ABSTRACT
Maintenance of a healthy pregnancy is reliant on a successful balance between the fetal and maternal immune systems. Although the maternal mechanisms responsible have been well studied, those used by the fetal immune system remain poorly understood. Using suspension mass cytometry and various imaging modalities, we report a complex immune system within the mid-gestation (17-23 weeks) human placental villi (PV). Consistent with recent reports in other fetal organs, T cells with memory phenotypes, although rare in abundance, were detected within the PV tissue and vasculature. Moreover, we determined that T cells isolated from PV samples may be more proliferative after T cell receptor stimulation than adult T cells at baseline. Collectively, we identified multiple subtypes of fetal immune cells within the PV and specifically highlight the enhanced proliferative capacity of fetal PV T cells.
KEY WORDS: Placenta, Immune cells, Pregnancy, T cells
Summary: Mass cytometry is used to identify a complex and diverse immune profile in the healthy mid-gestation human placenta at single-cell resolution.
INTRODUCTION
Successful pregnancy is dependent on balanced immune homeostasis, yet many of the factors required to maintain this homeostasis remain elusive. It is understood that the maternal immune system must balance pathogen defense while preventing rejection of the semi-allogenic fetus (Erlebacher, 2013; PrabhuDas et al., 2015). The progression of pregnancy is mirrored by distinct physiological states throughout the body requiring the maternal immunity to be dynamic and adaptive, a point illustrated by Agheepour and colleagues who tracked maternal immunological responses throughout pregnancy via mass cytometry (CyTOF) (Aghaeepour et al., 2017). Many studies have identified numerous mechanisms by which maternal immunity accommodates the fetus. These include: suppressive uterine natural killer (NK) cells (reviewed by Gaynor and Colucci, 2017), T regulatory (Treg) populations (Salvany-Celades et al., 2019), suppressive B cells (Huang et al., 2017), restricted access to plasmacytoid dendritic cells (pDCs) (Li et al., 2018) and a predominance of type 2 helper T cells (Miyazaki et al., 2003). The importance of the maternal immune system in pregnancy cannot be understated; however, recent findings suggest that the fetal immune system must also be considered.
Historically, the fetal and neonatal immune systems were thought to be immature. This hypothesis was supported by poor vaccine responses in neonates (Saso and Kampmann, 2017), high susceptibility to infection (Simonsen et al., 2014) and the predominance of naïve lymphocytes in human cord blood (Paloczi, 1999). Recent insights suggest that the fetal and neonatal immune systems are developed, although they potentially have altered functions. Work supporting this includes: in utero maturation following fetal Treg education (Mold et al., 2008), detection of novel immunosuppressive cell types present in neonates (Elahi et al., 2013; Halkias et al., 2019; Miller et al., 2018a), and the presence of in utero memory lymphocytes in many fetal tissues (Li et al., 2019; Odorizzi et al., 2018; Schreurs et al., 2019; Stras et al., 2019; Zhang et al., 2014). However, the presence of phenotypically mature fetal leukocytes in the mid-gestation human placenta has yet to be explored.
Recent single-cell RNA-sequencing studies of the first trimester fetal-maternal interface revealed previously undocumented PV cell types (Suryawanshi et al., 2018; Vento-Tormo et al., 2018). Similarly, detection of novel cell populations was observed in third trimester placental surveys (Pavličev et al., 2017; Pique-Regi et al., 2019). The work by Pique-Regi specifically identified PV-specific immune cell signatures, notably the presence of both resting and activated T cells of fetal origin in term PV (Pique-Regi et al., 2019). These data align with work detecting T cells with activated phenotypes in third trimester preterm rhesus macaque PV (Toothaker et al., 2020). Of note, these single-cell surveys lacked histological data and as such there is a gap in knowledge of the localization (fetal blood or PV stroma) of the immune cell types.
We hypothesized that the active PV immune system detected in the third trimester (Pique-Regi et al., 2019; Toothaker et al., 2020) is present at mid-gestation. Using RNA sequencing (RNAseq), CyTOF, imaging mass cytometry (IMC) and fluorescence microscopy, we investigated the PV immune profile from healthy mid-gestation (17-23 weeks) placental tissues. With this unique cohort, we detected multiple PV-specific immune signatures representative of both blood and PV stromal immune cells. We also identified that PD-L1 (CD274) expression on antigen-presenting cells is reduced in preterm placentas, highlighting the importance of regulation of PV immune cells in healthy pregnancy. Furthermore, using flow cytometry we uncovered that, although rare in abundance, T cells isolated from PV samples representing T cells in both the fetal blood and PV stroma are hyperproliferative compared with adult T cells from both matched maternal decidua and unrelated adult intestines.
RESULTS
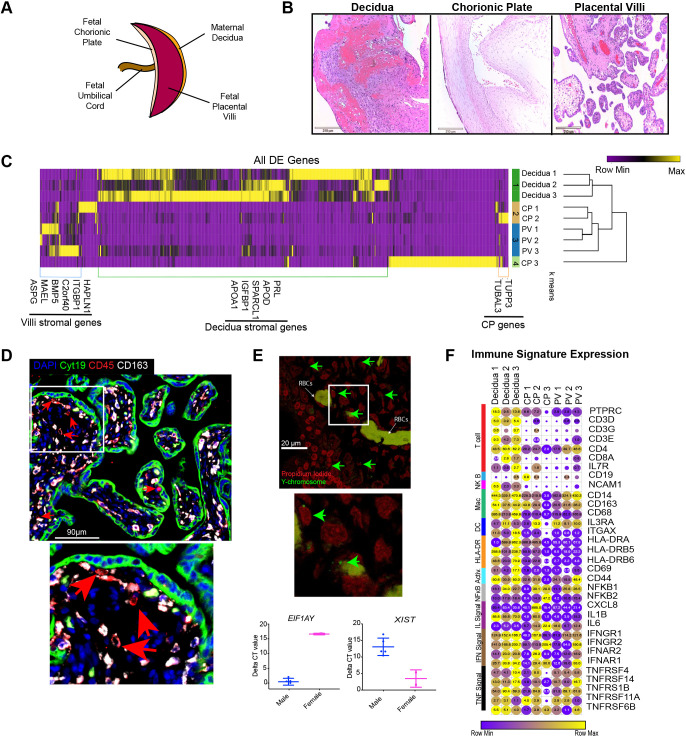
Human mid-gestation PV have tissue-specific immune signatures
We collected placental specimens from 19 second trimester products of conception, gestational age (GA) 17-23 weeks (Table S1). Maternal decidua and fetal chorionic/amniotic membranes covering the chorionic plate (CP) were separated from the PV (Fig. 1A) with forceps under a dissecting microscope. Separation of layers was initially confirmed by histology (Fig. 1B). Tissue was then either cryopreserved for CyTOF analysis, as previously described (Konnikova et al., 2018; Stras et al., 2019) and validated by comparison with fresh tissue (Fig. S1A), fixed with formalin prior to embedding in paraffin for IMC and immunofluorescence (IF) analysis or snap-frozen for bulk RNAseq. To verify separation of placental layers, we used bulk RNAseq from three matched cases (Table S1). Differential expression analysis (Table S2) and hierarchical clustering confirmed segregation of layers based on transcription profiles with the exception of one outlier sample (CP3), which was enriched for inflammatory signatures, likely upregulated during the dilation and evacuation procedure or secondary to undocumented in utero inflammation (Fig. 1C). Segregation of samples was further confirmed with k-means clustering, which grouped samples correctly by tissue with the exception of CP3 outlier (Fig. 1C). Moreover, we confirmed the enrichment of decidua- and PV-specific stromal genes previously identified (Pique-Regi et al., 2019; Suryawanshi et al., 2018; Vento-Tormo et al., 2018). To determine whether immune cells in the mid-gestation PV were solely reflective of the classical Hofbauer cell population, we used immunofluorescence to co-stain for CD45 (PTPRC), a marker of all hematopoietic cells, and CD163, a classical PV-resident Hofbauer cell marker (Reyes and Golos, 2018). Consistent with previous reports identifying non-Hofbauer immune subsets in the second (Bonney et al., 2000), first and third (Pique-Regi et al., 2019) trimester PV, we detected CD45posCD163lo cells within the mid-gestation PV (Fig. 1D) ranging in abundance from 30% to 70% of CD45pos nuclei per high-power field (Fig. S1B). As the PV are bathed in maternal blood (intervillous), we also confirmed that immune cells present in PV samples were reflective of cells contained within the trophoblast layers of the PV itself (intravillous) rather than resulting from contamination with maternal cells (Fig. 1D, Fig. S1B). Additionally, we detected the Y chromosome by in situ hybridization in many intravillous cells and observed enriched expression of Y chromosome-derived EIF1AY mRNA and low expression of the X chromosome inactivation transcript XIST in male PV samples, indicating that the majority of PV immune cells were fetal (Fig. 1E, Fig. S1C). We next assessed immune gene expression by RNAseq. Although most transcripts in the PV were expressed at lower levels than their decidual counterparts (indicated by color), transcripts for a large number of the immune subtypes analyzed were detected in PV samples (indicated by circle size) (Fig. 1F, Table S3).
Fig. 1.
Tissue-specific signatures in the mid-gestation placenta. (A) Diagram of placental tissues. (B) Hematoxylin & Eosin staining of placental tissues (n=19). (C) All differentially expressed genes between placental tissues with P<0.05, false-discovery rate<20% and fold change>absolute value 2 (n=3). (D) CD45pos CD163lo/neg cells within the intravillous space identified with immunofluorescence (n=19). (E) Top: Fluorescence in situ hybridization of Y chromosome in PV. Bottom: Delta CT values of Y (left) and X (right) chromosome genes in male and female PV (n=1 male, 1 female). (F) Expression values of selected immune genes. Circle size indicates expression value. Circle color indicates relative expression across row. n=3 per tissue type. DE, differentially expressed. Graphs show mean±s.e.m.
