Abstract
Aims
Hospitalization for heart failure (HF) constitutes a major healthcare and economic burden. Trends and characteristics of hospitalizations for HF for the recent years are not clear. We sought to determine the trends and characteristics of hospitalization for HF in the United States.
Method and results
A retrospective analysis of the National Inpatient Sample weighted data between 1 January 2004 and 31 December 2018, which included hospitalized adults ≥ 18 years with primary discharge diagnosis of HF using International Classification of Diseases‐9/10 administrative codes. Main outcomes were trends in hospitalizations for HF (per 1000 person) and inpatient mortality (%) between 2004 and 2018.
Conclusions
Hospitalizations for HF have been increasing across both sexes and age groups since 2013, whereas inpatient mortality has been decreasing over the study period. Blacks have the highest risk of hospitalization for HF, and Whites have the highest in‐hospital mortality. There are significant racial and geographic disparities related to hospitalizations for HF.
Keywords: Heart failure, Hospitalizations, Mortality, Characteristics, Age, Sex, Race, Season
Background
The prevalence of heart failure (HF) is projected to increase to more than eight million people in the United States (US) by the year 2030, and it is already the leading cause of hospitalization among older US adults and the second most common overall cause of hospitalization in the US. 1 , 2 , 3 , 4 These hospitalizations for HF are associated with significant morbidity, mortality, and healthcare expenditure, 5 and stakeholders have increasingly recognized the public health and economic impacts.
Aim
In this analysis, we sought to report the longitudinal trends in hospitalizations for HF between 2004 and 2018 according to age, sex, race, hospital location, and season and the associated inpatient mortality and length of stay (LOS).
Method
We conducted a retrospective analysis of discharge data from the National Inpatient Sample (NIS) between 1 January 2004 and 31 December 2018. We identified hospitalizations among patients 18 years or older in the NIS database with a primary discharge diagnosis of HF using International Classification of Diseases (ICD), 9th Revision (398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, and 428.xx) and 10th Revision (I09.81, I11.0, I13.0, I13.2, and I50.xx), Clinical Modification codes. 6 , 7 We estimated crude primary hospitalizations per 1000 US adults, the denominator for which was extracted from US Census Bureau estimates of US resident populations for each study year. 8 These were further age‐adjusted based on the US standard population from the year 2000. For subgroup analysis, hospitalizations have been reported per 1000 respective US subpopulation. Inpatient mortality was estimated as proportion of deaths in HF hospitalizations over total number of HF hospitalizations for adult patients. Inpatient mortality trend was adjusted for age via logistic regression. To account for the NIS sample redesign in 2012, we used the updated trend weights for the period between 2004 and 2011 and the original discharge weights for the years 2012 to 2018. As the missing data for the race categories were substantial, we applied multivariate imputation by chained equation to impute the missing data for race in order to accurately estimate the prevalence of HF hospitalizations stratified by race groups. Missing race/ethnicity was imputed using a multinomial logistic model using age, sex, comorbid conditions, and hospital characteristics.
We estimated overall trends of primary HF hospitalizations, stratified by age groups, gender, race, and rural/urban location of hospitals. We further explored trends in primary HF hospitalizations stratified by seasons.
Trends in crude and age‐adjusted hospitalizations, LOS, and inpatient mortality were examined using the Joinpoint Regression Programme. This programme identifies significant changes among annual trends through joinpoint regression, which fits models of linear segments where temporal variation occurred. We performed joinpoint regression under the assumption of constant variance and uncorrelated errors. Annual percentage change (APC) with 95% confidence intervals (CI) were calculated using the Monte Carlo permutation test among intervals identified by the joinpoint regression. Joinpoint regression was done using Joinpoint V 4.9.0.0 (available from National Cancer Institute). All other analyses were performed using Stata 16.1 (StataCorp, LP, College Station, Texas). Our analyses took into account survey design complexity by incorporating sampling weights, primary sampling units, and strata.
