic management can be beneficial for optimal disease control.
Keywords Inflammatory bowel disease (IBD), Shunters, 6-MMP/6-TGN ratio
144
Utility of adalimumab and anti-adalimumab estimation in management of inflammatory bowel disease
Mihika Dave1, Alpa Dherai2, Devendra Desai3, Bhamini Keny2, Valentina D’Cruz2, Dhanashri Shetty2, Tester Ashavaid2
Correspondence – Devendra Desai – dr_ddesai@hindujahospital.com
Departments of 1Research, 2Clinical Chemistry and Immunology, 3Gastroenterology, P D Hinduja Hospital and MRC, S V S Marg, Mahim, Mumbai 400 016, India
Introduction Availability of Adalimumab (ADA) biosimilars in India has remarkably helped in management of our patients with inflammatory bowel disease (IBD). Benefit of level-based dose optimization of anti-TNF agents is well documented. However, to apply the same for ADA biosimilar, the available assays need to be assessed prior to estimation.
Aim We aimed to validate the commercial kits for estimation of an ADA Indian Biosimilar Mabura and assess its clinical efficacy for measurement of serum ADA and antibodies to Adalimumab (ATA) levels in IBD patients.
Methods Commercially available ELISA kits was validated for precision, accuracy, recovery and specificity of Mabura and ATA estimation. Trough ADA and ATA levels were done in 15 and 7 patients respectively. Therapeutic ADA was considered as >7.5 μg/mL as per AGA guidelines while >10 ng/mL of ATA was considered significant. The levels were correlated with dose, disease activity and concomitant azathioprine therapy.
Results A dose of 40 mg every 2 week and per week was prescribed in 13 and 2 patients respectively. ADA <7.5 ug/mL and ATA <10 ng/mL was obtained in 3 patients with active IBD. In these patients increasing dose frequency to 40 mg/week may help in disease control. Five of our patients had severe disease of which 3 had ADA ~10 ug/mL suggesting that higher therapeutic target would be required amongst our patients. Two patients showed primary nonresponse (PNR) and had ADA of ~ 15 ug/mL. Concomitant thiopurine therapy was prescribed in 13 patients however no correlation could be established due to small size. None of our patients had developed ATA and hence timely dose optimization will help to achieve desired therapeutic outcome.
Conclusion Kits need to be validated thoroughly prior to biosimilar and antibody estimation. Level based dosing would help in identifying PNRs and also optimize the dosing frequency to obtain desired therapeutic outcome.
Keywords Inflammatory bowel disease, Biosimilar (Adalimumab), Therapeutic drug monitoring
145
Eosinophilic colitis presenting as portal vein thrombosis and superior mesenteric vein thrombosis – A rare case report
Jithin John , Avishek Chakravorty, Jacob Raja, S Srijaya, D Krishnadas
Correspondence – Jithin John – jithin4john@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor-Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Portal vein thrombosis and mesenteric vein thrombosis can be caused by various thrombophilic states. But thrombosis as a part of underlying hypereosinophilic states like eosinophilic colitis is among the rarest of presentations.
Case Scenario A 46-year-old male, with no prior comorbidities, had presented to our hospital with chronic epigastric dull aching pain and constipation for the past 6 months. There was no obstructive symptoms. He was evaluated elsewhere with ultrasound abdomen and upper GI endoscopy but no diagnosis could be made.
Physical examination revealed, moderately built and moderately nourished patient. His vitals were stable. Abdominal examination was normal. His routine blood investigations revealed significantly high eosinophil counts (absolute eosinophil count [AEC] – 2600).
His ultrasonography abdomen showed absent flow in the right branch of portal vein portal vein.
He underwent CECT abdomen, which showed portal vein thrombosis (PVT) and the superior mesenteric vein thrombosis.
Patient was worked up for thrombophilic states and hypereosinophilia. He also underwent colonoscopy for chronic constipation. Colonoscopy was normal but biopsy revealed eosinophilic colitis, with more than 60 eosinophils/HPF.
Subsequent work up for other thrombophilic states and hypereosinophilia were negative. Hence PVT was attributed to the hypereosinophilic state caused by the 120atient120d120s120 colitis. He was started on anticoagulation with heparin and steroids.
After 2 week of treatment, his abdominal pain reduced and the AEC came down to 800.
A repeat CT abdomen and colonoscopic biopsy after 3 months showed, complete recanalization of the portal vein and the superior mesenteric vein and the resolution of 120atient120d120s120 colitis.
Conclusion Eosinophilic colitis can rarely present as a portal vein thrombosis due to hypercoagulable state caused by hypereosinophilia.
Keywords Eosinophilic colitis, Hypereosinophilia, Portal vein thrombosis, Superior mesenteric vein thrombosis
146
Efficacy of rifaximin in patients with abdominal bloating or distension: A systematic review and meta-analysis
Umang Arora1, Karan Sachdeva2, Prerna Garg1, Upendra Baitha1, Saurabh Kedia2, Mani Kalaivani3, Vineet Ahuja2, Arvind Kumar1, Piyush Ranjan1, Naval Vikram1, Sanjeev Sinha1, Ashutosh Biswas1, Naveet Wig1
Correspondence – Upendra Baitha- drupendraraj14@gmail.com
Departments of 1Medicine, 2Gastroenterology and Human Nutrition, and 3Biostatistics, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Abdominal bloating is a common complaint in patients with functional and organic bowel disease. Rifaximin, a non-absorbable antibiotic, has been tried for the treatment of this disease. We performed a systematic review and meta-analyses on the available literature to study the efficacy of rifaximin in abdominal bloating and distension in patients with functional gastrointestinal disorders (FGID).
Methods We accessed four database (MEDLINE, Embase, SCOPUS, and Web of Science) to identify randomized placebo-controlled trials that utilized rifaximin for abdominal bloating or distension in patients diagnosed with FGID. We excluded observational studies, studies including patients with organic bowel disorders such as inflammatory bowel disease, or when rifaximin was given for another indication such as HE.
Results A total of 1426 articles were available. 813 articles were screened for eligibility after removing duplicates. Thirty-four articles were selected for full-text review. Finally, ten articles (nine full-texts and one abstract; 3326 patients) were included in the analysis. Rifaximin was administered in doses ranging from 400 to 1650 mg per day for one to two weeks. Rifaximin therapy led to higher likelihood of improvement in symptoms of bloating (44.6% vs. 34.6%, RR 1.22, 95% CI 1.11, 1.35; n=2401 patients) without significant heterogeneity. Further analysis for this outcome showed that doses less than 1200 mg/day were similar to placebo (p=0.09). Bloating was measured using different scales across studies (including Likert scale, VAS, IBS-SSS; n= 7 studies). Rifaximin led to greater reduction in bloating scores compared to placebo (SMD -0.3, 95% CI -0.51, -0.1, p=0.04) but carried significant heterogeneity (I2 =61.6%, p for heterogeneity = 0.01).
Conclusion Rifaximin therapy at doses of 1650 mg/day for 2 weeks led to an increased likelihood of improvement in bloating and distension as well as reducing subjective severity of these symptoms in patients with FGID. The protocol was registered on PROSPERO.
Keywords Irritable bowel syndrome, Rifaximin, Bloating
147
Case report of multiple primary malignant neoplasm with synchronous presentation of solid tumor and hematological malignancy
Manne Gowtam, P Ganesh, S Shanmuganathan, A K Koushik, T K Anand
Correspondence – Manne Gowtam – gowtam.manne@gmail.com
Department of Medical Gastroenterology, Sri Ramchandra Medical College, 1, Mount Poonamallee Road, Ramachandra Nagar, Porur, Chennai 600 116, India
Introduction Multiple primary malignant neoplasms are defined as two or more unrelated primary malignant tumors that originate from different organs and occur in the body at the same time or one after another.
A 67-year-old male presented with complaints of dull aching type of diffuse abdominal pain since 1-week, high-grade fever associated with chills and rigors in the last 10 days, excessive straining while defecation associated with the reduced caliber of stools for the period of past one month, and significant weight loss of 15 kg in 3 months. On general examination, pallor and firm non-tender lymph nodes were noted in bilateral upper, mid-cervical, and inguinal areas. Abdomen examination showed tenderness in the left iliac fossa and splenomegaly. On working up patient had normocytic normochromic anemia with Hb of 8.7 with normal total counts. PET CT done showed enlarged lymph node with increased FDG uptake in bilateral cervical, posterior triangle, supraclavicular, paratracheal, and inguinal. FDG avid circumferential thickening in the sigmoid colon. Multiple FDG avid hypodense lesions in the liver. Cervical lymph node biopsy showed non-Hodgkin lymphoma- peripheral T cell lymphoma NOS type. Colonoscopy done showed normal rectum and a friable circumferential ulcer proliferative growth noted in sigmoid colon 20 cm from anal verge causing severe luminal narrowing, scope could not be negotiated further. Colon biopsy revealed moderately differentiated adenocarcinoma with adjacent areas of high-grade dysplasia and focal areas of necrosis. Liver biopsy showed adenocarcinoma of the liver – metastatic. Bone marrow biopsy showed Reactive marrow with myeloid hyperplasia.
Final Diagnosis NHL- peripheral T cell type and Adenocarcinoma of sigmoid colon with Liver metastasis.
Discussion The synchronous occurrence of a solid tumor with a hematological malignancy is extremely rare, but even more so is the synchronous presentation of colorectal carcinoma and lymphoma, which has been estimated at 0.0002%.
Keywords Non-Hodgkin lymphoma, Adenocarcinoma of colon, Multiple primary malignant neoplasms
148
Fecal microbiota transplantation in patients with mild to moderate ulcerative colitis is associated with early clinical response
Shubi Virmani, Mukesh Kumar Singh, Bhaskar Kante, Peeyush Kumar, Sudheer Kumar Vuyyuru, Mukesh Kumar Ranjan, Sandeep Kumar Mundhra, Rithvik Golla, Govind Makharia, Saurabh Kedia, Vineet Ahuja
Correspondence – Vineet Ahuja – 122atien.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Fecal microbial transplantation (FMT) has been shown to be efficacious in patients of ulcerative colitis (UC). There is large knowledge gap in number of FMT sessions required for the response and timing of response to FMT.
Methods In this single centre (centre: All India Institute of Medical Sciences, New Delhi; duration: August 2019 – March 2020) study, patients with mild-moderate UC who were refractory to conventional therapy were subjected to FMT. Patients received up to 7 sessions of freshly prepared FMT once a week, administered colonoscopically (30 – 50 grams of stool). Clinical assessment using SCCAI (simple clinical colitis activity index) was done at each follow-up FMT session till 7 weeks. Clinical remission was defined as SCCAI ≤ 3 and response as decrease in SCCAI scores by 3 points.
Results Thirty patients with UC (mean age-33.4±10.82 years, 63.6% males, median disease duration-48.5 months, 53.3% left side colitis, 46.7 % pancolitis, median SCCAI at baseline-7) were included, of which 18 (60%) had clinical response, and 16 (53.3%) had clinical remission. There was no difference in baseline demographic, clinical, endoscopic and laboratory features between responders and non-responders (Table 1). Total of 181 FMT sessions were performed, of which 19, 4, 1, 2, 3, and 1 patients’ received 7, 6, 5, 4, 3 and 2 FMT sessions respectively. Median SCCAI at 8 weeks in responders was 1 (0-5) (Table 2). Median time to achieve clinical response and remission was 1 and 2 weeks respectively.
Conclusion Patients with mild to moderate ulcerative colitis refractory to conventional therapy achieved clinical response to FMT as early as 1 week. Studies including large number of patients are required to assess the requirement for the number of FMT sessions to achieve clinical response and remission.
Keywords Ulcerative Colitis, Dysbiosis, Fecal microbiota transplantation, Clinical response, Clinical remission
149
Reactivation of Cytomegalovirus in corona virus disease 2019 infection: A case series
Samarth Sharma, Rajat Kalra, Praveen Sharma, Ashish Kumar, Anil Arora
Correspondence – Samarth Sharma – samarth.kmcm@gmail.com
Institute of Liver, Gastroenterology, and Pancreaticobiliary Sciences, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Cytomegalovirus (CMV) is ubiquitous latent persistent viruses which is commonly seen in immunosuppressed status. Since the beginning of corona 123atie disease 2019 (COVID-19) epidemic, reactivation of latent infection secondary to rampant use of steroids/immunomodulators has been increased. We draw attention to reactivation of latent infections like CMV while treating severe COVID-19 pneumonia. We present a case series of CMV and severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) coinfection that manifested with hemorrhagic enterocolitis. This complication may have developed because of synergistic pathophysiologic mechanisms related to COVID-19 infection including T lymphocyte depletion and immune response dysregulation and use of corticosteroids.
Method This is a retrospective case series of 5 consecutive CMV colitis patients who had COVID-19 infection (covid antibody positive) and have received steroids during the course of COVID-19 treatment. Diagnosis was made through tissue CMV PCR. Patients were treated with ganciclovir and surgical intervention as a lifesaving procedure as and when required.
Result Five patients were included in the case series. The patients were of age group between 41-74 years with median age of 57 years. Four (80%) were males and 20% were females. Three (60%) of patients had severe covid pneumonitis and 80% of patients have received high dose steroids. Eighty percent have presented with massive gastrointestinal (GI) bleed. Median duration between onset of COVID-19 and diagnosis of CMV colitis were 35 days. All patients have received Gancyclovir and 1 patient underwent right hemicolectomy. Out of 5, 1 (20%) patient went leave against medical advice and 1 patient (20%) succumbed to CMV colitis.
Conclusion This case series highlights the importance of keeping a high index of suspicion and providing the correct diagnosis and treatment of CMV Colitis in COVID-19 infection. In COVID-19, the use of immunosuppressive therapy should be justified while being alert for signs and symptoms of CMV reactivation and other opportunistic infections.
Keywords Cytomegalovirus, COVID-19 pneumonitis, Immunosupression reactivation steroids
150
Proportion of patients with inflammatory bowel disease who need biological agents and reasons for discontinuation
Vinita Patil, Devendra Desai, Philip Abraham, Tarun Gupta
Correspondence – Vinita Patil – vinitapatil.91@gmail.com
Department of Gastroenterology, P D Hinduja National Hospital and Research Center, Veer Savarkar Marg, Mahim West, Mumbai 400 016, India
Background Biologic agents are highly effective in patients with inflammatory bowel disease (IBD). However, they are expensive and are associated with primary and secondary non-response and side effects.
Aim To study the proportion of patients with IBD in whom biologics are indicated, how many receive them, how many discontinue them, and the factors that limit their use.
Methods Two hundred and fifty consecutive patients with IBD were enrolled prospectively between June 2020 and June 2021. Demographic data, disease characteristics, and treatment details were noted. Numbers needing biologics, who discontinued them, and reasons for discontinuation were noted.
Results Two hundred and fifty patients (111 women) included 131 patients with ulcerative colitis (UC), 116 with Crohn’s disease (CD), and three with IBD-undifferentiated. Mean age was 39.6 years (SD 16.0). Median duration of UC was 10 years (Q3-Q1 interquartile range [IQR] 9) and of CD 8 years (IQR 8). Biologics were indicated in 73 (29.2%) but only 58 (UC 20, CD 38) received them; 11 patients were unwilling, 2 had financial constraints, one had recurrence of Hodgkin’s lymphoma, and one expired before initiation. Indications in these 58 included: fistulising disease (18), 124atient124d124s disease (13), non-response to conventional drugs (11), acute severe UC (10), and steroid-dependent (5) or steroid-refractory (1) UC. Forty-two patients received infliximab, 22 adalimumab, and three vedolizumab. Twenty-five (43.1%) patients discontinued biologics; reasons included unwillingness to continue (6), primary non-response (5), secondary loss of response (3), physician decision (2), non-affordability (2), reactivation of tuberculosis (2), remission (2), and infliximab-induced psoriasis, metastatic carcinoma of colon and pancytopenia (1 each).
Conclusion Biologics were indicated in about a fourth of our patients with IBD, more than previously described from India. This indicates changing IBD phenotype in India. They were discontinued in a large proportion of patients (43.1%), due to unwillingness to continue, non-response, and side effects. Patient education may reduce discontinuation.
Keywords Crohn’s disease, Ulcerative colitis, Treatment
151
Minimal risk of lymphoma despite long-term use of azathioprine in patients with inflammatory bowel disease: A longitudinal cohort analysis from northern India
Mukesh Ranjan1, Bhaskar Kante1, Sudheer Vuyyuru1, Peeyush Kumar1, Sandeep Mundhra1, Rithvik Golla1, Raju Sharma2, Prasenjit Das3, Peush Sahni4, Govind Makharia1, Saurabh Kedia1, Vineet Ahuja1
Correspondence – Vineet Ahuja – vinnet.aiims@gmail.com
Departments of 1Gastroenterology and Human Nutrition, 2Radio Diagnosis, 3Pathology, 4Gastrointestinal Surgery, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Thiopurines are widely used to maintain remission in both ulcerative colitis (UC) and Crohn’s disease (CD). Reported effectiveness and tolerability rates have been variable across studies. Moreover, there are only sparse data in the Asian population regarding the long-term efficacy and safety of azathioprine (AZT).
Methods Records of 5351 patients followed up at IBD clinic, All India Institute of Medical Sciences, New Delhi from 2004-2020 were evaluated retrospectively. Azathioprine efficacy was defined as no requirement of surgery, hospitalizations, anti TNFs agents, and minimum steroid (≤1 course in 2 years) requirement on follow-up. Safety was evaluated in terms of long-term adverse events and the development of malignancy.
Results Of 5351 patients with IBD, 1093 who received AZT for > 3 months (UC=788 [proctitis-1.9%, left sided colitis-44.9%, pancolitis-53.1%], CD=305 [inflammatory-42.6%, 125atient125d125s-46.9%, fistulizing-10.5%]) were included (60.8%-males, mean age at disease onset-31.69±12.34 years, median disease duration at AZT initiation-3 [1-5] years) (Table1). Follow-up and treatment duration on AZT were 7 (4-12) years and 39.41±40.27 months respectively. Mean initiation and maintenance dose of AZT was 1.09±0.45 mg/kg and 94.82±21.29, respectively. One,3,5, and 10 years relapse free survival was 85%,79%,76%, and 64%; 87%, 82%, 79% and 72%; and 78%, 72%, 68% and 61% in overall cohort, UC and CD patients, respectively (Log-rank p=0.001 between UC and CD) (Fig. 1). Median relapse free survival in UC and CD patients was 180 and 120 months respectively. Three hundred fifty-nine (UC:249 [31.6%]; CD:110 [36.07%]; p=0.158) patients developed adverse events (AE), commonest was myelosuppression (23.42%) followed by gastrointestinal intolerance (2.97%), flu like illness (1.7%), and arthralgia/myalgia (1.37%) (Table 2). Myelosuppression was the commonest cause of AZT withdrawal. No patient (including 254 patients on AZT for ≥5 years) developed lymphoma or non-melanoma skin cancer.
Conclusion Long-term Azathioprine monotherapy in patients with IBD is safe with minimal risk of lymphoma and non-melanoma skin cancer.
Keywords Ulcerative colitis, Crohn’s disease, Azathioprine, Lymphoma, Skin cancer
152
Superdonors for fecal microbiota transplantation in patients with mild-moderate ulcerative colitis are identified by higher abundance of Firmicutes and lower abundance of Actinobacteria
Saurabh Kedia, Mukesh Kumar Singh, Aditya Bajaj, Manasvini Markandey, Bhaskar Kante, Peeyush Kumar, Sudheer Kumar Vuyyuru, Shubi Virmani, Mehak Verma, Sambudh Kumar, Govind Makharia, Vineet Ahuja
Correspondence – Vineet Ahuja – 126atien.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, New Delhi, Delhi 110029, India
Background Fecal microbiota transplantation (FMT) has demonstrated moderate efficacy in mild-moderate ulcerative colitis (UC), and donor characteristic is a major determinant. However, there is heterogeneity on optimal donor signatures responsible for therapeutic benefit. We evaluated donor characteristics associated with better response to FMT in UC.
Methods Patients with mild-moderate UC on stable doses of 5-aminosalicylic acid, immunomodulators and steroids (<20 mg/day) who received FMT and anti-inflammatory diet were included. Of 36 potential donors, 13 were selected after questionnaire and investigations. FMT was freshly prepared from this pool with 2-5 donors in each batch and was administered colonoscopically every week till 6 weeks. Clinical response was decline in SCCAI>3, and remission as SCCAI<3. 16srRNA gene sequencing was done on donor stool to compare relative abundance of Firmicutes, Bacteroides, Actinobacteria, and Proteobacteria between effective and ineffective donors. For all donors, through a 2 x 2 contingency table approach, clinical response was compared between patients receiving FMT from a particular donor (1-13) vs. other donors, and donors associated with statistically significant higher clinical response were termed effective.
Results Twenty-nine patients underwent FMT with a total of 178 sessions. Eighteen (mean age-31.1+8.8 years, males-44%, disease duration-69 [28-84] months, pancolitis-44%) had a clinical response and 11 (mean age-35.7+11.4 years, males-27%, disease duration-48 [36-96] months, pancolitis-54%) didn’t. Baseline clinical, endoscopic and biochemical disease activity, and medications were similar between two groups. Of thirteen donors, numbers three (FMT with donor 3 vs. without donor 3, 69% vs. 0), six (75% vs. 33%), eight (82% vs. 33%), ten (87% vs. 36%), eleven (81% vs. 38%), and thirteen (100% vs. 47%) were effective (p<0.05 for all). Though not statistically significant, relative abundance of Firmicutes (66.6 [25.9-88.3] vs. 43.8 [40.6-47.7], p=0.2) was higher and Actinobacteria (15.6 [10.3-29.7] vs. 23.9 [16.5-40.9], p=0.1) was lower in effective than ineffective donors.
Conclusion Superdonors had higher abundance of Firmicutes and lower abundance of Actinobacteria, suggesting influence of donor microbial signatures on response to FMT in patients with UC.
Keywords Superdonor, Fecal microbiota transplantation, Ulcerative colitis, predictor
153
Partial enteral nutrition in combination with exclusion diet is not superior to standard medical therapy in mild to moderate ulcerative colitis: An interim analysis of quasi-experimental study
Sudheer Vuyyuru , Vineet Ahuja
Correspondence – Vineet Ahuja – vineet.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Unlike in Crohn’s disease (CD), the role of enteral nutrition and diet in the management of ulcerative colitis (UC) hasn’t been clear. Therefore, we designed this trial to evaluate efficacy of partial enteral nutrition combined with exclusion diet in patients with mild to moderate UC.
Methods In this quasi-experimental study we included patients with mild to moderate UC (SCCAI) and allocated them into experimental arm which received PEN combined with exclusion diet (ED) and standard of care arm (SOC). Disease activity was measured using simple clinical colitis activity index (SCCAI) and partial mayo score (PMS). We assessed clinical remission (SCCAI ≤2) at 2 and 4 weeks.
Results Out of 60 UC patients, 30 were included in PEN + ED arm and 30 were included in SOC arm. Both arms are comparable in baseline clinical and biochemical parameters like age (36.7 vs. 36.4, p=919, extent (E1, E2, E3, E2/E3: 6.7%, 15%, 36.7%, 6.7%), hemoglobin (g/L) (109 vs. 116, 0.164), SCCAI score (5 [4-6] vs. 5 [4-5.2], p=0.562), and PMS (4 [3-4.2] vs. 4 [3-4], p=912) were similar between both groups except serum albumin which is higher in SOC arm (g/L) (35 vs. 40, p=0.030). Clinical remission at 2 weeks was significantly higher in SOC arm compared to PEN+ED arm. However, it was not significant at 4 weeks. A numerically higher number of patients required steroids in SOC arm compared to PEN+ED arm, but it was not significant (16.7% vs. 23.3%, p=0.748). There was a significant increase in hemoglobin in PEN+ED arm at 4 weeks (mean delta Hb:2.9g/L), whereas in SOC arm there was decrease in hemoglobin (mean delta Hb:0.45 g/L, p=0.046). However, there was no difference in delta albumin levels.
Conclusion PEN in combination with exclusion diet does not improve rate of induction of clinical remission in addition to standard medical therapy in patients with ulcerative colitis. Further large randomized controlled studies are needed for definitive conclusions.
Keywords Partial enteral nutrition. Exclusion diet, Ulcerative colitis
154
Probing the cause of colonic thickening on CT – A tertiary care experience
Prakhar Garg , Vinod Kumar Dixit, Sunit Kumar Shukla, Dawesh Yadav, Anurag Tiwari, Vinod Kumar
Correspondence – Vinod Kumar Dixit – drvkdixit@gmail.com
Department of Gastroenterology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221 005, India
Introduction Increasing use of abdomino-pelvic CT for various indications has greatly increased the diagnosis of bowel wall thickenings. We aim to find out the correlation between bowel thickening with subsequent colonoscopic and histopathological findings.
Methods Data of patients referred for colonoscopy on basis of colonic thickening on CT were collected retrospectively between January 2020 and September 2021 and their histopathology reports were traced. Patients undergoing CT for known GI disease or known malignancy were excluded.
Results A total of 122 patients were identified. Mean age of patients was 35.8 years (15-80) with male to female ratio of 0.7:1. The most common location of thickening was ileocecal (68%, n=83), followed by ascending colon (16.3%, n=20) and rectosigmoid (12.2%, n=15). Colonoscopy was normal in 35.2% (n=43) cases. More than 75% patients underage group <40 years had ileocecal thickening and 42% of them had normal colonoscopy. The most common colonoscopic abnormality found was presence of ulcers and erosions (n=38, 31.1%), followed by growth (n=15, 12.2%) and stricture (n=12, 9.8%). Other less common findings included diverticulosis, telangiectasia, pseudomelanosis coli.
Nonspecific colitis was most commonly reported in patients undergoing colonoscopy (52%). Tuberculosis was diagnosed in 20.4% (n=25) mostly in pts with strictures. The diagnosis of IBD was made in 18.8% (n =23). Malignancy was found in 9% patients. Adenocarcinoma was most common (>90%) followed by lymphoma, metastatic and NET in remainder. Three patients had eosinophilic colitis. The diagnosis of malignancy was significantly more present in age group >40 years with most common site in them being rectosigmoid.
Conclusion Ileocecal thickening remain the most common reported site of thickening in CT. However, a significant proportion of patients may have normal colonoscopy and many have nonspecific colitis on histopathology especially in younger age group patients.
Keywords Colonic thickening, Colonoscopy, Colitis
155
Clinical and endoscopic profile of inflammatory bowel disease in a tertiary care hospital in north Karnataka
Mayur Dave , Santosh Hajare, Varadaraj Gokak
Correspondence – Mayur Dave – dr_mayurdave@yahoo.com
Department of Gastroenterology, KLE’s Dr. Prabhakar Kore Hospital and MRC, Belagavi 590 010, India
Introduction The term inflammatory bowel diseases (IBD) encompass a spectrum of diseases, of which ulcerative colitis (UC) and Crohn’s disease (CD) are the most familiar entities. Although the exact etiology is unknown, its triggering and perpetuation have been ascribed to various genetic, environmental, and immunological factors. Historically IBD was seen as the bane of Western countries, but recent reports suggest that numbers have been stealthily climbing up in Asia, special in India. We aim to study the clinical profile of IBD patients in a tertiary care hospital of north Karnataka.
Methods We retrospectively analyzed the clinical profiles of IBD patients who had presented to Department of Gastroenterology over a period of 2 years from September 2019 to September 2021. Demographic profile, clinical and endoscopic findings along with management and complications were taken into consideration.
Results The 145 patients, there were 139 (95.8%) patients with UC, 6 (4.2%) with CD. Chronic diarrhea (84%) and blood in stools (75.4%) were common in UC, whereas abdominal pain (60%) was common in CD. E2 (57.1%) was more common in UC, there were equal number of L2 (50%) and L3 (50%) in CD. Most of the patients had moderate to severe disease activity and responded well to pharmacotherapy. Few patients required biologicals for the remission.
Conclusion In our study, we found that IBD was common in rural population of north Karnataka and UC was more common than CD.
Keywords Inflammatory bowel disease, Ulcerative colitis, Crohn’s disease
156
Role of cytomegalovirus infection in patients of ulcerative colitis with relapse and impact of antiviral therapy – Valganciclovir on outcome in these patients
Vikas Raikwar , Sudhanshu Yadav, Shivesh Thakur, Amber Mittal, Shohini Sircar, Ajay Jain
Correspondence – Ajay Jain - ajayvjain@yahoo.com
Department of Gastroenterology, Choithram Hospital and Research Centre. 14, Manik Bagh Road, Indore 452 014, India
Introduction High mucosal cytomegalovirus (CMV) load has been associated with failure of IV steroid therapy in patients with acute severe ulcerative colitis. A recent meta-analysis suggested that determining CMV infection assists in the selection of a proper treatment strategy. Hence, we aimed to assess the prevalence of CMV viral load in patients of ulcerative colitis who presented with relapse of symptoms in OPD and their outcome after treatment with valganciclovir.
Methods Study subjects were all diagnosed patients of ulcerative colitis who presented to gastroenterology OPD from June 2020 to September 2021 with recent-onset symptoms suggestive of relapse. Relapse was defined as more than six stools per day mixed with blood and mucus and ulcerative colitis endoscopic index of severity (UCEIS) score of more than four on sigmoidoscopy. Exclusion criteria were patients with any solid organ transplantation or patients on biological therapy.
Results During the study period, 90 patients of diagnosed UC came for follow-up in OPD. Out of 90 follow-up patients, 47 had relapse of symptoms. Out of these 47 patients with relapse, 14 patients (29.7%) had CMV infection proven by reverse transcription–polymerase chain reaction (RT–PCR), for CMV on tissue sample taken from the rectum, while histopathologist suspected CMV infection on H & E stain in only one patient. All patients with CMV infection proven by RT-PCR responded to oral valganciclovir given in doses of 900 mg per day for 21 days. All patients had two to three well-formed stools without any mucus or blood at the end of therapy. None of the patients with relapse treated with valganciclovir required steroids or immune-modulatory drugs or admission to hospital.
Conclusions 1. The prevalence of CMV infection as a cause of relapse in this study is 29.7%. 2. All patients with CMV infection responded to oral antiviral with effective disease control without any step-up treatment for UC.
Keywords Ulcerative colitis, Cytomegalovirus, Valganciclovir
157
Azathioprine still remains the first step-up therapy in patients with inflammatory bowel disease in low-middle income countries
Mukesh Ranjan 1 , Peeyush Kumar 1 , Sudheer Vuyyuru 1 , Bhaskar Kante 1 , Pabitra Saju 1 , Sandeep Mundhra 1 , Rithvik Golla 1 , Mukesh Singh 1 , Shubi Virmani 1 , Raju Sharma 2 , Rajesh Panwar 3 , Prasenjit Das 4 , Govind Makharia 1 , Saurabh Kedia 1 , Vineet Ahuja 1
Co7respondence – Vineet Ahuja – 130atien.aiims@gmail.com
Departments of 1Gastroenterology and Human Nutrition, 2Radio Diagnosis, 3Gastrointestinal Surgery, and 4Pathology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Inflammatory bowel disease (IBD) including ulcerative colitis (UC) and Crohn’s disease (CD) is characterized by remitting/relapsing course. A proportion of patients with UC, and almost all patients with CD require long-term immunosuppression to maintain endoscopic and clinical remission and prevent disease progression. The present study aimed to evaluate the long-term efficacy of thiopurines, their predictors, and the effect of the early use of thiopurines on disease outcomes in patients with IBD.
Method A retrospective cohort analysis of IBD patients following up in IBD clinic at AIIMS, New Delhi, from 2004-2020. Efficacy was defined as a state of not requiring hospitalization, anti-TNF agents, surgery, and only minimum (≤ 1 steroid course in 2 years) steroid requirement during follow-up. Early thiopurine initiation was defined as commencement of thiopurines ≤2 years of disease onset.
Results Of 1264 consecutive patients on thiopurines (6-MP and azathioprine), 988 (UC:720, CD:268) were considered for efficacy analysis (males:60.8%, mean age at disease onset:31.69±12.34 years and thiopurine initiation:35±13.14 years). Time to event analysis showed median efficacy rates of 79% and 72% in UC, and 68% and 61% in CD at 5 and 10 years respectively. On multivariate analysis, only male sex (HR: 1.53, 95% CI: 1.05-2.23) in UC and ileal involvement (HR: 2.361, 95% CI: 1.115-4.99; p=0.025) and occurrence of any adverse events (HR: 0.514, 95% CI: 0.313-0.844; p=0.008) in CD were having a significant predictive value for relapse. Kaplan-Meier survival analysis showed no difference between the efficacy of early and late thiopurine groups, both in UC (Log-rank p=0.72) and CD (Log-rank p=0.76).
Conclusion Thiopurines still remain a viable long-term option for maintenance of remission in patients with IBD, especially in resource-limited countries. Their use can be further enhanced by optimizing their therapy and regular monitoring for adverse events.
Keywords Inflammatory bowel disease, Thiopurines, Azathioprine, Efficacy
158
Cyclosporine for steroid refractory ulcerative colitis
Ashok Kumar , Itish Patnaik, Anand Sharma, Rohit Gupta
Correspondence – Ashok Kumar – drashok.sgpgims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Virbhadra Road, Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Introduction Cyclosporine A (CsA) is a useful therapy for patients with steroidrefractory ulcerative colitis (UC). However, there is a paucity of data from Asian countries. We report our experience in the sub-Himalayan region of India with the use of CsA in patients with steroid-refractory UC.
Methods The database of all UC patients, hospitalized between June 2018 to September 2021, was analyzed for the need for CsA therapy for steroid-refractory UC. Demographic and clinical characteristics, response to and complications of CsA, steroid-free remission, and the need for colectomy were reviewed for all patients.
Results Of the 40 patients with moderate-severe UC, 7 patients (mean age 31.9 years; 4 women) had steroid-refractory UC. The majority (71.4%) of patients had pancolitis and remitting, relapsing course (mean number of prior exacerbations 2 (range 1-5) with mean disease duration of 3.7 years (range 0.1-13). All received intravenous CsA (2 mg/kg/day) for a mean of 5.57 days (range 5–7). The median time to clinical response (lichtiger score <10) was day 4 (range 2-6) of CsA and remission (lichtiger score <3) was achieved on a mean of 9 days (range 5-12) after CsA. All responders received oral CsA for a further 3 months followed by azathioprine. All of the patients remained steroid-free and colectomy-free for the mean follow-up period of 8.4 months (range 2–15 months). One patient each had infections (bacteremia due to klebsiella), paresthesias, and hypertrichosis with CsA therapy, but none of the patients required CsA discontinuation due to adverse events.
Conclusion Our study shows that cyclosporine therapy can provide steroid-free remission and avoid colectomy in steroid-refractory moderate-severe UC without significant drug toxicity.
Keywords Ulcerative colitis, Steroid refractory ulcerative colitis, Cyclosporine
159
Disseminated Cytomegalovirus infection a great masquerade of PUO in ulcerative colitis: A case report
Purna Sethy , Itish Patnaik, Anand Sharma
Correspondence – Anand Sharma – andy.mmc@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Virbhadra Road, Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Cytomegalovirus (CMV) is found in 10% with ulcerative colitis (UC) and presents as a flare. However, prolonged fever is an unusual presentation of CMV in patients with UC. We present a case of UC, who got admitted with exacerbation bloody diarrhea and fever of unknown origin and was subsequently diagnosed with disseminated CMV infection.
A 28-year-old male diagnosed with UC on Azathioprine and mesalamine presented with exacerbation of bloody large bowel bloody diarrhea for two months and intermittent high-grade fever for one month. An evaluation revealed deranged liver enzymes. Sigmoidoscopy revealed deep punched out ulcers in the rectum and sigmoid colon. Biopsies were taken for histopathology and immunohistochemistry for CMV. Blood CMV PCR was also sent. He was started on intravenous steroids; he remained febrile and continued to have bloody diarrhea. Awaiting histology and PCR reports, he underwent evaluation for fever, including blood cultures, computed tomography of the abdomen, echocardiography to rule out vegetations, and bone marrow biopsy, which were all non-contributory. Blood CMV PCR report was positive for CMV viremia HRCT thorax showed features of viral pneumonia. The colonic biopsy revealed CMV inclusion bodies with cytopathic changes.
For elevated liver enzymes workup for hepatotropic viruses (A, B, C, and E), Wilson disease, autoimmune hepatitis was negative. Percutaneous liver biopsy showed CMV inclusion bodies, and there was no evidence of liver cirrhosis. Ganciclovir was administered for 21 days, and the patient was discharged in a stable condition with the resolution of fever and normalization of liver enzymes.
Discussion CMV colitis is seen in 10% of patients with UC patients with flare. In a study, fever raised a high index of suspicion of CMV infection in IBD patients. Although CMV is a commonly identified culprit in a case of steroid-refractory UC, its presentation as a cause of prolonged fever with multi-system involvement is uncommon.
Keywords Cytomegalovirus, Ulcerative colitis
160
Tofacitinib in treatment of moderate to severe steroid dependent ulcerative colitis- Indian scenario
Rahul Kakkar , Sunil Dadhich, Narender Bhargawa, Sabir Hussain, Sewaram Chaudhary
Correspondence – Rahul Kakkar - kakkarrahul1805@gmail.com
Department of Medical Gastroenterology, Dr. S N Medical College, Residency Road, Near Sriram Excellency Hotel, Opposite Petrol Pump, Sector-D, Shastri Nagar, Jodhpur 342 003, India
Introduction Ulcerative colitis (UC) is a chronic inflammatory condition of the large intestine. Steroids are mainstay of treatment in moderate to severe UC. But some patients become steroid dependent. Azathioprine, anti TNF therapy and other drugs are used in steroid dependent patients for maintenance of remission. Tofacitinib is oral drug effective in UC. Aim of our study is to look for efficacy of tofacitinib in steroid dependent moderate to severe Indian UC patients.
Methods An open label, single arm prospective study conducted in 19 moderate to severe steroid dependent UC patients. Patients were induced with 40 mg prednisolone OD and 10 mg tofacitinib BD and were maintained on 5 mg tofacitinib BD. Primary outcome was absence of rectal bleeding at 16 weeks (sub-score of 0 for rectal bleeding in Mayo score). Secondary outcome was to look for serious adverse events.
Results Mean age was 38.7 years (SD=13.05 years). Median Mayo score at baseline was 9 (IQR-7,11). Median C-reactive protein (CRP) were 15.43 mg/L at baseline (IQR- 9.52,22.20). At 16 weeks, primary outcome was met by 16 patients (84.21%). Median mayo score at 16 weeks was 3 (IQR-3,3) with significant reduction compared to baseline (p value<0.001). Median CRP at 16 weeks were 2.56 (IQR-2.18,3.78) which also had a significant reduction compared to baseline (p value<0.001).
Conclusion Tofacitinib is effective oral drug in treatment of steroid dependent moderate to severe UC patients. Considering cost as an issue in a developing country like India, it is a cheaper alternative to anti-TNF therapy.
Keywords Tofacitinib, Steroid dependent ulcerative colitis, Moderate to severe ulcerative colitis
161
Morphology of dopaminergic neurons in the myenteric plexus of ulcerative colitis patients
Anjali Singh , Seema Singh
Correspondence – Anjali Singh – dranjalisingh2@gmail.com
Department of Anatomy, Maulana Azad Medical College, New Delhi 110 029, India
Introduction Ulcerative colitis (UC), type of inflammatory bowel disease (IBD) is a chronic debilitating gastrointestinal disorder that markedly impair quality of life. It causes high mortality and affect about a million people in the USA with an increased proportion in cases in developing countries like India with wide variety of food and lifestyle changes in recent years. Too it adds up to the risk of colorectal cancer up to 10% and adding up to morbidity and mortality. It involves mucosa and submucosa resulting inflammation and ulcers of the colon further causing gastro-intestinal symptoms. But, there are very few studies on the morphology of myenteric ganglia specially for the change in morphology in dopaminergic neuronal type in these patients.
Aim To study the morphology of the dopaminergic neurons of the myenteric plexus in the ulcerative colitis patients.
Methods Samples collected- 15 patients undergoing colectomy for ulcerative colitis in department of gastrointestinal surgery and 15 normal colonic tissues collected from the department of forensic medicine, All India Institute of Medical Sciences, New Delhi, after obtaining ethical clearance. Tissues were processed. Colonic tissues from the UC patients and normal specimens processed and stained by Hematoxylin and eosin staining and immunohistochemistry (IHC) done by Tyrosine hydroxylase(TH).
Results H&E stained sections showed decrease in number of enteric neuronal cells and increase in the number of infiltrating polymorphic neutrophil, leukocytes and other cells in the myenteric ganglion (MG) appeared with increasing inflammation in ulcerative colitis. Shape and size of MG became spheroid and small as compared to the normal colon. There is also decrease in TH in dopaminergic neurons and increase in neuropil.
Conclusion These results shows that there is decrease in neurons in myenteric plexus in UC patients which can be associated to clinical symptoms.
Keywords Ulcerative colitis, Myenteric plexus, Dopaminergic neurons, Enteric nervous system
Liver
162
5-day outcome of hepatitis E-induced acute liver failure in the intensive care unit
Debashis Chowdhury 1 , Farhana Mahmood 2 , Cathryn Edwards 3 , Faruque Ahmed 4 , Mahmud Hasan 5 , Simon Taylor Robinson 6
Correspondence – Debashis Chowdhury- debashis712003@yahoo.com
1Bangladesh Gastroenterology Society, Islami Bank Hospital, Chattogram, Bangladesh, 2Chattogram Maa O Shishu Hospital Medical College, 3British Gastroenterology Society, 4Sheikh Russel Gastro Liver Institute and Hospital, 5Bangladesh Gastroenterology Society, Bangladesh, 6Imperial College, London
Background Hepatitis E virus (HEV) is an important cause of acute liver failure (ALF) in Bangladesh with pregnant mothers being more vulnerable. Cerebral edema resulting in raised intracranial pressure (ICP) is an important cause of morbidity and mortality.
Aims of the study To study the baseline characteristics and clinical outcome of HEV-induced ALF. To detect raised ICP clinically and observe response to mannitol infusion.
Methods This was a prospective cohort study on baseline characteristics and clinical outcomes of 20 patients admitted to the intensive care unit (ICU) of Chattogram Maa-O-Shishu Hospital in Chattogram (Chittagong), Bangladesh with hepatitis E-induced ALF during an epidemic from June until August 2018. We diagnosed HEV infection by detecting anti-HEV IgM antibody in patients’ blood. All patients were negative for hepatitis B surface antigen (HbsAg) and hepatitis A (anti-HAV) IgM antibody. Data were collected on the 5-day outcome after admission to ICU, monitoring all patients for signs of raised ICP. An intravenous bolus of 20% mannitol was administered to all patients with raised ICP.
Results Twenty patients were included in the study. Ten (50%) patients, 7 (70%) females, received mannitol infusion. HE worsened in 8 (40%); 7 (87.5%) female and 3 (50%) pregnant. Glasgow Coma scores (GCS) deteriorated in 6 (30%); all (100%) females and 3 (50%) pregnant. Worsening of hepatic encephalopathy (HE) and GCS deterioration were not significantly different between pregnant and non-pregnant subjects, nor between those who received mannitol and those who did not. Six patients (30%) met Kings College Criteria for liver transplantation: all were female and 3 (50%) pregnant with one patient dying.
Conclusion Female patients developed a worse outcome than male patients. Pregnancy status was not associated with worse outcome in our cohort. Mannitol infusion was also not associated with a significant difference in outcome.
Keywords Hepatitis E, Acute liver failure, Intensive care unit, Hepatic encephalopathy
163
Management of ascites in cirrhosis, “Blanket” therapy to a “Buffet” approach: A AABHA Checklist
Pathik Parikh
Correspondence – Pathik Parikh – pathik269@gmail.com
Hepatology and Liver Transplant, Zydus Hospitals, Zydus Hospitals Road, Near Sola Bridge, Sarkhej – Gandhinagar Highway, Ahmedabad 380 054, India
Introduction The treatment strategy for ascites has remained a blanket therapy with consideration of different treatment options only once an individual develops refractory ascites. The concept of individualized care of ascites is recommended for early aggressive management and preventing the development of refractory ascites right from the diagnosis of ascites.
Methods All patients with cirrhosis and new onset ascites were included. Patients with acute-on-chronic liver failure (ACLF), recent gastrointestinal bleed, sepsis, hepatocellular carcinoma (HCC), cardio-renal disease were excluded. All patients were started on treatment as per the “AABHA” buffet approach. These patients were followed up every 15 days for 2 months. The primary outcome was control of ascites. The secondary endpoints looked after were the development of hypotension, electrolyte imbalance, acute kidney injury, and hepatic encephalopathy. These patients were compared with a retrospective cohort of 25 patients.
Results The baseline characteristics were similar between the two cohorts. At 2 months of follow-up 20/25 patients of the study group had complete response while remaining 5/25 had a partial response. In the retrospective cohort group, only 3/25 had a complete response while 18 had a partial response. The development of hyponatremia < 130 mEq/L (0/25 versus 2/25), and acute kidney injury (0/25 versus 3/25) were significantly higher in the retrospective cohort (p<0.05). MAP at 2 months was significantly higher in the study group (90±10 vs. 72±10, p<0.05). None developed overt hepatic encephalopathy in 2 months of follow-up. None of the patients required tolvaptan. Tapering of diuretics was possible only in the study group.
Conclusion Early aggressive individualized therapy for ascites rather than a blanket therapy may be considered. More randomized controlled trials for “Buffet” approach needs to be considered.
Keywords Midodrine, Refractory ascites, Diuretics, CLD
164
Vaccination practices in patients with cirrhosis of liver- The dismal Indian scenario!
Mayank Jain 1 , Jayanthi Venkataraman 2 , Uday Sanglodkar 3
Correspondence – Mayank Jain – mayank4670@rediffmail.com
1Department of Gastroenterology, Arihant Hospital and Research Centre, 283-A, Gumasta Nagar, Scheme 71, Indore 452 009, India, 2Department of Hepatology, Sri Ramachandra Medical College, 1, Mount Poonamallee Road, Ramachandra Nagar, Porur, Chennai 600 116, India, 3Department of Hepatology, Dr. Rela Institute of Medical Sciences, #7, CLC Works Road, Nagappa Nagar, Chromepet, Chennai 600 044, India
Aims To study the vaccination practices in patients suffering from cirrhosis of liver using a questionnaire survey.
Methods We included all patients who were willing for the study and had been seen by a gastroenterologist/hepatologist at least once. Patients offering incomplete information were excluded. Serological tests for confirmation of immunological response were not done. Details of counselling and vaccination status for hepatitis B, hepatitis A and pneumococcal infection were noted.
Results A total of 305 patients (272 males, 89%) formed the study cohort. The median age was 60 years (range 27-76 years) and median duration of liver disease was 12 months (1-120 months). The median MELD was 14 (range 7-35). Only 37 (12.1%) patients reported that they had been counselled for vaccination against these infections. The rates of vaccination were very low (<10%).
Conclusion Very dismal vaccination rates were noted in Indian patients with liver cirrhosis.
Keywords Liver, Cirrhosis, Vaccination, Hepatitis
165
Tuberculosis in patients referred for liver transplant
Pathik Parikh
Correspondence – Pathik Parikh – pathik269@gmail.com
Department of Hepatology and Liver Transplant, Zydus Hospitals, Zydus Hospitals Road, Near. Sola Bridge, Sarkhej – Gandhinagar Highway, Ahmedabad 380 054, India
Introduction Tuberculosis (TB) in patients being evaluated for liver transplant presents a unique challenge. There is scanty literature published on treatment of tuberculosis in such select group of patients. Most literature is on patients with early cirrhosis. There is no literature on treating Child-Turcotte-Pugh (CTP) C patients when they were being evaluated for liver transplant.
Methods In this single centre observational study, sequential patients presenting for liver transplant and diagnosed with TB were included.
Results Fifteen patients were diagnosed with TB in a span of 24 months. All were males with CTP-C ethanol related cirrhosis. Median age was 41 years and median Model for end-stage liver disease (MELD)-sodium was 30. Eight patients had pulmonary tuberculosis (PTB) while rest had extra-pulmonary TB (EPTB) (pleural 8/20, peritoneal 4/20). The diagnosis of PTB was made by bronchoalveolar lavage (BAL), while fluid aspiration was diagnostic for EPTB. The median number of fluid aspirations required for diagnosis was 3 (range 1-5). Combination of GenXpert acid-fast bacilli (AFB), adenosine deaminase (ADA), AFB staining and AFB culture was sent from each aspirated sample. Unilateral right hydrothorax was more commonly seen (4/8) as compared to bilateral effusion (3/8) and unilateral left sided effusion. All patients were treated with ethambutol and quinolone (EQ). Fifty percent patients died of complications of liver failure. Six patients (30%) recompensated after anti-tubercular treatment (ATT) and were treated with HREQ for 8 months. Their MELD sodium is now less than 15. Four patients are currently being treated with EQ >2 months and are awaiting cadaveric organs. None of the patients were transplanted after the diagnosis.
Conclusion The diagnosis of tuberculosis requires battery of investigations if index of suspicion is high. EPTB is more common and history of alcoholism is a risk factor. TB in these patients have high mortality and the treatment of tuberculosis needs further randomized studies to define the best treatment strategy and timing for transplant.
Keywords TB, Cirrhosis, CLD, Liver Failure
166
Long-term outcome of patients with acute severe autoimmune hepatitis
Pathik Parikh
Correspondence – Pathik Parikh – pathik269@gmail.com
Department of Hepatology and Liver Transplant, Zydus Hospitals, Zydus Hospitals Road, Near Sola Bridge, Sarkhej – Gandhinagar Highway, Ahmedabad 380 054, India
Background and Aim Acute severe autoimmune hepatitis (ASAIH) is a life threatening disease which often culminates into liver failure and need for urgent liver transplant. We report here long-term outcome of ASAIH patients.
Methods Retrospective analysis was done for patients getting admitted for ASAIH between July 2019 to July 2020. ASAIH was defines by first presentation with INR >2 and absence of cirrhosis/bridging fibrosis on liver biopsy with no evidence of use of herbal medicines or alternative medicines.
Results Fifteen patients were classified as ASAIH. Two-third were females with a mean age of 42 years. At baseline, mean bilirubin was 18 mg/dL, mean aspartate aminotransferase (AST) was 896 IU/L, mean alanine aminotransferase (ALT) was 650 IU/L, mean immunoglobulin (IgG) level 26.34 g/L, median INR of 4.3 and mean albumin of 3.4 g/dL. Autoantibodies were present in only six patients. Histological characteristics was plasma cell, lymphocyte and neutrophilic infiltration with interface hepatitis and lobular necrosis seen in all patients. Hydrocortisone followed by prednisolone was started in all patients with a mean of 45 days after onset of jaundice. Four patients failed to respond and died due to liver failure. Remaining patients responded to steroids and had normalization of bilirubin with a median of 56 days and are under follow-up with at least 12 months. Azathioprine was introduced in all patients once bilirubin became normal. Four patients were off immunosuppression at 12 months. All patients had normalized liver function on follow-up.
Conclusions Timely treatment may lead to resolution of ASAIH with excellent long-term outcomes in those who respond to steroids.
Keywords AIH, Steroids, Liver failure, Autoimmune liver disease
167
Treating insomnia in advanced liver disease
Pathik Parikh
Correspondence – Pathik Parikh – pathik269@gmail.com
Department of Hepatology and Liver Transplant, Zydus Hospitals, Zydus Hospitals Road, Near. Sola Bridge, Sarkhej – Gandhinagar Highway, Ahmedabad 380 054, India
Introduction Insomnia and classically difficulty falling asleep is a common problem seen in patients of advanced liver disease. Antihistaminics (138atient138d138s) has been used with minimal success.
Methods We retrospectively evaluated patients treated at our centre from January 2020 to December 2020 for advanced cirrhosis and insomnia as major complain. The treatment given and its ability to induce regular sleep at 30 days of use was considered (patient reported outcomes). Development of encephalopathy and excessive daytime somnolence (EDS) was looked for in these patients.
Results Thirty patients (mean age 42 years, all males) with advanced liver disease (CTP >6) had difficulty falling asleep as chief complain. Seven had nonalcoholic steatohepatitis (NASH) while remaining had alcohol related cirrhosis (ALD). Hydroxizine was used in 8 patients without any benefit. Zolpidem 10 mg was used in 24 patients for consecutive 30 days with all 7 patients of NASH while only 8/17 with ALD reported benefit with zolpidem use. Lorazepam 1 mg had been used in 10 patients with ALD with 70% reporting benefit in sleep induction. None of the patients developed encephalopathy after its use in 30 days. No Excessive daytime somnolence was reported by any patient although 5 patients reported better daytime efficiency after lorazepam use. After 30 days of regular use all 15 patients with Zolpidem use benefit reduced the usage to PRN basis while only 2/8 patients with Lorazepam use benefit reduced to PRN basis.
Conclusion Although benzodiazepines and Z drugs have not been considered safe in advanced liver disease, our patients benefited with sleep induction and may need larger studies to prove safety and efficacy.
Keywords EDS, Sleep induction, Liver cirrhosis
168
Case of spontaneous hemoperitoneum in a cirrhotic patient due to rupture of intra-abdominal varix
C K Adarsh, B S Puneeth, Bhuvan Shetty, Jairaj V Bomman, Pooja Krishnappa, A Vamshi
Correspondence – B S Puneeth – puneethbs1990@gmail.com
Department of Medical Gastroenterology, BGS Global Hospital, 67, Uttarahalli Main Road, Sunkalpalya, Bengaluru 560 060, India
Introduction Ectopic varices are dilated portosystemic collateral veins located in unusual sites other than gastroesophageal region. It constitute 1% to 5% of all variceal bleeds in patients with intrahepatic portal hypertension and 20% to 30% of those with extrahepatic portal hypertension. One of the most severe complications of ectopic varices is the rupture of intra-abdominal varices leading to hemoperitoneum. Most of these patients present with hypovolemic shock, with an estimated mortality of 70%.
Case report A 49-year-old male, known case of decompensated chronic liver disease, presented with increase in abdomen distension, pain abdomen and giddiness. Examination revealed hypotension (BP-80/50 mmHg), tachycardia (HR-112 bpm), Pallor, bilateral pitting pedal edema and free fluid in abdomen. Investigations showed hemoglobin 6 g %, platelet count- 90000 cells/cumm, INR-1.61. Contrast enhanced computed tomography (CECT) abdomen done showed dilated portosystemic collaterals in lower esophageal, perigastric, peripancreatic, perisplenic, umbilical region, anterior abdominal wall and in mesentery, along with splenorenal shunt, hyperdense area in pelvis measuring 12 cms x 7 cms extending up to umbilical region- suggestive of hematoma. Diagnosis of hemoperitoneum secondary to ruptured intra-abdominal varices was done, patient was treated with antibiotics and transfused with packed red blood cell (PRBC). Patient underwent TIPSS, followed by embolization of oozing superior mesenteric vein (SMV) ectopic varices at the umbilical region using coils. Preprocedure portal pressure was 37 mmHg, post-procedure portal pressure was 26 mmHg. Post coiling venogram showed no obvious contrast leak. There was no further fall in hemoglobin, patient was discharged and is on regular follow-up.
Conclusion Hemorrhage from ectopic varices generally are massive and life threatening. High clinical index of suspicion is required to make the diagnosis of ectopic varices. Due to the varied locations and complex manifestations, a multimodality approach is needed, including gastroenterologists, interventional radiologists and surgeons.
Keywords Ectopic varices, Hemoperitoneum, TIPSS
169
Associated risk of hepatic encephalopathy with use of proton pump inhibitors in cirrhotics: A systematic review and meta-analysis
Suprabhat Giri Giri . Aditya Kale, Harish Darak, Sanjay Kumar, Akash Shukla
Correspondence – Suprabhat Giri Giri – supg19167@gmail.com
Department of Gastroenterology, Seth G S Medical College and KEM Hospital, Parel, Mumbai 400 012, India
Background In patients with cirrhosis, proton pump inhibitors (PPI) overuse is common. Recently, use of long-term PPIs have associated with increased risk of complications including hepatic encephalopathy (HE), spontaneous bacterial peritonitis and mortality. However, due to study design limitations, no definite conclusions can be drawn. This meta-analysis was conducted to investigate the correlation between PPI use in cirrhosis and HE.
Methods Pubmed, Google scholar and Scopus were searched from 1990 to August 2021 for research studies that described HE incidence and PPI exposure in cirrhotics including acute-on-chronic liver failure (ACLF) and patients who had undergone transjugular intrahepatic portosystemic shunt (TIPS) placement. Meeting abstracts were excluded from analysis. The odds ratios (OR) were calculated by combining the data from the identified studies using a random effects model.
Results A total of ten studies were eligible for inclusion in the analysis which included four case-control and six cohort studies. Except for one study, rest all studies reported an association between use of PPI and increased risk of HE. Analysis showed that PPI users had an increased risk of HE compared with PPI non-users, with a pooled OR of 2.48 (95% CI 1.73–3.55). Statistical heterogeneity of Ors across studies was observed (Q statistic 128.60; p = 0.000; I2 = 93%). On subgroup analysis of two studies on incidence of HE after TIPS, the estimated OR was 3.191 (95% CI 2.03–5.01) without any significant heterogeneity. Begg’s test and Egger’s test for publication bias were not significant.
Conclusion Use of PPI is associated with increased risk of HE in patients with cirrhosis, including patients with ACLF and those who underwent TIPS. Inappropriate use of PPI should be avoided in cirrhotics. However, larger prospective studies are needed to guide clinical decision making.
Keywords Proton pump inhibitors, Cirrhosis, Hepatic encephalopathy
170
Correlation between serum ascites albumin gradient and esophageal varices in chronic liver disease patients with portal hypertension
Chilukuru Revanth Reddy, Sudhanva Kinhal, Venkata Ranga Reddy
Correspondence – Sudhanva Kinhal – sudhanvakinhal@gmail.com
Department of Gastroenterology, Kurnool Medical College, Budhwarpet Road, Budhawarapeta, Kurnool 518 002, India
Background Portal hypertension is the major complication of cirrhosis and is responsible for upper gastrointestinal bleeding due to esophageal varices. High incidence of esophageal varices in patients with portal hypertension increases the burden on endoscopy units to identify esophageal varices. Endoscopy procedure is semi-invasive, costly and not widely available, hence there is a need for non-invasive, cheap and easily available method to predict the presence of esophageal varices. The SAAG (Serum Ascites Albumin Gradient) is one such method that is thought to reflect the degree of portal hypertension and esophageal varices.
Method This study was conducted in the Department of Gastroenterology, Kurnool Medical College, Kurnool. One hundred cirrhotic patients with ascites of age more than 18 years were included in the study. All underwent upper gastrointestinal endoscopy (UGIE) to verify esophageal varices and calculated the SAAG on the same day.
Result Spearman’s Rho coefficient was used to correlate the grade of esophageal varices with SAAG levels. Our study showed that variceal grades correlated positively (p-value <0.001) with SAAG levels. SAAG >2.1 g/dL demonstrated grade 3 esophageal varices with sensitivity and specificity of 49% and 85% respectively.
Conclusion In patients with cirrhosis and ascites, SAAG could be used as a surrogate method for the presence and grading of EV, which would help to avoid multiple endoscopic procedures and reduce the cost burden.
Keywords Cirrhosis, SAAG, Esophageal varices
171
Correlation of aspartate aminotransferase to platelet ratio index score with esophageal varices in liver cirrhosis
Dharmendra Tyagi, V Venkata Ranga Reddy
Correspondence – Dharmendra Tyagi – drdtyagi89@gmail.com
Department of Gastroenterology, Kurnool Medical College, Budhwarpet Road, Budhawarapeta, Kurnool 518 002, India
Introduction Esophageal varices are the common complication of liver cirrhosis. Bleeding from esophageal varices increases the mortality and morbidity in cirrhotic patients. So screening of esophageal varices is essential in cirrhotic patients. Endoscopy is the gold standard method for screening and grading of esophageal varices. But endoscopy carries certain risks for patients, and it is also an invasive, expensive and uncomfortable procedure. Thus, there is a need to develop non-invasive methods to evaluate esophageal varices. Accordingly, aspartate aminotransferase to platelet ratio index (APRI) score has been developed for assessing esophageal varices.
Method An observational study was conducted in patients with liver cirrhosis who underwent endoscopy over a period of 18 months during 2019-2020 in the Department of Gastroenterology, Kurnool Medical College, Kurnool, Andhra Pradesh. Fifty patients of liver cirrhosis were enrolled for the study. Grading of esophageal varices was done by endoscopy, simultaneously APRI score was also calculated.
Result In this study, there was a positive correlation between esophageal varices and APRI score (p-value <0.001). APRI score >1.65 demonstrates large varices with sensitivity and specificity of 81.8% and 87.2% respectively.
Conclusion APRI score can indirectly predict the presence of esophageal varices in liver cirrhosis.
Keywords APRI score, Esophageal varices, Cirrhosis
172
Portal vein thrombosis – the common among rarities – A descriptive study from a tertiary care centre in South India
Nikhil Thomas , L Venkatakrishnan, S Mukundan, P Arun
Correspondence – Nikhil Thomas -nikhilkennythomas@gmail.com
Department of Medical Gastroenterology, PSG Institute of Medical Sciences and Research Center, Off Avanashi Road, Peelamedu, Coimbatore 641 004, India
Portal vein thrombosis (PVT) is one an important cause of portal hypertension.
In India, PVT in the absence of cirrhosis is a common cause of portal hypertension and variceal bleeding. With the current research into its genesis, majority now have an underlying prothrombotic state detectable. Acute non-cirrhotic PVT, chronic PVT (extrahepatic portal venous obstruction [EHPVO]), and PVT in cirrhosis are the three main variants of PVT with varying etiological factors and variability in presentation and management.
One hundred consecutive patients with PVT were evaluated. Sixty percent of cases were males. Splenomegaly was seen in 60 % of patients while 75% of patients had no clinical ascites. Varices were present in 53% of the subjects. Cirrhotics formed the major case group (63%) in our study, EHPVO was seen in 22 subjects. Fourteen patients has associated thrombosis of splenic vein and superior mesenteric vein, while 16 had associated either splenic or superior mesenteric vein thrombosis associated with PVT. Twelve patients had malignancy mostly hepatocellular carcinoma (HCC). Acquired prothrombotic states like polycythemia, antiphospholipid antibodies (APLA), homocystenemia, hyperuricemia, and Jak 2 mutation were found in our study and 4 patients had multiple prothrombotic states.
Anticoagulation is the mainstay of therapy for acute non-cirrhotic PVT, with supporting evidence for its use in cirrhotic population as well. Chronic PVT (EHPVO) required the management of portal hypertension as such and with role for anticoagulation in the setting of underlying prothrombotic state. Transjugular intrahepatic portosystemic shunt (TIPS), transarterial radioembolization (TARE) and liver transplant may be feasible even in the setting of PVT however proper selection of candidates and type of surgery is warranted.
Keywords Portal vein thrombosis, EHPVO, Cirrhosis
173
Diagnostic performance of non-invasive liver fibrosis risk scores in biopsy-proven non-alcoholic fatty liver disease patients in India
Manya Prasad, Sunanda Gupta, Nikky Kashyap, Umesh Kapil
Correspondence – Manya Prasad – manya.2311@gmail.com
Department of Epidemiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Background Non-alcoholic fatty liver disease (NALFD) is the most common chronic liver disease worldwide. India and other developing countries are witnessing an unprecedented rise in prevalence of NAFLD. As part of population level strategy at primary health care, an efficient risk stratification is crucial to ensure appropriate and timely referral of individuals who require care at secondary and tertiary levels. The present study was conducted to assess the diagnostic performance of two non-invasive risk scores for liver fibrosis, FiB-4 and NFS, in Indian patients of biopsy-proven NAFLD.
Methods We conducted a retrospective analysis of biopsy-proven NAFLD patients that reported to our centre between 2009 and 2015. Clinical and laboratory data were collected and two non-invasive fibrosis scores, NFS and FIB-4 score, were calculated using the original formulas. Liver biopsy was utilized as gold standard for diagnosis of NAFLD. Diagnostic performance was determined by plotting ROC (receiver operator characteristic) curves and area under the ROC curve (AUROC) was calculated for either score.
Results Two hundred and seventy-two participants were included. The mean age of patients was 40 (11.85) years and 187 (79.24%) were men. We found that the AUROCs for FiB-4 score (0.634) was higher for any degree of fibrosis as compared to NFS (0.566). The AUROC for Fib-4 for advanced liver fibrosis was 0.640 (.550-.730). The performance of the scores for advanced liver fibrosis was comparable with overlapping confidence intervals for both scores.
Conclusion The present study found an average performance of Fib-4 and NFS risk scores for detecting advanced liver fibrosis in Indian population. This study highlights the need for devising novel context specific risk scores for efficient risk stratification of NAFLD patients in India.
174
Predictors of severity and mortality of chronic liver disease with corona virus disease 2019
Shubham Jain, Sanjay Chandnani, Pravin Rathi, Sameet Patel, Partha Debnath, Pankaj Nawghare
Correspondence – Pankaj Nawghare - pankaj9ghare21@gmail.com
Department of Gastroenterology, Topiwala National Medical College, B Y L Nair Ch. Hospital, Mumbai 400 008, India
Background Corona virus disease 2019 (COVID-19) has become a major health emergency worldwide. The characteristics and outcome of COVID-19 in patients with chronic liver disease (CLD) remain unclear.
Aims CLD represents a major disease burden globally. Given this high burden, how different underlying liver conditions influence the outcome in patients with COVID-19 needs to be meticulously evaluated. So, we conducted this study to see the outcome of the patient and to look for predictors of severity and mortality in patients with CLD with COVID-19 infection.
Methods This was a single-center, observational study conducted at a tertiary care center. We recruit 50 consecutive patients of COVID-19 with CLD. Matched comparison group patients with CLD without COVID-19 collected retrospectively from historical data with 1:2 ratio using stratified sampling.
Results Mean age of the study population was 51 ± 12 years with the majority were male. Most patients (21/50) were presented with predominantly respiratory symptoms of which fever was the most common symptom (85%). Jaundice (70%) was the most common gastrointestinal symptom. Twenty patients had acute-on-chronic liver failure (ACLF). All patients with ACLF were having severe COVID-19 infection and succumb to multi-organ failure. Mortality was double in a patient with CLD with COVID-19 infection than historical control. Diabetes was the only comorbidity which was associated with severe infection. Patients in the severely ill subgroup had higher mortality, high creatinine, and raised D-dimer (p<0.05). CURB-65 (confusion, uremia, respiratory rate, BP, age ≥ 65 years) score on admission and Child-Turcotte-Pugh (CTP) score on admission correlates with mortality (p<0.05). Serum D-dimer level and reduced lymphocyte counts were associated with mortality on multivariate analysis.
Conclusion The presence of CLD in COVID-19 patients was associated with a poor outcome. Raised D-dimer on admission can predict severe infection. Child-Pugh and CRUB-65 scores were highly associated with non-survival among these patients.
Keywords COVID-19, Chronic liver disease, D-dimer
175
Non-alcoholic steatohepatitis with hepatic siderosis – are we missing porphyria ?
Vikash Prakash
Correspondence – Vikash Prakash -vikashprakashilbs@gmail.com
Department of Hepatology, D’Cosmedics Clinic, 82/A, Rash Behari Avenue, Kolkata 700 026, India
A 68-years-lady with hypertension and hypothyroidism presented with fatigue and transaminitis. Physical examination was largely normal except for a firm palpable liver of 16 cms.
Blood picture showing cholestasis a differential of primary biliary cholangitis, primary sclerosing cholangitis, autoimmune liver disease, infiltrative liver disease or simply non-alcoholic steatohepatitis (NASH) was kept in mind and patient evaluated further.
Magnetic resonance cholangiopancreatography (MRCP) was normal. Elastography showing CAP – 326 and LSM 10.8 a diagnosis of NASH with secondary iron overload was made. A liver biopsy was done to exclude differentials, assess the fibrosis and look for the amount and distribution of hepatic siderosis.
Biopsy showed – NASH with secondary siderosis (Scheuer grade 2). NAS CRN activity -6. Fibrosis 1 C. SAF score –S2A4F1C.
She was started on vitamin E, exercise and low-fat diet. She lost 8 kgs over 2 months from her initial weight of 90 kgs (BMI 32) however her facial darkening increased, and she developed itching on sun exposed parts. she was started on chelation with defepirone however her skin darkened further with involvement of hands and feet. She further lost 16 kgs of weight however her itching was intense and there was appearance of noninflammatory blisters and erosions on dorsum of hands and back. Patient was depressed and largely confined to home on account of poor quality of life, skin darkening and lesions on exposed parts.
In view of raised ferritin an occult malignancy was looked for. Heavy metals screen was also normal.
In view of all tests turning to be negative I looked back for a disease which affects both liver and skin and only one disease came to mind which is extremely rare in India namely 146atient146d. We tested urinary porphyrins which was 1564 mcg/day. Thus, a diagnosis of acquired porphyria cutanea tarda was made. Cheation had failed already. Phelobotomy was chosen over hydroxychloroquine on account of severe iron overload.
Keywords Porphyria, NASH, hemosiderosis
176
Loss of bone marrow hematopoietic stem cells reserves precedes regeneration failure and development of hepatic decompensation in cirrhosis
Nidhi Nautiyal1, Deepanshu Maheshwari2, Dhananjay Kumar2, Anupama Kumari2, Chhagan Bihari3, Rakhi Maiwall4, Subhrajit Biswas1, Anupam Kumar2, Shiv Kumar Sarin4
Correspondence – Shiv Kumar Sarin – shivsarin@gmail.com
1Amity Institute of Molecular Medicine and Stem Cell Research, Amity University, Greater Noida, AIMMSCR Department, Amity Road, Sector 125, Noida, 201 301, India, Departments of 2Molecular and Cellular Medicine, 3Pathology, and 4Hepatology, Institute of Liver and Biliary Sciences, D-1 Vasant Kunj, Delhi 110 007, India
Background and Aim Bone marrow (BM) is a reservoir for hematological and immune cells, and in response to injury these cells play a central role in resolution of the damage and tissue repair. Patients with liver cirrhosis have showed a progressive decline in hematopoietic stem cells (HSC) and their niche with an increase in severity of the disease. How this loss of HSC reserve affects the liver injury and regeneration is not well defined. In the current study we aim to understand the relation between bone marrow and liver regeneration in chronic liver injury.
Methodology C57BL/6(J) mice were used to develop chronic liver injury through intra-peritoneal administration of carbon tetrachloride (CCl4) for 15 weeks (0.1-0.5 mL/kg). Animals were culled at different time points (n=5 each group; week-3/6/10/15) to study the changes in liver injury, regeneration, and BM-HSC reserve.
Results Histological analysis of liver tissue (Fig. 1A) showed progressive increase (p=0.0079) in Masson’s trichrome (MT) positive area till week-10 with development of portal fibrosis at week-3, bridging fibrosis at week-6 and nodular fibrosis (cirrhosis) at week-10. From week 10 to week 15 while MT+ area was comparable there was significant increase (p<0.0001) in TUNEL+ hepatocyte (1D) with hepatic decompensation {ascites (SAAG 1.4 (1.1-1.7) g/dL) jaundice and rise in ammonia (p<0.001)}. With progression of liver fibrosis while number of PCNA+ hepatocyte increase till week-10, it significantly decreases from week-10 to week-15 (Fig. 1B). Flow cytometry analysis of BM-HSCs showed significant loss of long-term (LT)-HSC (p<0.001) from week-6 to week-10 and further at week-15 while number of multipotent progenitors (MPPs) increase with increase in severity (Fig. 1C).
Conclusion During the course of chronic liver injury loss of BM-HSC reserve precedes the regeneration failure leading to hepatic decompensation.
Keywords Liver cirrhosis, hepatic decompensation, Hematopoietic stem cells
177
Establishment of a murine model of acute-on-chronic liver failure with multi-organ dysfunction
Nidhi Nautiyal1, Deepanshu Maheshwari2, Dinesh Mani Tripathi2, Dhananjay Kumar2, Rekha Kumari2, Suchi Gupta3, Sachin Sharma1, Sujata Mohanty3, Anupama Parasar2, Chhagan Bihari4, Subhrajit Biswas1, Archana Rastogi4, Rakhi Maiwall5, Anupam Kumar2, Shiv Kumar Sarin5
Correspondence – Shiv Kumar Sarin – shivsarin@gmail.com
1Amity Institute of Molecular Medicine and Stem Cell Research, Amity University, AIMMSCR Department Amity Road, Sector 125, Noida 201 301, Departments of 2Molecular and Cellular Medicine, 4Pathology, and 5Hepatology, Institute of Liver and Biliary Sciences, D-1 Vasant Kunj, Delhi 100 007, India, and 3Stem Cells, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, Delhi 110 029, India
Background and Aims Acute-on-chronic liver failure (ACLF) is a distinct clinical entity with high probability of organ failure and mortality. Since patients generally present late, experimental models are needed to understand the pathophysiology and natural course of the disease.
Methodology To reproduce the syndrome of ACLF, chronic liver disease was induced in C57BL6 mice (6-8weeks; approximately 20-24 gm weight) by intra-peritoneal administration of carbon tetrachloride (CCl4) for 10 weeks followed by an acute injury with acetaminophen (APAP) and lipopolysaccharide (LPS). Blood, ascitic fluid and organs were collected to study cell death, regeneration and fibrosis.
Results At 24 hours post-APAP/LPS infusion, the liver tissue showed increased hepatocyte ballooning and endothelial cell TUNEL positivity. This was followed by progressive hepatocyte necrosis from perivascular region at day 7 to lobular region by day 11. ACLF (day 7 and day 11) animals showed increase in bilirubin (p<0.05), prothrombin time (p<0.0001), blood ammonia (p<0.001) and portal pressure post-acute hepatocellular injury similar to human ACLF. Ascites was noticed by day 11 with median serum-ascites albumin gradient of 1.2 (1.1-1.3) g/dL. In comparison to cirrhosis, ACLF group (day 7 and day 11) showed significant decrease in Sirius red (p<0.0001), collagen1 (p<0.0001) and a-SMA proportionate area (p<0.0001) with loss of hepatocytes regeneration (p<0.005). At day 11 ACLF animals also showed significant increase in serum creatinine (p<0.05) and acute tubular necrosis suggestive of organ failure, compared to cirrhosis animals.
Conclusion The CCL4/APAP/LPS (CALPS) model of ACLF mimics the clinical, biochemical and histological features of ACLF with demonstrable progressive hepatocellular necrosis, liver failure, impaired regeneration, development of portal hypertension and organ dysfunction in an animal with chronic liver disease.
Keywords Liver failure, ACLF, AKI, portal hypertension, Ascites
178
Hepatic dysfunction in medical intensive care unit patients predicts poor outcome
Sameet Patel, Parmeshwar Junare, Pankaj Nawghare, Sanjay Chandnani, Qais Contractor, Pravin Rathi
Correspondence – Sameet Patel - sameetpat8@gmail.com
Department of Gastroenterology, T N M C and B Y L Nair Ch. Hospital, Room No 717, Department of Gastroenterology, 7th Floor, OPD Building, Dr A Nair Road, Mumbai Central, Mumbai 400 008, India
Aim To evaluate the occurrence, etiology, clinical profile, laboratory profile and outcome of hepatic dysfunction in patients admitted to the medical intensive care unit (MICU). To evaluate the effect of model for end-stage liver disease (MELD) score on admission as a predictor of adverse short-term outcome in patients with hepatic dysfunction admitted in MICU.
Methods It was a prospective observational study, conducted from December 2017 to December 2018 in a tertiary care hospital. Two hundred and two patients admitted to the MICU with liver function tests (LFTs) as per the inclusion criteria were analyzed and their short-term outcome at 7 days was studied in relation to various parameters.
Results LFT abnormalities were present in 202/1126 (17.9%) of the patients admitted to MICU. Critical illness associated liver dysfunction was found in 172 (85.2%) patients, chronic liver disease (CLD) in 11 (5.4%) patients and acute viral hepatitis in 19 (9.4%) patients. Most common symptom was fever (68.3%) followed by vomiting (48.0% cases). Among LFT abnormalities, elevated transaminases, raised international normalized ratio and high MELD score on admission correlated with poor short-term outcome. Requirement for inotropes and mechanical ventilation correlated with poor short-term outcome. Mortality did not differ significantly between patients with CLD, patients with acute viral hepatitis and patients with critical illness associated hepatic dysfunction. Hepatic dysfunction in MICU was associated with poor outcome and a high short-term mortality of 114/202 (56.4%).
Conclusions Liver function abnormality is common in patients who are admitted to the MICU and its presence is an indicator of poor short-term outcome, hence early intensive management is necessary. Patients with chronic liver disease have similar outcome as patients with other critical illnesses and hence need to be treated aggressively.
Keywords Hepatic dysfunction, Abnormal Liver Function Test, Medical Intensive Care Unit
179
To study the relationship between of hepatic iron deposition and histologic severity in non-alcoholic fatty liver disease
Saurabh Bansal, Prasanta Debnath, Sameet Patel, Pankaj Nawghare, Shubham Jain, Sanjay Chandnani, Pravin Rathi
Correspondence – Saurabh Bansal – bansalsaurabh989@gmail.com
Department of Gastroenterology, Topiwala National Medical College and B Y L Nair Ch. Hospital, Mumbai 400 008, India
Introduction Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease and is present in up to 9% to 32% of the general population in India. Hepatic iron overload may be present in various chronic liver diseases and associated with the risk of toxicity and severity of the liver disease. Aim is to study the relationship between hepatic iron deposition and serum iron biomarker with histologic severity in NAFLD patients.
Methods It is an interim analysis of prospective study involving thirty adult subjects with metabolic syndrome and ultrasound sonography study of fatty liver with or without deranged liver function test. Other common causes of NAFLD were ruled out. These subjects underwent liver biopsy. On histopathological examination hepatic iron staining, hepatic steatosis, hepatic inflammation, ballooning degeneration, Hepatic fibrosis were seen. Serum iron biomarkers were measured prospectively.
Results Mean age of the study population was 45.5±23.4 years. M: F was 1.3:1. Out of 30 patients, non-alcoholic steatohepatitis (NASH) patients was 19/30 (63.3%) and non-alcoholic fatty liver (NAFL) was 11/30 (36.6). Increase serum ferritin was found in 26/30 (86.66%) of NAFLD in which 15/26 (57.7%) of NASH and 11/26 (42.3%) of NAFL. Fibrosis was present in 18/30 (60%) of NAFLD, in which mild fibrosis (F0-F1) 10/18 (55.5%) and moderate-severe fibrosis (≥F2) 8/18 (45.5%). Serum ferritin was raised in 15/18 (83.3%) of patients with fibrosis (p value=0.03). Hepatic iron staining was present in 8/30 (26.6%) of NAFLD patients in which 5/19 (26.3%) of NASH and 3/11 (27.2%) of NAFL. Hepatic iron staining was present in 5/18 (27.7%) of patients with fibrosis (p value=0.65). However, there was no association between the presence of hepatic iron deposits and serum ferritin with the NASH (p value=1.0 and 0.53 respectively). Non-invasive markers of fibrosis (NFS, FIB 4, and APRI) correlated with biopsy-proven hepatic fibrosis.
Conclusion Our study did not confirm the association between the presence of hepatic iron and serum ferritin and the severity of NASH in NAFLD.
Keywords Non-alcoholic fatty liver, Hepatic iron, Serum ferritin
180
A study of factors predicting treatment response, complications, and hepatic decompensation post conventional trans-arterial chemoembolization in patients with unresectable hepatocellular carcinoma
Suvarna Mikita Arun Meera, K Sandesh, T M Ramachandran
Correspondence – Suvarna Mikita Arun Meera - msuvarna7393@gmail.com
Department of Medical Gastroenterology, Government Medical College, 17, Mavoor Road, Kozhikode 673 008, India
Introduction According to the BCLC protocol, transarterial chemoembolization (TACE) is the first line of treatment for intermediate-stage hepatocellular carcinoma (HCC). Predicting efficacy before TACE is important for treatment planning as it can inform the decision to conduct early repeat treatment in responders or may facilitate switching to systemic therapy or second line locoregional treatment in non-responders. Also, repeated and unnecessary TACE in non-responders can aggravate impaired hepatic function in patients with liver cirrhosis. This study aims to assess the ability of various biochemical and radiological parameters to predict TACE response, decompensation post-TACE and other post-TACE complications.
Methods Sixty patients with intermediate-stage-HCC who underwent TACE were studied for up to 6 months, factors predicting TACE response, post-TACE complications including post-embolization syndrome (PES) and decompensation were assessed.
Results Sixty patients (male: female=41:19; mean age=57.95±6.48) with unresectable HCC undergoing TACE were followed-up up to a 6-month period. Twenty-seven (45%) patients achieved complete response (CR) whereas 14,12 and 7 patients had partial response, stable disease and progressive disease respectively; 4 (6.67%) had post-embolization syndrome (PES); 24 (40%) decompensated during the 6-month follow-up period. There was significant difference in MELD scores, AFP, HAP score, ESR, NLR, PLR, serum albumin, cumulative tumor size, number of tumours and >1 TACE sessions (p<0.05) between patients who had and hadn’t achieved CR. On univariate analysis, AFP<100, MELD<10, HAP<1, NLR<2, albumin>3.5 mg/dL, tumor size <3 cm, single tumour were significantly associated with CR; HAP>1, bilirubin >2 mg/dL were significantly associated with PES, clinically significant portal hypertension (CSPH), CTP score >6, MELD>10, HAP>1, NLR>2, bilirubin>2, albumin<3.5, tumor size >3 cm, tumor number>1 were significantly associated with decompensation within 6 months post TACE. On multivariate analysis AFP (p=0.013, AUROC:0.973, 95% CI:0.79-1.00), HAP <1 (p=<0.001, AUROC:0.818, 95% CI:0.708-0.928), number of TACE sessions >1 (p=<0.001) were significant predictors of response to TACE; HAP>1 (p=0.016, AUROC:0.802, 95% CI:0.681-0.923), albumin <3.5 mg/dL (p<0.001; AUROC:0.943, 95% CI:0.1-0.168) and multilobar tumor involvement (p=0.041) were significant predictors of decompensation within 6 months post-TACE. CSPH (p=.038), bilirubin >2 mg/dL (p=0.016; AUROC:0.953, 95% CI:0.756-1), multilobar tumor involvement (p:0.041) were significant predictors of post-TACE complications including PES.
Conclusion AFP<100, MELD<10, >1 TACE sessions were significantly associated with CR; patients with HAP>1, baseline Sr. albumin <3.5 mg/dL and multilobar tumor involvement are likelier to decompensate post TACE. Patients with CSPH, Sr. bilirubin >2 mg/dL and multilobar disease are likelier to develop post-TACE complications.
Keywords HCC, TACE
181
Sarcopenia as a predictor of mortality and complications in cirrhosis patients-A prospective cohort study
Nidhin Devadas, K Sandesh, K Sunilkumar1
Correspondence – Nidhin Devadas – niddas@gmail.com
Department of Medical Gastroenterology, Govt. Medical College, 17, Mavoor Road, Kozhikode 673 008, India, and 1Department of Medical Gastroenterology, Government Medical College, Gandhi Nagar, Kottayam 686 008, India
Introduction Sarcopenia is a promising tool for prognostication of cirrhosis. EWGSOP2 guidelines define sarcopenia based on muscle strength, muscle quantity or quality and physical performance. Many previous studies didn’t use a standardized definition of sarcopenia and was based on skeletal muscle measurement by CT or MRI. Ultrasound guided thigh muscle thickness (TMT) measurement is a validated, cost effective and easy method for assessment of muscle quantity. There is paucity of Indian studies analysing prognostic role of sarcopenia in cirrhosis.
Objectives To study the predictive role of sarcopenia on mortality and complications in cirrhosis patients.
Methods This was a prospective cohort study with 120 consecutive patients each in sarcopenia and no sarcopenia groups. Sarcopenia was diagnosed based on EWGSOP2 guidelines using ultrasound guided measurement of TMT. They were followed up for 6 months. Kaplan-Meier analysis with LogRank test was used to compare survival and Cox proportional hazards model was used for multivariate analysis to determine risk factors of mortality.
Results Cirrhosis patients with sarcopenia (N1=120,M:F=80:40, Median age-58yrs [51-64]) and without sarcopenia (N2=120, M:F=93:27, Median age-54 yrs [46.25-60]) were enrolled. Six (month cumulative survival was 56.7% and 76.7% in sarcopenia and no sarcopenia groups respectively [p=0.001]). Six month cumulative survival in severe and non-severe sarcopenia was 23.9% and 70% respectively (p=0.001). Age, sex, nutritional status, sarcopenia status, CTP score, MELD score, bilirubin, albumin, INR and sodium were significantly associated with survival. A multivariate analysis showed sarcopenia (HR=1.283, 95% CI 1.092-2.130, p=0.031), female sex (HR=1.851, 95% CI 1.106-3.097, p=0.019), CTP class C (HR=1.447, 95% CI 1.252-1.794, p=0.002) and MELD score>15 (HR=1.116, 95% CI 1.056-2.203, p=0.05) as independent predictors of mortality. Development of complications like ascites, HE, Covid infection and UGI bleed were significantly higher in sarcopenia group, while SBP, AKI, cellulitis, UTI, HCC and ACLF were not statistically significant between two groups.
Conclusion Sarcopenia is an independent prognostic marker of mortality in cirrhosis and is associated with increased risk of complications like ascites, HE, Covid infection and UGI bleed. Severe sarcopenia has even poorer outcome. It appears that addition of sarcopenia to existing scoring systems of cirrhosis will improve prognostication of patients.
Keywords Sarcopenia, Cirrhosis, Thigh muscle thickness
182
A comparative study of non-A-E hepatitis with acute viral hepatitis and acute onset autoimmune hepatitis
Siddhesh Rane, Shubham Jain, Partha Debnath, Rahul Deshmukh, Sanjay Chandnani, Sujit Nair, Qais Contractor, Pravin Rathi
Correspondence – Siddhesh Rane – sid.6173@gmail.com
Department of Gastroenterology, T N M C and B Y L Nair Charitable Hospital, Dr A L Nair Road, Mumbai Central, Mumbai 400 008, India
Introduction The objective was to compare clinical/laboratory features (and histopathology as needed) of non-A-E hepatitis with acute viral and acute onset autoimmune hepatitis (AIH) and determine whether etiology is likely to be viral or autoimmune.
Methods Cases of acute hepatitis were evaluated to segregate acute viral, autoimmune and non A-E hepatitis based upon viral markers and AIH-related autoantibodies. Patients with negative viral serology and revised AIH score between 10-14 (probable AIH) underwent liver biopsy. Patients with post-biopsy AIH score > 15 were diagnosed as AIH. Those with negative viral serology and post-biopsy AIH score <15 were considered as non A-E hepatitis. Patients were followed up for 3 months.
Results Out of 85 patients, 15 (17%) had non-A-E hepatitis, 25 (29%) AIH (acute presentations), 45 (53%) acute viral hepatitis (hepatitis A, B, E). Jaundice was the most common presentation (100%) of non-A-E hepatitis followed by anorexia (93%) and nausea (86%). Seven out of 15 (46.7%) patients with non-A-E hepatitis were males. Mean age was 39 years (range 15-55). Median total bilirubin was 10.7 mg/dL (range 6.5-15.4), aspartate and alanine aminotransferases were 512 and 670 U/L (range 450-777 and 649-1000 U/L, respectively). Five (33.3%) patients had anti-nuclear antibody and 1 (6.7%) had anti-smooth muscle antibody positive. Six (40%) had raised immunoglobulin G (mean 18.3 gm/L, range 12.2-29.0 gm/L). No patient developed liver failure or recurrent hepatitis. Bilirubin, aspartate and alanine aminotransferases, INR were not significantly different between all the groups. Non-A-E hepatitis is more likely to have albumin >3.5 gm/dL compared to autoimmune hepatitis (p=0.001). Patients with autoimmune hepatitis are more likely to have anti-nuclear and anti-smooth muscle antibodies (p=0.002 and <0.001, respectively), raised immunoglobulin G (p=0.003), interface hepatitis/lymphoplasmacytic infiltration/rosette formation on histopathology (p=0.0001) as compared to non-A-E hepatitis. After 3 months, AIH patients had significantly higher bilirubin and aspartate aminotransferases (p=0.02 and 0.009, respectively).
Conclusion Non-A-E hepatitis can present as a self-limiting illness. Etiology is less likely to be autoimmune.
Keywords Non-A-E hepatitis, Viral hepatitis, Autoimmune hepatitis
183
Evaluate the diagnostic accuracy of a nurse-led transient elastography in liver stiffness evaluation and competency of nurse operator to stage hepatic fibrosis in chronic liver diseases patients
Sanju Kumari 1 , Mini George 2 , Vinod Arora
Correspondence – Sanju Kumari – sanju_ilbs19@gmail.com
Department of Nursing, All India Institute of Medical Sciences, Phulwarisharif, Patna 801 505, India, and 2Departments of Con. and Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj Road, New Delhi 110 070, India
Background Once thought to be rare, liver disease is the emerging cause of significant morbidity and mortality. Recognizing the burden of disease, a competent workforce is essential to deliver quality healthcare to patients with diagnosis of, or at risk of developing liver disease. Staging of liver diseases (liver biopsy, the gold standard) is important in-patient management. Fibroscan (transient elastography) has gained importance recently as a non-invasive modality. This study examines the diagnostic accuracy of nurses-led transient elastography in staging hepatic fibrosis in chronic liver diseases (CLD).
Methods Audit of records for Fibroscan and liver biopsy done within six months of each other included 193 CLD cases in study. Data abstraction sheet and competency checklist were used. Content validity index and reliability of tool were above 0.9. Analyses was performed using SPSS V.25, with p values less than 0.05 level of significance. Diagnostic accuracy of liver stiffness evaluation (LSE) to grade hepatic fibrosis was tested against liver biopsy and a graphical plot, area under receiver operating characteristic (Figs. 1 and 2) that illustrates the diagnostic ability.
Results Spearman’s Rho correlation (Table 1) between LSE (by nurse-led Fibroscan) against liver biopsy was significant (p=0.01). One way ANOVA showed association between LSE and nurse competency in Fibroscan (p=0.001).
Conclusion Nurse-led transient elastography showed significant diagnostic accuracy in staging of hepatic fibrosis. This study can help build hospital policies to implement nurse-led Fibroscan.
Keywords Liver stiffness evaluation, Fibroscan, Nurse-led transient elastography, Liver biopsy
184
Bioenergetics failures underlie impaired monocyte function and increased mortality in acute-on-chronic liver failure
Deepanshu Maheshwari1, Rakesh Kumar Jagdish2, Dhananjay Kumar1, Nidhi Nautiyal1, Rekha Kumari1, Ashinikumar Hidam2, Rashi Sehgal1, Nirupama Trehanpati1, Sukriti Sukriti1, Guresh Kumar1, Meenu Bajpai3, Viniyendra Pamecha4, Chhagan Bihari5, Rakhi Maiwall2, Anupam Kumar1, Shiv Kumar Sarin2
Correspondence -Shiv Kumar Sarin – shivsarin@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Hepatology, 3Transfusion Medicine, 4HPB Surgery and Liver Transplant, and 5Pathology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 10 070, India
Background Monocyte-macrophage plays central role in the resolution of injury and immune defense against invading pathogens. Functional exhaustion of monocytes is associated with increased susceptibility to infection and sepsis in acute-on-chronic liver failure (ACLF). Underlying mechanism of disease-associated defects in ACLF monocyte are not fully understood. We aimed to study mechanism of functional exhaustion of monocytes in ACLF and its effect on patient outcome.
Methodology Monocytes were isolated from peripheral blood of ACLF patients (n=33) and matched healthy volunteers (HC, n=7). Phagocytic and oxidative burst functions were studied using commercial kits. Bioenergetics of monocytes was analysed using Xfe24 bioanalyzer.
Results Compared to HC, monocytes of ACLF patients (mean-age 43 years, AARC-8.9, etiology-alcohol 64%) showed a decrease in phagocytic (p<0.0001) and oxidative burst (p<0.0001) functions. Bioenergetic analysis showed defects in oxygen consumption rate (OCR) (p<0.0001) and extra cellular acidification rate (ECAR) (p<0.001) in ACLF compared to healthy (Fig. 1A). Out of 34 patients in which monocyte bioenergetics were done at time of admission, 22 died or underwent transplant (non-survivor) and 12 were alive (survivor) in 28 days of follow-up. In comparison to survivors, monocyte of non-survivor showed reduction in both mitochondrial respiration (basal respiration [BR]-p<0.001; maximum respiration [MR]-p<0.001) and glycolysis (ECAR-p<0.0001). In univariant cox regression analysis baseline ECAR (hazard ratio [HR]=9.1), OCR (HR=4.5) and MR (HR=3.5) were significantly correlated with short-term (28 days) mortality in ACLF patients. Patients with monocyte baseline ECAR <42.7 mpH/min (AUROC=0.901, sensitivity-86.9%, specificity-83.3%), BR <22.5 pmol/min (AUROC=0.81, sensitivity-75%, specificity-77.3%), and MR <37.9 pmol/min (AUROC=0.82, sensitivity-77.3%, specificity-75%) showed significant increase in mortality.
Conclusion Bioenergetic failure drives functional exhaustion of monocytes in ACLF which may underlie increased infection and sepsis in these patients. Non-survivors show increased defects in both mitochondrial as well as glycolytic function in monocytes as compared to survivors. Together these data suggest that loss of monocyte bioenergy adversely affects the outcome of ACLF patients.
Keywords Metabolism, Innate Immune Dysfunction, ACLF
185
Safety and efficacy of saroglitazar in non-diabetic non-alcoholic fatty liver disease/non-alcoholic steatohepatitis population – A 24-week, real world, single centre, retrospective study
Sobur Uddin Ahmed
Correspondence – Sobur Uddin Ahmed – drsobur1180@gmail.com
Department of Gastroenterology, Hayat Hospital, Hayat Hospital, Guwahati 781 034, India
Background and Aims Non-alcoholic fatty liver disease (NAFLD) is a spectrum of illness from non-alcoholic fatty liver to steatohepatitis, progresses to fibrosis and ultimately leads to cirrhosis, if not managed well. Saroglitazar 4 mg is only approved therapy for NAFLD/ non-alcoholic steatohepatitis (NASH). We tried to evaluate the efficacy and safety of Saroglitazar 4 mg OD in nondiabetic NAFLD/NASH in routine clinical practice.
Methods A total 40 documented NAFLD patients (Males 67.5%) prescribed on Saroglitazar 4 mg OD, were retrospectively analyzed for changes in liver biochemical parameters and lipid profile at 24 weeks. The study population was of mean age 40.6 and plusmn; 12.11 years and mean BMI 26.7 + 3.4 kg/m2. The mean NFS score at baseline was -1.7 + 1.2, with 52.5% (n=21) patients in intermediate NFS range. The data at baseline and 24 weeks was analyzed and statistical significance was established using paired sample T- test.
Results The study shows statistically significant improvements in all measured parameters from baseline. Also, there was significant improveme nt in overall NFS score by 52.7%, with 47.5% patients (n=19) in low NFS range at baseline increased to 95% (n=38), at 24 weeks. There was overall improvement in HbA1c by 0.8% (NS) from baseline, with no single episode of reported hypoglycemia.
Conclusions The study shows Saroglitazar 4 mg OD as a safe and effective treatment option for nondiabetic NAFLD/NASH, with significant improvement in all liver related parameters.
Keywords NAFLD, NFS Score, Saroglitazar
186
Predictors for mortality in dengue hepatitis
Ritesh Prajapati, Kamlesh Kumar Pravin Kumar, Rajiv Mehta, Mayank Kabrawala, Subhash Nandwani, Nisarg Patel, Mohit Sethia, Raj Tandel
Correspondence – Ritesh Prajapati – riteshprajapati87@gmail.com
Department of Gastroenterology, Surat Institute of Digestive Sciences Hospital and Research Centre, , Vijay Nagar Gate No-3, Besides Nirman Bhavan, Majura Gate, Ring Road, Surat 395 002, India
Background and Aims Hepatitis from non-hepatotrophic virus is increasing. Dengue hepatitis is the commonest cause of hepatitis from non-hepatotrophic virus in India. Hepatitis in dengue increases mortality in dengue fever by several fold. There are no prognostic markers for patients who develop dengue hepatitis.
Methods We retrospectively analyzed all patients with dengue infection admitted in two tertiary care hospitals from January 2016 to March 2021. Diagnosis of dengue fever and dengue hepatitis was confirmed by serology and standard criteria respectively
Results One hundred and ninety-nine patients with dengue hepatitis were studied of which 33 patients died. Thirty-two patients had (AKI) of which 14 required hemodialysis. Forty-five patients developed acute lung injury (ALI) of which 32 required non-invasive or invasive ventilatory support. Twelve patients developed encephalopathy. Eight patients developed acute liver failure (ALF). Level of bilirubin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), prothrombin time (PT) with international normalized ratio (INR), ferritin, platelet count, total leukocyte count (TLC) and AST-to-platelet ratio index (APRI); were not statistically different between survivors and non survivors. Lactate dehydrogenase (LDH) at presentation, creatinine and model for end-stage liver disease (MELD) score were higher among non survivors than survivors. When parameters peak ALT, peak AST, LDH on presentation, peak LDH, peak ferritin were divided by number of days from onset of fever (DF) they were found significantly higher in non survivors. peak LDH/df + peak ferritin/df was found to be significantly high in non survivors than survivors with area under the receiver operating curve (AUROC) of 0.854 and a value and GT; 9220 had sensitivity of 81% and specificity of 78%.
Conclusion Peak LDH/df + peak ferritin/df was found to be a good predictor of mortality in patients with dengue hepatitis.
Keywords Dengue, Hepatitis, Prognostic marker, Ferritin
187
Acute kidney injury among hospitalized patients with cirrhosis – Burden and risk factors
M Sandeep, K Sandesh, K Sunil Kumar, B Sithara, K Srijith
Correspondence – M Sandeep – sandu0089@gmail.com
Department of Gastroenterology, Government Medical College, 17, Mavoor Road, Kozhikode, Kerala 673 008, India
Introduction Acute kidney injury (AKI) in patients with cirrhosis is a major determinant of morbidity and mortality. Early diagnosis and management of AKI significantly influence the outcome in cirrhotic patients. We undertook this study because data on burden of AKI in hospitalized patients with cirrhosis lacks in our region.
Methods A cross-sectional study was done in our setting including 128 patients hospitalized with cirrhosis. AKI was diagnosed and staged as per ICA-AKI criteria. Risk factors for incident AKI events was recorded and their association was studied by Chi-square test. Their outcome at the end of hospital stay (in terms of survived or deceased) was recorded and mortality rate was calculated.
Results Prevalence of AKI among patients with cirrhosis admitted to hospital was 49.2% (63/128). Majority of patients who developed AKI had advanced decompensated cirrhosis at admission (CTP-A: 8, CTP-B: 18, CTP-C: 37) and early stages of AKI (Stage-1: 28, Stage-2: 20, Stage-3: 15) predominated in our study. Most common predisposing factors for AKI among cirrhotic patients were upper GI bleed (47.6%) and infections (33.3%; SBP-23.8%, other infections–9.5%), while diuretics (7.9%), non-steroidal anti-inflammatory drugs (NSAIDs) (3.1%) and prior large volume paracentesis (7.9%) were less common. Among patients with cirrhosis, AKI was found to be significantly associated with upper GI bleeding (Odds ratio [95% CI]: 5.000 [2.16-11.533], p-value < 0.05) and SBP (Odds ratio [95%CI]: 6.458 [1.768-23.593], p-value <0.05). Mortality rate among hospitalized cirrhotic patients with AKI in cirrhosis were 34.92%. Acute kidney injury was identified as a risk factor for mortality among patients with cirrhosis (Odds ratio [95%CI]: 3.823 [1.549-9.434], p-value < 0.05).
Conclusion Burden of AKI (49.2% prevalence and 34.92% mortality rate) among hospitalized patients with cirrhosis is significantly high in our region. Patients with definite predisposing factors require close monitoring for early detection of renal impairment.
Keywords Cirrhosis, AKI, Risk factors
188
Efficacy and Safety of Saroglitazar in metabolically obese versus non obese non-alcoholic fatty liver disease – A 24-week, single center, real world experience
Prabhat Ranjan
Correspondence – Prabhat Ranjan – ranjan.prabhat79@gmail.com
Department of Gastroenterology, Prabhat Ranjan Gastro Clinic, HIG Tower 5 Flat No 803, Uttorayon, Siliguri 734 010, India
Introduction Non-alcoholic fatty liver disease (NAFLD) is becoming a modern-day pandemic with prevalence almost 30% in Asian countries. The study was done to evaluate the efficacy of Saroglitazar 4 mg OD in lean vs. overweight/obese NAFLD patients, in routine clinical practice.
Methods A total 33 NAFLD patients (Males 87.9%) diagnosed on ultrasound sonography (USG) or fibroscan imaging or elevated liver function test (LFT) along with exclusion diagnosis, and prescribed on Saroglitazar 4 mg OD, were retrospectively analyzed for changes in fibroscan LFT (n=27) and other liver related parameters. The overall improvement and improvements in lean (mean BMI 24.3 + 1.4 kg/m2) vs. overweight/obese (mean BMI 27.8 + 1.5 kg/m2) NAFLD cohort, classified as per WHO Criteria of obesity, is measured at baseline and 24 weeks. The statistical significance was established using paired sample t-test.
Results The study shows significant improvements in all measured parameters from baseline in both lean vs overweight NAFLD cohort. The overall NFS score improved by 33.4% with 69.7% (n=23) patients in low NFS range at baseline increased to 93.9% (n=31) patients after 24 weeks.
Conclusions Saroglitazar 4 mg OD is found safe and equally effective in both normal weight and overweight/obese NAFLD. More studies, including well designed clinical trials will show more light on possible effect of Saroglitazar 4 mg in lean NAFLD.
Table 1: Baseline population demography (n=33)
Table 2: % Improvement in liver related end points at 24 weeks (Lean vs. over weight/obese cohort)
Keywords Lean NAFLD, NFS score, Overweight, Saroglitazar
189
Ultrasound sonography based elastography correlation with APRI, FIB 4, and non-alcoholic fatty liver disease fibrosis score in non-alcoholic fatty liver disease
Pradeep Nigam, S K Issar, Jeevanlal Gheedle, Pratibha Issar1, Pranav Chandak1
Correspondence – Pradeep Nigam – nigamsonal2012@gmail.com
Department of Gastroenterology, and 1Radiodiagnosis, Jawahar Lal Nehru Hospital and Research Center, Sector 9, Bhilai 490 009, India
Upsurge in the prevalence of the non-alcoholic fatty liver disease (NAFLD) has brought up it as one of the most frequent culprits of cirrhosis worldwide and features of metabolic syndrome have been found as the most common association, influencing its prognosis and progression to liver fibrosis. Even after one-fourth of the general population being affected worldwide, diagnosed NAFLD cases are the tip of the iceberg, with less than 10% being referred to specialists. Early diagnosis of advanced liver fibrosis in NAFLD remains an uphill task in clinical practice as these are at the greatest risk of developing complications. The gold standard liver biopsy being invasive has many inherent shortcomings, favoring the non-invasive tests.
Method Prospective observational study on 148 consecutive ultrasound sonography (USG) diagnosed NAFLD. Liver stiffness correlated with APRI, FIB 4, and NFS.
Results 51.36% have increased stiffness (> 5.7 Kpa). FIB4 <= 1.45, between 1.45 to 3.25 and > 3.25 were seen in 66.22%, 27.03% and 6.76% respectively. Those with FIB4 > 3.25, 60% patient had F2-3 fibrosis and 20% had F1 fibrosis. NFS <= -1.45 is found in 52.7% and 47.30% had > -1.45. patients with NFS <= -1.45, 69.23% and 30.77% have normal and F1 fibrosis respectively. NFS >= 0.675 45.83% and 41.67% have F2-3 and F1 fibrosis respectively. Metabolic syndrome was the most common association with NAFLD (77.7%) and have increased risk of liver fibrosis which further increases with the increased number of component of metabolic syndrome. Past history of NAFLD had increased risk of advanced fibrosis.
Conclusion APRI, FIB4, and NFS all correlate accurately in ruling out or in liver fibrosis, FIB4 and NFS in combination with USG elastography can be used for surveillance of NAFLD patients for early diagnosis of liver fibrosis and its progression to prevent complications and early referral to a specialist.
