Abstract
BACKGROUND
The most widely accepted treatment for pediatric supracondylar humeral fracture is closed reduction and percutaneous pinning (CRPP). However, there is debate regarding the technique that is utilized, whether crossed or lateral pinning, and the number of pins used.
AIM
To compare the functional and radiological outcomes of lateral and cross pinning in the management of humeral supracondylar fracture.
METHODS
A retrospective analysis was performed on 101 patients who were surgically managed by either one of the CRPP techniques from 2015 to 2019. Several clinical parameters were taken into account, including pre- and post-intervention Baumann angle, as well as scores for pain, range of motion, function, and stability. Statistical analysis was performed to study the outcomes of the utilized techniques.
RESULTS
Amongst our study sample, which included 63 males and 38 females with a mean age of 5.87 years, about one-third of the patients underwent crossed pinning fixation configuration and the remaining two-thirds were managed by lateral pinning configuration. Similar results were obtained in the two groups with no statistical difference regarding Mayo elbow performance scores (MEPS) and Baumann angle. The mean MEPS in the lateral and crossed pinning groups were 93.68 + 8.59 and 93.62 + 9.05, respectively. The mean Baumann angle was 72.5° + 6.46 in the lateral group and 72.3° + 4.70 in the crossed-pinning group (P = 0.878).
CONCLUSION
Both lateral pinning and crossed pinning fixation configuration for displaced pediatric supracondylar humeral fractures provide similar functional and radiological outcomes.
Keywords: Supracondylar fracture, Gartland, Pinning, Functional, Radiological
Core Tip: Closed reduction and percutaneous pinning is the mainstay in the management of pediatric supracondylar fracture. It is still controversial what pin configuration should be used (lateral vs cross pinning), and how many pins should be used. Both lateral and cross pinning techniques provide adequate stability for the fracture with nearly similar radiological and functional outcomes.
INTRODUCTION
A supracondylar humeral fracture happens through the thin part of the distal humerus above the growth plate level. These fractures are typical pediatric injuries, accounting for 60% of upper limb fractures and 13% of pediatric fractures. They are most commonly seen in children 5-7 years of age with no gender predilection[1-3].
These fractures may be complete or incomplete with varying degrees of severity. The Gartland classification system is a popular system for the evaluation and treatment of these fractures. It classifies them as type 1 - nondisplaced or minimally displaced, type 2 - displaced with intact posterior cortex, and type 3 - completely displaced without contact between fragments[3]. In addition, the modified Gartland classification is frequently used, describing one more type, type 4 - complete multidirectional displacement of fragments with periosteal disruption[4].
As for the management of these fractures, a trial of conservative management may be undertaken with type 1 fractures and minimally displaced type 2 fractures. This involves long arm casting with less than 90 degrees of elbow flexion[5].
Operative management is almost always required in more severe types, including closed reduction and percutaneous pinning (CRPP). Pinning is performed retrogradely, using two pins for type 2 fractures and three pins for type 3 fractures. Rarely, open reduction with percutaneous pinning is needed in open fractures and in cases of failed closed reduction[6]. The most commonly reported postoperative complication is pin migration[7].
Despite reported complications of neurovascular injuries[8], it has been well documented in the previous literature that pediatric supracondylar humerus fractures generally have good outcomes. Elbow range of motion (ROM) and function are usually preserved, provided that adequate reduction is achieved through surgical intervention or casts application[9].
CRPP has two techniques: Lateral pinning technique (Figure 1A) and cross pinning technique (Figure 1B). Controversy persists between the two perspectives regarding which is better in terms of fixation stability and risk of developing complications.
Figure 1.
