Abstract
Objectives
Temporomandibular joint disorders (TMDs) are progressive disorders which lead to development of arthralgia and functional disabilities of temporomandibular joint. The treatment of the TMDs is controversial; noninvasive and minimally invasive therapies have shown a success rate of 70 to 85% for its management. The objective of present study is to evaluate and compare the efficacy of intra-articular platelet-rich plasma (PRP) and arthrocentesis in management of TMDs.
Materials and Methods
Twenty-four patients with complaint of reduced mouth opening, joint noise, pain, jaw deviation, not responding to medicinal treatment and coming under group II/III of RDC/TMD were included. Patients were randomly and equally divided in two groups. In group A, arthrocentesis was performed, whereas group B patients underwent intra-articular injections of PRP. Patients were clinically evaluated preoperatively to 12 months postoperatively.
Result
Both the groups showed significant improvement in painless mouth opening (P < 0.01), lateral movements towards unaffected side (P < 0.05) and reduction in pain complaint (P < 0.01). Arthrocentesis group also showed significant improvement in maximum mouth opening (P < 0.01).
Conclusion
On comparison, both groups were found to have effective treatment modality. However, arthrocentesis has higher success rate for pain elimination, and PRP is more effective in correction of joint noise and jaw deviation.
Keywords: Temporomandibular joint disorders, Arthrocentesis, Platelet-rich plasma, PRP, Minimally invasive surgery, TMJ pain
Introduction
Temporomandibular joint (TMJ) is a compound joint, including temporal bone, mandible, numerous musculatures, articular disc and ligaments [1]. Temporomandibular joint disorders (TMDs) are progressive painful conditions and can manifest as limited range of mandibular motion, deviation or deflection upon mouth opening, locking of mouth, joint tenderness and clicking or crepitus [2].
Many aetiological factors are related to development of TMDs such as trauma, bruxism, clenching, occlusal abnormalities and orthodontic treatment. These factors cause repetitive microtrauma which leads to bleeding in joint, effusion and decrease in lubrication [3]. According to data, TMDs are found in 40–60% of general population, are more common in females and commonly affects 20 to 40 years of age group [3, 4].
TMDs were classified in 1992 as Research Diagnostic Criteria (RDC/TMD), which is broadly divided in three groups: muscles disorders (group I), disc displacement disorders (group II) and other TMJ disorders such as osteoarthritis and arthrosis (group III) [5].
The treatment of the TMDs is controversial, which has been divided into three categories: nonsurgical, minimally invasive and surgical. Nonsurgical methods have reported to cure 70% of TMDs, and these generally include soft food diet, behaviour modification, pharmacotherapy, physiotherapy, inter-occlusal splints and transcutaneous electrical nerve stimulation therapy [6]. Minimally invasive therapies include arthrocentesis, arthroscopic lysis and lavage and intra-articular injections of steroids, hyaluronic acid (HA) or material with regenerative properties such as platelet-rich plasma (PRP). Steroids have been reported to provide only anti-inflammatory property and are prone to cause irreversible damage to articular cartilage [7]. HA provides lubrication to the joint cartilage and have reported 70% success rate [8]. Various studies have reported that efficacy of PRP is better than HA [9, 10]. The last therapeutic resort remains with surgical management which includes disc or capsule tightening procedures, repair of perforated disc, condylotomy or eminectomy.
It has been found that arthrocentesis can produce long-term relief of dysfunction and pain in TMDs. Arthrocentesis is reported as 91% effective in managing patients with reduced mouth opening and 96% in pain reduction [11, 12]. Other studies show that effectiveness of arthrocentesis is temporary, and it does not rehabilitate the micro-architecture of TMJ [13]. One of the major researches is the incorporation of PRP for stimulating repair or replacing damaged cartilage. Research findings suggest that PRP is an effective treatment due to its biological properties. It has an anabolic effect on chondrocytes and synoviocytes with resultant increases in cell proliferation, cartilaginous extracellular matrix accumulation and hyaluronic acid secretion [1].
The objective of this study is to evaluate and compare the role of PRP and arthrocentesis alone in improvement of clinical symptoms in patients of RDC/TMD groups II and III at regular postoperative intervals.
