Abstract
Purpose
The aim of this study is to clinically and radiographically evaluate the stability of parasymphysis fracture managed with lag screws, miniplates and 3D miniplates.
Materials and Method
Ninety- eight patients diagnosed with parasymphysis fracture were treated using lag screws in group 1, two 4-hole miniplates in group 2 and 3D miniplates in group 3. Intraoperative stability and duration of fixation was assessed. Postoperative clinical evaluation was done at 1 week, 1 month, 3rd month, 6th month and 1 year for complications and oral function. Radiological evaluation was done at 3rd and 6th month. Only 92 patients were considered for statistical analysis since 6 patients were lost during follow-up.
Results
Road traffic accident (65.3%) was the primary cause of mandibular fractures. Postoperative pain score showed a statistically significant difference after 1 week and 1 month duration (P value < 0.001). ANOVA test showed VAS was significantly higher at pre-op followed by 1st day and 1 week, but no significant difference after 3 months in all groups. Radiographic analysis did not show significant difference in approximation of fracture segment among 3 groups after 6 months (P-value = 0.117). Chewing efficiency at 6 months and occlusion by surgeon evaluation at 3 months showed a significant difference (P value < 0.001).
Conclusion
Lag screw fixation was technique-sensitive, relatively inexpensive and was less time consuming method when compared to miniplates and 3D plates. Lag screws and 3D plates are superior in reducing the incidence of complications and better in oblique or sagitally displaced mandibular fractures.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12663-021-01647-5.
Keywords: Parasymphysis fracture, Lag screws, Conventional miniplates, Three-dimensional miniplates, Occlusion
Introduction
Maxillofacial region is associated with several important functions of daily life. The present modernization has led to increasing incidences of traumatic injuries to the maxillofacial skeleton as a result of road traffic accidents. Mandible is the second most commonly fractured bone of the maxillofacial skeleton after zygoma because of its position and prominence [1, 2]. In mandible, management of fractures particularly in the parasymphysis region is challenging due to its unique anatomy in the shape of parabola, blood supply, muscular attachments, curvature and thickness of cortical plates [1, 2].
Schede initially applied the concept of rigid internal fixation to the facial skeleton in 1888 [3]. Lag screws were introduced in the management of maxillofacial trauma in 1970 by Brons and Boering [4]. Principle of lag screw is based on axial compression of bone fragments where forces of functional loading are counterbalanced by thick bicortical screws. In 1973, Michelet et al. used small easily bendable, non-compression miniplates with monocortical screws for mandibular fractures [5]. Champy’s method of semirigid fixation uses adaptable monocortical miniplate along the “ideal osteosynthesis line.” Shortcomings of lag screws and miniplates led to the development of 3D (three-dimensional) miniplates by Mustafa Farmand in 1992 [6]. Considering the advantages and disadvantages of rigid and semirigid fixation techniques, this study was intended to compare the efficacy of lag screws, miniplates and 3D plates in the treatment of mandibular parasymphysis fractures.
Materials and Methods
In total, 163 patients were assessed for eligibility to participate in the study. Sixty-five patients were excluded from the study due to various reasons. Remaining 98 patients were randomly allocated into each group. Patients with isolated parasymphysis fracture of mandible without gross comminution of the fracture segments was included. Patients with large hematoma, severely infected fractures and grossly comminuted fractures with extensive damage of fractured bony segments, medically compromised condition and with any associated bone pathology were excluded from the study. Erich’s arch bars were placed preoperatively in all the patients. Preoperatively, all patients were given prophylactic antibiotics and were operated by the same surgical team under either general anesthesia or local anesthesia.
Patients were explained about the three fixation systems available and were blinded for the type of device used. Two lag screws with either of the sizes 2 × 16 mm, 2 × 18 mm were used based on the clinical necessity in group 1 (33) (Fig. 1). Two 4-hole with gap stainless steel miniplates were used in group 2 (34) with 2 × 8 mm monocortical screws (Fig. 2). Four-hole 3D stainless steel miniplates were used in group 3 (31), with 2 × 8 mm screws (Fig. 3). Six patients did not turn for follow-up, so 92 patients were analyzed and evaluated for different statistical variables. Intraoperatively, stability and duration of fixation (time from the initiation of exposure of fracture site till the completion of fixation) were assessed.
Fig. 1.
