Abstract
Backgrounds
Oral submucous fibrosis (OSMF) is a chronic, insidious disease and is said to have a multifactorial origin with varied clinical manifestation of repeated oral ulcers, intolerance to spicy food, mucosal blanching resulting in stiffness of the oral mucosa and formation of taut bands leading to reduced mouth opening. We designed this study to systematically review the literature on QOL in OSMF and hope to make recommendations for future course of QOL assessment in OSMF.
Methods
An electronic bibliographic search of studies was done from year 1900–2019 using specified keywords. The following databases were searched: PubMed, Ovid, Google Scholar and manual search were done from references of relevant articles. Of the screened 156 articles, finally 10 studies were included after screening for inclusion/exclusion criteria. Quality assessment of studies was completed using the Effective Public Health Practice Project (EPHPP) criteria for quantitative studies.
Results
Most instruments used in the studies were not disease specific for OSMF except one study. Six types of questionnaires were used. The heterogeneity in study population, study designs, QOL instruments and outcome measures made it difficult for a comparison. Therefore, a quantification analysis was not possible. Also pure OSMF data without the involvement of other lesions were less in number.
Conclusions
OSMF not only physically debilitates a patient, it has its repercussions on the social, physical, psychological domains as well. Another aspect is that apart from trismus, which is the most common and evident symptom associated with OSMF, a substantial part of the suffering that ensues is also because of the ulcerations, burning sensation and worsening of dental health. Another focus was the association of worse QOL with a higher grade of disease, longer and higher tobacco abuse contact duration. This review is unable to give a confident answer to the evidence on QOL in OSMF but definitely showers light on the evident lack of robust data on the same. Robust Powered by Editorial Manager® and ProduXion Manager® from Aries Systems Corporation methodological and adequately powered studies on assessing QOL in OSMF using only a reliable disease specific questionnaire is the need of the hour.
Clinical Trial Registration
PROSPERO Registration: CRD42018102874.
Keywords: Quality of life, QOL, OSMF, Oral submucous fibrosis, Trismus
Introduction
Oral submucous fibrosis (OSMF) is a chronic, insidious disease that affects the lamina propria of the oral mucosa and as the disease advances it involves tissues deeper in the submucosa of the oral cavity resulting in loss of fibroelasticity [1] leading to trismus. The evidence of its existence dates back to the era of Sushrutha who in his classification of mouth and throat maladies, mentioned a condition 'VIDARI' similar to submucous fibrosis [2]. OSMF was later described by Schwartz in 1952 among five Indian females living in Kenya, and he coined the term Atrophia idiopathica (trophica) mucosae oris [3].
The disease is said to have a multifactorial origin with varied clinical manifestation of repeated oral ulcers, intolerance to spicy food, mucosal blanching resulting in stiffness of the oral mucosa and formation of taut bands leading to reduced mouth opening. In India, the prevalence increased over the past four decades from 0.03% to 6.42% [4, 5]. Current burden of the disease in India is estimated to be over 5 million [6].
Mortality rate is significant because it transforms into oral cancer, particularly squamous cell carcinoma at a rate of 7 to 30% [7]. Quality of life (QOL) is an important health outcome measure that is relevant to the patients care. The QoL integrates several aspects of life, such as physical, psychological, social, economic, spiritual, cognitional and sexual dimensions which are interrelated.
A patient with oral submucous fibrosis not only suffers from the disease itself but with the associated addictions, socio-economic implications, compromised dental care and an imminent fear of malignancy. The burden of the disease is mostly underestimated in these patients. Therefore, the assessment of QOL stands its case strongly.
We designed this study to systematically review the literature on QOL in OSMF and hope to make recommendations for future course of QOL assessment in OSMF.
