Abstract
Internal joint derangement is a disruption of the internal aspects of the TMJ—disc displacements/adhesions/impingements, causing alterations in the normal dynamic motions of the joint. Clinicians must be diligent in establishing the correct diagnosis and cause of TMJID, which ultimately leads to the appropriate management of such patients. While many patients adapt over time or with non-surgical treatment, surgery may be indicated for those with ongoing problems. The surgical pyramid provides a stepwise progression for TMJ surgical patients. This paper aims to review TMJID and its management with special emphasis on arthroscopic minimally invasive surgery, as practised in other countries around the world, and compare this to current education, understanding and practice in India. Currently, India is lagging behind in providing the full scope of TMJ services as there are very few surgeons trained in the skill of arthroscopic techniques. There needs to be continued expansion of our understanding of TMJID treatment in India to bring it level with the rest of the world.
Keywords: Articular disc, Internal derangement, Arthroscopy, Temporomandibular joint surgery
Understanding Internal Derangement of TMJ Over the Decades
The term internal derangement is adopted from Orthopaedic literature and describes disturbances in the articulating components of the TMJ—internal structural damage and dysfunction of the joint associated with abnormal disc position [1]. The AAOMS position paper defines internal joint derangement as a disruption of the internal aspects of the TMJ—there may be either disc displacements or adhesions/impingements even in the face of normal disc position, causing alterations in the normal dynamic motions of the intracapsular elements [2].
Around the late 1970s and 1980s, it was thought that internal derangement of the TMJ (TMJID), synonymous with disc displacement, was the primary mechanical issue. Mc Carty and Farrar [1] in 1979 emphasized disc displacement and it was thought that the displaced disc was a progressive problem that would eventually lead to degenerative joint disease. Therefore, treatment included attempts at repositioning or replacing the disc, either by non-surgical or surgical means; but in the 1990s, it was realized that open joint surgery for disc repositioning or discectomy often led to progressive degenerative joint disease and fibrosis. In addition, patients who had undergone disc repositioning surgery often did well despite the fact that the disc was often not reliably maintained in its new position. Furthermore, arthroscopy was emerging as a reliable alternative to reduce pain and increase mouth opening without changing the disc position [3–6]. Therefore, there has been a conceptual shift from internal derangement and disc displacement being considered a primary diagnosis that required correction, towards our current understanding that disc displacement/internal derangement represents an endpoint of a process in which there has been biomechanical failure from a specific cause. This underlying aetiology must be identified and managed if treatment is to be successful in the long-term. We now know that disc malposition is present in approximately a third of the population and that through a process of adaptation the joints are asymptomatic despite the disc displacement [7, 8]. Several authors have studied the prevalence of ID in various regions of India and the range is 9–50% [9, 10].
The Indian Oral and Maxillofacial Surgeon has extensive training in the surgical management of TMJ ankylosis and probably has the largest collective experience in its management. This was pointed out by Dimitroulis in his invited review published in this journal in 2012 [11]. The high prevalence of ankylosis is thought to be due in part to limited access to health care in many parts of India. In the present day, we recognize that there are other TMJ disorders in addition to ankylosis affecting the burgeoning middle class of India, including internal derangement (ID), myofascial pain dysfunction syndrome, primary and secondary arthritis. This group of patients not only now have better access to health care, but now also demand treatment for diseases that in the past, were largely endured due to lack of resources and facilities. While the surgical management of ankylosis is challenging; the diagnosis and surgical aims are straightforward. Instead, other TMJ disorders like internal derangement present a greater diagnostic challenge and current understanding and management of ID is limited in India when compared to other countries. This is possibly due to lack of education, training and equipment in dental schools and hospitals.
This paper aims to review TMJID and its management as practised in other countries around the world. We then compare this to current education, understanding and practice in India having conducted a national survey of Indian oral and maxillofacial surgeons. We highlight arthroscopy as an important area of growth in India that needs to continue with future education and training in India.
Aetiology and Pathophysiology
An overloaded joint on account of any of the following may lead to synovitis, articular cartilage degeneration, disc displacement and therefore impaired biomechanics. This can lead to loading of the retrodiscal tissues, inflammation, failure of lubrication and impaired joint function.
Macro trauma—major impact to jaw, e.g. sports injury, assault
Microtrauma—parafunctional habits, e.g. clenching, bruxism
Systemic arthropathy—rheumatoid, psoriatic or infective arthritis, SLE, HLA-B27, etc.
An alternative etiologic framework could be:
A normal joint subjected to overload (trauma, parafunction)
An abnormal joint subjected to normal load (rheumatoid, SLE or psoriatic arthritis, osteochondroma, chondromatosis)
Yet another framework [12]:
Inflammatory/degenerative arthropathy: Joint overload causing inflammation and degeneration of intra-articular tissues
Systemic arthropathy: Systemic disorder causing TMJ disease
Localized atypical arthropathy: Intra-articular disorder not caused by joint overload
False arthropathy: Extra-articular disorder simulating/causing TMJ symptoms
Diagnostic criteria for TMD
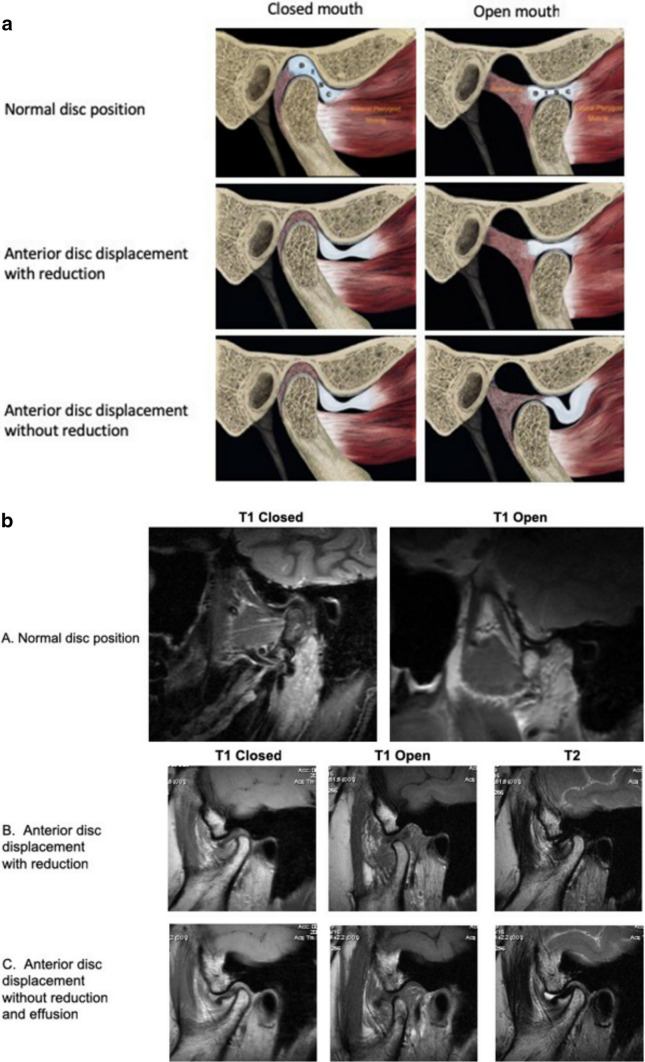
The diagnostic criteria for research and clinical purposes were recently updated in 2014 [12, 13] and include internal derangement, which may present as (Fig. 1a, b):
Disc displacement with reduction
Disc displacement with reduction and intermittent locking
Disc displacement without reduction with limited opening
Disc displacement without reduction without limited opening
Fig. 1.