Keywords Non-alcoholic fatty liver disease, Liver stiffness, FIB4
190
Circulating tumor cells assessment in patients with hepatocellular carcinoma by imaging flowcytometry and it`s relationship with staging – Interim analysis
Pravin Rathi1, Partha Debnath1, Kruti Dalal2. Bhavik Dalal2, Shreyasi Athalye2, Saurabh Bansal1, Rahul Deshmukh1, Shubham Jain1, Sanjay Chandnani1, Aruna Shankarkumar2
Correspondence – Partha Debnath – partha628@gmail.com
1Department of Gastroenterology, T N Medical College and B Y L Nair Ch. Hospital, Mumbai 400 008, India and 2Transfusion Transmitted Diseases Department, 13th Floor, New Multi-Storeyed Building, K E M Hospital Campus, Parel, Mumbai 400 012, India
Introduction Circulating tumor cells are considered as potential biomarkers for the detection of hepatocellular carcinoma (HCC). It is expected to play an important role in early diagnosis and dynamic monitoring. Aim of this study was to evaluate the relationship of circulating tumor cells with HCC Barcelona Clinic Liver Cancer (BCLC) staging.
Methods An imaging flowcytometry method, using immunofluorescence of cytokeratin, EpCAM (Epithelial Cell Adhesion Molecule), alpha-fetoprotein (AFP) together with the analysis of size, morphology and deoxyribonucleic acid (DNA) content for detection of circulating tumor cells was developed and applied to 20 HCC patients and 10 patients with cirrhosis of liver without any evidence of hepatic or extrahepatic malignancy.
Results Among 20 HCC patients 17 (85%) were male. Two patients were BCLC stage A, 5 were BCLC stage B and 13 were BCLC stage C. Out of 10 cirrhotic patients 7 were Child-Turcotte-Pugh (CTP) B and 3 were CTP C. Circulating tumor cells were detected in 20 of 20 patients of HCC and none among cirrhosis of liver patients. Mean number of circulating tumor cells were 9.9 (range 1- 20). Circulating tumor cells positive for EpCAM were detected in 18 patients with mean value of 4.6. Circulating tumor cells positive for cytokeratin were detected in 16 patients with mean value of 1.8. Circulating tumor cells positive for AFP were detected in all patients with mean value of 3.5. The number of circulating tumor cells were significantly associated with BCLC stage (p<0.0005) and portal vein thrombosis (p=0.025).
Conclusion This study shows the potential role of circulating tumor cells as a biomarker of HCC and also a significant association between the number of circulating tumor cells with BCLC staging and portal vein thrombosis.
Keywords Circulating tumor cells, Hepatocellular carcinoma
191
Elevated alpha-fetoprotein in the absence of hepatic malignancy in a patient with acute hepatitis
Jacklyn So Cabahug , Marc Lustre, Rafael Chan, Janus Ong
Correspondence – Jacklyn So Cabahug – jacklynmso@gmail.com
Section of Gastroenterology and Digestive Endoscopy, Manila Doctors Hospital, 667 United Nations Avenue, Ermita, Manila, 1000 Metro Manila, Manila 1000, Philippines
Introduction Patients with elevated alpha-fetoprotein (AFP) have long been associated with hepatic malignancy, but there are other benign causes of AFP elevation, especially in chronic liver disease. This case illustrates one such exemption. On the background of a previous EBV infection, patients can develop Epstein-Barr virus (EBV) hepatitis, EBV related autoimmune hepatitis, or autoimmune reaction to EBV. The history and the clinical profile of the patient is essential in directing the evaluation of these patients.
Methods Case report
Results The patient is a 26-year-old Asian male presenting with jaundice. He had no personal or family history of liver disease, occasional alcohol use, and denies drug or supplement use. Laboratory workup revealed hepatocellular type of liver injury (total bilirubin of 478 umol/L, direct bilirubin 401 umol/L, indirect bilirubin 77 umol/L, aspartate aminotransferase (AST) 1135 U/L, alanine transaminase (ALT) 1592 U/L, lactate dehydrogenase (LDH) 53 U/L, alkaline phosphatase (ALP) 139 u/L), elevated AFP (3337 IU/mL), elevated international normalized ratio (INR), positive autoimmune panel (ANA, anti-Sm, anti-TPO, anti-TG). Serological examinations revealed past infection with EBV and cytomegalovirus (CMV). Imaging tests did not show ductal obstruction or the presence of mass lesions. Subsequent liver biopsy demonstrated interface hepatitis. The patient was treated as a case of autoimmune hepatitis and was started on glucocorticoids with clinical and biochemical improvement including normalization of AFP levels.
Conclusion This study demonstrated the low specificity of AFP as it relates to these unusually elevated levels even as compared to other studies on non-malignant cases of liver disease. In this patient with acute hepatitis, AFP elevation may represent hepatic regeneration.
Keywords Case report, AFP, EBV, Acute hepatitis
192
Congenitally corrected transposition of great vessels with Crigller-Najjar syndrome type II and glucose-6-phosphate dehydrogenase deficiency- A rare association
Amit Joshi , K K Sharma 1
Correspondence – Amit Joshi – dradjoshirajkot@gmail.com
Departments of Gastroenterology and 1Cardiology, Tricolour Hospitals, Vikram Sarabhai Road, Near Genda Circle, Vadodara 390 007, India
Introduction Crigler-Najjar syndrome type II is a rare disorder of bilirubin conjugation characterized by severely reduced (<10%) UGT1A1 enzyme activity. Here we present a rare case of congenitally corrected transposition of great vessels with Crigler-Najjar syndrome type II and glucose-6-phosphate dehydrogenase (G6PD) deficiency.
Case Report Twenty-eight-year-old male patient, known case of congenitally corrected transposition of great arteries presented with dyspnea. Patient gave history of long-standing jaundice since 10 years without any history of cholestasis, or hepatic decompensation. On examination- he had scleral icterus and bilateral pitting pedal edema and features of cardiac failure with tender hepatomegaly.
His hemogram was unremarkable. His liver biochemistry panel showed total bilirubin of 11.4 mg/dl, direct bilirubin-2.45 mg/dL, indirect bilirubin 8.99 mg/dL, serum glutamic-oxaloacetic transaminase (SGOT) -76 U/L, serum glutamic pyruvic transaminase (SGPT) -112 U/L, alkaline phosphatase 65 U/L, gamma-glutamyl transferase (GGT) – 35 U/L, total protein- 7.01 g/dL, serum albumin- 3.71 g/dL, international normalized ratio (INR) – 1.13. His ultrasound abdomen was suggestive of enlarged liver (22 cm) with normal echotexture. Baseline echocardiogram was suggestive of atrial fibrillation with high ventricular rate and echocardiography was suggestive of congenitally corrected transposition of great vessels with biventricular failure. He was found to be deficient in G6PD enzyme. His serum ceruloplasmin was normal. His UGT1A1 gene polymorphism showed 7/7 TA repeats for UGT1A1*28/*28 which was suggestive of severely reduced activity of enzyme UDP glucuronyl transferase. Patient was started with low dose phenobarbitone. The work up for raised transaminase revealed IgM anti-HAV positive. However due to his pre-existing cardiac ailment patient went into refractory cardiogenic shock and ultimately succumbed to his disease.
Discussion Patient with Crigler-Najjar syndrome type II generally have indirect bilirubinemia (levels more than 5 mg/dL) with normal transaminases. As stress of congestive cardiac failure lead hyperbilirubinemia of such high levels and raised transaminases could be explained by acute hepatitis A and congestive hepatopathy secondary to congestive cardiac failure.
Keywords Crigler-Najjar syndrome type II
193
Hand grip strength: A effective bedside screening tool to detect sarcopenia and predict survival in patients with chronic liver disease
Gajanan Rodge , Usha Goenka 1 , Shivaraj Afzalpurkar, Surabhi Jajodia 1 , Vikas Prakash, Mahesh Goenka
Correspondence – Gajanan Rodge - grodge3@gmail.com
Institute of Gastrosciences and Liver, and 1Department of Clinical Imaging and Interventional Radiology, Apollo Multi-Speciality Hospital , 58, Canal Circular Road, Kolkata 700 054, India
Background Hand grip (HG) strength is measured by the hand grip dynamometer and is a simple bed side tool for assessment of nutritional status. L3 Psoas Muscle Index (PMI) is a CT based method for sarcopenia assessment. The aim of this study was to assess sarcopenia in cirrhotics by HG strength and its correlation with sarcopenia on CT scan.
Methods The hand grip strength was measured after the patient was rested on a chair and the handle of the dynamometer was adjusted. Patients were advised to hold the instrument away from the body and table and apply possible maximal strength with the dominant hand. Three readings were noted with a gap of more than 30 sec and the highest recorded value of HG strength was recorded.
Results Seventy-five consecutive patients were assessed for the HG strength and psoas muscle on CT scan. The cut off values for diagnosis of HG weakness and sarcopenia were derived from the local control group (n=75). HG weakness was seen in 41.3% (n=31) and sarcopenia assessed by PMI was seen in 36% (n=27) of the CLD patients. Fifty-three out of 75 patients completed the follow-up period of 1 year. Out of patients who succumbed to liver related illness on follow-up, 77.8% (n=7) had HG weakness, while 22.2% (n=2) without HG weakness expired during follow-up. The association of 1 year mortality and HG weakness was statistically significant (p value = 0.01). The Kappa measure of agreement between HG and sarcopenia assessment was 0.608 (good strength of agreement). The spearman’s rho correlation coefficient between HG weakness and PMI sarcopenia (Fig. 1) was 0.556 (p value <0.05).
Conclusions In conclusion, HG weakens, and PMI sarcopenia had a good strength of agreement and HG weakness predicted poor survival among patients with chronic liver disease.
Keywords Hand grip, Sarcopenia, CLD
194
A rare presentation of autoimmune hepatitis mimicking Wilson’s disease
Nilanjan Kar , Sujata Devi, Anupam Dey, Debananda Sahoo
Correspondence – Nilanjan Kar – Karnilanjan8@gmail.com
Department of General Medicine, All India Institute of Medical Sciences, Sijua, Patrapada, Bhubaneswar 751 019, India
Autoimmune hepatitis and Wilson’s disease are close differentials in middle aged female presenting with subacute hepatitis. Here we present a challenging case of autoimmune hepatitis mimicking Wilson’s disease. Fifty-two-year-old female presented to outpatient department with yellowish discoloration of sclera since one week which progressed over next one month. No history of complementary and alternative medication intake. On presentation, icteric sclera and mild bipedal edema were noted besides positive shifting dullness. Total bilirubin was raised 26 mg/dL with direct: indirect 0.85 with disproportionately raised aspartate aminotransferase (AST) (655 U/L) more than alanine aminotransferase (ALT) (251 IU/L) and normal alkaline phosphatase (ALP) (127 IU/L). total protein was 5.5 gm/dL with albumin: globulin 0.77and international normalized ratio (INR) was 1.55. ascitic fluid analysis revealed high saag low protein with no spontaneous bacterial peritonitis. viral serology were nonreactive. ana IFA was 1+(1:100), nuclear homogeneous pattern and DCT 1+(IGG). However, ana profile, anti SMA, anti LKM, anti SLA, serum ACE were negative. 24-hour urine protein was 312 mg. contrast-enhanced computed tomography (CECT) abdomen delineated hepatomegaly with mild ascites. upper GI endoscopy showed esophageal candidiasis with mild portal hypertensive gastropathy. Surprisingly serum ceruloplasmin was below 20 mg/dL with elevated urinary copper level 300 microgram. KF Ring was absent with normal brain magnetic resonance imaging (MRI) scan and magnetic resonance cholangiopancreatography (MRCP) with no evidence of cardiomyopathy on 2D echocardiography; but nerve conduction study delineated asymmetrical motor axonal neuropathy involving left lower and bilateral upper limbs. Possibility of both autoimmune hepatitis and Wilson’s disease were doing rounds. Hence, she underwent liver biopsy which confirmed the findings of autoimmune hepatitis (lymphoplasmacytosis, interface hepatitis, bridging fibrosis, focal pericholangitis) with no siderosis on Perls stain and quantitative copper content 60 microgram/gram of liver. She was started on oral steroids but unfortunate she became covid positive and ultimately succumbed to death shortly. This interesting case shows the importance of rulling out the possibility of more prevalent autoimmune hepatitis before reaching diagnosis of Wilson’s disease.
Keywords Subacute hepatitis, Wilson disease, Autoimmune hepatitis
195
To study the relationship between hepatic iron deposition and histologic severity in non-alcoholic fatty liver disease
Pravin Rathi, Saurabh Bansal, Prasanta Debnath, Sameet Patel, Pankaj Nawghare, Shubham Jain, Sanjay Chandnani
Correspondence – Saurabh Bansal – bansalsaurabh989@gmail.
Department of Gastroenterology, Topiwala National Medical College and B Y L Nair Ch. Hospital, Mumbai 400 008, India
Introduction Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease and is present in up to 9% to 32% of the general population in India. Hepatic iron overload may be present in various chronic liver diseases and associated with the risk of toxicity and severity of the liver disease. Aim is to study the relationship between hepatic iron deposition and serum iron biomarker with histologic severity in NAFLD patients.
Methods It is an interim analysis of prospective study involving thirty adult subjects with metabolic syndrome and USG s/o fatty liver with or without deranged LFT. Other common causes of NAFLD were ruled out. These subjects underwent liver biopsy. On histopathological examination hepatic iron staining, hepatic steatosis, hepatic inflammation, ballooning degeneration, hepatic fibrosis were seen. Serum iron biomarkers were measured prospectively.
Results Mean age of the study population was 45.5±23.4 years. M: F was 1.3:1. Out of 30 patients, non-alcoholic steatohepatitis (NASH) patients was 19/30 (63.3%) and non-alcoholic fatty liver (NAFL) was 11/30 (36.6). Increase S. ferritin was found in 26/30 (86.66%) of NAFLD in which 15/26 (57.7%) of NASH and 11/26 (42.3%) of NAFL. Fibrosis was present in 18/30 (60%) of NAFLD, in which mild fibrosis (F0-F1) 10/18 (55.5%) and moderate-severe fibrosis (≥F2) 8/18 (45.5%). S. ferritin was raised in 15/18 (83.3%) of patients with fibrosis (p value=0.03). Hepatic iron staining was present in 8/30 (26.6%) of NAFLD patients in which 5/19 (26.3%) of NASH and 3/11 (27.2%) of NAFL. Hepatic iron staining was present in 5/18 (27.7%) of patients with fibrosis (p value=0.65). However, there was no association between the presence of hepatic iron deposits and serum ferritin with the NASH (p value=1.0 and 0.53 respectively). Non-invasive markers of fibrosis (NFS, FIB 4, and APRI) correlated with biopsy-proven hepatic fibrosis.
Conclusion Our study did not confirm the association between the presence of hepatic iron and serum ferritin and the severity of NASH in NAFLD.
Keywords Non-alcoholic fatty liver, Hepatic iron, Serum ferritin
196
Severe hyponatremia as a prognostic indicator and mortality predictor in cirrhotic patients with refractory ascites – A prospective cohort study
Mithun K Unni
Correspondence – Mithun K Unni - mithunkunni@gmail.com
Department of Medical Gastroenterology, Government Medical College, 17, Mavoor Road, Kozhikode 673 008, India
Background In MELDNa score serum sodium concentrations numerically capped between 125 and 140 mmol/L. The prognostic value of severe hyponatremia (serum sodium <125 mmol/L) in cirrhotic patients with refractory ascites as an independent predictor of mortality and complications has to be studied.
Aim To assess the validity of severe hyponatremia in predicting mortality and complications in cirrhotic patients with refractory ascites. Also, to assess the prevalence of severe hyponatremia in these patients.
Methods One hundred and two consecutive cirrhotic patients with refractory ascites were included. They were classified into two groups A) with serum sodium < 125 meq/L and B) with serum sodium > 125 meq/L. Mortality at 3 months and 6 months were assessed. Readmissions and complications like infections, hepatic encephalopathy and hepatorenal syndrome were also studied.
Results Patients with refractory ascites (n=102) (M:F 76:26, mean age 53.6 years +/- 12.6 ) were followed up for a period of 6 months. At presentation, median serum sodium level was 129.5 meq/L and median MELDNa level was 29. 35.29 % patients had diuretic intractable ascites due to severe hyponatremia. Severe hyponatremia was significantly associated with early mortality and complications in patients with refractory ascites in univariate analysis. Serum sodium, MELD and CTP scores were independent predictors of mortality on multivariate analysis. Serum sodium (AUROC 0.91, 95% CI 0.87-0.95) was comparable to CTP score (AUROC 0.92, 95% CI 0.891-0.961) and better than MELDNa score (AUROC 0.74, 95% CI 0.64-0.80) in predicting death at 3rd and 6th months.
Conclusion Severe hyponatremia is comparable to CTP score and superior to MELDNa in predicting mortality and complications in refractory ascites.
Keywords Severe hyponatremia, Refractory ascites
197
Low levels of high-density lipoprotein (HDL-C) can predict risk of decompensation in patients with chronic liver disease
Siddharth Wable, B Harshavardhan Rao, Shine Sadasivan, G Rajesh, Anoop Koshy, Vinodkumar Ankarat, Priya Nair, Sandeep Nair
Correspondence – Harshavardhan Rao. B – harshavardhan@aims.amrita.edu
Department of Medical Gastroenterology, Amrita Institute of Medical Sciences, Peeliyadu Road, Ponekkara, Edappally, Ernakulam, Kochi 682 041, India
Introduction Systemic inflammation (SI) triggered by bacterial products like lipopolysaccharides in the circulation is an important factor leading to decompensation in patients with chronic liver disease (CLD). High density lipoprotein cholesterol (HDL-C), apart from its primary role in lipid homeostasis, has been shown to have a significant role in innate immune response to bacterial products in the circulation. In addition, HDL-C has been shown to modulate immune response by negatively regulating T-cell activation and influencing expression of inflammatory mediators in macrophages and dendritic cells. In this study, we have explored the role of HDL-C as a prognostic marker for decompensation in patients with CLD.
Methods This was a prospective, observational, cohort study where consecutive patients with CLD were included. Patients with cholestatic liver disease and hepatocellular carcinoma were excluded. Fasting lipids were measured in all patients at the time of recruitment. Each patient was carefully followed up for development of decompensation events such as new onset/worsening ascites, hepatic encephalopathy, or variceal bleed for a minimum period of one year during follow-up.
Results A total of 142 patients were included (Mean age 61 ± 10.98 years, M:F=6.1). At the end of follow-up, 83/142 patients (58.4%) had decompensation events. Mean HDL-C levels were significantly lower among patients with decompensation events (26.5 ± 13.58 mg/dL vs. 43.6 ± 14.2 mg/dL: p value 0.003). Using ROC analysis, cut-off for HDL-C of 35.6 mg/dL was identified. On multivariate analysis, HDL-C (OR = 5.661; 95% CI 2.19-14.59) was found to have an independent association with risk of decompensation.
Conclusions HDL-C levels (<35.6 mg/dL) is a reliable marker for risk of decompensation and can be a useful addition to existing prognostic scoring systems in CLD. It can be a valuable tool to streamline treatment protocols and prioritise liver transplantation.
Keywords Cirrhosis, Liver, Lipoprotein, Decompensation, Systemic, inflammation
198
Correlation of serum ammonia with grades of hepatic encephalopathy
Rajpreet Brar
Correspondence – Rajpreet Brar – rajpreetsingh811@gmail.com
Department of Gastroenterology, MMIMSR, E19 E Block, M M University, Mullana, Ambala 133 203, India
Background Hepatic encephalopathy (HE) is a serious neuropsychiatric complication of both acute and chronic liver disease. The affected patients exhibit alterations in psychomotor, intellectual, cognitive, emotional, behavioral and fine motor functions.
Methods Fifty-eight patients of HE were enrolled in our study for the duration of 2 years. We aimed to look for the correlation of grades of HE with serum ammonia levels. The data was compiled by SAS-6.50 version. Regression analysis was employed to find the significance of the relationship between encephalopathy grades and various clinical parameters of encephalopathy patients.
Results In our study, the correlation of serum ammonia was significant with the grade of encephalopathy. Hence, the serum ammonia correlated well with the grade of encephalopathy for the patients during their hospital stay, suggesting that the serum ammonia level was an indicator of the clinical outcome of the patients during their hospital stay.
Conclusion In our study, we found that there is a strong correlation between serum ammonia level and severity of liver disease. We found that high grade i.e. grade III and IV patients had significantly raised ammonia level.
Keywords Serum ammonia, Hepatic encephalopathy, Outcome
199
Correlation between B-type natriuretic peptide (BNP) and severity of disease and 90-day mortality in decompensated cirrhosis patients; A prospective study
Saumyaleen Roy
Correspondence – Saumyaleen Roy – saumyaleenroy1987@gmail.com
Department of Gastroenterology, Indira Gandhi Institute of Medical Sciences, Bailey Road, Sheikhpura, Patna 800 014, India
Introduction Fluid overload is the most frequent complication of end-stage liver disease, regardless of its etiology. Brain natriuretic peptide (BNP) is a cardiac neurohormone that is secreted from the ventricles in response to increased pressure or volume. The major physiological effects of BNP are vasodilation and natriuresis. In this study the prognostic role of BNP as a marker of severity of liver disease will be investigated
Aim of the Study Correlation of BNP with 90-day mortality, severity of disease and with number of paracentesis that the patient underwent during the 90 days period.
Methods It is a prospective observational study conducted in the Department of Gastroenterology, IGIMS. Inclusion Criteria Decompensated CLD patients diagnosed clinically and radiologically and having no systolic heart failure (ef >55%). Exclusion Criteria Patients with heart failure, arrhythmia, coronary artery disease, pulmonary hypertension, chronic kidney disease.
Results Out of 105 patients enrolled, 40 patients did not meet our inclusion criteria. A total of 65 patients were followed for 3 months and out of which 22 patients died. Majority of the patients were alcoholic, and cause of death were UGI bleed. Mean CTP and MELD Na levels were 11 and 24 in patients who died in 3 months and 9.8 and 20 in patients who survived. Mean number of paracenteses in alive patients were .54 and died patients were 1.16. Mean BNP levels were 270.19 who expired and 153.16 who were living with p value .057. BNP corelating with CTP and MELD Na scores with correlation coefficient .239 and .279 and p value .059 and .027.
Conclusion BNP positively corelating with severity of liver disease, 90 day mortality and number of paracentesis.
Keywords BNP, Mortality, Paracentesis
200
Osmotic demyelination syndrome mimicking hepatic encephalopathy in a chronic alcoholic with alcoholic liver disease
Nikita Sirohi, Arvind Sahni, Mohinish Chhabra
Correspondence – Mohinish Chhabra – mohinishchhabra@fortishealthcare.com
Department of Gastroenterology, Fortis Hospital, Jail Road, Sector 62, Sahibzada Ajit Singh Nagar, Mohali 160 062, India
Osmotic demylination syndrome (ODS) also called central pontine myelinosis (CPM), is defined as a acute, severe, non–inflammatory neurological disorder which is characterized by rapid destruction of myelin sheath, mainly of oligiodendritic cells with relatively well preserved axons and neuronal cell bodies. Pontis basalis is the most commonly affected site in the brain. The commonest precipitating cause of this syndrome is rapid correction of hyponatremia which results in rapid osmotic shifts and neuronal cell dehydration leading into damage of the myelin sheath.
Other precipitating causes of this syndrome include chronic alcoholism especially in the withdrawal phase, patients of chronic kidney disease (CKD) and dialysis, acute liver failure and post liver transplant.
Case Summary A 51-year-old male patient who had a background history of chronic alcohol consumption of more than 100 grams daily from 20 years presented with gait disturbances for 2 months and developed altered sensorium, tremors and quadriparesis needing intensive care unit (ICU) care. Magnetic resonance imaging (MRI) brain showed a well-defined focal, central trident shape area of hyperintensity T2 weighted image in the region of median pons consistent with a diagnosis of Central pontine myleinosis.
Conclusion CPM is frequently underdiagnosed and underreported in clinical setting. it may mimic hepatic encephalopathy. CPM may occur in a patient with chronic alcohol intake even without rapid correction of hyponatremia. overall CPM has a dismal prognosis with high mortality or permanent neurological sequalae in 33% to 50% cases. The mechanism of CPM in a chronic alcoholic patient includes, malnutrition, dyselectrolytemia, alcohol withdrawal and nutritional deficiencies. MRI brain must be done in all patients who have a significant history of alcohol intake and present with any acute neurological symptoms
Keywords Ods-osmotic demyelination syndrome
201
Corona virus disease 2019 and acute-on-chronic liver failure–A case presentation with literature review
Nikita Sirohi, Arvind Sahni, Deepak Bhasin
Correspondence – Deepak Bhasin – deepakbhasin@fortishealthcare.com
Department of Gastroenterology, Fortis Hospital, Mohali 160 061, India
SARS COV-2 is a newly emerging, highly transmissible and pathogenic corona virus which has caused a pandemic with global public health emergency and financial crisis.
Elderly patients, including patients with diabetes and obesity are more vulnerable to this disease. Patients with pre-existing liver disease particularly liver cirrhosis, are 4 times likely to die due to corona virus disease 2019 (COVID-19) infection. This severe disease translates in to increased hospitalization rates with increase in ICU care and the need for ventilation and RRT which in turn leads to high mortality.
Case Summary A 53-year-old male patient with non-alcoholic steatohepatitis (NASH) related liver cirrhosis who was listed for (ldltx). One week before his scheduled liver transplant, presented to OPD with generalized weakness, oliguria and hypotension. RT-PCR for COVID -19 was positive. Patient was admitted in MICU where he developed acute-on-chronic liver failure (ACLF) grade 3. Patient needed Inotrope support and mechanical ventilation for his disease progression. Despite optimal medical intensive care, patient did not survive.
Conclusions COVID-19 related mortality is significantly associated with severity of pre-existing liver cirrhosis. Majority (80%) of the patients with COVID-19 and ACLF die because of respiratory failure. COVID-19 can cause ACLF. Various mechanisms involved are –cirrhosis associated immune dysfunction, cytokine storm, persisting SIRS, multioragan damage and intestinal dysbiosis. Up to 80% of patients with cirrhosis who require ICU support will not survive.
There is urgent need to prioritize patient with CLD including those who need liver transplant to get vaccinated against COVID-19. The safety and immunogenicity of mRNA and Adeno viral vector vaccines is documented.
Keywords SARS COV2
202
Non-alcoholic steatohepatitis related cirrhosis, presenting as hepatic hydrothorax – Case report with literature review
Nikita Sirohi, Arvind Sahni, Mohinish Chhabra, Abhishek Prasad1
Correspondence – Mohinish Chhabra – mohinishchhabra@fortishealthcare.com
Departments of Gastroenterology, and 1Radology, Fortis Hospital, Mohali 160 062, India
Hepatic hydrothorax (HH) is rare presentation of PHTN which accounts for 2% to 3% of all pleural effusions. HH is defined as accumulation of transudative fluid more than 500 mL in pleural cavity in patients with decompensated cirrhosis after excluding cardiopulmonary and pleural diseases. The most accepted mechanism is direct passage of the fluid from the peritoneal to the pleural cavity through diaphragmatic defects. The treatment of HH is challenging and need a multidisplinary approach. Spontaneous bacterial empyema (SBE) is a complication of HH which is seen in 13% of cases. Management includes antibiotics and drainage. Liver transplant is the treatment of choice for HH and SBE.
Case report A 59-year-old female diabetic patient presented with progressive shortness of breath and cough since 6 weeks with h/o ATT drugs for 1 weeks prior to hospitalization. Analysis of pleural fluid is transudative and ascitic fluid shows high SAAG. Chest imaging reveal large Rt side pleural effusion with collapse CT abdomen was consistent with liver cirrhosis and PHTN. Pleural catheter was inserted and approximately 14 litre of fluid was drained over next 2 weeks, along with low sodium diet, albumin, fluid restriction and diuretics. Patient was councelled for liver transplant and underwent a live donor liver transplant (LdLT) within 2 months of admission.
Conclusion All patients of HH and SBE must be considered for liver transplant whenever feasible If transplant is not feasible TIPS should be considered. In addition to aggressive medical therapy indwelling pleural catheter have important role in management of HH and SBE. Long-term survival after liver transplant in HH and SBE is similar to patients transplanted for other indications.
Keywords Hepatic hydrothorax
203
Assessment of frailty by short physical performance battery in patients with liver cirrhosis and its ability to predict mortality and hospital re-admissions
Susheel Bhattad, L Sahitya, V Gopal Krishna, M Ramanna, M Uma Devi, B Ramesh Kumar
Correspondence – Susheel Bhattad – susheelbhattad@gmail.com
Department of Medical Gastroenterology, Osmania Medical College, 5-1-876, Turrebaz Khan Road, Troop Bazaar, Koti, Hyderabad 500 095, India
Introduction Cirrhosis of liver with its complications causes significant morbidity and mortality. Diminished physiological function and frailty can predict morbidity, hospitalizations, and mortality. Out of many frailty screening tools, short physical performance battery (SPPB) is a promising, quick, reliable, bedside tool that provides uniform, standard parameters.
Aim To evaluate frailty in cirrhotic patients by SPPB and its ability to predict 90 days mortality and hospital re-admissions.
Methods One hundred and three patients with liver cirrhosis presenting to OGH, Hyderabad were recruited. Clinical assessment, routine laboratory tests were performed and SPPB frailty index, CTP score, MELD-Na score were calculated on admission. Patients were followed up for re-hospitalizations and mortality for 90 days.
Results The mean age of patients was 44.89 ±10.02 years. Eighty-four were males and 19 were females. The most common etiology for cirrhosis was alcohol (69.69%). The mean SPPB score was 8.32 ± 2.87. 58.3% patients were frail (SPPB score <10). The SPPB score had significant positive correlation with Hb (p-0.028), mid arm circumference (p-0.004), BMI (p-0.028) and albumin (p-0.003) whereas it had significant negative correlation with age (p-0.028), CTP score (p<0.001), MELD-Na score (p<0.001). The overall 90-day mortality rate was 30.1% and readmission rate was 40.77%. The SPPB score differed significantly between survivors (9.29 ± 2.50) and non-survivors (6.06 ± 2.38) [p<0.001] as well as between re-admitted (7.83 ± 3.01) vs. non-re-admitted patients (8.66 ±2.74) [p-0.015].
Conclusion SPPB score is a helpful tool in assessing frailty in cirrhotic patients and can be used to predict mortality, hospital readmissions. Low SPPB scores are associated with poor outcomes.
Keywords Cirrhosis, Frailty, SPPB
204
Albumin bilirubin (ALBI) score: A new model to predict mortality in decompensated cirrhotic patients
Anand Pandey , L Sahitya, V Gopal Krishna, M Ramanna, M Uma Devi, B Ramesh Kumar
Correspondence – Anand Pandey - pandeyanand2002@gmail.com
Department of Medical Gastroenterology, Osmania Medical College, Osmania General Hospital, Afzalgunj, Hyderabad 500 012, India
Accurate prediction of mortality is important in decompensated cirrhosis. At present, CTP score and MELD-Na score are mainly used to predict the mortality in patients with decompensated cirrhosis of liver, but they have certain limitations. The ALBI score is simple and is easily calculated using only two laboratory parameters. However, it has not been evaluated in decompensated cirrhosis in terms of mortality.
Aim To evaluate the ability of ALBI score for assessing the 180 days mortality in decompensated cirrhotic patients.
Method One hundred patients with decompensated cirrhosis who presenting to the Department of Medical Gastroenterology (November 2019 to March 2021) were studied prospectively. After detailed clinical evaluation and laboratory investigations, CTP score, MELD-Na score, ALBI score and ALBI grade were calculated. We evaluated the 180 days outcome and its association with ALBI score, CTP score and MELD-Na score.
Results Out of the 100 patients, 59 patients had survived for 180 days (Group-A), 21 patients had expired within 90 days (Group-B1) while 20 patients had expired between 91-180 days (Group-B2). Male predominance was seen (88% vs. 22%) and mean age was 46.39 years. Ethanol was the most common etiology of cirrhosis (79% cases). We found that mortality both at 90 days and 180 days were high in patients with higher CTP score, MELD-Na score, ALBI score and ALBI grade (p <0.05). The value of AUC was high in ALBI score (.846) as compared to CTP score (.733) and MELD-Na score (.666). At a cut off -1.04, ALBI score was 68.3% sensitive and 89.8% specific. After logistic regression analysis, we found that one unit increase in ALBI was associated with 10 times increase in mortality.
Conclusion We found that ALBI score and ALBI grade predict mortality at 90 days and 180 days with high sensitivity and specificity in patients with decompensated cirrhosis.
Keywords Cirrhosis, ALBI, Mortality
205
Challenges in liver transplantation for a special situation – Thalassemia major
Ronak Tate
Correspondence – Ronak Tate – roontate@gmail.com
Department of Gastroenterology, E/204, Sukh Angan Building, Opp. S.T Depot, Nalasopara West, Palghar 401 203, India
Thalassemia syndromes are associated with iron overload leading to liver cirrhosis, cardiomyopathy, heart failure, diabetes, and other endocrine abnormalities. With improved transfusion techniques and patients living longer, there is an increasing prevalence of decompensated chronic liver disease and hepatocellular carcinoma secondary to hepatitis C infection and iron overload. However, there is only one case report in literature of a combined liver and cardiac transplant in patient with thalassemia and iron overload. We present the case of a 38 years old male with thalassemia major needing weekly blood transfusions soon after birth. He had undergone a splenectomy in the past and was on iron chelation therapy. During pre-op workup was found to have hepatitis C infection was treated with Sofosbuvir based therapy and sustained virological response (SVR) was achieved. He also had severe osteoporosis and hypogonadism. Despite achieving SVR, his liver decompensated in the last few years in the form of ascites, SBP and encephalopathy. This was attributed to excess iron overload in the liver demonstrated on T2* MRI. He underwent a deceased donor liver transplant for the same. The challenges included a difficult recipient hepatectomy because of the previous splenectomy. He needed multiple PRBC which had to be leuko-depleted to reduce alloimmunisation. Postoperatively, he had tacrolimus toxicity causing hypertension and seizures. The latter resulted in a pathological radius fracture. The osteoporosis was aggravated by steroids received post-transplant. He eventually recovered well and was discharged and is doing well 5 months post-transplant. He needed lesser PRBC transfusions(twice monthly) which are leuko-depleted and iron chelation to maintain serum ferritin <1000 mg/dL.
With regular monitoring of the iron overload status in addition to the routine post-transplant issues, it is possible to improve survival and quality of life in patients with thalassemia major with decompensated liver disease.
Keywords Thalasemia major, Liver transplant, Hepatitis C
206
An autosomal recessive cholestatic disease affecting all three children of a family
Vijaylaxmi Biradar, B Ramesh Kumar, L Sahitya
Correspondence – Vijaylaxmi Biradar – dr.viju21@yahoo.in
Department of Gastroenterology, Osmania General Hospital, Afzalgunj Road, Afzal Gunj, Hyderabad 500 001, India
Progressive familial intrahepatic cholestasis (PFIC) type 3 is an autosomal recessive (AR) disorder arising from mutations in the ATP-binding cassette subfamily B member 4 (ABCB4) gene encoding multidrug resistance protein-3 (MDR3) that acts as a hepatocanalicular floppase. It usually presents in infancy or childhood and often progress to end-stage liver disease before adulthood.
Case Report A 9-year-old boy born out of non-consanguineous marriage with gradually progressive jaundice since 3 months, pruritis since 15 days. The patient has significant family history with his elder two siblings who died at the age of 13 years and 10 years due to decompensated liver cirrhosis. Examination revealed hepatosplenomegaly with scratch marks over the body.
Investigations His work up showed Hb of 10.6 gm/dL, platelet of 1.47 lakh and total bilirubin:2.98, Direct fraction: 1.39, AST:536, ALT:229, ALP:314, albumin: 2.65, PT with INR:29 and 3 sec, GGT of 147. Evaluation done was negative for Wilson’s profile, autoimmune hepatitis profile, Alpha 1 antitrypsin levels were normal and upper GI endoscopy revealed no varices. Ultrasound abdomen shows liver of 12 cm, increased echotexture, spleen of 12 cm, with perisplenic, splenorenal, abdominal wall collaterals s/o portal hypertension. Liver biopsy showed distorted architexture by variably sized hepatic nodules, infiltrates of lymphocytes, neutrophils, prominent bile ductular proliferation, focal canalicular cholestasis with extensive bridging fibrosis favoring PFIC. Next generation sequencing reveals homozygous nonsense variation in exon 26 of ABCB4 mutation with autosomal recessive inheritance. The patient was listed for liver transplantation after which he started decompensating with ascites and raising bilirubin, nasobiliary drainage done, improved his jaundice and pruritis but patient developed AKI, hepatic encephalopathy leading to death inspite of efforts to manage the complications.
Conclusion PFIC 3, a AR disease, is an uncommon cholestatic disorder of childhood. Affecting all the children of a family being a rare entity, nasobiliary drainage can provide symptom control and can be an option for relief of pruritis and jaundice while awaiting liver transplantation.
Keywords PFIC, ABCB4, MDR 3
207
Overlap syndrome of autoimmune hepatitis, primary biliary cholangitis leading to decompensated cirrhosis in a patient of systemic lupus erythematosus: A case report of complex concomitant autoimmune disease
Dipankar Das
Correspondence – Dipankar Das – dipankar.das304@gmail.com
Department of Gastroenterology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221 005, India
Introduction Overlap syndrome is a spectrum of clinical manifestations of autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC). it’s unusual to occur overlap syndrome (AIH and PBC) in a patient with systemic lupus erythematosus (SLE).
Case Report A 30-year-old female patient with presented with multiple joints pain, abdominal distension evaluated and found to have cirrhosis (decompensated with ascites) pancytopenia, coagulopathy, esophageal varices, hypoalbuminemia, pleural effusion. Biochemical profile revealed elevated ALT, AST (> 2 X ULN), ALP (3 x ULN), bilirubin ( 3 x ULN). Viral hepatitis serology, iron studies, celiac panel, Wilson disease work up were insignificant. antinuclear antibody (ANA) titre increased > 1.80, anti-smooth muscle antibody (ASMA) negative, anti-LKM 1 negative, serum IgG level increased (2104 mg/dL), anti-mitochondrial antibody (AMA -M2), DsDNA level was elevated. Transjuglar liver biopsy could not be done due to non-consent. The patient met Paris criteria. 1. The patient was given treatment with oral prednisolone, mycophenolate mofetil, ursodeoxycholic acid and responded well.
Discussion The estimated overall frequency of an overlap syndrome in patients with classical AIH is 14% to 18%. 2 Currently it is uncertain whether con concomitant SLE, AIH -PBC occurs by chance, or they share some common immunological and/or genetic basis.
Conclusions It is advisable to work up for overlap syndrome in lupus hepatitis patients for co-existing AIH/PBC.
References
1. Manns ML. AASLD Practice Guidelines: Diagnosis and Management of Autoimmune Hepatitis. Hepatology 2010; 51: 1-31.
1. Heurgué A, Vitry F, Diebold MD, Yaziji N, Bernard-Chabert B, et al. Overlap syndrome of primary biliary cirrhosis and autoimmune hepatitis: A retrospective study of 115 cases of autoimmune liver disease. Gastroenterol Clin Biol. 2007; 31: 17-25.
Keywords Overlap syndrome, AIH, PBC, SLE
208
Efficacy and safety of sofosbuvir with NS5A inhibitors in hepatitis C virus infection in end stage renal disease patients on hemodialysis
Tejaswini Tumma , Ramesh Kumar Bhashyakarla, Umadevi Malladi, Ramanna Macherla, L Sahitya, V Gopalakrishna
Correspondence – Tejaswini Tumma – tejaswinitumma@gmail.com
Department of Medical Gastroenterology, Osmania Medical College, 5-1-876, Turrebaz Khan Road, Troop Bazaar, Koti, Hyderabad 500 095, India
Introduction Hepatitis C virus (HCV) infection is the most common hepatotoxic viral infection that affects patients on maintenance hemodialysis (MHD). Recommended regimens in ESRD patients are not available in India. Pangenotypic regimens containing sofosbuvir is the main stay of treatment. There is concern over safety of usage of full dose sofosbuvir in these patients as it is eliminated by kidneys. So, the aim of this study was to evaluate efficacy and safety of full dose daily sofosbuvir based DAA regimen in MHD patients with HCV infection in comparison to non-uremic patients.
Methodology One hundred and six patients (50 non uremic and 56 MHD ) chronic hepatitis C patients were included in the study. Before starting treatment HCV genotype, viral load, ultrasound abdomen and fibroscan were done. We started sofosbuvir(400mg)+velpatasvir(100mg) in patients with significant fibrosis and sofosbuvir (400 mg) + daclatasvir (60 mg) in patients without fibrosis, once daily for 12 weeks. Quantitative HCV RNA was done at 12 weeks after treatment.
Results Among 56 patients on MHD 6 patients were excluded from study. Most common genotype was GT1A seen in 80% of MHD group and 88% in non-uremic group (p>0.05) followed by GT 3B in 20% of MHD patients and 12% of non-uremic group (p>0.05). Significant fibrosis was seen in 5 patients (10%) in MHD group and 15 patients (30%) in non-uremic group. SVR12 was achieved in 96% of MHD group and 98% in non-uremic group (p>0.05). Ten (20%) patients from MHD group and 8 (16%) patients in non-uremic group had minor adverse events. Nausea and headache were common adverse events observed. None of them had serious adverse events requiring stopping of treatment.
Conclusions Full dose sofosbuvir containing regimens given daily showed similar efficacy, safety and tolerability in patients on MHD and non-uremic patients. Daily full dose sofosbuvir containing regimens can be recommended to patients with ESRD on MHD.
Keywords Sofosbuvir, Hepatitis C virus, End stage renal disease, Maintenance hemodialysis
209
Efficacy and safety of saroglitazar in compensated cirrhotic non-alcoholic fatty liver disease/non-alcoholic steatohepatitis patients – A 52-week, single center, prospective study
Sujit Chaudhuri, Agnibha Dutta, Sunilbaran Daschakraborty
Correspondence – Sujit Chaudhuri – sourjya_c@yahoo.com
Department of Gastroenterology, Advanced Medicare and Research Institute, Salt Lake, JC – 16 and 17 Salt Lake, Sector III, Bidhannagar, Kolkata 700 098, India
Introduction The potential role of saroglitazar in non-alcoholic fatty liver disease (NAFLD)/ non-alcoholic steatohepatitis (NASH) population is well established but the effect of saroglitazar on compensated cirrhosis is not well documented. In this study we tried to evaluate the efficacy and safety of saroglitazar 4 mg once daily in patients with compensated cirrhosis in routine clinical practice, by evaluating the biochemical parameters, and liver stiffness before and after 52 weeks of saroglitazar therapy.
Methods A total 37 compensated cirrhotic fatty liver patients (males 65%, mean age 57.43 + 8.7 years) diagnosed either based on clinical, ultrasound features and/or endoscopic evaluation (n=19) or on fibroscan LSM > 14 Kpa (n=18) with mean baseline LSM 26.3 + 9.9 kPa, were prescribed saroglitazar 4 mg once daily. None of the patients had a prior or present decompensation in the form of ascites, variceal bleed or hepatic encephalopathy. The improvements were assessed based on LSM parameters as primary endpoint and liver related biochemical parameters, and lipid profiles as secondary endpoints at 24 and 52 weeks. The data was analyzed and statistical significance was assessed using paired t- test.
Results There was statistically significant improvement of LSM values after 24 weeks (18.4 + 8.9 kPa) and 52 weeks (22.3 + 11.1 kPa) of therapy as compared with baseline (26.3 + 9.9 kPa). Similar trend was seen in CAP values with 20% reduction at 52 weeks from baseline. There was significant improvement in liver enzymes as well as in lipid profile. There was no history of treatment discontinuation due to drug related toxicity.
Conclusions Saroglitazar therapy is found as a safe and effective treatment option for compensated cirrhosis associated with NAFLD/NASH. Further well controlled clinical trials are needed to assess the potential role of saroglitazar in compensated cirrhosis patients.
Keywords NAFLD, Compensated cirrhosis, Saroglitazar
210
Real world prospective analysis of saroglitazar versus vitamin E in non-alcoholic steatohepatitis patients
Santosh Hajare , Sandesha Ghorpade
Correspondence – Santosh Hajare – drsantoshhajare@gmail.com
Department of Gastroenterology, KLES Dr Prabhakar Kore Hospital and MRC, Nehru Nagar, Belgaum 590 010, India
Introduction Non-alcoholic fatty liver disease (NAFLD)/non-alcoholic steatohepatitis (NASH) is an emerging public health issue, being a major cause of liver-related morbidity and mortality worldwide. It refers to a wide spectrum of liver disease ranging from steatosis, steatohepatitis, fibrosis, cirrhosis with liver failure and hepatocellular carcinoma. This study was done to compare the real-world efficacy of saroglitazar 4 mg vs. vitamin E 400 IU in reducing AST, ALT, serum triglycerides and liver stiffness measure on Fibroscan in NASH patients.
Methods This is a prospective study in which 50 patients each on saroglitazar 4 mg OD and Vitamin E 400 IU BD with USG evidence of fatty liver with abnormal LFT and or abnormal LSM were enrolled for a period of 1 year. All Patients were followed up for LFT, serum triglycerides and LSM, at an interval of 6 months and 1 year. Statistical analysis was done using paired sample t- test.
Results Significant improvement was observed in LFT, Serum lipids and LSM in the group treated with saroglitazar compared to Vitamin E.
Table 1 Saroglitazar changes in parameters, n=50
| Parameters | Baseline | 6 months | 1 year | % Reduction 1 year | p value |
| ALT (IU/L) | 54.76±26.31 | 34.94±16.99 | 32.27±12.84 | -41.08% | <0.001 |
| AST (IU/L) | 46.72±22.47 | 32.76±14.89 | 29.20±10.82 | -37.50% | <0.001 |
| TG (mg/dL) | 194.54±57.24 | 133.40±56.23 | 133.06±37.59 | -31.60% | <0.001 |
| LSM (kPa) | 12.24±10.17 | 9.58±4.62 | -21.70% | <0.05 |
Table 2 Vitamin E changes in parameters, n=50
| Parameters | Baseline | 6 months | 1year | % Reduction 1 year | p Value |
| AST (IU/L) | 32.88±14.77 | 26.36±10.67 | 25.18±8.35 | -23.42% | <0.001 |
| ALT (IU/L) | 42.64±17.10 | 36.18±14.06 | 32.92±11.35 | -22.80% | <0.001 |
| LSM (kPa) | 10.29±6.78 | 9.77±6.54 | -5.05% | <0.001 | |
| TG (mg/dL) | 178.50±67.10 | 170.92±55.05 | -4.25% | <0.05 |
Conclusions Saroglitazar 4 mg OD significantly improved LSM, serum triglycerides, AST and ALT compared to Vitamin E.
Keywords Saroglitazar, Vitamin E, NASH
211
Diagnostic accuracy of shear wave elastography in predicting esophageal varices in patients with compensated cirrhosis
Majid Khawaja , Madhu Sasidharan, Harish Kareem, K S Manoj, Amit Daphle, Ajit K Nair
Correspondence – Majid Khawaja – majidkhawaja8@gmail.com
Department of Gastroenterology, Kerala Institute of Medical Sciences, 1, Anayara Road, Anayara, Thiruvananthapuram 695 029, India
Background 2D shear wave elastography is an ultrasound based radiological technique which can be used to assess liver stiffness as a result of liver fibrosis The aim of this study was to evaluate the diagnostic accuracy of 2D shear wave elastography for predicting the presence and grade of esophageal varices in patients with compensated liver cirrhosis at risk for developing clinically significant portal hypertension.
Methods This diagnostic study included 78 patients with compensated chronic liver disease, who underwent 2D Shear wave elastography of liver using LOGIQ E9 2D system with transducer 1-6-D and esophago gastrodudenoscpy at Kerala Institute of Medical Sciences (KIMS-Health) Trivandrum from December 2019 to August 2021. Shear wave elastography of liver and endoscopy were performed within an interval of 3 weeks under all standard practices.
Results Of the 78 patients, 54 were males and 24 were females with a mean age of 55.50 ± 9.21 years. Esophageal varices were found in 53 patients out of which 26 had high risk varices. AUROC value of shear wave elastography (SWE) of (0.97) was higher than other non-invasive parameters like platelet count, APRI (AUROC 0.74) and FIB-4 (AUROC 0.78). At a cut off value of 10.45 kpa SWE had 96.1 % sensitivity, 92.7% specificity, 94.7% PPV and 100% NPV for the presence of varices. There was significant co-relation between SWE values and high risk esophageal varices. In this study SWE Values below 10.5 pka could rule out esophageal varices with 100% sensitivity with OGD as Gold standard whereas SWE value above 14.5 pka was significantly associated with high risk esophageal varices/varices needing treatment.
Conclusion Liver stiffness measurement by 2D shear wave elastography in patients with compensated cirrhosis is an effective non-invasive method for predicting the presence of varices of esophageal varices and varices needing treatment.
Keywords 2D shear wave elastography, Liver stiffness, Esophageal varices
212
Variations in liver function tests in obstructive jaundice due to malignant biliary tract involvement and common bile duct stones
Arun Solanki , K Premkumar, Caroline Selvi, K Muthukumaran, A Chezhian, Shubha Immaneni, A Aravind, R Murali
Correspondence – Arun Solanki – aurosolanki@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Chennai 600 003, India
Background Obstructive jaundice is believed only to be characterized by abnormalities of alkaline phosphatase (ALP), rather than aspartate transaminase (AST).
Aim To compare liver function tests (LFTs) pattern in obstructive jaundice in patients with malignant biliary obstruction with those of choledocholithiasis.
Methods LFTs were measured one day prior to undergoing endoscopic retrograde cholangiopancreatography (ERCP) in 102 patients presented with obstructive jaundice during the period from January 2021 to September 2021. For all patients, the highest bilirubin at any point preceding ERCP was documented. Patients were broadly divided into 2 groups based on etiology as Group A (39 patients) having patients with malignant biliary tract involvement and Group B (63 patients) with choledocholithiasis. Diagnosis of the etiology were confirmed with prior magnetic resonance cholangiopancreatography and other relevant investigation for each patient.
Results Group A had higher median bilirubin, ALP and AST levels compared to group B. In group A, median rise in ALP (4.6 x upper normal limit) compared vs. (2.2 x upper normal limit). At peak hyperbilirubinemia, median AST elevation (4.4 x upper normal limit, 168 IU/L) exceeded that for ALP (2.3 x upper normal limit, 299 U/L) in group B.
Discussion The conventional knowledge that ALP rises more than AST in obstructive jaundice remains true where the jaundice is due to malignant biliary obstruction, but in obstructive stone disease, the rise in AST may equal that in ALP, or even exceed it during period of maximum jaundice.
Conclusion Clinicians should consider the possibility of extrahepatic biliary obstruction, even when AST is the predominantly elevated enzyme.
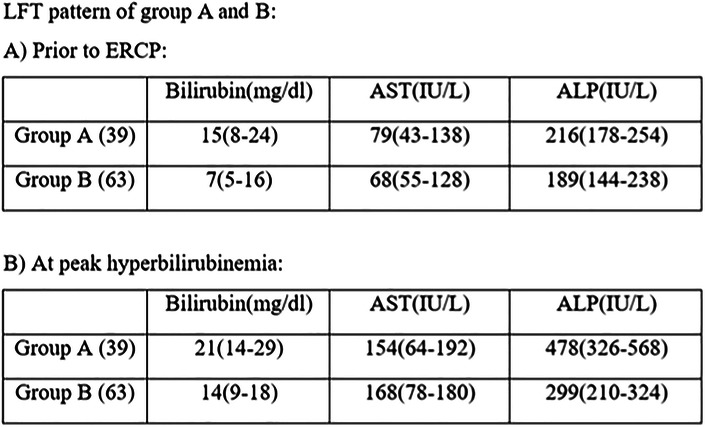
Keywords Jaundice, Malignant, Choledocholithiasis, ERCP
213
Decreased muscle-to-fat ratio is an independent predictor of advanced fibrosis in patients with non-alcoholic steatohepatitis
Puja Bhatia Kapoor1, Harshita Tripathi1, Jaya Benjamin1, Rakhi Maiwall2, Manoj Kumar Sharma2, Archana Rastogi3, Shalini Thappar4, Guresh Kumar5, Yogendra Kumar Joshi1, Shiv Kumar Sarin2
Correspondence – Jaya Benjamin – jayabenjaminilbs@gmail.com
Departments of 1Clinical Nutrition, 2Hepatology, 3Pathology, 4Radiology, 5Clinical Research, Institute of Liver and Biliary Sciences, D1, Vasant Kunj, New Delhi 110 070, India
Introduction Obesity is a known risk factor for disease progression in patients with non-alcoholic steatohepatitis (NASH); however, the body composition (BC) parameters affecting progression of NASH is not known.
Aim To study the BC parameters associated with advanced fibrosis (AF) in NASH.
Methods Biochemical, clinical and BC parameters of 75 patients with NASH were studied. BC was characterized by muscle-to-fat ratio (MFR) of skeletal muscle area (SMA [cm]2) and subcutaneous adipose tissue (SAT [cm]2) from a single slice CT image at L3 vertebra. Physical activity (PA) expressed in MET-minutes/week was assessed using International Physical Activity Questionnaire (IPAQ-short). AF was defined on the basis of liver stiffness measurement (LSM, ≥ 8 kPa) or liver biopsy.
Results NASH patients (M-66.6%; age 42±10.8 years; BMI 28.7±5 kg/m2; lean [16, 21.4%]; obese [59; 78.6%]) were classified as with (31; 41.3%) and without (44; 58.6%) AF. Patients with AF compared to no AF had comparable age: (42.7±10.9 vs. 39.9±10.5; p=0.28); gender (males): (67% vs. 65.9%; p= 0.55); and bilirubin: 1.1±0.08 vs. 0.89±0.55; p=0.33), however CAP (318±37 vs. 300±38; p=0.04); AST (68.4±40 vs. 47.1±31 IU/mL; p=0.015) and ALT (98.6 ±67 vs. 67.8±45.4 IU/mL; p=0.02) were higher in AF. Muscle mass (SMA: 152.7±29.6 vs. 140.2±24.2; p=0.18) was comparable; however subcutaneous adipose tissue (SAT: 237.5±91.2 vs. 168.4±43.3; p=0.008), and muscle to fat ratio (MFR: 0.70±0.17 vs. 0.84±0.46; p=0.02) were significantly higher in AF, and AF performed lower physical activity (MET min/week: 462 [0-6930] vs. 1080 [0-8316]; p=0.031). In logistic regression analysis, MFR (OR [95% CI]: 0.005 [0.00-0.496], p=0.02) was the independent factor associated with advanced fibrosis. MFR <0.75 (AUC-70.6; sensitivity 54.7 and specificity 58.8) is associated with more severe NASH.
Conclusion Patients with advanced fibrosis have high transaminases, low MFR and low physical activity. With every unit increase in MFR, the risk of advanced fibrosis decreases by 99.5%.
Keywords Obesity, Fibrosis, Muscle mass
214
Restricted protein intake in acute liver failure neither reduces ammonia levels nor improves cerebral edema but may increase risk of infection
Harshita Tripathi 1 , Jaya Benjamin 1 , Puja Bhatia Kapoor 1 , Rakhi Maiwall 2 , Vandana Saluja 3 , Prashant Agarwal 3 , Guresh Kumar 4 , Yogendra Kumar Joshi 5 , Shiv Kumar Sarin 2
Correspondence – Jaya Benjamin- jayabenjaminilbs@gmail.com
Departments of 1Clinical Nutrition, 2Hepatology, 3Anesthesia and Critical Care, 4Clinical Research, 5Clinical Nutrition and Hepatology, Institute of Liver and Biliary Sciences, D-1 Vasant Kunj, New Delhi 110 070, India
Background Improvement in cerebral edema (CE) and hepatic encephalopathy (HE) are vital in acute liver failure (ALF). Ammonia (NH3) originating from dietary proteins may promote CE; hence low dietary protein with slow increments is recommended.
Aim To study the association of protein intake on CE as measured by optic nerve sheath diameter (ONSD), NH3 and clinical outcomes in patients with ALF.
Methods Consecutive patients with ALF admitted to ICU were enrolled prospectively. Grade of HE, need for CRRT, new onset of infections (NOI), ONSD, NH3, calorie and protein intake were recorded daily. Enteral nutrition was initiated within two hours of admission, with the aim of providing 35-40 kcal and protein ranging from 0-2g per kg ideal body weight depending upon the clinical status and requirement for CRRT. Average protein intake of 7 days was categorized as low protein (LP: 0-1gm/d) or high protein (HP: 1.1-2 g/d). Resolution of HE and incidence of NOI was compared between LP and HP groups. Impact of daily protein intake on ONSD and NH3 was assessed using generalized linear model (GLM) also.
Results In 40 patients with ALF (M-52%, age 32 ± 14.7 years; etiology- viral-30 [75%]: DILLI-4 [10%]: others-6 [15%]; hyper acute- 38 [95%]: subacute- 2 [5%]; ONSD- 4.6 [2.7-5.7]; NH3 -257 μg/dL [89-839]), GLM assessment suggested no interaction of HP or LP with ONSD (beta=1.095; p=0.238) and NH3 (beta=198.11; p=0.391). With 24 (60%) patients receiving LP and 16 (40%) HP, resolution of HE (LP 6 [%] vs. HP 9 [%]; p=0.738) was comparable, though a trend to higher incidence of NOI was seen in LP group (LP vs. HP= 10 [25%] vs. 3 [7.5%]; p=0.45).
Conclusion Protein restriction in ALF is not helpful in preventing cerebral edema or lowering ammonia levels, moreover low protein intake may predispose to an increased risk of infection.
Keywords Protein, Encephalopathy, ONSD
215
Prognostic role of serum ammonia in cirrhotic patients
Karan Jain, M G Srinivas, K Sridhar Reddy, N Janaki Ram, Pravish Ghurde
Correspondence – Karan Jain – karanjain503@gmail.com
Department of Medical Gastroenterology, Narayana Medical College and Hospital, Chinthareddipalem, Nellore 524 002, India
Ammonia is central to the pathogenesis of hepatic encephalopathy (HE), but its prognostic role in cirrhotic patients with acute decompensation (AD) and ACLF is unknown. Ammonia homeostasis is a multi-organ process. The aims of this study were to determine the relationship between ammonia levels and severity of HE, association with organ dysfunction and short-term mortality.
Methodology We identified 50 patients at Department of Medical Gastroenterology, Narayana Medical College and Hospital as part of prospective observational studies in decompensated cirrhotic patients of any cause. Plasma ammonia levels were measured on admission and Chronic Liver Failure-Sequential Organ Failure Assessment criteria was used to determine the presence of organ failures. 28-day patient survival was determined.
Results The 28-day mortality in our study was 42%. Patients with Grade 3 HE had significantly increased mortality at 28-days (75%) compared to 33.3% and 41.7% mortality in patients with Grade 0/1 HE and Grade 2 HE respectively (p<0.05). An ammonia ≥79.5 μmol/L was significantly associated with higher frequency of organ failures (liver 54.2% vs. 38.4%, kidney 25% vs. 15.4%, brain 20.8% vs. 7.7%, coagulation 29.2% vs. 15.4% and respiratory 37.5% vs. 19.2%). A significantly larger proportion of patients with ammonia ≥79.5 μmol/L had ACLF (75% vs. 42.3%). The 28-day mortality was also significantly higher in patients with ammonia ≥79.5 μmol/L (62.5% vs. 23.1%; p<0.05). No change and increase in ammonia were associated with a 28-day mortality of 50% compared to 25% mortality in patients with decrease in ammonia. Ammonia levels correlate not only with the severity of HE but also the failure of other organs and is an independent risk factor for mortality. Lack of improvement in ammonia levels is associated with high risk of death making it an important biomarker and a therapeutic target.
Keywords Ammonia, ACLF, Hepatic encephalopathy
216
Creatinine dynamics in cirrhotic patients
Pravish Ghurde , M G Srinivas, Sridhar Reddy K, N Janakiram, Karan Jain
Correspondence – Pravish Ghurde – pravishghurde@outlook.com
Department of Medical Gastroenterology, Narayana Medical College and Hospital, Chinthareddipalem, Nellore 524 002, India
Background Renal failure is a complication in patients with liver cirrhosis. It is associated with increased mortality and morbidity. Diagnosis is a challenge because it is mainly based on serum creatinine, which does not seem to be an ideal measure of renal function in cirrhosis. This study aims to determine the relationship between change in creatinine during the disease course and mortality.
Method It is a prospective observational study conducted at an Institution. Patients were included in the study: 1) age ≥18 years and < 75 years. 2). Patients with DCLD of any cause. Patients were monitored for 3 months, and creatinine levels were done on days 1, 5, 30, and 90. Patients were treated as per the presence of hepatorenal syndrome and simultaneously any upper gastrointestinal bleed, ascites, subacute bacterial peritonitis, and hepatic encephalopathy. Prognostic scores (Child-Pugh, model for end-stage liver disease, CLIF-SOFA, and CLIF-C ACLF) were subsequently calculated using parameters obtained at baseline. Follow-up was done for 30 and 90-days from inclusion.
Results A total of 50 patients were included in the study. Of the 50 patients, all had liver failure, 13 patients developed renal failure, 43 patients had coagulopathy, sixteen patients developed circulatory failure and none of them developed respiratory failure. Mortality at day 30 was not found to be significant (p-value = 0.922) and mortality at 90 days of follow-up was significant (p-value = 0.374). CLIF-SOFA score enables accurate prediction of short-term mortality, while Charleston Comorbidity Index was found to be better in predicting mortality in long-term cases, thereby predicting survival of other cases.
Keywords Creatinine, Hepatorenal syndrome, Renal failure, Cirrhosis
217
Does etiology matter in prognosticating patients presenting with acute decompensation with underlying cirrhosis
Gaurav Padia, Roshan George, Sanjeev Sachdeva, Ashok Dalal, Ujjwal Sonika, Siddharth Srivastava, Barjesh Chander Sharma, Ajay Kumar
Correspondence – Ajay Kumar – ajaykumar.aiims@gmail.com
Department of Gastroenterology, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, 1-J L N Marg, New Delhi 110 002, India
Introduction Inflammatory response can result in acute decompensation (AD) in patients with underlying cirrhosis and the development of acute-on-chronic liver failure (ACLF) is associated with increased mortality. The role of etiology of cirrhosis in predicting outcomes in AD patients needs to be explored.
Methods Consecutive AD patients seen from January 2018 to June 2019 were included. Patients with previous decompensation, hepatocellular carcinoma (HCC), extrahepatic malignancy, pregnancy, expected survival less than 5 days, co-morbidities – chronic kidney disease, congestive heart failure, human immunodeficiency virus (HIV) and age >65 years and <18 years were excluded. Patients were followed for 90 days or until development of renal dysfunction (RD), ACLF or mortality. The patients were divided on the basis of etiology into two groups and outcomes were compared.
Results One hundred and twenty-four patients were screened; 88 patients were included. Thirty-eight (43.2%) patients had alcohol as etiology of liver disease, and 50 (56.8%) patients had non-alcohol etiology. On follow-up, 24 (27.27%) patients developed RD, 22 (25%) developed ACLF and 21 (24%) died. Baseline total leukocyte count, Interleukin-6 (IL-6), Child-Pugh score, model for end-stage liver disease (MELD) score were significantly higher in the alcohol etiology group. On 90 days follow-up, patients in the alcohol group more frequently developed RD (31.6% vs. 24%, p=0.43) and ACLF (39.4 % vs. 14 %, p=0.007), and the alcohol group had higher grades of ACLF compared to the non-alcohol group (Grade II/III- 18.4% vs. 4%, 0.007). CLIF-OF was higher in the alcohol group (7.81±2.36 vs. 6.4±1.55, p=0.003). Mortality was higher in the alcohol etiology group (31.6% vs. 18%, p=0.143).
Conclusion Alcohol etiology of chronic liver disease and AD is associated with higher risk of ACLF and mortality.
Keywords Acute decompensation, Renal dysfunction, Etiology, Alcohol
218
Study on the prevalence of hepatic fibrosis in patients on methotrexate therapy in a tertiary care center
Raghavendra Navi, M S Revathy, S Chitra
Correspondence – Raghavendra Navi – ragun90@gmail.com
Department of Medical Gastroenterology, Stanley Medical College, Old Jail Road, Chennai 600 001, India
Introduction Methotrexate (MTX) as a DMARD, is mainstay in the treatment of variety of autoimmune diseases including psoriasis and rheumatoid arthritis (RA). Although MTX has good efficacy and safety, hepatotoxicity has been well described. Fibroscan has found to be reliable, non-invasive method for the detection of hepatic fibrosis without any side effects. The present study is conducted to assess the degree and prevalence of hepatic fibrosis in patients on MTX therapy by Fibroscan.
Methods A observational study was carried out in Department of Medical Gastroenterology. Study duration 6 months from April 2021. Study included patients aged ≥ 18 years, who had been on MTX. Patients with cumulative dose > 1.5 g were subjected to Fibroscan to assess the degree of hepatic fibrosis and the cut off value of 7.1 kPa (kilopascal) was considered abnormal (liver fibrosis). Statistical methods Data was analyzed using SPSS version 21. Spearman’s rank test was used to assess the correlation between the cumulative dose of MTX and Fibroscan score and independent ’t’ test was used for continuous variables.
Results Total of 42 patients on methotrexate were included in the study, out of them 18 were males, 24 were females. Mean age of patients was 42 years. The mean CD- 1697 mg. The mean duration was 186 weeks. mean fibroscan value of 5.7kpa. mean dose 9.5 mg/week. Taking 7.1kpa as the upper limit of normal, we found that 4 patients had hepatic fibrosis, 4 of them had F-1 stage fibrosis. Fibroscan scores were significantly correlated with cumulative dose of MTX (r= 0.34, p=0.01) We found prevalence of hepatic fibrosis in 9.5% of patients on methotrexate therapy.
Conclusion The study revealed that long-term MTX therapy is associated with increased risk of liver 183atient183. Fibroscan is a useful tool for monitoring MTX-induced liver fibrosis.
Keywords Hepatic fibrosis, Methotrexate, Fibroscan
219
Study on the clinical and etiological profile of hepatocellular carcinoma in a tertiary care centre in south India
Silambarasan Selvam, M S Revathy, B Sumathi
Correspondence – Silambarasan Selvam – silambarasansjsk@gmail.com
Department of Medical Gastroenterology, Stanley Medical College, No.1, Old Jail Road, George Town, Chennai 600 001, India
Background Hepatocellular carcinoma (HCC) is the most common primary malignant tumor of liver occurring predominantly in patients with underlying chronic liver disease and cirrhosis with various clinical presentations. It is a major cause of cancer-related morbidity and mortality. The present study is conducted to analyse the clinical and etiological profile of HCC patients presenting to our hospital.
Methods This is a prospective cross-sectional study conducted in Department of Medical Gastroenterology, Government Stanley Medical College over a period of one year with sample size of 60 patients. Clinical details, demography, laboratory parameters and imaging findings are entered in pre-structured proforma.
Results Among 33 patients, 30 were males (90.9%) with male to female ratio of 3:1. Mean age of patients was 56.5 years. The predominant symptom among HCC patients was abdominal pain in 22 (78.5%) and abdominal distension in 12 patients (42.8%). Underlying cirrhosis was present in 23 patients (69.6%). The etiologies include Hepatitis B in 11 (33%), alcohol in 9 (27%), hepatitis C in 5 (15%), NAFLD in 3 (9.1%) and cryptogenic in 5 (15%) patients. AFP levels >400 ng/mL were observed in 15 cases (45.5%) with mean value of 6129 ng/mL and was normal in 4 cases. On imaging, multifocal lesions seen in 10 (30.3%) patients and vascular invasion in 15 (45.4%) patients. Most of the patients belong to BCLC stage C (57%), followed by stage B (33.3%) and stage A (9%). Patients were managed according to institutional protocol with either hepatectomy, TACE, systemic chemotherapy or combination of these modalities.
Conclusion Results of the study shows that abdominal pain is the most common presentation followed by abdominal distension. In our study HBV (33%), alcohol (27%) were the most common etiologies.
Keywords Hepatocellular carcinoma, Hepatitis B virus, Alcohol
220
Clinical profile and outcome of acute liver failure in northwest India: A tertiary care centre experience
B R Ajay , Rishabh Gupta, Sandeep Nijhawan, Gaurav Gupta
Correspondence – Rishabh Gupta – ajaybr23@gmail.com
Department of Gastroenterology, Sawai Man Singh Medical College, J L N Marg, Jaipur 302 004, India
Introduction Acute liver failure (ALF) is a rapidly progressive syndrome having high mortality rate with varied etiology. It is characterized by development of coagulopathy (INR >1.5), and encephalopathy within 4 weeks of the onset of symptoms in a patient without pre-existing cirrhosis. Geographical differences are seen in terms of etiology and outcome. Viral hepatitis is the commonest cause in India unlike drugs and toxins in the West. Thus, careful evaluation for the cause of ALF is important for the management and prognosis of the patient.
Aim of the Study To evaluate the etiology, clinical profile and outcome in patients with acute
liver failure.
Method It was a prospective observational study conducted in the Department of gastroenterology, S M S Medical College, Jaipur, India. All patients with the diagnosis of ALF as per IASL criteria were included between September 2018 to July 2020.
Results Total 124 patients were included out of which 66 were males and 58 females. Mean age was 36.68+/-18.44 years. Overall mortality in our study was 65/124 (52.4%), with highest being viral hepatitis 26/124 (20.96%), followed by indeterminate group 18/124 (14.5%). Viral hepatitis 63/124 (50.8%) was the most common cause of ALF, of which HEV being the commonest with 35 patients, followed by drug or toxin induced 30 (20.2%) and indeterminate group 18 (14.5%). Among drug induced acute liver failure, 25 had ATT induced ALF. Out of 58 females, 6 were pregnant. Predictors of outcome were age, etiology, hepatic encephalopathy grade, coagulopathy, deranged renal function, bilirubin, intracranial pressure and other complications.
Conclusion ALF is a disease having mortality of 52.4%. Viral hepatitis is the commonest cause in northwest India, like the rest of India. ATT is also an important cause of ALF. Prompt diagnosis and timely management of complications is required.
Keywords Acute liver failure, Viral Hepatitis, Predictors of outcome
221
Demographic, clinical, laboratory, and management profile in patients of amebic liver abscess from northern India
B R Ajay, Gireesh Dhaked, Rupesh Pokharna, Prachis Ashdhir
Correspondence – Gireesh Dhaked – ajaybr23@gmail.com
Department of Gastroenterology, Sawai Man Singh Medical College, J L N Marg, Jaipur 302 004, India
Background Amebic liver abscess (ALA) is a serious extraintestinal manifestation of amebiasis and major problem in developing countries. Due to rapid urbanization, improved sanitation and hygiene in India led to shift in disease epidemiology towards non-communicable disease, but recent changes in epidemiological and clinical pattern in ALA are not well studied. So, the present study aimed to evaluate recent demographic, clinical, laboratory and management profile in patient with ALA.
Methods It is a prospective observational study conducted in the Department of Gastroenterology, S M S Medical College, Jaipur, Rajasthan from June 2018 to December 2020. A predesigned semi structured questionnaire consisting of sociodemographic factors, risk factors, clinical, laboratory and management profile was used to collect data.
Results A total 508 patients of amoebic liver abscess were analyzed. Median age of presentation was 40 years, majority were male (90.4%) with chronic alcoholics (47.2%) and belong to lower socioeconomic class. Abdominal pain, fever and anorexia were the commonest symptoms. Majority had right lobe involvement (77.6%) and solitary abscess in 67.5%. Most of small liver abscess (68%) were managed by medical treatment alone. Percutaneous needle aspiration was done in 62.6% patients, mostly for abscess size 5-10 cm (93%) with 90% success. A Total 24.6% patients underwent percutaneous catheter drainage, all successfully done. Intraperitoneal rupture was seen in 10% patient. Mortality was 1.5%.
Conclusion There is no difference in sociodemographic, clinical and laboratory profile in the last 2-3 decades. Early initiation of a combined therapeutic approach leads to early symptomatic improvement, fewer complications, and better outcomes.
Keywords Amebic liver abscess, Non-communicable disease, Percutaneous needle aspiration
222
Prevalence and outcomes of acute kidney injury in patients with acute on chronic liver failure: A single centre experience
Chitta Ranjan Khatua
Correspondence – Chitta Ranjan Khatua – chittamedicine@yahoo.co.in
Department of Gastroenterology, Maharaja Krushna Chandra Gajapati Medical College, Medical College Campus, NH59, Brahmapur 760 004. India
Introduction Acute-on-chronic liver failure (ACLF) is a life-threatening condition in patients of chronic liver disease (CLD) and acute kidney injury (AKI) further decreases the survival of patients. There are scant data regarding the impact of AKI on survival in ACLF in this region of Asia. Hence, we performed a prospective study to evaluate the spectrum of ACLF and the impact of AKI in outcomes of these patients.
Methods This study was conducted in consecutive ACLF patients (defined as per EASL-CLIF Consortium criteria), hospitalized in S C B Medical College, India between October 2016 and December 2018. AKI was defined and classified as per AKIN criteria. Demographic, clinical, and laboratory parameters were recorded, and outcomes were compared during hospitalization and also at 28 days and 90 days.
Results Two hundred and thirty-nine (33.8%) out of 708 CLD patients had ACLF, of which 87.4% had AKI. 31% had stage 1, 37.4% had stage 2, and 31.6% had stage 3 AKI. Use of diuretics (53.1%), NSAIDS (5.4%), use of antihypertensive (ARB/ACEI), and hypovolemic conditions like diarrhoea and vomiting (26%) were common precipitants of AKI. Mortality during hospitalization increased with higher grades of AKI (p=0.002). Furthermore, they had decreased survival both at 28 days (p=0.005) and 90 days (p=0.018). ACLF patients with AKI had significantly higher serum creatinine, serum urea, total bilirubin, INR and higher MELD UNOS, MELD Na+, CTP score, and increased duration of hospitalization (p=0.002).
Conclusion In our institution, about one third of CLD patients had ACLF and over three fourth of them had AKI at the time of hospitalization. Use of diuretics and hypovolemic conditions were common precipitants of AKI, patients with AKI had prolonged hospital stay, and decreased survival during hospitalization, and also at 28 days and 90 days.
Keywords Acute kidney injury, Acute on chronic liver failure
223
Diagnosis by clinical criteria correlates poorly with histology in subacute and acute-on-chronic liver failure
P S Sairam1, Shailaja Balakumar2, Thomas Alex2, Uday Zachariah1, K Reka3, C E Eapen1, Ashish Goel1
Correspondence – Sairam P S – ssairam2611@gmail.com
Departments of 1Hepatology,2Pathology, and 3Biostatistics, Christian Medical College, Ida Scudder Road, Vellore 632 004, India
Introduction Liver biopsy may help to differentiate subacute hepatic failure (SAHF) and acute-on-chronic liver failure (ACLF). This study aims to assess the agreement between histological pattern and clinical criteria in SAHF/ACLF.
Methods Patient records with hyperbilirubinemia (S.bilirubin ≥5 mg/dL) and liver failure (ascites/encephalopathy) who underwent liver biopsy from January 2017-June 2021 were extracted. Patients with focal liver lesions, acute liver failure (ALF) and decompensated chronic liver disease (DCLD) were excluded. International Association for the Study of the Liver (IASL) and Asian Pacific Association for the Study of the Liver (APASL) criteria were applied retrospectively to classify patients as SAHF/ACLF. Liver histology was classified, based on pre-determined criteria, into definite sub-acute, definite chronic and indeterminate liver injury.
Results Of 589 patients who underwent liver biopsy, 104 had hyperbilirubinemia and liver failure. After excluding patients with ALF (16), DCLD (22) and focal liver lesions (32), 34 patients were included in this study. Nineteen patients (Males:11; age: 33,13-59 years; median, range; MELD: 24,15-39) had SAHF and 15 patients (Males:7; age: 30,17-46 years; MELD: 26,17-56) had ACLF. Most common acute insult for both SAHF (21%) and ACLF (27%) was idiosyncratic drug reaction. None of SAHF (13) and 2/10 of ACLF patients had large esophageal varices. On biopsy, definite sub-acute injury was noted in 8 (SAHF: 6, ACLF: 2), definite chronic in 24 (SAHF: 11, ACLF: 13) and indeterminate in 2 (SAHF: 2). Clinical criteria and histology had poor agreement (kappa: 0.27). SAHF clinical criteria (sensitivity: 0.8, specificity: 0.5) and ACLF clinical criteria (sensitivity: 0.5, specificity: 0.8) were suboptimal in predicting histological liver injury (overall misclassification rate: 38% [95% CI:29%-56%]).
Conclusion Diagnostic clinical criteria are inaccurate in predicting histological pattern of liver injury in SAHF/ACLF patients.
Keywords Subacute hepatic failure (SAHF), Acute-on-chronic liver failure (ACLF), Misclassification rate
224
Compliance on antiviral treatment for hepatitis B
Parveen Malhotra 1 , Vani Malhotra 2
Correspondence – Parveen Malhotra – drparveenmalhotra@yahoo.com
Departments of 1Gastroenteroloy, and 2Obstetrics and Gynaecology, Post Graduate Institute of Medical Sciences, Rohtak 124 001, India
Introduction Hepatitis B virus (HBV) remains to be an important cause of liver related morbidity and mortality all over the world. India is a moderately endemic country for chronic hepatitis B (CHB) infection. Hepatitis B surface antigen (HbsAg) positivity in Indian population varies from 2 % to 8% in different parts of country with an average of 4%. based on the result of an epidemiological study.
Aims and Objectives To determine the compliance among hepatitis B patients who were treated with Tablet Tenofovir 300 mg.
Methods It was prospective study conducted at Department of Medical Gastroenterology, Post Graduate Institute of Medical Sciences (PGIMS), Rohtak, over a period of ten years and nine months from 01.01.2011 to 30.09.2021. Out of five thousand and six hundred patients of chronic hepatitis B who reported in department in above duration, 1000 patients were started on treatment with tablet tenofovir 300 mg on daily basis. Out of these fifty patients expired, thus were excluded from final analysis. Hence, compliance was determined in the remaining 950 patients.
Results Out of 950 patients, 100 patients (10.53%) stopped treatment on their own leading to compliance rate of 89.47% which is good in view of prolonged course of treatment for hepatitis B.
Keywords Hepatitis B Virus, Tenofovir, Compliance, Cirrhosis, Dyspepsia
225
Usefulness of leukocyte ratios in predicting in-hospital mortality of patients with decompensated chronic liver disease – Experience from a tertiary care referral center
Vasista Palnati , Anirudh Karanam, K Pruthvi, Pukhraj Singh Jeji, Vybhav Venkatesh, Subhasis Pradhan, Debakanta Mishra, Jimmy Narayanan, Girish Kumar Pati, Manoj Kumar Sahu
Correspondence – Vasista Palnati – vasistapalnati10edu@gmail.com
Department of Medical Gastroenterology, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India
Introduction Different leucocyte ratios like neutrophil to lymphocyte ratio (NLR), monocyte to lymphocyte ratio (MLR) and neutrophil to monocyte ratio (NMR) have been used as markers of inflammation in various conditions. In the recent times, these ratios are being explored as markers for predicting mortality in patients with decompensated chronic liver disease (DCLD).
Aim To demonstrate the usefulness of leukocyte ratios as biomarkers for mortality prediction in decompensated CLD.
Methods A retrospective analysis of decompensated CLD patients managed at our center from January 2019 – June 2021 was performed. Besides demographic and etiologic information, leukocyte ratios were calculated from the available admission investigations and comparison was done between those who survived to hospital discharge (survivors) and those who did not (non survivors).
Results A total of 103 patients (mean age 51.2±9.7, 86.4% males) were included in the final analysis. Most common etiology of CLD was alcohol (67.9%), followed by non-alcoholic steato-hepatitis (NASH-13.6%) and chronic hepatitis B (CHB-11.7%). Ninety (87.4%) had some grade of ascites and encephalopathy was seen in 41 patients (39.8%). 29.1% (30) had acute-on-chronic liver failure as per the APASL definition. The in-hospital mortality of the cohort was 39.8% (41) and it was significantly higher in those who had ACLF (60% vs. 31.5%; p=0.007). Median NLR (10.6 vs. 4; p<0.001), NMR (20.6 vs. 11.5; p<0.001) and MELD score (29 vs. 22; p<0.001), but not MLR (0.5 vs. 0.3; p=0.58) were significantly elevated in non-survivors compared to survivors. On logistic regression, MELD score >32 (OR-3.1, 95% CI:1.04-9.1) and NLR>7 (OR-8.5, 95% CI:3.04-23.9) were significantly associated with in-hospital mortality.
Conclusions Leukocyte ratios, being simple and easily available, have a great potential to be used as biomarkers in decompensated CLD patients for mortality predictions. Further large-scale prospective studies are needed to accurately identify the association and their utility in routine practice.
Keywords Neutrophil-Lymphocyte-Ratio (NLR), Monocyte-Lymphocyte-Ratio (MLR), Neutrophil-Monocyte-Ratio (NMR)
226
“Stocking Glove” hepatocellular carcinoma (HCC) – A rare case of anti-Hu antibody positive peripheral neuropathy secondary to HCC
K H Vinod Gowda , Mallikarjun Patil, Harshad Devarbhavi
Correspondence – Vinod Gowda K H – vinodgowdakh@gmail.com
Department of Gastroenterology, St. Johns Medical College Hospital, Sarjapur Main Road, Bengaluru 560 034, India
A 64-year-old gentleman with chronic hepatitis B infection since nine year on 189atient189d came with tingling and burning sensation in both upper and lower limb since 6 months along with motor weakness in the form of slippage of footwear. Physical examination revealed presence of pheripheral neuropathy. Routine lab investigations along with CSF analysis, MRI brain and spine were normal. Nerve conduction studies showed sensory axonal neuropathy. Ultrasound showed mild altered echotexture of liver. Initial workup for peripheral neuropathy including autoimmune workup was negative. On further evaluation HBV DNA, AFP and liver stiffness was 34 IU/mL, 55.48 ng/mL and 8.6 kpa respectively. MRI abdomen showed a 1.8 x 1.8 cm LIRADS 5 lesion in segment 8. In view of HCC and peripheral neuropathy, paraneoplastic panel was done in which anti-Hu antibody was positive. Patient underwent radio frequency ablation and reports improvement in his neurological symptoms.
Keywords Paraneoplastic neurologic syndrome, Peripheral neuropathy, Hepatocellular carcinoma
227
Efficacy of ascitic fluid cholesterol compared to serum-ascites albumin gradient in detection of non-portal hypertension ascites and diagnosing mixed ascites
B R Ajay, Rishabh Gupta, Sandeep Nijhawan, Gaurav Gupta
Correspondence – Rishabh Gupta – ajaybr23@gmail.com
Department of Gastroenterology, Karnataka Gastro Centre, Between Modi and Nagapura Main Road, Mahalakshmi Puram, WCR, 748, 5th Main Road, West of Chord Road, Nagapura, Bengaluru 560 086, India
Introduction Ascites is the pathological accumulation of fluid in the peritoneal cavity. Several biochemical parameters like SAAG, ascitic fluid protein, LDH, glucose, triglyceride and tumour markers have proven to be useful in diagnosing the cause of ascites.
Aim To investigate the diagnostic performance of ascitic cholesterol in differential diagnosis of ascites.
Methods In this prospective cohort study, all patients with new onset ascites admitted to S M S Hospital, Jaipur from September 2018 to January 2021 were assessed. All information including clinical history, physical examination, blood examination, ascitic fluid analysis, imaging modalities, peritoneal biopsy, etc. Ascites samples obtained by paracentesis were collected in tubes and sent for routine biochemical assays and cytological examination. The ascitic fluid cholesterol was determined by the CHOD- PAP method using a cholesterol determination assay.
Results Most common cause of portal hypertension was cirrhosis (81%). Most common cause of non-portal hypertension was tuberculosis (54.8%) malignant ascites (35.48%). Among 60 patients of mixed ascites, 59% had portal hypertension with carcinoma without peritoneal mets. Ninety-one percent patients of malignant ascites had ascitic cholesterol >45 mg/dL, while 75 % had SAAG < 1.1 gm/dL. In tuberculous ascites, 100% patients had ascitic cholesterol > 45, while 90% had SAAG < 1.1 gm/dL. Among portal hypertension, 82% patients had ascitic cholesterol < 45 gm/dL and 89% had SAAG >1.1 gm/dL. Among patients with mixed ascites, 90% patients of PHTN and carcinoma without peritoneal mets. and 89% patients of PHTN and benign NPH without peritoneal involvement had ascitic cholesterol < 45 mg/dL, while 75% of mixed ascites with peritoneal mets and 100% patients of mixed ascites with benign NPH and peritoneal involvement had ascitic fluid cholesterol >45. This suggested that patients with mixed ascites with AF cholesterol > 45 had peritoneal lesions.
Conclusion These results indicated that SAAG is not helpful for identifying peritoneal lesion in mixed ascites.
Keywords Ascitic fluid, Portal hypertension
228
Plasma exchange improves in-hospital survival in acute on chronic liver failure patients with hyper-ferritinemia
Nicholas Rao1, Ashish Goel2, Uday Zachariah2. C E Eapen2, Balakrishnan Vijayalekshmi 3
Correspondence – Nicholas Rao – nickyvrao@gmail.com
Departments of 1Gastroenterology, 2Hepatology, and 3Wellcome Trust Research Laboratory, Division of GI Sciences, Christian Medical College, Vellore 632 004, India
Introduction Hyper-ferritinemia is common in acute-on-chronic liver failure (ACLF) and may be a part of hemophagocytic lymphohistiocytosis (HLH). In this study, we aim to assess impact of plasma exchange on short-term outcome in ACLF patients with hyper-ferritinemia.
Methods We retrospectively recruited in-patients with ACLF (defined as per Asia Pacific Association for Study of Liver, [APASL] criteria) over the past 1 year. HLH and hyper-ferritinemia (serum ferritin > 500 ng/mL) were defined as per HLH-2004 criteria. Clinical and laboratory, including reticuloendothelial activation (serum sCD163-macrophage activation and Von-Willebrand factor, VWF) markers were assessed. Patients were managed by standard medical therapy (SMT) and low-volume plasma exchange (PLEX-LV), was done as per treating clinician decision. We analyzed in-hospital outcome (adverse: death or discharge in terminal state) in these patients.
Results Of the 60 patients with ACLF (M: 48; age: 45, 19-70 years; median, range; most common etiology: ethanol: 38 (63.3%); MELD: 29.5 ,18-51), 49 had hyper-ferritinemia. 40/49 (82%) with hyper-ferritinemia and 5/11 with normal ferritin levels fulfilled HLH criteria. Patients with hyper-ferritinemia had higher serum creatinine (0.72,0.6-1.7 mg/dL vs. 1.3,0.4-5.4 mg/dL; p: 0.05) and plasma VWF (803, 336 – 1467 IU/dL vs. 404, 382-980 IU/dL, p: 0.05) levels. Serum ferritin did not correlate with MELD score and serum CD-163 levels. Overall in-hospital adverse outcome did not correlate with baseline hyper-ferritenemia (20/49 v/s 3/11, p-value: NS). Low volume therapeutic plasma exchange (PLEX-LV) was done in 25 patients (hyper-ferritinemia: 21). In patients with hyper-ferritinemia (adverse outcome- SMT:18/28, PLEX-LV: 2/21; p-value: <0.001), PLEX-LV improved outcome.
Conclusion Plasma exchange (PLEX-LV) improves in-hospital survival in ACLF patients with hyper-ferritinemia, compared to SMT.
Keywords Acute on chronic liver failure, Hyperferritinemia, Low volume plasma exchange
229
Prevalence of autonomic dysfunction in chronic liver disease in a tertiary care centre
Santhosh Rajendran
Correspondence – Santhosh Rajendran – santhosh12@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Chennai 600 101, India
Introduction Autonomic dysfunction in non-alcoholic cirrhosis is less frequently studied.
Aim To assess autonomic nervous system in patients of alcohol and non-alcohol related cirrhosis.
Methods This is a cross sectional study of 80 patients with cirrhosis (40 alcoholics and 40 non alcoholics). Autonomic profile included performance questionnaire and five autonomic function tests based on Ewing’s test .The extent of autonomic dysfunction was determined.
Results Sixty-two of (77.5%) the cirrhotic subjects were found to have evidence of autonomic neuropathy. Of these, 10 (12.5%) patients had early parasympathetic damage, 16 (20%) had definite parasympathetic damage, and 36 (45%) had combined (that is, both parasympathetic and sympathetic) damage. 38(95%) of the alcoholics and 31 (77.5%) of the non-alcoholics had autonomic dysfunction. Autonomic dysfunction was significantly more frequent in advanced liver disease compared with early liver damage. Forty-one (73%) out of 56 cirrhotic subjects belonging to CTP B and 20 (85.7%) of the 24 patients belonging to CTP C had autonomic neuropathy.
Conclusion This study shows that autonomic neuropathy is common in cirrhotic subjects and found with comparable frequency in alcoholics and non-alcoholics. It Increases in severity with increase in extent of liver damage.
Keywords Autonomic dysfunction, Ewing’s test, Cirrhosis
230
Acute leukemia presenting as acute hepatitis
N K Niranjan
Correspondence – Niranjan N K – niruat85@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Hepatitis is a known complication during the treatment phase of leukemia but the association of abnormal liver biochemistries at initial presentation of leukemia is poorly described.
Case Report A 17-year-old female with no known comorbidities presented with a history of intermittent fever for 15 days, mild, no chills or rigors, associated with abdominal pain dull aching in character and epigastric in location, continuous in nature non radiating. History of loose stools, watery in nature, on and off since 15 days not mixed with blood or mucus. H/o loss of weight of around 7 kg in last one month. No h/o jaundice, abdominal distension or pedal edema, bleeding manifestations. Personal history, family history were unremarkable. O/E vitals were stable, multiple subcentimetric b/l cervical lymph nodes were palpable, no pallor, icterus, clubbing or pedal edema. P/A examination was unremarkable except for mild epigastric tenderness, other systemic examination was within normal limits. On routine investigations CBC was normal, LFT showed elevated liver enzymes with AST – 222 and ALT – 324, ALP-84, GGT- 2O6, T.pro -7.3, Alb – 4.2, total and direct bilirubin were 1.2 and 0.4 respectively. RFT, X-ray chest were normal. USG and CT abdomen showed mild splenomegaly. A working diagnosis of acute hepatitis? infective etiology was made but all viral markers including HAV, HEV, HBV, HCV, CMV, EBV turned negative. Finally peripheral smear showed 37% blast cells s/o acute leukemia. A final diagnosis of acute hepatic injury secondary to acute leukemia was made.
Conclusion Acute elevation of transaminases can be a presenting feature of acute leukemias especially in young patients and hence possibility of acute leukemia as a cause of hepatitis can be considered if other aetiologies are ruled out.
Keywords Hepatitis, Leukemia, Transaminases
231
Assessment of nutritional status in cirrhotics using standard nutrition assessment tools and their correlation with severity of disease
V R Lohith Kumar , B Sukanya, N Sunil Kumar
Correspondence – Lohith Kumar V R – drlohithkumar@gmail.com
Department of Medical Gastroenterology, Nizam’s Institute of Medical Sciences, Somajiguda, Hyderabad 500 082, India
Introduction Malnutrition is not only common among cirrhotics but also an important prognostic factor. An ideal assessment tool for malnutrition in cirrhotics is not clear due to confounders like ascites and edema. Sophisticated nutritional assessment tools like Psoas muscle thickness to height (PMTH) and bioelectrical impedance analysis are also controversial.
Objective To assess the nutritional status in cirrhotics by using standard nutritional assessment tools and to correlate with the severity of disease.
Methods This prospective observational cross-sectional study was conducted in Nizam’s Institute of Medical Sciences. Nutritional status was assessed by subjective global assessment (SGA), anthropometry (body mass index, mid-arm muscle circumference [MAMC]), hand grip strength dynamometry (HGS), PMTH and bioelectrical impedance analysis (BIA).The above nutritional methods were assessed and compared with age and sex matched healthy controls.
Results Fifty patients (36-males,14-females) were recruited. Commonest etiology was Ethanol (92 %).18%, 44%, 38% of patients were in CTP-A, CTP-B, and CTP-C respectively. 38% and 62% had MELD<15 and MELD>15 respectively. Decompensated cirrhotics had significantly more malnutrition compared to compensated cirrhotics when assessed by SGA (p<0.00018) and PMTH (<0.0000049) in both males and females. HGS (p<0.00093), MAMC (p<0.001), Skeletal muscle percentage (p<0.00022) were significantly correlated with severity of cirrhosis in males but not in females.
Conclusion PMTH is the best nutritional assessment tool correlated with severity of cirrhosis followed by SGA. HGS, MAMC, BIA (Skeletal muscle percentage) are bedside tools for nutritional assessment in male cirrhotics. We did not find BMI, BIA (VAT, SAT) to be reliable indicators of malnutrition.
Keywords Cirrhosis, Malnutrition, Nutrition assessment
232
Acanthosis Nigricans- A rare cutaneous association in progressive familial intrahepatic cholestasis type 3
Rahul Vijayvargiya , L Sahitya, Gopala Krishna, M Ramanna, M Uma Devi, B Ramesh
Correspondence – Rahul Vijayvargiya – rahul.sanwariya1990@gmail.com
Department of Gastroenterology, Osmania Medical College, Afzal Gunj, Hyderbad 500 012, India
Introduction Progressive familial intrahepatic cholestasis (PFIC) refers to heterogeneous group of autosomal recessive disorders of childhood that disrupt bile formation and present with cholestasis of hepatocellular origin. Defects in ABCB4, encoding the multi-drug resistant 3 protein (MDR3), impair biliary phospholipid secretion resulting in PFIC3. Acanthosis nigricans is a cutaneous manifestation of an underlying condition. It usually develops in in skin folds, such as the back of the neck, axilla, and groin, where it presents as velvety hyper-pigmented patches with poorly defined borders.
Case Report A 12-year-old female who is known case of PFIC type 3 came for follow-up with chief complaints of pruritus and increased pigmentation over neck region and forehead. Dermatology opinion took for that and skin biopsy done which suggestive of acanthosis nigricans.
Discussion Acanthosis nigricans is most commonly associated with diabetes, insulin resistance, internal malignancy, hormone disorders or with the use of certain medications like systemic glucocorticoids and oral contraceptives. The pathophysiological process behind acanthosis nigricans appears to be related to the proliferation of fibroblasts and the enhanced stimulation of epidermal keratinocytes In literature association with PFIC is not mentioned. Here we reporting a case of acanthosis nigricans in PFIC type 3 patients.
Keywords Acanthosis nigricans, PFIC
233
To assess response to steroids in patients with autoimmune hepatitis
Harsh Gandhi , Pravin Rathi, Sanjay Chandnani, Shubham Jain, Rishikesh Malokar, Jay Chudasama
Correspondence – Harsh Gandhi – harshgandhi345@gmail.com
Department of Medical Gastroenterology, T N M C and B Y L Nair Charitable Hospital, Dr. A. L. Nair Road, Mumbai 400 008, India
Introduction Autoimmune hepatitis (AIH) is an acute, or more frequently chronic, inflammatory, immune-mediated liver disease which is defined by a rise in immunoglobulin G (IgG) levels, the presence of non-organ-specific autoantibodies and characteristic histological features such as interface hepatitis and plasma cell infiltration. In Autoimmune hepatitis, response to steroids and optimal timing of liver transplantation always remains controversial. Aim of study is to assess response to steroids at day 3,7,14 after starting steroids and to compare two groups responders and non responders to steroids.
Methods It is interim analysis of observational retrospective and prospective study involving 17 patients of AIH divided into acute AIH, acute severe (AS) AIH and AS-AIH with ALF (acute liver failure) . Response to steroids was assessed in these 3 groups of patients.
Results Out of 17 patients, 4 patients (23.5%) presented as acute AIH, 8 (47.1%) as AS AIH, 5 (29.4%) as AS AIH with ALF. Most common presentation is abdominal distension (52.9%). Out of AS-AIH ALF group, 2 patients died (non-responders to steroid). Rest 15 patients responded to steroids. T-bill, hemoglobin (Hb), CTP and MELD at Day 0 (before starting steroids) were compared between these two groups (responders and non-responders to steroids). T-bill (p = 0.856), Hb (p = 0.219), MELD (p= 0.226) and CTP (p= 0.125). So there was no correlation of T. bili, Hb, MELD, CTP at Day 0 between responders and non-responders to steroids.
Conclusion Study did not confirm the association of initial T. bilirubin, Hb, MELD and CTP values between responders and non-responders to steroids.
Keywords Autoimmune hepatitis, Steroids
234
To study the role of urinary NGAL (neutrophil gelatinase associated lipocalin) in predicting different types of renal dysfunction in cirrhosis
Kshitiz Sharan , Anand Sharma, Itish Patnaik, Rohit Gupta
Correspondence – Kshitiz Sharan – kshitizshd@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Virbhadra Road. Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Introduction Acute kidney injury (AKI) increases mortality in cirrhosis. Early identification of the cause of AKI helps in planning appropriate management. Neutrophil gelatinase associated lipocalin (NGAL) is upregulated following renal tubular injury and can serve as a novel biomarker to differentiate between hepatorenal syndrome (HRS) and acute tubular necrosis (ATN).
Method Consecutive hospitalized patients with cirrhosis and acute kidney injury were prospectively recruited and managed as per standard care. Acute-on-chronic liver failure (ACLF) was diagnosed as per the CANONIC criteria. Urine NGAL was measured by ELISA by Epitope Diagnostics Inc kit in all patients on admission and patients were followed up till hospital discharge.
Results One hundred consecutive patients (median [range] age 44 [28-81] years; 86% were males; ACLF 67.5%; acute decompensation [AD] 32.5%; MELD 27.5 [13-44] ; CTP 11 [8-15]) with cirrhosis and AKI were recruited. Alcohol was the most common etiology of cirrhosis (58.8%). Prerenal azotemia (PRA) was the most common cause of AKI (n=37) followed by HRS (n=26) and ATN (n=17). Urine NGAL was significantly elevated in ATN (1747 (6-6141) ng/mL than in HRS (435 [24-2320] ng/mL; p<0.0001 and PRA [147 ng/mL] [3.34-626]; p<0.0001). 52.9%patients with ATN, 15.4% patients with HRS and none with PRA required dialysis.19.2% patients with HRS and 47% with ATN died. Urine NGAL was significantly higher in patients who required hemodialysis than those who did not (1845 [286-6141] ng/mL vs. 239 [3.34-2360] ng/mL; p<0.0001]).
Conclusion Urine NGAL is a biomarker that can help differentiate between ATN and HRS in patients with cirrhosis.
Keywords AKI,HRS, NGAL
235
Simultaneous esophageal carcinoma and hepatocellular carcinoma: Case report and systematic review of literature
Anand Sharma, Itish Patnaik, Ashok Kumar, Rohit Gupta
Correspondence – Anand Sharma – andy.mmc@gmail.com
Department of Gastroenterology, All India institute of Medical Sciences, Virbhadra Road, Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Introduction Simultaneous occurrence of esophageal cancer (EC) and hepatocellular carcinoma (HCC) is very rare. We report such a case with a systematic review of literature.
Method We searched PubMed using terms (‘liver’ OR ‘hepatic’ OR ‘hepatocellular’ OR ‘hepatoma’) AND (‘cancer’ OR ‘malignancy’ OR ‘neoplasm’ OR ‘carcinoma’ OR ‘tumour’) AND (‘esophageal’ OR ‘gastroesophageal junction’) since inception. Only publications in English language in which both malignancies were diagnosed unequivocally in humans were included.
Results A 60-year-old male presented with progressive dysphagia to solids for 3 months, progressive abdominal distension for a month and significant weight loss. Evaluation revealed a gastrooesophageal junction growth, biopsy of which was suggestive of adenocarcinoma and a large liver tumor with typical enhancement of HCC on contrast imaging with portal venous and hepatic vein thrombosis. Alfafeto protein levels were 1000-fold elevated. Patient was offered palliation, in view of the advanced malignancies.
We found 7 articles from the above search and one from the references of the above. Together they reported 12 patients. Most cases were from Japan. Eleven patients had synchronous and one had metachronous malignancies. All patients were male (median [range] age 70 [54-84] years). Squamous cell carcinoma was the histological subtype of EC in all patients. Three patients had metastasis and one had a third malignancy in the form of sigmoid colon adenocarcinoma. Alcohol was the most common etiology of liver disease and 7 patients were Child-Pugh class A.
Surgical management of both malignancies was done in 5 patients (simultaneous resection in 2 patients and two step surgery in 3 patients). One patient underwent transarterial embolization and partial resection of HCC with endoscopic mucosal resection of EC at a later date. Six were managed conservatively. Of the 12 patients, only six lived beyond a year.
Conclusion Simultaneous EC and HCC is rare and carries a poor prognosis.
Keywords Esophageal carcinoma, Hepatocellular carcinoma, Dual malignancy, Multiple primaries
236
Prevalence of terlipressin induced diarrhea: A retrospective study
Nitesh Chauhan, Rajiv Baijal, Arun Kumar, Dinesh Singal, Nripen Saikia, Shubham Vatsya, Anil Khatri, Dinesh Kumar, Harshal Patel
Correspondence – Nitesh Chauhan – niteshchauhanpd@gmail.com
Department of Gastroenterology, Pushpawati Singhania Hospital and Research Institute, Press Enclave Marg, Sheikh Sarai, Phase-II, New Delhi 110 017, India
Background Terlipressin is a commonly used drug in patients with chronic liver disease for the management of hepatorenal syndrome and hematemesis. Despite being a very useful drug, it is associated with some adverse events. However, there is not much data related to adverse events of terlipressin.
Methods We retrospectively reviewed the history, laboratory investigations, radiological investigations, medication charts, vital charts and daily progress notes of patients with cirrhosis and hepatorenal syndrome who were treated with terlipressin at our department between January 2020 and July 2021. Data recorded were age, sex, etiology of cirrhosis, diarrhea and its grading, intervention for diarrhea and spontaneous bacterial peritonitis.
Results A total of 44 patients of cirrhosis with hepatorenal syndrome treated with IV terlipressin were analyzed. Diarrhea occurred in 9 (20.45%) patients among which 6 (66.66%) had severe diarrhea, 2 (22.22%) had moderate diarrhea and 1 (11.11%) had mild diarrhea. Among 6 patients of severe diarrhea, terlipressin had to be stopped in 3 (50%) and midodrine started but terlipressin was not restarted as creatinine had normalised till then. Terlipressin had to be stopped and restarted after recovery of loose stools in 2 (33.33%) patients, among them 1 (50%) patient had recurrence while the other 1 (50%) did not have recurrence of diarrhea. Terlipressin was decreased to twice a day in 1 (16.66%) patient with severe diarrhea and loose stools improved. Diarrhea was managed with racecadotril and iv fluids in patients with moderate diarrhea and terlipressin was continued.
Conclusions In our everyday clinical practice, terlipressin related adverse events are common, but often reversible.
Keywords Terlipressin, Diarrhea, Cirrhosis
237
Risk factors associated with bleeding after prophylactic endoscopic variceal band ligation in liver cirrhosis
Sudhir Kumar , Vijai Shankar Chidambaramanivasagam, Kannan Mariappan, Ramani Ratinavel, P B Sriram
Correspondence – Vijai Shankar Chidambaramanivasagam -- vijaishankar.c@gmail.com
Department of Medical Gastroenterology, Madurai Medical College, Panagal Road, Alwarpuram, Madurai 625 020, India
Background Prophylactic endoscopic variceal band ligation (EVBL) is frequently perform in patients with liver cirrhosis. The aim of our study was to identify factors associated with early upper gastrointestinal bleeding in cirrhosis patients after prophylactic EVBL.
Methods Study done on 50 consecutive nonemergency patients with liver cirrhosis who required prophylactic EVBL, in Madurai Medical College. These patients were followed up for 1 month and observed for any early upper gastrointestinal (UGI) bleed within 30 days of EVBL.
Results Within 30 days after EVBL 7 UGI bleed were observed (patients had minor UGI bleed and 2 patients had moderate to severe UGI bleed). Increased serum bilirubin level, low platelet count and higher model for end-stage liver disease (MELD) and Child score were independently associated with UGI bleed following EVBL with statistically significant p value (p<0.05). There was no statistically significant association between grade of varices, presence of red colour sign or increased prothrombin time and UGI bleed. No significant difference in sex, age or cirrhosis etiology was observed between patients with or without post EVBL UGI bleed.
Conclusion EVBL is a safe procedure and early post EVBL bleed is rare. Serum bilirubin, platelet count, MELD score and Child class are associated with early UGI bleed after EVBL. Grade of esophageal varices, red colour sign and prothrombin time are not associated with UGI bleed after EVBL.