Methods
Literature Search
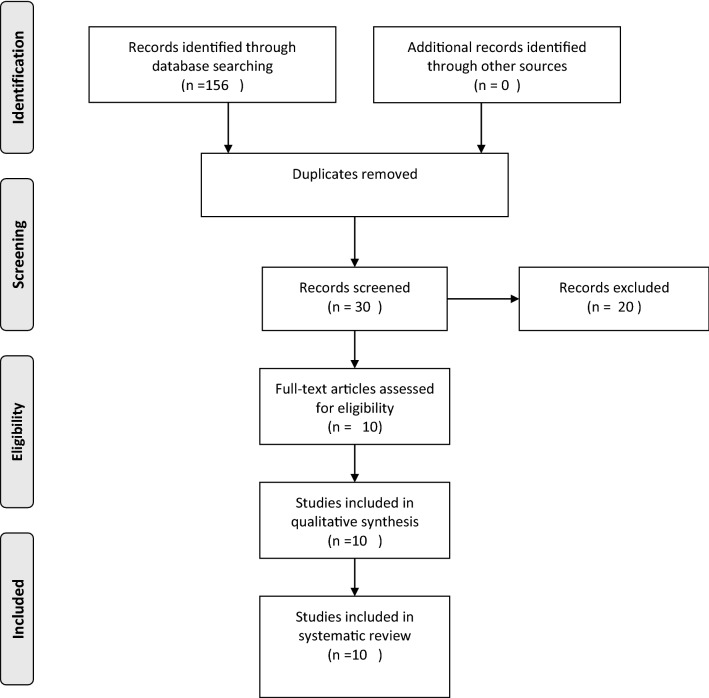
An electronic bibliographic search of studies was done from 1900 to 2019 using the following keywords: “Oral submucous fibrosis; OSMF; OSF; fibrosis; QOL; Quality of life; questionnaire; survey” The search was done independently by 2 investigators SK & KC. The following databases were searched: PubMed, Ovid, Google Scholar and manual search were done from references of relevant articles. Non-English citations were excluded. Fig. 1 shows the PRISMA flow chart depicting the study identification and selection process. The search yielded 30 articles after duplicate removal.
Fig. 1.
PRISMA 2009 Flow diagram
Screening and Eligibility
The articles were independently read by the two investigators KC & ND and screened through the inclusion and exclusion criteria to finalize its induction into the study. Any disagreements were sorted by mutual discussion and a final discussion with third investigator RB.
Article Selection
Exclusion Criteria:
Non standardized, non-validated questionnaires used for QOL assessment
No separate data available for OSMF
Non-English citations
Inclusion criteria:
Standardized validated QOL questionnaire
OSMF patients included in the study exclusively or with other lesions
Data Collection Process
The full text was read for all the included 30 articles, by both the investigators SK & KC, and the details of the QOL in OSMF were noted. Any article that did not give separate data for OSMF and clubbed it with a broader group of diseases was rejected. Any study that assessed QOL whether in baseline or at comparative level was included. Data were noted on a specified data extraction chart and were finally screened by author RB to determine accuracy.
Quality Assessment
Effective Public Health Practice Project (EPHPP) criteria for quantitative studies were used to assess the quality of included studies. The assessment was based on the following criteria: Selection bias, study design, confounders, blinding, data collection method, withdrawals and dropouts. The article was graded as strong, moderate, weak as part of overall quality grading.
Results
The PRISMA chart (Fig. 1) states information on the titles screened, considered eligible/ineligible and final inclusion in the review. Search on PubMed yielded 104 results, Google Scholar yielded 38 results, Ovid yielded 14 results. A total of 156 titles were screened by electronic search. Duplicates were removed, and manual search done. 30 articles were found relevant to further assess for inclusion/exclusion. Of these, 10 articles were found to meet the inclusion/ exclusion criteria and were finally included in the study.
Characteristics of studies
Quality assessment of studies was completed using the Effective Public Health Practice Project.
(EPHPP) criteria for quantitative studies. Each study was read in detail and scored according to the criteria and finally branded as being strong/moderate/weak for overall quality. Two investigators SK and AK independently reviewed each study and any discrepancy was settled by mutual discussion and final consultation with author KC. Out of ten studies seven were found to be of weak quality and only study by Jiang et al [8] was of strong quality and two studies [9, 10] by Chaudhry et al. were of moderate quality (Table 1).
Table 1.