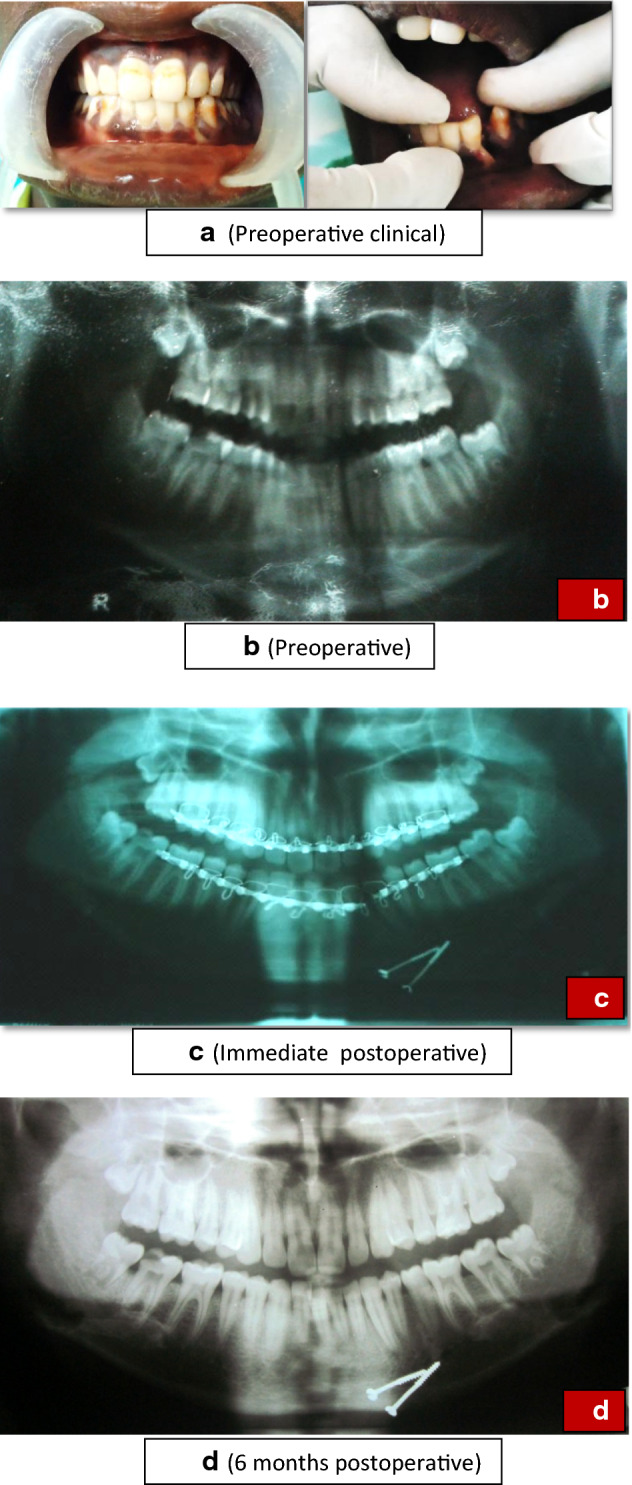
Lag screw group. a Preoperative clinical picture of lag screw group. b Preoperative radiograph of patient treated with lag screws. c Immediate postoperative radiograph of patient treated with lag screws. d 6 months postoperative radiograph of patient treated with lag screws
Fig. 2.