Keywords EVBL, UGI bleed, Risk factors, Cirrhosis
238
Herb-induced liver injury (HILI) – Tinospora cordifolia or Tinospora crispa? Lessons learnt to guide herb identification
Aabha Nagral1, Omkar Rudra2, Sherna Menezes1, Kunal Adhyaru1, Sasikumar Menon3, Sunita Shailajan4, Mausumee Mohanty5
Correspondence – Aabha Nagral – aabhanagral@gmail.com
1Departments of Gastroenterology, and 2Critical Care Medicine, Jaslok Hospital and Research Centre, 15, Pedder Road, Mumbai 400 026, India, 3Pharma Analytical Sciences, Institute for Advanced Research and Training in Interdisciplinary Sciences, Plot No. 194, Scheme No. 6, Road No. 15, Sion-Koliwada, Sion, Mumbai 400 022, India, 4Botany Ramnarain Ruia Autonomous College, Herbal Research Lab, Ramnarain Ruia Autonomous College, L. Nappo Road, Matunga, Mumbai 400 019, India, and 5Genomics Barcode Biosciences, No. 90 and 91, 4th Floor, 6th Cross, MCECHS Layout, Dr. Shivarama Karanth Nagar, Bangalore 560 077, India
Introduction Tinospora cordifolia (TC) is vastly consumed in India in the corona virus disease 2019 (COVID-19) pandemic. We published our experience of hepatotoxicity with self-medication with TC in 6 individuals [1]. Since hepatotoxicity has been described with Tinospora crispa (TCR), it was contested that our patients may have mistakenly consumed TCR which looks similar to TC.
Methods Samples of plant (n=4) and commercial preparations (n=2) consumed were collected. The 4 plant samples (stems and leaves) were analyzed morphologically and microscopically by a botanist, all 6 samples were sent for phytochemical analysis by HPTLC and DNA barcoding for confirmation of plant genus and species.
Results The 4 plant samples were shown to be TC based on morphological characteristics, microscopic studies, phytochemical analysis and DNA analysis. The 2 commercial samples could not be analysed on HPTLC or DNA barcoding as there were other ingredients which probably interfered with the analysis. The Table shows the morphological differences
| Tinospora Cordifolia | Tinospora Crispa | |
| Stem Morphology | Less prominent tubercules | Prominent blunt tubercles |
| Micromorphology of Stem |
Transverse section is wedge shaped. Cork layer has many lenticels. |
Transvers section is circular. Cork layer has few lenticels. |
| Leaf Morphology | Heart shaped, 10-20 cm long, acuminate apex with a 3-4 cm petiole | Heart shaped 6-12 cm long, caudate apex with a 5-15 cm petiole |
Conclusion Tinospora cordifolia has been confirmed to be the plant consumed by the patients in our study who presented with HILI. In India, we have the capability to identify the implicated plant with a combination of morphological, microscopic, phytochemical and DNA analysis. Future studies on causality need to focus on the identification of active herb/metabolites in human blood/tissues.
Reference 1. Nagral A, Adhyaru K, Rudra OS, Gharat A, Bhandare S. Herbal immune booster-induced liver injury in the COVID-19 pandemic– A case series. J Clin Exp Hepatol. 2021; doi: 10.1016/j.jceh.2021.06.021.
Keywords COVID-19, Giloy, Drug induced liver injury, Immune booster
239
Acute hepatitis B virus related acute liver failure-Successful outcome with oral antiviral treatment
Parveen Malhotra , Yogesh Sanwariya
Correspondence – Parveen Malhotra – drparveenmalhotra@yahoo.com
Department of Medical Gastroenterology, Post Graduate Institute of Medical Sciences, 128/19, Civil Hospital Road Rohtak 124 001, India
Case Report We present a young female of fourteen years who was admitted to the hospital with short duration of icterus, malaise, vomiting and diagnosed to be having acute hepatitis B. She went into acute liver failure (ALF) as evidenced by development of hepatic encephalopathy and coagulopathy. She was managed on lines of hepatic encephalopathy along with oral antiviral treatment. She recovered successfully and was discharged after two weeks in heamodynamically stable condition. After a gap of six months, she became hepatitis B surface (HbsAg) and hepatitis B e-antigen (HbeAg) negative and hepatitis B virus DNA (HBV DNA) was undetectable with normal liver function tests. She is on regular follow-up for last one year and is absolutely normal.
Conclusion Acute hepatitis B can go into acute liver failure in 1% of cases, treatment for which includes liver transplantation and oral antiviral treatment which is especially helpful in cases who cannot afford liver transplantation, as was in our case.
Keywords HbeAg, HBV DNA, Hepatic encephalopathy, Acute liver failure, Entecavir
240
Validation of non-invasive fibrosis scores in Indian patients with biopsy-proven non-alcoholic fatty liver disease
Priya Singh , Manu Mehta, Arka De, Suvradeep Mitra, Ashim Das, Ajay Duseja
Correspondence – Ajay Duseja – ajayduseja@yahoo.co.in
Department of Hepatology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Introduction Non-invasive scores for assessing hepatic fibrosis in non-alcoholic fatty liver disease (NAFLD) have not been validated in Indian patients. We aimed to validate AST-platelet ratio index (APRI), Fibrosis-4 (FIB-4) and NAFLD fibrosis score (NFS) in biopsy-proven patients with NAFLD.
Methods Prospectively collected data of 129 biopsy-proven NAFLD patients was reviewed retrospectively (Males – 86, mean age: 40.2 ± 10.3 years). Primary objective was to assess discriminatory ability of APRI, FIB-4 and NFS scores to detect significant (≥F2) and advanced fibrosis (≥F3) on liver histology. Secondary objectives were to assess diagnostic performance of conventional cut-offs of these scores for ruling-in and ruling-out significant and advanced fibrosis and define optimal cut-offs if required. Findings were internally validated using bootstrapping.
Results Out of 129, significant and advanced fibrosis on histology were present in 31 (24%) and 18 (14%) patients. All three scores had poor AUROCs for discriminating significant fibrosis on histology (APRI [0.61, 95% CI:0.49-0.71], FIB-4 [0.62,95% CI: 0.51-0.72] and NFS [0.65, 95% CI: 0.53-0.76]). For detecting advanced fibrosis, APRI (0.73,95% CI: 0.65-0.83) and FIB-4 (0.72, 0.64-0.83) had acceptable AUROCs but NFS fared poorly (AUROC [0.66, 95% CI: 0.55-0.74]). Conventional APRI cut-offs of <0.5 and >2.0 demonstrated good diagnostic performance for ruling-out (sensitivity: 0.94, specificity: 0.24, NPV: 0.96) and ruling-in (specificity: 0.91, sensitivity: 0.11, PPV: 0.17) advanced fibrosis. However, the diagnostic performance of conventional FIB-4 cut-offs of <1.45 and >2.67 for ruling-out (sensitivity: 0.72, specificity: 0.58, NPV: 0.92) and ruling-in (specificity: 0.88, sensitivity: 0.22, PPV:0.23) advanced fibrosis were suboptimal. Optimal FIB-4 rule-out and rule-in cut-offs in our cohort for discriminating advanced fibrosis were <0.82 (sensitivity: 0.94, specificity: 0.28, NPV: 0.97) and >2.81 (specificity: 0.91, sensitivity: 0.22, PPV:0.27) and performed better than the conventional cut-offs (p=0.02).
Conclusion APRI and FIB-4 have good AUROC for detecting advanced fibrosis in Indian patients with NAFLD; cut-offs however need to be recalibrated.
Keywords Fatty liver, FIB-4, APRI
241
A prospective, randomized, double-blind, placebo-controlled phase III, multicenter study to evaluate the immunogenicity and safety of recombinant hepatitis E vaccine in healthy adults and adolescents
Premashish Kar1, V G Mohan Prasad2, Rohidas Borse3, Neelam Nalinbi4, Lubna Zafar5, Sneha Bhoir6, Madhukar Pandey7, Krishnaprasad Anne8, Sumeet Jagtap9, Aditya Vardhan Singh10, Vijay Chamle11
Correspondence – Aditya Vardhan Singh – adi2k3aditya@gmail.com
1Department of Gastroenterology, Max Super Speciality Hospital, Vaishali A-Unit of Crosslay Remedies Ltd, W-3, Sector-1, Vashali, Gahaziabad 201012, India, 2VGM Gastro Centre, Trichy Road, Coimbatore 641 005, India, 3Department of General Medicine, B J Government Medical College and Sassoon General Hospitals, Sasson Road, Somwar Peth, Pune 411 001, India, 4Department of Gynecology, RIMS CIR, Indraprasth Colony, Bariatu, Ranchi 834 009, India, 5Department of General Medicine, Aligarh Muslim University, Medical Road, Aligarh 202 002, India, 6Department of Gynecology, St. Mother Teresa Mulitispecility, Satpala Naka, Pipri Dontalav, Virar West, Vasai-Virar 401 301, India, 7Department of Paediatrics, Shubham Sudbhawana Super Speciality Hospital, B31/80, 23B-Bhogabeer Lanka, Varanasi 221 005, India, 8Department of General Medicine, Pranaam Hospital,1-56/6/40 and 41, Pranaam Hospital Lane, Mythri Nagar, Madeenaguda 500 050, India, 9Sai Sneh Hospital and Diagnostic Centre, Pune-Satara Road, Katraj, Pune 411 046, India, 10Department of Gastroenterology, Paras HEC Hospital, Sector 3, HEC, Dhurwa Ranchi 834 004, India, and 11Urihk Pharmaceutical Ltd. (Subsidiary of Ureka Hong Kong Limited), 502, Sai Samarth Business Park, Near Wasan Motors, Deonar, Govandi (East), Mumbai 400 088, India
Introduction In India, hepatitis E virus (HEV) infection is responsible for 10% to 40% of acute hepatitis and 15% to 45% of acute liver failure (ALF). HEV is the most common cause of ALF in pregnant women leading to substantial maternal morbidity and mortality. Additionally, superimposed HEV is a leading cause of acute on chronic liver failure (ACLF). With limited drugs, vaccine against HEV is the effective approach to control the disease. Only available recombinant vaccine against HEV was approved in 2012 in China. In this phase III study, we will evaluate safety and efficacy of recombinant hepatitis E vaccine in Indian subjects.
Methods We will include healthy adults and adolescents (16 to 65 years), seronegative for anti-HEV antibody. Subjects with confirmed hepatitis and other conditions like uncontrolled epilepsy, neurological and blood disorder, etc. will be excluded. Enrolled subjects will be randomized in 1:1 proportion to receive either hepatitis E vaccine or a matching placebo. A single dose (0.5 mL) of vaccine or placebo will be administered at 0, 1 and 6 months after randomization. Primary objective will be rate of seroconversion. Secondary objective will be the mean change in anti-HEV antibodies and safety assessment. Assuming 99.9% seroconversion rate, 90% superiority margin and dropout rate of 20%, a sample size of 188 subjects (94/arm) will be recruited.
Results The Central Licensing Authority in India and Institutional Ethics Committees of total nine sites across the country including both Private and Government institutes have approved the study. We estimate that, required sample recruitment and study completion will be approximately done within a year of study initiation. Study findings will be submitted to regulatory bodies for its marketing authorization in India.
Conclusion Availability of this recombinant hepatitis E vaccine in India would be significant milestone in our efforts to control the morbidity and mortality associated with HEV.
Keywords Viral Hepatitis, Liver failure, HEV, Pregnancy, Recombinant hepatitis E vaccine
242
Management of autoimmune hepatitis related decompensated cirrhosis with immunosuppressive therapy in a non-transplant resource limited setting–An observational study
Vikramaditya Rawat, Shamshersingh Chauhan, Vikas Pandey, Mit Shah, B Kiran, Chintan Tailor, Pratik Sethiya, Mayur Gattani, Vipul Chaudhari, Rahul Jadhav, Meghraj Ingle
Correspondence – Meghraj Ingle – drmeghraj@gmail.com
Department of Medical Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai 400 022, India
Introduction Whether to treat patients of autoimmune hepatitis related decompensated cirrhosis with immunosuppression remains a dilemma. This observational study was conducted to look at the outcome with immunosuppressive therapy in patients with autoimmune hepatitis related decompensated cirrhosis.
Methods Retrospective data was collected from January 2017 to December 2020 of patients with autoimmune hepatitis related decompensated cirrhosis admitted at our tertiary care hospital. Patients with autoimmune hepatitis related decompensated cirrhosis were treated with steroids with/without immunomodulators using a predetermined treatment protocol and routine standard of care. Survival at the end of one year and change in MELD score (delta MELD) was calculated.
Results Thirty-five patients with autoimmune hepatitis related decompensated cirrhosis were studied. Mean age was 45.40 +/- 14.5 years. 54.3% of the patients were females. Ascites was the most common form of decompensation (91.4%). Mean CTP score was 9.89 +/- 1.6 and mean MELD score was 13.98 +/- 4.5 at the baseline. 65.7% of the patients were treated with a combination of oral corticosteroids and immunomodulators, 14.2% were treated with oral corticosteroids alone and 20% were not started on any of the immunosuppressants. At the end of one year, resolution of ascites was seen in more than half the patients (57.1%) with five patients succumbing to their illness. Most common cause of death was sepsis. SBP (17.1%) was the most common form of infection. MELD decreased by a mean of 3.72 points from baseline in patients who survived at the end of one year. There was no significant difference in the rates of infections (p=0.5), change in MELD (p=0.9), survival (p=1) and resolution of ascites (p=0.16) between those who received immunosuppression when compared to patients who did not receive therapy.
Conclusion In a non-transplant resource limited setting, immunosuppressive therapy did not improve survival in patients with autoimmune hepatitis related decompensated cirrhosis.
Keywords Autoimmune hepatitis, Decompensated cirrhosis, Immunosuppresants, Survival
243
Poor oral hygiene predicts the presence of ascitic fluid infection in patients with decompensated cirrhosis
B Kiran , Vikas Pandey, Shamshersingh Chauhan, Chintan Tailor, Vikramaditya Rawat, Mit Shah, Rahul Jadhav, Vipul Chaudhary, Pratik Sethiya, Saiprasad Lad, Vishal Dawalwar 1
Correspondence – Vikas Pandey – kiranmmc2k8@gmail.com
Departments of Gastroenterology, and 1Dentistry, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai 400 022, India
Background Ascitic fluid infection (AFI) is one of the important complications of cirrhosis which has poor prognosis. It may be classified as spontaneous bacterial peritonitis (SBP), culture negative neutrocytic ascites (CNNA) or bacteriascites. Bacterial translocation from gastrointestinal (GI) tract is considered to be the most important mechanism that leads to development of AFI. Poor oral hygiene may cause subclinical or persistent infections in cirrhotic patients may act as independent risk factor for adverse outcomes in cirrhotic patients including AFI.
Aim To assess the correlation between AFI in patients with decompensated cirrhosis having poor oral hygiene.
Methods All in patients of cirrhosis with ascites were examined for ascitic fluid analysis including total protein, albumin, glucose, PMN count. Fluid was also inoculated at bedside for cultures. Oral hygiene was examined for all patients by using the dental mirror. OHI-S was calculated after calculating calculus and Debris index to determine good /poor oral hygiene.
Results A total 200 patients of decompensated cirrhosis were enrolled in the study. With mean age of 50.9 + 9.85. There were 78 % males with a mean BMI of 18.9 + 1.9. Alcohol was the major cause of cirrhosis (72%). Mean MELD and CTP were 18.6+7.43 and 10.2 +1.28. Mean OHI- S was 1.8+1.07. AFI was found in 28%, SBP and CNNA27% was found in 1% and 27 % respectively. On univariate analysis CTP, MELD, BMI, hemoglobin, serum protein and albumin significantly associated with poor oral hygiene (p<0.001). Poor oral hygiene was found in 59.6 % in patients with AFI compared to 16.9 % in patients without SBP/CNNA (p<0.001). S – OHI so predicted presence of AFI with a AUROC of 0.83.
Conclusion We suggest screening for oral hygiene in all patients of decompensated cirrhosis as it may be a harbinger of ascitic fluid infection.
Keywords Decompensated cirrhosis, Ascitic fluid infection, S-OHI, Poor oral hygiene
244
Clinical profile of primary Budd-Chiari syndrome- A case series
Kondala Rao Yedupati , Kannan Mariappan, Ramani Ratinavel, Vijaishankar Chidambaramanivasagam, P Sriram
Correspondence – Vijaishankar Chidambaramanivasagam – vijaishankar.c@gmail.com
Department of Medical Gastroenterology, Madurai Medical College. Panagal Road, Alwarpuram, Madurai 625 020, India
Aim A case series of Budd-Chiari syndrome (BCS).
Methods Five cases of confirmed primary BCS taken and compared the demographic patterns, clinical features, various laboratory parameters, imaging studies, upper GI endoscopic features, various prognostic scores and treatment.
Results From the case series chronic presentation is more common than acute, mixed type BCS common than classic BCS. Demographic profile of the group showed mean age is 24.2. Majority is female population and low economic status. Clinical symptoms in acute BCS include pain abdomen, abdominal distension, pedal edema and without jaundice. In the chronic BCS group 50% presented with abdominal distension and UGI bleed, followed by jaundice, pain abdomen and pedal edema, one case had asymptomatic presentation. Acute BCS presented with hepatomegaly, splenomegaly, ascites. Chronic BCS 50% present with hepatomegaly,50% presented with splenomegaly, 75% have ascites, one case presented with dilated abdominal veins. In chronic BCS 75% have INR> 1.5. Doppler flow study can detect flow in hepatic veins but not in IVC. MRI abdomen can detect IVC thrombus when compared with Doppler. Endoscopy study in chronic BCS 50% cases showed grade 3 esophageal varices and EVBL done, other 50% cases showed grade 1 esophageal varices. In acute BCS grade 1 esophageal varices present. All cases both acute and chronic BCS started on anticoagulation. Acute BCS not responed to oral anticoagulation and diuretic treatment. In our current series of chronic BCS group two cases Child class C having MELD score >20 and Rotterdam class 3, but Clichy score < 6.6.
Keywords Acute and chronic BCS, Classic and mixed BCS
245
Impact of obesity and diabetes mellitus on the accuracy of APRI and FIB-4 in detecting advanced fibrosis in patients with non-alcoholic fatty liver disease
Manu Mehta1, Priya Singh1, Arka De1, Suvradeep Mitra2, Ashim Dass2, Ajay Duseja1
Correspondence – Ajay Duseja – ajayduseja@yahoo.co.in
Departments of 1Hepatology, and 2Histopathology, Post Graduate Institute of Medical Education and Research, Sector-12, Chandigarh 160 012, India
Introduction Non-invasive scores are important tools for assessing fibrosis in non-alcoholic fatty liver disease (NAFLD). Obesity and type 2 diabetes mellitus (DM) are important clinical predictors of fibrosis that are not incorporated in the commonly used non-invasive scores of APRI and FIB-4. Thus, the aim of the present study was to assess the discriminatory performance of APRI and FIB 4 for predicting the presence of advanced hepatic fibrosis (≥ F3 fibrosis) on histology in patients with obesity or DM compared to patients without these co-morbidities.
Methodology We retrospectively reviewed the prospectively collected data of 129 patients (males:86 [66.7%], age:40.2 ± 10.3 years) with biopsy proven NAFLD. Obesity was defined using Asia-Pacific cut-offs (BMI ≥25 kg/m2). Patients were included only if they had all laboratory parameters for calculating APRI and FIB 4 scores within one month of performing liver biopsy.
Results Advanced fibrosis on histology was present in 18 (14%) of 129 patients. In the whole cohort, both APRI (0.73,95% CI: 0.65-0.83, p<0.001) and FIB4 (0.72,95% CI: 0.64-0.83, p<0.001) showed acceptable AUROCs for detecting advanced fibrosis on histology. Eighty-seven (67.4%) patients were obese and 20 (15%) had DM. AUROCs of FIB4 (0.72 [95% CI: 0.56-0.85] vs. 0.72 [95% CI: 0.61 to 0.81], p=0.99) and APRI (0.74 [95% CI: 0.59-0.87] vs. 0.72 (95% CI: 0.62-0.81, p=0.85) for discriminating advanced fibrosis on histology were comparable in non-obese and obese patients, respectively. However, both APRI (AUROC: 0.60, 95% CI: 0.36-0.81, p=0.43) and FIB4 (AUROC: 0.64, 95% CI: 0.40-0.83, p=0.35) fared poorly in diabetic patients for predicting advanced fibrosis.
Conclusion Presence of diabetes but not obesity impacts the accuracy of APRI and FIB-4 for discriminating advanced fibrosis in patients with NAFLD.
Keywords NAFLD, APRI, FIB4, Liver biopsy
246
Cutaneous mucormycosis: An unusual cause of decompensation in a patient with ethanol-related cirrhosis with corona virus disease 2019 exposure
Sherna Menezes1, Janu Kumar2, Omkar Rudra3, Aabha Nagral1
Correspondence – Aabha Nagral – aabhanagral@gmail.com
Departments of 1Gastroenterology, 2Medicine, and 3Critical Care Medicine, Jaslok Hospital and Research Centre, 15, Pedder Road, Mumbai 400 026, India
Introduction Mucormycosis is an opportunistic fungal infection that leads to angio-invasion causing necrosis and eschar formation in the affected areas, with cutaneous forms being extremely rare. Patients with cirrhosis are at increased risk of fungal infections due to suppressed immunity, with an increased prevalence during the corona virus disease 2019 (COVID-19) pandemic.
Case Report We describe a rare case of cutaneous mucormycosis in a middle-aged male with ethanol-related chronic liver disease. He presented with symptoms of fever, breathlessness and altered mental status. On admission, he was in septic shock and acute respiratory distress syndrome (ARDS). He was noticed to have ruptured blisters in his left axilla. Although he was negative for COVID-19 RT-PCR, he had positive IgG antibodies for COVID-19. He was managed with broad-spectrum antibiotics, steroids, vasopressors as well as ventilation for ARDS. Over the course of his hospitalization, the axillary lesion progressed to a necrotizing ulcer with deep tissue invasion. Debridement and culture of the axillary ulcer revealed mucor species and therapy with antifungals was initiated. Unfortunately, he continued to deteriorate despite aggressive management and succumbed after a prolonged hospital course of 40 days.
Discussion Mucormycosis is an invasive fungal infection that is most commonly seen in the rhino-orbito-cerebral region and lungs. Cutaneous presentations are rare. We believe the immune suppression due to COVID-19 exposure and co-morbid chronic liver disease led to the development of mucormycosis. The infection was diagnosed late due to its unlikely location. The addition of steroids for septic shock during hospitalization could also be contributory to the exacerbation of the infection.
Conclusion Invasive fungal infections can lead to rapid decompensation in chronic liver disease patients and require a high degree of suspicion for diagnosis. Minimization of risk factors with early diagnosis and aggressive management is key in such cases.
Keywords Acute on chronic liver failure, Fungal infection, Alcohol liver disease
247
Study of prevalence and influence of nucleoside diphosphate-linked moiety X-type motif 15 (NUDT15) and thiopurine S methyltransferase (TPMT) variants in Indian patients with autoimmune liver diseases and post liver transplantation receiving azathioprine
Rahul Deotale, Aabha Nagral, Deepakkumar Gupta, Amey Sonavane, Shankar Bhanushali, Ronak Tate
Correspondence – Rahul Deotale – rahuldeotale23@gmail.com
Department of Medical Gastroenterology, Apollo Hospitals, Navi Mumbai 400 614, India
Background and Aim Thiopurine-induced leukopenia (TIL) is seen in patients receiving thiopurine drugs like azathioprine and 6-mercaptopurine used to maintain remission in patients of autoimmune hepatitis (AIH) and post liver transplantation. TPMT and Nucleoside diphosphate-linked moiety X-type motif 15 (NUDT15) gene variants have been shown to be associated with TIL. There are very few studies showing the influence of NUDT15 gene variants on Indian patients with AIH and post liver transplant. Our study aims to find the prevalence and influence of these gene variants in Indian patients with AIH and post liver transplant being treated with azathioprine.
Methods In a prospective observational study, 35 patients with AIH and post liver transplant being treated with azathioprine were enrolled for the study. Frequencies of NUDT15 C415T variant and TPMT gene variants (*2, *3A, *3B, *3C) was studied by PCR. CBC was monitored at baseline and at weeks 2, 4, 8 and 12.
Results Out of 35 patients, 4 found to have NUDT15 C415T variant (11.4%). All 4 were carrying heterozygous pathogenic variant, none were homozygous. Out of these, 2 developed leucopenia (50%), whereas 1 patient (3.2%) without NUDT15 gene variant developed leucopenia (p<0.029). Both patients with NUDT15 variant who developed leucopenia, TIL reversed within 12 weeks of stopping azathioprine. Patient with wild type NUDT15 variant with leucopenia was further evaluated for other less common NUDT15 gene variants, which were found to be negative. TPMT variants were not seen. The sensitivity and specificity for NUDT15 variant for TIL were 66.67% and 93.75% respectively.
Conclusion NUDT15 variant frequency was found to be 11.4% and 50% of them developed leucopenia, showing strong association for TIL. NUDT15 variants are more common than TPMT variants in Indian population and only NUDT15 variant may be tested. However, larger studies in Indian population are needed for further recommendations.
Keywords Azathioprine, NUDT15, TPMT, Autoimmune hepatitis, Post liver transplant, Indian
248
Baseline plasma metabotype correlates with direct acting antiviral therapy (DAA) nonresponse for HCV in HIV-HCV co-infected patients
Gaurav Tripathi , Sheetalnath Rooge, Manisha Yadav, Babu Mathew, Nupur Sharma, Vasundhra Bindal, Hamed Hemati, Ekta Gupta 1 , Jaswinder Maras
Correspondence – Jaswinder Maras – jassi2param@gmail.com
Departments of Molecular and Cellular Medicine, and 1Virology, Institute of Liver and Biliary Science, D1 Vasant Kunj, New Delhi 110 070, India
Introduction With the advent of direct-acting antiviral (DAA) therapy for HCV, cure is achieved at similar rates among co-infected with HIV as in HCV mono-infected patients. The present study evaluates host plasma metabolites as putative indicator in predicting the treatment response in baseline HIV-HCV patients.
Methods Non cirrhotic HIV-HCV (43) coinfected patients were treated with Sofosbuvir and Daclatasvir for 12 weeks. Plasma metabolite profiling pre and post therapy was analyzed in 20/43 patients. Of the 20 selected 10 (50%) attained the SVR (Responders) as defined by absence of HCV RNA at 12 weeks after the treatment and 10 (50%) didn’t attained the cure for HCV (non-responders).
Results A total of 565 features were annotated (metabolomic/spectral databases). Pre therapy, 39 metabolites differentiated (FC ±1.5, p<0.05) non-responders from responders. Of these 20 up- and 19 down-regulated were associated with tryptophan metabolism, nicotinamide metabolism and others. Post therapy, 62 plasma metabolite (12-up and 50-down, FC±1.5, p<0.05) differentiated non-responders from responders and highlighted significant increase in steroid, histidine metabolism and significant decrease in tryptophan metabolism, ascorbate, pyruvate metabolism in the non-responders. Based on random forest and multivariate linear regression analysis, baseline level of N-acetylspermidine (FC>2, AUC=0.940, Bfactor = -0.267) and 2-Acetolactate (FC>2, AUC=0.880, Bfactor = -0.713) significantly differentiate between non-responders from responders in HIV-HCV co-infection patients and were able to predict the failure of treatment response.
Conclusion Baseline increase in N-acetylspermidine and 2-Acetolactate levels is associated with likeliness of failure in attainment of cure for HCV in HIV-HCV co-infected patients
Keywords Metabolomics, HIV-HCV co-infection, Direct Acting Antivirals, DAA responders
249
Outcomes in cirrhosis patients with invasive candidiasis: A systematic review and meta-analysis
Nipun Verma 1 , Akash Roy 2 , Shreya Singh 3 , Pranita Mahajan 3 , Pratibha Garg 1 , Meenu Singh 3
Correspondence – Nipun Verma – nipun29j@gmail.com
Departments of 1Hepatology, and 3Mycology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh 160 012, India, 2Department of Hepatology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India, and 3Indian Council of Medical Research, Center for Evidence-Based Child Health , PGIMER, Chandigarh 160 012, India
Introduction Bacterial infections are the well-known determinant of poor prognosis in cirrhosis. However, little is known about the impact of invasive candidiasis (IC) on the outcomes in non-conventional high-risk cirrhosis patients. Therefore, we systematically reviewed the outcomes and factors influencing them in cirrhosis patients with IC.
Methods PubMed, Embase, Ovid, CINHAL, and Web of Science were searched for full-text observational studies describing mortality related to IC in cirrhosis. We did a systematic review and random-effects meta-analysis to pool the mortality estimates in cirrhosis patients with IC (point-estimate and comparative-odds). The estimate and rsquo;s heterogeneity was explored on sub-groups, outliers-test, and meta-regression. We evaluated the asymmetry in estimates on funnel plot and Eggers’s regression. Quality was assessed on the New-Castle Ottawa scale.
Results Of 3143 articles, 13 studies (611 patients) were included (good/fair quality: 6/7).; IC patients were sick with a high MELD (27.0, range: 17.0-38.0) and hospital stay (33.2 days, range: 25.0-43.0). The pooled mortality in IC patients was 54.7% (95% CI: 41.3-67.5), I2: 80%, P<0.01. Intensive care unit (ICU) admission (P<0.001), site of infection; viz. peritonitis and candidemia (p=0.014) and high MELD of cases (p=0.029) were predictors of high mortality. The odds of mortality due to IC was 4.4 times higher than controls, which was 8.5 and 3.3 times higher than non-infected and bacterially infected cirrhosis. Studies with ICU-admitted (OR: 5.0) or acute-on-chronic liver failure (ACLF, OR: 6.3) patients had higher odds of mortality than all-hospitalized cirrhosis patients (OR: 4.0). Insufficient data precluded us from analyzing IC-attributable mortality and the impact of antifungals.
Conclusions A substantial mortality; higher than bacterial infections is seen in cirrhosis patients with IC. ICU admission, ACLF, high MELD, peritonitis, and candidemia are key factors determining high mortality in cirrhosis patients with IC. Intense efforts are needed for early diagnosis and appropriate treatment of IC in cirrhosis.
Keywords Cirrhosis, Invasive candidiasis, Mortality
250
Sarcopenia is the independent predictor of mortality in critically ill patients with cirrhosis
Saniya Khan 1 , Jaya Benjamin 1 , Rakhi Maiwall 2 , Harshita Tripathi 1 , Puja Bhatia
Kapoor 1 , Varsha Shasthry 1 , Vandana Saluja 3 , Prashant Agarwal 3 , Shalini Thapar 4 , Guresh Kumar 5 , Yogendra Kumar Joshi 1 , Shiv Kumar Sarin 2
Correspondence – Jaya Benjamin – jayabenjaminilbs@gmail.com
1Departments of Clinical Nutrition, 2Hepatology, 3Anaesthesia and Critical Care, 4Radiology, and 5Clinical Research, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Background and Aim Sarcopenia is strongly associated with poor outcome in cirrhosis. There is little prospective data that sarcopenia influences outcomes in critically ill cirrhotics (CICs). Computed tomography (CT) is the gold standard for body composition assessment in the ICU, as it is independent of hydration status.
Aim To assess the prevalence of sarcopenia and study its impact on clinical outcomes in CICs.
Methods In this prospective observational study, CICs admitted to the liver ICU (LICU) between January 2020 to June 2020 were enrolled, if meeting inclusion (age 18-70 years, abdominal CT scan within three months prior to ICU admission) and exclusion criteria (survival likely to be <24 hours, coexisting chronic diseases). Clinical, hemodynamic, biochemical, nutritional parameters, including length of stay (LOS), duration of mechanical ventilation (MV), development of new onset infections (NOI), and overall survival were recorded. CT images at the L3 level were analyzed using slice-o-matic V4.3 software to assess the skeletal muscle index (SMI)- expressed as skeletal muscle area (cm2)/height (m2). Sarcopenia was defined if SMI was <50cm2/m2- males and <39cm2/m2- females. Data was analyzed using SPSS version 22.
Results Altogether 111 patients (M-83.8%; age 48.37±11.3 yrs; etiology: alcohol- 56 [50.5%], NASH-27 [24.3%], viral-12 [10.8%], others-16 [14.4%]; CTP-11.9±1.8; MELD-27.8±7.3; SOFA-10.5±4.1; APACHE-23±8; MV-54 [48.6%]) were enrolled. Of these, 76 (68.5%) were sarcopenic and 35 (31.5%) non-sarcopenic. Sarcopenic CICs had higher overall mortality (72.4%) compared to non-sarcopenics (48.6%) {p=0.015, OR [95% CI]- 2.77 [1.2-6.37]) and higher prevalence of sepsis at ICU admission (72.4% vs. 45.7%, p=0.007, OR [95% CI]- 3.1[1.35-7.15]) than non-sarcopenics. LOS, duration of MV, incidence of NOI, and overall survival were comparable between groups. Multivariate binary logistic regression showed that sarcopenia and APACHE score were independently associated with mortality.
Conclusion Two-thirds of critically ill cirrhotics have sarcopenia at ICU admission, with three times higher prevalence of sepsis and 2.8 times higher mortality in the ICU.
Keywords Nutrition in liver cirrhosis, Body composition by computed tomography, Sarcopenia
251
Abdominal tuberculosis – A Rare case of extrahepatic portal hypertension
Arathi S Gadwalkar, Rohit Mathur, D N Reddy
Correspondence – Arathi S Gadwalkar – arathigadwalkar15@gmail.com
Department of Gastroenterology, Asian Institute of Gastroenterology, Gachibowli, Hyderabad 500 084, India
Background Portal hypertension is an important cause of upper gastrointestinal bleeding. Although there are multiple causes of it there are a few rare causes of portal hypertension. Here we are presenting such a case of portal hypertension.
Clinical Case A 25-year-old male presented to our ER with malena. He was diagnosed with pulmonary tuberculosis which was detected during a routine VISA health check-up. He was on first-line antituberculosis (ATT) drugs since October 2019. Upper gastrointestinal endoscopy showed grade 2 varices with a red color sign, endoscopic banding was done. CECT abdomen showed abnormal soft tissue density mass in suprapancreatic and periportal region encasing portal vein and CBD causing IHBRD with collaterals with no evidence of portal vein thrombosis (Fig. 1). EUS guided biopsy from peripancreatic and periportal lymph nodes were suggestive of necrotizing granulomatous lymphadenitis implicative of tuberculosis (Fig. 2). His repeat scan showed a reduction of lymph node size to less than 50% of baseline size, decrease in the size of the portal vein and spleen with improvement in clinical parameters.
Conclusion Involvement of periportal lymph nodes in tuberculosis is exceptional1 and there is a handful of case reports of lymph nodes compressing the portal vein at porta hepatis and manifesting as portal hypertension (PH) causing upper gastrointestinal bleeding as evidenced in our case 2. The suggested mechanism of PH in our case is compression of the portal vein by enlarged lymph nodes at the hepatic hilum. Although rare it is a treatable condition.
Keywords Abdominal tuberculosis, Portal hypertension
252
Interaction of hepatitis B virus X protein (HBx) and FXR nuclear receptor for hepatocellular carcinoma progression
Afnan Quadri , Baibaswata Nayak
Correspondence – Baibaswata Nayak – baibaswat@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Hepatitis B virus infection is one of leading causes of hepatocellular carcinoma. HBV genome known carry nuclear response element in the enhancer region. The corresponding nuclear response can modulate HBV replication and may promote hepatocarcinogenesis. Therefore, we designed several deletion constructs and studied protein HBx-FXR interaction to evaluate its role in carcinogenesis.
Aim To study role of nuclear receptor in HBV induced hepatocarcinogenesis
Methodology The Hbx region was PCR amplified from full length HBV 1.3 mer plasmid. Full length HBx and C-terminal 14aa, 27 aa, 35 aa and 40aa deletion constructs with and without flag tag was designed cloned in pCDNA 3.1 vector. Mammalian expression of these proteins were checked by transfection using anti-HBx and anti-flag antibody. Interaction of full length HBx and DHBx with FXR was studied by co-immunoprecipitation assay. Weather binding of HBx or DHBx with FXR increases transcriptional activity will be checked by using luciferase reporter assay system.
Results Cloning of HBx and DHBx in pcDNA 3.1 was carried out with sequence confirmation. Mammalian expression of full length and deleted HBx was confirmed by anti-HBx and anti-flag antibody. Expression of nuclear receptor was checked by transfecting pCMV3-NR5A2-t3 (LRH-1), pCMV3-NR0B2-HA (SHP1), pCMV3-NR1H4-t6 (FXR) using anti-nuclear specific antibodies and anti-HA antibody. Co-immunoprecipitation study and western blot assay found interaction.
Conclusion HBx C-terminal truncation may play a significant role hepatocarcinogenesis through nuclear receptor mediated signalling.
Keywords HCC, HBV, HBX, Nuclear receptor, Cancer
253
A retrospective analysis of liver function tests in corona virus disease 2019 infection in a tertiary care centre
Arun Dhotra , A Anand, Kani Shaikh, A R Akilandeshwari, A Arun
Correspondence – Arun Dhotra – arun.dhotra88@gmail.com
Department of Digestive Health and Diseases, Government Kilpauk Medical College, 822, Poonamallee High Road, Kilpauk, Chennai 600 010, India
Introduction: Corona virus disease 2019 (COVID-19) pandemic has affected about 240 million people worldwide till now. Although COVID-19 patients usually present with respiratory symptoms, but involvement of other organ systems have also been reported. Few studies suggest that severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) is associated with liver dysfunction or damage. Our study aims to evaluate liver function test in COVID-19 infection and to observe any correlation between elevated LFTs and severity of disease.
Methods A retrospective study was carried out at Govt. KMC Hospital, Chennai. Two month study period was taken during second covid wave (1st May 2021 to 30th June 2021). All COVID-19 positive patients who were above 19 years of age and without any chronic liver disease, hepatitis B or hepatitis C were included in the study. Data was collected from case files. Record was made of the liver function tests and inflammatory markers (CRP, IL-6). Severe disease was defined as patients requiring ICU admission or mechanical ventilation. Collected data was analysed using appropriate statistical tests.
Results One hundred and thirty-two patients were included in the study. Out of these 59 patients (44.70%) had elevated LFTs. Maximum patients (42.37%) had hepatocellular pattern. 59.32% patients were males. Mean age of patients with elevated LFTs was 51.03±13.03 years. ICU admission was required in 40.68% of patients with deranged LFTs compared to 23.28% in patients with normal LFTs. A positive correlation was found between deranged LFTs and inflammatory markers (CRP, IL-6) (p<0.0001).
Conclusion Abnormal liver function tests are present in a significant number of COVID-19 positive patients. Elevated LFTs show a positive correlation with the inflammatory markers. Severe disease was more common in patients with abnormal liver function tests
Keywords COVID-19, Liver function test, Severe disease
254
Prevalence and predictors of non-alcoholic fatty liver disease among pregnant primigravida women in southern India
Pradip Vekariya 1 , Mohan Pazhanivel 1 , Haritha Sagili 2 , A Ramesh 3 , Sadishkumar Kamalanathan 4 , Senthamizh Selvan 1
Correspondence – Mohan Pazhanivel – dr.pazhani@gmail.com
Departments of 1Medical Gastroenterology, 2Obstetrics and Gynecology, 3Radioagnosis, and 4Endocrinology, Jawaharlal Institute of Postgraduate Medical Education and Research, Gorimedu, Puducherry, 605006, India
Introduction Non-alcoholic fatty liver disease (NAFLD) is a common cause of chronic liver disease worldwide and is strongly associated with obesity and insulin resistance. NAFLD has not been extensively studied in Indian pregnant women. We studied the prevalence of NAFLD and its association with clinical and metabolic profile in Indian primigravida women. We also defined the cut-off value of homeostatic model assessment of insulin resistance (HOMA-IR) for the prediction of NAFLD in pregnant women.
Methods In this cross-sectional study, consecutive primigravida women in their first trimester were screened for NAFLD using a liver ultrasound between August 2019 and March 2021. Those with pre-existing diabetes, hypertension, chronic liver disease, multiple pregnancies, or a history of alcohol consumption were excluded. The association between NAFLD with clinical and biochemical markers were assessed by univariate and multiple analysis. A cut-off value of HOMA-IR for NAFLD prediction was calculated using the area under the curve.
Results Of the 504 women screened, 23.1% (n=116; mild 83, moderate 33, nonsevere) had NAFLD. A total of 316 women (200 without and 116 with NAFLD) were included for analyzing the risk factors for NAFLD. Their median maternal age was 25 (22-27) years. The women with NAFLD had a higher BMI (23.7 vs. 21.5, p<0.0001), mean arterial pressure (85.06 vs. 81.57 mmHg, p<0.001), HOMA-IR (1.68 vs. 0.91, p<0.001) and a lower serum adiponectin concentration (7.14 vs. 11.12 μg/mL, p<0.001). On multivariable logistic regression; BMI, HOMA-IR and serum adiponectin concentration were independent predictors of NAFLD in pregnancy. The HOMA-IR cut-off value of 0.9 had 71% sensitivity and 50% specificity to predict NAFLD (AUC-0.63, p<0.001).
Conclusion This study reveals a silent epidemic of NAFLD affecting one in every four pregnant primigravida women. The presence of obesity, insulin resistance and low serum adiponectin concentration are independent markers for NAFLD in pregnancy
Keywords Adiponectin, Insulin resistance, Non-alcoholic fatty liver disease, Obesity, Primigravida
255
Molecular detection of HBV DNA in ascitic fluid of patients suffering from decompensated liver cirrhosis
Shiv Singh
Correspondence – Shiv Singh – spratap0305@gmail.com
Department of General Medicine, King George Medical University, Chowk, Lucknow 226 003, India
Background Hepatitis B is mostly transmitted vertically, however a significant number of infections occur horizontally via various body fluids. Various studies have evaluated different body fluids (e.g. urine, feces, tears, saliva, semen, breast milk, pleural fluid etc.) to look for HBV DNA and HbsAg as a source of horizontal transmission. To the best of our knowledge, no study has looked into ascitic fluid for evidence of HBV DNA or HbsAg. Our novel study was aimed to know the positivity of ascitic fluid for HBV DNA in patients with decompensated cirrhosis and to correlate and compare the serum HBV DNA levels.
Methods Five mL of serum and 5 mL of ascitic fluid were collected with proper aseptic precautions, from decompensated HBV related cirrhosis patients, admitted at the Department of Medicine after informed consent, and were sent to the Virology lab of Microbiology for laboratory testing (HBV DNA by RT PCR).
Results Among 61 patients with HBV related decompensated cirrhosis, 28 (45%) had ascites. Twenty-one patients with mean age 46.6 +10.7 years and 18 (85.7%) male and with detectable HBV DNA in serum were included for the study. Four patients (21%) were found to be positive for HBV DNA in ascitic fluid. The patient with detectable HBV DNA in ascitic fluid has high serum viral load (>105 IU/mL) while none of the patients with low viral load (<105 IU/mL) had detectable HBV DNA in ascitic fluid.
Conclusions We conclude that 21% of ascitic fluid from decompensated chronic liver disease patients have detectable HBV DNA and an important source of horizontal transmission. Further studies with larger sample size are needed to to make any definite conclusion.
Disclosures – Authors have nothing to disclose.
Keywords Hepatitis B virus
256
Predictors of early mortality and readmission in alcoholic cirrhosis patients presenting with acute decompensation
Sushrut Ingawale1, Suprabhat Giri2, Sidharth Harindranath2, Mohit Jain1, Pranav Garg1, Aditya Kale2, Akash Shukla2
Correspondence – Sushrut Ingawale – drsushrutingawale@gmail.com
Departments of 1General Medicine, and 2Gastroenterology, Seth G S Medical College and K E M Hospital, Parel, Mumbai 400 012, India
Introduction Alcohol is the commonest etiology of cirrhosis in India and decompensation of liver cirrhosis with jaundice, ascites, variceal bleeding or hepatic is associated with increased morbidity and mortality. This study aims to analyze the outcome of patients with alcoholic cirrhosis presenting with acute decompensation (AD).
Methods All patients of alcoholic cirrhosis presenting with first decompensation were included in this study and prospectively followed up for 90-days. Patients presenting as ACLF were excluded.
Results A total of 167 patients were included in this study. Most common first decompensation was ascites (79.04%) followed by variceal bleeding (20.95%). Ninety-days mortality was 32.33%. Patients with ascites had higher 90-days mortality compared to variceal bleed without ascites (36.36% vs. 17.14%, p=0.041). Patients with mortality were significantly older (49.44±9.86 vs. 45.08±10.41 years, p=0.010), had longer duration of alcohol intake (20.57±8.52 vs. 16.41±7.90 years, p=0.003), had higher serum creatinine (2.29±2.43 vs. 1.36±0.81 mg/dL p=0.008), PT-INR (2.05±0.89 vs. 1.53±0.42, p=0.000), and lower serum sodium (126.74±7.88 vs. 132.19±6.35 mEq/dL, p=0.000), serum protein (6.23±0.80 vs. 6.50±0.66 mg/dL, p=0.036) and serum albumin (2.76±0.49 vs. 3.01±0.49 mg/dL, p=0.003). All prognostic scores including Child-Pugh score, MELD, MELD-Na and CLIF-C AD score were significantly higher in patients who had mortality (p=0.000 for all scores). On multivariate analysis, only CLIF-C AD was an independent predictor of 90-days mortality (OR 1.206, 95% CI 1.070, 1.360, p=0.002). On analysis of the area under the ROC curve (AUROC) for predictive scores (CTP, MELD, MELD-Na, CLIF-AD), CLIF-C AD score (AUROC 0.855, 95% CI 0.792, 0.919) was the best predictor of mortality.
Conclusion Alcoholic cirrhosis patients presenting with ascites as first decompensation have poorer prognosis compared to presentation with variceal bleeding. Among the prognostic scores, CLIF-C AD score was the best and the only independent predictor of mortality in patients with AD.
Keywords Alcoholic cirrhosis, CLIF-C AD score, Variceal bleed
257
Admission bilirubin impacts the outcome of patients with sepsis
Jophin John , A Senthil Vadivu, P Senthil Kumar, V Arul Selvan, T Ravi Shankar
Correspondence – Jophin John – jophin525@gmail.com
Department of Medical Gastroenterology, Coimbatore Medical College Hospital, No.1619 A, Trichy Road, Coimbatore 641 018, India
Introduction We investigated the prognostic implications of early hepatic dysfunction (serum bilirubin >1.2 mg/dL within 48 hours of admission) in patients with sepsis. The purpose of our study is to determine the independent association of serum bilirubin with mortality in sepsis.
Methods We conducted a prospective observational study in medical intensive care unit at the Coimbatore Medical College Hospital. We collected data from adult patients >18 years old meeting the criteria for sepsis based on sepsis-3 definition in MICU. We identified the highest serum bilirubin within first 48 hours of admission and divided patients based on the bilirubin levels into 2 groups, 0.1-1.2 mg/dL (normal) and above 1.2 mg/dL. We used multivariable logistic regression to test the independent association of various risk factors with mortality using admission bilirubin levels as our primary predictor.
Results Out of 110 patients who met criteria for sepsis, 67 patients had bilirubin ≤1.2 mg/dL and 43 had a bilirubin of >1.2 mg/dL. Out of these 43 patients, 35 patients had a bilirubin >2 mg/dL. Mortality was 11.9%, 50 %, and 57.1% in persons with a bilirubin ≤1.2 mg/dL, 1.21 to 2 mg/dL, and >2 mg/dL, respectively. Compared to those with a bilirubin ≤1.2 mg/dL, odds of mortality in patients were 8.7 (95% confidence interval 3.3-22.4) times higher in patients with bilirubin levels >1.2 mg/dL. Length of hospital stay is also significantly higher in hyperbilirubinemia group (>1.2 mg/dL) when compared to patients with normal bilirubin (≤1.2 mg/dL) with an odds ratio of 4.4 and 214atient214d214 interval 2.2-7.50.
Conclusion Our study concludes that an elevated serum bilirubin on admission is independently associated with an increased risk of mortality in sepsis. Also, hyperbilirubinemia in first 48 hours is a predictor for increased length of hospital stay in patients with sepsis.
Keywords Sepsis, Hyperbilirubinemia, Mortality
258
Unusual case of decompensated liver disease with liver abscess
Umar Kalbi , Premashish Kar
Correspondence – Umar Kalbi – umar209517w@gmail.com
Department of Gastroenterology, Max Hospital, Vaishali, Ghaziabad 201 019, India
Introduction Decompensated liver disease is a disease entity which is usually not associated with liver abscess. There are instances of liver abscess which is very rare. However we had a case of liver abscess with underlying chronic liver disease.
Methods He was admitted at Max Hospital, Vaishali, Ghaziabad with complaints of fever, malaise, chills, pain abdomen in the right upper quadrant x 1 week duration. He was subjected to certain investigations which showed raised total leukocyte count and positive amebic serology and ultrasound showing liver abscess in the right lobe of the liver. He was managed with IV antibioitcs, IV fluids and IV metronidazole 800 mg thrice daily injectables x 5 days and discharged on tab metronidazole for 10 days. He responded well to the treatment and fever settled down and appetite improved. He was later discharged on tablets.
Results Forty-year-old male nondiabetic non hypertensive, euthyroid with no cardiac ailment had chronic liver disease possibly related to chronic alcohol intake presented with fever and positive amebic serology. He was treated with IV Flagyl and responded well amebic liver abscess was proven biochemically and radiologically. Although the incidence of chronic liver disease and liver abscess is unusual. Very few cases have been reported in the past.
Conclusion I am presenting a case of chronic liver disease with liver abscess who was admitted at Max Hospital, Vaishali. Although chronic liver disease and liver abscess is an unusual occurrence. There are few instances of such cases in the literature. In decompensated liver disease cases since the hepatocytes are replaced with fibroblasts and there is no space left in the liver for parasitic infection, but in this case liver abscess was seen harbouring within the liver parenchyme. It gave me immense pleasure to present this case in front of experts and so that it can be published in the literature for future reference.
Keywords Decompensated liver disease, Liver abscess, Amebic serology
259
Peripheral blood monocyte phenotype in acute liver failure due to rat-killer poisoning
B Vijayalekshmi 1 , Anita Chaudary 1 , Savit Prabhu 1 , Anand Sharma 2 , K A Balasubramanian 1 . B Ashish Goel 2 , Uday Zachariah 2 , C E Eapen 2
Correspondence – C E Eapen – eapen@cmcvellore.ac.in
1Wellcome Trust Research Laboratory, Division of G.I Sciences, and 2Hepatology, Williams Building, Christian Medical College, Ida Scudder Road, Vellore 632 004, India
Introduction Rat killer poisoning leading to acute liver failure (ALF) is increasingly seen in our hospital. Monocytes or macrophages play a significant role in the pathophysiology of ALF. In this study, we aim to study the peripheral blood monocyte phenotype and serum immune markers in ALF-RP.
Methods Patients with ALF-RP and age matched healthy controls were prospectively recruited from July 2019 to March,2020. Immune cell phenotyping was done on BDFACS AriaTM III and analyzed on Flow Jo. Serum markers were measured using Duo set ELISA.
Results Seven patients with ALF-RP (Age: 27 [15 – 37] years, median, range, M:4, MELD score: 36 [21 – 40]) and 7 healthy volunteers were recruited. ALF-RP patients showed a significant increase in classical monocytes and decrease in intermediate and patrolling monocytes. Classical monocytes from ALF-RP showed significantly reduced expression for surface marker HLA-DR and increased expression of CD163, CD64 and CCR2 compared to healthy controls. The phenotype noted in ALF-RP of HLA-Drlow CD163hi monocytes suggest impaired functional activity. Significantly reduced NK cell frequencies and increased serum levels of sCD163 and sCD25, noted in these patients, suggest uncontrolled macrophage activation. CD64hi monocytes and significantly increased serum IgG circulating immune complex level seen in these patients, indicate immune complex mediated injury. We also noted increase in expression of CCR-2 on monocytes and CCL2 levels in circulation, suggesting an active CCR2-CCl2 axis mediated infiltration of monocytes into inflamed liver.
Conclusion Alteration noted in circulating monocyte phenotype and immune markers, suggest monocyte infiltration and macrophage activation in patients with ALF secondary to rat-killer intake.
Keywords Acute liver failure, Rat-Killer poisoning, Monocyte phenotype
260
Liver stiffness is reduced after renal transplantation: A prospective cohort study
Pankaj Kumar , Amit Goel
Correspondence – Amit Goel – agoel.ag@gmail.com
Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014, India
Background Liver stiffness (LS) may be falsely increased in patients on maintenance hemodialysis (MHD) due to volume overload. Change in LS was measured by transient elastography (TE), in MHD patients after successful renal transplantation and achievement of normal renal function.
Method Adults on ≥2 years of MHD, without risk factor for liver fibrosis or volume overload and planned for renal transplantation were prospectively recruited. LS was measured on two occasions, i. e, within 2 weeks prior to transplantation and after ≥6 weeks after successful transplantation. The participants with pre-transplant LS ≤7.0 Kpa and >7.0 Kpa were classified as ‘Normal-LS’ and ‘Elevated-LS’ respectively. Categorical and numerical data are expressed as ratio/proportions and mean (SD) respectively.
Results Paired data from 43 participants (males 42 [97.7%]; age 32 [11] years) were analyzed. The pre-transplant and post-transplant LS of the entire cohort, measured at 307 (198) days of interval, was 8.5 (7.3) Kpa and 6.7 (3.1) Kpa respectively. LS was elevated in 21 (49%) and normal in 22 (51%) participants. Among elevated LS group, 12 (57%) showed LS normalization after 312 (182) days of transplantation. Among 22 patients in normal-LS group, three (13.6%) showed LS elevation to >7.0 Kpa after 303 (217) days of transplantation. The mean change in LS among overall cohort, elevated LS group, and normal LS groups were -1.8 Kpa, -4.1 Kpa, and +0.2 Kpa respectively.
Conclusion LS in people on MHD may be falsely elevated which is likely to normalize after successful renal transplantation.
Keywords Hemodialysis, Maintenance hemodialysis, Chronic kidney disease, End-stage renal disease
261
Correlation of sarcopenia with minimal hepatic encephalopathy in patients with chronic liver disease
U S Umashankar , A Anand, Kani Sheikh Mohammed, A R Akilandeshwari, N Arun
Correspondence – Uma Shankar U S – us14umashankar@gmail.com
Department of Digestive Health and Diseases, Kilpauk Medical College, 822, Poonamallee High Road, Kilpauk, Chennai 600 010, India
Introduction Hepatic encephalopathy (HE) and sarcopenia is one of the most important complications of chronic liver disease (CLD) that is found in approximately 40% of cirrhotic patients. Minimal hepatic encephalopathy (MHE) is considered as a preclinical stage of HE. MHE and sarcopenia impair the health-related quality of life and prognosis in patients with liver cirrhosis; however, the relationship between MHE and sarcopenia remains unclear. The aim of this study was to investigate the prevalence of sarcopenia and its relationship with MHE in cirrhotic patients
Methods One hundred cirrhotic patients attending our OPD were enrolled after informed consent. Sarcopenia was diagnosed using Asian working group. Psoas muscle thickness was measured using plain CT at L3 level and hand grip strength was measured using handheld dynamometer. MHE was diagnosed using Psychometric hepatic encephalopathy score.
Results Out of 100 cirrhotic patient’s male and females were 76 and 24. Mean age was 42±8 years. Etiology of cirrhosis was alcohol (60%), NASH (12%), HBV (16%), HCV (8%) and cryptogenic (12%). Mean MELD score was 24± 6. The prevalence of Sarcopenia was 59%, mean L3 psoas muscle index was 2.8±0.8 cm2/m2; mean hand grip strength was 18±2.6 kg. Sarcopenia was more common among CTP-C (73%). Prevalence of MHE was 42% and among patients with sarcopenia was 80%. There was a positive correlation between severity of CLD with MHE and sarcopenia (r=0.8).
Conclusion Sarcopenia and MHE are prevalent among cirrhosis, Severity increases with the severity of liver disease. MHE is more common among patients with Sarcopenia. Sarcopenia predicts MHE among cirrhotic patients.
Keywords Sarcopenia, Hepatic encephalopathy, Cirrhosis of liver
262
Reticuloendothelial activation correlates with disease severity in liver injury due to rodenticidal poisoning
B Vijayalekshmi 1 , Vijay Alexander 2 , Anand Sharma 2 , K A Balasubramanian 1 , Ashish Goel 2 , Uday Zachariah 2 , C E Eapen 2
Correspondence – Ashish Goel – drashishgoel@cmcvellore.ac.in
1Wellcome Trust Research Laboratory, Division of G.I Sciences, 2Department of Hepatology, Williams Building, Christian Medical College, Ida Scudder Road, Vellore 632 004, India
Introduction We aimed to study reticuloendothelial activation and its association with disease severity in rodenticide induced liver injury.
Methods We retrospectively analyzed markers of macrophage activation (Serum ferritin, sCD163 [normal <0.98 μg/mL], sCD25 [normal: 1,555-10,800 pg/mL] and Macrophage Activation Syndrome criteria [MAS]) and endothelial activation (plasma Von-Willebrand factor, VWF (normal: 50-150IU/dL) in patients admitted due to rodenticide induced liver injury between April, 2018 – June, 2021. Patients were classified into acute liver injury (ALI, alteration in liver function tests with raised prothrombin time -INR>1.5) and acute liver failure (ALF, presence of hepatic encephalopathy) based on their worst clinical status during admission. Baseline RE activation parameters were correlated to MELD score and in-hospital outcome.
Results Sixty-seven patients (23 [12-64] years; median [range], M:25, ALI: 38, ALF: 29, MELD:28 [7-40]) were recruited. RE activation parameters were elevated in most patients with rodential poisoning- VWF (423.5;103-1106 IU/dL, >150: 95%), sCD163 (4.59;0.11-12.7 μg/mL, > 0.98: 88%), sCD25 (3050;5.6-17300pg/mL, >2000: 72%), ferritin (927;10.3-34807 ng/mL, > 500 ng/mL: 84%). MAS criteria was noted in 61% patients.
VWF and sCD163 were higher in patients with ALF (509.4, 140.8-1106.8 IU/dL and 5.54, 1.61-12.70 μg/mL), compared to ALI (319, 103.1-659.10 IU/dL and 3.13, 0.11-11.98 μg/mL). Serum sCD25 and ferritin were similar in both groups (data not shown).
Serum ferritin (R=0.29), sCD163 (R=0.6), sCD25 (R=0.56) and VWF (R=0.46) levels showed significant correlation with MELD score.
Death/liver transplant or discharge in terminal state was noted in 16 patients (ALI: 3, ALF: 13). Of the 40 patients (ALI:19, ALF: 21), who underwent low volume therapeutic plasma exchange (PLEX-LV), 30 were discharged in stable state (ALI: 17, ALF: 13). Baseline RE activation parameters and MELD score did not predict in-hospital outcome.
Conclusion RE activation, noted in most patients with rodenticidal hepatoxicity, corelates well with liver disease severity. PLEX-LV may overcome the potential influence of RE activation on in-hospital survival.
Keywords Reticuloendothelial activation, Rodenticidal hepatotoxicity, VWF, sCD163
263
Cirrhosis and relative adrenal insufficiency
Sachin Chakarvarti
Correspondence – Sachin Chakarvarti – liverhospitals@gmail.com
Department of Hepatology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Background Relative adrenal insufficiency is a common problem in patients who are critically. There is enough evidence that relative adrenalin insufficiency is common in cirrhosis especially in sick patients. We conducted this study to look for the incidence of relative adrenaline insufficiency and its effects on short-term mortality in non-critically ill patients and to see the short-term outcomes of it.
Methods Non critically ill cirrhotic patients who were admitted from January 2021- April 2021 were assessed for basal serum cortisol levels and delta cortisol levels after standard dose synacthen test (SDSST). RAI was defined as delta cortisol of <9 mcg/dL with basal cortisol <35 mcg/dL. Patients were followed up and outcomes of patients with RAI and those without RAI were assessed at 30 and 90 days.
Results Total 40 patients. males n=29 (702.5%); females n=11 (27.5%) with mean age 48.4 years. Child A n=7 (17.5%); Child B n= 17 (42.5%); Child C n= 16 (40%). Of the 40 patients n=16 (40%) patients had RAI. MELD scores were higher in patients with RAI (19.4 vs. 14.3, p=0.03). In hospital mortality at 30 and 90 days in patients with RAI and without RAI were 10%%, 25%%, 32.5%, vs. 7.5%, 27.5%, 30.0% respectively (p=0.52).
Conclusions RAI is found in almost 40% of cirrhotic patients and is more common in patients with higher MELD scores. There is no much difference in the mortality rates in patients with and without RAI. RAI cannot be taken as a independent predictor of increased mortality. The mortality rather depends on severity of underlying liver disease corelating with MELD scores of the patient.
Keywords Cirrhosis, RAI, Adrenal insufficiency
264
Liver function test abnormalities in corona virus disease 2019 patients in a tertiary hospital
Tarun Beeram , Gurunath Dhyandev Bhange, D Sivaramakrishna Naik, Saikrishna Katepally, Shravan Kumar Porika
Correspondence – Tarun Beeram – tarunbrm@gmail.com
Department of Medical Gastroenterology, Gandhi Medical College, Musheerabad, Padmarao Nagar, Secunderabad 500 003, India
Introduction Severe acute respiratory syndrome coronavirus 2 (SARS-CO-2) is responsible for the ongoing pandemic of corona virus disease 2019 (COVID-19) and has caused >120,000 deaths. Although it is primarily a respiratory virus, SARS-COV2 also has extrapulmonary manifestations. Involvement of the liver is one of them.
Abnormal liver function tests (LFTs) are reported frequently in hospitalized COVID-19 patients. We studied liver function test abnormalities at the time of hospital admission and during the hospital stay in 100 COVID-19 positive patients admitted in our hospital during the pandemic. Abnormal liver function tests are observed in 64 patients. Among these patients, 46% of admitted COVID-19 patients had elevated plasma aspartate aminotransferase (AST) and 35% had elevated alanine aminotransferase (ALT) levels on admission and during their hospital stay. Elevations of both AST and ALT are mostly below 4 times the upper reference limit and are associated with severe disease. Mild elevations in bilirubin and ALP is also seen in some patients. Severe liver synthetic dysfunction is not seen in any of them. Prolongation of prothrombin time is seen in few patients on ventilator but it was attributed to disseminated intravascular coagulation. Patients with pre-existing liver diseases were excluded from the study. Detailed drug history was also taken into consideration. Most of the LFT abnormalities returned to normal without any treatment. Few patients with raised LFT died but the death was not attributed to the abnormal LFTs.
Conclusion Our observations suggest that the prevalence of abnormal LFTs is high in COVID-19 patients, but the clinical relevance is limited and treatment is not required.
Keywords COVID-19, LFT abnormalities, COVID Designated Hospital
265
The outcome after hospital discharge in cirrhosis is not worsened with corona virus disease 2019 infection: A propensity score-matched analysis
Manas Vaishnav, Shalimar, Anshuman Elhence, Sagnik Biswas, Vishwajeet Singh1
Correspondence – Shalimar – drshalimar@gmail.com
Departments of Gastroenterology, and 1Biostatistics, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Patients with cirrhosis and corona virus disease 2019 (COVID-19) have high in-hospital mortality. The information on the outcome of cirrhosis patients in the post-hospitalization period is limited. We aimed to study the outcome of cirrhosis patients with COVID-19 after hospital discharge.
Methods The records of the cirrhosis patients discharged after COVID-19 were reviewed. Their data were compared with similar number of cirrhosis without COVID-19 after propensity score matching for age, sex, etiology of cirrhosis, and model for end-stage liver disease (MELD) score.
Results Cirrhosis patients with (n=92) or without (n=92) COVID-19 were included in 1:1 ratio. The mortality among COVID-19 (22;23.9%) and non-COVID-19 (19;20.7%) were comparable (HR 1.224; 95% CI 0.663-2.263, p=0.520), over a similar duration of follow-up (186 [86-271] vs. 183 [103-274]). Among COVID-19 patients, 45; 48.9% developed a new acute decompensation- increased ascites (40;43.5%), hepatic encephalopathy (20;21.7%), or variceal bleeding (8;8.7%) whereas 25 (27.2%) patients needed re-hospitalization. A proportion of participants continued to have either fatigue/ weakness (24/80; 30.0%), sleep disturbances (11/80; 13.7%), or joint pains (16/80; 20.0%). The most common causes of death in patients of both groups were end-stage liver disease: 16 (72.7%) vs. 9 (47.4%), followed by multiorgan dysfunction: 4 (18.2%) vs. 6 (31.6%), GI bleeding: 2 (9.1%) vs. 4 (21.0%), p=0.484. A lower albumin level, higher international normalized ratio, bilirubin, Child-Turcotte-Pugh, and MELD scores at discharge predicted mortality in the COVID-19 group.
Conclusion Short-term outcomes of patients with cirrhosis who survive the initial insult of COVID-19 are not different from patients without COVID-19, and survival is determined by the severity of liver disease at discharge.
Keywords Covid-19, Cirrhosis, Liver disease
266
Unusual etiology for obstructive jaundice in a case of cirrhosis
Susan George, Vijay Narayanan, Devika Madhu, Rushil Solanki, A Shanid, D Krishnadas
Correspondence – Susan George – susanmathmoola@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Portal hypertension is a frequent consequence of cirrhosis and may lead to dilated venous collaterals. Usually, varices due to portal hypertension develop in the lower esophagus, stomach, or rectum and rarely in other parts of the digestive tract. Extraintestinal ectopic varices are very rare.
Here we report a case of 61 year old male who is a known case of decompensated liver disease for 8 years who had history of 221atient221d221s twice in past when endoscopic variceal banding was done. He was not under regular follow-up for last 4 years now he had presented with 2 weeks abdominal distension and pain along with gradually progressing type of cholestatic jaundice. Hepatocellular carcinoma or cholangiocarcinoma were the main differentials initially. On evaluation he had acute kidney injury and spontaneous bacterial peritonitis which got corrected with volume expansion and antibiotics, but his liver function continued to worsen and developed cholangitis. Tumor markers were negative ultrasound abdomen revealed dilated biliary radical on left, MRI abdomen revealed a large dilated tortuous channel of recanalized umbilical vein joining left portal vein at hepatic hilum, circling left hepatic duct proximally, causing significant mass effect on left hepatic duct proximally and upstream dilatation of left hepatic duct and intra hepatic biliary radicals. Biliary drainage was done and patient is doing well.
Another interesting finding of vesical varices were also seen in the patient. Patient was asymptomatic for vesical collaterals unlike the usual presentations wherein gross hematuria might be noticed.
Keywords Obstructive jaundice, Vesical varices, Periportalcollaterals, Cirrhosis
267
Efficacy of saroglitazar versus vitamion E versus lifestyle interventions in NAFLD/NASH population – A 24-week, real world, single centre study
Bhaskar Bikash Pal
Correspondence – Bhaskar Bikash Pal – dr_bbpal@yahoo.com
Department of Gastroenterology, Peerless Hospital and B K Roy Research Institute,360, Panchasayar, Kolkata 700 094, India
Background and Aims Non-alcoholic fatty liver disease (NAFLD), an umbrella term and is a most common chronic liver disease worldwide. We tried to evaluate the effectiveness of 3 different strategies for management of NAFLD/ non-alcoholic steatohepatitis (NASH) in routine clinical practice.
Methods The NAFLD/NASH patients in routine clinical practice prescribed on Saroglitazar 4mg OD (n=68) or Vitamin E (n=80) or lifestyle interventions (n=35), were analyzed for changes in steatosis (CAP) and fibrosis (LSM) measured though Echosens Fibroscan at 24 weeks. The data at baseline and 24 weeks was analyzed and statistical significance was established using paired sample T- test.
Results In the study, Saroglitazar 4 mg OD group has shown significant improvements in both steatosis (CAP) (10.9%) and Fibrosis (LSM) (20.2 %) compared to Vitamin E 400 mg group where improvement in CAP (5.9%) only is significant and in lifestyle intervention group none of the evaluated parameters shown significant improvement, from baseline.
Conclusions The study shows Saroglitazar 4 mg OD as an effective treatment option over Vitamin E or lifestyle interventions for NAFLD/NASH. In future, more studies including clinical trials will be needed to establish the comparative effectiveness of these agents.
Table 1 Improvement in Primary End Points at 24 weeks
| Evaluated Therapy | Baseline (Mean + SD) | At 24 wks (Mean + SD) | % Change | p-value (Stat Sig.) | ||||
| CAP (dB/m) | LSM (Kpa) | CAP (dB/m) | LSM(Kpa) | CAP | LSM | CAP | LSM | |
| Lifestyle intervention (n=35) | 273.1 + 61.9 | 16.9 + 14.9 | 266.1 + 53.5 | 16.1 + 14.3 | -2.6 % | -4.9 % | >0.05 (NS) |
>0.05 (NS) |
| Vit E (n=80) | 305.3 + 44.6 | 7.3 + 4.5 | 287.1 + 37.5 | 6.7 + 6.5 | -5.9 % | -8.3% | <0.001 (HS) | >0.05 (NS) |
| Saroglitazar (n=68) | 312.8 + 43.3 | 12.3 + 7.9 | 278.8 + 49.3 | 9.8 + 5.6 | -10.9 % | -20.2 % | <0.001 (HS) | <0.001 (HS) |
Keywords NAFLD, Saroglitazar, VIT. E
268
A rare case of hepatomegaly – Hepatic sarcoidosis in a post splenectomy patient
Jithin John, Shimabara Dhal Mohapatra, Aditya Verma, N Premalatha, D Krishnadas
Correspondence – Jithin John – jithin4john@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Hepatic sarcoidosis is a rare granulomatous disease of unknown etiology with a prevalence of 1-40:100,000. About 20% to 40% of patients have hepatomegaly or elevated liver enzymes on presentation.
Case Scenario A 36-year-old female with history of splenectomy in 2019 for refractory ITP in 2019 with diabetes mellitus, dyslipidemia and abdominal obesity as comorbidities, was evaluated in august 2021 for dragging pain in the right hypochondrium. Ultrasound abdomen was suggestive of hepatomegaly with multiple hypoechoic areas. She was managed in the line of NAFLD. But in view of rapid increase in liver size on follow-up, she was referred to our center. MRI abdomen revealed hepatomegaly with a liver span of 24.5 cm with multiple hypointense lesions, throughout the liver, suggestive of granulomatous etiology. Main differentials considered were tuberculosis and fungal granulomas, in view of immunocompromised state. Tuberculosis work up was negative. Her ACE levels were elevated and hence CT chest was taken which revealed mediastinal lymphadenopathy. For confirmation of the diagnosis she underwent liver biopsy, which showed multiple non caseating granulomas in background of macro and micro vesicular steatosis. Fungal staining was negative. In the background of elevated ACE levels and mediastinal lymphadenopathy, a diagnosis of hepatic sarcoidosis was made. However as there was no cholestasis and chronic liver disease, no specific treatment was started. She is kept under close follow-up.
Conclusion This case bring light towards the rare case scenario of hepatic sarcoidosis and the need to work up isolated hepatomegaly even in the background of metabolic syndrome.
Keywords Hepatomegaly, Splenectomy, Non caseating granulomas, Hepatic sarcoidosis
269
Safety and efficacy of sofosbuvir and daclatasvir in children and adolescents with thalassemia with chronic hepatitis C virus infection
Riten Samadder
Correspondence – Riten Samadder – ritzkr.samadder91@gmail.com
Department of Hepatology, Institute of Post-Graduate Medical Education and Research and Seth Sukhlal Karnani Memorial Hospital, SSKM Hospital Road, Bhowanipore, Kolkata 700 020, India
Introduction Thalassemia patients are susceptible to hepatitis C virus (HCV) infection due to lifelong dependency on blood transfusion. This patient population is at risk of progression of fibrosis or development of cirrhosis owing to both iron overload and HCV infection. Currently there are no published data of treating hepatitis C in thalassemic children with direct acting antivirals. This study was performed to determine efficacy and safety of sofosbuvir and daclatasvir in thalssemic children and adolescent.
Methods This Interventional non-randomized open label study was carried out in Hepatology Department of IPGMER, Kolkata from April 2020 to June 2021. All consecutive non-cirrhotic thalassemic patients with hepatitis C infection with detectable HCV RNA within age group of 6-18 years was treated with combination therapy with sofosbuvir-daclatasvir (200 mg+30 mg for age 6-11 years (Group-A) and 400 mg+60 mg for 12-18 years (Group-B) depending upon exclusion criteria of study. Primary efficacy endpoint of study was sustained virological response 12 weeks after completion of therapy (SVR 12).
Results The study cohort comprised of treatment-naïve noncirrhotic 69 patient (Group-A – 44 Male- 27 Female -17, Group- B- 25 Male – 12 Female- 13). The mean age was 8.5 years and 13.5 years for Group-A and Group –B respectively. Mean of HCV RNA level in Group A was 1899250 IU/mL (Range 607-35788327 IU/mL) and Group-B was 11439548 IU/mL (Range 6330 – 207000000 IU/mL). SVR was achieved in 42 patients in Group-A out of 44 (95.4%) and all patients in Group-B (100%). The most commonly reported adverse effects were bitter taste leading to poor compliance. Among two patients who didn’t achieve SVR12 in Group-A, one patient required termination of therapy due to development of urticaria and other patient had Genotype 1b.
Conclusion Generic sofosbuvir-based treatment in non-cirrhotic, treatment-© thalassemic children and adolescents infected with HCV was highly effective, safe and well tolerated.
Keywords Sofosbuvir-Daclatasvir, Thalassemia, Hepatitis-C
270
Tuberculosis as a common cause of post-liver transplant ascites
T R Sowmya , Anand V Kulkarni, Mithun Sharma, Nagarajarao Padaki, Duvvur Nageshwar Reddy 1
Correspondence – Sowmya T R – sowmyaiyengar.18@gmail.com
Departments of Hepatology, and 1Gastroenterology, AIG Hospitals, No 136, Plot No 2/3/4/5 Survey, 1, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Background Refractory ascites due to cirrhosis is one of the common indications for liver transplant (LT). Ascites is expected to resolve within 2-4 weeks following orthotopic liver transplant as the reversal of hemodynamic changes occur by then. New-onset ascites after transplant has varied causes. Most common causes for the development of ascites after LT are hepatic inflow or outflow obstructions, hepatitis C, graft rejection, prolonged cold ischemia time. In addition, extrahepatic causes like infections, chronic kidney diseases, or heart failure can lead to ascites.
In this retrospective study, we aimed to assess the incidence and causes of ascites in post-transplant patients during the last year.
Results A total of 95 patients underwent living donor liver transplantation (LDLT) in our institution. Seven out of 95 patients developed ascites post-liver transplant. The mean age of patients was 46±18.98 years. Fifty-seven percent of patients were females. The indication of LDLT was decompensated cirrhosis in all the seven patients. Three underwent LDLT for alcohol-related liver disease, one each for non-alcoholic steatohepatitis, chronic hepatitis B, Budd-Chiari syndrome, and Wilson disease. The mean time to ascites onset was 2.9 months. All the patients had ascites prior to liver transplant out of which 5 (71%) had refractory ascites. Five (71%) of them had hepatorenal syndrome prior to transplant. Cold ischemia time was 98±19 min. Five patients were diagnosed with tubercular ascites, one had tacrolimus related proteinuria and ascites formation, and one more patient developed IgA nephropathy causing significant proteinuria and ascites. None of the patients had concomitant pulmonary tuberculosis. Rifampicin, levofloxacin, and ethambutol were initiated with gradual introduction of isoniazid over next 15 days.
Conclusion Although global data suggest vascular etiologies as common cause of persistent ascites post-transplant, in Indian scenario tuberculosis should always be considered as a differential diagnosis while evaluating post-transplant patients.
Keywords Post-liver transplant persistent ascites, Tuberculosis, LDLT
271
Sarcopenia – Risk factor for frequent hospitalization and short-term mortality in liver cirrhosis
T K Surakshith , Samarth Sharma, Piyush Ranjan, Samarjit Singh Ghuman, Anil Arora
Correspondence – Piyush Ranjan – piyushranjan70@gmail.com
Department of Gastroenetrology, Sir Gangaram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Sarcopenia in cirrhosis of liver is associated with poor prognosis and more significant in Indians who have lower baseline muscle mass. We aim to establish the prevalence of sarcopenia in Indian patients with cirrhosis and its impact on their morbidity and short-term mortality.
Methods This was a prospective study of 156 consecutive patients with liver cirrhosis. The cross-sectional area of the right psoas muscle was measured at the level of L3-vertebra and Psoas muscle index (PMI) (mm2/m2) was calculated. Sarcopenia was defined based on the CT study of patients with non-specific abdominal pain (controls), as PMI less than 295 mm2/m2 and 356 mm2/m2 for females and males respectively.
Results Seventy-four (47.4%) patients had sarcopenia. Sarcopenia was more common in males and with alcohol-related liver disease (ALD);70%. There was a negative correlation between the PMI and severity of liver disease as assessed by Child and MELD scores (r= - 0.591 and -0.465 respectively). Patients with encephalopathy, ascites and coagulopathy had a higher prevalence of sarcopenia (Table 1). Fifty-five patients who had sarcopenia required readmission within 6 months of follow-up as compared to those without sarcopenia (74.3% vs. 22%) (p=0.0001). 6-months mortality was higher among patients with sarcopenia (24.3% vs. 3.7%; p=0.002). MELD score and PMI were independently associated with higher mortality. PMI Cut off value for predicting mortality obtained was 305.9 mm2/m2 with a sensitivity of 76.2% and a false positivity of 22.2% (AUC was 0.805; 95% confidence interval:0.69–0.91, p=0.001).
| Table 1 | |||
| Characteristics | No Sarcopenia(82) | Sarcopenia (74) | p value |
| Ascites | 49 | 64 | 0.003 |
| Encephalopathy | 5 | 28 | 0.0001 |
| Readmission | 18 | 55 | 0.0001 |
| Death | 3 | 18 | 0.0002 |
Conclusion Sarcopenia is seen in almost 50% of cirrhotic patients. It is commoner in males, ALD and with advanced disease. Patients with sarcopenia have worse prognosis, require frequent hospitalization, and negatively impacts short term survival.
Keywords Sarcopenia, Cirrhosis, Encephalopathy, Ascites, MELD, Child-Pugh, Psoas Muscle Index
272
Utility of red cell distribution width to platelet ratio (RPR) in the assessment of fibrosis in patients with chronic liver diseases
Dongre Pavan Sai Kumar Rao1, Preetam Nath2, Shubhransu Patro1
Correspondence – Shubhransu Patro -spatro@kims.ac.in
Departments of 1General Medicine, and 2Gastroenterology and Hepatology, Kalinga Institute of Medical Sciences, Campus No:5, KIIT Road, Patia, Bhubaneswar 751 024, India
Introduction Early diagnosis of cirrhosis of the liver can prevent complications and improve survival. The available modalities for the non-invasive assessment of liver fibrosis like FibroScan are expensive, whereas different non-invasive scores to access liver function are cumbersome to calculate. Hence, this study aims to develop a simple and non-cumbersome score that can be easily calculated and can predict the outcome of cirrhosis with greater diagnostic accuracy.
Methods This was a single centre, cross-sectional study conducted from September 2019 to September 2021 in a tertiary care hospital of Eastern Odisha. The study subjects were patients with chronic hepatitis with etiologies like chronic hepatitis B, chronic hepatitis C, alcohol-related liver disease, non-alcoholic fatty liver disease, primry biliary cirrhosis, and autoimmune hepatitis, who underwent transient elastography (FibroScan) of the liver. All clinical and demographic data were collected and hematological parameters, as well as liver function tests, were performed. Non-invasive scores (APRI [AST to platelet ratio] and FIB-4 [Fibrosis-4 score]), RPR (Red cell distribution width to platelet ratio) were calculated and their accuracy to predict cirrhosis (F4 fibrosis in FibroScan) were assessed by receiver operating characteristic curve (ROC curve).
Results The Area under the ROC Curve (AUROC) of APRI, FIB4, RPR and RPR*AST for predicting advanced fibrosis were 0.817, 0.799, 0.706 and 0.811 respectively. Likewise, the AUROC of these scores for predicting cirrhosis were 0.889, 0.858, 0.797 and 0.898 respectively. The product of RPR and AST was superior to the FIB-4 and APRI for the prediction of cirrhosis. A value of RPR*AST above 4.8175 can predict cirrhosis with a sensitivity of 85.7% and specificity of 85.5%.
Conclusion RPR is an easily available and inexpensive index for the prediction of cirrhosis. However, the product of RPR and AST can predict cirrhosis in chronic liver disease patients with even greater accuracy.
Keywords Chronic liver diseases, Cirrhosis, Non-invasive 226atient226d226 scores, FibroScan
273
A rare association between acute hepatitis and hyperthyroidism – A case series
Santosh Hajare, Aditi Rao
Correspondence – Aditi Rao – docaditi289@gmail.com
Department of Gastroenterology, Jawaharlal Nehru Medical College, JNMC KLE University Campus, Nehru Nagar, Belagavi 590 010, India
Introduction The thyroid and liver are intertwined in many ways. liver dysfunction ranges from mild liver test abnormalities to deep jaundice and acute hepatitis in patients. We present a case series of three patients who were diagnosed with acute hepatitis secondary to hypothyroidism and their management.
Aim The objective of this clinical case series to highlight this unusual cause of acute hepatitis and the challenges faced in treatment.
Cases Case 1 was 32/male admitted with loose stools, generalized weakness, abdominal pain, heat intolerance and weight loss in the last 6 months. He showed deranged LFTs and was found to have hyperthyroidism. Case 2 was a 27/male presented with complaint of jaundice, itching and h/o weight loss. Blood work up showed deranged LFT and low TSH. Case 3 was a 20/male presented with jaundice, pain abdomen and weight loss since one month. He had deranged LFTs and on further work up was found to have hyperthyroidism.
Results and Conclusion We conclude that hyperthyroidism is a rare cause of acute hepatitis that must be kept in mind especially in young males. Hyperthyroidism in the setting of liver disease poses many challenges in management as standard anti-thyroid drugs are hepatotoxic. There is a need for further our understanding regarding the mechanism of hepatic dysfunction in thyroid disease to improve the treatment modalities.
Keywords Acute hepatitis, Liver dysfunction, Hyperthyroidism, Autoimmune thyroiditis
274
Spectrum and profile of bacterial and fungal infection in patients with cirrhosis in a tertiary care center: A prospective study
Vishav Dev Dadwal, Amrish Sahney, Jagdish Chander Vij
Correspondence – Vishav Dev Dadwal – amrish.sahney@gmail.com
Department of Gastroenterology, BLK-Max Superspeciality Hospital, New Rajinder Nagar.New Delhi 110 060, India
Introduction Cirrhosis is a state of immune dysfunction leading to increased predisposition for infections as compared to general population. Infection in these patients result in excessive production of cytokines leading to organ failure and death.
Aims This study aims to study prevalence of infections, types of infections in cirrhotic patients in a tertiary care center and also help us to identify various risk factors as well as predictors of infections and mortality in these patients.
Methods We studied 349 consecutive cirrhotic patients in age group of 18-75 years admitted in our hospital July 2018 to April 2020. Demographic, clinical data, laboratory parameters and outcome were noted. Infections were defined as per standard definitions. Univariate and multivariate logistic regressions were applied for identifying clinical and laboratory parameters associated with increased risk of infections and mortality.
Results Of 349 patients, 152 (43.55%) presented with infections at admission with 141 (92.76%) bacterial and 11 (7.24 %) fungal infections. Spectrum of infections at admission was urinary tract infection 63 (41.45%), spontaneous bacterial peritonitis 59 (38.82%), blood stream infection 19 (12.50%), pneumonia 12 (7.89%), soft tissue infection 11 (7.24%), ascitic tuberculosis 11 (7.24%), others 10 (12.5%). E. coli was most common isolated bacteria followed by enterococcus. Multi drug resistant infections were seen in one third of patients with ESBL (extended spectrum beta-lactamase inhibitor) being most common. Patients with infections had longer hospital stay (10.11±9.56) days as compared to non-infected patients (7.01±4.86) days. Clinical and biochemical variables which independently predicted infections were CTP, procalcitonin (PCT), prior infection, AKI in hospital and fever (p< 0.05). Variables which predicted mortality independently were CTP, lactate, infections, new organ failures in form of HE (grade 3 or 4) and acute kidney injury (p < 0.05).
Conclusion Infection is one of the most common cause of admission in cirrhotic patients. Infections are responsible for prolonged hospitalization and increased mortality in these patients.
Keywords Cirrhosis, CTP- Child-Turcotte-Pugh score, MDR- Multi drug resistant
275
Portal vein thrombosis in non-cirrhotic patients – A prospective study
Shadiya Chirakkal, Arul Selvan, T Ravishankar, Senthil Kumar, Senthil Vadivu
Correspondence – Shadiya Chirakkal – shadiya22389@gmail.com
Department of Medical Gastroenterology, Government Coimbatore Medical College Hospital, 1, Vignesha Garden, K G K Road, Kuniamuthur, Coimbatore 641 008, India
Background Portal and mesenteric venous thrombosis (PVT) is an uncommon disease with serious consequences if not discovered early in order to prevent complications such as variceal bleeding and intestinal ischemia. The objective of this study was to describe the clinical presentation and outcome of patients with PVT. The study was restricted to patients with PVT not caused by underlying liver cirrhosis.
Methods To analyse important clinical characteristics of this entity we performed a prospective study of 20 non-cirrhotic patients seen in our hospital over a period of two years.
Results The main clinical symptom was abdominal pain (13 patients, 86%), sometimes in combination with diarrhoea and vomiting (5 patients, 33%), nausea and anorexia (3 patients). Causative factors included prothrombotic states (9 patients, 45%) and/or local factors (5 patients, 25%). Complications must be expected from portal hypertension (15 patients, 75%), which was associated with variceal bleeding in 6 patients (30%). Bowel ischemia (5 patients, 25%) and bowel infarction (2 patients) were less frequent. Treatment consisted of immediate anticoagulation in almost all cases (18 patients, 90%), while invasive approaches were followed in selected patients. The prognosis of PVT was good in patients without a severe underlying disease (median follow-up 12 months).
Conclusions Early diagnosis and treatment by immediate anticoagulation are important in preventing the serious consequences of portal and mesenteric vein occlusion. Since in 18 patients (90%) of the non-cirrhotic cases in the present series causative factors were found which may have therapeutic implications, aetiological screening seems worthwhile in every case with PVT.
Keywords Portal vein thrombosis, Thrombophilia, Cirrhosis, Portal hypertension, Anticoagulation
276
Registry of young cirrhosis – The changing trends
Shadiya Chirakkal, Arul Selvan, T Ravishankar, Senthil Vadivu, Senthil Kumar
Correspondence – Shadiya Chirakkal – shadiya22389@gmail.com
Department of Medical Gastroenterology, Government Coimbatore Medical College Hospital, 1, Vignesha Garden, K G K Road, Kuniamuthur, Coimbatore 641 008, India
Introduction The etiology and incidence of cirrhosis in adults has been well studied. However, there is scant data in younger patients. The aim of this study was to determine causes of cirrhosis in patients ≤40 years old.
Methods In this prospective study, patients ≤40-year-old with a diagnosis of cirrhosis were studied and the etiological cause was worked up. Results: We identified 140 patients (49 female, 91 male). Among <18-year-old patients, Metabolic and genetic diseases were also seen more commonly in this age group (14.7%, 20/140). In contrast, Alcoholic hepatitis were the most common cause of cirrhosis in 18-40-year-old patients (40%, 56/120) followed by NASH, viral hepatitis and autoimmune (22%, 28/120 and 16%, 21/120, 15/120,13% respectively). Cryptogenic cirrhosis (overall 9%, 12/140). Developmental and metabolic disorders are the most common causes of cirrhosis in children (<18), while alcoholic hepatitis, NASH and viral hepatits are leading causes in adolescents and young adults (18-40) similar to adults.
Conclusion In contrast to Western studies, The early development of cirrhosis in our young patients may be related to multiple hepatic injuries induced by alcohol.
Keywords Portal vein thrombosis, Cirrhfosis, Portal hypertension, alcohol, NASH
277
Association of chronic hepatitis C infection related depression, anxiety, and neurocognitive performance achieving SVR-12 with direct-acting antivirals: A prospective cohort study
Harmanpreet Kaur1, Radha K Dhiman2, Anand V Kulkarni1, Madhumita Premkumar1, Virendra Singh1, Ajay Kumar Duseja1, Sandeep Grover3, Gagandeep Singh Grover4, Akash Roy5, Nipun Verma1, Arka De1, Sunil Taneja1, Rohit Mehtani1, Saurabh Mishra1, Harpreet Kaur1
Correspondence – Madhumita Premkumar – drmadhumitap@gmail.com
Departments of 1Hepatology, 3Psychiatry, Postgraduate Institute of Medical Education and Research. Sector 12, Chandigarh 160 012. India, 2Director, 5Department of Hepatology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raebareli Road, Lucknow 226 014, India, 4Department of Health and Family Welfare State Programme Officer HCV, Room No. 506, Pariwar Kalyan Bhawan, Punjab Sector 34-A, Chandigarh 160 022, India
Background Chronic hepatitis C virus (HCV) infection is associated with neuropsychiatric changes. In addition, patients with cirrhosis may develop overt or minimal hepatic encephalopathy. With direct-acting antiviral agents (DAAs), the high sustained virological response (SVR) rate may improve the neuropsychiatric manifestations and quality of life (QoL) outcomes.
Methods Consecutive patients (with and without cirrhosis, all genders, aged 18-65 years) with viremic hepatitis C were assessed at enrolment and at 12 weeks after therapy completion for mood (Beck’s Depression Inventory [BDI]), anxiety (generalized anxiety disorder [GAD-7]), cognition (Montreal Cognitive Assessment [MoCA]), QoL (SF-36 ver.2) and computer based-tests for number connection (NCT), visual memory, digit span, vigilance, Stroop test and reaction times. The neurocognitive battery was custom designed using Psychology Experiment Building Language version 2.1.
Results We recruited 385 viremic chronic HCV patients (76.1% male, 21.0% cirrhotic, mean age 39.4 ± 14.2 years, 59.3% genotype 3, mean HCV RNA load 5.8 log). Overall SVR-12 rates were 90.6%, with cure rates 87.6% and 91.4% in patients with and without cirrhosis, respectively. Patients who achieved SVR-12 had mean percentage reduction in BDI (11.3%, p=0.000), GAD (8.6%, p=0.001), vigilance (8.7%, p=0.113) and Stroop test (58.4%, p=0.001), with improved NCT (1.7%, p=0.001) visual memory (13.7%, p=0.001) and digit span (23.8%, p=0.002). On multivariate logistic regression, adherence (OR,17.5 [95% CI 2.80 –110.50], p=0.000), high ALT (OR, 1.02 [95% CI 1.00 – 1.05]), BDI score (OR,1.73 [95%CI 1.42 – 3.26] p=0.039) predicted SVR-12. Age, gender, and presence of cirrhosis did not predict SVR-12. Achievement of SVR-12 was associated with increased recalled visual memory targets ≥ 5.5 (AUC 0.708; sensitivity 62.5%, specificity 63%, p=0.000), and %correct Stroop test responses >26.6% (AUC 0.918, sensitivity 94.4% specificity 80.4%, p=0.000).
Interpretation This prospective cohort of patients with chronic HCV showed significant improvement of psychological and cognitive scores after treatment with DAAs.
Keywords Chronic hepatitis, Alanine aminotransferase, Sustained virologic response
278
Hypereosinophilic syndrome presenting as hepatitis: A case report
Nuzil Moopan
Correspondence – Nuzil Moopan – iamnuzil@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Idiopathic hypereosinophilic syndrome (HES) represents a heterogeneous group of disorders with the common features of prolonged eosinophilia of more than 1,500 eosinophils per microliter (μL) of peripheral blood for at least 6 months, with signs or symptoms of organ system dysfunction, without detectable cause. Chronic hepatitis associated with hypereosinophilia has been very rarely reported worldwide. We report a case of chronic hepatitis in a case of hypereosinophilic syndrome which responded to treatment with oral steroids.
Case Summary Forty-one year old male, painter, with no prior comorbidities or addictions, presented with fatigue and yellowish discolouration of eyes. On evaluation, he had total bilirubin/direct bilirubin – 6.5/3.6, SGOT/SGPT – 281/417, ALP – 296 (124) and absolute eosinophil count of 9960/cmm. Bone marrow aspiration and trephine biopsy showed marked increase in eosinophil precursors. Percutaneous liver biopsy showed chronic active hepatitis with mild hepatocanalicular cholestasis, mild to moderate mixed inflammation comprising of abundant eosinophils with few neutrophils and focal mild periportal fibrosis. With this, he was diagnosed to have chronic active hepatitis due to hepatic involvement in hypereosinophilic syndrome and was started on oral prednisolone with which his icterus resolved and LFT normalised.
Discussion In this case report, the patient presented with clinical manifestations of active hepatitis with elevated liver enzymes and hyperbilirubinemia along with peripheral and marrow hypereosinophilia. This entity of liver involvement in HES has been mainly described at autopsy and very rarely at a patient’s clinical presentation. The patient responded to treatment with oral prednisolone and is on follow-up with tapering dose of oral steroids.
Conclusion In patients with hypereosinophilic syndrome, liver involvement can occur in the form of chronic hepatitis which responds to treatment with steroids.
Keywords Hypereosinophilic syndrome, Hepatitis, HES
279
Assessment of liver stiffness using transient elastography in patients with obstructive sleep apnea: An observational study
Ashwin Parchani1, Rohit Gupta2, Ravi Kant1, Ravi Gupta3, Lokesh Saini4
Correspondence – Ashwin Parchani – ashwinparchani@gmail.com
Department of 1Internal Medicine, 2Gastroenterology, 3Psychiatry and Sleep medicine, 4Pulmonary Medicine, All India Institute of Medical Sciences, Virbhadra Road Shivaji Nagar, Sturida Colony, Rishikesh 249 203, India
Introduction Recent clinical data have shown that obstructive sleep apnea (OSA), through its hypoxia related consequences 3s to tissue hypoxia , thereby resulting in oxidative stress, inflammation, and sympathetic system activation, and could therefore be an independent risk factor for non-alcoholic fatty liver disease. The primary aim of this observational study is to study the effect of obstructive sleep apnoea on the degree of liver stiffness, estimated using transient elastography, a novel technique to assess liver fibrosis.
Methods The study was conducted on outpatients and inpatients of a tertiary care center who are polysomnography (PSG) proven OSA patients and meet the eligibility criteria. Patients were enrolled to undergo transient elastography (fibroscan) and the following investigations – complete hemogram, liver function tests, serum lipid profile, serum fasting insulin and fasting blood sugar levels. The polysomnography, fibroscan and laboratory data was tabulated and analyzed.
Results A total of 36 participants were enrolled. 4 (11.1%) participants had mild OSA, 11 (30.6%) moderate OSA and 21 (58.3%) of the participants had severe OSA. The prevalence of liver steatosis was assessed to be 83.3% (30 patients) while hepatic fibrosis was noted in 11.2% (4 patients). Oxygen desaturation events, oxygen desaturation index, apnea-hypopnea index and percentage of sleep spent below 90% oxygen saturation (T90) were significant predictors of hepatic fibrosis.
Conclusion Patients with OSA have an increased risk for development of hepatic steatosis and fibrosis. The various PSG parameters can be helpful in predicting the presence of underlying liver disease and aid in screening.
Keywords Liver stiffness, Non-alcoholic fatty liver disease, Obstructive sleep apnea
280
Unusual site of metastasis in hepatocellular carcinoma
Hima Bindu Panta, Jagadeeshwara Reddy, B M Raghu, N Kayal Vizhi, Amit Yelsingakar, Anupama Nagar, Naresh Bhat
Correspondence – Hima Bindu Panta – bindu60579@gmail.com
Department of Gastroenterology, Aster CMI Hospital, #43/2, New Airport Road, NH-7, Outer Ring Road, Sahakar Nagar, Bengaluru 560 092, India
Introduction The common sites of metastasis in hepatocellular carcinoma (HCC) are lung, bone and peritoneum. Rare instances of metastasis to unusual sites like nail bed, orbit and retroperitoneum have been reported as well. We report a case of metastasis of HCC in the rectovesical pouch.
Case Report A 60-year-old gentleman with chronic hepatitis B related cirrhosis on regular treatment and follow-up was diagnosed with 3.8 cm lesion in segment V consistent with HCC in 2018. He has had one session of radiofrequency ablation in 2018 and a session of transarterial chemoembolization in 2019. Subsequently, serial imaging with multiphasic magnetic resonance imaging (MRI) did not reveal any recurrence of liver lesions. Over the last 6 months, there was a gradual increase in serum alpha-fetoprotein (AFP) levels. The last contrast enhanced CT abdomen done 2 weeks prior to this presentation revealed a rectovesical lesion 18 mm x 16 mm which was enhancing in the arterial phase. Transrectal endoscopic ultrasound (EUS) done revealed a hypoechoic lesion ~ 18 x14 mm in the rectovesical pouch. EUS guided fine-needle aspiration cytology was done which was suggestive of hepatocellular carcinoma.
Conclusion Rectovesical pouch is an unusual site of metastasis in HCC. Metastatic HCC should be considered in a patient with rising AFP levels with no liver lesions in a patient treated for HCC.
Keywords Rare site of 232atient232d232, HCC, Radiological stable disease
281
Experience with low volume plasma exchange via centrifugal technique using peripheral access in patients with liver diseases
Alok Bansal1, Snehil Kumar2, E Santosh Kumar1, S Gnanadeepam1, Ashish Goel1, Uday Zachariah1, Sukesh Nair2, Dolly Daniel2, C E Eapen1
Correspondence – C E Eapen – eapen@cmcvellore.ac.in
Departments of 1Gastroenterology, 2Transfusion Medicine, Willium’s Building, Christian Medical College Hospital, Vellore 632 004, India
Introduction Plasma exchange (PLEX) is an emerging therapeutic option for wide range of liver diseases. Central venous access requires technical expertise and can be complicated by local bleed and infection. Peripheral venous access may overcome these issues.
Aim To compare the safety and efficacy of low volume PLEX via centrifugal technique using peripheral versus central access in liver disease patients.
Methods Consecutive patients with liver diseases who underwent centrifugal PLEX between November 2019 to June 2021 were retrospectively studied. Patients with accessible peripheral veins underwent peripheral PLEX (pPLEX) while the rest underwent central PLEX (cPLEX) via femoral vein. Low volume PLEX (50% of total plasma volume) with 1:1 replacement with FFP was done and 3 sessions were targeted. Continuous variables were expressed in median (range).
Results Forty (67%) (age 41 [16-71], males 26 [70%]) and 20 (33%) (age 37 [19-63], males 13 [65%]) patients underwent cPLEX and pPLEX respectively. Indication for cPLEX/pPLEX were ACLF (20/9), ALF (7/2), ALI (5/2), SAHF (3/2), Cholestasis (3/4) and DCLD (2/1) with main etiologies alcohol, toxin and drugs. MELD score cPLEX 26.5 (12-41)/pPLEX 26.5 (12-38), p=0.4. pPLEX access was 18 Guage (n=18/17 for inlet/return). Three patients required access change from pPLEX to cPLEX. Targeted sessions were completed in 35 (87%) cPLEX and 15 (75%) pPLEX. Number of plex sessions, flow rate and procedure time for cPLEX/pPLEX was 3 (1-5)/3 (1-5), 35 (15-40)/22 (10-35) mL/min, p<0.001 and 75 (31-180)/90 (30-270) min. Volume processed, volume removed and plasma removal efficiency for cPLEX/pPLEX was 2275 (853-4500)/2076 (600-6000) mL, 1335 (404-1857)/1171 (495-1760) mL and 55.4 (23.6-94)/51.8 (20.6-99.7)%, p=0.3. Complications included sepsis (1), access site non-major bleed (1) in cPLEX and access site phlebitis (2), minor transfusion reaction (1) in pPLEX. Survival at discharge, 1, 3 and 6 months cPLEX/pPLEX was 34 (85%)/17 (85%), 31 (77.5%)/15 (75%), 27 (67.5%)/13 (65%) and 24 (60%)/13( 65%).
Conclusion Low volume centrifugal PLEX by peripheral venous access is feasible and appears equally efficient as central access in a spectrum of liver disease patients at significantly lower flow rates for the peripheral route.
Keywords Centrifugal plasma exchange, Plasma exchange, Liver disease, Liver failure syndromes
282
Hepatic visceral larva migrans
Saurabh Gaur, Mukesh Kalla, Ramesh Roop Rai, Aman Manocha1, Pankaj Shrimal, Alok Verma2, Sumit Patter
Correspondence – Saurabh gaur – saurabhgaur55@gmail.com
Departments of Gastroentrology, 1Radiologist, and 2Anesthetist, S.R Kalla Memorial Gastro and General Hospital, 78-79, Dhuleshwar Gdn, Panch Batti, C Scheme, Jaipur 302 001. India
Introduction Visceral larva migrans (VLM) is a systemic manifestation of migration of second stage larvae of nematodes through the tissue of human viscera. The liver is the most common organ to be involved due to its portal venous blood supply. Presenting a case of 16 -year-old boy from a rural background presented with intermittent abdominal pain, malaise, loss of appetite and restlessness for 3 months.
Method Blood investigation revealed microcytic hypochromic anemia and eosinophilia (blood eosinophil count being 27%, AEC-1610 cu/mm). Serum alkaline phosphatase raised (885 IU/L), other liver function parameters normal. Coagulation profiles were normal. Serum α-fetoprotein came normal (<0.5 IU/ mL).USG abdomen showed ill-defined hypoechoic lesions in right lobe of liver. Contrast-enhanced CT (CECT) scan of the abdomen showed large hypodense SOL with multiloculated cystic areas (5.7 x 6.4 x 7.2 cms) in segment 6/7 of liver. A provisional diagnosis of hepatic lesions associated with parasitic infestation was made. The stool examination for entamoeba histolytica, giardia and ascaris ova and cyst were negative along with their serology. The values of serum IgE levels were also high (1860 IU/L). USG guided FNAC of the lesion with Giemsa stains showed cellular smears comprising mixed inflammatory cells predominantly consisting of eosinophils with few degenerated cells were also seen. No parasites were identified in the smears. The findings were suggestive of eosinophilic abscess, thus with correlating radiological findings, a final diagnosis of visceral larva migrans was made.
Results The patient was empirically given 400 MG twice daily albendazole for 5 days. The patient was totally relieved of his symptoms and complete resolution of hepatic sol seen.
Conclusion We can say in developing countries patients with peripheral eosinophilia with hepatic Sol, one must keep the differential diagnosis of parasite infestation.
Keywords Visceral larva migrans
283
Change in quality of life and health promoting behaviors in patients with liver cirrhosis in corona virus disease 2019 pandemic with tele-consultation and counselling
Shankar Bhanushal1, Aabha Nagral1, Ritika Aggarwal2, Ojas Unavane3, Upali Anand3, Satyendra Badhe1, Deepakkumar Gupta1, Amey Sonavane1, Rahul Deotale1, Ronak Tate1, Maninder Setia4
Correspondence – Shankar Bhanushal – shankru07@gmail.com
1Department of Gastroenterology and Hepatology, Apollo Hospitals, Navi Mumbai 400 614, India, 2Department of Psychology, Jaslok Hospital, 15, Pedder Road, IT Colony, Tardeo, Mumbai 400 026, India, 3Department of Medicine, Seth G S Medical College and K E M Hospital, Parel, Mumbai 400 012, India, 4Department of Epidemology, M G M, HIS Sector 1, Kamothe, Navi Mumbai 410 209, India
Introduction In corona virus disease 2019 (COVID-19) pandemic, worsening of quality of life (QOL) in all patients is expected. Tele-consultation and online counselling became popular as patients were reluctant to visit hospitals.
Methods In a prospective single arm interventional study, QOL of 75 patients with cirrhosis was evaluated at the end of first wave of the pandemic through the SF36 and health promoting lifestyle (HPLP-II) questionnaires. Demographics, etiology and MELD scores were documented. Patients were trained in tele-consultation and were counselled about the disease, nutrition, exercise, and psychological aspects. In second wave of COVID-19 pandemic, they were re-evaluated with same questionnaires and MELD scores, pre and post intervention scores were compared.
Results Sixty-six patients (mean MELD score of 12.11+4.24) competing the study were analysed and showed significant improvement in the nutrition domain (p0.038) in HPLP-II and in domains of role limitation due to physical health (p0.006), emotional problems (p0.01), emotional wellbeing (p0.048) and general health in SF36. In those with worsening MELD scores (n=44), there was improvement in role limitation due to emotional problems and general health in SF36 with no significant change in health promoting behaviours (HPLP-II) while in those with improved/static MELD scores (n=22), improvement was seen in majority of the domains.