Quality Assessment Of Included Studies As Per Ephpp Tool
| S.No | Year/Author/Country | Quality of study (EPHPP Tool) |
|---|---|---|
| 1 |
2013 Saimdhavi8 India |
Weak |
| 2 |
2015 Jiang9 China |
Strong |
| 3 |
2015 Rimal10 Nepal |
Weak |
| 4 |
2017 Chole11 India |
Weak |
| 5 |
2017 Namrata12 India |
Weak |
| 6 |
2017 Tadakamadla13 India |
Weak |
| 7 |
2018 Jena14 India |
Weak |
| 8 |
2018 Chaudhry15 India |
Moderate |
| 9 |
2018 Gondivkar16 India |
Weak |
| 10 |
2019 Chaudhry17 2019 |
Moderate |
Study Populations
All of the included studies were polarized to the Asian continent with 9 out of the 10 studies coming from the Indian subcontinent and one from China [8]. Of the included studies, 3 studies analyzed QOL data in respect to therapeutic intervention for OSMF while the others analyzed QOL data at baseline(2), in comparison with control (2) or in comparison with other diseases (3). Sample size was taken as the number of OSMF cases that were included in the study, and it ranged from 7 to 206 in the given studies. A total number of 986 OSMF patients were assessed for their quality of life including 226 patients where assessment was done at least at two points of time.
Instruments Used
Most instruments (Table 2) used in the studies were not disease specific for OSMF except the study by Gondivkar et al [11] who used the OSMF specific OHRQoL-OSF instrument that was validated by the same authors in a previous study [12]. Six different types of questionnaires were used. General health QOL instrument like the WHOQoL-BREF (World Health Organization Quality of Life- Abbreviated version) was used in two studies. One study used the European Organization for Research and Treatment of Cancer Quality of Life head and neck 35 Questionnaire (EORTC QLQ-C35) that is health specific but was intended for head neck cancer patients. The oral health related QOL questionnaire, The Oral Health Impact Profile (OHIP)-14 was the most commonly used questionnaire, and its Nepalese version was tested as well. Amongst the disease specific oral health related QOL instruments, the spectrum starts from Chronic Oral Mucosal Diseases Questionnaire (COMDQ) to Oral Potentially malignant disease Questionnaire (OPMDQ) and the latest disease specific OHRQoL-OSF (Oral health related quality of life-oral submucous fibrosis) questionnaire.
Table 2.
Detailed description of included studies
| S.No | Year/Author/Country | Instrument used | No of instruments | Domains | Disease specific (Y/N) | Age Range/Mean age | Sample size for OSMF (n) | Measuring | Comparing with | Time points | Result | Limitation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
2013 Saimdhavi8 India |
OHIP-14 | 14 | Seven dimensions: Functional Limitation, Physical Discomfort, Psychological Discomfort, Physical Disability, Psychological Disability, Social Disability and Handicaps | N | > 20 yrs | 7 | Comparison of QOL | 2 groups Group 1: Chronic diseases like chronic abscess, lichen planus, pemphigus and oral submucous fibrosis Group 2: Acute diseases like acute abscess and acute ulcer | Baseline | Results: Moderately impaired quality of life was found among all the diseases investigated. On comparing the mean domain and total OHIP score between the two groups, the domain of psychological discomfort and disability and the total OHIP score showed statistically significant values in acute diseases. No significant differences were obtained on comparing the grades of QOL in between the two groups and among various diseases within the same group | Further studies are advocated to determine the association between education, harmful habits, and their oral health related QOL |
| 2 |
2015 Jiang9 China |
OHIP-14 | 14 | Seven dimensions: Functional Limitation, Physical Discomfort, Psychological Discomfort, Physical Disability, Psychological Disability, Social Disability And Handicaps | N | 20–50 yrs | 52 | Interventional with QOL | Group A received an intralesional injection of triamcinolone acetonide (TA) 2 mg Group B received an intralesional injection of Allicin 1 mg. Both given weekly for 16 weeks | Baseline, Week 40 | Six months after the end of treatment, the mean decline in OHIP 14 score in group B was significantly greater than that in group A (P = 0.001, vs. group A) At 40 weeks, the net gain in mouth opening and improvement in burning sensation was more in the Allicin group (Both statistically significant) | Patients enrolled in the clinical trial comprised only patients with stage II OSF, No control group was kept. Further clinical trials are needed to determine the exact dosage and frequency of application required |
