Abstract
Objectives
Journaling is a common non-pharmacological tool in the management of mental illness, however, no clear evidence-based guideline exists informing primary care providers on its use. We seek here to present this synthesis that may begin to inform future research and eventual evidence-based guideline development.
Design
Of the 3797 articles retrieved from MEDLINE, EMBASE, PsycINFO, 20 peer-reviewed randomised control trials (31 outcomes) met inclusion criteria. These studies addressed the impact of a journaling intervention on PTSD, other anxiety disorders, depression or a combination of the aforementioned.
Eligibility criteria
Peer reviewed, randomised control trials on the impact of journaling on mental illness were included.
Information sources
MEDLINE, EMBASE and PsycINFO.
Results
The data are highly heterogeneous (control arm=I2 of 71.2%, intervention arm=I2 of 83.8%) combined with a B-level Strength of Recommendation Taxonomy recommendation. It was additionally found that there is a significant pre–post psychometric scale difference between control (−0.01, 95% CI −0.03 to 0.00) and intervention arms (−0.06, 95% CI −0.09 to −0.03). This 5% difference between groups indicates that a journaling intervention resulted in a greater reduction in scores on patient health measures. Cohen’s d effect size analysis of studies suggests a small to moderate benefit.
Conclusion
Further studies are needed to better define the outcomes. Our review suggests that while there is some randomised control data to support the benefit of journaling, high degrees of heterogeneity and methodological flaws limit our ability to definitively draw conclusions about the benefit and effect size of journaling in a wide array of mental illnesses. Given the low risk of adverse effects, low resource requirement and emphasis on self-efficacy, primary care providers should consider this as an adjunct therapy to complement current evidence-based management.
Keywords: mental health; family medicine; physicians, primary care; health knowledge, attitudes, practice
Introduction
Although journaling is a widely used tool in the management of mental illness, there have been limited efforts to systematically review this paradigm in the Canadian context. There is additionally no current evidence-based guidance about the utility of journaling as a non-pharmacological treatment modality for family physicians. This is despite the fact that general practitioners represent a large majority of the front line of treatment for individuals suffering from mental illness.1
Similar to anything else that is prescribed, journaling as an intervention has several complexities which are important to consider when using this tool.2 These complexities include variables such as what is written, instruction provided on how to journal, duration of a journaling session and the optimal number of journaling sessions needed to see improvement.3 In respect to medications, the duration of effect with respect to pharmacokinetics is well understood among the scientific community.4 However, there is little known and understood about the duration of effect for journaling.
The two primary forms of journaling used in psychotherapy are expressive writing and gratitude journaling.5 Expressive writing is a journaling technique which is performed for 3–4 sessions about ‘one’s deepest thoughts and feelings’ for 20 min per session.6 A gratitude journal on the other hand is a diary of accounts for which one is grateful, and where attention is focused on the positive aspects of one’s life.7 Instruction on how to journal is essential in ensuring proper utility of the tool and instilling self-efficacy in the patient.3 The literature, however, is sparse in areas investigating these variables which moderate the effects of journaling.
This is the first study to examine the efficacy of journaling as an intervention for improving mental health outcomes with a meta-analysis.
We seek to state in terms relevant to primary care clinicians the current state of the data and provide further areas for study. To the best of our knowledge, this paper is the first to report a systematic review and meta-analysis of journaling as an intervention to improve mental health.