Treatable cause of cirrhosis (n=46) did not show any change in health promoting behaviors (HPLP-II) while in SF36 showed improvement in role limitation due to physical health, emotional problems and general health.
Those with non-treatable causes (n=20) showed improvement in role limitation in physical activity, nutrition and overall health promotion (HPLP-II) and physical functioning, role limitation due to physical health (SF36).
Conclusion Tele-consultation and counselling significantly improved the QOL in multiple domains in patients of liver cirrhosis during the second wave of COVID-19 pandemic in Mumbai in spite of worsening of MELD scores and having an untreatable etiology of liver cirrhosis.
Keywords Quality of life, Liver cirrhosis, COVID-19
284
NAFLD versus MAFLD: South Asian NAFLD patients reject the name change to MAFLD
Shivaram Singh1, Prajna Anirvan1, Amna Subhan Butt2, Ananta Shrestha3, Anuradha Supun Dassanayake4, Bashir Ahmad Shaikh5, Mamun Al Mahtab6
Correspondence – Shivaram Singh – scb_gastro_dept@hotmail.com
1Department. of Gastroenterology, S C B Medical College, Medical Road, Mangalabag, Cuttack 753 007, India, and 2Department. of Medicine, Aga Khan University Hospital, National Stadium Road, Karachi 74800, Pakistan, 3Department of Hepatology, Liver Foundation, Nepal Sitapaila Marg, Kathmandu 44600, Nepal, 4Faculty of Medicine, Colombo North Centre for Liver Disease, University of Kelaniya, Kelaniya, Colombo 11600, Sri Lanka, 5Department of Medicine, Chandka Medical College Hospital, Shaheed Mohtarma Benazir Bhutto Medical University (SMBBMU), University Road, Larkana 77150, Pakistan, 6Department of Hepatology, Bangabandhu Sheikh Mujib Medical University, Mymensing Road, Dhaka 1000, Bangladesh
Aim There have been strident attempts to change the name of non-alcoholic fatty liver disease (NAFLD) to MAFLD (metabolic associated fatty liver disease). The reasons proffered in favor of NAFLD included the presumed ill-founded demand by patient groups insisting on the name change. Besides, this assertion is not based on any evidence in its favor. South Asia is home to a fifth of the world’s population, besides being the capital of NAFLD. Therefore, we decided to conduct a survey among South Asian NAFLD patients to understand their attitudes and perspectives especially with regard to the change in name from NAFLD to MAFLD.
Methods This survey was conducted at multiple centres across South Asia between January 2021 and June 2021. A brief non validated questionnaire was developed and responses were obtained and analyzed.
Results Two hundred and eighteen NAFLD patients underwent the surveyed; 80.3% of the patients weren’t aware of the term ‘NAFLD’ before first diagnosis. 74.3% patients admitted to being questioned about alcohol intake at the time of initial diagnosis. Surprisingly, only 24.1% of female patients were questioned about this. Further, after being diagnosed as NAFLD, 92.1% patients were never grilled again about alcohol consumption. While 86.3% patients found the term ‘NAFLD’ consoling, 83% patients did not feel that ‘Non’ in NAFLD trivialised their problem (Table 1). Only 6.9% patients were scared of developing cardiovascular disease.
Conclusion Our study on South Asian NAFLD patients showed that the term ‘NAFLD’ destigmatizes patients of the taboo associated with alcohol use; repeated questioning about alcohol intake is embarrassing to patients in South Asia. Further, the term ‘NAFLD’ was perceived to be consoling to most patients and majority did not feel it trivialised their problem. The proponents of MAFLD need to understand these overwhelming sentiments in favour of NAFLD.
Keywords Steatohepatitis, NASH, Steatohepatitis, NASH, Nomenclature, South Asia, patients’ sentiments
285
A rare case of metastatic liver neuroendocrine tumors presenting with hepatic encephalopathy
M Indrakeela Girish, Amol S Dhawale, Debabrata Banerjee
Correspondence – Amol S Dahale – amolsd1986@gmail.com
Department of Medical Gastroenterology, D Y Patil Medical College and Research Center, Pune 411 018, India
Neuroendocrine tumors (NETs) of the liver represent a rare entity. Within this group of uncommon diseases, primary hepatic NET (PHNET) only represented 0.3% of all NETs. We report an unusual presentation of metastatic hepatic neuroendocrine tumor with hepatic encephalopathy .A 26-year-old male patient with presenting complaints c/o altered behavior and vomiting since 2 months. Also presents with Slow mentation with slow speech and response, altered sleep pattern. No weakness, abnormal movement. No constipation, melena, jaundice, abdominal distension. Similar episodes two times in last two months lasting for a week with partial recovery. Patient underwent investigations which showed elevated serum chromogranin levels 4760 ng/mL and USG abdomen: Multiple anechoic cysts in liver, PV-normal, spleen normal, kidney and pancreas –Normal. EEG s/o generalized background slowing with delta activi ty s/o encephalopathy. UGIE: multiple extrinsic impressions in distal body and antrum. No varices, PG. No e/o GOO.CE MRI brain showed no abnormality. CECT abdomen showed multiple cystic lesions with solid components inside the one of the cystic lesion n with 2*2 cm lesion at the ileum going into mesentery, compressed by enlarged liver. Ultrasound guided biopsy was done s/o metastatic NET. Patient was started on injection octreotide and symptomatic treatment .Initially patient showed improvement but alter after 1 week patient succumb. In conclusion patients with metastatic hepatic NET presenting with hepatic encephalopathy is very rare and treating patients is challenging. Accurate preoperative diagnosis of primary with metastatic NET remained an important yet difficult feature in the management of this rare tumor.
Keywords Metastatic NET, Hepatic encephalopathy, Octreotide, EEG
286
Combined arterial and venous thrombosis in a patient with hyperhomocystinemia and homozygous prothrombin gene mutation G20210A presented with Budd-Chiari syndrome – A case report
D Sivaramakrishna Naik, Gurunath D Bhange, Tarun Beeram, Prafulla Kumar Singh, Saikrishna Katepally, P Shravan Kumar
Correspondence – Sivaramakrishna D – sivaram.amc@gmail.com
Department of Medical Gastroenterology, Gandhi Medical College, Musheerabad, Padmarao Nagar, Secunderabad 500 003, India
Introduction Thrombophilic disorders are commonly detected in patients with Budd-Chiari syndrome (BCS). BCS with multiple thrombophilic disorders in a same patient may be present up to 20% to 25% of patients. We report here a case of BCS with multiple arterial and venous thrombotic episodes.
Case A 35-year-old female presented to us in October 2021 with 1 month history of pain abdomen followed by mild abdominal distension. Previously in 2017 she had severe pain in left flank for one week. Also, she had left lower limb pain in February 2018, diagnosed as deep venous thrombosis involving left femoral and popliteal vein, received treatment for 6 months (? anticoagulation). Thrombophilia workup was not done previously. In our admission CBP revealed hemoglobin 11.8g/dL, leukocytes 5890/mm3, and platelets 89000/mm3. Liver function tests were within normal limits. Contrast enhanced computed tomography (CECT) showed non-visualization of all the three hepatic veins and compressed intrahepatic IVC with caudate lobe hypertrophy, a spleen of 10.5 cm and very minimal ascites. Also, in CECT, left kidney was contracted and chronic thrombus seen in left renal artery. Upper gastrointestinal endoscopy showed no evidence of esophageal varices.
The patient’s thrombophilia workup is positive for homozygous mutation in the prothrombin G20210A gene. Analysis done with allele-specific polymerase chain reaction. Also, her serum homocysteine level was 42.26 μmol/L (3.7 – 13.9 μmol/L). genetic analysis for factor V mutation and Janus kinase -2 V617F were negative. protein C, protein S, antithrombin III activities were within normal limits.
Patient has been started on anticoagulation and advised to follow up after one week. Response for treatment is awaited.
Conclusion BCS with prothrombin gene mutation seen in 5% to 7% cases in west. In India one case report from Mumbai with heterozygous mutation. Ours is the first case in India with prothrombin gene homozygous mutation in BCS.
Keywords Budd-Chiari syndrome, Prothrombin gene G20210A homozygous mutation, Hyperhomocysteinemia
287
Palmitate induced hepatocytes inflammation is accompanied with decline in levels of NAD+and its precursors and overexpression of SIRT2 alleviates lipoinflammation
Savera Aggarwal 1 , Vipin Yadav 1 , Rakhi Maiwall 2 , Jaswinder Maeas 1 , Archana Rastogi 3 , Viniyendra Pamecha 4 , Shiv Sarin 2 , Nirupma Trehanpati 1 , Gayatri Ramakrishna 1
Correspondence – Gayatri Ramakrishna – rgayatri@ilbs.in
Department of 1Molecular and Cellular Medicine, 2Hepatology, 3Histopathology, 4Hepato-Pancreato-Biliary and Liver Transplant Surgery, Institute of Liver and Biliary Sciences, D1 Vasant Kunj, New Delhi 110 070, India
Introduction The fundamental hallmark of non-alcoholic fatty liver disease is metabolic dysregulation, which entails an inflammatory response. Lipid-induced hepatoctyte inflammation can then cause an immune-mediated inflammatory cascade to go into overdrive, exacerbating fatty liver disease. The mechanisms involved in hepatocyte inflammation mitigation are poorly known. The involvement of silent information regulator 2 (SIRT2), a NAD+-dependent deacetylase and important metabolic regulator, in palmitate (PA)-induced lipoinflammation was investigated.
Method Immortalized hepatocytes and hepatoma cells were treated with palmitate and markers of inflammation were monitored by real time qPCR for IL6, IL8, TNF-α, IL1α and IL1β.NAD levels and that of its precursors such as, nicotinamide riboside (NR) and nicotinamide (NAM) were checked both in vitro and the patient plasma samples using LC-MS spectroscopy technique. Also, levels of SIRT2 were found to be reduced in presence of lipid as well as in fatty liver patient samples.
Results Hepatocytes treated with palmitate (400 μM) showed significantly higher levels of inflammatory markers IL6 (p<0.0001), IL8 (p<0.0004), IL1α (p<0.0001), IL1 β (p<0.003) but not TNFα. The mRNA levels of NAMPT, a rate limiting enzyme in NAD synthesis, were decreased in both hepatocytes cell lines (IHH and HepG2). NR and NAD levels were found to be reduced in plasma of non-alcoholic fatty liver patients. Immunoblot revealed significantly low levels of SIRT2 in palmitate treated hepatocytes (p<0.04). Decline in levels of SIRT2 was also seen in biopsy of fatty liver subjects with raised activity score (NAS >5) and increased ALT levels (>40). Overexpression of SIRT2 or its activation by NAD+ precursor nicotinamide riboside decreased lipid induced hepatocyte inflammation (Fig.1).
Conclusion Decline in levels of NAD+ and SIRT2 is accompanied with lipoinflammation in hepatocytes. Elevating NAD+ levels by nicotinamide riboside appears promising strategy to dampen the inflamed hepatocyte.
Keywords NAFLD, NAD+, Sirtuins, Metabolomics
288
Comparative study of ALBI score with CTP, MELD Na, AARC score in patients of ACLF
Manjinder Singh
Correspondence – Manjinder Singh – mani23111985@gmail.com
Department of Gastroenterology, Indira Gandhi Institute of Medical Sciences, Bailey Road, Sheikhpura, Patna 800 014, India
Objectives To compare ALBI score with Child-Pugh score, MELD Na score and AARC score in patients of ACLF to predict in hospital mortality and mortality after discharge.
Methods Clinical history, general examination, radiological examination, biochemical evaluation was done. ALBI score was calculated at admission and after discharge and compared to CTP, MELD Na and AARC score to predict in mortality and organ failure. ACLF was defined as per APASL criteria. Organ failure was defined as per EASL CLIF criteria.
Statistical Analysis 1. The comparison of the variables which were quantitative in nature were analysed using independent t test. 2. The comparison of the variables which were qualitative in nature were analysed using Fisher’s exact test as atleast one cell had an expected value of less than 5. 3. Kaplan-Meier survival analysis curve was used to find out actuarial survival rate. 4. Receiver operating characteristic curve was used to predict organ failure and mortality and DeLong et al. test was used for comparison of area under curve p value of less than 0.05 was considered statistically significant.
Results For predicting day 1 and day 7 mortality CTP Score has the highest AUC (0.938), for day 3 mortality AARC score had the maximum AUC (0.968). For organ failure at day 1,3,7,30 and day 90 ALBI score has the maximum AUC(1, 0.867, 0.914, 0.889, 0.74) respectively.
Conclusion ALBI score is a relatively newer score. Its validated for HCC, and its role in ACLF is not well studied. As in this study ALBI Score was able to predict organ failure the best, it should be adopted widely in prognostication of ACLF patients.
Keywords ALBI, ACLF, Organ failure, Mortality
289
Clinical, demographic profile, indication and outcomes of liver biopsies performed at a tertiary care centre in north India: A retrospective observational study
Ram Gattani, Vinod Kumar Dixit, S K Shukla, Dawesh Yadav, Vinod Kumar, Anurag Tiwari
Correspondence – Vinod Kumar Dixit - drvkdixit@gmail.com
Department of Gastroenterology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221 005, India
Background Liver biopsy is a common procedure performed in Gastroenterology Department. Transjugular liver biopsy (TJLB) is needed when percutaneous liver biopsy is contraindicated. Percutaneous liver biopsies were performed in Gastroenterology ward under ultrasound guidance. When needed TJLB was done at Radiology department.
Methods A retrospective study was conducted of all the patients who underwent liver biopsy during the last 1-year period. From electronic database, patients’ clinical information, indication and outcome of liver biopsy and complications, if any, were analyzed.
Results Forty-five patients (40% female) underwent liver biopsy of which 15% had TJLB. Indications included-transaminitis, hepatocellular jaundice, cholestatic hepatocellular jaundice, ACLF where apparent cause could not be found. We found that 19 patients had DILI (42%) of which 12 had h/o Giloy (Tinospora cordifolia) intake, 4-CAM,1-Amoxicillin-clavulanate,1-Norethisteron, 1-olanzipine and lithium. Nine had AIH (20%), 6-NASH-cirrhosis, 3-AIH-overlap, 2-PBC, 2-acute viral hepatitis (Atypical) and 1 case each of congestive hepatopathy (DCMP), necrotizing granulomatous hepatitis, diabetic hepatopathy and adenocarcinoma. Ten patients had pain which was relieved with analgesics. None of the patient had any other complication.
Conclusion During the corona virus disease 2019 (COVID-19) pandemic there has been substantial increase in consumption of Giloy which resulted in rise in the number of case of DILI.
Keywords Liver biopsy
290
Efficacy of N-acetyl cysteine in remdesvir induced hepatotoxicity in corona virus disease 2019 patients
Aswin Krishna
Correspondence – Aswin Krishna – aswinkrishna1@gmail.com
Department of Hepatology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 001, India
Background Remdesvir has been approved as an emergency drug in SARS COVID infection. One of the side effects of remdesvir was found to be drug induced liver injury. There are case reports of progression to acute liver failure in such patients. N-acetyl cysteine has been proposed in non acetaminophenan induced liver injury for the prevention of acute liver failure. The scope of N acetyl cysteine in remdesvir induced DILI has been investigated through this study.
Aims: 1. Response to N-acetyl cysteine in patients with Remdesvir induced hepatotoxicity. 2. Role of N-acetyl cysteine in progression of acute liver failure in DILI patients due to Remdesvir. 3. Improvement of liver parameters after withdrawal of the drug in remdesvir induced liver injury patients. 4. Recovery from acute liver failure in NAC group.
Methods Patients without prior history of liver disease who develop DILI after giving remdesvir is divided into study and control group. The study population started on inj N-acetyl cysteine 1 g twice a day for 7 days and ALT was monitored on the 7th day. The complete LFT at the time of admission, day of intitation of NAC and day 7 was recorded. The results are compared.
Results NAC is potent in reducing serum ALT (control-76.4 ± 68.7 vs. NAC-50.4 ± 19.1, p<0.0001) and AST (control -67.2 ± 44.38 vs. NAC-43.6 ± 13.8), p<0.0001) levels when compared to withdrawal group. No progression to acute liver failure was noted in both the groups. In patients with acute liver failure, the recovery was higher and more reduction in liver enzymes was noted when compared to control group.
Conclusion In our study, N-acetyl cysteine was found to be effective in Remdesvir induced hepatotoxicity and found to be effective in recovery of acute liver failure.
Keywords DILI, N-acetyl cysteine, COVID
291
Comparison of definitions for identifying acute-on-chronic liver failure and its outcome
Suman Talukdar, Philip Abraham, Devendra Desai, Tarun Gupta
Correspondence – Philip Abraham – dr_pabraham@hindujahospital.com
Department of Gastroenterology, Veer Savarkar Marg, Mahim, Mumbai 400 016, India
Introduction In the natural course of chronic liver diseases (CLD), progression occurs at variable rates to cirrhosis, decompensation and finally death from complications. An intervening acute insult may lead to acute-on-chronic liver failure (ACLF) with reported high mortality. Unfortunately, there is no consensus on the definition of ACLF.
Aims and Objectives To compare the three international consensus criteria for the definition of ACLF (EASL-CLIF, NACSELD and APASL) in order to (a) determine the number of patients who satisfy these definitions, and (b) determine their accuracy in predicting mortality.
Methods In this prospective observational study, 341 consecutive patients with chronic liver disease (CLD) of any etiology were enrolled and followed up. All significant clinical events and changes in laboratory data were noted in order to classify patients into the three definitions for ACLF.
Results As etiology of CLD, 149 (43.7%) patients had non-alcoholic fatty liver disease, followed by alcohol (24.6%). Fifty-four (15.8%) patients met at least one definition of ACLF: 50 (92.6%) fulfilled the EASL-CLIF criteria, 31 (57.4%) NACSELD, and 22 (40.7%) APASL; the most common precipitating event (59.2%) was infection. Twenty-eight (52%) patients with ACLF died during the study period. Among these, 13 (46.4%) died within the first week, and 25 (89.2%) within the first month after diagnosis. The accuracy of the EASL-CLIF, NACSELD and APASL definitions in determining mortality was 79.7%, 86.3%, and 77.7%.
Conclusion Approximately 16% of patients with CLD developed ACLF by at least one of the three standard definitions; one-half of them died. The EASL-CLIF definition identified the maximum number of patients with ACLF, but the NACSELD definition had the highest accuracy for predicting mortality.
Keywords Alcoholic liver disease, Cirrhosis, Decompensation, NAFLD
292
Hyperfibrinolysis, endogenous heparinoids and altered plasminfactor XIII balance contribute to early rebleeding and mortality in cirrhosis with acute variceal bleeding
Harmanpreet Kaur 1 , Madhumita Premkumar 1 . Kushal Kekan 1 , Virendra Singh 1 , Ajay Kumar Duseja 1 , Jasmina Ahluwalia 2 , Harpreet Kaur 1 , Saurabh Mishra 1 , Rohit Mehtani 1 , Arka De 1 , Nipun Verma 1 , Sunil Taneja 1 , Narender Kumar 2 , Vamsidhar Reddy 1 , Amandeep Singh 1 , Kamal Kajal 3 , Smita Divyaveer 4
Correspondence – Madhumita Premkumar – drmadhumitap@gmail.com
Departments of 1Hepatology, 2Hematology, 3Anaesthesia, and 4Nephrology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Background Sepsis induced hyperfibrinolysis, endogenous heparinoids and coagulation dysfunction can lead to rebleeding after adequate endoscopic treatment in acute variceal bleeding (AVB). We prospectively assessed the association of coagulation failure and hyperfibrinolysis with rebleeding events, sepsis, and outcome in patients with AVB.
Methods Consecutive patients with AVB were assessed at presentation with conventional coagulation tests (D-Dimer, prothrombin time (PT) and activated partial thromboplastin time (aPTT)), viscoelastic tests (SONOCLOT™ [global and heparinase modified coagulation assay]) and specific assays for clotting factors including tissue plasminogen activator (tPA) and plasminogen activator inhibitor (PAI) using commercially available ELISA tests. Patients with recent blood transfusion or refractory shock were excluded. Presence of endogenous heparinoids was defined as difference in SONOCLOT™ traces for activated clotting time ([ACT] global –ACT h >40 sec).
Results Total 138 patients with AVB were screened, of which 80 patients were recruited (44.3 ± 11.7 years; 64% male). Thirteen (16.2%) had early re-bleeding (within 14 days). Endogenous heparinoids were noted in 32 patients (40%) at baseline and in 7 patients (68.5%) with re-bleeding (p=0.032). Standard coagulation tests did not differ between patients who did or did not re-bleed. ACT>155s and Clot Lysis >10% predicted re-bleeding with 88% and 82% sensitivity and 68% and 74% specificity respectively. Inflammatory markers (IL-1β and IL-6) were elevated in patients with rebleeding (42.4 pg/mL vs. 22.44 pg/mL and 43.3 vs. 14.5 pg/mL respectively). Baseline endogenous heparinoids predicted sepsis (HR 2.9; CI 1.4-5.3; p=0.012), re-bleeding events (HR 1.4; CI 1.1-5.3;p=0.034) and mortality (HR1.1; CI 1.0- 4.6; p=0.042). Baseline Factor VIII level (HR 2.3; CI 1.6-7.8; p=0.046) and INR (HR 1.9; CI 1.2-4.3; p=0.039) predicted mortality on multivariate analyses.
Conclusion Hyperfibrinolysis, systemic inflammation and endogenous heparinoids contribute to coagulation failure, early rebleed and mortality in cirrhosis with AVB. Viscoelastic testing is suitable for diagnosis of coagulation defects.
Keywords Endogenous heparinoids, Viscoelastic tests of coagulation, Acute variceal bleed, Hyperfibrinolysis
293
Fecal microbiota transplantation in steroid non responder severe alcoholic hepatitis: A pilot study
Ashok Kumar Vemulapati, Piyush Ranjan, Mandhir Kumar, Munish K Sachdeva
Correspondence – Ashok Kumar Vemulapati – drashok2005@gmail.com
Department of Gastroenterology, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Severe alcoholic hepatitis has a very high short-term mortality up to 50%. Steroids are the only therapeutic option in these patients, but only small proportion will be eligible for steroid therapy. Liver transplantation remains the option for these patients. Gut dysbiosis, leaky gut, microbiome reaching liver are the main culprits in the development of alcoholic hepatitis. The microbiota modulation by FMT as potential strategy in steroid ineligible or non-responder alcoholic hepatitis patients.
Methods This is a prospective pilot study which include all adults diagnosed with severe alcoholic hepatitis, not responded to steroids. Severe alcoholic hepatitis patients, who are eligible for steroids were given prednisolone 40 mg for a week and assessed for Lille score. If Lille score >0.45 were considered as non-responders and underwent FMT. FMT was performed by selecting patient relative as healthy donor after screening, underwent 5-6 cycles of FMT through colonoscopy route and assessed for response. Due to corona virus disease 2019 (COVID-19) pandemic sample size has been reduced.
Results We are presenting four severe alcoholic hepatitis patients who are non-responder to steroids, responded to FMT, in whom clinical, biochemical and liver disease severity scores improved post FMT three months follow up. FMT could be efficacious and safe treatment option in SAH not responding to steroids or steroid ineligible, as a bridge to liver transplantation or who are not willing or not ideal for transplantation for improvement in short-term transplant free survival.
Keywords Fecal microbiota transplantation, Alcoholic hepatitis, Steroid non-responder
294
Subclinical atherosclerosis in non-alcoholic fatty liver disease with advanced fibrosis – Is metabolic syndrome the mediator?
Ravindra Pal , David Mathew Thomas, H Vijay Narayanan, Devika Madhu, Nuzil Moopan, A Shanid, Krishnadas Devadas
Correspondence – Ravindra Pal – docravindrapal@gmail.com
Department of Medical Gastroenetrology. Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Advanced hepatic fibrosis is associated with cardiovascular organ damage in non-alcoholic fatty liver disease (NAFLD). Metabolic syndrome (MetS) is thought to contribute to accelerated atherosclerosis. Carotid intima-media thickness (CIMT) is a surrogate marker for subclinical atherosclerosis. This study was done to assess CIMT in NAFLD patients with and without advanced fibrosis and study its relationship with MetS components.
Methods An observational cross-sectional study done at Government Medical College, Trivandrum over 1.5 years. Patients with NAFLD were grouped into those with and without advanced fibrosis, based on transient elastography values. Anthropometry, blood investigations, and sonographic assessments of patients were done to compare and analyze the cardiometabolic risk between the two groups.
Results Out of the total 201 included patients, 27.4% (55) of patients had evidence of advanced fibrosis. Mean CIMT was significantly higher in patients with advanced fibrosis (0.59 mm ± 0.08 vs. 0.52 mm ± 0.07, p<0.001). When stratified according to the number of metabolic syndrome components, it was found that the mean CIMT was higher in the advanced fibrosis group even without the presence of metabolic syndrome.
Conclusions Mean CIMT values are significantly higher in NAFLD patients with advanced fibrosis. Advanced fibrosis may contribute to the development of subclinical atherosclerosis, even in the absence of metabolic syndrome. Patients with advanced fibrosis need diligent cardiovascular risk assessment.
Keywords NAFLD, Metabolic syndrome, CIMT, Advanced fibrosis
295
Effects of optimal protein diet therapy in patients of liver cirrhosis with hepatic encephalopathy: A randomized study
Akshay Rawat , Anurag Govil, Dinesh Agrawal, Harsh Udawat, Sandeep Vaishnav
Correspondence – Akshay Rawat – akshayrawat89@gmail.com
Department of Gastroenterology, Santokba Durlabhji Memorial Hospital cum Medical Research Institute, Bhawani Singh Marg, Jaipur 302 015, India
Background and Aims Hepatic encephalopathy (HE) portends a worse survival for cirrhotic patients compared to similar patients without HE, even after accounting for the MELD score. Restriction of dietary protein intake in HE has been practised, based on uncontrolled observations, which could predispose cirrhotics to malnutrition. This randomized study was conducted to evaluate the effects of optimal protein supplementation through daily diet in patients of liver cirrhosis with HE.
Methods This study was conducted in a tertiary hospital, enrolling patients of cirrhosis with HE and randomizing them into two groups – Group A patients were given optimal protein diet (1.5 g/kg/day) while Group B patients continued to take their routine diet. Patients were re-evaluated at one month for improvement/worsening in HE and for improvement in their nutritional parameters and Health Related Quality of Life (HRQOL).
Results Patients who were given optimal protein supplementation had statistically significant improvement in serum albumin, hand grip, skeletal muscle mass and HRQOL along with a non-significant improvement in CTP score, MELD Na, fasting arterial ammonia, Psychometric Hepatic Encephalopathy score, Mid Arm Circumference (MAC) and Triceps Skin Fold Thickness (TSF).
Conclusion This study highlights the potential benefits of providing adequate nutritional support to cirrhotic patients with HE. In fact nutritional parameters like MAC, TSF and skeletal muscle mass decreased in patients who were on unsupervised suboptimal diet which could further lead to protein energy malnutrition and sarcopenia.
Keywords Malnutrition, Sarcopenia, Hepatic encephalopathy
296
Point-of-care echocardiography with inferior vena cava dynamics, lactate clearance and NT-Pro-BNP are best predictors of hemodynamic status, diastolic dysfunction, response to fluids, and outcomes in cirrhosis with shock
Harpreet Kaur 1 , Madhumita Premkumar 2 , Kamal Kajal 2 , Virendra Singh 1 , Ajay Kumar Duseja 1 , Smita Divyaveer 3 , Nipun Verma 1 , Arka De 1 , Sunil Taneja 1 , Harish Bhujade 4 , Sreedhara B Chaluvashetty 4 , Saurabh Mishra 1 , Surender Singh 1 , Rohit Mehtani 1 , Sekar Longanathan 2 , Ankur Gupta 5 , Bhupendra Kumar Sihag 5 , Navneet Sharma 6 , Kushal Kekan 3 , Akash Gandotra 1 , Amandeep Singh 1 , Yogender Kumar 1 , Aenav Aggarwal 6
Correspondence – Madhumita Premkumar - drmadhumitap@gmail.com
Departments of 1Hepatology, 2Anaesthesia, 3Nephrology, 4Radiologist, 5Cardiology, 6Internal Medicine, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Background Point-of-care (POC) echocardiography is routinely used to determine left ventricular diastolic dysfunction (LVDD), inferior vena cava (IVC) dynamics and fluid responsiveness. We evaluated utility of echocardiography in patients with cirrhosis with shock and correlated it with conventional tools like central venous pressure (CVP), lactate clearance and cardiac biomarkers.
Methods Consecutive patients with cirrhosis admitted to the liver intensive care unit were screened by 2D echocardiography for assessing LVDD, stroke volume (SV), cardiac output (CO) and IVC indices at presentation. Forty-five patients (84% male, 70% ascites, 65% septic shock, 18.4% variceal bleed) were enrolled and were assessed at admission, 6h, 24h, and 7 days. The IVC collapsibility index (IVCCI) was measured every 6 hours till fluid resuscitation, vasopressor titration and hemodynamic stability were achieved. Cardiac biomarkers (Galectin3, N-Terminal pro-brain natriuretic peptide (NT-Pro-BNP), troponin-I, and plasma renin activity (PRA)) were performed at 0 and 48 hours.
Results Mean CVP was 12.8 ± 4.8 mmHg and mean IVCCI was 34.5 ± 10.9 % in patients with shock. Mean IVC diameter correlated with lactate clearance at 24h (r=0.763, p=0.041) and 48h (r=0.633, p=0.043) respectively but not with CVP (r=0.344, p=0.755). Strong negative linear correlation was observed between CVP and IVCCI (r = -0.827, p= 0.043). IVC diameter <1.4 cm predicted CVP <10 mmHg and indicated need for further volume resuscitation with 91% sensitivity and 79% specificity. IVCCI <20% indicated need for vasopressor usage alone with 74% sensitivity and 65% specificity. Overall survival was 40.9% at day 28. Predictors of 28-day mortality on multivariate analyses were lactate (HR 2.3; CI1.6-7.8; p=0.046) and LVDD grade ≥ 2 (HR 1.9; CI 1.2-4.3; p=0.039).
Conclusion POC echocardiography provides real-time non-invasive volume status assessment. End points like IVCCI and lactate clearance are better targets to guide fluids and vasopressors than conventional CVP targets in patients with cirrhosis.
Keywords Left ventricular diastolic dysfunction (LVDD), Cirrhosis with shock, Point-of-care echocardiography
297
Gastric antral vascular ectasia as first presentation of primary biliary cholangitis
Sugata Narayan Biswas, Anshuman Elhence, Uday C Ghoshal
Correspondence – Uday Ghoshal – udayghoshal@gmail.com
Department of Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow 226 014, India
Primary biliary cholangitis (PBC) is a chronic, autoimmune, cholestatic disease typically occurring in elderly women and most commonly presents with pruritus, fatigue, cholestasis, and its complications. Gastric antral vascular ectasia (GAVE) is an uncommon but significant cause of upper gastrointestinal bleeding often leading to transfusion-dependent chronic iron deficiency anemia. GAVE as a first presentation of PBC is uncommon and has been rarely reported in literature.
A 59-year-old female presented with recurrent melena and transfusion-dependent anemia for a year. She denied any history suggestive of jaundice, ascites or hepatic encephalopathy. Laboratory examination revealed iron deficiency anemia (hemoglobin 4.1 g/dL, 8.2% transferrin saturation, ferritin 7 ng/mL), with deranged liver function tests (total bilirubin 1.9 mg/dL, direct 1.2 mg/dL, alanine aminotransferase 67 IU/L, aspartate aminotransferase 221 U/L, alkaline phosphatase 261 U/L, total protein 7.8 g/dL and albumin level of 4.0 g/dL). Ultrasound showed a liver span of 12.6 cm with altered echotexture, mild splenomegaly (11 cm) and a dilated portal vein (13 mm). Endoscopic evaluation revealed erythematous linear stripes in the antrum suggestive of GAVE, without any esophageal or gastric varices. Fibroscan revealed a liver stiffness measurement (LSM) of 10.8 kPa (F3). Further etiological work up revealed negative viral markers for hepatitis B, C, A and E. Immunological tests were positive for antinuclear antibody (4+; 1:100), antimitochondrial antibody (4+; 1:40) and elevated IgM levels (624 mg/dL). Assessment of hepatic venous pressure gradient was suggestive of clinically significant portal hypertension (10 mmHg) while transjugular liver biopsy revealed distortion of lobular architecture with presence of portoportal bridging fibrosis, lymphocytic infiltration of bile duct epithelium with destruction of small and medium sized bile ductules, consistent with PBC. She was treated with iron supplementation and argon plasma coagulation. At 3 months of follow-up, she did not have further melena and her hemoglobin and liver function tests were normal.
Keywords Gastric antral vascular ectasia, Primary biliary cholangitis, Anemia
298
Tinospora Cordofolia induced DILI: Clinical presentation and outcomes; A multicentric retrospective analysis
Samriddhi Poyekar, Akash Shukla
Correspondence – Akash Shukla – drakashshukla@yahoo.com
Department of Gastroenterology, Seth G S Medical College and K E M Hospital, 9th Floor, New Building, Parel, Mumbai 400 012, India
Introduction The current corona virus disease 2019 (COVID-19) pandemic led to widespread consumption of various self – medications as “immunity boosters”. Tinospora cordofolia (TC) was one of the common immunity booster consumed by people. We came across cases of drug induced liver injury related to it.
Methods Fifty-five cases of suspected drug-induced liver injury (DILI) related to TC consumption were identified across 7 centers in India. Diagnosis of DILI was made as per the criteria of ‘International DILI expert Working group’ and causality assessment was done based on the Roussel Uclaf Casaulity Assessment Method. We analyzed the clinical presentation and the outcomes.
Results Out of 55, 54.5% were females. The most common form of consumption of TC was root/stem decoction with a median duration of consumption of 8 weeks (range 2- 48 weeks). The various clinical syndromes of presentation were acute hepatitis 22 (40%), acute on chronic liver failure (ACLF) 15 (27.3%), acute liver failure 10 (18.2%) and acute liver injury 8 (14.5%). Patterns of liver injury were hepatocellular 22 (40%), cholestatic 23 (41.9%) and mixed 10 (18.1%). Severe DILI was seen 20 (36.4%) of total patients. Out of 20 patients who underwent liver biopsy, 9 had features of autoimmune hepatitis. ANA (>1:40), ASMA (>1:40) and elevated IgG (1.1xUNL) were noted in 38.1%, 23.6% and 30.6% of patients respectively. Eleven (20%) patients died and 6 (10.9%) patients underwent liver transplant at 30 days from onset of symptoms. Presence of ascites, hepatic encephalopathy, higher mean bilirubin, international normalized ratio (INR) and lower total protein, albumin were found to be associated with higher mortality; while use of steroids was associated with lower mortality.
Conclusion TC can cause a spectrum of liver damage from hepatitis to ACLF. Autoimmune mediated liver injury was observed. Unsupervised consumption can be fatal. Steroids can lower mortality in selected cases.
Keywords Autoimmune, DILI, Hepatitis
299
High prevalence of hepatic steatosis in patients with ulcerative colitis from north India: Prospective observational study
Arti Gupta, Vineet Ahuja
Correspondence – Vineet Ahuja – vineet.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction There are no prospective studies evaluating the effect of NAFLD in patients with ulcerative colitis (UC).
Methods In this prospective cohort study, consecutive patients with UC were recruited, and all patients underwent fibro-scan, body composition analysis, bone densitometry, anthropometric measurements, baseline demographic assessment and subjective global assessment. Hepatic steatosis was diagnosed by controlled attenuation parameter (CAP) of >260 dB/m. To evaluate predictors of HS patients of UC with HS (n=29) were compared with age and sex-matched patients of UC without HS (n=27).
Results Among 107 patients with UC (mean age at onset- 29 ±10.6 years; males- 56%, median disease duration- 48 [IQR:24-84] months, 84%- left-sided/pancolitis), 27% (n=29) had HS. 54.7% (23/42) of patients with BMI >23 kg/m2 had HS, whereas only 10% (5/50) and 6.7% (1/15) of patients with normal (18-23 kg/m2) and low BMI (<18kg/m2) had HS. 68.7% (57/83) had decreased bone mineral density (BMD) (osteoporosis/osteopenia). Patients of UC with HS had high mean body mass index (BMI) (p<0.001), waist circumference, high-fat mass (p<0.001), but similar fat-free mass (p=0.798). There was no difference in immunosuppressant exposure between these two groups. Patients of UC without HS belonged to low socioeconomic status (SES) (44.4% vs. 17.2%, p=0.027) and had decreased BMD (77.8 vs. 40.9, p=0.027) compared to patients of UC with HS. At the end of follow-up (32months), there was no difference in steroid requirement, hospitalization due to exacerbation or requirement for biologics, or composite of all three outcomes. Dietary parameters including daily energy, protein, fat and carbohydrate intake were similar between the two groups. On univariate analysis, age greater than 40 years, high BMI positively predicted HS, whereas low SES negatively predicted HS. On multivariate analysis, high BMI and low SES remained significant.
Conclusion Ulcerative colitis is associated with a high prevalence of hepatic steatosis, and high BMI is associated with increased risk. IBD-related factors like disease activity and immunosuppressants are not associated with an increased risk of hepatic steatosis.
Keywords Fatty liver, Ulcerative colitis, Osteoporosis
300
Presence of advanced fibrosis and not fatty liver may be associated with high mortality among patients with corona virus disease 2019 pneumonia
Ruchi Rastogi 1 , Kaushal Madan 2 , Richa Bhargava 2 , Vineeta Dagar 1 , Vikas Singla 2 , Amit Sahu 1
Correspondence – Kaushal Madan – k_madan_2000@yahoo.com
Department of 1Radiodiagnosis, Department of Radiodiagnosis, and 2Centre for Gastroenterology, Hepatology and Endoscopy, Max Institute of Liver and GI Sciences, Max Hospitals, Saket, New Delhi 110 017, India
Introduction Fatty liver has been shown to be associated with severe disease and adverse outcomes in patients with corona virus disease 2019 (COVID-19). However, earlier studies have shown conflicting results related to its impact on mortality. So, we aimed to study the association of fatty liver with mortality and morbidity among patients with COVID-19 pneumonia.
Methods In a retrospective case control study, patients with COVID-19 pneumonia with available CT chest with upper abdominal cuts were included. Cases (fatty liver) were those who had liver to spleen attenuation index (LAI) < 5 and controls (without fatty liver) were those with LAI >5, on non-contrast CT cuts of upper abdomen. Primary outcome measure was difference in mortality. Secondary outcome measures were difference in oxygen requirement, ventilator requirement, ICU stay and hospital stay. FIB-4 was also calculated as a non-invasive marker of liver fibrosis to analyze its impact on mortality and morbidity.
Results Of 451 patients with COVID-19 pneumonia, 291 (64.5%) had fatty liver. The mortality rate was not different between with cases and controls (38/291 [13.05%] vs. 22/160 [13.75%]; p=0.836). Patients with fatty liver had a significantly higher CT severity index (13.22 [5.36] vs. 11.17 [5.99]; p=0.0001). Apart from this, there was no difference in the severity of COVID-19 between cases and controls. On subgroup analysis, patients with severe fatty liver also were not associated with increased mortality (10/77 [12.9%] vs. 50/374 [13.3%]) or morbidity. However, patients with advanced liver fibrosis (FIB-4 >3.25) had higher likelihood of requiring ventilatory support (12/12 [100%] vs. 27/65 [18.4%]; p=0.0001) and dying (10/43 [23.2%] vs. 40/356 [11.2%]; p=0.025) of COVID -19.
Conclusions Presence of fatty liver may not be associated with higher mortality or morbidity among patients with COIVD-19 pneumonia. However, non-invasively determined advanced liver fibrosis may be associate0d with higher mortality and need for ventilatory support in them.
Keywords Covid, Fatty liver, Fibrosis, Mortality
301
Case series on amebic liver abscess in patients with corona virus disease 2019
Rajat Kalra, Samarth Sharma, Praveen Sharma, Anil Arora, Ashish Kumar
Correspondence – Rajat Kalra – rajatkalra7@gmail.com
Department of Gastroenterology (ILGPS), Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Entameba histolytica causes human amebiasis. The most frequent intestinal and extraintestinal manifestations are amebic colitis and liver abscess respectively. There is a surge of amebic liver abscess cases post corona virus disease 2019 (COVID-19). This is a case series of patients presenting with amebic liver abscess complicating the course of COVID-19 pneumonia.
Methods This retrospective case series included consecutive patients with amebic liver abscess with history of COVID-19 pneumonia (or COVID antibody positive) and received some form of immunosuppression. Amebic liver abscess was diagnosed on the basis of amoebic serology, ultrasound or CECT abdomen. Patient received antibiotic treatment and percutaneous drainage of abscess when required.
Results A total of 19 patient were included. The patients were of age group between 28-74 years with median age of 50 years. Twelve (63%) were males and 7 (37%) were females. Nineteen (100%) patients had fever and abdominal pain. Three (15.7%) patients had malena. Ten (53%) patients received steroids for the management of COVID-19. Ten (53%) patients had multiple abscesses, 5 (26%) patients had large absceses (>8 cm) and 9 (47%) had single abscess. Seventeen (89%) patients had amebic serology positive. Three (16%) patients with lower GI bleed had colonic ulcers detected on colonoscopy. Median duration between COVID-19 symptoms and liver abscess diagnosis were 22 days. Ten (53%) patients required percutaneous drainage for their liver abscess. All 19 (100%) patients received antibiotics. Eighteen (95%) patients were cured and 1 (5%) patient with multiple abscesses died due to sepsis secondary to abscess rupture.
Conclusion Treating COVID-19 pneumonia with immunosuppressants increases the risk of infections like amebic liver abscess. Early signs of amebic liver abscess including fever and right upper quadrant pain after receiving immunosuppressive therapy for COVID-19 pneumonitis treatment should be considered an alarming sign and should urge the clinician to investigate for liver abscess to prevent life-threatening complication like rupture of abscess and sepsis.
Keywords Amebic liver abscess, COVID-19
302
Non-invasive biomarkers in assessment of liver fibrosis in patients with HbeAg positive and HbeAg negative chronic hepatitis B: A comparative study
Indra Singh
Correspondence – Indra Singh – dr_ik97@yahoo.co.in
Department of Medical Gastroenterology, Stanley Medical College, No.1, Old Jail Road, George Town, Chennai 600 001, India
Introduction Liver biopsy for evaluation of liver fibrosis has several adverse effects, for which reason non-invasive tests have been developed. Non-invasive biomarkers compared between HbeAg positive and HbeAg negative chronic hepatitis B.
Aim of Study To compare severity of fibrosis in HbeAg positive and HbeAg negative chronic hepatitis B by using non-invasive biomarkers.
Methods This study included 50 patients with HbeAg positive and 50 patients HbeAg negative CHB. All patients underwent laboratory and serology testing. The liver stiffness is measured with elastography. The patients are analysed for APRI, FIB-4 and elastography and comparison is made between HbeAg positive and HbeAg negative CHB.
Results and Discussion The data from our study indicate that the greatest probability for distinguishing fibrosis in patients with HbeAg-negative CHB has a FIB-4 index. The clinical significance and applicability of this index is based on the following observations: the progression of the liver disease is age-related, and the disease duration is proportional with severe fibrosis; more advanced fibrosis is associated with thrombocytopenia due to secondary hypersplenism and decreased production of thrombopoietin by liver cells .Our study revealed that non-invasive biomarkers FIB-4, APRI and elastography showing more fibrosis score in HbeAg negative CHB in comparison to HbeAg positive CHB.
Conclusion Non-invasive biomarkers FIB-4, APRI and Fibroscan showing more fibrosis in HbeAg negative CHB in comparison to HbeAg positive CHB. Combination of non-invasive blood biomarkers and imaging tests can provide better diagnostic accuracy and exclude the need for liver biopsy.
Keywords HbSAg positive, HbSAg negative, Non-invasive biomarkers, Liver fibrosis
303
Effect of Saroglitazar on reducing liver stiffness and liver enzymes in non-alcoholic fatty liver disease: A prospective single arm trial
Avisek Chakravorty , Swetha Sattanathan, Devika Madhu, Shivabrata Dhal Mohapatra, Jithin John, Krishnadas Devadas
Correspondence – Avisek Chakravorty – avisek.doc@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Non-alcoholic fatty liver disease (NAFLD) is becoming the leading cause of cirrhosis worldwide. Pharmacotherapy of NASH remains elusive. The dual PPAR agonist Saroglitazar was approved by DCGI in 2020 for treatment of NASH. So, this trial was initiated to study the effects of Saroglitazar on liver fibrosis, transaminases and lipid profile in NAFLD patients.
Methods Investigator initiated single arm prospective observational study. Consecutive patients of fatty liver (USG) with raised transaminases and LSM ≥7 kPa (TE) were started on Tab Saroglitazar 4 mg daily. Patients with concomitant liver disease due to other etiologies (alcohol, viral, autoimmune), as well as those with cirrhosis were excluded. AST/ALT, lipid profile and LSM were measured at baseline, 6 months and 1 year.
Results Seventy-six patients were started on Saroglitazar. Data was analyzed for all patients at 6 months and the 55 patients who had completed 1 year of therapy. Both at 6 months and 1 year, there was a significant reduction in transaminases (18.5% and 23.6% reduction for AST, 27% and 35.4% reduction for ALT, p=0.00006). Liver stiffness came down from 11.8 kPa at baseline to 9.3 at 6 months and 8.6 at 12 months (21.5% and 28.7% reduction, respectively, p=0.000001). For those with advanced liver fibrosis at baseline (TE ≥ 9.9 kPa), the reduction in LSM was 28.2% and 36% at 6 and 12 months, respectively. Total cholesterol, LDL and triglycerides reduced significantly (14.5%, 15.3% and 18.6% respectively at 1 year). Weight reduction while on Saroglitazar was also significant (3.3% and 3.9% at 6 and 12 months, respectively).
Conclusion Saroglitazar seems to be a promising option for reduction of liver stiffness and transaminitis in NAFLD. Whether there is a similar effect on liver histology has to be proven by biopsy-based studies.
Keywords Saroglitazar, NASH, Liver fibrosis, Transaminitis
304
Prevalence of gonadal dysfunction in male patients with Budd-Chiari syndrome and its reversibility with treatment
Kashmira Kawli 1 , Akash Shukla 1 , Nitin Ramani 1 , Abhijeet Karad 1 , Vinit Kahalekar 1 , Sridhar Sundaram 1 , Shobna Bhatia 1 , Ravi Shah 1 , Tushar Bandgar 2 , Hemant Deshmukh 3 , Sujata Patwardhan 3
Correspondence – Akash Shukla – drakashshukla@yahoo.com
Departments of 1Gastroenterology, 2Endocrinology, and 3Radiology, Seth G S Medical College and K E M Hospital, 9th Floor, M S Building, Parel, Mumbai 400 012, India
Background and Aims Budd-Chiari syndrome (BCS) commonly affects adolescents and adults. With improved survival, important quality of life parameters such as sexual life and fertility become more relevant. This study was aimed to assess the gonadal function in male patients with BCS and the effect of treatment on gonadal function.
Methods Thirty male patients with newly diagnosed BCS were prospectively assessed for the presence of gonadal dysfunction. Erectile function was assessed using standardized International Index of Erectile Function questionnaire (IIEF). Follicular stimulating hormone (FSH), luteinizing hormone (LH), sex hormone binding globulin (SHBG), estradiol, total testosterone (TT), calculated free testosterone (cFT), calculated bioavailable testosterone (cBT), sperm count, and sperm motility were compared at baseline and at 6 months of treatment for the assessment of gonadal function.
Results Sixteen out of 30 (53.3%) patients were sexually active at the time of study and 5/16 (31%) had erectile dysfunction. Hypogonadotropic hypogonadism (HH) was the most common pattern seen in 50% cases followed by hypergonadotropic hypogonadism (HyH) in 23% cases. Twenty-seven percent patients had eugonadism. At 6 months of treatment, 60% of patients in HH group became eugondal as compared to only 14% in HyH group. Proportion of patients with erectile dysfunction reduced (6.25% vs. 31%, p=0.009) after 6 months of therapy. The improvement in sperm count and sperm motility was not significant.
Conclusion Gonadal dysfunction is common in male patients with BCS. HH remains the most common type of hypogonadism BCS and the type which improves significantly after treatment.
Keywords Hypogonadism, Male infertility, Hepatic vein thrombosis, Cirrhosis, Portal hypertension
305
Liver specific arginase-1 reveal early metabolic alterations in high fat induced obesity in rats
Abhishak Gupta
Correspondence – Abhishak Gupta – abhigupta78@gmail.com
Department of Molecular and Cellular Medicine, Institute of Liver and Biliary Sciences, D1 Vasant Kunj, New Delhi 110 070, India
Prevalence of diet induced obesity has dramatically increased globally, making it essential to understand its accompanying metabolic changes in the liver. Obesity causes many health issues, both independently and in association with other chronic diseases such as diabetes, insulin resistance and non-alcoholic fatty liver disease and also considered as the major risk factor for development of non-alcoholic steatohepatitis and liver cirrhosis. In the present study we aimed to understand the molecular mechanisms underlying hepatic mitochondrial alterations in the pathophysiology of high fat diet induced obesity in rats. Early hepatic proteins profiles of normal and high fat fed induced obesity at 24 weeks were analyzed using two-dimensional difference gel electrophoresis (DIGE) and mass spectrometry for protein identification. Fifty-two protein spots were identified by MALDI-TOF and computer-assisted DIGE image software analysis showed 18 major proteins significantly differentially expressed between the comparable groups more than 2.0 to 4.0 fold changes. These proteins were modulated in response to the high-fat diet. Differentially expressed proteins were involved in important metabolic pathways including lipid metabolism, energy metabolism, detoxification, urea cycle and calcium homeostasis in the liver. Further, western blot and immunohistochemistry of liver specific Arginase-1 showed significantly over expression in high fat fed rat liver (p>0.01). Interestingly, Arginase-1 expression differentiates NASH progression. High fat in the diet might influence changes in metabolic pathways in the liver such as lipid metabolism, urea cycle and mitochondrial dysfunction could be the therapeutic targets in management of obesity related liver disease. Arginase-1 expression might be a potential pathological marker to assess liver disease progression.
Keywords Two-dimension electrophoresis (2DE), Two-dimensional difference gel electrophoresis (DIGE)
306
Effect of pre-transplant donor liver fat content (estimated by MR spectroscopy) on post-hepatectomy donor recovery
Aniket Bhardwaj , Hitendra Kumar Garg
Correspondence – Hitendra Kumar Garg – drhitendragarg@yahoo.com
Department of Gastroenterology, Indraprastha Apollo Hospital, New Delhi 110 076, India
Introduction Implantation of donor liver grafts with severe steatosis is associated with early dysfunction of graft liver with delayed functional recovery. Appropriate donor selection optimizes both donor safety and recipient outcomes.
Methods We studied total of 101 living liver donors undergoing right hepatectomy between April 2018 to April 2020 at Indraprastha Apollo Hospital, New Delhi. We used MR spectroscopy for hepatic fat quantification and accordingly subjects were divided in 3 groups: <5%, 5% to 10% and >10% liver fat. Postoperative parameters like LFT, PT/INR, blood counts, hospital stay duration, need of blood products and complication rates were compared between the 3 groups in the early postoperative period. Kruskal-Wallis test and Chi-square test were used for quantitative and qualitative variables respectively. P-value <0.05 was considered statistically significant.
Results Total 101 donors were included, 58 with <5% liver fat, 24 with 5% to 10% liver fat and 19 with >10% steatosis. Clinical parameters like median duration of hospital stay, need for post-hepatectomy blood products transfusion (p-value <0.01), percentage of patients having postoperative bile leak (p-value <0.05) were higher in steatotic donors when comparison made across groups. Total of 25 patients (24.75%) showed post-hepatectomy complications (classified as per modified Clavien criteria), when complication rates compared across groups then showed no significant difference. No mortality was observed. Post-hepatectomy peak median levels of serum bilirubin level (p-value 0.01), ALT (p value-0.003), AST (p-value 0.009) were higher in group with >10% liver steatosis as compared to other 2 groups in the early postoperative period. However, recovery of coagulation function (INR value) and albumin levels showed no significant difference between groups (p-value >0.5).
Conclusion Degree of donor liver steatosis impacts liver function recovery and donor recovery in early post-hepatectomy period. Thus, hepatic fat quantification should be an integral part of preoperative assessment of living liver donors.
Keywords Liver donor steatosis, Post-hepatectomy donor recovery
307
3D decellularized liver bioscaffolds for hepatic cells cultures – A practical approach towards artificial liver development
Abhishak Gupta , Dinesh Tripathi, Savneet Kaur, Shiv Sarin
Correspondence – Abhishak Gupta – abhigupta78@gmail.com
Department of Molecular and Cellular Medicine, Institute of Liver and Biliary Sciences, D1 Vasant Kunj, New Delhi 110 070, India
Introductions Liver cells possess diminished functional ability in the standard 2-dimensional in vitro cultures and also demonstrate limited efficacy after in vivo transplantations, thus limiting their clinical and regenerative applications. 3-dimensional (3D) cultures need to be optimized for their applications. In this regard, decellularized tissue matrix has emerged as a natural scaffold that is used to enhance the in-vitro properties of a variety of cell types. The primary goal of this study was to create a decellularized liver (DCL) matrix for 3-dimensional (3D) cultures of hepatic cells.
Methods DCL was developed by portal vein cannulation and perfusion with detergents and characterized by histology. Enzymatically digested DCL matrix was mixed with commercially available 254atient254. Hepatocytes cell lines (Huh7) were cultured in 3D conditions with or without DCL-matrigel for 14 days. Phenotypic and functional analysis of cultured cells was done by cell morphology, gene expression, immunostaining and albumin assays at day7 and 14.
Results Huh7 cells demonstrated significantly increased proliferation in 3D conditions with DCL-matrigel than in cultures with 255atient255 alone. Gene expression of hepatocyte specific markers, asialoglycoprotein receptor 1 (ASGR-1), HNF-4a, and CK19 was increased more than 2 and 4 folds at day 7 and 14 in 3D-DCL-matrigel conditions. Liver-specific (ASGR-1) immunostaining also showed significantly enhanced expression in 3D-DCL-matrigel conditions at day14. Also, in presence of DCL-matrigel, secretion of hepatocyte marker albumin in Huh7 cells, was significantly increased in the supernatants at day7 and 14, respectively as compared to 255atient255 alone.
Conclusion We conclude that 3D cultures of hepatic cells with DCL-matrigel enhances the viability and functionality of hepatic cells. Optimised 3D protocols could allow generation of mature liver cells and an alternative approach towards artificial liver scaffold for regenerative applications.
Keywords Decellularized liver (DCL), 3-Dimensional (3D), Asialoglycoprotein Receptor 1(ASGR-1), Cytokeratin-19 (CK-19)
308
Detour confusion
Shashank Devarasetty , Avinash Balekuduru, L V Lokesh
Correspondence – Avinash Balekuduru – avinashbalekuduru@gmail.com
Department of Medical Gastroenterology, B E L M S Ramaiah Nagar, RIT Post, M S Ramaiah Nagar, Mathikere, Bengaluru 560 054, India
Introduction Hepatic encephalopathy (HE) is a neuropsychiatric syndrome most often seen in the setting of cirrhosis with portal hypertension (type C). Percutaneous embolization of large portosystemic shunts (PSSs) is a rescue treatment for patients who have persistent encephalopathy or recurrent overt hepatic encephalopathy (OHE). In this case report we present a successful percutaneous embolization of portosystemic shunt.
Case Report A 70-year-old female, a known case of Hep C – cirrhosis with CTP-B presented with altered sensorium, with history of recurrent episodes in the past 6 months requiring multiple admission to hospital. On examination patient had splenomegaly and asterixis. Patient was evaluated for precipitating factors of hepatic encephalopathy. Endoscopy was done and showed no esophageal varices. CT showed surface and parenchymal nodularity of the liver, narrowing of portal vein (5.5 mm) and portorenal shunt of size 16 mm. Patient underwent percutaneous embolization of portorenal shunt via a femoral vascular access and the shunt was selectively catherized and extra sling amplat wire was placed, later amplatzer vascular plug 2 was deployed into the shunt. Post procedure period was uneventful, and patient later underwent imaging which showed increase in size of portal vein diameter when compared to pre-procedure. Patient is on regular follow-up till date and is symptomatically better, did not have any episodes of hepatic encephalopathy.
Conclusion Embolization of large PSSs in carefully selected cirrhosis patients suffering from recurrent or persistent HE lowers the risk of overt HE in the long-term.
Keywords Hepatic encephalopathy, Porto-systemic shunts
309
Comparison of carotid intimal medial thickness and 10-year Framingham risk score between lean and non-lean non-alcoholic fatty liver disease patients for assessing risk of atherosclerotic cardiovascular disease
Avisek Chakravorty , Devika Madhu, Shivabrata Dhal Mohapatra, Jithin John, Krishnadas Devadas
Correspondence – Avisek Chakravorty – avisek.doc@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Non-alcoholic fatty liver disease (NAFLD) has historically been associated with obesity. It is considered the hepatic manifestation of the metabolic syndrome. However, recent studies have indicated that patients who are not obese can also present with NAFLD; this is known as “lean NAFLD”. Cardiovascular Disease remains the most common cause of all-cause mortality in NAFLD. Yet, the CV risk in lean NAFLD has not been compared till date with that of non-lean NAFLD patients. Thus, to compare the risk of atherosclerotic cardiovascular disease between patients of lean and non-lean NAFLD, by measuring CIMT and 10-year FRS-CVD risk, this study was conducted
Methods A prospective observational study. Consecutive patients > 18 years age with NAFLD diagnosed according to 2018 AASLD criteria were enrolled. Those with liver cirrhosis or established CV disease (CAD, CVA, PAD) were excluded. Lean NAFLD was defined as having a BMI ≤ 23 kg/m2. CIMT was measured using standard protocol and FRS score was calculated.
Results One hundred and ten patients of non-lean NAFLD and 65 patients of lean NAFLD were enrolled in the study. Age group specific analysis of CIMT and FRS-CVD risk score, by unpaired t-test, revealed no significant difference between the two arms. When patients were divided into 3 groups 18-40 years, 41-60 years and >60 years, CIMT and 10Y FRS-CVD score was seen to rise according to advancing age groups, in both the arms. (CIMT – 0.54 vs. 0.50, 0.54 vs. 0.55, 0.57 vs. 0.58, 10Y FRS-CVD 10.2 vs. 10.1, 14.6 vs. 15.3, 18.5 vs. 19.1 respectively). In all groups, average CV risk was greater than the regional average.
Conclusion From the present study, there appears to be no significant difference in the CV risk parameters between lean and non-lean NAFLD patients. As such, CV evaluation of all NAFLD patients irrespective of body habitus should remain a priority.
Keywords Lean NAFLD, Cardiovascular disease, CV risk, CIMT, Framingham risk score
310
APRI, FIB 4, and AST/ALT ratio correlation with Fibroscan in predicting severe/not severe fibrosis
V Y Bhargav , Shaurav Khanna, S Thamarai Selvan, Mu Karthikeyan, Jayanthi Venkataraman
Correspondence – Bhargav V Y – 257atient257.b4@gmail.com
Department of Hepatology, Sri Ramachandra Medical College, Porur. Chennai 600 116, India
Background Metabolic-associated fatty liver disease (MAFLD) leading to steatohepatitis, fibrosis, and cirrhosis of the liver is the global burden currently that is rapidly increasing in incidence. Hence early diagnostic and screening tools which are non-invasive are required to identify the disease.
Aim To identify a non-invasive score among Fibrosis-4 (FIB 4), AST platelet ratio index (APRI), and AST/ALT ratio, that can correlate with fibro scan in predicting liver fibrosis accurately in MAFLD patients.
Methods A Cross-sectional study was conducted on patients diagnosed with fatty liver (Grade I, II, III) based on USG abdomen. The study period was from September 2020 to March 2021. These patients underwent a Fibro scan and fibrosis scores were measured in Kpa (kilopascals) were categorized into not severe fibrosis (F0, F1, F2) and severe fibrosis (F3, F4). FIB 4, APRI, and AST/ALT ratio were measured based on the patient’s lab data. Previously known or underlying liver disease, significant alcohol consumption patients were excluded from the study. The results of the above scores were compared with fibro scan results in predicting severe/not severe fibrosis.
Results The results of 302 patients were analyzed among which 186 (61.8%) were males, 24.9% had diabetes mellitus, 18.9% had hypertension,18.6% had dyslipidemia. Fibrosis severity in the study showed 127 (42.2%) had severe (F3, F4) and 174 (57.8%) had non-severe fibrosis (F0, F1, F2). The mean body mass index (BMI) in severe fibrosis patients was 28.9 kg/sq.m. Among the scores, FIB 4 and APRI were predictive of severe fibrosis which was statistically significant (0.005 and 0.009). FIB 4 showed a specificity of 93.7%, positive predictive value (PPV) of 74.4%, and APRI showed a specificity of 89.1%, PPV of 65.5%.
Conclusion FIB 4 and APRI were the better scores in predicting severe and non-severe fibrosis. Among both, FIB 4 had better specificity and PPV.
Keywords Fatty liver, Fibrosis, FIB 4, APRI, AST/ALT ratio, Fibro scan
311
Portal vein reconstruction-transjugular intrahepatic shunt: Novel approach in management of chronic portal vein thrombosis
Malla V A Gangadhar Rao , Gaurav Pande, Samir Mohindra, S Rakesh Kumar, Preetam Das, Dhruv Thakur, Dhruv Yadav 1 , Sanket Kulkarni 1
Correspondence – Gaurav Pande – drgauravpandey@yahoo.com
Departments of Gastroenterology, and 1Radiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014, India
Portal vein thrombosis is a potential cause of portal hypertension and its sequelae like portal cavernoma and biliopathy. Treatment of chronic portal vein thrombosis involves mainly reduction of portal hypertension and its complications. Portal vein reconstruction-transjugular intrahepatic shunt (PVR-TIPS) can reduce portal hypertension and biliopathy by restoring blood flow along portal vein. Here we report a case of 60-year-old male with chronic liver disease and chronic calcific pancreatitis with chronic portal vein thrombosis with portal cavernoma and biliopathy presented with cholangitis. MR portovenography with MRCP showed portal vein and splenic vein thrombosis with cavernoma and dilated bilateral moderate IHBR with biliopathy. Patient was treated with biliary stenting for cholangitis. PVR-TIPS was done using right IJV access and then through right hepatic vein, tract was made through hepatic parenchyma up to major collateral followed by placement of 10*80 mm Fluency graft. Under guidance it was extended till SMV by 10*100 mm Luminex bare metal stent. After reconstruction there is good hepatopetal flow through SMV-metal stent-collateral-TIPS axis. Post procedure patient developed hepatic encephalopathy which was treated conservatively with lactulose and LOLA. On follow up for 12 months, repeat cholangiogram showed resolution of biliopathy. Patient was on DOAC and no further recurrence of jaundice. In summary PVR-TIPS is a novel safe and effective approach in reducing portal pressure and biliopathy, especially when shunt surgery and conventional or trans-splenic PVR-TIPS is not feasible.
Keywords Portal vein, TIPS, Cavernoma, Biliopathy, DOAC
312
Enhanced liver fibrosis score – Is it useful for evaluation of fibrosis severity in chronic hepatitis C infection?
Roshan George , Manish Gupta, Sanjeev Sachdeva, Ujjwal Sonika, Ashok Dalal, Ajay Kumar
Correspondence – Ajay Kumar – ajaykumar.aiims@gmail.com
Department of Gastroenterology, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, J L N Marg, New Delhi110 002. India
Introduction The assessment of liver fibrosis is important in patients with chronic hepatitis C (CHC). In recent years non-invasive tests like enhanced liver fibrosis (ELF) have been developed as alternative to liver biopsy for estimating the severity of liver fibrosis. We aimed to assess whether the ELF score can be used for fibrosis severity estimation using liver biopsy as the gold standard.
Methods Forty-nine patients with CHC were enrolled in the study. Liver biopsy, ELF and transient elastography (TE) were done in all patients and severity of fibrosis on histopathology was assessed by METAVIR score. The diagnostic performance of ELF was evaluated by receiver operator characteristic curve (ROC) analyses and liver biopsy histopathology was taken as the gold standard for severity of liver fibrosis.
Results The area under receiver operator characteristic curve (AUROC) for significant fibrosis of ELF score was 0.64 (95% confidence interval [CI], 0.48-0.79) and of TE was 0.85 (95% CI,0.73-0.96). The AUROC for advanced fibrosis of ELF was 0.77 (95% CI, 0.57-0.97) and TE was 0.98 (95% CI,0.94-1.0). The calculated cut-offs of ELF overestimated fibrosis in 53.06% (26/49) of patients and underestimated fibrosis in 6.12% (3/49) patients. AUROC of TE was found to be significantly better than ELF for diagnosis of significant fibrosis (p=0.004) and advanced fibrosis (p=0.034).
Conclusion The ELF score can be used as marker for advanced fibrosis in HCV patients but it is inferior to TE in estimation of liver fibrosis severity.
Keywords ELF, Transient elastography, HCV, Liver biopsy
313
Prognostic nutritional index as a predictor of overall survival in cirrhotic patients with hepatocellular carcinoma
Devika Madhu , Ravindra Pal, Avisek Chakravaroty, Susan George, Srijaya Sreesh, N Premaletha, Krishnadas Devadas
Correspondence – Devika Madhu – devikamadhu86@gmail.com
Department of Medical Gastroenterology, Trivandrum Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction There is increasing evidence that the presence of an ongoing systemic inflammatory response is a stage-independent predictor of poor outcome in patients with cancer. The aim of this study was to investigate whether an inflammation-based prognostic score, the prognostic nutritional index (PNI), is associated with overall survival (OS) in cirrhotic patients with hepatocellular carcinoma (HCC).
Methods All cirrhotic patients with HCC from September 2019 to March 2021 (n=82) were included and followed up for 6 months. De-novo HCC and other malignancies were excluded. Demographic and clinical data were collected. PNI was calculated as (10 × serum albumin [g/dL]) + (0.005×lymphocytes/μL). Univariate and multivariate analysis were performed to identify clinicopathological variables associated with OS.
Results Eighty-two cirrhotic patients with HCC were included and followed up for 6 months. After 6 months 28 patients (34%) had died. Univariate analysis showed that PNI (p<0.001), BCLC score (p<0.001), PVT (p-0.038), hepatic encephalopathy (p<0.001), CHILD status (p<0.001) were all predictors of OS. Multivariate analysis showed that PNI was an independent predictor of OS. PNI was calculated for all patients and an optimum cut-off value of 34.8 was established using the receiver operater curve (ROC) analysis (sensitivity-89.29, specificity-90.74, positive predictive value 83.3, negative predictive value- 94.2). ROC of PNI (0.92), BCLC (0.84), CLIP (0.77), HKLC (0.78) and neutrophil leukocyte ratio (NLR) (0.76) was compared, from which PNI had the maximum area under ROC (AUROC). Multivariate comparison of the prognostic power of PNI and BCLC was done using Cox regression model which showed PNI had a hazard ratio of 17.96 vs. 2.1 for BCLC.
Conclusion The presence of a systemic inflammatory response, as measured by the PNI < 34.8 is an independent predictor of poor OS in patients with HCC. The prognostic power of PNI was better than BCLC.
Keywords PNI, HCC, Overall survival
314
WPSU (wellness programme for substance user) – for alcohol relapse prevention: A New Avenue
Neeraj Nagaich 1 , Radha Sharma 2
Correspondence – Neeraj Nagaich – drneerajn@gmail.com
1Department of Gastroenterology, Fortis Escorts, Jaipur 302 020, India, and 0Department of Pathology, RUHS CMS Medical College, Jaipur 302 020, India
Objectives A large unmet need for a robust system for relapse prevention in alcohol dependent. Meditation is an emerging non pharmacologic treatment for alcohol relapse prevention. This 16-week prospective study was done to evaluate efficacy of wellness programme for substance user (WPSU) (a combination of meditation, motivation, coping strategies and group support) for relapse prevention.
Methods Seventy-two adult alcohol-dependent patient were enrolled for online WPSU. Sixty-eight patients completed the 7 day online WPSU meditation course supplemented by at-home meditation and “standard of care” therapy. Outcome measures included relevant surveys.
Results Fifty-nine patients (86.76 %) were abstinent for 30.9 (SD=22.2) days at 260atient260d. Completers (n = 59) attended 85% of meditation course sessions and meditated on average 4.6 (SD=1.1) days per week; they were abstinent on 94.5% (SD=7.4) of study days, with 49% reporting complete abstinence and 51% reporting 1 or more heavy drinking days. Their severity of depression, anxiety, stress (p<0.05), and craving (p<0.08), documented relapse triggers, decreased, and the degree of mindfulness increased (p<0.05). The WPSU course was rated as a “very important” (8.7/10, SD=1.8) and “useful relapse prevention tool” (8.5/10, SD=2.1); participants reported being “very likely” to continue meditating (9.0/10, SD=1.5). “Gaining skills to reduce stress,” “coping with craving,” and “good group support” were the most common qualitative comments about the course value. There were no adverse events or side effects.
Conclusions Meditation may be an effective adjunctive therapy for relapse prevention in alcohol dependence. Needs revalidation in larger RCT.
Keywords WPSU (wellness programme for substance user), Alcohol dependence, Meditation, Relapse prevention addiction, Substance use disorders
315
Untargeted plasma metabolomics identifies altered nicotinate-nicotinamide and D-glutamine-glutamate metabolism in patients with hepatitis E virus induced acute liver failure
Anoushka Saxena 1 , Prabhjyoti Pahwa 1 , Siddiqui Siddiqui 1 , Jaswinder Singh Maras 1 , Rashi Sehgal 1 , Sharda Patra 2 , Shiv Kumar Sarin 3 , Nirupma Trehanpati 1
Correspondence – Nirupma Trehanpati – trehanpati@gmail.com
Departments of 1Department of Molecular and Cellular Medicine, 2Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India, and 2Department of Gynaecology and Obstetrics, Lady Hardinge Medical College, New Delhi 110 070, India
Introduction Acute viral hepatitis due to hepatitis E virus (AVH-E) infection is often serious in pregnancy and could result in acute liver failure (ALF) and mortality in up to 65% cases. Better biomarkers are needed to predict the outcomes. We studied comprehensive metabolite profile to understand the pathogenesis of AVH-E and progression to ALF-E. We undertook the multivariate analysis to identify the common and specific metabolites and pathways in ALF-E and AVH-E.
Methods We performed plasma metabolomics in pregnant (P) patients with AVH-E (Gr.1, =10, 4.5±2 yr), ALF-E (Gr.2, n=12, 26±2 yr) and in HC (Gr.3, n=7, 24.5±2 yr) and compared with non-pregnant (NP) acute HEV (Gr.4, n=10, 28±3 yr), ALF-E (Gr. 5, n=8, 35±1 yr). Common and specific metabolites and pathways associated with outcomes were identified using ultra-high performance liquid chromatography tandem mass spectrometry (UHPLC-MS/MS) coupled to multivariate statistical analyses.
Results Plasma metabolomics identified a total of 278 metabolites in HEV infected patients compared to healthy controls. Multivariate principal component analysis (PCA) identified closer relationship between P-AVH-E and HC-P than ALF-E (Fig. A). Twenty unique metabolites specific to nicotinate nicotinamide and D-glutamine-glutamate metabolism were significantly upregulated (p<0.05) in Gr.1, and 71 metabolites related to nicotinate-nicotinamide and D-arginine-D-ornithine metabolism, were upregulated in Gr.2 (Fig. B). It was observed that 11 metabolites belonging to nicotinate and nicotinamide metabolism were significantly upregulated in both Gr.1 and Gr.2 (Fig. C). However, the level of enrichment progressively increased from healthy pregnant to acute HEV to HEV-ALF pregnant females. We also found that D-glutamine-glutamate metabolic pathway was down regulated in HEV-ALF only in pregnant women (Gr.2).
Conclusion Our results show that significantly upregulated nicotinate and nicotinamide pathway contribute in pathogenesis of hepatitis-E virus. However, significantly downregulated D-glutamine and glutamate pathways, can predict ALF-E in pregnant patients.
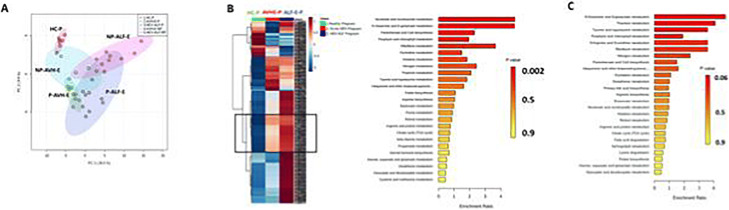
Keywords Hepatitis-E, Acute liver failure, Metabolomics
316
Changes in patterns of alcohol consumption and its impact on liver disease pre and during corona virus disease 2019 pandemic
Sidharth Harindranath , Ankita Singh, Michael Kuruthukulangara, Nitish Patwardhan, Mayur Satai
Correspondence – Sidharth Harindranath – h.sidharth@gmail.com
Department of Gastroenterology, Seth G S M C and K E M Hospital, 9th Floor, MSB, Parel, Mumbai 400 012, India
Introduction Emerging evidence suggests that alcohol consumption has increased during the corona virus disease 2019 (COVID-19) pandemic. We performed a cross-sectional survey to assess changes in drinking behaviours during the pandemic and its impact on the course of liver disease.
Methods We conducted a cross-sectional survey of patients presenting to the Liver clinic or inpatients at a tertiary care centre from May 2020 to September 2021. Demographic details, drinking patterns and status of liver disease Pre and post COVID-19 pandemic were noted.
Results One hundred and fifteen patients were included in the study (Male – 100%, Mean age – 38 years, Range – 32-75 years). Most of the patients 106 (92%) had consumed alcohol in the past 1 year. 49 patients (42.1%) reported consuming 3-4 standard drinks per day. Sixty-five patients (56.5%) reported episodes of binge drinking. Of the patients who reported drinking 70 (60.6 %) reported that their drinking had increased compared to pre-COVID 19. Of those 56 patients (80%) reported that their drinking had increased because of increased stress. 21.7% reported decreased drinking as compared to pre-COVID 19, and most common reason reported was fear of death due to liver decompensation (42.9%). Majority of patients (59.1%) were non-compliant to alcohol dependence therapy advised by psychiatrist. Pre-COVID 19 CTP score was 7-9 in 45.8% and 10-15 in 16.7% of patients, whereas post COVID-19 CTP score was 10-15 in 47.6% of patients and 33.3% of patients had a CTP score of 7-9. Majority of the patients (83.3%) remained decompensated post COVID-19 pandemic.
Conclusions Patients reported being stressed by the pandemic consumed more drinks and had a higher incidence of liver decompensation as compared to pre-COVID-19.
Keywords COVID-19, Alcohol drinking, Liver disease
317
Role of therapeutic plasmapheresis (PLEX) in acute liver failure (ALF) due to rodenticide paste {yellow phosphorous (YP)} poisoning
Sandheep Janardhanan, Allwin James, Alagammai Palaniappan
Correspondence – Sandheep Janardhanan - sandheepjanardhanan47@gmail.com
Department of Gastroenterology, Meenakshi Mission Hospital and Research Centre, Lake Area, Melur Main Road, Madurai 625 107, India
Background Rodenticide paste containing yellow phosphorous (YP) poisoning is very common in, state of Tamilnadu. Acute liver failure (ALF) occurs in 21% of such cases. PLEX is a grade 1 recommendation in the management of ALF, there have been very few studies in the context of this new intervention.
Objective The aim of this study was to study the efficacy of plasmapheresis in acute liver failure due to yellow phosphorous poisoning and to evaluate the predictive factors in determining the success of this novel method.
Methods A total of 53 patients underwent plasmapheresis for ALF due to YP poisoning, over two years (December 2018-December 2020). Demographic data and biochemical parameters were recorded before and overall transplant-free survival was analyzed.
Results Of all patients, (67%) completely recovered, while 19% worsened, and referred to transplant units or while the rest expired (14%). The study showed mean difference and significant improvement in total leukocyte count (before and after – TLC mean±Std, 4638±2820 ; 6130±2274 p=<0.003*), total bilirubin (before and after – total bilirubin mean±Std were 3.7± 3; 2.2±1.9, p=0.003*), SGOT (before and after SGOT mean±Std were 252±136; 48±33, p=0.01*), prothrombin time (before and after, PT mean±Std were 56±43; 23±14 p=0.01*) and international normalized ratio (INR) (before and after INR mean±Std were 2.1± 1.4 ;1.8 ± 1.1, p=0.024*), pre and post PLEX (p < 0.05) .There was a significant association between the success of treatment and time taken to reach the hospital and quantity of toxin consumed. Interestingly, leukopenia, due to toxin-induced myelosuppression was a major early and independent predictor of mortality which preceded hepatic manifestations. Early initiation of PLEX in such patients have significant survival benefits.
Conclusion PLEX appears to be a novel intervention providing survival benefit in ALF due to YP poisoning and appears to be a feasible nontransplant treatment option in the absence of a liver transplant (LT) unit.
Keywords Plasmapheresis, Yellow phosphorous poisoning
318
Serial saliva proteomic analysis predicts the outcome of therapeutic plasma exchange in severe alcoholic hepatitis patients
Babu Mathew1, Gaurav Tripathi1, Manisha Yadav1, Gaurav Yadav1, Nupur Sharma1, Vasundhra Bindal1, Meenu Bajpai2, Jaswinder Singh Maras1, Shiv Sarin2
Correspondence – Shiv Sarin – shivsarin@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Transfusion Medicine, and Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Introduction Severe alcoholic hepatitis has high mortality with limited medical treatment options. As response to patients undergoing TPE procedures is variable and decision for further TPE remains empirical, we explored the utility of baseline saliva proteomics in identifying patients who are unlikely to survive or require additional TPE.
Methods Saliva cotton swab from patients (n=20) undergoing TPE was collected at baseline and 24-hour after TPE. Proteins were isolated and were subjected to reduction-alkylation-trypsin digestion followed by label-free quantification using nano-HPLC coupled to high-resolution mass spectrometry. Most significant determinants in non-survivors were correlated with severity and subjected to evaluation of their diagnostic accuracy.
Results A total of 1149 proteins were identified in the saliva samples of SAH patients. Baseline saliva showed 12 upregulated proteins linked to glycosphingolipid metabolism, starch and sucrose metabolism whereas 232 downregulated proteins were linked to TLR cascades, necroptosis and Rho GTPases signaling (FC> ±1.5; p<0.05). As compared to baseline SAH, Post-TPE SAH patients who survived, showed 92 differently expressed proteins, of which 16 were upregulated and linked to pyruvate and purine metabolism, citrate cycle, purine salvage and erythrocyte function (FC> ±1.5; p<0.05). SAH patients who died post-TPE, showed 92 DEPs of which 76 were upregulated; linked to MAPK signaling, necroptosis, cellular senescence, toll like receptor 4 (TLR4) cascade, interleukin-3,5 and GM-CSF signaling. Inflammatory pathways were significantly increased in non-survivor’s post TPE. Inflammation linked proteins; secretory carrier membrane protein 3 (SCAMP3), cysteine rich secretory protein 3 (CRISP3), and transformer 2 beta homolog (TRA2B) significantly correlated with the severity (r>0.3; p<0.05) and documented highest diagnostic efficiency for predicting non-survival (AUC>0.85; p<0.05) in SAH patients.
Conclusions Post-TPE measurement of SCAMP3, CRISP3 and TRA2B in saliva could predict the outcome in SAH patients and could serve as a simple and non-invasive way for serial assessment of SAH patients undergoing TPE.
Keywords Severe Alcoholic Hepatitis Proteomics Saliva Plasmapheresis
319
Safety and efficacy of saroglitazar in non-alcoholic fatty liver disease population – A real world, single centre, observational study
Dipak Shah
Correspondence – Dipak Shah – docdipak71@gmail.com
Department of Gastroenterology,1, Proton Clinic, 291/A, Rabindra Sarani, Kolkata 700 006, India
Background and Aims Non-alcoholic fatty liver disease (NAFLD) is an increasingly prevalent and one of the fastest emerging manifestations of the metabolic syndrome worldwide. Saroglitazar 4 mg OD is only approved treatment for NAFLD associated with metabolic comorbidities and non-cirrhotic NASH. We tried to evaluate the efficacy and safety of Saroglitazar 4mg OD in NAFLD/NASH in routine clinical practice.
Methods A total 50 documented NAFLD patients prescribed on Saroglitazar 4 mg OD, were retrospectively analyzed for changes in liver biochemical parameters and lipid profile at 12 weeks. The data at baseline and 12 weeks was analyzed and statistical significance was established using paired sample t- test.
Results The study shows statistically significant improvements in ALT by 41.9%, AST by 28.9%, serum TG by 46.5%, LDL by 21.3%, total cholesterol by 25.6% and HDL by 4.33%. Overall NFS score improved by 15.7% (p value=0.031). There was no any treatment related side effects during the study.
Conclusions The study shows Saroglitazar 4 mg OD as a safe and effective treatment option for NAFLD, with significant improvement in all liver related parameters and non-invasive NAFLD fibrosis score.
Table 1 Baseline Population Demography (n=50)
| Age (Mean +SD) in Yrs | 48.1 +11.7 |
| Weight (Mean +SD) in Kg | 73.44 +9.3 |
| BMI (Mean +SD) in kg/m2 | 28.2 +3.8 |
| % Male (total count) | 66 (n=33) |
| % Non-Diabetic (total count) | 66 (n=33) |
| % Non Dyslipidemic (total count) | 86 (n=43) |
| % Non-Hypertensive (total count) | 60 (n=30) |
| Negative Family history of liver disorder | 54 (n=27) |
Fig 1 Improvement in LFT Fig 2 Improvement in lipid profile (after 12 wk)
Keywords NAFLD, NFS score, Saroglitazar
320
2D-Shear wave elastography is as good as vibration controlled transient elastography in compensated liver cirrhosis
Devika Madhu, P Arun, Ravindra Pal, Avisek Chakravaroty, T S Prasanth, A Shanid, Krishnadas Devadas
Correspondence – Devika Madhu – devikamadhu86@gmail.com
Department of Medical Gastroenterology, Trivandrum Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background We compared the diagnostic performance of 2D-Shear wave elastography (2D-SWE) and transient elastography (TE) in patients with compensated cirrhosis.
Aims To compare the diagnostic performance of 2D-SWE and TE in patients with compensated liver cirrhosis.
Methods One hundred and eight patients with compensated cirrhosis undergoing 2D-SWE, TE and endoscopy were enrolled. We compared both methods using Bland-Altman scatter plot and Passing-Bablok regression analysis.
Results There were 64 males and 44 females, with a mean age of 51.73 ± 11.35 years. NASH (40%) and alcohol (27%) were the main etiologies. Esophageal varices were found in 63 patients. Thirty-six had high-risk varices. The optimal liver stiffness cut-off value for 2D-SWE and TE for predicting the presence of esophageal varices was 21.1 kPa and 22 kPa respectively. Both TE and 2D-SWE had a significant positive correlation in predicting the presence of esophageal varix. Passing and Bablok regression analysis was also used to compare the two methods. It showed that there was no systematic difference (Intercept A -0.2874, 95% CI-1.50 to 1.30), and no proportional difference (Slope B 0.9381, 95% CI 0.8778 to 1.00) between the two tests. Cusum test for linearity showed no significant deviation from linearity, which means both tests are comparable.
Conclusion The performance of 2D-SWE was comparable to TE in the assessment of fibrosis. This, to our knowledge is the first study to directly compare the two techniques in patients with compensated cirrhosis. Given the various advantages of 2D-SWE, including performing real2D-SWE, including performing real time ultrasound scan, it may replace TE as the non-invasive method of choice in assessing liver fibrosis.
Keywords Esophageal varices, Liver stiffness, Shear wave elastography, Transient elastography
321
Hepatocellular carcinoma: A population based cross sectional study in tertiary care centre in south India
Siddharth Badola , K Narayanasamy
Correspondence – Siddharth Badola - sssbd12345@gmail.com
Department of Hepatology, Madras Medical College, Rajiv Gandhi General Hospital, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Hepatocellular carcinoma (HCC) is the most common primary liver malignancy. The distribution of HCC vary significantly between different study populations around the world. With medical advances, early identification of HCC can be curable with resection, ablation and liver transplantation (LT). The study aims to investigate the distribution of HCC according to age ,gender and etiology, so as to identify high risk groups, that can help in better implementation of screening programmes and preventive measures.
Methods This is a cross sectional study done in a tertiary care centre in south India between October 2019 to September 2021. All new cases as well as follow-up cases of HCC who attended hepatology OPD or admitted in ward/ICU were included. Data was collected and analysed.
Results The total of 118 patients of HCC were identified. The most common age group of HCC was found to be 50-65 years (62.7%). The male to female ratio was 5.2:1. The etiology in most cases was chronic HBV infection (41.5%) followed by Ethanol abuse (30.5%). Other causes include chronic HCV infection (13.6%), combined chronic HBV infection and Ethanol abuse (6.8%), chronic HBV/HCV coinfection (3.4%), and cryptogenic/NASH/other (4.2%). Out of 118 cases, 81.4% had underlying chronic liver disease (CLD), while 18.6% had HCC without CLD, and most of these were positive for chronic HBV infection (63.6%).
Conclusion In this study, HCC was commonly presented after the age of 50 years. Male predominace was higher than in most parts of the western world. The most common risk factor was found to be chronic HBV infection followed by Ethanol abuse. chronic HCV infection and NASH are less common cause of HCC in southern India compared to the western world. Early presentation of HCC with majority having chronic HBV infection, suggested that vertical transmission of HBV is still 267atient267d in this region
Keywords Hepatocellular carcinoma, Chronic HBV, Ethanol abuse, Chronic HCV
322
Secondary bile acids regulate angiocrine gene expression in liver sinusoidal endothelial cells during liver regeneration
Impreet Kaur . Rajnish Tiwari, Pinky Juneja, Ashwini Vasudevan, Indu Sharma, Hamed Hemati, Shiv Sarin, Dinesh Tripathi, Savneet Kaur
Correspondence – Savneet Kaur – savykaur@gmail.com
Department of Molecular and Cellular Medicine, Institute of Liver and Biliary Sciences, D1, Vasant Kunj, New Delhi 110 070, India
Background Bile acids (BA) play an inseparable role in hepatocyte proliferation and liver regeneration. In the current study, we analyzed BA pool in portal and peripheral blood in partial hepatectomy (Phx) models and studied how Bas interacted with primary liver cells to affect liver regeneration.
Methods We performed BA profiling in peripheral and portal serum by LC-MS/MS in rat models of 70% PHx at day 2 and day 5 post Phx. Primary rat hepatocytes, liver sinusoidal endothelial (LSEC) and hepatic stellate cells (HSC) were isolated by in vivo collagenase digestion. Gene and protein expression of BA receptors in primary liver cells was investigated. The effects of specific Bas were studied on liver cells by in vitro assays.
Results We identified 28 individual Bas both in peripheral and portal circulation. BA pool was inversely correlated in these two compartments in both sham and Phx animals. In portal serum, lithocholic acid (LCA, 1.6-fold, p<0.05) and taurolithocholic acid (TLCA, 1.8-fold each, p<0.05) were significantly enhanced in Phx (day 2) compared to sham. With respect to BA receptors, expression of TGR5 was significantly elevated in HSCs and LSECs (3. 4 fold, p<0.05 and 6.7-fold, p<0.001) in Phx (day 2) compared to sham. A high protein expression of TGR5 was also validated in LSECs of Phx rats. LCA treatment of LSECs enhanced the expression of angiocrine genes, GATA-4 (2-fold), Wnt-2 (4-fold) and CXCR7 (2.5-fold) (p<0.05 each) and secretion of Wnt2 (3-fold, p<0.01), in vitro. An incubation of hepatocytes with conditioned medium of LCA-treated LSECs induced a significant proliferation of hepatocytes with increased expression of FoxM1B (2.4-fold, p<0.05).
Conclusion Increased LCA and TLCA in portal serum, interact with LSECs via TGR5 and modulate their angiocrine signaling and thus hepatocyte proliferation. Our findings provide a key link between secondary Bas in the portal blood and LSEC-mediated liver regeneration.
Keywords Bile acid receptors, Angiocrine factors, Liver regeneration
323
Hypoglycemia a paraneoplastic manifestation of hepatocellular carcinoma: A case series
Gourab Bhaduri , Anand Sharma
Correspondence – Gourab Bhaduri - gourab.bhaduri@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Virbhadra Road Shivaji Nagar, Near Barrage, Sturida Colony, Rishikesh 249 203, India
Introduction Hypoglycemia occurs in 5% cases of hepatocellular carcinoma (HCC) and is rarely the first manifestation. Here we report 2 cases of HCC associated with hypoglycemia.
Case 1 A 59-year-old female presented with recurrent hypoglycemia requiring multiple hospital admissions. On evaluation she was diagnosed with hepatitis C (HCV) related cirrhosis with multiple liver lesions and 1000-fold elevated alfa-feta protein. Imaging features were characteristic of HCC and biopsy stained positive for arginase, negative for RCC ag, vimentin, consistent with HCC. She was started on frequent carbohydrate rich meals following which hypoglycemia did not recur. Considering the advanced stage of malignancy, she was offered palliative treatment.
Case 2 A 70-year-old male patient, diagnosed previously with hepatitis B virus related cirrhosis and HCC presented with seizures. He was found to have hypoglycemia in emergency. His insulin and c peptide levels were 0.37 mcIU/mL and 0.05 ng/mL, consistent with non-islet cell etiology. He had persistent hypoglycemia even with frequent meals with carbohydrate content of 1500 g/day and hourly glucose orally. He was started on prednisolone 40 mg once daily. Hypoglycemic episodes did not recur following this. Thereafter sorafenib was started.
Discussion Two types of hypoglycemia occur in HCC: Type A occurs in late stages of HCC due to impaired gluconeogenesis and is less severe than Type B, which occurs in early stages of HCC due defective processing of pro IGF II to IGF II. Big IGF II binds IGF I receptor and inhibits GH secretion. Definitive treatment of the HCC prevents the recurrence of hypoglycemia. Steroid can prevent hypoglycemia by stimulating gluconeogenesis through ternary complex formation comprising pro IGFII , @-labile subunit and IGFBP3 thereby lowering free pro IGF II.
Conclusion Hypoglycemia is a rare paraneoplastic manifestation of HCC, and occurs rarely as a presenting manifestation.
Keywords Hepatocellular carcinoma, Hypoglycemia, Paraneoplastic
324
Venous ammonia-predictor of sarcopenia and minimal hepatic encephalopathy
Harish Gupta , Amrish Sahney, Manav Wadhawan, Ajay Kumar, Neha Berry
Correspondence – Manav Wadhawan – drharishgupta108@gmail.com
Department of Gastroenterology, BLK S S Hospital, Pusa Road, Rajendra Place, New Delhi 110 005, India
Background and Aim Sarcopenia and myosteatosis have been associated with presence of minimal hepatic encephalopathy (MHE) in western studies. We aimed to evaluate association of MHE with sarcopenia and myosteatosis in patients with cirrhosis along with correlation of venous ammonia level with these parameters.
Methods Consecutive cirrhotic patients presenting to out-patient department of gastroenterology department at BLK Hospital, New Delhi, between January 2020 to June 2021 were screened for presence of MHE, sarcopenia and myosteatosis. Patients with MMSE ≥24 underwent PHES battery tests and PHES ≤ -5 was considered diagnostic of MHE. Transverse CT image at L3 level was selected for quantitative analysis of muscle mass. Sarcopenia was defined as L3 SMI < 31.83 cm2/m2 for females and < 39.59 cm2/m2 for males (validated in Indian population). Myosteatosis was defined as < 41 HU in patients with BMI (kg/m2) ≤ 24.9 and < 33 in those with BMI ≥ 25.
Results Total 100 patients (70% males) underwent PHES test, venous ammonia measurement and CT evaluation. Mean age and corrected BMI (dry body weight) of study population were 51.50 ± 9.28 years and 25.58 ± 3.60 kg/m2 respectively. Prevalence of MHE, sarcopenia and myosteatosis was 54%, 28% and 36% respectively. Mean venous ammonia level (ug/dL) in sarcopenia/non-sarcopenia and MHE/non-MHE were (79.99±16.13 vs. 63.04±22.68 [p<0.001]) and (81.59±15.14 vs. 51.57 ± 18.13 [p<0.001]) respectively. MHE was significantly associated with sarcopenia (p=0.002, OR [odds ratio] 4.58]) and showed trends toward significance with myosteatosis (p=0.057, OR 2.27). On multivariate analysis, other predictors of MHE were MELD-Na (p=0.034, OR 1.32) and venous ammonia level (p<0.01, OR 1.48).
Conclusion MHE is significantly associated with sarcopenia. Venous ammonia is strong predictor of both sarcopenia and MHE. Future studies should be directed towards ammonia lowering therapy as treatment option for sarcopenia
Keywords Cirrhosis. PHES. Sarcopenia. Myosteatosis. MELD-Na. Venous ammonia
325
Frailty index and nutritional assessment in patients with cirrhosis: A single centre experience
Praveen Sharma , Ashish Kumar, Anil Arora, Shayesta Jan, Ishrat Ara
Correspondence – Praveen Sharma - drpraveen_sharma@yahoo.com
Department of Gastroenterology, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Frailty is associated with increased mortality and hospitalization in patients with cirrhosis. There is scarcity of data on nutritional assessment and liver frailty index in cirrhosis in Indian patients.
Aim To assess liver frailty index (LFI) and its correlation with severity of liver disease and nutritional status in patients with cirrhosis.
Method Patients (age;18 yr) with cirrhosis were enrolled. Each patient underwent anthropometric testing including BMI (body mass index), dry BMI calculation, HGS (hand grip strength), MAC (mid arm circumference), MAMC (mid arm muscle circumference) and CM (calf muscle). Dietary intake was determined by 24-h diet recall and food frequency questionnaire and Frailty Index with frail defined as LFI ;4.5.<strong.
Results One hundred and eighty-seven patients screened and 150 patients enrolled. One hundred and twenty-ome (81%) males and 29 (19%) were female. Mean age VB 54 and plusmn;14 years and Child’s A:B:C:39:62:49. Fifty-nine of 150 patients (39%) were frail according to LFI. There is significant difference between CTP score, SGA score, MAMC, CC and total calories and protein intake between frail patients and non- frail patients. There was no difference in MELD score between frail and non-frail patients. In multivariate analysis MAMC (p=0.01, 1.20 [1.03-1.4]), CC (p=0.02, 0.83 [0.72-0.97]), age (p=0.003, 1.05 [1.01-1.08]), CTP score (p=0.02,1.3 [1.03-1.65]) and SGA (p=0.004,0.16 [0.04-0.55]) to significantly correlated with liver frailty index.
Conclusion Frailty is common (39%) in patients with cirrhosis and is correlated with MAMC, CC, age, CTP score and SGA score and showed no correlation with MELD score.
Keywords Liver Frailty index, Cirrhosis, Nutrition
326
Fabrication of extracellular matrix-based nanofiber scaffolds to support functional hepatocytes
V Ashwini, Indu Sharma, Impreet Kaur, Sundarrajan Subramanian1, Dinesh Mani
Tripathi, Savneet Kaur
Correspondence – Savneet Kaur – savykaur@gmail.com
Departments of Molecular and Cellular Medicine, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj Road, New Delhi 110 070, India, and 1Mechanical Engineering Scientist, National University of Singapore, Singapore 119077. Singapore
Background and Aim Native extracellular matrix can affects cell viability and modulate cell functions. Keeping in mind the important role of the ECM, here we fabricated novel nanofiber scaffolds using liver extracellular matrix (LEM) to promote functions of primary hepatocytes in culture.
Methods Eight-week-old Sprague Dawley rat liver was decellularized with detergents and characterized with H&E staining and DNA content estimation. The nanofiber scaffolds were prepared by electrospinning method with PLA (Poly Lactic Acid) and powdered 10% LEM in the ratio 1:1 with HFIP (Hexafluroisopropanol) as solvent. The scaffolds were electrospun at 1.5 mL/h at a distance of 12 cm and at 15 kv. The fabricated scaffolds were characterized by scanning electron microscopy. Primary hepatocytes were isolated using collagenase perfusion and cultured on PLA, collagen and LEM nanoscaffolds. Plated cells were characterized for viability and functions by molecular methods after two weeks of cultures.
Results The histology based microscopic analysis revealed a complete absence of cells in histology in the decellularized liver. Masson’s Trichrome (MT) staining for collagen depicted a significant staining for this matrix protein. DNA content analysis showed complete nuclei removal and significant DNA decrease in the decellularized liver in comparison to the control liver. The pore size and fiber diameter of the newly developed LEM-nanoscaffolds; (44 + 2.5 um) was similar to that of the native liver. There was an increase in viability and albumin-positivity by about 2-fold and 4-fold respectively in hepatocytes plated on LEM-nanoscaffolds as compared to those plated on collagen alone. Also the levels of secreted albumin was significantly higher in cells plated on LEM-nanoscaffolds as compared to those plated on PLA or collagen alone (P;lt; 0.05 each).
Conclusion Hepatocytes seeded on novel;LEM based nanofibrous scaffolds show enhanced functions and can serve as an excellent platform for varied applications such as ex vivo; drug testing.
Keywords Liver extracellular matrix, Nanofibers, Hepatocytes, Electrospinning, Albumin, Drug testing
327
Direct measurement of intra-abdominal pressure as a short-term predictor of hepatorenal syndrome: A prospective study
Shivabrata Dhal Mohapatra , Srijaya S Sreesh, Asif N Iqbal, Rushil Solanki, Krishnadas Devadas
Correspondence – Srijaya S Sreesh – srijaya_sreesh@rediffmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background Hepatorenal syndrome (HRS) is a serious complication of cirrhosis associated with a short survival. It is characterized by renal arterial vasoconstriction, which may precede clinically manifest renal dysfunction. The primary aim of our study was to obtain the best cut-off value of IAP in predicting HRS occurrence in decompensated cirrhosis over 6 months. We also tried to find out other clinical and biochemical factors associated with the development of HRS.
Methods A prospective follow-up study of 60 decompensated cirrhotics with tense ascites; was done. All underwent intraabdominal pressure measurement by direct method at the time of initial admission. Baseline clinical and laboratory results were obtained. Patients were followed up for 6 months to look for the development of HRS
Results IAP was measured in 60 patients with tense ascites and we got values ranged from 10 cms of ascitic fluid to 25 cms of ascitic fluid with a mean value of 17.12 cms with a median value of 16 cms. ROC curve was plotted and cut off value of 17 cm (AUROC: 0.935 [0.840; 0.982]) was deriv ed, with 83.33% sensitivity and 94.44% specificity for predicting the occurrence of HRS in 6 months. Correlation of IAP with other variables was studied and found that RRI has a significant correlation with IAP (r=0.617, p 0.001). We compared the 2 groups (IAP 17 vs. IAP; 17) (n=22 vs. 38), We found that higher blood urea, higher S. creatinine, higher RRI values was more in patients with IAP; 17 (p=0.05). In multivariate analysis we found that IAP;17 cms of ascitic fluid is a significant predictor of development of HRS and mortality over a period of 6 months (p;0.005).
Conclusion IAP is a novel non-invasive diagnostic screening tool to predict the development of HRS in decompensated cirrhosis.
Keywords Decompensated cirrhosis, IAP, RRI, HRS.
328
Hepatorenal syndrome-acute kidney injury in decompensated cirrhosis versus acute-on-chronic liver failure: A comparison of response rates and predictors of response to therapy with terlipressin and albumin
H Vijay Narayanan , Ravindra Pal, Rushil Solanki, Antony George, N Premaletha, Krishnadas Devadas
Correspondence – Vijay Narayanan H – vijaynh@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction A combination of terlipressin and albumin is the first-line pharmacologic treatment for hepatorenal syndrome-acute kidney injury (HRS-AKI). The early identification of patients with a low likelihood of response to treatment is crucial, as they can be fast-tracked for liver transplantation. There is limited data on the use of vasoconstrictors for HRS-AKI in acute-on-chronic liver failure (ACLF). We aimed to compare the response rates to terlipressin-albumin therapy in patients with decompensated chronic liver disease (DCLD) and ACLF and determine early predictors of treatment response.
Methods Patients diagnosed to have HRS-AKI (based on IAC criteria) and treated with terlipressin and albumin were included. ACLF was determined by the APASL definition. Univariate and multivariate logistic regression analysis was used to determine parameters that were predictive of HRS reversal.
Results One hundred and twenty-two patients with HRS-AKI were included- 84 had DCLD and 38 ACLF. In DCLD patients, there was complete response (CR) to therapy in 54.8%, partial response in 14.3%, and no response in 31%. The independent predictors of complete response to treatment were the presence of systemic inflammatory response syndrome (SIRS) at baseline (p=0.016, OR-6.19 [CI:1.40-27]) and reduction in renal resistive index (RRI) >5% by day3 (p=0.001, OR=24.2 [CI:3.4-168.6]). Other factors associated with CR were baseline creatinine< 2.5 mg/dL (p<0.001) and rise in mean arterial pressure (MAP) >5 mmHg by day 3 (p<0.001). Non-responders had higher 6-month mortality (74% vs. 45%, p=0.024)
In ACLF patients, there was CR in 57.9% ,10.5% partial response and 31.6% non-responders. APASL grades 1,2,3 had response rates of 75%, 62.5% and 40% respectively. Factors associated with CR were bilirubin <10 mg/dL (p=0.03), baseline creatinine <2.5 mg/dL (p=0.017), resolution of SIRS by day-3 (p=0.004), RRI reduction>5% by day-3 (p<0.001), MELD<30 (p=0.002) and AARC score<10 (p=0.032). Non-responders had higher 28-day mortality (62% vs. 37% p=0.002).
Conclusion SIRS and RRI are simple parameters to predict treatment response in HRS-AKI. RRI reflects intrarenal vasoconstriction and SIRS reflects exaggerated systemic inflammation, both of which are reversed by terlipressin, leading to an enhanced treatment response.
Keywords Acute kidney injury, ACLF, Cirrhosis, Hepatorenal syndrome, Terlipressin
329
Prognosticating stage 3 acute kidney injury in liver cirrhosis: A prospective study
A Deiva1, M Jayakumar1, V Y Bhargav2, Jayanthi Venkataraman2
Correspondence – Bhargav V Y – varanasi.b4@gmail.com
Departments of 1Nephrology, and 2Hepatology, Sri Ramachandra Medical College, Porur. Chennai 600 116, India
Background Renal failure is a common complication in patients with chronic liver disease and it is one of the most important risk factors associated with increased mortality. The development of acute kidney injury (AKI) in patients with cirrhosis has significant prognostic importance. Stages of AKI determine the prognosis and mortality in chronic liver disease.
Aim To determine the risk factors, clinical profile and treatment response in cirrhotic patients with AKI.
Methods The study included 130 patients with liver cirrhosis diagnosed clinically, biochemically, and confirmed with imaging (USG abdomen or CT abdomen). Patient profile was noted and followed up in subsequent admissions. AKI criteria were charted based on creatinine or urine output and was recognized. The criteria-based staging was done into AKI stages 1, 2 and 3 and treatment was given with albumin alone or with albumin + terlipressin. Response to treatment noted and prognostication done.
Results Among 130 patients with cirrhosis, 117 were males (90%); the mean age was 50.43 +10.2 years. The overall prevalence of AKI in the study was 27.7%. Complications like hepatic encephalopathy (0.020), spontaneous bacterial peritonitis (0.02), sepsis (<0.001), and shock (0.002) were significant in those with AKI and were statistically significant. Patients with stage 3 AKI were significantly older than those belonging to Stages 1 and 2 (0.043). Mortality was significantly high in those with AKI compared with no AKI (<0.001). More patients in Stage 3 required terlipressin infusion along with albumin therapy (0.0409) with a lower AKI recovery (0.008) and high mortality (0.001).
Conclusion Stage 3 AKI had decreased responsiveness to terlipressin with a poor prognosis and increased mortality.
Keywords Acute kidney injury, Cirrhosis of liver, Albumin, Terlipressin
330
Comparison of performance of 5 prognostic scores in predicting short term mortality in acute on chronic liver failure
Rushil Solanki , Nidhin Raveendran, Vijay Narayanan, Shivabrata Dhal Mohapatra, Krishnadas Devadas
Correspondence – Rushil Solanki – rushilsolanki808@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background Acute-on-chronic liver failure (ACLF) is having a very high short term mortality and a rapid downhill course. Apart from the traditional prognostic indices used in cirrhosis, various agencies have proposed scores to predict the survival of these conditions. Their validity remains to be tested in outside cohorts. This study analysed and compared the accuracy of 5 important prognostic scores in ACLF.