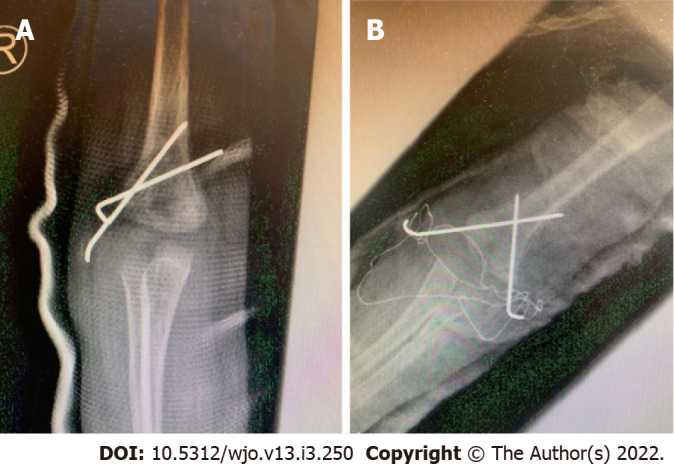
Postoperative AP view radiographs. A: Lateral pinning; B: Cross pinning.
Theoretically, crossed pinning is superior in providing biomechanical stability, yet this construct increases the risk of iatrogenic ulnar nerve injury due to the medial pin position. Conversely, lateral pinning may be less stable biomechanically but avoids ulnar nerve injury[10-12].
Therefore, this study aimed to study the difference in stability and functional outcomes between patients managed by lateral pinning and those managed by crossed pinning for displaced supracondylar fracture of the humerus. The null hypothesis was that there is no difference between the treatment groups.
In order to compare the two techniques, the well-validated Mayo elbow performance score (MEPS) was used as a standardized functional outcome measure[13,14]. Other measures with clinical-radiological value may be considered as well. These may include measurement of Baumann angle (Figure 2), carrying angle, the development of complications, and the necessity to re-operate.
Figure 2.
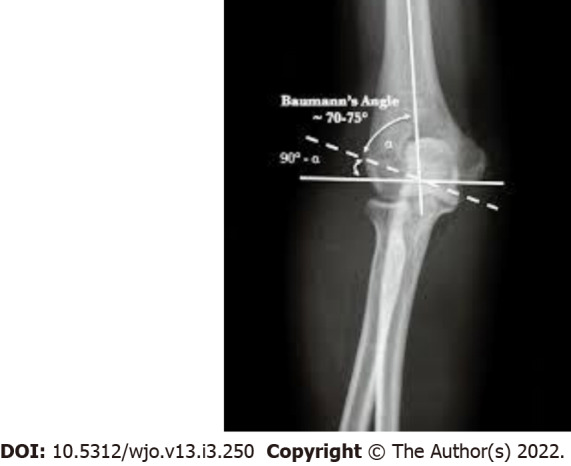
Lateral radiograph demonstrating Baumann's angle (angle between the long axis of humeral shaft and growth plate of lateral humeral condyle).
MATERIALS AND METHODS
We conducted a single-blinded retrospective cohort study at the Department of Orthopedics of King Abdullah University Hospital (KAUH). Before conducting this study, ethical approval was obtained from the Institutional Review Board (IRB) committee of KAUH. This study reviewed a total of 101 cases of children with supracondylar humeral fractures that were presented to the emergency department of KAUH between 2015 and 2019. Multiple parameters were reviewed, including gender, age, and surgical intervention, as well as scores for pain, ROM, function, and stability. A convenience sampling method was used to obtain our sample.
Our inclusion criteria for the study involved any patient up to the age of 13 years who had a supracondylar humeral fracture and underwent closed reduction with percutaneous pinning within 24 h of the insult and with no neurological or vascular injury prior to the operation. The pinning was either lateral or crossed configuration with medial and lateral wires. Our exclusion criteria included patients who did not respond to our call, patients with bilateral fractures, patients with multiple surgeries in the same limb, and those who ever had a previous elbow fracture. This was to avoid the confounding effects of previous fractures and surgeries on our results. However, unknown confounders might still be present.
An orthopedic specialist reviewed the patients' radiographic images (Figure 3) and categorized them using the Gartland classification system. Then, surgery was performed and techniques were standardized in regards to pin location, pin size, stability, and positioning of the elbow. They were performed by a well-trained orthopedic surgeon.