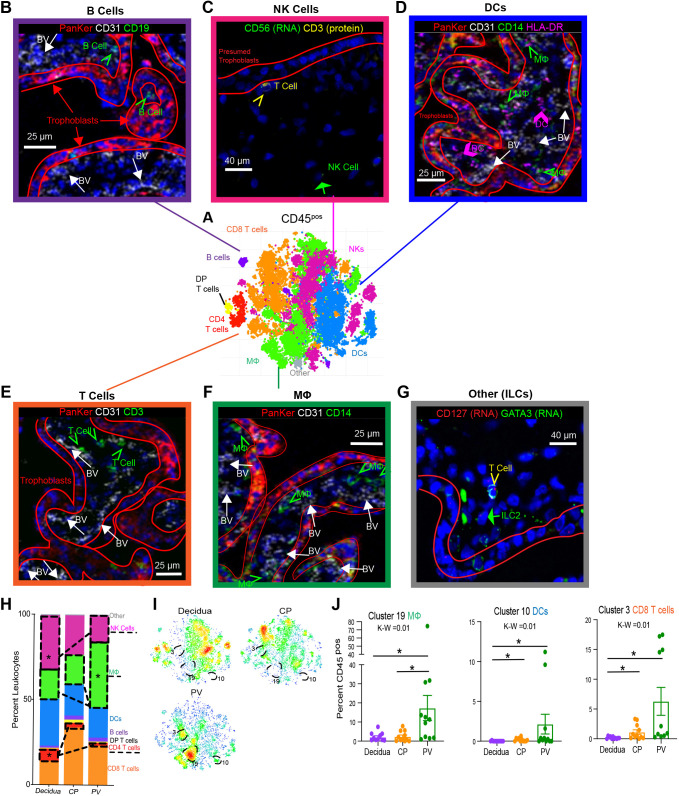
To survey the CD45pos populations in the PV, we used 38 metal-conjugated antibodies (Table S4) and performed CyTOF analysis on 12 placenta-matched decidua, CP and PV samples (Table S1). Briefly, cryopreserved tissues were batch-thawed and digested to make single-cell suspensions, stained with antibodies and analyzed using CyTOF (Konnikova et al., 2018) (Fig. S1A). FCS files from CyTOF analysis were pre-gated for DNApos, single, live, non-bead, CD45pos cells (Fig. S2A). After omitting samples with insufficient cell numbers (>750 CD45pos cells) we were left with 11 samples for each tissue (Table S5). CD45pos cells were clustered using PhenoGraph (Fig. 2A) and identified based on surface markers from Clustergrammer-generated associated heatmaps (Table S6, Fig. S2B).
Fig. 2.
Global immune landscape of second trimester placenta. (A) Merged t-distributed stochastic neighbor embedding (t-SNE) of CD45pos cells from maternal decidua (n=11), CP (n=11) and PV (n=11) from PhenoGraph clustering of CyTOF data. (B) IMC identifying B cells (green arrows) located within the trophoblast boundary (red outlines) and outside the fetal blood vessels (BV) (white arrows). PanKer, pan-keratin (stains for trophoblasts). (C) Dual in situ hybridization and IF identifying NK cells (green arrow) distinct from T cells (yellow arrowhead) in PV. (D) IMC identifying DCs (pink arrows) and HLA-DRpos macrophages (green arrows). (E) IMC identifying T cells (green arrows). (F) IMC identifying macrophages (green arrows). (G) Dual in situ hybridization and IF identifying ILC2s (green arrow) distinct from T cells (yellow arrowhead) in PV. (H) Stacked bar graph summarizing all clusters belonging to the same immune subsets from CyTOF data. (I) Density plot of the populations shown in A segregated by tissue of origin. Clusters significantly enriched in the PV are outlined. (J) Quantification of PV-enriched cluster abundance. K-W, Kruskal–Wallis test. *P<0.05 following post-hoc analysis. Graphs show mean±s.e.m. Mφ, macrophage.
To confirm that the PV immune subsets identified were not solely reflective of blood leukocytes in the fetal circulation, we used IF and IMC with a panel that included 23 markers (Table S8) on six total regions of two individual PV samples (Table S1). Using IMC, we validated that B cells, dendritic cells (DCs), T cells and macrophages were outside the fetal vasculature [using CD31 (PECAM1) as an endothelial marker] in the PV stroma (Fig. 2B,D-F). To identify NK cells and innate lymphoid cells (ILCs), we used dual in situ hybridization and IF (Fig. 2C,G). Although it is likely that some PV immune cells detected with CyTOF represent blood leukocytes, we conclude that a proportion of the PV immune cells are stromal.
To characterize these cells further, we used CyTOF analysis consisting of 31 unique clusters of immune cells within the second-trimester placenta, belonging to macrophage, DC, NK, CD4T cell, CD8T cell, double-positive (DP) T cell, B cell and other immune cell type subsets (Fig. 2H, Fig. S2B). Overall, immune cell subsets were in the minority with respect to the abundance of all live cells found in the placenta (Fig. S2C). However, each layer of the placenta still housed a unique and complex immune profile (Fig. S2D). When all clusters belonging to the same immune subset were combined, the decidua had a greater abundance of NK cells compared with PV (Fig. 2H), consistent with previous studies (King et al., 1991; Koopman et al., 2003). Additionally, there was a higher proportion of CD4T cells in the decidua than in either of the fetal layers (Fig. 2H). In contrast, the PV had a larger proportion of macrophages (potentially Hofbauer cells) (Fig. 2H).
When each cluster abundance was directly compared, 11/31 CD45pos clusters were differently distributed between the three layers of the placenta (Fig. 2I,J, Fig. S2E). The PV was uniquely enriched for cluster 19 CCR7neg macrophages (Fig. 1I,J). This robust cluster similarly suggests the presence of Hofbauer cells (as prior reports show most Hofbauer cells are CCR7neg; Joerink et al., 2011) in the PV and confirms the tissue specificity of Hofbauer cells in our data set as this cluster was largely undetectable in decidua and CP samples (Fig. 2J). Interestingly, we also found cluster 10, CCR7neg DCs, and cluster 3, CD69neg CD8 T cells, to be enriched in the PV over decidua (Fig. 2I,J). CCR7 is highly expressed by DCs homing to secondary lymphoid structures from peripheral tissues after antigen encounter (Ohl et al., 2004). CD69 is found to be transiently upregulated in activated T cells (Cibrián and Sánchez-Madrid, 2017) and constitutively upregulated in tissue-resident memory T cells (Kumar et al., 2017). As PV-enriched clusters 9 and 3 lacked these respective markers, we hypothesize that PV are poised to execute mature immune function, such as antigen presentation, but may not be actively performing such functions in utero. To explore this idea further, we next analyzed each immune cell subset more thoroughly.
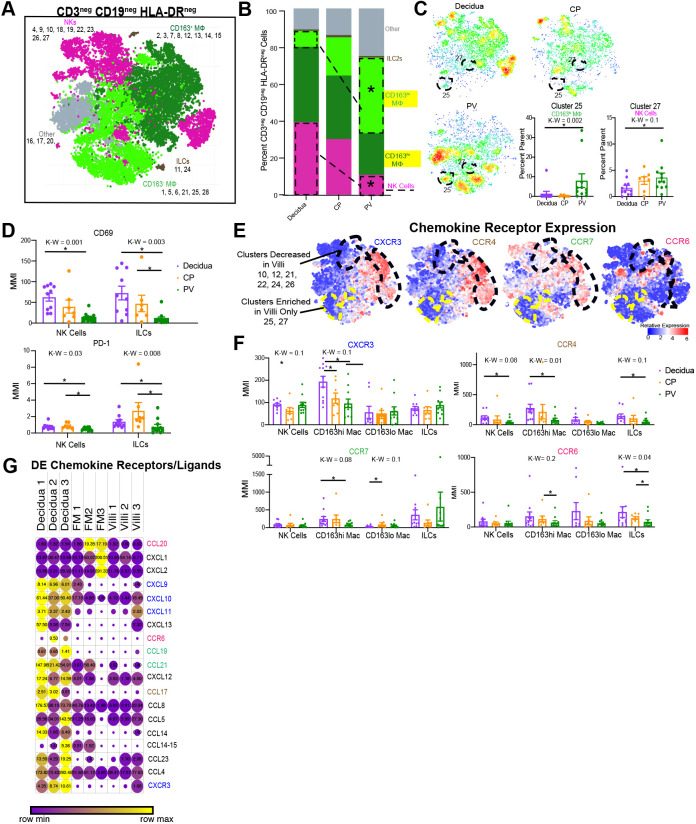
PV innate cells have quiescent phenotypes
To evaluate PV non-antigen-presenting innate cells, which represent the first cells to sense foreign antigens, we clustered on CD3negCD19negHLA-DRneg cells (Fig. S3A). We identified macrophages, ILCs, NK cells and multiple other immune cell populations, the phenotypes of which we were unable to identify with our panel (Table S4), (Fig. 3A, Fig. S3B). When comparing subtypes of immune cells, we confirmed our findings from the CD45 expression level clustering (Fig. 2A), with the decidua having a larger proportion of NK cells and the PV having a larger proportion of macrophages (Fig. 2H). The increased granularity of focusing on HLA-DRneg innate cells revealed that the PV contains CD163hi macrophages, likely Hofbauer cells, and a significant proportion of CD163lo macrophages, presumably other non-classical Hofbauer cell macrophages; Hofbauer cells that had downregulated CD163 expression; or fetal blood monocytes (Fig. 3B). HLA-DRneg macrophages in the decidua, by contrast, were largely CD163hi, consistent with previous data on the phenotype of decidual macrophages (Jiang and Wang, 2020) and with the enriched CD163 gene signatures seen in the decidua over CP from RNAseq data (Fig. 1F). The macrophage profile in the CP was more equally split between the two CD163lo phenotypes (Fig. 3B). At the individual cluster level, multiple clusters were enriched in either the decidua and/or CP (Fig. S3C). PV were enriched in cluster 25, CD163lo macrophages, and cluster 27, NK cells (Fig. 3C). Whereas cluster 27 NK cells were abundant in all three placental layers and only slightly elevated in the PV, cluster 25 macrophages were specific to the PV and were only minimally present in decidua and CP (Fig. 3C).
Fig. 3.