Methods One hundred and forty-three patients with ACLF according to the APASL criteria were included in the study. Base line characteristics, CTP, MELD, AARC, CLIF C, and CLIF C ACLF scores were assessed within 24 hours of admission to the hospital. Survival after 28 days was recorded. The diagnostic performances of different scores were calculated and compared using ROC curve statistics.
Results Alcohol (34%) followed by HBV (24.1%) were the most common acute events. The 28-day mortality was 28%. Mortality was 3% in grade 1, 17.1% in grade 2 and 76.5% in grade 3 ACLF. 52.4% of the patients also satisfied EASL CLIF definition of ACLF with mortality of 47%. AUROCs for CTP, MELD, CLIF C, CLIF C ACLF and AARC scores were 0.737, 0.789, 0.837, 0.843 and 0.847, on ROC analysis. AARC score has the highest AUROC (0.85) among patients with alcoholic hepatitis and CLIF C ACLF has the highest AUROC (0.90) among patients with HBV reactivation.
Conclusion Patients with ACLF defined by APASL criteria has high short term mortality. AARC score is the best predictor of short-term survival and is superior to CTP and MELD scores.
Keywords ACLF, Predictors of ACLF, Prognostic factors in ACLF
331
Living donor liver transplant in a rare case of argininemia
Monalisa Sahu 1 , Dharmesh Kapoor 2
Correspondence – Dharmesh Kapoor - dkapoor@gmail.com
Departments of 1Infectious Diseases, and 2Hepatology and Biliary Diseases, Yashoda Hospitals, Alexander Road, Kummari Guda, Shivaji Nagar, Secunderabad 500 003, India
Introduction A three-year-old girl child, born out of consanguineous marriage, presented initially at the age of one-and a half years with complaints of difficulty in walking, for which she was evaluated by pediatrician, and diagnosed to have spastic paraplegia. She also had two episodes of UTI in last 4 months.
Methods Her MRI brain showed delayed white matter of pons, medulla oblongata, bilateral cerebellar hemishpheres, bilateral fronto-temperoparietal and occipital lobes at subcortical and juxtaventricular regions, suggestive of dysmyelination disorder secondary to inborn errors of metabolism. She was worked up in detail, and detected to have argininemia, a urea cycle defect. Her USG abdomen showed hepatomegaly with altered echotexture. Triphasic CT abdomen showed hepatomegaly, patent hepatic arterial tree, patent splenoportal axis, and hepatic veins. It also showed bilateral pyelonephritis with focal nephrosis in left kidney. Her electrophysiological study was suggestive of multiple epilectic activity over both hemispheres, predominantly over right anterior mid temporal region.
She was evaluated for liver transplantation at our centre and was deemed fit for the same after a multidisciplinary team meeting comprising of hepatologist, pediatrician, transplant surgeon, infectious disease specialist, cardiologist, nephrologist, neurologist, psychiatrist and anesthesiologist. Her father, a 32-year-old man, healthy came forward to donate a portion of his liver and was found suitable and fit.
The living related donor liver transplant (left lateral segment) was undertaken.
The recipient liver was nodular, cirrhotic, with no obvious SOL. The post-operative period was uneventful, and she was discharged on D14 of the surgery. At 3 months follow-up, the graft liver (LDLT) was normal in architecture and no focal lesion. The child is doing well at 9-month follow-up.
Conclusion The difficult and rare case of urea cycle defect, with multiple other co-morbidities was taken up for transplantation, and with multi-disciplinary approach, ensuring a successful outcome.
Keywords Argininemia, Spastic paraplegia, Liver transplant
332
A unique presentation of obstructive jaundice, severe cholangitis and ascites in a post chemoradiation patient
Shivabrata Dhal Mohapatra , N Premaletha, Srijaya S Sressh, Jithin John, Avisek Chakravorty, Aditya Verma, A S Jacob Raja
Correspondence – Shivabrata Dhal Mohapatra – dilumkcg2@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Hydatid cystis caused by Ecchinococcous granulosus and multilocularis. Humans (accidental host) get infected by eating food contaminated with dog (definitive host) feces. Liver is the most common site (70%) followed by lungs (20%), kidneys, spleen, brain and bone. One of the rare presentation is obstructive jaundice with ascites.
Case Summary Sixty-nine-year-old female with prior history of carcinoma cervix treated 2 years back with chemoradiotherapy was admitted with painless progressive obstructive jaundice of 3 weeks duration and 5 days history of fever and chills. On examination there was icterus and hepatomegaly. Investigation showed Hb-11.1 gm%, TLC-14200/cumm neutrophil predominant, bilirubin (T/D)-24.5/13.1, SGOT/SGPT-132/100, ALP-401 (125), total protein/albumin-6.2/2.8, CRP-66 (5), blood urea/creatinine-42/1.1, tumor markers -not elevated. Ascitic fluid analysis- low SAAG (0.7), highprotein (3.8g%). Ultrasound abdomen- multiple cystic lesions in liver, IHBRD and ascites impression :- cystic metastasis and malignant ascites. MRI revealed multiple lesions markedly hyperintense on T2 with peripheral hypointense rim and the finding of cyst within cyst appearance was consistent with hydatid cyst. There was capsular breach with subdiaphragmatic extension of one cyst with rupture and moderate ascites. Another cyst was seen to compress the biliary confluence to produce bilateral IHBRD with features of cholangitis and multiple cholangitic abscesses. Confirmatory test Ecchinococcal serology (ELISA) was positive. Ascitic fluid cytology was suggestive of Hydatidosis. Antibiotics Meropenem and Tigecycline were initiated. In view of ECOG status 4, she underwent percutaneous biliary drainage. After 14 days of antibiotics along with Albendazole 400 mg BD she improved and became fit for discharge.
Conclusion This case brings attention to the unique presentation of hepatic hydatid cyst from a non-endemic region causing obstructive jaundice, severe cholangitis and rupture, in the setting of previous malignancy. This underlies the need to consider other etiologies also for cystic lesions liver in a patient with malignancy.
Keywords Hydatid cyst, Obstructive jaundice
333
Chemokine (CXCL12-CXCR4) axis is the key player in pulmonary remodeling and development of porto-pulmonary hypertension in experimental cirrhosis
Dinesh Tripathi 1 , Akash Kumar Mourya 1 , Impreet Kaur 1 , Pinky Juneja 1 , Ashwani Vasudewan 1 , Vivek Kumar 2 , M P K Reddy 2 , Kailash Kohle 3 , Savneet Kaur 1 , Shiv Kumar Sarin 4
Correspondence – Dinesh Tripathi – dineshmanitripathi@gmail.com
Departments of 1Liver Physiology and Vascular Biology, Molecular and Cellular Medicine, 2Cardio-Respiratory Physiology and Appld. Physiology Defence Inst. of Physiology and Alld. Sciences, 3Gastroenterology, and 4Hepatology, Institute of Liver and Billiary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Background and Aim Porto-pulmonary hypertension (PoPH) is a clinical indication occurring due to portal hypertension (PHT). Endothelin (ET), thromboxane A2, glucagon, known to be associated with PoPH. The mechanisms underlying PoPH remain enigmatic due to lack of representative animal models. The present study investigated the underlying mechanism of PoPH.
Methods Semaxnib (VEGFR-antagonist, 20 mg/kg) used to induce pulomary arterial hypertension. Healthy controls (Gr1), + Semaxnib (Gr2), CCl4 cirrhotic rats (Gr3), + Semaxinib (Gr4) were compared. Right ventricular systolic pressure (RVSP) and portal pressure (PP) were assessed. Heart and pulmonary artery function was monitored with 2D echocardiography, histomorphological, cellular and molecular analysis.
Results Cirrhotic animals showed significantly raised PP (15.57±0.6; +117% (Gr3), 14.97±2.0; +109% (Gr4); p=0.01, vs. 7.15±0.8 (Gr1), 8.75±0.5 mmHg (Gr2) with increased hepatic vascular resistance (HVR, p=0.001) and portal blood flow (PBF, p=0.05) in comparison to non-cirrhotics. RVSP was significantly (p=0.01) higher (36.3±3.4, +100% (Gr2), 42.72±2.6, +137% (Gr3), 40±7.9, +122% (Gr4) in comparison to Gr1 (18.2±1.73 mmHg). Echocardiography analysis revealed RV hypertrophy and dilation, confirming PoPH in Gr3, Gr4 and PAH in Gr2. Investigations indicated endothelial/smooth muscle proliferation, thickening, and narrowing of PA including pulmonary fibrosis (Gr3 and Gr4 vs. Gr1 and Gr2, p<0.05) and raised inflammatory cells infiltration. Mechanistically, in lungs of Gr2, 3 and 4 animals, SMC specific genes were significantly upregulated (p<0.05), ET-1 (+18,+7,+21), ETAR (+5,+3,+5), CXL12 (+15,+6,+14), CXCR4 (+2,+2,+7) and its effectors, PDGF (+9,+4,+5), anti-apoptotic BCL2 (+10,+2,+10), in comparison to Gr1. The significant (p<0.05) differential expression of CD31 (+13, +9, +8) and ETBR (-3,-4,-3), confirming the endothelial dysfunction in lungs (+/- fold change).
Conclusion This study demonstrated first time a raised RVSP in cirrhosis, further aggravated with VEGFR antagonist, providing an evidence for PoPH establishment with PHT. Preliminary data revealed the involvement of chemokine axis in pulmonary remodeling in the development of POPH, which needs further clinical evaluation.
Keywords Portal hypertension, Pulmonary arterial hypertension, Vascular remodelling
334
A case of persistent transaminitis due to rhabdomyolysis due to entecavir in chronic hepatitis B patient with underlying chronic kidney disease
Viswanath Reddy Donapati
Correspondence – Viswanath Reddy Donapati - viswanathdr@yahoo.com
Department of Gastroenterology, Yashoda Hospital, Alexander Road, Kummari Guda, Shivaji Nagar, Secunderabad 500 003, India
Background Oral antivirals for hepatitis B treatment are known to cause rhabdomyolysis in a small proportion of patients. We hereby describe a case of patient with chronic kidney disease who had high transaminases due to Hepatitis B and rhabdomyolysis.
Methods/Case Report Fifty-two-year old male, a patient of chronic kidney disease due to diabetic nephropathy, was initiated on dialysis and in a few weeks was screened positive for hepatitis B with high viral load. Antiviral entecavir was initiated elsewhere and within 5 days presented with pain and weakness in all 4 limbs. He also complained of itching and anorexia. On evaluation, he had elevated liver enzymes, LDH and CPK levels. Entecavir was stopped and tenofovir alafenamide was initiated twice a week and the transaminases improved gradually. He was given liver supportive therapy. His transaminases took time to normalise as well as weakness which recovered more slowly.
Results/Conclusions We describe a case of drug induced rhabdomyolysis in a patient with chronic hepatitis B, presenting with hepatitis and quadriparesis. His transaminases and quadriparesis took time to improve and was doing well with change of antiviral to tenofovir alafenamide. Entecavir may be avoided in the patients with chronic kidney disease in whom tenofovir alafenamide may be safer.
Keywords Drug induced rhabdomyolysis, Entecavir, Tenofovir alafenamide, Chronic kidney disease, Transaminitis
335
Elasticity characterization of malignant and benign liver lesions by two-dimensional shear wave elastography
H Vijay Narayanan , Bony George, Jijo George, Antony George, Krishnadas Devadas
Correspondence – Vijay Narayanan H – vijaynh@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background Detection and characterization of focal liver lesions (FLLs) poses a frequent challenge in clinical practice. 2D-Shear Wave elastography (2D-SWE) is a recent technique which uses acoustic radiation force to induce mechanical vibrations and assess tissue elasticity.
Aims To study the elasticity characteristics of focal liver lesions by 2D shear wave elastography and to determine whether it can be used to differentiate benign from malignant lesions.
Methods All patients with FLL underwent 2D-SWE and elasticity quantification. Contrast enhanced CT or MRI findings were used as the reference method for the diagnosis of FLLs.
Results Two hundred and sixteen patients with FLL were evaluated by the 2D-SWE. One hundred and thirty patients had malignant FLLs of which 90 had hepatocellular carcinoma (HCC), 20 had intrahepatic cholangiocarcinoma (IHCC) and 20 had metastatic lesions. Of the 86 benign FLL, there were 36 hemangiomas, 12 FNH, 24 simple cysts, 4 complex cysts, and 10 abscesses. Mean liver stiffness of various lesions by 2D-SWE was 65.7 (IHCC), 60.5 (HCC), 45.4 (metastases), 7.6 (hemangioma), 16.9 (FNH), 9.14 (abscess), 8.62 (simple cyst) and 2.95 (complex cyst). ROC analysis revealed that a SWE cut off of 40 kPa could distinguish between benign and malignant lesions with sensitivity of 100% and specificity of 80%. (AUROC of 0.871).
Stiffness Ratio = Shear wave of lesion/Shear wave of background liver parenchyma.
The lesion to background liver parenchyma stiffness ratio in cirrhotic patients was 4.81 for IHCC, 3.16 for metastasis and 1.93 for HCC. Therefore in cirrhotic patients, a lesion to liver stiffness ratio < 2 along with SWE of lesion more than 40 kpa favors HCC. However, in non-cirrhotic livers, there was no statistically significant difference between stiffness ratio of various malignant focal lesions.
Conclusion 2D-SWE could be a useful non -invasive method for the differentiation of benign and malignant focal lesions of liver.
Keywords Focal liver lesion, Lesion stiffness, 2D-SWE, Stiffness ratio
336
Post transarterial chemoembolization (TACE) hepatocellular carcinoma response assessment by modified response evaluation criterion in solid tumors and short-term post TACE survival
H Vijay Narayanan , Bony George, Susan George, Krishnadas Devadas
Correspondence – Vijay Narayanan H – vijaynh@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Transarterial chemoembolization (TACE) can improve the overall survival of patients with intermediate-stage hepatocellular carcinoma (HCC). A modified response evaluation criterion in solid tumours (mRECIST) is used for evaluation of the treatment response in patients after TACE. We tried to evaluate the response and survival in patients after TACE.
Methods Patients underwent superselective TACE with Epirubicin. The mRECIST response was calculated after 6 weeks using MRI. Predictive factors were calculated for response and survival.
Results Forty-two patients with intermediate HCC were analyzed. The mean age was 59.12 ± 8.74 years. The predominant etiology was NASH in 31% and alcohol in 23.8%. Twenty-three patients had complete response(CR), 8 patients had partial response (PR), 4 patients had stable disease (SD) and 7 patients had progressive disease (PD), as per mRECIST criteria. Objective response (OR) was defined as patients having either CR or PR and poor response (PoR) as patients having either SD or PD. 73.8% had an objective response and 26.2% had a poor response. HAP score (p=0.003) and CHILD stage (p=0.011) were the most important predictive variables for the mRECIST response. Mortality was highest among the patients with poor response, 8/11 (72.7%). 10/31 (32.2%) patients with objective response died during the follow-up period. Mean survival was significantly higher in patients with OR (25.64 months) than in patients with PoR (13.1 months), p=0.001. mRECIST response predicted survival among the patients on univariate analysis (HR=1.08, p=0.02). The independent predictors for survival were post-TACE decompensation (B-1.43, p=0.03), ECOG performance status (B-1.41, p=0.010), and the number of lesions (HR 2.20, p=0.017).
Conclusion Use of TACE in intermediate stage HCC patients gives a significant survival advantage when objective response is achieved as per mRECIST. Proper selection of the patients for TACE is important for objective response and survival.
Keywords TACE, mRECIST, OR, HAP score
337
Risk factors associated with nontumoral portal venous thrombosis in patients with decompensated cirrhosis: A case control study
Shivabrata Dhal Mohapatra , N Premaletha, Rushil Solanki Harjivan, Avisek Chakravorty, A S Jacob Raja, Asif N Iqbal, Srijaya S Sreesh, Krishnadas Devadas
Correspondence – Srijaya S Sreesh - srijaya_sreesh@rediffmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background Portal vein thrombosis (PVT) is defined as occlusion of the portal vein or its branches of splenoportal axis. Incidence of PVT in compensated liver disease is 0.6% to 5% and up to 25% in DCLD. Presence of PVT is associated with significant morbidity and mortality. Identification of the factors associated with benign PVT can help in early goal directed therapy.
Aim To assess the prevalence and factors associated with PVT in decompensated cirrhotics without HCC, with patients without PVT as the control group.
Methods We prospectively enrolled 243 patients with decompensated cirrhosis at the Government Medical College, Thiruvananthapuram from September 2020-September 2021. All patients underwent detailed clinical history and evaluation, baseline investigation and ultrasonography. CECT Abdomen was performed in patients with USG evidence of PVT or alteration in portal flow dynamics.
Results Thirty-three patients were excluded. On analysis of selected variables of 210 patients- 30 had PVT (12.3%). NASH related (43.3% vs. 17%), duration of cirrhosis >4 years (56.7% vs. 24.4%), first decompensation as UGIB (66.7% vs. 27.8%), >1 UGIB (56.7% vs. 22.2%), >1 EVL (60% vs.17.2%), low platelet (<64000) (50% vs. 27.7%), SAAG>1.9 (78.9% vs. 45.9%), ascitic fluid albumin <0.7 g% (87% vs. 14.4%), PV diameter >13.7 mm (70% vs. 14.4%), PVV <12 cm/sec (73.3% vs. 13.9%) and spleen size>13.6 cm (79.3% vs. 42.9%) were significantly associated with PVT. There was no difference between CHILD B/C status or MELD Na among the 2 groups.
On Logistic regression analysis, ascitic fluid albumin, SAAG, EVL sessions, PV diameter were significant risk factors for the development of PVT in DCLD (p<0.001).
Conclusion Disarray of the delicate coagulation cascade occurs in tandem with the severity of liver disease. In our study the association of low ascitic fluid albumin, high SAAG, low platelet as markers of extent of cirrhosis, low PVV indicating sluggish flow and multiple EVL sessions that trigger thrombosis in the splenoportal axis have been significantly associated with PVT in DCLD, with NASH as independent etiology.
Keywords Decompenated cirrhosis, Non-tumoral portal vein 281atient281d281, Risk factors
338
Down-regulation of EOMES but high T-bet and BLIMP drives exhaustion and short-lived effector CD8 T-cells in HbsAghi © chronic hepatitis B virus infected patients
Ravinder Singh 1 , Mojahidul Islam 1 , Jayesh Kumar Sevak 1 , Manoj Kumar Sharma 2 , Shiv Kumar Sarin 2 , Nirupama Trehanpati 1
Correspondence – Nirupama Trehanpati- trehanpati@gmail.com
Departments of 1Molecular and Cellular Medicine, and 2Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi 110 070, India
Background and Aim Persistence of chronic HBV infection is due to depletion and dysfunctional CD8 T cells. Eomesodermin (EOMES) is a T-box transcription factor and act as a key regulator and modulator for the expression of inhibitory molecules like PD-1, TIM3, CTLA-4, CD39. Our aim was to investigate mechanism of immune cells exhaustion in HbsAglo and HbsAghi © CHBV patients.
Methods We have included 36 © CHBV (nCHBV; not on any anti-viral treatment) patients with HbsAg < 2000 IU/mL (HbsAglo Gr. I, n=9) and HbsAg > 2000 IU/mL (HbsAghi) (Gr. II, n=27), HBV DNA (<2,000 IU/mL or >2,000 IU/mL) with increased ALT/AST >1.2 x ULN, and healthy controls (HC, n=10). Blood sample was used for virological assessment, plasma analytes and high dimensional flow cytometry to analyze co-expressing inhibitory molecules and transcription factors on CD4/CD8 T and B cells.
Results Peripheral blood CD8 and CD4 T cells showed significantly (p< 0.05) high expression of PD1 in © CHBV infected patients compared to HC. Further nCHBV patients with HbsAghi, showed significantly low expression of EOMES expressing CD8 T cells but with high BLIMP (p=0.011) and high T-bet (p=0.034), a phenotypic character of short-lived effector cells (SLEC) compared to HbsAglo patients. Additionally, cytokine bead array revealed lower levels of IFNγ, TNF-α and higher soluble PD1, TIM3, CTLA4, LAG3, PDL1, in plasma of nCHBV patients.
Conclusion In HBSAghi nCHBV patients, lower expression of EOMES drive short lived effector T cells with terminal exhaustion of CD8 T by PD1 which helps in persistence of chronic HBV infection.
Keywords © chronic hepatitis B virus (nCHBV), EOMES, T-bet, Tim3, CTLA4
339
Maturation defect in erythroid progenitors is the unknown cause of severe anemia in cirrhotic patients
Deepika Lal 1 , Rakhi Maiwall 2 , Aniruddha Dayama 2 , Sukriti Baweja 1 , Chhagan Bihari 3 , Anupam Kumar 3 , Shiv Kumar Sarin 2
Correspondence – Anupam Kumar – dr.anupamkumar.ilbs@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Hepatology, and 3Pathology, Institute of Liver and Biliary Sciences, D1, Vasant Kunj, New Delhi 110 070, India
Background and Aim Anemia is seen in nearly 70% patients with cirrhosis. It is often nonresponsive to nutritional supplements. Bone marrow (BM) in these patients shows erythroid hyperplasia with dyserythropoiesis. In this study, we aim to investigate the alterations in erythropoiesis in cirrhotic patients.
Methods BM aspirates were collected from 32 cirrhotic patients (16 alcoholics, 16 non-alcoholic steatohepatitis) with mean age 50 including both male (n=22) and female (n=10) without nutritional deficiency. MELD-Na score of patients ranges from 6-40. Control sample (n=3) were taken from non-liver disease patients. Erythroid differentiation was investigated using antibodies CD34+, CD71+ (early erythroid cell marker), CD235a+ (mature erythroid cell marker) through flow cytometry. Cellular reactive oxygen species were measured by 2’,7’-dichlorodihydrofluorescein diacetate fluorescent probe. The levels of genes associated with hemoglobin synthesis were measured using quantitative real time – polymerase chain reaction.
Results Total CD34+ cells population (p=0.02) was significantly reduced and early erythroid progenitors CD71+ population (ALD p=0.009, NASH p=0.002) was significantly high in cirrhotic group as compared to control. Intermediate erythroid progenitors (CD71+CD235a+) population (ALD p=0.004, NASH p=0.0003) was significantly reduced whereas matured erythroid progenitor (CD71-CD235a+) population (ALD p=0.03, NASH p<0.0001) was increased with increase in MELD-Na score (> 10), (Fig. A). Moreover, mean flouroscence intensity (MFI) of CD235a+ marker was found to be decreased to moderate or dim with decrease level of hemoglobin (Fig. B). ROS generation in CD34+ and erythroid progenitors was significantly increased (CD34+ p= 0.02, ROS CD34+ p=0.012, CD71+ p=0.02, CD235a+ p=0.003) in cirrhotic patients (Fig. C). Genes associated with hemoglobin synthesis ALAS1, HMOX, BACH1 and Alfa globin1 were found to be 2-fold down regulated in cirrhotic patients than controls.
Conclusion A decrease in CD71+ erythroid progenitor cell population and a defect in their maturation in the bone marrow contributes to anemia of chronic liver disease.
Keywords Anemia, Cirrhosis, Erythropoiesis
340
Changing pattern in hepatocellular carcinoma
Sreevidya Pillai
Correspondence – Sreevidya Pillai - drsreevidyapillai@gmail.com
Department of Medical Gastroenterology, Lakeshore Hospital and Research Centre, NH 47 Byepass, Nettoor, Maradu, Ernakulam 682 040, India
Background and Aim Hepatocellular carcinoma (HCC) is a major health problem in emerging world. In recent years, the epidemiological scenario has been changing, incidence of HCC due to NAFLD is increasing worldwide. Our study is to analyse current changing pattern in HCC and to compare profile of HCC with non-alcoholic steatohepatitis (NASH) and non-NASH etiology.
Methods We did a prospective observational study of 127 newly diagnosed patient of age >18 years who came to the Department of Gastroenterology, Lakeshore Hospital during January 2019 to 283atient 2021. Statistical analysis done using SPSS and students t test.
Results Out of 127 HCC patients analyzed males comprised 89% and females 11%. Etiology being NASH (34%), alcoholic (52%), hepatitis B (10%) and hepatitis C (3%). Majority of patients presented without jaundice (NASH [80%] vs, non-NASH [84%]) and ascites (NASH [72%] vs. non-NASH [61%]). Portal vein thrombus in NASH (26%) vs. non-NASH (30%). NASH and non-NASH group showed no statistical difference in parameters including liver span -0.214 (-1.08 – 0.66) (p 0.628), max tumor diameter -0.617 (-2.2-0.97) (p 0.444), number of tumor 0.35 (-0.43-1.129) (p 0.372), total tumor diameter 0.34 (-2.57- 1.886) (p 0.762). In both group response to treatment was same, modalities used were TACE (59%), Sorafenib (29%), microwave (19%), liver transplantation (14%), RFA (8%), surgical resection (3%) and TARE (1%).
Conclusion Changing pattern of HCC epidemiology is increasingly noticed . Previous national and international surveys showed NASH as the etiology only in 10% of cases. In our study it is clearly evident that NASH as an etiology has increased to 34%. Also it is showed that there is no statistical difference between behavior of tumor in NASH and non-NASH group. Patients with high risk of NASH cirrhosis and HCC should be carefully screened for early detection of tumor.
Keywords Hepatocellular carcinoma, Non-alcoholic steatohepatitis
341
Spur cell anemic Child C cirrhotic patients have elevated levels of VWF and D-dimer
Deepika Lal 1 , Chhagan Bihari 2
Correspondence – Deepika Lal – deepika18021@gmail.com
Departments of 1Molecular and Cellular Medicine, and 2Pathology, Institute of Liver and Biliary Sciences, D1, Vasant Kunj, New Delhi 110 070, India
Objectives Spur cell anemia is a chronic form of anemia defined as a consequential condition in cirrhosis and generally associated with poor prognosis. the association between D-dimer and VWF in spur cell anemia has not been elucidated yet. Therefore, we aimed to evaluate the levels of VWF and D-dimer in liver cirrhosis patients with spur cell anemia.
Method Total 3 mL blood sample were collected in citrate tube from 2 subgroups of CLD patients with Child C. Total 27 CLD patients, in which without spur cells (group 1), 20 case in 7 patients in group 2 with spur cell anemia. Simultaneously, sonoclot assay were performed and then plasma was obtained by centrifugation at 3000 r·min-1 for 10 min used for VWF and D-dimer ELISA assay. Clinical and laboratory parameters including liver dysfunction and MELD-Na score were assessed.
Results Spur cells <10% (group 1) and >10% (group 2) mean plasma levels of VWF were significantly (5.98 ± 2.37 vs. 7.96 ± 1.82, p<0.05) and D-dimer levels were high in (48.92 ±33.86 vs. 65.42 ±37.00, p<0.05) in group 2. In Sonoclot revealed, platelet function were significantly better in group 1 (1.05 ± 0.99, 2.07 ± 1.49, p=0.05) whereas clot rate and ACT (26.97 ±10.12, 24.63 ±14.18, p=051; 189.33 ± 30.72, 215.86 ± 50.42, p>0.05) showed no significant difference between two groups. Other clinical parameters including hemoglobin (7.82 ± 1.71, 7.43 ± 1.1, p>0.05), platelets (70.11 ± 23.75, 68 ± 29, p>0.05) also were not significantly different.
Conclusion Elevated levels of VWF and D-dimers were noted in patients with spur cell anemia in Child C class in comparison to those without spur cell anemia. Both these factors indicates the increased probability of microvascular thrombi.
Keywords Spur cell, Cirrhosis, VWF, D-dimer
342
Liver abnormalities in patients with corona virus disease 2019
Archita Makharia , Manoj Lakhotia, Vineet Tiwari, K G Barupal
Correspondence – Archita Makharia – archita.makharia@gmail.com
Department of General Medicine, Dr Sampurnanand Medical College, Department of Medicine, Mahatama Gandhi Hospital, Olympic Road, Jalori Gate Circle, Jodhpur 342 001, India
Introduction Other than respiratory tract, many other organs, including liver, are affected in corona virus disease 2019 (COVID-19). COVID-19 can lead to deterioration of preexisting liver disease or can lead to hepatocellular damage. In a prospective, we reviewed the liver function abnormalities in patients with COVID-19.
Methods In a prospective study, we recruited 185 hospitalized patients with COVID-19. The diagnosis of COVID-19 was made on the basis of a positive RT-PCR report. Their clinical characteristics and the laboratory parameters were recorded in a proforma.
Results The mean age of patients was 52.7+16.2 years (66 females), 66 (34.2%) of whom were of age more than 60 years. Based on the clinical criteria 70.4%, 20.9% and 8% patients had mild, moderate and severe COVID-19 infection, respectively. The mean hemoglobin was 12.4+2.1 g/dL. 57.8% patients had elevated levels of either alanine aminotransferase (ALT) or aspartate aminotransferase (AST). 35.1 % had an elevation of ALT and 32.4 % had an elevation in both ALT and AST. Serum bilirubin was elevated in 10.6% and 48.9% had low serum albumin. While a correlation was observed between low albumin and severity of COVID-19, there was no correlation between severity of COVID-19 and hypertransaminasemia.
Conclusions One third of patients with COVID-19 had raised transaminases and half of them had low albumin. There was a correlation between low albumin and severity of COVID-19 infection.
Keywords COVID 19, Transaminases, Albumin
343
Elevated levels of systemic bacterial vesicles in autoimmune hepatitis are associated with non-response to corticosteroid therapy
Swati Thangariyal 1 , P Debishree Subudhi 1 , Purnima Tyagi 1 , Chhagan Bihari 2 , Shiv Kumar Sarin 3 , Sukriti Baweja 1
Correspondence – Sukriti Baweja – sukritibiochem@gmail.com
Departments of 1Molecular and Cellular Medicine, 2Pathology, and 3Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj Road, New Delhi 110 070. India
Introduction Autoimmune hepatitis (AIH) is characterized by self-perpetuating immune-mediated inflammatory liver damage with or without fibrosis. Corticosteroids remain the main stay of treatment. Microbiome-liver axis has been recognised as a major modulator of autoimmunity and sepsis. We investigated the presence and activity of bacterial Evs (BEVs) in plasma and their interactions with immune cells in AIH patients and their association with steroid response.
Methods Fractionated pre-therapy plasma of AIH patients (n=38, biopsy proven- noncirrhotic, F<4, international simplified score ³7, HAI score >4, ALT [148±58.4 U/mL], AST [140.7±60.2 IU/mL] [26 responders [R] and 12 non-responders [NR]) to corticosteroid therapy, and healthy controls (n=12) for BEVs (by ultracentrifugation using anti-OMPA [outer membrane protein A] and anti-LPS quantified using flow cytometry and western blot). PBMCs of AIH patients were primed with bacterial vesicles (OMVs-2 ug/mL) and (OMV+dynasore-80 uM, to block the entry of OMVs inside the cells) for 24 hour and analysed for frequency, activation of total T (CD3+CD4+CD8+) cells, mucosal associated invariant T (CD3+CD161+TCRva7.2+) cells, intracellular IL-17A and granzyme B release and B (CD19+) cells using multi-color flowcytometry.
Results Levels of systemic BEVs (OMPA+LPS+) were higher in AIH patients than controls (28.3±5.6 vs. 2.4±1.1 EV/uL; p<0.001), and were higher in moderate to severe than minimal to mild hepatic histological activity (p=0.042). At baseline, NR to corticosteroids had higher BEVs than R (39.6±10.8 EV/uL vs. 12.4±3.2; p<0.001 with AUC =0.71 CI [0.79-0.83]. Protein blots confirmed higher BEV-associated LPS and OMPA in plasma fractions of NRs than R (p=0.003). OMVs in NR PBMCs strongly stimulated the secretion of IL-17A (p=0.015) and granzyme B (p=0.052) from MAIT cells and also increased the frequency of activated MAIT cells (% MAIT+CD69+) (p=0.001) than R. Even with OMV+ dynasore treatment, no inhibition was found in cytokine release in NR, suggesting overwhelming presence of OMVs in the cells of NR and continuous cellular activation.
Conclusion Increased systemic OMPA and LPS-positive BEVs are present at baseline in AIH patients and are able to induce marked immune activation through MAITs cells, which could contribute to corticosteroid resistance.
Keywords Autoimmune hepatitis, Bacterial extracellular vesicles, Ultracentrifugation
344
The dynamics of hepatocardiac axis: A case-control study of left ventricular dysfunction in liver cirrhosis
Rushil Solanki , Srijaya S Sreesh, Thomas Varghese Attumalil, Shivabrata Dhal Mohapatra, Vijay Narayanan, Aditya Verma, Krishnadas Devadas
Correspondence – Rushil Solanki - rushilsolanki808@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Background Left ventricular diastolic dysfunction (LVDD) is formè frusté of cirrhotic cardiomyopathy. However, the clinical significance of its presence in patients with cirrhosis has not been clearly defined. The aim of our study was to evaluate the relationship of LVDD with the etiology of liver cirrhosis (LC), severity, musculoskeletal dysfunction, and the outcome of the patients.
Methods We prospectively enrolled 167 patients with LC, at Government Medical College, Thiruvananthapuram, from August 2020 to September 2021. All patients underwent investigation including 2D echocardiography with tissue Doppler imaging. The diagnosis of LVDD was based on the American Society of Echocardiography guidelines 2016.
Results Two hundred and ten patients were enrolled in this study. Out of these 167 patients were included and 43 patients were excluded. Among the 167 patients, 100 (59.88%) had LVDD (Case) and 67 (40.11%) did not have LVDD (Control). Of the LVDD patients, 61 (61%) had grade 1 LVDD and 39 (39%) had grade 2 LVDD and no patients (0%) had grade 3 LVDD. Child-Pugh had significant correlation with LVDD (p=0.001). We found that ascites (p<0.001), multiple LVP (p<0.001), HE (p<0.002) and AKI (p<0.001) had significant correlation with LVDD. 72.23% (n=49) confirmed sarcopenia has LVDD, however there was no difference between the grades of LVDD. Among LVDD group, grade 2 LVDD had higher mortality than grade 1 LVDD and no LVDD groups. It was found that LVDD had significant correlation with survival (p<0.01) of LC patients. We identified hypertension, dyslipidemia and obesity as confounders. ROC curve of these parameters to predict LVDD showed greater significance for ascitic protein than ascitic albumin to predict LVDD.
Conclusion NASH etiology is at higher risk to develop LVDD. Child-Pugh score, sarcopenia, ascites, HE and AKI are significantly associated with LVDD. Ascitic fluid protein>0.8 is indicator of LVDD. Survival has linear relationship with LVDD.
Keywords Left ventricular diastolic dysfunction, Liver cirrhosis, Cirrhotic cardiomyopathy
345
Prevalence and microbiological profile of bacteremia in cirrhotic patients presenting with upper gastrointestinal bleed in a tertiary care hospital
Dhanush Thomas , Venkatakrishnan Leelakrishnan, Rathi Bhaskaran
Correspondence – Dhanush Thomas - dhanush26@gmail.com
Department of Medical Gastroenterology, P S G Institute of Medical Sciences, Off, Avinashi Road, Peelamedu, Coimbatore 600 024, India
Introduction Bacterial infections are common in patients with chronic liver disease who present with upper gastrointestinal (GI) bleed, occurring in 20% within 48 hours .The aims of this study were to determine the incidence of bacterial infections in patient presenting with upper GI bleed and also analyse the microbiological profile of the infection
Methods All patients presenting with upper GI bleed admitted through emergency department in our centre from a period of 2019 to 2021. Patients who has had history of antibiotics in the last 1 week or has had infections were excluded.
Results Total of 380 patients presented to the emergency department with upper GI bleed and blood cultures were taken at admission. Culture 288atient288d288 was seen in around 36% patients. Blood culture was positive in 20%, urine culture was positive in 13% and asitic culture was positive in 3.2%.among the blood culture positive patients E.coli was isolated in 62% of patients , Klebseilla was isolated in 20%, enterococcus in 9%, Stenotrophomonas in 4%, staph aureus in 3%. Urine culture showed 78% klebsiella, 10% enterococcus fecalis. Ascitic fluid culture showed 68% E. coli, 10% 288atient288d288, 9.4% Staphylococci.
Conclusion Bacteremia was present in 36% of the patients presented with upper GI bleed and predominantly the organism isolated were gram negative organisms and hence appropriate antibiotics have to be started prophylactically at presentation to prevent mortality.
Keywords Bacteremia, Cirrhosis, Upper GI bleed
346
A study of comparison of various fibrosis scores (APRI, NAFLD fibrosis score and FIB 4 score) with the results of Fibroscan and acoustic radiation force impulse (ARFI) imaging in type 2 diabetics mellitus patients
S Jagadeeswar , L R S Girinadh, Satya Sahi Adapa, D Vamsi Yadav
Correspondence – Jagadeeswar S - jagadeeswar25@gmail.com
Department of Gastroenterology and Hepatology, King George Hospital, KGH Down Road, Maharani Peta, Visakhapatnam 531 011, India
Introduction NAFLD and T2DM often coexist. Prevalence of NAFLD in patients with type 2 diabetes mellitus is more than 2-fold HIGHER than in the general population.
Aims To compare various fibrosis scores (APRI, NAFLD Fibrosis score and FIB 4 score) with the results of Fibroscan and Acoustic Radiation Force Impulse imaging.
Methods Patients with overt liver disease, congestive heart failure, ascites, positive for HIV/HbsAg/HCV, alcohol intake (men who consumed >20 g and women who consumed >10 g of alcohol per day), Usage of drugs known to cause steatosis, BMI > 35 kg/m2 were excluded.
Results Mean Fibroscan value is 8.94 ± 2.71. 38% of subjects are in the F3 group i. e. advanced fibrosis. 47% of subjects fall in the category of advanced fibrosis/cirrhosis group. 53% subjects comprise the F0 – F2 group. Nineteen subjects have fallen in the F4 category in ARFI whereas only subjects are in F4 group according to Fibroscan. There is significant association between Fibroscan and ARFI regarding each Fibrosis stage, the p value being < 0.001. Indeterminate or intermediate values constituted 21%, 51%, 38% of the total values in APRI, NFS, FIB 4 respectively. Of these intermediate values, 19%, 29%, 22% constituted the advanced fibrosis(F3/F4) group respectively.
Conclusions 47 % of subjects had advanced fibrosis (F3/F4). ARFI had significant correlation with Fibroscan for predicting advanced fibrosis (p<0.001; r = 0.93). APRI, NFS and FIB 4 correlated significantly with Fibroscan (r=0.374, p<0.001; r=0.594, p<0.001; r=0.411, p<0.001 respectively). ARFI and FIB4 had higher accuracy for prediction of advanced fibrosis (p<0.001). NFS and APRI had intermittent accuracy (p=0.003; p=0.002). Fibroscan and ARFI are useful in assessing the subjects in the 289atient289d289s289 zones of the various non-invasive scores.
Keywords NAFLD, FIBROSCAN, Type 2 diabetes mellitus, APRI, NAFLD fibrosis score and FIB 4
Biliary tract
347
Successful endoscopic retrograde cholangiopancreatography in patient with total situs inversalis by “Twist Method”: A case report from Western India
Rohan Badve
Correspondence – Rohan Badave – rbadave@gmail.com
Department of Gastroenterology, Maniapl Hospital, Dr E Borges Road, Dona Paula, Panaji, Goa 403 004, India
Background Situs inversus is a very rare anomaly in which the internal organs are reversed, as if in a mirror image of their normal position. The anatomy of the left and right sides is reversed; hence, it is more difficult to perform endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy in patients with situs inversus than in normal patients.
A 42-year-old male presented with epigastric pain and jaundice of 2 days duration. On evaluation he was diagnosed to have cholecystolithiasis, dilated intrahepatic biliary radicles, common bile duct (CBD) and CBD stone of size 9 mm in addition to total situs inversalis. His total bilirubin was 2.5 mg/dL with alanine aminotransferase (ALT) 422 IU/L and aspartate aminotransferase (AST) 240 IU/L. ERCP was performed for removal of CBD stone. During ERCP patient was placed in right lateral position with endoscopist standing on right side. First, the duodenoscope was rotated 180° counter clockwise in the stomach, and was then shortened by turning 180° the counter clockwise again in the duodenum. Ampulla in the endoscopic view was deviated to right side and right-upward direction. The cholangiogram revealed a large filling defect and diffuse dilatation of the CBD. After performing a sphinterotomy and sphincteroplasty, bile duct stone was removed, and clearance of CBD achieved. His bilirubin decreased to 1.5 mg/dL and ALT to 84 IU/L. He underwent laproscopic 289atient289d289s28is289 during same hospital stay.
Results and Conclusion ERCP procedures are challenging in the presence of anatomical abnormalities and even a skilled endoscopist can encounter technical difficulties when performing ERCP in patients with situs inversus. There have been only a few reports on ERCP in patients with situs inversus. We performed successfully ERCP in total situs inversus patient using right lateral position with “twist method”.
Keywords ERCP, Situs inversus, Stone
348
Case reports of in situ DPT plastic stents causing duodenal perforation
Ram Teja , Debakanta Mishra
Correspondence – Debakanta Mishra – debakanta87@gmail.com
Department of Gastroenterology, Department of Gastrointestinal and Hepatobiliary Sciences, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India
Biliary stents are treatment modality for biliary decompression of biliary obstruction.
Intestinal perforation is rare but potentially life-threatening complication. Case reports of duodenal perforation of displaced stents are present, but cases of duodenal perforation within situ DPT stents are extremely rare.
We present 2 cases of in situ DPT plastic stent causing duodenal perforation.
A 71-year-old male, a case of advanced periampullary carcinoma with obstructive jaundice in whom biliary decompression has been done using biliary SEMS + plastic stent 10 Fr *8 cm placement, presented to emergency after the procedure with pain abdomen. ultrasonogram (USG) abdomen done which revealed stent in-situ with mild perihepatic collection. Laboratory tests revealed that the patient’s white blood cell (WBC) count of 12.1 × 109/L, neutrophils (n%) was 85%, alanine aminotransferase (ALT) was 46 U/L, aspartate aminotransferase (AST) was 56 U/L, total bilirubin (TB) was 4 mg/dL, and direct bilirubin was 2.7 mg/dL. Endoscopic retrograde cholangiopancreatography (ERCP) has been done which showed the distal tip had penetrated the duodenal wall opposite the papilla. The plastic stent is successfully retracted and removed using rat tooth forceps.
Perforation has been closed with 2 hemoclips, DPT 10 Fr * 8 cm plastic stent placed into metallic stent and patient recovered.
A 56-year-old male underwent ERCP + DPT plastic stent placement 4 weeks back for choledocholthiasis with cholangitis, came to our centre for elective stent removal. ERCP done which revealed distal tip of plastic stent had penetrated the duodenal wall opposite the papilla.
The plastic stent has been successfully retracted and removed using rat tooth forceps. One hemoclip has been applied over the duodenal perforated site.
These 2 reports are rare cases of in-situ plastic stent causing perforation which has been managed endoscopically, without the need for surgical intervention.
Keywords Biliary stent, Perforation, Plastic stent
349
Myeloid sarcoma: An unusual case of obstructive jaundice
Swarup Patnaik 1 , Pukhraj Singh Jeji 1 , Manas K Behera 2 . Debakanta Mishra 1 , Girish K Pati 1 , Jimmy Narayan 1 , Kanishka Uthansingh 1 , Subhasis Pradhan 1 , Ram Gopal Teja 1 , Srinith Patil 1 , Radhika Nitala 1 , Manoj K Sahu 1
Correspondence – Manoj K Sahu – manojsahu@soa.ac.in
1Institute of Medical Sciences and SUM Hospital, Siksha O Anusandhan deemed to be University, K 8, Kalinganagar, Bhubaneswar 751 003, India, 2Department of Hepatology, S C B Medical College, Manglabag, Mangalabag, Cuttack 753 007, India
Background and Aim Billiary obstruction secondary to malignancy is a common clinical problem. Rarely, biliary obstruction is due to leukemia and obstructive jaundice in these patients usually presents late in the course of the disease. Hence, our aim of the study was to establish the diagnosis of hematological malignancy causing obstructive jaundice through biopsy and immunohistochemistry (IHC) evaluation and early starting of chemotherapy leading to complete resolution of the obstruction and normalization of liver function test (LFT).
Method All the clinical data were recorded after necessary clinical examination. Clinical routine examinations were complete blood count (CBC), LFT, lactate dehydrogenase (LDH), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), ultrasonogram (USG) abdomen, magnetic resonance cholangiopancreatography (MRCP) and contrast-enhanced computed tomography (CECT) abdomen. For histopathological examination, biopsy was taken from the thigh and shoulder mass with IHC markers.
Result MRCP revealed periampullary mass lesion causing dilated common bile duct (CBD) and intrahepatic biliary radicals (IHBRs), hence endoscopic retrograde cholangiopancreatography (ERCP) with plastic stenting was done. Biopsy from shoulder lesion revealed mesenchymal tumor and IHC confirmed that the lesion as myeloid sarcoma. Following stenting after normalization of LFT, chemotherapy started.
Discussion and Conclusion Myeloid sarcoma is an extramedullary tumor, a subtype of acute myeloid leukemia. Myeloid sarcoma can cause biliary stricture leading to obstructive jaundice along with multiple skin nodular ulcers, even with normal hemogram report. ERCP with plastic stenting combined with early institution of chemotherapy after normalization of bilirubin may lead to complete resolution of jaundice within 3 to 4 weeks.
The patient showed improvement of skin lesions and normalization of LFT after 3 weeks of chemotherapy.
Keywords Acute myeloid leukemia, obstructive jaundice, myeloid sarcoma, MRCP
350
Acquired immunodeficiency syndrome cholangiopathy – What lies beneath
Nikhil Thomas , L Venkatakrishnan, S Mukundan, Prudhvi Krishna Chandolu, R K Karthikeyan
Correspondence – Nikhil Thomas -nikhilkennythomas@gmail.com
Department of Medical Gastroenterology, P S G Institute of Medical Sciences and Research, Off Avanashi Road, Peelamedu, Coimbatore 641 004, India
Acquired immunodeficiency syndrome (AIDS) cholangiopathy is a syndrome of acalculous biliary obstruction resulting from infection-associated strictures of the biliary tract, usually seen in patients with a CD4 count well below 100/mm3. C. parvum is the most common pathogen associated with AIDS cholangiopathy. Other pathogens include cytomegalovirus (CMV), microsporidium, 292atient292d292, and histoplasma.
Forty-three-year-old female presented with loose stools of 3 months duration with history of significant weight loss. Patient is a known case of retroviral disease for last 10 years on combination antiretroviral therapy (cART) for 10 years . She had history of similar complaints two years ago which was treated with antibiotics. Clinical examination was unremarkable except for mild pallor and a low body mass index (BMI) of 17.6 kg/m2.
On evaluation, complete blood count (CBC) showed normocytic hypochromic anemia. Prothrombin Time and International Normalized Ratio (PT/INR) was normal. Liver function test (LFT) showed elevated alkaline phosphatase (ALP) and Gamma-glutamyl transferase (GGT). Erythrocyte sedimentation rate (ESR) was mildly elevated. Renal function test (RFT) was normal. CA 19-9 was mildly elevated. Stool routine two samples was negative for cryptosporidium and other opportunistic organisms. Serum lactate dehydrogenase (LDH) was normal. Human immunodeficiency virus (HIV) viral load was 13,400 IU/mL, CD4 count was 20. Magnetic resonance cholangiopancreatography (MRCP) showed mild to moderate dilatation of intra and extra hepatic biliary channels with abrupt cut off of terminal Common bile duct (CBD), soft tissue thickening causing luminal irregularity of the terminal CBD, prominent main pancreatic duct.
Endoscopic biopsies from ileum revealed lymphoplasmacytic infiltrates with blue basophilic organisms resembling Cryptosporidium. Endoscopic retrograde cholangiopancreatography (ERCP) biopsies taken from distal CBD- revealed extensive denudation and focal ulceration covered by granulation tissue and the epithelial cell lining shows few large cells with eosinophilic nuclear and cytoplasmic inclusions and granular basophilic cytoplasm suggestive of Cytomegalovirus infection.
She was managed with intravenous (IV) fluids, IV antibiotics, ursodeoxycholic acid (UDCA), proton pump inhibitors (PPIs), IV analgesics, anti-protozoal (nitazoxanide) and other supportive measures.
Opportunistic infections can coexist (as in our case Cryptosporidium and CMV). So complete evaluation is mandatory.
Keywords AIDS cholangiopathy, Cryptosporidium, Cytomegalovirus
351
Clinical profile of cholangitis in a tertiary care center in north India and role of serum procalcitonin in prediction of severe cholangitis
Bilal Mir , Ashish Chauhan, Shaheena Parveen 1 , Tahir Majeed
Correspondence – Bilal Mir – mir13bilal@gmail.com
Department of Gastroenterology, Indira Gandhi Medical College, Shimla 171 006, India, and 1Department of Gastroenterology, Government Medical College, SMHS Hospital, Srinagar 190 001, India
Background Cholangitis is one of the commonest emergencies encountered by gastroenterologists which in most of the cases warrant drainage of biliary system. Serum procalcitonin is an important biomarker of cholangitis with a potential to guide therapeutic decision.
Methods We did a retrospective analysis of prospectively maintained data of patients admitted in the hospital from March 2018 to September 2019 with a diagnosis of acute cholangitis based on Tokyo 13 guidelines (TG 13). All the demographic parameters, biochemical and hematological parameters, and the result were recorded.
Results Forty-one patients were admitted to our hospital with a mean age of 51.07±7.99 years, among which 58.5% (24/41) were females with most common etiology being choledocholithiasis (31.7%). Fever, jaundice, and abdominal pain were seen in 78% (32/41), 73.3% (30/41), and 76.9% (30/41) of patients, respectively. Organ failure was seen in 29.3% (12/41) of patients with most common organ failure being acute kidney injury. Mild, moderate, and severe cholangitis as per TG 13 was seen in 43.9%, 26.8%, and 29.3% of patients respectively. Elevated Procalcitonin levels were associated with severe disease (66.7% vs 26.5%, p=0.05). 43.9% patients were managed conservatively while the majority of remaining needed endoscopic intervention.
Conclusion In this retrospective analysis we showed that most common etiologies in our set up was choledocholithiasis. Raised serum procalcitonin levels were significantly associated with increased severity of cholangitis.
Keywords Cholangitis, Tokyo grade (TG 18), Procalcitonin, Endoscopic retrograde cholangiopancreatography
352
A rare case of asymptomatic cholecystocolonic fistula: Diagnostic dilemma
Maitrey Patel , Aastha Jha, Apurva Shah, Shravan Bohra
Correspondence – Maitrey Patel – ptlmaitrey@gmail.com
Department of Medical Gastroenterology, Apollo Hospital International Limited, Plot No 1A, Gandhinagar – Ahmedabad Road, GIDC Bhat, Estate, Ahmedabad 382 428, India
Cholecystocolonic fistula (CCF) is a rare, diagnosed 1 per 10,000 cholecystectomies and common in females, Mean age is 68.9 years. In only 7.9% of patients the diagnosis is made before surgery. In our case A 56-year male, newly detected type II DM with history of cholelithiasis (single episode of biliary colic 4 years back), was advised laparoscopic cholecystectomy but refused for same at that time. Now came as with history of global sensation since 3 months. Physical examination was absolutely normal. Considering past history all though he was asymptomatic, was evaluated and USG abdomen which showed grade I fatty liver with ill-defined area of hypoechogenicity in pericholecystic and GB fossa ?focal fatty sparing SOL and his routine blood investigation were within normal limit except HBA1c 8.9. Gastroscopy showed LAX LES, Grade B esophagitis. Contrast CT scan abdomen (Fig. 1) which was suggestive of changes of xanthogranulomatous cholecystitis with sealed off CCF or early neoplastic etiology. To confirm CCF preoperative colonoscopy was done which showed a small fistulous opening (<1 cm) seen at the level of hepatic flexure, surrounded by granulation tissue and pouring out some white cheesy material (likely pus) consistent with CCF (Fig. 2). Patient underwent laparoscopic exploration plus cholecystectomy and primary closure of fistulous opening of colon and during surgery frozen section of fistulous margin and surgical specimen of GB showed active chronic cholecystitis with extensive Rokitansky-aschoff sinuses and follicle formation, Liver tissue was normal and no malignance was seen. Colon was viable, non-necrotic so only primary suturing of fistulous opening was performed and drain was put. Postoperative patient had no complication was discharged on Day 5. In conclusion radiologist should be aware of CCF along with other hepatobiliary anomaly and preoperative diagnosis of CCF reduces complications, surgery duration and hospital stay.
Keywords Cholecystocolonic fistula, Gall stone complication
353
Spontaneous perforation of gallbladder: A case report
K Pruthvi, Vybhav Venkatesh, Manoj Kumar Sahu, Anirudh Karanam, Vasista Palnati, Pukhraj Singh Jeji, Jimmy Narayan, Girish Kumar Pati, Debakanta Mishra, Subhasis Pradhan
Correspondence – K Pruthvi – pruthvireddy89@gmail.com
Department of Medical Gastroenterology, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India
Introduction Cholecystitis is one of the most common causes of pain abdomen in the gastroenterology practice. Gallbladder (GB) perforation is a dreaded complication of acute calculous or acalculous cholecystitis with an incidence ranging from 2% to 18% and associated with high morbidity and mortality. Elderly individuals are more prone to GB perforation owing to reduced blood supply either from atherosclerosis, focal vasospasm or vasculitis.
Case A 70-year-old man, presented to us with right upper quadrant abdominal pain, jaundice and distension of abdomen for 7 days. He had comorbidities in the form of chronic obstructive pulmonary disease and hypertension. Examination revealed a distended abdomen with tenderness and guarding in the right upper quadrant. Investigations were suggestive of anemia, hyperbilirubinemia (total bilirubin- 3.4 mg/dL) and raised transaminases (AST- 54 IU/L, ALT- 62 IU/L, ALP- 171 IU/L). Ultrasound of the abdomen showed sludge filled distended GB with edematous wall thickening, septate perihepatic collection and free fluid. Contrast enhanced computed topography of the abdomen revealed a perforation of GB with associated perihepatic and subhepatic collections. Blood and ascitic fluid culture came positive for Klebsiella pneumoniae. A diagnosis of spontaneous GB perforation (type 2 according to the Niemeier classification) secondary to gangrenous acalculous cholecystitis was made and he was managed with appropriate antibiotics. Supportive treatment was continued, and ultrasound guided drainage of the collections was done. Patient had uneventful recovery and discharged with a plan for interval cholecystectomy.
Conclusion GB perforation should be considered in differential diagnosis of elderly patients presenting with abdominal pain and peritonitis. Early diagnosis and prompt treatment would help in reducing the associated morbidity and mortality.
Keywords Cholecystitis, Calculous, Acalculous, Elderly, Gallbladder, Perforation
354
Endoscopic trimming of 295atient self-expanding metallic stents by argon plasma coagulation: A case report
Mohd Rafiq Najar, Monika Jain, Gurwant Singh Lamba, Aeshal Parmar
Correspondence to – Mohd Rafiq Najar – dmrfqn@gmail.com
Department of Gastroenterology, Sri Balaji Action Medical Institute, Paschim Vihar, New Delhi 110 063, India
Introduction The endoscopic placement of self-expanding metallic stents (SEMS) for palliation of malignant obstruction of biliary tract is an established practice. The distal end of stent may sometimes impinge on the wall of duodenum and may cause erosion of duodenal wall and subsequent bleeding.
Methods A 67-year-old male with carcinoma of gallbladder with obstruction to common bile duct (CBD) due to tumor invasion underwent biliary SEMS placement. This patient presented with melena after a week of SEMS placement. During upper gastrointestinal endoscopy (UGI) endoscopy, distal end of SEMS was seen abutting the duodenal wall and ulcerations were found on posterior and lateral wall of 2nd part of duodenum. The distal end of SEMS was shortened by 2.0 cm using argon plasma coagulation (60 watts and 1.8L/min) to cut the meshes of SEMS, so that the lower end of SEMS is no longer in contact with duodenal wall. Stent fragment was removed using a catheter with a retrieval net. The patient experienced no complications during procedure and on follow-up. Duodenal ulceration disappeared on follow-up endoscopy.
Results Biliary SEMS trimming was successfully done using argon plasma coagulation (APC) without any untoward side effects.
Conclusion APC is an effective and safe way for trimming of metallic SEMS.
Keywords APC, biliary SEMS trimming
355
Acute cholangitis in malignant biliary obstruction: Clinical presentation and outcome
Saroj Sahu 1 , Ayaskanta Singh, Jimmy Narayan
Correspondence – Saroj Sahu – saroj31121987@gmail.com
1Department of Gastroenterology, Sum Ultimate Medicare, Kalinga Nagar, Bhubaneswar 751 003, India, and Department of Gastroenterology, IMS and SUM Hospital, Kalinga Nagar, Bhubaneswar 751 003, India
Introduction Acute cholangitis is a common complication in benign biliary strictures and choledocholithiasis. Cholangitis is rare in malignant biliary obstruction and the dilemma continues with regard to clinical presentation and management. In this study, we aimed at clinical presentation, management, and therapeutic outcome of acute cholangitis in malignant biliary obstruction.
Methods We conducted a retrospective analysis of 11 consecutive hospitalized adult patients with malignant biliary obstruction and biliary drainage confirmed-acute cholangitis between 1st September 2020 and 31st August 2021. Clinical presentation, laboratory data, and management records were collected. Outcomes were assessed in terms of post-procedure symptomatic improvement and 3-month mortality.
Results Eleven patients had malignant biliary obstruction and cholangitis. The ratio of males to females was 0.57. The mean age of presentation was 61.6 ± 8.4 years. Five patients had naïve presentation with acute cholangitis, and 6 had stent block. The etiology of biliary obstruction in those with naïve presentation was carcinoma gallbladder, hilar cholangiocarcinoma, and carcinoma head of the pancreas in 3, 1, and 1 case respectively jaundice, right hypochondrium pain, and drowsiness at presentation were found in 100%, 80%, and 80% cases respectively. No patient had fever. Recurrent hypoglycemia and hypoglycemic encephalopathy complicated 4 (100%) and 2 (50%) cases of hilar obstruction with acute cholangitis respectively. Endoscopic retrograde cholangiopancreatography (ERCP) and biliary stenting, and percutaneous transhepatic biliary drainage were done in 3, and 2 cases (both Ca GB) respectively. Post-biliary drainage hypoglycemia improved in 2 cases (1 Ca GB, and 1 hilar CCA). Three-month survival was 33.3% in ERCP cases and 0% in PTBD cases (both died within 1 month and had hypoglycemic encephalopathy).
Conclusion Acute cholangitis is not an uncommon naïve presentation of malignant biliary obstruction. Altered sensorium and hypoglycemia may denote underlying cholangitis sepsis in malignant hilar biliary obstruction. ERCP and biliary stent placement provide the best outcome.
Keywords Cholangitis, Malignant biliary obstruction, Endoscopic retrograde cholangiopancreatography
356
Histological types of cholecystectomy specimens obtained from patients with right hypochondriac pain suspected for gallbladder pathology
Soumik Ghosh1, Atrayee Chatterjee2, Wasiful Haque3, Kalidas Biswas1
Correspondence – Soumik Ghosh – drsoumikghosh@gmail.com
1Department of Medical Gastroenterology, Medical College and Hospital, Kolkata, A-401, Sanmilita Housing Society, P-231 CIT Road, Scheme-VII (M), Kankurgachi, Kolkata 700 054, India, 2Departments of Pathology, and 3Radiotherapy, Burdwan Medical College, Purba Bardhaman, A-401, Sanmilita Housing Society, P-231 CIT Road, Scheme-VII (M), Kankurgachi, Kolkata 700 054, India
Introduction Patients present at Hospital with pain in right hypochondrium are clinically and sonologically suspected gallbladder pathology undergo cholecystectomy. In this study we evaluated the histological types of cholecystectomy specimens which were clinically and radiologically suspected of gallbladder pathology.
Method Retrospective records were analyzed from January 2018 to February 2020 in Department of General Surgery, Medical College and Hospital, Kolkata. Presenting symptoms, preoperative USG whole abdomen report, clinical findings and postoperative histopathological findings were noted.
Result Record of total 112 patients of above 18 years of age were evaluated. Among them 26 were male (23.2%) and 86 were females (76.8%). Mean age was 43. The histological types were as follows-chronic calculus cholecystitis 51.8% (58), chronic acalculus cholecystitis 12.5% (14), chronic acalculus cholecystitis with cholesterosis 10.7% (12), acute acalculus cholecystitis 7.1% (8), acute calculus cholecystitis 4.5% (5), carcinoma gallbladder 4.5% (5), empyema gallbladder 4.5% (5), chronic acalculus cholecystitis with cholesterol polyp 1.8% (2), chronic calculus cholecystitis with adenomatous polyp 0.9% (1), mucocoele gallbladder 0.9% (1), xanthogranulomatous cholecystitis 0.9% (1).
Conclusion Combined evaluation with history, clinical findings, physical examination and ultrasonography of whole abdomen study can suspect gallbladder pathology excluding normal gallbladder status. Histopathological examination is a must to confirm the type of the pathological pattern.
Keywords Gallbladder, Cholecystectomy, Histology
357
Prevalence of Salmonella typhi chronic carrier state in patients of chronic cholecystitis and cholelithiasis – A tertiary institutional observation from Eastern India
Soumik Ghosh , Atrayee Chatterjee 1 , Kalidas Biswas
Correspondence – Soumik Ghosh – drsoumikghosh@gmail.com
Department of Medical Gastroenterology, Medical College and Hospital, A-401, Sanmilita Housing Society, P-231 CIT Road, Scheme-VII (M), Kankurgachi, Kolkata 700 054, India, and 1Department of Pathology, Burdwan Medical College, Purba Bardhaman, A-401, Sanmilita Housing Society, P-231 CIT Road, Scheme-VII (M), Kankurgachi, Kolkata 700 054, India
Introduction World-wide prevalence of Salmonella typhi (S. typhi) chronic carrier state in gallbladder is ~ 1-2.5% as per recent epidemiological evidence states. But the S. typhi carrier state in chronic cholecystitis and cholelithiasis patients were found much higher as per our analysis demonstrating the presence of S. typhi isolated and demonstrated from gallbladder tissues by polymerase chain reaction (PCR).
Method One hundred (100) paraffinized blocks of gallbladder tissue samples of histologically proven chronic cholecystitis and cholelithiasis were collected. Among them, thirty-six (36) samples were of chronic cholecystitis (Male-6, Female- 30) and sixty-four (64) were of cholecystitis with cholelithiasis (Male-9, Female-55). The samples were tested for S. typhi DNA PCR through steps of extraction of gallbladder tissues by paraffin removal, DNA extraction from it, S. typhi DNA identification, amplification and DNA sequencing and analysis.
Result Seven samples were positive for S, typhi chronic carrier state (six in cholecystitis with 298atient298d298s298is samples, one in chronic cholecystitis sample); in percentage it is seven percent (7%), which is much higher than the overall prevalence of S. typhi carrier state which is only ~ 2.5% as per present epidemiological data states.
Keywords Salmonella, Prevalance, Cholecystitis and cholelithiasis
358
Expression of p53 gene in gallbladder tissue of chronic cholecystitis and cholelithiasis patients
Soumik Ghosh1, Atrayee Chatterjee2, Kalidas Biswas1
Correspondence – Soumik Ghosh – drsoumikghosh@gmail.com
1Department of Medical Gastroenterology, Medical College and Hospital, Kolkata, A-401, Sanmilita Housing Society, P-231 CIT Road, Scheme-VII (M), Kankurgachi, Kolkata 700 054, India, and 2Department of Pathology, Burdwan Medical College, Purba Bardhaman, A-401, Sanmilita Housing Society, P-231 CIT Road, Scheme-VII (M), Kankurgachi, Kolkata 700 054, India
Introduction Tumor suppressor gene p53 has been shown to be involved in the development and progression of gallbladder carcinoma (CAGB). The prognostic significance of p53 over-expression has been reported in CAGB. About half of the tissue samples of CAGB show over expression of p53 gene by immunohistochemical examination (IHC). Early detection of positive IHC expression for p53 gene in gallbladder tissue of chronic cholecystitis and cholelithiasis patients may be helpful for cancer prevention and early treatment. In this study we observed IHC for p53 gene of gallbladder tissues of chronic cholecystitis and cholelithiasis patients.
Method Gallbladder tissues of one hundred patients (100) in paraffin blocks with confirmed diagnosis of chronic cholecystitis (36) and cholecystitis with cholelithiasis (64) were collected. Paraffin were removed by Xylene method to isolate gallbladder tissue. IHC for p53 were performed by immunoperoxidase and diaminobenzidine staining method. Scoring was done by observing percentage of staining of cells in tissue; more than ten percent tissue staining was considered as positive.
Result Among the one hundred (100) samples, ten (10%) samples were found positive of IHC for p53 gene expression (nine samples weakly positive and one sample moderately positive). Among cholecystitis with cholelithiasis samples, nine were found weakly positive whereas one sample was moderately positive. Only one sample of chronic cholecystitis was found weakly positive.
Conclusion Positive expression of p53 gene may be demonstrated by IHC method in cholecystitis with cholelithiasis. As positive expression of p53 gene predicts increased risk of development of CAGB in inflammatory conditions, risk is more in cholecystitis with cholelithiasis patients than chronic cholecystitis patients.
Keywords p53, Immunohistochemistry, Cholecystitis, Cholelithiasis
359
Case report of a foreign body in the common bile duct
Pavankumar Evuri , Caroline Selvi
Correspondence – Pavankumar Evuri - pavankumar.evuri@gmail.com
Institute of Medical Gastroenterology, Rajiv Gandhi Government General Hospital, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Biliary drainage with T-tube after bile duct surgery has advantages. However, the use of T-tube is associated with some complications. Retained T-tube fragment is a rare complication. We present an unusual case of retained T-tube.
Case Report A 28-years-old male patient after road traffic accident presented with abdominal pain and distension. An abdominal ultrasound (USG) abdomen showed free fluid in abdomen. Diagnostic peritoneal aspiration showed bile and blood. Contrast enhanced computerized tomography (CECT) abdomen showed 7 cm size laceration in the right lobe of liver with free fluid in the abdomen and pelvis. Emergency laparotomy with cholecystectomy and choledochotomy with T-tube placement was done. On post operative day 15 patient accidentally removed T-tube. Magnetic resonance cholangiopancreatography (MRCP) done showed hepatic hyper intensity suggestive of old laceration, T tube fragment noticed in the common bile duct (CBD), fluid collection in hepatorenal pouch. Patient got discharged against medical advice. After 2 months he presented with right hypochondrial pain. MRCP showed T2 hypointense material noted with in the dilated CBD and proximal CBD dilated (8.4 mm). Endoscopic retrograde cholangiopancreatography (ERCP) cholangiogram showed T – tube in the CBD extending into the right system. Sphincterotomy with Balloon trawling done, and T-tube retained fragment removed. 7 Fr X 8 Cm stent deployed into the right system. Post procedure patient was stable and discharged after 2 days.
Conclusion Retained T tube fragments is a very rare complication with few case reports. Removal can be both endoscopic and surgical, however endoscopic methods are less invasive. Hence retained T tube fragment in biliary tree should be removed as early as possible to prevent complications.
Keywords Blunt hepatic injury, Cholangitis, Cholecystectomy, T-tube complications
360
Post corona virus disease 2019 cholangiopathy: A novel entity
Amal Velse, A R Akhilandeshwari
Correspondence – A R Akhilandeshwari - amalvelse16oct@gmail.com
Department of Medical Gastroenterology, Government Kilpauk Medical College, Chennai 600 010, India
Introduction Corona virus disease 2019 (COVID-19) is a predominantly respiratory tract infection with the ability to affect multiple organ systems. Abnormal liver tests, mainly transaminase elevations, have been reported in hospitalized patients. We describe a case of cholangiopathy in a patient who recovered from severe COVID-19 characterized by marked elevation in serum alkaline phosphatase (ALP) accompanied by evidence of bile duct injury on imaging and liver biopsy.
Case report 72-year-old male with no previous history of liver disease and history of recovery from severe cardiopulmonary COVID-19 infection 45 days back presented with history of jaundice and pruritus of 2 weeks duration. Bile duct injury was identified by abnormal liver tests with serum ALP > 3x upper limit of normal and abnormal findings on magnetic resonance cholangiopancreatography (MRCP) which showed edema around common bile duct (CBD) and intrahepatic biliary tree. Liver biopsy exhibited extensive degenerative cholangiocyte injury. His other notable labs included negative viral, tumor markers, negative autoimmune workup and bile duct brush cytology.
Discussion A diagnosis of post COVID-19 cholangiopathy was made on the basis of clinical, imaging and liver biopsy findings. Patient was given symptomatic management with follow-up of gastrointestinal and liver-related symptoms along with liver enzymes levels. Ultimately, the patients labs steadily improved and was symptom free in few days. Post-COVID-19 cholangiopathy is a special entity of liver injury that has been suggested as a variant of secondary sclerosing cholangitis in critically ill patients. It is characterized by marked cholestasis associated with ongoing jaundice that persists long after pulmonary recovery.
Conclusion Severe hospitalized COVID-19 patients are at significant risk of cholangiopathy and post COVID-19 follow-up must include regular liver functional check-up. This case is being reported to provide reference and guidance for possible liver related COVID-19 complications.
Keywords COVID-19, Cholestasis, Cholangiopathy
361
Role of disposable elevator tip in the prevention of persistent bacterial contamination of reprocessed duodenoscopes
Chandu Gopala Krishna, Siddharth Kanta, B Harshavardhan Rao, Sandeep V Nair, SharonP Methala, Priya Nair, Anoop K Koshy, G Rajesh, Shine Sadasivan, Rama P Venu
Correspondence – Chandu Krishna – drchgopalakrishna@gmail.com
Department of Gastroenterology, Amrita Institute of Medical Sciences, Amrita Nagar, Edappally, Kochi 682 041, India
Introduction Studies have shown an increasing incidence of sepsis with multidrug-resistant organisms (MDRO) caused by persistent contamination of duodenoscopes. Prevalent practices of scope reprocessing seem to be inadequate in completely eradicating the microbial load. The elevator tip has been shown to be a potential source for persistent contamination. In this study, we have assessed the role of a disposable elevator tip to prevent scope contamination.
Methods This was a case-control study conducted in a high volume tertiary center. In the control group, the standard duodenoscopes (Olympus TJFQ180V) was used, while in the test group, a duodenoscope with disposable elevator tip (Pentax ED3490TK), was used. Reprocessing was carried out by dedicated trained technicians in accordance with ESGE guidelines. Bacterial contamination was confirmed by performing surveillance cultures on the scopes as per CDC guidelines. The cultures for the test group were performed after the disposal of the elevator tip. Contamination was defined as microbial growth with ≥20 CFU/20 mL of any type of microorganism (AM20). The prevalence of scope contamination, type of bacteria and procedure related cholangitis was compared between the two groups.
Results A total of 106 cultures were taken (test group – 74 samples, control group – 32 samples). A significantly higher proportion of contaminated scopes were seen in controls as compared to the test group (29/32 samples vs. 41/74 samples, p value 0.05). Six patients (10.5%) had cholangitis following procedure of which 4 patients were from the control group. Among the high priority organisms, pseudomonas aeruginosa and Klebsiella pneumoniae were the most common (10 positive samples each).
Conclusions The use of a disposable elevator tip can result in a significant reduction of bacterial contamination of the duodenoscope. Reduced bacterial contamination can lead to lower rates of post-procedure cholangitis.
Keywords Cultures, Cholangitis, Multidrug-resistant organisms
362
To estimate the diagnostic role of endoscopic ultrasonography in biliary duct dilatation with inconclusive cross-sectional imaging
Ankit Mahajan, Debashis Misra, Kshaunish Das
Correspondence - Ankit Mahajan - amahajan1090@gmail.com
Department of Gastroenterology, Institute of Post-Graduate Medical Education and Research, Kolkata, School of Digestive and Liver Disease, A J C Bose Road, Bhawanipore, Kolkata 700 020, India
Background Computed tomography (CT) scan of abdomen and magenetic resonance cholangiopancreatogram (MRCP) are often inconclusive for diagnostic evaluation of dilated bile duct despite having high sensitivity and specificity. This study was undertaken to estimate the role of endoscopic ultrasonography (EUS) in etiological diagnosis of dilated bile duct where cross sectional imaging is inconclusive.
Methods This prospective study was carried out in Gastroenterology Department of Institute of Post-Graduate Medical Education and Research (IPGMER) Kolkata from January 2020 to June 2021. All patients with inconclusive etiology of dilated bile duct (>6 mm MRCP, >7 mm ultrasonography [USG], > 8 mm CT scan with GB in situ and > 10 mm on MRCP in post cholecystectomy) underwent EUS in our department and were followed up clinically and radiologically till 6 months after procedure.
Results The study cohort was comprised of 67 patients (29 male and 38 female) with mean age of 48.95±15.29 years. The most common symptom at presentation was abdominal pain (89.3%). On EUS, we found ampullary (19.4%), pancreatic (13.4%), common bile duct (CBD) (5.9%), gallbladder (GB) lesions (1.49%), intrabdominal lymph nodes (4.4) and CBD calculus (2.98%) as the etiology. In 31.3% of the patients, no etiologies could be ascertained after EUS. Proportion of patients with jaundice and significant weight loss at baseline were significantly higher in the group having etiological diagnosis after EUS (<0.0001). Mean diameter of bile duct (in USG, CT, MRCP and EUS) was significantly greater in the same group (<0.001). After 6 months of follow-up, only 3 patients out of 67 had variation from the initial EUS diagnosis. The sensitivity, specificity, negative predictive value and positive predictive value of EUS in detecting such lesions are 97%, 93.9%, 96.8% and 93.9% respectively.
Conclusion EUS is beneficial in etiological evaluation of dilated bile duct after inconclusive cross sectional abdominal imaging and it has high sensitivity and negative predictive value.
Keywords EUS, Biliary tract, MRCP and CT abdomen
363
Bacteriological spectrum in bile in patients of acute bacterial cholangitis
Roshan George , Arpan Jain, Gaurav Padia, Sanjeev Sachdeva, Ajay Kumar, Barjesh Chander
Sharma, Ujjwal Sonika, Siddharth Srivastava, Ashok Dalal
Correspondence – Ashok Dalal – drashokdalal83@gmail.com
Department of Gastroenterology, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, 1-J L N Marg, New Delhi 110 002, India
Introduction Acute cholangitis is a life threatening condition, requiring antibiotics and biliary decompression. With indiscriminate use of antibiotics, newer strains of resistant organisms are emerging which pose a major therapeutic challenge. We aimed to analyse the demographic, clinical, biochemical, etiological, and microbial profile of patients with acute bacterial cholangitis.
Method A retrospective observational study was conducted. Consecutive patients with cholangitis, who underwent endoscopic retrograde cholangiopancreatography (ERCP) from January 2020 to August 2021 were included. Bile culture reports were obtained, and clinical parameters were recorded from patient records.
Results One hundred and sixteen patients were included. Seventy-five (64.7%) patients were females. Mean age of patients was 47.56±13.58. Most common symptoms were abdominal pain (89.6%), jaundice (84.4%) and fever (56.8%). 25.8% patients had organ failure (renal failure-24.1%, hypotension-10.3%, respiratory failure-2.5% and encephalopathy- 0.8%). Baseline total leukocyte count was 13700 (10575-19300), bilirubin was 8.45 (4.3-14.4), Alkaline phosphatase was 415 (289-694). 62.1% patients had benign disease. Choledocholithiasis was the most common benign etiology (75%). Carcinoma gallbladder (45.5%) and periampullary carcinoma (31.8%) were the most common malignancies. 81.9% had positive bile culture and 17.9% of bile cultures showed polymicrobial growth. 92.9% of the organisms were gram negative bacteria (GNB). Escherichia coli (45.13%) was the most common organism, followed by pseudomonas aeruginosa (29.2%), Klebsiella pneumoniae (13.27%). Enterococcus spp. (7 %) was the most common gram-positive organism. GNB had highest sensitivity to aminoglycosides (69.6-78.4%), tigecycline (80-88.4%) and had lowest sensitivity to cephalosporins (21.5-33.3%), fluoroquinolones (18.1-26.7%). Sensitivity of GNB to carbapenems was 42.4-62.7%, and to beta-lactam beta-lactamase inhibitors was 27.2-60%. Mortality was 10.3%. Using the multiple logistic regression model, hypotension, longer hospital stay, inotropic requirement and ICU stay were independent predictors of mortality. Multi-drug resistance was not associated with mortality.
Conclusion Indiscriminate antibiotic use has resulted in increasing prevalence of multi-drug resistant organisms, with emergence of carbapenem resistant organisms posing a major therapeutic challenge.
Keywords Acute cholangitis, Bile culture, Multi-drug resistance, Mortality
364
Lemmel syndrome – A rare cause of cholangitis
Rathod Vivek , A Anand
Correspondence – A Anand – rathodrockzz@gmail.com
Department of Medical Gastroenterology, Kilpauk Medical College, Chennai 600 010, India
Introduction Lemmel syndrome is a rare cause of the biliary mechanical compression by the juxtapapillary pseudodiverticulum, in the absence of gallstones or periampullary tumors. Most periampullary diverticula are asymptomatic. However, complications may occur in about 5%, including diverticulitis, pancreatitis, cholangitis, choledocholithiasis, enterolith, bezoar formation, intestinal obstruction, bleeding and perforation.
Case Report A 60-year-old woman presented with abdominal pain, fever, and jaundice of acute onset. She was hemodynamically stable except for a fever of 101°F. Initial blood work revealed a WBC 14,500/mm3, ALT 118 IU/L, AST 189 IU/L, ALP 356 IU/L, T bilirubin 7.2 mg/dL. computerized tomography (CT) and magnetic resonance imaging MRI of abdomen revealed peri ampullary diverticulum compressing distal common bile duct causing proximal dilatation. Biliary findings were consistent with Lemmel syndrome. It was concluded that she had experienced a transient biliary obstruction as a result of Lemmel syndrome. Patient was managed with broad spectrum antibiotics and other supportive measures in view of cholangitis. Patient underwent endoscopic retrograde cholangiopancreatography (ERCP) with common bile duct (CBD) stenting. Patient’s lab parameters improved steadily and was asymptomatic in few days.
Discussion Our patient had abdominal pain associated with leukocytosis and cholangitis due to extrinsic compression of the distal CBD. Lemmel syndrome can be transient in nature as a result of a periampullary duodenal diverticulum causing extrinsic compression of the CBD. This can sometimes progress to cholangitis, as seen in our patient. Early diagnosis is necessary to avoid extensive and invasive workup. Management is often supportive, although in some cases with recurrent infection or persistent biliary obstruction, surgical diverticulectomy can be considered.
Conclusion Lemmel syndrome should be kept as a rare differential when evaluating patients with biliary obstruction.
Keywords Lemmel, Diverticulum, Cholangitis
365
Spy cholangioscopy — A savior from the dreadful Whipple’s
Komal Kalla, Mukesh Kalla, Anant Gupta
Correspondence – Anant Gupta – dranantg@gmail.com
Department of Medical Gastroenterology, S R Kalla Hospital, 78-79, Dhuleshwar Garden, Panch Batti, C Scheme, Jaipur 302 001, India
Introduction IgG4-related sclerosing cholangitis (IgG4-SC) is the biliary manifestation of IgG4-related disease (IgG4-RD). It is a systemic fibro-inflammatory condition, characterized by mass lesions and/or strictures with classical histopathological findings in involved organs. IgG4-SC is associated with type 1 autoimmune pancreatitis (AIP) in more than 90% of cases. It is challenging to diagnose IgG4-SC in the absence of associated AIP.
Case History A 32-year-old female had ~ 6 week history of easy fatiguability, pruritus, non-significant loss of weight. At the onset, she had features of cholestatic jaundice, which on evaluation was due to mid – lower CBD stricture. Etiology of the stricture could not be ascertained even after cross sectional imaging (CT scan) and endoscopic biliary brushings. Patient underwent endoscopic plastic biliary stenting across the stricture and was advised for a Whipple’s surgery for an indeterminate stricture. She presented to us for a second opinion. We decided to re-attempt tissue diagnosis.
Evaluation Endoscopic retrograde cholangiography showed single, mid to lower CBD stricture with dilated common hepatic duct and intra-hepatic biliary radicals. For tissue diagnosis, single operator cholangioscopy showed a smooth fibrotic stricture, with indurated and friable margins. It showed lympho-plasmocytic infiltrate rich in IgG4 positive plasma cells (>15/HPF).
Treatment As per standard of care, patient was started on oral prednisolone 0.6 mg/kg body weight/day.
Discussion IgG4-SC can mimic malignancy, is steroid-responsive and has good prognosis. Inability to ascertain etiology of biliary stricture may lead to surgical resection. As per the existing data, ~10% patient have a benign pathology after Whipple’s surgery done for presumed malignancies.
Conclusion IgG4SC is less common, but a judicious and timely use of spy cholangioscopy, which is a milestone technology helps in accurate diagnosis and may avoid major surgical procedure. Our patient could avoid Whipple’s surgery which is a major surgical procedure and unnecessary for her.
Keywords Spy cholangioscopy, Indeterminate biliary stricture
366
Bile leak after abdominal trauma: A tertiary centre experience
Jagveer Singh , L Sahitya, Gopal Krishna, M Ramanna, M Uma Devi, B Ramesh Kumar
Correspondence – Jagveer Singh – jagveer21@gmail.com
Department of Gastroenterology, Osmania Medical College and Hospital, Afzalgunj Road, Afzal Gunj, Hyderabad 500 012, India
Background Traumatic bile leaks often results in high morbidity and prolong hospital stay that require multimodality management because of associated multiorgan injury. Data on endoscopic management of bile leaks are scarce.
Aim To evaluate the efficacy of endoscopic management of a traumatic bile leak.
Methods We performed a retrospective case review of patients who were referred for endoscopic retrograde cholangiopancreatography (ERCP) after traumatic bile duct injury secondary to blunt trauma (motor vehicle accident or fall from height) and stab wounds for management of bile leaks at our tertiary hospital. Thirty-five patients underwent ERCP, biliary sphincterotomy and stenting for the traumatic bile leak over a 11-year period. All were monitored periodically 1-2 weeks after discharge. Endoscopic therapy was considered successful if there was no drain out. Endo biliary stent was removed after a period of 3 months.
Results The etiology included blunt trauma from motor vehicle accident in 22 patients, fall from height accident in 12 patients, stabbing by bull horn in one, liver injuries were grade III in 12 patients, grade IV in 23 patients. All patients were treated by biliary stent placement, and the outcome was successful in 35 of 35 cases (100%). Right hepatic duct injury in 10 (33%), left in 12 (36%), both associated with liver Laceration. CHD in 4 (12%), CBD injury in 6 (17%), GB perforation in 3 (8.5%). The mean duration of follow-up was 90 days. There were no ERCP-related complications. In our case review, endoscopic management with endo biliary stent placement was found to be successful and resulted in resolution of the bile leak in all 35 patients.
Conclusion Based on our study results, ERCP should be considered as first-line therapy in the management of traumatic bile leaks.
Keywords Traumatic bile leak, Endoscopic management, Abdominal trauma
367
Biliary tuberculosis uncommon presentation of a common disease
Gurunath Bhange , D Sivaramakrishna Naik, Tarun Beeram, Saikrishna Katepally, P Shravan Kumar
Correspondence – Gurunath Bhange – gurunathb6@gmail.com
Department of Medical Gastroenterology, Gandhi Hospital, Secunderabad 500 003, India
Introduction Hepatic involvement in disseminated tuberculosis (TB) is seen in 50% to 80% cases. Isolated hepatic involvement is rare. We present a case of tuberculous distal CBD stricture presenting with obstructive jaundice.
A 15-year-old female presented with complaints of abdominal pain for 2 months and progressive jaundice for 15 days with pruritus and acholic stools. She also had intermittent fever with night sweats for 2 months and weight loss of 5 kg with poor appetite. There was a history of appendicitis at the age of 8 years and appendectomy was done. Patient’s father had a history of pulmonary TB 3 years back. He was noncompliant with anti-tuberculous therapy (ATT) and later succumbed to his illness.
Examination revealed pallor, jaundice and right hypochondrial tenderness. Laboratory parameters include Total bilirubin- 3.2 mg/dL, AST-42 u/L, ALT-32 u/L, ALP- 333 u/L, GGT- 362 U/L and ESR 70 mm/1hour. Ultrasound revealed multiple enlarged lymph nodes in periportal and peripancreatic location. There was dilated CBD (12 mm) and mild central IHBRD. MRCP revealed dilated CBD 10 mm with distal CBD stricture with choledocholithiasis. ERCP revealed smooth distal CBD stricture with dilated proximal CBD. Only sludge was retrieved with balloon sweeps. A 8 Fr double pigtail stent was deployed. Brush cytology revealed lymphocytes. EUS showed multiple hypoechoic periportal and peripancreatic lymph-nodes. FNAC revealed lymphocytes, Langerhans giant-cells, epithelioid cells and caseous necrosis suggestive of tuberculous lymphadenitis. Chest radiograph was normal. Standard tuberculin test showed 20 mm infiltrate. QuantiFERON gold test was positive. CA 19-9 and IgG4 were normal. Patient was started on four-drug ATT. At 4 weeks, her liver chemistries were normal and USG showed regression of lymph nodes. At 6 months, she had resolution of symptoms.
Conclusion A high index of suspicion is necessary in young patients residing in endemic areas of TB. Early identification and initiation of ATT will prevent morbidity as well as mortality.
Keywords Biliary tuberculosis
368
Ectopic opening of the common bile duct into the third part of duodenum: A rare congenital anomaly
Ravindra Pal, V Jineesh1, A Shanid, D Krishnadas, Susan George
Correspondence – Susan George – susanmathmoola@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Ectopic opening of the common bile duct (CBD) into the gastrointestinal (GI) tract is a rare congenital anomaly. The CBD typically opens into the posteromedial aspect of the second portion of the duodenum. Ectopic openings of the CBD to other segments of the duodenum, pyloric canal and stomach have been described. During embryogenesis, disproportional elongation, and early subdivision of the primitive hepatic furrow, as it develops from the pars cystica results in ectopic opening and leads to biliary tract diseases like bile duct stones, cholangitis and acute pancreatitis.
Here we report a 56-year-old man who had presented with painless progressive obstructive jaundice, cholangitis for 1 month with associated loss of appetite. On evaluation he had elevated bilirubin, liver enzymes and tumor marker. Cross sectional imaging revealed dilated intrahepatic biliary radicles with dilated CBD showing distal smooth tapering. On endoscopic retrograde cholangiopancreatography (ERCP) periampullary bulge was noted, CBD was cannulated with difficulty but on cholangiogram the stent was noted in an unusual site. Hence, due to clinical suspicion, Magnetic resonance cholangiopancreatography (MRCP) was done on the same day, which revealed ectopic opening of CBD with distal CBD stricture but the possibility of a malignant stricture could not be ruled out. Patient underwent PTBD and brush cytology which came negative for malignancy. Due to persistent symptoms, he underwent choledochoduodenostomy. Post-surgery patient is doing well.
Malfunction of the valve mechanism in the distal CBD permits influx of intestinal bacteria and gastric contents into the biliary system, which could cause a transient obstruction and recurrent subclinical cholangitis which lead to distal CBD stricture and presentation in our patient. If an ectopic opening of the CBD is suspected at endoscopy, careful inspection for bile flow, use of EUS, cautious cannulation and contrast injection can help delineate the anatomy. In conclusion, management of such cases require multidisciplinary teamwork.
Keywords Ectopic opening of CBD, PTBD, ERCP, Third portion of duodenum
369
Comparative assessment of non-invasive imaging modalities and endoscopic retrograde cholangiopancreatography in obstructive jaundice
Navin Kumar
Correspondence – Navin Kumar – navinpmch85@gmail.com
Department of Gastroenterology, Government Stanley Medical College, Chennai 600 001, India
Background Accurate diagnosis of the cause is crucial in the management of obstructive jaundice. Non-invasive modalities like ultrasonography (USG) multidetector computed tomography (MDCT) magnetic resonance cholangiopancreatography (MRCP) and invasive modality like endoscopic retrograde cholangiopancreatography (ERCP) play the pivotal roles.
Objective To compare the diagnostic accuracy of ultrasonography, MRCP, computed tomography with endoscopic retrograde cholangiopancreatography in obstructive jaundice.
Methods Sixty patients with clinical and laboratory features suggestive of biliary obstruction were included in this study. At least one non-invasive imaging modalities were used in each patient. Cause of obstruction was evaluated by each modality. The findings were compared with the ERCP findings. Data and findings of non-invasive modalities and ERCP were correlated and statistically analyzed.
Results The study included 60 patients in which were 29 females and 31 were males. Mean age of presentation was 49.56 (range 20-82 years). Most of the patients were in the 5th decade of life. Predominant symptoms were jaundice (67%) followed by pain abdomen, pruritus, fever and weight loss. The most common cause of obstruction was choledocholithiasis (77%). Benign causes constituted 82.4% and malignant causes constituted 17.54%. USG, CT and MRCP was able to diagnose accurately the cause of obstruction in 60%, 90% and 91% of the cases respectively compared to ERCP findings.
Conclusion Non-invasive modalities (USG and CT) is considered the first-choice option in the diagnostic imaging of obstructive biliary disease. MRCP findings correlated most accurately among non-invasive modalities with ERCP findings.
Keywords Obstructive jaundice, Endoscopic retrograde cholangiopancreatography, Magnetic resonance cholangiopancreatography
370
Role of change in the levels of inflammatory markers post drainage in predicting outcome in acute cholangitis
Abhinav Jain1, Anuraag Jena2, Vikas Gautam3, Jayanta Samanta2, Atul Saroch1, Harjeet Singh4, Pankaj Gupta5, Vishal Sharma1, Usha Dutta1, Harshal Mandavdhare1
Correspondence – Harshal Mandavdhare – hmandavdhare760@gmail.com
Departments of 1Internal Medicine, 2Gastroenterology, 3Microbiology, 4Surgery, and 5Radiodiagnosis, Post Graduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Background Acute cholangitis (AC) is a gastrointestinal emergency associated with significant mortality. Role of change in the levels of inflammatory markers post drainage in predicting outcome in acute cholangitis is uncertain.
Aim To evaluate the predictive value of changes in CRP and procalcitonin levels after biliary drainage in relation to outcomes (survival or mortality) at one month.
Methods A prospective observational study of consecutive adults presenting with AC was performed. At admission and at 48 hours post biliary drainage, procalcitonin and CRP were sent.
Results Between August, 2020 till December, 2020 we recruited 72 consecutive patients of AC The median age of the patients was 55 years (range 43-62 years) and 42 (58.33%) were females. The etiology of obstruction in AC was due to benign causes in 45 (62.5%) patients and underlying malignancy was present in 27 (37.5%) patients. Fourteen (19.4%) patients had a previous history of endoscopic retrograde cholangiopancreatography (ERCP) performed for biliary diseases while 13 (18.05%) patients had underwent cholecystectomy. Three patients (4.1%) had biliary-enteric anastomosis in the past. Although the delta change in serum procalcitonin (p value<0.001) and CRP (p value<0.001) 48 hours post drainage was significant, it had no bearing on the outcome. Altered sensorium and INR were independently associated with mortality at 1 month. The 30-day mortality prediction of Day 0 procalcitonin was measured by receiver operating characteristic (ROC) analysis which resulted in an area under the curve (AUC) of 0.697 with a 95% confidence interval (95% CI) of 0.545-0.849. The optimal cut-off of procalcitonin would be 0.57 ng/mL with a sensitivity and specificity of 80% and 60% respectively to predict mortality.
Conclusion Change in serum procalcitonin and CRP levels at 48 hours post drainage although significant, had no impact on the outcome of acute cholangitis.
Keywords Procalcitonin, CRP, Acute cholangitis, Biliary drainage, Outcome
371
Estrogen receptor 1 (ESR1) gene variants in patients with gallstones from southern part of India
Jayanthi Venkataraman
Correspondence – Jayanthi Venkataraman – vjglobal2018@gmail.com
Department of Hepatology, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai 600 116, India
Background Regional differences in type and composition of gallstones have been reported from the Indian subcontinent. Compared to north and north eastern parts of the country, most gallstones from southern states of India are either mixed (60%) or pigment (25%). Bile is also less lithogenic, and non-infective in South India; hemolytic anemia is absent. The reasons for these regional differences in the gallstone and bile composition are not clear. UGTA1 gene polymorphism has been reported in pigment gallstones from Hyderabad, south India. Estrogen receptor 1 gene polymorphism has been reported in north Indian patients with gallstones.
Aim of the study was to explore the role of two genetic variants, IVS1-397 T>C (rs2234693) and IVS1-351 A>G (rs9340799) in ESR in a south Indian population with gallstones.
Methods The present case control study recruited 40 subjects including 20 cases diagnosed with gallstones and 20 age and gender matched controls. Gallstones were collected from cases after cholecystectomy and morphological analysis was performed to determine the type of gallstone (cholesterol, pigment or mixed). Peripheral blood samples were collected and DNA was isolated and PCR-RFLP method was used for genotyping. Representative samples were sequenced to confirm the genotypes.
Results Majority of the stones were mixed (80%) and remaining were pigment. There were no cholesterol gallstones. On comparing the genotype frequency distribution in those with gallstone with healthy subjects, the heterozygous variant genotype, ESR1-397 TC (rs2234693) polymorphism (p-value:0.0026) and a haplotype combination of C allele of rs2234693 and A allele of rs9340799 were risk factors for gallstone disease (OR: 4.30).
Conclusion The preliminary findings of the present small sample size study provide factual information that ESR1-397T>C (rs2234693) gene polymorphic variant could be a susceptible factor for gallstone disease similar to that reported in a north Indian population.
Keywords Estrogen receptor cholesterol gallstone
372
Predictors of effective drainage during biliary stenting of hilar strictures with liver volume assessment
Rishikesh Malokar, Prasanta Debnath, Pravin Rathi, Sanjay Chandanani, Shubham Jain, Harsh Gandhi, Jay Chudasama
Correspondence – Rishikesh Malokar - malokarr@gmail.com
Department of Gastroenterology, Topiwala National Medical College, B Y L Nair Hospital, Mumbai 400 008, India
Introduction Hilar strictures can be both benign and malignant. The optimal strategies for drainage of hilar strictures are still controversial, mainly regarding the extent of drainage required and unilateral or bilateral stenting. The aim of this study was to identify predictors of successful biliary drainage mainly by liver volumetry.
Methods Prospective observational study was conducted. Total 14 patients of hilar strictures of Bismuth type II, III, or IV were studied who had either endoscopic or percutaneous biliary drainage. CT volumetry of 3 main hepatic sectors (left, right anterior, and right posterior) was calculated. The liver volume drained was estimated and classified into 2 classes: less than 50% (Group A) and more than 50% (Group B) of the total volume. Main outcome measurements: Primary outcome was effective drainage which was defined as a more than 50% fall in bilirubin at day 28 post-intervention. Secondary outcomes studied include complications, reintervention, and survival and mortality rates.
Results Mean age of study population was 55 years with 78.65% females. The commonest symptom other than jaundice was weight loss (85%). Most common type of block was type 2 (57.1%) followed by type 4 (35.7%) with commonest etiology being cholangiocarcinoma (57.1%), Ca gallbladder (35.7%). Nine patients (64.3%) had more than 50 % drainage (Group A) and 5 patients (35.7%) (Group B) had lesser than 50%. Mean total bilirubin in Group A on Day 0 was 16.43, Group B was 19.4, Day28 was 0.77 and 1.125 respectively. Difference in mean total bilirubin on Day 28 was not statistically significant (p value 0.46). Group B patients had more complications and lesser survival.
Conclusion Draining more than 50% of the liver volume is not required for 50% fall in bilirubin but had better survival and lesser complications. Type 2 Hilar block is most common type and has best prognosis. A pre-ERCP assessment of hepatic volume distribution on cross-sectional imaging may optimize endoscopic procedures.
Keywords Effective drainage, Hilar block, Group A, Group B, Liver volumetry
373
Unusual cause of obstructive jaundice- Eosinophilic gastroenteritis
Mandar Doiphode
Correspondence – Mandar Doiphode – mandardoiphode22@gmail.com
Department of Endoscopy, Gastrohub Clinic, Aundh, Pune 411 045, India
Introduction Eosinophilic gastroenteritis (EGE) is a rare condition of unknown etiology. It is characterized by peripheral blood eosinophilia and eosinophilic infiltration of the gut wall. The presenting symptoms depend on the site and depth of intestinal involvement and varies from abdominal pain, vomiting to acute bowel obstruction, ascites. Obstructive jaundice is an uncommon symptom of EGE.
Case Report We report a 47-year-old man who presented with abdominal pain, vomiting and jaundice. Investigations revealed abnormal liver tests, and peripheral blood eosinophilia. Ultrasonography of abdomen was suggestive of moderately dilated common bile duct (CBD) and intrahepatic biliary radicles due to 16 x 9 mm size calculus in distal CBD. On endoscopic retrograde cholangiopancreatography, the ampulla was irregular and bulging with stricture in the distal CBD with no obvious calculus. Biopsies from peripapillary duodenal mass showed evidence of eosinophilic gastroenteritis. Patient underwent biliary stenting and then was started on oral corticosteroids. He responded very well to that with complete resolution of the mass.
Conclusion Eosinophilic gastroenteritis is a comparatively rare but treatable cause of obstructive jaundice which can masquerade as malignancy and it should be kept in mind particularly in patient with peripheral eosinophilia.
Keywords Eosinophilic gastroenteritis, Obstructive jaundice
374
Comparison of perioperative outcomes of early versus late laparoscopic cholecystectomy in patients with biliary plastic endoprosthesis
Siva Sirasapalli1, Mohan Pazhanivel1, Senthamizhselvan Kuppusamy1, Kalayarasan Raja2, Kadambari Dharanipragada3
Correspondence – Mohan Pazhanivel – dr.pazhani@gmail.com
Departments of 1Medical Gastroenterology, 2Surgical Gastroenterology, and 3General Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Gorimedu, Puducherry 605 006, India
Background In patients with cholelithiasis and choledocholithiasis, there is no clear consensus on the timing of laparoscopic cholecystectomy (LC) following the removal of common bile duct (CBD) stones by endoscopic retrograde cholangiopancreatography (ERCP). An elective interval laparoscopic cholecystectomy (LC) is commonly performed in resource poor settings. The aim of the present study was to compare the outcomes of early LC with delayed LC after ERCP clearance of CBD stones and placement of a biliary stent.
Methods This was a retrospective study conducted between January 2019 and July 2021, including patients who underwent ERCP for removal of CBD stones followed by placement of a biliary stent. They were categorized into early (< 30 days) and delayed (> 30 days) LC groups based on the timing of surgery after ERCP. The outcomes of LC that were studied included: conversion of LC to open cholecystectomy (OC), bile leak, post-operative fever, length of hospital stay (LOS) (> 5 days) and surgical site infection. Chi-square test was used to compare the outcomes.
Results A total of 44 patients had ERCP and biliary stent before LC. Their mean age was 47.3 ± 13.6 years with slight female preponderance. Diabetes, hypertension and hypothyroidism were present in 25%, 22.7% and 9.3% patients respectively. 17 patients (38.6%) underwent early LC and 27 (61.4%) underwent delayed LC. LC was converted to OC in 10 (22.7%) patients. There was no significant difference in the conversion to OC (11.8% vs. 29.6%, p= 0.27), LOS (35.3 % vs. 37.1 %), postoperative fever (5.9% vs. 7.4%) and surgical site infection (11.8% vs. 11.1%) between the two groups. Bile leak occurred in one patient in delayed LC group.
Conclusion The timing of LC post ERCP stone clearance and biliary stenting did not influence the surgical outcomes in patients with gall stones and CBD stones.
Keywords Endoscopic retrograde cholangiography, Laparoscopic cholecystectomy, Choledocholithiasis
375
Enteroscopy assisted endoscopic retrograde cholangiopancreatography (e-ERCP) for the treatment of retained common bile duct (CBD) stone in a patient with post CBD exploration with T-tube in place and with surgically altered upper gastrointestinal anatomy: A case report
B Sidhartha, Praveen Mathew, Prasant Kanni, Chandra Babu, Manoj Gowda, Raghuveer Balabhadra, H N Nithin Kumar
Correspondence – Praveen Mathew – drpraveenmathew@yahoo.com
Department of Medical Gastroenterology, Vydehi Institute of Medical Sciences and Research Center, Bangalore 560 066, India
Introduction Endoscopic retrograde cholangiopancreatography (ERCP) for extraction of common bile duct (CBD) stones in patients with surgical anatomy remains technically challenging, due to the difficulty of not only reaching the papilla but also performing biliary cannulation or stone extraction, compared to those with normal anatomy. Enteroscopy assisted ERCP (e-ERCP) is most commonly used for biliary access in patients with surgically – altered upper gastrointestinal anatomy with reported suboptimal clinical success rates between 48% and 70%.
Open surgery with CBD exploration and T tube drainage are still traditionally performed in a large amount of selected patients with cholelithiaisis and choledocholithiasis who underwent failed ERCP. Complications of post CBD exploration include bile leak (3%), retained stone (6% -14%), T-tube wound infection (10%), main wound infection (13%) and wound dehiscence (6%).
Presentation of a case: A 63-year-old man who underwent gastrojejunostomy for gastric outlet obstruction 6 years back presented developed cholelithiasis with choledocholithiasis. Patient underwent open cholecystectomy and CBD exploration with T-tube placement. Patient developed post-surgery complications like cholangitis, retained CBD stone, bile leak, wound dehiscence and wound infection. An upper GI endoscopy was done and could not be negotiated beyond 10 cms from stoma. Patient was referred to our tertiary care center for enteroscopy assisted ERCP. In our center, patient underwent e- ERCP, balloon sphincteroplasty and stone extraction was done.
Conclusion Therapeutic e- ERCP for CBD stones in a surgically altered upper GI anatomy is feasible and safe. In this challenging case, s/p gastrojejunostomy and with multiple post-op complications, the e-ERCP method was performed safely and complete CBD clearance was achieved avoiding further surgical procedures.
Keywords Bile duct stones, Endoscopic retrograde cholangiography, Enteroscopy, Post CBD exploration
376
Gangrenous acute acalculous cholecystitis following corona virus disease 2019 infection: A case series of 5 patients
Awadhesh Narayan , Praveen Sharma, Ashish Kumar, Anil Arora
Correspondence – Awadhesh Narayan – drawadhesh2k14@gmail.com
Department of Gastroenterology, Sir Gangaram Hospital, Rajinder Nagar, New Delhi 110 060, India
Introduction Acute acalculous cholecystitis (ACC) accounts for approximately 10% of all cases of acute cholecystitis, mostly seen in critically sick patient and is associated with a high mortality. Here we present series of 5 cases who developed gangrenous AAC after covid infection.
Case report
| Serial No. | Age/Sex | Date of presentation | Duration of symptoms | Covid status | Imaging Findings | Comobidities |
| 1 | 46/M | 03/06/2021 | 2 days | Severe disease in April 2021 | MRCP- sloughed off membrane | None |
| 2 | 40/M | 22/07/2021 | 3 days | Mild disease in May 2021 | CECT- perforation with gangrene | T2 DM/CAD |
| 3 | 75/M | 26/07/2021 | 20 days | Mild disease in April 2021 | USG- wall edema, pericholecystic fat stranding | T2DM |
| 4 | 56/M | 28/072021 | 2 days | Severe disease in May 2021 | USG- wall edema and pericholecystic fluid | None |
| 5 | 37/F | 18/08/2021 | 5 days | Moderate disease in October 2020 | CECT- perforation with gangrene | None |
After diagnosis all patients underwent laparoscopic cholecystectomy and were discharged in stable condition. Histopathological examination of the surgical specimen revealed following findings.
| Histopathological Findings | |||||
| Serial no. | Transmural necrosis | Fibrinoid necrosis | Fibrin thrombi | Nerve hypertrophy | Vasculitis |
| 1 | + | + | - | + | + |
| 2 | + | + | + | + | - |
| 3 | + | + | - | + | - |
| 4 | + | + | - | + | + |
| 5 | + | 2+ | + | + | + |
Discussion It is difficult to prove but indirect evidences like- history of covid infection, ambulatory state at the time of presentation and histopathological findings typical of corona virus disease 2019 (COVID-19) ischemic gangrenous cholecystitis points towards its etiological basis.
SARS-CoV-2 entry inside human body is mediated by ACE2 receptors which is well expressed in GB beside vascular endothelium. It is quite possible that the COVID-19 might cause endothelitis in the gallbladder leading to inflammation and necrosis.