Figure 3.

Pre-operative AP view radiograph.
Patients were scheduled for follow-up visits; the follow-up period was customized according to patient cases individually, with a timeframe ranging from 1 mo postoperatively to 1 year. They underwent pin removal and cast change and were inspected for symptoms and ROM. Radiographs were taken to guarantee proper healing and reduction (Figure 4).
Figure 4.
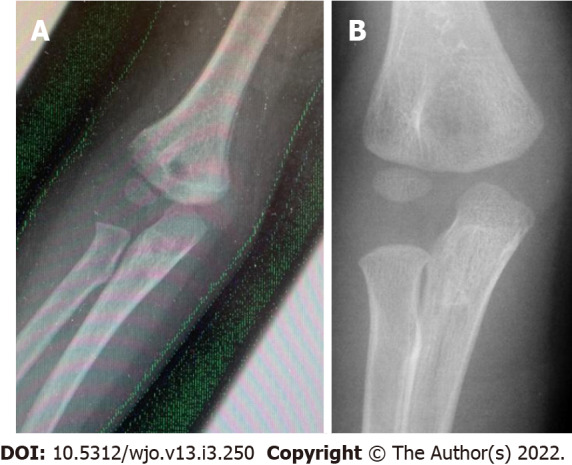
AP radiographs post pin removal. A: Lateral pinning B: Crossed pinning.
All fractures were also assessed by altering their Baumann angle, which was measured both postoperatively and during the last follow-up in January-March 2020. Baumann angle refers to the angle between the long axis of the humeral shaft and the growth plate of the lateral condyle. A difference in the angle of more than 5 degrees between the two limbs was considered abnormal. All measurements were performed by a single calibrated examiner. The interclass correlation coefficient for the angle measurement was above 90%.
MEPS was used to assess functional limitations of the elbow on daily activities and administered during January-March 2020 via patient interviewing and physical examination in the clinic. Elbow function was measured across four domains: Pain (45 points), ROM (20 points), stability (10 points), and daily function (25 points). Clinical information from these four subscales was rated on a 100-point scale and categorized as follows: < 60, poor; 60-74, fair; 75-89, good; and 90-100, excellent[13,14].
All of our patients were eligible to participate in our study. Matching by age and gender was not performed due to the small number of patients in the crossed pinning group and the portability of introducing bias. Case selection bias was minimal because we applied strict inclusion and exclusion criteria, and the outcome of interest was clear for all categories. In addition, information bias was controlled by excluding all patients with missing information.
Data was entered and analyzed using IBM SPSS statistics version 23. We looked at MEPS, Gartland type, type of fixation, and Baumann angle. We classified the patients according to the technique used (crossed pinning vs lateral pinning); the lateral pinning group was further sub-classified into 2 pins vs 3 pins. Patients were also categorized according to Gartland type, MEPS score, and gender. Using the t-test, we measured if there was a difference in Baumann angle according to the type of fixation, and whether it was lateral pinning or crossed pinning. Using multiple linear regression, we measured the factors that affect Baumann angle and MEPS. Using ANOVA, we measured if there was a difference between two lateral pins, three lateral pins, and crossed pinning groups in their effect on Baumann angle and MEPS. Results were considered significant at P < 0.05.
RESULTS
A total of 101 patients with supracondylar fractures were qualified to join our study. All patients responded and were included in the analysis. Of these patients, 63 (62.4%) were male, and 38 (37.6%) were female. The mean age of patients was 5.87 ± 1.5 years, with the youngest patient being 35 d of age and the eldest being 13.0 years of age.
We subdivided them by type of fixation into a cross pinning group with 28 patients (28.7%) and a lateral group with 72 patients (71.3%). Patients were further subdivided by Gartland type and MEPS (Table 1). As for Gartland type distribution, none had type I, 21 (20.8%) had type II, 43 (42.6%) had type III fractures, 28(27.7%) had type IV, and 9 (8.9%) had flexion type supracondylar fracture. The mean time for the last follow-up was 24.65 and 20.55 mo in the lateral pinning and cross pinning groups, respectively.