a Normal and displaced disc positions, with and without reduction (modified with the permission of Dr. Robert Talley). b MRI scan—T1 and T2 images in closed and open mouth positions. A normal disc position. B Anterior disc displacement with reduction. C Anterior disc displacement without reduction and superior joint space effusion
The 2001 Wilkes Classification (Table 1), the Research Diagnostic Criteria, 2014 for TMDs and the American Association of Orofacial Pain Taxonomic Classification categorize the extent of damage to the joint tissues and thus, communicate severity and guide treatment. However, these classifications mostly do not recognize the underlying aetiology, without recognition and management of which, treatments often fail, as the cause persists. Therefore, Israel [12] proposed the essential components of patient management as control of risk factors causing intra-articular changes, reduction of pain and improvement of function.
Table 1.
Wilkes staging classification for internal derangement of the TMJ.
Adapted from Bronstein and Thomas [2]
| I. Early stage |
| Early opening reciprocal clicking, no pain, no reduction in mouth opening, slight anterior disc displacement |
| II. Early/intermediate stage |
| Pain, mid to late opening click, transient locking, anterior disc displacement, early anatomic disc deformity |
| III. Intermediate stage |
| Multiple episodes of pain, locking, reduced mouth opening, anterior disc displacement with anatomic disc deformity, no hard tissue changes |
| IV. Intermediate/late stage |
| Increase in severity of degenerative changes, hard tissue degenerative remodelling, disc adhesions but no perforations |
| V. Late stage |
| Crepitus, increased pain, chronic restriction of mouth opening, disc perforation, gross anatomic deformity of disc and hard tissues, degenerative arthritic changes |
Clinical Features, History and Diagnosis [14]
The most common presenting complaints in ID include pain, joint noises (click or crepitation) and functional limitations; including a mechanically obstructive click, locking, changes in occlusion, restricted mouth opening and loss of masticatory function. Muscle disorders will often accompany these intra-articular problems.
When taking a history, questions relating to onset and evolution of the problem are helpful in reaching a diagnosis. In addition, a history of trauma, parafunctional habits and symptoms in other joints will point to the underlying aetiology. Therefore, enquiry into the patient’s physical, dental, emotional and psychosocial status is essential.
Clinical examination should include the muscles of mastication, TMJ, occlusion and looking for signs of parafunction. Direct (Mahan’s) and indirect pressure loading tests will help identify retrodiscitis and muscle disorders. Occasionally, a diagnostic local anaesthetic block may be required to distinguish arthralgia for other muscular or neuropathic causes of pain.
History and clinical examination is supplemented with MRI scans to evaluate the disc position, effusions and degenerative osseous changes. CT scans are used to evaluate osseous changes and ankylosis. Occasionally, Technetium bone scans are necessary to evaluate metabolic activity in condylar hyperplasia or tumours such as osteochondroma.
In cases of condylar resorption or when primary inflammatory arthritis is suspected, serological tests including rheumatoid factor, anti-cyclic citrullinated peptide antibodies, antinuclear antibodies and HLA-B27 are required.
Treatment of Internal Derangement
Pain itself is not a disease. “Pain merely halts the function to allow healing”. The goals of management of ID [12] are to identify and control the causative factors, decrease functional load, reduce inflammation, allow adaptive articular remodelling, thereby decreasing pain, increasing range of motion and restoring function.
Non-surgical Treatment
This includes patient education, diet modification, improving sleep, parafunctional habit awareness, biofeedback, non-steroidal anti-inflammatory medication, muscle relaxants, botulinum toxin, passive-motion exercises, masticatory muscle massage and heat, physical therapy and occlusal stabilization oral appliances. Many patients recover with only jaw rest and soft diet, while others may require a combination of these treatments.
In the 1930s and 1940s, Temporomandibular joint disorders (TMD) used to be seen as problems related to occlusal or skeletal disharmony. Costen first suggested the link between occlusion, TMJ disorders and ear symptoms based on his observations in 11 patients [15]. This evolved into orthotics and occlusal therapies being used for the treatment of TMD in the 1940s and 1950s. Occlusal appliances or orthotics were thought to not only produce occlusal disengagement but also relax jaw musculature, restore vertical dimension of occlusion, unload the joints, or reposition the condyle and/or disc; but until the 1960s, there were no well-controlled, well-designed, systematic studies evaluating the treatment of TMD.
However, our understanding of orthotic devices has changed significantly over time. Lundh [16] compared outcomes of 2 treatment groups of symptomatic TMJ disc displacement—no treatment versus occlusal appliance. At 1 year, there was pain resolution in 33% patients in both groups. Forty per cent reported increased pain in the occlusal appliance group compared to 16% in the no treatment group. Truelove [17] evaluated 200 patients with symptomatic TMJID divided into 3 groups; basic non-surgical treatment versus hard flat plane occlusal appliance versus soft splint. Success outcomes after 3 and 12 months suggested no significant difference between the groups. Furthermore, the use of occlusal appliances may occasionally increase parafunctional habits, increase pain or may even result in occlusal changes; especially with long-term use of partial coverage devices (e.g. NTI and Gelb appliances). Although the evidence for oral appliances in the literature is generally poor, these devices still have a role in non-surgical management when used appropriately.
In Klasser’s evidence-based review of the literature [18], he states that occlusal appliances should be viewed as “oromandibular crutches”, that are analogous to ankle support and back brace devices in providing symptomatic relief, while the patient recovers. Furthermore, he states that there are only 3 likely indications for OA use in TMJID:
In patients with acute TMJ pain, OAs may reduce muscle activity and redirect loading inside the TMJ;
For sleep bruxers who wake with TMJ pain due to nocturnal muscle activity, an OA worn at night could be helpful to reduce pain and dysfunction;
For patients whose TMJs become “locked” at night, but who are able to successfully click open during the day, an OA can reduce the frequency of these episodes or prevent their occurrence in some cases.