Innate HLA-DRneg cells in PV. (A) Combined CyTOF t-SNE for CD45pos CD3neg CD19neg HLA-DRneg cells (n=12). (B) Stacked bar graph showing the abundance of major immune subtypes. (C) Density plots separated by tissue of the cell populations shown in A. Statistically significantly abundant clusters in the PV are outlined. Graphs show cumulative data of PV-abundant clusters (outlined in the density plots). (D) MMI of CD69 (top) and PD-1 (bottom) for 2D-gated NK and ILC populations. (E) Expression heatmaps for chemokine receptors mapped to the cells identified in A. (F) MMIs of chemokine receptors on innate cell subsets from 2D gating. (G) Expression from RNAseq of differentially expressed chemokine ligand/receptor genes between tissues (n=3). Circle size indicates expression value, and circle color reflects relative expression across row. Differentially expressed genes were determined as: P<0.05, false-discovery rate<20% and fold change>absolute value 2. *P<0.05 upon post-hoc analysis after Kruskal–Wallis (K-W) test. DE, differentially expressed. Graphs show mean±s.e.m. Mac, macrophages.
To determine whether PV NK and ILCs express activation markers, we compared the mean metal intensities (MMIs) of CD69 and PD-1 (CD279) on these cells and found that PV NK cells and ILCs expressed significantly lower amounts of both CD69 and PD-1 (Fig. 3D). Next, to examine whether PV innate cells have migratory or tissue-retentive phenotypes we compared chemokine receptor (CCR) expression among subsets. Illustrated both visually (Fig. 3E) and graphically (Fig. 3F), we show that multiple populations of PV innate cells, including NK cells, ILCs and CD163hi macrophages, had reduced expression of four CCRs. Interestingly, the expression of these markers between the three compartments was similar for the CD163lo macrophages (Fig. 3F). To determine whether other chemokine receptor/ligand pairs were also reduced in the PV, we identified 19 chemokine receptors/ligands that were differentially expressed between PV, CP and decidua using bulk RNAseq (Fig. 3G, Table S7). These results validated the CyTOF findings of reduced expression of CCR6 and CXCR3 specifically, as well as at least one ligand for CCR7 and CCR4. Nine other chemokine ligand/receptors were implicated in this dataset (Fig. 3G).
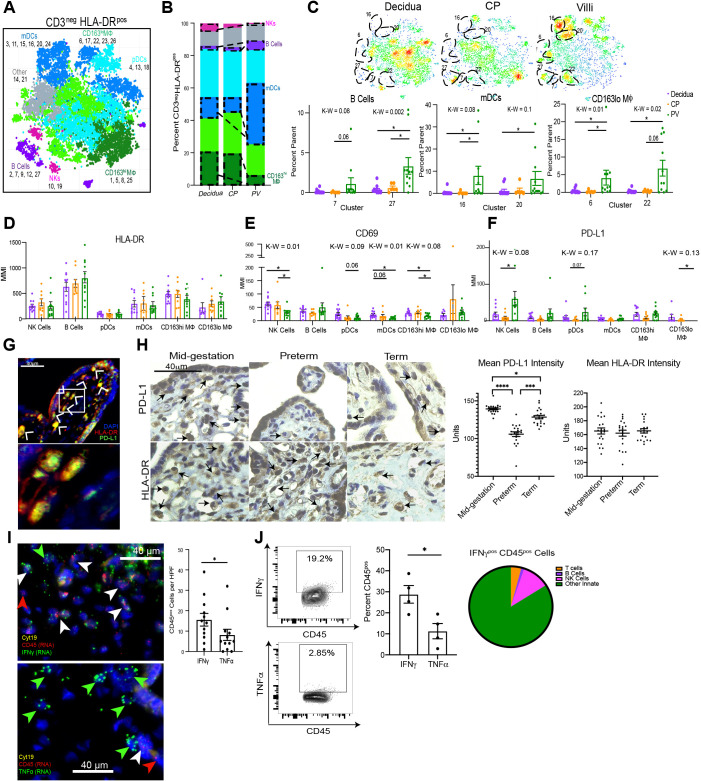
PV antigen-presenting cells are diverse and phenotypically immunosuppressive
Next, we examined antigen-presenting cell (APC) populations within each placental layer by clustering on CD45pos CD3neg HLA-DRpos cells (Fig. S4A). We identified seven subtypes of APCs, including myeloid DCs (mDCs), pDCs, CD163hi macrophages, CD163lo macrophages, B cells, NK cells and other cell types that we could not identify based on the available markers (Fig. 4A, Fig. S4B). In confirmation of our previous findings (Figs S2 and S3), NK cells were again more prevalent in the decidua compared with the PV (Fig. 4B). HLA-DRpos NK cells that are capable of independently presenting antigens to CD4T cells have been described (Roncarolo et al., 1991). In contrast to HLA-DRneg innate cells (Fig. 3), numerous individual APC clusters were enriched in the PV (Fig. 4C). Of note, multiple populations were enriched in the decidua and CP as well (Fig. S4C). Specifically, B cell clusters 7 and 27, mDC clusters 16 and 20, and CD163lo CD4neg macrophage clusters 6 and 22 were significantly more abundant in the PV than in either decidua or CP (Fig. 4C). In agreement with this finding, CD4posCD163hi macrophages (cluster 26) were reduced in the PV compared with decidua and CP (Fig. S4C). CD4pos macrophages have been shown to be long-lived tissue-resident macrophages in the intestine and perhaps they serve a similar role in the decidua (Shaw et al., 2018). The large number of APC clusters (11 in total) that were differentially abundant between the PV and decidua/CP suggests that antigen presentation in the PV may be functioning through non-classical mechanisms at mid-gestation.
Fig. 4.
Antigen-presenting cells in the PV. (A) Cumulative CyTOF t-SNE for CD45pos CD3neg HLA-DRpos cells. (B) Stacked bar graph showing the abundance of major immune subtypes. (C) Top: Density plots separated by the tissue of origin from the data shown in A. Statistically significantly abundant clusters in the PV are outlined. Bottom: Cumulative data of PV abundant clusters (outlined in density plots). (D-F) MMI of HLA-DR (D), CD69 (E) and PD-L1 (F) for 2D-gated populations. *P<0.05 upon post-hoc analysis after Kruskal–Wallis (K-W) test. (G) PD-L1pos APC populations in PV. Boxed area is shown at higher magnification below. Arrowheads indicate positive staining of the transcript marked by the same color in the image key. (H) Representative images (left) and quantification of average stain intensity per stromal nuclei (right) for PD-L1 and HLA-DR IHC. n=2. (I) Representative images (left) and quantification of automated image analysis with CellProfiler (right) for dual RNA in situ hybridization and immunofluorescence in PV (n=12). (J) Flow plots and quantification for cytokine-positive PV immune cells by flow cytometry. n=4. Pie-chart shows major immune subset abundance of IFNγpos immune cells from flow cytometry. *P<0.05, ***P<0.001 and ****P<0.0001 (Mann–Whitney test). K-W, Kruskal–Wallis test P-value. CyTOF analysis starting with n=12 for each analysis; see Table S5 for omitted cases. Graphs show mean±s.e.m.
To investigate phenotypes unique to PV APCs, we examined the expression of both activation and immunosuppressive markers on each APC subset identified in Fig. 4B. In contrast to the hypothesis that PV APCs have altered ability to function as APCs compared with those in decidua and CP, we found no difference in HLA-DR expression among APC subsets (Fig. 4D). However, consistent with the hypothesis of PV APCs being more inhibited than their decidua and CP counterparts, we identified significantly reduced expression of the activation marker CD69 in the PV CD163hi macrophages, NK cells, pDCs and mDCs (Fig. 4E). Furthermore, when we examined the inhibitory ligand PD-L1, we documented its increased expression in multiple APC subsets, significantly so on CD163lo macrophages and HLA-DRpos NK cells (Fig. 4F). This observation of high PD-L1 expression in PV APCs was confirmed by IF staining; almost every observable PV HLA-DRpos cell co-expressed PD-L1 (Fig. 4G, Fig. S4D).
To explore the PD-L1 and HLA-DR signature further, we labeled both PD-L1 and HLA-DR in the PV stroma by immunohistochemistry (IHC) of healthy mid-gestation placentas (21-23 weeks' gestation), preterm placentas from complicated pregnancies (29-35 weeks' gestation) and healthy placentas delivered at full-term (39 weeks' gestation) (Fig. 4H). Consistent with our CyTOF findings, mid-gestation stromal cells had high nuclear expression of PD-L1 and PD-L1 staining patterns were congruent with stromal HLA-DR staining, indicating that the PD-L1pos cells analyzed were likely APCs (Fig. 4H). Of note, we discovered that stromal PD-L1 expression in preterm PV was significantly lower than that of mid-gestation and term PV. Furthermore, term PV also had significantly reduced PD-L1 expression on stromal cells compared with mid-gestation PV (Fig. 4H). In contrast, we observed increased PD-L1 expression on preterm trophoblasts compared with mid-gestation trophoblasts (Fig. S4E). To confirm that the reduction of stromal PD-L1 was not an artifact of reduced APC abundance in preterm and term placentas, we compared mean HLA-DR expression between all three groups and found no differences (Fig. 4H). These results suggest that PD-L1 expression on PV APCs may be important for maintaining a healthy pregnancy.
To investigate the regulation of constitutive PD-L1 expression we measured the expression of interferon (IFNγ), a well-documented regulator of PD-L1 (Garcia-Diaz et al., 2017). We found preferential transcription of IFNγ over TNFα at baseline by PV immune cells (Fig. 4I, Fig. S4F). Additionally, PV immune cells transcribed comparable levels of IFNγ, but transcribed less TNFα than decidual immune cells (Fig. S4G). The preferential production of IFNγ over TNFα was confirmed in PV immune cells by flow cytometry. We report that IFNγ was mostly derived from non-NK innate immune cells (Fig. 4J). As such, it is possible that PV immune cells produce IFNγ to drive expression of PD-L1 on APCs.