Keywords Gangrenous acute acalculous cholecystitis, COVID-19 infection, ACE2 receptors
377
Prolonged extrahepatic cholestasis despite repeated endoscopic retrograde cholangiopancreatography- Endoscopic ultrasound to rescue
Kondal Reddy Mogili , Rakesh Kumar Adi, Natraj Goud Burra
Correspondence – Kondal Reddy Mogili – kondal14r@gmail.com
Department of Medical Gastroenterology, Gleneagles Global Hospital, Lakdi-ka-pul, Opposite to Dwarka Hotel, Hyderabad 500 004, India
Introduction A 45-years-old male presented with acute cholangitis with progressive jaundice for 1 week. Computed tomography (CT) of abdomen showed abrupt narrowing of distal common bile duct (CBD) with dilatation of rest of CBD with mild central intrahepatic biliary dilatation (IHBD). For which he underwent endoscopic retrograde cholangiopancreatography (ERCP) and CBD stenting elsewhere. Brush cytology showed few atypical cells. As there was no improvement in liver chemistry parameters, redo ERCP was done after 2 weeks elsewhere. Based on cholangiogram they thought that it was a hilar stricture with Type III cholangiocarcinoma, hence stricture was dilated with Soehendra biliary dilation catheter (SBDC) and double pigtail biliary stent was placed (Fig. 1). As there was no improvement in liver chemistry even after two weeks. Came for further management.
Methods Planned for repeat ERCP and may take help of EUS for completion of the procedure.
Results ERCP was repeated for third time. On duodenoscopy CBD stent was seen in situ and removed with forceps. CBD canulation was done. Cholangiogram showed no filling of CBD and its biliary radicles-? False tract parallel to CBD (Fig. 2). Hence ERCP was attempted in rendezvous manner with aid of endoscopic ultrasound (EUS), after entering the CBD in antegrade manner (Fig. 3). EUS showed distal CBD stricture with IHBD. Biliary self-expandable metallic stent (SEMS) placed retrogradely (Figs. 4 and 5).
Conclusion For complex ERCP, biliary imaging is necessary prior to procedure 1. During ERCP, good understanding of biliary anatomy is required before stenting. When in doubt, EUS can be used for better understanding of biliary anatomy in the same setting 2. Complex ERCP are better done by an expert at high volume centers.
Keywords Cholangiopancreatography, Endoscopic retrograde, Endoscopic ultrasound
378
Comparison of ejection fraction in patients with gallstones with healthy subjects – A systematic review and meta-analysis
Deepak James 1 , Pankaj Gupta 2 , Deepa Kumar 1 , Harish Hooda 1 , Nishant Jaiswal 3 , Neelima Chadha 4 , Dimple Kalsi 1 , Usha Dutta 1
Correspondence – Usha Dutta – ushadutta@gmail.com
Departments of 1Gastroenterology, 2Radiodiagnosis and Imaging, 3Pediatrics, and 4Library, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Introduction Gallbladder (GB) stasis is one of the contributing factors for gallstone formation. We performed a systematic review and meta-analysis to determine the gallbladder ejection fraction (GBEF) among patients with gallstones and compare it with healthy subjects. We also examined if the GBEF varied depending on the methods used to elicit GB contraction or on the imaging modality
Methods The protocol for the study was registered in PROSPERO (Reg No. CRD42020201909). We searched PubMed, Embase, and Cochrane databases on 9 September 2020. All RCTs and cohort studies including abstracts that reported GBEF were eligible for screening. A preliminary search yielded 4584 studies. One hundred and thirty-three studies were included in the final analysis. The quality of the studies was assessed by Newcastle Ottawa Scale and the RoB2 tool. Data on study setting, subjects, baseline characteristics, diseases and comorbidities, symptom profile, and methodology for inducing gallbladder contraction and assessing GBEF was recorded. The I2 statistic was used to test heterogeneity and Egger’s test and funnel plot for publication bias.
Results We identified 133 studies for qualitative analysis and 102 studies for quantitative analysis. The mean GBEF among patients with gallstones (53.7% [CI 50.8% to 56.6%] [p<0.001]) was significantly lower than that of healthy subjects (69.9% [CI 68.7% to 71.1%] [p<0.001]) (mean difference of 17.8% [CI 13.9% to 31.7%] [p<0.001]). Among patients with gallstones, 22% (CI 10% - 34%) (p<0.001) had static GB (GBEF < 35%). The mean GBEF assessed using HIDA or ultrasound was similar. The mean GBEF elicited using fatty meal and cholecystokinin administration was also similar.
Conclusion Patients with gallstones have lower GBEF and more often have static GBs than healthy subjects. Ultrasound and HIDA scans yield similar results. Cholecystokinin and fatty meal stimulus also yield similar results.
Keywords Gallbladder ejection fraction, GBEF, Gallstone, HIDA, Cholecystokinin
379
Gallbladder neuroendocrine carcinoma, an impostor of gallbladder adenocarcinoma: A case report
S Rakesh Kumar , Akash Mathur, Ankur Yadav, Manoj Jain1, Uday C Ghoshal
Correspondence – Uday C Ghoshal – udayghoshal@gmail.com
Departments of Gastroenterology, and 1Pathology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India
Background Gallbladder neuroendocrine neoplasms (GB-NEN) are rare tumors. With a prevalence of 0.5%, they account for 2.1% of all gallbladder tumors. GB-NEN typically presents with right upper quadrant pain, nausea, and non-specific symptoms, often mimicking stone disease or gallbladder polyp, resulting in clinical misdiagnosis. We present here a rare case of GB-NEN. Case report: A 48-year-old female with no known comorbidities presented with dull aching pain abdomen and a progressively increasing abdominal lump. There were no signs of GI bleeding, bowel obstruction, jaundice, or features of carcinoid syndrome. On examination, she had a palpable hard and non-tender intraperitoneal abdominal lump in the right upper quadrant. Her blood investigations were normal. Computerized tomography (CT) imaging showed a mass lesion in the gallbladder fundus with transmural spread into pericholecystic fat and contiguous infiltration into adjacent liver segments with multiple peripherally enhancing mass lesions. FNA from liver SOL showed poorly differentiated adenocarcinoma. However, there was no biliary obstruction even with significant radiological disease burden, an atypical enhancement pattern on imaging, and a well-preserved patient, an alternate pathology was suspected, and biopsy was done. Truecut biopsy from GB mass showed WHO grade III neuroendocrine carcinoma with a Ki Index of 30%.
Conclusion GB-NEN are rare and fatal, but its symptoms are non-specific, and its diagnosis relies on histology and immunohistochemistry. A high degree of clinical suspicion is essential for identifying and managing the disease at the early stage.
Keywords Neuroendocrine tumors, Gallbladder, Adenocarcinoma
380
Patients with gallstones have static and sluggish gallbladders
Deepak James1, Harish Hooda1, Deepa Thakur1, Pankaj Gupta2, Raghuraman Soundararajan 2, Harish Reddy1, Rimpi Singla3, Mohammed Talha Noor1, Prashant Shah1, M Ravikiran1, Sanjay Chaudhary1, Kuldip K Solanki1, Tejinder Kaushal4, Alok Kumar4, Nikhil Bush1, Gayathri Petluri4, Dimple Kalsi1, Priyanka Popli1, Lileswar Kaman5, Anish Bhattacharya6, Anupak Kumar Singh1, Jimil Shah1, Harshal S Mandavdhare1, Vishal Sharma1, Usha Dutta1
Correspondence – Usha Dutta - ushadutta@gmail.com
Departments of 1Gastroenterology, 2Radiodiagnosis, 3Obstetrics and Gynaecology, 4Internal Medicine, 5General Surgery, and 6Nuclear Medicine and Imaging, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Introduction Gallbladder (GB) stasis promotes gallstone formation. Dissolution therapy is effective only in patients without GB stasis. We studied GB contractile function using prospectively collected data in a structured format in patients with gallstone disease and compared it with normal subjects.
Methods We analyzed prospectively collected data of subjects who underwent GB ejection fraction (GBEF) assessment in a tertiary care center in North India. We compared their baseline characters, demographics, symptom profile, investigations, and GBEF. GBEF was assessed 30 minutes and 60 minutes after a standard fatty meal using ultrasonography or HIDA scan. GBEF < 35% was defined as GB stasis. If the peak GB contraction was attained after 30 minutes of the meal, it was defined as sluggish GB. Both sluggish and static GB were regarded as having GB dysfunction.
Results There were 501 patients with gallstones (mean age 45.8, SD 14 years 76% females) and 85 healthy controls (mean age 36.4, SD 12 years, 35% females). The median GBEF (25th, 75th centile) among the groups were: patients with gallstone 31% (17%, 50%) and healthy subjects 54% (48%, 62%). The GBEF was significantly low in patients with gallstones when compared to normal subjects (p 0.014). Patients with gallstones more often had sluggishly contracting GBs than healthy controls (75% vs. 10%, p<0.001). 62% of the static GBs were sluggish also.
Conclusion GB is static and sluggish in patients with gallstones
Keywords Gallbladder ejection fraction, GBEF, Gallstone
381
Assessment of physical, chemical, and bacteriological nature of gallstones and their relation to gallbladder mucosal inflammation and preneoplastic lesions
Dimple Kalsi 1 , Deepak James 1 , Deepa Thakur 1 , Harish Hooda 1 . Pallab Ray 2 , Uma Nahar 3 , Shalmoli Bhattacharya 4 , Lileswar Kaman 5 , Arunanshu Behera 5 , Divya Dahiya 5 , Pankaj Kumar 3 , Ravi Kanojia 6 , Harshal Mandavdhare 1 , Vishal Sharma 1 , Jimil Shah 1 , Anupam Kuma Singh 1 , Usha Dutta 1
Correspondence – Usha Dutta – ushadutta@gmail.com
Departments of 1Gastroenterology, 2Medical Microbiology, 3Histopathology, 4Biophysics, 5General Surgery, and 6Pediatric Surgery, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Introduction Gallstones (GS) are pivotal in the pathogenesis of chronic cholecystitis and gallbladder (GB) carcinoma. Physical, chemical and biological nature of GS in high incidence areas for chronic cholecystitis have not been characterized. We determined the nature of GS among patients undergoing cholecystectomy and its association with GB inflammation.
Methods A prospective study was performed among patients undergoing cholecystectomy (n=220) and control (n=29) without stones (Whipple’s procedure [n=26) and children with choledochal cyst [n=3]). Clinical and demographic profile was recorded. GS were collected at the time of cholecystectomy were analyzed for their physical and chemical (Fourier Transform Infra-Red spectroscopy, total cholesterol estimation) nature. GS and GB tissue were analyzed for bacterial presence by MALDI-TOF and 16S rRNA sequencing. Gallbladder tissue, processed and stained with H&E and PAS-AB; inflammation and metaplasia was characterized.
Results The mean age (SD) of patients with gallstones was 40 (15.4) and 50 (20.4) years in the control group. The proportion of females among GSD group was 70% and 48% among controls (p=0.025). On analysis of the physical nature of stones, 75% were multiple, 80% were sinking, 45% had a rough surface. Analysis of chemical nature revealed 89% (195) cholesterol stones and 11% (25) mixed stones by FTIR with 78% (171) stones had >70% cholesterol on quantitative analysis. GBs with inflammation had significantly larger (1.65 mL and 1.98 mL, p=0.01), heavier (2.19 mg vs. 2.96 m, p=0.04) and harder (3395 N vs. 3909 N, p=0.006) stones. Mucosal tissue from GB with stones had positive cultures more often than those without stones (82% vs. 31%, p<0.001). GSD group more often had severe inflammation (94% vs. 6%, p=0.001), hyperplastic lining epithelium (51% vs. 14% p<0.001%) and metaplasia (15% vs. 0%, p=0.025) than the control group. Age more than 50 years increased the risk for metaplasia by 3 times in GSD cases.
Conclusion Gallstones which were multiple, had rough surface, larger, heavier, harder, and sinking were more often associated with inflammation. Inflammation and metaplasia was more frequent in GBs with stones.
Keywords Gallbladder, Gallstone, Inflammation, Metaplasia
Pancreas
382
Diclofenac induced severe pancreatitis – A rare case study
Mayank Chugh
Correspondence – Mayank Chugh - mayank19@yahoo.com
Department of Gastroenterology, Chugh Multispeciality Hospital, Meham Gate, Circular Road, Bhiwani 127 021, India
Acute pancreatitis is sudden inflammation of the pancreas that may be mild or life threatening but usually subsides. Acute pancreatitis is an acute inflammatory process of the pancreas with varying involvement of regional tissues or remote organ systems. Gallstones and alcohol abuse are the main causes of acute pancreatitis. Severe abdominal pain is the predominant symptom. Blood tests and imaging tests, such as computed tomography, help the doctor make the diagnosis. Whether mild, moderate, or severe, acute pancreatitis usually requires hospitalization. Here case reported with a history of tooth removal and given analgesic – nonsteroidal anti-inflammatory drugs (NSAIDs) – Diclofenac post intake patient develop severe pain abdomen, vomiting and restlessness. Patient being hospitalized for the same and regular investigation done suggestive of acute pancreatitis. Patient recovered as per standard treatment given.
Keywords Acute pancreatitis, Diclofenac, Serum amylase
383
Association of severity of acute pancreatitis with presence of asymptomatic fatty liver disease
Naveen Chand Make, Babu Vinish, J Kayalvizhi, B S Ramakrishna
Correspondence – Naveen Chand Make – navnchand9@gmail.com
Department of Medical Gastroenterology, SRM Institutes for Medical Sciences, No. 1, Jawaharlal Nehru Street, Vadaplani, Chennai 600 026, India
Introduction Acute pancreatitis (AP) is a common disease which is associated with significant mortality when severe. Fatty liver disease is common in the general population and is associated with an inflammatory state. We hypothesized that the presence of fatty liver in an individual with AP may be associated with the severity of pancreatitis. The aim of this study was to investigate a possible association of fatty liver with severity of AP.
Methods Consecutive patients admitted with AP, diagnosed as per standard criteria, were enrolled in the study. Severity of AP was assigned based on the 2012 Atlanta classification. Fatty liver was defined as liver-to-spleen attenuation ratio of less than one on computed tomography scan of the abdomen. Patients were followed for outcomes including length of hospital stay, days in intensive care unit, presence of organ failure, local complications, and mortality.
Results In this ongoing study, among 58 patients recruited so far, fatty liver was found in 28 (48.27%) while 30 (51.72%) had normal liver attenuation. Compared with patients without fatty liver, the severity of pancreatitis was significantly higher in fatty liver patients (Table 1). The prevalence of local complications (11 vs. 6), persistent organ failure (8 vs. 2) and deaths (2 vs. 0) were higher in patients with fatty liver compared to those without.
Table 1 Comparison of acute pancreatitis patients with and without fatty liver
| Fatty liver | No fatty liver | P value | |
| Number | 28 | 30 | |
| Severity | |||
| Mild | 9 | 22 | |
| Moderate | 11 | 6 | 0.0053 |
| Severe | 8 | 2 |
Conclusion Fatty liver may play a prognostic role in AP and could be incorporated into future predictive scoring models.
Keywords Acute pancreatitis, Fatty liver, Severity
384
Usefulness of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in acute pancreatitis: A prospective observational study
Radhika Nittala, Manas Behera1, Girish Pati, Vybhav Venkatesh, Manoj Sahu, Jimmy Narayan, Debakanta Mishra, Subhasis Pradhan, Vasista Palnati
Correspondence – Radhika Nittala- drnradhika@gmail.com
Department of Gastroenterology, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India and 1Hepatology, S C B Medical College, Kalinga Nagar, Bhubaneswar 751 003, India
Background Acute pancreatitis (AP) is a severe and complex disease associated with significant mortality and morbidity. Several scoring systems and prognostic indicators are in use for assessing the severity of AP and predicting the outcomes, however, they have not yet proved to be accurate. We conceptualised this study to evaluate the usefulness of simple and relatively inexpensive tools: the neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR)in predicting the severity and outcome of patients with AP.
Methods A prospective study was conducted in a tertiary care referral centre of Odisha from March 2020 to April 2021. One hundred and eight consecutive patients of AP were enrolled and the NLR and PLR were calculated. Severity of AP was classified as per the revised Atlanta classification.
Results The median age of patients was 38 (29,45) years with a male predominance (79%). Alcohol was most common etiology (62%) followed by biliary (30%). Mild and severe AP were seen in 52.7% (57) and 47.3 % (51) respectively (moderately severe-28; severe-23). The overall mortality was 8% (9). Median NLR and PLR were significantly higher in the severe AP as compared to mild AP (NLR-11.9 [8.2,14.8] vs. 7.9 [4.7,12.1], p=0.004; PLR-191.4 [129,303.6] vs. 152 [115.3, 209.6], p=0.005]). Similarly, median NLR (13.2 vs. 9.3, p=0.015) and PLR (384.6 vs. 159.1, p<0.001) values were significantly higher in the non-survivors when compared to the survivors. Also, these ratios had significant but weak positive correlation with BISAP and APACHE II scores.
Conclusion NLR and PLR are simple, cheap, easily available biomarkers which can be useful given their association with the severity and mortality in patients with AP.
Keywords Acute Pancreatitis, Severity, NLR and PLR
385
Hemosuccus pancreaticus- A single tertiary care centre experience
K H Vinod Gowda, Mallikarjun Patil, Harshad Devarbhavi, Sunu Sara Kurien, Syed Shafiq
Correspondence – Vinod Gowda K H – vinodgowdakh@gmail.com
Department of Gastroenterology, St. Johns Medical College Hospital, Sarjapur Road, Koramangala, Bangalore 560 036, India
Introduction Hemosuccus pancreaticus (HP) is a rare complication of acute and chronic pancreatitis and usually presents with gastrointestinal bleeding and abdominal pain. The studies about HP are sparse and limited to case reports and small case series, hence present study was aimed at studying the various clinical features, imaging findings, treatment, and outcome.
Methods We retrospectively analyzed the data of all acute and chronic pancreatitis patients presenting with HP between January 2015 and September 2021. All suspected patients of HP underwent side viewing endoscopy, CT angiography and subsequently conventional angiography and coil embolization in whom pseudoaneurysm was seen.
Results There were 21 patients who presented with UGI bleed and was diagnosed with HP. Mean age was 42.3 years with 90.5% (19) men. Melena was the most common symptom (80.95%). Median duration of bleeding before diagnosis was 5 days. Overall, 85.7% patients had chronic pancreatitis and 14.3% had acute pancreatitis.
Visceral artery pseudoaneurysm was noted in 57.1% of cases. Splenic artery (41.6%) and gastroduodenal artery (41.6%) pseudoaneurysms were the common source of bleed. Selective arterial embolization was done in 57.1% and was successful in 91.6% while 9.5% underwent surgery. Seven patients were managed conservatively due to varied reasons. Overall rebleeding rate was 8.3%.
Conclusions Hemosuccus pancreaticus is most commonly associated with chronic pancreatitis. Predominantly affected are males (90.5%) with most common symptoms of melena (80.95%) and pain abdomen (57.1%). Most commonly involved vessels are splenic artery and the gastroduodenal arteries. All patients should undergo prompt initial angiographic evaluation and embolization if feasible. Patient with unsuccessful embolization should undergo emergency surgery. Multidisciplinary team approach and a well-defined management protocol is essential to reduce the mortality and morbidity.
Keywords Hemosuccus pancreaticus, angioembolisation, chronic pancreatitis
386
Acute pancreatitis as an initial manifestation of systemic lupus erythematosus: An uncommon presentation
Anirudh Karanam, Manoj Kumar Sahu, Girish Kumar Pati. Jimmy Narayan, Debakanta Mishra, Vybhav Venkatesh, K Pruthvi, Vasistha Palnati, Pukhraj Singh, Uppu Pooja1, Subhasis Pradhan
Correspondence – Anirudh Karanam – Anirudhkaranam71@gmail.com
Depts of Medical Gastroenterology, and 1General Medicine, IMS and SUM Hospital, Kalinga Nagar, Bhubaneshwar 751 003, India
Introduction Systemic lupus erythematosus (SLE) is a multi-system disorder mostly affecting females. Gastrointestinal manifestations are known to occur in SLE and acute pancreatitis (AP) is a rare manifestation which has been reported in the range of 0.2% to 8.2%, usually in already diagnosed SLE cases. Here we describe a 40-year-old gentleman with AP as the initial manifestation of SLE.
Case report A 40-year-old man presented with fever and abdominal pain for 20 days. The pain was localized to the epigastric region with radiation to back. On examination, his vitals were stable and there were multiple oral ulcers. Abdomen was tender and other systemic examination was unremarkable. Laboratory investigations revealed anemia (7.7 g/dL), thrombocytopenia (11,040 cells/mm3), deranged kidney function (creatinine-2.61 mg/dL), elevated amylase (1088 U/L) and lipase (1841 U/L). In view of fever, additional work up for other etiologies was done which showed negative results for malaria and dengue; sterile blood and urine cultures, and 3+ urine proteinuria. Ultrasound abdomen showed bulky pancreas with peripancreatic fat stranding. Computed tomography (CT) scan was suggestive of AP with a CT severity of 6. He was managed with intravenous fluids, analgesics and additional supportive management (naso-jejunal feeds were initiated in view of oral feed intolerance) to which he responded well. In view of oral ulcers, anemia, thrombocytopenia and proteinuria, a possibility of SLE was considered. Further investigations showed a positive anti-nuclear antibodies (3+; homogenous) and positive anti-ds DNA antibodies (2+). As per the Systemic Lupus International Collaborating Clinics (SLICC) criteria, a final diagnosis of SLE was made and appropriate treatment was initiated.
Conclusion Besides being a complication in generalized flare of the disease, AP can be a presenting manifestation in SLE. Presence of systemic manifestations in a case of AP, should alert the clinician in search for other possible etiologies.
Keywords Acute pancreatitis, SLE, Inflammation
387
Role of statins in the treatment of pancreatic ductal adenocarcinoma
Raghuram Tangirala , Priya Nair, Anoop K Koshy, Harshavardhan Rao B, Rama P Venu, Krishna Priya, Renjitha Bhaskaran
Correspondence – Raghuram Tangirala – raghuramtangirala@gmail.com
Department of Gastroenterology, Amrita Institute of Medical Sciences, Floor Two Block One, Department of gastroenterology, Ponekkara 682 041, Kerala
Introduction Pancreatic ductal adenocarcinoma (PDAC) is an aggressive cancer with a dismal prognosis. Statins, apart from its action as cholesterol lowering agent, have also been demonstrated to have anti-tumour effects by inhibiting angiogenesis, preventing metastasis, and inducing apoptosis. However, the efficacy of statins in improving overall survival in patients with PDAC has not been established.
Methods We conducted an observational, prospective cohort study in which all consecutive histologically proven PDAC patients between January 2016 to December 2019 were included. Statin users were defined as those who had taken statins for a minimum period of 3 months. All relevant demographics, diagnostic procedures and treatment details were recorded in pre-designed proformas. Patients were then followed up for a minimum duration of 1 year. Primary outcome of the study was overall survival. Stratified analysis was performed with respect to stage (metastatic vs. non-metastatic) and treatment modality offered (curative resection, palliative chemotherapy, palliative biliary drainage).
Results A total of 153 patients diagnosed with PDAC were included (mean age 61±11.76, M: F=1.55). Thirty patients (19.6%) were classified as statin-users. On univariate analysis, median survival was significantly longer among statin-users (482 days) as compared to patients not on statins (119 days) (p value 0.019). Statins were found to have an independent association with overall survival (HR – 0.47, 95% CI 0.247 – 0.897, p value 0.022) on multivariate analysis. There were no differences in the overall survival among the different types and dosage of statins. In stratified analysis, statins provided a significant survival benefit in patients on conservative management (p value 0.04) and patients with metastatic disease (p value 0.05).
Conclusions Statins provided a significant survival advantage in patients with PDAC and reduced the risk of mortality by 53%. The effect of statins was most evident among patients on conservative management and among patients with metastatic disease.
Keywords Adenocarcinoma, Metastatic, Statins, Survival
388
Intestinal permeability changes in L-Arginine model of chronic pancreatitis
Ambika Prasanna, Aparna Jakkampudi, Subhaleena Sarkar, Priyanka Sarkar, D Nageshwar Reddy1, Rupjyoti Talukdar2
Correspondence – Rupjyoti Talukdar – rup_talukdar@yahoo.com
Department of Wellcome DBT India Alliance Labs, Institute of Basic and Translational Research Mindspace Road, Gachibowli, Hyderabad 500 032, India, 1Department of Medical Gastroenterology, Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India, and 2Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs. Asian Institute of Gastroenterology, Institute of Basic and Translational Research, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Background Chronic pancreatitis (CP) is characterized by abdominal pain, pancreatic exocrine insufficiency and endocrine dysfunction/diabetes. Our clinical studies demonstrated alterations in the intestinal microbiota in patients with CP. Intestinal microbial dysbiosis has been associated with gut barrier alterations across several studies. The present study aims to evaluate such intestinal changes in an experimental model of CP.
Methods 11-14 weeks old male C57BL/6J mice were administered weekly intraperitoneal injections of 9% (450 mg/100 g BW) L-Arginine hydrochloride for 6 weeks. Body weights and feed intake were monitored twice weekly. After the last injection, the mice were euthanized using intraperitoneal administration of 100 mg/kg ketamine and 10 mg/kg xylazine. Pancreata and intestines were resected aseptically, fixed in 10% formalin and processed for paraffin embedding. Fibrosis in the pancreatic tissues was assessed by H&E staining and confirmed using picro-sirius red (PSR) staining. The jejunal tissues were subjected to immunohistochemical staining for the gut barrier integrity markers ZO-1 and Caspase-3. The stained area was quantified from the total area on Image J software.
Results At the end of 6th week severe CP was induced that was characterized by adipocyte infiltration and progressive acinar cell damage in pancreatic tissues. PSR positive staining confirmed parenchymal fibrosis. From 3rd to 6th week there was a 2.33-fold increase in fibrosis, which was statistically significant (p< 0.05). Quantification of ZO-1 showed decreased staining whereas Caspase-3 showed increased staining in 6th week experimental mice than in sham controls.
Conclusions Our study suggests gut permeability changes in L-Arginine model of chronic pancreatitis.
Keywords Chronic pancreatitis, Experimental, L-arginine model, Intestinal permeability
389
An uncommon cause of gastrointestinal bleeding: Hemosuccus pancreaticus due to proximal gastroduodenal artery pseudoaneurysm
Antony George , Rushil Solanki, Vijay Narayanan, A Shanid, Krishnadas Devadas
Correspondence – Antony George – anthony00590@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Hemosuccus pancreaticus is a rare cause of gastrointestinal bleeding, posing a significant diagnostic and therapeutic dilemma. The diagnostic clues are gastrointestinal bleeding associated with abdominal pain in the background of chronic pancreatitis. Hemosuccus pancreaticus secondary to gastroduodenal artery pseudoaneurysm is rarely reported in the literature. We report the case of a 28-year-old male, with a history of chronic pancreatitis on PERT, who presented with a history of abdominal pain associated with upper gastrointestinal bleeding. He had a history of three similar episodes over the past seven months. At presentation, the patient had features of anemia and postural hypotension. Blood investigations revealed hemoglobin levels of 4.5 g/dL and peripheral smear revealed hypochromic microcytic anemia. His amylase/lipase levels were normal. He was treated with whole blood transfusions. Initial esophagogastroduodenoscopy (EGD) revealed a normal study. During hospital admission, the patient developed an episode of severe abdominal pain and hematemesis. Emergency EGD done within 30 minutes revealed blood oozing from the ampulla of Vater. Abdominal contrast-enhanced computed tomography revealed features of chronic calcific pancreatitis with multiple pseudocysts. The gastroduodenal artery was seen coursing anterior to a pseudocyst of size 2.4 x 2.7 x 3.9 cm in the region of the head of the pancreas and a small (4-5 mm) proximal gastroduodenal artery pseudoaneurysm was identified. In the same setting, he underwent “sandwich method” angiographic coil embolization using 5x5 mm and 5x7 mm coils. Post-procedure, the patient had no further symptoms and was discharged. The patient was followed up at two months and, he had no further abdominal pain or bleeding. Hemosuccus pancreaticus is a life-threatening cause of upper gastrointestinal bleed. A high index of clinical suspicion is required for early detection. A multidisciplinary approach is required for effective management involving gastroenterologists, vascular surgeons, and interventional radiologists. It can be successfully treated with angiographic coil embolization.
Keywords Hemosuccus pancreaticus, Chronic pancreatitis, Gastroduodenal artery pseudoaneurysm, Angiographic embolization
390
The impact of personalized education on pain, depression, and quality of life parameters in patients with chronic pancreatitis: Results from a pilot study
Subhalena Sarkar1, Priyanka Sarkar1, M Revanth2, Ambika Prasanna1, Misbah Unnisa3, Aparna Jakampudi1, D Nageshwar Reddy3, Rupjyoti Talukdar4
Correspondence – Rupjyoti Talukdar – rup_talukdar@yahoo.com
1Department of Welcome DBT Indian Alliance Labs., Institute of Basic and Translational Research, Asian Healthcare Foundation, Mindspace Road, Gachibowli, Hyderabad 500 032, India, 2Department of Radiodiagnosis, Asian Institute of Gastroenterology, Gachibowli, Hyderabad 500 032, India, 3Department of Gastroenterology, Asian Institute of Gastroenterology, Gachibowli, Hyderabad 500 032, India, 4Department of Medical Gastroenterology; Welcome DBT Indian Alliance Labs., Asian Institute of Gastroenterology, Institute of Basic and Translational Research, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Introduction Chronic pancreatitis (CP) is associated with depression [RT1] [sS2] and poor quality of life. Pain in CP tend to recur after treatment. Patients with CP has misperceptions regarding CP. The impact of ignorance on the response to treatment is unknown. In this prospective study, we aimed to evaluate the impact of the disease related education on depression, QOL and symptoms in patients with CP.
Methods [RT1] [sS2] Ninety patients with painful CP were screened of which 64 patients were analyzed. We recorded demography (age/education/socioeconomic), disease details (pain details [VAS], diabetes, intervention), depression status (Beck depression inventory [BDI] II), and QOL (EORTC QLQ c30). Patients were then provided disease related education based on their disease characteristics (personalized education). Re-evaluation done for clinical outcomes was done after 3 months.
We also performed magnetic resonance spectroscopy (MRS) in a subset of patients to evaluate brain glutamate/glutamine (Glu/Glx), myoinositol, N-acetyl aspartate (NAA), creatine in the pre-frontal cortex (PFC), hippocampus (H), basal ganglia (BG), and anterior cingulate cortex (ACC), and assess the correlations with pain and QOL.
Pre-post data comparison was performed using the Wilcoxon matched-pair signed rank test, and the extended Mantel-Haenszel (MH) c2 test for linear trend, as appropriate.
Results The mean age (SD) of patients was 37.6 (12.10). There were 47 (77%) male and 25 (39%) diabetics. On follow-up, there was a significant improvement in the frequency of depression (MH χ2 linear trend- 5.9; p=0.015). Significant improvement was observed in BDI II score (p=0.001), pain episodes (p=0.009) and VAS for pain (p=0.02). Significant improvement was also observed the role and emotional functions of EORTC QLQc30 (adj. p=0.008 and 0.026 respectively).
The metabolites myoinositol in the right ACC and Glu/Glx in the left BG had a negative and positive correlation respectively with pain scores.
Conclusion Personalized education could improve clinical outcomes of CP by improved coping via metabolomic alterations within the brain.
Keywords Chronic pancreatitis; pain, Quality of life, Depression, Metabolites, Personalized education
391
Characteristics of idiopathic recurrent acute pancreatitis in a large cohort of Indian patients
Misbah Unnisa1, V V Ravikanth2, Steffie Avanthi2, Govardhan Bale2, D Nageshwar Reddy3, Rupjyoti Talukdar3
Correspondence – Rupjyoti Talukdar – rup_talukdar@yahoo.com
1Department of Medical Gastroenterology, Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India, 2Department of Genetics Institute of Basic and Translational Research, Asian Healthcare Foundation, Gachibowli, Hyderabad 500 032, India, and 3Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs., Asian Institute of Gastroenterology, Institute of Basic and Translational Research, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Introduction Recurrent acute pancreatitis (RAP) is defined as occurrence of two or more episodes of documented acute pancreatitis (AP) with complete resolution of symptoms and laboratory abnormalities between episodes. In this cross-sectional study we evaluate the genetic associations of idiopathic RAP.
Methods We enrolled 805 consecutive patients (discovery coort) with AP from January to November 2018 and 190 patients in a validation cohort of RAP from June to September 2021. All patients with documented RAP were subjected to magnetic resonance cholangiopancreatography (MRCP) to evaluate for early changes of CP and structural anomalies. We evaluated for the various genetic polymorphisms including SPINK1, PRSS1, CTRC, CTSB, claudin, MORC4 and BACH2. Demographic characteristics, genotype data, duration and number of recurrent episodes and details of other etiologies were recorded. We divided patients into 3 age groups which is <18 years, 18-30 years and >30 years. Clinical data were compared using Chi-square test/Fischer’s exact test.
Results Mean (SD) age of patients in discovery and validation cohorts were 32±13.7 and 28.6±11.4 respectively. Number of AP and RAP patients in discovery cohort was 412 (51.1%) and 393 (48.8%) respectively. In the discovery cohort, a significantly higher number of idiopathic cases was found in <18 years age group (118 [76.15%]). The most commonly identified genetic polymorphism was claudin rs7057398 (in 43 [27.7%]), followed by PRSS1 rs10273639 (in 41 [26.5%]) and 29 (18.7%) CTSB rs12338 in this cohort. In the validation cohort, 24 (49%) had CTSB rs12338 followed by 19 (38.7%) BACH2rs9111 and 16 (32.6%) MORC4 rs12688220. Early changes of chronic pancreatitis was significantly higher in the 18-30 years age group (60 [26.7%]).
Conclusion In this study we found the presence of genetic polymorphism in <18 years old idiopathic recurrent acute pancreatitis to be more in comparison to other age groups, while early CP changes were greater in the age group of 18-30 years.
Keywords Recurrent acute pancreatitis, Idiopathic, Genetic polymorphisms
392
Jejunal microbiome in patients with chronic pancreatitis: A pilot study
Priyanka Sarkar 1 , Subhaleena Sarkar 1 , Misbah Unnisa 2 , Ambika Prasanna 1 , Aparna Jakkampudi 1 , D Nageshwar Reddy 2 , Rupjyoti Talukdar 2
Correspondence – Rupjyoti Talukdar – rup_talukdar@yahoo.com
1Department of Welcome DBT Indian Alliance Labs., Institute of Basic and Translational Research, Asian Healthcare Foundation, Mindspace Road, Gachibowli, Hyderabad 500 032, India, and 2Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs., Asian Institute of Gastroenterology, Institute of Basic and Translational Research, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Background We earlier reported the significant differences in fecal bacteriome of chronic-pancreatitis (CP) patients with and without diabetes. In this study, we evaluate the jejunal bacterial flora in patients with CP.
Methods A well characterized 10 CP patients (diabetic=4, non-diabetic=6) and 1 healthy controls (HC) were recruited. 2-3 mL jejunal fluid was aspirated using sterile enteroscope, followed by fluid collection using a sterile syringe. Metagenomic DNA extraction were performed followed by V3-V4 region of 16SrDNA based on Miseq (2*250bp). The raw reads were annotated based on the Greengene database using QIIMEv1.9.1 with 95% similarity.
Results We observed significant differences in the bacterial profiles between the patients and control. There were a total of 23 phyla in the patients while 7 in HC. Additionally, 1888 bacterial species in patients and 188 in healthy control were observed. The patients with CP who had diabetes were dominated by Prevotella copri, however, the nondiabetics had more Fusobacterium nucleatum and Veillonella dispar in their jejunum. We, then studied the association among the FBS (fasting blood sugar) level and C-peptide with the patients’ bacterial profile. We observed the beneficial flora viz. Faecalibacterium prausnitzii, Eubacterium rectale, and Prevotella copri to be positively associated with FBS in diabetic and negatively in non-diabetic cohorts, suggesting a possible alteration of the beneficial flora-host crosstalk in the diabetic cohort. C-peptide exhibited negative correlations with butyrate producing bacteria, Abiotrophia para-adiacens and positive correlations with Faecalibacterium prausnitzii and Eubacterium rectale in diabetic cohort. In non-diabetic patients C-peptide was found negatively associated with Eubacterium rectale, Gemella sanguinis and positively with Faecalibacterium prausnitzii.
Conclusion In this study, we are reporting for the first time the jejunal microbiome in patients with CP.
Keywords Chronic pancreatitis, Jejunal microbiome, Diabetes
393
Plasma metabolomic alterations in patients with chronic pancreatitis with pancreatic head mass: Potential to differentiate between a benign and a malignant lesion
A vadh Patel 1 , Priyanka Sarkar 2 , Subhaleena Sarkar 2 , Aparna Jakkampudi 2 , Ambika Prasanna 2 , D Nageshwar Reddy 3 , G V Rao 1 , Rupjyoti Talukdar 4
Correspondence – Rupjyoti Talukdar – rup_talukdar@yahoo.com
1Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India, 2Department of Wellcome DBT Indian Alliance Labs., Institute of Basic and Translational Research, Asian Helathcare Foundation, Gachibowli, Hyderabad 500 032, India, 3Department of Medical Gastroenterology, Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India, and 4Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs., Asian Institute of Gastroenterology, Institute of Basic and Translational Research, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Introduction Differentiating between a malignant and an inflammatory head of pancreas mass often poses clinical dilemma. In this study, we aimed to explore the plasma metabolites in patients with chronic pancreatitis with head of pancreas mass (malignant and inflammatory), its potential utility in diagnostics.
Methods We recruited 84 patients and 11 healthy controls (HC) for the study and the plasma metabolites were studied on gas chromatography mass spectrometry (GCMS) platform using an untargeted approach. We performed methanol extraction, followed by pyridine-MSTFA derivatisation as sample preparation method. The differences were tested using partial least square deviation analysis (PLSDA) plot, constructed in Metaboanalyst 4.0 and the significances were tested using Mann-Whitney U test or Kruskal–Wallis H test as appropriate in the Statistical Package of Social Scientists (SPSS), (IBM SPSS 20, SPSS Inc, Chicago, IL, USA).
Results In this abstract, we are reporting metabolome data for a total of 45 individuals (patients-34, HC-11). We investigated 160 metabolites out of the 450 observed in this study. Distinct metabolite profiles have been observed malignant and inflammatory mass cohort. Decreased level of benzaldehyde derivatives were observed in the malignant cohort compared with benign (<0.05). Additionally, we found elevation of 18 metabolites in the inflammatory mass group and 16 metabolites in the malignant mass group, including more concentrations of cholestenol and succinic acid and less amount of palmitic acid in the malignant group.
Conclusion Our data suggested the potential use of plasma metabolite in differentiating the benign and malignant head of pancreas mass in clinical practise. However, it will require further cross validation using a large cohort.
Keywords Chronic pancreatitis, Pancreatic mass lesion, Plasma metabolome
394
New-onset prediabetes/diabetes after acute pancreatitis: A prospective cohort study with 12-month follow-up
Wahid Akbar , Misbah Unnisa, Manu Tandon, D. Nageshwar Reddy, Rupjyoti Talukdar
Correspondence – Rupjyoti Talukdar – rup_talukdar@yahoo.com
Department of Medical Gastroenterology, Welcome DBT Indian Alliance Labs., Asian Institute of Gastroenterology, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Background Acute pancreatitis (AP) is known to result in endocrine dysfunction (prediabetes and diabetes). The objective of this study was to determine the temporal incidence of endocrine dysfunction after onset of AP and determine the risk factors in Indian patients.
Methods In this prospective study, enrolled patients diagnosed with AP between February 2019 to May 2019 were followed at 3, 6, and 12 months. Patients with RAP, CP and pre-existing endocrine dysfunction were excluded. Demographic and disease severity (clinical, laboratory and radiological) data were recorded. Mann-Whitney U and Chi-square tests were used to compare groups. Temporal trend for development of endocrine dysfunction was evaluated using the Extended Mantel Haenszel Chi-square test for trend. Logistic regression was used to identify independent risk factors.
Results Eighty-six patients (males 66, median [IQR]) age 33.0 (26.0-44.2) years who fulfilled enrolmentcriteria were finally analyzed. The most common etiology was alcohol (n=31 [36%]) followed by gallstones (n=17 [19.8%]). The proportion of patients with moderately severe and severe AP were 59.3% and 15.1%, respectively. Overall, the frequency of prediabetes and diabetes increased temporally across the follow-up period. These were respectively 2 (2.33%) and 1 (1.16%) at 3 months, 11 (12.8%) and 5 (5.81%) at 6 months and 20 (23.2%) and 9 (10.5%) at 1-yr. On multivariable logistic regression, intervention for walled-off necrosis (WON) emerged as the single independent risk factor for endocrine dysfunction (OR 9.01 [2.3-35.5]; p=0.002).
Conclusions Endocrine dysfunction is frequent after an episode of AP. Interventions for WON is an independent risk factor for endocrine dysfunction.
Keywords Acute pancreatitis, Diabetes, Risk factor, Interventions
395
A rare case of obstructive jaundice
Arun Solanki , Shubha Immaneni, A Aravind, Caroline Selvi, K Premkumar, A Murali, K Muthukumaran, Chezhian Annasamy
Correspondence – Arun Solanki – aurosolanki@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Primary gist in the pancreas is distinctly uncommon and very few cases been reported in the literature till date. We report a case of primary pancreatic GIST with liver metastasis presenting with obstructive jaundice.
Case report A 46-year-old diabetic female presented with complaints of painless progressive jaundice for 3 months with pruritis and clay-coloured stools, along with loss of appetite and weight. She had no prior history of any abdominal surgery, no fever and no gastrointestinal bleed. On examination, patient had icterus with palpable liver having firm consistency, nodular surface, palpable 6 cm below RCS and a 4 x 5 cm vague mass in epigastrium with firm consistency. Patient’s investigations showed total bilirubin-9 mg/dL, direct bilirubin-7.9 mg/dL, ALP- 567 IU/L, CA 19-9: 5 IU/mL, CEA: 0.84 IU/mL, CA 125: 32 IU/mL. Ultrasound abdomen showed hypoechoic lesions in head and uncinate process of pancreas and a hypoechoic nodule in segment 8 of liver. USG guided FNAC from liver and pancreatic lesion showed atypical spindle shaped cells, which on immunohistochemistry were CD34 and CD117 positive. CECT abdomen showed hypodense lesion arising from head and uncinate process of pancreas with abrupt cut off of distal CBD and dilatation of proximal CBD and multiple hypodense lesions in right lobe of liver. As patient already had liver metastasis, curative surgery could not be done and so was managed with palliative therapy with ERCP and CBD stenting by an uncovered SEMS and was started on Tab imatinib.
Conclusion Early diagnosis and treatment would save life of many patients of GIST; it requires indefinite follow-up post therapy.
Keywords Gastrointestinal stromal tumor (GIST), Jaundice, Imatinib, CD117
396
A great 331atient331d331 in upper gastrointestinal bleed patient
Debapratim Routh, Chezhian Annaswamy, Caroline Selvi, I Shubha, K Muthukumaran, R Murali, K Premkumar
Correspondence – Debapratim Routh – debapratimraja@gmail.com
Institute of Medical Gastroenterology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Hemosuccus pancreaticus is a rare cause of upper gastrointestinal bleeding. It is well known complication of acute and chronic pancreatitis. Gastrointestinal bleeding is due to rupture of pseudoaneurysm, most commonly splenic artery pseudoaneurysm into main pancreatic duct.
Case report A 35-year-old male with history of alcohol abuse presented with abdominal pain, 332atient332d332s and melena.On examination pallor was present with tender epigastric mass. On investigation there was hemoglobin drop during the course of admission and initial raised amylase and lipase. USG abdomen showed bulky pancreas. CT abdomen revealed well-formed intra pancreatic necrotic collection. Upper GI endoscopy showed fresh blood in duodenum. CT angiography suggestive of splenic artery pseudoaneurysm within walled of necrosis containing hemorrhagic content. Final diagnosis was splenic artery pseudoaneurysm ruptured within walled of necrosis resulting hemosuccus pancreaticus. Patient was managed by splenic artery coil embolization. 2 detachable nitinol coils were used. Post procedure improvement of hemoglobin noticed and CT abdomen suggestive of multiple splenic infarct. Post procedure vitals were stable, and patient was discharged 4 days after the procedure.
Conclusion Patient with hemosuccus pancreaticus required high clinical suspicion with regular follow-up and multidisciplinary approach.
Keywords Hemosuccus pancreaticus, Pseudoaneurysm, Walled of necrosis, Angiography, Coil embolization
397
A stent in time saves knives: Case report
S Rajeevan, R Murali, A Aravind, I Shubha, S Caroline, K Premkumar, K Muthukumaran, A Chezhian
Correspondence – Rajeevan S - rjvn2013@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction Multiple pseudoaneurysms in acute pancreatitis is a rare phenomenon. We report a case of two pseudoaneurysms in a patient, treated in two different ways.
Clinical Summary A 32-year-old male with alcohol-use-disorder was admitted with dull aching, boring type of upper abdominal pain radiating backwards of 1 month duration and an episode of hematemesis 2 weeks back followed by melena. He had no comorbidities. On examination, patient had pulse: 110/minute; BP: 100/60 mmHg and respiratory rate: 20/minute. He was pale. Abdominal examination revealed mild epigastric tenderness without any palpable mass. Melena was noted during digital rectal examination. Serial lab investigations showed falling hemoglobin levels from 9.8 g/dL to 6.5 g/dL. Serum amylase and lipase were 1038 and 437 U/L respectively. Coagulation workup, renal and liver function tests were normal. Ultrasound abdomen showed WON of pancreas compressing body and tail. CECT abdomen showed acute necrotizing pancreatitis involving body and tail with WON (8x6.4x6.7 cm) in the left anterior sub-hepatic space. UGI endoscopy showed 0.5x0.5 cm clean based ulcer in the body of the stomach with no fresh or altered blood in the lumen. CT abdominal angiogram showed 2 aneurysms, one from proximal splenic artery and another from gastro-epiploic artery. This was confirmed by DSA. Coil embolization of right gastro-epiploic artery aneurysm was done. Covered stenting was done for splenic artery aneurysm to maintain vessel patency. Post-procedure angiogram revealed complete exclusion of the aneurysms. USG guided aspirate of WON revealed 100ml of necrotic fluid with high amylase levels, following which its walls collapsed. Patient’s melena and abdominal pain subsided, and hemoglobin remained stable. CT abdomen after 2 weeks showed coils and stent in place and no intra-abdominal fluid collections.
Conclusion Pseudoaneurysm in acute pancreatitis is a life-threatening situation. Early diagnosis and timely intervention is the key to saving patient’s life.
Keywords Upper gastrointestinal bleed, Pancreatitis, Pseudoaneurysm, Covered stenting
398
A rare but fatal complication of acute pancreatitis – Pulmonary thromboembolism
Arun Dhotra, N Lavanya, Kani Shaikh, A Anand, R Akilandeshwari, N Arun, Vaishnavi Priya
Correspondence – Arun Dhotra – arun.dhotra88@gmail.com
Department of Digestive Health and Diseases, Government Kilpauk Medical College, Chennai 600 010, India
Introduction Acute pancreatitis is an inflammatory condition associated with local and systemic inflammatory response. Pulmonary thromboembolism is a very rare and life-threatening complication of acute pancreatitis. Several explanations have been proposed for this like systemic inflammatory response resulting in a hypercoaguable state or inflammatory mediators causing intrinsic endothelial damage or extrinsic damage of the veins from adjacent edema, fibrosis and cellular infiltration or compression of the vein by a pseudocyst or enlarged pancreatic parenchyma.
Case A 47-years-old male, chronic alcoholic presented with complaints of pain abdomen – 15 days and abdominal distension- 10 days. All baseline investigations were normal except serum amylase of 793 IU/mL. USG abdomen- pancreas –obscured by bowel shadows, gross ascites. Ascitic fluid analysis- low SAAG, high protein with amylase of 7141. CECT and MRCP abdomen S/O-acute pancreatitis with pseudocyst. V.OGD – pangastritis. A diagnosis of acute pancreatitis with pancreatic ascites was made and patient was planned for ERCP and PD stenting. On day 5 of admission patient complained of pain and swelling in right lower limb and Doppler was suggestive of DVT of popliteal vein. Patient was started on Inj. UFH. Next day patient developed shortness of breath. ECG – sinus tachycardia with T inversion. CT chest with pulmonary angiography suggestive of pulmonary thromboembolism. Patient was thrombolysed and was started on anticoagulants. Patient underwent ERCP and PD stenting. Patient responded to treatment and is on follow-up.
Conclusion Pulmonary thromboembolism in acute pancreatitis is a rare but life-threatening complication. Various risk factors have been implicated for the prothrombotic state in acute pancreatitis. Familiarity with this complication will help in its early diagnosis. Treatment with intravenous heparin followed by warfarin is effective.
Keywords Pancreatitis, Pulmonary thromboembolism, Ascites
399
Clinical implication of post-endoscopic retrograde cholangiopancreatography (post-ERCP) hyperamylasemia and its predictive role in post-ERCP pancreatitis
Vinoth Sermadurai, Kannan Mariappan, Ramani Ratinavel, Vijai Shankar Chidambaramanivasagam, P B Sriram
Correspondence – Vinoth S – vinothsermadurai@gmail.com
Department of Gastroenterology, Madurai Medical College, Panagal Road, Alwarpuram, Madurai 625 020, India
Aim Our aim is to identify the prevalence of post-endoscopic retrograde cholangiopancreatography (post-ERCP) hyperamylasemia and its role in predicting post-ERCP pancreatitis (PEP).
Methods Our study includes 34 patients who underwent ERCP procedure in Madurai Medical College during the study period from 1st February 2021 to 30th September 2021. All patients had normal preoperative serum amylase in our study. Patient who had preoperative pancreatitis, abnormal renal function tests were excluded. After obtaining written informed consent, serum amylase concentrations were measured 3 hrs and 48 hrs after the procedure.
Results In our study, post-ERCP pancreatitis occurred in 5.9% patients, 3 h hyperamylasemia in 26.5% patients. Elevated serum amylase levels at 48 hrs equal to or greater than 123 mg/dL was considered as a predictor factor for post-ERCP pancreatitis (p<0.05) with sensitivity of 97.3% and specificity of 90%. There was significant decrease in amylase levels after 48 hrs in non-PEP group comparing to PEP group. Bivariate logistic regression showed that pancreatic duct cannulation had increased risk of developing PEP and early hyperamylasemia. We had no significant association of individual risk factors with PEP and amylase level.
Conclusion Serum amylase levels at 48 h has more predictive role in post-ERCP pancreatitis than 3 h serum amylase levels. Pancreatic duct cannulation has increased risk of early hyperamylasemia and PEP. Fall in amylase value from 3 hrs to 48 hrs exclude the chance of development of post-ERCP pancreatitis. We should always suspect PEP if patient related, procedure related risk factors are present even though early serum amylase is normal. Post- ERCP, early normal serum amylase level doesn’t rule out PEP. Further studies are needed to know the significant association between additive risk factors and PEP.
Keywords Endoscopic retrograde cholangiopancreatography, Post-ERCP pancreatitis, Serum amylase
400
Role of neutrophil-lymphocyte ratio as a prognostic factor in patients with pancreatic ductal adenocarcinoma
Rajesh Chandra , Harshvardhan Rao, Sandeep V Nair, Sharon Paul Methala, Priya Nair, Anoop K Koshy, G Rajesh, Shine Sadasivan, Rama P Venu
Correspondence – Rajesh Chandra – rajeshchandra88@gmail.com
Department of Medical Gastroenterology, Amrita Institute of Medical Sciences, Peeliyadu Road, Ponekkara, Edappally, Ernakulam, Kochi 682 041, India
Pancreatic ductal adenocarcinoma (PDAC) continues to have a dismal prognosis despite treatment. Systemic inflammation (SI) has been linked to various cancers and several inflammatory mediators have been shown to be elevated in patients with PDAC. Neutrophil-lymphocyte ratio (NLR) is an easily available and inexpensive marker of SI. In our study we looked into the role of NLR as a prognostic marker in patients with PDAC.
Methods Prospective observational cohort study was conducted over a period of 3 years, where all consecutive patients with histologic evidence of PDAC were included. All relevant data was recorded in a pre-designed proforma. Patients were followed up for a minimum period of 1 year. Primary outcome was overall survival. Stratified analysis was performed with respect to stage (metastatic vs non-metastatic) and treatment modality offered (curative resection, palliative chemotherapy, palliative 335atient drainage).
Results A total of 161 patients with PDAC were included (mean age 62±11.91, M: F=1:4). NLR (at cut-off 2.78) was found to have a significant association with overall survival. Moreover, on multivariate analysis, NLR (at cut-off 2.78) was found to have an independent association with overall survival (HR -2.943, 95% CI 1.23 – 7.035, p value 0.015). In stratified analysis, NLR was a significant prognostic factor among both metastatic and non-metastatic disease (p value 0.011 and 0.036 respectively). In addition, NLR also showed a significant association with overall survival in patients who were managed with palliative chemotherapy (p value 0.004).
Conclusion Elevated NLR was found to be a significant, independent predictor of overall survival in our study. NLR as a prognostic factor was especially useful in patients treated with palliative chemotherapy.
Keywords Prognostic factors, Overall survival, Metastatic and non-metastatic disease
401
Clinical profile of patients with pancreaticopleural fistula from a tertiary care center
V Pradeep Kumar, M Kannan, R Ramani, C Vijai Shankar, Sriram
Correspondence – Pradeep Kumar V – drpradeepkumardoc@gmail.com
Department of Medical Gastroenterology, Madurai Medical College, Panagal Road, Alwarpuram, Madurai 625 020, India
Objectives To study the clinical profile of patients with pancreaticopleural fistua complicating acute pancreatitis (AP).
Methods All patients with acute pancreatitis diagnosed to have pancreaticopleural fistula on magnetic resonance cholangiopancreatography (MRCP) from a period of 6 months from April 2021 to September 2021 are considered for the study. Data regarding demographics, risk factors, presenting symptoms, biochemical tests, imaging and outcome were collected and analyzed.
Results Male sex, alcohol abuse, severe AP and infected necrosis are risk factors for development of internal fistulae. Smoking was the additional risk factor in our study. Because of non-GI presentations, a high degree of clinical suspicion is often required to diagnose PPF. As with the other studies, dyspnea was the most common presenting symptom in 50% of patients. Most common site of duct disruption is in the body of pancreas. When the duct disruption is in the distal body, patient had bilateral effusion and when in tail, patient had left pleural effusion. A delay in diagnosis of PFs can lead to increase in length of stay, intensive care unit stay, and even in mortality. Development of fistula in acute pancreatitis is likely to extend the hospital stay, mean stay was 33.6 days in our study. Octreotide is less likely to help with internal fistula except pancreaticopleural fistula where success rates of reducing fistula output and time to fistula closure. 3 patients responded to conservative treatment, one patient improved after pancreatic duct sphincterotomy, one patient underwent laparoscopic cystogastrostomy and another patient responded to pancreatic duct stenting.
Keywords Pancreaticopleural fisula, Acute pancreatitis, Chronic pancreatitis
402
Endotherapy of pancreatic duct disruption – Our experience
Dinesh Kumar Dugganapalli, L Sahitya, V Gopal Krishna, M Ramanna, M Uma Devi, B Ramesh Kumar
Correspondence – Dinesh Kumar Dugganapalli – mabhdisu143@gmail.com
Department of Medical Gastroenterology, Osmania Medical College, 5-1-876, Turrebaz Khan Road, Troop Bazaar, Koti, Hyderabad 500 095, India
Introduction Pancreatic duct disruption is a major complication in acute and chronic pancreatitis, rarely due to trauma, results in severe symptoms, morbidity and mortality. Endotherapy in the form of pancreatic duct stenting, sphincterotomy are the main modalities in treating patients to avoid surgery.
Aim To evaluate efficacy of pancreatic endotherapy as primary management in pancreatic duct disruption.
Methods Twenty-five cases of pancreatic duct disruptions admitted in Osmania Hospital were studied prospectively from January2019 to August2021 and followed periodically.
Results Among 25 cases, 22 males, 3 females, 12 patients are in 31-40 age group. Eighteen patients had chronic alcoholic pancreatitis, 4 had acute pancreatitis with WON, 2 due to blunt abdominal trauma, one 12 years old had MTCD. After clinical and lab assessment. All are kept on NJ feeds, antibiotics. ERCP attempted with mean duration 7-10 days. Majority of leaks noticed in genu 9 (36%), body 6 (24%), head 3 (12%) and multiple leaks in one (WON), 4 associated with portal hypertension, pancreatic duct stones in 3, pseudocyst in 3, pancreatic pleural fistula in 6 patients. Pancreatic sphincterotomy done in all patients (100%) and pancreatic duct stenting done in 20 patients (80%). In five no stenting done. One with multiple leaks and 3 with tail leaks were subjected to surgery. One responded to sphincterotomy. Twenty patients were followed periodically with symptoms improvement and USG scan. Mean duration of healing was 18 days (12 to 26 days). Eighteen patients responded after first session of endotherapy, 2 patients needed second session after 2 months for residual collection. Ninety percent patients with head and body, genu collections healed after pancreatic duct stenting, only 50% (3/6) patients with tail collections responded to endotherapy. No major complications and mortality were encountered.
Conclusion Pancreatic endotherapy in the form of sphincterotomy and stenting is effective and associated with less morbidity and early recovery.
Keywords Pancreatic duct disruption, Endotherapy, Sphincterotomy
403
Clinical features and management of pancreatic fluid collections: A case series
Raghuveer Balabhadra, Praveen Mathew, Prashant Kanni, Chandrababu Devarapu, Manoj Gowda, H N Nithin Kumar, Sidharth Bhumireddy, Amogh Chandrasekhar
Correspondence – Praveen Mathew – drpraveenmathew@yahoo.com
Department of Medical Gastroenterology, Vydehi Institute of Medical Sciences and Research, 80, EPIP Area, Whitefield, Bengaluru 560 066, India
Introduction Pancreatic fluid collections are seen as a sequala of pancreatitis and range from pseudocyst to walled off pancreatic necrosis. We present the pertinent clinical features as well as the management of the pancreatic fluid collections in our tertiary care centre.
Aims To evaluate and study the clinical profile of cases of pancreatic fluid collections in our tertiary care centre. It was obtained by performing an audit of all patients presenting with pain abdomen in Vydehi Institute of Medical Sciences and Research Centre from 2012-2021.
Method Data were collected from 1 September 2012 to 10 September 2021. All relevant investigations including CECT abdomen, EUS was done. Management of cases was done as per guidelines.
Observations A total of 85 cases were enrolled in the study. Mean age of patients was 40.38 years (74 Male, 11 Female). The mean size of the fluid collection was 6.7 X 5.7 cm. Majority patients presented with abdominal pain. Fluid collections could be well detected on both contrast-enhanced computed tomography and EUS. 58 patients had pseudocysts; 17 patients had walled off pancreatic necrosis. Significant debris was seen in 17 patients. Majority of the fluid collections were in the head (48), followed by body (28), and the tail (9). Thirty-one patients were managed conservatively. Thirteen patients underwent FNAC. Thirty-nine patients were endoscopically managed (EUS guided 28 (27 cystogastrostomy and 1 cysto duodenostomy, 11 patients underwent ERCP). Twenty-seven patients were treated with transmural drainage, 11 patients were treated with trans papillary drainage alone, while combined percutaneous and trans papillary drainage was performed in 1 patient. The pancreatic fluid collections resolved in all patients within 6-16 weeks. There were no complications and no patient had recurrence of fluid collections over a follow-up period.
Keywords Pseudocyst, Cystogastrostomy, Endoscopic ultrasound
404
A case of acute pancreatitis in beta thalassemia major
Rahul Vijayvargiya, L Sahitya, Gopala Krishna, M Ramanna, M Uma Devi, B Ramesh
Correspondence – Rahul Vijayvargiya - rahul.sanwariya1990@gmail.com
Department of Gastroenterology, Osmania Medical College, Afzal Gunj, Hyderbad 500 012, India
Introduction Thalassemia major presents early between 6 and 24 months and characterized by feature of severe anemia. To maintain effective hemoglobin level of 9 to 10 mg/dL for growth, patient undergoes regular blood transfusion program leading to iron overload state.
Case Report A 19-year-old male, who is known case of beta thalassemia major since 2005 underwent splenectomy in 2012 and received more than 300 unit blood transfusion. Laboratory investigation showed iron profile- serum ferritin- 2126 ng/mL, serum iron – 46 ug/dL, TIBC- 121 ug/dL. CECT abdomen suggestive of – acute cecrotizing pancreatitis with per pancreatic fluid CT severity index is 8/10 (Figs. 1 and 2).
Discussion Classical thalassemia is reported to be associated with acute pancreatitis; however, the etiology is biliary as gallstones are typical in these patients. But here we report this case of acute pancreatitis in beta thalassemia which is not because of gallstones. In this patient, etiology of acute pancreatitis may be because of iron overload as iron profile study in our patient show iron overload state. So, in patients with beta thalassemia major having iron overload state, we should keep in mind acute pancreatitis as differential diagnosis.
Keywords Beta thalassemia, Pancreatitis, Iron overload
405
Follow-up of patients with asymptomatic walled off necrosis: A prospective observational study
Manish Kumar , Siddharth Srivastava, Ujjwal Sonika, Sanjeev Sachdeva
Correspondence – Siddharth Srivastava – docsiddharth1@mail.com
Department of Gastroenterology, G B Pant Hospital, 1, J L N Marg, New Delhi 110 002, India
Introduction Studies on follow-up of patients with asymptomatic walled off necrosis (WON) arscarce. This is the first prospective study for patients with asymptomatic WON. This study aims to identify infection on follow-up in these patients and its predictors.
Methods: Thirty patients with acute pancreatitis with WON from November 2018 to April 2020 were enrolled. All patients were followed and patient developing complications were analyzed based on their baseline clinical, laboratory and radiological parameters to find any predictor for development of complications. Unpaired t-test or Mann-Whitney ‘U’ test was used for quantitative data and Chi-square or Fisher’s exact was used for qualitative data. “P” value <0.05 was considered statistically significant.
Results Thirty patients were enrolled for the study, 83.3% were males. Alcohol was the most common etiological factor. 26.6 % patients developed infection after 72.48±16.3 days from onset of pancreatitis. Mean age of patients was 36.38±11.45 years in infection group and 28.45±7.55 years in asymptomatic group, p=0.03. Patients with infection were managed by drainage, percutaneously (50%), endoscopically (37.5%), both combined (12.5%). Size of largest collection in infection and asymptomatic group was 157.50±33.59 mm and 81.95±26.22 mm respectively, p<0.001. CTSI in the infection and asymptomatic group was 9.50±0.93 and 7.82±1.37 respectively, p<0.01. CRP in infection group was 76 (56.2-91) mg/L and in asymptomatic group, 9.5 (3-16.6), p<0.001. Other parameters that were significantly different between the two groups were BISAP score, IL-6, TNF-alpha levels, and pancreatic necrosis. WON size cut-off of 117 mm has a sensitivity of 100% and specificity of 91% with AUROC 0.977 for predicting infection.
Conclusion Parameters like age, BISAP score, CRP, IL-6, TNF-alpha levels, WON size and CTSI can be used to predict infection in asymptomatic WON patients.
Keywords Predictors, Infection, Asymptomatic, Walled off necrosis
406
Complications of retained non-retrievable or forgotten pancreatic duct stents: A case series
Gaurav Mahajan, Pankaj Kapoor, Surinder Rana, Rajesh Gupta1
Correspondence – Gaurav Mahajan – gaurav.mahajan10@gmail.com
Department of Gastroenterology, and 1Surgical Gastroenterology, Postgraduate Institute of Medical Education and Research, Chandigarh 160 012, India
Introduction Pancreatic duct (PD) stents are routinely placed for various indications and are usually kept in situ for a short duration. They are subsequently removed as they can result in recurrent pancreatitis, infection, perforation, and stenosis of PD. There is paucity of data on the consequences of prolonged indwelling PD plastic stents. This study was done to retrospectively evaluate the consequences of prolonged indwelling PD plastic stents.
Methods Retrospective analysis of database of 16 patients ([13 Male, median age 32 years [range 23–42]) who underwent PD stenting from 2003 to 2021 was done to identify patients who had retained non-retrievable or forgotten PD stents. The indications, duration and complications of these indwelling PD stents were retrieved from this database.
Results The indications for PD stenting were external pancreatic fistula (EPF) post percutaneous drainage of acute necrotic collection in 9 (56.2%), painful chronic calcific pancreatitis (CCP) in 6 (37.5%) and PEP prophylaxis in 1 (6.3%) patient. Eleven (68.7%) patients had 5 Fr stents while 5 (31.3%) had 7 Fr stents with pancreatic sphincterotomy being done in 6 (37.5%) patients. The median duration of retained PD stents was 78 (range 48–128) months. Thirteen (81%) patients remained asymptomatic during this period. Of these 13 patients, 8 had EPF and upstream migrated stents could not be retrieved endoscopically. In 5 patients with CCP, the stent had either fragmented (n=2) or migrated inwards (n=3) and could not be removed endoscopically. Three (18.75%) patients (post EPF, PEP and CCP respectively) developed abdominal pain 36-58 months after stent insertion. Of these 3, stent was removed surgically in two patients and endoscopically in one patient.
Conclusion Retained PD stents can result in complications in patients with normal PD and preserved pancreatic parenchyma. However, in advanced chronic pancreatitis and in patients with atrophied pancreatic parenchyma, retained PD stents may not result in symptoms or complications.
Keywords Retained pancreatic duct stents, Prolonged indwelling PD stents, Pancreatic duct
407
Hypertriglyceridemia and alcohol – Acute pancreatits with dual etiologies – A case series
Pukhraj Jeji, Manoj Kumar Sahu, Girish Kumar Pati, Jimmy Narayan, Debakanta Mishra, Vybhav Venkatesh, Subhasis Pradhan, K Pruthvi, Anirudh Karanam, Vasista Palnati
Correspondence – Pukhraj Jeji – pukhrajsingh93@gmail.com
Department of Gastroenterology, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India
Introduction Acute pancreatitis (AP) is a serious gastrointestinal disorder with a wide array of etiologies. The diagnosis of AP requires 2 of the following 3 features: (1) abdominal pain characteristic of AP, (2) serum amylase and/or lipase ?3 times the upper limit of normal, and (3) characteristic findings of AP on imaging. Alcohol is the etiological factor in 25% cases of acute pancreatitis, while hypertriglyceridemia is the third most common cause of acute pancreatitis but is relatively rare and occurs when TG levels are >1000 mg/dL. Although alcohol intake can lead to secondary hypertriglyceridemia, however which of these is the contributing etiology is difficult to ascertain.
Cases We experienced 3 cases in our center who came with complaints of recent onset pain abdomen. All patients were male aged 32-48 years. One patient aged 48 years had history of familial hypertriglyceridemia and was on treatment for the last 2 years but had no regular follow-up and came with complaints of pain abdomen after binge alcohol intake with elevated triglycerides found on evaluation. 2nd case is a known case of hypertriglyceridemia, on regular follow-up, with history of alcohol related pancreatitis in 2015. He quit alcohol after index episode but present with recent onset pain abdomen and investigations showed highly elevated triglyceride levels. Another case presented with pain abdomen after binge alcohol intake and was found to have high TG levels on evaluation. All 3 cases had mild pancreatitis and were managed with adequate intravenous fluids and insulin infusions along with other supportive treatment. All 3 patients were discharged and are on strict follow-up. These 3 cases demonstrate the need for thorough evaluation for etiology and workup of patients with acute pancreatitis in spite of obvious etiological causes based on history for better patient care.
Keywords Acute pancreatitis, Triglyceride, Alcohol
408
Knowledge, attitude, and the practices in prevention of post endoscopic retrograde cholangiopancreatography pancreatitis among advanced endoscopists
Chintan Tailor , B Kiran, Vikramaditya Rawat, Mit Shah, Mayur Gattani, Shamshersingh Chauhan, Swapnil Walke, Deepti Vishwanathan, Vipul Chaudhari, Rahul Jadhav, Kailash Kolhe, Meghraj Ingle, Vikas Pandey
Correspondence – Vikas Pandey – drvikas_pandey@rediffmail.com
Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai 400 022, India
Background and Aims Post endoscopic retrograde cholangiopancreatography pancreatitis (PEP) is the most dreaded complication of endoscopic retrograde cholangiopancreatography (ERCP). We sought to capture the various practise methods amongst advanced endoscopists regarding measures taken for prevention of PEP.
Methods An anonymous online 31-item survey was sent to advanced endoscopists by digital medium like WhatsApp, Twitter, and E-mail. The responses were collected over a period of 2 weeks.
Results Of the 600 endoscopists who were invited to participate, 123 responded. Thirty seven percent use intravenous hydration only in patients deemed as high risk for PEP. Majority (91.8%) use Ringer’s lactate solution for the prevention of PEP. Standard hydration was the norm in using IV fluids in prevention of PEP amongst most endoscopists (67.5%). Forty percentage endoscopists put pancreatic ductal (PD) stent after more than 2 inadvertent PD cannulation. About 11 % endoscopists felt that there was no therapeutic benefit of PD stenting after inadvertent cannulation. About ninety-seven percentage endoscopists use rectal nonsteroidal anti-inflammatory drugs (NSAIDs) if there are no contraindication to use. Sixty-nine percentage endoscopists use rectal NSAIDs in high-risk patients only. About sixty percentage endoscopists use rectal NSAIDs after ERCP. Diclofenac 100 mg was the most commonly used rectal NSAID. Eighty-nine percentage of endoscopists use combined therapy for PEP. The most commonly used combination is rectal NSAID with standard hydration. If pancreatic ductal stenting is done due to inadvertent cannulation, 72 % endoscopists would still use intravenous hydration with rectal NSAID as additional mode of prophylaxis. Eighty-seven percentage endoscopists believe, 1% to 5 % patients develop PEP even after using appropriate prophylactic measures.
Conclusions As per our survey, rectal NSAIDs was the most common method and standard hydration was the least common method used to prevent PEP amongst practising endoscopists.
Keywords Post ERCP pancreatitis, Rectal NSAIDS, Pancreatic duct stenting, Hydration therapy
409
Acute pancreatitis with corona virus disease 2019 in COVID designated tertiary care hospital
D Sivaramakrishna , Tarun Beeram, Gurunath Dhyandev Bhange, Saikrishna Katepally, P Shravan Kumar
Correspondence – Sivaramakrishna D – sivaram.amc@gmail.com
Department of Medical gastroenterology, Gandhi Medical College, Musheerabad, Secunderabad 500 003, India
Introduction Severe acute respiratory syndrome coronavirus 2 (SARS-CO-2) is responsible for the ongoing pandemic of corona virus disease 2019 (COVID-19) and has caused >120,000 deaths. Although it is primarily a respiratory virus, SARS-COV2 also has extrapulmonary manifestations. Involvement of the pancreas is one of them.
More than 1000 patients undergone treatment for COVID-19 during period of 2020 – 21 in Gandhi Hospital, Secunderabad, India. We present a series of 11 COVID 19 +ve cases presented with acute pancreatitis admitted during this period. Out of 11 cases, 7 cases were admitted with pain abdomen as presenting complaint with covid 19 symptoms (fever, cough, and breathlessness) and diagnosed as acute pancreatitis. Other 4 cases developed pain abdomen after 4 to 6 days of admission. other causes of pain abdomen were ruled out in all these patients. Other possible causes of acute pancreatitis (alcohol, gallstone, drug-induced, hypercalcemia, hypertriglyceridemia) were ruled out by history and appropriate laboratory investigations. Six of 11 patients had mild symptoms and minimal abnormal laboratory parameters related to respiratory system and pancreas, also recovered within one week. Three patients had severe respiratory involvement requiring mechanical ventilation. One of these patients had acute pancreatic necrotic collection and sepsis required higher antibiotic support. The other two patients had moderately severe acute pancreatitis with mild respiratory involvement and recovered with conservative management.
Mechanism supporting COVID-19 causing pancreatitis is ACE2 mediated direct injury of the pancreas as exocrine glands and islet cells of pancreas express ACE2. Other possible mechanisms are systemic inflammatory response, circulatory proinflammatory cytokines, virus induced lipotoxicity, and microvascular injury.
Conclusion Pancreas is one of the extrapulmonary organs to involve in COVID-19 infection. It is important to consider COVID-19 infection in patients with acute pancreatitis when there is no other cause found.
Keywords COVID-19, Acute pancreatitis, COVID Designated Hospital
410
Pancreatic squamous cell carcinoma presenting as acute pancreatitis- A case report
Gautham Morupoju, Ch Saidulu, G Sagar, K Abhishek, V Lohit, N Sunil Kumar, B Sukanya
Correspondence – Gautham Morupoju – m.gautham36@gmail.com
Department of Medical Gastroenterology, Nizam’s Institute of Medical Sciences, Punjagutta, Hyderabad 500 082, India
Introduction Squamous cell carcinoma (SCC) of the pancreas is a rare condition representing 0.5% to 5% of all pancreatic exocrine neoplasms. Its clinical presentation is similar to that of pancreatic adenocarcinoma with the majority of patients presenting with abdominal pain (78%), weight loss (57%) and jaundice (28%). To our knowledge, this is the first reported case of a pancreatic SCC presenting as acute pancreatitis (AP).
Case Outline A 45-year-old lady with a history of Type 2 diabetes mellitus detected 3 months prior, presented with mild AP. Initial etiological workup for AP was inconclusive. She presented with persistent pain abdomen a month later, when a contrast enhanced computed tomography (CECT) abdomen done showed a mass lesion in the pancreaticoduodenal groove. CA19-9 level was within normal limits. Endoscopic ultrasound (EUS) confirmed a 4 x 4 cm hypoechoiec lesion in the uncinate process. EUS guided fine needle aspiration (FNA) of the pancreatic mass was performed. Histopathological examination of the pancreatic specimen revealed SCC. An extensive metastatic workup did not reveal an extrapancreatic origin for this SCC. Hence, a diagnosis of primary SCC of the pancreas was established.
Discussion This is a newly reported mode of presentation of a rare pancreatic exocrine neoplasm.
Keywords Pancreas, Squamous cell carcinoma, Acute pancreatitis
411
Acute necrotizing pancreatitis secondary to ascaris infestation– A case report
Matta Rakesh, Avinash Balekuduru, Lokesh Locheruvapalli
Correspondence – Matta Rakesh – rakeshkumar.matta@gmail.com
Department of Gastroenterology, M S Ramaiah Memorial Hospital, B E L M S Ramaiah Nagar, RIT Post, M S Ramaiah Nagar, Mathikere, Bengaluru 560 054, India
Introduction Ascaris lumbricoides is one of the most common parasitic infestations of human gastrointestinal tract. Intestinal ascariasis is mostly asymptomatic, on rare occasions the round worm may invade the biliary tract and main pancreatic duct causing obstruction and leading to acute pancreatitis and ascending cholangitis. Here we presenting a case report of ascariasis induced acute necrotizing pancreatitis.
Case Report A 53-year-old female patient known case of type 2 DM/IHD, no addictions presented to emergency department with pancreatic type of abdominal pain for 2 days and multiple episodes of vomitings, with no h/o similar complaints in the past. The patient was hemodynamically stable, on per abdomen examination- epigastric tenderness was noted and bowel sounds were normal. Patient was treated with IV fluids/IV analgesics. On routine investigations: normal HB /total count was noted; normal liver enzymes, serum triglycerides and serum calcium with elevated serum amylase (2700 IU/L), serum lipase( 3000 IU/L) levels were noted. CECT abdomen and pelvis revealed acute necrotizing pancreatitis (CTSI-6), with no evidence of gallstones. UGI endoscopy revealed round worm in duodenum invading in to ampulla. stool testing for parasites and ova were negative.
Conclusion Ascaris lumbricoides is an uncommon cause of biliary obstruction leading to complications such as cholangitis, biliary colic, acute pancreatitis. Although biliary complications are rare, these can cause severe morbidity and mortality. Therefore, early diagnosis and management are essential. Endoscopic removal of the worm is the treatment of choice, in addition to anti-helminthic medication, and supportive management.
Keywords Acute pancreatitis, Biliary ascariasis
412
A study of pregnancy outcomes in early onset idiopathic chronic pancreatitis
Gauri Kumbhar 1 , Sudipta Dhar Chowdhury 1 , Ajith Thomas 1 , Rajeeb Jaleel 1 , Santosh Benjamin 2
Correspondence – Gauri Kumbhar – gaurik92@gmail.com
Departments of 1G. I. Sciences, and 2Obstetrics and Gynaecology, Christian Medical College, Vellore 632 002, India
Introduction Early onset idiopathic chronic pancreatitis (EOICP) is a disease which affects young individuals in the prime of their lives. The present study was done with an aim to assess the pregnancy outcomes in patients with EOICP and the effect of pregnancy on the course of EOICP.
Methods Patients with EOICP who had disease onset prior to their pregnancy were recruited. All patients were interviewed using structured questionnaire. Baseline data as regards demographic variables, duration of disease, pregnancy outcomes, mode of delivery and course of illness was noted.
Results Twenty-seven patients had been diagnosed with EOICP, before pregnancy. Mean age of onset of symptoms was 19.18 (SD 6.16) years and the mean age of diagnosis was 24.47 (SD 6.19) years. Mean age at the time of childbirth was 24.2 (SD 4.73) years. Twenty-two (81%) patients had pancreatic calcifications, 21 (78%) had pancreatic exocrine insufficiency and one patient (4%) had diabetes mellitus. There were total 40 pregnancies. Early foetal loss was recorded in 6 (15%). Thirty-one pregnancies were carried to term and 3 were preterm deliveries. Caesarean section was performed in 19 (56%). Mean foetal birth weight was 2.84 kgs. One baby required NICU admission and there was one neonatal death. Pancreatic pain during pregnancy was reported in 12 (30%) pregnancies. No patients had any complication related to chronic pancreatitis.
Conclusions The rates of early fetal loss in patients with EOICP is similar to that of healthy individuals (15-20%). The present study shows that mothers affected with EOICP have pregnancy outcomes similar to healthy women. The incidence of LSCS appeared to be higher in the present study and this needs to be explored further in subsequent long-term studies.
Keywords Early onset idiopathic chronic pancreatitis, Pregnancy outcomes
413
A rare case of paraduodenal pancreatitis presenting as gastric outlet obstruction
Khwaja Aminoddin Siddiqui, Ameet Kumar Mandot
Correspondence – Khwaja Aminoddin Siddiqui – siddiqui.amin@yahoo.com
Correspondence – Khwaja Aminoddin Siddiqui – siddiqui.amin@yahoo.com
Department of Gastroenterology, Bombay Hospital and Institute of Medical Sciences, 12 New Marine Lines, Mumbai 400 020, India
Introduction Paraduodenal pancreatitis, also called as groove pancreatitis, is a rare entity seen in patients with recurrent pancreatitis or chronic pancreatitis. It presents with repeated vomiting, abdominal distension and pain. Gastric outlet obstruction at presentation is rare.
Methods A 50-year-old male patient presented with recurrent episodes of post-prandial non-bilious vomiting and abdominal distension since six months. The recurrent symptoms of gastric outlet obstruction led to significant weight loss of over 10-12 kilograms and malnutrition. He had history of significant alcohol consumption for 10-15 years. For the above complaints, he was admitted thrice in a span of six months. Aspiration of gastric content via nasogastric tube provided symptomatic relief. CT abdomen revealed severe mural thickening D2 causing complete luminal compromise and inhomogenous attenuation and post contrast enhancement in the groove between D2 and pancreatic head with focal hypoenhancing cystic areas. Upper gastrointestinal endoscopy revealed obstruction at junction of first and second part of duodenum (D2), and scope was not negotiable across the stricture. Endoscopic ultrasound (EUS) showed features of chronic pancreatitis and duodenal wall edema with cystic spaces and paraduodenal fat stranding s/o groove pancreatitis. EUS guided aspiration cytology was negative for malignancy.
Results After conservative measures failed and patient refused EUS guided gastrojejunal bypass stenting, patient underwent laparoscopic gastrojejunostomy. Post procedure patient was relieved of symptoms of gastric outlet obstruction. His oral intake improved, and patient started gaining weight.
Conclusion Paraduodenal pancreatitis is a relatively rare and difficult condition to diagnose. Less radical surgeries like gastrojejunal bypass without pancreaticoduodenectomy can offer good symptomatic relief if malignancy is ruled out.
Keywords Groove pancreatitis, Gastrojejunal bypass, Duodenal obstruction
414
IgG4 related gastrointestinal disorders– Experiences from a tertiary care center in India
Aadish Jain, Sridhar Sundaram, Unique Tyagi, Kiran Mane, Prachi Patil, Shaesta Mehta
Correspondence – Sridhar Sundaram – drsridharsundaram@gmail.com
Department of Digestive Diseases and Clinical Nutrition, Tata Memorial Hospital, Homi Bhabha National Institute (HBNI), Dr. E Borges Road, Parel, Mumbai 400 012, India
Background IgG4-related disease (IgGRD) describes a group of fibro inflammatory diseases that affecting various organs resulting in tumor-like effect and organ dysfunction. Majority of the literature is from Japan with no strong evidence to suggest a predilection for Asian populations. Data from India remains sparse.
Methods Retrospective review of outpatient and inpatient database between January 2013 and July 2021 was done to identify patients having IgG4-related disease. Demographic details, details of site of disease, symptoms, mode of diagnosis and overall final management plan were noted.
Results Forty-eight patients were diagnosed with IgG4-related diseases, of which 28 patients were found to have IgG4-related gastrointestinal (GI) disorders (mean age 56 ± 13 years, M:F-6:1). Among these, 19 (68%) had autoimmune pancreatitis, 4 (14%) had IgG4-related GB mass, 3 (11%) had IgG4-related retroperitoneal mass, 2 (7%) had IgG4-related liver mass. The most common mode of presentation was abdominal pain in 21 (75 %), followed by jaundice in 14 (50 %). One patient had extra-abdominal involvement (IgG4-related retropharyngeal mass).18 (65%) patients were diagnosed using endoscopic ultrasound or CT-guided sampling, while 10 (35%) patients on the surgically resected specimen. Lymphoplasmacytic infiltrate with an increase in IgG4 cells and increased IgG4:IgG ratio was seen in all patients.IgG4 level is raised in 19 (68 %) patients (Median IgG4 240 mg/dL). Eighteen (64 %) patients were treated with steroids. Among these patients, 13 (72 %) showed complete response. Among partially responded patients, one underwent surgery and two responded to treatment after adding azathioprine. Among the patients who responded to steroids, 3 (23 %) patients with autoimmune pancreatitis had relapsed on follow-up, who then responded to retrial with steroid and azathioprine maintenance therapy.
Conclusion IgG4-related diseases are commonly misdiagnosed as malignancies. Appropriate medical management with steroids and immunomodulators is associated with optimal response in these patients.
Keywords IgG4 related GI disorder, IgG4 related disease, Autoimmune pancreatitis
415
Incidence of pancreatic exocrine insufficiency following episode of acute pancreatitis – A prospective observational study
Ahmad Yousuf, J C Vij, Neha Berrry, Ajay Kumar, Manaw Wadhawan, Amrish Sahney
Correspondence – Ahmad Yousuf – wajeedyousuf@gmail.com
Department of Gastroenterology and Hepatology, B L K Max Super Speciality Hospital, New Delhi, India
Introduction AP patients may develop local, systemic complications including endocrine and exocrine insufficiency. This may persist beyond hospital admission. This study explores incidence of PEI following episode of AP and at 6 months follow-up.
Methods Between December 2019 to June 2021, among 130 AP patients presenting to BLK Max Hospital, 90 were included in the study as per inclusion criteria. These were classified into mild, moderately severe or severe pancreatitis as per revised Atlanta classification. Fecal elastase, fecal sudan stain was performed at the time of discharge (in mild pancreatitis) or after restarting feeding (moderately severe or severe pancreatitis) and at follow-up time of 6 months. PEI was diagnosed if fecal elastase was <200 ug/g or a positive sudan stain.
Results Ninety patients of AP were screened (mild 53, moderately severe 25, severe 12). Forty-eight (18 mild, 17 moderately severe, 12 severe) developed PEI at admission. These were followed for 6 months. Seven patients expired and 2 were lost to follow. Thirty-nine patients were included in final analysis. None among 18 patients with mild pancreatitis had PEI at follow-up. Four (23.5%) out of 17 patients with moderately severe pancreatitis persisted with PEI. Among 12 severe pancreatitis with PEI, 4 patients with PEI at the index admission persisted with PEI at follow-up. Severity of pancreatitis correlated with PEI at follow-up (p<0.001). Seven patients with necrotizing pancreatitis persisted with PEI on follow as compared to only one without necrosis (p< 0.001). Five patients with PEI had necrosis of more than 50% vs. 2 patients with 30% to 50% vs none with <30% of necrosis (p<0.001). Seven patients of ANC with local complications persisted with PEI as compared to 1 patient without any local complications (p<0.001).
Conclusion PEI corelated with severity of pancreatitis, degree of necrosis and local complications.
Keywords Acute pancreatitis, Pancreatic enzyme insufficiency, Acute necrotic
416
Role of endoscopic ultrasound in management of autoimmune pancreatitis
Nikhil Sonthalia, Vikram Uttam Patil, Awanish Tewari, Mahesh Kumar Goenka
Correspondence – Mahesh Kumar Goenka -mkgkolkata@gmail.com
Department of Gastroenterology, Apollo Multispecialty Hospital, 58, Canal Circular Road, Kolkata 700 054, India
Introduction Endoscopic ultrasound (EUS) is a well-established modality for diagnosing pancreatic masses. Autoimmune pancreatitis (AIP) often masquerades as a pancreatic cancer as clinical features and imaging findings are similar in between two. Accurate differentiation amongst them may help definitive cure, prevent surgery and morbidity as well as mortality. Here we describe a challenging case series of patients presenting with obstructive jaundice and pancreatic mass diagnosed as AIP with the help of EUS.
Methods We describe case series of 3 patients presenting with pancreatic mass and obstructive jaundice for evaluation. All the patients had serum IgG4 levels tested and underwent baseline EUS with fine needle biopsy (FNB). HISORt criteria was used to diagnose the cases as AIP.
Results In clinical features jaundice and weight loss were seen in all, however pain was absent in one case. There was no lump palpable. All had elevated serum IgG4 levels. Every case underwent endoscopic retrograde cholangiopancreatography for significant jaundice. All of them were treated with tapering dose of steroids with good response. Common EUS features of autoimmune pancreatitis includes increase gland volume, echopoor mass formation, echogenic interlobular septa, narrowing with thickening of main pancreatic duct (Fig. 1), whereas hyperechoic areas and focal enlargement is seen in pancreas cancer. Follow-up EUS was done in one which showed significant reduction in bulkiness of the pancreas, disappearance of mass formation in the head region with persistent hypoechoic coarse echotexture and hyperechoic septa (Fig. 2).
Conclusion Our series highlights significant role of EUS in diagnosing and management of challenging pancreatic masses. High degree of suspicion with accurate selection of site for FNB is crucial for making diagnosis and avoiding surgery.
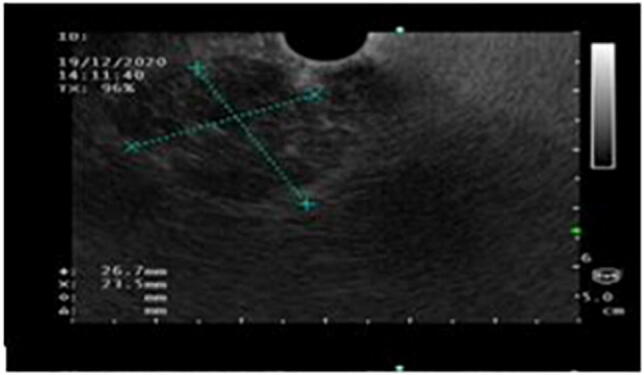
Keywords Autoimmune pancreatitis, Endoscopic ultrasound
417
Prevalence and risk factors of post-endoscopic retrograde cholangiopancreatography pancreatitis – A cross-sectional study
Thasneem Taj, Arul Selvan, Ravi Shankar, Senthil Kumar, Senthil Vadivu
Correspondence – Thasneem E – thasneemtaje@gmail.com
Department of Medical Gastroenterology, Government Medical College, Avinashi Road, Peelamedu, Civil Aerodrome Post, Coimbatore 641 018, India
Introduction Endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP) remains one of the most serious complications after ERCP with the reported incidence ranging from 1.3% to 15.1% in most prospective series. Multiple factors can lead to the development of unpredictable PEP. Awareness of the risk factors for PEP is essential for the recognition of high-risk cases in which ERCP should be avoided if possible, or in which protective endoscopic or pharmacologic interventions should be considered. This study aimed to to study the prevalence of post-ERCP pancreatitis in our centre and to identify risk factors for it.
Methods Fifty-six patients who underwent ERCP at our centre between January 2020 to August 2021 were included in this cross-sectional study. A total of 25 risk factors for PEP, either patient, procedure or operator related risk factors, were identified, and evaluated on the basis of earlier multivariate analyses from prospective studies. Prevalence of PEP was analyzed and risk factors were assessed by univariate and multivariate analysis using SPSS software .
Results ERCP was done for 56 patients – 48 patients (85.7%) with benign obstructive jaundice including 38 patients (67.8%) for choledocholithiasis, 8 patients (14.2%) for benign biliary stricture, 4 patients (7.1%) for postoperative biliary leakage and 6 patients with malignant obstructive jaundice. Post-ERCP pancreatitis occurred in 7 patients (7.1%). All cases were mild and was managed conservatively without any significant mortalilty and morbidity. On univariate and multivariate analysis, female gender and pancreatic duct cannulation were found to be statistically significant risk factors.
Conclusion Female gender and pancreatic duct cannulation are significant risk factors for post ERCP pancreatitis.
Keywords Endoscopic retrograde cholangiopancreatography, Post-ERCP pancreatitis, Pancreatic duct cannulation
418
Acute pancreatitis masquerading an acute attack of acute intermittent porphyria: A rare manifestation
Pritam Das, Samir Mohindra
Correspondence – Samir Mohindra – mohindrasamir@yahoo.com
Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014, India
Acute intermittent porphyria is an autosomal dominant porphyria characterized by a partial deficiency of porphobilinogen deaminase, also known as hydroxymethylbilane synthase (HMBS), an enzyme involved in heme biosynthesis.
Twenty-four years male, known case of acute intermittent porphyria, with known family history of porphyria present in family (grandmother, father and sister), presented with chief complaints of pain abdomen since 1 day, DOO 24/06/2021, severe, non-colicky, diffuse, continuous, non-radiating, not relieved with analgesics. Urine porphyrinogen was positive and managed in line of acute episode of AIP with DNS at 100 mL/hour and 25% D. The patient developed breathlessness with drop in spO2 on 26/06/2021. The patient again developed pain abdomen, severe, VAS 9, non-radiating on 12/07/2021, CT abdomen was done, suggestive of acute necrotizing pancreatitis, CTSI 10/10 with lesser sac collection extending to left anterior pararenal space. The patient was managed on step up approach, predominantly percutaneous. The complications were managed with percutaneous drain placement with subsequent upsizing and repositioning. ERCP was done on 18/08/2021, on dye injection, MPD 2-3 mm in diameter, free leak seen from papilla in the region of the pigtail. No upstream ductal stricture identified, since duct is narrow and adequate EPT done, no stent placed. The patient was further planned for check ERP at time of removal of transgatric catheter, glue obliteration if leak still persists.
There are two school of thoughts, first one being toxin induced, accumulation of upstream products like delta-aminolevulinic acid (ALA) and porphobilinogen (PBG), which may be amplified by certain medications, alcohol, infections, low caloric intake, or hormonal imbalances during menstrual cycle and pregnancy, the other one being autonomic neuropathy associated with AIP with spastic obstruction of the sphincter of Oddi.
Keywords Acute intermittent porphyria, Acute pancreatitis, Sphincter of Oddi, Toxin
419
Predictors of need of surgery in patients with acute necrotic collections treated with percutaneous drainage
J Sachin1, Mandeep Kang1, Ujjwal Gorsi1, Arihant Jain2, Deba Prasad Dhibar2, Archana Angrup3, Rajesh Gupta4, Surinder Rana1
Correspondence – Sachin J – sachin.h.j.69@gmail.com
Departments of 1Gastroenterology, 2Internal Medicine, 3Microbiology, and 4Surgical Gastroenterology, Post Graduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 022, India
Background Patients with acute necrotic collections (ANC) maybe managed conservatively or with percutaneous drainage (PCD)/surgery. Surgery entails high mortality rate and PCD has high failure rate. Early and timely intervention is important and predictors of failure of percutaneous therapy can help in management.
Methods Patients admitted with AP between July 2019 and July 2021 who developed acute necrotic collections were prospectively enrolled and we studied the predictors of failure of PCD.
Results Among 21 patients with ANCs studied, 9 (42.6%) were successfully managed with PCD alone. Twelve (57.14%) patients did not improve despite PCD and either underwent necrosectomy or succumbed to the illness. Percentage of males was higher (83.3% vs. 33.33% p=0.03) and mean day of placement of PCD was later (20.5 vs. 15.1 p=0.023) in the PCD failure group. SIRS at admission (2.92 vs. 2.33 p=0.102) and at 48 hours (3.5 vs. 2.89 p=0.12) and APACHEII score (7.8 vs. 7.0 p=0.508) were higher in the PCD failure group. Mean ferritin (2916.9 vs. 1033.4 ng/mL p= 0.394) and qCRP levels (249.5 vs. 209.6 ng/mL p=0.508) were higher in the PCD failure group and mean corrected calcium (9.0 vs. 8.3 gm/dL p=0.069) levels were lower in the PCD failure group. Maximum size of PCD drainage catheter was larger in the PCD success group (16.2 F vs. 14.7F p=0.277).
Conclusion Male gender, delayed PCD drainage, higher SIRS, APACHE II score, CRP and ferritin levels and lower calcium levels are predictors of need of surgery following PCD in patients with ANC.
Keywords Pancreas, Acute pancreatitis, Acute necrotic collection, Predictive factors, Percutaneous drainage
420
Role of Interleukin-6 and CRP in predicting systemic complications in patients with acute pancreatitis
Krishna Chaitanya Reddy Ramireddy
Correspondence – Krishna Chaitanya Reddy Ramireddy – rchaitanya13@yahoo.com
Department of Medical Gastroenterology, Government Medical College Hospital, Subbaiahpuram, Thoothukudi 628 002, India
Introduction In acute pancreatitis (AP), early assessment of severity is an important measure for effective management. The aim of our study is to determine the prognostic value of interleukin (IL) 6, C-reactive protein (CRP) as predictors of systemic complications in AP.
Methods A 100 patients with confirmed AP were enrolled in the study. The severity of AP was defined based on Atlanta criteria. Interleukin-6 was measured on the first day of admission. CRP level was assessed on admission day and after 48 hours. ROC analysis was performed for these parameters.
Results Interleukin-6 significantly differentiated patients with systemic complications from those without. Elevation of IL-6 showed the highest significance as a predictor (p=0.002). CRP levels did not differ between mild and severe cases on admission, but had statistical significance when measured on the third day (p= 0.001)
Conclusion This study confirmed that IL-6 measured on admission, and CRP measured on third day of admission serve as valuable prognostic factors of severity and systemic complications of AP.
Keywords Acute pancreatitis, Severity, Interleukin-6, CRP, Systemic complications
421
Acute pancreatitis as an index presentation of multiple myeloma
Vaibhav Karoliya, Dawesh Yadav, Vinod Kumar Dixit, Anurag Tiwari, Vinod Kumar, S K Shukla
Correspondence – Vaibhav Karoliya – vaibhavkaroliya@gmail.com
Department of Gastroenterology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221 005, India
Introduction Hypercalcemia is one of the less common cause of pancreatitis. Multiple myeloma, a plasma cell malignancy can cause pancreatitis by causing hypercalcemia.
We report a case of an elderly female with multiple myeloma with pancreatitis as an index presentation.
Case We present the case of a 62-year-old female who presented to the hospital with a eight-day history of nausea, vomiting, and epigastric pain. In the emergency department, patient was found to have Hb – 4.3 gm/dL, calcium 10.4 mg/dL, albumin 2.4 gm/dL, total protein 9.2 gm/dL, creatinine 7.2 mg/dL (no baseline creatinine was available), lipase 5000 U/L, and normal liver enzymes. 24-hour urinary protein was 1200 mg/day and USG KUB was s/o bilateral increased renal echogenicity and partial loss of CMD. In light of these investigations, possibility of multiple myeloma was kept. Subsequent testing of SPEP was abnormal with a monoclonal IgA kappa spike identified. Beta 2 microglobulin was 3107 ng/mL. X-ray skull displayed lytic lesions consistent with multiple myeloma. Bone marrow biopsy confirmed the diagnosis with 46% plasma cells. Patient was managed with 2 sessions of hemodialysis and other conservative treatment. In view of no history of alcohol/tobacco use, no gallstones, normal triglyceride level, no trauma, no viral illness, and no medications pancreatitis was attributed to multiple myeloma.
Conclusion Multiple myeloma is associated with pancreatitis in the setting of hypercalcemia. Multiple myeloma should be strongly suspected as an etiology in patients of pancreatitis with hypercalcemia in presence of anaemia and A-G reversal.
Keywords Multiple myeloma, Hypercalcemia, Pancreatitis
422
Pancreatic tuberculosis: Great mimicker of pancreatic malignancy
Malla V A Gangadhar Rao , Samir Mohindra, Gaurav Pande, S Rakesh Kumar, Dhruv Thakur, Preetam Das
Correspondence – Samir Mohindra - mohindrasamir@yahoo.com
Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Raibareli Road, Lucknow 226 014, India
Pancreatic tuberculosis is a rare condition with clinical and radiological features similar to pancreatic malignancy, hence a diagnostic challenge. Here we report two cases of young adults with pancreatic tuberculosis. One patient presented with pancreatic head mass, loss of weight, loss of appetite and gastric outlet obstruction. CT abdomen showed pancreatic head mass with dilated MPD, CBD and IHBR. Lesion is abutting D2, Main portal vein and encasement of Superior mesenteric vein along with multiple peripancreatic, periportal, para-aortic, aortocaval lymph nodes and multiple liver SOLs. EUS guided FNAC from lymph node was taken which was positive for Gene Xpert. Second patient, a known case of chronic kidney disease presented with pancreatic head mass and extra hepatic biliary obstruction. CT abdomen showed pancreatic head mass with dilated MPD, CBD and IHBR with surrounding celiac and peripancreatic lymph nodes. EUS guided FNAC from head mass was suggestive of granulomatous pathology with positive Gene Xpert. ERC and stenting done for biliary drainage. Both patients were started on Anti tubercular treatment and symptoms improved significantly. Despite its rarity, pancreatic tuberculosis should be considered in differential diagnosis of pancreatic mass lesions especially in endemic countries. Clinical suspicion and accurate diagnostic approach are needed for diagnosis of this potentially curable disease and to prevent unnecessary laparotomy.
Keywords Pancreas, Tuberculosis, Malignancy, Gene Xpert
423
Study of variations in demographics, management and clinical outcomes in patients of acute pancreatitis in a tertiary care hospital center in south India
Ganesh Koppad, H V Acharya, H P Nandeesh, Deepak Suvarna, T R Vijaykumar, M R Hitesh, K K Sharath Chandra
Correspondence – Maj Aradya H V - aryandr@rediffmail.com
Department of Medical Gastroenterology, J S S Medical College, Bangalore - Mysore Road, Bannimantap A Layout, Bannimantap, Mysuru 570 015, India
Introduction Acute pancreatitis is a global leading cause of gastrointestinal (GI)-related hospital admissions. Over the last decade multiple advances have occurred in management of acute pancreatitis such as development of revised Atlanta classification of disease severity, introduction on early goal directed IV fluid resuscitation and implementation of step-up approach in subjects with necrotizing pancreatitis/collections. Large multicenter studies in acute pancreatitis from national registries have been published, results from these have revealed heterogeneity in patient characteristics such as demographics, etiology and risk factors for severe disease, This study aims to evaluate demographic differences, management and outcomes across all patients admitted at JSS Hospital, Mysore.
Methods We collected data retrospectively of patients admitted at J S S Hospital, Mysore from January 2020 to September 2021 (21 months) with a diagnosis of acute pancreatitis and information with respect to etiology, severity, management –IV fluid therapy, pain management, interventions, complications, radiological findings and clinical outcomes and patient satisfaction – patient were called up telephonically. Our final analysis includes 130 patients who were admitted in various Departments of the hospital (Gen Medicine/Gen surgery/Med Gastroenterology, etc.) and inter-departmental management strategies were compared.
Results Ethanol was the most common cause of acute pancreatitis, Rest of the statistical data is still under analysis.
Conclusion This study aims to compare the differences of patient demographics, etiology, management approaches and clinical outcomes of patients with acute pancreatitis.
Keywords Acute pancreatitis, Demographics, Management, Outcomes
424
A single centre observational study of clinical profile of patients with chronic pancreatitis with special reference to pancreatic endocrine insufficiency and pancreatic exocrine insufficiency
Milindkumar Prajapati , P P Bose
Correspondence – Milindkumar Prajapati – milindprajapati102@gmail.com
Department of Gastroenterology, Peerless Hospital, Panchasayar, Kolkata 700 094, India
Aims and Objectives To study manifestation of pancreatic exocrine and endocrine insufficiency of chronic pancreatitis presenting to tertiary care centre and to identify patients having underlying FCPD.
Introduction Chronic pancreatitis is a disease involving inflammation, fibrosis, and loss of acinar and islet cells, which can manifest in unrelenting pancreatic-type abdominal pain, malnutrition, derangements in pancreatic function and visible pancreatic damage on imaging studies. Exocrine pancreatic insufficiency is defined as the presence of clinical steatorrhea and its improvement by pancreatic enzyme supplementation or fecal pancreatic elastase level <200 μg/g of stool. Pancreatic endocrine insufficiency diagnosed by fasting plasma glucose ≥126 mg%, postprandial plasma glucose ≥200 mg%, and/ or HbA1c ≥6.5%. FCPD is a subtype of tropical chronic pancreatitis comprising calcifying, non-alcoholic chronic pancreatitis affecting younger generally malnourished individuals from the tropical regions of Asia, Africa and South America particularly males.
Methodology A single centre prospective observational clinical study conducted at Department of Gastroenterology, Peerless Hospital, Kolkata for one year.
Result and Discussion Mean age of study-population was 39.82 years. It consisted of 11 (31.4%) females and 24 (68.6%) males. Nineteen patients were <=40 years age. Most-common cause was idiopathic followed by alcoholism in 10 (28.6%) and smoking in 8 (22.9%). Most common presenting compliant was abdominal pain in 31 (88.6%). Eighteen (51.4%) of them were diabetic. Three (8.6%) patients had steatorrhea. Fifteen patients had fecal elastase test done, all (100%) were suggestive of PEI and 13 (86.7%) had severe PEI with FE levels. Nine of 25 non-alcoholic patients had PEI as suggested by low FE levels. However genetic studies of these patients could have been more advantageous for the study.
Keywords Chronic pancreatitis, Fecal elastase, Pancreatic exocrine insufficiency
425
A unusual case of acute pancreatitis: A case report and review of literature
Hitesh Ramesh
Correspondence – Hitesh Ramesh – hi5474@gmail.com
Department of Medical Gastroenterology, J S S Medical College, Bangalore - Mysore Road, Bannimantap A Layout, Bannimantap, Mysuru 570 015, India
Introduction A wide variety of causes of acute pancreatitis have been reported; however, it is always difficult to be certain about the cause in a given patient. However, an attempt must be made in every patient to ascertain a cause by a thorough history, physical examination, laboratory tests, and imaging before labelling it as “idiopathic acute pancreatitis”. We present a patient diagnosed to have acute pancreatitis secondary to hypercalcemia. Further work up for hypercalcemia revealed hyperparathyroidism.
Methods A 47-year-old lady, teetotaller, with no previous co-morbidities was admitted with complains of pain abdomen and vomiting since 1 week. Investigations revealed serum amylase-1200 u/L and lipase-980 u/L. Fasting lipid profile was normal. Serum calcium was 15.0 mg/dL, serum albumin was 4.1 g/dL. Serum PTH was 150 pg/mL (normal range : 18.5-88 pg/mL). CECT abdomen showed diffuse peri-pancreatic fat stranding, fluid in peri-pancreatic, bilateral anterior para-renal and splenic hilar region, features suggestive of acute pancreatitis (CT Severity Index -4/10).Ultrasound neck showed heterogeneously hypoechoic lesion in relation to lower pole of left lobe of thyroid suggestive of parathyroid adenoma. Radionuclide parathyroid scan (99 mtc-sestamibi) showed hyper-functioning solitary parathyroid adenoma in pre/para tracheal region below the lower pole of the left lobe of thyroid gland. patient underwent left inferior parathyroidectomy. Postoperative period was uneventful. parathyroid biopsy revealed features suggestive of parathyroid adenoma.