Lastly, it has been suggested that any pathology in the TMJ region nonresponsive to non-surgical therapy within 6 to 8 weeks was most likely intracapsular [14]. Unfortunately, many clinicians lack training and familiarity with surgical joint pathology thereby making them reluctant to refer the patient for surgery. This may lead to a concoction of endless non-surgical therapies that do not address the intra-articular problem. Eventually, patients may become depressed, making psychological counselling necessary [11].
Surgical Treatment
Approximately 90% of TMD patients experience symptom resolution either spontaneously or with non-surgical treatment [19] due to the underlying adaptive capacity of the TMJ. Clinical research [20, 21] into the natural progression of TMJ internal derangement has shown that 25–33% of patients who do not improve even after 1 year are older patients, especially those with MRI evidence of advanced disease [12]. Non-surgical therapy should at least be rendered for 1–2 months before considering surgical intervention in most situations [22].
Patient Selection and Management [22]
An etiologic classification of TMJID patient has been developed by Mc Cain, with treatment specific to each type. The problematic patient, however, may exhibit characteristics of one or more types. History, clinical and radiological signs determine whether the patient is an appropriate candidate for surgery [11].
Type 1: MPDS (Direct Microtrauma)
They are characterized by bruxism, symptoms increased by stress, history of joint clicking, dull pain in muscles of mastication, more in the morning. Their treatment protocol includes stress management with psychological counselling, physical therapy and occlusal flat plane splint with centric occlusion, 2 mm posterior thickness providing anterior guidance, cuspid protection and posterior disocclusion.
These patients may be considered for surgery only after their myofascial problem is brought under control as much as possible.
Type 2: Dental Facial Deformity and Malocclusions (Direct Microtrauma)
The most common type of type 2 patient is the one with mandibular retrusion. They posture the mandible habitually forward and thereby stretch the capsular attachment, thereby loosening it. This may lead to subluxation or dislocation and may also be accompanied by muscle pain.
Two protocols have been established for these patients, one includes orthodontic management and the other orthognathic surgery, both accompanied by arthroscopy and physical therapy.
Type 3: Direct Macrotrauma
It involves a direct blow to the mandible with or without fracture. The characteristics would be a singular recallable event, painful snapping of the joint, decreased mouth opening and joint-specific pain. According to Boering [23], there is a potential for cartilage damage to occur from direct condylar trauma. Other literature on arthroscopic evaluations of condylar fractures reveals more trauma to the fractured than the nonfractured side [24].
Trial splint therapy may be tried before surgical intervention, except in direct trauma cases, where protracted splint therapy is not recommended [22].
Type 4: Indirect Macrotrauma
This occurs due to acceleration–deceleration injuries of the head and neck with progressive symptoms from muscle splinting to joint pain and noise, affecting mandibular motion.
They may be treated by splint therapy and physical therapy for about 6 months, followed by arthroscopic surgery and physical therapy again.
Type 5: Systemic Diseases
Those affecting the TMJ include rheumatoid arthritis, SLE, psoriatic and HLA-B27. They may exhibit progressive jaw deformity, change in occlusion, joint crepitation, focal joint pain and reduced mouth opening.
Treatment includes splint therapy, medical management, Arthroscopy [25] followed by physical therapy.
Arthrocentesis
Arthrocentesis was introduced as an effective yet minimally invasive means of treating patients with symptomatic internal derangement [26–28]. Murakami first described TMJ arthrocentesis in 1987 by using a single needle pumping technique to create hydraulic distention of the upper joint space [29]. Nitzan and Dolwick [26] subsequently used 2 needles to perform lysis and lavage of the upper joint space, using an inflow needle, an outflow needle and at least 300 ml Ringer Lactate’s solution. The lysis and hydraulic distention breaks the adhesions, restores lubrication and synovial fluid flow and thereby improves the range of motion. The lavage removes the inflammatory mediators, cytokines, matrix metalloproteinases, proteolytic enzymes and debris. The success rates range from 70 to 95% [26–28].
Sanroman [30] studied 26 patients with sudden onset persistent reduction in mouth opening, with MRI signs of articular discs fixed to the glenoid fossa. Both arthroscopy and arthrocentesis gave good results for patients with this anchored disc phenomenon.
The Western world regards TMJ arthrocentesis as the panacea for all TMJID, regardless of the significance of the joint disease. However, in reality, arthrocentesis has limited applications, with higher success rates reported in acute onset closed lock and is not of value in advanced joint disease [12]. Although arthrocentesis requires less surgical skill and is performed at a lower cost, it has its limitations and does not permit direct joint visualization, biopsy, debridement and removal of pathologic tissue [11]. Arthroscopy not only has the advantage of direct visualization and documentation but also if required, the possibility to perform a level 2 or 3 in the same sitting.
Arthroscopy
Arthroscopy was introduced in the TMJ by Ohnishi using a fibreoptic light source and arthroscopic device in 1974. In 1982, Murakami and Hoshino illustrated TMJ arthroscopic anatomy [31]. Then, in the 1980s, the cause of TMJ arthroscopic surgery was furthered in the USA by Joseph McCain, Bruce Sanders, Holmlund, Moses and others [2, 32].
Arthroscopy involves not only direct visualization of the joint but also lysis of adhesions, biopsy, debridement of degenerative articular cartilage and other pathologic tissues and direct injection of medications into the synovium. It provides a more effective approach to the management of chronic or recalcitrant cases of closed lock [11], which most often have significant intra-articular adhesions.
A correlation in finding of 91% Arthroscopy and surgical exploration has been reported, while the same is true only in 58% cases of Arthrography to surgical exploration for knee injuries [33]. In 54 cadavers, Holmund and Hellsing compared TMJ arthroscopy with dissection findings. They found arthroscopy 100% accurate for osteoarthritis deformans but only 57% for joints with subtle remodelling changes [34].
Indications and Contraindications
Diagnostic arthroscopy is performed for unexplained persistent TMJ pain with the absence of positive findings on conventional imaging, unresponsive to medical therapy or to allow biopsy of suspected lesions. Operative arthroscopy is indicated for synovitis, intra-articular adhesions, disc displacements with obstruction, painful subluxations and degenerative joint disease [22]. Overlying skin infections and risks associated with malignant tumour seeding represent relative contraindications [14].