| 3 |
2015 Rimal10 Nepal |
Nepalese OHIP-14 | 14 | Seven dimensions: Functional Limitation, Physical Discomfort, Psychological Discomfort, Physical Disability, Psychological Disability, Social Disability And Handicaps | N | Mean 36 yrs | 74 | Interventional with QOL |
All patients were given a potent vasodilator pentoxifylline Pentoxifylline 400 mg TDS X 1 months + Intralesional dexamethasone 4 mg/ml biweekly for first 2 weeks, then in combination with hyaluronidase 1500 IU for the next 4 weeks biweekly for a total period of 6 weeks |
Baseline, 6 months |
Median OHIP-14 score at baseline 18 (0–45), was significantly (p < 0.001) different from 6 months’ follow-up [5(0–15)]. Impact score at baseline was mainly influenced by age, frequency and duration of habit. In the baseline, most impact was in the psychological domain followed by physical pain. Baseline VAS for burning sensation was significantly different from 6-month follow-up. VAS and OHIP-14 scores were also significantly different between males and females both before and after treatment of OSF |
It needs to be used in larger longitudinal studies to evaluate the sensitivity of Nepalese version of OHIP-14 on other oral diseases in different age groups. OHRQoL |
| 4 |
2017 Chole11 India |
European Organization for Research and Treatment of Cancer Quality of Life head and neck 35 Questionnaire (EORTC QLQ-C35) | 35 | Seven scales Pain, Swallowing, Senses, Speech, Social Eating, Social Contact, Sexuality | N | Not specified | 100 | Intervention Response & QOL |
Group A (n = 50) received oral Spirulina capsule 500 mg BD Group B (n = 50) received oral Spirulina capsule 500 mg BD + topical triamcinolone acetonide 0.1% |
Baseline, 1,2 3 Month |
At 3 month post treatment, there was a decrease in the pain, problems relating to swallowing, speech, eating in a social environment, socializing with other people, feeling sick, loss of sexual desire and in opening mouth. Group B had better outcome in mouth opening, burning sensation, pain, swallowing, senses (taste/smell), speech, social eating, social contact, teeth, dry mouth, sticky saliva, and feeling ill, but with statistically significant difference in pain, senses (taste/smell), speech, social eating, social contact, teeth and opening mouth |
Not mentioned |
| 5 |
2017 Namrata12 India |
Chronic Oral Mucosal Diseases Questionnaire | 26 | 4 domains: Pain And Functional Limitation, Medications And Side Effects, Social And Emotional And Patient Support | N | Not specified | 26 | Comparison of QOL | QOL amongst 5 diseases oral lichen planus, recurrent aphthous ulcers, pemphigus, leukoplakia, and OSMF | Baseline | Maximum mean of scores is seen in recurrent aphthae, followed by pemphigus, then OSMF, followed by leukoplakia and finally lichen planus. Recurrent aphthous ulcers and OSMF adversely affected the QOL more than the other COMD subgroups did | The limitation is that the study is based on a sample of convenience and had no control group |
| 6 |
2017 Tadakamadla13 India |
OPMDQoL | 20 | 4 dimensionsL: Difficulties with diagnosis, Physical impairment and functional limitations, Psychological and social well-being and Effect of treatment on daily life | N | Mean age 39.8 years | 50 | Comparison of QOL | Comparison in three premalignant diseases Oral Leukoplalia (OL), Oral Lichen Planus (OLP) and oral submucous fibrosis (OSF) | Baseline | OLP patients reported higher scores for the subscale ‘Difficulties with diagnosis’ than OL and OSF patients. OLP and OSF have a significant impact on the QoL of affected individuals: OL less so. OL patients also had better scores for ‘Physical impairment and functional limitations’ than those with OLP and OSF. There were no differences between the three OPMDs for the dimensions, ‘effect of their treatment on daily life’ and’ psychological and social wellbeing’. Increasing stage of the disease is associated with worsening QoL. Subjects who smoked 6–10 cigarettes per day had better QoL than those who were smoking more than ten cigarettes per day. Areca nut usage with or without tobacco for 1–5 years and 1–5 times per day reported better QoL than those who used for more than ten years and greater than ten units per day respectively | Cross sectional study so findings cannot be considered as causal; Study was limited to one teaching hospital so might not be accurate to generalize to rest of country or ethnic groups |
| 7 |
2018 Jena14 India |