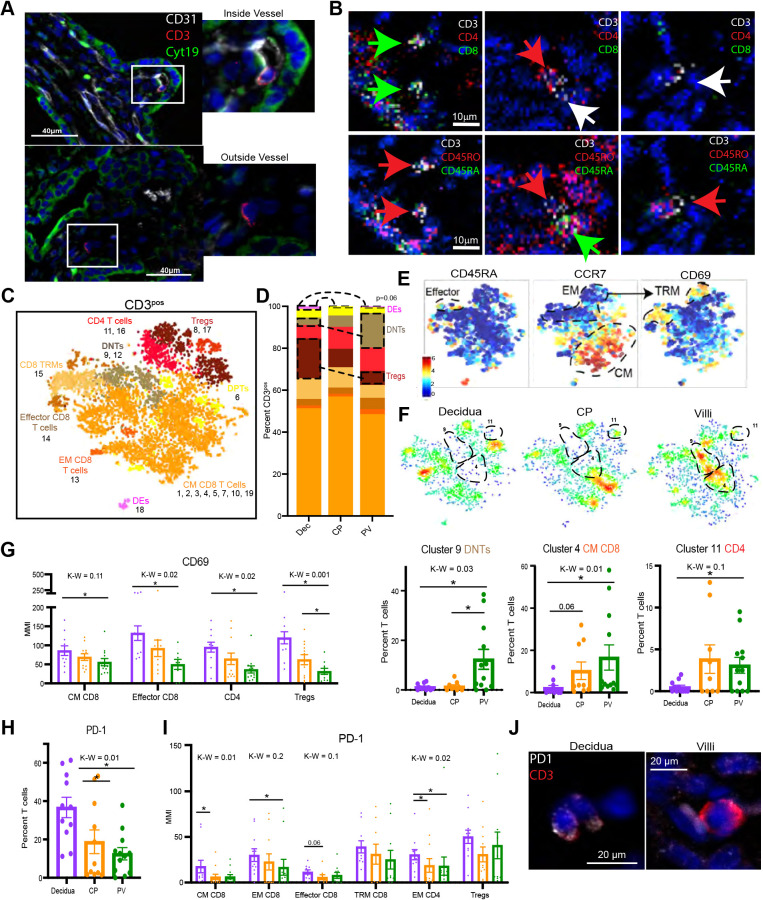
The second trimester placenta is dominated by memory CD8T cells
As we observed high PD-L1 expression on APCs, we next explored whether there were T cells present in the PV that could potentially be inhibited by immunosuppressive APCs. We identified both circulating (within blood vessel) and potentially tissue-resident T cells in the PV (Fig. 5A, Fig. S5A). Moreover, using IMC, we surprisingly identified non-circulating T cells of CD4, CD8 and double negative (DN) phenotypes that expressed CD45RO, a marker upregulated after antigen experience and absent on naïve T cells (Fig. 5B, Fig. S5B). Turning to our CyTOF data, when clustering specifically on T cells (Fig. S5C), we found that all three layers of the placenta had a T cell profile dominated by CD8T cells (Fig. 5C,D, Fig. S5D). Based on the initial detection of CD45RO by IMC, we found that the majority of T cells in the PV were of memory phenotypes, delineated by their lack of expression of CCR7 and CD45RA (Fig. 5E). Additionally, we found CD8T cells with tissue-resident memory (TRM) phenotype in all three layers (Fig. 5E). We detected CD69pos T cells both as a marker of TRMs on CCR7neg CD45RAneg T cells and also among other T cell subsets (Fig. 5E). The expression of CD69 on multiple T cell populations strongly suggests that some populations of PV T cells are stromal and not reflective of fetal blood T cells, because recent work has shown that blood CD8T cells do not express CD69 (Buggert et al., 2020). The detection of both CD69neg and CD69pos CD8T cells in the PV is consistent with the enrichment of one cluster of CD69neg CD8T cells from our initial CD45pos clustering (Fig. 2). CD8 and CD4 non-Treg cell subtypes were evenly distributed between all three layers (Fig. 5D). However, CD4 Tregs were enriched in the decidua compared with the PV (Fig. 5D). The abundance and importance of Tregs throughout pregnancy in the decidua is well documented (Mjösberg et al., 2010; Salvany-Celades et al., 2019), but the role of Tregs in the CP and the PV is unclear, although we have shown that PV Tregs function abnormally during intra-amniotic inflammation (Toothaker et al., 2020). Moreover, there was an enrichment of CD4neg CD8neg that were also CD56neg DN T cells in the PV (Fig. 5D, Fig. S5D). These DN T cells could potentially be γδ T cells, the presence of which has been described in the first trimester PV (Bonney et al., 2000).
Fig. 5.
T cell subsets in placental tissues. (A) Representative images of T cells inside (top) and outside (bottom) fetal vasculature (CD31) in PV. (B) IMC images of T cell subtypes in PV. Green arrows indicate CD8pos (top) or CD45RApos (bottom), red arrows indicate CD4pos (top) or CD45ROpos (bottom) and white arrows indicate CD3pos (T cells). (C) Cumulative CyTOF t-SNE for PV, CP and decidua CD45pos CD3neg HLA-DRpos cells. (D) Stacked bar graph showing the abundance of major immune subtypes. (E) Relative expression of memory T cell markers in the PV cell populations shown in C. (F) Density plot separated by tissue of origin (C). Statistically significantly abundant clusters in the PV are outlined. Graphs show cumulative data of PV-abundant clusters (outlined in density plots). (G) MMI of CD69 from 2D gating of populations. (H) Abundance of PD-1pos T cells by 2D gating. (I) PD-1 MMI from 2D-gated subsets. CyTOF analysis starting at n=12 for each analysis; see Table S5 for omitted cases. (J) PD-1 expression on T cells in PV and decidua. *P<0.05 upon post-hoc analysis after Kruskal–Wallis (K-W) test. CM, central memory; EM, effector memory; TRM, tissue-resident memory. Graphs show mean±s.e.m.
The detection of PV T cells expressing memory markers in human mid-gestation PV is novel. To investigate T cell signatures unique to the PV, we next compared the abundance of individual T cell clusters. Although two clusters were enriched in the decidua (Fig. S5E), cluster 9 CD4neg CD8neg T cells, cluster 4 CM CD8T cells and cluster 11 CD4T cells were enriched in the PV (Fig. 5F). Cluster 11T cells were CCR4posCXCR3negCCR6neg (Fig. 5F, Fig. S5D), surface marker expression pattern suggestive of a TH2 phenotype; however, further analysis for detection of TH2-specific transcription factors (e.g. GATA3) is needed for confirmation.
Resting phenotypes define PV T cell subsets
We next explored whether a resting phenotype was consistent among the PV T cell subsets identified in Fig. 5D. Among non-TRM T cells, PV T cell subsets exhibited reduced expression of CD69 (Fig. 5G, Fig. S5F). Moreover, the PV housed fewer PD-1pos cells (Fig. 5H) and reduced PD-1 per T cell compared with decidual counterparts (Fig. 5I,J). Although PD-1 is a marker of T cell exhaustion, it is also upregulated upon activation of the TCR (summarized by Xu-Monette et al., 2017). We propose that this is the more likely role of the observed downregulation of PD-1 in PV T cells as it is consistent with the downregulation of CD69.
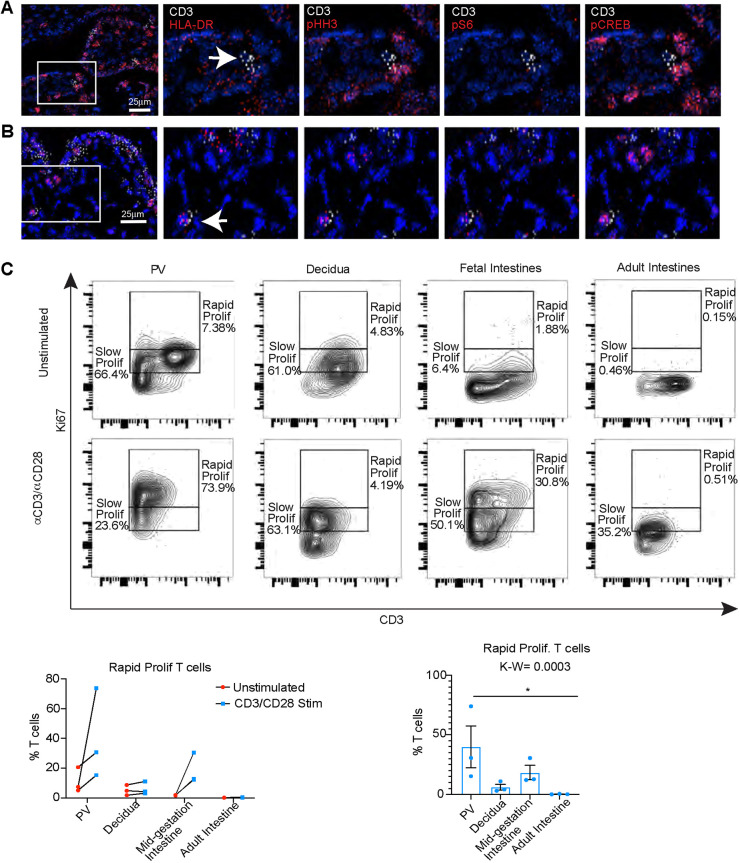
PV T cell activation potential
To determine whether PV T cells have a reduced activation profile, we scanned for activated T cells by staining for HLA-DR, phosphorylated histone H3, phosphorylated S6 and phosphorylated CREB in T cells using IMC. We identified both resting (Fig. 6A) and activated (Fig. 6B) T cells in the PV. We next questioned whether mid-gestation PV T cells could be activated in a TCR-dependent manner. To test the functionality of the TCR pathway in PV T cells, we stimulated single-cell suspensions from PV with soluble anti-CD3 and anti-CD28 antibodies for 4 h. We observed an increase in the abundance of rapidly proliferating T cells by high Ki67 (MKI67) expression (Miller et al., 2018b) in fetal T cells (placenta and intestine) compared with adult T cells (decidua and intestine) (Fig. 6C, Fig. S6B), validating our previous findings that PV T cells are fetal in origin and unique from the decidua. Of note, the placenta had the highest proportion of rapidly proliferating cells across all organs and ages following stimulation (Fig. 6C).
Fig. 6.
T cell activation in PV. (A) IMC images of inactive T cells in PV. (B) IMC images of activated T cells in PV. In A,B, boxed areas are shown at higher magnification in images to the right. Arrows indicate CD3pos (T cells). (C) Flow plots (top) and quantification (bottom) for proliferating (Ki67hi) T cells after stimulation across the tissues indicated. n=3 (all experiments). Graphs show mean±s.e.m.