Jeff Moses analysed 419 joints who had undergone Arthroscopy for TMJID with a follow-up of over 10 months and confirmed successful results in 97% patients [35]. Mc Cain, Sanders and colleagues conducted a 6-year multicentre retrospective study of 4831 joints for six diagnostic categories—ID with closed lock & painful click, arthritis, hypermobility, arthralgia and fibrous ankylosis and measured four outcomes—range of motion, pain, diet and disability. Over 90% of patients had excellent results in each outcome measure, with only 4% having complications [5]. McCain describes different levels of arthroscopy based on the number of cannulas and portals [22].
Level 1 Arthroscopy
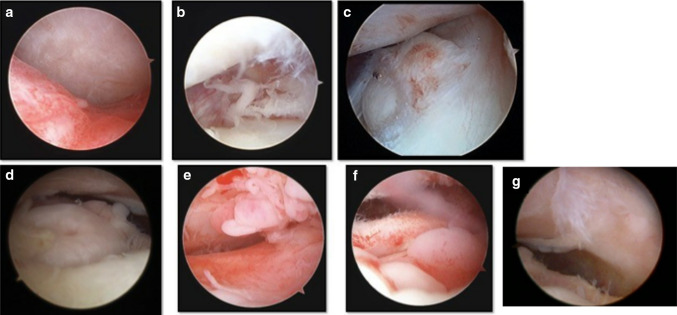
Arthroscopy begins with examination under anaesthesia (EUA) of the TMJ so that the surgeon may anticipate what to expect when the joint is entered arthroscopically [22]. The range of condylar translation and joint noises are evaluated in the EUA. Hypermobility with subluxation can be identified, whereas limited translation or merely hinge movements may point towards a disc displacement without reduction, adhesions or fibrous arthrosis. Clicks indicate disc reduction, while bone on bone crepitations indicate a retrodiscal perforation (Fig. 2).
Fig. 2.
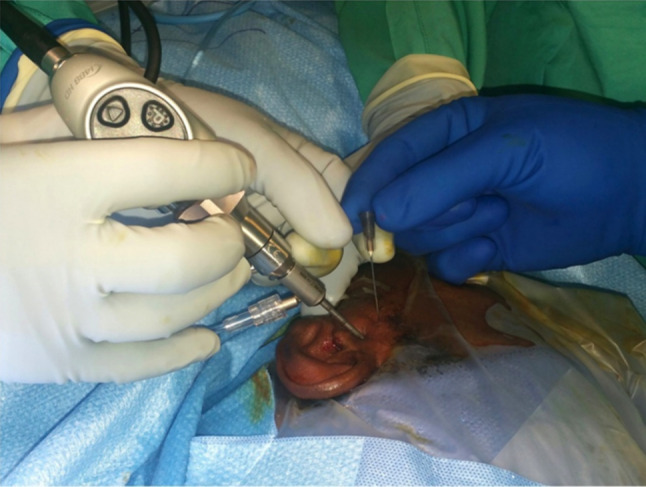
Level 1—arthroscopy
The superior posterolateral puncture approach is used most commonly to access the superior joint space [14]. Anatomic areas examined by a diagnostic sweep include the medial synovial drape, pterygoid shadow, retrodiscal synovium, posterior slope of articular eminence and glenoid fossa, articular disc, intermediate zone and the anterior recess [22].
Internally deranged joints may generally have varying degrees of anterior disc displacement with the condyle articulating against the retrodiscal tissue and even causing perforation. Sometimes the disc may be firmly adherent to the fossa [36]. Arthroscopic findings may include synovitis (polypoid, villonodular, etc.), chondromalacia, exophytic formations, floating debris, chondromatosis, adhesions, meniscal perforations and degenerative changes (Fig. 3).
Fig. 3.
Arthroscopic pathology. a Retrodiscitis, b adhesions, c small disc tear/perforation, d large perforation with condyle visible, e villonodular synovitis, f polypoid synovitis, g grade 4 chondromalacia
Passive mobilization exercises should be started within 24 h of surgery and repeated 3/4 times daily for 15 min, for at least 2 months. Physical therapy can be added, but this is not a replacement for these exercises. Gentle stretching of the mandible prevents formation of adhesions released during arthroscopy and helps to stimulate the synovial fluid to provide nutrition to articular cartilage chondrocytes [12].
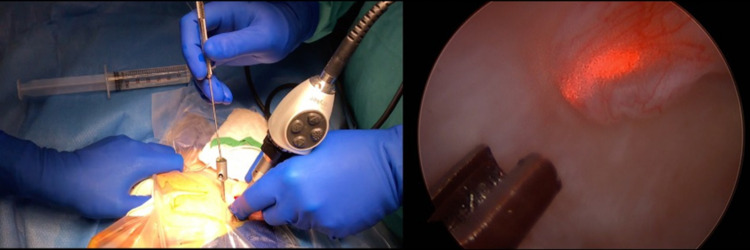
Level 2 Arthroscopy
This includes a second puncture and cannula allowing for additional procedures such as disc mobilization, biopsy and debridement with laser or coblation to be performed. Double puncture techniques vary in different anatomic situations, namely, normal anterior recess volume, lateral adhesions and cases of arthrofibrosis [22] (Fig. 4).
Fig. 4.
Level 2 arthroscopy—laser ablation of a synovial polyp
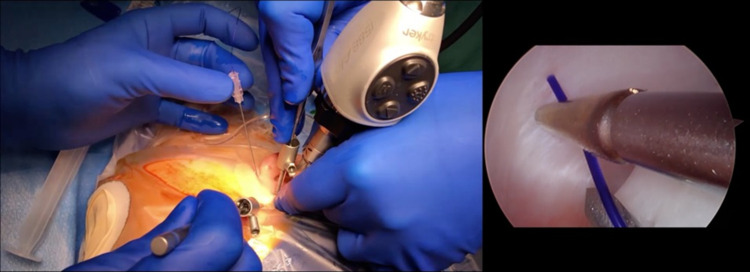
Level 3 Arthroscopy
Multiple cannulas allow for more the advanced techniques of disc repositioning and fixation, although success in the early reports of different arthroscopic disc repositioning techniques was not high [37–39]. Disc fixation can be accomplished by suture/wire discopexy or by more rigid fixation with either resorbable or titanium screws. It is ideally performed when there is sufficient posterior joint space without collapse and an articular disc that is displaced but does not show degenerative changes, perforation or significant changes in morphology. With these criteria in mind most patients who are suitable for arthroscopic disc repositioning fall into Wilkes II, III and occasionally early IV joint disease [40]. Given the success rates of Level 1 arthroscopy without disc repositioning, it is the opinion of the authors that Level 3 arthroscopy should be performed primarily for functional reasons, e.g. a mechanically obstructive click, closed lock or subluxation (Fig. 5).