Materials and Methods
A randomized prospective study was performed from 2017 to 2019 with a 12-month follow-up. Total 24 patients (15 females and 9 males) who reported to department of Oral and maxillofacial Surgery, Subharti Dental College and Hospital with chief complaint of pain, reduced mouth opening, pathological joint noise, deviation on mouth opening, tenderness on palpation or not responding to conservative management and who were coming under groups II and III of RDC were included in study. Patients with connective tissue disease, neurological, psychological disorders, thrombocytopenia or in RDC/TMJ group I were excluded. Orthopantomography was performed to exclude any TMJ pathology and dental-related pain. Patients on long-term NSAIDs were also excluded to avoid impaired platelets for PRP fabrication. All the patients were divided equally into two groups of 12 patients each. In group A, arthrocentesis was performed and intra-articular injection of PRP was injected in group B. Written consent was obtained from the patients prior to procedure. Ethical clearance was priorly taken from the ethical committee of Subharti University, Meerut (Reference No. SDC/E.C/2018/402).
Preoperative Phase
Pain was assessed on a visual analogue scale (VAS) from 0: no pain to 10: the worst imaginable pain. Induction of a pathologic noise (such as clicking or crepitus) was assessed by auscultation using stethoscope. Painless maximal mouth opening (PMO), maximum mouth opening (MMO), lateral movement of mandible towards unaffected side (LMTUS) were recorded. Deviation upon mouth opening and tenderness on palpation were also documented. All variables were measured preoperatively and repeated by the same physician at 1 week, 3 months, 6 months and at 12 months intervals postoperatively.
Operative Phase
Under aseptic protocol, Holmlund–Hellsing line (HH) was drawn and 1 ml of local anaesthesia were given to anesthetize auriculotemporal nerve.
Group A
20-gauge needle was inserted into the superior joint space at 10:2 mm (10 mm on the line from mid tragus and 2 mm below this point) location. Approximately 2 ml of Ringer’s lactate solution was injected to distend the joint space and then a second 20-gauge needle was injected into the distended compartment at 20:10 mm location (20 mm on the line from mid tragus and 10 mm below this point) to establish a free outflow of the solution (Fig. 1). A total of 100 ml of solution was used, during which time the outlet needle was momentarily blocked with finger pressure to distend and break up the joint adhesion (Fig. 2). After removal of needles, the patient’s jaw was manipulated for lateral, vertical and protrusive movements.
Fig. 1.
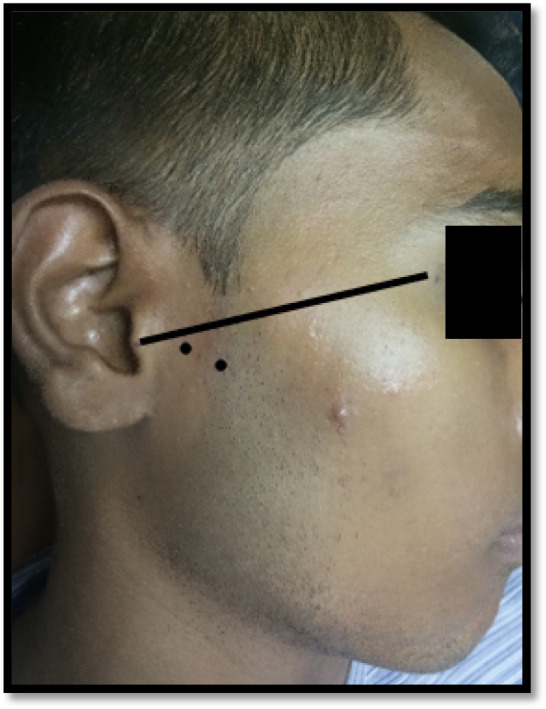
Figure depicting marking of Holmlund–Hellsing line and points for needle insertion
Fig. 2.