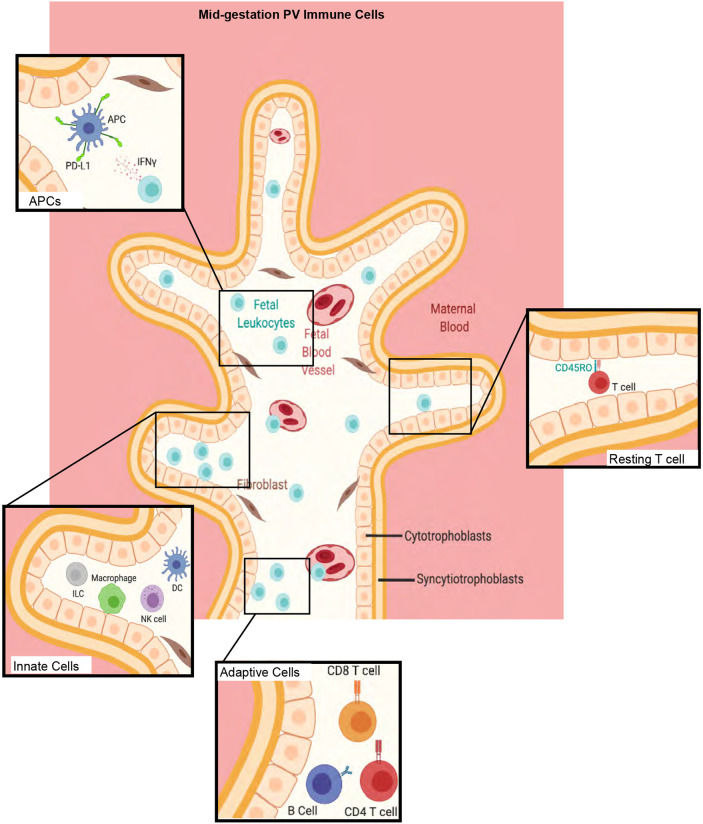
In summary (Fig. 7), we demonstrate that the intravillous compartment of the healthy second trimester PV contains a diverse immune landscape comprising innate cells, such as macrophages, NK cells and ILCs, as well as APCs, including B cells, and memory T cells (Fig. 2). Moreover, we show that the immune cells in the PV maintain decreased levels of activation markers at baseline as a potential mechanism for preventing in utero inflammation. The mechanisms described include reducing chemotaxis by reduced expression of chemokine receptors on innate cells and low transcription of chemokine ligands in the PV overall (Fig. 3). Moreover, PV APCs constitutively express PD-L1, possibly regulated by the high expression of IFNγ by PV immune cells (Fig. 4). Finally, phenotypically mature PV T cells (Fig. 5) proliferate upon activation through the TCR pathway (Fig. 6).
Fig. 7.
Summary of major findings in study. Schematic of immune cell populations identified in the PV in this study. Image created with BioRender.com.
DISCUSSION
Preserving tolerance at the fetal-maternal interface is crucial for maintaining a healthy pregnancy. How leukocytes within the PV contribute to immune homeostasis has yet to be fully elucidated. Single-cell studies of first trimester (Suryawanshi et al., 2018; Vento-Tormo et al., 2018) and full term (Pavličev et al., 2017; Pique-Regi et al., 2019) placenta highlighted the diversity of immune cells within the PV. We hypothesized that the activated leukocytes detected in humans (Pique-Regi et al., 2019) and non-human primates (Toothaker et al., 2020) may be present in the PV earlier in gestation. We analyzed placental tissue and confirmed that there are diverse immune cells of fetal origin in second trimester PV samples within the intravillous space. Although it is possible that our analysis of PV immune cells included a proportion of maternal cells, ethical limitations precluded maternal peripheral blood collection. Future studies are needed to determine the exact origin of individual immune cell populations as either fetal blood immune cells within the PV vasculature and PV-resident cells in the stroma.
Previous studies suggest that PV fetal immune cells are limited to Hofbauer cells (Thomas et al., 2021). The increased granularity provided by single-cell methods allowed for the detection of T cells, B cells and NK cells in healthy term placentas (Pique-Regi et al., 2019). Moreover, a recent study identified infiltrating cells in the PV to be largely of fetal origin in infectious villitis (Enninga et al., 2020) and Erbach et al. isolated T cells from single-cell suspension at 18-24 weeks' gestation (Erbach et al., 1993). It is important to note that studies using cell suspensions make the delineation of immune cells from the PV vasculature indistinguishable from those in the stroma. By combining CyTOF and multiple imaging modalities, we identified both innate and adaptive immune cells, present outside the fetal vasculature in the intravillous space.
Thomas et al. reported that Hofbauer cells in the first trimester are HLA-DRneg (Thomas et al., 2021). Consistent with this, we found an increased abundance of macrophages in the PV compared with the decidua. Surprisingly, we report that many of these HLA-DRneg macrophages in the PV had reduced expression of CD163, a marker reported to be expressed in all Hofbauer cells (Reyes and Golos, 2018; Schliefsteiner et al., 2017). It is possible that CD163lo macrophages reflect downregulation of CD163 by Hofbauer cells during cell isolation (Tang et al., 2011). It is also possible that Hofbauer cells are more diverse than previously thought and therefore CD163 should be used in combination with other macrophage markers in future studies.
We identified phenotypes consistent with an anti-inflammatory state for multiple subsets of PV immune cells. We found that innate non-APCs expressed lower levels of multiple chemokine receptors than their decidual counterparts, consistent with histological evaluation of Hofbauer cells showing a lack of CCR7 staining (Joerink et al., 2011). This, coupled with reduced expression of multiple chemokine pathways, could suggest that innate cells in the PV are either static or are mobile in a non-targeted manner at baseline. We also identified HLA-DRpos cells, including mDCs, pDCs, B cells, macrophages and a population of HLA-DRpos NK cells. An antigen-presenting role for NK cells has been previously described (Roncarolo et al., 1991). The identification of fetal HLA-DRpos macrophages contrasts with the recent findings of Thomas et al. (2021). It should be noted that some of these HLA-DRpos macrophages in our study may reflect contaminant maternal macrophages repairing breaks in the trophoblast layer. However, the location of HLA-DRpos cells by both immunofluorescence and IMC show that some cells are located at a distance from the trophoblast layer and suggest that HLA-DRpos macrophages appear in the stroma after the time period studied by Thomas et al. It would be interesting to determine the fetal versus maternal origin of these HLA-DRpos macrophages and evaluate whether the Hofbauer cell population from 18-23 weeks is transcriptionally distinct from those in prior studies (Vento-Tormo et al., 2018).
Irrespective of PV APC ontogeny, we determined that PV APCs express more PD-L1 per cell than their decidual counterparts. The function of PD-L1 as a co-inhibitory molecule has been extensively studied (Sun et al., 2018). Moreover, PD-L1 expression can be mediated through IFNγ (Garcia-Diaz et al., 2017). We found that PV immune cells produce IFNγ preferentially to TNFα. In further validation, we found that preterm PV have significantly reduced expression of PD-L1 on PV stromal cells compared with mid-gestation PV, although it is not possible to determine whether PD-L1 reduction precedes or is the consequence of preterm delivery.
Detection of memory T cells within the PV justifies the need for PV APCs to limit T cell activation. Memory T cells have been detected in multiple fetal human organs (Angelo et al., 2019; Halkias et al., 2019; Li et al., 2019; Schreurs et al., 2019; Stras et al., 2019), and within the non-human primate PV (Toothaker et al., 2020). Additionally, activated and resting T cells have been detected in PV samples post-delivery (Pique-Regi et al., 2019) and central memory T cell can be found in human cord blood (Frascoli et al., 2018). We found that PV T cells express low activation signatures, potentially suggesting that PV T cells have been previously educated but remain quiescent owing to either the lack of antigens or direct inhibition from APCs.
The presence of a fetal microbiome as a source of antigens remains highly contested (Aagaard et al., 2014; de Goffau et al., 2019; Kuperman et al., 2020; Leiby et al., 2018; Mishra et al., 2021; Rackaityte et al., 2020; Theis et al., 2020). Our group recently showed that bacterial metabolites are present in the fetal intestine at 14 weeks' gestation (Li et al., 2020). As such, it is possible that maternal bacteria-derived peptides similarly cross the placenta and educate fetal T cells. Fetal T cell activation by maternal antigens has also been implicated in preterm birth (Frascoli et al., 2018). Our data indicate that PV T cells can be stimulated through activation of the TCR signaling (anti-CD3/CD28 antibodies). Collectively, these findings have identified the unique hyper-proliferative potential of PV T cells compared with adult T cells and fetal intestinal T cells and suggest that antigens could stimulate a PV T cell response in utero.
Our study had several limitations, in particular the lack of genetic information to segregate fetal from maternal cells. It would be very interesting for a future cohort to determine definitively the origin of each PV immune cell subset identified in this work using dual in situ hybridization and immunodetection techniques. Legal limitations prevented the collection of maternal and fetal blood to use for comparison.
The ability of fetal immune cells to execute mature functions has recently been validated in multiple fetal organs (Angelo et al., 2019; Frascoli et al., 2018; Halkias et al., 2019; McGovern et al., 2017; Schreurs et al., 2019; Stras et al., 2019). The detection of immunosuppressive mechanisms to control this fetal immune response and prevent in utero inflammation is crucial. We have identified previously understudied immune cell populations within the mid-gestation PV. This work has implications for future studies to improve our understanding of the roles of fetal and maternal immune cells within the placenta and of immune tolerance in multiple diseases.
MATERIALS AND METHODS
Placental tissue collection
Human products of conception were obtained through the University of Pittsburgh Biospecimen core after IRB approval (IRB# PRO18010491). Tissue was collected only from subjects that signed an informed consent to allow use for research purposes. Preterm placentas resultant from a variety of obstetric complications were obtained from the University of Pittsburgh MOMI Biobank. Term placentas were collected both at the University of Pittsburgh through the MOMI biobank and through the Yale University YURS Biobank from C-section deliveries devoid of obstetric complications (Table S1). The n values for each experiment are provided as a checklist in Table S1. Placental villi were separated using forceps under a light dissection microscope (Fisherbrand, 420430PHF10) from the chorionic and amniotic membranes lining the CP and from the decidua basilis (referred to as decidua throughout the article) on the basal plate side of the placenta. Tissue was thoroughly washed with sterile PBS prior to cryopreservation and subsequent single-cell isolation as previously described (Konnikova et al., 2018).
