Abstract
Abdominal pregnancy is a rare but life-threatening variation of ectopic pregnancy that is often treated with laparoscopic management; however, we present a case successfully treated using only minimally invasive techniques. A 36-year-old female G1P0 with a history of infertility is diagnosed with 11-weeks abdominal pregnancy by transvaginal ultrasound. She presented with vaginal bleeding and abdominal pain, and her beta-human chorionic gonadotropin was 53,680 mIU/mL. The location of the fetal sac was not amenable to surgery or percutaneous injection. We performed bilateral uterine artery embolization and subsequent intramuscular methotrexate injection. The procedure was successful with no complications. The patient was followed at postoperative week 11, and beta-human chorionic gonadotropin was 2 mIU/mL, and at 3 months, a transvaginal ultrasound revealed resolution of the abdominal pregnancy.
Keywords: UAE, Embolization, Uterine artery, Ectopic, Pregnancy, Abdominal
Introduction
An ectopic pregnancy that lies within the peritoneal cavity but evades involvement of the fallopian tubes, ovaries and broad ligament is referred to as an abdominal pregnancy. This variant, while rare, constitutes a disproportionately large portion of the morbidity, and mortality related to ectopic pregnancies. Representing around 1% of all ectopic pregnancies, abdominal pregnancy is a serious condition that can have even greater mortality rates when not managed appropriately [1]. This has often resulted in uterine artery embolization combined with laparoscopy or laparoscopy alone as the primary form of treatment. To the best of our knowledge, this is the first report describing an endovascular technique as the primary approach in patients with abdominal ectopic pregnancy. We report a case of a patient with an 11-week abdominal ectopic pregnancy who underwent bilateral uterine artery embolization. The patient was managed successfully without laparoscopic intervention and experienced no complications.
Case report
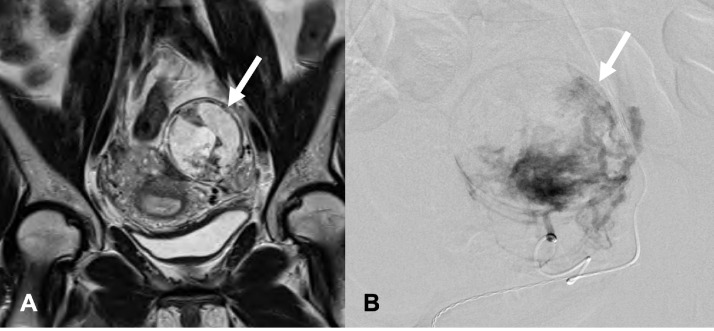
A 36-year-old female G1P0 with a 7-year history of failure to conceive presents at 11 weeks’ gestation transferred from an outside hospital with light vaginal bleeding and mild abdominal pain after transvaginal ultrasound (TVUS) suggested an ectopic abdominal pregnancy. On initial evaluation, the patient's beta-human chorionic gonadotropin (beta-HCG) was 53,680 mIU/mL. The patient was hemodynamically stable, and the physical examination was unremarkable. Magnetic resonance imaging (MRI) and repeat TVUS confirmed ectopic pregnancy within the posterior cul-de-sac (Figs. 1A and B). The patient was admitted to the Maternal-Fetal Medicine (MFM) service and consented to KCl injection to terminate fetal cardiac activity; though, this procedure was no longer a good option after decreased visibility of gestational sac on TVUS. Inpatient management of the patient's abdominal pregnancy was recommended; however, she declined continued admission, and was discharged with scheduled follow-up. Upon readmission 4 days later, Interventional Radiology was consulted to evaluate for possible intervention. A written consent was obtained before the procedure. Under conscious sedation, the right femoral artery was accessed via the Seldinger technique, and after catheter advancement, an abdominal aortogram was performed to guide placement into the contralateral common femoral artery. Once access to the left uterine artery was achieved, angiography revealed increased vascularity, and vascular blush in the region of the abdominal pregnancy (Fig. 1B). Embolization of the left uterine artery was performed with 6 vials of 500-micron Embosphere Microspheres, followed by 1 vial of microparticles 700-900 microns. In a similar fashion, the right uterine artery was selectively catheterized, and embolization was performed with 1 vial of 500-micron Embosphere Microspheres followed by 1 vial of microparticles 700-900 microns. Embolization proceeded to near stasis bilaterally, and a pelvic aortogram demonstrated a significant decrease in vascularity of the placenta upon completion of the procedure. The patient tolerated the procedure well with minimal blood loss and successful hemostasis after manual compression.