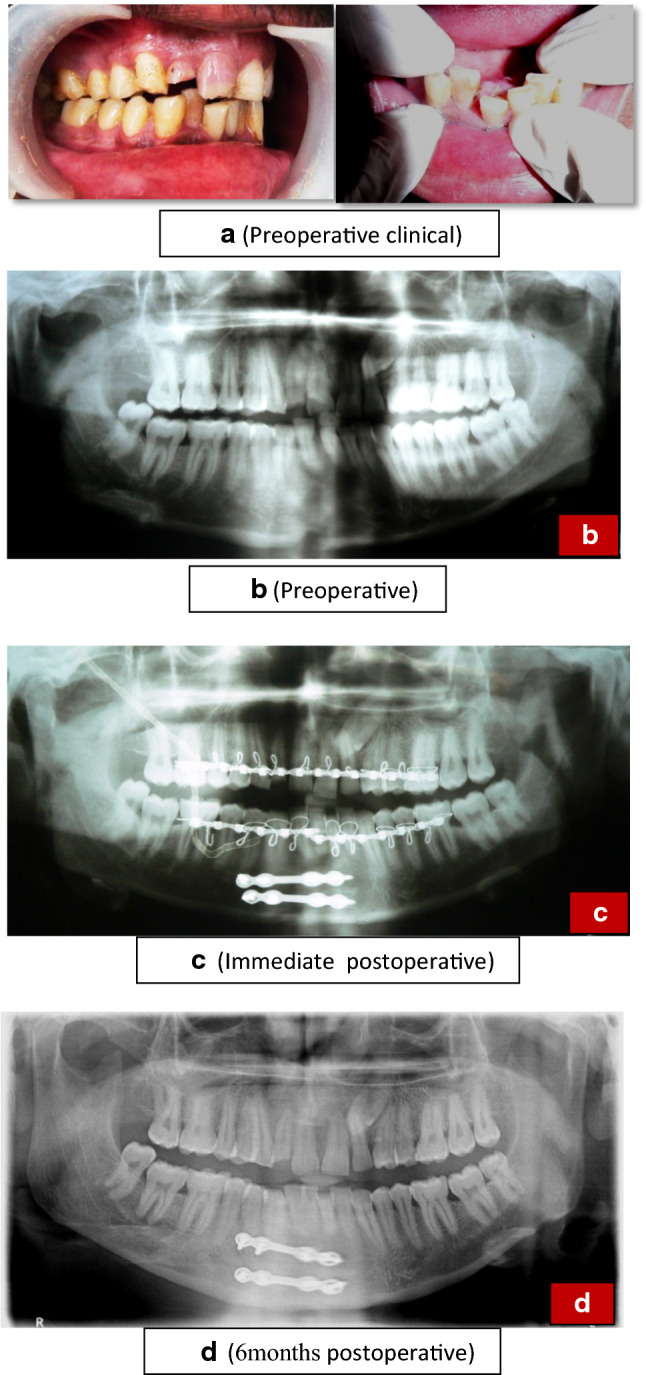
Miniplate group. a Preoperative clinical picture of miniplate group. b Preoperative radiograph of patient treated with miniplates. c Immediate postoperative radiograph of patient treated with miniplates. d 6 months postoperative radiograph of patient treated with miniplates
Fig. 3.
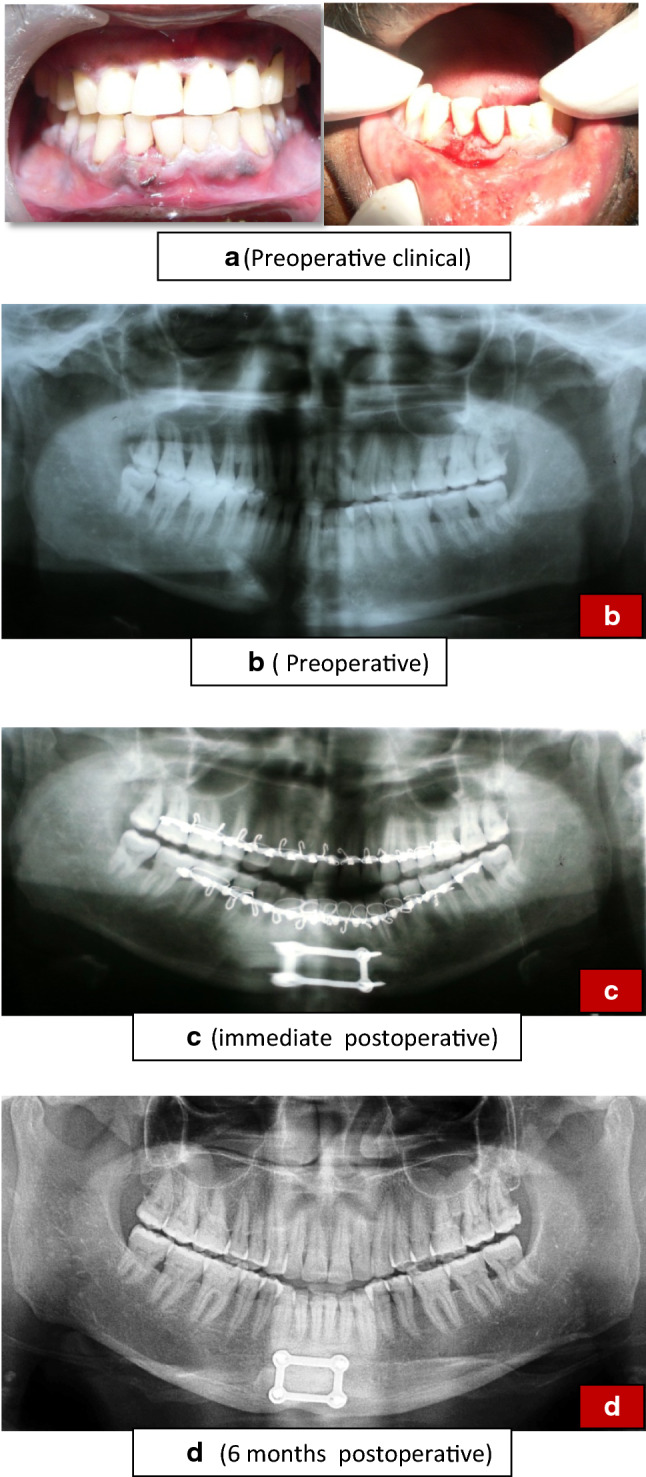
3D miniplate group. a Preoperative clinical picture of 3D plate group. b Preoperative radiograph of patient treated with 3D miniplates. c Immediate postoperative radiograph of patient treated with 3D miniplates. d 6 months postoperative radiograph of patient treated with 3D miniplates
Postoperative assessment was done by one of the clinicians who were not a part of the surgical team and were blinded for the type of device used for fixation of parasymphysis fracture. Patients were analyzed at 1st week, 4th week, 3rd month, 6th month and 1 year for complications like pain, infection, wound dehiscence, neurological deficit, mobility of fragments, plate fracture. Evaluation for neurological deficit was done by 2-point discrimination and pinprick tests. Evaluation of osteosynthesis (infection, plate fracture, mobility of fracture segments, chewing, occlusion and interincisal opening) was done by using the treatment scoring system given by Uglesic in 1993 [7]. Proper intercuspation was considered to be a good occlusion while an open bite or step