RNAseq
Snap-frozen placental tissues were shipped on dry ice to MedGenome for mRNA extraction and library preparation. RNA extractions were completed with the QIAGEN All Prep Kit (80204). cDNA synthesis was prepped with the Takara Bio SMART-seq kit (634894) and Nextera XT (FC-131-1024, Illumina) was used to fragment and add sequencing adaptors. Quality control was completed by MedGenome using a Qubit Fluorometric Quantitation (Q33327) and TapeStation BioAnalyzer (G2991BA). Libraries were sequenced on the NovaSeq 6000 for Paired End 150 base pairs for 90 million reads per sample.
RNAseq analysis
FASTQ files were imported and subsequently analyzed with CLC Genomics Workbench 20.0 (https://digitalinsights.qiagen.com). Briefly, paired reads were first trimmed with a quality limit of 0.05, ambiguous limit of 2 with automated read through adapter trimming from the 3′-end with a maximum length of 150. Trimmed reads were then mapped to the homo_sapiens_sequence_hg38 reference sequence. Differential gene expression was computed in CLC Genomics with an ‘across groups’ ANOVA-like comparison. Significantly differentially expressed genes were delineated as those with P<0.05, false-discovery rate<20% and fold change>absolute value of 2. Heatmaps for gene expression were created with Morpheus (https://software.broadinstitute.org/morpheus).
RNA in situ hybridization
Formalin-fixed samples were sectioned and embedded in paraffin by the Pitt Biospecimen Core. Staining was completed per manufacturer's instructions for the RNAScope multiplex V2 detection kit (ACD Bio) coupled with immunofluorescent protein staining for cytokeratin 19 (ab52625, Abcam, 1:250). Echo Revolve microscope at 20× was used to image sections. All images were batch processed using Fiji (Schindelin et al., 2012), and all edits were made to every pixel in an image identically across all patients per experiment. Quantification of cell populations was carried out using a custom pipeline in CellProfiler (McQuin et al., 2018).
Fluorescence in situ hybridization
In situ hybridization for the Y chromosome was adapted from the protocol outlined by Enninga et al. (2020). Briefly, slides were deparaffinized with a series of xylene and ethanol washes. Target retrieval was performed at 95°C for 10 min, then slides were placed in 70% ethanol, 85% ethanol and 100% ethanol for 2 min each. DYZ3 probe (D5J10-034, Abbott Laboratories) was diluted 1:10 in LSI/WCP hybridization buffer (D6J67-011, Abbott Laboratories) and incubated for 5 min at 83°C prior to overnight hybridization at 37°C. Slides were soaked in SSC/0.1% NP-40 (ab142227, Abcam) to remove cover slips and placed in 2× SSC/0.1% NP-40 for 2 min at 74°C before mounting with antifade plus propidium iodide (p36935, Invitrogen). Slides were imaged on an LSM 710 (Leica Biosystems) confocal microscope at the Yale Center for Cellular and Molecular Imaging.
RNA extraction and qPCR
RNA was extracted from snap-frozen villi samples using the RNAEasy Minikit (217004, QIAGEN). RNA was converted to cDNA using iScript (1708891, Bio-Rad) reagents according to the manufacturer's protocol. Samples were run on a Taqman StepOnePlus Real-Time PCR System (Applied Biosciences) machine with probes for ACTB (Hs01060665_g1) as housekeeping gene and with either XIST (Hs01079824_m1) or EIF3AY (Hs01040047), all from QIAGEN. Values undeterminable were given cycle values of 40 for quantification purposes.
Immunofluorescence staining
Slides with 10 μm sections of FFPE tissue were deparaffinized with a series of xylene and ethanol washes. Antigen retrieval was performed in a Biocare Medical LLC decloaking chamber (NC0436641) for 1 h with citrate-based antigen retrieval buffer (H-3300, Vector Laboratories) and washed with PBS. Slides were then blocked for 30 min with 10% horse serum prior to overnight incubation at 4°C with primary antibodies in 2% horse serum. Primary antibodies used were cytokeratin 19 (ab192751, Abcam, 1:1000); CD45 (20103-1-AP, Proteintech, 1:200); CD163 (ab87099, Abcam, 1:200); CD3 (ab135372, Abcam, 1:100); CD31 (ab9498, Abcam, 1:1000). Slides were washed with PBS and incubated with Alexa Fluor secondary antibodies (donkey anti-rabbit IgG H&L 555, ab150074; donkey anti-mouse IgG H&L 647, ab150107; goat anti-guinea pig IgG H&L 488, ab150185; 1:750) in 2% horse serum for 45 min at room temperature. Slides were mounted with VECTASHIELD Antifade Mounting Medium plus DAPI (H-1300).
Imaging mass cytometry
Slides with 4 μm sections of FFPE tissue were deparaffinized with a series of xylene and ethanol washes. Antigen retrieval was performed at 95°C for 20 min using 1× Antigen Retrieval Buffer (CTS013 R&D Systems) and washed with water and dPBS. Slides were then blocked for 30 min with 3% bovine serum albumin in dPBS prior to overnight incubation at 4°C with a primary antibody cocktail (Table S8). Slides were rinsed and co-stained with 191/193 DNA-intercalator (Fluidigm), rinsed and air dried for at least 20 min prior to analysis. Slides were analyzed on a Hyperion Mass Cytometer with an ablation energy of 4 and frequency of 100 Hz for ∼30 min per section. Representative images were generated using Histocat++ software (Catena et al., 2018).
CyTOF staining
Samples were stained with antibody cocktail (Table S4) per previously published protocol (Stras et al., 2019) and incubated with 191Ir/193Ir DNA intercalator (Fluidigm) and shipped overnight to the Longwood Medical Area CyTOF Core. Data were normalized and exported as FCS files, downloaded and uploaded to the Premium Cytobank platform (https://premium.cytobank.org/cytobank/login). Any files with insufficient cell numbers were excluded from analysis (Table S5). Gating and analysis were completed with cytofkit (Chen et al., 2016) as published (Stras et al., 2019). Cluster abundance was extracted, and statistically analyzed using R.
Stimulation of PV T cells
Cells were isolated from cryopreserved PV samples as described throughout the article. Dead cells were removed prior to stimulation using a Millitenyl dead cell removal kit (130-090-101, Millitenyl Biotec). Cells were incubated with anti-CD3 (clone HIT3a, 300302, BioLegend) and anti-CD28 (clone CD28.2, 302902, BioLegend) soluble antibodies for 4 h rotating at 37°C+5% CO2 in the presence of GolgiPlug (51-2301K2, BD Biosciences) and GolgiStop (51-2092K2, BD Biosciences).
Flow cytometry
Post-stimulation cells were washed with PBS and incubated with Zombie Aqua live/dead stain (BioLegend 77143). Viability marker was washed out and cells were resuspended and spun down in FACS buffer then incubated with Human TruStain FcX (BioLegend) for 10 min prior to the addition or a surface antibody cocktail (Table S9). Cells were washed with FACS buffer and permeabilized with FoxP3 fix/perm (Invitrogen) overnight. Cells were washed with 1× FoxP3 Wash Buffer (Invitrogen) and incubated with intracellular antibodies then cells were washed, fixed for 10 min with 4% paraformaldehyde and resuspended in FACS buffer. All samples were run on a BD LSRII (BD Biosciences) at the Yale University Flow Cytometry core (all other stimulations). Output FCS files were analyzed with FlowJo.
Statistics
R version 3.6.1 was used with Kruskal–Wallis analysis and Dunn's multiple comparison test for post-hoc analysis among groups. A one-tailed t-test was used to compare groups of two. Comparisons of mean expression values were corrected using the Bonferroni method. P-values of 0.05 or less were considered significant.
Plot generation
Plots comparing multiple groups were generated using Prism GraphPad 8. In each plot, each data point represents one subject as per figure description.
Supplementary Material
Acknowledgements
This project used the UPMC Hillman Cancer Center and Tissue and Research Pathology/Pitt Biospecimen Core shared resource which is supported in part by award P30CA047904. This research was supported in part by the University of Pittsburgh Center for Research Computing through the resources provided. We thank Yale Flow Cytometry for their assistance with LSRII service. The Core is supported in part by an NCI Cancer Center Support Grant from the National Institutes of Health (P30 CA016359). We also thank Ansen Burr and the Hand Lab at The University of Pittsburgh for their help with RNA-sequencing analysis, and Meghan Mooring and Dean Yimlamai for help with confocal microscopy and BioRender images. We thank the Yale CyTOF core for help with IMC data acquisition.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Author contributions
Conceptualization: J.M.T., L.K.; Methodology: J.M.T., B.T.M., C.C.M., T.N.S., R.M.C., P.L., D.Y.; Validation: J.M.T., L.K.; Formal analysis: J.M.T., O.O., C.C.M., R.M.C., P.L.; Resources: D.Y., L.K.; Data curation: J.M.T., B.T.M., C.C.M., T.N.S., R.M.C., P.L.; Writing - original draft: J.M.T.; Writing - review & editing: T.N.S., D.Y., G.T., L.K.; Visualization: J.M.T., B.T.M., T.N.S.; Supervision: G.T., L.K.; Project administration: L.K.; Funding acquisition: L.K.
Funding
J.M.T. was supported by the National Institutes of Health (5T32AI089453-10) and the University of Pittsburgh. L.K. is supported by previous startup funds from the University of Pittsburgh and current start-up funds from Yale University, the Binational Science Foundation (2019075), and the National Institutes of Health (R21TR002639 and R21HD102565). No National Institutes of Health funds were used for the fetal work of these studies. Deposited in PMC for release after 12 months.
Data availability
Bulk mRNA extracted from three issues isolated from matched placentas have been deposited in the NCBI Gene Expression Omnibus database under accession number GSE178152.
Peer review history
The peer review history is available online at https://journals.biologists.com/dev/article-lookup/doi/10.1242/dev.200013.