Table 1.
Demographic characteristics
|
|
Lateral group
|
Cross pin group
|
|
| Male | 43 (59.7%) | 20 (69%) | |
| Female | 29 (40.3%) | 9 (31%) | |
| Extension type 2 | 15 (20.8%) | 6 (20.7%) | |
| Extension type 3 | 36 (50%) | 7 (24.1%) | |
| Extension type 4 | 15 (20.8%) | 13 (44.8%) | |
| Flexion type | 6 (8.3%) | 3 (10.3%) | |
| Age mean | 5.7920 | 6.0693 | |
| Age SD | 3.17336 | 3.0422 | |
| MEPS mean | 93.6806 | 93.6207 | |
| MEPS SD | 8.59877 | 9.05307 | |
| MEPS | Poor | 0 (0%) | 0 (0%) |
| Fair | 1 (1.4%) | 1 (3.4%) | |
| Good | 26 (36.1%) | 10 (34.5%) | |
| Excellent | 45 (62.5%) | 18 (62.1%) | |
| Bumann angle mean | 72.5139 | 72.3103 | |
| Bumann angle SD | 6.46114 | 4.70640 | |
SD: Standard deviation.
Regarding outcomes in the lateral pinning group, 62.5% of the patients had excellent outcomes, 36.1% had good outcomes, and 1.4% had fair outcomes. There were no reports of poor outcomes. Meanwhile, in the crossed pinning group, 62.1% of patients had excellent outcomes, 34.5% had good outcomes, and 3.4% had fair outcomes with no reports of poor outcomes.
There was no statistical difference in functional outcome according to MEPS (P = 0.06). The mean MEPS in the lateral pinning and crossed-pinning groups were 93.68 ± 8.6 and 93.62 ± 9.0, respectively. Multiple linear regression analysis was performed to determine the relationship between MEPS and different clinical parameters for functional outcomes. However, there was no statistical difference found in functional outcome regardless of gender (P = 0.220), fracture type (P = 0.647), and type of fixation (P = 0.888).
There was no statistical difference between the groups according to Baumann angle (P = 0.878). The means in the lateral pinning and crossed pinning groups were 72.5° ± 6.5 and 72.3° ± 4.7, respectively. Multiple linear regression analysis was also performed with Baumann angle with no result of statistical difference regardless of gender (P = 0.115), fracture type (P = 0.949), and type of fixation (P = 0.995).
We further subdivided the lateral group into 2 wires lateral (36 patients) and 3 wires lateral (36 patient) groups; there was no statistically significant difference between the three groups using one-way ANOVA according to MEPS (P = 0.694) and Baumann angle (P = 0.115).
DISCUSSION
The management of pediatric supracondylar humeral fractures includes non-operative and operative treatments. Fractures are further individualized based on the presentation (open or closed fracture), Gartland classification, the degree of the displacement, and the physician preference[5,7,10]. Regarding operative treatments, CRPP is the mainstay of treatment for displaced extension type supracondylar fracture. However, controversy regarding the optimal technique, whether lateral pinning or crossed pinning, remains under discussion[7,15,16].
In this study, we retrospectively evaluated 101 patients; some managed by crossed pinning (27.8%) and others by lateral pinning (72.1% [2 pins in 50% and 3 pins in the remaining 50%]). Supracondylar fracture incidence was higher in males, nearly 2 times more than in females. The mean age was 5.87, ranging from 35 d to 13 years, with a peak incidence of 5-7 years. This result is comparable to the series done by Patel et al[17], where they reported a peak incidence in the 6-8-year-age group with an average age of 7.48 years. Also, male predominance was noted in Patel et al[17], Wilkins et al[18], and Solak et al[19] series. Most clinical and radiological studies used Baumann angle, Flynn grade, and fracture complications to assess clinical outcomes[20]. In our study, we used the MEPS and Baumann angle for this purpose. There was no statistically significant difference between the treatment groups.