Fig. 5.
Level 3 arthroscopy—suture discopexy
In McCain’s publication on arthroscopic discopexy [41], the success rate in 42 joints was 86.7% in Wilkes II and III but only 25% in Wilkes IV and V which emphasizes that case selection is a key element to success. Zhang and Yang [42] initially performed arthroscopic disc repositioning in 764 joints with MRI images taken after a week and reported success rates as high as 95.4%. They then used a modified version of Mc Cain’s technique and in their experience in 2622 joints over 10 years, performing partial and later complete release of the anterior disc attachment, reported better results in the latter part of their study [43]. However, although this study claimed excellent long-term results, they did not support it with MRI confirmation of stable disc repositioning.
Post-operatively, all patients notice malocclusion with slight mandibular deviation to the contralateral side after discopexy [43]. However, the majority of these malocclusions resolve within 2–3 weeks. Along with soft diet and parafunctional habit control, patients are instructed to perform “limited range of motion” exercises for the first 3 weeks to minimize the risk of the fixation failing or tearing through the disc. This is followed by daily stretching exercises. Associated myalgias may improve after arthroscopy, but often concomitant non-surgical treatment of the muscle disorder is also required.
A summary of progressive pathological changes, clinical features and their arthroscopic management options is summarized in Table 2.
Table 2.
| Stage | Pathology | Clinical features | Conservative management | Treatment |
|---|---|---|---|---|
| 1. Inflammation | Synovitis | ADD with reduction, clicking, pain, mouth opening normal |
Rule out systemic and local synovial joint disorder Education Rest NSAID Physiotherapy Orthotic appliance Identification and reduction of joint overload factors |
Level I arthroscopy |
| 2. Fibrosis | Proliferative synovitis, disc displacement with or without adhesion, synovial plicae | ADD without reduction, no clicking, pain, mouth opening reduced | Level I and II arthroscopy | |
| 3. Bony remodelling and disc migration | Disc displacement with or without adhesion, hyperplastic eminence, degenerative joint disease | ADD without reduction, pain, crepitus, MRI degenerative changes |
If sufficient posterior joint space—Level III arthroscopy If not—TJR |
Viscosupplementation
At the end of the arthroscopic procedure, there is the option of injecting medications including hyaluronic acid (HA) to restore the viscosity of the synovial fluid and platelet-rich plasma (PRP) for beneficial effects in joint degeneration and tendinopathy. However, both have shown conflicting results in the literature and so uncertainty exists regarding the effectiveness of viscosupplementation using hyaluronic acid and PRP in the TMJ [44–46].
Arthroscopy in Condylar Trauma
Use of arthroscopy in Acute TMJ trauma dates back to 1990 when Goss et al. [24] found that 38/40 condylar fractures had intra-articular soft tissue damage, haemarthrosis with disc shredding being the most common finding. Hirjak et al. [47] studied 29 condylar head fractures and found disc displacement in 26 joints, hyperaemia and hypervascularity in all joints, but no haemarthrosis or tear of the posterior band. Tripathi in 2015 [48] conducted an MRI study on the associated soft tissue injuries in condylar fractures, in which he found disc displacement in 37/54 joints, 12 capsular tears, 42 haemarthrosis and 5 disc perforations.
However, trauma as an indication of arthroscopy may be considered with a word of caution. The reasons are the uncertainty about the preexisting position and integrity of the disc and also the uncertainty whether the joint may adapt following trauma even in the presence of disc injury or displacement, thereby raising a question over the need for arthroscopy in the acute setting.
He et al. [49] opened 160 condylar head fractures and observed inferomedial displacement of the condylar segment and disc in 97.6% cases, adhesion of the disc in 23.1% and retrodiscal tissue tear with disc displacement 74.4% cases. The condylar fragments and the discs were reduced and fixed. Post-operative MRI was done only in 42 cases, 40 of which showed that the disc was reduced to its normal position.
Complications
They may include fluid extravasation, neurologic injury, intra-articular and retrodiscal haemorrhage, iatrogenic intra-articular joint surface scuffing, instrumental breakage, injury to the external auditory canal, tympanic membrane, middle ear ossicles, permanent hearing loss and infections.
A total of only 1.34% complication rate was found in a retrospective analysis of 670 arthroscopic procedures by Gonzaez-Garcia, with most being only lacerations of the external auditory canal, a lesion of the auriculotemporal nerve, paresis of the facial nerve and a case of alteration of visual acuity of the ipsilateral eye [50].
Open Joint Surgery and Arthroplasty
The effectiveness of minimally invasive procedures such as arthrocentesis and arthroscopy has significantly reduced the frequency and volume of open joint disc repositioning or discectomy surgeries.
McCarty and Farrar [1] first claimed disc repositioning success rates of 94% using a wedge resection and suture plication technique. However, other studies showed poor long-term stability of the suture plication techniques [51].
In 2001, Wolford reported a more rigid fixation open technique using a Mitek mini bone anchor to fixate the repositioned disc into the posterior condyle [52] after releasing the anterior and lateral disc attachments and its junction with the retrodiscal tissue. Although MRI evaluation of disc position was not done, it did result in significant reduction in pain, TMJ sounds and improved jaw function.
Zhou and He et al. used a self-drilling mini screw and performed a complete anterior release and over corrected the disc position for better stability in 149 joints. With their average follow-up of 23.4 months (12–84 months), they reported that 95.3% discs were still in position on post-operative MRI. They also reported new condylar bone formation in 74.5% of joints and even greater (90%) in young patients, suggesting that adolescents may have growth ability after disc repositioning [53].
For those patients with discs that are not salvageable, discectomy is the next step in the surgical pyramid. This involves removal of the disc and the area surrounding any perforation in the retrodiscal tissue and possible replacement of the disc as an option. Disc replacement options have been explored in attempts to reduce the crepitation arising out of remodelling effects on the condyle which radiologically appears as osteoarthrosis.
Many autogenous and alloplastic tissues have been used to replace the disc over the years but the long-term outcomes in pain and function appear to be similar to no disc replacement. The only advantage may be a reduction in the crepitation [54, 55]. The authors use abdominal fat for this purpose and Dimitroulis reported good results using abdominal dermal fat as an interpositional material [56]. In case of severe end-stage damage, total joint replacement then is indicated.