References
- Aagaard, K., Ma, J., Antony, K. M., Ganu, R., Petrosino, J. and Versalovic, J. (2014). The placenta harbors a unique microbiome. Sci. Transl. Med. 6, 237ra65. 10.1126/scitranslmed.3008599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aghaeepour, N., Ganio, E. A., Mcilwain, D., Tsai, A. S., Tingle, M., Van Gassen, S., Gaudilliere, D. K., Baca, Q., McNeil, L., Okada, R.et al. (2017). An immune clock of human pregnancy. Sci. Immunol. 2, eaan2946. 10.1126/sciimmunol.aan2946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelo, L. S., Bimler, L. H., Nikzad, R., Aviles-Padilla, K. and Paust, S. (2019). CXCR6+ NK cells in human fetal liver and spleen possess unique phenotypic and functional capabilities. Front. Immunol. 10, 469. 10.3389/fimmu.2019.00469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonney, E. A., Pudney, J., Anderson, D. J. and Hill, J. A. (2000). Gamma-delta T cells in midgestation human placental villi. Gynecol. Obstet. Invest. 50, 153-157. 10.1159/000010315 [DOI] [PubMed] [Google Scholar]
- Buggert, M., Vella, L. A., Nguyen, S., Wu, V. H., Chen, Z., Sekine, T., Perez-Potti, A., Maldini, C. R., Manne, S., Darko, S.et al. (2020). The identity of human tissue-emigrant CD8+ T cells. Cell 183, 1946-1961.e15. 10.1016/j.cell.2020.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catena, R., Montuenga, L. M. and Bodenmiller, B. (2018). Ruthenium counterstaining for imaging mass cytometry. J. Pathol. 244, 479-484. 10.1002/path.5049 [DOI] [PubMed] [Google Scholar]
- Chen, H., Lau, M. C., Wong, M. T., Newell, E. W., Poidinger, M. and Chen, J. (2016). Cytofkit: a bioconductor package for an integrated mass cytometry data analysis pipeline. PLoS Comput. Biol. 12, e1005112. 10.1371/journal.pcbi.1005112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cibrián, D. and Sánchez-Madrid, F. (2017). CD69: from activation marker to metabolic gatekeeper. Eur. J. Immunol. 47, 946-953. 10.1002/eji.201646837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Goffau, M. C., Lager, S., Sovio, U., Gaccioli, F., Cook, E., Peacock, S. J., Parkhill, J., Charnock-Jones, D. S. and Smith, G. C. S. (2019). Human placenta has no microbiome but can contain potential pathogens. Nature 572, 329-334. 10.1038/s41586-019-1451-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elahi, S., Ertelt, J. M., Kinder, J. M., Jiang, T. T., Zhang, X., Xin, L., Chaturvedi, V., Strong, B. S., Qualls, J. E., Steinbrecher, K. A.et al. (2013). Immunosuppressive CD71+ erythroid cells compromise neonatal host defence against infection. Nature 504, 158-162. 10.1038/nature12675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enninga, E. A. L., Raber, P., Quinton, R. A., Ruano, R., Ikumi, N., Gray, C. M., Johnson, E. L., Chakraborty, R. and Kerr, S. E. (2020). Maternal T cells in the human placental villi support an allograft response during noninfectious villitis. J. Immunol. 204, 2931-2939. 10.4049/jimmunol.1901297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbach, G. T., Semple, J. P., Milford, E., Goguen, J., Osathanondh, R. and Kurnick, J. T. (1993). Phenotypic characteristics of lymphocyte populations isolated from middle gestation human placenta. J. Reprod. Immunol. 25, 1-13. 10.1016/0165-0378(93)90038-J [DOI] [PubMed] [Google Scholar]
- Erlebacher, A. (2013). Immunology of the maternal-fetal interface. Annu. Rev. Immunol. 31, 387-411. 10.1146/annurev-immunol-032712-100003 [DOI] [PubMed] [Google Scholar]
- Frascoli, M., Coniglio, L., Witt, R., Jeanty, C., Fleck-Derderian, S., Myers, D. E., Lee, T.-H., Keating, S., Busch, M. P., Norris, P. J.et al. (2018). Alloreactive fetal T cells promote uterine contractility in preterm labor via IFN-γ and TNF-α. Sci. Transl. Med. 10, eaan2263. 10.1126/scitranslmed.aan2263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Diaz, A., Shin, D. S., Moreno, B. H., Saco, J., Escuin-Ordinas, H., Rodriguez, G. A., Zaretsky, J. M., Sun, L., Hugo, W., Wang, X.et al. (2017). Interferon receptor signaling pathways regulating PD-L1 and PD-L2 expression. Cell Rep. 19, 1189-1201. 10.1016/j.celrep.2017.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaynor, L. M. and Colucci, F. (2017). Uterine natural killer cells: functional distinctions and influence on pregnancy in humans and mice. Front. Immunol. 8, 467. 10.3389/fimmu.2017.00467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkias, J., Rackaityte, E., Hillman, S. L., Aran, D., Mendoza, V. F., Marshall, L. R., MacKenzie, T. C. and Burt, T. D. (2019). CD161 contributes to prenatal immune suppression of IFNγ-producing PLZF+ T cells. J. Clin. Invest. 129, 3562-3577. 10.1172/JCI125957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, B., Faucette, A. N., Pawlitz, M. D., Pei, B., Goyert, J. W., Zhou, J. Z., El-Hage, N. G., Deng, J., Lin, J., Yao, F.et al. (2017). Interleukin-33-induced expression of PIBF1 by decidual B cells protects against preterm labor. Nat. Med. 23, 128-135. 10.1038/nm.4244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, X. and Wang, H. (2020). Macrophage subsets at the maternal-fetal interface. Cell. Mol. Immunol. 17, 889-891. 10.1038/s41423-020-0435-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joerink, M., Rindsjö, E., van Riel, B., Alm, J. and Papadogiannakis, N. (2011). Placental macrophage (Hofbauer cell) polarization is independent of maternal allergen-sensitization and presence of chorioamnionitis. Placenta 32, 380-385. 10.1016/j.placenta.2011.02.003 [DOI] [PubMed] [Google Scholar]
- King, A., Balendran, N., Wooding, P., Carter, N. P. and Loke, Y. W. (1991). CD3− leukocytes present in the human uterus during early placentation: phenotypic and morphologic characterization of the CD56++ population. Dev. Immunol. 1, 169-190. 10.1155/1991/83493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konnikova, L., Boschetti, G., Rahman, A., Mitsialis, V., Lord, J., Richmond, C., Tomov, V. T., Gordon, W., Jelinsky, S., Canavan, J.et al. (2018). High-dimensional immune phenotyping and transcriptional analyses reveal robust recovery of viable human immune and epithelial cells from frozen gastrointestinal tissue. Mucosal Immunol. 11, 1684-1693. 10.1038/s41385-018-0047-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopman, L. A., Kopcow, H. D., Rybalov, B., Boyson, J. E., Orange, J. S., Schatz, F., Masch, R., Lockwood, C. J., Schachter, A. D., Park, P. J.et al. (2003). Human decidual natural killer cells are a unique NK cell subset with immunomodulatory potential. J. Exp. Med. 198, 1201-1212. 10.1084/jem.20030305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, B. V., Ma, W., Miron, M., Granot, T., Guyer, R. S., Carpenter, D. J., Senda, T., Sun, X., Ho, S.-H., Lerner, H.et al. (2017). Human tissue-resident memory T cells are defined by core transcriptional and functional signatures in lymphoid and mucosal sites. Cell Rep. 20, 2921-2934. 10.1016/j.celrep.2017.08.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuperman, A. A., Zimmerman, A., Hamadia, S., Ziv, O., Gurevich, V., Fichtman, B., Gavert, N., Straussman, R., Rechnitzer, H., Barzilay, M.et al. (2020). Deep microbial analysis of multiple placentas shows no evidence for a placental microbiome. BJOG 127, 159-169. 10.1111/1471-0528.15896 [DOI] [PubMed] [Google Scholar]
- Leiby, J. S., McCormick, K., Sherrill-Mix, S., Clarke, E. L., Kessler, L. R., Taylor, L. J., Hofstaedter, C. E., Roche, A. M., Mattei, L. M., Bittinger, K.et al. (2018). Lack of detection of a human placenta microbiome in samples from preterm and term deliveries. Microbiome 6, 196. 10.1186/s40168-018-0575-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y., Lopez, G. E., Vazquez, J., Sun, Y., Chavarria, M., Lindner, P. N., Fredrickson, S., Karst, N. and Stanic, A. K. (2018). Decidual-placental immune landscape during syngeneic murine pregnancy. Front. Immunol. 9, 2087. 10.3389/fimmu.2018.02087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, N., van Unen, V., Abdelaal, T., Guo, N., Kasatskaya, S. A., Ladell, K., McLaren, J. E., Egorov, E. S., Izraelson, M., Chuva de Sousa Lopes, S. M.et al. (2019). Memory CD4+ T cells are generated in the human fetal intestine. Nat. Immunol. 20, 301-312. 10.1038/s41590-018-0294-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y., Toothaker, J. M., Ben-Simon, S., Ozeri, L., Schweitzer, R., McCourt, B. T., McCourt, C. C., Werner, L., Snapper, S. B., Shouval, D. S.et al. (2020). In utero human intestine harbors unique metabolome, including bacterial metabolites. JCI Insight 5, e138751. 10.1172/jci.insight.138751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern, N., Shin, A., Low, G., Low, D., Duan, K., Yao, L. J., Msallam, R., Low, I., Shadan, N. B., Sumatoh, H. R.et al. (2017). Human fetal dendritic cells promote prenatal T-cell immune suppression through arginase-2. Nature 546, 662-666. 10.1038/nature22795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuin, C., Goodman, A., Chernyshev, V., Kamentsky, L., Cimini, B. A., Karhohs, K. W., Doan, M., Ding, L., Rafelski, S. M., Thirstrup, D.et al. (2018). CellProfiler 3.0: Next-generation image processing for biology. PLoS Biol. 16, e2005970. 10.1371/journal.pbio.2005970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, D., Romero, R., Unkel, R., Xu, Y., Vadillo-Ortega, F., Hassan, S. S. and Gomez-Lopez, N. (2018a). CD71+ erythroid cells from neonates born to women with preterm labor regulate cytokine and cellular responses. J. Leukoc. Biol. 103, 761-775. 10.1002/JLB.5A0717-291RRR [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, I., Min, M., Yang, C., Tian, C., Gookin, S., Carter, D. and Spencer, S. L. (2018b). Ki67 is a graded rather than a binary marker of proliferation versus quiescence. Cell Rep. 24, 1105-1112.e5. 10.1016/j.celrep.2018.06.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra, A., Lai, G. C., Yao, L. J., Aung, T. T., Shental, N., Rotter-Maskowitz, A., Shepherdson, E., Singh, G. S. N., Pai, R., Shanti, A.et al. (2021). Microbial exposure during early human development primes fetal immune cells. Cell 184, 3394-3409.e20. 10.1016/j.cell.2021.04.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki, S., Tsuda, H., Sakai, M., Hori, S., Sasaki, Y., Futatani, T., Miyawaki, T. and Saito, S. (2003). Predominance of Th2-promoting dendritic cells in early human pregnancy decidua. J. Leukoc. Biol. 74, 514-522. 10.1189/jlb.1102566 [DOI] [PubMed] [Google Scholar]