Results Post left inferior parathyroidectomy, serum calcium was 9.2 mg/dL, serum PTH was 42 pg/mL (normal range : 18.5-88 pg/mL).
Conclusion Hypercalcemia must be considered in all patients presenting with acute pancreatitis.
Keywords Acute pancreatitis, Hypercalcemia, Parathroid adenoma resection
426
Diagnostic performance of fecal Elastase-1 in detection of steatorrhea in chronic pancreatitis: Real world experience
Srikanth Gopi , Jatin Yegurla, Mohammad Tabish, Samagra Agarwal, Sumaira Qamar, Namrata Singh, Deepak Gunjan, Anoop Saraya
Correspondence – Anoop Saraya – ansaraya@yahoo.com
Department of Gastroenterology and Human Nutrition Unit, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Pancreatic exocrine insufficiency (PEI) is an important complication of chronic pancreatitis (CP). Seventy-two-hour or 24-hour fecal fat estimation is considered a gold standard to estimate steatorrhea (fecal fat excretion >7g/day) but it is cumbersome and inconvenient. So, fecal elastase-1 (FE) <200 g/μg stool is proposed to be good alternative but data on its performance in Indian patients is limited.
Methods This retrospective study included adult patients (≥18 years) diagnosed with chronic pancreatitis whose both 24-hour fecal fat estimation and FE estimation were done within a time frame of 6 months were included in the study. The objective was to evaluate the diagnostic performance of FE compared to 24-hour fecal fat.
Results A total of 147 patients were included with mean age of 32.5±10.8 years and the etiologies of CP were idiopathic (76.2%) and alcohol (23.8%). The prevalence of steatorrhea was 34% (50/147) based on standard 24-hour fecal fat estimation >7g, while history of greasy/oily stools was present only in 8.2%. The sensitivity, specificity, positive and negative predictive value of FE was 90%, 28.9%, 39.5% and 84.8% at cut-off of <100 g/μg stool and 96%, 11.3%, 35.8% and 84.6% at cut-off of <200 g/μg stool, respectively. The optimal cut-off of FE for maximum area under ROC of 0.70 (0.61-0.80) was 20 g/μg stool and the sensitivity and specificity were 66% and 69% at FE <20 g/μg stool.
Conclusion FE ≥100 g/μg stool has good negative predictive value to rule out steatorrhea and FE <20 g/μg stool is the best possible cut-off to diagnose steatorrhea in Indian settings.
Keywords Chronic pancreatitis, Exocrine insufficiency, Fecal fat estimation, Fecal elastase
427
Bone disease in chronic pancreatitis
K R Nithin
Correspondence – Nithin K R – nith.kr@gmail.com
Department of Medical Gastroenterology, Kilpauk Medical College, Chennai 600 010, India
Introduction Bone disease (osteopenia or osteoporosis) is a highly prevalent condition in society and presents a tremendous, preventable public health burden. The association of bone disease has been recognized in several diseases of the gastrointestinal tract, resulting in established guidelines for screening in patients with malabsorptive disorders such as inflammatory bowel disease and celiac disease. Increasingly, the risk of bone disease has been recognized in patients with chronic pancreatitis (CP), who share similar risk factors as patients with other gastrointestinal disorders.
Methods This single-centre study was carried out in Department of Digestive Health and Diseases, Kilpauk Medical College. This study population consisted of 40 patients who were image confirmed cases of chronic pancreatitis.
• History of smoking, alcohol use was taken, BMI was measured.
Dual-energy x-ray absorptiometry scan was used to examine bone mineral density for the lumbar spine and bilateral femoral neck.
Results Of the 40 patients, 27 were male, and 13 were female.
• 12 patients were chronic smokers and 23 patients had history of significant alcohol use.
• The prevalence of osteoporosis (combined estimate for femoral neck and lumbar spine) in this patient group was 30 % (12) in patients with CP compared to Indian prevalence of 18.3% in previous studies.
• The prevalence of osteoporosis for the femoral neck was 18.5 % in CP, for the lumbar spine, the estimates were 16.9%.
The prevalence of osteopenia was 57.5% (23) in patients with CP compared to Indian prevalence of 49.9% in previous studies.
Conclusion Bone disease in CP can be attributed to several risk factors which act synergistically in propagating abnormal bone metabolism and increase the risk of fractures. Osteoporosis and osteopenia are underappreciated sources of morbidity in patients of CP. Bone health management guidelines are urgently required in patients with chronic pancreatitis.
Keywords Dexa scan, Chronic pancreatitis, Osteoporosis
428
A rare case report of pancreatic tuberculosis presenting as pancreatic abscess, leading to chronic pancreatitis with ductal stricture
Poorva Haridas, Amit Maydeo, Prabha Sawant, Ankit Dalal, Gaurav Patil
Correspondence – Poorva Haridas – prh2091@gmail.com
Department of Gastroenterology, Global Hospitals, Dr E Borges Road, Opp Shirodkar School, Parel, Mumbai 400 012, India
Tuberculosis of the pancreas is extremely rare, being reported in only about 0% to 4.7%. It is usually described in immunocompromised individuals. Here we describe a case of TB pancreas in a previously healthy, immunocompetent 46-year-old male, who presented to us in April 2020 with complaint of diffuse abdominal pain and weight loss. CECT showed 6.4 x 5.8 x 4.7 cm necrotic collection in mid body of pancreas with a dilated duct (4 mm) and necrotic intraabdominal lymphadenopathy. EUS showed a large bilobed collection of size 7.8 x 6.7 cm, communicating with the pancreatic duct. EUS guided FNAC was positive for TB (GeneXpert and culture). Consequently he was started on a 9 month course of AKT, to which he responded. A recent MRCP with MRI abdomen done in Oct 21 revealed complete resolution of the cystic lesion. However, atrophy of pancreatic parenchyma and pancreatic duct stricture involving body and tail was seen, with upstream dilatation of the duct (8.7 mm). No evidence of calcification was noted. The patient is asymptomatic currently with no evidence of endocrine/exocrine insufficiency. He has been prophylactically prescribed a course of pancreatic enzymes therapy. Other etiological work up of chronic pancreatitis was negative.
Conclusion Tuberculosis of the pancreas, being an uncommon entity, requires a high degree of suspicion for its early diagnosis, followed by prompt initiation of anti-Kochs therapy.
Keywords Pancreatic tuberculosis, Abscess, Ductal stricture, Chronic pancreatitis
Endoscopy
429
Endoscopic management of Bouveret syndrome: A case report
Aeshal Parmar , Monika Jain, Gurwant Singh Lamba
Correspondence – Aeshal Parmar – aeshal.6@gmail.com
Department of Gastroenterology, Sri Balaji Action Medical Institute, Paschim Vihar, New Delhi 110 063, India
Introduction Bouveret syndrome is characterized by gastric outlet obstruction caused by presence of ectopic gall stone in stomach or duodenum. It is a rare complication of gallstone disease.
Methods A 53-years-old male presented with recurrent vomiting and abdominal pain in the epigastric region for one week. On clinical examination, abdomen was soft and nontender. Routine investigations like complete blood count, liver function tests, renal function tests, serum amylase and serum lipase were within normal limits. A computed tomography (CT) scan abdomen was suggestive of cholecystoduodenal fistula with calcified lesion (35 X 27 mm) in antropyloric region of stomach. An upper gastrointestinal (GI) endoscopy was done which showed a large rounded stone in antropyloric region and a fistulous opening in duodenal bulb. Based on the above findings, a diagnosis of gallstone disease with Bouveret syndrome was made. A double channel upper GI endoscope was used to perform electrohydraulic lithotripsy (EHL) to fragment the stone. However, it was difficult to perform EHL due to mobile nature of the stone. So, the stone was grasped with polypectomy snare and EHL under water immersion was performed. The stone was fragmented into multiple pieces. The fragments were then removed with the Roth basket. Post procedure period was uneventful with post procedure hospital stay of 24 hours. On follow-up for six months, patient was asymptomatic.
Results Bouveret syndrome was successfully managed by endoscopic treatment with electrohydraulic lithotripsy and stone extraction without any periprocedural untoward effects.
Conclusion Surgical management of Bouveret syndrome carries high morbidity and mortality. Endoscopic treatment is minimally invasive, successful, and safe which significantly reduces duration of hospital stay, morbidity and mortality in these patients.
Keywords Bouveret syndrome, Gall stone, Endoscopic treatment
430
The role of endoscopic ultrasound in the evaluation of upper abdominal pain of unknown etiology
Dhruv Mishra, Yogesh Batra
Correspondence – Yogesh Batra – dryogeshbatra@gmail.com
Department of Gastroenterology, Indraprastha Apollo Hospital, Mathura Road, Jasola Vihar, New Delhi 110 076, India
Aim To assess the diagnostic efficacy and cost effectiveness of endoscopic ultrasound (EUS) in patients presenting with upper abdominal pain for >6 weeks with normal imaging and endoscopic findings.
Methods The study included patients with upper abdominal pain lasting greater than 6 weeks with no identifiable cause despite blood investigations (as previously specified), Upper gastrointestinal endoscopy, ultrasonography abdomen and either a computed tomography (CT) or magnetic resonance imaging (MRI) abdomen.
Results Thirty-eight patients were included (F- 21, M- 17). Eight of these patients had deranged liver function tests (LFTs) and two had raised amylase/lipase levels (<3x upper limit of normal [ULN]). Upon endoscopic ultrasound (radial/linear), Six patients (15.7%) had visible sludge in the gallbladder, four (10.5%) had sludge/stones in the common bile duct (CBD) and two had combined gallbladder (GB) and CBD sludge (5.2%). Abnormalities of the pancreatic duct or evidence of chronic pancreatitis was seen in five patients (13.1%) whereas irregular narrowing/stricture of the lower end of the CBD were noted in two patients (5.2%). Nineteen patients of 38 (50%) had a normal EUS study.
Fourteen of the 19 patients (73.6%) patients underwent a therapeutic procedure based on the EUS findings (endoscopic retrograde cholangiopancreatography [ERCP] and surgery) and pain relief was obtained in 12 of these patients.
Conclusion EUS is an investigative modality with diagnostic superiority in evaluating hepato-pancreato-biliary causes of pain. Routine use of EUS in these patients not only has significant diagnostic and therapeutic implications but can also prove to be a simple and cost effective measure in the recognition of hepato-pancreato-biliary disorders.
Keywords Endoscopic ultrasound, Obscure abdominal pain, EUS vs MRI
431
A unique case of mesh migration after laproscopic incisional hernia repair: A case report
Yash Gangadia, Gurvant Singh Lamba, Monika Jain, Yogesh Kumar Goyal
Correspondence – Yash Gangadia – yash_g2511@yahoo.com
Department of Gastroenterology, Sri Balaji Action Medical Institute, A3/ 281, Paschim Vihar, New Delhi 110 063, India
Introduction Mesh migration after laproscopic incisional hernia repair into a hollow viscus is a rare consequence. Completely intraluminal migration of mesh into bowel is very rare.
Methods A 53-year-old hypertensive morbidly obese, female was admitted with complaints of upper abdominal pain associated with nausea and vomiting since 1 month. She had history of open cholecystectomy for cholelithiasis. After 1 year of cholecystectomy, she presented with incisional hernia at local site, for which laproscopic repair was done with intraperitoneal on lay Goretex mesh.
Routine investigations for pain abdomen were within normal limits. Contrast-enhanced computed tomography (CECT) whole abdomen showed foreign body with metal tecklers in transverse colon. A colonoscopy was done which showed metal mesh with tecklers and prolene sutures, which had eroded into lumen. The standard treatment of such mesh migration is surgical. But we attempted to remove the mesh endoscopically by cutting the prolene sutures with argon plasma coagulation. The mesh was folded into a roll with the help of foreign body forceps using a double channel through endoscope. The mesh was removed through anal opening successfully. Post procedure period was uneventful and patient was discharged on next day.
Conclusion Endoscopic treatment for mesh migration into bowel is possible. It is a minimally invasive procedure which reduces morbidity, mortality and hospital stay for the patients as compared to surgery.
Keywords Migrated Mesh, Colonoscopy, Foreign body forceps
432
Diagnostic and therapeutic efficacy, safety and clinical utility of novel motorized power spiral enteroscopy – A single-centre experience from India
Pankaj Singh, Sawan Bopana, T K Surakshit, Muzaffer Rashid Shawl, Vikas Singla
Correspondence – Pankaj Singh – pankajdoc06@gmail.com
Department of Gastroenterology and Hepatology, Max Super Speciality Hospital, Saket, New Delhi 110 017, India
Introduction The small intestine has always been an area that has been difficult to access by endoscopist, being so long, convoluted and beyond the reach of normal endoscope. Motorized power spiral enteroscopy (PSE) is the latest minimally invasive technology that has created a paradigm shift in the small bowel diagnostic and therapeutic, with speed and ease adding to the attractiveness of the procedure.
Method Retrospective study of 20 consecutive patients with suspected small bowel disease over last 7 months. Patients were judiciously selected for PSE based on an objective evidence of small bowel disease on prior capsule endoscopy or small bowel radiologic studies. Patients were assessed in terms of diagnostic and therapeutic yield, technical success, total enteroscopy rate (TER), depth of maximal insertion (DMI), median insertion time and adverse events.
Results Twenty patients (mean age of 39 ± 15.59 years) underwent PSE in seven months. Technical success rate (TSR) was 95% (antegrade route) and 75% (retrograde route). Pan-enteroscopy rate (TER) was 30%, antegrade enteroscopy to the cecum was achieved in 33.33%. No enteroscopy associated major adverse effect seen, minor adverse effect seen in 50%. Median depth of maximal insertion was 450 cm (range 220-550) (antegrade route) and 150 cm (range 80-220) (retrograde route). Median insertion time to DMI was 70 min (range 45- 110) (antegrade route) and 45 min (range 20- 60) (retrograde route). Most common findings were ulcero-stricturing lesion (57.89%) followed by vascular lesion (15.78%). Most common histopathologic diagnosis was Crohn’s disease in 36.84%. Overall diagnostic and therapeutic yield were 75% and 57.89% respectively.
Conclusion PSE is a promising alternative technique for diagnostic and therapeutic enteroscopy that works on the same principle of spiral enteroscope with a specialized self-propulsive motor. It scores favorably over the existing deep enteroscopy devices in terms of procedural ease, duration, safety, and yields.
Keywords Power spiral enteroscopy, Small bowel
433
Effectiveness of an evidence-based protocol on reprocessing of endoscopes in terms of practice of reprocessing among healthcare professionals
Anjali Arora1, Mini George1, Vikram Bhatia2
Correspondence – Anjali Arora – anjaliarora.94@gmail.com
1College of Nursing, 2Professor, Institute of Liver and Biliary Sciences, New Delhi 110 070, India
Introduction In the Endoscopy Unit, endoscopes are reused countless times and are contaminated with native flora that warrants “Reprocessing” by the Healthcare Professionals (HCPs). Appropriate reprocessing provides quality care for patients undergoing gastrointestinal endoscopy.
Methods Using quantitative approach a one group pre-test and post-test designed study was conducted in Endoscopy Unit, ILBS during October – November 2020. The Fishbone Model was used to conceptualize the study. A pilot study was carried out in August 2020. After ethics clearance and informed consent of HCPs, the practice of reprocessing among HCPs and microbial surveillance of endoscopes were assessed before and after the implementation of Evidence Based Protocol (EBP). A validated (CVI=0.98) and reliable (TRT=0.852) Practice Checklist and Microbial Surveillance of Endoscopes was used. This EBP (adapted from SGNA Guidelines) was taught through demonstration method by the certified researcher. Data was analysed by descriptive and inferential statistics.
Results Majority of HCPs were male (71.42%) and 57.14% were nurses. Practice of reprocessing was at the ‘unacceptable’ level before EBP and 77.5% best practice after EBP. Microbial samples taken from the outer surface of the endoscopes showed ‘no growth’ from before to after EBP; while samples from suction channel (after HLD or high-level disinfection) showed reduction in pseudomonas alcaligenes from 20% to 0%, aeromonas salmonicidia from 12.5% to 5%, E. coli from 5% to 2.5%, pseudomonas aeruginosa from 5% to 0%, from before to after EBP.
Effect of EBP on practice of reprocessing was assessed by paired ‘t’ test (t=-23.86; p<0.00) and on microbial growth by ‘Fisher Exact’ test (F=11.07; p<0.003). Both were found statistically significant.
Conclusion This EBP was found effective in improving Practice of reprocessing of endoscopes and reduction in microbial growth and could go a long way in patient safety and reducing outbreaks.
Keywords Practice of endoscope reprocessing, Microbial surveillance in GI endoscopes, Endoscope
434
A rare presentation of iatrogenic perforation in a case of ileocecal tuberculosis
Susan George, Devika Madhu, T S Prasanth, D Krishnadas
Correspondence – Susan George – susanmathmoola@gmail.com
Department of Medical Gastroenterology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Colonoscopy is a relatively safe procedure with a few, rare complications like perforation and bleeding. Complications occur more with therapeutic than diagnostic colonoscopies. It is mandatory for endoscopist to be acquainted with atypical presentations of such complications as early identification reduces morbidity and mortality. Colonic perforation is a dreaded complication of colonoscopy. Perforations can be extraperitoneal, intraperitoneal or combined. Perforation may be consequence of mechanical trauma, barotrauma, or electrocautery injury and they can be extraperitoneal, intraperitoneal or combined. The greater part of perforations are intraperitoneal. Worldwide, till date, only 11 cases of isolated extraperitoneal perforation and 22 cases of concomitant perforation have been described. Out of these reported cases only in 3 cases cecum was described as the site of perforation. We intend to report a case of extraperitoneal colonic perforation in a young lady with ileocecal tuberculosis who had presented with colicky abdominal pain in right iliac fossa for 6 months associated with evening rise of temperature, fatigue, and significant weight loss. The patient was not on any regular medication, had no comorbidities and never underwent endoscopic procedures or surgery previously. She comes from a low socioeconomic status with family history of pulmonary tuberculosis. Colonoscopy revealed loss of vascularity, erythema, edema with deep ulcers noted extending from sigmoid to ileum, deformed Bauhin’s valve, ulcerated valve lip and pulled up cecum. Patient had mild epigastric pain at the time of cecal intubation, otherwise colonoscopy was uneventful. Due to minimal discomfort patient had, immediately after the procedure, abdominal X-ray was planned. Meanwhile patient developed shortness of breath and subcutaneous emphysema of the neck which was gradually progressive in nature. She underwent emergency right hemicolectomy and didn’t have intra operative findings of peritonitis. Patient was started on antituberculosis treatment post-surgery and is doing well.
Keywords Retroperitoneal cecal perforation, Ileocecal tuberculosis, Iatrogenic, Colonoscopy
435
Correlation of clinical and endoscopic profile of patients with upper gastrointestinal bleeding in a tertiary care hospital
Rajpreet Brar
Correspondence – Rajpreet Brar – rajpreetsingh811@gmail.com
Department of Gastroenterology, MMIMSR, E19 E Block, M M University, Mullana, Ambala 133 203, India
Background Bleeding from the upper gastrointestinal tract (GIT) is about 4 times more common than bleeding from the lower GIT and is associated with significant morbidity and mortality. Early, judicious use of endoscopy can be of benefit from the standpoint of diagnosis, therapy, and prognosis. The presentation of bleeding depends on the amount and location of hemorrhage. The aim of study was to study clinical profile, etiology and correlation between clinical and endoscopic diagnosis of patient with upper gastrointestinal bleed (UGIB).
Methods Eighty-six patients above the age of 18 years, irrespective of gender presented to our hospital with UGIB during the study period and were subjected to endoscopy to identify the etiology. The clinical and endoscopic profile was also analyzed.
Results Majority of the patients were between 21-40 years of age that is 47.6%. Most of them were males (82.5%) and male to female ratio was 4.7:1. The most common cause of UGIB was esophageal varices seen in 40.7% of patients, duodenal ulcer was seen in 20.9% patients, Superficial mucosal erosions in 16.2%, gastric ulcer in 9.3% patients, esophageal and gastric malignancy 6.9% and Mallory–Weiss tear was seen in 1%. The overall mortality rate was 13.9% and mortality because of UGIB was 5.8%.
Conclusion In our study variceal bleed was the most common cause of UGIB, followed by duodenal ulcer bleed. Endoscopy could pick up correct diagnosis in 96.5% cases of UGIB as compared to 75.6% cases via clinical diagnosis based on detailed history and examination.
Keywords Upper gastrointestinal bleed, Endoscopy, Varices
436
Epidemiology of adenomatous colorectal polyps in asymptomatic Indian population: A prospective cohort study
Shivaraj Afzalpurkar, Bhageerath Raj, Gajanan Rodge, Mahesh Goenka
Correspondence – Shivaraj Afzalpurkar – drshivaraj62@gmail.com
Department of Gastroenterology, Day Care Building, Fourth Floor, Institute of Gastrosciences and Liver, Apollo Gleneagles Hospital, EM Bypass Road, 58 Canal Circular Road, Kolkata700 054, India
Background Worldwide colorectal cancer is the third most common malignancy with an incidence of 10.2% and second highest cause of cancer mortality (9.2%) after lung cancer. There is scant data on the incidence and prevalence of colorectal polyps from Asian countries particularly Indian subcontinent.
Aim To estimate the incidence of adenomatous polyps in India and to study the correlation between epidemiological factors and adenoma detection rate during colonoscopy.
Methods Consecutive patients with gastrointestinal symptoms who underwent full colonoscopy in our institution between January 2019 to February 2021 were included. Patients with alarm symptoms (hematochezia, weight loss, abdominal or rectal mass), recent change (<3 months) in bowel habits, failed caecal intubation and poorly prepared bowel were excluded.
Results Polyps were seen in 168 of 1121 patients (14.99%) who underwent complete colonoscopies and mainly belonged to ≥ 50 years age group (71%, p<0.0001, OR 2.72) with a mean age of 55.8 years. Polyps were common in men compared to women (76.3% vs. 23.7%, p=0.011, OR 1.89). Adenomatous polyps or malignancy was detected in 93 (55.36%) patients while remaining 75 (44.62%) had hyperplastic polyps or inflammatory polyps. Adenoma incidence was higher in smokers when compared to non-smokers (71.4% vs. 28.6%, p<0.0001, OR 3.84), patients consuming non vegetarian diet (80% vs. 20%, p=0.004, OR 2.64) and in obese individuals (62.9% vs. 37.1%, OR 1.63). Distribution of adenoma or carcinoma in colon was 46 (30.06%) in right colon, 17 (11.11%) in transverse colon, 45 (29.41%) in left colon, 16 (10.46%) in sigmoid colon, 29 (18.95%) in rectum (Fig. 1).
Conclusion Incidence of colorectal polyps is significant in India though compared to western countries it is still lower. Smoking, red meat and high body mass index were predominant risk factors. Polyps were more commonly distributed in right and transverse colon.
Keywords Adenoma detection, Risk factors, Adenomatous polyps, Smoking, Red meat
437
Endoscopy in era of corona virus disease 2019 pandemic
Parveen Malhotra
Correspondence – Parveen Malhotra – drparveenmalhotra@yahoo.com
Department of Medical Gastroenterology, Post Graduate Institute of Medical Sciences, 128/19, Civil Hospital Road, Rohtak 124 001, India
Introduction Corona virus disease 2019 (COVID-19) caused by SARS-CoV-2 forced temporary postponement of elective endoscopic procedures but emergency procedures had to be done with the lowest possible risk of exposing patients, staff, and providers. It is widely accepted that COVID-19 is mainly spread via droplets and contact, but airborne spread is possible during aerosol-generating procedures (AGPs).
Review of Literature Endoscopy is a high-risk procedure as pulmonary and gastric secretions, as well as fecal material, may contain large viral loads. Infection prevention and control measures must be implemented to enhance patient safety, avoid nosocomial outbreaks, protect HCP, and ensure rational use of limited personal protective equipment (PPE). Multiple endoscopy societies and expert groups have offered recommendations and position statements for endoscopy during the COVID-19 pandemic. Patients should be screened with a pre-procedure COVID-19 questionnaire upon arrival to the endoscopy facility. Staff should be similarly screened prior to starting each workday. Physical distancing rules need to be adhered to by patients and staff, except during intervals of close contact required by providers to prepare the patient for a procedure. As an Endoscopist, the first mandatory thing was to clearly differentiate between the elective and emergency endoscopic procedures which were- upper or lower gastrointestinal bleed, foreign body ingestion, suspected malignancy and dysphagia. The patients requiring emergency endoscopy procedures were divided into three categories- confirmed COVID-19 cases, suspected COVID-19 cases and non Covid cases.
Result In Covid suspect or non-Covid patients, emergency endoscopic procedures were not denied on basis of pending Covid testing report and procedures were done using PPE kits in case of suspected Covid patient and in gown, hairnet, face shield, goggles, N-95 face mask, double gloves and gum shoes. In total 400 procedures were done following above guidelines in which 316 (79%) were endoscopy and 84 (21%) were colonoscopy.
Keywords Endoscopy, COVID-19 pandemic, PPE kits
438
Endoscopic glue injection versus endoscopic human thrombin injection for bleeding gastric varices – A randomized controlled trial
Gireesh Dhaked, Mayank Ametha, Ashok Jhajharia, Rupesh Pokharna
Correspondence – Gireesh Dhaked – dr.gireeshdhaked2210@gmail.com
Department of Gastroenterology, Sawai Man Singh Medical College, J L N Marg, Jaipur 302 004, India
Introduction Acute gastric variceal bleeding (AGVB) is a potentially fatal consequence of portal hypertension, accounting for 10% to 30% of all variceal bleeding. Although endoscopic cyanoacrylate glue injection is a common treatment for acute hemostasis, it has been linked to significant side effects. In the treatment of AGVB, there is limited evidence of the efficacy and relative safety of endoscopic human thrombin injection over glue injection.
Methods A total of 52 AGVB patients were randomised to receive either thrombin injection (25 patients) or glue injection (27 patients). The primary outcome was the incidence of any glue or thrombin injection-related post-therapy complications. Initial hemostasis, rebleeding, and mortality were all secondary end goals. The study was approved by the ethical committee of SMS Medical College, Jaipur and registered with CTRI at No. CTRI/2020/07/026466.
Results Both groups had comparable baseline data. Hemostasis of active bleeding at endoscopy was 100.0 % (10/10) in the thrombin group and 87.5 % (7/8) in the glue group (p=0.44). Treatment failure after 5 days occurred in two patients (6.1%) in the glue group compared to none in the thrombin group (p=0.165). Between 6 and 42 days after index bleeding, rebleeding occurred in 4 patients in the thrombin group compared to 12 patients in the glue group (p< 0.03). In the thrombin group, none of the patients had post treatment ulcers on gastric varices compared to 14.81% (4/27) that occurred in the glue group (p<0.045). Overall, complications occurred in 4 (20%) and 11 (40.7%) patients in the thrombin and glue groups, respectively (p=0.105). Two patients in glue group died.
Conclusion In order to achieve successful AGVB hemostasis, endoscopic thrombin injection was identical to glue injection. However, glue injection may be linked to a higher rate of rebleeding and post-therapy gastric varices ulcerations.
Keywords Acute gastric variceal bleeding (AGVB), Cyanoacrylate glue injection, Human thrombin injection
439
Comparative study of individual versus combination therapy of rectal diclofenac and intravenous ringer’s lactate in prevention of post endoscopic retrograde cholangiopancreatography pancreatitis in high-risk patients
Vivek Sharma, Amit Mathur
Corresponding – Vivek Sharma – vivekmohansharma@gmail.com
Department of Gastroenterology, National Institute of Medical Science and Research, NIMS University, Jaipur 303 121, India
Background and Aims Pancreatitis is the most common serious complication of endoscopic retrograde cholangiopancreatography (ERCP), with incidence ranging from 8.8% in average-risk to 14.1% in high-risk patients. Rectal diclofenac and aggressive hydration with intravenous Ringer’s lactate are proven therapies for prevention of post ERCP pancreatitis (PEP). We performed a randomized trial to establish whether combination of rectal Diclofenac and aggressive hydration with intravenous Ringer’s lactate is superior to individual therapy for prevention of PEP in high-risk group.
Methods Single centre randomized clinical trial. A total of 102 patients at high risk for PEP were randomly assigned (1:1:1) to 3 groups- Group A (rectal diclofenac), Group B (Ringer’s lactate), Group C (combination of rectal diclofenac and Ringer’s lactate). PEP was defined as more than three times increase in serum levels of pancreatic enzymes within 24 hours of the procedure accompanied with symptoms. Primary outcome was incidence of PEP. Secondary outcomes were severity of PEP, length of hospital stay and post ERCP amylase and lipase levels.
Results Seven patients in Group A, 9 patients in Group B and 7 patients in group C developed PEP. Majority of the patients had mild PEP. Length of hospital stay was up to 3 days in most of the patients. Majority of the patients who developed PEP were females, less than 60 years of age and with serum bilirubin levels <2 mg/dL. Benign conditions were more commonly associated with PEP than malignant cases.
Conclusion Combination prophylactic therapy with NSAIDs plus aggressive hydration does not seem to have additional clinically important benefits in preventing PEP.
Keywords Rectal diclofenac, Ringer’s lactate, PEP
440
Efficacy of intralesional triamcinolone injection for benign refractory esophageal strictures
Lavanya Narayanan, Kani Shaikh Mohamed, A R Akilandeswari, A Anand
Correspondence – Lavanya Narayanan – lavanya12@gmail.com
Department of Digestive Health and Diseases, Kilpauk Medical College, Government Peripheral Hospital, Anna Nagar, Chennai 600 102, India
Introduction Refractory esophageal strictures are defined as an anatomic restriction because of cicatricial luminal compromise that results in dysphagia. They may occur as the result of either an inability to successfully achieve a diameter of 14 mm over 5 SG dilatation sessions at 2-week intervals (refractory) or as a result of an inability to maintain a satisfactory luminal diameter for 4 weeks once the target diameter of 14 mm has been achieved (recurrent). Treatment is difficult but dilatation combined with intralesional triamcinolone injection has been shown to reduce need of recurrent dilatations.
Methods Ten patients with refractory esophageal stricture were selected for the study. All patients received triamcinolone (40 mg) injected via 23G-EST needle in a four quadrantic manner-0.5 mL each into the proximal end of the stricture and also into the stricture itself after dilatation. Patients were followed up for a period of 1 year. The intervals between dilations and frequency of dilations were calculated before and after injections. A periodic dilation index (defined as number of dilations required per month) before and after the triamcinolone injections was calculated.
Results Out of the 10 patients included in the study, 3 had a post corrosive stricture, 3 were post radiation, 2 anastomotic site stricture and 2 peptic stricture. The mean number of sessions of intralesional triamcinolone was 3 with corrosive strictures requiring more sittings (average 4) and peptic strictures requiring the least (average 2). The periodic dilation index showed a decrease in all 10 patients with a mean of 1.7 prior to procedure to 0.6 after injection. The interval period between dilatations also increased. There were no major complications like bleeding or perforation in our study.
Conclusions Intralesional triamcinolone injection combined with Savary-Gilliard dilatation is a safe and effective method for management of benign refractory esophageal strictures.
Keywords Triamcinolone, Refractory stricture
441
Endoscopic argon plasma coagulation in the management of gastrointestinal bleeding-Tertiary care experience
Paila Ramesh
Correspondence – Paila Ramesh – pailaramesh549@gmail.com
Department of Medical Gastroenterology, Madras Medical College, Poonamallee High Road, Park Town, Chennai 600 003, India
Introduction: Gastrointestinal bleeding is associated with substantial patient morbidity, necessitating frequent hospital admission and repeated blood transfusions. The endoscopic use of argon plasma coagulation to achieve hemostasis for gastrointestinal bleeding has not been adequately evaluated in controlled trials. This study aimed to evaluate the APC for treatment of various causes of gastrointestinal hemorrhage, initial hemostasis rate, rate of requirement of recurrent procedure.
Methods This was a retrospective study in which data is collected from patients undergoing APC for various causes of GI hemorrhage (excluding variceal bleeding) between October 2019 to September 2021 at Madras Medical College, Chennai.
Results Of the 88 patients studied 22 (25%) were males and 66 (75%) were females, mean age group for males 56.2 years, for females 51.35 years. Out of 88 patients 82 (93.18%) achieved initial hemostasis in first sitting, 6 (6.81%) patients required second time APC. Out of 88 patients studied 43 (48.86%) were radiation proctitis, 27 (30.68%) were GAVE,2 (2.27%) were tumor bleeding, 4 (4.54%) were portal hypertensive gastropathy, 3 (3.40%) were portal colopathy secondary to CKD, 6 (6.81%) were telangiectasia in rectum, 1 (1.13%) was Dieulafoy’s lesion, 1 (1.13%) was angiodysplasia stomach, 1 (1.13%) was telangiectasia in stomach
Discussion The argon plasma coagulation appears most efficacious in the treatment of vascular lesions such as radiation proctopathy and GAVE, other indiactions were angioectasia, angiodysplasia, tumor bleeding, portal hypertensive gastropathy, portal colopathy, Dieulafoy’s lesion.
Conclusion In this study most common indication for APC was radiation proctitis followed by GAVE. Overall endoscopic hemostasis using APC is an easy, safe, fast and effective method of controlling various types of gastrointestinal hemorrhage. APC can be powerful tool for endoscopic hemostasis and should be used more widely in future.
Keywords Endoscopy, APC, GAVE
442
ROSE in patients with pancreatic solid lesions (PSLs) undergoing endoscopic ultrasound guided biopsy- Single centre prospective parallel comparative study
Utkarsh Chhanchure, Sridhar Sundaram, Vishalkumar Seth, Prachi Patil, Shaesta Mehta
Correspondence – Sridhar Sundaram - drsridharsundaram@gmail.com
Department of Digestive Diseases and Clinical Nutrition, Tata Memorial Hospital, E. Borges Road, Parel, Mumbai 400 012, India
Introduction There have been significant advances in endoscopic ultrasound (EUS) guided tissue sampling, with better acquisition using biopsy needles. Whether Rapid On-site examination (ROSE) increases yield in patients who undergo biopsy has been a matter of debate. We aimed to compare yield of EUS guided biopsy with smear cytology with adequacy confirmed by ROSE, acquired using the same needle.
Methods Consecutive patients with solid pancreatic lesions (PSLs) referred for EUS-guided sampling were prospectively enrolled. Sampling was done using 22G AcquireTM needle in all cases using slow stylet pull-through method, with patient either under conscious sedation or general anaesthesia. During each sampling ROSE was done for adequacy before assessing for cytology. The endoscopist then collected sample for histopathology, adequacy of which was confirmed by MOSE. Number of passes (overall and for ROSE adequacy) were noted. Final cytology and histopathology reports were compared for diagnostic accuracy.
Results Seventy patients were enrolled in the study (mean age 57.2 + 13 years; 54% male, 84% lesions in head of pancreas). Median largest dimension of lesions was 3.7 cm (Range 1.5 to 5.9 cm). Final diagnosis was malignancy in 59 (adenocarcinoma-50, NET-7, SPEN-1, Lymphoma-1) with negative for malignancy in 11 (autoimmune pancreatitis-1, tuberculosis-2). Median number of passes required were 4 (3 passes in 25 [35.7%] patients; 4 passes in 27 [38.6%]). In 9 (13%) patients more than one pass was required for confirming adequacy on ROSE. Sensitivity and specificity for malignant PSLs for ROSE+cytology was 96.7% and 100% respectively. Final HPR could diagnose malignant PSLs with sensitivity and specificity of 95% and 100% respectively. Comparison using McNemar Chi-square for paired nominal data showed no significant difference between final HPR and ROSE+cytology taken with FNB needle.
Conclusion EUS FNB has high diagnostic accuracy in PSLs. ROSE may not increase diagnostic yield in solid pancreatic lesions sampled using EUS biopsy needle.
Keywords EUS sampling, ROSE, FNB, Pancreatic solid lesions
443
A cross-sectional study on profile of endoscopic findings in patients presenting with upper gastrointestinal bleed in tertiary care center in north-east India
C P Ganesh1, Suraj Kumar Nongthombam2
Correspondence – Ganesh C P - ganesh4joy@gmail.com
Departments of 1General Medicine, and 2Gastroenterology, Jawaharlal Nehru Institute of Medical Sciences, Porompat, Imphal, Manipur 795 004, India
A common presentation in the emergency departments worldwide is upper gastrointestinal bleeding causing a great number of admissions in hospitals which in third world countries causes a huge impact on the economy and becomes a big health issue. Upper gastrointestinal bleeding, which most commonly arises from mucosal erosive diseases, accounts for up to 20,000 deaths annually. Already a study regarding the prevalence of Helicobacter pylori infection in patients with acute peptic ulcer bleeding was conducted in JNIMS which showed the importance of actively looking for non-variceal causes for acute UGI bleed. The overall incidence of acute upper gastrointestinal hemorrhage has been estimated to be 50-100 per 1,00,000 person per year. Bleeding from the upper gastrointestinal tract is approximately five times more common than bleeding from the lower gastrointestinal tract. Bleeding may be massive or trivial, obvious, or hidden.
Keywords Upper gastrointestinal endoscopic finding in acute setting
444
Predictors of failure of endoscopic retrograde cholangiopancreatography in clearing bile duct stones during index procedure
K Abhishek , B Sukanya, V R Lohith Kumar, Chevigoni Saidulu
Correspondence – K Abhishek – abhisheksmrt6@gmail.com
Department of Medical Gastroenterology, Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad 500 082, India
Background/Aims A common indication for performing an endoscopic retrograde cholangiopancreatography (ERCP) is the removal of biliary stones. Although the majority of cases are amendable to clearance of the biliary system during a single session, there remains a portion where repeated procedures are required, due to factors pertaining to the anatomy of the biliary system or the stones themselves. This study aimed to identify factors predictive of failure of ERCP in clearing common bile duct (CBD) stones during index procedure.
Methods This is a prospective study from December 2020 to September 2021. A total of 120 patients with bile duct stones confirmed on imaging were included in this study. Patients who had prior attempts at bile duct clearance were excluded.
Results In our study, the factors that are associated with lower success of clearing CBD stones include- older age (>50 years, p=0.03), the presence of cholangitis (p=0.05), large stone size (>10 mm, p=0.001), larger number of filling defects (>3, p=0.002) and presence of a stricture distal to a stone (p=0.02). The use of an extraction balloon was associated with higher success of clearing the biliary system when compared to using extraction baskets (p<0.01). Other factors, including sex of the patient, shape of the stone, presence of periampullary diverticulum, CBD diameter and use of EPLBD did not significantly affect the chances of complete bile duct clearance.
Conclusion Identifying factors that might predict cases where biliary system clearance would be challenging will give the health-care provider an opportunity to allocate better resources during index procedure; provide prior information to patients about possible need for further intervention like lithotripsy or surgical exploration.
Keywords CBD stone, ERCP, Index procedure
445
Comparison of diagnostic yield with and without rapid on-site evaluation for endoscopic ultrasound and fine needle aspiration of gastrointestinal lesions
John George, Rajeeb Jaleel, Ajith Thomas, Lalji Patel, Anoop John, Amit Dutta, Ebby Simon, A J Joseph
Correspondence – John George – johntgeorg@gmail.com
Department of Gastroenterology, Christian Medical College, Vellore 632 004, India
Introduction The role of rapid on-site evaluation (ROSE) for endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) of the gastrointestinal system has long been debated. The European Society of Gastrointestinal Endoscopy recommends EUS-FNA with or without ROSE, as the current evidence available is not concordant. Limited availability of onsite cytopathologist is the main challenge with ROSE, which has been highlighted during the SARS-CoV-2 pandemic.
Methodology In this retrospective study we wish to compare the need for repeat biopsies, adequacy of smears, cellularity of smears and diagnostic yield in those undergoing EUS-FNA with and without ROSE. The results of patients who underwent EUS-FNA a year before the SARS-CoV-2 pandemic, when ROSE was available was compared with the results of patients who underwent EUS-FNA within a year after the SARS-CoV-2 pandemic, when ROSE was unavailable. Only patients with solid lesions were included. Repeat procedures were excluded.
Results ROSE was done in 116 of the 228 patients who underwent EUS – FNA. Pancreatic lesions accounted for more than 50% the lesions in both the groups. There was no difference in the diagnostic yield (66.4% vs. 67.2%; p=0.92), cellularity of smears, adequacy of smears (86.3% vs. 75%, p=0.06) and need for repeat samples (5.2% vs. 4.4%, p= 1.0). The number of passes made was significantly lesser in the ROSE group (3.1 vs. 3.6, p=0.002). In a subgroup analysis of lesions, smears from luminal lesions were significantly more adequate (100% vs. 53%, p=0.01) when ROSE was used. No other significant differences were noted on subgroup analysis.
Conclusion The utilisation of ROSE during EUS–FNA of the GI system does not affect the diagnostic yield, the adequacy or cellularity of smears and the need for repeat samples but reduces the number of passes needed for acquiring tissue samples.
Keywords ROSE, EUS-FNA, Diagnostic yield
446
The role of prophylactic octreotide in preventing endoscopic retrograde cholangiopancreatography induced pancreatitis
Achal Garg , Praveen Mathew
Correspondence – Achal Garg – drvibhutigarg17@gmail.com
Department of Medical Gastroenterology and Hepatology, Vydehi Institute of Medical Sciences, Kalyan Nagar, Bengaluru 560 043, India
Background and Aim Post ERCP pancreatitis (PEP) has been defined into 3 categories as mild moderate and severe according to revised ATLANTA Classification. Octreotide is a synthetic somatostatin analogue with a longer half-life. Similar to somatostatin, octreotide is a potent inhibitor of pancreatic enzyme secretion and effect on the contractility of sphincter of Oddi.
The European Society of Gastrointestinal Endoscopy (ESGE) 2020 guidelines recommends that future studies to evaluate the efficacy of octreotide in a dose greater than or equal to 0.5 mg.
Methods The present is a double blinded randomised control study which was carried out in the Department of Gastroenterology and a total of 75 patients were taken which were divided into 2 groups as control (n=35) and study group (n=40). Two mL of normal saline and octreotide were given according to respective groups subcutaneously 1 hour before procedure followed by 6 hour and 12 hours after ERCP and serum amylase and lipase were measured along with clinical features. The following protocol was followed based on previous studies.
Results: The overall mean age of the study population including study and control group was 52 years. Most common indications for ERCP was choledocholithiasis (50%) followed by malignant cause (30%), benign biliary stricture (10-15%). Clinical and ERCP related risk factors according to ESGE Guidelines were present in nearly 50% to 60%. Hyperamylasemia was present in study group in 19 patients (47.5%) and amongst control group in 16 patients (45.7%). Incidence of post ERCP pancreatitis was present in only 5% in study group and 11.4% in control group though statistically it was not significant (p=0.47)
Conclusion Though, there is decrease in the incidence of post ERCP pancreatitis in the group receiving octreotide, the same was not statistically significant as compared with the control (5% vs. 11.4%).
Keywords Prevention, Post ERCP pancreatitis
447
Effectiveness of cleaning and disinfection on the bioburden on gastrointestinal endoscopes
Phaniraj Kokkirala, Suresh Shetty, Suchitra Shenoy1, B Vishwanath Tantry, Sandeep Gopal, Anurag Shetty
Correspondence – Phaniraj Kokkirala – 371atient.phaniraj@gmail.com
Departments of Gastroenterology, and 1Microbiology, Kasturba Medical College Hospital, Nandigudda Road, Attavar, Mangalore, 575 001, India
Background and Study Aim: Endoscopes have revolutionized health care by providing minimally invasive techniques for diagnosis and treatment of diseases. However, these endoscopes could be heavily contaminated with body fluids and tissues during the procedure. There is risk of transmission of infections through the endoscopes, if the disinfection process is inadequate. Current disinfection method being commonly used is high level disinfection with 2 % glutaraldehyde.
Methods We conducted a prospective, observational, single center study in a tertiary care center over a period of 18 months, to know the effectiveness of cleaning and disinfection process on the bioburden on gastrointestinal endoscopes. Random samples from GI endoscopes were cultured, one sample immediate post disinfection and the other sample after storage period. A total of 101 random samples from GI endoscopes were analyzed for microbiological growth using chrome agar medium. The pathogenic microorganisms were identified by Gram’s stain and standard culture. Antibiotic susceptibility of the organism was documented.
Results Our study showed that the contamination rate of GI endoscopes is 9.9%. Mean bacteriological burden is 99 CFU/mL. Pseudomonas aeruginosa is the predominant organism identified followed by Klebsiella pneumoniae. The contamination rate of colonoscopes (16.5%), side viewing duodenoscopes (20%) and endoscopic ultrasound scopes (20%) is higher than the gastro duodenoscopes (5.5%). Immediate post disinfection contamination rate is 6.9% and after storage period is 12.8%.
Conclusion Our study showed that the current disinfection method being used for cleaning of endoscopes has its limitations. Side viewing duodenoscopes and endoscopic ultrasound scopes have higher contamination rate than gastroduodenoscopes and colonoscopes. We assume that the elevator mechanism is responsible for higher contamination rate. We recommend repeat disinfection of endoscopes just before use to decrease the higher contamination rate associated with post storage period.
Keywords Endoscope, Disinfection, Contamination rate
448
Use of a gastroscope for distal duodenal stent placement in patients with malignant obstruction
Saurabh Gaur, Mukesh Kalla, Ramesh Roop Rai, Pankaj Shrimal, Alok Verma1, Nikhil Atoliya, Anant Gupta, Sumit Patter
Correspondence – Saurabh Gaur – saurabhgaur55@gmail.com
Departments of Gastroentrology, and 1Anesthetist, S R Kalla Memorial Gastro and General Hospital, Shastri Nagar, Jaipur 302 016, India
Introduction Duodenal stent placement can be 37atient372d effectively and safely by using a Gastroscope in patients with an obstruction at the level of the distal duodenum. Patients with gastrointestinal malignancies may develop an obstruction at the level of the duodenum. Stent placement is a commonly used palliative treatment because this modality is less invasive. However, stent placement in the distal part of the duodenum (second half of the horizontal part and ascending part of the duodenum) with a therapeutic gastroscope can be difficult. The main factors limiting the use of a gastroscope for distal duodenal stenting are the relatively short endoscope length, and shaft flexibility, which may cause looping of the scope into the stomach.
Method Seventy-five-year- old male, presented to us with c/o recurrent vomiting, patient was evaluated on imaging USG abdomen s/o- large lobulated soft tissue mass lesion in tail region of pancreas abutting DJ flexure/proximal jejunum, finding confirmed by gastrograffin swallow, CECT scan done s/o large pancreatic tail malignancy, infiltrating DJ flexure/proximal jejunum. USG guided FNAC s/o well differentiated adenocarcinoma. SEMS placement done and hemoclip applied to prevent stent migration, as compared to earlier cases, the approach and negotiation was much easier. The length of the stricture was determined using contrast fluoroscopy of the duodenum during the procedure. A guide wire was then introduced through the stricture and the stent was advanced over the wire. Stent length was chosen to aim at a length of 1–2 cm more than the stricture. Endoscopy and fluoroscopy were used to follow stent deployment. Immediately after the procedure, an upright abdominal X-ray was performed to assess that no perforation had occurred during the procedure.
Results Success of deployment of SEMS, easy deployment and minimal negotiation requirement.
Keywords Gastric outlet obstruction (GOO)
449
Endotherapy with hemostatic coils with absorbable gelatin sponge: An under-utilized modality for treatment of gastric varices
Saurabh Gaur, Mukesh Kalla, Ramesh Roop Rai, Pankaj Shrimal, Alok Verma1, Saurabh Gaur
Correspondence – Saurabh Gaur – saurabhgaur55@gmail.com
Departments of Gastroentrology, and 1Anesthesia, S R Kalla Memorial Gastro and General Hospital, Jaipur 302 001, India
Introduction Gastric fundal variceal (GV) bleed is associated with high morbidity and mortality. Routine endoscopic therapies are predominantly based on using cyanoacrylate injection which is technically challenging, carries risk of embolization and endoscope damage. We present a case of GV treated with endoscopic ultrasound (EUS)-guided coil injection in combination with hemostatic absorbable gelatin sponge (AGS).
Case History A 55-year-old male presented with first episode of hematemesis and malena for 3 days.
Examination Conscious, oriented. Heart rate 96/min, blood pressure 96/54 mmHg. On examination abdomen was soft, non-tender, spleen ~6 cms below the left costal margin. Chest auscultation, cardiac and neurologic examination were normal.
Diagnosis/Investigations Hemogram showed a hemoglobin of 7.7 g/dL, MCV 76 fl, TLC 8200 cells/cumm, platelet count 3.7 lakhs/cumm, Total bilirubin 1.40 mg/dL, SGOT 48 U/L (normal 40), SGPT 46 U/L (normal 40), alkaline phosphatase 145 U/L (normal 130), albumin 3.91 g/dL, globulin 2.4 g/dL, creatinine 1.32 mg/dL. PT 22 sec (normal range 13-18 sec). US abdomen revealed chronic thrombus of portal vein with portal cavernoma and moderate splenomegaly.
Treatment Linear echo-endoscopy was done, large fundal varices (GOV 2) 3 x 3 cm was confirmed. Coil embolization (3 coil 10 mm diameter 6*5*3 mm) and gel foam (1:1 with contrast) injected using 19 G needle. 48 hours later, re-look EUS showed complete obliteration of the varix.
Discussion Traditionally, endotherapy for GV is based on injecting coils followed by cyanoacrylate. These may be associated with a long certain learning curve, systemic embolization, failed withdrawal of needle from variceal nest and deep ulceration resulting in re-bleeding. Absorbable gelatin sponge is uncommonly used in endotherapy. Unlike cyanoacrylate, it is not associated with post-injection ulcerations and damage to scopes. It is an under-utilized endoscopic intervention for the treatment of gastric varices.
Keywords Gastric varices (GV)
450
Endoscopic ultrasound guided gallbladder drainage in high surgical risk patients – A case series
Atul Gawamde, Shrikant Mukewar, Bhushan Bhaware, Ravi Daswani, Saurabj Mukewar
Correspondence – Saurabj Mekewar - saurabhmukewar@gmail.com
Department of Gastroenterology, Midas Heights, Central Bazar Road, Ramdaspetrh, Nagpur 440 010, India
Introduction The gold standard for acute cholecystitis is cholecystectomy. Ultrasound guided gallbladder drainage (EUS-GBD) EUS-GBD is a promising alternative to cholecystectomy in surgically high-risk patients with cholecystitis or biliary obstruction. However, EUS-GBD has not been reported in surgically high-risk patients with biliary colic or choledocholithiasis in whom cholecystectomy is indicated. Here, we present a case series of four patients with high-surgical risk who underwent EUS-GBD for symptomatic gallstones.
Methods Four patients (2 males and 2 females) underwent this procedure. Average age was 84.5 (67–85) years. Comorbidities included: two patients with ischemic heart disease, one patient with hypertension, atrial fibrillation, and compensated cirrhosis, and one patient with hypertension. The indication for GBD was biliary colic in two patients and choledocholithiasis in two patients. In both patients with choledocholithiasis, EUS-GBD done after the ERCP and common bile duct clearance. All patients were considered high risk for surgery (ASA grade 3 or more).
Results Two underwent GBD with cautery enhanced lumen apposing metal stent (LAMS) and in two, a cold LAMS was placed following fistula creation and balloon dilation. The stent location was transgastric in three and transduodenal in one. All four patents tolerated the procedure well with 100% technical success rate. There were no intraprocedural or postprocedural adverse events in any patient. One patient is followed for 7 months, one for 3 months, and another two patients were followed for 2 and 1 month respectively. All patients are pain free with no complications. In three patients LAMS was removed within 4-6 weeks of procedure and was replaced with double pigtailed plastic stent for cholecysto-gastric fistula. One patient is awaiting follow-up.
Conclusion EUS-GBD is safe and successful in management of surgically high-risk patients with symptomatic gallstones (biliary colic and choledocholithiasis).
Keywords Gallstones, Gallbladder drainage, Endoscopic ultrasound
451
Efficacy and safety of Shankha Prakshalana, a yogic technique versus polyethylene glycol solution for bowel preparation in colonoscopy: A randomized controlled trial
Manas Panigrahi1, Mohd Imran Chouhan1, Rajesh Manik2, Chandan Kumar1, R U Ajay Ghosh1, Biswa Mohan Padhy3
Correspondence – Manas Panigrahi - manaskumarpanigrahi@gmail.com
Departments of 1Gastroenterology, 2Ayush, and 3Pharmacology, All India Institute of Medical Sciences, Sijua, Patrapada, Bhubaneswar 751 019, India
Introduction Bowel preparation is an important part of colonoscopy. The traditional yogic technique of “Shankha Prakshalana” (SP) has been known to clean the bowel, but its efficacy for colonoscopy preparation has not been studied till date. We aimed to compare the efficacy and safety of SP with polyethylene glycol (PEG) in bowel cleaning for colonoscopy.
Methods This was a single-blinded, randomized controlled trial including 94 adult patients requiring colonoscopy who were randomized into two groups: SP group (n=47) and PEG group (n=47). Patients were advised to drink 400 mL of lukewarm saline water followed by five asanas (exercises) of SP (Tadasana, Tiryaka tadasana, Katichakrasana, Tiryaka bhujangasana and Udarakarshanasana), each done eight times. This cycle was done for a total of six times. The patients in the PEG group were given split dose preparation of PEG 3350 as recommended by various endoscopy societies. All the patients were advised low-fiber diet (< 10 g/day) for one day before colonoscopy. Boston bowel preparation scale (BBPS) was used to assess the bowel preparation in each group.
Results Mean BBPS score for whole colon in SP group (8.15 ±1.02) was more than that in PEG group (7.55 ±1.08), Δ Mean (SD) 0.6 (± 0.22), p=0.01. The difference in mean BBPS between PEG and SP group was 0.59 (95% CI [1.03-0.17]). Nausea (31.9% in PEG group and 4.30% in SP group, p=0.001), bloating (27.7% in PEG group and none in SP group, p<0.0001) and disturbed sleep (63.8% in PEG group and 12.8 % in SP group, p<0.0001) were significantly higher in PEG group as compared to the SP group.
Conclusion The traditional yogic technique of “Shankha Prakshalana” is overall better than the standard PEG-electrolyte solution, as a method for colonoscopy preparation with better tolerability and less adverse effects.
Keywords Colonoscopy, Bowel preparation, Polyethylene glycol, Yoga
452
Short- and long-term outcomes of endoscopic bilateral self-expanding metal stents placement in patients with malignant hilar obstruction
Vishalkumar Seth , Sridhar Sundaram, Utkarsh Chhanchure, Prachi Patil, Shaesta Mehta
Correspondence – Sridhar Sundaram – drsridharsundaram@gmail.com
Department of Digestive Diseases and Clinical Nutrition, Tata Memorial Hospital, Dr E Borges Road, Parel, Mumbai 400 012, India
Introduction Placement of biliary self-expanding metal stents (SEMS) has been effective for palliation of unresectable hilar malignant biliary obstruction. Optimal drainage in hilar obstruction may require placement of multiple stents. Data on multiple SEMS placement in hilar obstruction from India is sparse.
Methods Retrospective review of patients with unresectable malignant hilar obstruction who underwent endoscopic bilateral SEMS insertion from 2015 to 2021 was done. Demographic details, technical success and functional success (decrease in the bilirubin value below 3 mg /dL at 4 weeks), immediate complications with 30-days mortality, requirement of re-intervention and stent patency (till re-intervention or death) were studied.
Results Forty-three patients were included (Mean age 54.9 years, 51.2% females). 36/43 (83.7%) had Ca gallbladder, 5/43 (11.6%) had cholangiocarcinoma while 2/43 (4.6%) had colorectal cancer. 17/43 (39.5%) were locally advanced unresectable cancers while 26/43 (60.5%) were metastatic. Cholangitis was seen in 4/43 (9.3%). On cholangiogram, 26/43 (60.4%) had Bismuth type II block, 12/43 (27.8%) had type IIIA/B, 5 (11.6%) had type IV block. Technical success was achieved in 41/43 (95.3%) patients. Functional success was achieved in all patients (100%). In 38/41 (92.7%) patients’ side-by-side bilateral SEMS were placed while in 3/41 (6.7%) patients, stents were placed in Y fashion (SEMS within SEMS). Complications included post ERCP pancreatitis in 6/43 (13.9%) patients, cholangitis in 3/43 (6.9%) patients and post procedure hypertension in 1 patient (2.32%). Post-procedure 30-days mortality was seen in 1 patient. Post-procedure hospitalization days was median 5 days (2-31 days). Median stent patency was 137 days (range 8-790 days) and delayed re-intervention in the form of PTBD was required in 4/43 patients (9.3%) after mean 295.7 days.
Conclusion Endoscopic bilateral SEMS in malignant hilar obstruction has good outcomes in the form of technical success, functional success and stent patency and can be considered in progressed blocks as well.
Keywords Malignant, Hilar, Obstruction, Endoscopic, Bilateral, SEMS, Outcomes
453
Ectopic duodenal varices presenting as massive hemorrhage treated with acrylate glue- Case report
Mayur Dave
Correspondence – Mayur Dave – dr_mayurdave@yahoo.com
Department of Gastroenterology. KLE’s Dr. Prabhakar Kore Hospital and MRC, Nehru Nagar, Belgavi 590 010, India
Introduction Ectopic varicose veins refer to varicose veins with portal hypertension different with the esophageal and gastric varices, which may exist alone or with varices in other parts. About 17% of ectopic varicose veins occur in the duodenum, and it can occur in any part of the duodenum. Duodenal variceal bleed accounts for about 5% of portal hypertension hemorrhage and can lead to a mortality rate of up to 35% to 40%. There are no standard guidelines for treatment of ectopic duodenal variceal bleed. We report a case of ectopic duodenal variceal bleed treated successfully with acrylate glue in emergency setting. CASE
Presentation A 42-year-old man with a past medical history of noncirrhotic portal hypertension presented to the emergency department; with complaint of massive hematemesis and malena. Patient was initially found to be hemodynamic unstable. He was intubated in view of poor GCS and Inj. Somatostain, pantoprazole drips, Intraveous fluid and blood transfusion started as part of initial treatment. Emergent esophagoduodenoscopy (EGD) is done, showed a large varix in the second part of the duodenum. It showed evidence of recent bleeding with a red wale sign. At the time, the varix was not amenable to banding due to variceal size. A 4 mL cyanoacrylate injection was used for hemostasis. A total of 6 units packed red blood cells were transfused during his course in hospital. He was discharged uneventfully with close follow-up and advised for TIPS.
Conclusion The therapies have been reported to be efficacious for duodenal variceal bleed, including endoscopic variceal ligation, endoscopic injection sclerotherapy and TIPS along with conservative management. In our case report 377atient with massive bleed treated successfully with inj. Cynoacrylate glue as emergency endoscopy treatment for primary hemostasis.
Keywords Ectopic duodenal varices, Massive bleed, Acrylate glue
454
Endoscopic ultrasound sonograghy guided pancreatogastrostomy in non-dilated pancreatic duct for pancreatic ascites
Bhushan Bhaware , Saurabh Mukewar, Ravi Daswani, Shrikant Mukewar
Correspondence – Saurabh Mukewar – saurabhmukewar@gmail.com
Department of Gastroenterology, Midas Institute, Central Bazar Road, Ramdaspeth, Nagpur 440 010, India
Introduction Endoscopic retrograde pancreatography (ERP) is considered first-line therapy for management of symptomatic pancreatic duct obstruction or leaks. Technical failure with ERP occurs when the main pancreatic duct cannot be cannulated. Endoscopic ultrasound sonograghy (EUS)-guided drainage of the pancreatic duct is a minimally invasive alternative to surgery for failed conventional ERP. Here, we report a case of acute on chronic pancreatitis with pancreatic duct (PD) stricture in the head and leak from tail, which was successfully treated with EUS guided pancreaticogastrostomy.
Methods Here, we report a case of acute on chronic pancreatitis with PD stricture in the head and leak from tail, which was successfully treated with EUS guided pancreaticogastrostomy.
Results
Conclusion In conclusion, PD stricture can be treated endoscopically using EUS guided PD drainage, and it seems to be safe and effective. However, this procedure should be performed in expert centres with interventional radiology and surgery back up.
Keywords EUS pancreatic duct (PD) stenting, Pancreatogastrostomy, Pancreatic ascites, Non- dilated PD
455
Novel technique of Spy-Basket guided bile duct stone extraction: First case series from India
Mahesh Goenka1, Shivaraj Afzalpurkar1, Gajanan Rodge1, Sanjay Mahawar2, Usha Goenka3
Correspondence – Shivaraj Afzalpurkar – drshivaraj62@gmail.com
Departments of 1Gastroenterology, 2Anaesghesia, and 3Radiology, Institute of Gastrosciences and Liver, Apollo Hospital Day Care Building, Fourth Floor, Apollo Gleneagles Hospital, EM Bypass Road, 58 Canal Circular Road, Kolkata 700 054, India
Background Peroral cholangioscopy is being increasingly used for assessment of common bile duct during endoscopic retrograde cholangiopancreatography (ERCP). Extraction of bile duct stone using SpyBasket is a novel technique and there are very few cases reported in literature.
Methods In this series we report 10 patients in whom bile duct stone extraction was done using cholangioscopy guided SpyBasket. All the patients had undergone imaging prior to the procedure to assess the bile duct diameter, location, and size of stone.
Results This series includes 10 patients (80% female, 20% male) with mean age of 45.7 years (18 -63) and the mean size of the stone was 6.05 mm. Majority of the patients (8/10) had stone in the common bile duct. One patient each had stone in cystic duct and right anterior sectoral duct. In 6 patients’ radiation free extraction of stone was done using cholangioscopy guided Spy-Basket and in remaining 4 patients SpyBasket was used after initial failed attempt to extract stone using extraction balloon.
Conclusion All the patients had successful extraction of stone using SpyBasket with no procedure related adverse events. This is the first case series from India reporting the novel technique of SpyBasket guided bile duct stone extraction.
Keywords SpyBasket, Bile duct, Stones, Cholangioscopy
456
Novel ‘LoopTip wire technique’ for double guidewire placement during endoscopic ultrasound guided drainage of pancreatic fluid collection
Anudeep Katrevula , Goutham Reddy Katukuri, Asif Shujaath, Azimuddin Haza, Anirudh Pratap Singh, Hardik Rughwania, Mohan Ramchandani, Rakesh Kalapala, Rajesh Gupta, Zaheer Nabi, Jahangeer Basha, Raghavendra Yarlagadda, Nitin Jagtap, Nageshwar Reddy Duvvuru, Sundeep Lakhtakia
Correspondence – Sundeep Lakhtakia – drsundeeplakhtakia@gmail.com
Department of Medical Gastroenterology, AIG Hospitals, Mindspace Road, Gachibowli, Hyderabad 500 032, India
Background LoopTip wire (LTW) is used for selective endoscopic retrograde cholangiopancreatography (ERCP) cannulation. We improvised the use of LTW during endoscopic ultrasound (EUS) guided pancreatic fluid collection (PFC) drainage thereby reducing one extra-step and safely place >1 plastic stent (LoopTip wire technique). Aim was to evaluate feasibility and safety of novel ‘LoopTip wire technique’ for placing double guidewires during PFC drainage using MPS.
Methods All patients undergoing EUS guided drainage using plastic stents from November 2019 to May 2021 were included. Any of the 3 methods (double lumen cannula, wide bore pusher tube, LoopTip wire guide) were used to place guidewires based on operator preference. In ‘LoopTip wire technique’, the second guidewire is LoopTip wire (Wilson-Cook Medical Inc, 0.035”, 480 cm), that is garlanded and slid over the first wire into the PFC. In all methods of DGW placement, the initial steps of EUS guided drainage remain same. Technical success (adequate insertion of DGW into PFC followed by MPS) and clinical success (clinical improvement plus size reduction by ≥50% at 4weeks) were noted.
Results Ninety-seven patients (49 pseudocyst, 48 WOPN) underwent drainage using DGW technique using either LoopTip wire (43), double lumen catheter (30), or 10 Fr pusher tube (24). Placement of DGW was successful in all except one, who had wire shearing with double lumen cannula requiring SEMS. LTW was passed either under endoscopic (20) or EUS guidance (23). Technical challenge occurred in 5/20 using endoscopy guidance (overcome in all) and none using EUS view. Dissection of wall occurred pusher tube in 2. Technical success achieved in 96/97. Clinical success achieved in 48/49 with pseudocyst, and 34/48 with WOPN.
Conclusion For draining PFC, LoopTip wire technique is safe and effective for DGW placement and avoids extra-step for placing multiple plastic stents. Passage of LoopTip wire into PFC is better under EUS view.
Keywords LoopTip wire, PFC drainage, Double-lumen cannula
457
Safety and efficacy of endoscopic ultrasound guided liver biopsy: An initial experience from a tertiary care center
Ashish Gandhi , Harshal Gadhikar, Amol Bapaye, Sachin Palnitkar, Rajendra Pujari, Shitall Biradar 1
Correspondence – Harshal Gadhikar – gadhikarhp@gmail.com
Shivanand Desai Centre for Digestive Disorders, Shivanand Desai Center for Digestive Disorders, and 1Department of Pathology, Deenanath Mangeshkar Hospital and Research Center, Pune 411 004, India
Background and Aims Liver biopsy (LB) remains the gold standard tool for diagnosis and staging of liver disorders. Traditional approaches for LB – percutaneous or transjugular – have their inherent complications. Though transjugular route is the preferred approach in patients with coagulopathy, it is an expensive modality with limited availability. Endoscopic ultrasound guided liver biopsy (EUS-LB), a newer approach with promising results, is being considered strongly as a replacement for percutaneous approach. We aimed to assess the efficacy and safety of EUS-LB in patients with undiagnosed liver disorders.
Methods All patients undergoing EUS-LB were included; Retrospective analysis of prospectively maintained database was performed. EUS-LB was performed under GA using 19G FNB (AcquireTM, Boston Scientific) needle. Left lobe of liver was targeted; 1 or 2 passes were done; <5 to-and-fro movements during each pass; Dry heparin technique was used to facilitate tissue acquisition. Tissue acquired was sent in 10% formalin container for histopathological examination. Total specimen length (TSL); complete portal triads (CPT), diagnostic yield and procedure related complications were assessed.
Results N=12; M:F – 1:1 (6,6); mean age – 47 (10-66) y; symptoms – pain -3; jaundice-5; fever-1; pruritus-2; coagulopathy–6/12; esophageal varices–4 (low risk-2; high risk-2); ascites-5; needle-heparinised 19G; technical success – 100% (12/12); liver segment punctured–2 (if no esophageal varices)/3 (with varices); no. of passes -1 (4), 2 (8); concomitant band ligation-2; diagnostic yield 100% (AIH-4; PSC-3; steatohepatitis-1; cirrhotic nodules-1; chronic cholangiopathy-1; mild chronic hepatitis-1; normal-1); mean CPT-9 (range 5-12); median longest TSL–10 mm (IQR 5-15); complications–nil; pain–none; analgesic requirement–Nil; admission status–OP (5), daycare (5), IP (2).
Conclusion EUS-LB appears to be a safe and effective approach for tissue acquisition during evaluation of liver diseases. EUS-LB provides high diagnostic yield and can be safely performed on OP/day-care basis.
Keywords Endoscopic ultrasound, EUS guided liver biopsy, EUS-LB, Safety, Efficacy
458
Prevalence of Helicobacter pylori infection in patients undergoing upper gastrointestinal endoscopy in a tertiary referral hospital in the state of Telangana
Musunuri Asha Subbalakshmi , Abdul Wadood
Correspondence – Musunuri Asha Subbalakshmi - asha.musunuri@gmail.com
Department of Gastroenterology and Hepatology, Quality Care India Limited, Ace Atlantis, Khajaguda 500 075, India
Introduction Helicobacter pylori is a common cause of dyspeptic symptoms in the Indian Subcontinent.
Objective To study the prevalence of H. pylori associated gastritis in patients undergoing UGI endoscopy for dyspeptic symptoms in a tertiary referral hospital in the state of Telangana, Department of Gastroenterology and Hepatology, Care Hospitals, Hi-tech City, Hyderabad.
Methods This prospective study between May 2019 and October 2021 included patients presenting with symptoms of dyspepsia and were subjected to upper gastrointestinal endoscopy using Olympus EVIS EXERA-III, CV-190 series endoscope and investigated for H. pylori infection through rapid urease test of the biopsy specimen. Diagnosis of H. pylori infection was made if test results were positive.
Results A total of 2560 upper GI endoscopies were performed. Male: female ratio was 1.05:1. Age range – 3 to 85, mean age: 35 years. 72.7% patients were Indians (n=1860) and 27.3% (n=700) were international patients mainly from Middle East and Africa. H. pylori infection was diagnosed by RUT (rapid urease test) in 93.1% (2384/2560) of the patients screened of which 1637 were Indian and 686 were international patients. The most commonly recognized presenting symptoms were pain abdomen: 1986 (77.6%), abdominal bloating: 2250 (87.9%), belchings: 1730 (67.5%), Abdominal burning sensation: 1596 (62.3%), reflux of food: 1370 (53.5%), nausea: 752 (29.4%), vomiting: 106 (4.1%), GI bleed: 24 (0.9%).
Conclusion The prevalence of H. pylori infection in our study is significantly high (93.1%) even in the urban population which can be attributed to their lifestyle. H pylori infection was significantly higher in international patients (98%) as compared to Indians (88%). Previous studies done previously in the Indian Subcontinent show H. pylori positivity at around 88% to 92%. Most common presentations were abdominal bloating and pain abdomen.
Keywords Upper GI endoscopy, Dyspepsia, Helicobacter pylori
459
Intraluminal suture bezoar- An unusual complication of Roux-en-Y gastric bypass
Natraj Burra , Rami Reddy Yalaka, Lakshmi Kona, Kondal Reddy Mogili, Sasanka Vangara, Sridhar Chappidi
Correspondence – Natraj Burra – natrajb27@gmail.com
Department of Medical Gastroenterology, Gleneagles Global Hospital, Lakdi-ka-pul, Hyderabad 500 004, India
Introduction With the rise in obesity pandemic, the number of patients undergoing laparoscopic Roux-en-Y gastric bypass (RYGB) is also rising, so do the complications related to the procedure. Bezoars are collections of undigested foreign material that accumulate in the gastrointestinal tract (1). The most common are phytobezoars, which are formed from plant fibres (2). Patients who have undergone bariatric surgery are prone to bezoar formation due to reduced gastric motility, loss of pyloric function and hypoacidity (3). Bezoars can also form around a suture material which migrates intraluminally. It may be seen from months to years post operatively. Most common presentation is with post prandial pain abdomen. Other manifestations include obstruction, perforation, ulceration and gastritis (3). Endoscopic examination plays a key role in the diagnosis and management of this complication (4). Other management options include chemical dissolution or surgical exploration (5).
Methods A 50-year-old patient who underwent RYGB 2 years back elsewhere for morbid obesity presented with pain abdomen for 20 days, aggravated on taking food. UGI endoscopy showed a phytobezoar formed around a suture material in the efferent limb causing partial lumen obstruction (Fig. 1). The phytobezoar was made into pieces with help of rat tooth forceps and the entire bezoar was cleared with Roth net basket (Fig. 2).
Results Contrast-enhanced computed tomography (CECT) abdomen was done the next day which showed normal calibre of both afferent and efferent limbs. No intra luminal filling defects (Fig. 3). Patient was prescribed a syrup containing papain and fungal diastase. Advised to take low fibre diet. On follow-up he had no further episodes of pain abdomen.
Conclusion Intraluminal suture bezoar is rare complication following RYGB. High index of suspicion is needed to diagnose it. Therapeutic options include chemical dissolution, endoscopic removal and surgical exploration.
Keywords Obesity, Bezoar, Roux-en-Y gastric bypass (RYGB)
460
Safety and efficacy of full thickness over-the-scope clips: Clinical audit from a tertiary care center
Jaseem Ansari , Ashish Gandhi, Hameed Raina, Harsh Bapaye 1 , Sachin Palnitkar, Rajendra Pujari, Harshal Gadhikar, Amol Bapaye
Correspondence – Amol Bapaye – amolbapaye@gmail.com
Shivanand Desai Center for Digestive Disorders, Deenanath Mangeshkar Hospital and Research Center, Erandwane, Near Nal Stop, Pune 411 004 India, and 1Department of Medicine, Byramjee Jeejeebhoy Govt. Medical College, Pune 411 004, India
Introduction Endoclips play a crucial role in endoscopic interventions particularly in several lifesaving indications – control of bleeding and closure of leaks, fistulas, or perforations. Though through-the-scope (TTS) clips have inherent limitations, recently developed over-the-scope (OTS) clips have shown promising results. This study evaluates clinical efficacy of OTS clips in a tertiary care setting.
Methods Retrospective analysis of prospectively maintained database of all patients treated with OTS clips (Padlock clip, Steris™ or Ovesco, Ovesco™). Abstracted data-demographics, clinical status, indication for clip application, technical success, clinical success, adverse events (Aes). Primary outcome – arrest of bleed or closure of perforation/fistula/leak.
Results N=43; number of clips=46. M: F 27:16; mean age – 59 years (28-88); Indications – GI bleeds – 11 (25.5%; duodenal ulcer–9, rectal ulcer–1, Post GJ stomal ulcer–1); acute perforations-18 (42%; esophageal–3, gastric–6, duodenal–6, recto-sigmoid–3; spontaneous-3, post-surgical-1, post-endoscopic resection – 14 – [EFTR–10;ESD–3;EMR–1]); chronic leaks/fistulas–14 (32.5%; enterocutaneous fistulas–3 [duodenum – 1, colonic – 2], persistent esophageal leak post-stent placement–2, post-TB tracheaesophageal fistula–1, post-surgical recto-vaginal fistula–1; anastomotic leaks–6 [esophagojejunal–1, jejunoileal–1; post sleeve gastrectomy–1; gastrojejunostomy – 1; hemicolectomy-2]); multiple clips–3 patients (large esophageal tear – 2 patients – 2 clips each; esophagojejunal anastomotic dehiscence – 2 clips); no procedure related Aes. Technical success–43/43 (100%), clinical success–35/43 (81.4%). Failures – rebleed–2/11 (18.1%), persistent chronic leaks/fistulas–5/14 (35.7%; 1-delayed duodenal fistula recurrence after initial sealing), persistent acute perforation–1/18 (5.5%); Mortality–4/43 (sepsis in post-surgical leak–1; sepsis in chronic esophageal perforation–1; hemorrhagic shock in uncontrolled GI bleed–1; unrelated–1).
Conclusion OTS clip is safe and effective for control of GI bleeds and perforation/leak/fistula closure. Outcomes are best for closure of acute perforations, moderate for bleed control, and poorest for chronic fistula or leak closure.
Keywords Over the scope clips, OTSC, Perforation, Leaks, Fistula closure
461
Long-term efficacy of a specially designed fully covered removable self-expandable metal stent in management of post-surgical benign biliary strictures
Sachin Palnitkar, Ashish Gandhi, Jaseem Ansari, Hameed Raina, Harsh Bapaye1, Rajendra Pujari, Hars Gadhikar, Amol Bapaye
Correspondence – Amol Bapaye – amolbapaye@gmail.com
Shivanand Desai Centre for Digestive Disorders, Deenanath Mangeshkar Hospital and Research Center, Erandwane, Near Nal Stop, Pune 411 004, India, and 1Department of Medicine, Byramjee Jeejeebhoy Govt. Medical College, Pune 411 004, India
Introduction Post-surgical benign biliary strictures (BBS) are commonly reported – particularly in post liver transplant or post cholecystectomy interventions. Traditional management for short, non-complex BBS involves endoscopic approach – sequential multiple plastic stenting is preferred. However, fully covered metal stents have shown quicker stricture resolution rates and require fewer endoscopic interventions compared to plastic stents. This study aims to assess long term efficacy of specially designed fully covered metal stent for stricture resolution.
Methods Retrospective analysis of prospectively maintained database of all the patients undergoing KaffesTM (TaeWoong NITI-STM) placement for post-surgical BBS was performed. Abstracted data – demographics, disease characteristics, prior endotherapy/percutaneous interventions, No. Of ERCPs required, complications, stent indwell time, stricture resolution/recurrence rates and follow-up was recorded.
Results N=10; M:F – 8:2; indication: BBS – post liver transplant – 2 (1-duct –1; 2-duct – 1), post cholecystectomy – 8; median interval between surgery and stricture formation – 5-mo (IQR 8.5); prior interventions – 10/10 (100%; 10 – ERCP plastic stenting; 1 – PTBD + ERCP rendezvous, 1 – percutaneous stenting); mean no. of ERCPs after FCSEMS placement – 2.5 (1-4); stricture resolution – 8/10 (80%; external FCSEMS migration – 1; lost to follow-up – 1); mean stent indwell time – 5.6(3 – 10) m; stent removal – 8; stricture recurrence – 2/8 (25%; 1 – post cholecystectomy requiring surgical reconstruction, 1 – post liver transplant requiring stricture dilatation); mean stricture recurrence duration after FCSEMS removal – 3 (2-4)-mo; complications – 3 (33.3%; stent occlusion – 2, external migration – 1); median follow-up – 50-mo (IQR 51).
Conclusion FCSEMS is effective and provides long lasting stricture resolution for post-surgical benign biliary strictures with fewer endoscopic interventions. FCSEMS can be considered as first-line therapy for BBS requiring endotherapy instead of multiple plastic stents.
Keywords Benign biliary strictures, BBS, FCSEMS, Postsurgical stricture
462
Concomitant endoscopic fundoplication after per-oral endoscopic myotomy (POEM+F) for prevention of post POEM gastroesophageal reflux – Short-, medium- and long-term outcomes
Ashish Gandhi , Hameed Raina, Jay Bapaye 1 , Rajendra Pujari, Jaseem Ansari, Amol Bapaye
Correspondence – Amol Bapaye - amolbapaye@gmail.com
Shivanand Desai Centre for Digestive Disoders, Deenanath Mangeshkar Hospital and Research Center, Erandwane, Near Nal Stop, Pune 411 004, India, and 1Department of Gastroenterology, Rochester General Hospital, Portland, Rochester, New York 14621, United States
Introduction Post per-oral endoscopic myotomy (POEM) gastroesophageal reflux (GER) has been frequently reported. Concomitant fundoplication (POEM+F) has shown promising short-term results in preventing post POEM GER. This single center study reports short-, medium- and long-term outcomes of POEM+F to prevent post POEM GER.
Methods Retrospective analysis of prospectively maintained database of patients undergoing POEM+F. Abstracted data–demographics, achalasia type, pre-POEM Eckardt score (ES), procedure duration, complications and 3 monthly follow-up for 2years–post POEM Eckardt score, GerdQ scores, EGD–wrap integrity and esophagitis, pH studies. Subjective assessment – GerdQ, objective – Lyon consensus.
Results N=39; M:F=20:19; mean age–42.7 years (+/-13.66); significant symptomatic improvement in all; (mean (SD) pre- and post-POEM ES – 8.51 [1.08] and 0.89 [0.3] respectively, p < 0.05). Mean total procedure and fundoplication time (SD)–111.97 (22.2) and 41.7 (10.4) minutes respectively. Mean duration of short-, medium- and long-term follow-up – 5 (4-6), 11 (6-12) and 25 (13-31) months respectively.
Follow-up – (A) short-term–n=39; GERDQ>8–4/39 (10.25%;1–loose wrap, no esophagitis, 2–adequate wrap, no esophagitis,1–adequate wrap, Gr. C esophagitis, HP gastritis). Conclusive GER (Gr. C esophagitis, abnormal EAET)–4/39 (10.25%); borderline GER (Gr. A esophagitis, normal EAET)–4/39 (10.25%); endoscopy–Wrap integrity–adequate (36), loose (1), indistinct (2); Gr. C esophagitis–1/39 (2.5%; Wrap–adequate; abnormal EAET); Gr. A esophagitis–5/39 (12.82%; wrap – indistinct – 2, adequate – 3, EAET – abnormal – 1 , normal – 4).
(B) Medium term–n=37; GERDQ>8 –2/37 (5.4%; Gr. B esophagitis – 1). One patient from short-term improved with anti-H. pylori therapy;1 diagnosed as recurrent achalasia. No new patient developed GER.
© Long-term–n=29; total symptomatic refluxers (GERDQ) –3/29 (10.3%); new refluxers –2/29 (6.9%; previously–no symptoms; EGD–no esophagitis and adequate wrap); persistent refluxer –1/29 (3.4%).
Conclusion Concomitant endoscopic fundoplication (POEM+F) is effective and durable to prevent post POEM GER. Outcomes are sustained at mean/median two-year follow-up. Limitations–objective long-term assessment and larger studies recommended.
Keywords Endoscopic fundoplication, POEM+F, Gastroesophageal reflux, GER, post POEM GER
463
Patients with non-celiac gluten sensitivity exhibit distinct small intestinal and whole gut microbiota than that with irritable bowel syndrome and it changes with gluten-free diet
Anam Ahmed 1 , Kunal Dixit 2 , Dhiraj Dhotre 3 , Alka Singh 1 , Ashish Chauhan 1 , Vikas Jindal 1 , Mahendra Singh Rajput 1 , Ashish Agarwal 1 , Abhinav Anand 1 , Wajiha Mehtab 4 . Sunil Saroj 2 . Vineet Ahuja 1 , Yogesh Shouche 3 , Govind K Makharia 1
Correspondence – Govind K Makharia – govindmakharia@gmail.com
Department of 1Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India, 2Department of Biological Science, Symbiosis School of Biological Science, Pune 411 042, India, 3Nationl Centre for Cell Science, Pune 411 007, India and 4Department of Science, Delhi University, New Delhi110 001, India
Introduction While overlapping clinical presentation between non-celiac gluten sensitivity (NCGS) and irritable bowel syndrome (IBS) making the diagnosis difficult. Gut-microbiota has been suspected to have a role in their pathophysiology. We characterized and studied whole gut, small and large intestinal microbiota of IBS and NCGS patients at baseline and post 6-weeks of gluten-free diet (GFD) to find their role in disease development.
Methods Patients with IBS (n=493) were screened and recruited based on Rome-IV criteria, where IgA-tTG, IgA-AGA and IgG-AGA negative were, categorized as IBS and who turned-out IgA-tTG negative while IgA-AGA and/or IgG-AGA positive were categorized as likely NCGS, were put on 6-weeks GFD. Microbiome analysis was carried out for both IBS (stool=130, duodenum l=12, colon=10) and NCGS patients with baseline and follow-up samples (stool=30, duodenum=30, colon=30). Sixteen NCGS patients responded post 6-weeks GFD by claiming >30% reduction in symptoms, 14 agreed for follow-up and gluten rechallenge to check symptoms recurrence. Next-generation sequencing was performed, and data was analyzed using relevant analysis pipeline and R statistics.
Results Lower microbial diversity was observed in case of NCGS compared to controls and IBS, whereas inter-individual diversity was higher in IBS compared to NCGS. Microbiota of IBS and NCGS were significantly different especially in the duodenum, indicating gut dysbiosis. Lower abundances of common naturally occurring bacterial genera such as Alloprevotella, Succinivibrio, Lachnospira, Butyrivibrio, Blautia and higher abundances of Bacillus, Escherichia/Shigella, Pseudomonas were observed in NCGS compared to IBS. Changes in the gut microbiota were evident in duodenal microbiome as compared to colonic and whole gut microbiome. Increase in co-occurrence networking was observed after GFD in NCGS patients compared to baseline.
Conclusion Significant lower microbial diversity in duodenum of NCGS compared to IBS suggests it’s possible role in pathogenesis of NCGS. GFD improves symptoms, bacterial load, and taxa abundances while total diversity does not change.
Keywords Gluten related disorders, non-celiac gluten sensitivity, irritable bowel syndrome, gut
Motility disorders
464
Gastrointestinal motility services during corona virus disease pandemic: the past and the present
Mayank Jain, Vinodini Agrawal
Correspondence – Mayank Jain – mayank4670@rediffmail.com
Department of Gastroenterology, Arihant Hospital and Research Centre, 283- A, Gumasta Nagar, Scheme 71, Indore 452 009, India
Background Corona virus disease 2019 (COVID-19) pandemic has affected delivery of gastrointestinal endoscopy and physiology services. We highlight our experience where we maintained strict adherence to locally developed protocols based on patient demographics.
Methods We retrospectively analyzed our database and accessed the data of patients referred to our unit between June 2019 and March 2021. We divided the study period into two equal time zones of ten months each- time zone 1 (June 2019 to March 2020) and time zone 2 (June 2020 to March 2021).
Results A total of 195 procedures were done during the study period- 105 in time zone 1 and 90 in time zone 2. There was a reduction of 14.3% in overall procedures between time zone 1 and 2. Symptom screening and monitoring of vitals was done for all patients. However, screening tests like radiological investigations and molecular diagnostics were done in few patients based on patient risk profile and logistic or economic constraints. Protective measures were followed by the staff members in more than 80% of cases with use of gloves, FFP-2 mask and face shields in 100% of cases. Use of personal protective equipment (PPE) with or without a water-resistant gown was done in all cases. These measures led to an increase in the charges of the procedure with a price hike of 40% compared to pre pandemic period. In addition, nearly one third patients had to pay for additional tests like radiology and antigen/reverse transcription–polymerase chain reaction (RT-PCR) tests.
Conclusions Number of cases at our centre dropped by 14.3% in time zone 2 compared to time zone 1. Moreover, with the adoption of protective strategies, the price of procedures went up by 20% to 233% and procedures were predominantly done for patient management altering indications.
Keywords Motility, Esophagus, Anorectum, PH Metry
465
Normal values of high-resolution anorectal manometry of healthy Indians
Rahul Deshmukh 1 , Akash Shukla 2 , Sanjay Chandnani 1 , Pravin Rathi 1 , Pratik Tibdewal 2 , Shubham Jain 1
Correspondence – Rahul Deshmukh – drdeshmukhrahul@gmail.com
1Department of Gastroenterology, T N M C and B Y L Nair Hospital, Mumbai Central, Mumbai 400 008, India, and 2Department of Gastroenterology, Seth G S Medical College, K E M Hospital, Parel, Mumbai 400 012, India
Introduction High-resolution manometry (HRM) measures anal sphincter function and anorectal co-ordination. This study aims to provide normal data for HRM and evaluate the effect of gender, age, and body mass index (BMI) on anorectal functions in healthy Indian subjects.
Methods HRM was performed on 93 healthy volunteers using a 20-channel, water-perfused Catheter. We evaluated anorectal pressures, rectal sensation, and balloon expulsion time. Measurements were recorded during rest, squeeze, and simulated defecation (push).
Results Median anal resting pressure (88 vs. 94 mmHg, p=NS), anal squeeze pressure (165 vs. 147 mmHg, p=NS) were not significantly different between males and females. Rectal pressure (70 vs. 54 mmHg, p=0.024) and anal pressure (82 vs. 63 mmHg, p=0.008) during simulated evacuation without rectal distention, were higher in males. The threshold for the first sensation was lower in females (40 vs. 30 mL, p=0.021) but desire to defecate (105 vs. 90 ml, p=NS) and maximum tolerable volume (160 vs. 140 mL, p=NS) were not significantly different in males and females. Anal residual pressure (median 83 vs. 71 mmHg, p=0.025) was higher in subjects <40 years of age. Maximum anal squeeze pressure (185 vs. 165 mmHg, p=0.024) and maximum rectal pressure (75 vs. 62 mmHg, p=0.032) during push higher in BMI <23 kg/m2.
Conclusion The present study provides normal data for the Indian population that can be used for comparison and further work. Age, gender, and BMI affect anorectal parameters in HRAM and should be considered while reporting.
Keywords Normal data, Indian subjects, Manometry, Body mass index
466
Long-term gastrointestinal sequelae in corona virus disease 2019 infection” A prospective follow-up cohort study
Rithvik Golla 1 , Bhaskar Kante 1 , Peeyush Kumar 1 , Himanshu Narang 1 , Saurabh Kedia 1 , Govind Makharia 1 , Vineet Ahuja 1
Correspondence – Vineet Ahuja –vineet.aiims@gmail.com
1Department of Gastroenterology and Human Nutrition Unit, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction A novel corona virus (CoV) named ‘2019-nCoV’ by the World Health Organization (WHO) is responsible for the current pandemic that started at the beginning of December 2019 in Wuhan City, China. Many studies have shown that IBS may follow after an episode of acute gastroenteritis called as post-infectious irritable bowel syndrome (IBS). We prospectively studied the frequency and spectrum of PI-FGID’s among corona virus disease 2019 (COVID-19) cases compared with healthy controls.
Methods Two hundred and eighty-six patients with COVID-19 admitted at AIIMS, New Delhi and 286 healthy controls were prospectively followed up after 3 months of infection using validated Rome IV criteria to evaluate the frequency of chronic intestinal disorders following recovery from COVID-19 infection.
Results The study included 286 post COVID recovered patients, out of which 12 had lost to follow-up, hence a total of 274 cases and controls each were analyzed. The cases were comparable with the healthy controls in age (36.5 ± 11.9 y vs. 36.9 ± 21.3 y respectively; p=NS) and gender (142[49.5%] vs. 139 [48.5%]; males; p=NS). Based on severity, 194 (67.5%) had mild, 70 (24.4%) had moderate and 10 (3.5%) had severe disease. At 3 months, 15 (5.4%) (M: 5, F: 10) (Mild: 8, Moderate: 7), 13 (4.7%) (M: 4, F: 8) (Mild: 8, Moderate: 5), 4 (1.4%) (M: 3, F: 1) (Mild: 3, Moderate: 1), 8 (2.9%) (M: 4, F: 4) (Mild: 2, Moderate: 5, Severe: 1), 5 (1.8%) (M: 2, F: 3) (Mild: 3, Moderate: 2) developed FD, PI-IBS, FC, FD and FAB/D like symptoms respectively; among healthy controls, none developed any GI complaints (p<0.01). Risk factors for development of post COVID-19 FGIDs at 3 months included female sex and presence of GI symptoms at time of infection.
Conclusion This study shows that COVID-19 alike other acute GI infections can lead to development of PI-FGID.
Keywords Post prandial distress syndrome (PPDS), Post infectious-irritable bowel syndrome (PI-IBS), Functional constipation (FC), Functional diarrhea (FD), Functional abdominal bloating/distension (FAB/D)
Pediatric gastroenterology
467
Is it necessary to document mucosal healing in abdominal tuberculosis in children?
Vignesh Vinayagamoorthy , Ujjal Poddar, Anshu Srivastava, Moinak Sen Sarma
Correspondence – Ujjal Poddar - ujjalpoddar@hotmail.com
Department of Pediatric Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Rae Bareli Road, Lucknow 226 014, India
Background and Aim: Clinical differentiation between intestinal tuberculosis (TB) and Crohn’s disease (CD) is challenging. We aimed to document endoscopic mucosal healing and/or radiological resolution of the lesion in abdominal TB at the end of antitubercular therapy (ATT) as missing cases of other etiology like CD, multidrug resistant-TB, and gastrointestinal malignancies, leads to morbidity and mortality.
Methods In this prospective cohort, consecutive children received ATT after microbiological confirmation or with presumptive diagnosis of abdominal TB were followed up. Clinical response was assessed monthly for 3 months and then at sixth month. Baseline CT abdomen in all and colonoscopy was done when there was suspicion of luminal involvement and repeated at 2-3 months of ATT in non-responders (symptom) and in responders at 6 months.
Results Forty-six children (12.5 [0.5-17.5] years) were enrolled of which 44 children (2 died) were followed up. Forty-one percent had microbiological confirmation and 59% received empirical ATT of which 35 (79.5%) children were diagnosed to have TB and 9 (20.4%) had CD on follow-up. In CD cases, clinical response with ATT was seen in 77% at 2 months, 45% at 6 months as compared to all (100%) with abdominal TB (p<0.001). Endoscopic mucosal healing was documented in all (100%) bacteriological confirmed cases as compared to 43% cases on empirical ATT. Fifty-seven percent with no mucosal healing were eventually diagnosed as CD. Repeat imaging at the end of ATT showed non-resolution in 11% of cases of which one had MDR TB.
Conclusions Simple clinical assessment alone is not enough in cases with a presumptive diagnosis of abdominal TB and repeat colonoscopy is must at 2-3 months in those with no clinical response and at 6 months even with good clinical response. Persistence of lesion in a proportion of cases substantiates the need for repeat imaging before stopping ATT.
Keywords Abdominal tuberculosis, Follow-up, Antitubercular therapy
468
A rare case of protein-losing enteropathy in young boy
Viswanath Kamisetty, L Sahitya, V Gopal Krishna, M Ramanna, M Uma Devi, B Ramesh Kumar
Correspondence - Viswanath Kamisetty - vissu.ksp@gmail.com
Department of Medical Gastroenterology, Osmania Medical College, 5-1-876, Turrebaz Khan Road, Troop Bazaar, Koti, Hyderabad 500 095, India
Introduction Protein-losing enteropathy (PLE) is a rare intestinal disorder characterized by protein loss through the gastrointestinal tract, resulting in hypoproteinaemia. The disease can be caused by abnormalities of the intestinal lymphatic system or impaired integrity of the mucosa. Rapunzel syndrome (RS) rarely present with PLE due to mechanical obstruction of intestinal lumen and intestinal lymphatic drainage with large trichobezoars.
Case Report A 9-year-old boy with no past medical history presented with facial puffiness and lower extremity swelling for 2 weeks. On examination, he appeared malnourished (height and weight below 3rd percentile for age) with mild pallor, bilateral pedal oedema and distended abdomen. Laboratory workup revealed microcytic hypochromic anaemia with hemoglobin of 9.8 g/dL, hypoalbuminemia of 1.4 g/dL, and hypoproteinaemia of 3.5 g/dL; creatinine and urinalysis were normal. Serum IgA tissue transglutaminase levels were normal. Abdominal ultrasound showed dilated bowel loops with minimal ascites. Stool levels of alpha-1-antitrypsin were significantly elevated confirming PLE. Upper gastrointestinal endoscopy revealed a large trichobezoar extending from stomach into the small bowel, thus classified as Rapunzel syndrome. Further questioning elicited a history of trichophagia. The giant trichobezoar was removed by exploratory laparotomy with anterior gastrotomy and the child subsequently tolerated advancement of the diet with improvement in serum protein levels. This signifies the rare manifestation of Rapunzel syndrome as PLE. Trichotillomania and trichophagia are more common in females who have other psychiatric comorbidities or developmental delay. This patient’s presentation is unusual in many aspects including his male gender, young age, and lack of obvious developmental delay and comorbidities.
Conclusion This case demonstrates the importance of considering Rapunzel syndrome in the differential diagnoses for a young patient with protein-losing enteropathy of not obvious etiology regardless of gender. Accurate history is crucial in the evaluation as delays in diagnosis are common because of its rare presentation.
Keywords Protein-losing enteropathy, Hypoproteinaemia, Rapunzel syndrome, Trichobezoar
469
Comparison of bougie versus balloon dilatation for short benign esophageal strictures in children
Devarapalli Venkata Umesh Reddy , Ujjal Poddar, Anshu Srivastava, Moinak Sen Sarma, Surender Kumar Yachha
Correspondence – Ujjal Poddar - ujjalpoddar@hotmail.com
Department of Pediatric Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India, and 1Department of Pediatric Gastroenterology, Sakra Hospital, Bangalore 560 037, India
Introduction Traditionally it is believed that balloon is superior to bougie, however, there is no head-to-head comparison in children with benign esophageal strictures. We aimed to compare the efficacy and safety of endoscopic bougie and balloon dilatation for single, short esophageal strictures in children.
Methods A prospectively kept database of 188 children who presented with single short esophageal strictures between June 1994 to March 2020 was analyzed retrospectively. Comparative analysis was done for 77 cases where an exclusive bougie (n=54) or balloon (n=23) dilatation was performed. Assessment of stricture length (short if <5cm), number, and site were done at baseline by contrast esophagogram. Dilatation was considered adequate if the esophageal lumen could be dilated to 15 mm (11mm for < 2 years,12 mm between 2-5years) with complete relief of symptoms for at least 2 months.
Results The etiology of strictures (130 boys, median age 2 [0.83-4.1] years) include anastomotic 92 (48.94%) followed by corrosive stricture 42 (22.34%), peptic 20 (10.6%), congenital 18 (9.6%), post endoscopic sclerotherapy 13 (6.9%), and others 3 (1.6%). Complete data set was available for 77 cases who underwent either exclusive balloon (n=23) or bougie (n=54). Balloon dilatation was significantly better than bougie for short strictures in requiring fewer sessions to achieve adequate dilatation (4 [2-6] vs. 6 [3-9], p<0.035). There was no significant difference in perforation rates for bougie 0.35% (3/856) and balloon 0.54% (3/560) dilatation (p=0.591). Over a median follow-up of 16 (8-34) months, children who were successfully dilated showed significant improvement in their weight and height z-scores for overall as well as in both bougie and balloon groups.
Conclusion Endoscopic balloon was more effective than bougie in achieving adequate dilatation for short esophageal strictures in children. Dilatation by either bougie or balloon is safe for short strictures and resulted in significant improvement in growth on follow-up.
Keywords Esophagus, Stricture, Bougie, Balloon
470
Does endoscopic dilatation improve growth in children with benign esophageal strictures? A large single-center experience of 259 cases
Devarapalli Venkata Umesh Reddy, Ujjal Poddar, Anshu Srivastava, Moinak Sen Sarma, Surender Kumar Yachha1
Correspondence – Ujjal Poddar - ujjalpoddar@hotmail.com
Department of Pediatric Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India, and 1Department of Pediatric Gastroenterology, Sakra Hospital, Bangalore 560 037, India
Introduction Endoscopic dilatation is the primary management of esophageal strictures in children, however, literature on long-term success especially on growth is lacking. Hence, we analyzed our experience on esophageal strictures, their etiology, endoscopic management, and long-term outcomes in a large cohort of Indian children.
Methods A prospectively kept database of 259 children from June 1994 to March 2020 with esophageal strictures was analyzed retrospectively. Dilatation was performed 2-3 weekly by using either the bougies or CRE balloon dilators and was considered successful if the esophageal lumen could be dilated to 15 mm (11 mm in <2 years,12 mm in 2-5 years of age) with complete relief of symptoms for at least 2 months. Children were grouped by their etiology and nature of stricture for comparisons. To assess the impact of dilatation on growth, baseline and follow-up weight and height z-scores were calculated.
Results The most common etiology of the whole group (177 boys, median age 2.5 [1.08-5.5] years) was anastomotic stricture in 99 (38.2%) cases, followed by corrosive stricture in 96 (37.1%). The outcome analysis could be done in 186 with 73 cases having lost to follow-up. The dilatation was successful in 168 of 186 (90.32%). Corrosives required a significantly higher number of sessions to achieve adequate initial dilatation as compared to other etiology (11 [7-19] vs. 6 [4-10], p<0.001). Fourteen esophageal perforations occurred during a total of 2580 dilatation sessions (0.54%) with one death. Over a median follow-up of 17 (6-39) months, there was significant improvement in both the weight z-score (-2.56 [-3.58 to-1.40] vs. -1.56 [-2.6 to -0.64], p<0.001) and height z-score (-2.18 [-3 to -0.87] vs. -1.24 [-2.42 to -0.17], p<0.001) in children who were successfully dilated.
Conclusion Endoscopic dilatation is safe and effective in the management of esophageal strictures in children with successful dilatation resulting in significant improvement in growth on follow-up.
Keywords Esophagus, Stricture, Endoscopy, Growth
471
Spectrum of motor dysphagia in the pediatric population: A single center experience
Amrit Gopan , Harish Darak, Michael Kuruthukulangara, Nitish Patwardhan, Megha Meshram, Aditya Kale, Akash Shukla
Correspondence - Amrit Gopan - amrit.kem@gmail.com
Department of Gastroenterology, Seth G S Medical College and K E M Hospital, 9th Floor, New Multistory Building, Parel, Mumbai 400 012, India
Introduction Non-mechanical causes of dysphagia are difficult to diagnose and manage in children, which renders it imperative to identify and profile them for appropriate treatment.
Methods Retrospective data was retrieved from a prospectively maintained motility laboratory database from July 2016 to July 2021 to identify children between 0-18 years with motor dysphagia. Clinical history, contrast esophagogram, esophagoscopy and esophageal manometry findings were noted. Manometry was performed using 36 channel water perfusion system (Medical Measurement Systems v 9.6e).
Results Nineteen children (8 male, 42%), median 14 years (1-18 y) were included. Onset of dysphagia was in 1st decade in one-thirds (36.84%). Nearly half (47%) reported dysphagia to both solids and liquids, and one fifth had documented weight loss from symptom onset. Postural maneuvers or use of liquids for bolus propulsion was seen in 15.8%. On high resolution manometry, achalasia formed the most common diagnosis (11 [57.8%], with type 1 [21%], type 2 [21%] and type 3 [15.8%]). Esophagogastric junction (EGJ) outflow obstruction was seen in 2 (10.5%), ineffective esophageal motility in 2 (10.5%), ineffective solid motility in 1 (5.3%) and no obvious abnormality in 3 (15.8%) patients. Among achalasia patients, barium swallow showed distal narrowing with dilated esophagus in 8 (73%), sigmoid esophagus in 1 (9%), and contrast hold-up on delayed films in 2 (18%). Among non-achalasia, none had a sigmoid esophagus and hold-up of contrast was seen in one patient with EGJ outflow obstruction. Among achalasia, dilated esophagus on upper endoscopy was seen in 7 (64%) and food or liquid residue in esophagus in 5 (45%). Median (range) integrated relaxation pressure was 27.9(16.1, 59.7) mm, abnormal distal latency (<4.5 seconds) seen in 71% and ineffective contraction (DCI<450 mmHg.s.cm) in 57%. No technique related adverse events were observed.
Conclusion Achalasia cardia constitutes a major proportion of esophageal motility disorders in children with motor dysphagia. Manometry is safe and an effective diagnostic tool even in young children.
Keywords Motor dysphagia, Pediatric, Achalasia
472
Profile of extrahepatic portal vein obstruction in infants and young children: Does early onset imply poorer growth indices?
Ankita Singh , Amrit Gopan, Nagma Khan, Prajakta Mane, Aditya Kale, Akash Shukla
Correspondence - Amrit Gopan - amrit.kem@gmail.com
Department of Gastroenterology, Seth G S Medical College and K E M Hospital, 9th Floor, New Multistorey Building, Parel, Mumbai 400 012. India
Introduction Extrahepatic portal vein obstruction (EHPVO) is the most common cause of portal hypertension in children. We studied the profile of infants and young children with EHPVO in under-five age group and compared the burden of growth failure with older children and adolescents.
Methods Data of EHPVO patients from September 2000 to September 2021 with index presentation at <5 years were analysed from a prospectiely maintained liver clinic database. Anthropometric data were compared with those presenting between 5-18 years.
Results One hundred and eighty-one patients were identified with diagnosis of EHPVO at <18 years of age. Of these, 61 (33.7%) were <5 years. After excluding for paucity of data, 40 (21 [52.5%] male) under 5 years formed the study cohort and 32 (20 [62.5%] male) in 5-18 years as comparison cohort. Median age at presentation in study group was 40.5 (1-60) months. 9 (22.5%) were preterm (<40 weeks gestation), 14 (35%) had low birth weight (LBW, <2500 grams). Of those with LBW, 8 (57%) had a neonatal intensive care unit stay for >7 days and 5 (35.7%) had early or late neonatal sepsis. Index presentation was upper gastrointestinal bleed (24 [60%]), abdominal lump (7 [17.5%]), left hypochondriac discomfort (6 [15%]) or incidentally detected (3 [7.5%]). In <5 years, 16 (40%) had weight <3rd centile ([wasted], WHO MGRS charts 2006), 13 (32.5%) had height <3rd centile (stunted), while both stunting and wasting was seen in 12 (30%). The LBW subgroup had significantly more wasting at presentation compared to normal birth weight cohort (p=0.003).) Among 5-18 year olds, weight < 3rd centile was seen in 15.6% (vs. 40% in < 5 y, p=0.023) and height <3rd centile in 6.25% (vs. 32.5% in <5y, p= 0.006).
Conclusion EHPVO in infants and children less than 5 years has more severely affected growth indices, possibly due to early deprivation of adequate portal blood flow. A significant impairment in catch-up growth may result in infants with low birth weight developing EHPVO.
Keywords Infants, Extrahepatic portal vein obstruction, Pediatric, Growth failure
473
Spectrum of gastrointestinal bleeding in pediatric population of hill state of north India
Shruti Sharma1, Yash Pal Sharma2, Shikha Sood3, Mukesh Surya3
Correspondence - Shruti Sharma - shrutichail@gmail.com
Department of 1Pediatric Gastroenterology and Hepatology Unit, 2Otorhinolaryngology, and 3Radiology, Indira Gandhi Medical College, Ridge Sanjauli Road, Lakkar Bazar, Shimla 171 001, India
Introduction Gastrointestinal bleeding (GIB) in children is a common condition with low mortality but can lead to immense anxiety in parents. These children should be timely evaluated for the etiology to decrease morbidity.