OHIP 14 | 14 | Seven dimensions: Functional Limitation, Physical Discomfort, Psychological Discomfort, Physical Disability, Psychological Disability, Social Disability And Handicaps | N | Mean age Study vs Control group 28.74 ± 5.60 and 28.59 ± 6.03 years, respectively | 121 | Comparison of QOL | Comparison with control | Baseline | The mean and median OHIP-14 scores were statistically higher in the study vs the control group subjects. Mean score of all the seven domains of OHIP-14 was significantly more in OSF subjects (P < 0.001). All the OSF subjects had one or more negative effects on OHRQoL. Physical pain and psychological discomforts were most severely affected in OSF subjects. Stage-4 of the OSF had maximum effect on QOL compared to other stages | Suggested to study Odia language based QOL on its population, Further QOL of various treatment modalities on QOL |
| 8 |
2018 Chaudhry15India |
WHOQoL Bref | 26 | 4 domains: Physical Health (7 Items), Psychological Health (6 Items), Social Relationships (3 Items), And Environmental Health (8 Items) | N | Not specified | 150 | Comparison of QOL | Comparison with control | Baseline | The participants without OSMF have a significantly higher QOL in comparison with those with OSMF. The highest mean difference of QOL scores was observed in the environmental heath domain (1.09) and it was significant statistically (P value = 0.00) | QOL was not assessed according to the grading which might reduce the precision of results. Suggestion for further cross-sectional studies to evaluate the individual factors in each domain of WHOQOL-BREF |
| 9 |
2018 Gondivkar16 India |
OHRQoL-OSF scale (Original) | 17 | 4 subscales: Discomfort And Functional Impairment, Psychological Wellness, Physical Wellness And Social Wellness | Y | 20–65 yrs | 206 | QOL | None | Baseline | Discomfort and functional impairment’ dimension was highly prevalent among patients with all stages. Stage IV OSF (25.94 ± 4.05) patients reported higher OHRQoL-OSF scores as compared to stage III and stage II OSF. OHRQoLOSF scores increase with advancing stages of OSF | Recommends multicentric studies with larger sample size |
| 10 |
2019 Chaudhry17 2019 |
WHOQoL Bref | 26 | 4 domains: Physical Health (7 Items), Psychological Health (6 Items), Social Relationships (3 Items), And Environmental Health (8 Items) | N | Not mentioned | 200 | QOL | None | Baseline | The QOL was significantly affected negatively in all the four domains for age > 40 years. The individual with the OSMF affecting till the extraoral cavity/ EO have shown lower levels of QOL score when compared to the individuals where OSMF is affecting only oral cavity proper/OCP and the difference is statistically significant in all the domains. The QOL was better (statistically) in patients with habit abuse duration < 5 years as compared to ones with duration > 5 years in all domains | Recommends a focused assessment using an OSMF specific questionnaire |
Baseline studies
7 studies analyzed the QOL data for OSMF whether at baseline level with or without comparison to other diseases. When compared with other diseases, a study [13] using OHIP 14 revealed that acute oral diseases like ulcers or abscess may have more psychological discomfort and disability than chronic diseases like OSMF or chronic abscess. Another study12 using COMDQ to compare the QOL amongst 5 diseases oral lichen planus, recurrent aphthous ulcers, pemphigus, leukoplakia and OSMF found that recurrent aphthous ulcers and OSMF adversely affected the QOL more than the other COMD subgroups did.
A study [14] using OPMDQ to assess QOL in 3 premalignant diseases Oral leukoplakia (OL), Oral lichen planus (OLP), OSMF found that OLP and OSF have a significant impact on the QoL of affected individuals in comparison to OL. Increasing stage of the disease, smoking more than ten cigarettes per day, using areca nut with or without tobacco for more than ten years and greater than ten units per day respectively, each is associated with worsening QoL.
When comparing QOL in OSMF patients vs normal patients, a study [9] used WHOQOL-BREF Questionnaire and found that the participants without OSMF had a significantly higher quality of life in comparison with those with OSMF. Statistically the highest mean difference of QOL scores was observed only in the environmental heath domain. Another study [15] compared the same using OHIP-14 found that all the OSF subjects had one or more negative effects on OHRQoL compared to 64.34% of healthy subjects. Although mean score of all the seven domains of OHIP-14 was significantly more in OSF subjects, physical pain and psychological discomforts were most severely affected in OSF subjects compared to healthy subjects. Stage 4 of the OSF had maximum negative impact on quality of life compared to other stages.