The loss of reduction in our study was 0%. In a recent meta-analysis done by Dekker et al[20] comparing the two techniques, the loss of reduction occurred in 11.6% of patients treated by crossed pinning and 12.4% of patients treated with lateral pins. Yet, there was no statistically significant difference between the two groups. In addition, there was no significant difference according to the Flynn criteria, ROM, and measures of radiographic outcome.
Patel et al[17] also used MEPS for comparing lateral and crossed pinning technique outcomes. For the crossed pinning group, they reported that 90% of the patients had excellent outcomes, 10% had good outcomes, and 0% had poor outcomes. Lateral pinning showed 83.33% excellent and 16.66% good outcomes with no reports of poor outcome. While in our study, 62.5% of the patients in the lateral pinning group had excellent outcomes, 36.1% had good outcomes, and 1.4% had fair outcomes with no poor outcomes. Crossed pinning showed 62.1% excellent outcomes, 34.5% good outcomes, and 3.4% fair outcomes. Both studies showed no statistically significant difference between the two treatment groups. It could be that the difference in the percentages is due to the difference in the interpretation of the MEPS, as 15 points were considered a clinically negligible difference.
Several biomechanical studies demonstrated that crossed pinning is more stable than lateral pinning, especially on rotational testing and valgus and varus loading[21-23]. On the other hand, other studies reported no statistically significant differences radiologically and clinically between the two groups[15,16]. Although crossed pins seem to provide more stabilization, their major disadvantage is the iatrogenic ulnar nerve injury. The studies estimated it to occur 3 to 5 times more than lateral pins alone[15,16,20]. Conversely, Chen et al[24] reported no significant difference in the biomechanical stability between divergent lateral pins and crossed pins in terms of resisting varus, internal rotation, and extension forces. Also, Hamdi et al[25] suggested that two or three divergent lateral pins provide optimal fracture stability. These studies support the concept that properly placed lateral pins provide adequate biomechanical stability.
The limitations of our study include it being a retrospective study, not a randomized prospective clinical trial. Another major limitation was the uneven number of cases in each group in addition to them only being followed for short intervals. Furthermore, we included patients with flexion type supracondylar fractures, and these patients may constitute a different population from those with the extension type. Moreover, we did not analyze or report complications. Thus, a randomized controlled trial involving larger samples and evenly distributed cases with long-term follow-up is warranted in future studies.
CONCLUSION
Within the limitations of our study, the two techniques for displaced pediatric supracondylar humeral fractures promote similar postoperative results. There is no significant difference between lateral and crossed pinning techniques regarding the functional and radiological outcomes.
ARTICLE HIGHLIGHTS
Research background
The most widely accepted treatment for pediatric supracondylar humeral fracture is closed reduction and percutaneous pinning. However, there is debate regarding the technique that is utilized, whether crossed or lateral pinning, and the number of pins used.
Research motivation
To compare the functional and radiological outcomes of lateral and cross pinning in the management of humeral supracondylar fracture.
Research objectives
To compare the functional and radiological outcomes of lateral and cross pinning in the management of humeral supracondylar fracture.
Research methods
A retrospective analysis was performed on 101 patients who were surgically managed by either one of the CRPP techniques from 2015 to 2019. Several clinical parameters were taken into account, including pre- and post-intervention Baumann's angle, as well as scores for pain, range of motion, function, and stability. Statistical analyses were performed to study the outcomes of the utilized techniques.
Research results
Amongst our study sample, which included 63 males and 38 females with a mean age of 5.87 years, about one-third of the patients underwent crossed pinning fixation configuration and the remaining two-thirds were managed by lateral pinning configuration. Similar results were obtained in the two groups with no statistical difference regarding Mayo elbow performance scores (MEPS) and Baumann's angle. The mean MEPS in the lateral and crossed pinning groups were 93.68 + 8.59 and 93.62 + 9.05, respectively. The mean Baumann's angle was 72.5 + 6.46 in the lateral group and 72.3 + 4.70 in the cross-pinning group (P = 0.878).