Methods We retrospectively analyed the data of children (birth to 18 years of age) referred to Pediatric Gastroenterology and Hepatology Unit in Indira Gandhi Medical College with GIB from September 2019 to August 2021, with the aim of finding out the spectrum of GIB. Those who improved on medication or did not get endoscopic evaluation were excluded.
Results Among 128 cases included, causes of upper GIB were 53.1% (n=68) and lower GIB were 46.9% (n=60). In upper GIB, non-variceal (n=58, 85%) causes were- acid peptic disease (APD) (n=47, 69.1%) and miscellaneous (n=11, 16.1%). Variceal (n=10, 14.7%) causes were- extrahepatic portal vein obstruction (n=8, 11.7%) and chronic liver disease (n=2, 3%; [1=autoimmune hepatitis, 1=Caroli’s disease]). Among miscellaneous causes, 4 cases were Munchausen syndrome, 2 were Malory-Weiss tear and one each were intussusception, arteriovenous malformation, idiopathic thrombocytopenic purpura, pulmonary tuberculosis (? swallowed sputum) and hepatic artery pseudoaneurysm. Sixteen cases (34 %) of APD had H pylori infection. Among causes of lower GIB, colorectal polyps (n=24; 40%), infective diarrhea (n=9; 15 %), internal haemorrhoids (n=8, 13.3%), solitary rectal ulcer (n=6, 10%), cow milk protein allergy (n=5, 8.3%), Inflammatory bowel disease (n=4, 6.6%) and one case each of intussusception, post anastomotic ulcers, rectal prolapse and HSP were seen. One patient underwent digital subtraction angiography and coiling for hepatic artery ps eudoaneurysm. A significant bleed was seen in 25 % of the cases, while the mortality was 2.3% (3 cases). One patient underwent an open laparotomy following perforated peptic ulcer.
Conclusion Our causes of Pediatric upper GIB are different from that of other centres, with APD being the most common cause, however, spectrum of lower GIB is comparable to previous data.
Keywords Gastrointestinal bleeding, Colorectal polyp, Portal vein obstruction, Internal hemorrhoids
474
Thromboelastographic evaluation of factors affecting coagulation status of children with decompensated chronic liver disease and sepsis
Vignesh Vinayagamoorthy1, Anshu Srivastava1, Indranil Das2, Anupam Verma2, Prabhakar Mishra3, Moinak Sen Sarma1, Ujjal Poddar1, Surender Kumar Yachha4
Correspondence – Anshu Srivastava - avanianshu@yahoo.com
Departments of 1Pediatric Gastroenterology, 2Transfusion Medicine, 3Biostatistics and Health Informatics, Sanjay Gandhi Postgraduate Institute of Medical Sciences, RaeBareli Road, Lucknow 226 014, India, and 4Pediatric Gastroenterology, Sakra World Hospital, Marathahalli, Bangalore 560 103, India
Objective To evaluate the coagulation status of children with decompensated chronic liver disease (DCLD) and infection by thromboelastography (TEG) and study the effect of systemic inflammatory response syndrome (SIRS), infection severity and resolution, and bleeding on the coagulation status.
Methods Children admitted with DCLD, and infection were prospectively enrolled. Coagulation was assessed by INR, platelet count and TEG (reaction time [R], kinetic time [K], α-angle [AA], maximum amplitude [MA], coagulation index [CI], and lysis index [LY 30]) at admission and after 7-14 days. CI of <-3 represents hypocoagulable state. Clinical profile including SIRS, infection severity, bleeding, treatment response and outcome were noted.
Result Thirty children (21 boys, age 78 [15.7-180] months with DCLD were studied. At admission, 29 (96.7%) had prolonged INR, 24 (80%) had thrombocytopenia and 17 (56.6%) were hypocoagulable by TEG. 10/13 cases had normal TEG but deranged INR and platelets. 19 (63.3%) had SIRS, patients with and without SIRS had similar TEG findings. In follow-up, SIRS resolved in 15 and persisted in 4 cases. Hypocoagulable state was more common in persistent than resolved SIRS (100% vs. 33%; p=0.03) and severe sepsis (n-11) than sepsis/infection alone (81.1% vs. 42.1%; p=0.05). Patients with persistent SIRS had significantly lower MA, α-angle and LY30 as compared to resolved SIRS. Children with persistent infection (n-10) had worse INR (4.2 vs. 1.9; p=0.04), Rtime (7.35 vs. 5.4; p=0.1) and poorer clot lysis (0 vs. 0.7; p=0.08) than those with resolved infection (n-15). Bleeders (n-8) had longer Rtime (7.8 [5.6-13.32] vs. 5.44 [4.17-6.75]; p=0.03), smaller MA (30.2 [21.72-52.75] vs. 47 [42.2-56.52]; p=0.05), α-angle (40.45 [24.85 -60.4] vs. 62.9 [48.6-67]; p=0.03) but similar INR and platelets than non-bleeders. Non-survivors (n-6) had longer R time than survivors (n-24). R time ≥8.5 min predicted poor outcome with 83% sensitivity and 100% specificity.
Conclusions 57% children with DCLD and infection have hypocoagulable state by TEG. TEG parameters are more deranged in patients with bleeding, severe sepsis, persistent SIRS and infection despite therapy. TEG identifies bleeders better than INR/platelets.
Keywords Thromboelastography, Decompensated chronic liver disease, Coagulopathy, Sepsis, Pediatric
Surgical gastroenterology
475
Association of Meckel's diverticulum with infected urachal cyst
Anant Singh, Rohit Chaudhary, Aditya Tolat
Correspondence - Anant Singh - anantsingh895@gmail.com
Department of General Surgery, VMMC and Safdarjung Hospital, D-2/203, Golf City, Sector 75, Noida 201 301, India
Meckels’s diverticulum and urachal cyst most commonly affects younger age group ultrasound abdomen, contrast enhanced computed tomography has failed to identify the association of Meckel’s diverticulum with urachal cyst. To our knowledge, there are very few case reports with co-existence of Meckel’s diverticulum and urachal cyst. It is relevant to investigate for Meckel’s diverticulum in cases with urachal abnormalities and vice versa due to the complications associated with both of them. Surgical excision of both have to be carried out when they co-exist presenting with symptoms of either of the disease. We report a case of Meckel’s diverticulum with infected urachal cyst.
Keywords Meckel's diverticulum, Urachal cyst
476
Advantages of routine milking of common bile duct during combined laparoscopic cholecystectomy with endoscopic retrograde cholangiopancreatography procedure
C G Sridhar , C Palanivelu, Mohammad Juned Khan, Anabhra Sharma
Correspondence - Anabhra Sharma - anabhra.sharma@yahoo.com
Department of Gastroenterology, GEM Hospital, 45-A, Pankaja Mills Road, Ramnathapuram, Coimbatore 641 045, India
Background Approximately fifteen percent of patients with gallbladder stones also have common bile duct (CBD) stones. endoscopic retrograde cholangiopancreatography (ERCP) when combined with laparoscopic cholecystectomy (LC) for concomitant CBD stone and other complications was historically not preferred due to various technical difficulties. We aimed this study to evaluate the role of CBD milking to minimize complications and to increase probability of selective biliary cannulation in ERCPs post-LC.
Method This study included all cases undergoing combined LC with ERCP as one-step procedure at GEM Hospital, Coimbatore in the period from December 2020 to August 2021. All complications and percentage of biliary or pancreatic duct (PD) cannulations were noted to compare them with conventional method of single-step procedure. Patients undergoing LC with ERCP as two-step procedure were excluded.
Result Out of total 68 cases, biliary cannulation failed in 8 patients whereas 1 failure was noted when milking of CBD was performed intra-operatively. Average anaesthesia time of 106.5 minutes in milking group was less than conventional 122.8 minutes with decreased hospital stay and lesser financial burden. Complications like retained calculi were higher in non-milking group (11 vs. 5). Postoperative pancreatitis and inadvertent PD cannulation was observed in 4 and 9 cases respectively but in 1 case each if milking was done.
Conclusion Milking of CBD although difficult in some cases of LC, has definite benefit in success rate of ERCP with reduced operative time and complication rates probably due to increased intraductal pressure effects on sphincter of Oddi. Follow-up is required to make it standardized technique in conventional one-step combined LC with ERCP.
Keywords ERCP, Laparoscopic cholecystectomy, Milking of common bile duct
477
Unusual case of feculent vomiting
Prasanna Gore, Gaurav Mehta
Correspondence - Prasanna Gore- drprasannagore@gmail.com
Department of Medical Gastroenterology, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Rao Saheb Achutrao Patwardhan Marg, Four Bungalows, Andheri West, Mumbai 400 053, India
A 49-year-old male presented with complaints of weight loss 8-10 kgs since 1 year, decreased appetite, chronic diarrhea and breathlessness on exertion. Patient was taking treatment from private practitioner in view of above symptoms and on investigation found to have severe iron deficiency anemia and was kept of oral iron supplements. Patient had progressive breathlessness on exertion, and had feculent vomitus hence brought to our hospital. On examination patient had Severe pallor, tachycardia, and signs of anemic failure. Patients HB was 3.6 gm and severe iron deficiency. Patient was transfused 3 units PRBC with Lasix. CECT abdomen suggestive of Large ill-defined heterogeneously enhancing centrally necrotic mass along the greater curvature of stomach and is contiguous with transverse colon. Hence patient was posted for EGD which was suggestive of large ulcerated mass along greater curvature of stomach with feculent material oozing through fistulous tract the lesion biopsy suggestive of mixed adenocarcinoma. Colonoscopy revealed circumferential mass with luminal narrowing in descending colon, Biopsy revealed low grade adenocarcinoma. PET CT revealed FDG uptake in curvature of stomach, transverse colon and splenic flexure. IHC revealed carcinoma of gastric origin hence patient started on neoadjuvant chemotherapy with CAPEOX regime each cycle every 21 days for 4 cycles, later on posted of surgery distal gastrectomy with extended right hemicolectomy. Gastric fistula is rare presentation of both benign and malignant diseases of gastrointestinal tract. Malignant gastrocolic fistula is most commonly associated with adenocarcinoma of the transverse colon in the western world. But in our case unusual was Mixed adenocarcinoma of gastric origin causing gastro-colic fistula, which is a rare complication of gastric carcinoma.
Keywords Feculent vomiting, Adenocarcinoma, Gastro-colic fistula
Nutrition
478
Association of lifestyle characteristics in non-diabetic non-alcoholic fatty liver disease patients
Swapna Chaturvedi1, Neena Bhatia2, Naval Vikram3, Kumble S Madhusudan4, Ravindra Mohan Pandey5
Correspondence – Swapna Chaturvedi - swapnaaiims@gmail.com
1Departments of Dietetics, 3Medicine, Metabolic Research Group, 4Radiodiagnosis, and 5Department of Biostatistics, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India, 2Department of Food and Nutrition, Lady Irwin College, University of Delhi, New Delhi 110 070, India
Introduction Non-alcoholic fatty liver disease (NAFLD) has emerged as a public health problem against the backdrop of diabetes, dyslipidemias and central obesity. Lifestyle characteristics may have a major impact on liver related morbidity and mortality.
Objective To identify the lifestyle characteristics associated with NAFLD.
Methods In a hospital-based case control study a total of 320 subjects (160 per group) constituted the study population based on inclusion and exclusion criteria. Sample size was been calculated using the formula for comparing two means (Mean 1 ± SD1, Mean 2 ± SD2), with statistical power of 80% and level of significance as 5%. Lifestyle characteristics were assessed in addition to socio demographic, anthropometric, clinical, and biochemical factors. Lifestyle characteristics included assessment of nutrient intake (using 24 recall and FFQ) and dietary pattern, physical activity pattern (using GPAQ Questionnaire), sleep patterns, intake of snacks, alcohol and smoking habits by face to face interviews.
Results The life characteristics that showed a significant association with NAFLD were family history of diabetes (OR [95 % CI] [1.8] 1.08-3.20, p=0.023), central obesity (waist circumference >80 cm in females and >90 cm in males) (3.8 [2.37-6.17], p=<0.001), low physical activity (2.6 [1.69-4.20], p=<0.001), higher intake of edible oil (>25 g for males and > 20 g for females) (2.5 [1.24-5.01], p=0.010), saturated fats (> 8 % of total calories [2.0]1.17-3.47) p= 0.011, evening snack (2.1 [1.23-3.60], p=0.006) and alcohol (2.0 [1.10-3.81], p=0.024).
Conclusion It was found that unfavorable combinations of lifestyle characteristics, play an important role in development of hepatic steatosis. Screening and counseling sessions should be conducted for individuals with these lifestyle characteristics to prevent the progression of NAFLD to its severe forms.
Keywords NAFLD, Lifestyle characteristics. Nutrients, Physical activity
479
Evaluation of nutritional status in patients with inflammatory bowel disease
Arshdeep Singh, Shruti Verma, Vandana Midha1, Ramit Mahajan, Ramandeep Kaur, Dharmatma Singh, Namita Bansal, Ajit Sood
Correspondence – Ajit Sood - ajitsood10@gmail.com
Department of Gastroenterology, and 1Medicine, Dayanand Medical College and Hospital, Tagore Nagar, Civil Lines, Ludhiana 141 001, India
Background Inflammatory bowel disease (IBD) is associated with an increased risk of malnutrition and sarcopenia. There is paucity of data on the nutritional status in patients with IBD from Asia.
Methods This is a single centre cross-sectional analysis of adult (age>18 years) patients with IBD (ulcerative colitis [UC] and Crohn’s disease [CD]) who underwent anthropometry (body mass index [BMI]), mid upper arm circumference (MUAC) and triceps fold thickness (TSF), body composition analysis (fat mass, lean mass, fat mass index [FMI] and fat free mass index [FFMI]) and assessment for sarcopenia handgrip strength and skeletal muscle index (SMI) at L3 vertebral level at a tertiary care centre in north India. Age and gender matched healthy adults were taken as controls. The European Society of Clinical Nutrition and Metabolism (ESPEN) criteria was used to define malnutrition.
Results A total of 406 patients (336 [82.76%] UC and 70 [17.24%] CD; mean age 40.56±13.67 years; 215 [52.95%] males) with IBD and 100 healthy controls (mean age [38.69±10.90] years; 56 [56%] males) were enrolled; of which 102 (25.12%) were found to be malnourished. The mean BMI, MUAC and TSF thickness were lower in patients with IBD as compared to controls (23.32±4.82 kg/m2, 25.59±3.83 cm and 13.21±6.84 mm vs. 24.92±3.74 kg/m2, 27.70±3.25 cm and 21.36±7.74 mm; p=0.002, <0.0001 and <0.0001 respectively). Patients with IBD also had lower fat mass and lean mass (19.04±8.28 kg vs. 20.92±6.46 kg; p=0.04 and 43.44±9.79 kg vs. 47.18±8.53 kg; p<0.0001). The FMI and FFMI related inversely with disease severity. The mean handgrip strength and L3SMI were greater in controls. No significant differences were observed in anthropometric measurements, body composition and sarcopenic measures between patients of UC and CD.
Conclusion Malnutrition and sarcopenia are common in IBD compared to healthy controls. Patients with both UC and CD are at equal risk. FM I and FFMI have the potential to be used as predictors of disease course.
Keywords Malnutrition, Nutritional status, Body composition, Ulcerative colitis
480
Wernicke's encephalopathy precipitated by refeeding after water-only fasting for 30 days in an non-alcoholic individual improved with thiamine supplementation
Venkatakrishnan Iyer 1 , Manik Kaur 2
Correspondence - Venkatakrishnan Iyer - vhiyer78@gmail.com
1Department of Gastroenterology, Sahaj Gastro Care and Sarjan Fertility Centre, Bhavnagar
364 002, India, and 2Radiology Department, Sarvoday Imaging Centre, Swastik Square, Kalanala, Bhavnagar 364 002, India
We present a case of a non-alcoholic individual, who after prolonged fasting developed Wernicke's encephalopathy, which improved with prompt administration of thiamine.
A 24-year-old unmarried female from the Jain community had undertaken a difficult penance of water only fasting for 30 days. Within a week of refeeding, she had vomiting 6-8 times/day, immediately after consuming any liquid or food. She was treated with iv fluids, PPI and anti-emetics but with no improvement. Electrolytes showed low serum potassium (2.9 mEq/L) which was promptly corrected. Other metabolic parameters and a sonography abdomen were normal. An upper GI endoscopy showed gastric erythema with no evidence of any ulcer or obstruction. On detailed history taking, she had complained of diplopia, difficulty in walking and maintaining balance, which she attributed to weakness due to her prolonged fasting. On clinical examination, she was fully conscious and oriented. She had bilateral 6th nerve palsy (Right>left) and horizontal gaze nystagmus with positive cerebellar signs on clinical examination, causing difficulty in walking independently. A neurologist was invoked, who after a clinical evaluation suggested an MRI brain. It showed multiple bilateral thalamic, peri aqueductal midbrain and corpus callosal altered signal intensities (T1 hypo T2 hyper intense), suggesting Wernicke’s/metabolic encephalopathy. After administration of iv thiamine in the dose of 600 mg/day, she showed remarkable improvement in diplopia, gait disturbance and ataxia.
The classic triad of Wernicke’s encephalopathy (WE) includes encephalopathy, oculomotor dysfunction and gait ataxia. Clinically, WE is diagnosed in patients with two of the following four Caine criteria: dietary deficiency, oculomotor abnormalities, cerebellar dysfunction and either of altered mental status or mild memory impairment. Our patient had three of the four Caine criteria. She promptly responded to IV thiamine. Our case highlights the need to have a high index of suspicion to diagnose Wernicke's encephalopathy, especially in non-alcoholic individuals.
Keywords Wernicke's encephalopathy, Fasting, Thiamine supplementation
481
Cost and nutrient comparison of gluten-free foods with their gluten containing counterparts
Wajiha Mehtab , Samagra Agarwal, Tamoghna Ghosh, Harsh Agarwal, Shubham Prasad, Ashish Chauhan, Namrata Singh, Anita Malhotra 1 , Vineet Ahuja, Govind K Makharia
Correspondence - Govind K Makharia – govindmakharia@gmail.com
Department of Gastroenterology and Human Nutrition, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India, and 1Department of Home Science, Lakshmibai College, University of Delhi, Ashok Vihar III - Ashok Vihar, Delhi 110 052, India
Background A lifelong gluten-free diet is the only available treatment for patients with celiac disease. Nutritional quality of gluten-free food products is very important as patients consume these products for life-long. There is paucity of data on the nutritional content and cost of GF-food products compared with their gluten containing counterparts from India and Asia.
Study After a detailed market survey, the packaged and labeled gluten-free food products (n=485) and their packaged gluten containing counterparts (n=790) from the supermarkets of Delhi (India) and e-commerce websites were included. Nutritional content and cost per 100 gram food (in US dollars) were calculated using the nutritional contents and prices mentioned on food label.
Results Gluten-free food products were 232% (Range: 118%-376%) more expensive than their gluten containing counterparts. Energy content of all gluten-free food products was similar to their gluten containing counterparts, except cereal-based snacks. Both the protein and dietary fiber content were significantly lower in gluten-free pasta and macaroni products (single-grain, multigrain), cereal flours (single-grain) and nutritional-bars than their gluten containing counterparts. Gluten-free bread and confectionary items, biscuits and cookies and snacks had higher total-fats and trans-fat content than their gluten containing counterparts. Gluten-free cereal-based snack foods had higher sodium content than their gluten containing counterparts. Seventy three percent of gluten-free food products were classified as ultra-processed foods.
Conclusion Gluten-free food products are significantly more expensive than their gluten containing counterparts, thus increasing the economic burden to the patients, and potentially acting as a barrier to adherence to gluten-free diet. Majority of packaged gluten-free food products are highly processed and contain less protein and dietary fiber and higher fat, trans-fat and sodium.
Keywords Gluten-free foods, Gluten-containing food, Nutritional quality, Cost, Celiac disease
482
Barriers in the adherence to gluten-free diet in adult patients with celiac disease
Wajiha Mehtab1,2, Alka Singh1, Anam Ahmed1, Ashish Chauhan3, Mahendra Singh Rajput1, Lalita Mehra1, Vikas Banyal1, Shubham Prasad1, Shubham Mehta1, Namrata Singh1, Vineet Ahuja1, Anita Malhotra2, Govind K Makharia1
Correspondence – Govind K Makharia - govindmakharia@gmail.com
Departments of 1Department of Gastroenterology and Human Nutrition, 2Department of Home Science, 3Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Introduction Lifelong and strict adherence to gluten-free diet (GFD) is the only definite treatment for patients with celiac disease (CeD) at this point of time. Following a GFD is a challenging task for patients and families with CeD. There are many barriers in maintaining a strict adherence to GFD. The adherence to GFD is influenced by multiple factors present at various ecological levels of human-development and decision-making, including intra-personal, inter-personal, organizational, community and system-based levels. We therefore determined the factors influencing the adherence to GFD at these levels in adult patients with CeD.
Methods A questionnaire was developed based on review of literature, group discussions and expert group meetings. The questionnaire was administered to patients with CeD attending Celiac Clinic and following GFD for >1 year.
Results Overall, 545 patients (females: 335.median age: 29 years, inter-quartile range: 22-46 years) were included. We observed many barriers including intra-personal such as lack of a separate gluten-free flour mill at home in 165 (30.2%) patients; inter-personal barrier such as inadvertent intake of gluten-containing food products while dining-out with family/friends in 128 (23.5%) patients; organizational barrier such as non-availability and high cost of packaged GF-food products in nearby markets in 215 (39.2%) and 140 (25.7%) patients respectively and non-membership of celiac support group in 248 (45.5%) patients. The barrier at the community level was non-awareness of complexity of their dietary needs in 153 (28.1%) patients. Additionally, at the system level, there is lack of appropriate infrastructure and strategy for maintenance of GF lifestyle such as inappropriate counselling by dietician and the physician in almost one third of patients.
Conclusions In India, there are multiple barriers to the adherence of GF lifestyle. There is a need to create infrastructure for removal of these barriers at various levels of ecosystem.
Keywords Barriers, adherence, gluten-free diet , celiac disease, ecological levels, ecosystem
483
Exclusive enteral nutrition refurbishes beneficial gut microbiota in patients with acute severe ulcerative colitis
Manasvini Markandey , Vineet Ahuja
Correspondence – Vineet Ahuja - vineet.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029, India
Background Exclusive enteral nutrition (EEN) acts as an adjunctive therapy to intravenous corticosteroids in patients with ASUC. Recently reported by Sahu et.al., patients with ASUC undergoing EEN showed reduced corticosteroid failure rates compared with standard-of-care (SOC) group. While the mechanism of action of EEN is unclear, EEN is known to cause marked alterations in the gut microbiome. The present study extending the findings of Sahu et.al., aims to decipher the compositional changes in gut microbiome accompanying the EEN-augmented steroid responsiveness.
Methodology In an open-label RCT, patients with ASUC were randomized 1:1 to EEN and SOC groups. Patients on EEN received a semi-elemental formula for 7 days along with SOC. The primary outcome was steroid failure, defined by the need for salvage medical intervention. Fecal microbial analysis was performed on day-0 and day-7 by 16S-rRNA gene sequencing. Processing of raw reads, ASV tables, diversity, and core microbiome analysis was done using QIIME2-2021.4. Differential abundance analysis (DAA) was performed using Deseq2.
Results The α and β diversity indices showed deviation neither in EEN nor in SOC groups. EEN caused a shift in core microbiota of patients with ASUC, adding Streptococcus and Fecalibacterium prausnitzii, while SOC could not change the core microbiota. DAA on the pre- and post-treatment samples showed that EEN resulted in diminished Ruminococcus gnavus, Escherichia sp., Bifidobacterium longum and Enterococcus sp., while the SOC led to reduction in beneficial F. prausnitziiand enhanced Escherichia.
DAA between steroid responders and steroid non-responders in the EEN group, showed significant enhancement of Veillonella, Ligilactobacillus, Limosilactobacillus, Gamella, Enterococcus and Eggerthella in the SR group, while Schaalia, R. gnavus, Lactobacillus, Bifidobacterium, Haemophilus were elevated in SNR group.
Conclusions ASUC accompanies gut dysbiosis. EEN refurbishes certain beneficial gut microbial genera, which may account for its augmentation of the steroid responsiveness in patients with ASUC.
Keywords Exclusive enteral nutrition, Gut microbiota, Acute-severe ulcerative colitis
484
Correlation of sarcopenia with increased risk of decompensation of cirrhosis
Rakesh Jha
Correspondence – Rakesh Jha - jharakesh2006@gmail.com
Department of Medical Gastroenterology, Government Stanley Medical College, No.1, Old Jail Road, George Town, Chennai, Tamil Nadu 600001, India
Background Sarcopenia is a generalized and progressive loss of skeletal muscle mass, strength, function seen in 70% of patients with cirrhosis. Sarcopenia leads to physical disability and functional decline, thereby leading to poor quality of life (QOL). Hepatic encephalopathy is an independent predictor of mortality in cirrhosis, various studies has shown its correlation with CTP Score and MELD score. Sarcopenia is well established a predictor of hepatic encephalopathy, spontaneous bacterial peritonitis.
Aim Correlation of sarcopenia with increased risk of hepatic encephalopathy, spontaneous bacterial peritonitis, upper gastrointestinal bleed and hepatorenal syndrome-acute kidney injury spectrum type-I.
Methods Psoas muscle index calculated at L3 vertebrae on CECT imaging and adjusted to body surface area to calculate SMI other scoring calculated, number and types of decompensation noted in past.
Results Total 25 patients were included in study MELD-Na score minimum was 7 and maximum 30 with mean 22.28 with SD±6.15, SMI measured among subjects was having minimum value of 29 and maximum value of 60 with mean of 43.2±9.15. When Chi-square test was applied for SMI with MELD-Na, (p-value 0.003), Number of hepatic encephalopathy in past (p-value 0.004), HRS-AKI in past (p-value 0.005), 6min walk test (p-value 0.003).
Conclusion Sarcopenia is an important factor to determine risk of decompensation in patients with cirrhosis.
Keywords Sarcopenia, Skeletal muscle index, Model for end-stage liver disease
485
Development and validation of a digital health platform (IBD NutriCare) for telenutrition in patients with Inflammatory bowel disease
Arti Gupta , Namrata Singh, Divya Madan, Maryam Farooqui, Neha Singh, Mukesh Singh, Shubi Virmani, Mehak Verma, Aditya Bajaj, Manasvini Markandey, Bhaskar Kante, Sudheer Kumar, Peeyush Kumar, Pabitra Sahu, Govind Makharia, Saurabh Kedia, Vineet Ahuja
Correspondence – Vineet Ahuja - vineet.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences. Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi, Delhi 110029, India
Introduction Telenutrition with digital health platforms is the future step towards improving patient care in patients with inflammatory bowel disease (IBD). Additionally, it offers an advantage of conducting multicenter longitudinal dietary intervention studies.
Aim To develop and validate a digital health platform for patients with IBD to provide nutrition care and record longitudinal diet data on a large-scale basis.
Methods The development of the digital health platform was done from October 2019 -June 2021 by gastroenterologists and dieticians. For validation, patients with IBD at All India Institute of Medical Sciences, New Delhi recorded 7 days diet in the App. 24-hours diet recall for 3 days at random during the same week was also done. Energy, protein, carbohydrate, fat, fiber, cereals, fruits, vegetables, grain, legumes, milk products were compared between two methods.
Results An Android and iOS-based digital health platform, IBDNutriCare; was developed in English and 7 Indian languages. This user-friendly interface can be downloaded by the patients free of cost from Google store and App store. This platform provides a recording of diet variables based on 600 Indian food recipes, patient parameters like subjective global assessment, medications, and clinical activity scores. It also provides a graphical representation of nutrient analysis, with web applications generating comprehensive reports to enable large-scale data analysis. Forty-nine patients with IBD were enrolled in a validation study comparing :IBDNutricare; based analysis with dietary recall method. The mean intake of all food groups and macronutrients was comparable between the two methods. There was a significant interclass correlation (excellent for macronutrients and all food groups except vegetables (moderate, 0.79) and Bland-Altman plot analysis showed good agreement between the two methods.
Conclusion This study developed and validated a digital health platform for telenutrition in patients with IBD. This app helps in real-time tracking of dietary details and recording the data on a large scale.
Keywords Digital health platform, Telenutrtion, Inflammatory bowel disease, IBD, validation
Miscellaneous
486
Extra pulmonary manifestation of corona virus disease 2019 (COVID-19) i. e. gastrointestinal symptoms in COVID-19 received in OPD/IPD of Chugh multispecialty hospital – A single centric study
Mayank Chugh
Correspondence - Mayank Chugh - mayank19@yahoo.com
Department of Gastroenterology, Chugh Multispeciality Hospital, Meham Gate, Circular Road, Bhiwani 127 021, India
The virus that causes corona virus disease – 19 (COVID-19) is mainly transmitted through droplets generated when an infected person coughs, sneezes, or exhales. These droplets are too heavy to hang in the air, and quickly fall on floors or surfaces.
You can be infected by breathing in the virus if you are within close proximity of someone who has COVID-19, or by touching a contaminated surface and then your eyes, nose or mouth. COVID-19 affects different people in different ways. Most infected people will develop mild to moderate illness and recover without hospitalization.
The above statistics observed and drawn inferences as the out of 85 patients with gastrointestinal tract (GIT) symptoms in COVID symptoms the most common being the loose stools and nausea being the least one. Patients do have the combination of all also considered
COVID-19 presents with different kind of variation including pulmonary and extra pulmonary. The study conducted here from Mid-March to Mid-May received total 85 patients as shown in the data. The study comprises of all patients received in OPD and IPD during the period. The keynote message made from the study that the COVID in multivariate in different systems and gastrointestinal symptoms cannot be overlooked.
Keywords COVID-19, GIT, GUT
487
Liver angiosarcoma: Rare tumor associated with a poor prognosis- Case report
Sajith Sebastian, Sunil K Mathai, Jenny Roy1
Correspondence – Sajith Sebastian - gastroentrologistkerala@gmail.com
Department of Gastroenterology, M G M Muthoot Hospitals, 37/1546-A, Nethaji Nagar Road, Near Jawahar Nagar, Kadavanthra, Cochin, Kochi 682 020, India, and 1Department of Peridontology, Mount Zion Medical College, Near Jawahar Nagar, Kadavanthra, Near Jawahar Nagar, Kadavanthara 682 020, India
Angiosarcoma is an relatively rare tumor of mesenchymal origin affecting the liver, representing between 0.1% to 2% of all primary tumours of the liver. Angiosarcoma of liver affects mainly men in their sixth or seventh decade of life and carries a high mortality. No optimal treatment protocol and follow-up are yet available. Case reports of partial and total hepatectomy with neo adjuvant therapy are providing a fair survival in recent literature.
Presentation of Case A 42-year-old male, of south Indian origin living in Middle east presented with persistent high-grade fever for 2 months duration. He was diagnosed with IBS 20 years back with chronic diarrhea and was on follow-up. Investigations suggestive of a liver abscess like mass and was referred here for persisting fever despite multiple antibiotics. He was evaluated here and found to have a large liver mass with a consistency of abscess on imaging with underlying cirrhosis. Tumor markers and other sepsis and parasitic workup were negative, expect for elevated CRP. He was attempted liver aspiration which showed a blood admixture filled tissue.so further aspiration was deferred and sent for HPE, which showed prominent vascular channels with adjourning necrotic tissues. Repeat assessment and IHC with further imaging were suggestive of a primary angiosarcoma of the liver along with changes of cirrhosis. Liver cells were immunohistochemistry for neoplastic cells CD31 and CD34 were positive. Patient was deemed candidate for a partial hepatectomy and was referred to a transplant unit. He was started on reductive chemotherapy which showed only marginal benefit. In spite best efforts he succumbed to the illness within a month.
Conclusion Partial hepatectomy as surgical management, followed by adjuvant therapy, for liver angiosarcoma continues to prove favorable results and prognosis compared to liver transplantation.
Keywords Angiosarcoma, Liver abscess, Cirrhosis
488
Change in frequency of patients with presenting gastrointestinal tumors in last decade in tertiary cancer institute in North India
Pankaj Tyagi1, Pragya Shukla2, Mayur Churhe1
Correspondence – Pankaj Tyagi -drpankajtyagi@gmail.com
1Departments of Gastroenterology, and 2Radiation oncology, DSCI, Dilshad Garden, Delhi 110 095, India
Introduction Gastrointestinal (GI) malignancies are a big burden on the society and nation. With the increasing awareness, upcoming investigations and increase in number of the hospitals there is increasing number of the malignancy patients visiting the cancer institutes. Thus, we intend to see the change in number and frequency of the GI tumors in the span of last decade.
Methods Retrospectively we analyzed the frequency and the number of different tumors presenting to over tertiary cancer institute, that is Delhi state cancer institute. From the total tumor burden we also analyzed the respective GI tumors frequency and numbers. We took the patient load of 2012 and 2019.
Results Total number of the cancer patients who presented to our tertiary institute in 2012 year were 9327 out of which GI tumors were 1647 (17.6%). Out of 1647 all GI tumor esopahgus were 216, stomach 115, small intestine 17, colon 128, rectosigmoid 92, anal canal 39, hepatic 260, gallbladder 684 , biliary tract 37 and pancreas 84. In 2019 total number all cancer patients were 13864 out of which GI tumors were 1227 (8.8%). Out of 1227 all GI tumors esophagus was 215, stomach 115, small intestine 20, colon 116, rectosigmoid 144, anal 35, hepatic 152, gallbladder 340, biliary tract 30 and pancreas 60.
Conclusion Total number of patients presenting to our institute increased from 2012 to 2019 however there was decrease in frequency of the GI tumors from 2012 to 2019.
Keywords Frequency, Gastointestinal malignancy
489
Intestinal methanogenic overgrowth: A neglected microbiome
Arun Prasannan , L Venkatakrishnan, Mukundan Swaminathan, P Thirumal,R K Karthikeyan
Correspondence - Arun Prasannan - arunvani9496@gmail.com
Department of Medical Gastroenterology, PSG Institute of Medical Sciences and Research, Peelamedu, Coimbatore 641 004, India
Introduction Methanogenic small intestinal bacterial overgrowth (SIBO) has been renamed as intestinal methanogenic overgrowth. Methane production in human body is contributed predominantly by archae microbe Methanobrevibacter smithii. A methane producer is identified by detection of 10 ppm of methane anytime during lactulose breath test. Methanogenic SIBO population will be having mainly bloating, constipation and weight gain. Treatment of this SIBO will be combination of Rifaximin along with Neomycin or cyclical antibiotic therapy.
Methods Patients having symptoms of SIBO were evaluated with routine investigations, endoscopy and breath tests and breath test were analysed for methanogenic overgrowth.
Results In our study of 45 patients suspected to have SIBO, 34 patients had intestinal methanogenic overgrowth. Twenty-four patients had hydrogen producing SIBO and 23 had combination of M-SIBO and H-SIBO. Only one patient with positive hydrogen breath test didn’t have associated methanogenic bacterial overgrowth, rest all had. Predominant complaints associated with methanogenic SIBO was constipation (44%), bloating (37%), flatulence (19%). Three percent of M-SIBO had associated weight gain rather than weight loss commonly associated with malabsorption due to SIBO. When compared to H-SIBO, M-SIBO contributed to 75% of total SIBO population. Baseline methane level was elevated in 10 patients out of 34 M-SIBO patients.
Conclusion Incidence of methanogenic overgrowth is on rise in South Indian population. Baseline methane levels are high in 30% patients. Further studies are needed to validate a baseline methane level for Indian population. M-SIBO is equally as important as H-SIBO and should be given priority during breath test in Indian population and adequately treated.
Keywords SIBO, Methanogenic overgrowth, Breath test
490
Mechanical dysphagia from around the voice box: A case report
Shruti Sagar Bongu , Avinash Balekuduru
Correspondence - Shruti Sagar Bongu - sagar1292@gmail.com
Department of Gastroenterology, 3rd Floor, M S Ramaih Memorial Hospital, B E L M S Ramaiah Nagar, RIT Post, M S Ramaiah Nagar, Mathikere, Bengaluru 560 054, India
Introduction Posterior pharyngeal lesions constitute as one of the rare causes of dysphagia and we report a case of lethal midline granuloma presenting as dysphagia.
Case Report A 41 year old male, from middle-east without any comorbidities or addictions presented with painless progressive dysphagia to solids more than liquids and hoarseness of voice since 8 years. On examination, he was severely malnourished with severe muscle wasting. Inspiratory stridor, scarred palate and perforated anterior nasal septum were noted. All routine hematological, biochemical, virological and autoimmune investigations were normal. Nasopharyngolaryngoscopy showed scarred nasopharynx, floppy epiglottis and ankylosed cricoarytenoids. In view of stridor, computed tomography of neck and thorax were done which was not contributory. Endoscopy showed posterior pharyngeal wall ulceration and cricopharyngeal stricture which required balloon dilation (Fig. 1A, C). Rest of the esophagus, stomach and duodenum were normal. Biopsies were obtained from the posterior pharyngeal wall. He also had vocal cord palsy. A percutaneous endoscopic gastrostomy tube was placed to improve the nutrition status. He underwent tracheostomy to relieve frequent hypoxic episodes during his sleep. Histopathology showed nonspecific granulomatous tissue with sheets of lymphocytes. Immunohistochemistry (Fig.1D) revealed atypical lymphocytes positive for CD 20 and LCA markers and a diagnosis of lethal midline granuloma was made in consultation liaison with rheumatologist. He was started on prednisolone 1 mg/kg for 2 weeks, tapered over 8 weeks and maintenance therapy was given with Mycophenolate mofetil and hydroxychloroquine. He came for follow-up after 2 years with 11 kg weight gain, removal of tracheostomy tube and significant relief of dysphagia on MMF maintenance.
Conclusion Midline granuloma is an uncommon and rare etiology that needs to be considered in differential diagnosis for persistent dysphagia.
Keywords Dysphagia midline granuloma
491
A rare case of diarrhea-Case presentation
Sambit Bhuyan, K Muthukumaran, R Murali, K Premkumar, Caroline Selvi, A Aravind, A Chezhian
Correspondence - Sambit Bhuyan - rajubhuyan87@gmail.com
Institute of Medical Gastroenterology, Madras Medical College, Near Park Town Station, Park Town, Chennai 600 003, India
Clinical Summary A 42-year-old male presented with right upper quadrant non-colicky dull aching pain and loose stools i.e. small volume 8-10 episodes /day associated with blood in stool, not a/w urgency, tenesmus for last 3 months. He also compla ins of paresthesia and tripping of both feets during walking. He was diagnosed with bronchial asthma 1-year back. On examination vitals were stable, no pallor, no cyanosis, no clubbing, no lymphadenopathy. P/A examination was unremarkable except slight tenderness in right upper quadrant. On nervous system examination there was decreased sensation on lateral side of both lower limb and sluggish ankle reflex. On investigation Hb- 13.1 g/dL, TPC - 3.18 lakh/mm3 , TLC - 17000/ mm3, DC (N- 25,L -15, E-60) , AEC- 8100, ESR- 60 mm , Stool- pus cell- 2-4/HPF, RBC- 12-14/HPF. Other tests like RFT, LFT, serum electrolyte, thyroid profile were normal. Colonoscopy showed features of pancolitis, HPE- eosinophilic colitis, CT abdomen showed long segment circumferential wall thickening with submucosal edema with luminal narrowing involving ascending colon. Nerve conduction study - mononeuritis multiplex pattern with b/l asymmetric sensory motor neuropathy involving b/l common peroneal and b/l tibial nerve, HRCT thorax- patchy ground glass opacity likely indicating pulmonary infiltrate in Churg-Strauss syndrome, bone marrow study showed cellular narrow showing myeloid proliferation in all stages of maturation with increased eosinophilic precursors. Left sural nerve biopsy showed features of vasculitic neuropathy. ANA profile - normal, C ANCA – 80 (N < 5 mL). Final diagnosis eosinophilic granulomatosis with polyangitis, mononeuritis multiplex - vasculitic neuropathy with eosinophilic colitis.
Conclusion Eosinophilic granulomatous polyangitis can present with abdominal pain, vomiting and diarrhea. Small bowel most commonly involved followed by stomach and colon. Steroid is the treatment of choice.
Keywords Eosinophilic granulomatosis with polyangitis, Eosinophilic colitis, Eosinophilia
492
Abdominal tuberculosis diagnosis by colonoscopy
Mayank Maheshwari, A Anand, A R Akilandeswari, Kani Shaikh Mohammed
Correspondence - Mayank Maheshwari - maheshwari.mayank31@gmail.com
Department of Digestive Health and Diseases, Government Kilpauk Medical College, 822, Poonamallee High Road, Kilpauk, Chennai 600 010, India
Background Histopathological confirmation in abdominal tuberculosis is difficult due to suboptimal non-invasive access to the involved area. Colonoscopy provide semi-invasive access to the large intestine and ileocecal area. Information on the diagnostic yield of this investigation in abdominal tuberculosis is scarce.
Objective To evaluate the role of colonoscopy in the diagnosis of abdominal tuberculosis.
Methods Between October 2020 to October 2021, patients were diagnosed to have abdominal tuberculosis on the basis of colonoscopy. The case records of these patients were still retrospectively reviewed to assess the usefulness of colonoscopy in the diagnosis of abdominal tuberculosis.
Results Data for 65 consecutive patients in whom a diagnosis of intestinal tuberculosis was made during the last 1 year in hospital were reviewed. Clinical findings and the frequency of endoscopic findings were evaluated. Thirty patients had clinical symptoms (anorexia, abdominal pain and weight loss), 10 patients had only abdominal pain 10 patients had altered bowel habits, 10 patients had anorexia and 5 patients had no symptoms. Mucosal lesions were classified into 4 types: type 1, circumferential ulceration with nodules; type 2, round or irregularly shaped small ulcers, arranged circumferentially, without nodules; type 3, multiple erosions restricted to the large intestine; and type 4, small ulcers or erosions restricted to the ileum. The frequency of type 1, 2, 3, and 4 endoscopic findings was, respectively, 26,21 ;12 and 6 patients. The classical histological features are seen in only 15 patients (caseating necrosis, conglomerate epithelioid histiocytes, and disproportionate submucosal inflammation whereas presence of granulomas was seen in 50 patients.
Conclusion When colonoscopy is performed in patients, it is important to be aware of subtle endoscopic findings that are characteristic for intestinal tuberculosis. Recognition of such findings may lead to a correct diagnosis of early-stage intestinal tuberculosis.
Keywords Tuberculosis, Colonoscopy, Abdominal pain
493
Eosinophilic gastroenteritis – A case series
Parag Papalkar, B S Ramakrishna, D Babu Vinish, J Kayalvizhi
Correspondence - Parag Papalkar - parag_papalkar@yahoo.co.in
Department of Gastroenterology, S R M Institutes for Medical Science, No. 1, Jawaharlal Nehru Salai, Vadapalani, Chennai 600 026, India
Introduction Primary eosinophilic gastroenteritis (EGE) is an uncommon inflammatory disorder of the gastrointestinal tract. Clinical presentation depends on the segment and the layer of the gastrointestinal tract affected. We present a series of cases with EGE seen over the last four years in our hospital.
Method The case records of patients seen with EGE in our hospital were retrieved and the data analyzed.
Results Among 20 patients (females 10, median age 43.5 years) diagnosed with EGE, the presenting symptoms included abdominal pain (75%), diarrhoea (30%), weight loss (5%), vomiting (20%) and abdominal fullness (20%). The diagnosis was made by endoscopic biopsies in 19 patients and by surgical biopsy in one patient. The level of involvement included esophagus in one, stomach in five, small bowel in nine, large bowel in three, and ileocolonic in six patients. Blood tests showed peripheral eosinophilia in 13 cases. Biopsies showed eosinophil counts >50/high power field in nine patients with eosinophilic cryptitis and crypt abscesses in seven patients. IgE levels were elevated in four patients. There was no evidence of systemic involvement in most patients. Most common layer involved was mucosa while five patients had muscularis and three had serosal involvement. Most of the patients were treated successfully with tapering corticosteroids and montelukast.
Conclusions Diagnosing EGE requires a high index of suspicion and remains a diagnostic challenge for the clinician. EGE may mimic functional bowel disorders.
Keywords Eosinophilia, Abdominal pain, Corticosteroids
494
Upper gastrointestinal endoscopy finding in diabetic versus nondiabetic dyspeptic patients
Akshay Kodmalwar , A Anand, Akilandeshwari, N Arun, Kani Shaikh Mohamed
Correspondence - Akshay Kodmalwar - akshaykodmalwar19@gmail.com
Department of Digestive Health and Diseases, Government Kilpauk Medical College and Hospital, 822, Poonamallee High Road, Kilpauk, Chennai 600 010, India
Background and Aims This study aims to assess endoscopic findings in diabetic and non-diabetic patients presented with complaints of dyspeptic symptoms.
Methods This was a observational cross sectional study conducted in Department of Digestive Health and Disease over a period of 1 year. A total of 108 patients above the age of 18 years of which 54 patients diagnosed with DM, 54 patients with no DM with dyspeptic symptoms were included and underwent endoscopic examination of upper gastrointestinal system. Endoscopic findings of two groups were documented.
Results A total of 54 patients, 24 female and 30 male in the DM group, and 54 patients, 25 female and 49 male in the non-DM group, were included in the study. Findings in DM patients in decreasing order of frequency pangastritis 35, antral gastritis 18, esophagitis 17, gastric ulcer 5, duodenal ulcer 2, duodenitis 3, hiatus hernia 2, LES dysfunction 1. Findings in non DM patients in decreasing order of frequency pangastritis 30, antral gastritis 18, esophagitis 17, gastric ulcer 2, duodenal ulcer 2, duodenitis 1, hiatus hernia 2, LES dysfunction 5. Findings such as pangastritis, gastric ulcer, duodenitis were more common in diabetic patients compared to non-diabetics. This difference was statistically significant (p=0.027).
Conclusion When Endoscopic findings in patients with dyspeptic complaints were analyzed, significant difference was found between the diabetic and non-diabetic groups in terms of endoscopic findings like gastric ulcer, pangastritis, duodenitis (more common in DM).
Keywords Diabetic Nondiabetic Endoscopy
495
Spontaneous hemoperitoneum in a case with Factor XIII deficiency: Resolved with conservative management
Venkatakrishnan Iyer 1 , Nidhi Vasani 2 , Chirag Nayak 3
Correspondence - Venkatakrishnan Iyer - vhiyer78@gmail.com
Departments of 1Gastroenterology, and 2Obstetrics, Gynecology and IVF Sahaj Gastro Care and Sarjan Fertility Centre. Bhavnagar 364 002, India, and 3Radiology Department, Nityam Radiodiagnostic Clinic, Samved Complex, Jail Road, Bhavnagar 364 002, India
We report a case of a 22-year-old female with a rare coagulation disorder, who presented to us with spontaneous hemoperitoneum, which resolved with conservative management.
A 22-year-old female, a known case of Factor XIII (Fibrin Stabilizing Factor) deficiency presented to us with abdominal pain since 5 days. Pain was mild to moderate, constant, non-colicky and not related to food. She had no history of trauma over abdomen. On evaluation, hemoglobin was 5.4 g%. Platelet count, PT, and aPTT were normal. A CT abdomen was suggestive of hemoperitoneum without any laceration of internal organs.
In her early childhood, she had bled profusely from the umbilicus after trauma. A surgeon took sutures on the umbilicus, but the bleed worsened. On evaluation by hematologist then, a urea solubility test was positive, confirming factor XIII deficiency. Urea solution will dissolve a clot, if the clot contains fibrin monomers. But cross-linked fibrin will not dissolve in urea.
This spontaneous hemoperitoneum was probably due to ovulation. The corpus luteum cyst generally stops bleeding in normal individuals but in Factor XIII deficiency the fibrin clot is formed, but cross linking is not possible without factor XIII. Failure of secondary hemostasis, leads to late bleeding, causing hemoperitoneum.
Factor XIII has a long half-life (3-4 weeks). Fresh frozen plasma or cryoprecipitate concentrate is indicated as treatment. Corifact (FXIII Concentrate) is FDA approved in USA, but unfortunately is not available in India. We treated her with blood transfusion and 2 mL/kg of FFP. We repeated the same dose every monthly for 3 months.
For 3 months, she was started on continuous oral contraceptive pills to avoid ovulation. At the end of 3 months, a repeat CT imaging confirmed the resolution of hemoperitoneum.
Thus, this patient with spontaneous hemoperitoneum, resolved with conservative management.
Keywords Factor XIII deficiency, Spontaneous hemoperitoneum, Fresh frozen plasma
496
Alopecia totalis as an early manifestation of Azathioprine induced myelosuppression – A case report of auto immune hepatitis with NUDT15 mutation
Maitrey Patel , Aastha Jha, Apurva Shah, Shravan Bohra
Correspondence - Maitrey Patel - ptlmaitrey@gmail.com
Department of Medical Gastroenterology, Apollo Hospital International Limited, Plot No. 1A, Gandhinagar, Ahmedabad Road, GIDC Bhat, Ahmedabad 382 428, India
Azathioprine (AZA) is used for various autoimmune, inflammatory conditions and prevention of transplant rejection. AZA induced myelosuppression is dose dependent and life threatening if not identified earlier. Mutations in the genes thiopurine S-methyltransferase (TPMT) and nucleoside diphosphate-linked moiety X-type motif 15 (NUDT15) have been identified to predispose to severe myelosuppression with AZA. We report case of a 41-year old woman with history of hypothyroidism, diagnosed as autoimmune hepatitis (AIH) in June 2021 and started on AZA 50mg per day with prednisolone 40 mg/day with tapering dose on 28th June 2021. On 2nd August 2021 she presented with hair loss, sore throat, weakness and malaise since one week. On examination she had alopecia totalis. On evaluation she found to have myelosuppression (Hb 10.1 gm/dL, total count 2402 (absolute neutrophil count 216), platelet count 234200, with normal biochemical investigations and throat swab cultures. In view of myelosuppression, AZA was kept hold and low dose steroid omnacortil 10 mg/day was continued. After 5 days she had fever so empirical antibiotics (meropenem, amikacin and fluconazole) was started as per hematologist advise. Her neutropenia was worsening as mentioned in investigation chart and she was started on granulocyte colony stimulating factor. Her genetic testing for NUDT 15 *2 or *3 (c415C>T) heterozygous detected and No TPMT mutation detected. Gradually she was improving clinically and her leukopenia improved but thrombocytopenia persisted and for same she was evaluated by bone marrow study, Immunoglobulin profile and anti PF 4 antibodies which were normal and treated with Romiplostim. To conclude simple clinical clue such as alopecia can be a predictor of severe myelosuppression in patients on AZA apart from regular hemogram (as mentioned in Table 1). Further it is important to look for NUDT15 mutation apart from TPMT in patients before starting AZA in Indian population.
Keywords Azathioprine toxicity, Myelosuppression, NUDT 15, TPMT, Alopecia
497
Upper gastrointestinal endoscopy findings in diabetic versus nondiabetic dyspeptic patients
Akshay Kodmalwar, A Anand, A R Akilandeshwari, N Arun, Kani Shaikh Mohamed
Correspondence - Akshay Kodmalwar - akshaykodmalwar19@gmail.com
Department of Digestive Health and Diseases, Government Kilpauk Medical College and Hospital, and CRRI Gents Hostel, Government Kilpauk Medical College and Hospital, Chennai 600 010, India
Background and Aims This study aims to assess endoscopic findings in diabetic and nondiabetic patients presented with complaints of dyspeptic symptoms.
Methods This was a observational cross sectional study conducted in Department of Digestive Health and Disease over a period of 1 year. A total of 108 patients above the age of 18 years of which 54 patients diagnosed with DM, 54 patients with no DM with dyspeptic symptoms were included and underwent endoscopic examination of upper gastrointestinal system. Endoscopic findings of two groups were documented.
Results A total of 54 patients, 24 female and 30 male in the DM group, and 54 patients, 25 female and 29 male in the non-DM group, were included in the study. Findings in DM patients in decreasing order of frequency pangastritis 35, antral gastritis 18, esophagitis 17, gastric ulcer 5, duodenal ulcer 2, duodenitis 3, hiatus hernia 2, LES dysfunction 1. Findings in non DM patients in decreasing order of frequency pangastritis 30, antral gastritis 18, esophagitis 17, gastric ulcer 2, duodenal ulcer 2, duodenitis 1, hiatus hernia 2, LES dysfunction 5. Findings such as pangastritis, gastric ulcer, duodenitis were more common in diabetic patients compared to non-diabetics. This difference was statistically significant (p=0.027).
Conclusion When endoscopic findings in patients with dyspeptic complaints were analyzed, significant difference was found between the diabetic and non-diabetic groups in terms of endoscopic findings like gastric ulcer, pangastritis, duodenitis (more common in DM).
Keywords Diabetic nondiabetic endoscopy
498
Anorexia nervosa – Atypical eating disorder in an adolescent male
Maitrey Patel, Apurva Shah, Shravan Bohra, Aastha Jha
Correspondence - Apurva Shah – apurvashah411@gmail.com
Department of Medical Gastroenterology, Apollo Hospital International Limited, Plot No. 1A, Gandhinagar, Ahmedabad Road, GIDC Bhat, Ahmedabad 380 015, India
Anorexia nervosa is an eating disorder characterized by excessive restriction on food intake and irrational fear of gaining weight, often accompanied by a distorted body self-perception. We report a case of 15-year-old male who presented with complaints of anorexia, postprandial abdominal pain, constipation, insomnia and weight loss of 10 kilograms since two years. On examination, BMI was 12 kg/m2. No signs of malabsorption were present he looked cachectic, emaciated with prominent maxillary prominences (Fig. 1). Systemic examination was unremarkable, his all blood investigations were within normal limits except mild iron deficiency anaemia Hb 11.9 gm/dl and low vitamin D3 24.6. Other investigations for weight loss evaluation like CRP, ESR, TSH, cortisol, growth hormone, testosterone, HIV, renal function test, liver function test, ANA were within normal limits. Antibody to tissue transglutaminase and anti endomysial antibody were negative. Gastroscopy, full colonoscopy, CXR, CT abdomen and ECG were within normal limits. After excluding all organic causes, we discussed with his parents, his father gave history that since last two years he is insisting on eating less he is getting irritated and short tempered. So multidisciplinary approach was considered he was diagnosed as atypical eating disorder of anorexia nervosa, he was started on olanzapine, fluoxetine, and daily counselling. He was hospitalized for 5 days and slowly his diet and calorie intake were increased under observation he was observed for refeeding syndrome by monitoring electrolytes. On follow-up after 6 months, he gained weight approximately 20 kilograms to 35 kilograms, BMI 18 kg/m2, he was now cheerful, having good appetite and taking parts in all sports in school (Fig. 2). By reporting this case we want to create awareness among doctors which help in early diagnosis of eating disorder and prevent unnecessary investigations.
Keywords Anorexia nervosa, Atypical eating disorder, Adolescent
499
Visceral artery aneurysms/pseudoaneurysms–An Indian gastroenterologists’ perspective
Mit Shah , Shamshersingh Chauhan, Vikas Pandey, Vikramaditya Rawat, Chintan Tailor, B Kiran, Chaitanya Atre, Gaurav Singh, Vivek Ukirde, Meghraj Ingle
Correspondence – Meghraj Ingle - drmeghraj@gmail.com
Department of Medical Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai 400 022, India
Introduction To evaluate the etiology, presentation, risk factors for rupture, management, and outcomes at 1 month in a tertiary care center for mesenteric aneurysms and pseudoaneurysms.
Methods We performed retrospective analysis of data from 2017-2021 at a tertiary care centre in Western India of all the patients who were diagnosed with mesenteric aneurysms and pseudoaneurysms.
Results Fifty-seven aneurysms and 48 pseudoaneurysms in 74 patients were studied. The most commonly involved vessels were splenic artery (69.5%) and gastroduodenal artery (GDA) (17.1%). About 75.6% patients were symptomatic, 51.3% had gastrointestinal bleeding (GI bleeding) and 24.3% abdominal pain. The most common etiologies noted were - chronic pancreatitis (35.1%) and decompensated cirrhosis (20.1%). Almost all patients with pseudoaneurysms were symptomatic (p<0.0001). True aneurysms were more likely to be multiple, as compared to pseudoaneurysms (1.84+1.93 vs. 1.12+0.32; p=0.009). There was no significant difference in mortality and rebleed at one month between aneurysms and pseudoaneurysms (p=0.4887 and p=0.873). Male patients were found to have a higher risk of GI bleeding, irrespective of etiology (p=0.006), whereas female patients were more likely to have complications post intervention (p=0.04). Interventional radiology guided treatment was offered in the form of angiographic coiling (40.5%), angiographic glue injection (17.6%) and angiographic glue+coiling respectively (5.4%). There was no significant difference between the risk of rebleeding or mortality amongst the modes of interventional therapy. Four percent patients died due to aneurysm rupture or rebled post intervention. Size >2 cm did not correlate with GI bleeding or hemodynamic instability. Around 8.1% patients had complications post intervention, most common being Gram negative septicemia; all managed medically with no mortality and were commonly seen with interventions relating to the splenic artery.
Discussion Pseudoaneurysms must be treated. Radiological intervention in form of coil or glue is safe and effective.
Keywords Visceral artery aneurysms, Pseudoaneurysms
500
Vaccination status of patients with inflammatory bowel disease
Sumanth Koppolu , Ebby George Simon, Amit Kumar Dutta, A J Joseph, Amit Kumar Dutta. A J Joseph, Sudipta Dhar Chowdhury, Rajiv Zachariah 1
Correspondence - Sumanth Koppolu - sumanthgmc@gmail.com
Department of Gastroenterology, and 1Well Baby Clinic, Child Health-Unit 1, Christian Medical College, Vellore 632 002, India
Background and Aim Patients with inflammatory bowel disease (IBD) are at increased risk for infections owing to altered cellular and humoral immunity. Predisposing factors include age, co-morbidities, protein energy malnutrition, use of immunosuppressive medications and surgery. Various vaccine preventable diseases in IBD can be avoided by administration of the concerned vaccines. There is limited information on vaccination status in patients with IBD. We aimed to assess vaccination status in this population for the recommended vaccines.
Methods IBD patients aged greater than 18 years and fulfilling inclusion criteria were included in the study after taking informed consent. We utilized a questionnaire to capture patient data which was subsequently analyzed. The prevalence of the recommended vaccines and reasons for not adhering to the vaccination schedule were assessed.
Results Eighty-nine IBD patients were recruited, of which 44 (49%) patients had ulcerative colitis and 45 (51%) had Crohn’s disease. Forty-five (51%) patients were on immunomodulators. Sixty-five (73%) patients were unvaccinated, 24 (27%) were partially vaccinated while only 4 (4.5%) completed the recommended vaccine schedule. Lack of knowledge (59.2%) and financial reasons (43.5%) were the most common reasons for non-adherence to the vaccine schedule.
Conclusion Vaccination appears to be underutilized in our IBD population. More effort needs to be taken to motivate these patients to get vaccinated and thereby reduce the risk of preventable diseases.
Keywords Vaccination, IBD, Immunosuppression
501
Rare cause of severe diarrhea in a post-corona virus disease patient
Deepanshu Khanna , Subhashish Mazumdar
Correspondence - Deepanshu Khanna - drdeepanshukhanna@gmail.com
Department of Gastroenterology, Max Superspeciality Hospital, Sector 1, Vaishali 201 012, India
MIS-A first came to light in June 2020, when the CDC received reports of patients with delayed and multi-systemic illness involvement, with a clinical history that resembled multisystem inflammatory syndrome in children (MIS-C). This report presents a case of MIS-A in which the patient presented with severe diarrhea eight weeks after first being exposed to corona virus disease 2019 (COVID-19). Her clinical history was consistent with the CDC's working description of MIS-A. Clinical recovery was achieved with aggressive supportive treatment in the intensive care unit, the use of temporary cardiac pacing, and immunomodulatory therapies (steroids, intravenous immunoglobulin). More research is required on treatment modalities and clinical predictors of MIS-A.
Keywords MIS-A, Diarrhea, Post COVID Complication
502
To study the clinical profile, risk factors and treatment outcomes of Clostridoitis difficile associated diarrhea. An observational retrospective study in a tertiary hospital from western India
Harshal Gadhikar1, Hameed Raina1, Sampada Patwardhan2, Ashish Gandhi1, Prayag Parikshit3, Amol Bapaye4, Sanjana Bhagwat1
Correspondence - Harshal Gadhikar - gadhikarhp@gmail.com
Departments of 1Gastroenterology, 2Microbiology, 3Infectious disease, 4Gastroenterology and Endoscopy, Deenanath Mangesh Hospital and Research Centre, Erandwane, Pune 410 004, India
Background and Aims Clostridoitis difficile is recognized globally as an important enteric pathogen associated with considerable morbidity and mortality. We have been experiencing increasing incidence of Clostridoitis difficile associated diarrhea (CDAD) in our hospital. To evaluate the same, we took up this study.
Methods All adult patients of diarrhea, who presented to our hospital for last six months and whose samples were sent for stool testing for Clostridoitis difficile were included in the study. All demographic and clinical profile, possible risk factors and treatment response were evaluated. Clostridoitis difficile associated diarrhea (CDAD) was confirmed with detection of Toxin A or B or both with ELISA technique.
Results Total of 255 patients with diarrhoea were studied. The prevalence of only toxin positive cases was 22.35% (57/255) and only glutamate dehydrogenase (GDH) antigen positive cases was 7.45% with an overall prevalence of 29.8 %. Nosocomial infection, community acquired and hospital associated comprised of 59.64% 35.08% and 5.28%, respectively. Multivariate analysis revealed that recent antibiotic use (cephalosporins and carbapenems), PPI use more than 5 days, steroid use more than 2 weeks, ICU stay and chemotherapy were independent risk factors associated with CDAD. Nasogastric intubation was observed to be a protective factor against CDAD. Response rates to vancomycin and metronidazole were 85.94%. Non-responders were treated with teicoplanin with response rate of 62.54%. Fecal microbiota transplant (FMT) was done in 3 patients, and all responded to it. The recurrence rate of CDI was 7.01%. Thirty-day mortality rate was 3.5%.
Conclusion CDAD is one of the main causes of acute diarrhea, including in the community set up. PPIs, antibiotics, chemotherapy agents, steroids and ICU stay are the main risk factors for CDAD. Vancomycin and metronidazole are good first line treatment options for CDAD. Teicoplanin or FMT can be used in unresponsive cases.
Keywords Clostridoitis difficile infection, C. difficile toxin A and B, Vancomycin, Metronidizol
503
Overweight and obesity is as frequent as underweight in Indian patients with inflammatory bowel disease
K J Umesh, Amit Kumar Dutta, Ajith Thomas, Anoop John, Rajeeb Jaleel, Sudipta Dhar
Chowdhury, Ebby George Simon, A J Joseph
Correspondence - Umesh K J - akdutta1995@gmail.com
Department of Gastroenterology, Christian Medical College, Williams Building, Ida Scudder Road, Vellore 632 004, India
Introduction Malnutrition and low body weight are frequently observed in inflammatory bowel disease (IBD), especially Crohn’s disease (CD). However, data on frequency of overweight/obesity IBD is limited from India. We aimed to assess the frequency of overweight/obesity in Indian patients with IBD and determine its associations with disease characteristics.
Methodology The case records of patients with CD or ulcerative colitis (UC) seen in the out-patient department were retrospectively reviewed. The type of IBD (CD or UC) and clinical details including body mass index (BMI) were recorded on a structured form. The value of BMI was categorized into three groups according to the Asian-Pacific classification: Underweight (<18.5 kg/m2); Normal weight (18.5–22.9 kg/m2); Overweight/obese (>23 kg/m2). Complicated disease behaviour in CD was defined as structuring (B2) and/or penetrating (B3) and/or perianal disease (P). Statistical tests were done to assess for associations and p value of <0.05 was considered significant.
Results The study included 230 patients with IBD (Mean age 37.5+12.2 years, males 62.2%). 122 had CD (Mean age 37.1+13.2 years, males 63.8 % ) and 108 had UC (Mean age 37.9+11 year, males 60.2 %). Overall, 31.30 % (95% CI 25.7 – 37.6) of IBD patients were overweight/ obese and 28.7% (95% CI 23.2 - 34.9) patients were underweight, suggesting a similar frequency for both categories. 35.6% women were overweight/obese compared to 28% men with IBD (p=0.28). On evaluation of relationship with disease type, overweight/obesity was present in 35.18% patients with UC and 27.86% patients with CD (Fig. 1). This difference was not significant statistically (p=0.29). Complicated disease behavior was noted in 53.3% of patients with CD and was not associated with overweight/obesity (p=0.43).
Conclusion About one-third of patients with IBD are overweight/obese which is similar to the frequency of underweight patients. Overweight/obesity is frequent in both UC and CD.
Keywords Inflammatory bowel disease, Underweight, Obesity
504
A rare case of melioidosis presenting as splenic abscess
K H Vinod Gowda 1 , Mallikarjun Patil 1 , Harshad Devarbhavi 1 , Teena Thomas 2 , Mary Dias
Correspondence - Vinod Gowda K H - vinodgowdakh@gmail.com
Departments of 1Gastroenterology, and 2Microbiology, St. John’s Medical College Hospital, Sarjapur Main Road, Bengaluru 560 034, India
Introduction Melioidosis is a systemic infectious disease caused by Burkholderia pseudomallei. Diabetes, renal disease, thalassemia, and occupational exposure to environmental contaminants are some of the risk factors for severe melioidosis. Splenic abscess is very rare, with only a few reports in the literature. We are reporting a case of splenic abscess due to B. pseudomallei infection.
Case Report A HbE thalassemic 60-year-old male farmer from West Bengal with a past history of cholecystectomy in 2014 presented to our OPD with left upper abdominal pain, on and off fever and 20 kg weight loss since 2015. Patient had received multiple courses of antibiotics and also empirical ATT of 6 months with no improvement in symptoms. Abdominal examination revealed nontender moderate splenomegaly. Laboratory investigations revealed microcytic hypochromic anemia with hemoglobin-7g/dL. CECT abdomen showed splenomegaly with splenic and peri-splenic abscesses,17 mm in maximum width. USG guided peri-splenic abscess aspirate showed pus with total counts >1.0 lakh/mL, predominantly neutrophilic (78%). Aspirate culture grew Burkholderia pseudomallei sensitive to ceftazidime and cotrimoxazole. The patient was treated with ceftazidime intravenously for 14 days and discharged with oral cotrimoxazole for a duration of 3 months. Patient was afebrile after 2 days of starting ceftazidime.
Discussion Clinical manifestations of melioidosis include septicaemia, community- acquired pneumonia localized soft tissue lesions and visceral abscesses. Affected patients usually have well-known predisposing factor. Pre-existing thalassemia and wound inoculation during previous surgery could have hypothetically contributed to melioidosis in our patient.
Conclusion B pseudomallei is a potential causative organism of splenic abscess in patients with risk factors who reside in endemic areas. A high index of suspicion is needed for diagnosis due to its varied clinical presentations. Isolation of organism from the infection site is the only diagnostic method for visceral abscess melioidosis. Appropriate antibiotics and abscess drainage contributes to a successful outcome.
Keywords Melioidosis, Burkholderia pseudomallei, Splenic abscess
505
A retrospective analysis of percutaneous endoscopic gastrostomy at tertiary care center
Khwaja Aminoddin Siddiqui , Vaibhav Somani, Niranjan Banka, Noopur Mehta, Vishal Shriwastav, Viral Surani
Correspondence - Khwaja Aminoddin Siddiqui - siddiqui.amin@yahoo.com
Department of Gastroenterology, Bombay Hospital and Institute of Medical Sciences, 12, Vitthaldas Thackersey Marg, New Marine Lines, Marine Lines, Mumbai 400 020, India
Introduction Percutaneous endoscopic gastrostomy (PEG) tube is an endoscopic procedure for enteral nutrition in patients unfit for per oral feeding. Indications of PEG tube include neurological conditions compromising swallow mechanism like stroke, in some post craniotomy cases, dementia etc. It is also done for maintaining nutrition in elderly debilitated individuals and in rarer instances, gastric decompression in gastric volvulus.
Methods This was a retrospective analysis of a prospectively maintained data. We report the data from 01/01/2018 till 31/08/2021 of PEG tube insertion done in our center. Contraindications like active systemic infection, ascites, hemodynamic instability and bleeding diathesis were ruled out before patient selection. Written informed consent was obtained. Anticoagulants were stopped 12 hours prior to procedure. Patients were administered intravenous antibiotic Ceftriaxone 1 g 12 hours prior to procedure and post-procedural 12 hourly for 48 hours. PEG tube was placed using “pull” through technique. PEG tube feeding was started 3 hours after the procedure, and 360-degree counter-rotation manoeuvre was done 12 hours after procedure. Pre-existing PEG tube were changed if the tube was blocked or kinked after prolonged use.
Results Total 88 patients underwent PEG tube insertion. Out of which, 75 were first time procedures and in 13 patients, change of pre-existing PEG tube was done from same stoma. In one patient (1.13%), PEG tube had to be removed because of stoma site infection and peritonitis. Two patients developed buried bumper syndrome (2.27%) eight- and 10-months post-procedure, for which PEG tube was changed from the same stoma site after removal of previous tube using snare polypectomy forcep.
Conclusions PEG is a therapeutic procedure with high utility in maintaining enteral nutrition of patients unfit for per oral enteral feeds or requiring prolonged nasogastric feeds. Complication rates are low if done with all precautions and good care of stoma.
Keywords Pull through technique, Endoscopy, Buried bumper syndrome
506
Effect of SARS–CoV-2 pandemic on gastrointestinal endoscopy procedures - An experience from tertiary care centre of eastern India
Saumyaleen Roy , Ravikant Kumar, Sanjeev Kumar Jha, Vishnu Mohan Dayal, Ashish Kumar Jha
Correspondence - Saumyaleen Roy - saumyaleenroy1987@gmail.com
Department of Gastroenterology, Indira Gandhi Institute of Medical Sciences, Sheikhpura, Patna 800 014, India
Introduction To contain the spread of infection and reduce the burden on healthcare infrastructure, many countries all over the globe adopted lockdown strategy for SARS–CoV-2 pandemic. Hospitals were converted to dedicated corona virus disease 2019 (COVID-19) centers and all the non-COVID patients were intervened on triage basis, and only the emergency procedures were performed.
Methods Data related to clinical profile, indication and endoscopic procedure performed in reverse transcription polymerase chain reaction (RT-PCR) negative patients with use of personal protective kits in the Department of Gastroenterology, IGIMS, Patna, Bihar from March 25 to September 30th, 2020, were retrieved, analyzed and compared with the historical control (25th March – 30th September 2019).
Results A total of 2282 patients were admitted, and 391 procedures were carried out with an interventional rate of 17.14%. The most common procedure was upper gastrointestinal endoscopy (228, 58.13%) followed by endoscopic retrograde cholangiopancreatography (88, 22.50%). Seventy-five patients (19.20%) underwent colonoscopy/sigmoidoscopy. Chronic liver disease (144 pts) followed by malignancy (111 pts) were the commonest diagnosis. 1st phase of lockdown (March to May) only 41 procedures were performed (41 vs. 506). None of the patients undergone endoscopic ultrasound. During the same time frame in 2019, 4501 patients were admitted, and 1224 procedures carried out with interventional rate of 27.19 (p<0.0001). None of the staff of Gastroenterology Department developed symptomatic SARS-CoV-2 infection during this period.
Conclusion There were significant drop in endoscopic procedures during lockdown period and most of the esophagoduodenoscopy were done for chronic liver disease and ERCP for biliary tract malignancy. Endoscopic procedures done on RT-PCR for nCoV -2019 negative patients were safe using personal protective kits.
Keywords COVID-19, Endoscopy, Lock down; Pandemic
507
Portal vein thrombosis, mesenteric artery thrombosis with corona virus disease 2019 pneumonia: An under diagnosed and under reported Covid complication
Vijay Sharma, Richa Sharma
Correspondence – Vijay Sharma - vijaysadashiv@gmail.com
Department of Gastroenterology, Regional Institute of Health Medicine and Research, Jaipur 302 016, India
Corona virus causes severe pneumonia in 5% cases rarely gastrointestinal (GI) problem, we present case series.
Forty-nine male corona virus disease 2019 (COVID-19) pneumonia acute abdomen, WBC increased, D-dimer high, CT angiography abdomen superior mesenteric vein thrombosis, dilated inflamed jejunal ileal bowel loops, started on LMW heparin supportive care, recovered.
Sixty-two years old obese, diabetic hypertensive male with severe covid, acute abdomen. CECT abdomen thrombosis of superior mesenteric artery, D-dimer high Injection Alteplase, injection Enoxaparin expired.
Twenty-eight years female COVID-19 presented with acute abdomen, D-dimer 15 ng/mL, CECT abdomen confirmed portal vein thrombosis. managed with enoxapain and supportive treatment, recovered well.
Thirty-seven-year-old male alcoholic liver Covid pneumonia, Covid toe, abdominal distension. Abdominal Doppler confirmed portal vein thrombosis, D–dimer 9500 ng/mL. Started on steroid, anticoagulant improved well clinically, recovered started on oral feed but developed gross GI bleed, cardiogenic shock expired.
One male 55-year-old with h/o covid pneumonia 5 months back presented with acute abdomen on CECT abdomen PV and PMV thrombosis diagnosed, D-dimer 4750 ng/mL, started on anticoagulant, conservatively managed.
Thrombosis in COVID-19 is due to endothelial injury by acute phase reactants, activation of tissue factor pathway, excess thrombin fibrin generation, fibrinolysis shutdown. We are first from India to reports two cases with portovein thrombosis, one case each with SMV and SMA thrombosis. We could save two young cases with low D-dimer and less severe Covid pneumonia and no comorbidities.
COVID-19 can cause portal vein and SMA thrombosis, patient may present with GI emergency, awareness of these complication and timely therapy can save lives.
COVID-19 induced procoagulant state can cause mesenteric artery and portal vein thrombosis, purpose of this case series is to increase awareness and diagnosis of this complication in cases with acute abdomen for timely intervention parallel to respiratory support.
Keywords Postal vein thrombosis, Mesenteric artery thrombosis, Covid, Acute abdomen
508
The role of Fibroscan in predicting the risk of variceal bleed in patients with cirrhosis
Harinder Chhabra, Sandeep Gopal, B V Tantry, Suresh Shetty, Anurag Shetty
Correspondence - Harinder Chhabra - harinder.singh.chhabra@gmail.com
Department of Medical Gastroenterology, Kasturba Medical Ccollege Hospital, Ambedkar Circle, Mangalore 575 001, India
Background and Study Aim Variceal bleeding is a life-threatening event that has an incidence of 5% and 15 % in patients with small and large esophageal varices respectively. Endoscopic screening for esophageal varices in cirrhotic patients is mandatory. The aim was to study the role of liver stiffness measurement (LSM) and spleen stiffness measurement (SSM) in predicting the risk of variceal bleed in patients with cirrhosis.
Methods Single centre longitudinal study conducted on chronic liver disease patients (CLD) who underwent fibroscan over a period of 12 months from October 2020 to October 2022. A total of 70 patients were included in this study. LSM and SSM values of cirrhotics with history of UGI bleed (cases) were compared to those without any history of UGI bleed (controls).
Results The median LSM value in controls was 34.8 kpa and in cases was 37.6 kpa. The median SSM value in controls was 41.4 kpa and in cases was 59.5 kpa. The median values of LSM in CLD patients with no varices, grade 1, grade 2 and grade 3 varices were 25.1 kpa, 27.2 kpa, 33.5 kpa and 34.4 kpa respectively. The median values of SSM in CLD patients with no varices, grade 1, grade 2 and grade 3 varices were 34.3 kpa, 34.8 kpa, 51 kpa and 59.4 kpa respectively.
Conclusions This study shows that LSM and SSM values were higher in CLD patients with UGI bleed. SSM values are better correlated with UGI bleed. LSM and SSM values increase as the grade of varices increase in CLD patients. However, it is not reliable enough to replace gastroscopy to know the grade of varices.
Keywords Fibroscan, Liver stiffness measurement, Spleen stiffness measurement, UGI bleed, Esophageal-varices
509
An association between azathioprine induced pancreatitis in patients with inflammatory bowel disease and HLA -DQA1*02:01–DRB1*07:01: A retrospective stud
B Rajeshwari1, Anand Deshpande1, J Suchita2, Devendra Desai3
Correspondence - Devendra Desai - devendracdesai@gmail.com
1Department of Blood Bank and HLA Laboratory, 2HLA laboratory, and 3Medicine-Gastroenterology, P D Hinduja Hospital, Veer Savarkar Marg, Mahim, Mumbai 400 016, India
Background Azathioprine (AZA)-induced pancreatitis is an unpredictable and dose independent adverse event affecting 2% to 7% of patients with inflammatory bowel disease (IBD) patients treated with AZA. There are no test in clinical practice to identify individuals at risk of developing pancreatitis on exposure to Aza. An association of HLA -DQA1*02:01–DRB1*07:01 with azathioprine induced pancreatitis has been described in the western literature. In this pilot study, we analysed this HLA association with the risk of development of pancreatitis.
We studied an association between azathioprine induced acute pancreatitis in patients with IBD and HLA -DQA1*02:01–DRB1*07:01.
Methods In this retrospective study patients who were diagnosed with IBD and developed azathioprine induced pancreatitis were recruited. Between the period 2005 and 2021 total of 1412 patients were diagnosed to have IBD and of these 222 received azathioprine and 11 patients developed pancreatitis. Risk factors for pancreatitis such as smoking, alcohol intake, steroid administration, previous history pancreatitis and duration of azathioprine intake were analysed in these patients.
Results Out of 11 patients who developed azathioprine induced pancreatitis, 10 underwent HLA typing after written informed consent. Of these 10 patients 8 had HLA association with HLA-DQA1*02–DRB1*07 (positive prevalence of 80%). Only one patient had history of smoking, and none had alcohol intake. All of them were on steroid at the time of azathioprine induction. These patients developed pancreatitis within 2 to 28 days after taking azathioprine. None had a history of pancreatitis in the past. Re-challenge in one patient resulted recurrent episode of pancreatitis.
Conclusions There was significant association between azathioprine induced pancreatitis and class II HLA -DQA1*02 –DRB1*07. Additional studies are needed to decide if pre-emptive HLA typing canminimize the risk of developing pancreatitis.
Keywords Immunomodulator, Pancreatitis, HLA typing
510
Similar risk of infection with SARS-CoV-2 in immunocompromised and immunocompetent patients with inflammatory bowel disease and healthy controls
Bhaskar Kante, Sudheer Kumar Vuyyuru, Ritu Gupta1, Tanima Dwivedi2, Peeyush Kumar, Sandeep Kumar Mundhra, Rithvik Golla, Shubi Virmani, Mehak Verma, Govind Makharia, Vineet Ahuja, Saurabh Kedia
Correspondence – Saurabh Kedia - dr.saurabhkedia@yahoo.com
Departments of Gastroenterology, 1Laboratory Medicine, and 2Laboratory Oncology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, Ansari Nagar East, New Delhi 110 029. India
Background The information on seroprevalence rates of corona virus disease 2019 (COVID-19) infection among patients with inflammatory bowel disease (IBD) and its comparison to healthy controls is sparse. We compared the seroprevalence rates in immunocompromised and immunocompetent IBD patients and healthy controls.
Methods Patients with IBD under follow-up at the IBD clinic, All India Institute of Medical Sciences, New Delhi, were included. After obtaining informed consent, patients underwent SARS-CoV-2 antibody testing (chemiluminescent immunoassay: Seimens kit IgG against antigen S1RBD) and information on demography, drug history, past history of COVID infection and vaccination status were noted. Patients with IBD on 5-aminosalicylic acid or not on any treatment were considered immunocompetent and those who had received steroids, thiopurines or methotrexate within 6 months of sample collection were considered immunocompromised.
Results Two hundred and thirty-five patients (51.9%-males; mean age at enrolment-38.7±12.4 years; median disease duration-60 months [IQR:36-120]) (UC-69.4%, CD-28.9%, IBDU-1.7%) and 73 healthy controls (HCs- mean age-39.6± 10.9 years, 79% males) were enrolled from July 2020 - April 2021 (Table 1). One hundred and twenty-eight (54.5%) patients were immunocompromised and 107 were immunocompetent (treatment details: 5 ASA-72.3%, steroids-15.3%, Thiopurines-40%, methotrexate-2.6%). Seventy-four (31.5%) patients were positive for IgG antibody against SARS CoV2, 2 patients (0.9%) had previous history of COVID infection, and none received COVID vaccine. Seroprevalence rates between immunocompromised and immunocompetent patients with IBD and healthy controls was similar (28.1% vs. 36% vs. 28%, p>0.05) (Fig. 1). Demographic and disease characteristics such as age, gender, disease type, disease activity in last 6 months, disease duration and medication use was similar between patients with positive and negative serology (Table 2). There was progressive increase in seroprevalence from July 2020 to April 2021.
Conclusion Up to 1/3rd patients with IBD were seropositive for IgG SARS Cov2 antibody indicating asymptomatic COVID-19 infection. The seroprevalence was similar to healthy controls and was not different between immunocompromised and immunocompetent patients with IBD.
Keywords Inflammatory bowel disease, COVID-19, SARS CoV2, seroprevalence, Immunosuppression, Steroids, Thiopurines
511
Acute kidney injury due to fish gallbladder ingestion: A case report
Radhika Nittala, Jimmy Narayan, Manoj Sahu, Girish Pati, Debakanta Mishra
Correspondence - Radhika Nittala - drnradhika@gmail.com
Department of Gastroenterology, Institute of Medical Sciences and SUM Hospital, K8 Kalinga Nagar, Shampur, Bhubaneswar 751 003, India
We report the case of a 22-year-old woman with a 5-day history of watery stool, generalized abdominal pain, repeated vomiting, and decreased urine output following the consumption of fish gallbladder for self-treatment of obesity. She was admitted and received empirical antiemetic, proton pump inhibitor, and intravenous saline treatment. Urine output reduced drastically with markedly elevated urea and creatinine, and she underwent urgent hemodialysis (HD). Based on thorough history taking and prompt biochemical investigations that showed extremely high urea and creatinine levels, we made a diagnosis of acute kidney injury (AKI) secondary to fish gallbladder poisoning. Renal function improved over a period of 5 weeks. Fish gallbladder poisoning is infrequent in India. The condition is commonly reversible, and therefore proper history taking is important and prompt biochemical investigations including blood urea and creatinine are needed to enable early diagnosis and fast institution of treatment, which may include HD.
Keywords Gallbladder ingestion, Kidney injury
512
Clinical, biochemical, and molecular predictors of non-response to anti-TNF therapy in patients with inflammatory bowel disease
Peeyush Sewalia, Sudheer Kumar Vuyurru, Prasenjit Das, Bhaskar Kante, Pabitra Sahu, Mukesh Kumar Ranjan, Sandeep Mundra, Rithvik Gola, Raju Sharma, Govind Makharia, Saurabh Kedia, Vineet Ahuja
Correspondence – Vineet Ahuja - vineet.aiims@gmail.com
Department of Gastroenterology, All India Institute of Medical Sciences, Sri Aurobindo Marg, Ansari Nagar, New Delhi 110 029, India
Background Patients with inflammatory bowel diseases (IBD) not amenable to conventional therapy are treated with anti-TNF agents. Primary nonresponse (PNR), as well as secondary loss of response (LOR), is often seen and hence there is an unmet need for defining factors that can predict response to anti TNF agents.
Aim The present study aimed at identifying clinical, biochemical and molecular markers that predict PNR at week 14 after induction dosing and SLR at week 54 in patients with IBD: ulcerative colitis (UC) and Crohn’s disease (CD).
Methods Patients with IBD who were treated with anti-TNF agents from January 2005 to October 2020 were included in this retrospective study. Data concerning clinical and biochemical predictors of response was retrieved from a prospectively maintained database. Mucosal biopises taken before initiation of anti-TNF therapy were available from a biorepository which is maintained for patients with IBD. Immunohistochemistry (IHC) stains for expression of Oncostatin M (OSM-M), Oncostatin M receptor (OSM-R) and IL-7 R receptor were done in mucosal biopsies.
Results: One hundred and sixty-eight patients (104 CD, 64 UC) received anti-TNF therapy. The mean age at initiation of anti-TNFα agents was 34.6±13.7 years and the median disease duration before anti TNF initiation was 60 months (Range:34-108). PNR was seen in 11.5% and 23.5% and LOR was seen in 74% and 45% of patients with CD and UC respectively. In CD, stricturing disease (OR [CI]:5.0 [1.0-22.0], p=0.004) and anemia (8.1±1.6 vs. 9.5±7.7, p=0.025) predicted PNR at 14 weeks. In CD, higher expression of epithelial OSM predicted LOR at 54 weeks (non-responders vs. responders: 5.3+2.7 vs. 2.7+0.9, p=0.036). In UC, no clinical, biochemical, or molecular marker was found predictive of response.
Conclusion In this pilot study, anaemia and stricturing disease were predictors of PNR in patients with CD. Higher baseline expression of OSM in epithelial cells predicted LOR in patients with CD.
Keywords Predictors of non-response, anti-TNF, IBD.
513
Health related quality of life in patients with inflammatory bowel disease
Ravindra Pal , H Vijay Narayanan, Devika Madhu, Nuzil Moopan, S Srijaya, Krishnadas Devadas
Correspondence - Ravindra Pal - docravindrapal@gmail.com
Department of Medical Gastroenetrology, Government Medical College, Ulloor - Akkulam Road, Chalakkuzhi, Thiruvananthapuram 695 011, India
Introduction Inflammatory bowel disease (IBD) is associated with considerable impairment of patients’ health-related quality of life (HRQoL). Knowledge of factors that affect IBD patients’ HRQoL can contribute to better patient care. However, the HRQoL of IBD patients in India is limited. Hence, we assessed the HRQoL of IBD patients to know associated factors.
Methods A cross-sectional study was conducted at the Department of Medical Gastroenterology, Government Medical College, Thiruvananthapuram. The HRQoL of IBD patients was assessed using the IBD questionnaire (IBDQ), Short Form-36 questionnaire (SF36). Independent samples t-test was used to compare HRQoL between Crohn’s disease (CD) and ulcerative colitis (UC). Determinants of HRQoL were identified through multiple linear regression.
Results A total of 60 IBD patients (39 UC, 21 CD) with a mean disease duration of 7.8 years were included. The mean IBDQ score was 121.8 ± 29.01. The SF36 scores were significantly lower than the population normal. There was no significant difference in the scores between UC and CD patients, whereas there was a significant difference between those with active disease vs. remission. The scores were lower when compared to the normal population even during remission. In the multiple linear regression analysis, it was found that presence of active disease (b=−0.250), Presence of EIMs (b=-0.584), and occupation status (b=0.289) were significantly associated with lower HRQoL in IBDQ scores.
Conclusions HRQoL is impaired among patients with IBD, even during periods of remission when disease activity indices may be normal. Active disease, presence of EIM and unemployment due to illness, were found to be significantly associated with a reduction in HRQoL. Greater awareness of the impact of various factors on patients’ HRQoL would improve the holistic management of IBD patients.
Keywords IBD, Qol, IBDQ, SF36, Quality of life, Inflammatory bowel disease
514
Prevalence of the Helicobacter pylori oipA and babA genes and their correlation with virulent genes in gastroesophageal reflux disease (GERD) and non-GERD patients
Sarika Singh , Shweta Mahant, Rajashree Das
Correspondence – Shweta Mahant - smahant@amity.edu
Amity Institute of Biotechnology, Amity University, Sector 125, Noida 201 301, India
Background The aim of our study was to evaluate the prevalence and clinical relevance of oipA and babA genes of Helicobacter pylori in gastroesophageal reflux disease (GERD) and non-GERD patients. The interplay of outer membrane protein (OMP) coding genes along with virulence genes cagA vacA of H. pylori is responsible for expression of pathogenic factors in host. A group of 33 genes, the outer membrane protein coding genes (OMP) encoded by approximately 4% of the genes of H. pylori, plays a pivotal role in persistence and colonization of bacteria.
Method Culture DNA of 39 H. pylori positive strains were isolated from collected GERD non-GERD samples. DNA was assayed for oipA, babA by polymerase chain reaction (PCR). cagA vacA status was also evaluated by PCR
Results Out of 39 H. pylori positive samples GERD non-GERD status is 19/39 and 20/39. In 34 oipA+ve samples 50% were each GERD and non-GERD positive. In 23 babA+ve samples 68.4% had GERD while 50% were non-GERD. Cag+ve GERD/non-GERD patients were 31.5% and 60% respectively. vacs1m1/s1m2 for GERD is 21.0% and 78.9% while for non-GERD it is 55% and 45% respectively.
Conclusion Our results show there were no correlation between the presence or absence of the oipA/babA and cag+ve/cag-ve in GERD and non-GERD patients. However, vacs1m1/s1m2 with p<0.05 was significantly associated with GERD non-GERD disease. Thus, although the oipA and babA genes did not represent important individual virulence markers in GERD, non-GERD they may act synergistically with vacs1m1/s1m2 for clinical outcome.
Keywords GERD, non-GERD, Helicobacter pylori, Outer membrane protein coding genes
515
An unusual case of celiac disease with associated non-cirrhotic portal hypertension and autoimmune gastritis with squamous cell carcinoma
Prasanna Gore , Dattatray Solanke
Correspondence – Prasanna Gore - drprasannagore@gmail.com
Department of Medical Gastroenterology, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Rao Saheb, Achutrao Patwardhan Marg, Four Bungalows, Andheri West, Mumbai 400 053, India
A 42-year-old male came with complaints of easy fatiguability, generalized weakness, loss of appetite, breathlessness on exertion, failure to gain weight, early satiety. Patient has history of chronic iron deficiency anemia. On examination patient had pallor, cachexia. Investigation showed severe iron deficiency anemia, hypoalbuminemia, mild deranged LFT. Patient was transfused IV iron, albumin and all the supportive medication. Patient was posted for upper GI endoscopy which revealed UES web dilated through scope, esophageal varices banded, atrophic gastric folds biopsy taken, scope (adult) could not be negotiated further to pylorus due to the stricture hence pediatric scope used and D2 had scalloping hence biopsy taken. Gastric biopsy showed autoimmune gastritis. D2 biopsy showed MARSH grade 3, simultaneously tTg-IgA levels sent which was 170. He was kept on gluten-free diet. Patient USG abdomen showed changes of liver cirrhosis with changes of portal hypertension. Patient was evaluated for cause of cirrhosis, HIV negative, HbSAg negative, anti-HCV negative, HAV and HEV IgM negative, Kayser–Fleischer (KF) ring not seen, serum ceruloplasmin normal. Hence as the cause of cirrhosis was not known patient was posted for Liver biopsy which was done and suggestive of non-cirrhotic portal hypertension. Patient later on follow-up had neck mass, fine needle aspiration cytology (FNAC) of which showed squamous cell carcinoma with unknown primary, which was operated.
Unusual things in the case is non-cirrhotic portal hypertension associated celiac and autoimmune gastritis associated with celiac. Association with squamous malignancy likely due to long-term malabsorption with multivitamin deficiency.
Keywords Celiac, Non-cirrhotic portal hypertension, Autoimmune gastritis
516
Online wellness programme a useful tool for irritable bowel syndrome patients
Neeraj Nagaich 1 , Radha Sharma 2
Correspondence – Neeraj Nagaich - drneerajn@gmail.com
1Department of Gastroenterology, Fortis Escorts, Jaipur 302 020, India, 2Department of Pathology, RUHS CMS Medical College, Jaipur 302 020, India
Objectives Irritable bowel syndrome (IBS) is a chronic and debilitating functional gastrointestinal disorder which affects nearly 5% to 11% of the population and behavioral approaches have shown efficacy in reducing IBS symptoms. A large unmet need for non-pharmacologic tool for IBS patients. Lifestyle changes may be helpful in subgroup of patients. This prospective and retrospective study was done to evaluate efficacy of lifestyle changes implemented via wellness programme in IBS patients.
Methods Wellness programme comprise of daily Swasthi sadhana, dietary and other lifestyle changes. In this study 51 patients who completed online wellness programme (5 day) and followed lifestyle changes as instructed for 8 weeks. Observations of symptoms was done a decrease was seen in GIQLI domains of core symptoms psychological symptoms and physical symptoms, there was also lesser requirement of medicine.
Results In all the patients a significant decrease was reflected in the GIQLI symptoms, psychological symptoms and physical symptoms there was also lesser requirement of medicine in the patients following wellness program as compared to other patients of IBS not following life style changes of wellness programme.
Conclusions Online Wellness programme is an useful approach to implement lifestyle changes and may help IBS patients. Needs revalidation in larger cohort in future studies.
Keywords Wellness programme. Life style changes, IBS
517
Modification of nasopharyngeal airway tube for better control of airway management during sedation for ERCP and endosonography
Viswanath Donapati , Vijayanand Reddy, Sashi Kiran, Ravi Shankar Bagepally, Guduru Raghavendra Srinivas Rao, Rakesh Kumar Adi, I Bharani, V Vamshidhar Reddy, Anil Kumar Mannava
Correspondence – Viswanath Donapati - viswanathdr@yahoo.com
Department of Gastroenterology, Yashoda Hospital, Alexander Road, Kummari Guda, Shivaji Nagar, Secunderabad 500 003, India
Introduction Endoscopic ultrasound and endoscopic retrograde cholangiopancreatography (ERCP) are high end therapeutic endoscopic procedures performed under sedation often in high-risk settings where patients are at high risk of desaturation during procedure. Literature suggests we use the option of elective endotracheal intubation prior to the procedures particularly for those with higher ASA score. The next best option is to maintain the natural airway using Nasopharyngeal tube with oxygen through nasal prongs oxygen. We hereby describe a modification of the nasopharyngeal airway tube for giving sedation during the procedures.
Aims To analyze the safety and efficacy of a modified nasopharyngeal airway for airway management during ERCP and endosonography procedures.
Methods Retrospective data of 100 patients who underwent endosonography and ERCP during a period of 3 months at Yashoda Hospital of Hyderabad was reviewed. Patient-specific and procedure specific data was extracted. Desaturation was defined by fall of pulse oximeter saturation below 90% and its relation to patient specific high risk-factors was analyzed.
Results We had 100 patients who underwent the endoscopic procedures using the modified nasopharyngeal airway. Only 10 patients had transient de-saturation below 90% without any residual sequlae. There was no interruption to the endoscopic procedure and there was no significant relation between desaturation episodes and patients higher ASA status or modified Mallampati (MMP) class. The desired optimal oxygenation and airway patency was maintained during the procedures with high degree of success using modified nasopharyngeal airway with oxygen supplementation in all patients.
Conclusions The sedation for the high end endoscopic procedures using the modification of the Nasopharyngeal airway was safe and successful in providing secure airway without any interruption of procedures.
Keywords Airway in endoscopic retrograde cholangiopancreatography, Endosonography, Anesthesia, Modified nasopharyngeal airway
518
Comparison of ABC score with AIMS65, Rockall and GBS score for predicting 30 mortalities in patients with upper and lower GI bleed
M S Revathy, B Sumathi, S Chitra, M Manimaran, G Sathya, Rakesh Jha
Correspondence – Rakesh Jha - jharakesh2006@gmail.com
Department of Medical Gastroenterology, Government Stanley Medical College, No.1, Old Jail Road, George Town, Chennai 600 001, India
Introduction Several pre/post-endoscopy risk scoring systems have been developed to predict outcomes likes mortality, need for hospital-based intervention, and need for endoscopic therapy. Implementation of Glasgow-Blatchford score (GBS) is associated with a 15% to 20% reduction in the number of hospital admissions with upper gastrointestinal bleeding (UGIB) and is therefore recommended to identify very low-risk patients who could be managed as outpatients.
Aim Comparison of ABC score with AIMS65, Rockall and GBS score for predicting 30 mortalities in patients with upper and lower gastrointestinal bleed.
Methodology An observational prospective study, patients enrolled and clinical details, blood parameters, endoscopic findings noted, appropriate therapeutic intervention done, and all patient followed up for 30 days to look for mortality.
Results Fifty-four patients were included. Data showed age ≥75 years, creatinine >150 μmol/L, low albumin, PR 100 beats/min, altered mental status increased 30-day mortality. Score showed 30-day mortality (AUROC (95% CI) 0.81 (0.74 to 0.88)) in present cohort. Based on AUROCs, score was better at predicting 30-day mortality as compared with AIMS65 (AUROC (95% CI) 0.64 (0.59 to 0.69); admission Rockall score (AUROC [95% CI] 0.72 [0.69 to 0.75]; p<0.001), full Rockall score (AUROC [95% CI] 0.77 [0.68 to 0.86]; p<0.001) and GBS (AUROC [95% CI] 0.78 [0.74 to 0.82]; p<0.001). Association of ABC score and mortality as follow patients with a score of ≤3 (62% of patients) had a very low risk (1.8%), score of 4–7 (29% of patients) moderate risk (7.9%), and score of ≥8 (9% of patients) had a very high mortality rate of 48% respectively.
Conclusions ABC score can predict mortality in both UGI/LGI bleed.
Keywords Upper gastrointestinal, Lower gastrointestinal, Glasgow-Blatchford score
519
Curious case of diarrhea !!!
Bhushan Bhaware, Saurabh Mukewar, Atul Gawande, Shrikant Mukewar, Ravi Daswani
Correspondence – Ravi Daswani - daswaniravi@yahoo.co.in
Department of Gastroenterology, Midas Hospital, 10-A Racheda, Jaripatka, Nagpur 440 014, India
A 28-year-old female presented with episodic painless diarrhea 6 to 7 months associated with weight loss of 12 kgs over last 7 months. She gave H/O- “not having meals with fear of increasing loose stools”. She had received two units of PRBC at native place for anemia. Her symptoms used to subside with antibiotics and metronidazole. However generalised weakness persisted. Over the last 2 -3 months she noticed tingling numbness in lower limb which had progressed to inability to walk since 2 weeks. Relatives also complained of increased irritability and refusal for admission and investigations.
On examination she was cachexic, pale and had stable vitals. CNS examination revealed dysdiadokokinesia, ataxia, dysmetria, sensory neuropathy signs and power in all four limb was 5/5. Lab investigations revealed microcytic anemia with iron deficiency and normal UGI endoscopy. D2 biopsy showed nonspecific changes. I g A TTG and anti-DGP was negative.
NCV revealed distal symmetrical axonal sensory polyneuropathy. Opthalmology evaluation and VEP revealed prolonged P100 latency in both eyes.
MRI brain revealed B/L altered signal in dentate, dorsal pons and medulla. Cerebellum was normal
What is the diagnosis?
Keywords Diarrhea, Drug toxicity, CNS toxicity, Metronidazole
520
Age based normal hand grip metrics (HGM) in a group of healthy medical students
Kirthika Arunachalam , Kavin Chakravarthy, Keerthana Menon, Y V Bhargav, Jayanthi Venkatraman
Correspondence – Kirthika Arunachalam - akirthika98@gmail.com
Department of Hepatology, Sri Ramachandra Institute for Higher Education and Research, No.1, Ramachandra Nagar, Porur, Chennai 600 116, India
Introduction Hand grip strength (HGS) is a measure of the maximum static force that a hand can squeeze using a dynamometer. There are variations in HGS depending on race, sex, and age. HGS is measured for normal subjects and normative reference data dependent on sex and age are being used in clinical practice. We set out to establish the same amongst the Indian population.
Aim To determine normal hand grip metrics in young adult population.
Methods This cross-sectional descriptive study recruited 458 healthy male and female medical students between the age of 18 and above from a tertiary university hospital in Southern India. Their basic profilic data including age, gender, height, weight, food habits, place of origin(state) were collected. BMI was calculated. Hand grip strength was assessed in the dominant hand by using a Camry Hand Dynamometer with a mean of three values.
Results Statistical analysis done. Mean BMI in the study group was 23.7 kg/sq.m. Age groups divided into three groups as 18-19, 20-24 and 25-30 and above among males and females. Mean value of three hand dynamometer measurements determined. Normal reference range was compared with the values obtained for weak, normal or strong hand grip strength among males and females.
Conclusion BMI and dietary habits did not correlate with hand grip strength measurements. Males of age group 20-24 had highest normal range when compared with others and was statistically significant.
Keywords Hand dynamometer, Hand grip strength, Body mass index
521
Real time assessment of mucosal impedance as a marker of mucosal pathology: A prospective study
Priyanka Arora 1 , Jaspreet Singh 2 , Anuraag Jena 1 , Ritambhra Nada 3 , Lileshwar Kaman 4 , Amol Patil 5 , Usha Dutta 1
Correspondence – Usha Dutta - ushadutta@gmail.com
Departments of 1Gastroenterology, 2Semiconductor Laboratory, 3Histopathology, 4Surgery, 5Pharmacology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh 160 012, India
Background Inflamed/malignant tissues are not only visually abnormal but also physiologically abnormal in the form leaky tight junctions. This is associated with decrease in mucosal impedance (MI).
Aim The aim was to study the role of MI assessment to differentiate apparently normal region from those in inflamed/ malignant region.
Methods Consecutive patients undergoing surgery at our tertiary care center were recruited after informed consent. Immediately after surgery, resected specimens were laid into tray and analyzed for MI. MI catheter was designed after multiple iterations and was validated with a commercially available impedance measuring tool. Average of three MI readings of visually uninvolved region (apparently normal) and involved region (inflamed/ malignant) were taken. Statistical analysis was done after data entry into excel sheet.
Results Total of 261 patients who had undergone surgery were enrolled. Mean age was 46.98 ± 15.33 years (females, 64.4%). The median MI of involved areas was significantly lower than non-involved areas of the tissue specimens (1884 [877] ohm vs. 2699 [1514] ohm; p<0.001). In cases of malignancy (n=57), MI of malignant regions was significantly lower than the impedance of uninvolved regions (1878 [842] ohm vs. 2624 [1408] ohm; p<0.001). Similarly, in cases with inflammation (n=71), it was found that MI of inflamed regions was significantly lower than of uninvolved regions (1836 [686] vs. 2548 [1091] ohm; p<0.001). Our catheter was validated with the commercially available MI tool (n=51 readings). It showed a high degree of significant correlation (p<0.001). The Regression equation was inhouse impedance catheter= 2.02+1.051* Standard impedance tool (R2=0.452). Our impedance catheter was found to be easy to use and provided in real time reproducible assessment of MI.
Conclusion MI is reduced in the inflamed/malignant region of the gut. It is likely to become an useful tool for real time assessment of mucosal health.
Keywords Mucosal Impedance, Malignancy, Inflammation
519
Fecal calprotectin in patients with corona virus disease 2019: A preliminary report of an ongoing case-control study
Ujjala Ghoshal
Correspondence – Ujjala Ghoshal - ujjalaghoshal@yahoo.co.in
Department of Microbiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India
Background Infection with severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) causing corona virus disease 2019 (COVID-19) involves gastrointestinal (GI) tract. Inflammation may be responsible for GI symptoms. Data on fecal calprotectin (FC), which may be raised in GI inflammation, however, are scanty.
Methods Fecal samples of patients with COVID-19 and healthy controls were tested for FC using immune enzymatic test (IET) Calprest NG (Eurospital, Spain) and a rapid semiquantitative test (Certest, Biotech, Spain). The samples were also screened for GI infection by microscopy, bacterial culture on Mac Conkey agar, Deoxycholate citrate agar and Modified Kinyoun and Trichrome stains (for opportunistic parasites).
Results Of 44 patients (51.9-y±13.5, 6 [14%] female) studied, 40 had symptomatic (13 had GI symptoms) and 4 asymptomatic COVID-19. The comorbid conditions included diabetes mellitus (19/44, 43%), hypertension (27/44, 61%), chronic kidney disease (9/44, 20%), prior kidney transplantation (5/44, 11%), chronic lung disease (2/44, 4%), congestive heart failure (3/44, 6%), malignancy (2/44, 4%). The rapid test was negative in all the patients. By IET, the median FC value was 19.3 mg/Kg (range 1.0 to 90.5). In 4/44 (9%) patients, FC was abnormal (>50 mg/Kg; all in symptomatic patients except one). Patients with GI symptoms more often had abnormal FC value than those without (3/13 vs. 1/27; p=0.049).
Conclusions FC is raised in 9% patients with COVID-19, particularly those with symptoms, especially the GI symptoms. The rapid test was found inferior to IET for detection of FC among them.
Keywords COVID-19, Gastrointestinal infection, Gut inflammation
Author Index
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.