Disc Position Versus Function
In an MRI study by Moses in 92 patients both before and after arthroscopic surgery, consistently no change in disc position was found [57]. However, the study did reveal an increase in disc mobility following arthroscopic release, which was directly correlated with pain reduction and restoration of mandibular function.
Based on a review of the literature, there seems to be limited evidence that any surgical procedure, treatment, or appliance repositions and maintains the disc in a normal position [12]. The mobilization of tissues within the joint along with reduction of load enhances mesenchymal cell reprogramming, allowing adaptive formation of pseudodisc articulations and condylar remodelling. Although disc position may be indicative of pathologic history, its immobility appears to be more closely related to pathologic presence. Also, the chronicity of the patient’s history may lead to articular remodelling in the absence of pain and limitation of motion in the post-operative period [14].
Case Report
A 55-year-old female patient reported with pain in the left TMJ region since 5 years, during which time, she was conservatively treated for MPDS elsewhere. MRI was suggestive of minimal granulomatous changes with synovial effusion. With a past history of Tuberculosis, a provisional diagnosis of TB Granuloma was made. Arthroscopic examination revealed multiple yellowish nodules of varying sizes of 5–10 mm. Being too big for arthroscopic removal, the arthroscopy was converted into open joint surgery. Histopathological examination confirmed the diagnosis of synovial chondromatosis. These may not always be visible on CT/MRI, as the MRI did not show such a picture at all. Not only did the arthroscopy enable the diagnosis, but also, if they had been less than 2 mm, they could be removed arthroscopically.
This case underlines the importance of TMJ Arthroscopy in the surgical armamentarium to aid in diagnosis and treatment of TMJ disorders.
Present Status of TMJ Surgery in India and Training Opportunities
An online survey was conducted in India by the authors about the present status of TMJ surgery education, training and treatment options for internal derangement in India. A total of 596 surgeons responded, of which 503 were consultants, either in private practice or in teaching institutions. Of these 503, 89% felt confident in diagnosing ID, but almost 70% felt that their training in TMJ was poor or non-existent during their residency or later. Although 40% saw more than 10 patients with ID per month and 83% felt that minimally invasive surgery (arthrocentesis/arthroscopy) has a definite role in ID, only 4% perform arthroscopy. The most significant outcome of this survey was that 81% expressed interest in arthroscopy training. The survey performed depicted increasing interest in India in the field of TMJ arthroscopy and joint replacement in India.
Arthroscopy has been embraced by most countries throughout the world and for many is a first-line surgical intervention. In India though, it is just beginning to emerge; still lagging behind on account of expensive equipment and inadequate training. Although there are many 2–3-day training courses in arthroscopy around the world, the authors believe that reaching a safe level of competency in TMJ Arthroscopy takes much longer that a weekend course. A unique skill set is required for arthroscopy and a transfer of skills from open joint surgery is no substitute.
Unfortunately, there are few options available for comprehensive training courses. The TMJ Surgery Mini Residency in the USA is the only course of its kind in the world and provides an extensively mentored cadaveric hands-on training over four 3-day weekends (a total of 80 h of CE). This course provides the opportunity for extensive training in arthroscopy.
Along similar lines, the Amrita TMJ course was established in 2017 at Amrita Hospital, Kochi. A basic and an advanced course is offered over three days every year which teaches diagnosis and management of every aspect of TMJ disease including arthroscopy, total joint replacement and management of condylar trauma.
The Indian society of TMJ surgeons (ISTMJS) was formed in 2019 at Kochi to further the cause of TMJ education and training in India.
Conclusion
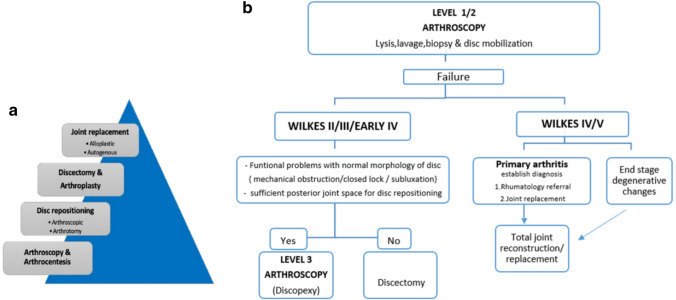
Clinicians must be diligent in establishing the correct diagnosis and cause of TMJID, which ultimately leads to the appropriate management of such patients. While many patients adapt over time or with non-surgical treatment, surgery may be indicated for those with ongoing problems. The surgical pyramid provides a stepwise progression for TMJ surgical patients (Fig. 6a, b).
Fig. 6.
a Surgical management, b surgical management algorithm
Currently, India is lagging behind in providing the full scope of TMJ services as there are very few surgeons trained in the skill of arthroscopic techniques. Excellent education and hands-on training courses do exist for those Oral and Maxillofacial Surgeons who want to provide arthroscopic temporomandibular joint surgery as an effective minimally invasive option for their patients. There needs to be continued expansion of our understanding of TMJID treatment including arthroscopic minimally invasive surgery in India to bring it level with the rest of the world.
Funding
This study was not supported by any funding.