Methods
Study design and search strategy
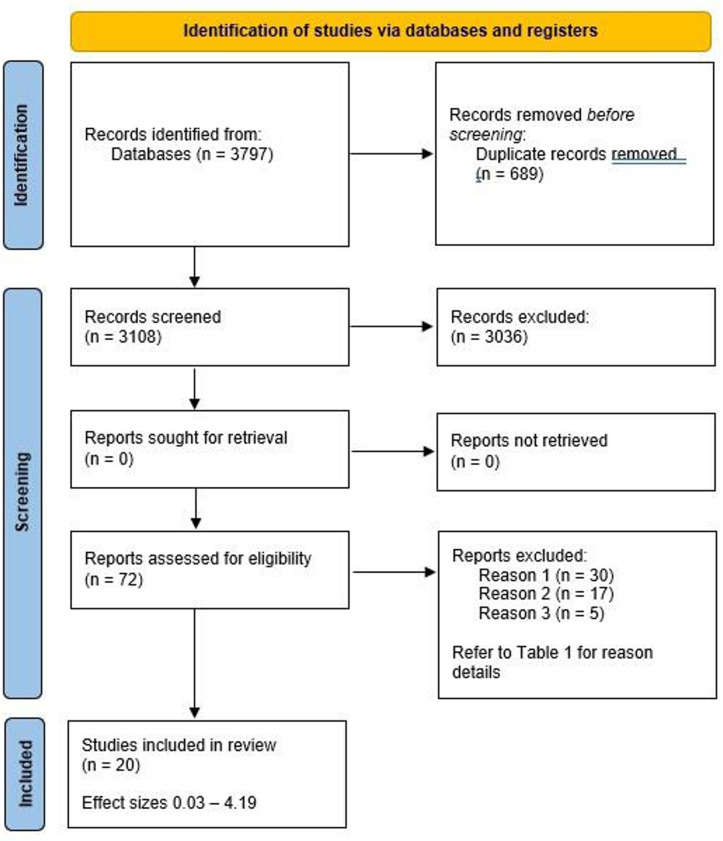
A systematic review and meta-analysis of the literature focused on journaling interventions to improve mental health outcomes was conducted. The different phases of the systematic review are displayed in figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 flow diagram.
The following databases were searched: MEDLINE, EMBASE and PsycINFO (March 2020). The main search concepts used as both subject headings and keywords journaling and mental health. Detailed MEDLINE search strategy can be seen in online supplemental appendix 1. Initial screening of titles and abstracts was done by MS and BSD. The initial screening involved reading titles and abstracts.
fmch-2021-001154supp001.pdf (102.5KB, pdf)
Articles were included and excluded based on the criteria outlined in table 1. Secondary screening involved reading full-length articles and was done by MS, BSD and PS. Disagreements over study eligibility were resolved through discussion with HSG. The list of selected articles can be seen in online supplemental appendix 2.
Table 1.
Inclusion and exclusion criteria used in primary and secondary screenings
| Inclusion criteria | Exclusion criteria |
| Peer reviewed | Studies which examined the effect of multiple types of journaling |
| Randomised control trials | Studies with insufficient or missing data which was required to perform a meta-analysis |
| Studied the impact of a journaling intervention on mental illness | Studies which examined the effects of a journaling intervention on well-being only |
Statistical analysis
Meta-analysis statistics
The effect measure was calculated by subtracting poststudy scores from baseline scores and then dividing this number by the total maximum score allocatable on the questionnaire used, to assess percentage change. This method was selected, as the majority of studies in this review implemented different measures for scoring changes in mental health status. All questionnaires and health measures used in the studies included in this review indicate that a higher score is suggestive of more severe mental illness. MEDCALC Software was used to calculate 95% CIs and SE for the effect measures. A random effects linear meta-regression analysis was performed on both the intervention and control groups. A forest plot was generated using STATA V.13 software.
Meta-regression statistics
Meta-regression, a form of moderator analysis, was used to determine sources of heterogeneity within the sample of studies and to test whether the relationship between two variables depends on (is moderated by) the value of a third variable. The analysis was performed on the following variables: type of journaling, intervention duration, journal collection/analysis, sample size, participant sex and age, and geographical region where the studies were conducted. Additionally, type of mental illness was also investigated as a source of heterogeneity with anxiety as the reference category in relation to PTSD and depression. The meta-regression was conducted on all included articles, as well as the symptom subgroups of anxiety, PTSD and depression individually.