At baseline without any comparison, using WHOQOL-BREF, another study by Chaudhry et al [10] found that, worse QOL was associated with participants more than forty years of age, OSMF extending to Extra Oral Cavity (defined in the study for simplifying the quality of life assessment as per the site of lesion, bands extending till the buccal mucosa were quantified as oral cavity proper (OCP) and when they further extended to involve the lip and vestibule they were termed to be extraoral cavity (EO)), habit abuse duration of more than 5 years and greater restriction of mouth opening. The study [11] using disease specific tool OHRQol-OSF found out that Discomfort and functional impairment’ dimension was highly prevalent among OSMF patients with all stages (P < 0.001). Stage IV OSF patients reported worse QOL compared to stage III and stage II OSF patients. The majority of the participants rated their overall oral health status ‘fair’ (34.95%) to ‘very poor’ (26.21%) whereas overall well-being was rated as moderate (33.00%) to good (31.55%).
Interventional studies
Two studies [8, 16] assessed the therapeutic effect of intervention using the OHIP 14 (1 English and 1 nepalese). The first study [8] was based on China that compared effect of intralesional injection of triamcinolone acetonide (TA) 2 mg vs intralesional injection of Allicin 1 mg given for 16 weeks. At end of 6 months, the improvement in QOL was significantly more in the Allicin group. At 40 weeks, the net gain in mouth opening and improvement in burning sensation was more in the Allicin group (Both statistically significant).
The Nepalese OHIP [16] was used in a study to assess the QOL after a therapeutic intervention using Pentoxifylline, Intralesional dexamethasone and Injection hyaluronidase 1500 IU protocol. The QOL significantly improved at 6 months compared to baseline values. Impact score at baseline was mainly influenced by age, frequency of habit and duration of habit. The greatest impact was on the psychological domain followed by physical pain. VAS for burning sensation also significantly improved at 6 months.
The therapeutic effect of Spirulina tablet with and without topical triamcinolone acetonide 0.1% was assessed using EORTC QLQ-C35 [17]. At the end of 3rd month after the treatment, there was a decrease in the pain, in swallowing problems, in speech problems, in problems with eating in a social environment, in problems with socializing with other people, in feeling sick, in loss of sexual desire and in opening mouth.
Discussion
Quality of life (QOL) is a broad multidimensional concept that usually includes subjective evaluations of both positive and negative aspects of life [18]. Over the last few years, literature has become replete with data on Health related quality of life.
The effect of oral health on quality of life is finding its footing in comparison to general health considering that a google scholar search of terms “Oral health & Quality of life” vs “General health & Quality of life” yields almost similar result hits.
The data are available at individual, group and community level and therefore is a tool with a capability to interpret data regarding individuals’ perception of disease, their sufferings as well as to identify potential areas of intervention at any level i.e., individual/ group or community.
Amongst the oral health QOL, a very limited data are available on premalignant or potentially malignant lesions. A systematic review [19] on Oral potentially malignant disorders concluded that there was a substantial lacunae in the literature on QoL issues in patients with OPMD, in spite of the potential of these disorders to significantly affect oral function, oro-facial appearance and social interaction. Most of this data are dominated by oral lichen planus or leukoplakia.
Amongst most of the OPMD’s, OSMF is a condition of special need as it has a much more physical restriction, along with recurrent oral ulcerations, burning sensation, habit abuse, economical burden, fear of impending malignancy. Yet, most of the assessment of QOL data in OSMF are by non-disease specific questionnaires.
Amongst the studies that were included, most (7) rated “ weak” on the quality assessment with 2 moderate ratings [9, 10] and only 1 strong rating [8]. Most of the data available on QOL assessment in OSMF are clouded by flawed study designs, lack of confounder adjustment, low sample size, lack of representative population and other study flaws. Lack of strong evidence on QOL is a major setback for a disease that has evolved to its modern epidemic stature. Almost all of these studies are polarized to a single continent, Asia. Considering that the disease is polarized mostly to the same continent as well, one definitely expects more robust strong quality data from the same.