in the occlusion was considered as major occlusal discrepancy while a gap of less than 3 mm between intercuspation was considered as minor occlusal discrepancy. Self-evaluation of chewing was analyzed based on scoring system given by V Uglesic. −5 points: not able to chew, 0 points: on soft diet, + 3 points: on normal diet, but can chew only on one side, + 5 points: on normal diet. Radiologically, approximation of the fracture segment (decrease in fracture gap, displacement or no displacement), screw loosening, plate fracture, bone healing (reduction in fracture gap), adverse reactions in screw vicinity were assessed in OPG for 3 groups, and occlusal radiograph was also taken in case of lag screws for evaluating proper anatomic reduction.
Results
This study consisted of 83 male and 9 female patients. Road traffic accident was the common cause of mandibular fractures accounting for 60 (65.3%) cases, followed by fall in 14 (15.2%) cases, assault in 14 (15.2%) cases and occupational trauma in 4 (4.3%) case. ANOVA with post hoc Tukey’s test compared the duration and fixation time among 3 groups (Table 1). Group 2 had highest mean duration followed by Group 3 with least being Group 1. Mean time in Group 1, Group 2 and Group 3 was 5.13 min, with a standard deviation of 0.85, 11.23 min with a standard deviation of 1.78 and 9.23 min with standard deviation of 1.48, respectively (P value < 0.001).
Table 1.