Results
Trends in heart failure hospitalization, in‐hospital mortality, and length of stay
Between 2004 and 2013, crude HF hospitalizations declined from 5.26 hospitalizations per 1000 US adults compared with 3.96 hospitalizations per 1000 US adults with an APC of −3.4 [95% CI (−3.8, −2.9)]; however, this was followed by an increase up to 4.9 hospitalizations per 1000 US adults in 2018 with an APC of 4.7 [95% CI (3.6, 6)]. After adjusting for age, the same trend was observed with an APC of −4.1 [95% CI (−4.6, −3.7)] for age‐adjusted HF hospitalization between 2004 and 2013 and an APC of 3.5 [95% CI (2.3, 4.7)] for age‐adjusted HF hospitalization between 2013 and 2018.
Between 2004 and 2007, in‐hospital mortality for HF hospitalization declined from 4.0% to 3.2% with an APC of −5.9 [95% CI (−8.5, −3.2)] followed by a less steep decline to 2.6% in 2018 with an APC of −1.9 [95% CI (−2.3, −1.5)].
Between 2004 and 2006, mean LOS for HF hospitalizations decreased from 5.5 to 5.3 days [slope estimate −0.09; SE (0.03); P value = 0.02] followed by a less steep decline to 5.1 days in 2011 [slope estimate −0.02; SE (0.01); P value = 0.02]. Following that, an increase in the mean of LOS of HF hospitalization occurred up to 5.4 days in 2018 [slope estimate 0.03; SE (0.004); P value = 0.01; Figure 1 ].
Figure 1.
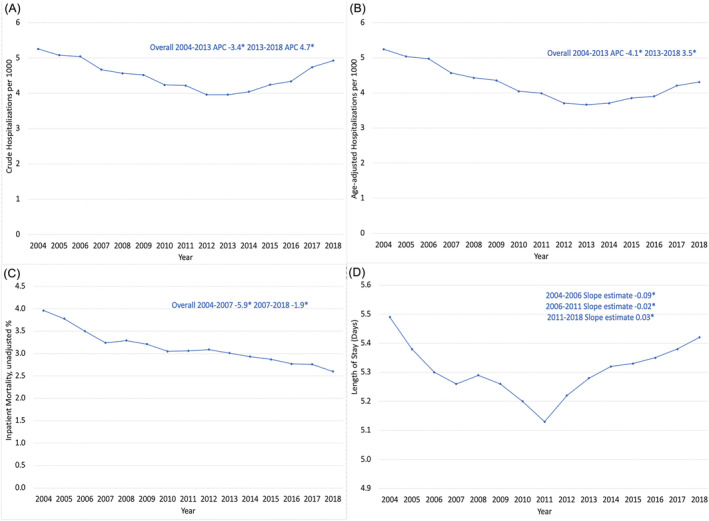
(A) Trends of crude hospitalization for heart failure between 2004 and 2018. (B) Trend of age‐adjusted hospitalization for heart failure between 2004 and 2018. (C) Trends in inpatient mortality for heart failure hospitalizations between 2004 and 2018. (D) Trends in length of stay of heart failure hospitalizations between 2004 and 2018 [* means annual percentage change (APC) or slope estimate is significantly different from zero at α = 0.05].
Trends according to age, sex, race, and hospital location
Overall, mean age of HF hospitalizations was 72.3 [mean (standard error) 0.04] years and female patients accounted for 50% of these hospitalizations. Over the study period, Whites accounted for 67.2% of HF hospitalizations, Blacks accounted for 20.2% of HF hospitalizations, and Hispanics accounted for 8.0% of HF hospitalizations. About 85.8% of HF hospitalizations were in urban hospitals and 14.2% were in rural hospitals. Trends in age‐adjusted HF hospitalizations according to age, sex, race, and hospital location are shown in Figure 2 .
Figure 2.