Cohen’s d effect size
Our preferred manner of stating the results from this review was in an ORs and number needed to treat. However, the data did not present in a manner that allowed for us to calculate these numbers. Given our inability to calculate a proper OR for the studies, we calculated a Cohen’s d to give a perspective of significance. Cohen’s d effect size was calculated using means, SD, and sample sizes of the intervention group at baseline and postintervention. Three particular reference points have been established for interpreting Cohen’s d effect size. Effect sizes are classified as small (d = 0.2), medium (d = 0.5) and large (d≥0.8).8 According to Cohen, ‘a medium effect of 0.5 is visible to the naked eye of a careful observer’.8 A small effect of 0.2 is noticeably smaller than medium but not so small as to be trivial. A large effect of 0.8 is the same distance above the medium as small is below it. Increasing effect sizes indicate a larger difference between the means of the intervention and control groups.
Risk of bias assessment
The revised Cochrane risk of bias tool (ROB-2)9 for randomised control trials was used to assess outcomes at the study level for each article included in this review. This tool scores studies on five domains including randomisation (domain 1), effect of assignment to the intervention (domain 2), missing outcome data (domain 3), measurement of the outcome (domain 4), selection of the reported result (domain 5), and lastly, the overall risk of bias.9 Please see Sterne et al’s paper9 for more information on the ROB-2 tool.
Strength of Recommendation Taxonomy
The Strength of Recommendation Taxonomy (SORT) tool was used to determine the strength and quality of evidence for the studies included in this systematic review and meta-analysis.
The SORT has three levels of recommendation of evidence including A-level, B-level and C-level. The definitions of each SORT level of recommendation are quoted below as per Ebell et al.10
‘An A-level recommendation is based on consistent and good quality patient-oriented evidence. A B-level recommendation is based on inconsistent or limited quality patient-oriented evidence. A C-level recommendation is based on consensus, usual practice, opinion, disease-oriented evidence, or case series for studies of diagnosis, treatment, prevention or screening.’10
Results
Search outcomes
An initial search of the databases generated a total of 3797 articles. A total of 689 duplicate articles were removed from the initial pool of articles and 3108 articles remained for primary screening. The primary and secondary screenings resulted in a total of 20 articles which were analysed for the purposes of this meta-analysis. Online supplemental appendices 3,5 for details the demographic variables, results, questionaries and measure used to calculate outcomes across studies.
A total of 20 articles and 31 outcomes are presented in this paper. There are more outcomes than articles as several articles examined the effects of a journaling intervention on more than one symptom of mental illness (eg, anxiety and depressive symptoms, or anxiety, depression and PTSD). All articles employed either an expressive writing (17) or gratitude journaling (3) intervention. As seen in table 2, most studies used a different measure to determine changes in mental health. In order to standardise each outcome, the postintervention scores were subtracted from baseline scores and then divided by the maximum score possible on the respective questionnaire to determine percentage change. Data from the intervention and control groups were calculated and analysed separately. Online supplemental appendix 4 details the journaling type, mental illness symptom studied, effect size and significance of outcomes across individual studies.
Table 2.
Intervention parameters including journaling duration, journal analysis and/or collection and preparatory session administration preintervention
| Study | Journaling session duration (min) |
No of journaling sessions | Journals collected and/or analysed (yes/no) |
Preparatory session* (yes/no) |
| Alparone et al (2015) | 20 | 3 | Yes | No |
| Bernard et al (2006) | 15 | 3 | Yes | No |
| Dennick et al (2015) | 20 | 3 | Yes | No |
| Di Blasio et al (2015) | Unspecified | 2 | No | No |
| Ducasse et al (2018) | Unspecified | 7 | No | No |
| Graf et al. (2008) | 20 | 2 | No | No |
| Horsch et al (2016) | 15 | 3 | Yes | No |
| Jensen-Johansen et al (2012) | 20 | 3 | No | No |
| Barton & Jackson (2008) | 20 | 3 | Yes | No |
| Koopman et al (2005) | 20 | 4 | No | No |
| Barry and Singer (2001) | 20 | 4 | Yes | No |
| Lovell et al (2016) | 20 | 3 | Yes | No |
| Suhr, Risch and Wilz (2017) | Unspecified | 3 | No | No |
| Martino et al (2012) | Unspecified | 2 | No | No |
| Meshberg-Cohen et al (2014) | 20 | 4 | Yes | No |
| Possemato et al (2010) | 15 | 3 | Yes | No |
| Rabiepoor et al (2019) | 15 | 21 | No | No |
| Rawlings et al (2018) | 20 | 4 | Yes | No |
| Schache et al (2019) | Unspecified | 32 | No | No |
| Wong and Mak (2016) | 20 | 3 | Yes | No |
*A preparatory session refers to an educational session given to participants preintervention which outlines the mechanisms and theories underlying the efficacy of journaling as well as how to journal in the most effective manner.