Comparision of duration of fixation, pain score and mouth opening among Lag screw, Miniplate and 3D miniplate groups
| Lag screws | Miniplates | 3D miniplates | F-value | P-value | |
|---|---|---|---|---|---|
| Mean SD | Mean SD | Mean SD | |||
| Duration of fixation (minutes) | 5.13 ± 0.85 | 11.23 ± 1.78 | 9.23 ± 1.45 | 149.637 | < 0.001 |
| VAS pre-op | 6.81 ± 1.08 | 6.97 ± 1 | 6.84 ± 1.41 | .156 | .855 |
| VAS 1 day post-op | 3.42 ± 0.50 | 3.97 ± 1.40 | 3.32 ± 0.80 | 3.911 | .024 |
| VAS 1 week post-op | 1.71 ± 0.64 | 2.53 ± 0.81 | 1.81 ± 0.60 | 12.817 | < 0.001 |
| VAS 1 month post-op | 0.52 ± 0.50 | 1.40 ± 0.97 | 0.81 ± 0.60 | 11.994 | < 0.001 |
| VAS 3 month post-op | 0 ± 0 | 0.10 ± 0.40 | 0 ± 0 | 1.914 | .153 |
| VAS 6 month post-op | 0 ± 0 | 0 ± 0 | 0 ± 0 | 0 | 0 |
| Mouth opening 6 months post-op | 40.52 ± 1.46 | 39.83 ± 1.62 | 39.90 ± 1.23 | 2.049 | .135 |
After 1 week, postoperative infection was noticed in 4 patients in Group 2 (P-value = 0.041). Soft tissue infection was noticed in these patients and managed with antibiotics and analgesics. In one of these patients, postoperatively arch bars were removed after 15 days of surgery upon patient insistence and eyelet wiring was done after 20th post-op day and was put on IMF for stabilization of fracture. After 1 month all the patients in 3 groups showed no signs of infection. Pain score showed a statistically significant difference postoperatively after 1 week and 1 month duration (P value < 0.001). ANOVA test showed that the VAS was significantly higher preoperatively followed by 1st day and 1 week, but no significant difference was noticed after 3 months in all the groups (Table 1). This difference is attributed to immediate postoperative infection in 4 patients in Group 2. None of the patients revealed neurological deficit.
Postoperative radiographic assessment showed properly reduced fracture segments with gradual bone healing and disappearance of the fracture line by 6 months in all patients. Statistical analysis did not show significant difference of approximation of fracture segment among 3 groups after 6 months (P-value = 0.117). Preoperative interincisal opening in most of the patients in all the 3 groups had moderate mouth opening (16–30 mm). Postoperatively there is a gradual increase in mouth opening during follow-up visits. No statistically significant difference was observed among the 3 groups. Postoperative evaluation of osteosynthesis was done using ANOVA with post hoc Tukey’s test (Table 2). Chewing efficiency at 6 months and occlusion evaluation by surgeon at 3 months showed a significant difference (P value < 0.001).
Table 2.
Evaluation of osteosynthesis among Lag screw, Miniplate and 3D miniplate groups by treatment scoring system
| Scoring criteria | Lag screws | Miniplates | 3D miniplates | X2 value | P-value | |
|---|---|---|---|---|---|---|
| Complication at 1 week | 0 | 31 | 27 | 31 | 6.409 | 0.041 |
| − 1 | 0 | 3 | 0 | |||
| − 2 | 0 | 0 | 0 | |||
| − 3 | 0 | 0 | 0 | |||
| − 5 | 0 | 0 | 0 | |||
| Complication at 1 month | 0 | 31 | 28 | 31 | 4.225 | .376 |
| − 1 | 0 | 1 | 0 | |||
| − 2 | 0 | 0 | 0 | |||
| − 3 | 0 | 0 | 0 | |||
| − 5 | 0 | 1 | 0 | |||
| Complication at 3 months | 0 | 0 | 0 | 0 | 0 | 0 |
| Chewing at 3 months | − 5 | 0 | 3 | 0 | 13.782 | .008 |
| 0 | 0 | 6 | 0 | |||
| + 3 | 6 | 3 | 6 | |||
| + 5 | 25 | 21 | 25 | |||
| Chewing at 6 months | − 5 | 0 | 0 | 0 | 13.265 | .001 |
| 0 | 0 | 6 | 0 | |||
| + 3 | 0 | 6 | 0 | |||
| + 5 | 31 | 24 | 31 | |||
| Occlusion—surgeon at 3 months | − 5 | 0 | 0 | 0 | 21.781 | .00 |
| − 3 | 0 | 0 | 0 | |||
| + 1 | 0 | 6 | 0 | |||
| + 3 | 3 | 9 | 3 | |||
| + 5 | 28 | 15 | 28 | |||
| Occlusion—self at 3 months | − 5 | 0 | 0 | 0 | 13.782 | .008 |
| − 3 | 0 | 0 | 0 | |||
| + 1 | 0 | 6 | 0 | |||
| + 3 | 6 | 3 | 6 | |||
| + 5 | 25 | 21 | 25 | |||
| Occlusion—surgeon at 6 months | − 5 | 0 | 0 | 0 | 6.910 | .032 |
| − 3 | 0 | 0 | 0 | |||
| + 1 | 0 | 0 | 0 | |||
| + 3 | 3 | 6 | 0 | |||
| + 5 | 28 | 24 | 31 | |||
| Occlusion—self at 6 months | − 5 | 0 | 0 | 0 | .005 | .997 |
| − 3 | 0 | 0 | 0 | |||
| + 1 | 0 | 0 | 0 | |||
| + 3 | 6 | 6 | 6 | |||
| + 5 | 25 | 24 | 25 |
Discussion
Management of parasymphysis fractures is always challenging due to its unique anatomy, blood supply, muscular attachments, curvature and thickness of cortical plates [8]. Concepts of tension at superior border and compression at inferior border hold true for body and angle fractures due to the action of masseter and temporalis muscles; this concept is inverted for parasymphysis fractures due to the action of suprahyoid musculature [9], and thus, unique biomechanical behavior can be expected with the point of rotation about the condyle [10]. The present study was done to compare the outcome of parasymphysis fracture managed with 3 different fixation systems available in the literature, i.e., lag screws, miniplates and 3D plates.