Research conclusions
Both lateral pinning and crossed pinning fixation configuration for displaced pediatric supracondylar humeral fractures provide similar functional and radiological outcomes.
Research perspectives
A randomized controlled trial involving larger samples and evenly distributed cases with long-term follow-up is warranted in future studies.
Footnotes
Institutional review board statement: This work was approved by the institutional review board (IRB) committee of King Abdullah University Hospital (KAUH).
Conflict-of-interest statement: Radaideh, Rusan, Obeidat, AL-Nusair, Albustami, Mohaidat and Sunallah declare that they have no conflict of interest.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Academy of Orthopedic Surgeon; Royal College of Surgeons (Ireland).
Peer-review started: August 7, 2021
First decision: September 29, 2021
Article in press: February 12, 2022
Specialty type: Orthopedics
Country/Territory of origin: Jordan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu J S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
Contributor Information
Ahmad M Radaideh, Department of Special Surgery, Orthopaedic Division, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan. ahmadmr1970@yahoo.com.
Mohammad Rusan, Department of Special Surgery, Orthopaedic Division, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan.
Omar Obeidat, School of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan.
Jowan Al-Nusair, School of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan.
Iyad S Albustami, School of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan.
Ziyad M Mohaidat, Department of Special Surgery, Orthopaedic Division, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan.
Abdulkarim W Sunallah, Department of Special Surgery, Orthopaedic Division, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan.
Data sharing statement
The original anonymous dataset is available on request from the corresponding author at ahmadmr1970@yahoo.com.
References
- 1.Al-Omari AA, Rusan M, Obeidat O, Almomani Z, Albustami IS, Alrawashdeh MA. Spontaneous Full Recovery of High Radial Nerve Palsy Following Closed Reduction and Percutaneous Pinning of Gartland IV Supracondylar Fracture: A Case Report. Am J Case Rep. 2021;22:e930277. doi: 10.12659/AJCR.930277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soon-Hyuck L. Upper Extremity Fractures in Children-Prospective Epidemiological Study of Tertiary Medical Institutes. J Korean Orth Assoc. 2007:270–275. [Google Scholar]
- 3.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109:145–154. [PubMed] [Google Scholar]
- 4.Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J Bone Joint Surg Am. 2006;88:980–985. doi: 10.2106/JBJS.D.02956. [DOI] [PubMed] [Google Scholar]
- 5.Milbrandt TA. Common elbow injuries in children: evaluation, treatment, and clinical outcomes. Current Opinion in Orthopaedics. 2004;15:286–294. [Google Scholar]
- 6.Diesselhorst MM, Deck JW, Davey JP. Compartment syndrome of the upper arm after closed reduction and percutaneous pinning of a supracondylar humerus fracture. J Pediatr Orthop. 2014;34:e1–e4. doi: 10.1097/BPO.0b013e3182933c69. [DOI] [PubMed] [Google Scholar]
- 7.Vuillermin C, May C, Kasser J. Closed Reduction and Percutaneous Pinning of Pediatric Supracondylar Humeral Fractures. JBJS Essent Surg Tech. 2018;8:e10. doi: 10.2106/JBJS.ST.16.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bashyal RK, Chu JY, Schoenecker PL, Dobbs MB, Luhmann SJ, Gordon JE. Complications after pinning of supracondylar distal humerus fractures. J Pediatr Orthop. 2009;29:704–708. doi: 10.1097/BPO.0b013e3181b768ac. [DOI] [PubMed] [Google Scholar]