The systematic review revealed 68% of the intervention outcomes were effective, with a significant difference between the control and intervention groups supporting the efficacy of journaling. As shown in table 3, of the nine outcomes regarding PTSD (all employed an expressive writing intervention), six showed significant reductions in symptoms postintervention. Of the four outcomes that involved a gratitude journaling intervention, three showed significant improvements in symptomology postintervention. Of the 27 outcomes that implemented an expressive writing intervention, 19 showed significant improvements postintervention.
Table 3.
Results of meta-regression without subgroups
| Study arm | Intervention arm | Control arm | ||||
| Variable | Regression coefficient | P value | Regression coefficient | P value | ||
| Sample size | 0.023 | 0.445 | −0.025 | 0.247 | ||
| Type of journaling | −0.043 | 0.176 | −0.036 | 0.124 | ||
| Study duration | −0.052 | 0.183 | −0.043 | 0.147 | ||
| Journal analysis | −0.064 | 0.021* | −0.026 | 0.254 | ||
| Sex | 0.052 | 0.063 | 0.030 | 0.158 | ||
| Age | 0.019 | 0.503 | −0.034 | 0.111 | ||
| Region-Europe | −0.097 | 0.217 | 0.502† | −0.023 | 0.714 | 0.971† |
| Region-North America | −0.122 | 0.150 | −0.022 | 0.750 | ||
| Region-Australia | −0.060 | 0.596 | −0.042 | 0.635 | ||
| Depression‡ | 0.060 | 0.122 | 0.266 | 0.006 | 0.838 | 0.763 |
| PTSD‡ | 0.030 | 0.459 | 0.022 | 0.51 | ||
*Sample size <30 or>30.
†When regions analysed in aggregate.
‡Depression and PTSD regression analyses were calculated using anxiety as the reference category.
PTSD, post-traumatic stress disorder.
As seen in table 2, a considerable majority (85%) of the studies implemented a short-term journaling intervention ranging from 2 to 4 journaling sessions. Three studies implemented a long-term journaling intervention ranging from 7 to 32 journaling sessions. Additionally, 55% of the studies collected and or analysed participant journal entries. Out of the 20 studies, none implemented a preparatory/educational session at the preintervention phase.
Table 3 summarises the results from the meta-regression analyses performed on multiple study variables, examining also the three symptom subgroups of anxiety, depression and PTSD. Variables assessed to determine moderators of heterogeneity included: type of journaling, length of intervention, age, region, sex, mental illness symptom (depression and PTSD with anxiety as the reference category), sample size (<30 or>30 participants), and journals analysis and/or collection. Of these variables, the only significant moderator was journal analysis and/or collection (r=−0.064; p=0.021), which indicates that when journals are not collected or analysed the efficacy of journaling is greater. The remaining variables were not deemed as significant moderators contributing to the heterogeneity of the data for the whole group.
We explored this further in a meta-regression on symptom subgroups, please refer to tabulated summaries in online supplemental appendix 6. We found that the anxiety subgroup showed poorer pre/post scores for both intervention and control arms for studies with mixed genders compared with a single gender (intervention r=0.178 p=0.038, control r=0.181 p=0.002). From this, we can infer that journaling works better for women and this improvement in health outcomes is also supported in the literature.6
Depression subgroup analysis showed that journaling length >30 days compared with <30 days improved pre–post scores by 10.4% (r=−0.104, p=0.005), indicating a longer intervention is optimal.
PTSD subgroup showed age as a relevant moderator for the intervention arm (r=0.073, p=0.012), whereby pre/post scores worsened with age: journaling is less effective the older one gets.