The male dominance in the present study was also reported by Haug et al. [11]. RTA (35.6%) was the primary cause of parasymphysis fracture followed by fist fights (31.8%), occupational (11.6%) and sports injuries (3.3%). This was similar to the findings in previous studies [12]. Intraoperatively, time duration for miniplate fixation was higher compared to 3D plate and lag screw fixation. This was due to time taken in contouring the miniplates and application of additional screws to stabilize the fracture. Ellis and Ghali [13], and Schaaf et al. [14] also reported that lag screws could be applied more rapidly than miniplates. But, miniplates were easily maneuverable in case of fractures running through mental foramina, in which plates were placed superior and inferior to the foramina and proved to be more advantageous over 3D miniplates and lag screws.
Average preoperative pain score was similar in all groups. Significant difference was noticed postoperatively after 1 week and 1 month among three groups, because 4 patients in Group 2 had infection at the surgical site and was managed by antibiotics and analgesics. CDC and Johnson et al.’s [15] criteria were used for evaluating surgical site infection in our study. The literature reveals that ORIF is associated with 3% to 32% of postoperative infection. [16] Few studies reported incidence of infection with 3D plates as 5.4—9% and 2.4—11.7% for lag screws. [17, 18] The current study reported 0% incidence of infection in lag screws and 3D plates.
Postoperatively, 15 patients in Group 2 had minor occlusal discrepancy which was corrected by placing guiding elastics for a period of 2 weeks. But, one patient was put on IMF with the help of eyelet wiring as arch bars were removed postoperatively after 15 days. Postoperative occlusion was satisfactory in all patients of Groups 1, 2 and 3 after 3 months. Minor occlusion discrepancy was reported in 9 out of 30 patients treated with lag screw fixation in a study by Zacharaides et al. [19]. This was due to inability to place the second screw exactly perpendicular to the fracture line which results in malocclusion. So, lag screws should always be placed perpendicular to the bevel of the fracture to prevent displacement of fragments when screws are tightened and the bones are compressed.
Neurological deficit was not seen in any of the patients in our study but some studies revealed 2% neurological deficit following the parasymphysis fracture management with various fixation devices [15, 20, 21]. Previous studies revealed incidence of wound dehiscence to be 3.4% in miniplate group, 1.2% in lag screw group [4, 9, 13] and 0% in 3D plates [22, 23]. Complication rates of lag screw osteosynthesis range approximately 2.4% to 11.7% and 3.8% to 28% for miniplates and 0% to 10% for 3 D plates [2, 3, 24–29]. A meta-analysis showed that lag screw is superior to miniplates in reducing the incidence of postoperative complications [30].
Recently, an in vitro study has evaluated the biomechanical behavior of four different types of rigid fixation systems with semirigid fixation system and proposed that 3D struts plates had greater resistance to compression loads than the miniplates [31]. In contrast to this, lag screw facilitates more accurate reduction, good stability, rigidity and less operating time and early functional improvement [32].
According to Uglesic [7], the success of mandibular fracture osteosynthesis depends on the incidence of complications and the ability of fractured jaw to resume normal oral functions and we used these treatment scoring criteria to evaluate the outcome of patients in our study. Results in our study showed some incidence of complications immediately after surgery in miniplate group, but over a long period of time all the three fixation devices proved to be effective in restoring normal oral function by showing clinical improvement in occlusion, chewing efficiency and mouth opening. Results of the present study suggest that fixation of mandibular parasymphysis fracture with 3D plates and lag screws would give a promising outcome with less number of complications in simple oblique fractures with minimal or no displacement and miniplates would be the viable option in case of fracture running through the mental foramina.