Figure depicting arthrocentesis procedure under local anaesthesia
Group B: Preparation and Injection Technique of Platelet-Rich Plasma
10 cc of blood was drawn in a glass tube of 3.2% sodium citrate under aseptic protocol. Double centrifugation cycle was used for preparation of PRP. The first cycle (separating cycle) involves centrifugation of blood at 1800 rpm for 15 min to separate erythrocytes. After centrifugation, plasma and buffy coat layer were transferred to other plain tube and centrifuged at 3500 rpm for 10 min to concentrate platelets (concentration cycle). At the end, two layers are formed: the upper 2/3rd of platelet-poor plasma (PPP) and lower 1/3rd of PRP (Fig. 3), which is further separated and loaded in syringe. PRP was injected into the upper joint space; the point of injection was marked 10 mm from the middle tragus on HH line and 2 mm below this point (Fig. 4).
Fig. 3.
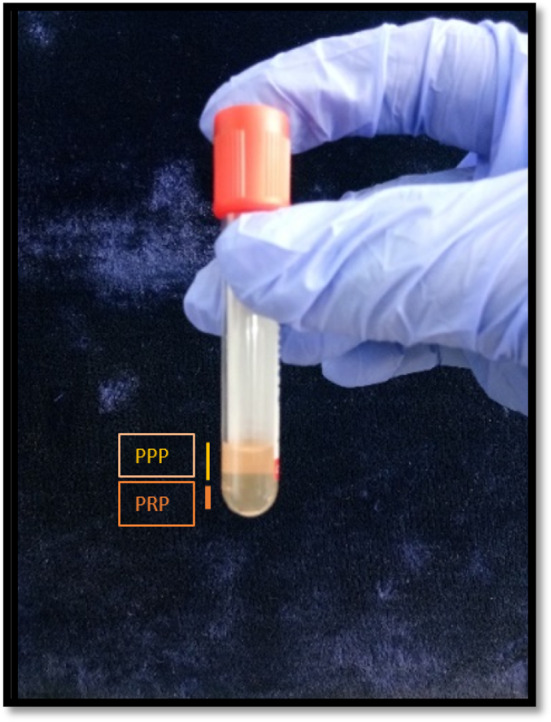
Figure depicting upper 2/3rd part of platelet-poor plasma and lower 1/3rd as platelet-rich plasma
Fig. 4.

Figure depicting intra-articular injection of PRP in supra joint space
The Postoperative Phase
In both groups, tablet paracetamol 500 mg three times a day and tablet tramadol hydrochloride 50 mg SOS (in severe pain) for 1 week were prescribed. Patients were instructed for soft diet for 6 days. Occlusal splint therapy was advised after 6 months in cases of persistent pain associated with deep bites.
Statistical Analysis
All statistical analyses were carried out using the IBM SPSS version 19.0. Intragroup comparisons were performed using paired t test, Wilcoxon test and Chi-square test. The changes were calculated, and intergroup comparisons were performed using independent t test.
Results
The present study consisted of five females and seven males in arthrocentesis group; their age ranged from 16 to 28 years (mean 22.17 ± 3.61). PRP group consisted of 10 females and 2 males; their age ranged from 14 to 50 years (mean 27.83 ± 11.71). As per Wilkes classification, four patients of stage II (early-intermediate), four patients of stage III (intermediate) and four patients of stage IV (Intermediate-late) were in arthrocentesis group. Five patients of stage II, three patients of stage III and four patients of stage IV were in the PRP group.
The mean preoperative PMO was 24.7 ± 8.3 mm in group A, 31.2 ± 7.2 mm in group B and postoperative at 12 months increased to 35.4 ± 6.9 mm and 39.1 ± 9.6 mm, respectively. The mean preoperative MMO was 33.9 ± 10 mm in group A, 41.7 ± 8.5 mm in group B (P > 0.05) and at 12 months mean increased to 39.2 ± 6.2 mm and 42.5 ± 8.1 mm, respectively (P > 0.05). The mean preoperative LMTUS was 6.5 ± 3.1 mm in group A, 6.9 ± 3.3 mm in group B (P > 0.05) and at 12 months mean increased to 7.7 ± 2.1 mm and 9.2 ± 2.7 mm, respectively (P > 0.05). The mean preoperatively pain score was 5.6 ± 2.3 in group A, 5.5 ± 2.1 in group B (P > 0.05) and postoperatively mean pain score decreased to 1.3 ± 2.2 and 1.5 ± 2.4 in respective groups (Table 1).
Table 1.