The forest plot in figure 2 illustrates that following standardisation of the data there is a significant difference between control (−0.01, 95% CI −0.03 bto 0.00, p≤0.001) and intervention arms (−0.06, 95% CI −0.09 to −0.03, p≤0.001) between all groups. This 5% difference between groups is statistically significant and indicates that a journaling intervention resulted in a greater reduction in scores on patient health measures when compared with the control arm.
Figure 2.
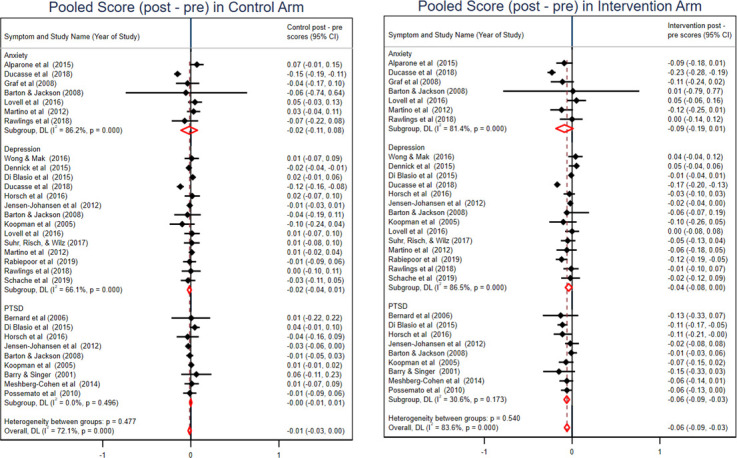
Standardised forest plot for control and intervention groups.
Subgroup analysis further indicated that when studies examining journaling in anxiety disorders, a reduction in pre–post intervention scores was 9%–0.09 (95% CI −0.19 to 0.01, p≤0.001) compared with control scores at 2%–0.02, (95% CI −0.11 to 0.08, p≤0.001).
In the depression subgroup, the intervention scores difference was 4%–0.04 (95% CI −0.08 to 0.00, p≤0.001) compared with the control scores 2%–0.02 (95% CI −0.04 to 0.01, p≤0.001).
In the PTSD subgroup, intervention scores showed a difference of 6%–0.06 (95% CI −0.09 to −0.03, p≤0.001) compared with control scores (95% CI −0.01 to 0.01, p=0.496).
The data, however, have a high degree of heterogeneity indicated by an I2 of 71.2% in the control arm and an I2 of 83.8% in the intervention arm. There was lower heterogeneity in the PTSD subgroup at I2 of 30.6%, in comparison to anxiety (I2=86.5%) and depression (I2=81.4%) subgroups.
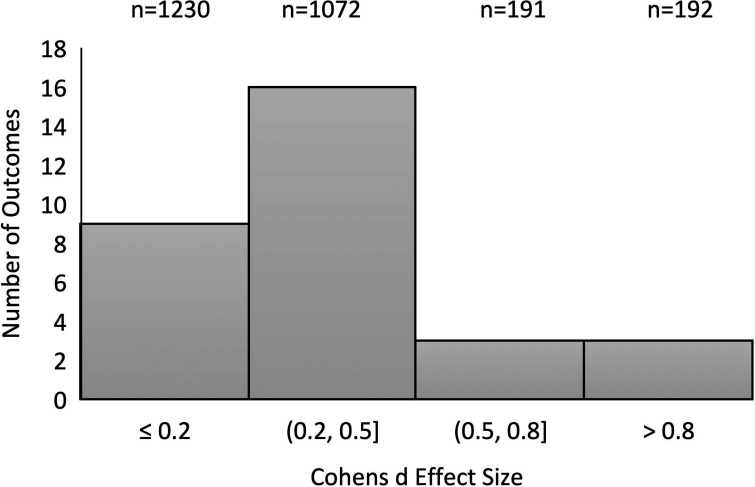
Figure 3 illustrates a histogram depicting Cohen’s d effect size8 for the 31 outcomes. Cohen’s d effect size provides a standardised representation of the distribution of means between the control and intervention group. For the purpose of calculating Cohen’s d effect size for this histogram, postintervention scores of the control and intervention groups were used. A total of nine outcomes indicated a Cohen’s effect size <0.2 (small effect size). Sixteen outcomes fall between 0.2 and 0.5 (small to moderate effect size) and the remaining six outcomes are above 0.5 (moderate to large effect size).