Our study showed that only one study [11] used disease specific questionnaire and the same still needs multicentric, large scale validation for a recommended use in OSMF QOL assessment.
Most of the instruments used in this review focus on the functional and physical limitation, social effects, psychological affect. In contrast to others, the EORTC QLQ-C35 which originally focuses on head neck cancer patients also takes into account the sexual affects, COMDQ takes into account the medications and side effects and patient support, OPMDQOL measures the effect of treatment on daily life in addition to the previous mentioned factors. The disease specific OHRQoL-OSF measures 4 domains discomfort & function, psychological wellness, physical wellness, social wellness.
To the best of our knowledge, this is the first article that has systematically reviewed the literature on QOL in OSMF. The heterogeneity in study population, study designs, QOL instruments and outcome measures makes it difficult for a comparison. Therefore a quantification analysis was not possible. Also pure OSMF data without the involvement of other lesions were less in number.
Although the literature gap on OSMF QOL is quite evident from this review, we did have a few take away information on QOL in OSMF.
The first and foremost is that OSMF not only physically debilitates a patient, it has its repercussions on the social, physical, psychological domains as well. Identification of these target areas as parallel intervention can improve the QOL in these patients drastically. Another aspect is that apart from trismus, which is the most common and evident symptom associated with OSMF, a substantial part of the suffering that ensues is also because of the ulcerations, burning sensation and worsening of dental health. The improvement in these symptoms, as seen in the interventional studies, definitely improves the QOL substantially even if the disease per se is not treated.
Another very important aspect was that QOL worsened with the progression of the disease, longer and higher tobacco abuse contact duration. The higher grade of disease is obviously associated with a greater degree of restriction and symptoms leading to worse QOL. But the often unaccounted and hugely ignored aspects of this are the alteration in taste, tongue atrophy, dryness, change in voice and deafness that is experienced by many patients. The higher amount and longer tobacco abuse could translate into a more severe disease leading to worse QOL. Another ignored aspect is the fact that these patients have greater tobacco dependence, de-addiction pressure and struggles, economical pressure, potentially strained family dynamics due to addiction and all these factors may contribute to further worsening of QOL.
This review is unable to give a confident answer to the evidence on QOL in OSMF but definitely showers light on the evident lack of robust data on the same. Robust methodological and adequately powered studies on assessing QOL in OSMF using only a reliable disease specific questionnaire is the need of the hour.
Conclusion
OSMF not only physically debilitates a patient, it has its repercussions on the social, physical, psychological domains as well. Identification of these target areas as parallel intervention can improve the QOL in these patients drastically. The fear of impending malignancy, psychosocial impact, financial burden, correlation of alleviation of symptoms with QOL, Correlation of disease progression/ resolution with QOL is potential areas that need further attention in studies of OSMF QOL. Moreover, there is a need to formulate a homogenous assessment of QOL using a disease specific questionnaire.
Funding
This article does not receives any funding.
Complaince with ethical standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kirti Chaudhry, Email: chaudhry_kirti@yahoo.com.
Shruti Khatana, Email: shru.k85@gmail.com.
Rishi Bali, Email: rshbali@hotmail.co.uk.
Amanjot Kaur, Email: amanjotkaur1992@yahoo.com.
Naveen Dutt, Email: drnaveendutt@yahoo.co.in.
References
- 1.Warnakulasuriya S. Semi-quantitative clinical description of oral submucous fibrosis. Ann Dent. 1987;46:18–21. [PubMed] [Google Scholar]
- 2.Mukherjee AL, Biswas SK. Oral Submucons fibrosis, A search for an aetiology. Indian J Otolaryngol. 1972;24(1):11–15. doi: 10.1007/BF02991934. [DOI] [Google Scholar]
- 3.Schwartz J 1952 Atrophia idiopathica (tropica) mucosae oris. Demonstrated at the 11th International Dental Congress, London.