Compliance with Ethical Standards
Conflict of interest
None of the authors has any conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McCarty WL, Farrar WB. Surgery for internal derangements of the temporomandibular joint. J Prosthet Dent. 1979;42(2):191–196. doi: 10.1016/0022-3913(79)90174-4. [DOI] [PubMed] [Google Scholar]
- 2.Bronstein SL, Thomas M. Arthroscopy of the temporomandibular joint. Philadelphia: W.B. Saunders Co.; 1991. pp. 347–350. [Google Scholar]
- 3.Sanders B, Buoncristiani R. Diagnostic and surgical arthroscopy of the temporomandibular joint: clinical experience with 137 procedures over a 2-year period. J Craniomandib Disord. 1987;1(3):202–213. [PubMed] [Google Scholar]
- 4.Moses JJ, Poker ID. TMJ arthroscopic surgery: an analysis of 237 patients. J Oral Maxillofac Surg. 1989;47(8):790–794. doi: 10.1016/s0278-2391(89)80035-7. [DOI] [PubMed] [Google Scholar]
- 5.McCain JP, Sanders B, Koslin MG, Quinn JH, Peters PB, Indresano AT, et al. Temporomandibular joint arthroscopy: a 6-year multicenter retrospective study of 4831 joints. J Oral Maxillofac Surg. 1992;50(9):926–930. doi: 10.1016/0278-2391(92)90047-4. [DOI] [PubMed] [Google Scholar]
- 6.Dimitroulis G. A review of 56 cases of chronic closed lock treated with temporomandibular joint arthroscopy. J Oral Maxillofac Surg. 2002;60(5):519–524. doi: 10.1053/joms.2002.31848. [DOI] [PubMed] [Google Scholar]
- 7.Kircos LT, Ortendahl DA, Mark AS, Arakawa M. Magnetic resonance imaging of the TMJ disc in asymptomatic volunteers. J Oral Maxillofac Surg. 1987;45(10):852–854. doi: 10.1016/0278-2391(87)90235-7. [DOI] [PubMed] [Google Scholar]
- 8.Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. 1996;54(2):147–153. doi: 10.1016/s0278-2391(96)90435-8. [DOI] [PubMed] [Google Scholar]
- 9.Muthukrishnan A, Sekar GS. Prevalence of TMDs in Chennai. J Indian Acad Oral Med Radiol. 2015;27(4):508. [Google Scholar]
- 10.Karthik R, Hafila MI, Saravanan C, Vivek N, Priyadarsini P, Ashwath B (2017) Assessing prevalence of temporomandibular disorders among university students: a questionnaire study. J Int Soc Prevent Communit Dent [serial online] 2017 [cited 2020 Sep 30] 7(Suppl S1):24–29 [DOI] [PMC free article] [PubMed]
- 11.Dimitroulis G. Temporomandibular joint surgery: what does it mean to India in the 21st century? J Maxillofac Oral Surg. 2012;11(3):249–257. doi: 10.1007/s12663-012-0419-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Israel HA. Internal derangement of the temporomandibular joint new perspectives on an old problem. Oral Maxillofac Surg Clin N Am. 2016;28:313–333. doi: 10.1016/j.coms.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Fac Pain Headache. 2014;28(1):6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moses JJ (2006) TMJ arthrocentesis and arthroscopy: rationale and techniques. In: Peterson’s principles of oral and maxillofacial surgery, pp 963–988
- 15.Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. 1934. Ann Otol Rhinol Laryngol. 1997;106:805–819. doi: 10.1177/000348949710601002. [DOI] [PubMed] [Google Scholar]
- 16.Lundh H, Westesson PL, Eriksson L, Brooks SL. Temporomandibular joint disk displacement without reduction. Treatment with flat occlusal splint versus no treatment. Oral Surg Oral Med Oral Pathol. 1992;73(6):655–658. doi: 10.1016/0030-4220(92)90003-9. [DOI] [PubMed] [Google Scholar]
- 17.Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc. 2006;137(8):1099–1107. doi: 10.14219/jada.archive.2006.0348. [DOI] [PubMed] [Google Scholar]
- 18.Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):212–223. doi: 10.1016/j.tripleo.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 19.Randolph CS, Greene CS, Moretti R, Forbes D, Perry HT. Conservative management of temporomandibular disorders: a posttreatment comparison between patients from a university clinic and from private practice. Am J Orthod Dentofacial Orthop. 1990;98(1):77–82. doi: 10.1016/0889-5406(90)70035-B. [DOI] [PubMed] [Google Scholar]
- 20.Sato S, Goto S, Nasu F, Motegi K. Natural course of disc displacement with reduction of the temporomandibular joint: changes in clinical signs and symptoms. J Oral Maxillofac Surg. 2003;61(1):32–34. doi: 10.1053/joms.2003.50005. [DOI] [PubMed] [Google Scholar]
- 21.Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res. 1998;77(2):361–365. doi: 10.1177/00220345980770020401. [DOI] [PubMed] [Google Scholar]
- 22.McCain JP, editor. Principles and practice of temporomandibular joint arthroscopy. St. Louis: Mosby; 1996. [Google Scholar]
- 23.Boering G (1966) Arthrosis deformans van het Kaakgewricht (thesis). University of Groninger, Groninger
- 24.Goss AN, Bosanquet AG. The arthroscopic appearance of acute temporomandibular joint trauma. J Oral Maxillofac Surg. 1990;48(8):780–783. doi: 10.1016/0278-2391(90)90330-5. [DOI] [PubMed] [Google Scholar]
- 25.Holmlund A (1990) Presented at the fifth international symposium on TMJ arthroscopy, Dec 2–4, 1990. New York
- 26.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49(11):1163–1167. doi: 10.1016/0278-2391(91)90409-f. [DOI] [PubMed] [Google Scholar]
- 27.Dimitroulis G, Dolwick MF, Martinez A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: a follow-up study. Br J Oral Maxillofac Surg. 1995;33(1):23–26. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 28.Hosaka H, Murakami K, Goto K, Iizuka T. Outcome of arthrocentesis for temporomandibular joint with closed lock at 3 years follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(5):501–504. doi: 10.1016/s1079-2104(96)80193-4. [DOI] [PubMed] [Google Scholar]
- 29.Murakami KI, Iizuka T, Matsuki M, Ono T. Recapturing the persistent anteriorly displaced disk by mandibular manipulation after pumping and hydraulic pressure to the upper joint cavity of the temporomandibular joint. Cranio. 1987;5(1):17–24. doi: 10.1080/08869634.1987.11678169. [DOI] [PubMed] [Google Scholar]
- 30.Sanromán JF. Closed lock (MRI fixed disc): a comparison of arthrocentesis and arthroscopy. Int J Oral Maxillofac Surg. 2004;33:344–348. doi: 10.1016/j.ijom.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Murakami K-I, Hoshino K. Regional anatomical nomenclature and arthroscopic terminology in human temporomandibular joints. Okajimas Folia Anat Jpn. 1982;58:4–6. doi: 10.2535/ofaj1936.58.4-6_745. [DOI] [PubMed] [Google Scholar]
- 32.McCain JP (1985) Proceedings of the abstract sessions, American association of oral and maxillofacial surgeons annual meeting. Washington, DC, September 1985
- 33.Gillquist J, Hagberg G. Findings of arthroscopy and arthrography in knee injuries. Acta Orthop Scand. 1978;49:398–402. doi: 10.3109/17453677809050095. [DOI] [PubMed] [Google Scholar]