Figure 3.
Histogram of Cohen’s d effect size of journaling efficacy. n indicates the numbers of participants within each Cohen’s effect size classification.
The ROB-2 tool9 was used to determine the risk of bias at the individual study level for all articles included in this review. The majority of the studies (12) fall under a ‘low-risk’ categorisation with three falling under a ‘high-risk’ categorisation and five falling under the ‘some concerns’ categorisation. Refer to online supplemental appendix 7 for a detailed presentation of ROB-2 results.
The SORT taxonomy was used to determine quality of evidence of all studies included in this article. The articles included in this review are graded as a B-level recommendation. A B-level recommendation indicates that ‘the data are inconsistent, or limited quality patient-oriented evidence’.10
Discussion
This is the first study to examine the efficacy of journaling as an intervention for improving mental health outcomes with a meta-analysis. The results of this work revealed that a journaling intervention resulted in an average statistically significant 5% reduction in patient scores on mental health measures compared with control arms, with a greater benefit in anxiety (9%) and PTSD (6%) symptom subgroups, and a lesser benefit in depression subgroup (2%). Due to heterogeneity of the scales used, we are unable to comment on whether this finding is clinically significant (as that varies depending on the scale used), though our findings would support the wide use of journaling in many forms of psychotherapy for a broad range of mental illnesses.11
The high degree of heterogeneity of the data in the intervention arm (I2=83.8%) as well as the B-level SORT recommendation indicates that it is difficult to draw any robust conclusions from this meta-analysis, although the PTSD subgroup had moderate heterogeneity (I2=30.6%) which allows for greater confidence in the 6% reduction of symptom scales seen with journaling for these patients.
The meta-regression yielded some clues as to sources of heterogeneity including study population, age and gender composition, length of time of journaling intervention (<30 days or >30 days), and whether journals were collected/analysed. The identification of these variables as sources of heterogeneity in this meta-analysis demonstrates the need for a mixed gender/age population that represents family physician clinical populations in future studies, as well as encouraging journaling intervention >30 days in duration and recommending against collecting journals.
This last factor of journal collection and/or analysis is critical to acknowledge given this was revealed to be a statistically significant moderator. Eleven studies (18 outcomes) collected and/or analysed participant journals. This would likely have adversely affected results. Much of the efficacy of journaling comes from the ability of one to write openly and honestly, without the fear of judgement, safe in the knowledge that the journal will not be read by others.12 While some involved in those studies were only collecting journals to ensure compliance, some were in fact analysed for content. Both practices in our opinion are counterproductive to optimal journaling practices.
We also note that a detailed preparatory/educational training session is vital in allowing the patient to understand why journaling works and how to effectively journal.3 Although all 20 studies in this paper provided some limited written and/or verbal guidance, no study implemented a training session or provided participants with an opportunity to practice with a trained instructor or ask questions. It could be argued that any efficacy that may be attributable to journaling may well be diminished due to the lack of a training/preparatory session. Journaling is an intervention that requires education, coaching and practice, in order to be undertaken in a manner that ensures optimal effects.2
We intended to calculate an OR or ‘number needed to treat’ for journaling, however, the data did not present in a manner that allowed us to do so. Due to differences in study designs, comparisons of behaviour change/non-pharmacological interventions (eg, journaling) to conventional pharmacological treatments such as antidepressant efficacy are challenging. However, we were able to find a meta-analysis and systematic review done by Fournier et al13 on antidepressant efficacy using Cohen’s d effect size. Fournier’s findings depict that most antidepressant therapy studies show a moderate effect size and antidepressants are most effective in a population suffering from very severe depression. Interestingly, our findings for journaling show small to moderate effect sizes, suggesting that journaling interventions show promise to become a highly efficacious evidence-based therapy once more well-designed trials are completed.