- 4.Pindborg JJ, Mehta FS, Gupta PC, et al. Prevalence of oral submucous fibrosis among 50,915 Indian villagers. Br J Cancer. 1968;22(4):646–654. doi: 10.1038/bjc.1968.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazarey VK, Erlewad DM, Mundhe KA, et al. Oral submucous fibrosis: a study of 1000 cases from central India. J Oral Pathol Med. 2007;36(1):12–17. doi: 10.1111/j.1600-0714.2006.00485.x. [DOI] [PubMed] [Google Scholar]
- 6.Shahid RA. Coming to America: betel nut and oral sub mucous fibrosis. JADA. 2010;141(4):423–428. doi: 10.14219/jada.archive.2010.0194. [DOI] [PubMed] [Google Scholar]
- 7.Shevale VV, Kalra RD, Shevale VV, et al. Management of oral sub-mucous fibrosis: a review. Indian J Dent Sci. 2012;2(4):107–114. [Google Scholar]
- 8.Jiang X, Zhang Y, Li F, et al. Allicin as a possible adjunctive therapeutic drug for stage II oral submucous fibrosis: a preliminary clinical trial in a Chinese cohort. Int J Oral Maxillofac Surg. 2015;44(12):1540–1546. doi: 10.1016/j.ijom.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhry K, Bali R, Patnana AK, et al. Impact of Oral Submucous Fibrosis on Quality of Life: A Cross-Sectional Study. J Maxillofac Oral Surg. 2018 doi: 10.1007/s12663-018-1114-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhry K, Bali R, Patnana AK, et al. Impact Of Oral Submucous Fibrosis On Quality Of Life: A Multifactorial Assessment. J Maxillofac Oral Surg. 2019 doi: 10.1007/s12663-019-01190-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gondivkar SM, Bhowate RR, Gadbail AR, et al. Impact of oral submucous fibrosis on oral health-related quality of life: A condition-specific OHRQoL-OSF instrument analysis. Oral Dis. 2018;24(8):1442–1448. doi: 10.1111/odi.12921. [DOI] [PubMed] [Google Scholar]
- 12.Gondivkar SM, Bhowate RR, Gadbail AR, et al. Development and validation of oral health-related quality of life measure in oral submucous fibrosis. Oral Dis. 2018;24(6):1020–1028. doi: 10.1111/odi.12857. [DOI] [PubMed] [Google Scholar]
- 13.Saimadhavi N, Raju M, Reddy RS, et al. Impact of oral diseases on quality of life in subjects attending out-patient department of a dental hospital. India J Orofac Sci. 2013;5:27–31. doi: 10.4103/0975-8844.113690. [DOI] [Google Scholar]
- 14.Tadakamadla J, Kumar S, Lalloo R, et al. Impact of oral potentially malignant disorders on quality of life. J Oral Pathol Med. 2018;47(1):60–65. doi: 10.1111/jop.12620. [DOI] [PubMed] [Google Scholar]
- 15.Jena AK, Rautray S, Mohapatra M, et al. Oral health-related quality of life among male subjects with oral submucous fibrosis in a tertiary care hospital. Indian J Public Health. 2018;62:271–276. doi: 10.4103/ijph.IJPH_179_17. [DOI] [PubMed] [Google Scholar]
- 16.Rimal J, Shrestha A. Validation of Nepalese Oral Health Impact Profile14 and Assessment of Its Impact in Patients with Oral Submucous Fibrosis in Nepal. J Nepal Health Res Counc. 2015;13(29):43–49. [PubMed] [Google Scholar]
- 17.Chole RH, Patil R. Assessment of the quality of life and performance status in patients with oral submucous fibrosis in central India. Clujul Med. 2018;91(2):203–208. doi: 10.15386/cjmed-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The WHOQOL Group The World Health Organization Quality of Life Assessment (WHOQOL). Development and psychometric properties. Soc Sci Med. 1998;46:1569–1585. doi: 10.1016/S0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 19.Tadakamadla J, Kumar S, Johnson N. Quality of life in patients with oral potentially malignant disorders: a systematic review, Oral Surgery, Oral Medicine. Oral Pathol and Oral Radiol. 2015 doi: 10.1016/j.oooo.2015.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Namrata M, Kumar VJ. Assessment of quality of life in patients with chronic oral mucosal diseases: A questionnaire based study. Int J Orofac Biol. 2017;1:24–27. [Google Scholar]