Inter- and intragroup comparisons of outcome variables
| Variables | Preop | 1-week follow-up | P (on comparison with preoperative values) | 3-month follow-up | P (on comparison with preoperative values) | 6-month follow-up | P (on comparison with preoperative values) | 12-month follow-up | P (on comparison with preoperative values) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Painless mouth opening | Gp A | 24.7 ± 8.3 | 29.5 ± 7.6 | < 0.05 (0.010)b | 31.3 ± 7.6 | < 0.05 (0.001)b | 33.6 ± 7.0 | < 0.05 (0.000)b | 35.4 ± 6.9 | < 0.05 (0.000)b |
| Gp B | 31.2 ± 7.2 | 32.9 ± 9.5 | > 0.05 (0.434)b | 36.0 ± 9.8 | > 0.05 (0.115)b | 37.8 ± 10.2 | < 0.05 (0.051)b | 39.1 ± 9.6 | < 0.05 (0.020)b | |
| P value | > 0.05 (0.054)a | > 0.05 (0.357)a | > 0.05 (0.199)a | > 0.05 (0.260)a | > 0.05 (0.286)a | |||||
| Maximum mouth opening | Gp A | 33.9 ± 10.0 | 35.7 ± 7.7 | > 0.05 (0.249)b | 37.2 ± 6.6 | > 0.05 (0.104)b | 37.2 ± 6.2 | < 0.05 (0.041)b | 39.2 ± 6.2 | < 0.05 (0.004)b |
| Gp B | 41.7 ± 8.5 | 39.4 ± 10.4 | > 0.05 (0.109)b | 39.7 ± 8.9 | > 0.05 (0.275)b | 41.3 ± 8.8 | > 0.05 (0.795)b | 42.5 ± 8.1 | > 0.05 (0.605)b | |
| P value | > 0.05 (0.052)a | > 0.05 (0.340)a | > 0.05 (0.444)a | > 0.05 (0.206)a | > 0.05 (0.284) | |||||
| Pain (VAS) | Gp A | 5.6 ± 2.3 | 2.0 ± 2.1 | < 0.05 (0.003)c | 1.6 ± 2.3 | < 0.05 (0.005)c | 1.9 ± 2.6 | < 0.05 (0.004)c | 1.3 ± 2.2 | < 0.05 (0.003)c |
| Gp B | 5.5 ± 2.1 | 2.9 ± 1.7 | < 0.05 (0.009)c | 2.5 ± 3.0 | < 0.05 (0.013)c | 1.8 ± 2.3 | < 0.05 (0.003)c | 1.5 ± 2.4 | < 0.05 (0.003)c | |
| P value | > 0.05 (0.92)a | > 0.05 (0.260)a | > 0.05 (0.459)a | > 0.05 (0.936)a | > 0.05 (0.864)a | |||||
| Lateral movements towards unaffected side | Gp A | 6.5 ± 3.1 | 6.6 ± 2.1 | > 0.05 (0.908)b | 6.3 ± 2.1 | > 0.05 (0.718)b | 7.5 ± 2.3 | > 0.05 (0.074)b | 7.7 ± 2.1 | < 0.05 (0.036)b |
| Gp B | 6.9 ± 3.3 | 7.6 ± 3.1 | > 0.05 (0.191)b | 8.6 ± 2.4 | < 0.05 (0.035)b | 8.6 ± 3.4 | > 0.05 (0.103)b | 9.2 ± 2.7 | < 0.05 (0.025)b | |
| P value | > 0.05 (0.804)a | > 0.05 (0.378)a | < 0.05 (0.024)a | > 0.05 (0.378)a | > 0.05 (0.154)a | |||||
Bold values indicate that P-value is significant as it is less than 0.05
Gp Group
aIndependent t test
bPaired t test
cWilcoxon test
Intragroup comparison of these variables at 12 months showed that PMO (P < 0.01), MMO (P < 0.01) and LMTUS (P < 0.05) increased significantly and pain complaint (P < 0.01) decreased significantly in group A. In group B, PMO (P < 0.05) and LMTUS (P < 0.05) increased significantly, pain complaint (P < 0.01) reduced significantly and improvement in MMO was insignificant (P > 0.05) (Table 1). Intergroup comparisons of these variables showed that there were no significant differences between both the groups (P > 0.05) (Table 1).