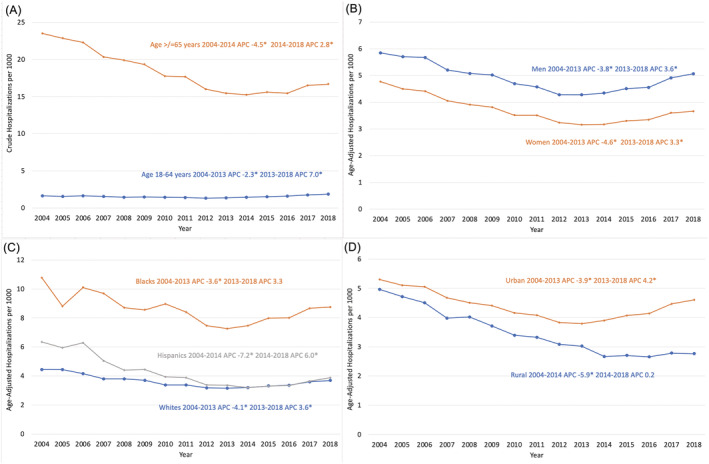
(A) Trends of hospitalization for heart failure according to age between 2004 and 2018. (B) Trends of hospitalization for heart failure according to sex between 2004 and 2018. (C) Trends of hospitalization for heart failure according to race between 2004 and 2018. (D) Trends of hospitalization for heart failure according to hospital location between 2004 and 2018 [*means annual percentage change (APC) is significantly different from zero at α = 0.05].
Whites had the highest in‐hospital mortality rate for HF hospitalization with a mortality rate of 3.6%. Between 2004 and 2018, both age‐adjusted and unadjusted in‐hospital mortality rate for HF hospitalizations decreased across all races (Figure 3 ). For Whites, age‐adjusted in‐hospital mortality decreased from 3.8% in 2004 to 3.2% in 2007 with an APC of −6.2 [95% CI (−8.8, −3.5)] followed by a less steep decline to 2.6% in 2018 with an APC of −1.8 [95% (−2.1, −1.4)] between 2007 and 2018. For Blacks, age‐adjusted in‐hospital mortality decreased from 2.8% in 2004 to 2.0% in 2009 with an APC of −5.8 [95% CI (−7.2, −4.3)] followed by a less steep decline to 1.9% in 2018 with an APC of −0.8 [95% (−1.4, −0.2)] between 2009 and 2018. For Hispanics, age‐adjusted in‐hospital mortality decreased from 3.3% in 2004 to 2.3% in 2010 with an APC of −5.9 [95% (−8.7, −2.9)] followed by a statistically nonsignificant increase to 2.6% in 2013 with an APC of 4.4 [95% CI (−12.9, 25.2)] between 2010 and 2013. This was followed by a statistically nonsignificant decrease to 2.1% in 2013 with an APC of −3.3 [95% CI (−7.1, 0.7)] between 2013 and 2018.
Figure 3.
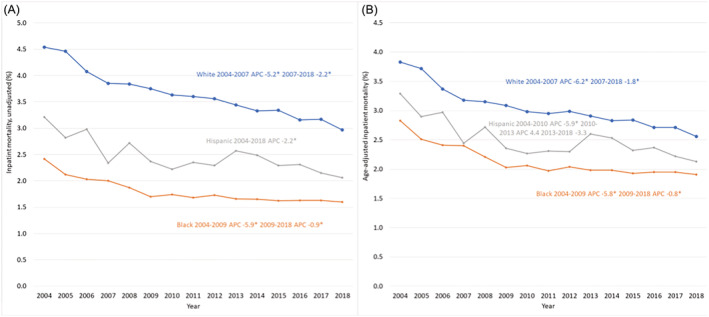
(A) Trends of unadjusted inpatient mortality of hospitalization for heart failure according to race between 2004 and 2018. (B) Trends of age‐adjusted inpatient mortality of hospitalization for heart failure according to race between 2004 and 2018.
Trends according to season
Between 2004 and 2018, 27.1% of HF hospitalization occurred in January to March, 25.4% occurred in October to December, 24.9% occurred in April to June, and 22.6% occurred in July to September. Trends in HF hospitalization according to season between 2004 and 2018 are shown in Figure 4 .
Figure 4.
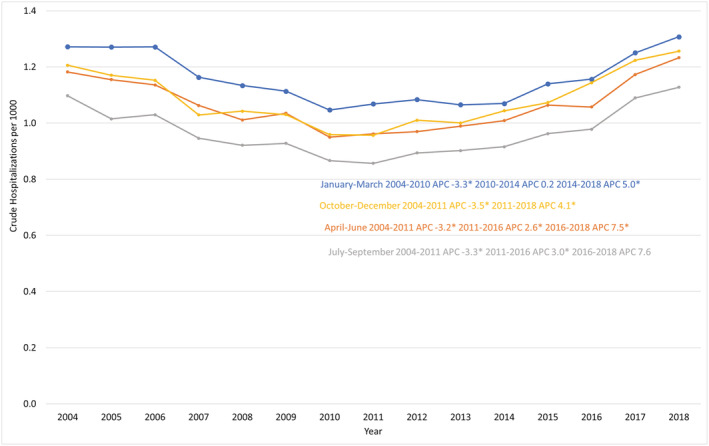
Trends of heart failure hospitalization according to season between 2004 and 2018 (* means a statistically significant difference).