- 34.Holmund A, Hellsing G. Arthroscopy of the temporomandibular joint—an autopsy study. Int J Oral Surg. 1985;14:169–175. doi: 10.1016/s0300-9785(85)80089-2. [DOI] [PubMed] [Google Scholar]
- 35.Moses JJ, Poker ID. TMJ arthroscopic surgery: an analysis of 237 patients. J Oral Maxillofac Surg. 1989;47:790–794. doi: 10.1016/s0278-2391(89)80035-7. [DOI] [PubMed] [Google Scholar]
- 36.Goss AN, Bosanquet A, Tideman H. The accuracy of temporomandibular joint arthroscopy. J Craniomaxillofac Surg. 1987;15:99. doi: 10.1016/s1010-5182(87)80026-4. [DOI] [PubMed] [Google Scholar]
- 37.McCain JP, Podrasky AE, Zabiegalski NA. Arthroscopic disc repositioning and suturing: a preliminary report. J Oral Maxillofac Surg. 1992;50(6):568–579. doi: 10.1016/0278-2391(92)90435-3. [DOI] [PubMed] [Google Scholar]
- 38.Zhu Y, Zheng C, Deng Y, Wang Y. Arthroscopic surgery for treatment of anterior displacement of the disc without reduction of the temporomandibular joint. Br J Oral Maxillofac Surg. 2012;50(2):144–148. doi: 10.1016/j.bjoms.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Goizueta-Adame CC, Pastor-Zuazaga D, Orts Bañón JE. Arthroscopic disc fixation to the condylar head. Use of resorbable pins for internal derangement of the temporomandibular joint (stage II–IV). Preliminary report of 34 joints. J Craniomaxillofac Surg. 2014;42(4):340–346. doi: 10.1016/j.jcms.2013.05.023. [DOI] [PubMed] [Google Scholar]
- 40.McCain JP, Hossameldin RH. Advanced arthroscopy of the temporomandibular joint. Atlas Oral Maxillofac Surg Clin. 2011;19:145–167. doi: 10.1016/j.cxom.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 41.McCain JP, Hossameldin RH, Srouji S, Maher A. Arthroscopic discopexy is effective in managing temporomandibular joint internal derangement in patients with Wilkes stage II and III. J Oral Maxillofac Surg. 2015;73(3):391–401. doi: 10.1016/j.joms.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 42.Zhang S-Y, Liu X-M, Yang C, Cai X-Y, Chen M-J, Haddad MS, et al. New arthroscopic disc repositioning and suturing technique for treating internal derangement of the temporomandibular joint: part II—magnetic resonance imaging evaluation. J Oral Maxillofac Surg. 2010;68(8):1813–1817. doi: 10.1016/j.joms.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 43.Yang C, Cai X-Y, Chen M-J, Zhang S-Y. New arthroscopic disc repositioning and suturing technique for treating an anteriorly displaced disc of the temporomandibular joint: part I—technique introduction. Int J Oral Maxillofac Surg. 2012;41(9):1058–1063. doi: 10.1016/j.ijom.2012.05.025. [DOI] [PubMed] [Google Scholar]
- 44.Ferreira N, Masterson D, Lopes de Lima R, de Souza Moura B, Oliveira AT, Kelly da Silva Fidalgo T, et al. Efficacy of viscosupplementation with hyaluronic acid in temporomandibular disorders: a systematic review. J Craniomaxillofac Surg. 2018;46(11):1943–1952. doi: 10.1016/j.jcms.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 45.Bouloux GF, Chou J, Krishnan D, Aghaloo T, Kahenasa N, Smith JA, et al. Is Hyaluronic acid or corticosteroid superior to lactated ringer solution in the short term for improving function and quality of life after arthrocentesis? Part 2. J Oral Maxillofac Surg. 2017;75(1):63–72. doi: 10.1016/j.joms.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 46.Haigler MC, Abdulrehman E, Siddappa S, Kishore R, Padilla M, Enciso R. Use of platelet-rich plasma, platelet-rich growth factor with arthrocentesis or arthroscopy to treat temporomandibular joint osteoarthritis: systematic review with meta-analyses. J Am Dent Assoc. 2018;149(11):940–942. doi: 10.1016/j.adaj.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 47.Hirjak D, Galis B, Beno M, Machon V, Mercuri LG, Neff A. Intraoperative arthroscopy of the TMJ during surgical management of condylar head fractures: a preliminary report. J Cranio-Maxillofac Surg. 2017 doi: 10.1016/j.jcms.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 48.Tripathi R, Sharma N, Dwivedi AN, Kumar S. Severity of soft tissue injury within TMJ following condyle fracture as seen on MRI and their impact on outcome of functional management. J Oral Maxillofac Surg. 2015 doi: 10.1016/j.joms.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 49.Chen M, Yang C, He D, Zhang S, Jiang B. Soft tissue reduction during open treatment of intracapsular condylar fracture of the temporomandibular joint: our institution's experience. J Oral Maxillofac Surg. 2010;68:2189–2195. doi: 10.1016/j.joms.2009.09.063. [DOI] [PubMed] [Google Scholar]
- 50.González-García R, RodríguezCampo FJ, Escorial-Hernández V, Muñoz-Guerra MF, et al. Complications of temporomandibular joint arthroscopy: a retrospective analytic study of 670 arthroscopic procedures. J Oral Maxillofac Surg. 2006;64:1587–1591. doi: 10.1016/j.joms.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 51.Walker RV, Kalamchi S. A surgical technique for management of internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 1987;45(4):299–305. doi: 10.1016/0278-2391(87)90347-8. [DOI] [PubMed] [Google Scholar]
- 52.Mehra P, Wolford LM. The Mitek mini anchor for TMJ disc repositioning: surgical technique and results. Int J Oral Maxillofac Surg. 2001;30(6):497–503. doi: 10.1054/ijom.2001.0163. [DOI] [PubMed] [Google Scholar]
- 53.Zhou Q, Zhu H, He D, Yang C, Song X, Ellis E. Modified temporomandibular joint disc repositioning with mini-screw anchor: part II—stability evaluation by magnetic resonance imaging. J Oral Maxillofac Surg. 2019;77(2):273–279. doi: 10.1016/j.joms.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 54.HolrMund AB, Axelsson S. Temporomandibular arthropathy: correlation between clinical signs and symptoms and arthroscopic findings. Int J Oral Maxillofac Surg. 1996;25:178–181. doi: 10.1016/s0901-5027(96)80024-5. [DOI] [PubMed] [Google Scholar]
- 55.McKenna SJ. Discectomy for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2001;59:1051–1056. doi: 10.1053/joms.2001.26682. [DOI] [PubMed] [Google Scholar]
- 56.Dimitroulis G. A critical review of interpositional grafts following temporomandibular joint discectomy with an overview of the dermis-fat graft. Int J Oral Maxillofac Surg. 2011;40:561–568. doi: 10.1016/j.ijom.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 57.Moses JJ, Poker I. Correlation studies of effects of TMJ arthroscopic surgical lysis of superior joint compartment adhesions and lavage. J Oral Maxillofac Surg. 1989;47:674–678. doi: 10.1016/s0278-2391(89)80004-7. [DOI] [PubMed] [Google Scholar]