At the 6-month follow-up, 1 patient in group A and 3 patients in group B presented with persistent pain associated with deep bite. These patients were given occlusal appliance therapy for 1 month. After 1 month except one patient in group B, all patients were pain free. Comparing these values, it was observed that postarthrocentesis or PRP along with occlusal appliance had 75% of success rate. At a complete 12-month follow-up, two patients in group A and three patients in group B complained of pain. Pain elimination noted in 10 patients in arthrocentesis group showed success rate of 83%, whereas pain elimination in nine patients with PRP group showed success rate of 75%.
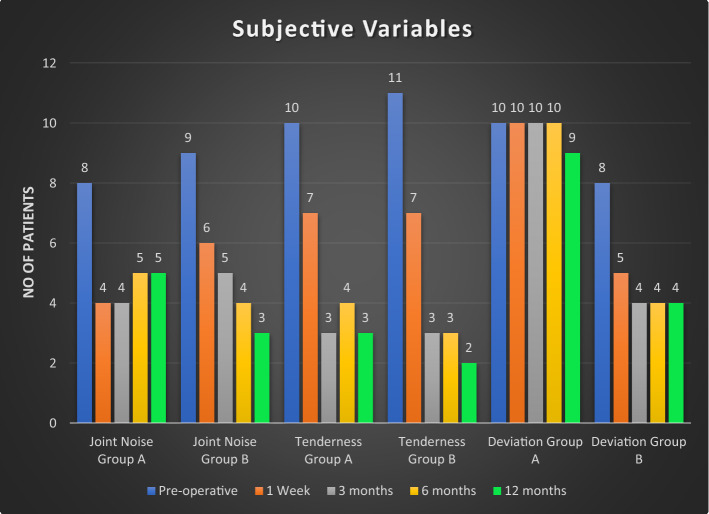
On subjective evaluation, eight patients in group A and nine patients in group B had detectable joint noise. At the end of 12 months, joint noise was eliminated in three patients in group A and six patients in group B. Joint noise elimination showed success rate of 37.5% for arthrocentesis, whereas 66.6% for PRP. Joint tenderness was noted in 10 patients in group A and 11 patients in group B, preoperatively. At the end of 12 months, tenderness was eliminated in seven patients in group A and in nine patients in group B, which showed a success rate of 70% for arthrocentesis and 81.8% for PRP. Deviation on mouth opening was noted in 10 patients in group A and eight patients in group B preoperatively. At the end of 12 months, deviation was corrected in only one patient in group A and four patients in group B, which showed a success rate of only 10% for arthrocentesis and 50% for PRP (Fig. 5).
Fig. 5.
Graphical representation of subjective variables
No adverse events were observed during treatment or follow-up period.
Discussion
Temporomandibular joint disorders are difficult to manage and cannot be fully cured; these are managed only symptomatically. Conservative therapy is generally the first-line management. A meta-analysis by Bessa-Nogueira et al. [6] indicates the success rate of nonsurgical treatment is approximately 70% and that of surgical treatment is 83%; he also stated approximately 40% to 70% TMDs have shown self-improvement without any treatments.
In a Cochrane database review, it was reported that there is insufficient evidence either for or against the use of oral-appliance therapy. However, with appropriate conservative management, these devices may play a role in alleviating the pain and dysfunction in 70–90% of patients [14]. In present study, we used bite appliance therapy in management of TMD associated with deep bite (four patients) after arthrocentesis or PRP injection, three patients got relief in pain and dysfunction which showed a success rate of 75%.
TMJ arthrocentesis has been considered as a superior treatment option for the reduction of pain when compared with other conservative therapies for TMD [15]. Arthrocentesis is the process of irrigating and distending the superior joint space with Ringer’s lactated solution (RL) to reduce pain by removing inflammatory mediators, degrading proteins and increasing mandibular mobility by disrupting immature adhesions or a stuck disc, eliminating the negative pressure within the joint, recovering disc and fossa space and improving disc mobility [16]. RL is preferred as irrigating solution because it is close to human serum, and the fibrous tissue of the articular disc has a better tolerance [17]. The volume of solution used for TMJ arthrocentesis mentioned in various studies ranged from 50 ml to 500 ml. There is paucity of controlled clinical studies to answer the question “how much volume of lavage fluid is optimum for arthrocentesis?”. Based upon specific assumptions about role of certain proteins, Zardeneta et al. [18] reported approximately 100 ml of total perfusate is sufficient for therapeutic lavage. In the present study, we have used around 100 ml of RL fluid in all the cases of arthrocentesis. For arthrocentesis, there are generally two techniques described in the literature: two needle puncture technique and double lumen single puncture technique. In our study, double-puncture arthrocentesis technique originally described by Nitzen was used [12]. In a study by Alper Alkan, it was observed that it is difficult to enter the narrow joint spaces with double lumen single puncture arthrocentesis needle [19].