- 9.Leiblein M, Lustenberger T, Schulz AK, Schmitz-Rixen T, Marzi I. Neurovascular complications after supracondylar humerus fractures in children. Trauma Case Rep. 2017;8:16–19. doi: 10.1016/j.tcr.2017.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isa AD, Furey A, Stone C. Functional outcome of supracondylar elbow fractures in children: a 3- to 5-year follow-up. Can J Surg. 2014;57:241–246. doi: 10.1503/cjs.019513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning vs lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007;27:181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- 12.Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop. 2010;30:253–263. doi: 10.1097/BPO.0b013e3181d213a6. [DOI] [PubMed] [Google Scholar]
- 13.Cusick MC, Bonnaig NS, Azar FM, Mauck BM, Smith RA, Throckmorton TW. Accuracy and reliability of the Mayo Elbow Performance Score. J Hand Surg Am. 2014;39:1146–1150. doi: 10.1016/j.jhsa.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 14.Longo UG, Franceschi F, Loppini M, Maffulli N, Denaro V. Rating systems for evaluation of the elbow. Br Med Bull. 2008;87:131–161. doi: 10.1093/bmb/ldn023. [DOI] [PubMed] [Google Scholar]
- 15.Prashant K, Lakhotia D, Bhattacharyya TD, Mahanta AK, Ravoof A. A comparative study of two percutaneous pinning techniques (lateral vs medial-lateral) for Gartland type III pediatric supracondylar fracture of the humerus. J Orthop Traumatol. 2016;17:223–229. doi: 10.1007/s10195-016-0410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kocher M, Kasser J, Waters P, Bae D, Snyder B, Hresko M, et al. Lateral Entry Compared with Medial and Lateral Entry Pin Fixation for Completely Displaced Supracondylar Humeral Fractures in Children. J Bone & Joint Surg. 2007;89:706–712. doi: 10.2106/JBJS.F.00379. [DOI] [PubMed] [Google Scholar]
- 17.Patel N, Patil P, Gaonkar K, Kulkarni H, Gupta K. A comparative study of outcomes of percutaneous crossed vs lateral divergent pinning in the treatment of displaced (grade - 3) supracondylar fractures of humerus in children. J Evidence Based Med Healthcare. 2015;2:789–798. [Google Scholar]
- 18.Wilkins K. The Operative Management of Supracondylar Fractures. Orthopedic Clinics of North America. 1990;21:269–289. [PubMed] [Google Scholar]
- 19.Solak S, Aydin E. Comparison of two percutaneous pinning methods for the treatment of the pediatric type III supracondylar humerus fractures. J Pediatr Orthop B. 2003;12:346–349. doi: 10.1097/01.bpb.0000060288.16932.08. [DOI] [PubMed] [Google Scholar]
- 20.Dekker AE, Krijnen P, Schipper IB. Results of crossed vs lateral entry K-wire fixation of displaced pediatric supracondylar humeral fractures: A systematic review and meta-analysis. Injury. 2016;47:2391–2398. doi: 10.1016/j.injury.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76:253–256. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22:440–443. [PubMed] [Google Scholar]
- 23.Feng C, Guo Y, Zhu Z, Zhang J, Wang Y. Biomechanical analysis of supracondylar humerus fracture pinning for fractures with coronal lateral obliquity. J Pediatr Orthop. 2012;32:196–200. doi: 10.1097/BPO.0b013e318242a99a. [DOI] [PubMed] [Google Scholar]
- 24.Chen T, He C, Zheng T, Gan Y, Huang M, Zheng Y, et al. Stiffness of various pin configurations for pediatric supracondylar humeral fracture. J Pediatr Orthop. 2015;24:389–399. doi: 10.1097/BPB.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 25.Hamdi A, Poitras P, Louati H, Dagenais S, Masquijo JJ, Kontio K. Biomechanical analysis of lateral pin placements for pediatric supracondylar humerus fractures. J Pediatr Orthop. 2010;30:135–139. doi: 10.1097/BPO.0b013e3181cfcd14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original anonymous dataset is available on request from the corresponding author at ahmadmr1970@yahoo.com.