Conclusion
Lag screws, miniplates and 3D plates were found to restore normal anatomic function of mandibular parasymphysis fracture in long run. But the major difference is duration of fixation and postoperative complications as seen in our study. Lag screws and 3D plates are better in oblique or sagitally displaced mandibular fractures in which they were quicker to apply and allow early functional improvement than conventional miniplates. Conventional miniplates proved to be better in case of comminution and fractures running through mental foramina. Considering the stress shielding effect of lag screws and extended time duration for fixing the miniplates, one can choose the fixation device by weighing the risks over benefits.
Supplementary Information
Below is the link to the electronic supplementary material.
Authors contribution
RKS conceived and designed the study/review/case series, gave the final approval of the manuscript and is the guarantor of the manuscript. RKS and AKV acquired the data did laboratory or clinical/literature search. RS drafted the article and/or critical revision. UKU analyzed and interpreted the data collected.
Funding
None.
Declarations
Conflict of interest
The authors declare that they have no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Uppada UK, Sinha R, Susmitha M, Praseedha B, Kiran BR (2020) Mandibular fracture patterns in a rural setup: a 7-year retrospective study. J Maxillofac Oral Surg In Press [DOI] [PMC free article] [PubMed]
- 2.Kumar SR, Sinha R, Uppada UK, Reddy BVR, Paul D. Mandibular third molar position influencing the condylar and angular fracture patterns. J Maxillofac Oral Surg. 2015;14(4):956–961. doi: 10.1007/s12663-015-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dorrance G, Bransfield J, Mann J (1941) The history of treatment of fractured jaws. Privately published, Philadelphia
- 4.Kallela I, llzuka T, Laine P et al (1996) Lag-screw fixation of mandibular parasymphyseal and angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 81:510–516 [DOI] [PubMed]
- 5.Michelet FX, Deymes J. Osteosynthesis with miniaturized screwed plates in maxillofacial surgery. J Oral Surg. 1973;1:79–84. doi: 10.1016/s0301-0503(73)80017-7. [DOI] [PubMed] [Google Scholar]
- 6.Farmand M, Dupoirieux L. The value of 3-dimensional plates in maxillofacial surgery. Rev Stomatol Chir Maxillofac. 1992;93(6):353–357. [PubMed] [Google Scholar]
- 7.Uglesic V, Virag M, Aljinovic N, et al. Evaluaion of mandibular fracture treatment. J Cranio-Maxillofac Surg. 1993;21(6):251–257. doi: 10.1016/S1010-5182(05)80042-3. [DOI] [PubMed] [Google Scholar]
- 8.Matthew JM, Christopher AM, Richard HH (2008) A biomechanical evaluation of plating techniques used for reconstructing mandibular symphysis/parasymphysis fractures. J Oral Maxillofac Surg 66:2012–2019 [DOI] [PubMed]
- 9.Dhananjay HB, Anupama M, Fareedi MA et al (2014) Efficacy of 3-dimensional plates over Champys miniplates in mandibular anterior fractures. J Int Oral Health 6(1):20–26 [PMC free article] [PubMed]
- 10.Rudderman RH, Mullen RL. Biomechanics of the facial skeleton. Clin Plast Surg. 1992;19:11. doi: 10.1016/S0094-1298(20)30893-2. [DOI] [PubMed] [Google Scholar]
- 11.Haug RH, Prather J, Indrasano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926. doi: 10.1016/0278-2391(90)90004-L. [DOI] [PubMed] [Google Scholar]
- 12.Schuchardt K, Schwenzer N, Rottke B et al (1966) Ursachen Haufigkeit und Lokalisation der Frakturen des Gesichtsschadels. Fortschr. 11: 1–6 [PubMed]
- 13.Ellis E, Ghali GE (1991) Lag screw fixation of anterior mandibular fractures. J Oral Maxillofac Surg 49(1):13–21; discussion 21–2 [DOI] [PubMed]
- 14.Schaaf H, Kaubruegge S, Streckbein P, et al. Comparison of miniplate versus lag screw for fractures of the mandibular angle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:34–40. doi: 10.1016/j.tripleo.2010.03.043. [DOI] [PubMed] [Google Scholar]