Conclusion
There are several important findings in this NIS analysis of the characteristics and trends of HF hospitalizations between 2004 and 2018. First, despite an initial decline, there has been an increase in HF hospitalizations after 2013. Second, this trend of increase in HF hospitalizations is consistent across both sexes and age groups (i.e. those who are ≥65 years old or younger). HF hospitalizations increased in both Whites and Hispanics, where remained stable in Blacks during the latter part of the study period. Despite this plateau, Blacks have the highest overall rate of hospitalization for HF of all races. Third, Whites have the highest in‐hospital mortality for HF. Fourth, in‐hospital mortality for HF has decreased over the study period.
The increasing trend of HF hospitalization in the recent years is likely due to: (i) changing in the profile of patients' characteristics (i.e. improved overall survival of HF with increasing ageing population and high burden of comorbidities) and (ii) systematic failure in the healthcare system, for example, while the introduction of the Hospital Readmissions Reduction Programme in the US, which targeted readmissions from HF, acute myocardial infarction, and pneumonia and penalized hospitals with excess readmission rates, resulted in a reduction in 30 day and 1 year risk of readmissions for HF, this programme was associated with an increase in 30 day and 1 year mortality in patients with HF. 9 , 10 As these findings may signal a compromise in optimizing the factors associated with survival in patients with HF (e.g. initiating/up‐titrating guideline‐directed medical therapy and addressing risk factors), most of which are also associated with an increased risk of hospitalization for HF, coupled with an increase in the complexity of the comorbidities of these patients, the cumulative adverse effect may have led to an increase in the long‐term risk of hospitalization for HF (i.e. >1 year risk) and patients with a more severe and complex form of HF with recurrent hospitalizations. The racial and geographic disparities observed in our study may relate to inequitable access to HF therapies. 11
Consistent with recent NIS analyses showing an increasing trend of HF hospitalization since 2014, 12 , 13 we show similar findings, but we also show that despite this trend, in‐hospital mortality for HF hospitalization has been declining. We also show that this trend is consistent regardless of the sex or age group. We also show significant racial disparities related to HF hospitalization as manifested by higher HF hospitalizations among Blacks compared with other races, whereas Whites have the highest in‐hospital mortality for HF hospitalizations. In a prior NIS analysis between 2002 and 2013, 14 Whites also had the highest in‐hospital mortality for HF hospitalization; in our analysis, this trend continued beyond 2013. We also show geographic disparities manifested by a higher burden of HF hospitalization in urban hospitals compared with rural hospitals in the recent years.
Several limitations should be acknowledged in our study. First, this was a retrospective analysis of the NIS, which is mainly an administrative database that uses codes for billing purposes. Second, the analysis was based on data related to hospital discharges rather than individual patients; therefore, patients with recurrent hospitalization may have affected the data and its interpretation. Third, both ICD9 and ICD10 were included due to the switch in ICD coding in 2015.
In summary, hospitalizations for HF have been increasing since 2014 among both sexes and age groups. Despite a decline in in‐hospital mortality, racial and geographic disparities exist with the highest hospitalizations for HF being among Blacks and highest in‐hospital mortality for HF being among Whites along with higher burden of HF hospitalization in urban hospitals compared with rural hospitals.