In Nitzan’s study, arthrocentesis was performed in 17 patients, with an average follow-up of 9 months; the mean improvement in MMO was found to be 18.6 mm [12]. Dimitroulis found MMO improvement of 17.7 mm over an average follow-up period of 21 months [20]. In our study, PMO preoperatively was 24.7 mm which had increased to 35.4 mm postoperatively; similarly preoperative MMO was 33.9 mm which improved to 39.2 mm at 12-month follow-up. This compares favourably with the above-mentioned studies.
Concerning pain reduction property of arthrocentesis, Diraçoğlu et al. and Vos et al. reported that arthrocentesis provides a significant improvement in pain compared to nonsurgical treatments [21, 22]. In various studies, Neeli, Fridrich et al. and Nitzan et al. reported 75–95% of success rate [11, 12, 22]. In our study, arthrocentesis in accordance with pain elimination showed a success rate of 83%.
For joint noise elimination, Hanci et al. [2] performed arthrocentesis in 12 patients and found 58.4% of success rate at 6-month follow-up. Present study demonstrated a success rate of 37.5% on follow-up of 12 months. These studies suggest that arthrocentesis is a moderately efficient method for joint noise elimination.
TMD usually involves structural alteration and enzymatic degradation of cartilage and subchondral bone. Hanci et al. recommend PRP in order to prevent these degenerative and destructive changes. He also suggested that volume expanding effect, anabolic and regenerative properties of PRP reduce these degenerative processes [2]. In the literature, there is paucity regarding arthrocentesis v/s PRP for management of TMDs. Hassan reported preoperative mean MMO of 34.3 mm which reached to 42.8 mm at 6-month follow-up after PRP [1]. In present study, PMO preoperatively was 31.2 mm which increased to 39.1 mm; similarly preoperative MMO was 41.7 mm which improved to 42.5 mm postoperatively. These results obtained show significant changes when preoperative and postoperative values were compared, even for previously achievable normal mouth opening.
Several authors have reported good efficacy of PRP for pain reduction [1, 23, 24]. Similarly, present study showed significant reduction in pain with a success rate of 75%. In a study by Hassan, EF showed success rate of 44.4% for joint noise reduction [1]. In present study, nine patients had joint noise preoperatively; at the end of 12 months, only three patients remained with joint noise, which showed a success rate of 66.6%. Patients in both groups had joint tenderness which decreased postoperatively with the success rate of 70% for arthrocentesis and 81% for PRP. The results obtained in both the groups correlate with results obtained in their respective studies [12, 23, 24].
Hassan and Lin et al. found insignificant differences comparing PRP and arthrocentesis for TMJ pain [1, 25]. Present study has also not found any significant difference for arthralgia.
The patients of arthrocentesis exhibited significant improvements in mouth opening within 1 week, attributed to immediate removal of inflammatory mediators, removal of intra-articular adhesions and elimination of the negative pressure. PRP takes longer time due to their molecular effects on joint structure for regeneration.
Conclusion
TMDs are progressive disorders which lead to development of arthralgia and functional disabilities of TMJ, when comparing the clinical outcomes improvement was observed in all parameters of both the groups except deviation correction and joint noise elimination in arthrocentesis group which showed minimal improvement. Intergroup comparison was found to be insignificant, thus demonstrating the effectiveness of both methods; however, arthrocentesis has higher success rate for pain elimination; better statistical results were found in clinical outcomes of range of jaw motion, whereas PRP was found to be more effective in elimination of joint noise, tenderness and improvement in jaw deviation on mouth opening.