Fig. 1.
(A) Coronal T2-weighted MRI of the pelvis reveals gestational sac within the rectouterine pouch (arrow). (B) DSA image of the distal left uterine artery demonstrating vascularity of the abdominal pregnancy (arrow).
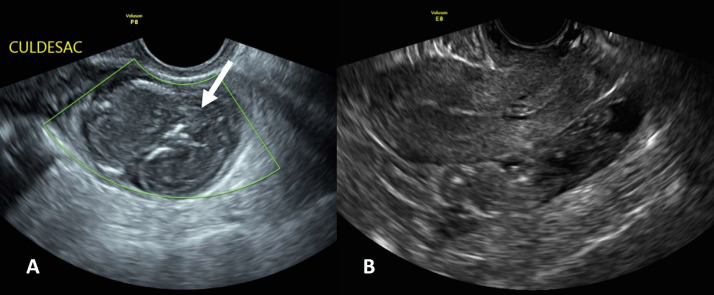
The patient was admitted overnight and did well post-procedurally. The pain was controlled with a patient-controlled anesthesia pump, and the patient was transitioned to an oral pain control regimen. Fetal heart tones were noted to be absent at post-procedure day 1 (Fig. 2). The patient was discharged on post-procedure day 1 with antibiotics, stool softeners, pain medication, and scheduled follow-up with the clinic. The patient received intramuscular methotrexate on post-procedure day 2. The patient's beta-HCG level at 1-week post-procedure was 1355 mIU/mL and was followed to 11 weeks post-procedure which then showed a nadir value of 2 mIU/mL. Follow-up TVUS after 3 months proved the resolution of pregnancy (Fig. 2).
Fig. 2.
(A) Post-embolization ultrasound indicating cessation of fetal cardiac activity at post-procedure day 1 (arrow). (B) Transvaginal ultrasound performed at 3 months demonstrates resolution of pregnancy with resolved gestational sac.
Discussion
Ectopic pregnancies are relatively common, accounting for 1%-2% of all pregnancies. However, abdominal pregnancies, defined by any pregnancy within the peritoneal cavity without the involvement of the broad ligament, fallopian tubes, or ovaries, account for 1% of ectopic pregnancies [1]. While rare, these forms of pregnancies carry the highest risk for maternal morbidity, including bowel obstruction, fistulae, hemorrhage, and death. Risk factors associated with abdominal pregnancy include pelvic inflammatory disease, tubal scarring, multiparity, and endometriosis [2]. Other than 7 years of infertility, this patient had no identifiable obstetric or gynecologic history, although infertility, and abdominal pregnancy share similar risk factors.
Endovascular procedures have been used as adjunctive measures when treating abdominal pregnancy. Preoperative UAE has been shown to be effective prior to a laparoscopic procedure. This form of targeted embolization additionally has evidence of reducing maternal morbidity and mortality in other variations of ectopic pregnancies [3], [4]. This case highlights the possibility of using UAE as the sole procedural option in treating abdominal ectopic pregnancy without the need for further interventions such as laparotomy. Additionally, no serious complications were observed during the procedure or upon follow-up. A study by Hirakawa et al. demonstrated that a combination of UAE and methotrexate could be an effective non–surgical option in managing cervical ectopic pregnancies, a finding that can be extrapolated to the management strategy in our report [5].