This meta-analysis provides further affirmation that journaling as an intervention has merit and can be an efficacious adjunct when prescribed and implemented properly. The findings of this study can be applied in primary care practice by using journaling as a low risk, low-resource intensive adjunct to standard therapy for patients with mental health concerns. This study can also guide future research by highlighting the criteria required for robust studies. Journaling is a promising intervention for the treatment of mental health disorders but requires more robust high-quality longitudinal studies to appropriately assess its efficacy. In addition to this, participants require adequate preparation and the opportunity to practice if we are to fully investigate how journaling could benefit patients.2 We also recommend not sharing the participants’ personal journal with the study team.
Even though the included studies were found to have a low risk of bias, one of the limitations of this meta-analysis include a lack of high-quality studies with low heterogeneity, thus curbing the ability to draw clinically relevant conclusions. In addition, we only included randomized controlled trials (RCTs) in this study and thus, may have missed important studies on journaling which used different study designs. Finally, because meta-regression was performed within subgroups (anxiety, depression and post-traumatic stress disorder (PTSD), the number of studies within subgroups became less than 10 across several groups, and meta-regression is generally not recommended with fewer than ten studies in a meta-analysis.
Conclusion
Journaling is an adjunct low-cost, low-side effect therapy that can help family physicians in the management of common mental health symptoms that is supported by randomised controlled trials as summarised in this systematic review with meta-analysis. While study quality is overall low, the cost–benefit ratio is in favour of family physicians advocating for use of this modality as an adjunct to other therapies for common mental health conditions. Further studies are required to better evaluate the parameters that can further optimise journaling efficacy as an intervention on mental health outcomes.
Acknowledgments
Mohammad Ziaul Islam Chowdhury (PhD Candidate) - tasks performed: statistical analysis; Gursharan Kaur Dalam - tasks performed: data extraction; Melissa Marshall, PhD (final manuscript revision); Chantal Hansen, MGIS (final manuscript revision).
Footnotes
Contributors: MS: planning, data collection, data analysis, synthesis, editing. PS: planning, data collection. BSD: planning, data analysis, synthesis. HG: concept, editing, final revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Wang J, Langille DB, Patten SB. Mental health services received by depressed persons who visited general practitioners and family doctors. Psychiatr Serv 2003;54:878–83. 10.1176/appi.ps.54.6.878 [DOI] [PubMed] [Google Scholar]
- 2.Hayman B, Wilkes L, Jackson D. Journaling: identification of challenges and reflection on strategies. Nurse Res 2012;19:27–31. 10.7748/nr2012.04.19.3.27.c9056 [DOI] [PubMed] [Google Scholar]
- 3.Hubbs DL, Brand CF. The paper mirror: understanding reflective Journaling. J Exp Educ 2005;28:60–71. 10.1177/105382590502800107 [DOI] [Google Scholar]
- 4.Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet 2018;391:1357–66. 10.1016/S0140-6736(17)32802-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong YJ, Owen J, Gabana NT, et al. Does gratitude writing improve the mental health of psychotherapy clients? Evidence from a randomized controlled trial. Psychother Res 2018;28:192–202. 10.1080/10503307.2016.1169332 [DOI] [PubMed] [Google Scholar]
- 6.Pennebaker JW, Chung CK. Expressive writing and its links to mental and physical health. Oxford Handb Heal Psychol 2011. [Google Scholar]
- 7.Waters L. A review of school-based positive psychology interventions. Aust Educ Dev Psychol 2011. [Google Scholar]
- 8.Larner AJ. Effect size (Cohen's D) of cognitive screening instruments examined in pragmatic diagnostic accuracy studies. Dement Geriatr Cogn Dis Extra 2014;4:236–41. 10.1159/000363735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 10.Ebell MH, Siwek J, Weiss BD. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract 2004;69:548–56. [DOI] [PubMed] [Google Scholar]
- 11.Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med 2002;24:244–50. 10.1207/S15324796ABM2403_10 [DOI] [PubMed] [Google Scholar]
- 12.Phipps JJ. E-journaling: achieving interactive education online. Educ Q 2005. [Google Scholar]
- 13.Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 2010;303:47–53. 10.1001/jama.2009.1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
fmch-2021-001154supp001.pdf (102.5KB, pdf)