Outcome of our study suggests future study should compare arthrocentesis along with PRP intra-articular injection in managing TMD, as mechanical action of arthrocentesis and regenerative properties of PRP may be effective method in TMD management compared to arthrocentesis alone.
Abbreviations
- TMJ
Temporomandibular joint
- TMDs
Temporomandibular joint disorders
- RDC
Research diagnostic criteria
- PRP
Platelet-rich plasma
- HA
Hyaluronic acid
- OPG
Orthopantomography
- VAS
Visual analogue scale
- PMO
Painless mouth opening
- MMO
Maximal mouth opening
- LMTUS
Lateral movemeents towards opposite side
- HH
Holmlund–Hellsing
- Fig
Figure
- PPP
Platelet-poor plasma
- Et al.
And others
- %
Percentage
- RL
Ringer’s lactated
Authors’ Contribution
All authors whose names appear on the submission (1) made substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data used in the work, (2) drafted the work or revised it critically for important intellectual content, (3) approved the version to be published, and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AR. The first draft of the manuscript was written by AR, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. VB and AR helped in conceptualization. VB, PD and AR contributed to methodology. AR was involved in formal analysis and investigation. AR contributed to writing—original draft preparation. VB, PD and Dr Ankit Kapoor contributed to writing—review and editing. VB contributed to resources. VB and PD were involved in supervision. VB and PD helped in validation. AR, VB, PD and AK helped in visualization. AR contributed to data curation. AR and AK performed formal analysis. AR and VB were involved investigation. VB and PD helped in project administration.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Compliance with Ethical Standards
Conflict of interest
The author declares that he does not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Akash Rajput, Email: dr_akashrajput@yahoo.co.in.
Vishal Bansal, Email: drbansalvishal@rediffmail.com.
Prajesh Dubey, Email: drprajeshdubey@gmail.com.
Ankit Kapoor, Email: dr.ankitkapoor14@gmail.com.
References
- 1.Hassan EF, Ali TM, Abdulla N. The clinical efficiency of platelet rich plasma in the treatment of temporomandibular joint disorders. Alex Dent J. 2016;41(3):226–231. doi: 10.21608/adjalexu.2016.58021. [DOI] [Google Scholar]
- 2.Hancı M, Karamese M, Tosun Z, Aktan TM, Duman S, Savaci N. Intra-articular platelet-rich plasma injection for the treatment of temporomandibular disorders and a comparison with arthrocentesis. J Cranio Maxillofac Surg. 2015;43(1):162–166. doi: 10.1016/j.jcms.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Hosgor H, Bas B, Celenk C. A comparison of the outcomes of four minimally invasive treatment methods for anterior disc displacement of the temporomandibular joint. Int J Oral Maxillofac Surg. 2017;46(11):1403–1410. doi: 10.1016/j.ijom.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Okeson JP. Management of temporomandibular disorders and occlusion-E-book. Amsterdam: Elsevier; 2014. [Google Scholar]
- 5.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord Facial Oral Pain. 1992;6(4):301. [PubMed] [Google Scholar]
- 6.Bessa-Nogueira RV, Vasconcelos BC, Niederman R. The methodological quality of systematic reviews comparing temporomandibular joint disorder surgical and non-surgical treatment. BMC Oral Health. 2008;8(1):27. doi: 10.1186/1472-6831-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fouda AA. Association between intra-articular corticosteroid injection and temporo-mandibular joint structure changes. Int Arch Oral Maxillofac Surg. 2018;2:015. [Google Scholar]
- 8.Guarda-Nardini L, Tito R, Staffieri A, Beltrame A. Treatment of patients with arthrosis of the temporomandibular joint by infiltration of sodium hyaluronate: a preliminary study. Eur Arch Otorhinolaryngol. 2002;259(5):279–284. doi: 10.1007/s00405-002-0456-z. [DOI] [PubMed] [Google Scholar]
- 9.Cerza F, Carnì S, Carcangiu A, Di Vavo I, Schiavilla V, Pecora A, et al. Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosis. Am J Sports Med. 2012;40(12):2822–2827. doi: 10.1177/0363546512461902. [DOI] [PubMed] [Google Scholar]