Conflict of interest
S.J.G. receives research support from the American Heart Association, Amgen, AstraZeneca, Bristol‐Myers Squibb, Merck, and Novartis; serves on advisory boards for Amgen and Cytokinetics; and serves as a consultant for Amgen and Merck. A.P.A. is supported by a Mentored Patient‐Oriented Research Career Development Award (K23HL150159) through the National Heart, Lung, and Blood Institute; has received relevant research support through grants to his institution from Amarin Pharma, Inc., Abbott, and Novartis; and has received modest reimbursement for travel from Novartis. M.V. receives grant support or serves on advisory boards for American Regent, Amgen, AstraZeneca, Bayer AG, Baxter Healthcare, Boehringer Ingelheim, Cytokinetics, and Relypsa, and participates on clinical endpoint committees for studies sponsored by Galmed, Novartis, and the NIH. M.F. was supported by NHLBI K23HL151744 from the National Heart, Lung, and Blood Institute (NHLBI), the American Heart Association Grant 20IPA35310955, Mario Family Award, Duke Chair's Award, Translating Duke Health Award and Bayer. He receives consulting fees from AxonTherapies, Daxor, Edwards LifeSciences, NXT Biomedical. All other authors report no relevant disclosures.
Salah, H. M. , Minhas, A. M. K. , Khan, M. S. , Khan, S. U. , Ambrosy, A. P. , Blumer, V. , Vaduganathan, M. , Greene, S. J. , Pandey, A. , and Fudim, M. (2022) Trends and characteristics of hospitalizations for heart failure in the United States from 2004 to 2018. ESC Heart Failure, 9: 947–952. 10.1002/ehf2.13823.
Husam M. Salah and Abdul Mannan Khan Minhas are primary co‐authors.
References
- 1. Pfuntner A (Truven Health Analytics) WLTHA, Stocks C (AHRQ). Most frequent conditions in U.S. hospitals, 2011. HCUP Statistical Brief #162. 2013.
- 2. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Piña IL, Trogdon JG. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013; 6: 606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol 2016; 13: 368–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salah HM, Minhas AMK, Khan MS, Pandey A, Michos ED, Mentz RJ, Fudim M. Causes of hospitalization in the USA between 2005 and 2018. Eur Heart J Open 2021; 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJV, Granger CB, Yusuf S, Swedberg K, Young JB, Michelson EL, Pfeffer MA. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 2007; 116: 1482–1487. [DOI] [PubMed] [Google Scholar]
- 6. Nazir S, Minhas AMK, Kamat IS, Ariss RW, Moukarbel GV, Gomez JCP, Fedson S, Nair A, Bozkurt B, Jneid H. Patient characteristics and outcomes of type 2 myocardial infarction during heart failure hospitalizations in the United States. Am J Med 2021; 134: 1371–1379.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kichloo A, Minhas AMK, Jamal S, Shaikh AT, Albosta M, Singh J, Khan MZ, Aljadah M, Wani F, Wazir MHK, Kanjwal K. Trends and inpatient outcomes of primary heart failure hospitalizations with a concurrent diagnosis of acute exacerbation of chronic obstructive pulmonary disease (from the National Inpatient Sample Database from 2004 to 2014). Am J Cardiol 2021; 150: 69–76. [DOI] [PubMed] [Google Scholar]
- 8. Bureau TUC . The US Census Bureau estimates of US populations
- 9. Fonarow GC. Unintended harm associated with the hospital readmissions reduction program. JAMA 2018; 320: 2539–2541. [DOI] [PubMed] [Google Scholar]
- 10. Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, Hernandez AF, Peterson ED, Matsouaka RA, Yancy CW, Fonarow GC. Association of the hospital readmissions reduction program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol 2018; 3: 44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mwansa H, Lewsey S, Mazimba S, Breathett K. Racial/ethnic and gender disparities in heart failure with reduced ejection fraction. Curr Heart Fail Rep 2021; 18: 41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Agarwal MA, Fonarow GC, Ziaeian B. National trends in heart failure hospitalizations and readmissions from 2010 to 2017. JAMA Cardiol 2021; 6: 952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Salah HM, Khan Minhas AM, Khan MS, Khan SU, Ambrosy AP, Blumer V, Vaduganathan M, Greene SJ, Pandey A, Fudim M. Trends in hospitalizations for heart failure, acute myocardial infarction, and stroke in the United States from 2004‐2018. Am Heart J 2021; 243: 103–109. [DOI] [PubMed] [Google Scholar]
- 14. Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National differences in trends for heart failure hospitalizations by sex and race/ethnicity. Circ Cardiovasc Qual Outcomes 2017; 10: e003552. [DOI] [PMC free article] [PubMed] [Google Scholar]