- Mjösberg, J., Berg, G., Jenmalm, M. C. and Ernerudh, J. (2010). FOXP3+ regulatory T cells and T helper 1, T helper 2, and T helper 17 cells in human early pregnancy decidua. Biol. Reprod. 82, 698-705. 10.1095/biolreprod.109.081208 [DOI] [PubMed] [Google Scholar]
- Mold, J. E., Michaëlsson, J., Burt, T. D., Muench, M. O., Beckerman, K. P., Busch, M. P., Lee, T.-H., Nixon, D. F. and McCune, J. M. (2008). Maternal alloantigens promote the development of tolerogenic fetal regulatory T cells in utero. Science 322, 1562-1565. 10.1126/science.1164511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odorizzi, P. M., Jagannathan, P., McIntyre, T. I., Budker, R., Prahl, M., Auma, A., Burt, T. D., Nankya, F., Nalubega, M., Sikyomu, E.et al. (2018). In utero priming of highly functional effector T cell responses to human malaria. Sci. Transl. Med. 10, eaat6176. 10.1126/scitranslmed.aat6176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohl, L., Mohaupt, M., Czeloth, N., Hintzen, G., Kiafard, Z., Zwirner, J., Blankenstein, T., Henning, G. and Förster, R. (2004). CCR7 governs skin dendritic cell migration under inflammatory and steady-state conditions. Immunity 21, 279-288. 10.1016/j.immuni.2004.06.014 [DOI] [PubMed] [Google Scholar]
- Paloczi, K. (1999). Immunophenotypic and functional characterization of human umbilical cord blood mononuclear cells. Leukemia 13 Suppl. 1, S87-S89. 10.1038/sj.leu.2401318 [DOI] [PubMed] [Google Scholar]
- Pavličev, M., Wagner, G. P., Chavan, A. R., Owens, K., Maziarz, J., Dunn-Fletcher, C., Kallapur, S. G., Muglia, L. and Jones, H. (2017). Single-cell transcriptomics of the human placenta: inferring the cell communication network of the maternal-fetal interface. Genome Res. 27, 349-361. 10.1101/gr.207597.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pique-Regi, R., Romero, R., Tarca, A. L., Sendler, E. D., Xu, Y., Garcia-Flores, V., Leng, Y., Luca, F., Hassan, S. S. and Gomez-Lopez, N. (2019). Single cell transcriptional signatures of the human placenta in term and preterm parturition. Elife 8, e52004. 10.7554/eLife.52004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PrabhuDas, M., Bonney, E., Caron, K., Dey, S., Erlebacher, A., Fazleabas, A., Fisher, S., Golos, T., Matzuk, M., McCune, J. M.et al. (2015). Immune mechanisms at the maternal-fetal interface: perspectives and challenges. Nat. Immunol. 16, 328-334. 10.1038/ni.3131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rackaityte, E., Halkias, J., Fukui, E. M., Mendoza, V. F., Hayzelden, C., Crawford, E. D., Fujimura, K. E., Burt, T. D. and Lynch, S. V. (2020). Viable bacterial colonization is highly limited in the human intestine in utero. Nat. Med. 26, 599-607. 10.1038/s41591-020-0761-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes, L. and Golos, T. G. (2018). Hofbauer cells: their role in healthy and complicated pregnancy. Front. Immunol. 9, 2628. 10.3389/fimmu.2018.02628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncarolo, M. G., Bigler, M., Haanen, J. B., Yssel, H., Bacchetta, R., de Vries, J. E. and Spits, H. (1991). Natural killer cell clones can efficiently process and present protein antigens. J. Immunol. 147, 781-787. [PubMed] [Google Scholar]
- Salvany-Celades, M., van der Zwan, A., Benner, M., Setrajcic-Dragos, V., Bougleux Gomes, H. A., Iyer, V., Norwitz, E. R., Strominger, J. L. and Tilburgs, T. (2019). Three types of functional regulatory T cells control T cell responses at the human maternal-fetal interface. Cell Rep. 27, 2537-2547.e5. 10.1016/j.celrep.2019.04.109 [DOI] [PubMed] [Google Scholar]
- Saso, A. and Kampmann, B. (2017). Vaccine responses in newborns. Semin. Immunopathol. 39, 627-642. 10.1007/s00281-017-0654-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schindelin, J., Arganda-Carreras, I., Frise, E., Kaynig, V., Longair, M., Pietzsch, T., Preibisch, S., Rueden, C., Saalfeld, S., Schmid, B.et al. (2012). Fiji: an open-source platform for biological-image analysis. Nat. Methods 9, 676-682. 10.1038/nmeth.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schliefsteiner, C., Peinhaupt, M., Kopp, S., Lögl, J., Lang-Olip, I., Hiden, U., Heinemann, A., Desoye, G. and Wadsack, C. (2017). Human placental hofbauer cells maintain an anti-inflammatory M2 phenotype despite the presence of gestational diabetes mellitus. Front. Immunol. 8, 888. 10.3389/fimmu.2017.00888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreurs, R. R. C. E., Baumdick, M. E., Sagebiel, A. F., Kaufmann, M., Mokry, M., Klarenbeek, P. L., Schaltenberg, N., Steinert, F. L., van Rijn, J. M., Drewniak, A.et al. (2019). Human fetal TNF-α-cytokine-producing CD4+ effector memory T cells promote intestinal development and mediate inflammation early in life. Immunity 50, 462-476.e8. 10.1016/j.immuni.2018.12.010 [DOI] [PubMed] [Google Scholar]
- Shaw, T. N., Houston, S. A., Wemyss, K., Bridgeman, H. M., Barbera, T. A., Zangerle-Murray, T., Strangward, P., Ridley, A. J. L., Wang, P., Tamoutounour, S.et al. (2018). Tissue-resident macrophages in the intestine are long lived and defined by Tim-4 and CD4 expression. J. Exp. Med. 215, 1507-1518. 10.1084/jem.20180019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsen, K. A., Anderson-Berry, A. L., Delair, S. F. and Davies, H. D. (2014). Early-onset neonatal sepsis. Clin. Microbiol. Rev. 27, 21-47. 10.1128/CMR.00031-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stras, S. F., Werner, L., Toothaker, J. M., Olaloye, O. O., Oldham, A. L., McCourt, C. C., Lee, Y. N., Rechavi, E., Shouval, D. S. and Konnikova, L. (2019). Maturation of the human intestinal immune system occurs early in fetal development. Dev. Cell 51, 357-373.e5. 10.1016/j.devcel.2019.09.008 [DOI] [PubMed] [Google Scholar]
- Sun, C., Mezzadra, R. and Schumacher, T. N. (2018). Regulation and function of the PD-L1 checkpoint. Immunity 48, 434-452. 10.1016/j.immuni.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suryawanshi, H., Morozov, P., Straus, A., Sahasrabudhe, N., Max, K. E. A., Garzia, A., Kustagi, M., Tuschl, T. and Williams, Z. (2018). A single-cell survey of the human first-trimester placenta and decidua. Sci. Adv. 4, eaau4788. 10.1126/sciadv.aau4788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, Z., Tadesse, S., Norwitz, E., Mor, G., Abrahams, V. M. and Guller, S. (2011). Isolation of hofbauer cells from human term placentas with high yield and purity. Am. J. Reprod. Immunol. 66, 336-348. 10.1111/j.1600-0897.2011.01006.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theis, K. R., Romero, R., Greenberg, J. M., Winters, A. D., Garcia-Flores, V., Motomura, K., Ahmad, M. M., Galaz, J., Arenas-Hernandez, M. and Gomez-Lopez, N. (2020). No consistent evidence for microbiota in murine placental and fetal tissues. mSphere 5, e00933-19. 10.1128/mSphere.00933-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, J. R., Appios, A., Zhao, X., Dutkiewicz, R., Donde, M., Lee, C. Y. C., Naidu, P., Lee, C., Cerveira, J., Liu, B.et al. (2021). Phenotypic and functional characterization of first-trimester human placental macrophages, Hofbauer cells. J. Exp. Med. 218, e20200891. 10.1084/jem.20200891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toothaker, J. M., Presicce, P., Cappelletti, M., Stras, S. F., McCourt, C. C., Chougnet, C. A., Kallapur, S. G. and Konnikova, L. (2020). Immune cells in the placental villi contribute to intra-amniotic inflammation. Front. Immunol. 11, 866. 10.3389/fimmu.2020.00866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vento-Tormo, R., Efremova, M., Botting, R. A., Turco, M. Y., Vento-Tormo, M., Meyer, K. B., Park, J.-E., Stephenson, E., Polański, K., Goncalves, A.et al. (2018). Single-cell reconstruction of the early maternal-fetal interface in humans. Nature 563, 347-353. 10.1038/s41586-018-0698-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu-Monette, Z. Y., Zhang, M., Li, J. and Young, K. H. (2017). PD-1/PD-L1 blockade: have we found the key to unleash the antitumor immune response? Front. Immunol. 8, 1597. 10.3389/fimmu.2017.01597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X., Mozeleski, B., Lemoine, S., Dériaud, E., Lim, A., Zhivaki, D., Azria, E., Le Ray, C., Roguet, G., Launay, O.et al. (2014). CD4 T cells with effector memory phenotype and function develop in the sterile environment of the fetus. Sci. Transl. Med. 6, 238ra72. 10.1126/scitranslmed.3008748 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.