- 10.Hegab AF, Ali HE, Elmasry M, Khallaf MG. Platelet-rich plasma injection as an effective treatment for temporomandibular joint osteoarthritis. J Oral Maxillofac Surg. 2015;73(9):1706–1713. doi: 10.1016/j.joms.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 11.Neeli AS, Umarani M, Kotrashetti SM, Baliga S. Arthrocentesis for the treatment of internal derangement of the temporomandibular joint. J Maxillofac Oral Surg. 2010;9(4):350–354. doi: 10.1007/s12663-010-0155-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49(11):1163–1167. doi: 10.1016/0278-2391(91)90409-F. [DOI] [PubMed] [Google Scholar]
- 13.Kiliç SC, Güngörmüş M, Sümbüllü MA. Is arthrocentesis plus platelet-rich plasma superior to arthrocentesis alone in the treatment of temporomandibular joint osteoarthritis? A randomized clinical trial. J Oral Maxillofac Surg. 2015;73(8):1473–1483. doi: 10.1016/j.joms.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 14.Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359(25):2693–2705. doi: 10.1056/NEJMra0802472. [DOI] [PubMed] [Google Scholar]
- 15.Tvrdy P, Heinz P, Pink R. Arthrocentesis of the temporomandibular joint: a review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015;159(1):31–34. doi: 10.5507/bp.2013.026. [DOI] [PubMed] [Google Scholar]
- 16.Do Egito Vasconcelos BC, Bessa-Nogueira RV, Rocha NS. Temporomandibular joint arthrocententesis: evaluation of results and review of the literature. Braz J Otorhinolaryngol. 2006;72(5):634–638. doi: 10.1016/S1808-8694(15)31019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shinjo H, Nakata K, Shino K, Hamada M, Nakamura N, Mae T, Miyama T, Horibe S, Yoshikawa H, Ochi T. Effect of irrigation solutions for arthroscopic surgery on intraarticular tissue: comparison in human meniscus-derived primary cell culture between lactate Ringer’s solution and saline solution. J Orthop Res. 2002;20(6):1305–1310. doi: 10.1016/S0736-0266(02)00062-1. [DOI] [PubMed] [Google Scholar]
- 18.Zardeneta G, Milam SB, Schmitz JP. Elution of proteins by continuous temporomandibular joint arthrocentesis. J Oral Maxillofac Surg. 1997;55(7):709–716. doi: 10.1016/S0278-2391(97)90583-8. [DOI] [PubMed] [Google Scholar]
- 19.Guarda-Nardini L, Manfredini D, Ferronato G. Arthrocentesis of the temporomandibular joint: a proposal for a single-needle technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2008;106(4):483–486. doi: 10.1016/j.tripleo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Dimitroulis G, Dolwick MF, Martinez A. Temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: a follow-up study. Br J Oral Maxillofac Surg. 1995;33(1):23–27. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 21.Dıraçoğlu D, Saral İB, Keklik B, Kurt H, Emekli U, Özçakar L, Karan A, Aksoy C. Arthrocentesis versus nonsurgical methods in the treatment of temporomandibular disc displacement without reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2009;108(1):3–8. doi: 10.1016/j.tripleo.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Vos LM, Slater JH, Stegenga B. Arthrocentesis as initial treatment for temporomandibular joint arthropathy: a randomized controlled trial. J Cranio Maxillofac Surg. 2014;42(5):e134–e139. doi: 10.1016/j.jcms.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 23.Machoň V, Řehořová M, Šedý J, Foltán R. Platelet-rich plasma in temporomandibular joint osteoarthritis therapy: a 3-month follow-up pilot study. J Arthritis. 2013;2(2):2–5. [Google Scholar]
- 24.Pihut M, Szuta M, Ferendiuk E, Zeńczak-Więckiewicz D. Evaluation of pain regression in patients with temporomandibular dysfunction treated by intra-articular platelet-rich plasma injections: a preliminary report. BioMed Res Int. 2014 doi: 10.1155/2014/132369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin SL, Tsai CC, Wu SL, Ko SY, ChiangWF Yang JW. Effect of arthrocentesis plus platelet-rich plasma and platelet-rich plasma alone in the treatment of temporomandibular jointosteoarthritis. Medicine. 2018;97(16):e0477. doi: 10.1097/MD.0000000000010477. [DOI] [PMC free article] [PubMed] [Google Scholar]