Other methods of treatment can also be used in the management of these patients. Intracardiac KCl injection under TVUS guidance has been used to terminate ectopic pregnancies with similar success rates to the injection of methotrexate [6]. In this case, a KCl injection could not be performed due to the unreliable ultrasound window of the pregnancy. Methotrexate is available as the primary therapy in the treatment of ectopic pregnancies. However, it is not recommended as the only treatment when beta-HCG levels are above 10,000 mIU/mL, as was the case in this patient [7]. Notably, there is significant ultrasound diagnostic error in detecting these pregnancies and can often go unrecognized until more severe symptoms arise and the beta-HCG crosses above this threshold [8]. These considerations further illustrate the need for alternative management techniques.
Abdominal pregnancies are a rare variation of ectopic pregnancy, which carries a greater risk of maternal mortality. The risk of mortality in these pregnancies is 7.7 times larger than the risk of ectopic tubal pregnancy and 90 times greater than a typical intrauterine pregnancy [9]. Therefore, improving the diagnosis, and management of this condition is essential in advancing women's healthcare. A multidisciplinary approach is highly advised in the treatment of this often-complex entity, and endovascular therapy should be part of the discussion.
Patient consent
Verbal and written consent was obtained from the patient.
Footnotes
Acknowledgments: None.
Competing Interests: No conflict of interests to declare.
References
- 1.Baffoe P, Fofie C, Gandau BN. Term abdominal pregnancy with healthy newborn: a case report. Ghana Med J. 2011;45(2):81–83. doi: 10.4314/gmj.v45i2.68933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ludwig M, Kaisi M, Bauer O, Diedrich K. The forgotten child–a case of heterotopic, intra-abdominal and intrauterine pregnancy carried to term. Hum Reprod. 1999;14(5):1372–1374. doi: 10.1093/humrep/14.5.1372. [DOI] [PubMed] [Google Scholar]
- 3.Frischhertz S, Eubanks-Bradley J, Gilbert P. Endovascular therapy for abdominal pregnancy. Ochsner J. 2019;19(2):74–76. doi: 10.31486/toj.18.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozen M., Momin S., Myers C.B., Hoffman M., Raissi D. Primary bilateral ovarian artery embolization for uterine leiomyomatosis in the setting of a rare anatomic variant - hypoplastic uterine arteries. Radiol Case Rep. 2021;2;16(9)(2426–2428) doi: 10.1016/j.radcr.2021.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirakawa M, Tajima T, Yoshimitsu K, Irie H,, Ishigami K, Yahata H,, et al. Uterine artery embolization along with the administration of methotrexate for cervical ectopic pregnancy: technical and clinical outcomes. AJR Am J Roentgenol. 2009;192(6):1601–1607. doi: 10.2214/AJR.08.1921. . PMID: 19457824. [DOI] [PubMed] [Google Scholar]
- 6.Monteagudo A, Minor VK, Stephenson C, Monda S, Timor-Tritsch IE. Non-surgical management of live ectopic pregnancy with ultrasound-guided local injection: a case series. Ultrasound Obstet Gynecol. 2005;25(3):282–288. doi: 10.1002/uog.1822. [DOI] [PubMed] [Google Scholar]
- 7.Lipscomb GH, McCord ML, Stovall TG, Huff G, Portera SG, Ling FW. Predictors of success of methotrexate treatment in women with tubal ectopic pregnancies. N Engl J Med. 1999;341(26):1974–1978. doi: 10.1056/NEJM199912233412604. [DOI] [PubMed] [Google Scholar]
- 8.Nassali MN, Benti TM, Bandani-Ntsabele M, Musinguzi E. A case report of an asymptomatic late term abdominal pregnancy with a live birth at 41 weeks of gestation. BMC Res Notes. 2016;9:31. doi: 10.1186/s13104-016-1844-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kun KY, Wong PY, Ho MW, Tai CM, Ng TK. Abdominal pregnancy presenting as a missed abortion at 16 weeks gestation. Hong Kong Med J. 2000;6(4):425–427. [PubMed] [Google Scholar]