- 15.Jain MK, Manjunath KS, Bhagwan BK, et al. Comparison of 3-dimensional and standard miniplate fixation in the management of mandibular fractures. J Oral Maxillofac Surg. 2010;68:1568–1572. doi: 10.1016/j.joms.2009.07.083. [DOI] [PubMed] [Google Scholar]
- 16.William of Saliceto (1982) Chirurgia. In: Arschirurgicaguidonischauliacivenetiis. Pp 303–361. Cited from Kruger E and Schilli W. Oral and Maxiloofacial Traumatology. Vol I; Quintessence, p 23
- 17.Guimond C, Johnson JV, Marchena JM (2005) Fixation of mandibular angle fractures with a 2.0 mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg 63:209–214 [DOI] [PubMed]
- 18.Feledy J, Caterson Edward J, Shon S et al (2004) Treatment of mandibular angle fractures with a matrix miniplate: a preliminary report. Plast Reconstr Surg 114:1711–1718 [DOI] [PubMed]
- 19.Zacharaides N, Mezitis M, Papademetrion I. Use of lag screws for the management of mandibular trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:164. doi: 10.1016/S1079-2104(96)80407-0. [DOI] [PubMed] [Google Scholar]
- 20.Emam and Stevens Can an arch bar replace a second lag screw in management of anterior mandibular fractures? J Oral Maxillofac Surg. 2012;70:378–383. doi: 10.1016/j.joms.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Ellis E. Is lag screw fixation superior to plate fixation to treat fractures of the mandibular symphysis? J Oral Maxillofac Surg. 2012;70:875–882. doi: 10.1016/j.joms.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 22.Khalifa ME, El-Hawary HE, Hussein MM (2012) Titanium three dimensional miniplate versus conventional titanium miniplate in fixation of anterior mandibular fractures. Life Sci J 9(2)
- 23.Gear AJL, Apasova E, Schmitz JP et al (2005) Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg 63:655–663 [DOI] [PubMed]
- 24.Bhatnagar A, Bansal V, Kumar S, et al. Comparative analysis of osteosynthesis of mandibular anterior fractures following open reduction using stainless steel lag screws and mini plates. J Maxillofac Oral Surg. 2013;12(2):133–139. doi: 10.1007/s12663-012-0397-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cawood JI. Small plate osteosynthesis of mandibular fractures. Br J Oral Maxillofac Surg. 1985;23:77–91. doi: 10.1016/0266-4356(85)90057-9. [DOI] [PubMed] [Google Scholar]
- 26.Smith WP. Delayed miniplate osteosynthesis for mandibular fractures. Br J Oral Maxillofac Surg. 1991;29:73–76. doi: 10.1016/0266-4356(91)90083-H. [DOI] [PubMed] [Google Scholar]
- 27.Pavan Kumar B, Jeevan Kumar, Mohan AP et al (2012) A comparative study of three dimensional stainless steel miniplates in the management of mandibular Parasymphysis fracture. J Biol Innov 1(2):19–32
- 28.Hughes PJ. 3D plate versus the lag screw technique for treatment of fractures of anterior mandible. J Oral Maxillofac Surg. 2000;58:23. doi: 10.1016/S0278-2391(00)80008-7. [DOI] [Google Scholar]
- 29.Mohd YQ, Reddy S, Sinha R, Agarwal A, Fatima U, Abidullah M. Three dimensional miniplate: for the management of mandibular parasymphysis fractures. Ann Maxillofac Surg. 2019;9(2):333–339. doi: 10.4103/ams.ams_172_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wusiman P, Taxifulati D, Weidong L, Moming A. Three-dimensional versus standard miniplate, lag screws versus miniplates, locking plate versus non-locking miniplates: management of mandibular fractures, a systematic review and meta analysis. J Dent Sci. 2019;14(1):66–80. doi: 10.1016/j.jds.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alkan A, Celebi N, Ozden B, et al. Biomechanical comparision of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:752–756. doi: 10.1016/j.tripleo.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Jadwani S, Bansod S. Lag screw fixation of fracture of the anterior mandible: a new minimal access technique. J Maxillofac Oral Surg. 2011;10(2):176–180. doi: 10.1007/s12663-011-0176-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


